Restraint Alternatives and Safe Restraint Use
- • Define the key terms and key abbreviations in this chapter.
- • Describe the purpose of restraints.
- • Identify the risk factors related to restraint use.
- • Identify restraint alternatives.
- • Explain the legal aspects of restraint use.
- • Explain how to use restraints safely.
- • Perform the procedure described in this chapter.
- • Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
chemical restraint Any drug used for discipline or convenience and not required to treat medical symptoms
convenience Any action taken to control or manage a person's behavior that requires less effort by the staff; the action is not in the person's best interest
discipline Any action taken by the agency to punish or penalize a patient or resident
enabler A device that limits freedom of movement but is used to promote independence, comfort, or safety
freedom of movement Any change in place or position of the body or any part of the body that the person is able to control
medical symptom An indication or characteristic of a physical or psychological condition
physical restraint Any manual method or physical or mechanical device, material, or equipment attached to or near the person's body that he or she cannot remove easily and that restricts freedom of movement or normal access to one's body
remove easily The manual method, device, material, or equipment used to restrain the person that can be removed intentionally by the person in the same manner it was applied by the staff
Key Abbreviations
| CMS | Centers for Medicare & Medicaid Services |
| FDA | Food and Drug Administration |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| ROM | Range-of-motion |
| TJC | The Joint Commission |
Chapters 13 and 14 have many safety measures. However, some persons need extra protection. They may present dangers to themselves or others (including staff).
The Centers for Medicare & Medicaid Services (CMS) has rules for using restraints. Like the Omnibus Budget Reconciliation Act of 1987 (OBRA), CMS rules protect the person's rights and safety. This includes the right to be free from restraint. Restraints may be used only to treat a medical symptom or for the immediate physical safety of the person or others. Restraints may be used only when less restrictive measures fail to protect the person or others. They must be discontinued as soon as possible.
The CMS uses these terms.
- • Physical restraint—any manual method or physical or mechanical device, material, or equipment attached to or near the person's body that he or she cannot remove easily and that restricts freedom of movement or normal access to one's body.
- • Chemical restraint—any drug used for discipline or convenience and not required to treat medical symptoms. The drug or dosage is not a standard treatment for the person's condition.
- • Freedom of movement—any change in place or position of the body or any part of the body that the person is able to control.
- • Convenience—any action taken to control or manage a person's behavior that requires less effort by the staff; the action is not in the person's best interest.
- • Discipline—any action taken by the agency to punish or penalize a patient or resident.
- • Remove easily—the manual method, device, material, or equipment used to restrain the person that can be removed intentionally by the person in the same manner it was applied by the staff. For example, the person can put bed rails down, untie a knot, or unclasp a buckle.
History of Restraint Use
Restraints were once used to prevent falls. Research shows that restraints cause falls. Falls occur when persons try to get free of the restraints. Injuries are more serious from falls in restrained persons than in those not restrained.
Restraints also were used to prevent wandering or interfering with treatment. They were often used for confusion, poor judgment, or behavior problems. Older persons were restrained more often than younger persons were. Restraints were viewed as necessary devices to protect a person. However, they can cause serious harm, even death. See “Risks From Restraint Use” on p. 203.
Besides the CMS, the Food and Drug Administration (FDA), state agencies, and The Joint Commission (TJC—an accrediting agency) have guidelines for restraint use. They do not forbid restraint use. They require considering or trying all other appropriate alternatives first.
Every agency has policies and procedures for restraints. They include identifying persons at risk for harm, harmful behaviors, restraint alternatives, and proper restraint use. Staff training is required.
Restraint Alternatives
Often there are causes and reasons for harmful behaviors. Knowing and treating the cause can prevent restraint use. This is very important for persons with speech or cognitive problems. The nurse tries to find out what the behavior means.
- • Is the person in pain, ill, or injured?
- • Is the person short of breath? Are cells getting enough oxygen (Chapter 39)?
- • Is the person afraid in a new setting?
- • Does the person need to use the bathroom?
- • Is clothing or a wound dressing (Chapter 36) tight or causing other discomfort?
- • Is the person's position uncomfortable?
- • Are body fluids, secretions, or excretions causing skin irritation?
- • Is the person too hot or too cold? Hungry or thirsty?
- • What are the person's life-long habits?
- • Does the person have problems communicating?
- • Is the person seeing, hearing, or feeling things that are not real (Chapters 48 and 49)?
- • Is the person confused or disoriented (Chapter 49)?
- • Are drugs causing the behaviors?
Restraint alternatives for the person are identified in the care plan (Box 15-1). The care plan is changed as needed. Restraint alternatives may not protect the person. The doctor may need to order restraints.
Safe Restraint Use
Restraints can cause serious injury and even death. CMS, OBRA, FDA, and TJC rules and guidelines are followed. So are state laws. They are part of the agency's policies and procedures for restraint use.
Restraints are not used to discipline a person. They are not used for staff convenience. Restraints are used only when necessary to treat medical symptoms. A medical symptom is an indication or characteristic of a physical or psychological condition. Symptoms may relate to physical, emotional, or behavioral problems. Sometimes restraints are needed to protect the person or others. That is, a person may have violent or aggressive behaviors that are harmful to self or others or that are threatening to others.
See Focus on Surveys: Safe Restraint Use.
Physical and Chemical Restraints
According to the CMS, a physical restraint includes these points.
- • May be any manual method, physical or mechanical device, material, or equipment.
- • Is attached to or next to the person's body.
- • Cannot be removed easily by the person.
- • Restricts freedom of movement or normal access to one's body.
Physical restraints are applied to the chest, waist, elbows, wrists, hands, or ankles. They confine the person to a bed or chair. Or they prevent movement of a body part. Some furniture or barriers also prevent freedom of movement.
- • A device used with a chair that the person cannot remove easily. The device prevents the person from rising. Trays, tables, bars, and belts are examples (Fig. 15-3).
 FIGURE 15-3 This lap-top tray is a restraint alternative. It is a restraint when used to prevent freedom of movement. (Image courtesy Posey Company, Arcadia, Calif.)
FIGURE 15-3 This lap-top tray is a restraint alternative. It is a restraint when used to prevent freedom of movement. (Image courtesy Posey Company, Arcadia, Calif.) - • Any chair that prevents the person from rising.
- • Any bed or chair placed so close to the wall that the person cannot get out of the bed or chair.
- • Bed rails (Chapter 14) that prevent the person from getting out of bed. For example, 4 half-length bed rails are raised. They are restraints if the person cannot lower them.
- • Tucking in or using Velcro (or other device) to hold a sheet, fabric, or clothing so tightly that freedom of movement is restricted.
Drugs or drug dosages are chemical restraints if they:
Drugs cannot be used for discipline or staff convenience. They cannot be used if they affect physical or mental function.
Sometimes drugs can help persons who are confused or disoriented. They may be anxious, agitated, or aggressive. The doctor may order drugs to control these behaviors. The drugs should not make the person sleepy and unable to function at his or her highest level.
Enablers.
An enabler is a device that limits freedom of movement but is used to promote independence, comfort, or safety. Some devices can be restraints or enablers. When the person can easily remove the device and it helps the person function, it is an enabler. For example:
- • A chair or wheelchair with a lap-top tray for meals, writing, and so on (see Fig. 15-3). The chair is an enabler. If used to limit freedom of movement, the chair is a restraint.
- • A person chooses to have raised bed rails. The bed rails are used to move in bed and to prevent falling out of bed. The bed rails are enablers, not restraints.
Risks From Restraint Use
Box 15-2 lists the risks from restraints. Injuries can occur as the person tries to get free of the restraint. Injuries also occur from using the wrong restraint, applying it wrong, or keeping it on too long. Cuts, bruises, and fractures are common. The most serious risk is death from strangulation.
Restraints are medical devices. The Safe Medical Devices Act applies if a restraint causes illness, injury, or death. Also, CMS requires the reporting of any death that occurs:
Laws, Rules, and Guidelines
Laws (federal and state) and rules (CMS, FDA) for restraint use are followed. So are accrediting agency (TJC) guidelines. Remember:
- • Restraints must protect the person. They are not used for staff convenience or to discipline a person. Using restraints is not easier than properly supervising and observing the person. A restrained person requires more staff time for care, supervision, and observation. A restraint is used only when it is the best safety measure for the person. Restraints are not used to punish or penalize uncooperative persons.
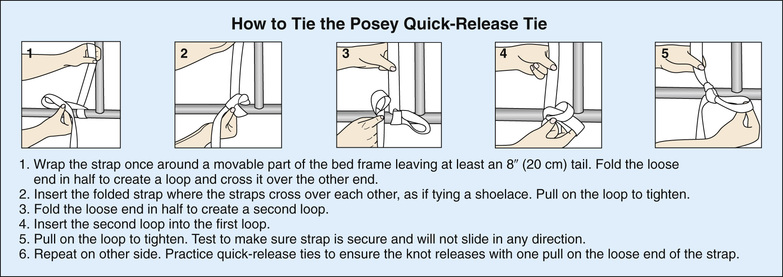
- • A doctor's order is required. OBRA, CMS, state laws, FDA warnings, TJC, and other accrediting agencies protect persons from unnecessary restraints. If restraints are needed for medical reasons, a doctor's order is required. The doctor gives the reason for the restraint, what body part to restrain, what to use, and how long to use it. This information is on the care plan and your assignment sheet. In an emergency, the nurse can decide to apply restraints before getting a doctor's order.
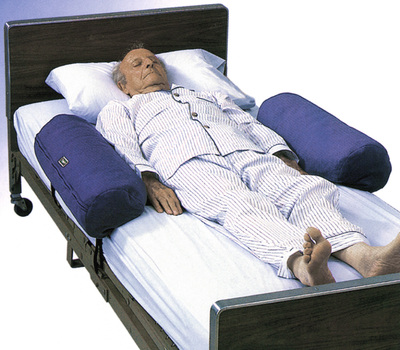
- • The least restrictive method is used. It allows the greatest amount of movement or body access possible. Some restraints attach to the person's body and to a fixed (non-movable) object. They restrict freedom of movement or body access. Vest, jacket, ankle, wrist, hand, and some belt restraints are examples. Other restraints are near but not directly attached to the person's body (bed rails or wedge cushions). They do not totally restrict freedom of movement and are less restrictive. They allow access to certain body parts.
- • Restraints are used only after other measures fail to protect the person (see Box 15-1). Some people can harm themselves or others. The care plan must include measures to protect the person and prevent harm to others. Many fall prevention measures are restraint alternatives (Chapter 14).
- • Unnecessary restraint is false imprisonment (Chapter 5). You must clearly understand the reason for the restraint and its risks. If not, politely ask about its use. If you apply an unneeded restraint, you could face false imprisonment charges.
- • Informed consent is required. The person must understand the reason for the restraint. The person is told how the restraint will help the planned medical treatment. The person is told about the risks of restraint use. If the person cannot give consent, his or her legal representative is given the information for purposes of giving consent. Consent must be given before a restraint can be used. The doctor or nurse provides needed information and obtains the consent.
Safety Guidelines
The restrained person must be kept safe. Follow the safety measures in Box 15-3. Also remember these key points.
- • Observe for increased confusion and agitation. Restraints can increase confusion and agitation. Whether confused or alert, people are aware of restricted movements. They may try to get out of the restraint or struggle to pull at it. Some restrained persons beg others to free or to help release them. These behaviors often are viewed as signs of confusion. Some people become more confused because they do not understand what is happening to them. Restrained persons need repeated explanations and reassurance. Spending time with them has a calming effect.
- • Protect the person's quality of life. Restraints are used for as short a time as possible. The care plan must show how to reduce restraint use. The person's needs are met with as little restraint as possible. You must meet the person's physical, emotional, and social needs. Visit with the person and explain the reason for the restraint.
- • Follow the manufacturer's instructions. They explain how to safely apply and secure the restraint. The restraint must be snug and firm but not tight. Tight restraints affect circulation and breathing. The person must be comfortable and able to move the restrained part to a limited and safe extent. You could be negligent if you do not apply or secure a restraint properly.
- • Apply restraints with enough help to protect the person and staff from injury. Persons in immediate danger of harming themselves or others are restrained quickly. Combative and agitated people can hurt themselves and the staff when restraints are applied. Enough staff members are needed to complete the task safely and quickly.
- • Observe the person at least every 15 minutes or as often as directed by the nurse and the care plan. Restraints are dangerous. Injuries and deaths can result from improper restraint use and poor observation. Prevent complications. Breathing and circulation problems are examples.
- • Remove or release the restraint, re-position the person, and meet basic needs at least every 2 hours. Or do so as often as noted in the care plan.
- • Remove or release the restraint for at least 10 minutes.
- • Provide for food, fluid, comfort, safety, hygiene, and elimination needs. Also give skin care.
- • Perform ROM exercises or help the person walk (Chapter 30). Follow the care plan.
See Focus on Communication: Safety Guidelines, p. 208.
See Teamwork and Time Management: Safety Guidelines, p. 209.
Reporting and Recording
Restraint information is recorded in the person's medical record (see Fig. 15-15). If you apply restraints or care for a restrained person, report and record:
- • The type of restraint applied.
- • The body part or parts restrained.
- • The reason for the application.
- • Safety measures taken (for example, bed rails padded and up, call light within reach).
- • The time you applied the restraint.
- • The time you removed or released the restraint and for how long.
- • The person's vital signs.
- • The care given when the restraint was removed and for how long.
- • Skin color and condition.
- • Condition of the limbs.
- • The pulse felt in the restrained part.
- • Changes in the person's behavior.
Report the following complaints at once.
 Applying Restraints
Applying Restraints
Restraints are made of cloth or leather. Cloth restraints (soft restraints) are mitts, belts, straps, jackets, and vests. They are applied to the wrists, ankles, hands, waist, and chest. Leather restraints are applied to the wrists and ankles. Leather restraints are used for extreme agitation and combativeness.
Wrist Restraints.
Wrist restraints (limb holders) limit arm movement (Fig. 15-16). They may be used when the person:

Mitt Restraints.
Hands are placed in mitt restraints. They prevent finger use. They allow hand, wrist, and arm movements. They have the same purpose as wrist restraints. Most mitts are padded (Fig. 15-17).

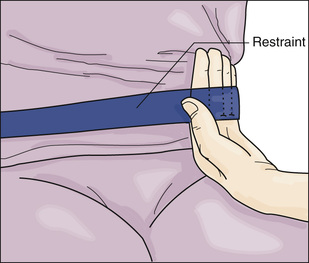
Belt Restraints.
A belt restraint (Fig. 15-18) may be used when injuries from falls are risks or for positioning during a medical treatment. The person cannot get out of bed or out of a chair. However, a roll belt allows the person to turn from side to side or to sit up in bed.

The belt is applied around the waist and secured to the bed or chair (lap belt). It is applied over a garment. The person can release the quick-release type. It is less restrictive than those that only staff can release.
Vest Restraints and Jacket Restraints.
Vest and jacket restraints are applied to the chest. They have the same purpose as belt restraints. The person cannot turn in bed or get out of a chair.
A jacket restraint is applied with the opening in the back. For a vest restraint, the “V” neck is in front and the vest crosses in the front (see Fig. 15-4). Vest and jacket restraints are never worn backward. Strangulation or other injuries are risks if the person slides down in the bed or chair. The restraint is always applied over a garment. (NOTE: The straps of vest and jacket restraints cross in the front. A vest or jacket restraint may have a positioning slot in the back [Fig. 15-19]. Criss-cross straps following the manufacturer's instructions.)

Vest and jacket restraints have life-threatening risks. Death can occur from strangulation. If caught in the restraint, it can become so tight that the person's chest cannot expand to inhale air. The person quickly suffocates and dies. Correct application is critical. You are advised to only assist the nurse in applying them. The nurse should assume full responsibility for applying a vest or jacket restraint.
See Focus on Communication: Applying Restraints.
See Focus on Children and Older Persons: Applying Restraints, p. 212.
See Delegation Guidelines: Applying Restraints, p. 212.
See Promoting Safety and Comfort: Applying Restraints, p. 212.
See procedure: Applying Restraints, p. 213.
Review Questions
Circle T if the statement is TRUE or F if it is FALSE.
1. T F Restraint alternatives fail to protect a person. You can apply a restraint.
2. T F A restraint restricts a person's freedom of movement.
3. T F Some drugs are restraints.
4. T F Restraints can be used for staff convenience.
5. T F A device is a restraint only if it is attached to the person's body.
6. T F Bed rails are restraints if the person cannot lower them.
7. T F Restraints are used only for a person's specific medical symptom.
8. T F Unnecessary restraint is false imprisonment.
9. T F You can apply restraints when you think they are needed.
10. T F You can use a vest restraint to position a person on the toilet.
11. T F Restraints are removed or released at least every 2 hours.
12. T F Restraints are tied to bed rails.
13. T F Wrist restraints are used to prevent falls.
14. T F A vest restraint crosses in front.
15. T F Bed rails are left down when a vest restraint is used.
Circle the BEST answer.
16. Which is a restraint alternative?
a Positioning the person's chair close to the wall
c Giving a drug that restricts movement
d Padding walls and corners of furniture
a Can be removed easily by the person
d Are safer than chemical restraints
18. The following can occur because of restraints. Which is the most serious?
19. A belt restraint is applied to a person in bed. Where should you secure the straps?
c To the movable part of the bed frame
20. A person has a restraint. You should check the person and the position of the restraint at least every
21. A person has mitt restraints. Which will you report to the nurse at once?
a The hands are clean, warm, and dry.
b The person has numbness in the hands.
c You removed the restraints for 10 minutes.
d You felt a pulse in both arms.
22. When applying restraints, you should
a Know when to apply and release them
b Use force if the person is agitated
c Allow plenty of slack in the straps
d Apply a restraint you have not used before
23. A person has a vest restraint. To check for snugness, slide
a A fist between the vest and the person
b 1 finger between the vest and the person
c An open hand between the vest and the person
d 2 fingers between the vest and the person
24. The correct way to apply any restraint is to follow the
See Review Question Answers at the back of the text.