10 Biomechanical Implications in Shoulder and Knee Rehabilitation
Biomechanical analysis of rehabilitation exercises has gained recent attention in sports medicine and orthopedic practice. Several investigators have sought to quantify the kinematics, kinetics, and electromyographic (EMG) activity during common rehabilitation exercises in an attempt to fully understand the implications of each exercise on the arthrokinematics and soft tissues of the shoulder and knee. Advances in understanding the biomechanical factors associated with rehabilitation have led to enhancement of rehabilitation programs that place minimal strain on specific healing structures while returning the injured athlete to competition as quickly and safely as possible. The purpose of this chapter is to provide an overview of the biomechanical implications associated with rehabilitation of the athlete’s shoulder and knee.
Biomechanical implications of shoulder rehabilitation
The glenohumeral joint exhibits the greatest amount of motion of any articulation in the human body, although little inherent stability is provided by its osseous configuration. Functional stability is accomplished through the integrated functions of the joint capsule, ligaments, and glenoid labrum, as well as through neuromuscular control and dynamic stabilization of the surrounding musculature, particularly the rotator cuff muscles.1-4 The rotator cuff musculature maintains stability of the glenohumeral joint by compressing the humeral head into the concave glenoid fossa during upper extremity motion.5 Thus, the glenohumeral muscles play a vital role in normal arthrokinematics and asymptomatic shoulder function.
Rehabilitation programs for the shoulder joint often focus on restoring maximum strength and muscular balance, particularly of the rotator cuff and scapulothoracic joint. The majority of research on shoulder biomechanics has focused on quantifying the EMG activity of particular muscles during common rehabilitation exercises, the goal of which is to determine the most optimal exercise to recruit specific muscle activity and maximize shoulder strength and efficiency.
Electromyographic analysis of shoulder exercises
Townsend et al6 conducted one of the first comprehensive studies analyzing EMG activity in the shoulder musculature during rehabilitation exercises. Dynamic fine-wire EMG activity in the four rotator cuff muscles, pectoralis major, latissimus dorsi, and the three portions of the deltoid was studied in 15 healthy male subjects during 17 common shoulder exercises. The authors quantified the exercises that produced the most activity in each specific muscle (Table 10-1).
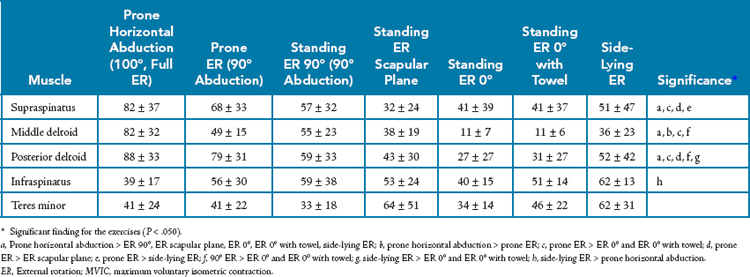
Table 10-1 Electromyographic Analysis of Glenohumeral Musculature*

For the anterior deltoid, exercises involving elevation of the shoulder, such as scaption with internal rotation (empty can), scaption with external rotation (full can), and forward flexion, produced the greatest amount of activity at approximately 70% manual muscle test activity (70% MMT). This was also consistent with results for the middle deltoid, although exercises in the prone position involving horizontal abduction produced approximately 80% MMT. The posterior deltoid showed the greatest amount of activity in the prone position during such exercises as horizontal abduction and rowing at approximately 90% MMT.
Similar to the anterior deltoid, the supraspinatus muscle was most active during shoulder elevation movements, although the military press (from 0° to 30°) produced the greatest amount of supraspinatus activity at 80% MMT. Comparing the empty can and full can exercises, the authors found 74% MMT during the empty can and 64% MMT during the full can.
The exercises with the most activity in the subscapularis muscle also included those involving shoulder elevation, though at a moderate intensity of approximately 55% MMT. Interestingly, the side-lying internal rotation exercise was not found to produce significant activity in the subscapularis, although the similar exercise of internal rotation at 0° abduction with exercise tubing was shown to have 52% maximal voluntary contraction by Hintermeister et al.7 Others have recommended motions involving lifting the hand off the lower part of the back and motions that replicate a tennis forehand with internal rotation and horizontal adduction.
The infraspinatus and teres minor muscles showed similar results with high activity during the side-lying external rotation exercise (85% for the infraspinatus and 80% for the teres minor). Exercises in the prone position involving horizontal abduction also produced high activity in the external rotators, with up to 88% MMT (range, 68% to 88% MMT) in the infraspinatus during prone horizontal abduction with external rotation.
The press-up exercise was found to elicit the most activity in the latissimus dorsi (55% MMT) and the pectoralis major (84%). This is consistent with the prime function of shoulder depression for each of these muscles. In comparison, the push-up produced 64% MMT in the pectoralis major.
Townsend et al6 studied 17 exercises and recommended inclusion of the empty can exercise, shoulder flexion, prone horizontal abduction with external rotation, and the press-up in shoulder rehabilitation programs based on the high activity in each muscle examined during these exercises.
Several research studies have since expanded on the work of Townsend et al.6 In particular, researchers have sought to compare the effectiveness of several exercises for the external rotators, supraspinatus, deltoid, and scapulothoracic musculature. The following sections discuss each one in detail.
External Rotators
An overhead throwing athlete requires the rotator cuff to maintain an adequate amount of glenohumeral joint congruency for asymptomatic function.8 Strength of the infraspinatus and teres minor is integral during the overhead throwing motion to develop a compressive force equal to body weight (BW) at the shoulder joint to prevent distraction.9 Andrews and Angelo10 found that overhead throwers most often have rotator cuff tears located from the mid–supraspinatus posterior to the midinfraspinatus area, which they believed to be a result of the compressive force produced to resist distraction, horizontal adduction, and internal rotation at the shoulder during arm deceleration. Thus, the external rotators are muscles that often appear weak and are affected by different pathologic shoulder conditions, such as internal impingement,11,12 joint laxity, labral lesions, and rotator cuff lesions,13,14 particularly in overhead throwing athletes.15,16 Consequently, many authors have advocated emphasis on strengthening of external rotation during rehabilitation or athletic conditioning programs to enhance muscular strength, endurance, and dynamic stability in overhead throwing athletes.
Several studies have documented the EMG activity in the glenohumeral musculature during specific shoulder exercises.6,17-25 Variations in experimental methodology have resulted in conflicting outcomes and controversy in the selection of exercises. As discussed previously, Townsend et al6 evaluated infraspinatus and teres minor activity during 17 shoulder exercises. The authors determined that the exercise eliciting the most EMG activity in the infraspinatus muscle was prone horizontal abduction with external rotation (88% MMT) and that the most effective exercise for the teres minor muscle was side-lying external rotation (80% MMT).
Similarly, Blackburn et al18 performed EMG analysis of the rotator cuff muscles in 28 healthy subjects during a series of 23 common posterior rotator cuff–strengthening exercises. The authors reported high levels of EMG activity in the infraspinatus (80% EMG activity) and teres minor (70% EMG activity) when the prone horizontal abduction movement at 90° and 100° of abduction with full external rotation was performed by 28 healthy subjects.
Conversely, Greenfield et al20 compared shoulder rotational strength in the scapular and frontal planes during isokinetic testing in 20 healthy subjects. The authors reported that no significant differences were found in internal rotation strength between positions; however, external rotation strength was significantly higher in the scapular plane, thus suggesting that the plane of the scapula may be a more effective position to exercise the external rotators.
Ballantyne et al17 compared EMG activity in the external rotators during side-lying external rotation and during external rotation in the prone position at 90° of abduction in 40 subjects. The authors reported similar EMG findings for the infraspinatus and teres minor during both exercises, with approximately 50% normalized activity for each muscle. Conversely, in the previously cited study by Blackburn et al,18 the authors compared side-lying external rotation and prone external rotation exercises and noted greater EMG activity during prone external rotation in the infraspinatus (prone, 80%; side lying, 30%) and teres minor (prone, 88%; side lying, 45%).
Reinold et al analyzed several different exercises commonly used to strengthen the external rotators to determine the most effect exercise and position to recruit muscle activity in the posterior rotator cuff.26 Integrated EMG activity in the infraspinatus, teres minor, supraspinatus, posterior deltoid, and middle deltoid in 10 asymptomatic subjects (5 male and 5 female subjects; mean age, 28.1 years; range, 22 to 38 years) was analyzed during seven exercises: prone horizontal abduction at 100° of abduction, full external rotation and prone external rotation at 90° of abduction, standing external rotation at 90° of abduction, standing external rotation at 45° in the scapular plane, standing external rotation at 0° of abduction, standing external rotation at 0° of abduction with a towel roll, and side-lying external rotation at 0° of abduction.
Based on the results of this study, the exercise that elicited the most combined EMG activity in the infraspinatus and teres minor was side-lying external rotation (infraspinatus, 62% maximum voluntary isometric contraction [MVIC]; teres minor, 67%), followed closely by external rotation in the scapular plane (infraspinatus, 53%; teres minor, 55%), and finally prone external rotation in the 90° abducted position (infraspinatus, 50%; teres minor, 48%) (Table 10-2).
Exercises in the 90° abducted position are often incorporated to simulate the position and strain on the shoulder during similar overhead activities such as throwing. This position produced moderate activity in the external rotators but also increased activity in the deltoid and supraspinatus to stabilize the shoulder. It appears that the amount of infraspinatus and teres minor activity progressively decreases as the shoulder moves into an abducted position whereas activity in the supraspinatus and deltoid increases. This may imply that as the arm moves into a position of less shoulder stability, the supraspinatus and deltoid are active to assist in the external rotation movement while providing some degree of glenohumeral stability through muscular contraction.
In the standing position, external rotation at 90° of abduction may have a functional advantage over 0° of abduction, and in the scapular plane, because of the close replication of this position in sporting activities the combination of abduction and external rotation places strain on the shoulder’s capsule, particularly the anterior band of the inferior glenohumeral ligament.27,28 When the arm is not in an abducted position, external rotation places less strain on this portion of the joint capsule. Therefore, although muscle activity was low to moderate during external rotation at 0° of abduction, this rehabilitation exercise may be worthwhile when strain of the inferior glenohumeral ligament is a concern. Side-lying external rotation may be the most optimal exercise to strengthen the external rotators based on the highest amount of EMG activity observed during this study.
Theoretically, external rotation at 0° of abduction with a towel roll provides both low capsular strain and also good balance between the muscles that externally rotate the arm and the muscles that adduct the arm to hold the towel. Our clinical experience has shown that adding a towel roll to the external rotation exercise provides assistance to the patient by ensuring that proper technique is observed without muscle substitution (Fig. 10-1). With the addition of a towel roll to the exercise, a tendency toward higher activity in the posterior rotator cuff was consistently seen as well. An approximately 20% to 25% increase in infraspinatus and teres minor EMG activity was noted with the use of a towel roll.
Furthermore, external rotation in the scapular plane may be an effective exercise during rehabilitation because of the moderate amount of muscular activity in each of the muscles tested, with a moderate amount of capsular strain occurring in the 45° abducted position (Fig. 10-2). This exercise may offer a compromise between strengthening and stabilization.
The exercises that produced the greatest amount of activity in the external rotators were side-lying external rotation, external rotation in the scapular plane, and external rotation at 90° of abduction (both standing and in the prone position).
Supraspinatus and Deltoid
Numerous investigators have studied EMG activity in the supraspinatus during rehabilitation exercises. Controversy exists regarding the optimal exercise to elicit muscle activity. Jobe and Moynes29 were the first to recommend elevation in the scapular plane with internal rotation, or the empty can exercise. The authors recommended this exercise for strengthening the supraspinatus because of the high EMG activity observed during this movement. The recommendation for the empty can exercise was further strengthened by the work of Townsend et al,6 who reported greater amounts of EMG activity in the supraspinatus and deltoid muscles during the empty can exercise than during exercises consisting of elevation in the scapular plane with external rotation, or the full can exercise, although statistical analysis was not performed to compare the exercises (see Table 10-1).
In clinical studies, numerous authors have suggested that the empty can exercise may provoke pain in many patients by encroaching on soft tissue within the subacromial space during this impingement-type maneuver. Numerous authors have since compared the empty can exercise with several other common supraspinatus exercises to determine whether exercises that place the shoulder in less of a disadvantageous position elicit similar amounts of supraspinatus activity.
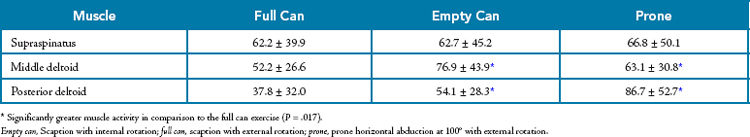
Blackburn et al18 compared EMG activity in the rotator cuff during several exercises and reported no significant differences in supraspinatus activity during the empty can and full can exercises. However, the authors did report a statistically significant increase in supraspinatus activity during prone horizontal abduction at 100° with full external rotation (Fig. 10-3).
Worrell et al25 compared the amount of supraspinatus activity during the empty can exercise recommended by Jobe and Moynes29 and the prone horizontal abduction exercise recommended by Blackburn and associates.18 The authors performed fine-wire EMG and handheld dynamometer measurements in 22 healthy subjects and reported greater supraspinatus activity during the prone exercise but less total force production than during the empty can exercise. The authors hypothesized that although supraspinatus activity was greater in the prone position, a greater amount of surrounding muscular activity was noted during the empty can exercise.
The effect of increased deltoid activity during arm elevation is a concern for the rehabilitation specialist, especially when a patient with subacromial impingement or pathologic rotator cuff conditions is being rehabilitated. Morrey et al30 examined the resultant force vectors of the deltoid and supraspinatus during arm elevation at various degrees of motion. Deltoid activity alone exhibited a superiorly orientated force vector from 0° to 90° and a compressive force on the glenohumeral joint at 120° to 150°. Conversely, the supraspinatus muscle produced a consistent compressive force throughout the range of elevation (Fig. 10-4). In patients with subacromial impingement, weak posterior rotator cuff muscles, inefficient dynamic stabilization, or pathologic changes in the rotator cuff, exercises that produce high levels of deltoid activity may be detrimental because of the amount of superior humeral head migration observed when the rotator cuff does not efficiently compress the humeral head within the glenoid fossa. Superior humeral head migration may be disadvantageous to patients with rotator cuff pathology or decreased stability of the glenohumeral joint. Superior humeral head migration may result in subacromial impingement, subdeltoid bursa trauma, and bursal thickening. The previously mentioned pathologies can result in tendon degeneration and eventually failure of the rotator cuff. Therefore, exercises are often chosen that minimize the opportunity for the deltoid to overpower the rotator cuff musculature during arm elevation.31
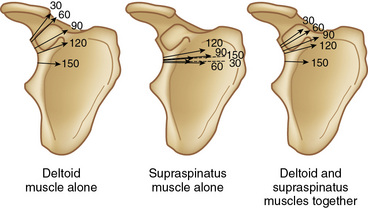
Figure 10-4 Direction of the magnitude of the resultant force vector for different glenohumeral joint positions as a function of different muscle activity.
(From Morrey, B.F., Itoi, E., and An, K.N. [1998]: Biomechanics of the shoulder. In: Rockwood, C.A., and Matsen, F.A. [eds]. The Shoulder, 2nd ed. Philadelphia, Saunders, pp. 233–276.)
Based on the hypothesis of Worrell et al,25 Malanga et al22 examined EMG activity in the supraspinatus and deltoid muscles during the empty can and prone exercises in 17 healthy subjects. The authors reported no significant differences in supraspinatus EMG activity during the two exercises (empty can, 107%; prone, 94%). However, a statistically significant increase in posterior deltoid EMG activity was observed during the prone exercise (empty can, 76%; prone, 96%) and significantly greater anterior deltoid EMG activity during the empty can exercise (empty can, 96%; prone, 65%). Middle deltoid EMG activity was high during both exercises (empty can, 104%; prone, 111%).
In a similar study, Kelly et al32 compared isometric EMG activity in the supraspinatus and deltoid muscles during the full can and empty can exercises in 11 healthy subjects. The authors again reported no significant difference in supraspinatus activity; however, they did note that the least amount of surrounding muscle activity was observed during the full can position and therefore recommended this position for manual muscle testing of the supraspinatus.
Takeda et al33 examined the most effective exercise for strengthening the supraspinatus by comparing magnetic resonance imaging (MRI) T2 relaxation times in the shoulders of six healthy subjects. The authors reported an increase in relaxation time that correlated well with concentric and eccentric muscle contractions. Subjects performed the empty can, full can, and prone exercises, and MRI scans were obtained immediately before and after each exercise. The change in relaxation in the supraspinatus was significantly higher during the empty can (10.5 msec) and full can (10.5 msec) exercises than during the prone exercise (3.6 msec). The least amount of deltoid activity was observed during the full can exercise.
Reinold et al34 were the first to examine both supraspinatus and deltoid muscle activity dynamically during all three exercises—empty can, full can, and prone. The authors measured fine-wire EMG activity in the dominant shoulder of 22 healthy subjects (15 male and 7 female subjects; mean age, 27 ± 5 years) (Table 10-3). EMG activity was normalized to MVIC and analyzed with a one-way repeated measures analysis of variance. The authors reported no significant difference in supraspinatus activity, which ranged from 62% to 67% MVIC during each exercise. However, post hoc analysis revealed significant differences in deltoid activity during the three exercises. The posterior deltoid showed the greatest activity during the prone full can exercise, whereas the middle deltoid displayed the greatest activity during the empty can and prone full can exercises. This information is important to consider when creating a strength program to maximize strength gains in the supraspinatus.
Biomechanically, Poppen and Walker35 examined the resultant force vectors of the glenohumeral joint during elevation with the arm positioned in neutral, internal rotation, and external rotation, similar to the empty can and full can exercises, respectively. The authors reported that at angles below 90° of abduction, the empty can position resulted in a superiorly orientated force vector whereas the full can position produced a compressive force from 0° to 120° (Fig. 10-5). These results of Poppen and Walker35 may correlate well with the previously mentioned studies reporting increased deltoid activity and thus superior humeral head migration during the empty can exercise.
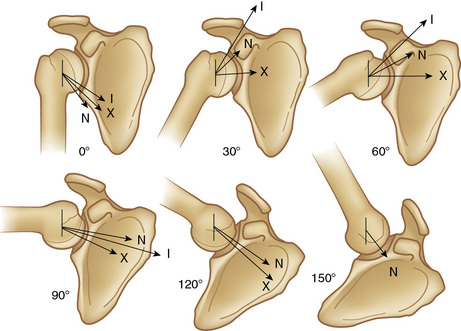
Figure 10-5 Position of the resultant force vector of the shoulder for different positions of arm elevation in (N) neutral rotation, (I) internal rotation, and (X) external rotation.
(From Poppen, N.K., and Walker, P.S. [1978]: Forces at the glenohumeral joint in abduction. Clin. Orthop. Relat. Res., 135:165–170.)
The empty can and full can exercises have also been examined to determine the accuracy of each when lesions of the supraspinatus tendon are detected. Itoi et al36 performed the two tests in 143 shoulders before MRI scans to detect a full-thickness tear of the rotator cuff. The authors considered a test positive if the subject exhibited pain, weakness, or both. The authors reported 75% accuracy with the full can test versus 70% with the empty can test. However, the empty can test also provoked greater pain.
Anatomically, internal rotation of the humerus during the empty can exercise does not allow the greater tuberosity to clear from under the acromion during arm elevation, which may increase risk for subacromial impingement because of decreased acromial space width. Biomechanically, shoulder abduction performed in extreme internal rotation progressively decreases the abduction moment arm of the supraspinatus from 0° to 90° of abduction. A diminished mechanical advantage may result in the supraspinatus needing to generate more force, thereby increasing tensile stress on an injured or healing tendon. This may also make the exercise more challenging for patients with weakness and facilitate compensatory movements such as the shoulder shrug.31
Scapular kinematics is also different between these exercises. Scapular internal rotation, or “winging“ (which occurs in the transverse plane with the scapular medial border moving posteriorly away from the trunk) and anterior tilt (which occurs in the sagittal plane with the scapular inferior angle moving posteriorly away from the trunk), is greater with the empty can exercise than with the full can exercise. This occurs in part because internal rotation of the humerus in the empty can position places tension on both the posteroinferior capsule of the glenohumeral joint and the rotator cuff (primarily the infraspinatus). Tension in these structures contributes to anterior tilt and internal rotation of the scapula, both of which contribute to scapular protraction. This is clinically important because scapular protraction has been shown to decrease the width of the subacromial space and thereby increase risk for subacromial impingement. In contrast, scapular retraction has been shown to increase the width of the subacromial space and supraspinatus strength potential (enhanced mechanical advantage) when compared with a more protracted position. These data also emphasize the importance of strengthening the scapular retractors and maintaining a scapular retracted position during shoulder exercises. We routinely instructed patients to emphasize an upright posture during shoulder exercises.31
The full can position is recommended for strengthening the supraspinatus muscle because the amount of muscle activity is similar to that for the empty can and prone exercises, with less activity in the deltoid and surrounding muscles, which possibly minimizes the amount of superior humeral head migration.
Therefore, based on the numerous EMG investigations, the full can exercise may be the best exercise for the supraspinatus because it produces moderate amounts of muscle activity with the least amount of pain provocation and surrounding muscle activation.
Scapulothoracic Joint
The scapulothoracic joint is often overlooked; however, it plays a critical role in movement of the upper extremity. During humeral elevation, the scapula rotates upwardly in the frontal plane at a ratio of 1° for every 2° of humeral elevation. After 120° of elevation, the scapula and humerus elevate at a 1:1 ratio. Total scapula upward rotation is minimal at 45° to 55°. A properly functioning scapula also tilts posteriorly (20° to 40°) and rotates externally (15° to 35°).31
EMG activity in muscles of the scapulothoracic joint have also been studied by several authors. Moseley et al37 examined eight muscles—the upper, middle, and lower trapezius, levator scapula, rhomboids, pectoralis minor, and middle and lower serratus anterior—during 16 commonly performed exercises in nine healthy subjects (Table 10-4). The authors reported the peak EMG activity in each muscle and noted that the majority of the muscles had assisted in more than one scapular function. Based on the results of the study, the authors recommended that a core program of exercises, including shoulder scaption, prone rowing, push-ups with a plus, and press-ups, should be included in shoulder and scapular rehabilitation programs.
More specifically, Decker et al38 documented the EMG activity in the serratus anterior during several different scapulohumeral rehabilitation exercises. The authors analyzed serratus anterior activity during eight common rehabilitation exercises in 20 healthy subjects. The authors developed a rank order of exercises that elicited the greatest amount of serratus activity. The three exercises that were suggested were the push-up with a plus (Fig. 10-6), the dynamic hug (Fig. 10-7), and a standing serratus anterior punch exercise (Fig. 10-8).

Figure 10-6 Push-up on a tabletop with a plus. The patient is instructed to fully protract the shoulder blade at the top of the push-up.

Figure 10-7 Dynamic hug exercise. Using resistance, the patient horizontally adducts the shoulder at 60° of elevation while protracting the scapula.
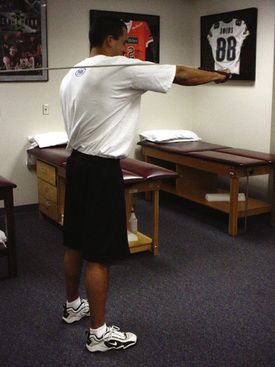
Figure 10-8 Standing serratus anterior punch exercise. The patient protracts the shoulder blade against resistance.
Ekstrom et al39 also looked at serratus activity during common exercises. The results of his study suggested that the serratus anterior has increased activity when performing movement that causes simultaneous upward rotation and protraction. A good example of this is the serratus anterior punch performed at 120° of abduction (Fig. 10-9) and during diagonal exercises that involve protraction with shoulder flexion, horizontal adduction, and external rotation.31

Figure 10-9 Supine punch performed at 120° of shoulder flexion to increase activation of the serratus anterior.
Hardwick et al40 looked at serratus anterior activity during the wall slide, wall push-up with a plus, and the full can exercise. The wall slide (Fig. 10-10, A to C) produced similar serratus anterior activity as did scapular abduction above 120° with no resistance. The wall slide might be advantageous in that patients report that it is less painful to perform. This may be due to the support that the upper extremities have when placed against the wall during the exercises. Placing the upper extremities against the wall might also compress the humeral head into the glenoid and thus improve glenohumeral stability during the early phases of rehabilitation.31
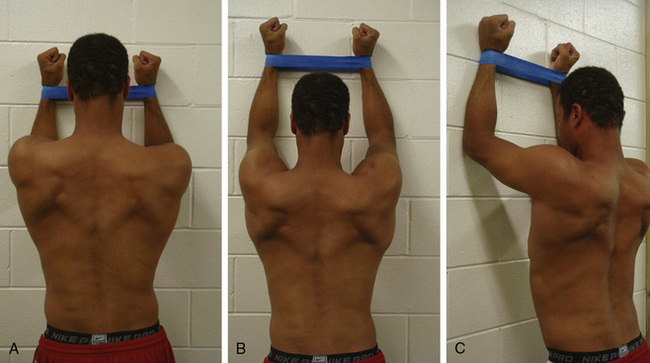
Figure 10-10 Wall slides performed with use of a Thera-Band to promote contraction of the external rotators of the glenohumeral joint. A, The patient begins the exercises with the elbows bent and shoulders below 90°. B, and C, Keeping the shoulders externally rotated, the patient slides his arms vertically up the wall as high as possible while maintaining both forearm contact with the wall and external rotation of the glenohumeral joint.
Biomechanical effects of pathologic shoulder conditions
Although the majority of biomechanical research on shoulder rehabilitation has involved healthy subjects, certain pathologic conditions may affect biomechanical function of the shoulder and require modification of the rehabilitation program.
Reddy et al41 evaluated EMG activity in the four rotator cuff and middle deltoid muscles in 15 healthy subjects and 15 subjects with subacromial impingement during elevation in the scapular plane. The diagnosis of impingement was based on radiographic evidence and confirmed after testing at the time of arthroscopic subacromial decompression. The authors reported an overall decrease in EMG activity in each muscle throughout the exercise in patients with impingement. A statistically significant decrease in EMG activity was observed in the infraspinatus, subscapularis, and middle deltoid from 30° to 60° of elevation. In addition, the infraspinatus muscle demonstrated a statistically significant decrease in EMG activity from 60° to 90° of elevation in patients with impingement.
The authors suggested that the decreased EMG activity in the shoulder musculature observed during arm elevation may lead to subacromial impingement. Furthermore, the decreased activity of the infraspinatus and subscapularis force couple along with normal activity of the supraspinatus may allow superior migration of the humeral head rather than glenohumeral joint compression and cause impingement within the subacromial space.
McMahon et al42 compared EMG activity in the rotator cuff and scapulothoracic muscles in 15 normal shoulders and 23 shoulders with anterior instability. EMG testing of abduction, scaption, and forward flexion was performed before surgical intervention for unidirectional anterior stabilization. The authors reported a statistically significant decrease in supraspinatus activity during abduction and scaption from 30° to 60° in subjects with instability. During all three movements, a statistically significant decrease in serratus anterior activity was also observed in subjects with instability. This occurred in the range of 30° to 120° of abduction and at 0° to 120° of scaption.
The authors suggested that the decreased amount of supraspinatus activity may result in disadvantageous superior humeral head migration and affect the amount of abnormal glenohumeral translation. Blasier et al43 reported that the supraspinatus muscle is highly active in stabilization of the shoulder joint, with an 18% reduction in force needed for subluxation of the glenohumeral joint when the supraspinatus muscle was not active.
Furthermore, the finding of decreased serratus anterior activity is also important in patients with shoulder instability. Decreased serratus anterior activity has likewise been observed in baseball pitchers with anterior instability44 and in swimmers with shoulder pain.28 The authors suggested that the decreased amount of serratus anterior activity may result in an inability to place the scapula in an upward position during shoulder elevation and thus alter the position and length-tension relationship of the static and dynamic stabilizers of the shoulder.
EMG activity in the rotator cuff is decreased in shoulders with subacromial impingement and anterior shoulder instability.
Based on the EMG results of these studies, the Thrower’s Ten Exercise Program (see Appendix A) is recommended for athletes to strengthen the glenohumeral and scapulothoracic muscles so that they can perform competitively.
Biomechanical implications of knee rehabilitation
Several methods of biomechanical analysis have been used to study rehabilitation of the knee, including cadaveric, EMG, kinematic, kinetic, mathematic modeling, and in vivo strain gauge measurements. To best evaluate these studies, it is helpful to delineate the findings based on the tissue or structure being examined, such as the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and patellofemoral joint.
Anterior Cruciate Ligament
The majority of biomechanical research during rehabilitation of the knee has focused on the ACL. The efficacy of open kinetic chain (OKC) and closed kinetic chain (CKC) exercises has been heavily scrutinized after years of theoretic and anecdotal assumptions. Markolf et al45 examined the effect of compressive loads on cadaveric knees to simulate BW. The authors reported that when compared with OKC exercises, compressive forces reduce strain on the ACL, thus providing a protective mechanism. Fleming et al46 investigated this theory with in vivo strain gauge measurements within the ACL. The use of in vivo strain gauge measurements within the ACL has allowed a method to directly measure ACL strain during activity. The authors noted that strain on the ACL increased from − 2.0% during non–weight bearing to 2.1% in a weight-bearing position. Although an increase in ACL strain was observed in a weight-bearing position, it is still unclear whether a 2% strain is detrimental to the healing ACL graft, although clinical experience has shown that early weight bearing has not resulted in poor functional outcomes of ACL reconstructions postoperatively.
CKC exercises have also been theorized to reduce ACL strain by providing cocontraction of the hamstrings and quadriceps. Wilk et al47 examined EMG activity in the quadriceps and hamstrings during CKC squat, leg press, and OKC knee extension. The authors noted that cocontraction occurred from 30° to 0° during the ascent phase of the squat, when the body is positioned directly over the knees and feet, but did not occur at other ranges of motion or during the CKC leg press or OKC knee extension. Thus, not all CKC exercises produce cocontraction of the quadriceps and hamstrings. Rather, it appears that several factors affect muscle activation during CKC exercises, including knee flexion angle, body position relative to the knee, and direction of movement (ascending or descending). Clinically, exercises performed in an upright and weight-bearing position with the knee flexed to approximately 30°, such as squats and lateral lunges, may be used during knee rehabilitation to promote cocontraction of the quadriceps and hamstrings.
Wilk et al47 also used mathematic modeling to estimate the shear forces at the tibiofemoral joint during the squat, leg press, and knee extension exercise (Fig. 10-11). The authors reported that a posterior tibiofemoral shear force was observed throughout the entire range of motion during both CKC squatting and leg press (peak, 1500 N) and during deep angles of OKC knee extension from 100° to 40° (peak, 900 N). Anterior tibiofemoral shear force (peak, 250 N) and theoretically ACL strain were observed during the OKC knee extension exercise from 40° to 10°.
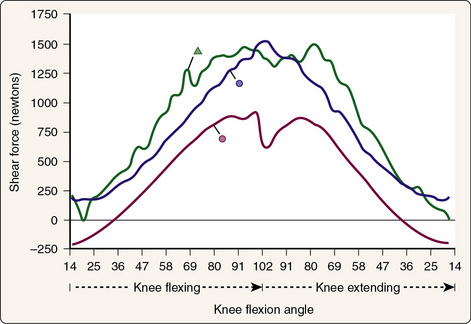
Figure 10-11 Shear forces at the tibiofemoral joint during the squat (triangle), leg press (blue circle), and knee extension exercises (red circle).
(Data from Wilk, K.E., Escamilla, R.F., Fleisig, G.S., et al. [1996]: A comparison of the tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am. J. Sports Med., 24:518–527.)
Similar to the results of Wilk et al,47 Beynnon et al48 reported that the greatest amount of ACL strain (2.8%) occurred from 40° to 0° during OKC knee extension using in vivo strain gauge measurements. This strain was found to significantly increase in a linear fashion with the application of an external 45-N boot (3.8%). However, the authors also reported ACL strain of 3.6% during the CKC squat exercise. In contrast, application of external loading did not significantly increase the amount of strain on the ACL (4.0%). Based on the results of these studies,46-48 both OKC and CKC exercises are performed, although the patient is often limited to 90° to 40° during the OKC knee extension when heavy resistance is applied.
Recent research has looked at the different stresses placed on the ACL during some common exercises used during the rehabilitation process to strengthen the lower extremity. Escamilla et al49 investigated the strain placed on the ACL during lunges with different step lengths. They found that minimal strain was placed on the ACL during both long- and short-stride lunges. ACL loading occurred only during lunges with a short stride (0 to 50 N between 0° and 10° of flexion). In a different study, Escamilla et al50 examined ACL forces during the side lunge and compared them with the forward lunge. They found that side lunges placed no additional strain on the ACL. Thus, both forward and side lunges appear to be safe and effective methods of strengthening the lower extremity during all phases of ACL rehabilitation.
Additionally, Escamilla studied the impact of different squat variations on the ACL. He showed that low anterior shear forces occur during the dynamic squat, especially in the early ranges of motion (0° to 60°) of knee flexion.51 Furthermore, Escamilla et al49 also assessed anterior shear forces in the knee during one-legged squats and wall squats. They found that wall squats with both legs close to the wall and with the legs farther away from the wall yielded no increased strain on the ACL. Anterior shear forces did increase during the one-legged squat from 0° to 40° of knee flexion (59 ± 52 N).
Also commonly used during ACL rehabilitation are the bicycle and stair-climbing machines. Fleming et al52 analyzed six different bicycle-riding conditions induced by manipulating speed and power. The authors found no significant differences between conditions, with a minimal mean ACL strain of 1.7%. The greatest amount of strain was observed when the knee reached the greatest amount of extension. Similarly, Fleming et al53 analyzed two cadences of stair climbing (80 and 112 steps per minute) and noted a similar 2.7% strain on the ACL. Again, the most amount of strain was observed during terminal knee extension. Thus, when compared with other rehabilitation exercises, both bicycling and stair climbing are safe exercises that place low strain on the ACL (Table 10-5). Furthermore, the greatest amount of strain was observed as the knee moved into terminal knee extension, similar to the results of Wilk et al47 and Beynnon et al48 during OKC and CKC exercises.
Table 10-5 In Vivo Strain on the Anterior Cruciate Ligament
| Exercise | Strain (%) |
|---|---|
| Isometric quadriceps contraction at 15° | 4.4 |
| Squatting with resistance | 4.0 |
| Active knee flexion with resistance | 3.8 |
| Lachman test (150 N of anterior shear at 30°) | 3.7 |
| Squatting without resistance | 3.6 |
| Active knee flexion without resistance | 2.8 |
| Quadriceps and hamstring cocontraction at 15° | 2.7 |
| Isometric quadriceps contraction at 30° | 2.7 |
| Stair climbing | 2.7 |
| Anterior drawer test (150 N of anterior shear at 90°) | 1.8 |
| Stationary bicycle | 1.7 |
| Quadriceps and hamstrings cocontraction at 30° | 0.4 |
| Passive knee range of motion | 0.1 |
| Isometric quadriceps contraction at 60° and 90° | 0.0 |
| Quadriceps and hamstrings cocontraction at 60° and 90° | 0.0 |
| Isometric hamstring contraction at 30°, 60°, and 90° | 0.0 |
Modified from Fleming, B.C., Beynnon, B.D., Renstrom, P.A., et al. (1999): The strain behavior of the anterior cruciate ligament during stair climbing: An in vivo study. Arthroscopy, 15:185–191.
OKC knee extension may be performed from 90° to 40° with progressive resistance to minimize strain on the ACL.
Weight bearing and CKC exercises may be performed immediately without placing excessive strain on the ACL.
Posterior Cruciate Ligament
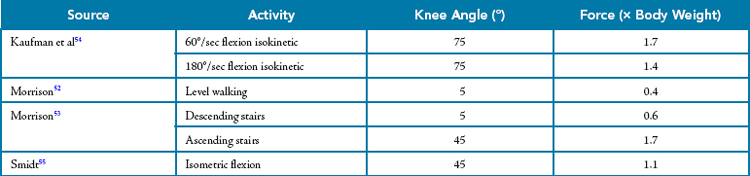
Historically, the results of rehabilitation after PCL injury have been mixed. Poor functional outcomes have often been attributed to the residual laxity present after surgical reconstruction. The biomechanics of the tibiofemoral joint during exercise must be understood so that the rehabilitative process will not create deleterious effects on the PCL. The posterior tibiofemoral shear forces that occur during specific activities, such as level walking,54 ascending and descending stairs,55 and resisted knee flexion exercises56,57 have previously been documented.58,59 Level walking and descending stairs produce a relatively low posterior tibiofemoral shear force of 0.4 × BW and 0.6 × BW, respectively (Table 10-6). However, high posterior shear force has been noted during several commonly performed activities of daily living, such as climbing stairs (1.7 × BW at 45° of knee flexion)55,60 and squatting (3.6 × BW at 140° of knee flexion), and may have an effect on residual laxity postoperatively. Further studies show that isometric knee flexion at 45° places a posterior shear force of 1.1 × BW on the tibiofemoral joint.57
Tremendous shear forces on both the PCL and the tibiofemoral joint occur during OKC resisted knee flexion. Posterior tibial displacement is attributed to the high EMG activity in the hamstring muscle while resistive knee flexion is performed. Lutz et al reported a maximum shear force of 1780 N at 90° of flexion, 1526 N at 60°, and 939 N at 30° during isometric knee flexion (Fig. 10-12). Kaufman et al56 also noted a PCL load of 1.7 × BW at 75° of flexion during the isokinetic knee flexion exercise. Because PCL stress increases with knee flexion angle, isolated OKC knee flexion exercises should be avoided for at least 8 weeks postoperatively and until symptoms subside in nonoperative cases.
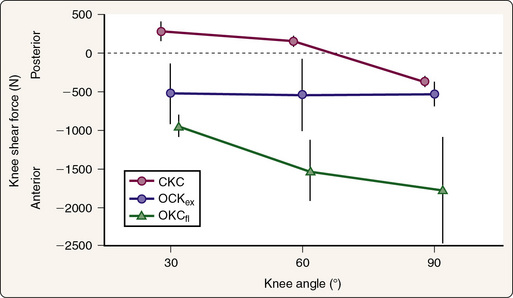
Figure 10-12 Shear force at the tibiofemoral joint during squatting, knee extension, and knee flexion. CKC, Closed kinetic chain; OKCex, open kinetic chain extension; OKCfl, open kinetic chain flexion.
(Data from Lutz, G.E., Palmitier, R.A., An, K.N., and Chao, E.Y. [1993]: Comparison of tibiofemoral joint forces during open and closed kinetic chain exercises. J. Bone Joint Surg. Am., 75:732–735.)
Excessive stress on the PCL has also been observed during deeper angles of OKC knee extension. Several studies have proved that resisted knee extension at 90° of flexion causes a posterior tibiofemoral shear force and potential stress on the PCL.47,56,61-63 Wilk et al47 documented a posterior shear force from 100° to 40° with resisted OKC knee extension (see Fig. 10-11). The highest amount of stress on the PCL was found at angles of 85° to 95° during knee flexion. Conversely, the lowest amount of posterior shear force occurred from 60° to 0° of resisted knee extension.47 Kaufman et al56 also reported that posterior shear forces take place until 50° to 55° of knee flexion. Furthermore, Jurist and Otis62 also documented stress on the PCL at 60° of flexion during an isometric knee extension exercise when resistance was applied at the proximal end of the tibia. To reduce the excessive posterior shear force placed on the PCL, OKC resisted knee extension should be performed from 60° to 0°.58,59
The stress applied to the PCL while CKC exercises are performed is relative to the knee flexion angle produced during the exercise. Wilk et al47,64 reported an increase in posterior shear force as the knee flexion angle increases during CKC exercise (see Fig. 10-11). Meglan et al65 also documented a linear increase in posterior shear force from 40° to 100° of knee flexion during the front squat maneuver. Escamilla et al49 assessed the load applied to the PCL during the wall and single-leg squat. They found that the wall squat with the legs farther away from the wall and thus a greater flexion angle was associated with significantly greater posterior shear force than was the wall squat with the feet closer to the wall and less knee flexion. The wall squat with a greater flexion angle of the knee also produced higher posterior shear forces than did the one-legged squat. Therefore, to reduce PCL stress during CKC exercises, leg presses and squats are performed from 0° to 60° of knee flexion.58,59
Escamilla et al investigated the tension placed on the PCL during forward lunge with a short step, forward lunge with a long step, and side lunge.47,48 They found that PCL tension increased as the stride became longer in the forward lunge, which resulted in deeper knee flexion angles. They also determined that as knee flexion increased in the side lunge, so did posterior shear forces at the knee. It is recommended that clinicians use caution when prescribing both forward and side lunges during PCL rehabilitation, especially during the early phases of rehabilitation. It is crucial to monitor and limit the amount of knee flexion that occurs during the lunge exercise when rehabilitating the PCL.
OKC knee flexion produces high posterior tibiofemoral shear forces and should initially be limited to minimize strain on the PCL.
Patellofemoral Joint
When one is rehabilitating a patient with a known lesion of the patellofemoral joint, it is important to first understand normal patellofemoral joint arthrokinematics. Articulation between the inferior margin of the patella and the femur begins at approximately 10° to 20° of knee flexion.66 As the knee proceeds into greater degrees of knee flexion, the contact area of the patellofemoral joint moves proximally along the patella. At 30°, the area of patellofemoral contact is approximately 2.0 cm.1,66 The area of contact gradually increases as the knee is flexed. At 90° of knee flexion the contact area increases up to 6.0 cm.1,66
Alterations in the Q angle are often associated with patellofemoral disorders and may change the contact areas and thus the amount of joint reaction forces on the patellofemoral joint. Huberti and Hayes67 examined in vitro patellofemoral contact pressures at various degrees of knee flexion from 20° to 120°. The maximum contact area occurred at 90° of knee flexion with a force estimated to be 6.5 × BW. An increase or decrease in the Q angle of 10° resulted in increased maximum contact pressure and a smaller total area of contact throughout the range of motion. This information may be applied when one prescribes rehabilitation interventions so that the exercises are performed in ranges of motion that place minimal strain on damaged structures.
The effectiveness and safety of OKC and CKC exercises during patellofemoral rehabilitation have been heavily scrutinized in recent years. Whereas CKC exercises replicate functional activities such as ascending and descending stairs, OKC exercises are often desired for isolated muscle strengthening when specific muscle weakness is present.68
Steinkamp et al69 analyzed patellofemoral joint biomechanics during leg press and extension exercises in 20 normal subjects. Patellofemoral joint reaction force, stress, and moments were calculated during both exercises (Fig. 10-13). From 0° to 46° of knee flexion, patellofemoral joint reaction force was less during the CKC leg press. Conversely, from 50° to 90° of knee flexion, joint reaction forces were lower during the OKC knee extension exercise. Joint reaction forces were minimal at 90° of knee flexion during the knee extension exercise.
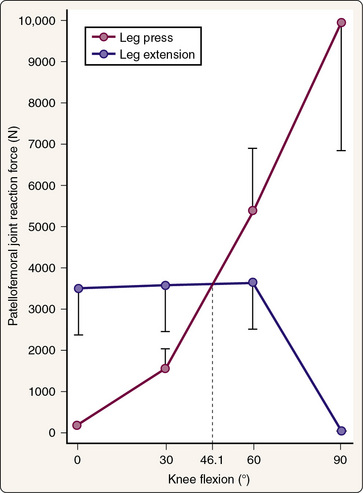
Figure 10-13 Patellofemoral joint reaction forces during leg press and leg extension exercises.
(Data from Steinkamp, L.A., Dillingham, M.F., Markel, M.D., et al. [1993]: Biomechanical considerations in patellofemoral joint rehabilitation. Am. J. Sports Med., 21:438–444.
Escamilla et al70 observed the patellofemoral compressive forces during OKC knee extension and CKC leg press and vertical squat. The results were similar to the findings of Steinkamp et al69; OKC knee extension produced significantly greater force at angles less than 57° of knee flexion, whereas both CKC activities produced significantly greater force at knee angles greater than 85°.
Escamilla et al71,72 studied compressive force on the knee during the lunge exercise both with and without a stride. The results of their study showed a direct relationship between knee force and the amount of knee flexion performed during the lunge exercise. As knee flexion increases, the amount of patellofemoral compressive force increases linearly, and compressive force decreases as knee flexion decreases. Furthermore, they found that knee compressive force is greater in lunges performed with a stride than in lunges performed without a stride. The side lunge caused more compressive force on the patellofemoral joint than the forward lunge did.71
When analyzing the biomechanics of OKC knee extension, Grood et al73 reported that quadriceps force was greatest near full knee extension and increased with the addition of external loading. The small patellofemoral contact area observed near full extension, as discussed previously, and the increased amount of quadriceps force generated at these angles may make the patellofemoral joint more susceptible to injury. As the knee approaches terminal extension, the large magnitude of quadriceps force is focused onto a more condensed location on the patella. When one applies the results of Steinkamp et al,69 Escamilla et al,70 and Grood et al,73 it appears that during OKC knee extension, as the contact area of the patellofemoral joint decreases, the force of quadriceps pull subsequently increases, thereby resulting in a large magnitude of patellofemoral contact stress being applied to a focal point on the patella. In contrast, during CKC exercises, quadriceps force increases as the knee continues into flexion. However, the area of patellofemoral contact also increases as the knee flexes, which leads to wider dissipation of contact stress over a larger surface area.
Witvrouw et al74 prospectively studied the efficacy of OKC and CKC exercises during nonoperative patellofemoral rehabilitation. Sixty patients participated in a 5-week exercise program consisting of either OKC or CKC exercises. Subjective pain scores, functional ability, quadriceps and hamstring peak torque, and hamstring, quadriceps, and gastrocnemius flexibility were all recorded before and after rehabilitation, as well as at 3 months after intervention. Both treatment groups reported a significant decrease in pain, an increase in muscle strength, and an increase in functional performance 3 months after intervention.
Thus, it appears that both OKC and CKC exercises may be used to maximize outcomes in patients with patellofemoral joint problems if performed within a safe range of motion. Exercises are based on clinical assessment. If CKC exercises are less painful than OKC exercises, that form of muscular training is encouraged. Additionally, in postoperative patients, regions of articular cartilage wear are carefully considered before an exercise program is designed. For the most part, we allow OKC exercises such as knee extension from 90° to 40° of knee flexion. This range of motion provides the lowest amount of patellofemoral joint reaction force while exhibiting the greatest amount of patellofemoral contact area. CKC exercises, such as leg presses, vertical squats, lateral step-ups, and wall squats (slides), are performed initially from 0° to 30° and then progressed from 0° to 60° when patellofemoral joint reaction forces can be tolerated. As the patient’s symptoms subside, the ranges of motion that are performed are progressed to allow greater muscle strengthening in larger ranges. Progression of exercises is based on the patient’s subjective reports of symptoms and clinical assessment of swelling, range of motion, and painful crepitus.
OKC knee extension may be performed from 90° to 40° to produce the lowest amount of patellofemoral joint reaction force with the greatest amount of patella surface contact.
CKC exercise may be performed initially at 0° to 45° and be progressed to 0° to 60° as the patient’s condition improves to produce the lowest amount of patellofemoral joint reaction force.
Exercise prescription should be based on the location of the symptoms and symptom reproduction during exercises.
A thorough understanding of the biomechanical factors associated with rehabilitation is necessary to return the injured athlete to competition as quickly and safely as possible. Various factors are associated with specific pathologic conditions that will alter the rehabilitation program to minimize stress on healing structures. Knowledge of the biomechanical implications discussed in this chapter may be used when rehabilitation programs are designed for patients with pathologic rotator cuff, ACL, PCL, and patellofemoral joint conditions.
Conclusion
Overview
Shoulder Rehabilitation
1 Apreleva M., Hasselman C.T., Debski R.E., et al. A dynamic analysis of glenohumeral motion after simulated capsulolabral injury. J. Bone Joint Surg. Am.. 1998;80:474-480.
2 Cain P.R., Mutsehler T.A., Fu F.H. Anterior stability of the glenohumeral joint. A dynamic model. Am. J. Sports Med.. 1987;15:144-148.
3 Harryman D.T.II, Sidles J.A., Clark J.A., et al. Translation of the humeral head on the glenoid with passive glenohumeral motion. J. Bone Joint Surg. Am.. 1990;72:1334-1343.
4 Saha A.K. Dynamic stability of the glenohumeral joint. Acta Orthop. Scand.. 1971;42:491-505.
5 Wilk K.E., Arrigo C.A., Andrews J.R. Current concepts: The stabilizing structures of the glenohumeral joint. J. Orthop. Sports Phys. Ther.. 1997;25:364-379.
6 Townsend H., Jobe F.W., Pink M., Perry J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am. J. Sports Med.. 1991;19:264-272.
7 Hintermeister R.A., Lange G.W., Schultheis J.M., et al. Electromyographic activity and applied load during shoulder rehabilitation exercises using elastic resistance. Am. J. Sports Med.. 1998;26:210-220.
8 Wilk K.E., Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J. Orthop. Sports Phys. Ther.. 1993;18:365-378.
9 Fleisig G.S., Barrentine S.W., Escamilla R.F., Andrews J.R. Biomechanics of overhand throwing with implications for injuries. Sports Med.. 1996;21:421-437.
10 Andrews J.R., Angelo R.L. Shoulder arthroscopy for the throwing athlete. Tech. Orthop.. 1988;3:75.
11 Jobe F.W., Kvitne R.S., Giangarra C.E. Shoulder pain in the overhand or throwing athlete. The relationship of anterior instability and rotator cuff impingement. Orthop. Rev.. 1989;18:963-975.
12 Walch G., Boileau P., Noel E., Donell T. Impingement of the deep surface of the infraspinatus tendon on the posterior glenoid rim. J. Shoulder Elbow Surg.. 1992;1:239-245.
13 Neer C.S.II, Craig E.V., Fukuda H. Cuff tear arthropathy. J. Bone Joint Surg. Am.. 1983;65:1232.
14 Rockwood C.A., Matsen F.A. The Shoulder 1990 Saunders Philadelphia 755-795
15 Wilk K.E., Andrews J.R., Arrigo C.A., et al. The internal and external rotator strength characteristics of professional baseball pitchers. Am. J. Sports Med.. 1993;21:61-66.
16 Wilk K.E., Meister K., Andrews J.R. Current concepts in the rehabilitation of the overhead throwing athlete. Am. J. Sports Med.. 2002;30:136-151.
17 Ballantyne B.T., O’Hare S.J., Paschall J.L., et al. Electromyographic activity of selected shoulder muscles in commonly used therapeutic exercises. Phys. Ther.. 1993;73:668-677.
18 Blackburn T.A., McLeod W.D., White B. EMG analysis of posterior rotator cuff exercises. Athl. Train.. 1990;25:40-45.
19 Bradley J.P., Tibone J.E. Electromyographic analysis of muscle action about the shoulder. Clin. Sports Med.. 1991;10:805.
20 Greenfield B.H., Donatelli R., Wooden M.J., Wilkes J. Isokinetic evaluation of shoulder rotational strength between the plane of the scapula and the frontal plane. Am. J. Sports Med.. 1990;18:124-128.
21 Kronberg M., Nemeth G., Brostrom L.A. Muscle activity and coordination in the normal shoulder—An electromyographic study. Clin. Orthop. Relat. Res.. 1990;257:76-85.
22 Malanga G.A., Jenp Y.N., Growney E.S., An K.A. EMG analysis of shoulder positioning in testing and strengthening the supraspinatus. Med. Sci. Sports Exerc.. 1996;28:661-664.
23 McCann P.D., Wootten M.E., Kadaba M.P., Bigliani L.U. A kinematic and electromyographic study of shoulder rehabilitation exercises. Clin. Orthop. Relat. Res.. 1993;288:179-188.
24 Moynes D.R., Perry J., Antonelli D.J., et al. Electromyographic motion analysis of the upper extremity in sports. Phys. Ther.. 1986;66:1905-1911.
25 Worrell T.W., Corey B.J., York S.L., Santiestaban J. An analysis of supraspinatus EMG activity and shoulder isometric force development. Med. Sci. Sports Exerc.. 1992;24:744-748.
26 Reinold M.M., Wilk K.E., Fleisig G.S., et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J. Orthop. Sports Phys. Ther.. 2004;34:385-394.
27 O’Brien S.J., Neves M.C., Arnoczky S.P., et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am. J. Sports Med.. 1990;18:449-456.
28 Scovazzo M.L., Browne A., Pink M., et al. The painful shoulder during freestyle swimming. An electromyographic cinematographic analysis of twelve muscles. Am. J. Sports Med.. 1991;19:577-582.
29 Jobe F.W., Moynes D.R. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am. J. Sports Med.. 1982;10:336-339.
30 Morrey B.F., Itoi E., An K.N. Biomechanics of the shoulder. In: Rockwood C.A., Matsen F.A., editors. The Shoulder. 2nd ed. Philadelphia: Saunders; 1998:233-276.
31 Reinold M.M., Escamilla R.F., Wilk K.E. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J. Orthop. Sports Phys. Ther.. 2009;39:105-117.
32 Kelly B.T., Kadrmas W.R., Speer K.P. The manual muscle examination for rotator cuff strength: An electromyographic investigation. Am. J. Sports Med.. 1996;24:581-588.
33 Takeda Y., Kashiwaguchi S., Endo K. The most effective exercise for strengthening the supraspinatus muscle: Evaluation by magnetic resonance imaging. Am. J. Sports Med.. 2002;30:374-381.
34 Reinold M.M., Ellerbusch M.T., Barrentine S.W., et al. Electromyographic analysis of the supraspinatus and deltoid muscles during rehabilitation exercises. J. Orthop. Sports Phys. Ther.. 32, 2002. A-43
35 Poppen N.K., Walker P.S. Forces at the glenohumeral joint in abduction. Clin. Orthop. Relat. Res.. 1978;135:165-170.
36 Itoi E., Kido T., Sano A., et al. Which is more useful, the “full can test“ or the “empty can test,“ in detecting the torn supraspinatus tendon. Am. J. Sports Med.. 1999;27:65-68.
37 Moseley J.B.Jr., Jobe F.W., Pink M., et al. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am. J. Sports Med.. 1992;20:128-134.
38 Decker M.J., Hintermiester R.A., Faber K.J., Hawkins R.J. Serratus anterior muscle activity during selected rehabilitation exercises. Am. J. Sports Med.. 1999;27:784-791.
39 Ekstrom R.A., Donatelli R.A., Soderberg G.L. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J. Orthop. Sports Phys. Ther.. 2003;33:247-258.
40 Hardwick D.H., Beebe J.A., McDonnell M.K., Lang C.E. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. J. Orthop. Sports Phys. Ther.. 2006;36:903-910.
41 Reddy A.S., Mohr K.J., Pink M.M., et al. Electromyographic analysis of the deltoid and rotator cuff muscles in person with subacromial impingement. J. Shoulder Elbow Surg.. 2002;9:519-523.
42 McMahon P.J., Jobe F.W., Pink M.M., et al. Comparative electromyographic analysis of shoulder muscles during planar motions: Anterior glenohumeral instability versus normal. J. Shoulder Elbow Surg.. 1996;5:118-123.
43 Blasier R.B., Guldberg R.E., Rothman E.D. Anterior shoulder stability: Contributions of rotator cuff forces and the capsular ligaments in a cadaveric model. J. Shoulder Elbow Surg.. 1992;1:140.
44 Glousman R., Jobe F., Tibone J., et al. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J. Bone Joint Surg. Am.. 1988;70:220-226.
45 Markolf K.L., Gorek J.F., Kabo J.M., Shapiro M.S. Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J. Bone Joint Surg. Am.. 1990;72:557-567.
46 Fleming B.C., Renstrom P.A., Beynnon B.D., et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J. Biomech.. 2001;34:163-170.
47 Wilk K.E., Escamilla R.F., Fleisig G.S., et al. A comparison of the tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am. J. Sports Med.. 1996;24:518-527.
48 Beynnon B.D., Johnson R.J., Flemming B.C., et al. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension: A comparison of an open and closed kinetic chain exercise. Am. J. Sports Med.. 1997;25:823-829.
49 Escamilla R.F., Zheng N., Imamura R., et al. Cruciate ligament force during the wall squat and the one-leg squat. Med Sci Sports Exerc.. 2009;41:408-417.
50 Escamilla R.F., Zheng N., MacLeod T.D., et al. Cruciate ligament tensile forces during the forward and side lunge. Clin. Biomech. (Bristol, Avon). 2002;25:213-221.
51 Escamilla R.F. Knee biomechanics of the dynamic squat exercise. Med. Sci. Sports Exerc.. 2001;33:127-141.
52 Fleming B.C., Beynnon B.D., Renstrom P.A., et al. The strain behavior of the anterior cruciate ligament during bicycling: An in vivo study. Am. J. Sports Med.. 1998;26:109-118.
53 Fleming B.C., Beynnon B.D., Renstrom P.A., et al. The strain behavior of the anterior cruciate ligament during stair climbing: An in vivo study. Arthroscopy. 1999;15:185-191.
54 Morrison J.B. The biomechanics of the knee joint in relation to normal walking. J. Biomech.. 1970;3:51.
55 Morrison J.B. The biomechanics of the knee joint in various knee activities. Biomech. Eng.. 1969;4:573-578.
56 Kaufman K.R., An K.N., Litchy W.J., et al. Dynamic joint forces during knee isokinetic exercise. Am. J. Sports Med.. 1991;19:305-316.
57 Smidt G.L. Biomechanical analysis of knee extension and flexion. J. Biomech.. 1973;6:79-83.
58 Wilk K.E. Rehabilitation of isolated and combined posterior cruciate ligament injuries. Clin. Sports Med.. 1994;13:649-677.
59 Wilk K.E., Andrews J.R., Clancy W.G., et al. Rehabilitation programs for the PCL-injured and reconstructed knee. J. Sport Rehabil.. 1999;8:333-361.
60 Clancy W.G. Repair and reconstruction of the posterior cruciate ligament. In: Chapman M.W., editor. Operative Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 1988:2093-2107.
61 Daniel D.M., Stone M.L., Barnett P., et al. Use of quadriceps active test to diagnose posterior cruciate ligament disruptions and measure posterior laxity of the knee. J. Bone Joint Surg. Am.. 1988;70:386-390.
62 Jurist K.A., Otis J.C. Anteroposterior tibiofemoral displacements during isometric extension efforts. Am. J. Sports Med.. 1985;13:254-258.
63 Lutz G.E., Palmitier R.A., An K.N., Chao E.Y. Comparison of tibiofemoral joint forces during open and closed kinetic chain exercises. J. Bone Joint Surg. Am.. 1993;75:732-735.
64 Wilk K.E., Zheng N., Fleisig G.S., et al. Kinetic chain exercise: Implication for the ACL patient. J. Sport Rehabil.. 1997;6:125-143.
65 Meglan D., Lutz G., Stuart M. Effects of closed kinetic chain exercises for ACL rehabilitation upon the load in the capsular and ligamentous structures of the knee Presented at the Orthopedic Research Society Meeting, San Francisco, February 15–18 1993
66 Hungerford D.S., Barry M. Biomechanics of the patellofemoral joint. Clin. Orthop. Relat Res.. 1979;144:9-15.
67 Huberti H.H., Hayes W.C. Patellofemoral contact pressures. J. Bone Joint Surg. Am.. 1984;66:715-724.
68 Wilk K.E., Reinold M.M. Closed kinetic chain exercises and plyometric activities. In: Bandy W.D., Sanders B., editors. Therapeutic Exercise: Techniques for Intervention. Baltimore: Lippincott Williams & Wilkins; 2001:179-211.
69 Steinkamp L.A., Dillingham M.F., Markel M.D., et al. Biomechanical considerations in patellofemoral joint rehabilitation. Am. J. Sports Med.. 1993;21:438-444.
70 Escamilla R.F., Fleisig G.S., Zheng N., et al. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med. Sci. Sports Exerc.. 1998;30:556-569.
71 Escamilla R.F., Zheng N., MacLeod T.D., et al. Patellofemoral compressive force and stress during the forward and side lunges with and without a stride. Clin. Biomech. (Bristol, Avon). 2008;23:1026-1037.
72 Escamilla R.F., Zheng N., MacLeod T.D., et al. Patellofemoral joint force and stress between a short- and long-step forward lunge. J. Orthop. Sports Phys Ther.. 2008;38:681-690.
73 Grood E.S., Suntay W.J., Noyes F.R., Butler D.L. Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. J. Bone Joint Surg. Am.. 1984;66:725-734.
74 Witvrouw E., Lysens R., Bellemans J., et al Open versus closed kinetic chain exercises for patellofemoral pain A prospective, randomized study. Am. J. Sports Med. 28 2000 687-694