CHAPTER 1 Functional Anatomy of the Shoulder Complex
The glenohumeral joint is the most complex joint in the human body. The glenohumeral joint combined with the scapulothoracic, sternoclavicular, and acromioclavicular joints comprise the shoulder joint complex. All these joints are critical to normal pain-free function. The glenohumeral joint has the greatest amount of motion of any joint in the human body.
The overall function of the upper extremity is related to the shoulder complex, with the ultimate purpose of this mechanism being the placement and full use of the hand. The joint mechanisms of the limb permit the placement, functioning, and control of the hand directly in front of the body, where the functions can be observed.1 Manipulation of the hand is controlled by the shoulder complex, which positions and directs the humerus, the elbow, which positions the hand in relation to the trunk, and the radioulnar joints, which determine the position of the palm.2,3 Sports that involve actions such as throwing, using a racket, and swimming require excessive glenohumeral joint motion. For example, the excessive motion required to throw a baseball is accomplished through the integrated and synchronized motion of the various joints in the upper quadrant, most significantly the glenohumeral and scapulothoracic joints.
The shoulder complex provides the upper limb with a range of motion exceeding that of any other joint mechanism.4 This range of motion is greater than that required for most daily functional activities. For example, use of the hand in limited activities of daily living is possible when the shoulder complex is immobilized with the humerus held by the side. Compensation for absent shoulder motion is provided by the cervical spine, elbow, wrist, and finger joint mechanisms.5,6
The shoulder complex consists of four joints that function in a precise, coordinated, synchronous manner. Position changes of the arm involve movements of the clavicle, scapula, and humerus. These movements are the direct result of the complex mechanism comprised of the sternoclavicular, acromioclavicular, and glenohumeral joints and the scapulothoracic gliding mechanism.4,7,8
COMPONENTS
Sternoclavicular Joint
The sternoclavicular joint is the only joint connecting the shoulder complex to the axial skeleton.9,10 Although the structure of this synovial joint is classified as plain, its function most closely resembles a ball-and-socket articulation.4,11,12 The articular surfaces lack congruity. Approximately one half of the large, rounded medial end of the clavicle protrudes above the shallow sternal socket. An intra-articular disc is attached to the upper portion of this nonarticular segment of the clavicle. The articular surface is saddle-shaped, anteroposteriorly concave, and downwardly convex.2,4
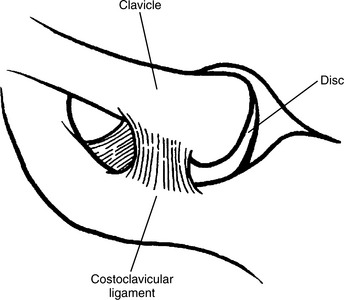
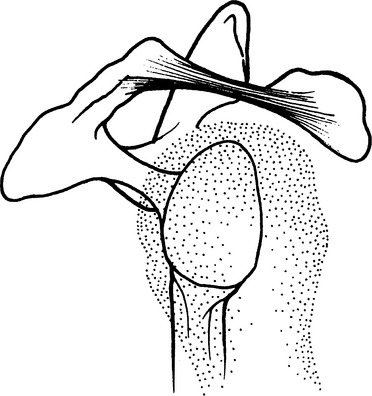
The medial end of the clavicle is bound to the sternum, the first rib and its costal cartilage. Ligaments strengthen the capsule anteriorly, posteriorly, superiorly, and inferiorly. The main structures stabilizing the joint, resisting the tendency for medial displacement of the clavicle and limiting clavicular movement, are the articular disc and the costoclavicular ligament (Fig. 1-1).4,13
The articular disc is a strong, almost circular fibrocartilage that completely divides the joint cavity.14 The disc is attached superiorly to the upper medial end of the clavicle and passes downward between the articular surfaces to the sternum and first costal cartilage.4 This arrangement permits the disc to function as a hinge, a mechanism that contributes to the total range of joint movement. The areas of compression between the articular surfaces and intra-articular disc vary with movements of the clavicle. During elevation and depression, most motion occurs between the clavicle and articular disc (Fig. 1-2A and B). During protrusion and retraction, the greatest movement occurs between the articular disc and sternal articular surface (see Fig. 1-2C and D).2 The combination of taut ligaments, pressure on the disc and articular surfaces is important for maintaining stability in the plane of motion.
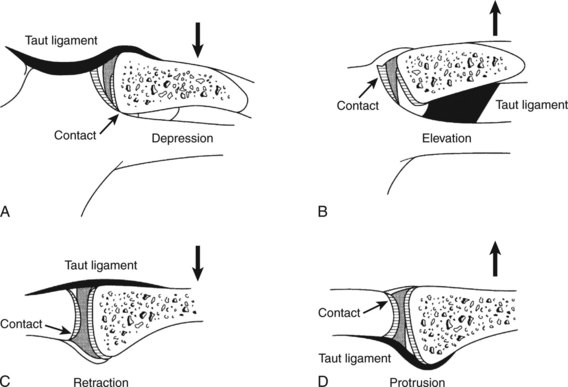
Figure 1-2 Sternoclavicular joint illustrating compression of articular disc. A, Depression. B, Elevation. C, Retraction. D, Protrusion.
(From Dempster WT: Mechanisms of shoulder movement. Arch Phys Med Rehabil 46:49, 1965.)
The articular disc also stabilizes the joint against forces applied to the shoulder, which are transmitted medially through the clavicle to the sternum. Without this attachment, the clavicle would tend to override the sternum, resulting in medial dislocation. Forces acting on the clavicle are most likely to cause fractures of the bone medial to the attachment of the coracoclavicular ligament but rarely cause dislocation of the sternoclavicular joint.5
The costoclavicular ligament is a strong bilaminar structure attached to the inferior surface of the medial end of the clavicle and first rib. The anterior component of the ligament passes upward and laterally; the posterior aspect upward and medially. The ligament is a major stabilizing structure and strongly binds the medial end of the clavicle to the first rib. The ligament becomes taut when the arm is elevated or the shoulder protracted.4
The joint capsule is supported by oblique anterior and posterior sternoclavicular ligaments. Both ligaments pass downward and medially from the sternal end of the clavicle to the anterior and posterior surfaces of the manubrium and limit anteroposterior movement of the clavicle. An interclavicular ligament runs across the superior aspect of the sternoclavicular joint, joining the medial ends of the clavicles. This ligament, with deep fibers attached to the upper margin of the manubrium, provides stability to the superior aspect of the joint.4,9
The sternoclavicular joint allows elevation and depression, protraction and retraction, and long-axis rotation of the clavicle. The axis for both angular movements lies close to the clavicular attachment of the costoclavicular ligament.9
Acromioclavicular Joint
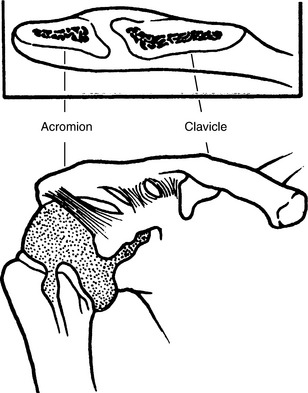
The acromioclavicular joint is a synovial plane joint between the small, convex, oval facet on the lateral end of the clavicle and a concave area on the anterior part of the medial border of the acromion process of the scapula.4,9
The joint line is oblique and slightly curved. The curvature of the joint permits the acromion, and thus the scapula, to glide forward or backward over the lateral end of the clavicle. This movement keeps the glenoid fossa continually facing the humeral head. The oblique nature of the joint is such that forces transmitted through the arm will tend to drive the acromion process under the lateral end of the clavicle, with the clavicle overriding the acromion (Fig. 1-3). The joint also contains a fibrocartilaginous disc that is variable in size and does not completely separate the joint into two compartments.9,14 The acromioclavicular joint is important because it contributes to total arm movement in addition to transmitting forces between the clavicle and acromion.4,15
The acromioclavicular joint has a capsule and superior acromioclavicular ligament that strengthen the upper aspect of the joint.4,11 The main ligamentous structure stabilizing the joint and binding the clavicle to the scapula is the coracoclavicular ligament. Although this ligament is placed medially and is separate from the joint, it forms the most efficient means of preventing the clavicle from losing contact with the acromion.4,5,8,9,15,16
The coracoclavicular ligament consists of two parts, the trapezoid and the conoid. These two components, functionally and anatomically distinct, are united at their corresponding borders. Anteriorly, the space between the ligaments is filled with adipose tissue and, frequently, a bursa. A bursa also lies between the medial end of the coracoid process and the inferior surface of the clavicle. In up to 30% of subjects, these bony components may be opposed closely and may form a coracoclavicular joint.2,16 The coracoclavicular ligament suspends the scapula from the clavicle and transmits the force of the upper fibers of the trapezius to the scapula.2
The trapezoid ligament, the anterolateral component of the coracoclavicular ligament, is broad, thin, and quadrilateral. It is attached from below to the superior surface of the coracoid process. The ligament passes laterally almost horizontally in the frontal plane and is attached to the trapezoid line on the inferior surface of the clavicle.4,9 The primary function of this ligament is to prevent overriding of the clavicle on the acromion.5,17
The conoid ligament is located partly posteriorly and medially to the trapezoid ligament. It is thick and triangular, with its base attached from above to the conoid tubercle on the inferior surface of the clavicle. The apex, which is directed downward, is attached to the “knuckle” of the coracoid process (i.e., medial and posterior edge of the root of the process). The conoid ligament is oriented vertically and twisted on itself.4,17 The ligament limits upward movement of the clavicle on the acromion. When the arm is elevated, the rotation of the scapula causes the coracoid process to move and increases the distance between the clavicle and coracoid process. This movement increases the tension on the conoid ligament, resulting in dorsal (posterior) axial rotation of the clavicle. Viewed from above, the clavicle has a shape resembling a crank. The taut coracoclavicular ligament acts on the outer curvature of the cranklike clavicle and effects a rotation of the clavicle on its long axis.11,18 This clavicular rotation allows the scapula to continue to rotate and increase the degree of arm elevation. During full elevation of the arm, the clavicle rotates 50 degrees axially.11 When the clavicle is prevented from rotating, the arm can be abducted actively to only 120 degrees.4,8
Movement of the acromioclavicular joint is an important component of total arm movement. A principal role of the joint in the elevation of the arm is to permit continued lateral rotation of the scapula after about 100 degrees of abduction when sternoclavicular movement is restrained by the sternoclavicular joint ligaments. The acromioclavicular joint has three degrees of freedom. Movement can occur between the acromion and lateral end of the clavicle about a vertical axis, around a frontal axis, or about a sagittal axis. Functionally, the two main movements at the acromioclavicular joint, however, are a gliding movement as the shoulder joint flexes and extends and an elevation and depression movement to conform with changes in the relation between the scapula and humerus during abduction.5,9,16
Glenohumeral Joint
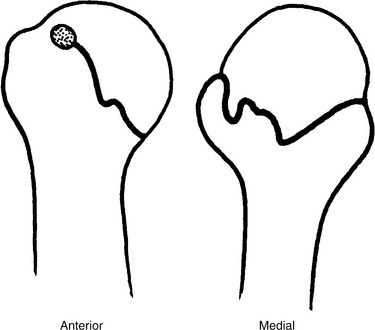
The glenohumeral joint is a multiaxial ball-and-socket synovial joint. This type of joint geometry permits a tremendous amount of motion; however, the inherent stability is minimal (Fig. 1-4). The articular surfaces, head of the humerus, and glenoid fossa of the scapula, although reciprocally curved, are oval and are not sections of true spheres.4 Because the head of the humerus is larger than the glenoid fossa, only part of the humeral head can be in articulation with the glenoid fossa in any position of the joint. At any given time, only 25% to 30% of the humeral head is in contact with the glenoid fossa.19-21 The surfaces are not congruent, and the joint is loose-packed. Full congruence and the close-packed position are obtained when the humerus is in full elevation.22,23

Figure 1-4 Osseous structure of the glenohumeral joint. The large convex humeral head is in a relatively small glenoid fossa.
The design characteristics of the joint are typical of an incongruous joint. The surfaces are asymmetrical, the joint has a movable axis of rotation, and muscles related to the joint are essential in maintaining stability of the articulation (Box 1-1).9 The humeral articular surface has a radius of curvature of 35 to 55 mm. The humeral head and neck make an angle of 130 to 150 degrees with the shaft and are retroverted about 20 to 30 degrees with respect to the transverse axis of the elbow.24,25
The topic of retroversion has received increased attention because of the implications of its effect on glenohumeral joint motion. Nowhere is this point more evident than with the overhead athlete, who exhibits excessive external rotation and a limitation of internal rotation. Crockett and colleagues26 have studied professional baseball pitchers and noted a bilateral difference in humeral retroversion. The investigators noted a 17-degree difference, with the throwing shoulder exhibiting greater external rotation and loss of internal rotation. This difference was not observed in the control group of non–overhead throwing athletes. Other investigators have also reported bilateral differences in retroversion in overhead athletes, in whom the throwing side exhibits greater retroversion.27-29
The glenoid fossa is somewhat pear-shaped and resembles an inverted comma (Fig. 1-5). The surface area is 25% to 33%, the vertical diameter 75%, and the transverse diameter 55% of that of the humeral head.25 In 75% of subjects, the glenoid fossa is retroverted an average of 7.4 degrees in relation to the plane of the scapula.30,31 Furthermore, the glenoid fossa has a slight upward tilt of about 5 degrees in reference to the medial border of the scapula32; we refer to this as the inclination angle. It has been suggested that this relation is important in maintaining horizontal stability of the joint and counteracting any tendency toward anterior displacement of the humeral head.25,30,31 However, this concept has not been supported by subsequent studies.33,34 The articular cartilage lining the glenoid fossa is thickest in the periphery and thinnest in the central region.
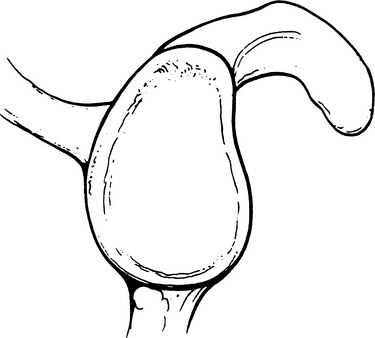
Figure 1-5 Lateral view of the glenoid fossa. Note the pear-shaped appearance and similarity to an inverted comma.
Because of the amount of pathology involving the acromion and head of the humerus, the acromion has been studied extensively. Bigliani and Morrison35 have classified the shapes of the acromion into three categories. Type I acromions are those with a flat undersurface and have the lowest risk for impingement syndrome and its sequelae. Type II acromions have a curved undersurface and type III acromions have a hooked undersurface (Fig. 1-6). Type III has the highest correlation with impingement syndromes, rotator cuff pathologies or both. Nicholson and associates36 have reported that the shape of the acromion is congenital and does not develop over time. The acromions have epiphysis and occasionally may not fuse, leading to acromion deformity, often referred to as os acromiale.37
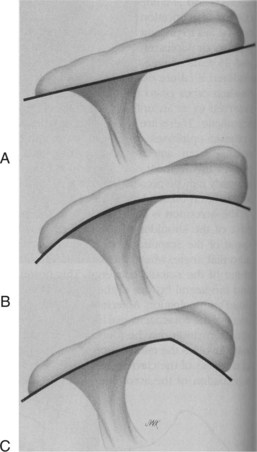
Figure 1-6 Acromial shapes. A, Type 1, flat acromion. B, Type II, curved acromion. C, Type III, hooked acromion.
The resting position of the scapula in reference to the trunk is anteriorly rotated about 30 to 40 degrees,21,38 with respect to the frontal plane as viewed from above. This has been referred to as the scapular plane. The scapula is also rotated upward about 3 degrees and tilted forward approximately 20 degrees.38,39
Glenoid Labrum
The glenoid labrum consists of fibrocartilage and fibrous tissue.4,40 This rim of fibrocartilaginous tissue attaches around the margin of the glenoid fossa.40 The inner surface of the labrum is covered with synovium; the outer surface attaches to the capsule and is continuous with the periosteum of the scapular neck. The shape of the labrum adapts to accommodate rotation of the humeral head, adding flexibility to the edges of the glenoid fossa. The tendons of the long head of the biceps brachii muscle contribute to the structure and reinforcement of the labrum. The long head of the biceps brachii attaches to the superior region of the labrum. The width and thickness of the glenoid labrum vary. The anterior labrum appears thicker and at times larger than the posterior labrum.
It has been suggested40 that the labrum protects the edges of the glenoid, assists in lubrication of the joint, and deepens the glenoid cavity, thus contributing to stability of the joint.4,5,9,41 Others have stated that the labrum does not increase the depth of the concave surface substantially, and that the glenoid labrum is no more than a fold of capsule composed of dense fibrous connective tissue that stretches out anteriorly with external rotation and posteriorly with internal rotation of the humerus.40 The main function of the labrum may be to serve as an attachment for the glenohumeral ligaments.4,40 When that attachment is compromised, it represents a Bankart lesion, in which the capsular-labral complex is detached from the glenoid rim (Fig. 1.7; see Fig. 1-6).
Capsule
The capsule surrounds the joint and is attached medially to the margin of the glenoid fossa beyond the labrum. Laterally, it is attached to the circumference of the anatomic neck, and the attachment descends about ½ inch onto the shaft of the humerus. The capsule is loose-fitting, allowing the joint surfaces to be separated 2 to 3 mm by a distractive force.4 Matsen and colleagues42 have shown 22 mm of inferior, 6 mm anterior, and 7 mm posterior translation in normal subjects.
The capsule is relatively thin and, by itself, would contribute little to the stability of the joint. The integrity of the capsule and maintenance of the normal glenohumeral relationship depend on the reinforcement of the capsule by ligaments and attachment of the muscle tendons of the rotator cuff mechanism.4,9,16
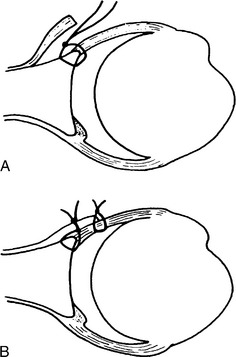
The superior part of the capsule, together with the superior glenohumeral ligament, is important in strengthening the superior aspect of the joint and resisting the effect of gravity on the dependent limb.4,43 Anteriorly, the capsule is strengthened by the anterior glenohumeral ligaments and attachment of the subscapularis tendon (Fig. 1.8).44 Posteriorly, the capsule is strengthened by the attachment of the teres minor and infraspinatus tendons.45 Inferiorly, the capsule is relatively thin and weak and contributes little to the stability of the joint. The inferior part of the capsule is subjected to considerable strain because it is stretched tightly across the head of the humerus when the arm is elevated.
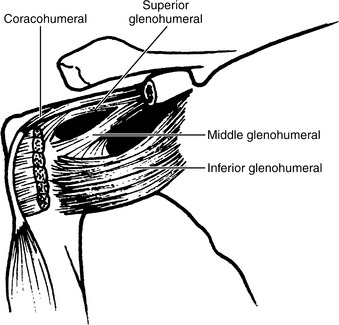
Figure 1-8 Coracohumeral and glenohumeral ligaments. Note the deficiencies between the glenohumeral ligaments and the Z arrangement of the three components of the ligament.
The inferior part of the capsule, the weakest area, is lax and lies in folds when the arm is adducted. Kaltsas46 has compared the collagen structure of the shoulder joint capsule with that of the elbow and hip. When the joint capsules were subjected to a mechanical force, the shoulder joint capsule showed a greater capacity to stretch than to rupture. When the capsule was tested to failure, the structure ruptured anteroinferiorly.46,47 Also, Reeves47 has demonstrated that the force required to cause glenohumeral joint dislocation is less in those younger than 20 years and greater in those older than 50 years.
O’Brien and coworkers48 have described the glenohumeral capsule and its ligamentous structures and noted that the anterior capsule is comprised of three ligamentous portions—the superior glenohumeral ligament (SGHL), middle glenohumeral ligament (MGHL), and inferior glenohumeral ligament complex (IGHLC) (Fig. 1-9). The IGHLC is comprised of the anterior band (AB), posterior band (PB), and axillary pouch (AP). The study noted that during abduction and external rotation, the anterior band acts as a hammock, resulting in anterior displacement of the humerus (see Fig. 1-9). Conversely, with abduction internal rotation, the posterior band functions as a ligamentous restraint to posterior displacement. The axillary pouch functions as a redundancy to the capsule, allowing excessive mobility. Fealy and colleagues49 have examined the glenohumeral joint in 51 fetal shoulders ranging from 9 to 40 weeks of gestation. The authors noted distinct capsules with ligaments present, especially a prominent inferior glenohumeral ligament complex. A coracohumeral ligament and rotator cuff interval were also present.
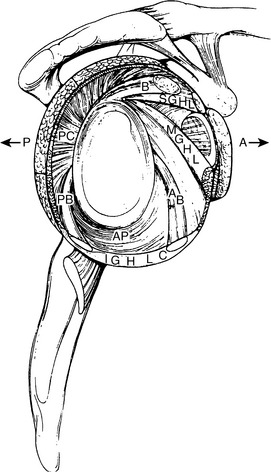
Figure 1-9 Glenohumeral joint capsule. Note the superior glenohumeral ligament (SGHL), middle glenohumeral ligament (MGHL), and inferior glenohumeral ligament complex (IGHLC). AB anterior band; AP, axillary pouch; PB posterior band.
Johnston23 has stated that, with the arm by the side, the capsular fibers are oriented with a forward and medial twist. This twist increases in abduction and decreases in flexion. The capsular tension in abduction compresses the humeral head into the glenoid fossa. As abduction progresses, the capsular tension exerts an external rotation moment. This external rotation untwists the capsule and allows further abduction. The external rotation of the humerus that occurs during coronal plane abduction may therefore be assisted by the configuration of the joint capsule.23
The capsule is lined by a synovial membrane attached to the glenoid rim and anatomic neck inside the capsular attachments.4 The tendon of the long head of the biceps brachii muscle passes from the supraglenoid tubercle over the superior aspect of the head of the humerus and lies within the capsule, emerging from the joint at the intertubercular groove (Fig. 1-10). The tendon is covered by a synovial sheath to facilitate movement of the tendon within the joint. The structure is susceptible to injury at the point at which the tendon arches over the humeral head, and the surface on which it glides changes from bony cortex to articular cartilage.5
Coracohumeral Ligament
The coracohumeral ligament is an important ligamentous structure in the shoulder complex.43 The ligament is attached to the base and lateral border of the coracoid process and passes obliquely downward and laterally to the humerus, blending with the supraspinatus muscle and the capsule. Laterally, the ligament separates into two components that insert into the greater and lesser tuberosities, creating a tunnel through which the biceps tendon passes.50 Inferiorly, the coracohumeral ligament blends with the superior glenohumeral ligament. The anterior border of the ligament is distinct medially and merges with the capsule laterally. The posterior border is indistinct and blends with the capsule.4,9
It has been suggested that the downward pull of gravity on an adducted arm is counteracted largely by the superior capsule, coracohumeral ligament, and inferior glenohumeral ligament (Table 1-1).50,51 As the arm is abducted, the restraining force is shifted to the inferior structures and the primary restraining force is the inferior glenohumeral ligament.52 Because the coracohumeral ligament is located anteriorly to the vertical axis about which the humerus rotates axially, the ligament checks lateral rotation during arm elevation between 0 and 60 degrees. When the humerus, in a position of neutral rotation, is elevated in the sagittal plane, the movement is limited to approximately 75 degrees by the coracohumeral ligament. For elevation to continue, the humerus is medially rotated and moves toward the scapular plane by the dynamic tension in this ligament.22
TABLE 1-1 Stability of the Glenohumeral Joint
| Position | Structure |
|---|---|
| Dependent | |
| Elevation (degrees) | |
| Lower range (0-45) | |
| Middle range (45-75) | |
| Upper range (>75) | Inferior glenohumeral ligament (anterior band; axillary pouch) |
| Throughout elevation | Dynamic activity of rotator cuff |
Glenohumeral Ligaments
The three glenohumeral ligaments lie on the anterior and inferior aspect of the joint. They are described as being thickened parts of the capsule.4 The superior glenohumeral ligament passes laterally from the superior glenoid tubercle, upper part of the glenoid labrum, and base of the coracoid process to the humerus, between the upper part of the lesser tuberosity and anatomic neck.50,51 The ligament lies anterior to and partly under the coracohumeral ligament. The superior glenohumeral ligament, together with the superior joint capsule and rotator cuff muscles, assist in preventing downward displacement of the humeral head.51,53
The middle glenohumeral ligament has a wide attachment, extending from the superior glenohumeral ligament along the anterior margin of the glenoid fossa down as far as the junction of the middle and inferior thirds of the glenoid rim.51 From this attachment, the ligament passes laterally, gradually enlarges, and attaches to the anterior aspect of the anatomic neck and lesser tuberosity of the humerus. The ligament lies under the tendon of the subscapularis muscle and is intimately attached to it.25,50 Note the large variation in size of the middle glenohumeral ligament; it can be 2 cm wide but is absent in some individuals. This structure exhibits the greatest amount of structural variation. The middle glenohumeral ligament and subscapularis tendon limit lateral rotation from 45 to 75 degrees of abduction and are important anterior stabilizers of the glenohumeral joint, particularly effective in the lower to middle ranges of abduction (see Table 1-1).
The inferior glenohumeral ligament is the thickest of the glenohumeral structures and is the most important stabilizing structure of the shoulder in the overhead athlete. The ligament attaches to the anterior, inferior, and posterior margins of the glenoid labrum and passes laterally to the inferior aspects of the anatomic and surgical necks of the humerus.4,25 The ligament can be divided into three distinct portions—the anterior band, axillary pouch, and posterior band (see Fig. 1-9).48 The inferior part is thinner and broader and is termed the axillary pouch. The anterior band strengthens the capsule anteriorly and supports the joint most effectively in the upper ranges (more than 75 degrees) of abduction.48 The anterior band of the inferior glenohumeral ligament provides a broad buttresslike support for the anterior and inferior aspects of the joint, preventing subluxation in the upper part of the range (see Table 1-1).51
O’Brien and associates48 have demonstrated that with the arm abducted to 90 degrees and externally rotated, the anterior band of the inferior glenohumeral ligament complex wraps around the humeral head like a hammock to prevent anterior humeral head migration. This structure provides stability during the throwing motion, tennis serve motion, freestyle stroke, or any overhead arm position.
Tightening of the inferior glenohumeral ligament during coronal plane abduction limits elevation to an average of 90 degrees. To continue to elevate, the humerus must move toward the scapular plane and laterally rotate. Gagey and coworkers22 have stated that both movements occur because of dynamic tension in the inferior glenohumeral ligament.
The coracohumeral and glenohumeral ligaments viewed from the front form a Z pattern. This arrangement creates potential areas of capsular weakness above and below the middle glenohumeral ligament. The subscapularis bursa communicates with the joint cavity through the superior opening, or foramen of Weitbrecht, between the superior and middle glenohumeral ligaments. Ferrari50 has also reported the presence of an inferior subscapular bursa, between the middle and inferior glenohumeral ligaments. This bursa was present in all 14 specimens in those younger than 55 years and could be seen up to the age of 75 years. When the middle glenohumeral ligament is attenuated or absent, this anterior defect is enhanced and may contribute to anterior instability of the joint.50
Inside the glenohumeral joint capsule is negative pressure in comparison with outside the joint capsule. This is referred to as negative intra-articular pressure and provides a stabilizing effect on the shoulder joint.54 Wulker and colleagues55 have demonstrated that venting the capsule (creating a cut into the capsule, thus eliminating the negative intra-articular pressure) may increase translation of the humerus on the glenoid by 19% to 50%.
Rotator Cuff: Dynamic Stability
The rotator cuff is the musculotendinous complex formed by the attachment to the capsule of the supraspinatus muscle superiorly, the subscapularis muscle anteriorly, and the teres minor and infraspinatus muscles posteriorly. These tendons blend intricately with the fibrous capsule and the adjacent rotator cuff tendon.56 They provide active support for the joint and can be considered true dynamic ligaments that provide dynamic stability.8 The capsule is less well protected inferiorly because the tendon of the long head of the triceps brachii muscle is separated from the capsule by the axillary nerve and posterior circumflex humeral artery.4
The rotator cuff tendons insert into a large contact point onto the greater and lesser tuberosities of the humerus and not a small insertion point, as was once thought. Dugas and associates57 have reported that the rotator cuff inserts less than 1 mm from the articular margin. Curtis and coworkers58 later reported that the insertional anatomy in cadaveric shoulders exhibits a consistent pattern and noted interdigitation of the muscles, particularly between the supraspinatus and infraspinatus. The average insertional lengths and widths for the rotator cuff muscles were as follows: supraspinatus 23 × 16 mm, subscapularis 40 × 20 mm, infraspinatus 29 × 19 mm, and teres minor 29 × 11 mm. Bassett and colleagues59 have studied the cross-sectional area of the rotator cuff muscles as they cross the glenohumeral joint capsule (Table 1-2); they found that the larger the cross-sectional area, the more significant the contribution to shoulder stability. Miller and associates60 have described a space between the supraspinatus and infraspinatus and referred to this area as the posterior rotator cuff interval. They went on to discuss the importance of releasing this area when rotator cuff repairs are performed in specific types of patients who exhibit supraspinatus retraction and scarring.
TABLE 1-2 Cross-Sectional Area of Rotator Cuff Muscles Crossing the Glenohumeral (GH) Joint Capsule
| Muscle | Area (cm2) | Contribution of Muscle Crossing GH Joint (%) |
|---|---|---|
| Biceps (LH) | 2.01 | 2 |
| Biceps (SH) | 1.11 | 2 |
| Deltoid | 18.2 | 17.7 |
| Deltoid (posterior) | 5.0 | 5 |
| Infraspinatus and teres minor | 13.7 | 13 |
| Latissimus dorsi | 12.0 | 11.7 |
| Pectoralis major | 13.3 | 13 |
| Subscapularis | 16.3 | 16 |
| Supraspinatus | 5.7 | 5.6 |
| Teres major | 8.77 | 8.5 |
| Triceps | 3.0 | 3.8 |
From Bassett R, Browne A, Morrey BF, et al: Glenohumeral muscle force and moment mechanics in a position of shoulder instability. J Biomech 23:405, 1990.
It is generally accepted that the deltoid and the rotator cuff muscles are prime movers of glenohumeral abduction.61-63 These muscles have been found to contribute equally to torque production in functional planes of motion.63 With the arm at the side, the directional force of the deltoid muscle is almost vertical.25,64 Thus, most of the deltoid force will cause a superior shear force of the humeral head that, if unopposed, would cause the humeral head to contact the coracoacromial arch, resulting in impingement of soft tissues.65 The force vectors of the infraspinatus, subscapularis, and teres minor muscles are such that each tends to have a compressive component as well as a rotational force.39,65 Each muscle’s compressive force offsets the superior shear force of the deltoid.39 The infraspinatus, teres minor, and subscapularis thus form a force coupled with the deltoid and act to stabilize the humeral head on the glenoid fossa, allowing the deltoid and supraspinatus to act as abductors of the humerus.66 We often refer to the rotator cuff muscles as the compressive cuff. In studies on a mechanical model, Comtet and coworkers61 have determined that the depressor forces are at their maximum between 60 and 80 degrees of elevation and disappear beyond 120 degrees. The supraspinatus has a small superior shear component, but its main function is compression because of the horizontal orientation of the muscle fibers39; thus, it opposes the upward superior shear action of the deltoid.
Lesions of the rotator cuff mechanism can occur as a response to repetitious activity over time or to overload activity that causes a spontaneous lesion.67 Stress applied to a previously degenerated rotator cuff may cause the cuff to rupture. Often, this stress also tears the articular capsule, resulting in a communication between the joint cavity and subacromial bursa. Rotator cuff tears result in considerably reduced force of elevation of the glenohumeral joint. In attempting to elevate the arm, the patient shrugs the shoulder. If the arm is abducted passively to 90 degrees, the patient should be able to maintain the arm in the abducted position.9
The space between the supraspinatus and superior border of subscapularis has been termed the rotator interval. This space is triangular, with its base located medially at the coracoid process. The rotator interval contains the coracohumeral ligament, superior glenohumeral ligament, glenohumeral capsule, and biceps tendon.68-72 The medial aspect consists of two layers and the lateral portion is composed of four layers. The superficial layer of the medial rotator interval is comprised of the coracohumeral ligament and the deep layer consists of the superior glenohumeral ligament and joint capsule. The coracohumeral ligament also represents the superficial layer of the lateral portion of the rotator interval. The second layer is composed of the fibers of the supraspinatus and subscapularis. The third layer consists of the deep fibers of the coracohumeral ligament and the fourth layer is the superior glenohumeral ligament and lateral capsule.68,69 The size of the rotator cuff interval varies. The larger the interval, the greater the inferior and posterior laxity.72
The function of the long head of the biceps is controversial. Some believe that it contributes to the stability of the glenohumeral joint by preventing upward migration of the head of the humerus during powerful elbow flexion and forearm supination. Lesions of the long head of the biceps, therefore, may produce instability and shoulder dysfunction.73 Conversely, other physicians74-76 have reported performing biceps tenotomy in patients with refractory biceps pain. Once the biceps was released, pain was eliminated in over 70% of patients and no functional limitations, instability, or weakness were reported. Thus, the function of the proximal long head of the biceps brachii is still being debated.
The scapula plays a vital role in normal shoulder function. Normal scapulothoracic joint motion and rhythm are critical to pain-free normal shoulder function. Numerous muscles about the scapula play a critical role in accomplishing this function. The trapezius muscle is the largest and most superficial scapulothoracic muscle. This muscle originates from the spinous processes of the C7 through T12 vertebrae. The muscle is classified into upper, middle, and lower fibers. Insertion of the upper fibers is over the distal third of the clavicle. The lower cervical and upper thorax fibers insert over the acromion and spine of the scapula. The lower portion of the trapezius inserts into the base of the spine of the scapula. The rhomboids function similarly as the midportion of the trapezius.77 The origin of the rhomboids is from the lower ligamentum nuchae, C7 and T1 for the rhomboid minor and T2 through T5 for the rhomboid major. The rhomboid minor inserts onto the posterior portion of the medial base of the spine of the scapula. The rhomboid major inserts onto the medial border of the scapula. The levator scapulae muscle proceeds from its origin on the transverse processes from C1 through C3 (and sometimes C4) and inserts onto the superior angle of the scapula. The serratus anterior takes its origin from the ribs on the lateral wall of the thoracic cage. The serratus has three divisions, upper, middle and lower. The upper fibers originate from ribs 1 and 2, the middle fibers from ribs 2 through 4, and the lower from ribs 5 through 9. The serratus anterior muscle orientation is in individual slips from each rib. The serratus inserts onto the superior angle, medial border, and inferior angle of the scapula, respectively. The pectoralis minor runs from the second through fifth ribs upward to the medial base of coracoid. Somewhat frequently, approximately 15% incidence, there will be an aberrant slip from the pectoralis minor to the humerus, glenoid, clavicle, or scapula.78,79 The subclavius muscle is a small muscle that originates from the first rib and inserts as a muscle onto the inferior surface of the medial third of the clavicle. This muscle stabilizes the sternoclavicular joint.
Coracoacromial Arch
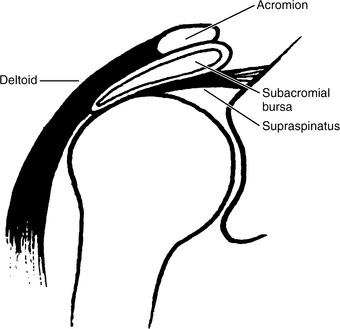
The coracoacromial ligament is triangular with the base attached to the lateral border of the coracoid process (Fig. 1-11). The ligament passes upward, laterally, and slightly posteriorly to the superior aspect of the acromion process.4,80 Superiorly, the ligament is covered by the deltoid muscle. Posteriorly, the ligament is continuous with the fascia that covers the supraspinatus muscle. Anteriorly, the coracoacromial ligament has a sharp, well-defined, free border. Together with the acromion and the coracoid processes, the ligament forms an important protective arch over the glenohumeral joint.9 The arch forms a secondary restraining socket for the humeral head, protecting the joint from trauma from above and preventing upward dislocation of the humeral head. The supraspinatus muscle passes under the coracoacromial arch, lies between the deltoid muscle and the capsule of the glenohumeral joint, and blends with the capsule. The supraspinatus tendon is separated from the arch by the subacromial bursa (see Fig. 1-11).9 The space between the inferior acromion and head of the humerus (subacromial distance) has been measured on radiographs and is used as an indicator of proximal humeral subluxation.81,82 The distance was found to be between 9 and 10 mm in 175 asymptomatic shoulders and was greater in men than in women.81 A distance of less than 6 mm was considered pathologic and was thought to be indicative of supraspinatus tendon attenuation or rupture.81
During elevation, with internal rotation of the arm in abduction and flexion, the greater tuberosity (the supraspinatus tendon) of the humerus may apply pressure against the anterior edge and inferior surface of the anterior third of the acromion and coracoacromial ligament. This is in part because of the anterior orientation of the supraspinatus tendon. In some cases, the impingement also may occur against the acromioclavicular (AC) joint. This often occurs when the AC joint exhibits degenerative joint disease or spurring, or both. Most upper extremity functions are performed with the hand placed in front of the body, not lateral to it. When the arm is raised forward in flexion, the supraspinatus tendon passes under the anterior edge of the acromion and acromioclavicular joint. For this movement, the critical area for wear is centered on the supraspinatus tendon and also may involve the long head of the biceps brachii muscle.
Flatow and colleagues83 have examined the concept of impingement, compression between the supraspinatus and acromion. The investigators measured the distance between the undersurface of the acromion and humeral head at various degrees of abduction. At 0 degrees adduction (arm at the side), the acromiohumeral space was approximately 11 mm, at 90 degrees of abduction it was 5.7 mm, and at 120 degrees of abduction less than 5 mm (4.8 mm). Furthermore, the investigators placed Fuji contact film, which measures pressure per square area, on the acromion and humeral head. They found that with arm abduction from 60 degrees to full elevation, there was contact between the acromion and humeral head. Therefore, Flatow and associates83 have reported that contact between the humeral head and acromion is normal.
Bursae
Several bursae are found in the shoulder region.4 Two bursae particularly important to the clinician are the subacromial and subscapular bursae.15 Other bursae located in relation to the glenohumeral joint structures are between the infraspinatus muscle and capsule, on the superior surface of the acromion, between the coracoid process and capsule, under the coracobrachialis muscle, between the teres major and long head of the triceps brachii muscles, and in front of and behind the tendon of the latissimus dorsi muscle. Because bursae are located where motion is required between adjacent structures, they have a major function in the shoulder mechanism. The subacromial bursa (Fig. 1-12) is located between the deltoid muscle and capsule, extending under the acromion and coracoacromial ligament and between them and the supraspinatus muscle. The bursa adheres to the coracoacromial ligament and to the acromion above and rotator cuff below. The bursa does not frequently communicate with the joint; however, a communication may develop if the rotator cuff is ruptured.80 The subacromial bursa is important for allowing gliding between the acromion and deltoid muscle and rotator cuff. It also reduces friction on the supraspinatus tendon as it passes under the coracoacromial arch.9,80 Often, with repetitive overhead motion, the bursae may become inflamed and thickened, which may decrease the critical space in the subacromial region.
The subscapular bursa lies between the subscapularis tendon and neck of the scapula. It protects this tendon where it passes under the base of the coracoid process and over the neck of the scapula. The bursa communicates with the joint cavity between the superior and middle glenohumeral ligaments9,51 and often between the middle and inferior glenohumeral ligaments.40,50
Vascular Supply
The rotator cuff is a frequent site of pathologic conditions, usually degenerative and often in response to fatigue stress.17 Because degeneration may occur even with normal activity levels, the nutritional status of the glenohumeral structures is of great importance. The blood supply to the rotator cuff comes from the posterior humeral circumflex and suprascapular arteries.4 These arteries supply principally the infraspinatus and teres minor muscle areas of the cuff. The anterior aspect of the capsular ligamentous cuff is supplied by the anterior humeral circumflex artery and occasionally by the thoracoacromial, suprahumeral, and subscapular arteries. Superiorly, the supraspinatus muscle is supplied by the thoracoacromial artery. The supraspinatus tendon has a region of relative avascularity 1 cm proximal to the humeral insertion, often including its insertion into the humerus.84,85 Rothman and Parke85 have reported hypovascularity in the tendon in 63% of 72 shoulders studied. In a study by Rathbun and MacNab,84 an avascular area was found in all specimens and was unrelated to age. Abduction of the arm resulted in relaxation of the tension on the supraspinatus muscle and complete filling of vessels throughout the tendon. In addition, with increasing age, the area of avascularity also increases67; thus, the potential for healing decreases with age. The other cuff tendons generally demonstrate good vascularity, except for an occasional zone of hypovascularity in the superior portion of the insertion of the infraspinatus tendon.84,85
Articular Neurology
Innervation of the shoulder region is derived from C5, C6, and C7; C4 also may add a minor contribution. The nerves supplying the ligaments, capsule, and synovial membrane are axillary, suprascapular, subscapular, and musculocutaneous nerves. Branches from the posterior cord of the brachial plexus also may supply the joint structures.
Occasionally, the shoulder may receive a greater supply from the axillary nerve than from the musculocutaneous nerve; the reverse may also be true. The complex overlapping innervation pattern makes denervation of the joint difficult. The nerve supply follows the small blood vessels into periarticular structures.4,5
The skin on the anterior region of the shoulder complex is supplied by the supraclavicular nerves from C3 and C4 and by the terminal branches of the sensory component of the axillary nerve. The articular structures on the anterior aspect of the glenohumeral joint are supplied by the axillary nerve and, to a lesser degree, by the suprascapular nerves. The subscapular nerve and posterior cord of the brachial plexus may also innervate the anterior aspect of the joint after piercing the subscapularis muscle.4,5,9
The supraclavicular nerves supply the skin on the superior and upper posterior aspects of the shoulder region. The lower, posterior, and lateral aspects of the shoulder are supplied by the posterior branch of the axillary nerve.
The periarticular structures on the superior aspect of the joint obtain part of their innervation from the suprascapular nerve. The axillary and musculocutaneous nerves and the lateral pectoral nerve may also contribute to the innervation of the superior aspect of the joint. Posteriorly, the main nerve supply is from the suprascapular nerve, which supplies the proximal part of the joint, and the axillary nerve, which supplies the distal region.3-59
The acromioclavicular joint is innervated by the lateral supraclavicular nerve from the cervical plexus (C4) and by the lateral pectoral and suprascapular nerves from the brachial plexus (C5 and C6). The sternoclavicular joint is innervated by branches from the medial supraclavicular nerve from the cervical plexus (C3 and C4) and subclavian nerve from the brachial plexus (C5 and C6).4,9
SUMMARY
The shoulder complex is more mobile than any other joint mechanism of the body because of the combined movement at the glenohumeral and scapulothoracic articulations. This wide range of motion permits positioning of the hand in space, allowing performance of numerous gross and skilled functions. Shoulder complex stability is also required during dynamic activity, particularly when the distal extremity encounters resistance. The glenohumeral joint is inherently unstable because of the shallowness of the glenoid fossa as well as the disproportionate size and lack of congruency between the articular surfaces. During dynamic activities, stabilization of the humeral head on the glenoid fossa depends on an intact capsule and glenohumeral ligaments, as well as on coordinated and synchronous activity in the deltoid and rotator cuff muscles. Injury or disease of any of these structures can lead to instability and impingement of subacromial structures, resulting in pain and dysfunction in the shoulder region.
1 Kelley DL. Kinesiological Fundamentals of Motion Description. Englewood Cliffs, NJ: Prentice-Hall, 1971.
2 Dempster WT. Mechanisms of shoulder movement. Arch Phys Med Rehabil. 1965;46:49.
3 DePalma AF. Surgery of the Shoulder, 2nd ed. Philadelphia: JB Lippincott, 1973.
4 Warwick R, Williams P, editors. Gray’s Anatomy, 35th ed., London: Longman, 1973.
5 Bateman JE. The Shoulder and Neck. Philadelphia: WB Saunders, 1971.
6 Brantigan OC. Clinical Anatomy. New York: McGraw-Hill, 1963.
7 Bechtol CO. Biomechanics of the shoulder. Clin Orthop. 1980;146:37.
8 Inman VT, Saunders JB, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg. 1944;26:1.
9 Moore KL. Clinically Oriented Anatomy. Baltimore: Williams & Wilkins, 1980.
10 Perry J. Normal upper extremity kinesiology. Phys Ther. 1978;58:265.
11 Abbott LC, Lucas DB. The function of the clavicle: Its surgical significance. Ann Surg. 1954;140:583.
12 Ljungren AE. Clavicular function. Acta Orthop Scand. 1979;50:261.
13 Bearn JG. Direct observations on the function of the capsule of the sternoclavicular joint in clavicular support. J Anat. 1967;101:159.
14 Moseley HF. The clavicle: Its anatomy and function. Clin Orthop. 1968;58:17.
15 Kent BE. Functional anatomy of the shoulder complex. Phys Ther. 1971;51:867.
16 Frankel VH, Nordin M. Basic Biomechanics of the Skeletal System. Philadelphia: Lea & Febiger, 1980.
17 Kessler RM, Hertling D. Management of Common Musculoskeletal Disorders: Physical Therapy Principles and Methods. New York: Harper & Row, 1983.
18 Dvir Z, Berme N. The shoulder complex in elevation of the arm: Mechanism approach. J Biomech. 1978;11:219.
19 Bost FC, Inman VTG. The pathological changes in recurrent dislocations of the shoulder. J Bone Joint Surg. 1942;24:595.
20 Codman EA. The Shoulder. Boston: Thomas Todd, 1934.
21 Steindler A. Kinesiology of Human Body Under Normal and Pathological Conditions. Springfield, Ill: Charles C Thomas, 1955.
22 Gagey O, Bonfait H, Gillot C, et al. Anatomic basis of ligamentous control of elevation of the shoulder (reference position of the shoulder joint). Surg Radiol Anat. 1987;9:19.
23 Johnston TB. The movements of the shoulder-joint: A plea for the use of the “plane of the scapula” as the plane of reference for movements occurring at the humeroscapular joint. Br J Surg. 1937;25:252.
24 Norkin C, Levangie P. Joint Structure and Function: A Comprehensive Analysis. Philadelphia: FA Davis, 1983.
25 Sarrafian SK. Gross and functional anatomy of the shoulder. Clin Orthop. 1983;173:11.
26 Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20.
27 Reagan KM, Meister K, Horodyski MB, et al. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30:354.
28 Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball players. Am J Sports Med. 2002;3:347.
29 Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26:247-253.
30 Saha AK. Dynamic stability of the glenohumeral joint. Acta Orthop Scand. 1971;42:491.
31 Saha AK. Mechanics of elevation of glenohumeral joint: Its application in rehabilitation of flail shoulder in upper brachial plexus injuries and poliomyelitis and in replacement of the upper humerus by prosthesis. Acta Orthop Scand. 1973;44:668.
32 Basmajian JV, Bazant FJ. Factors preventing downward dislocation of the adducted shoulder joint. J Bone Joint Surg Am. 1959;4:1182.
33 Cyprien JM, Vasey HM, Burdet A, et al. Humeral retrotorsion and glenohumeral relationship in the normal shoulder and in recurrent anterior dislocation (scapulometry). Clin Orthop. 1983;175:8.
34 Randelli M, Gambrioli PL. Glenohumeral osteometry by computed tomography in normal and unstable shoulders. Clin Orthop. 1986;208:151.
35 Bigliani LU, Morrison DS, April EW. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:228.
36 Nicholson GP, Goodman DA, Flatow EL. The cromion: Morphologic condition and and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1.
37 Lieberson F. Os acromiale’a contested anomaly. J Bone Joint Surg. 1937;19:683.
38 Laumann U. Kinesiology of the Shoulder Joint. In: Kolbel R, editor. Shoulder Replacement. Berlin: Springer-Verlag, 1987.
39 Morrey BF, An KN. Biomechanics of the shoulder. In: Rockwood CA, Matsen FA, editors. The Shoulder. Philadelphia: WB Saunders; 1990:235.
40 Moseley HF, Overgaard B. The anterior capsular mechanism in recurrent anterior dislocation of the shoulder: Morphological and clinical studies with special reference to the glenoid labrum and the gleno-humeral ligaments. J Bone Joint Surg Br. 1962;44:913.
41 Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med. 1983;2:247.
42 Matsen FA, Harryman DT, Didles JA. Mechanics of glenohumeral instability. In: Hawkins RJ, editor. Clinics in Sports Medicine: Basic Science and Clinical Application in the Athlete’s Shoulder. Philadelphia: WB Saunders, 1991.
43 Basmajian JV, Bazant FJ. Factors preventing downward dislocation of the adducted shoulder joint. J Bone Joint Surg Am. 1959;41:1182.
44 Ovesen J, Nielsen S. Anterior and posterior shoulder instability: A cadaver study. Acta Orthop Scand. 1986;57:324.
45 Ovesen J, Nielsen S. Posterior instability of the shoulder: A cadaver study. Acta Orthop Scand. 1986;57:436.
46 Kaltsas DS. Comparative study of the properties of the shoulder joint capsule with those of other joint capsules. Clin Orthop. 1983;173:20.
47 Reeves B. Experiments on the tensile strength of the anterior capsular structures of the shoulder in man. J Bone Joint Surg Br. 1968;50:858.
48 O’Brien SJ, Neeves MC, Arnoczky SN, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:451.
49 Fealy S, Dodeo SA, Dicarlo EF, O’Brien SJ. The developmental anatomy of the glenohumeral joint. J Shoulder Elbow Surg. 2000;9:217.
50 Ferrari DA. Capsular ligaments of the shoulder: Anatomical and functional study of the anterior superior capsule. Am J Sports Med. 1990;18:20.
51 Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208.
52 Bowen MK, Warren RF. Ligamentous control of shoulder stability based on selective cutting and static translation experiments. Clin Sports Med. 1991;10:757.
53 Schwartz E, Warren RF, O’Brien SJ, et al. Posterior shoulder instability. Orthop Clin North Am. 1987;18:409.
54 Hurchler C, Wulker N, Mendilia M. The effect of negative intraarticular pressure and rotator cuff force on glenohumeral translation during simulated active elevation. Clin Biomech. 2000;15:306.
55 Wulker N, Rossig S, Korell M, Thren K, Dynamic stability of the glenohumeral joint. A biomechanical study. Sportverletz Sportschaden. 1995;9:1.
56 Clark JM, Harryman DT2nd. Tendons, ligamentous and capsule of the rotator cuff. J Bone Joint Surg Am. 1992;74:713.
57 Dugas JR, Campbell DA, Warren RF, et al. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg. 2002;11:98.
58 Curtis AS, Burbank KM, Tierney JJ, et al. The insertional footprint of the rotator cuff: An anatomic study. Arthroscopy. 2006;22:609.
59 Bassett R, Browne A, Morrey BF, et al. Glenohumeral muscle force and moment mechanics in a position of shoulder instability. J Biomech. 1990;23:405.
60 Miller SL, Gladstone JN, Cleeman E, et al. Anatomy of the posterior rotator interval: Implications for cuff mobilization. Clin Orthop Relat Res. 2003;408:152.
61 Comtet JJ, Herberg G, Naasan IA. Biomechanical basis of transfers for shoulder paralysis. Hand Clin. 1989;5:1.
62 deLuca CJ, Forrest WJ. Force analysis of individual muscles acting simultaneously on the shoulder joint during isometric abduction. J Biomech. 1973;6:385.
63 Howell SM, Imobersteg AM, Seger DH, Marone PJ. Clarification of the role of the supraspinatus muscle in shoulder function. J Bone Joint Surg Am. 1986;68:398.
64 Lucas DB. Biomechanics of the shoulder joint. Arch Surg. 1973;107:425.
65 Poppen NK, Walker PS. Forces at the glenohumeral joint in abduction. Clin Orthop. 1978;135:165.
66 Saha AK. Mechanism of shoulder movements and a plea for the recognition of “zero position” of the glenohumeral joint. Clin Orthop. 1983;173:3.
67 Brewer BJ. Aging of the rotator cuff. Am J Sports Med. 1979;7:102.
68 Hunt SA, Kwon YW, Zuckerman JD. The rotator interval: Anatomy, pathology, and strategies for treatment. J Am Acad Orthop Surg. 2007;15:4.
69 Jost B, Koch PP, Gerber C. Anatomy and functional aspects of the rotator interval. J Shoulder Elbow Surg. 2000;9:336.
70 Nobuhara K, Ikeda H. Rotator interval lesion. Clin Orthop. 1987;223:44.
71 Fitzpatrick MJ, Powell SE, Tibone JE, Warren RF. The anatomy, pathology, and definitive treatment of rotator interval lesions: Current concepts. Arthroscopy. 2003;19:70.
72 Harryman DT, Sidles JA, Harris SL, Matsen FA. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53.
73 Kumar VP, Satku K, Balasubramaniam P. The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop. 1989;244:172.
74 Kelly Am, Drakos MC, Fealy S, et al. Arthroscopic release of the long head of the biceps tendon: Functional outcome and clinical results. Am J Sports Med. 2005;33:208.
75 Walch G, Edwards TB, Boulahia A, et al. Arhtroscopic tentomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238.
76 Boileau P, Baque F, Valerio L, et al. Isolated arthroscopic biceps tentomy or tendodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747.
77 Inman VT, Saunders JB, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg. 1944;26:1.
78 Lambert AE. A rare variation in the pectoralis minor muscle. Anat Rec. 1925;31:193.
79 Vare AM, Indurak GM. Some anomalous findings in the axillary muscles. J Anat Soc India. 1965;14:34.
80 Rothman RH, Marvel JP, Heppenstall RB. Anatomic considerations in the glenohumeral joint. Orthop Clin North Am. 1975;6:341.
81 Petersson CJ, Redlund-Johnell I. The subacromial space in normal shoulder radiographs. Acta Orthop Scand. 1984;55:57.
82 Weiner DS, MacNab I. Superior migration of the humeral head: A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1970;52:524.
83 Flatow EL, Soslowsky LJ, Tcker JB, et al. Excursion of the rotator cuff under the acromion. Patterns of subacromial contact. Am J Sports Med. 1994;22:779.
84 Rathbun JB, MacNab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg Br. 1970;52:540.
85 Rothman RH, Parke WW. The vascular anatomy of the rotator cuff. Clin Orthop. 1965;41:176.
Hawkins RJ, Abrams JS. Impingement syndrome in the absence of rotator cuff tear (states 1 and 2). Orthop Clin North Am. 1987;18:373.
Neer CS. Impingement lesions. Clin Orthop. 1983;173:70.
Neviaser TJ. The role of the biceps tendon in the impingement syndrome. Orthop Clin North Am. 1987;18:383.
Ovesen J, Nielsen S. Stability of the shoulder joint: Cadaver study of stabilizing structures. Acta Orthop Scand. 1985;56:149.
Porterfield JA, DeRosa C. Musculature of the shoulder complex. In: Porterfield JA, DeRosa C, editors. Mechanical Shoulder Disorders. Philadelphia: WB Saunders; 2004:47.
Post M, Cohen J. Impingement syndrome: A review of late stage II and early stage III lesions. Clin Orthop. 1986;207:126.
Watson MS. Classification of the painful arc syndromes. In: Bayley JI, Kessel L, editors. Shoulder Surgery. New York: Springer-Verlag, 1982.