CHAPTER 2 Clinical Biomechanics of the Shoulder Complex
Shoulder function is the result of the complex interplay of the muscular, osseous, and supporting structures of the shoulder girdle. The lower extremity and trunk initiate and accumulate forces expressed at the shoulder and distal upper extremity. Ultimately, the shoulder positions the hand for precise movements necessary for activities of daily living and athletic performance.
The articulations of the shoulder complex provide the shoulder with a range of motion that far exceeds that of any other joint. This movement is dependent on controlled and synchronous motion of all joints of the shoulder.1
RESTING POSITION
Ideally, the shoulder girdle musculature should be well balanced with respect to muscle strength and length to allow proper osseous orientation for optimal upper extremity function. Shoulder girdle suspension is reliant on the sternoclavicular ligaments,2 upper trapezius,3,4 levator scapulae, sternocleidomastoid, fascia,5 and atmospheric pressure.
The resting position of the shoulder girdle also depends on thoracic spine alignment and muscular linkages from the thoracic and cervical spine to the shoulder’s bony components.6,7 Shoulder girdle resting position is highly variable, depending on postural habits, hand dominance, occupation, muscle tone, and age.8 For example, the dominant shoulder of a competitive baseball pitcher tends to exhibit increased anterior tilt, depression, and abduction of the scapula compared with the nondominant side. The repetitive throwing cycle may result in abnormal and pathologic alterations. Burkhart and colleagues9 have described the asymmetrical malposition of the scapula in the throwing athletes as the SICK scapula (scapular malposition, inferior medial border prominence, coracoid pain and malposition, and dyskinesis of scapular movement). Altered scapular position may produce scapular dyskinesis dynamically in the throwing cycle, affecting glenohumeral and acromioclavicular joint kinematics. This syndrome often manifests itself with pain and impaired throwing accuracy and velocity, along with altered scapular kinematics.10
PLANES OF MOTION
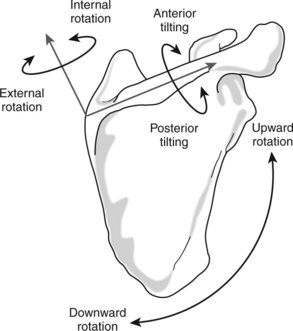
Motion of the shoulder complex is described in relation to the cardinal planes—sagittal, coronal, and horizontal (Fig. 2-1). Shoulder flexion and extension occur in the sagittal plane, abduction and adduction in the coronal plane, and horizontal abduction and adduction in the horizontal plane. Internal and external rotation occur through the long axis of the humerus, affording a high degree of mobility in an infinite number of planes. This is typically assessed at 90 degrees of coronal plane abduction or with the arm at the side.
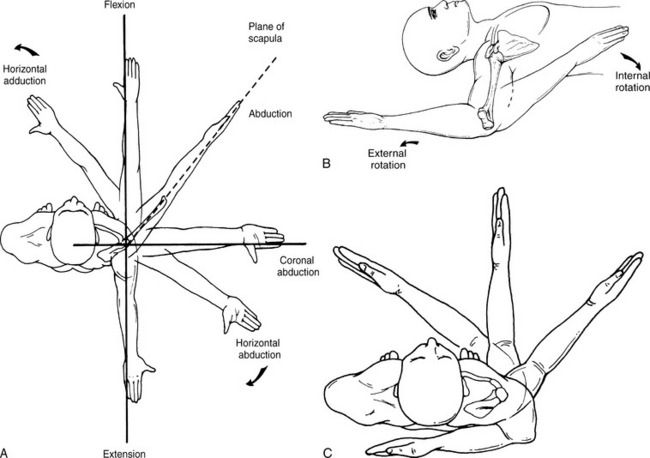
Figure 2-1 Motion of the shoulder complex. A, Planes of motion (superior view). B, Humeral external and internal rotation at 90 degrees of coronal plane abduction. C, Pure glenohumeral rotation at neutral and functional internal rotation.
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 68.)
The American Academy of Orthopaedic Surgeons (AAOS) no longer differentiates the plane of motion in which the arm is brought overhead; instead, they have adopted the term elevation.8 For the purposes of this chapter, shoulder elevation will be used to describe the flexion or abduction of the shoulder complex in the plane of the scapula or cardinal planes. Flexion and abduction will be specifically designated where applicable.
Plane Of The Scapula
In the resting position, the concave ventral surface of the scapula floats on the convex posterior thoracic wall, thus directing the glenoid fossa anteriorly approximately 30 to 45 degrees anterior to the coronal plane. This is referred to as the plane of the scapula (Fig. 2-2).11-13 The scapula has a slight anterior tilt in the sagittal plane,14 and the glenoid fossa exhibits a slight upward inclination in the resting position.15,16
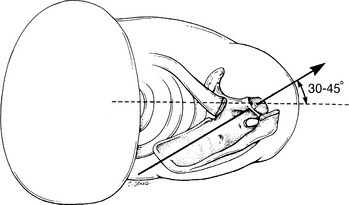
Figure 2-2 Scapular orientation in the plane of the scapula.
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 65.)
Motion in the scapular plane is actually arm movement relative to the scapula as opposed to the trunk. This suggests that the plane of the scapula is not truly fixed, because the scapula translates forward during elevation.4
There are several unique biomechanical and anatomic features of scapular plane elevation:81
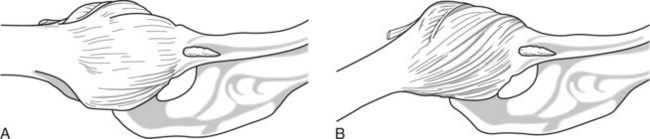
Figure 2-3 Inferior view of the glenohumeral joint and capsuloligamentous complex. A, Scapular plane abduction. B, Coronal plane abduction.
(From Johnston TB: The movements of the shoulder joint. A plea for the use of the “Plane of the Scapula” as the plane of reference in movements occurring at the humero-scapular joint. Br J Surg 25:252, 1937.)
These characteristics, specific to the scapular plane, can greatly enhance shoulder rehabilitation. By performing strengthening exercise in the plane of the scapula, rotator cuff muscle strength can be optimized whereas unwanted passive tension on the rotator cuff tendons and capsuloligamentous complex (CLC) can be minimized. In the athlete with shoulder instability, the clinician can strengthen and perform range-of-motion exercises in the scapular plane, reducing potential anterior and posterior translation by eliminating stress on the deficient static restraints.
OSTEOKINEMATICS AND ARTHROKINEMATICS
Scapulothoracic Joint
Scapulothoracic joint function enhances arm-trunk motion and glenohumeral stability as the scapula orients the glenoid to the humeral head. It also serves as a protective mechanism, because the joint and surrounding musculature absorb energy with a fall onto an outstretched arm.8 Kibler10 has described five distinct roles of the scapula: (1) it represents a stable part of the glenohumeral articulation; (2) allows for retraction and protraction along the thoracic wall; (3) elevates the acromion to decrease impingement and coracoacromial arch compression in the throwing and serving motion; (4) serves as a base for muscle attachment; and (5) functions as a link in the proximal to distal sequencing of the kinetic chain. The failure of the scapula to perform these roles causes inefficient physiology and biomechanics, and therefore, inefficient shoulder function.10
The scapula is suspended on the axial skeleton by the sternoclavicular ligaments, indirectly through the clavicle,2 descending axioscapular muscles,3,5 coracoclavicular ligaments, atmospheric pressure,4 and fascia.5 Glenohumeral joint stability is maximized as the glenoid adjusts to support the humeral head.19 At rest, the scapula is positioned in the scapular plane. Scapular movement is primarily mediated by the oblique axioscapular muscles. The scapulothoracic joint is described with five degrees of freedom, three rotations and two translations (Fig. 2-4).20
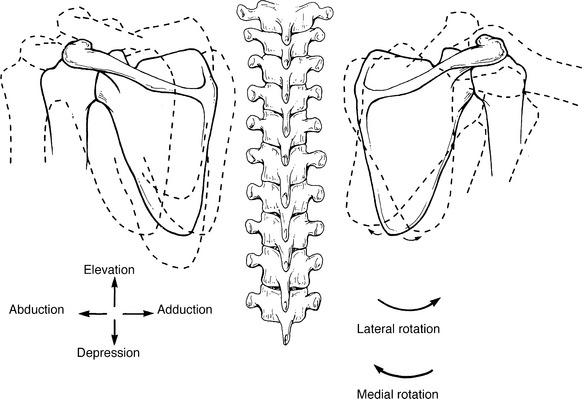
Figure 2-4 Motions of the scapulothoracic joint.
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 75.)
Elevation and Depression
Although gliding occurs between the scapula and thorax, the true fulcrum for motion is the sternoclavicular joint.8 Scapular elevation, movement of the scapula superiorly on the thorax (see Fig. 2-4),21 occurs primarily from activation of the upper trapezius4 and levator scapulae22; the rhomboid elevates with retraction.
Depression is movement of the scapula inferiorly on the thorax, and occurs in conjunction with scapular anterior or posterior tilting (see Fig. 2-4). Contraction of the pectoralis minor and serratus anterior causes depression and anterior tilting (protraction), whereas depression and posterior tilting are mediated by the lower trapezius.8 When a patient assumes the prone position, the shoulder girdle falls into a relatively elevated and protracted state. This is why muscle testing of the middle and lower trapezius requires manual setting of the scapula into an anatomic position.
Abduction and Adduction
Abduction is the movement of the medial border of the scapula away from the vertebral column (see Fig. 2-4).21 This motion is powered by the serratus anterior and pectoralis minor.3 The pectoralis major contributes to abduction by pulling on the fixed humerus, which then moves the scapula.8
Adduction is defined as movement of the medial border of the scapula toward the vertebral column (see Fig. 2-4).21 The rhomboids,22 middle trapezius,3 and lower trapezius23 are responsible for adduction.24 The levator scapulae are inactive unless elevation occurs.
Posterior and Anterior Tilt
Posterior and anterior tilt is scapular rotation about an oblique medial-lateral axis.25 Posterior tilt occurs as the acromion moves backward and anterior tilt occurs as the acromion moves forward (Fig. 2-5).
Internal and External Rotation
Internal and external rotation are described as scapular rotation about an oblique superior-inferior axis.25 External rotation can be visualized as the acromion moving posteriorly with the medial border of the scapula moving in an anterior direction; internal rotation can be visualized as the acromion moves anteriorly while the medial border moves posteriorly (see Fig. 2-5).
Downward (Medial) and Upward (Lateral) Rotation
Scapular downward and upward rotation occurs about an axis in the scapular body.25 Downward rotation is defined by rotation of both the glenoid downward and the inferior angle of the scapula toward the spine (see Fig. 2-4). This is mediated by the rhomboids, levator scapulae, and pectoralis minor.4
Upward rotation is the rotation of the glenoid superiorly and movement of the inferior angle away from the spine. This motion is considered critical to shoulder performance. The scapula’s axis of rotation has been found to be slightly inferior to the scapular spine, approximately equidistant from the axillary and vertebral borders.26
A number of investigations have used three-dimensional techniques to quantify scapular movement relative to the thorax.27-32 McClure and associates31 have reported a mean ratio of glenohumeral to scapulothoracic motion of 1.7:1 in eight healthy shoulders in vivo using bone pin insertion directly into the scapula. During scapular plane elevation, the scapula was found to rotate upwardly (mean 50 degrees), rotate externally (mean 24 degrees), and tilt posteriorly (mean 30 degrees), whereas the clavicle elevated (mean 10 degrees) and retracted (mean 21 degrees). It was also found that scapular upward rotation and clavicular rotation occur approximately linearly throughout humeral elevation, especially beyond 50 degrees of elevation. Posterior tilting and external rotation motions were nonlinear, with the majority of these motions not occurring until after 90 degrees of arm elevation. Ebaugh and coworkers33 have reported that beyond 90 degrees elevation, the scapula moves into an anterior tilt, with external rotation motion having reached a plateau. These findings are similar to those of Ludewig, Lukasiewicz, Ebaugh, and their colleagues.29,30,33,34
Clinical assessment of scapular rotation during arm elevation should be examined as this is essential for normal shoulder function. The scapula should begin to migrate into lateral rotation by 60 degrees of elevation.8 If delayed, abnormal scapulohumeral rhythm may exist, possibly resulting in rotator cuff and bursa impingement because the glenoid and acromion have not begun their superior travel as the greater tuberosity approaches.
Scapulohumeral Rhythm
Proper scapular motion and stability are considered to be crucial to normal function of the shoulder31; therefore, scapulohumeral rhythm is an essential concept in the understanding of shoulder function. This phenomenon describes the relationship of motion between the scapula and humerus; however, the sternoclavicular and acromioclavicular joints also influence scapulohumeral rhythm.
With active humeral elevation up to 30 degrees in the coronal or scapular abduction planes and up to 60 degrees of sagittal plane flexion, the scapula seeks a position of stability. This initial phase, called the setting phase, is variable and individualized.35 The scapula continues to rotate laterally around 60 degrees elevation,17 stabilizing against the thoracic wall with little superior or inferior migration. During the first 90 degrees of motion, significant superior acromioclavicular joint migration occurs, corresponding to the clavicular elevation. At approximately 100 degrees of elevation, the coracoclavicular ligament begins to tighten, pulling on the posterior lip of the clavicle and producing clavicular upward rotation.36 The scapula continues to rotate, causing the center of rotation to shift toward the glenoid, resulting in medial and continued superior movement of the glenoid and lateral migration of the scapular inferior angle.16 Along with lateral rotation, the scapula orients the glenoid fossa anteriorly toward the sagittal plane.8 The scapula posteriorly tilts as the superior angle moves away from the thoracic wall with concomitant movement of the inferior angle toward the thoracic wall. Ten more degrees of acromioclavicular contribution occur after 135 degrees. In all, the scapula rotates approximately 60 degrees.3,14
Following the initial phase, the humerus and scapula maintain a particular relationship during arm elevation, described as a ratio of movement. This ratio has been investigated and quantified radiographically, goniometrically, and through the use of three-dimensional techniques.
The classic work by Inman and colleagues35 has found a 2:1 ratio during both sagittal plane flexion and coronal plane abduction between 30 and 170 degrees of motion. Other studies have examined elevation of the glenohumeral joint in the scapular plane. Saha13 has reported a ratio of 2.3:1, similar to the findings by Inman and associates. Freedman and Munro15 have observed a 3:2 ratio from 0 to 135 degrees, with a decreased scapulothoracic contribution from 135 degrees to maximum elevation. Doody and coworkers14 have goniometrically determined a 1.74:1 ratio from 0 to 180 degrees, with varied inputs from the scapulothoracic and glenohumeral joints at different stages; the former contributes more during the middle phases of abduction (90 to 140 degrees). Poppen and Walker16 have discovered a 4.3:1 ratio from 0 to 30 degrees, followed by a 1.25:1 or 5:4 ratio from 30 to 180 degrees of elevation. McClure and colleagues31 have reported a mean ratio of glenohumeral-to-scapulothoracic motion of 1.7:1 in eight healthy shoulders in vivo using bone pin insertion directly into the scapula.
McQuade and Smidt32 have demonstrated that during dynamic humeral elevation, the scapulohumeral rhythm changes, depending on the phase of elevation and amount of external load on the arm. For unloaded elevation, the scapulohumeral rhythm ranges from 7.9:1 to 2.9:1, for light load elevation, 3.1:1 to 4.3:1; and for heavy load elevation, 1.9:1 to 4.5:1. Graichen and associates37 have noted a ratio of 1.5:1 at 60 degrees to 2.4:1 at 120 degrees for passive scapular plane abduction, using open magnetic resonance imaging and three-dimensional image processing. Passive elevation follows a pattern similar to that of active elevation, except that the scapula tends to move into a position of internal rotation,33 with less upward rotation early and more upward rotation in the last two phases.32
Borstad and Ludewig27 have examined the effect of eccentric versus concentric control on three-dimensional scapular kinematics. They found a decrease in scapular anterior tilt and increase in scapular internal rotation during the eccentric phase of arm elevation at 80, 100, and 120 degrees. No significant difference was noted in scapular position with eccentric and concentric trials for any scapular variable below 80 degrees. Overhead shoulder function, especially eccentric lowering, may alter scapular kinematics and predispose athletes to injury. Throwing athletes demonstrate increased scapular upward rotation, internal rotation, and retraction.38 This adaptation may allow for clearance of the subacromial space and improve throwing performance.
The results for scapulohumeral rhythm vary somewhat because of the type of measurement technique used (Table 2-1). However, the relationship between glenohumeral and scapulothoracic motion is critical and is generally considered to be 2:1, culminating in 120 and 60 degrees, respectively. Caution is required when comparing passive and active glenohumeral-to-scapulothoracic ratios and their phases of contribution.8 During passive motion, the muscles that drive the scapula are inactive; thus, initiation of scapular movement will lag compared with active motion, being dependent on the glenohumeral capsuloligamentous structure’s elasticity and expansion. This explains why during passive movement, scapular motion may not be detected until 70 to 90 degrees. Viewed another way, scapular upward rotation is partly related to tension developed in the CLC during elevation. Patients with hyperelastic tissue or instability probably demonstrate less upward scapular rotation during active elevation because there is more “play” in the CLC. The scapula will move earlier with movement of the humerus if adhesions exist in the capsuloligamentous complex. Therefore, passive rather than active assessment of scapulohumeral rhythm tends to be more sensitive in determining restrictions of the capsuloligamentous complex.
TABLE 2-1 Comparison of Ratios of Active Glenohumeral to Scapulothoracic Rhythm in the Plane of Scapula
| Study, Year | Ratio (Average) |
|---|---|
| Inman et al, 194435 | 2:1 |
| Saha, 196113 | 2.3:1 |
| Freedman and Munro, 196615 | 3:2 |
| Doody et al, 197014 | 1.74:1 |
| Poppen and Walker, 197616 | 1.25:1 or 5:4 |
| McClure et al, 200131 | 1.7:1 |
| Graichen et al, 200037 | 1.5:1 to 2.4:1 |
| McQuade and Smidt, 199832 | 7.9:1 to 2.1:1 (passive range of motion); 1.9:1 to 4.5:1 (with load) |
Effect of Shoulder Pathology on Shoulder Rhythm.
Quantitative scapular kinematics studies have shown abnormal scapular motion associated with certain pathologies.39,40 Unfortunately, the equipment used to attain these measurements is not clinically applicable. The clinician is left with visual inspection and linear measurements that have low reliability.41 Active movement assessment of the shoulder complex is necessary to determine whether a dysfunctional scapulohumeral rhythm exists, because this is often associated with muscular weakness or abnormal activation patterns.8 Dramatic or subtle scapular dyskinesia may be visualized on active arm elevation in the sagittal plane, possibly indicating a nerve palsy, instability, or motor dyskinesia (Fig. 2-6). Weakness of the rotator cuff muscles typically results in compensation by the patient shrugging or excessive scapular elevation. Pain or contracture of the glenohumeral capsuloligamentous complex will manifest during active arm motion by increased scapular elevation and lateral rotation.

Figure 2-6 Patient with a long thoracic nerve palsy. Note the prominence of the medial border of the scapula, with active elevation of the right shoulder.
Shoulder pathology has been demonstrated to have an adverse effect on scapulothoracic rhythm. Paletta and coworkers,39 using a two-plane radiograph series, found that subjects with shoulder instability and subjects with a rotator cuff tear demonstrate altered glenohumeral-scapulothoracic motion relationships. Mell and colleagues42 have reported that shoulder kinematics are altered in subjects with a rotator cuff tear. The scapula was found to elevate more for the same amount of humeral elevation than in normal shoulders or shoulders with tendonopathy. The presence of this kinematic alteration in cuff tear patients and not in tendinosis patients suggests that it is related to loss of cuff strength and function rather than pain.
In shoulders with known instability, Von Eisenhart-Rothe and colleagues43 have demonstrated an increase in scapular internal rotation in the transverse plane and a malcentering of the humeral head in the direction of the instability. Their study suggested that scapular positioning is relevant for humeral head decentering and should be considered in the treatment of different forms of atraumatic shoulder instability.
Lukasiewicz and associates30 have reported that subjects with impingement syndrome demonstrate significantly less posterior tilt, greater superior translation at the horizontal, and maximal elevation when compared with nonimpaired individuals. Ludewig and Cook34 have demonstrated decreased posterior tilt, external rotation, and upward rotation in subjects with impingement. The presence of posterior tilting may be important functionally to allow for clearance of the humeral head and rotator cuff tendons under the anterior aspect of the acromion during elevation.31 Limited scapular posterior tilt could result from a shortened pectoralis minor, restricted scapular mobility, and inadequate shoulder complex muscle activity. Altered kinematics may result as patients tend to rotate the scapula to a greater degree to avoid impingement and reduce the requirement for elevation at the glenohumeral joint.42
Effect of Posture on Shoulder Rhythm.
Scapulohumeral rhythm and strength may also be influenced by postural changes and adaptively shortened muscular structures. Increased thoracic kyphosis may lead to a decrease in posterior tilt and lateral scapular rotation with humeral elevation.44 Smith and coworkers45 have found a reduction in isometric shoulder strength in protracted and retracted scapular positions when compared with neutral, suggesting compromised shoulder muscle function and deviation from normal resting scapular position.
During active arm elevation, the pectoralis minor becomes passively lengthened by scapular upward rotation, external rotation, and posterior tilting.31,34 Individuals with a shortened pectoralis minor exhibited decreased scapular upward rotation, external rotation, and posterior tilting during elevation.46 The finding of a short pectoralis minor muscle suggests an increased risk for impingement in this population and may contribute to altered mechanics in throwers.9
Deviating patterns of external rotation or the inability to rotate the humerus externally change the scapulohumeral rhythm substantially.47 Anterior tightening procedures, such as the Putti-Platt or Magnuson-Stack procedure or a tight Bankart repair, are likely to result in a loss of external rotation and elevation.48 Athletes with limited external rotation range of motion tend to exhibit an altered scapulohumeral rhythm, which may affect throwing performance and overhead function. Excessive restriction of external rotation caused by an overtightened anterior-inferior CLC increases posterior translation, exacerbating wear on the posterior glenoid and ultimately leading to the long-term complication of secondary osteoarthritis.48-50
Sternoclavicular Joint
The sternoclavicular joint represents the single bony articulation between the axial skeleton and upper extremity. This is a monumental responsibility, particularly because the amount of articular contact is the least of all the major joints in the body.51
The sternoclavicular joint serves as the pivot point for scapular elevation-depression and abduction-adduction. Clavicular elevation and depression occur through an axis in the sagittal plane. The sternoclavicular joint is reported to allow for 45 to 60 degrees of elevation and 5 degrees of depression.14,52 Elevation is limited by tension on the costoclavicular ligament.2,4,51,53,54 Depression of the sternoclavicular joint is limited by the superior joint capsule and interclavicular ligament, and contact between the clavicle and first rib.21 Although only 5 degrees of active depression is available, greater excursion results, particularly when the clavicular suspensory muscles are lacking.
Clavicular protraction and retraction occur through an axis in the transverse plane,4 allowing approximately 15 degrees of motion in each direction.52 Because the axis is oblique, retraction is accompanied by elevation and protraction is combined with depression.2 Protraction is limited by the posterior fibers of the costoclavicular ligament, posterior sternoclavicular capsule, and posterior fibers of the interclavicular ligament.51,55 Retraction is restricted by the anterior costoclavicular fibers and anterior sternoclavicular capsule (Fig. 2-7). Rotation occurs through the longitudinal axis of the clavicle. During flexion and abduction, Inman and colleagues35 have demonstrated approximately 40 degrees of upward rotation, as defined by the direction of the anterior edge of the clavicle. The upward rotation motion begins at approximately 90 degrees of elevation, and becomes increasingly greater at the end range. Tension of the coracoclavicular ligaments regulates this upward rotation. As the scapula moves into elevation, the base of the coracoid process, which is the insertion of the coracoclavicular ligaments, begins to move distally. This produces a downward pull on the posterior clavicle, thus causing upward rotation. Approximately 10 degrees of downward rotation are available.
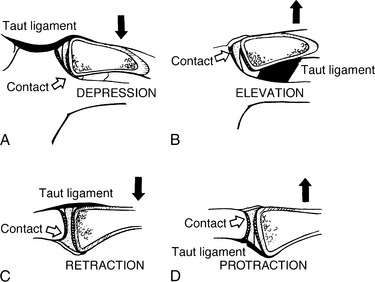
Figure 2-7 Sternoclavicular motion through two axes. Illustrated are depression (A) and elevation (B) through the sagittal axis, and retraction (C) and protraction (D) through the superomedial to inferolateral oblique axis.
(From Dempster WT: Mechanisms of shoulder movement. Arch Phys Med Rehabil 46:49-70, 1965.)
Even with trauma to the sternoclavicular joint, close to normal range of motion and full function are achieved, but pain acts as the limiting factor. In patients with hypomobility of this joint, shoulder elevation may be limited to 100 degrees, with abduction and internal rotation the most painful movements.
Acromioclavicular Joint
The acromioclavicular joint is a plane-type joint formed by the articulation of the distal clavicle with the acromion of the scapula. Three degrees of freedom are available at the acromioclavicular joint; however, they rarely occur individually.52 Motion occurs in a vertical, anterior-posterior, and medial-lateral direction (Fig. 2-8).
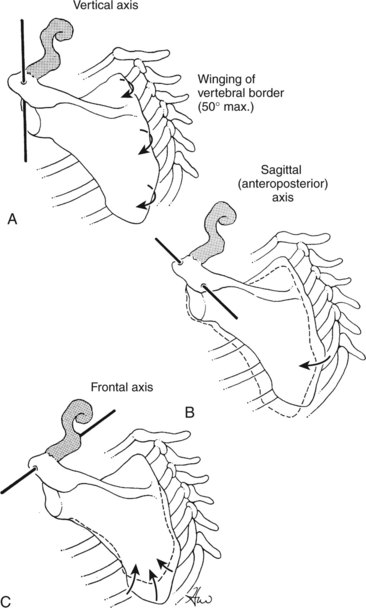
Figure 2-8 Three axes of motion shown through the acromioclavicular joint. A, Vertical axis allows the glenoid to face toward the sagittal or coronal plane. B, Sagittal axis allows slight medial and lateral rotation. C, Coronal axis allows anterior and posterior tilting.
(From Moseley HF: The clavicle: Its anatomy and function. Clin Orthop 58:17-27, 1958.)
The vertical axis allows the scapular vertebral border to “wing” and the glenoid fossa to face anteriorly.51,52 The acromion glides forward and backward as the scapula’s medial border swings away from and into the thorax—scapular internal and external rotation. This motion is checked by tension in the conoid and trapezoid ligaments. Motion about the anteroposterior axis results in enlarging or shrinking the angle formed by the clavicle and spine of the scapula in the frontal plane.21 This axis allows for scapular abduction and adduction, as described by Mosley.52 An axis through the coronal plane permits anterior tilting of the superior angle, causing the inferior angle to lift posteriorly. Anterior tilting is restricted by the anterior acromioclavicular and trapezoid ligaments, whereas posterior tilting is restricted by the thorax and posterior acromioclavicular and conoid ligaments.51
Inman and associates35 have demonstrated that approximately 10 degrees of motion occur at the acromioclavicular joint during the first 30 degrees of flexion and abduction, and then again in the last 45 degrees of motion. The acromioclavicular joint contributes greater motion at the end range of elevation,3 although total motion is restricted to about 5 to 8 degrees per axis.56 When irritation of this joint exists, clinical findings reveal pain at all shoulder end ranges, particularly during horizontal adduction. The acromioclavicular joint may compensate for lost motion in the presence of glenohumeral joint restriction.57
Inman and coworkers35 have warned against screw fixation negating acromioclavicular joint motion. Several investigators have found screw fixation or coracoclavicular ossification to have little or no effect on shoulder elevation.58,59 In fact, when Kirschner wires were attached to the clavicle of a patient whose distal clavicle was fixated to the coracoid by a screw, full clavicular rotation was observed.60 Kennedy and Cameron58 have reported that patients older than 50 years have less satisfactory results and painful end range abduction with screw fixation. It was concluded that this group relies more on the coracoclavicular ligamentous play than younger patients.
Glenohumeral Joint
The glenohumeral joint is a classic ball-and-socket joint between the humeral head and glenoid fossa of the scapula, and is the most mobile joint in the body.1,21,61 This high level of mobility challenges the inherent stability, as evidenced by the articulation between the larger convex humeral head and shallow concave glenoid fossa. This joint is an intricate complex with a sometimes fragile system of checks and balances; its vulnerability is demonstrated by the number of patients seen with pathology of associated static and dynamic components.
The glenohumeral joint has three axes of motion along the cardinal planes of the body: sagittal, frontal, and horizontal. Sagittal plane flexion and frontal plane abduction require concomitant humeral rotation. The humerus externally rotates with abduction11,12,4,62 and internally rotates with flexion.23,63,64 With scapular plane elevation, no external rotation is required.14
Only 25% to 30% of the humeral head is covered by the glenoid surface in any given anatomic position.11 The average humeral head diameter is 44 mm compared with a glenoid diameter of 25 mm. The fossa is deepened by a 2-mm ridge of labral fibrocartilage tissue.65 Although the bony surfaces of the humeral head and glenoid fossa have slightly different curvatures, their cartilaginous articular surfaces have approximately the same radius of curvature.21,66-68 The radius of curvature quantifies the amount of curve in a surface by describing the radius of the circle from which the surface is derived. These surfaces have similar curvatures; thus, there is a high degree of congruence, which helps disperse loads across a larger surface area, reducing articular surface stress.
The concept of glenohumeral motion occurring with a certain degree of rotation (spin), roll, and glide is well accepted (Fig. 2-9). MacConnail and Basmajian64 have developed the term roll-gliding to describe joint motion between incongruent, concave, and convex surfaces. The direction of rolling and gliding components is dependent on whether the concave or convex surface is moving. The convex-concave theory of arthrokinematics dictates that if a convex surface moves on a concave surface, then gliding occurs in the opposite direction to the rolling; if a concave surface moves on a convex surface, then rolling and gliding occur in the same direction. The more congruent the surfaces, the more gliding occurs and the more incongruent, the more rolling takes place.69 The disproportion between the glenohumeral articular surfaces would then dictate that rolling dominates. In other investigations, however, these findings were not validated.
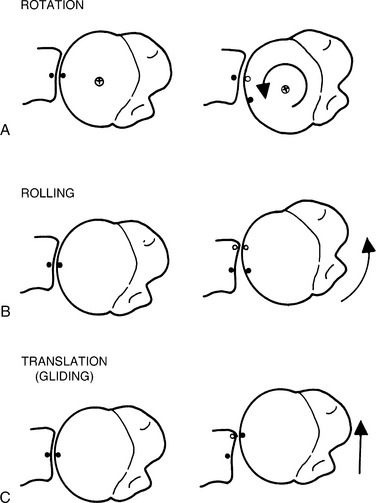
Figure 2-9 Three types of articular movement occur at the glenohumeral joint. A, Rotation. B, Rolling. C, Gliding.
(From Matzen FA III, Zuckerman J: Biomechanics of the shoulder. In Frankel VH, Mordin M [eds]: Basic Biomechanics of the Musculoskeletal System, 2nd ed. Philadelphia, Lea & Febiger, 1989, p 231.)
There has been much debate regarding the translatory motion of the glenohumeral joint. Calliet6 and Saha13,70 have stated that humeral head rolling on the glenoid is the predominant motion and that this is accompanied by some amount of gliding. Perry5 has stated that gliding is the primary component motion and that rolling is not significant to glenohumeral motion, other than the first 3 mm of superior excursion. Howell and colleagues71 have noted that rotation is the dominant movement, with gliding as the initial movement. Poppen and Walker16 have radiographically determined the initial 30 degrees of scapular plane elevation; often, from 30 to 60 degrees, the humeral head glides upward on the glenoid fossa approximately 3 mm. After this initial phase, the humerus center of rotation remains constant, moving 1 to 2 mm upward or downward relative to the glenoid center. It was concluded that after the initial rise, the humeral head will rotate or spin on a more or less fixed center, with little if any excursion. Harryman and associates72,73 have reported an average superior migration of 0.7 mm during abduction and 0.8 mm during flexion.
Using a three-dimensional technique of stereophotogrammetry on cadaver shoulders, Kelkar and coworkers74 have found an average vertical excursion of 1.29 mm occurring through an arc of 180 degrees of scapular plane abduction and an average of 0.94 mm of superior glide in the first 30 degrees of motion (Fig. 2-10). In support of Poppen and Walker’s findings,16 they concluded that the initial superior rise occurs because of the dependent (inferior) state of the humerus when unloaded but after 30 degrees, pure glenohumeral joint rotation occurs. Yamaguchi and colleagues75 have demonstrated a progressive superior translation of the humeral head on the glenoid, with increasing arm elevation in patients with symptomatic and asymptomatic rotator cuff tears. The symptomatic and asymptomatic rotator cuff tear groups exhibit an increase in superior head migration from 30 to 150 degrees during scapular plane elevation, as well as a disruption of normal glenohumeral kinematics. However, shoulder pain is not always present with the superior migration.
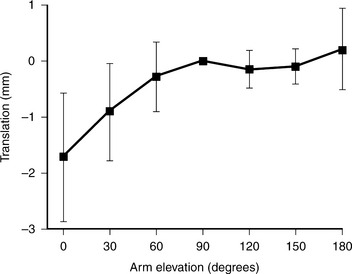
Figure 2-10 Normal superior glide during plane of the scapula abduction.
(From Kelkar R, Flatow E, Bigliani L, et al: A stereophotogrammetric method to determine the kinematics of the glenohumeral joint. Adv Bioeng 19:143, 1992.)
It is important for the clinician to realize that the humeral head does not truly “depress” with elevation, and that gliding is both superior and inferior.8 The humeral head center of rotation remains relatively constant with the center of the glenoid. What changes, through rotation and subtle gliding of 1 to 2 mm (roll-glide), is the humeral articular contact point moving inferiorly to superiorly on the humeral head.16,74,76 The greater tubercle “depressing” (as the humerus elevates) during palpation must not be mistaken for a sign of humeral head inferior gliding. Instead, greater tubercle movement represents medial migration beneath the acromion.
Controversy also exists regarding the translation or gliding of the humeral head in the anterior and posterior directions. Howell and associates71 have radiographically evaluated anterior and posterior translation with the arm positioned in varying degrees of horizontal adduction/abduction and rotation (Fig. 2-11). It was concluded that the humeral head normally translates 4 mm posteriorly in 90 degrees of abduction, full external rotation, and maximal horizontal abduction, but subjects with known anterior instability demonstrate anterior, not posterior, translation in the same position. Harryman and coworkers73 have performed a biomechanical analysis on cadavers using telemetry; they found approximately 3.8 mm of anterior translation with flexion and 5 mm of posterior translation with extension. With tightening of the posterior capsule, there is a significant increase in anterior translation and, to some extent, superior humeral head translation. Additionally, it was noted that external rotation and internal rotation, performed with the humerus at the side, produces posterior and anterior gliding, respectively.
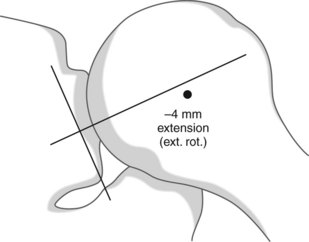
Figure 2-11 Axillary view (inferior through the glenohumeral joint) in 90 degrees of abduction, full external rotation, and horizontal abduction. The geometric center of the humeral head is 4 mm posterior to the center of the glenoid fossa, demonstrating normal posterior, not anterior, translation. ext. rot., external rotation.
(From Howell SM, Galinat BJ, Renzi AJ, Marone PJ: Normal and abnormal mechanics of the glenohumeral joint in the horizontal plane. J Bone Joint Surg Am 70:227-232,1988.)
Werner and colleagues77 have examined the effects of capsular tightening on humeral head translation in cadavers. The capsular plication causes a translation directed away from the plication site. Moore and associates78 have studied the kinematics of glenohumeral joint translation, with varying degrees of internal and external rotation at 90 degrees abduction. With increasing external rotation, anterior translation decreases and the humeral head moves in the posterior direction.
These studies have concluded that the direction of translation is dictated by tightening of the capsuloligamentous complex opposite the side of translation (Fig. 2-12). Shoulder movement causes the static restraints to become taut; they not only serve to counteract but to reverse humeral head movement. If the static restraints are stretched or their attachments compromised, abnormal translation occurs.8 For example, in the presence of a Bankart lesion or loose anterior and inferior capsule, the humeral head would translate anteriorly when placed in abduction and external rotation, as opposed to posteriorly.
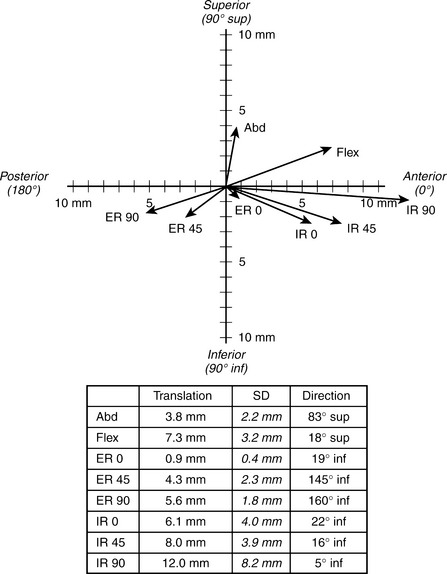
Figure 2-12 Translation at the end of several movements with intact capsule. The values indicated are mean translations in the actual directions (directions are defined relative to a strictly anterior direction: 0 degrees, posterior direction; 180 degrees, superior and inferior parts, respectively). Abd, abduction; Flex, flexion; ER 0, external rotation at 0 degrees of abduction; ER 45, external rotation at 45 degrees of abduction; ER 90, external rotation at 90 degrees of abduction; IR 0, internal rotation at 0 degrees of abduction; IR 45, internal rotation at 45 degrees of abduction; IR 90, internal rotation at 90 degrees of abduction.
(From Werner CM, Nyffeler RW, Jacob HA, Gerber C: The effect of capsular tightening on humeral head translations. J Orthop Res 22:194-201, 2004.)
In summary, an initial superior glide occurs with elevation, not inferior, until the head centers and rotation occurs. During shoulder extension and external rotation, the humeral head glides posteriorly and, with shoulder flexion and internal rotation, the humeral head glides anteriorly.21,67,73,79-81 This is likely because of the constraints of the capsular tissue and glenohumeral ligaments. These findings contradict the traditionally taught kinematics—the concave-convex rule.21
Performing joint glides to re-establish proper joint mechanics based on the traditionally accepted idea of joint motions is questionable. Joint mobilization is essential for relieving pain, producing muscular relaxation, and increasing joint range of motion. These techniques are effective because directional mobilizations “stretch” isolated portions of the capsuloligamentous complex. By improving capsuloligamentous pliability in any direction, regardless of the directions in which the humeral head translates during motion, proper joint mechanics and range of motion are restored in all ranges of motion and planes.8
STABILITY
Stability of the glenohumeral joint is provided by the articulating surfaces, capsular and ligamentous structures, and synchronous activity of the rotator cuff, biceps, deltoid, and scapular muscles.82 Stability or instability research has been based primarily on cadaveric and operative investigations. Focus has been on anterior instability because this is most commonly seen, followed by posterior instability and inferior instability. Four structures are considered to be the main factors in stability of the shoulder—articular surfaces, labrum, capsuloligamentous complex, and rotator cuff. Scapular muscle function will be discussed separately. Related factors will also be addressed in this section.
Articular Surfaces
The glenohumeral articular surfaces have been shown to provide static stability to the joint.83 The surface of the glenoid fossa has been found to be one third to one quarter that of the humeral head,70,84-87 and this difference in the size of the articular surfaces allows a large degree of mobility. Saha,36 using cadaveric radiographic studies, has determined that the normal glenoid is retroverted approximately 7.4 degrees, serving to discourage anterior humeral translation. Of 21 shoulders with anterior instability, 80% demonstrated 2 to 10 degrees of glenoid anteversion. A corresponding increase in humeral retroversion was believed to predispose the joint to anterior instability. Basmajian and Bazant57 have discovered that a 5-degree superior tilt of the glenoid assists in preventing inferior humeral migration.
Congruence can be defined as the difference in the radii of the humeral head and glenoid articulating surfaces.82 The closer this difference is to zero, the more congruent is the joint. Soslowsky and coworkers83 have demonstrated excellent congruency between the glenoid and humeral head using three-dimensional stereophotogrammetry to quantify the articular geometry in 32 cadavers. They found an average ratio of the radii of curvature between the two surfaces of 0.99 ± 0.05. This conformity of surfaces dictates that pure rotation with minimal translation occurs at this joint.74 The articulating cartilage surfaces are much more conforming than the underlying bone surfaces, resulting in a misleadingly flat glenoid shape on radiographs.88
A built-in safeguard promoting articular stability, often forgotten, is the effect of scapular motion.8 Scapular mobility allows the glenoid to adjust, providing a stable osseous platform for the humeral head.89 This movable base may compensate for articular deficiencies.
Labrum
The glenoid labrum is a wedge-shaped ring of fibrocartilage that encircles the bony glenoid, deepening the glenoid cavity and serving to bridge bone to the glenohumeral ligaments and biceps tendon (Fig 2-13). Using cadavers, Howell and Galinet65 have found the average depth of the socket and labrum to be 9 mm superiorly-inferiorly and 5 mm anteriorly-posteriorly. The labrum was found to contribute approximately 50% of the total depth of the socket, and detachment of the labrum anteriorly, as in a Bankart lesion, may reduce the depth of the socket in the anterior-posterior direction. Regional variation in the labrum exists; the inferior portion is immobile and firmly attached to the glenoid and the superior portion is attached more loosely, allowing for substantial range of motion of the glenohumeral joint.88

Figure 2-13 Labral insertion to the glenoid rim.
(From O’Brien SJ, Arnoczky SP, Warren RF, Rozbruch RA: Developmental anatomy of the shoulder and anatomy of the glenohumeral joint. In Rockwood CA, Matsen FA (eds): The Shoulder. Philadelphia, WB Saunders, 1990, p 14.)
The labrum is the weak link (younger than 30 years) when a continuous progressive low load is exerted across the anterior capsular mechanism.90 Hara and colleagues91 have reported that the anterior-inferior portion of the labrum is relatively weak, consistent with clinical findings of lesions commonly identified in anterior shoulder dislocation.
Bankart,92 Rowe,93 and Rowe and Sakellarides,19 proponents of labral stability influence, have emphasized the importance of the labrum linking the capsule to the glenoid bony rim as opposed to a buttress effect, in which the labrum acts as a physical block to humeral head displacement. Recurrent instability tends to erode the articular cartilage of the anterior inferior glenoid rim and decreases concavity.88 With the labrum intact, the humeral head resists tangential forces as much as 60% of the compressive load.94 The amount of humeral head translation needed to produce anterior glenohumeral dislocation clinically requires inferior glenohumeral ligament plastic deformation in addition to the Bankart lesion. Resection of the glenoid labrum has been reported to reduce the effectiveness of compression-stabilization by approximately 10% to 20%.95 Chondral-labral defects reduce the height of the glenoid, which in turn significantly reduces the stability ratio.96
Compression by muscle activity and capsuloligamentous tightening increases the stability of the labrum.94 Rodosky and associates,97 using dynamic cadaveric shoulder models, have created superior labral lesions and found that these shoulders show a decreased ability to resist external rotation when abducted and internally rotated. Superior labral defects have been found to decrease torsional rigidity and increase inferior glenohumeral ligament strain, which contributes to anterior instability.88
Capsuloligamentous Complex
The glenohumeral joint capsule provides passive stability at the extremes of glenohumeral motion.77 The capsule does not only limit rotation and prevent excessive translations, but also causes a coaptation and obligate translation of the humeral head on the glenoid at the end of passive movements. The glenohumeral ligaments and coracohumeral ligaments reinforce the capsule and serve as static restraints (Fig. 2-14).98-104 Ligaments attach bone to bone and act to guide and limit motion, with their constraining function evident as these structures become taut. Essentially, ligaments fulfill a dual stabilizing role—to provide a barrier against translation103 and to increase articular compressive forces as they tighten.51 The extreme of this is seen in the presence of capsular adhesions. In the presence of fibrotic capsuloligamentous tissue, glenohumeral articular compression can be so oppressive that normal rotation is obliterated.8
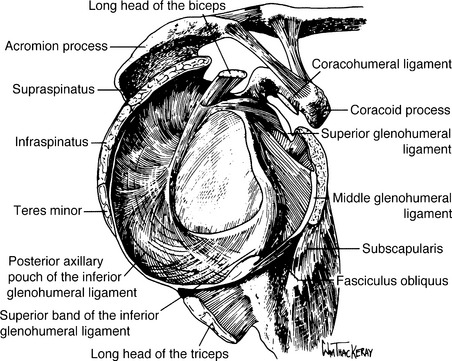
Figure 2-14 Lateral view of the glenoid showing the capsuloligamentous complex attachments in relation to the deep muscles and tendons.
(From Turkel SJ, Panio MW, Marshal JL: Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am 63:1208-1217, 1981.)
The role of any specific component of the stabilizing system varies with glenohumeral joint position and direction of the opposing force.88 A functional interplay or interdependence exists between anterior and posterior and superior and inferior components of the capsuloligamentous system. This circle concept of capsuloligamentous stability implies that excessive translation in one direction may damage the restraints on both the same and opposite sides of the joint.105 The capsule is a continuous structure; injury or repair to one region of the capsule may have an adverse effect on the properties of the neighboring regions and on joint function.106
Coracohumeral Ligament
The coracohumeral ligament (CHL) is intimately related to the rotator cuff and actually reinforces the supraspinatus superiorly and inferiorly.107 The CHL and superior glenohumeral ligament join to make up the rotator cuff interval, which bridges the supraspinatus and subscapularis (Fig. 2-15).23,73 The rotator cuff interval is the primary restraint against inferior and posterior translation of the adducted shoulder. Sectioning the interval increases anterior and posterior translation, whereas imbricating it significantly reduces translation in both directions. Harryman and coworkers73 have found that tightening the rotator cuff interval leads to an 8-degree loss of flexion and an 18-degree loss of extension. This is consistent with the study by Terry and colleagues,102 who found the CHL to be a primary restraint in flexion and extension. Harryman and associates73 have also found external rotation performed with the arm adducted decreased by 38 degrees and adduction by 8 degrees when the interval was imbricated. Gerber and coworkers,108 using cadavers, have found that closure of the rotator interval limits external rotation of the adducted arm by a mean of 30.1 degrees (56.4% of normal), whereas it had no significant effect on external rotation of the abducted arm. In addition to preventing inferior instability with the arm at the side, the CHL restricts external rotation and extension.72,85,100,102,109
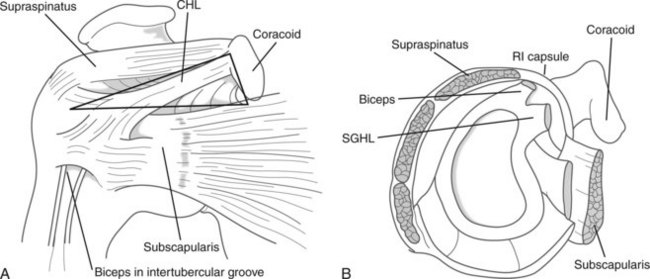
Figure 2-15 Schematic of the rotator cuff interval. A, Anterior view. B, Cross-sectional lateral view. CHL, coracohumeral ligament; RI, rotator interval; SGHL, superior glenohumeral ligament.
(From Fitzpatrick MJ, Powell SE, Tibone JE, Warren RF: The anatomy, pathology, and definitive treatment of rotator interval lesions: Current concepts. Arthroscopy 19:70-79, 2003.)
The significance of the coracohumeral ligament is not only important in stability but in the presence of supraspinatus pathology. Because the CHL limits external rotation when the arm is adducted, exercising into excessive external rotation while the arm is adducted should be approached with caution. The passive tension developed in the CHL translates directly to the compromised supraspinatus, causing pain or further disruption.8 Additionally, release of the interval and subsequent suturing during a rotator cuff repair need to be respected by limiting postoperative external rotation motion when the arm is at the side.
Superior Glenohumeral Ligament
The superior glenohumeral ligament (SGHL) prevents inferior displacement of the humeral head,84,110 limits external rotation at 0 degrees of rotation,100,102,104 and acts as a restraint during extension. A lesion of the rotator cuff interval, which is associated with anterior and inferior instability of the glenohumeral joint,111 may be caused by a deficiency in the superior glenohumeral ligament. The SGHL and anterior band of the coracohumeral ligament also serve as restraints up to 50 degrees abduction and external rotation.112 Both ligaments have been implicated as the source of fatigue pain when a mild downward load is placed on the arm.113 Following shoulder surgery, and in the presence of reflex inhibition, tension that develops in these ligaments may partly explain postoperative pain.8 Once these ligaments have stretched, as in hemiplegia, it is difficult to regain stability.57
Middle Glenohumeral Ligament
Turkel and associates104 have investigated the stabilizing mechanisms of the glenohumeral joint that prevent anterior dislocation by sequentially incising the glenohumeral anterior and posterior soft tissue structures. The subscapularis was initially cut, followed by the SGHL, middle glenohumeral ligament (MGHL), and inferior glenohumeral ligament (IGHL). It was found that anterior dislocation occurs at neutral when externally rotated, with the subscapularis muscle providing primary stability. At 45 degrees of abduction, primary stability is provided by the subscapularis, MGHL, and anterosuperior fibers of the IGHL. Approaching 90 degrees of abduction, the inferior glenohumeral ligament prevents dislocation during external rotation. At 90 degrees of abduction and full external rotation, the joint remains stable, until the posterior cuff was cut, which resulted in anterior dislocation. This study104 was performed with scapular fixation while abducting the humerus to 90 degrees, which does not take into consideration scapular rotation; 90 degrees in this investigation corresponds to approximately 120 to 135 degrees of true shoulder elevation.8 A limitation of this study was that it did not introduce horizontal abduction or apply any anterior force.
Gerber and coworkers108 have studied the effect of capsular contractures on the passive range of movement of the glenohumeral joint. Their data suggest that anterior plications restrict external rotation, whereas posterior plications restrict internal rotation. Plications of the superior aspect of the capsule are largely responsible for restrictions of motion with the arm in an adducted position. Conversely, plications of the inferior aspect of the capsule have more influence on motion of the abducted arm. The results of this study have demonstrated that contracture of the posterosuperior aspect of the capsule may limit internal rotation and flexion, whereas contracture of the anteroinferior aspect of the capsule, including the anteroinferior glenohumeral ligament complex, increasingly limits motion with increasing abduction of the arm. Contracture of the posterior aspect of the capsule plays an important role in limiting internal rotation, flexion, and abduction, even without inferior plication.
The MGHL was found to have stabilizing effects at 0 and 45 degrees of abduction.8 External rotation at these positions causes tightening of the MGHL, providing a barrier against anterior displacement.104,114 Turkel and colleagues104 have reported that this ligament is loose at 90 degrees of abduction and full external rotation. Other investigations have shown that the MGHL, along with the SGHL, is similar to the IGHL in regard to abduction and external rotation,100,115 and that the MGHL is found to tighten during flexion combined with external rotation.102 The MGHL also functions to support the arm and provide anterosuperior stability.112
Inferior Glenohumeral Ligament
The IGHL is the thickest of the glenohumeral ligaments, with an anterior band, posterior band, and axillary pouch. As with the other glenohumeral ligaments, the IGHL’s ability to restrict motion depends on humeral elevation and rotation. At 0 degrees abduction, the anterior band becomes the primary stabilizer,112 tightening when the humerus is externally rotated at neutral and when the humerus is abducted without external rotation.102 When external rotation is performed at 90 degrees of abduction, the entire IGHL tightens while the superior or anterior band wraps snugly across the humeral head, checking anterior displacement.99,102,104,114,116 O’Connell and colleagues100 have found the greatest amount of strain through the IGHL at 90 degrees of abduction and full external rotation. Kuhn and associates117 have suggested that the inferior glenohumeral ligament is the most important restraint to external rotation in both the neutral and abducted positions. The clinical implication is that external rotation may contribute to failure of the inferior glenohumeral ligament in patients with shoulder instability.
The IGHL has the ability to stretch considerably before ligament failure, suggesting that lateral translation of the humeral head is possible under loads that would allow the head to override the glenoid rim.88,118 This supports the clinical finding that certain patients can sublux without disruption of the capsule or its insertion sites. Repetitive loading of the inferior glenohumeral ligament at increasing levels of subfailure strain shows a dramatic increase in peak force with elongation, suggesting that the capsule may be subject to plastic deformation, especially after trauma.101,119
The IGHL appears to be a single identifiable complex that stabilizes against abnormal anterior and posterior humeral head translation, becoming taut wit hexternal and internal rotation, respectively, during arm elevation.99 Conversely, it can be appreciated how adhesions or contracture of this structure could limit external rotation, internal rotation, and elevation.
Internal rotation performed at 90 degrees of abduction causes the posterior band and axillary pouch to fan out and cradle the humeral head posteriorly, restricting posterior subluxation of the humeral head.99,114 Tightness of the posterior capsular ligamentous structures has been hypothesized to cause glenohumeral internal rotation deficit (GIRD) and a higher incidence of SLAP (superior labral anterior-posterior) lesions.120 GIRD is defined as the loss (in degrees) of glenohumeral internal rotation of the throwing shoulder compared with the nonthrowing shoulder, as measured in the supine position at 90 degrees of abduction. SLAP lesions were first described by Snyder and coworkers.121 Andrews and colleagues122 have hypothesized that during the follow-through phase of pitching, the biceps contracts eccentrically to decelerate the extending elbow. The resulting force might transmit proximally to the glenoid tubercle and stress, if not tear, the anterosuperior labrum. Burkhart and Morgan123 have proposed that pitchers and overhead athletes develop SLAP lesions because of the peel back mechanism. In a series of 53 overhead athletes who had surgery for type II SLAP lesions, they quantified a loss of internal rotation at 90 degrees of abduction of 25 degrees or greater. They proposed that the tight postero-inferior capsule wraps inferiorly when the arm is in the late cocking phase (90 degrees of abduction and full external rotation [ER]), resulting in the humeral head to shift or be pushed superiorly and posteriorly.123 Additionally, the long head of the biceps is oriented vertically and posteriorly and, as it contracts, it causes the posterior-superior labrum to peel back over the glenoid rim.
Conclusion
Understanding the unique position-related constraining characteristics of the glenohumeral ligaments, the clinician can gain insight into capsuloligamentous pathology and anatomic appreciation of the unstable shoulder. The interdependency of the capsuloligamentous-labral complex becomes evident when examining the literature; thus, it can be concluded that the complex should be considered a functional unit.8 With regard to anterior stability with the arm at 0 degrees abduction, the SGHL and MGHL are the primary restraints, with the posterior capsule as the secondary restraint.124 At 45 degrees of abduction, the primary restraint is the MGHL, with secondary restraints being the posterior capsule, IGHL, and MGHL. With the arm at 90 degrees, the primary restraint is the IGHL and secondary restraints are the MGHL and posterior capsule. The IGHL appears to function in a dual role; it is the main restraint against anterior humeral head displacement when in external rotation at 90 degrees of abduction and also forms a substantial posterior barrier when the arm is internally rotated in the abducted position.8 The posterior rotator cuff and capsule are the primary restraints against posterior instability; the anterior capsuloligamentous complex assists with posterior stability and the posterior structure assists with anterior stability.102
Dynamic Stability
The dynamic system of the glenohumeral joint is the fourth line of defense against shoulder instability (see Fig. 2-13). The musculotendinous units surrounding the glenohumeral joint assist the static restraints in stabilizing responsibilities, while also providing the power for motion.
Under normal conditions, forces transmitted by the supraspinatus, infraspinatus, teres minor, and subscapularis provide significant stability to the glenohumeral joint. This is achieved in several ways:
Active stability is achieved through coordinated shoulder muscle activity that compresses the humeral head into the glenoid and allows concentric rotation of the humeral head on the glenoid (Fig. 2-16).16,71,92,115,125-127 This mechanism, termed concavity-compression, depends on both shoulder muscle forces and the shape of the articular surfaces, principally the glenoid.94 The shoulder muscles may be the primary stabilizers of the glenohumeral joint during the midranges of motion, in which the capsuloligamentous structures are lax. Concavity-compression may also be important at the end ranges of motion, because glenohumeral joint forces are increased.127-129 Shoulder muscle activity protects the capsuloligamentous structures at the end ranges by limiting the joint’s range of motion130 and decreasing strain on these structures.
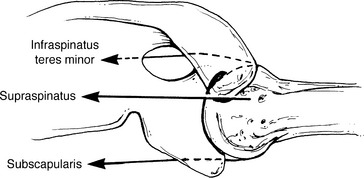
Figure 2-16 Dynamic effect of the rotator cuff causing compression as well as superior, anterior, and posterior barrier effects.
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 85.)
The effectiveness of the concavity-compression mechanism depends on characteristics of the shoulder muscle forces and the articular surfaces.94 Muscle forces acting on the shoulder joint can be divided into three components—compressive forces, superiorly-inferiorly directed forces, and anteriorly-posteriorly directed forces. The compressive forces stabilize the glenohumeral joint and the anteriorly, posteriorly, inferiorly, and superiorly directed forces, or translational forces, destabilize the glenohumeral joint.127 Glenohumeral joint stability may be quantified by the ratio between the translational forces in any direction and the compressive forces.96 As the ratio between the translational forces and compressive forces decreases, stability of the glenohumeral joint increases, and vice versa.95 Glenohumeral joint stability through concavity-compression is greater in neutral than in an abducted position, which may contribute to the dislocation of the shoulder anteriorly. The rotator cuff muscles and long head of the biceps actively compress the humeral head into the glenoid cavity, along with the outer sleeve of the shoulder muscles, such as the deltoid, pectoralis major, and latissimus dorsi. Shoulders with weakened or deficient rotator cuff mechanisms are likely to have compromised stability from impaired concavity-compression.88
Although the rotator cuff muscles, along with the deltoid, are considered stabilizers of the glenohumeral joint, the subscapularis is considered important for anterior integrity. DePalma and colleagues131 have advocated that the role of the subscapularis is to provide a “dynamic buttress” effect. Morrey and Chao98 have calculated forces at the glenohumeral joint during 90 degrees of coronal plane abduction in external rotation and determined that the anterior shear force increases from 12 to 42 kg in the unloaded upper extremity when the arm moves into 30 degrees of horizontal abduction. The combined tensile strength of the subscapularis and capsuloligamentous complex is calculated as 120 kg,90 allowing stability of the glenohumeral joint to be maintained. Anterior shear increases under higher speeds and greater loads and, when the force exceeds the tensile strength of the anterior structures, dislocation occurs.8 With an incompetent capsuloligamentous complex, the subscapularis muscle becomes the primary structure to stabilize against the impeding translation. This becomes increasingly difficult for the subscapularis with subsequent dislocations because evidence of tendon lengthening has been reported.131-133 Inherent lengthening of this structure leads to inefficient translation of tension from the muscle to bone and the buttress effect is lost.
Turkel and coworkers’104 sequential incising study has revealed a significant increase (mean 18 degrees) in external rotation in the neutral position once the subscapularis is cut. No significant increase in anterior translation is noted at 45 and 90 degrees of abduction and the joint cannot be dislocated. These findings were similar to those of Oversen and Nielsen.101 Interestingly, the inferior border of the subscapularis was noted to rise above the inferior humeral head at 90 degrees of abduction and external rotation; thus, the subscapularis is an ineffective barrier against dislocation in this position. This finding provides insight as to why patients with a deficient CLC, Bankart lesion, or both recurrently dislocate in the abducted and externally rotated position, even though they possess significant strength of the subscapularis.8
Karduna and associates125 have concluded that activation of the rotator cuff muscles serves to limit rotation and translation of the glenohumeral joint compared with passive positioning. Cain and coworkers,130 using abducted cadaveric shoulders under passive external rotation, have demonstrated that the strain on the inferior glenohumeral ligament is decreased by increasing the force applied to the tendons of the infraspinatus and teres minor. However, muscle forces may promote anterior humeral head translation in the apprehension position, and predispose the glenohumeral joint to anterior instability when other stabilizing mechanisms are not functioning normally.134 Graichen and colleagues79 have found a decrease in glenohumeral translation with active shoulder motion because muscular activity centralizes that humeral head when compared with passive motion. A 50% decrease in the rotator cuff muscle force results in an almost 50% increase in anterior displacement of the humeral head in response to external loading at all glenohumeral joint positions.129 Mild recruitment of the internal rotators, including the subscapularis, has been shown to create an anterior translation constraint in the apprehension position.135
The role of the posterior rotator cuff structures is to assist dynamically in anterior stability of the glenohumeral joint. Cain and associates130 have demonstrated that the posterior cuff, particularly the infraspinatus and teres minor, pull the humeral head posteriorly when contracting, therefore reducing the anterior shear. Lee and coworkers136 have found that the infraspinatus and teres minor generate posterior shear forces and increase compressive forces in the anterior instability position, thereby enhancing joint stability. Conversely, the supraspinatus generates a large anterior shear force in the apprehension position, which may destabilize the joint anteriorly.
Combined contraction of the subscapularis and infraspinatus forms a force couple, providing stability throughout the midranges of elevation.88 Electromyography has demonstrated that the subscapularis and infraspinatus contract to stabilize the glenohumeral joint in abduction at 60 to 150 degrees.131 This type of activity, in conjunction with known decreased tensile strength of the rotator cuff,90 explains the high incidence of rotator cuff tears in individuals older than 45 years when they anteriorly dislocate137; excessive translation in the presence of a degenerative cuff causes tearing. Tear location has the most significant effect on stability in the inferior and anterior directions for smaller tears and on the anterior direction for larger tears.88
Passive tension of the posterior cuff may also play a role in stability. With incision of the infraspinatus and teres minor, significant posterior displacement occurs.101 It could logically be concluded that if passive tension of these muscles maintains significant stability, then active contraction would further enhance stability.8 Saha70 concluded the infraspinatus and teres minor are horizontal steerers that maintain stability. The importance of the posterior rotator cuff and deltoid to posterior stability is seen clinically; patients with posterior instability have responded well with external rotation strengthening.138 This is particularly true if the patient is a subluxator as opposed to a dislocator.139
Lee and An140 have quantified the contribution of the deltoid muscle to glenohumeral joint stability. At 60 degrees of abduction in the scapular plane, deltoid activity increases glenohumeral joint stability; however, at 60 degrees of abduction in the coronal plane, deltoid activity is found to decrease glenohumeral joint stability. Strengthening the middle and posterior portions of the deltoid may provide more stability to a patient with anterior instability, because they may work to generate higher compressive force and lower shear force than the anterior head.
The superior labrum serves as an attachment for the long head of the biceps and the superior glenohumeral ligament.61 The long head of the biceps tendon has an important role as a dynamic restraint to external rotation in the abducted shoulder.117 It has been suggested that the biceps becomes more important than the rotator cuff as an anterior stabilizer with decreased stability of the capsuloligamentous structures.141 Injury may represent a traction phenomenon, secondary to activity in the biceps, or possibly a compression phenomenon.88 Repetitive movement into extreme external rotation may excessively load the biceps tendon and predispose the overhead athlete to a biceps-labral complex injury, as noted earlier.142
As long as the scapula is positioned so that the glenoid fossa accepts the net forces acting on the humeral head, the glenohumeral joint will remain stable.88 A redundant capsule may allow excessive glenohumeral angles that exceed the scapulohumeral balancing mechanism,143 allowing instability to occur before the capsuloligamentous structures have sufficiently tightened to provide restraint.
Other Stabilizing Factors
Other forces that influence shoulder stability are atmospheric pressure and the adhesion-cohesion mechanism. Normal negative intra-articular pressure has been demonstrated to contribute to the stability of the glenohumeral joint.78 Kumar and Balasubramaniam144 have radiographically demonstrated significant inferior subluxation following percutaneous puncture of the capsule without dependence on muscle suspension, allowing atmospheric air to enter the joint. Harryman and associates72 have evaluated humeral head translation and the effect of capsular venting and found a slight increase in anterior translation during flexion and horizontal adduction. Matsen and coworkers132 have described this phenomenon as disruption of “finite joint volume.” Finite joint volume combined with the adhesion-cohesion mechanism enhances joint stability.8 Adhesion is described as fluid holding to a surface, whereas cohesion is the joining of two surfaces by fluid. Adhesion-cohesion is best demonstrated by wet microscope slides sticking together but able to slide on one another. The glenohumeral joint mimics this phenomenon at the contact area between the humerus and glenoid.
To summarize, the interplay of the various active and passive components contributes to the stability of the glenohumeral joint. The IGHL appears to be the primary structure in providing anterior stability, with the subscapularis contributing to anterior stability through the compressive forces imparted on the joint. The labrum is significant, being the weak link in the chain attaching the IGHL to the bony glenoid rim.8 Regardless of the direction of shoulder instability, efficient control of the rotator cuff is essential to function. Posterior stability is dependent on the anterior capsule and structures. Accepting the capsuloligamentous-labral complex as a functional unit explains why global laxity of this complex leads to multidirectional instability and why a capsular shift surgical procedure is required to address global laxity. Finally, atmospheric pressure and the adhesioncohesion mechanism also add to the stability of the shoulder joint. The clinician needs to consider all factors related to glenohumeral instability to implement safe and effective treatment during conservative and postoperative rehabilitation of the athlete.
MUSCLE ACTIVITY
Oatis21 has classified the muscles of the shoulder complex into axioscapular, axioclavicular, scapulohumeral, and axiohumeral muscles. Box 2-1 presents a listing of these categories.
Axioscapular and Axioclavicular
Muscles of the axioscapular and axioclavicular groups all attach to both the axioskeleton and scapula or clavicle.21 These muscles act on the sternoclavicular and scapulothoracic joints, and ultimately on the acromioclavicular joint. They provide a stable yet mobile base from which the glenohumeral joint and associated muscles can function. Loss of these muscles, particularly the trapezius or serratus anterior, consequently affects scapulohumeral rhythm and shoulder function.
Functional stability of the scapula requires optimal positioning, smooth muscular balance in the force couple around the scapula, and correct timing of muscle activity of the scapula rotators.145 A force couple is defined as equal forces producing a rotation by pulling in the opposite direction. The serratus anterior and trapezius force couple is a key component for normal function of the shoulder (Fig. 2-17). This force couple serves four paramount functions:8 (1) rotates the scapula, maintaining the glenoid surface in an appropriate position; (2) through scapular rotation, positions the deltoid to maintain efficient length, thereby enhancing power and stability (without scapular rotation, only 90 degrees of active abduction is available35,146); (3) prevents impingement of the subacromial structures on the coracoacromial arch; and (4) provides a stable base, enabling the axiohumeral and scapulohumeral muscles to move the arm against resistance.88 Trying to move the humerus without the trapezius, serratus, or both is analogous to trying to push against a solid wall while on roller skates.8
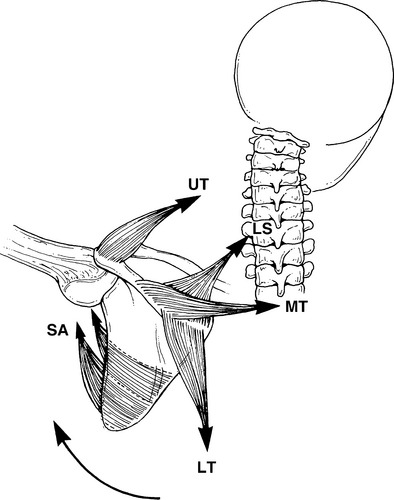
Figure 2-17 Serratus anterior (SA) and trapezius force couple generating scapular rotation. LS, levator scapulae; LT, lower trapezius; MT, middle trapezius; UT, upper trapezius.
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 100.)
This force couple can be divided into upper and lower components, both of which function in all planes of elevation. The upper component is comprised of the upper trapezius, levator scapulae, and upper portion of the serratus anterior. The lower component is comprised of the lower trapezius and lower portion of the serratus anterior.35
For the upper component, the upper trapezius and levator scapulae act to elevate the scapula during shoulder elevation. Activity of the upper trapezius, which is fairly constant in flexion and abduction, continues in a linear fashion as the scapula rotates about its axis.35,147 The upper trapezius is active as a scapular elevator and rotator through its insertion at the acromion. The fibers of the upper portion of the serratus anterior also assist in upward rotation.
For the lower component, the lower trapezius pulls inferiorly from its insertion at the base of the scapular spine to direct the glenoid upward. The lower trapezius contribution increases with increasing abduction. In flexion, activity plateaus between 70 and 120 degrees, after which activity significantly increases to coincide with the abduction curve.35,147
The force couple is now complete as the serratus anterior lower fibers pull the inferior angle forward and laterally. The scapula translates forward on the thoracic wall, directing the glenoid toward the sagittal plane, with the serratus anterior pulling the scapula forward. Progressive activity of the serratus anterior with humeral elevation should contribute to posterior tipping and external rotation of the scapula, as well as upward rotation.29 Electromyographic activity is equal for the scapular rotators at end range flexion and abduction, because the scapula always achieves the same terminal position with elevation, regardless of plane.148 The differences of scapular migration between flexion and coronal plane abduction are explained by the differences in activity of the lower trapezius, middle trapezius, and rhomboids; all have greater action potential values in abduction.8 The downward and medially directed fibers of the lower trapezius may assist in producing posterior tipping and external rotation moments as the humerus is elevated.
Individuals with impingement have been shown to exhibit decreased levels of serratus anterior activity and scapular upward rotation34 and a delay in middle and lower trapezius activation.145 A delayed response of the middle and lower trapezius muscles compared with the upper trapezius may lead to supremacy of the upper trapezius muscle, causing an abnormality in scapulohumeral rhythm. The upper and lower trapezius and serratus anterior muscles play a role in the production of scapular upward rotation throughout the range.33
Clinically, a long thoracic nerve palsy is more common, and results in greater functional impairment, than a spinal accessory nerve palsy.8 A prolonged, complete trapezius palsy can be debilitating because of the loss of scapular suspension and subsequent depression of the shoulder girdle (Fig. 2-18). A patient with an isolated spinal accessory nerve palsy will demonstrate weak sagittal plane motion, but frontal plane abduction will be significantly impaired. With a complete long thoracic nerve palsy, patients typically will be unable to flex or abduct the involved shoulder fully.
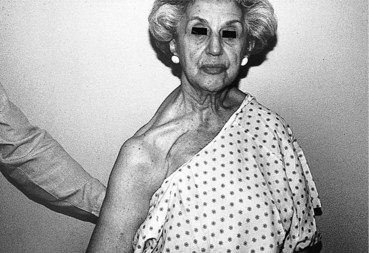
Figure 2-18 Patient with chronically denervated trapezius. Note shoulder girdle depression caused by loss of trapezius suspension effect.
A synergy also exists between the scapular adductors, particularly the middle and lower trapezius, with the motion of external rotation. When resisting shoulder external rotation in neutral, the trapezius and rhomboids work to stabilize the vertebral border of the scapula.8 In individuals with a spinal accessory nerve palsy, this relation becomes evident. Resisted external rotation results in a flip sign because the middle and lower trapezius cannot oppose the pull of the external rotators from their fixed origins.149,150 Clinically, we have seen up to a 25% reduction of internal and external torque output in patients with a serratus anterior or trapezius nerve palsy caused by loss of this synergy.
Recognition of scapulothoracic contribution to shoulder function is imperative. The clinician must evaluate for scapulothoracic muscle dysfunction because significant impairment of these muscles often exists in the presence of shoulder pathology. A muscular imbalance from weakness or shortening can result in impaired stabilization of the scapula. This concept becomes especially important for the thrower, who depends on the proper coordination and sequencing of the entire shoulder complex.
Scapulohumeral Muscles
The scapulohumeral muscles provide motion and dynamic stabilization to the glenohumeral joint.10,19,21 These muscles are crucial for function of the shoulder complex because the glenohumeral joint contributes to a significant amount of motion.
In the normal shoulder, the middle deltoid is active in all planes of elevation,128,151-153 whereas the anterior and posterior heads command flexion and extension, respectively.8 Although the anterior fibers dominate motion in flexion, the middle fibers become more involved at 60 degrees.147 This occurs because of relative humeral realignment toward the scapular plane as the scapula translates forward over the thoracic wall. Also, the obligatory internal rotation with flexion moves the deltoid’s insertion forward, providing the middle deltoid with a more efficient line of pull. Poppen and Walker128 have found that as the line of pull improves, so does the deltoid moment arm. The improvement in the line of pull and moment arm during abduction would be meaningless to the deltoid if the scapula did not rotate, functionally lengthening the deltoid. Without scapular rotation, the deltoid would excessively shorten by 90 degrees of abduction and the arm could not actively raise past this point; this is called active insufficiency.35,146 The deltoid is able to maximize function by a complex interplay of mechanical adjustments as the insertion rises overhead and the scapula rotates.
The other component of the scapulohumeral muscles is the rotator cuff, which provides the core dynamic control about the glenohumeral joint. Comprised of four muscles and associated tendons, the rotator cuff dynamically maintains articular congruity, thus providing the larger and more powerful shoulder muscles with the ability to move against great resistance.8
The dynamic effect of the supraspinatus is to stabilize the humeral head in the glenoid fossa centrally.5,11,35,70,98,128,154 This muscle also provides a depressive force because of tendon compression of the superior humeral head.155,156 A dysfunctional rotator cuff is unable to mitigate the upward shear from the deltoid, leading to impingement of the supraspinatus tendon and subacromial bursa against the coracoacromial arch.42 This mechanism may lead to humeral head superior migration in patients with chronic rotator cuff tears.157-159 Fatigue of the deltoid and rotator cuff complex also has been found to produce abnormal glenohumeral kinematics of superior migration of the humeral head on the glenoid.160
The second force couple of the shoulder complex is from the action of the deltoid, supraspinatus, infraspinatus, teres minor, and subscapularis (Fig. 2-19). The line of pull to the glenoid face of the infraspinatus and subscapularis has been estimated at 45 degrees, and the teres minor at 55 degrees.5 These three muscles have a negligible moment arm as abductors.33 Their responsibility in the force couple is to exert a predominantly downward shear, which peaks at 60 degrees of elevation, as well as a compressive load.3,35,70 As the deltoid draws the humeral head upward, the depressors tug downward, allowing humeral rotation while maintaining glenohumeral joint conformity.74,128 Compromise of the humeral head depressors results in an imbalanced struggle against the opposing deltoid shear, leading to superior humeral head displacement, loss of the effective fulcrum, and impaired strength.
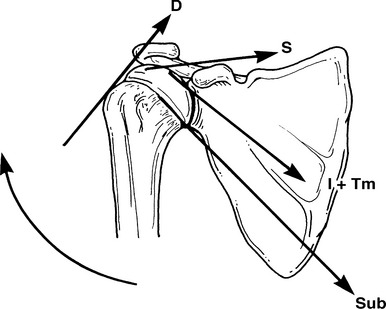
Figure 2-19 Deltoid and rotator cuff force couple
(From Kelley MJ, Clark WA: Orthopedic Therapy of the Shoulder. Philadelphia, Lippincott Williams & Wilkins, 1995, p 92.)
The supraspinatus and deltoid are in optimal alignment in the scapular plane.12 The supraspinatus is active in all planes of elevation,35,147,151,153 contrary to its originally being regarded as the isolated initiator of abduction. This has been clearly disproved by electromyographically induced nerve palsy studies162-164 and clinical observations.165,166 In fact, 40% to 60% of elevation torque output has been attributed to the supraspinatus and infraspinatus.167 With scapular plane elevation of the glenohumeral joint, the supraspinatus pulls the humeral head into the glenoid cavity and remains active during the movement.168 Scepi and colleagues168 have determined that at the beginning of scapular plane elevation, the anterior portion of the deltoid works synergistically with the supraspinatus.
There remains some controversy over the stabilizing versus abducting effect. Celli and associates169 have defined a stabilizer as a structure that demonstrates constant activity by electromyography compared with a mover, whose activity increases with motion. It was found that the deltoid is the abducting force (mover) whereas the supraspinatus is a stabilizer. Ito147 has found a linear progression of electrical activity in the supraspinatus and deltoid during abduction.
The infraspinatus and teres minor have also been found to be active throughout elevation,35,151,153 fulfilling two responsibilities—force couple requirements and serving as a posterior barrier against translation. The infraspinatus also contributes to the generation of abduction glenohumeral torque and stabilization of the humeral head against superior subluxation.170 The infraspinatus demonstrates a linear progression in activity throughout coronal35 and scapular plane abduction.70,147 Activity differs somewhat in flexion, being higher and peaking at between 60 and 120 degrees. Activity is enhanced because of muscle demand created when the elbow is flexed to 90 degrees, producing a moment toward internal rotation.8 The subscapularis acts synergistically with the posterior cuff muscles to depress and compress the humeral head and is more active in abduction than flexion.
Significant activity of the teres minor and infraspinatus is noted in full external rotation and horizontal extension.171-173 This is the late cocking phase position in throwing and is advocated for strengthening the posterior cuff muscles.174 Strong eccentric activity occurs in the subscapularis during the late cocking phase of throwing.171,175 Further discussion of the throwing cycle and pitching mechanics will be presented in subsequent chapters.
Clinically, strengthening of the posterior cuff muscles is essential for rehabilitating the nonoperative and postoperative athlete. Proper strength and balance of these muscles are key components of optimal shoulder function.
Axiohumeral Muscles
The axiohumeral muscles, pectoralis major and latissimus dorsi, attach the thorax to the humerus.21 They have large physiologic cross-sectional areas and are believed to provide additional strength to shoulder movement.113 Controversy exists regarding activity of the latissimus dorsi and pectoralis muscles in unresisted rotation.8 These muscles produce the forces required to accelerate the arm and object velocity.
Other Muscles
The biceps brachii, coracobrachialis, and triceps brachii also act on the shoulder joint. The biceps, although predominantly an elbow flexor and forearm supinator, can be an effective elevator and functions to stabilize the humeral head in the glenoid, preventing upward migration.85,146,176 Also, humeral external rotation places the long head laterally, causing it to act like a pulley and assisting in arm elevation.
SUMMARY
This chapter has discussed the biomechanics and principals behind the function of the shoulder complex. There is an impressive interdependency among muscle action, ligamentous stability, and osseous orientation to shoulder function. Understanding this relationship is paramount to the successful diagnosis and treatment of shoulder pathology and dysfunction.
1 Culham E, Peat M. Functional anatomy of the shoulder complex. J Orthop Sports Phys Ther. 1993;18:342-350.
2 Bearn JG. Direct observations on the function of the capsule of the sternoclavicular joint in clavicular support. J Anat. 1967;101:159-170.
3 Bateman J. The Shoulder and Neck. Philadelphia: WB Saunders, 1971.
4 Steindler A. Kinesiology of the Human Body Under Normal and Pathological Conditions. Springfield, Ill: Charles C Thomas, 1955.
5 Perry J. Biomechanics. In: Rowe C, editor. The Shoulder. New York: Churchill-Livingstone, 1988.
6 Calliet R. Shoulder Pain. Philadelphia: FA Davis, 1977.
7 Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945-950.
8 Kelley M, Clark W. Orthopedic Therapy of the Shoulder. Philadelphia: JB Lippincott, 1995.
9 Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder. Spectrum of pathology. Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641-661.
10 Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325-337.
11 Codman E. The Shoulder. Boston: Thomas Todd, 1934.
12 Johnston T. The movements of the shoulder joint. A plea for the use of the “Plane of the Scapula” as the plane of reference in movements occurring in the humero-scapular joint. Br J Surg. 1937;25:252.
13 Saha AK. Theory of Shoulder Mechanism: Descriptive and Applied. Springfield, Ill: Charles C Thomas, 1961.
14 Doody SG, Freedman L, Waterland JC. Shoulder movements during abduction in the scapular plane. Arch Phys Med Rehabil. 1970;51:595-604.
15 Freedman L, Munro RR. Abduction of the arm in the scapular plane: Scapular and glenohumeral movements. A roentgenographic study. J Bone Joint Surg Am. 1966;48:1503-1510.
16 Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195-201.
17 Dvir Z, Berme N. The shoulder complex in elevation of the arm: A mechanism approach. J Biomech. 1978;11:219-225.
18 McGregor L. Rotation at the shoulder: A critical injury. Br J Surg. 1937;24:425-438.
19 Rowe CR, Sakellarides HT. Factors related to recurrences of anterior dislocations of the shoulder. Clin Orthop. 1961;20:40-48.
20 Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol Avon). 2003;18:369-379.
21 Oatis CA. Kinesiology: The Mechanics and Pathomechanics of Human Movement. Philadelphia: Lippincott Williams & Wilkins, 2004.
22 De Freitas V, Vitti M, Furlani J. Electromyographic study of levator scapulae and rhomboideus major muscles in movements of the shoulder and arm. Electromyogr Clin Neurophysiol. 1980;20:205-216.
23 Duchenne G, Kaplan E. Physiology of Motion. Philadelphia: JB Lippincott, 1949.
24 Kendall F, McCreary E. Muscle Testing and Function, 3rd ed. Baltimore: Williams & Wilkins, 1982.
25 Karduna AR, McClure PW, Michener LA. Scapular kinematics: Effects of altering the Euler angle sequence of rotations. J Biomech. 2000;33:1063-1068.
26 van der Helm FC. A finite element musculoskeletal model of the shoulder mechanism. J Biomech. 1994;27:551-569.
27 Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech (Bristol Avon). 2002;17:650-659.
28 Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J Biomech Eng. 2001;123:184-190.
29 Ludewig PM, Cook TM, Nawoczenski DA. Three-dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J Orthop Sports Phys Ther. 1996;24:57-65.
30 Lukasiewicz AC, McClure P, Michener L, et al. Comparison of three-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574-583.
31 McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct three-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269-277.
32 McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: The effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998;27:125-133.
33 Ebaugh DD, McClure PW, Karduna AR. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech (Bristol Avon). 2005;20:700-709.
34 Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276-291.
35 Inman V, Saunder J, Abbot L. Observations on the function of the shoulder joint. J Bone Joint Surg. 1944;26:1.
36 Saha AK. Mechanism of shoulder movements and a plea for the recognition of “zero position” of glenohumeral joint. Indian J Surg. 1950;12:153-165.
37 Graichen H, Stammberger T, Bonel H, et al. Magnetic resonance-based motion analysis of the shoulder during elevation. Clin Orthop Relat Res. 2000;370:154-163.
38 Myers JB, Laudner KG, Pasquale MR, et al. Scapular position and orientation in throwing athletes. Am J Sports Med. 2005;33:263-271.
39 Paletta GAJr, Warner JJ, Warren RF, et al. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516-527.
40 Warner JJ, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moire topographic analysis. Clin Orthop Relat Res. 1992;285:191-199.
41 Kibler WB, Uhl TL, Maddux JW, et al. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550-556.
42 Mell AG, LaScalza S, Guffey P, et al. Effect of rotator cuff pathology on shoulder rhythm. J Shoulder Elbow Surg. 2005;14(suppl):58S-64S.
43 von Eisenhart-Rothe R, Matsen FA3rd, Eckstein F, et al. Pathomechanics in atraumatic shoulder instability: Scapular positioning correlates with humeral head centering. Clin Orthop Relat Res. 2005;433:82-89.
44 Finley MA, Lee RY. Effect of sitting posture on three-dimensional scapular kinematics measured by skin-mounted electromagnetic tracking sensors. Arch Phys Med Rehabil. 2003;84:563-568.
45 Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83:367-370.
46 Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227-238.
47 Stokdijk M, Eilers PH, Nagels J, Rozing PM. External rotation in the glenohumeral joint during elevation of the arm. Clin Biomech (Bristol Avon). 2003;18:296-302.
48 Ahmad CS, Wang VM, Sugalski MT, et al. Biomechanics of shoulder capsulorrhaphy procedures. J Shoulder Elbow Surg. 2005;14(suppl):12S-18S.
49 Hawkins RJ, Angelo RL. Glenohumeral osteoarthrosis. A late complication of the Putti-Platt repair. J Bone Joint Surg Am. 1990;72:1193-1197.
50 Lusardi DA, Wirth MA, Wurtz D, Rockwood CAJr. Loss of external rotation following anterior capsulorrhaphy of the shoulder. J Bone Joint Surg Am. 1993;75:1185-1192.
51 Dempster WT. Mechanisms of shoulder movement. Arch Phys Med Rehabil. 1965;46:49-70.
52 Moseley HF. The clavicle: Its anatomy and function. Clin Orthop. 1958;58:17-27.
53 Cave A. The nature and morphology of the costoclavicular ligament. J Anat. 1961;95:170-179.
54 McArdle PJ, Kalbassi R, Ilankovan V. Stability of the sternoclavicular joint. A retrospective study. Br J Oral Maxillofac Surg. 2003;41:12-15.
55 Spencer EE, Kuhn JE, Huston LJ, et al. Ligamentous restraints to anterior and posterior translation of the sternoclavicular joint. J Shoulder Elbow Surg. 2002;11:43-47.
56 Shaffer BS. Painful conditions of the acromioclavicular joint. J Am Acad Orthop Surg. 1999;7:176-188.
57 Basmajian J, Bazant F. Factors preventing downward dislocation of the adducted shoulder joint. An electromyographic and morphological study. Am J Orthop. 1959;41A:1182-1186.
58 Kennedy JC, Cameron H. Complete dislocation of the acromio-clavicular joint. J Bone Joint Surg Br. 1954;36:202-208.
59 Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen FA3rd, editors. The Shoulder. Philadelphia: WB Saunders; 1990:413-416.
60 Kapandji I. The Physiology of Joints, vol 1. Baltimore: Williams & Wilkins. 1970.
61 Curl LA, Warren RF. Glenohumeral joint stability. Selective cutting studies on the static capsular restraints. Clin Orthop Relat Res. 1996;330:54-65.
62 DePalma A. Surgery of the Shoulder. New York: JB Lippincott, 1973.
63 Blakely RL, Palmer ML. Analysis of rotation accompanying shoulder flexion. Phys Ther. 1984;64:1214-1216.
64 MacConail M, Basmajian J. Muscles and Movements: A Basis for Human Kinesiology. Baltimore: Williams & Wilkins, 1969.
65 Howell SM, Galinat BJ. The glenoid-labral socket. A constrained articular surface. Clin Orthop RelatRes. 1989;243:122-125.
66 Iannotti JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491-500.
67 Soslowsky LJ, Flatow EL, Bigliani LU, et al. Quantitation of in situ contact areas at the glenohumeral joint: A biomechanical study. J Orthop Res. 1992;10:524-534.
68 Van der Helm FC, Veeger HE, Pronk GM, et al. Geometry parameters for musculoskeletal modelling of the shoulder system. J Biomech. 1992;25:129-144.
69 Kaltenborn F. Mobilization of the Extremity Joints. In Examination and Basic Treatment Techniques. Oslo: Olaf Bokhandel; 1980.
70 Saha AK. Dynamic stability of the glenohumeral joint. Acta Orthop Scand. 1971;42:491-505.
71 Howell SM, Galinat BJ, Renzi AJ, Marone PJ. Normal and abnormal mechanics of the glenohumeral joint in the horizontal plane. J Bone Joint Surg Am. 1988;70:227-232.
72 Harryman DT2nd, Sidles JA, Clark JM, et al. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334-1343.
73 Harryman DT2nd, Sidles JA, Harris SL, Matsen FA3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53-66.
74 Kelkar R, Flatow E, Bigliani L, et al. A stereophotogrammetric method to determine the kinematics of the glenohumeral joint. Adv Bioeng. 1992;19:143-145.
75 Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: A comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6-11.
76 Nobuhara K. The Shoulder: Its Function and Clinical Aspects. Tokyo: Igaku-Shoin, 1977.
77 Werner CM, Nyffeler RW, Jacob HA, Gerber C. The effect of capsular tightening on humeral head translations. J Orthop Res. 2004;22:194-201.
78 Moore SM, Musahl V, McMahon PJ, Debski RE. Multidirectional kinematics of the glenohumeral joint during simulated simple translation tests: Impact on clinical diagnoses. J Orthop Res. 2004;22:889-894.
79 Graichen H, Stammberger T, Bonel H, et al. Glenohumeral translation during active and passive elevation of the shoulder’a 3D open-MRI study. J Biomech. 2000;33:609-613.
80 Moseley HF, Overgaard D. The anterior capsular mechanism in recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br. 1962;44:913-927.
81 Novotny JE, Woolley CT, Nichols CE3rd, Beynnon BD. In vivo technique to quantify the internal-external rotation kinematics of the human glenohumeral joint. J Orthop Res. 2000;18:190-194.
82 Bigliani LU, Kelkar R, Flatow EL, et al. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;330:13-30.
83 Soslowsky LJ, Flatow EL, Bigliani LU, Mow VC. Articular geometry of the glenohumeral joint. ClinOrthop. 1992;285:181-190.
84 Jobe CM, Iannotti JP. Limits imposed on glenohumeral motion by joint geometry. J Shoulder Elbow Surg. 1995;4:281-285.
85 Kent BE. Functional anatomy of the shoulder complex. Phys Ther. 1971;51:867-874.
86 Peat M. Functional anatomy of the shoulder complex. Phys Ther. 1986;66:1855-1865.
87 Sarrafian SK. Gross and functional anatomy of the shoulder. Clin Orthop Relat Res. 1983;173:11-19.
88 Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002;400:48-57.
89 Rowe CR. The Shoulder. New York: Churchill-Livingstone, 1988.
90 Reeves B. Experiments on the tensile strength of the anterior capsular structures of the shoulder in man. J Bone Joint Surg Br. 1968;50:858-865.
91 Hara H, Ito N, Iwasaki K. Strength of the glenoid labrum and adjacent shoulder capsule. J Shoulder Elbow Surg. 1996;5:263-268.
92 Bankart A. The pathology and treatment of recurrent dislocation of the shoulder. Br J Surg. 1938;26:23-29.
93 Rowe CR, Patel D, Southmayd WW. The Bankart procedure: A long-term end-result study. J Bone Joint Surg Am. 1978;60:1-16.
94 Lippitt SB, Vanderhoof JE, Harris SL, et al. Glenohumeral stability from concavity-compression: A quanitative analysis. J Shoulder Elbow Surg. 1993;2:27-34.
95 Halder AM, Kuhl SG, Zobitz ME, et al. Effects of the glenoid labrum and glenohumeral abduction on stability of the shoulder joint through concavity-compression: An in vitro study. J Bone Joint Surg Am. 2001;83:1062-1069.
96 Lazarus MD, Sidles JA, Harryman DT2nd, Matsen FA3rd. Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am. 1996;78:94-102.
97 Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121-130.
98 Morrey BF, Chao EY. Recurrent anterior dislocation of the shoulder. In: Dumbleton J, Black J, editors. Clinical Biomechanics. London: Churchhill Livingstone, 1981.
99 O’Brien SJ, Neves MC, Arnoczky SP, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449-456.
100 O’Connell PW, Nuber GW, Mileski RA, Lautenschlager E. The contribution of the glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med. 1990;18:579-584.
101 Ovesen J, Nielsen S. Anterior and posterior shoulder instability. A cadaver study. Acta Orthop Scand. 1986;57:324-327.
102 Terry GC, Hammon D, France P, Norwood LA. The stabilizing function of passive shoulder restraints. Am J Sports Med. 1991;19:26-34.
103 Townley CO. The capsular mechanism in recurrent dislocation of the shoulder. J Bone Joint Surg Am. 1950;32:370-380.
104 Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208-1217.
105 Flatow EL, Warner JI. Instability of the shoulder:complex problems and failed repairs: Part I. Relevant biomechanics, multidirectional instability, and severe glenoid loss. Instr Course Lect. 1998;47:97-112.
106 Moore SM, McMahon PJ, Azemi E, Debski RE. Bi-directional mechanical properties of the posterior region of the glenohumeral capsule. J Biomech. 2005;38:1365-1369.
107 Clark JM, Harryman DT2nd. Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713-725.
108 Gerber C, Werner CM, Macy JC, et al. Effect of selective capsulorrhaphy on the passive range of motion of the glenohumeral joint. J Bone Joint Surg Am. 2003;85:48-55.
109 Ferrari DA. Capsular ligaments of the shoulder. Anatomical and functional study of the anterior superior capsule. Am J Sports Med. 1990;18:20-24.
110 Bowen MK, Warren RF. Ligamentous control of shoulder stability based on selective cutting and static translation experiments. Clin Sports Med. 1991;10:757-782.
111 Nobuhara K, Ikeda H. Rotator interval lesion. Clin Orthop Relat Res. 1987;223:44-50.
112 Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res. 2002;400:32-39.
113 Basmajian J. Muscles Alive, 4th ed. Baltimore: Williams & Wilkins, 1979.
114 Gagey OJ, Boisrenoult P. Shoulder capsule shrinkage and consequences on shoulder movements. Clin Orthop Relat Res. 2004;419:218-222.
115 Blasier RB, Guldberg MS, Rothman ED. Anterior shoulder stability: Contributions of rotator cuff forces and the capsular ligaments in a cadaver model. J Shoulder Elbow Surg. 1992;1:140-150.
116 O’Brien SJ, Schwartz RS, Warren RF, Torzilli PA. Capsular restraints to anterior-posterior motion of the abducted shoulder: A biomechanical study. J Shoulder Elbow Surg. 1995;4:298-308.
117 Kuhn JE, Huston LJ, Soslowsky LJ, et al. External rotation of the glenohumeral joint: Ligament restraints and muscle effects in the neutral and abducted positions. J Shoulder Elbow Surg. 2005;14(suppl):39S-48S.
118 Bigliani LU, Pollock RG, Soslowsky LJ, et al. Tensile properties of the inferior glenohumeral ligament. J Orthop Res. 1992;10:187-197.
119 Pollock RG, Wang VM, Bucchieri JS, et al. Effects of repetitive subfailure strains on the mechanical behavior of the inferior glenohumeral ligament. J Shoulder Elbow Surg. 2000;9:427-435.
120 Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part I: Pathoanatomy and biomechanics. Arthroscopy. 2003;19:404-420.
121 Snyder SJ, Karzel RP, Del Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274-279.
122 Andrews JR, Kupferman SP, Dillman CJ. Labral tears in throwing and racquet sports. Clin Sports Med. 1991;10:901-911.
123 Burkhart SS, Morgan CD. The peel-back mechanism: Its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14:637-640.
124 Wilk KE, Andrews JR, Arrigo CA. The physical examination of the glenohumeral joint: Emphasis on the stabilizing structures. J Orthop Sports Phys Ther. 1997;25:380-389.
125 Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: Influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14:986-993.
126 Kelkar R, Wang VM, Flatow EL, et al. Glenohumeral mechanics: A study of articular geometry, contact, and kinematics. J Shoulder Elbow Surg. 2001;10:73-84.
127 Labriola JE, Lee TQ, Debski RE, McMahon PJ. Stability and instability of the glenohumeral joint: The role of shoulder muscles. J Shoulder Elbow Surg. 2005;14(suppl):32S-38S.
128 Poppen NK, Walker PS. Forces at the glenohumeral joint in abduction. Clin Orthop Relat Res. 1978;135:165-170.
129 Wuelker N, Korell M, Thren K. Dynamic glenohumeral joint stability. J Shoulder Elbow Surg. 1998;7:43-52.
130 Cain PR, Mutschler TA, Fu FH, Lee SK. Anterior stability of the glenohumeral joint. A dynamic model. Am J Sports Med. 1987;15:144-148.
131 DePalma AF, Cooke AJ, Prabhakar M. The role of the subscapularis in recurrent anterior dislocations of the shoulder. Clin Orthop Relat Res. 1967;54:35-49.
132 Matsen FA3rd, Thomas SC, Rockwood CA. Anterior glenohumeral instability. In: Rockwood CA, Matsen FA3rd, editors. The Shoulder. Philadelphia: WB Saunders; 1990:526-622.
133 Symeonides PP. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br. 1972;54:476-483.
134 Labriola JE, Jolly JT, McMahon PJ, Debski RE. Active stability of the glenohumeral joint decreases in the apprehension position. Clin Biomech (Bristol Avon). 2004;19:801-809.
135 McQuade KJ, Murthi AM. Anterior glenohumeral force/translation behavior with and without rotator cuff contraction during clinical stability testing. Clin Biomech (Bristol Avon). 2004;19:10-15.
136 Lee SB, Kim KJ, O’Driscoll SW, et al. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion. A study in cadavera. J Bone Joint Surg Am. 2000;82:849-857.
137 Hawkins RJ, Misamore GW, Hobeika PE. Surgery for full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1985;67:1349-1355.
138 Schwartz E, Warren RF, O’Brien SJ, Fronek J. Posterior shoulder instability. Orthop Clin North Am. 1987;18:409-419.
139 Detrisac D, Johnson L. Arthroscopic Shoulder Anatomy. Thorofare, NJ: Slack, 1986.
140 Lee SB, An KN. Dynamic glenohumeral stability provided by three heads of the deltoid muscle. Clin Orthop Relat Res. 2002;400:40-47.
141 Itoi E, Newman SR, Kuechle DK, et al. Dynamic anterior stabilisers of the shoulder with the arm in abduction. J Bone Joint Surg Br. 1994;76:834-836.
142 Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: Three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14:553-565.
143 Neer CS2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897-908.
144 Kumar VP, Balasubramaniam P. The role of atmospheric pressure in stabilising the shoulder. An experimental study. J Bone Joint Surg Br. 1985;67:719-721.
145 Cools AM, Witvrouw EE, Declercq GA, et al. Scapular muscle recruitment patterns: Trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31:542-549.
146 Ito N. Electromyographic study of shoulder joint. Nippon Seikeigeka Gakkai Zasshi. 1980;54:1529-1540.
147 Laumann U. Kinesiology of the shoulder joint. In: Kôlbel R, Helbig B, Blauth W, editors. Shoulder Replacement. Berlin: Springer-Verlag; 1987:23-31.
148 Kelley M. Clinical evaluation of the shoulder. In: Mackin E, Callahan A, Skirven T, editors. Rehabilitation of the Hand and Upper Extremity. 5th ed. St. Louis: Mosby; 2002:1311-1350.
149 Kelley M, Brenneman S: The scapular flip sign: An examination sign to identify the presence of a spinal accessory nerve palsy. Presented at the APTA Combined Sections Meeting, New Orleans, February 2000.
150 Nuber GW, Bowman ID, Perry JP, et al. EMG analysis of classical shoulder motion. Trans Orthop Res Soc. 11, 1986.
151 Shevlin MG, Lehmann JF, Lucci JA. Electromyographic study of the function of some muscles crossing the glenohumeral joint. Arch Phys Med Rehabil. 1969;50:264-270.
152 Sugahara R. Electromyographic study of shoulder movements. Jpn J Rehab Med. 1974;11:41-52.
153 Lucas DB. Biomechanics of the shoulder joint. Arch Surg. 1973;107:425-432.
154 Radin EL. Biomechanics and functional anatomy. In: Post M, editor. The Shoulder: Surgical and Nonsurgical Management. 2nd ed. Philadelphia: Lea & Febiger; 1988:54-60.
155 Matsen FA3rd. Biomechanics of the shoulder. In: Frankel VH, Nordin M, editors. Basic Biomechanics of the Skeletal System. Philadelphia: Lea & Febiger; 1980:221-242.
156 Zuckerman JD, Matsen FA3rd. Biomechanics of the shoulder. In: Zuckerman JD, Matsen FA3rd, editors. Basic Biomechanics of the Musculoskeletal System. Philadelphia: Lea & Febiger; 1989:225-247.
157 Deutsch A, Altchek DW, Schwartz E, et al. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186-193.
158 Hawkins RJ, Bell RH, Hawkins RH, Koppert GJ. Anterior dislocation of the shoulder in the older patient. Clin Orthop Relat Res. 1986;206:192-195.
159 Weiner DS, Macnab I. Superior migration of the humeral head. A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1970;52:524-527.
160 Chen SK, Simonian PT, Wickiewicz TL, et al. Radiographic evaluation of glenohumeral kinematics: A muscle fatigue model. J Shoulder Elbow Surg. 1999;8:49-52.
161 De Duca CJ, Forrest WJ. Force analysis of individual muscles acting simultaneously on the shoulder joint during isometric abduction. J Biomech. 1973;6:385-393.
162 Colachis SCJr, Strohm BR. Effect of suprascapular and axillary nerve blocks on muscle force in upper extremity. Arch Phys Med Rehabil. 1971;52:22-29.
163 Colachis SCJr, Strohm BR, Brechner VL. Effects of axillary nerve block on muscle force in the upper extremity. Arch Phys Med Rehabil. 1969;50:647-654.
164 Howell SM, Imobersteg AM, Seger DH, Marone PJ. Clarification of the role of the supraspinatus muscle in shoulder function. J Bone Joint Surg Am. 1986;68:398-404.
165 Markhede G, Monastyrski J, Stener B. Shoulder function after deltoid muscle removal. Acta Orthop Scand. 1985;56:242-244.
166 Staples OS, Watkins AL. Full active abduction in traumatic paralysis of the deltoid. J Bone Joint Surg. 1943;25:85.
167 Kuhlman JR, Iannotti JP, Kelly MJ, et al. Isokinetic and isometric measurement of strength of external rotation and abduction of the shoulder. J Bone Joint Surg Am. 1992;74:1320-1333.
168 Scepi M, Faure JP, Ridoux N, et al. A three-dimensional model of the shoulder girdle. Forces developed in deltoid and supraspinatus muscles during abduction. Surg Radiol Anat. 2004;26:290-296.
169 Celli L, Balli A, de Luise G, Rovesta C. Some new aspects of the functional anatomy of the shoulder. Ital J Orthop Traumatol. 1985;11:83-91.
170 Mura N, O’Driscoll SW, Zobitz ME, et al. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: A biomechanical study. J Shoulder Elbow Surg. 2003;12:179-184.
171 Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12:218-220.
172 Kadefors R, Petersen I, Herberts P. Muscular reaction to welding work: An electromyographic investigation. Ergonomics. 1976;19:543-548.
173 Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med. 1983;2:247-270.
174 Blackburn T, McLeod W, White B, Wofford L. Analysis of posterior rotator cuff exercise. Athl Train. 1990;25:40-45.
175 Jobe FW, Tibone JE, Perry J, Moynes D. An EMG analysis of the shoulder in throwing and pitching. A preliminary report. Am J Sports Med. 1983;11:3-5.
176 Kumar VP, Satku K, Balasubramaniam P. The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop Relat Res. 1989;244:172-175.