Mast Cell Tumors
The neoplastic proliferation of mast cells referred to as a mast cell tumor (MCT; histiocytic mastocytoma, mast cell sarcoma) represents the most commonly encountered cutaneous tumor in the dog and the second most common cutaneous tumor in the cat.1-5 Systemic forms of the disease are often referred to as mastocytosis. Canine and feline forms of the disease will be considered separately in this chapter because many differences exist with regard to histologic type, biologic behavior, therapy, and prognosis.
Canine Mast Cell Tumors
Mast cell precursors leave the bone marrow and migrate to various tissues throughout the body where they undergo differentiation into mature mast cells with their characteristic cytoplasmic granules, which stain metachromatically with Giemsa and toluidine blue.6 These granules contain a number of bioactive substances, including heparin, histamine, preformed tumor necrosis factor-α (TNF-α), and several proteases.6 The nature and composition of mast cell granules are highly influenced by the microenvironment in which the mast cells mature. For example, in dogs, mast cells in the gastrointestinal (GI) tract express primarily chymase, whereas mast cells in the skin express both chymase and tryptase.7 When stimulated, mast cells can rapidly produce a variety of proteases (chymase, tryptase), cytokines (TNF-α, interleukin-6 [IL-6]), chemokines (CCL2, CXCL1), growth factors (vascular endothelial growth factor [VEGF], basic fibroblast growth factor [bFGF]), and lipid mediators (prostaglandin D2 [PGD2], leukotriene C4 [LTC4]).6 Through this process, mast cells participate in several biologic activities, including wound healing, induction of innate immune responses, antiparasite activity, and modulation of reaction to insect and spider venoms.6,8
Normal canine mast cells can be generated from bone marrow–derived hematopoietic precursors.9,10 These cells, known as canine bone marrow–derived mast cells (cBMMCs), have been used to characterize the functional properties of mast cells in this species. As with normal human mast cells, their differentiation requires the presence of the growth factor stem cell factor (SCF) and can be influenced by the presence of other cytokines.9,10 When stimulated, these cells rapidly release histamine, monocyte chemotactic protein-1 (MCP-1), TNF-α, and tryptase, and they produce several additional cytokines and chemokines, including IL-3, IL-13, granulocyte-macrophage colony-stimulating factor (GM-CSF), and macrophage inflammatory protein 1α (MIP1α).9,10 Interestingly, the cBMMCs are extremely sensitive to chemical degranulation, which may help to explain why dogs exhibit such a high degree of hypersensitivity to several chemical agents, including polysorbate 80, Cremophor EL, and doxorubicin.9 The function of cBMMCs can be modulated by cytokines, steroids, and nonsteroidal antiinflammatory drugs (NSAIDs).9-11
Incidence and Risk Factors
MCTs represent the most common cutaneous tumor in the dog, accounting for between 16% and 21% of all cutaneous tumors.1,3,5,12 Although MCTs are primarily a disease of older dogs (mean age approximately 8 to 9 years), they have also been reported in younger dogs and there is no apparent gender predilection.1,3,5,13 Most tumors occur in mixed breeds; however, several breeds are at an increased risk for MCTs, including dogs of bulldog descent (Boxers, Boston terriers, English bulldogs, pugs), Labrador and golden retrievers, cocker spaniels, schnauzers, Staffordshire terriers, beagles, Rhodesian ridgebacks, Weimaraners, and Shar-Peis.1,5,14-16 The increased incidence of MCTs in certain breeds suggests the possibility of an underlying genetic cause,15 and studies are ongoing to identify these putative genetic risk factors. Interestingly, although dogs of bulldog ancestry are at higher risk for MCT development, it is generally accepted that MCTs in these dogs are more likely to behave in a benign fashion.1 Additionally, it was recently demonstrated that pugs may develop multiple MCTs that behave in a benign fashion.17 In contrast, anecdotal evidence suggests that Shar-Peis develop MCTs that may be more biologically aggressive. Spontaneously regressing MCTs in young animals have been described in cats, pigs, horses, and humans. Multiple cutaneous MCTs that regressed within 27 weeks were reported in a 3-week-old Jack Russell terrier.18 This syndrome of spontaneous regression in young animals may indicate a hyperplastic or dysplastic syndrome rather than a true neoplastic lesion.
The etiology of MCTs in the dog is for the most part unknown. Historically, MCTs have been associated with chronic inflammation or the application of skin irritants; however, the epidemiology of disease in dogs does not support the role of a topical carcinogen.19-21 Unequivocal evidence is lacking for a viral etiology, although MCTs have been transplanted to very young or immunocompromised laboratory dogs using tumor cell tissues and rarely by cell-free extracts.22-24 No C-type or other identifiable virus particles have been observed, and no epidemiologic evidence exists to suggest horizontal transmission. Chromosomal fragile site expression, a phenomenon thought to genetically predispose humans to develop certain tumors, was shown to be increased in Boxers with MCTs.25 However, the control population for this study was young, non–tumor-bearing Boxers, and the increased expression of chromosomal fragile sites may be due to this age difference.
The genetic changes that predispose dogs to MCTs are incompletely understood. Alterations in the p53 tumor suppressor pathway have been identified in some canine MCTs,26-28 but p53 sequencing in a limited number of cases has revealed no mutations.29 Perturbations in expression of the proteins p21 and p27, which are cyclin-dependent kinase inhibitors (CDKIs) that contribute to regulation of the cell cycle, have been identified in many canine MCTs.30 Cytosolic receptors for estrogen and progesterone have also been detected in canine MCTs.31 Their role in the etiopathogenesis of MCT is poorly understood, but evidence exists that estrogen and progesterone may influence mast cell function.32 One European study reported that female dogs with MCTs had a more favorable prognosis with chemotherapy.33 Although the majority of studies performed in the United States have failed to detect such an association, the relatively higher frequency of intact females present in the European population may have allowed the effect of sex hormones to have a greater statistical impact on biologic behavior.
Perhaps the best-described molecular abnormality in canine MCT involves the receptor tyrosine kinase (RTK), KIT. KIT is expressed normally on a variety of cells, including hematopoietic stem cells, melanocytes, and mast cells, among others.34-36 The ligand for KIT, SCF, induces KIT dimerization, subsequent phosphorylation, and generation of intracellular signaling that promotes the proliferation, differentiation, and maturation of normal mast cells.34-36 SCF is essential for the differentiation of mature mast cells from CD34+ hematopoietic stem cells in vitro, and inhibition of KIT signaling induces apoptosis of cBMMCs.10,35,36 KIT expression has been demonstrated on canine MCTs, and aberrant cytoplasmic localization of KIT in MCTs may be associated with dysregulated KIT function.37-40 A significant proportion of canine MCTs possess mutations in the c-kit gene involving either the juxtamembrane domain (exons 11 and 12) or extracellular domain (exons 8 and 9).41-45 These mutations result in SCF-independent activation of KIT and subsequent unregulated KIT signal transduction.43,44 In dogs, activating c-kit mutations appear to be present in 25% to 30% of intermediate-grade and high-grade MCTs, and evidence suggests that they are linked to increased risk of local recurrence, metastasis, and a worse prognosis.41,44,46-48 The reason for the high rate of c-kit mutations in dog MCTs is unknown; however, it is clear that these mutations are not germline in nature.
History and Clinical Signs
The vast majority of MCTs in dogs occur in the dermis and subcutaneous tissue,5,49 and most are solitary in nature, although 11% to 14% of dogs present with multiple lesions.50-52 Approximately 50% of cutaneous MCTs occur on the trunk and perineal region, 40% on the limbs, and 10% on the head and neck.20,53,54 MCTs have also been reported to occur on other sites, including the conjunctiva, salivary gland, nasopharynx, larynx, oral cavity, ureter, and spine.55-59 A visceral form of MCT, often referred to as disseminated or systemic mastocytosis, has also been documented, although it is usually preceded by an aggressive primary lesion.60-64 Infiltration of abdominal lymph nodes, spleen, liver, and bone marrow is commonly observed in the setting of visceral disease, and pleural/peritoneal effusions containing neoplastic mast cells have been documented. A case series of dogs with primary GI MCTs was recently reported in which most dogs presented with vomiting, diarrhea, and melena. Only 40% of the dogs were alive at 30 days after first admission, and fewer than 10% were alive at 6 months.28
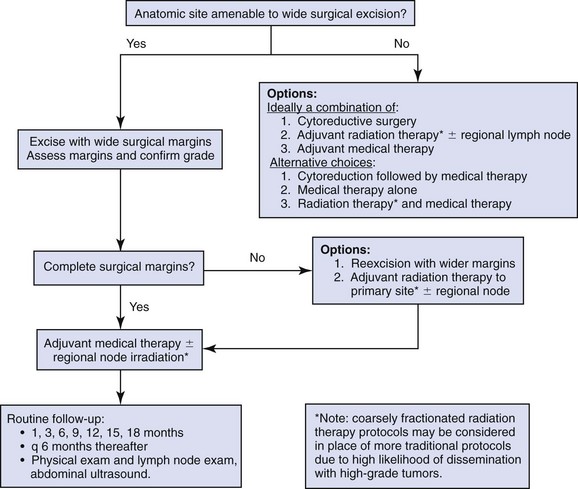
It is important to note that cutaneous MCTs have an extremely varied range of clinical appearances, and they are sometimes inadvertently mistaken for nonneoplastic lesions. Well-differentiated MCTs tend to be solitary, small, slow-growing tumors that may have been present for several months. They are not typically ulcerated, but overlying hair may be lost. Undifferentiated MCTs tend to be rapidly growing, ulcerated lesions that cause considerable irritation and attain a large size. Surrounding tissues may become inflamed and edematous. Small satellite nodules may develop in surrounding tissues. Tumors of intermediate differentiation fill the spectrum between these two extremes. A subcutaneous form of MCT that is soft and fleshy on palpation is often misdiagnosed clinically as a lipoma (Figure 20-1).
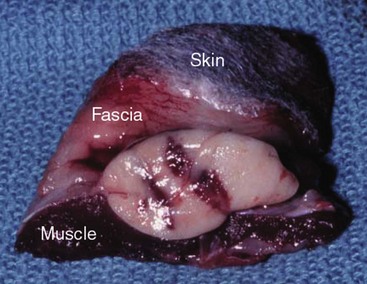
Figure 20-1 Subcutaneous MCT from the shoulder of a dog. This mass was originally misdiagnosed as a lipoma based on palpation alone. Note tumor extension through fascia and muscle. Wide surgical excision to include deep muscle layer is necessary to achieve complete (“clean”) surgical margins.
The history and clinical signs of dogs with MCTs may be complicated by signs attributable to the release of histamine, heparin, and other vasoactive amines from mast cell granules. Occasionally, mechanical manipulation during examination of the tumor results in degranulation and subsequent erythema and wheal formation in surrounding tissues. This phenomenon has been referred to as Darier’s sign (Figure 20-2)51 and can also occur spontaneously; dog owners may describe the tumor as increasing and decreasing in size. GI ulceration has been documented in 35% to 83% of dogs with MCTs that underwent necropsy.65,66 Histamine released from MCT granules is thought to act on parietal cells via H2 receptors, resulting in increased hydrochloric acid secretion. Plasma histamine concentrations have been shown to be high in dogs with MCTs, and there is preliminary information that monitoring of plasma histamine concentrations may be useful in assessing disease progression.67 These dogs also have decreased concentrations of plasma gastrin, which is normally released by antral G-cells in response to increased gastric hydrochloric acid concentrations, acting as a negative feedback loop. Dogs with substantial MCT burden (i.e., large tumors, metastatic disease, systemic disease) are much more likely to present with clinical signs related to the release of mast cell mediators. These may include vomiting, diarrhea, fever, peripheral edema, and, rarely, collapse.

Figure 20-2 Erythema and wheal formation occurred in surrounding skin following manipulation of this cutaneous MCT. This phenomenon, resulting from the release of vasoactive amines from mast cell granules, is known as Darier’s sign.
Perioperative degranulation of MCTs and subsequent release of histamine and other less-characterized vasoactive substances may also result in potentially life-threatening hypotensive events during surgery. It is thought that prostaglandins in the D series secreted by tumor cells may mediate the hypotensive effects observed in humans with mast cell diseases.68,69 Coagulation abnormalities, also reported in dogs with MCTs, are likely due to heparin release from mast cell granules.63,70 Although clinical evidence of hemorrhage is not typically associated with this phenomenon, localized hemorrhage at the time of surgery as the result of degranulation following tumor manipulation can be a serious complication, even in the presence of normal presurgical coagulation parameters.
Prognostic Factors
A discussion of prognostic factors associated with canine MCTs will precede sections on diagnosis and treatment because steps followed in those sections are predicated on the presence or absence of these prognostic factors. Table 20-1 lists factors known to be predictive of biologic behavior and clinical outcome in dogs with MCTs. It is important to note that no one factor is entirely predictive of biologic behavior; thus all prognostic indicators should be taken into consideration when evaluating a patient.
Table 20-1
Prognostic Factors for Mast Cell Tumors in Dogs
| Factor | Comment |
| Histologic grade | Strongly predictive of outcome. Dogs with undifferentiated tumors typically die of their disease following local therapy alone, whereas those with well-differentiated tumors are usually cured with appropriate local therapy. |
| Clinical stage | Stages 0 and I, confined to the skin without local lymph node or distant metastasis, have a better prognosis than higher-stage disease. |
| Location | Subungual, oral, and other mucous membrane sites are associated with more high-grade tumors and worse prognosis. Preputial and scrotal tumors are also associated with a worse prognosis. Subcutaneous tumors may have a better prognosis. Visceral or bone marrow disease usually carries a grave prognosis. |
| Cell proliferation rate | MI, relative frequency of AgNORs, percentage of PCNA, or Ki67 immunopositivity are predictive of postsurgical outcome. |
| Growth rate | MCTs that remain localized and are present for prolonged periods of time (months or years) without significant change are usually benign. |
| DNA ploidy | There is a trend toward shorter survival times and higher-stage disease in dogs with aneuploid tumors. |
| Microvessel density | Increased microvessel density is associated with higher grade, a higher degree of invasiveness, and a worse prognosis. |
| Recurrence | Local recurrence following surgical excision may carry a more guarded prognosis. |
| Systemic signs | The presence of systemic illness (e.g., anorexia, vomiting, melena, GI ulceration) may be associated with higher-stage disease. |
| Age | Older dogs may have shorter median DFIs when treated with RT than younger dogs. |
| Breed | MCTs in Boxers (and potentially other brachycephalic breeds) tend to be low or intermediate grade and are thus associated with a better prognosis. |
| Sex | Male dogs had a shorter survival time than female dogs when treated with chemotherapy. |
| Tumor size | Large tumors may be associated with a worse prognosis following surgical removal and/or RT. |
| c-kit mutation | The presence of an activating mutation in the c-kit gene is associated with a worse prognosis. |
MI, Mitotic index; AgNORs, argyrophilic nucleolar organizer regions; PCNA, proliferating cell nuclear antigen; MCTs, mast cell tumors; GI, gastrointestinal; DFIs, disease-free intervals; RT, radiation therapy.
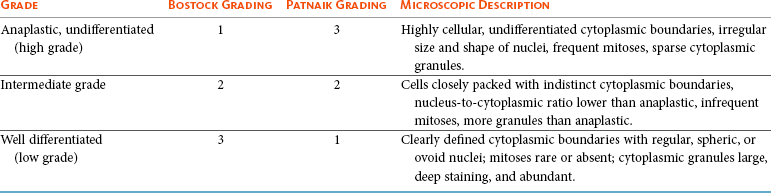
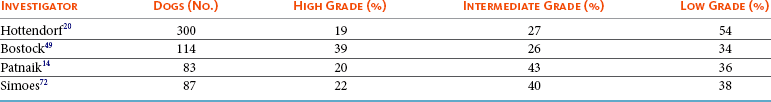
Histologic grade is considered the most consistent and reliable prognostic factor available for dogs with MCTs, although it will not predict the behavior of every tumor.14,49,71,72 Several investigators have applied histologic grading systems to canine MCTs based on degree of differentiation (Table 20-2). The number grades used in these studies are at odds. Therefore, for the sake of clarity, the three differentiation groups should be simply referred to as undifferentiated (high) grade, intermediate grade, and well-differentiated (low) grade. Table 20-3 lists the relative distribution of MCT grades encountered in larger series. Survival following surgical excision based on grade is presented in Table 20-4. The vast majority of dogs with well-differentiated tumors (80% to 90%) and approximately 75% of dogs with intermediate-grade tumors experience long-term survival following complete surgical excision.50,71,74-77 Metastatic rates for undifferentiated tumors range from 55% to 96%, and most dogs with these tumors die of their disease within 1 year.49,78 The majority disseminate first to local lymph nodes, then to the spleen and liver. Other visceral organs may be involved; however, lung involvement is infrequent. Neoplastic mast cells may be observed in the bone marrow and peripheral blood in cases of widespread systemic dissemination.63
Table 20-4
Survival Times of Dogs with Surgically Treated Mast Cell Tumors According to Histologic Grade*
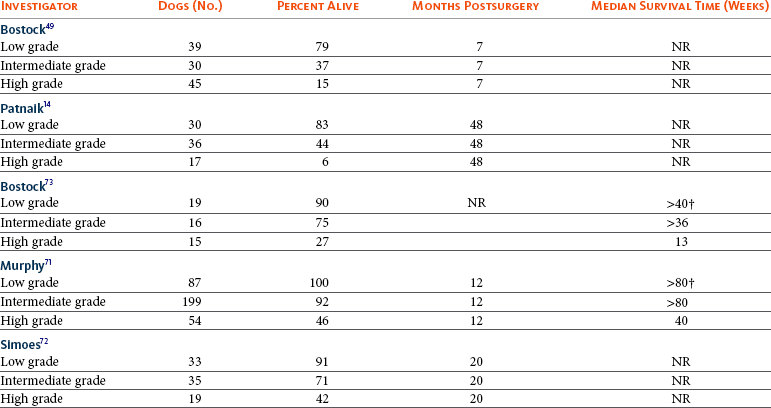
*Unclear in these studies if death due to metastasis or local recurrence.
†Medians not reached at the time of last follow-up (i.e., >50% alive).
The current histopathologic grading system does not detect a small percentage (15% to 30%) of those well-differentiated or intermediately differentiated MCTs that result in the death of affected dogs; this is complicated by the fact that there is disagreement in tumor grading among pathologists. In one study, there was significant variation among pathologists in grading a specific set of MCTs (p < 0.001), although this was found to be less so if all pathologists strictly employed the system described by Patnaik.14,79,80 Recently, an attempt was made to develop a new grading system that would separate tumors into high or low grade based on one of four features identified on histopathologic evaluation.81 In this setting, tumors would be classified as high grade if they possessed (1) at least seven mitotic figures/10 HPF, (2) at least three multinucleated cells/10 HPF, (3) at least three bizarre nuclei/10 HPF, or (4) karyomegaly. In a series of 95 dogs evaluated by both the Patnaik system and this alternative system, the alternative system was somewhat better at predicting which dogs would be more likely to die of disease81; however, further validation of this new two-tiered system will be necessary to determine whether it is truly better than the more commonly used Patnaik three-tiered system for predicting the biologic behavior of MCTs.
Several markers of proliferation have been evaluated to assist in determining whether an MCT is likely to behave in a more aggressive manner.47,72,82-90 Ki67 is a protein found in the nucleus, the levels of which appear to correlate with cell proliferation. In one study, the mean number of Ki67-positive nuclei was significantly higher for dogs that died of MCTs than for those that survived.83 In another study, the Ki67 score was used to divide intermediate-grade MCTs into two groups with markedly different expected survival times.84 Silver colloid staining of paraffin-embedded sections can be used to determine the relative presence of argyrophilic nucleolar organizer regions (AgNORs), another surrogate marker of proliferation. These have been correlated with histologic grade and postsurgical outcome.72,73 In a study of 50 dogs with cutaneous MCTs, the AgNOR frequency was as predictive or more predictive of biologic behavior than histologic grade.73 Finally, proliferating cell nuclear antigen (PCNA), another indicator of cell proliferation, has been used to determine the biologic behavior of MCTs, although this is probably not as reliable as the other markers.72,73,91 The previously discussed markers of proliferation all require the use of special stains. In contrast, the mitotic index (MI), or number of mitoses/10 HPF in hematoxylin and eosin (H&E) sections, has been used to assess the biologic behavior of canine MCTs.92 In one study, those dogs with tumors possessing an MI of 5 or lower had a median survival time (MST) of 80 months, compared to 3 months for those possessing an MI of more than 5, suggesting that the MI is a strong predictor of overall survival for dogs with MCTs. Additional studies have also found a role for MI in MCT prognosis.81,90,92-95
Other cellular assessments have been employed to evaluate the biologic behavior of MCT. A study of DNA ploidy determined by flow cytometric analysis suggested a trend toward shorter survival and higher clinical stage of disease in aneuploid tumors compared to diploid tumors.96 Recent studies have found a correlation between intratumor microvessel density and invasiveness, mitotic rate, and prognosis82,97 and a correlation between nuclear characteristics (assessed by computerized morphometry) and outcome and grade.98,99 The potential role of KIT dysregulation in MCT prognosis was investigated by assessing KIT immunohistochemical staining patterns on histopathologic specimens.100 Three distinct patterns were identified: membrane, focal/stippled, and diffuse cytoplasmic staining. Although there was some evidence that dogs with diffuse cytoplasmic KIT staining patterns did not live as long as those with other patterns, no group reached an MST and most dogs in each of the KIT staining groups evaluated experienced extremely long survival times postsurgery.100 In contrast, the presence of c-kit–activating mutations has been associated with a higher rate of local recurrence, metastasis, and death from disease, suggesting that KIT dysregulation confers a more aggressive phenotype to MCTs.41,46,47 Finally, investigators have attempted to correlate histologic grading of MCTs with a combined Ki67/PCNA/AgNOR/KIT immunohistochemical scoring.101 No significant correlation was found for KIT staining and MCT grade, but high Ki67/PCNA/AgNOR scores all did correlate positively with tumor grade (i.e., higher scores for higher grade). This suggests that proliferation indices increase with increasing grade and are ultimately reflected in the eventual biologic behavior of the tumor.
Tumor location has been investigated as a potential prognostic indicator.50,102-108 Tumors in the preputial/inguinal area, subungual (nailbed) region (Figure 20-3), and other mucocutaneous sites, including the oral cavity and perineum, have been associated historically with aggressive behavior. Two reports did not show a negative prognosis for tumors occurring in the inguinal and perineal region; however, when preputial and scrotal regions were specifically evaluated, they were indeed associated with a poorer prognosis.106,107 Approximately 50% to 60% of dogs with MCTs located in the muzzle present with regional lymph node metastasis.108,109 Interestingly, this does not necessarily indicate a worse long-term prognosis because the MST for dogs with metastatic disease was 14 months.108 MCTs that originate in the viscera (GI tract, liver, spleen) or bone marrow carry a grave prognosis.62,63 Recent data indicate that MCTs arising in the subcutaneous tissues have a favorable prognosis, with extended survival time and low rates of recurrence and metastasis. In one study of 306 dogs with subcutaneous MCTs, metastasis occurred in 4% of dogs and 8% experienced local recurrence.95 The estimated 2- and 5-year survival probabilities were 92% and 86%, respectively. Decreased survival was linked to MI higher than 4, infiltrative growth pattern, and presence of multinucleation. Finally, conjunctival MCTs were found to have a good prognosis, with 15/32 dogs disease free at a mean of 21.4 months postsurgery; no dogs in this study died of MCT-related disease.110

Figure 20-3 Subungual undifferentiated MCT in an English bulldog. As with some MCTs in this location, early lymph node metastasis has occurred.
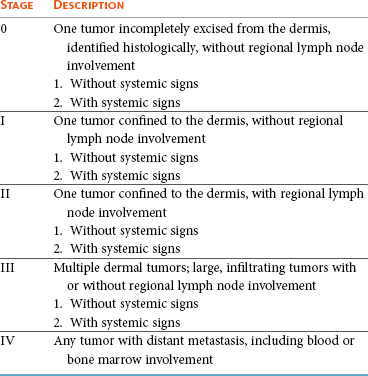
Clinical stage, represented in Table 20-5, is also predictive of outcome.33,49,96,105,111 There is controversy regarding the effect of multiple MCTs on prognosis, and as such, this part of the staging scheme may not accurately correlate with outcome. Several studies indicate that there is no difference in outcome between patients with a single cutaneous MCT and those with multiple MCTs,50,112-114 whereas others have suggested an inferior outcome in dogs with multiple tumors.94,115 It is uncertain at this time whether this phenomenon represents an atypical form of metastasis or multiple, unrelated tumors arising independently, although one study demonstrated a clonal origin for two distant cutaneous tumors arising over years.116 The effect of lymph node metastasis on prognosis is also somewhat controversial. In two studies, the presence of mast cells in the regional lymph node was a negative prognostic factor for survival and disease-free interval (DFI)113,117; however, an additional study revealed that dogs with intermediately differentiated MCTs and lymph node metastasis treated with radiation therapy (RT) postsurgery achieved long-term survival.118 Other studies have shown that dogs with intermediately differentiated MCT with lymph node metastasis may have a good prognosis if the affected lymph node is removed and adjuvant chemotherapy is administered.113,114,119 For poorly differentiated tumors, the presence of metastatic disease resulted in an MST of 194 days compared to 503 days for dogs with no metastasis.78 For these dogs, treatment of the lymph node improved survival time (240 days) compared to those dogs whose lymph nodes were not treated (42 days).78 As with all cases, clinical judgment regarding lymph node metastasis is probably important. A dog with an effaced enlarged lymph node will be more likely to fail therapy when compared to a dog with a lymph node that is not clinically enlarged but has cytologic evidence of metastasis.
Several miscellaneous factors have been linked to prognosis in dogs with MCTs. Certain breeds of dogs such as Boxers, pugs, and dogs of bulldog descent appear to develop MCTs that often behave in a more benign fashion.1,17,49 Recent rapid growth has been associated with a worse outcome. For example, in one study, 83% of dogs with tumors present for longer than 28 weeks prior to surgery survived for at least 30 weeks, compared to only 25% of dogs with tumors present for less than 28 weeks.49 Systemic signs of anorexia, vomiting, melena, widespread erythema, and edema associated with vasoactive substances from mast cell degranulation are more commonly associated with visceral forms of MCT and carry a more guarded prognosis.50,63,64 In 16 cases of visceral MCTs, an MST of 90 days was reported and all dogs with follow-up died of their disease.103 Local tumor ulceration, erythema, or pruritus has been associated with a worse prognosis in some studies.50,113 Finally, recurrence of MCT following surgical excision has also been associated with a more guarded prognosis.113 Thus appropriate aggressive therapy at the time of first presentation, rather than at the time of recurrence, may improve the long-term prognosis in patients with MCTs.
Diagnostic Technique and Work-Up
MCTs are initially diagnosed on the basis of fine-needle aspiration (FNA) cytology. The Romanowsky or rapid hematologic-type stains used in most practices will suffice. Mast cells appear as small to medium-sized round cells with abundant, small, uniform cytoplasmic granules that stain purplish red (metachromatic; see Figures 7-2 and 7-5).1,120 A small percentage of MCTs have granules that do not stain readily, giving them an epithelial or macrophage-like appearance that has often been referred to as a “fried-egg” appearance (see Figure 7-2). In these cases, a Wright-Giemsa or toluidine blue stain will often reveal granules; however, histologic assessment may ultimately be necessary. Highly anaplastic, agranular MCTs can sometimes be challenging to definitively diagnose by routine light microscopy. Immunohistochemical techniques have been applied in an attempt to differentiate these from other anaplastic round cell tumors. MCTs are vimentin positive, and the majority are tryptase and CD117 (KIT) positive.37,121-123 Other markers that could potentially be useful include chymase, MCP-1, and IL-8.9,10
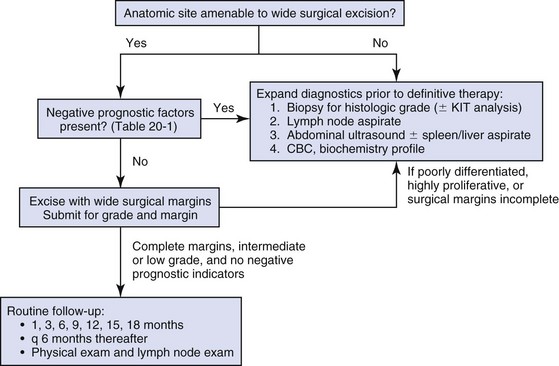
Historically, complete staging has included a minimum database (complete blood count [CBC], serum biochemistry profile), a buffy coat smear to document peripheral mastocytosis, cytologic assessment of regional lymph nodes, abdominal ultrasound (US) with cytologic assessment of spleen or liver if warranted, thoracic radiographs, and bone marrow aspiration cytology. It is now likely that an extensive work-up is not necessary for dogs with MCTs that do not exhibit the previously discussed negative prognostic factors. Figure 20-4 illustrates the diagnostic steps and the order in which they are pursued in the authors’ practice. If the MCT is in a location amenable to wide surgical excision and no negative prognostic indicators are present (see Table 20-1), no further tests other than the minimum database and FNA of the regional lymph node (if possible) are performed prior to wide surgical excision. FNA cytology is not sufficient to grade MCT; thus histologic assessment following excision is strongly recommended to provide guidance regarding necessary further diagnostics and therapeutics.
If the tumor presents at a site that is not amenable to wide surgical excision (e.g., distal extremity) or if negative prognostic factors exist in the history or physical examination, ancillary diagnostics to further stage the disease are recommended prior to definitive therapy. An incisional/needle biopsy may be performed at this point for determination of histologic grade. The minimum staging that is advisable in those cases requiring presurgical staging consists of a minimum database, FNA cytology of the regional lymph node (even if normal size), and abdominal US. With respect to cytologic evaluation of lymph nodes, definitive criteria for metastatic disease can be challenging if mast cells are present in low numbers because mast cells are normally found in lymph nodes and their numbers can be increased in the presence of infection and ulceration, which are sometimes observed in MCTs. For example, in 56 healthy beagle dogs, approximately 24% of lymph node aspirates contained mast cells (range of 1 to 16 mast cells/slide, mean of 6.4 cells/slide).124 Therefore an occasional solitary mast cell is not indicative of metastasis; rather, clustering and aggregates are more worrisome (Figure 20-5).111 Surgical removal of a cytologically suspicious lymph node for histologic assessment may be necessary to accurately determine whether mast cells present in the lymph node truly represent metastatic disease. Abdominal US is now considered an important diagnostic test for the evaluation of dogs with potentially aggressive MCTs. Although FNA cytology of structurally normal livers or spleens is generally unrewarding,125,126 the presence of negative prognostic indicators (e.g., metastatic lymph node, clinical signs) is sufficient justification to perform cytologic evaluation of these organs even if they appear normal on US.127
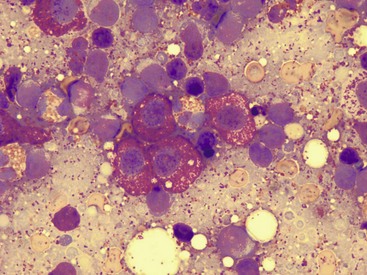
Figure 20-5 Regional lymph node aspirate from a dog with a cutaneous MCT. Note the clustering of mast cells in a background of lymphocytes that is more indicative of true metastasis.
Thoracic radiographs rarely demonstrate metastasis; however, it is reasonable to procure them prior to an expensive or invasive procedure to rule out occult cardiopulmonary disease that could complicate anesthesia or unrelated disease processes (e.g., primary lung tumor). Occasionally, thoracic lymphadenopathy may be observed as a result of MCT metastasis. Knowledge of the extent of MCT margins prior to surgery, usually accomplished by digital palpation and occasionally local radiographs, can be enhanced with the use of diagnostic US or computed tomography (CT). Dogs bearing cutaneous MCTs or soft tissue sarcomas had the extent of local tumor margins upgraded in 19% and 65% of cases when imaged by US and CT, respectively.128 Such information allows more appropriate planning of definitive surgery or RT. The cost effectiveness of such a study depends on the location of the tumor and whether wide excision is technically simple or difficult.
With respect to evaluation of buffy coat smears for evidence of systemic mast cell disease, peripheral mastocytosis (1 to 90 mast cells/µL) is reported in dogs with acute inflammatory disease (in particular, parvoviral infections), inflammatory skin disease, regenerative anemias, neoplasia other than MCTs, and trauma.129-131 One study revealed that peripheral mastocytosis is actually more likely to occur and may be more dramatic in dogs with diseases other than MCTs.130 Therefore this test is no longer routinely performed in the staging of MCT patients. In a report evaluating 157 dogs with MCTs, the incidence of bone marrow infiltration at initial staging was only 2.8%.132 Although the presence of bone marrow involvement is indicative of systemic mast cell disease, it is usually easier to find evidence of systemic involvement in other organs (liver, spleen).63 This is in contrast to dogs that present with visceral MCTs, in which 37% of buffy coat smears are positive for mast cells and 56% of bone marrow aspirates reveal mast cell dissemination103; however, these constitute a small minority of all MCT cases. Therefore, with the exception of the extremely rare case of primary mastocytic leukemia,133,134 involvement of marrow or peripheral blood in the absence of disease in regional lymph node or abdominal organs is unlikely.132
Treatment
Treatment decisions are predicated on the presence or absence of negative prognostic factors and on the clinical stage of disease. In tumors localized to the skin in areas amenable to wide excision, surgery is the treatment of choice. Historically, surgical excision to include a 3-cm margin of surrounding normal tissue has been recommended for MCT. More recently, evidence exists that 1- to 2-cm lateral margins may be sufficient for complete excision of many MCTs, particularly those that are lower grade and small.135,136 Indeed, in 100 dogs with 115 resectable MCTs (primarily intermediate and low grade), no local recurrence or metastasis was noted for greater than 2 years following excision with lateral histologic margins of 10 mm or larger and deep histologic margins of 4 mm or larger.76 It should be noted that these microscopic, formalin-fixed margin parameters may not accurately reflect margin size at surgery: tissue shrinkage (up to 30% for cutaneous tissues) can occur subsequent to formalin fixation.137-139 Considering that the majority of naïve dermal MCTs encountered in practice are intermediate- or low-grade tumors, it can be said that most MCTs can be cured with surgery alone, provided the site is amenable to adequate surgical resection. The quality of the deep margin is as important as that of the lateral margins, and it is recommended that one uninvolved fascial plane deep to the tumor be removed in continuity with the tumor. If necessary, muscle layers may also be removed deep to the tumor. All surgical margins should be evaluated histologically for completeness of excision. It is recommended that tumors in areas not amenable to wide surgical margins, such as distal extremities, be evaluated by biopsy to determine histologic grade prior to definitive therapy.
If a distal extremity MCT is low or intermediate grade and complete excision is not achievable, four primary therapy options exist. The most aggressive option is amputation; however, although wide margins are guaranteed, it results in the least functional outcome and is generally not recommended given the availability of other effective therapies. The second option is external-beam RT alone, which produces varying control rates in the literature when used as a primary therapy; doses between 40 and 50 Gy result in 1-year control rates of approximately 50%.105,140-145
The third and, in the authors’ opinion, the ideal option for low- or intermediate-grade MCTs in areas where wide surgical excision is not possible is a combination of surgery and RT. The veterinary literature has established that the complementary use of surgery to achieve clinical stage 0 disease (i.e., microscopically incomplete margins) and external-beam RT is associated with long-term control. Two-year control rates of 85% to 95% can be expected for low- or intermediate-grade stage 0 tumors.105,117,146-148 Some authors advocate prophylactic irradiation of cytologically negative regional lymph nodes (prophylactic nodal irradiation [PNI]).114,117,118,149 Due to the generally low risk of postsurgical metastasis in low- to intermediate-grade tumors, PNI is probably unwarranted in this group of patients, and at least one study has demonstrated no advantage in terms of disease-free or overall survival when PNI is employed in this group of dogs148; however, in MCTs at high risk for metastasis, PNI may provide improvement in outcome over local site irradiation only.114,149
The last option for low- or intermediate-grade MCTs in areas where wide surgical excision is not possible is a combination of surgery and chemotherapy (discussed later). There are now several published studies that have demonstrated a low rate of recurrence in dogs with incompletely excised MCTs that receive some form of chemotherapy postsurgery.150,151 Although not considered optimal, this approach can be used in cases in which RT is unavailable or unaffordable. Regardless of the local therapy chosen, dogs with low- and intermediate-grade tumors should be reevaluated regularly for local recurrence and possible metastasis. Local site and regional lymph node evaluation, complete physical examination, and aspiration of any new cutaneous masses or enlarged lymph nodes are performed at these intervals. More complete staging, including abdominal US, should be included if the dog has an MCT with negative prognostic indicators.
For cases in which planned curative excisional surgery is unsuccessful and histologic margins are incomplete, further local therapy is warranted. A second excision of the surgical scar with additional wide margins should be performed if possible (Figure 20-6) or adjuvant RT can be used in cases in which re-excision is not an option. Not all MCTs with surgically incomplete margins will recur; in some studies, only 20% to 30% of MCTs with histologically confirmed incomplete margins recurred.84,152 Although recurrence rates vary by study, several studies have demonstrated increased recurrence rates and/or decreased overall survival in dogs with incompletely resected MCTs.28,71,73,113 Figure 20-7 summarizes the treatment recommendations for clinical stage 0 and I, histologically low- or intermediate-grade MCTs. Alternative local therapies for MCTs have been reported and include hyperthermia in combination with RT,153 intralesional brachytherapy,154,155 photodynamic therapy,156,157 intralesional corticosteroids,158 cryotherapy, and electrochemotherapy.159-161 Although some have advocated the use of intralesional deionized water at the site of an incompletely removed MCT, clinical data indicate that this approach is not effective at preventing local recurrence and should therefore not be used.162-167 It is important to note that none of these alternative local therapies are as thoroughly investigated, clinically effective, or practical as surgery, RT, or a combination of the two. Finally, despite its common use, there is no information available to suggest that adjuvant corticosteroid therapy is beneficial in cases of individual intermediate-grade MCTs that have been either excised completely or treated with local RT postsurgery.

Figure 20-6 Re-excision of an MCT from the skin of a golden retriever. The first surgery resulted in incomplete surgical margins; thus 3-cm margins were taken around and deep to the previous incision and the entire sample was again submitted for margin analysis by the pathologist.
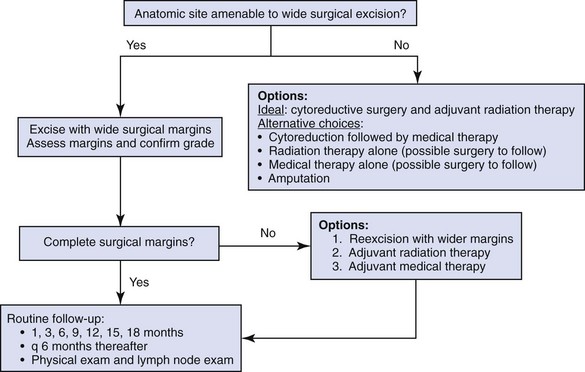
Figure 20-7 Suggested treatment approach for clinical stage 0 and stage I low- or intermediate-grade canine MCTs.
The treatment of anaplastic or undifferentiated MCTs remains a frustrating undertaking. This designation includes dogs with intermediate-grade tumors with regional or distant metastasis or high proliferative activity as assessed by MI or special stains, as well as those arising from a mucous membrane or mucocutaneous junction. There is some evidence to suggest that intermediate-grade tumors with only regional node involvement have a better prognosis than high-grade tumors.108,114 In the authors’ opinion, until convincing evidence exists, such tumors should be treated as if they have a high capacity for metastasis. Figure 20-8 summarizes the treatment recommendations for high-grade MCTs. The long-term prognosis for such dogs is less favorable because regional and distant metastases are more likely.
Poorly differentiated and metastatic MCT will, in most instances, progress to kill the dog in the absence of effective postsurgical intervention. Systemic adjuvant therapy should be offered in such cases in an attempt to decrease the likelihood of systemic involvement, or at least potentially improve DFIs. Corticosteroids such as prednisone have been reported for many years in preclinical or anecdotal settings to be of some benefit.168-172 Although corticosteroids can inhibit canine MCT proliferation and induce tumor cell apoptosis in vitro,173 they may also contribute to apparent antitumor response by decreasing peritumoral edema and inflammation. The Veterinary Cooperative Oncology Group (VCOG) studied the efficacy of single-agent systemic prednisone therapy for intermediate- and high-grade canine MCTs.172 Of 21 dogs receiving 1 mg/kg daily by mouth (PO), only one complete response (CR) and four partial responses (PR) were noted, and these were short-lived, lasting only a few weeks in the majority of cases. More recent studies have reported 70% to 75% response rates; however, tumors were excised or irradiated following short-term prednisone treatment, thus duration of response was not evaluable.145,171 A recent study found that response of MCT to corticosteroids was dependent on expression of the glucocorticoid receptor; those dogs with tumors that expressed low levels of this receptor had MCTs that were resistant to prednisolone therapy.174 These data suggest that a subset of MCT may indeed benefit from corticosteroid therapy if there is adequate expression of the glucocorticoid receptor.
Recently, a number of studies have evaluated the response rates of measurable canine MCT to various cytotoxic chemotherapy drugs and protocols (Table 20-6).* Objective response rates as high as 64% have been reported, and accumulating evidence suggests that multiagent protocols may confer a higher response rate than single-agent therapy.† It is important to note that in most instances, the response of a bulky MCT to any chemotherapy protocol tends to be short-lived, stressing the need for local control of disease prior to institution of adjuvant therapy.
Table 20-6
Response to Medical Therapy in Measurable Canine Mast Cell Tumors
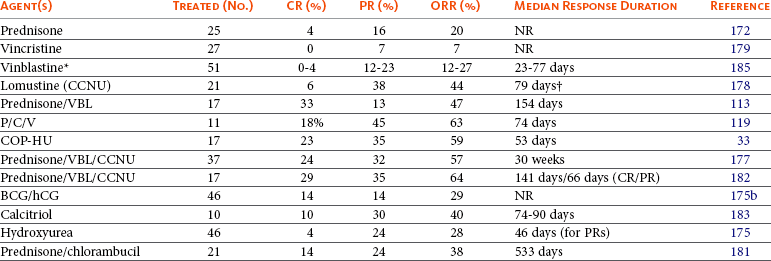
CR, Complete response; PR, partial response; ORR, overall response rate; NR, not reported; VBL, vinblastine; P/C/V, prednisone/cyclophosphamide/vinblastine; COP-HU, cyclophosphamide, vincristine, prednisone, hydroxyurea; BCG/hCG, Bacillus Calmette-Guérin/human chorionic gonadotropin.
*Two different dosages/schedules evaluated.
†Excludes patient that experienced a CR, euthanized without evidence of disease after 440 days.
A few single-arm studies have attempted to evaluate the efficacy of chemotherapy for “high-risk” MCTs in the postsurgical setting. One study evaluated the use of postoperative prednisone and vinblastine (VBL) for dogs with MCT considered to be at high risk for metastasis (node-positive, mucous membrane origin, or high histologic grade). In this study, dogs with high-grade MCTs had an MST of 1374 days.114 A second study reported 70% 1- and 2-year disease-free survival percentages following prednisone/VBL in high-grade MCT.184 A combination of prednisone, lomustine, and VBL has been used for residual microscopic disease in dogs at high risk for dissemination. Dogs with microscopic disease had a median progression-free survival time of 35 weeks and an overall survival of 48 weeks.177 Combination therapy using cyclophosphamide, VBL, and prednisone also yielded promising results in the microscopic residual disease setting for dogs considered at high risk of recurrence or metastasis. The reported progression-free and overall survival times were 865 days and more than 2092 days, respectively.119 Most of the studies described used a dose of 2 mg/m2 VBL; although there is now information suggesting that dogs may tolerate higher doses,185-187 it remains to be seen if dose escalation of VBL will translate into improved efficacy.
As previously discussed, virtually all canine mast cell neoplasms express the KIT RTK, and a large minority of canine MCTs (20% to 40%, depending on the study) possess a mutation in the c-kit gene, which renders the KIT protein constitutively active.41,44,48,188 New, orally available molecules have been developed that inhibit signaling through KIT called small molecule TKIs. The two veterinary-approved TKIs in this class are toceranib (Palladia, Pfizer) and masitinib (Masivet/Kinavet, AB Science); limited studies have also been performed with the human KIT inhibitor imatinib (Gleevec, Novartis).
Following encouraging in vitro and early-phase clinical trials,45,189,190 a multicenter, placebo-controlled, double-blind, randomized study of toceranib was performed in dogs with recurrent or metastatic intermediate- or high-grade MCT.191 During the blinded phase of the study, the objective response rate in toceranib-treated dogs (n = 86) was 37.2% (7 CR, 25 PR) versus 7.9% (5 PR) in placebo-treated dogs. When all 145 dogs that received toceranib were analyzed, including those that switched from placebo to drug, the objective response rate was 42.8% (21 CR, 41 PR), with an additional 16 dogs experiencing stable disease for an overall biologic activity of 60%. The median duration of objective response and time to tumor progression were 12.0 and 18.1 weeks, respectively. Interestingly, dogs whose MCT harbored activating mutations in the c-kit gene were roughly twice as likely to respond to toceranib as those with wild-type c-kit (69% versus 37%). GI toxicity, in the form of inappetence, weight loss, diarrhea, and occasionally vomiting or melena, was the most common adverse effect and was generally manageable with symptomatic therapy, drug holidays, and dosage reductions as necessary. Other adverse effects reported include mild-to-moderate leukopenia and occasional muscle pain.191 Recent clinical experience with toceranib suggests that equivalent antitumor activity and reduced adverse effects may be observed if dosages lower than the label dosage are employed. A dosage of 2.5 to 2.75 mg/kg every other day or 3 days per week (Monday, Wednesday, Friday) is currently utilized by many.192,193
A clinical trial of similar design was recently completed with masitinib in dogs with recurrent or unresectable MCT.194 This study demonstrated significantly improved time to progression in masitinib-treated versus placebo-treated dogs, and outcome again was improved in dogs with MCTs harboring activating c-kit mutations. Subsequent follow-up of patients treated with long-term masitinib identified an increased number of patients with long-term disease control compared to those treated with placebo (40% versus 15% alive at 2 years),195 underscoring the potential for long-term disease stabilization to be an acceptable and clinically meaningful outcome in patients treated with this class of agent. GI adverse effects (vomiting or diarrhea) were most common but were mild in the majority of cases and self-limiting. Myelosuppression was also observed and was mild in most cases. A small percentage of dogs developed a protein-losing nephropathy leading to edema. Increases in urea and creatinine were observed in some dogs, and hemolytic anemia was observed rarely.194
Finally, small studies have evaluated the efficacy of imatinib for the treatment of measurable canine MCTs.196-198 Imatinib was well tolerated, and objective antitumor responses were observed in dogs with both c-kit mutant and wild-type MCTs. It is important to note that no studies have yet been performed in dogs with MCTs to assess the pharmacokinetics of imatinib; thus current dosing recommendations are based on observed clinical activity, not pharmacokinetic and pharmacodynamic relationships.
At this time, there are only a few published studies regarding the safety and efficacy of combination therapy with KIT inhibitors and standard forms of therapy such as RT or cytotoxic chemotherapy, and evidence of benefit when used in the postoperative setting has yet to be demonstrated. One recent clinical trial evaluated a combination of toceranib and VBL in dogs with measurable MCTs. Significant reductions in VBL dosage and frequency were necessary because of additive myelosuppression resulting in a maximally tolerated dose of VBL of 1.6 mg/m2 every other week in combination with toceranib given every other day.199 Nevertheless, encouraging biologic activity (71% objective response rate) was observed despite the necessary dosage reductions, indicating that future evaluation of this combination regimen is warranted. Finally, another study investigated the combination of toceranib, prednisone, and hypofractionated RT in dogs with nonresectable and/or metastatic MCT.192 The overall response rate (ORR) was 76.4%, with 58.8% of dogs achieving CR and 17.6% PR. The overall MST was not reached, and the median follow-up was 374 days. The combination of hypofractionated RT and toceranib was well tolerated and demonstrated efficacy in the majority of dogs, indicating that this may be a viable treatment option for nonresectable MCT.
Novel medical approaches that may hold promise for the future treatment of MCT include histone deacetylase inhibitors,200-202 heat shock protein 90 (HSP90) inhibitors,203,204 retinoids,205-207 TNF-related apoptosis-inducing ligand (TRAIL),208 and polo-like kinase-1 inhibitors.209
Ancillary therapy to address the systemic effects of mast cell mediators is sometimes warranted in dogs with MCTs. Minimizing the effects of histamine release can be accomplished by administering the H1 blockers diphenhydramine (2 to 4 mg/kg PO twice a day [BID]) or chlorpheniramine (0.22 to 0.5 mg/kg three times a day [TID]) and the H2 blockers cimetidine (4 to 5.5 mg/kg PO TID), famotidine (0.5 to 1 mg/kg BID), or ranitidine (2 mg/kg BID). Omeprazole (0.5 to 1 mg/kg daily), a proton pump inhibitor, may be more effective, particularly in bulky mast cell disease. These agents are generally used in the setting of gross disease, particularly those cases in which (1) systemic signs are present, (2) the tumor is likely to be entered or manipulated at surgery (i.e., cytoreductive surgery), or (3) treatment is undertaken where gross disease will remain and degranulation is likely to occur in situ (e.g., RT or medical therapy for tumors that are not cytoreduced). For cases with active evidence of gastric or duodenal ulceration, the addition of sucralfate (0.5 to 1.0 g PO TID) and occasionally misoprostol (2 to 4 µg/kg PO TID) to histamine blockers is prudent. Some experimental data suggest that the use of H1 and H2 blockers could also be beneficial for the prevention or resolution of histamine-mediated wound breakdown,32,210,211 but this has not been systematically evaluated. The use of protamine sulfate, a heparin antagonist, has been mentioned by some for use in cases of severe hemorrhage.104
Feline Mast Cell Tumors
Unlike MCTs in the dog, which are primarily cutaneous/subcutaneous in nature, MCTs in the cat typically occur in three distinct syndromes, although there is some overlap among them. These syndromes are cutaneous MCT, splenic/visceral mast cell disease, and intestinal MCT. The etiology of feline MCTs is currently unknown and appears unrelated to viral infection.212 However, it is now evident that feline MCTs also possess somatic activating mutations in c-kit.213-215 In one study, 42/62 (67%) of cutaneous and splenic/visceral MCT had c-kit mutations that were primarily present in exons 8 (28/62) and 9 (15/62), both of which encode the fifth immunoglobulin domain of KIT. Similar to the canine juxtamembrane domain mutations, these feline c-kit mutations induce ligand-independent activation of KIT, which can be inhibited by imatinib in vitro.215
The granules present in feline MCTs stain blue with Giemsa and purple with toluidine blue.1,2,4 As in the dog, granules present in feline mast cells contain vasoactive substances, such as heparin and histamine.2,216 In culture, feline mast cells express surface-bound immunoglobulins and are capable of secreting histamine, heparin, and probably other vasoactive compounds when appropriately stimulated.216 Feline mast cells also have phagocytic capability and can endocytose erythrocytes in both experimental models and clinical samples.217 Complications associated with degranulation of MCT can also occur in the cat, including coagulation disorders, GI ulceration, and anaphylactoid reactions.2,218,219 Since the biologic behavior of the three feline MCT syndromes is different, they will be described individually.
Cutaneous Feline Mast Cell Tumors
MCTs represent the second most common cutaneous tumor in the cat, accounting for approximately 20% of cutaneous tumors in this species in the United States.2,4,12 The incidence of MCTs in cats appears to have increased dramatically since 1950.2 Interestingly, MCTs appear to occur much less frequently in the United Kingdom than in the United States, accounting for only 8% of all cutaneous tumors.1 The typical feline cutaneous MCT is a solitary, raised, firm, well-circumscribed, hairless, dermal nodule between 0.5 and 3 cm in diameter.2,4,220,221 They are often white in appearance, although a pink erythematous form is occasionally encountered. Approximately 20% are multiple, although one series reported multiple lesions in the majority of cases.1 Superficial ulceration is present in approximately one-fourth of cases. Other clinical forms that have been described include a flat pruritic plaquelike lesion similar in appearance to eosinophilic plaques and discrete subcutaneous nodules.
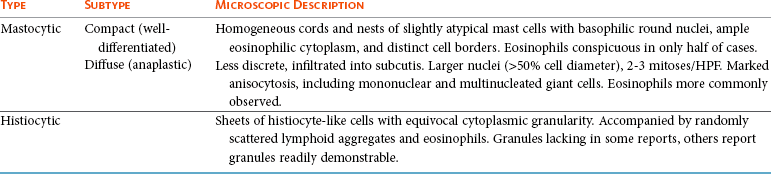
Two distinct types of cutaneous MCTs in the cat have been reported (Table 20-7): (1) the more typical mastocytic MCT, histologically similar to MCTs in dogs, and (2) the less common histiocytic MCTs, with morphologic features characteristic of histiocytic mast cells, that may regress spontaneously over a period of 4 to 24 months.221,222 An overall mean age of 8 to 9 years is reported for cats with MCTs; however, the mastocytic and histiocytic forms occur at mean ages of 10 and 2.4 years, respectively.2,4,220 Siamese cats appear to be predisposed to development of MCTs of both histologic types.2,4,220-222 The distinct histiocytic form of MCTs in cats is reported to occur primarily in young (<4 years of age) Siamese cats, including two related litters.222 In contrast to these reports, Siamese cats were not more likely to develop the histiocytic form of MCT than the mastocytic form in another series of cases.4 Earlier studies reported a male predilection for development of MCT219,220; however, larger, more recent series have failed to confirm such a predilection.2,4
The mastocytic form can be further subdivided on histologic appearance into two categories, previously referred to as compact (representing 50% to 90% of all cases) and diffuse (histologically anaplastic), which may be of prognostic significance.2,222,223 Well-differentiated compact tumors tend to behave in a benign manner, and metastasis is uncommon.220,224,225 In contrast, anaplastic tumors may have a high MI and marked cellular and nuclear pleomorphism, with infiltration into the subcutaneous tissues.221 These tumors have been reported as behaving in a more malignant manner with metastasis to lymph nodes and the abdomen, although a more recent study evaluated pleomorphic cutaneous MCTs from 15 cats and found that the majority were behaviorally benign; only one cat was euthanized due to disease progression.226
Unlike in the dog, the head and neck are the most common site for MCTs in the cat, followed by the trunk, limbs, and miscellaneous sites (Figure 20-9).2,4,220 Tumors on the head often involve the pinnae near the base of the ear. They rarely occur in the oral cavity. Intermittent pruritus and erythema are common, and self-trauma or vascular compromise may result in ulceration. Darier’s sign, which is the erythema and wheal formation following mechanical manipulation of the tumor, has been reported in the cat.219 Affected cats are usually otherwise healthy. The spontaneously regressing histiocytic form of cutaneous MCTs usually presents as multiple, nonpruritic, firm, hairless, pink, and sometimes ulcerated subcutaneous nodules (Figure 20-10).4,222
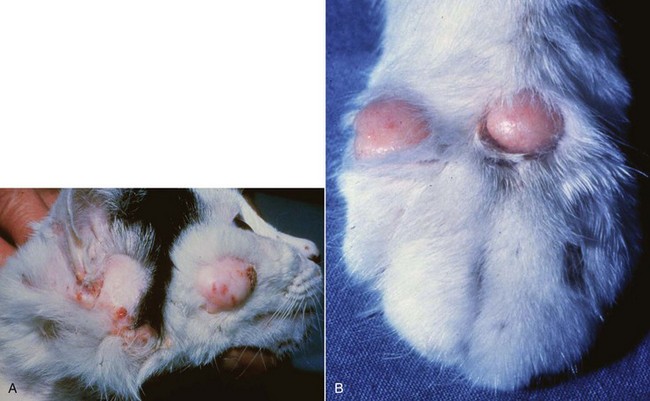
Figure 20-9 A, Multiple MCTs on the head of a cat. The head and neck are the most commonly encountered location for MCTs in the cat. They often involve the area near the base of the ear. B, MCTs in the cat are less common on the limbs. (Courtesy S. Helfand, Oregon State University, Corvallis, OR.)

Figure 20-10 Histiocytic MCTs on the head of a young Siamese cat. This form of MCTs in cats typically regress spontaneously, as was the case in the cat pictured here. (Courtesy Dr. K. Moriello, University of Wisconsin-Madison.)
As with canine tumors, most feline MCTs are usually easily diagnosed by cytologic examination of fine needle aspirates. In contrast, the uncommon histiocytic form of feline MCTs is more challenging to diagnose both by FNA and histopathology.221,222 Mast cells may comprise only 20% of the cells present, with the majority being sheets of histiocytes that lack distinct cytoplasmic granules and accompanied by randomly scattered lymphoid aggregates and eosinophils. In contrast, one report readily demonstrated metachromatic granules in seven cases of the histiocytic subtype. These tumors can be initially misdiagnosed as granulomatous nodular panniculitis or deep dermatitis.
Cats with cutaneous MCTs should be evaluated for evidence of additional tumors, as well as potential splenic involvement by abdominal US, because one study found that some cats with multiple cutaneous MCTs also had splenic disease.224 In addition, a minimum database is recommended, along with careful examination of local lymph nodes for evidence of lymphadenopathy. Interestingly, unlike dogs, cats rarely exhibit evidence of circulating mast cells on buffy coat smears when healthy or ill from non–mast cell-related causes.227 In contrast, one study demonstrated that 43% of cats with mast cell disease have positive buffy coats, although most of these cats tended to have the splenic/visceral form of the disease.228
Feline MCTs are usually positive for vimentin, α-1 antitrypsin, and KIT.229,230 Although the histologic grading system described for canine MCT has provided no prognostic information for the cat in several series and is not used,220,231 tumors with a high MI appear to be at greatest risk for local recurrence and metastasis, suggesting that this histopathologic feature may be useful for predicting biologic behavior.221,226 A more recent study evaluated the prognostic value of histologic and immunohistochemical features in feline cutaneous MCTs. Multiplicity of lesions, pleomorphic phenotype, KIT immunoreactivity score, MI, and Ki67 index correlated with an unfavorable outcome, although MI was the strongest predictive variable.232
The definitive treatment for cutaneous feline MCT is surgical excision. In a series of 32 cats with cutaneous MCTs, five tumors recurred following surgical excision, although none of the cats in this study died of disease. Completeness of excision and histopathologic factors such as nuclear pleomorphism and MI were not associated with tumor recurrence.225 In a more recent series of cats with MCTs of the eyelids, local tumor control in 19/23 cats was achieved with surgery alone and another 3 cats experienced control with surgery plus RT or cryotherapy, resulting in an MST of 945 days.233 Despite the fact that only 50% of the tumors were completely removed, only one cat developed disseminated cutaneous tumors and no cats developed metastatic disease to the lymph nodes or abdomen. Other reports have demonstrated local recurrence rates following excision between 0% and 24%.2,220,221,224,226 These data suggest that most cutaneous feline MCTs are behaviorally benign, and wide surgical margins may not be as critical in the cat as in the dog. Frequency of systemic spread following surgical excision varies from 0% to 22%, although those that metastasize are more likely to be anaplastic tumors.220,221,224-226 Therefore, for histologically anaplastic tumors or those with a high MI more likely to recur postsurgery or to metastasize, a more aggressive approach similar to that utilized for canine MCTs may be prudent.226,234 Following biopsy confirmation, conservative resection or a “wait and see” approach may be taken with the histiocytic form in young cats with multiple masses because these may spontaneously regress.2,4,222
RT may be considered for tumors that are incompletely excised. In one study of feline cutaneous MCT, a 98% control rate was achieved with strontium-90 irradiation, with an MST of greater than 3 years.235 Limited information exists concerning the utility of chemotherapy in cats with MCTs. It is generally believed that feline MCTs are less responsive to prednisone than their canine counterparts; biologic activity of corticosteroids in cats with the histiocytic variant was found to be equivocal.222 Objective responses to lomustine (CCNU) have been reported in cats.236,237 Of 20 cats with cutaneous MCTs, 10 exhibited CR (n = 2) or PR (n = 8) to lomustine.237 The authors have observed evidence of clinical activity in cats treated with prednisone and VBL as well. Some investigators have utilized a combination of prednisone and chlorambucil to treat metastatic or multiple tumors. This is generally well tolerated, although its effectiveness is not known.
Biologic activity of imatinib has been observed in cats with MCTs expressing activating mutations in c-kit, although the responses were all partial in nature.214,215,238 Studies in healthy cats have demonstrated that masitinib may be safe to administer to clinically normal cats, and plasma concentrations associated with MCT inhibitory activity are likely achievable. Cats should be monitored very closely for neutropenia, proteinuria, and increases in creatinine.239,240 Neither masitinib nor toceranib have been formally evaluated in cats with MCTs.
Splenic/Visceral Feline Mast Cell Tumors
MCTs represent the most common differential for splenic disease in cats, accounting for 15% of submissions in a series of 455 pathologic specimens.241 This disease primarily affects older animals (mean age 10 years) with no sex or breed predilection.2,224,241 The majority of cats with splenic MCTs do not have a history of cutaneous MCTs, although recent evidence suggests that some cats with multiple cutaneous MCTs may also have splenic involvement.224 Although the spleen is the primary site affected by this disease, other organs may also be involved.2,218 Necropsy data on 30 cats with splenic MCTs revealed dissemination in the following organs in decreasing order of frequency: liver (90%), visceral lymph nodes (73%), bone marrow (40%), lung (20%), and intestine (17%).2 Up to one-third of cases have peritoneal and pleural effusions rich in eosinophils and mast cells.2,218 Peripheral blood mastocytosis has been reported in 40% to 100% of cases with peripheral mast cell counts up to 32,000 cells/µL.2,228 In one clinical report of 43 cases, 23% had bone marrow involvement.218
Cats with splenic MCTs may present with signs of systemic illness, including vomiting, anorexia, and weight loss.2,218 Dyspnea may be evident if pleural effusion is present. Abdominal palpation usually reveals a markedly enlarged spleen and/or liver. Other common differential diagnoses for splenomegaly in the cat include lymphoma, myeloproliferative disease, accessory spleen, hemangiosarcoma, hyperplastic nodules, and splenitis.241 Clinical signs associated with the release of mast cell mediators, such as GI ulceration, hemorrhage, hypotensive shock, and labored breathing, may also be noted. Cats with suspected splenic MCTs should undergo a standard work-up, including a minimum database, as well as abdominal US and thoracic radiographs. FNA cytology is usually diagnostic for splenic MCTs, as is evaluation of thoracic or abdominal fluid. Anemia is a common hematologic finding, with eosinophilia less likely to be observed.2,218 In one report of 43 cats with splenic MCT, 90% had an abnormal coagulation profile, although this did not appear to be clinically significant.218 Hyperglobulinemia has also been reported in cats with splenic MCTs, the cause of which remains unknown.
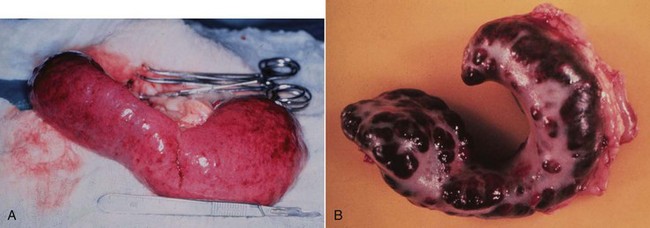
Splenectomy is the treatment of choice for cats with splenic MCTs, even if other organ involvement is noted. Pretreatment with H1 and H2 blockers prior to therapy is indicated; intraoperative death may occur due to the release of mast cell mediators. Two gross forms of splenic involvement are possible: a diffuse, smooth form and a less common nodular form (Figure 20-11).125,242 Surprisingly, even in the face of significant bone marrow and peripheral blood involvement, long-term survival with good quality of life is the norm following splenectomy, with MSTs from 12 to 19 months reported,2,218,243-245 although one recent study reported an MST of only 132 days following splenectomy.246 Anorexia, significant weight loss, and male gender were found to be negative prognostic indicators in one study.218 Although peripheral mastocytosis usually does not completely resolve, it usually declines significantly and cats experience good quality of life for long periods of time. Cats should be followed postoperatively with buffy coat smears because a rise in the number of mast cells in the periphery may indicate disease progression. Adjunctive chemotherapy with prednisone, VBL, lomustine, and/or chlorambucil has been attempted in a limited number of cases, but it is not clear if these therapies are clinically valuable. As discussed previously, recent data indicate that cats with MCTs may respond to the KIT inhibitor imatinib if activating mutations in c-kit are present.214,215
Feline Intestinal Mast Cell Tumor
Intestinal MCT is the third most common primary intestinal tumor in cats after lymphoma and adenocarcinoma.2 No breed or gender predilection is known. Older cats appear to be at risk, with a mean age of 13 years; however, cats as young as 3 years have been reported.247 Most cats have a history of vomiting, diarrhea, and anorexia, and a solitary palpable abdominal mass is usually evident on physical examination.2,247 Intestinal MCT more commonly involves the small intestine (equally divided between duodenum, jejunum, and ileum), with colonic involvement reported in less than 15% of cases; lesions can be solitary or multiple.2,247,248 Diarrhea with or without hematochezia is commonly observed with the intestinal form, and fever may be present. Affected cats may have been ill for several months. Metastasis is common with this disease; thus enlarged mesenteric lymph nodes and/or hepatomegaly may be noted on physical examination. A peritoneal effusion may be present, and this often contains mast cells and eosinophils. Diagnosis is usually made by FNA of the mass or involved organs; mast cells from intestinal lesions are often less differentiated than those of skin tumors and cytoplasmic granules may be less prominent, making diagnosis challenging in certain cases. Cats with intestinal MCTs should be staged with a minimum database, thoracic radiographs, and abdominal US, which may be required to determine the extent of intestinal involvement and presence of visceral dissemination. Buffy coat smear may also be performed, although unlike splenic MCT, peripheral mastocytosis is rarely associated with intestinal MCT and only two reports of peripheral eosinophilia exist in the literature.247
Intestinal MCTs in cats often have a poor prognosis2,247,248 because metastasis is commonly found at the time of diagnosis and many cats either die or are euthanized soon after they are diagnosed. Surgery is the treatment of choice, and wide surgical margins are necessary (5 to 10 cm) because the tumor typically extends histologically well beyond the obvious gross disease.2,247 Recently, a variant of feline intestinal MCT, termed sclerosing MCT, was described in 50 cats.248 Metastatic disease to the lymph nodes and/or liver was present in 23/36 cases evaluated. Of the 25 cases with clinical follow-up information, 23 died or were euthanized within 2 months of diagnosis, supporting the aggressive nature of this disease. Limited information exists regarding the use of chemotherapy for feline intestinal MCTs, although anecdotal responses to lomustine and chlorambucil have been reported. Recently, two cats exhibited objective responses (one CR, one PR) following treatment with lomustine, suggesting that this agent may be useful in cats with intestinal MCTs.237 The role of KIT inhibitors in the treatment of this disease is not yet known.
Comparative Aspects of Mast Cell Tumors
Neoplastic diseases of mast cells are considered rare in humans and present as three main clinical entities.176,249-252 Cutaneous mastocytosis, also known as urticaria pigmentosa, is a benign disease in which mast cell infiltration is confined to the skin. It primarily occurs in young children and usually regresses spontaneously before progression into adulthood. Systemic mastocytosis (SM) occurs primarily in adults and includes four major subtypes: (1) indolent SM, the most common form involving mainly skin and bone marrow that does not progress to aggressive disease; (2) a unique subcategory termed SM with an associated non–mast cell clonal hematologic disease; (3) aggressive SM, usually presenting without skin lesions; and (4) mast cell leukemia, probably representing the rarest variant of human leukemias. Finally, rare localized extracutaneous MCTs (either benign or malignant) have been reported. Dysregulation of KIT is also found commonly in human neoplastic mast cell diseases and is primarily driven by a point mutation in exon 17 of c-kit that induces ligand-independent activation.250,253 More recently, mutations have also been identified in exons 8 to 11, most of which are also activating.250,253
Treatment of the benign human mast cell disorders is primarily focused on supportive therapy, including H1 and H2 antagonists, and topical or systemic therapy with corticosteroids. Unfortunately, there is no good therapy for cases of aggressive mastocytosis or mast cell leukemia. Treatment with interferon-α (IFN-α) and/or cladribine is often used, although response rates are typically low.249,253 Most of the currently available small molecule KIT inhibitors, including imatinib, nilotinib, and dasatinib, have not been effective in treating human mastocytosis.253 This may in part be due to the fact that inhibiting phosphorylation of KIT-expressing activating exon 17 mutations is extremely challenging. More recently, the protein kinase C inhibitor, midostaurin, has demonstrated activity in human mast cell disease.253
References
1. Bostock, DE. Neoplasms of the skin and subcutaneous tissues in dogs and cats. Br Vet J. 1986;142:1–19.
2. Carpenter, JL, Andrews, LK, Holzworth, J. Tumors and tumor-like lesions. In: Holzworth J, ed. Diseases of the cat: medicine and surgery. Philadelphia: WB Saunders, 1987.
3. Finnie, JW, Bostock, DE. Skin neoplasia in dogs. Aust Vet J. 1979;55:602–604.
4. Miller, MA, Nelson, SL, Turk, JR, et al. Cutaneous neoplasia in 340 cats. Vet Pathol. 1991;28:389–395.
5. Rothwell, TL, Howlett, CR, Middleton, DJ, et al. Skin neoplasms of dogs in Sydney. Aust Vet J. 1987;64:161–164.
6. Kumar, V, Sharma, A. Mast cells: emerging sentinel innate immune cells with diverse role in immunity. Mol Immunol. 2010;48:14–25.
7. Noviana, D, Mamba, K, Makimura, S, et al. Distribution, histochemical and enzyme histochemical characterization of mast cells in dogs. J Mol Histol. 2004;35:123–132.
8. Metz, M, Piliponsky, AM, Chen, CC, et al. Mast cells can enhance resistance to snake and honeybee venoms. Science. 2006;313:526–530.
9. Lin, TY, London, CA. A functional comparison of canine and murine bone marrow derived cultured mast cells. Vet Immunol Immunopathol. 2006;114:320–334.
10. Lin, TY, Rush, LJ, London, CA. Generation and characterization of bone marrow-derived cultured canine mast cells. Vet Immunol Immunopathol. 2006;113:37–52.
11. Lin, TY, London, CA. Characterization and modulation of canine mast cell derived eicosanoids. Vet Immunol Immunopathol. 2010;135:118–127.
12. Brodey, RS. Canine and feline neoplasia. Adv Vet Sci Comp Med. 1970;14:309–354.
13. Brodey, RS, Riser, WH. Canine osteosarcoma. A clinicopathologic study of 194 cases. Clin Orthop. 1969;62:54–64.
14. Patnaik, AK, Ehler, WJ, MacEwen, EG. Canine cutaneous mast cell tumor: morphologic grading and survival time in 83 dogs. Vet Pathol. 1984;21:469–474.
15. Peters, JA. Canine mastocytoma: excess risk as related to ancestry. J Natl Cancer Inst. 1969;42:435–443.
16. White, CR, Hohenhaus, AE, Kelsey, J, et al. Cutaneous MCTs: Associations with spay/neuter status, breed, body size, and phylogenetic cluster. J Am Anim Hosp Assoc. 2011;47:210–216.
17. McNiel, EA, Prink, AL, O’Brien, TD. Evaluation of risk and clinical outcome of mast cell tumours in pug dogs. Vet Comp Oncol. 2004;4:2–8.
18. Davis, BJ, Page, R, Sannes, PL, et al. Cutaneous mastocytosis in a dog. Vet Pathol. 1992;29:363–365.
19. Dunn, TB, Patter, H. A transplantable mast cell neoplasm in the mouse. J Natl Cancer Inst. 1957;18:587–601.
20. Hottendorf, GH, Nielsen, SW. Pathologic survey of 300 extirpated canine mastocytomas. Zentralbl Veterinarmed A. 1967;14:272–281.
21. Peterson, SL. Scar-associated canine mast cell tumor. Canine Pract. 1985;12:23–29.
22. Bowles, CA, Kerber, WT, Rangan, SRS, et al. Characterization of a transplantable, canine, immature mast cell tumor. Cancer Res. 1972;32:1434–1441.
23. Lombard, LS, Moloney, JB. Experimental transmission of mast cell sarcoma in dogs. Fed Proc. 1959;18:490–495.
24. Nielson, SW, Cole, CR. Homologous transplantation of canine neoplasms. Am J Vet Res. 1961;27:663–672.
25. Stone, JM, Jacky, PB, Prieur, DJ. Chromosomal fragile site expression in boxer dogs with mast cell tumors. Am J Med Genetics. 1991;40:223–229.
26. Ginn, PE, Fox, LE, Brower, JC, et al. Immunohistochemical detection of p53 tumor-suppressor protein is a poor indicator of prognosis for canine cutaneous mast cell tumors. Vet Pathol. 2000;37:33–39.
27. Jaffe, MH, Hosgood, G, Taylor, HW, et al. Immunohistochemical and clinical evaluation of p53 in canine cutaneous mast cell tumors. Vet Pathol. 2000;37:40–46.
28. Ozaki, K, Yamagami, T, Nomura, K, et al. Mast cell tumors of the gastrointestinal tract in 39 dogs. Vet Pathol. 2002;39:557–564.
29. Mayr, B, Reifinger, M, Brem, G, et al. Cytogenetic, ras, and p53: studies in cases of canine neoplasms (hemangiopericytoma, mastocytoma, histiocytoma, chloroma). J Hered. 1999;90:124–128.
30. Wu, H, Hayashi, T, Inoue, M. Immunohistochemical expression of p27 and p21 in canine cutaneous mast cell tumors and histiocytomas. Vet Pathol. 2004;41:296–299.
31. Elling, H, Ungemach, FR. Sexual hormone receptors in canine mast cell tumour cytosol. J Comp Pathol. 1982;92:629–630.
32. Macy, DW. Canine and feline mast cell tumors: Biologic behavior, diagnosis, and therapy. Sem Vet Med Surg (Sm Anim). 1986;1:72–83.
33. Gerritsen, RJ, Teske, E, Kraus, JS, et al. Multi-agent chemotherapy for mast cell tumours in the dog. Vet Q. 1998;20:28–31.
34. Galli, SJ, Zsebo, KM, Geissler, EN. The kit ligand, stem cell factor. Adv Immunol. 1994;55:1–95.
35. Roskoski, R, Jr. Structure and regulation of Kit protein-tyrosine kinase—the stem cell factor receptor. Biochem Biophys Res Commun. 2005;338:1307–1315.
36. Roskoski, R, Jr. Signaling by Kit protein-tyrosine kinase—the stem cell factor receptor. Biochem Biophys Res Commun. 2005;337:1–13.
37. Kiupel, M, Webster, JD, Kaneene, JB, et al. The use of KIT and tryptase expression patterns as prognostic tools for canine cutaneous mast cell tumors. Vet Pathol. 2004;41:371–377.
38. London, CA, Kisseberth, WC, Galli, SJ, et al. Expression of stem cell factor receptor (c-kit) by the malignant mast cells from spontaneous canine mast cell tumours. J Comp Pathol. 1996;115:399–414.
39. Morini, M, Bettini, G, Preziosi, R, et al. C-kit gene product (CD117) immunoreactivity in canine and feline paraffin sections. J Histochem Cytochem. 2004;52:705–708.
40. Reguera, MJ, Rabanal, RM, Puigdemont, A, et al. Canine mast cell tumors express stem cell factor receptor. Am J Dermatopathol. 2000;22:49–54.
41. Downing, S, Chien, MB, Kass, PH, et al. Prevalence and importance of internal tandem duplications in exons 11 and 12 of c-kit in mast cell tumors of dogs. Am J Vet Res. 2002;63:1718–1723.
42. Jones, CL, Grahn, RA, Chien, MB, et al. Detection of c-kit mutations in canine mast cell tumors using fluorescent polyacrylamide gel electrophoresis. J Vet Diagn Invest. 2004;16:95–100.
43. Letard, S, Yang, Y, Hanssens, K, et al. Gain-of-function mutations in the extracellular domain of KIT are common in canine mast cell tumors. Mol Cancer Res. 2008;6:1137–1145.
44. London, CA, Galli, SJ, Yuuki, T, et al. Spontaneous canine mast cell tumors express tandem duplications in the proto-oncogene c-kit. Exp Hematol. 1999;27:689–697.
45. London, CA, Hannah, AL, Zadovoskaya, R, et al. Phase I dose-escalating study of SU11654, a small molecule receptor tyrosine kinase inhibitor, in dogs with spontaneous malignancies. Clin Cancer Res. 2003;9:2755–2768.
46. Webster, JD, Yuzbasiyan-Gurkan, V, Kaneene, JB, et al. The role of c-KIT in tumorigenesis: evaluation in canine cutaneous mast cell tumors. Neoplasia. 2006;8:104–111.
47. Webster, JD, Yuzbasiyan-Gurkan, V, Thamm, DH, et al. Evaluation of prognostic markers for canine mast cell tumors treated with vinblastine and prednisone. BMC Vet Res. 2008;4:32.
48. Zemke, D, Yamini, B, Yuzbasiyan-Gurkan, V. Mutations in the juxtamembrane domain of c-KIT are associated with higher grade mast cell tumors in dogs. Vet Pathol. 2002;39:529–535.
49. Bostock, DE. The prognosis following surgical removal of mastocytomas in dogs. J Small Anim Pract. 1973;14:27–41.
50. Mullins, MN, Dernell, WS, Withrow, SJ, et al. Evaluation of prognostic factors associated with outcome in dogs with multiple cutaneous mast cell tumors treated with surgery with and without adjuvant treatment: 54 cases (1998-2004). J Am Vet Med Assoc. 2006;228:91–95.
51. Tams, TR, Macy, DW. Canine mast cell tumors. Comp Cont Ed Pract Vet. 1981;27:259–263.
52. Van Pelt, DR, Fowler, JD, Leighton, FA. Multiple cutaneous mast cell tumors in a dog: A case report and brief review. Can Vet J. 1986;27:259–263.
53. Cohen, D, Reif, SS, Brodey, RS. Epidemiological analysis of the most prevalent sites and types of canine neoplasia observed in a veterinary hospital. Cancer Res. 1974;34:2859–2868.
54. Thamm, DH, Vail, DM. Mast cell tumors. In: Withrow SJ, MacEwen EG, eds. Small animal clinical oncology. ed 3. Philadelphia: WB Saunders; 2001:261–282.
55. Crowe, DT, Goodwin, MA, Greene, CE. Total laryngectomy for laryngeal mast cell tumor in a dog. J Am Anim Hosp Assoc. 1986;22:809–816.
56. Iwata, N, Ochiai, K, Kadosawa, T, et al. Canine extracutaneous mast-cell tumours consisting of connective tissue mast cells. J Comp Pathol. 2000;123:306–310.
57. Moore, LE, Garrett, LD, Debey, B, et al. Spinal mast cell tumor in a dog. J Am Anim Hosp Assoc. 2002;38:67–70.
58. Patnaik, AK, MacEwen, EG, Black, AP, et al. Extracutaneous mast-cell tumor in the dog. Vet Pathol. 1982;19:608–615.
59. Steffey, M, Rassnick, KM, Porter, B, et al. Ureteral mast cell tumor in a dog. J Am Anim Hosp Assoc. 2004;40:82–85.
60. Davies, AP, Hayden, DW, Klausner, JS, et al. Noncutaneous systemic mastocytosis and mast cell leukemia in a dog: case report and literature review. J Am Anim Hosp Assoc. 1981;17:361–368.
61. Lester, SL, McGonigle, LF, McDonald, GK. Disseminated anaplastic mastocytoma with terminal mastcythemia in a dog. J Am Anim Hosp Assoc. 1981;17:355–360.
62. Takahashi, T, Kadosawa, T, Nagase, M, et al. Visceral mast cell tumors in dogs: 10 cases (1982-1997). J Am Vet Med Assoc. 2000;216:222–226.
63. O’Keefe, DA, Couto, CG, Burke-Schwartz, C, et al. Systemic mastocytosis in 16 dogs. J Vet Intern Med. 1987;1:75–80.
64. Pollack, MJ, Flanders, JA, Johnson, RC. Disseminated malignant mastocytoma in a dog. J Am Anim Hosp Assoc. 1991;27:435–440.
65. Fox, LE, Rosenthal, RC, Twedt, DC, et al. Plasma histamine and gastrin concentrations in 17 dogs with mast cell tumors. J Vet Intern Med. 1990;4:242–246.
66. Howard, EB, Sawa, TR, Nielsen, SW, et al. Mastocytoma and gastroduodenal ulceration. Gastric and duodenal ulcers in dogs with mastocytoma. Pathol Vet. 1969;6:146–158.
67. Ishiguro, T, Kadosawa, T, Takagi, S, et al. Relationship of disease progression and plasma histamine concentrations in 11 dogs with mast cell tumors. J Vet Intern Med. 2003;17:194–198.
68. Roberts, LJ, II., Sweetman, BJ, Lewis, RA, et al. Increased production of prostaglandin D2 in patients with systemic mastocytosis. N Engl J Med. 1980;303:1400–1484.
69. Scott, HW, Parris, WCV, Sandidge, PC, et al. Hazards in operative management of patients with systemic mastocytosis. Ann Surg. 1983;197:507–514.
70. Hottendorf, GH, Nielsen, SW, Kenyon, AJ. Canine mastocytoma: I. Blood coagulation time in dogs with mastocytoma. Pathol Vet. 1965;2:129–141.
71. Murphy, S, Sparkes, AH, Smith, KC, et al. Relationships between the histological grade of cutaneous mast cell tumours in dogs, their survival and the efficacy of surgical resection. Vet Rec. 2004;154:743–746.
72. Simoes, JP, Schoning, P, Butine, M. Prognosis of canine mast cell tumors: a comparison of three methods. Vet Pathol. 1994;31:637–647.
73. Bostock, DE, Crocker, J, Harris, K, et al. Nucleolar organiser regions as indicators of post-surgical prognosis in canine spontaneous mast cell tumours. Br J Cancer. 1989;59:915–918.
74. Michels, GM, Knapp, DW, DeNicola, DB, et al. Prognosis following surgical excision of canine cutaneous mast cell tumors with histopathologically tumor-free versus nontumor-free margins: a retrospective study of 31 cases. J Am Anim Hosp Assoc. 2002;38:458–466.
75. Seguin, B, Leibman, NF, Bregazzi, VS, et al. Clinical outcome of dogs with grade-II mast cell tumors treated with surgery alone: 55 cases (1996-1999). J Am Vet Med Assoc. 2001;218:1120–1123.
76. Weisse, C, Shofer, FS, Sorenmo, K. Recurrence rates and sites for grade II canine cutaneous mast cell tumors following complete surgical excision. J Am Anim Hosp Assoc. 2002;38:71–73.
77. Schultheiss, PC, Gardiner, DW, Rao, S, et al. Association of histologic tumor characteristics and size of surgical margins with clinical outcome after surgical removal of cutaneous mast cell tumors in dogs. J Am Vet Med Assoc. 2011;238:1464–1469.
78. Hume, CT, Kiupel, M, Rigatti, L, et al. Outcomes of dogs with grade 3 mast cell tumors: 43 cases (1997-2007). J Am Anim Hosp Assoc. 2011;47:37–44.
79. Northrup, NC, Harmon, BG, Gieger, TL, et al. Variation among pathologists in histologic grading of canine cutaneous mast cell tumors. J Vet Diagn Invest. 2005;17:245–248.
80. Northrup, NC, Howerth, EW, Harmon, BG, et al. Variation among pathologists in the histologic grading of canine cutaneous mast cell tumors with uniform use of a single grading reference. J Vet Diagn Invest. 2005;17:561–564.
81. Kiupel, M, Webster, JD, Bailey, KL, et al. Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Vet Pathol. 2011;48:147–155.
82. Preziosi, R, Sarli, G, Paltrinieri, M. Prognostic value of intratumoral vessel density in cutaneous mast cell tumors of the dog. J Comp Pathol. 2004;130:143–151.
83. Abadie, JJ, Amardeilh, MA, Delverdier, ME. Immunohistochemical detection of proliferating cell nuclear antigen and Ki-67 in mast cell tumors from dogs. J Am Vet Med Assoc. 1999;215:1629–1634.
84. Scase, TJ, Edwards, D, Miller, J, et al. Canine mast cell tumors: correlation of apoptosis and proliferation markers with prognosis. J Vet Intern Med. 2006;20:151–158.
85. Seguin, B, Besancon, MF, McCallan, JL, et al. Recurrence rate, clinical outcome, and cellular proliferation indices as prognostic indicators after incomplete surgical excision of cutaneous grade II mast cell tumors: 28 dogs (1994-2002). J Vet Intern Med. 2006;20(4):933–940.
86. Webster, JD, Yuzbasiyan-Gurkan, V, Miller, RA, et al. Cellular proliferation in canine cutaneous mast cell tumors: associations with c-KIT and its role in prognostication. Vet Pathol. 2007;44:298–308.
87. Maglennon, GA, Murphy, S, Adams, V, et al. Association of Ki67 index with prognosis for intermediate-grade canine cutaneous mast cell tumours. Vet Comp Oncol. 2008;6:268–274.
88. Ozaki, K, Yamagami, T, Nomura, K, et al. Prognostic significance of surgical margin, Ki-67 and cyclin D1 protein expression in grade II canine cutaneous mast cell tumor. J Vet Med Sci. 2007;69:1117–1121.
89. Sakai, H, Noda, A, Shirai, N, et al. Proliferative activity of canine mast cell tumours evaluated by bromodeoxyuridine incorporation and Ki-67 expression. J Comp Pathol. 2002;127:233–238.
90. Thompson, JJ, Yager, JA, Best, SJ, et al. Canine subcutaneous mast cell tumors: cellular proliferation and KIT expression as prognostic indices. Vet Pathol. 2011;48:169–181.
91. Kravis, LD, Vail, DM, Kisseberth, WC, et al. Frequency of argyrophilic nucleolar organizer regions in fine-needle aspirates and biopsy specimens from mast cell tumors in dogs. J Am Vet Med Assoc. 1996;209:1418–1420.
92. Romansik, EM, Reilly, CM, Kass, PH, et al. Mitotic index is predictive for survival for canine cutaneous mast cell tumors. Vet Pathol. 2007;44:335–341.
93. Elston, L, Sueiro, FA, Cavalcanti, J, et al. The importance of the mitotic index as a prognostic factor for canine cutaneous mast cell tumors - a validation study. Vet Pathol. 2009;46:362–365.
94. Preziosi, R, Sarli, G, Paltrinieri, M. Multivariate survival analysis of histological parameters and clinical presentation in canine cutaneous mast cell tumours. Vet Res Commun. 2007;31:287–296.
95. Thompson, JJ, Pearl, DL, Yager, JA, et al. Canine subcutaneous mast cell tumor: characterization and prognostic indices. Vet Pathol. 2011;48:156–168.
96. Ayl, RD, Couto, CG, Hammer, AS, et al. Correlation of DNA ploidy to tumor histologic grade, clinical variables, and survival in dogs with mast cell tumors. Vet Pathol. 1992;29:386–390.
97. Patruno, R, Arpaia, N, Gadaleta, CD, et al. VEGF concentration from plasma-activated platelets rich correlates with microvascular density and grading in canine mast cell tumour spontaneous model. J Cell Mol Med. 2009;13:555–561.
98. Strefezzi Rde, F, Xavier, JG, Catao-Dias, JL. Morphometry of canine cutaneous mast cell tumors. Vet Pathol. 2003;40:268–275.
99. Strefezzi Rde, F, Xavier, JG, Kleeb, SR, et al. Nuclear morphometry in cytopathology: a prognostic indicator for canine cutaneous mast cell tumors. J Vet Diagn Invest. 2009;21:821–825.
100. Webster, JD, Kiupel, M, Kaneene, JB, et al. The use of KIT and tryptase expression patterns as prognostic tools for canine cutaneous mast cell tumors. Vet Pathol. 2004;41:371–377.
101. Bergman, PJ, Craft, DM, Newman, SJ, et al. Correlation of histologic grading of canine mast cell tumors with Ki67/PCNA/AgNOR/c-Kit scores: 38 cases (2002-2003). Vet Comp Oncol. 2004;2:98.
102. Moriello, KA, Rosenthal, RC. Clinical approach to tumors of the skin and subcutaneous tissues. Vet Clin North Am Small Anim Pract. 1990;20:1163–1190.
103. O’Keefe, DA. Canine mast cell tumors. Vet Clin North Am Sm Anim Pract. 1990;20:1105–1115.
104. Richardson, RC, Rebar, AH, Elliott, GS. Common skin tumors of the dog: A clinical approach to diagnosis and treatment. Comp Cont Ed Pract Vet. 1984;6:1080–1086.
105. Turrel, JM, Kitchell, BE, Miller, LM, et al. Prognostic factors for radiation treatment of mast cell tumor in 85 dogs. J Am Vet Med Assoc. 1988;193:936–940.
106. Cahalane, AK, Payne, S, Barber, LG, et al. Prognostic factors for survival of dogs with inguinal and perineal mast cell tumors treated surgically with or without adjunctive treatment: 68 cases (1994-2002). J Am Vet Med Assoc. 2004;225:401–408.
107. Sfiligoi, G, Rassnick, KM, Scarlett, JM, et al. Outcome of dogs with mast cell tumors in the inguinal or perineal region versus other cutaneous locations: 124 cases (1990-2001). J Am Vet Med Assoc. 2005;226:1368–1374.
108. Hillman, LA, Garrett, LD, de Lorimier, LP, et al. Biological behavior of oral and perioral mast cell tumors in dogs: 44 cases (1996-2006). J Am Vet Med Assoc. 2010;237:936–942.
109. Gieger, TL, Theon, AP, Werner, JA, et al. Biologic behavior and prognostic factors for mast cell tumors of the canine muzzle: 24 cases (1990-2001). J Vet Intern Med. 2003;17:687–692.
110. Fife, M, Blocker, T, Fife, T, et al. Canine conjunctival mast cell tumors: a retrospective study. Vet Ophthalmol. 2011;14:153–160.
111. Krick, EL, Billings, AP, Shofer, FS, et al. Cytological lymph node evaluation in dogs with mast cell tumours: association with grade and survival. Vet Comp Oncol. 2009;7:130–138.
112. Murphy, S, Sparkes, AH, Blunden, AS, et al. Effects of stage and number of tumours on prognosis of dogs with cutaneous mast cell tumours. Vet Rec. 2006;158:287–291.
113. Thamm, DH, Mauldin, EA, Vail, DM. Prednisone and vinblastine chemotherapy for canine mast cell tumor–41 cases (1992-1997). J Vet Intern Med. 1999;13:491–497.
114. Thamm, DH, Turek, MM, Vail, DM. Outcome and prognostic factors following adjuvant prednisone/vinblastine chemotherapy for high-risk canine mast cell tumour: 61 cases. J Vet Med Sci. 2006;68:581–587.
115. Kiupel, M, Webster, JD, Miller, RA, et al. Impact of tumour depth, tumour location and multiple synchronous masses on the prognosis of canine cutaneous mast cell tumours. J Vet Med A Physiol Pathol Clin Med. 2005;52:280–286.
116. Zavodovskaya, R, Chien, MB, London, CA. Use of kit internal tandem duplications to establish mast cell tumor clonality in 2 dogs. J Vet Intern Med. 2004;18:915–917.
117. LaDue, T, Price, GS, Dodge, R, et al. Radiation therapy for incompletely resected canine mast cell tumors. Vet Radiol Ultrasound. 1998;39:57–62.
118. Chaffin, K, Thrall, DE. Results of radiation therapy in 19 dogs with cutaneous mast cell tumor and regional lymph node metastasis. Vet Radiol Ultrasound. 2002;43:392–395.
119. Camps-Palau, MA, Leibman, NF, Elmslie, R, et al. Treatment of canine mast cell tumours with vinblastine, cyclophosphamide and prednisone: 35 cases (1997-2004). Vet Comp Oncol. 2007;5:156–167.
120. Clinkenbeard, KD. Diagnostic cytology: Mast cell tumors. Comp Cont Ed Pract Vet. 1991;13:1697–1704.
121. Mederle, O, Mederle, N, Bocan, EV, et al. VEGF expression in dog mastocytoma. Rev Med Chir Soc Med Nat Iasi. 2010;114:185–188.
122. Rabanal, RH, Fondevila, DM, Montane, V, et al. Immunocytochemical diagnosis of skin tumours of the dog with special reference to undifferentiated types. Res Vet Sci. 1989;47:129–133.
123. Sandusky, GE, Carlton, WW, Wightman, KA. Diagnostic immunohistochemistry of canine round cell tumors. Vet Pathol. 1987;24:495–499.
124. Bookbinder, PF, Butt, MT, Harvey, HJ. Determination of the number of mast cells in lymph node, bone marrow, and buffy coat cytologic specimens from dogs. J Am Vet Med Assoc. 1992;200:1648–1650.
125. Sato, AF, Solano, M. Ultrasonographic findings in abdominal mast cell disease: a retrospective study of 19 patients. Vet Radiol Ultrasound. 2004;45:51–57.
126. Stefanello, D, Valenti, P, Faverzani, S, et al. Ultrasound-guided cytology of spleen and liver: a prognostic tool in canine cutaneous mast cell tumor. J Vet Intern Med. 2009;23:1051–1057.
127. Book, AP, Fidel, J, Wills, T, et al. Correlation of ultrasound findings, liver and spleen cytology, and prognosis in the clinical staging of high metastatic risk canine mast cell tumors. Vet Radiol Ultrasound. 2011;52:548–554.
128. Hahn, KA, Lantz, GC, Salisbury, SK. Comparison of survey radiography with ultrasonography and X-ray computed tomography for clinical staging of subcutaneous neoplasms in dogs. J Am Vet Med Assoc. 1990;196:1795–1798.
129. Cayatte, SM, McManus, PM, Miller, WH, Jr., et al. Identification of mast cells in buffy coat preparations from dogs with inflammatory skin diseases. J Am Vet Med Assoc. 1995;206:325–326.
130. McManus, PM. Frequency and severity of mastocytemia in dogs with and without mast cell tumors: 120 cases (1995-1997). J Am Vet Med Assoc. 1999;215:355–357.
131. Stockham, SL, Basel, DL, Schmidt, DA. Mastocytemia in dogs with acute inflammatory diseases. Vet Clin Pathol. 1986;15:16–21.
132. Endicott, MM, Charney, SC, McKnight, JA, et al. Clinicopathological findings and results of bone marrow aspiration in dogs with cutaneous mast cell tumours: 157 cases (1999-2002). Vet Comp Oncol. 2007;5:31–37.
133. Plier, ML, MacWilliams, PS. Systemic mastocytosis and mast cell leukemia. In Feldman BF, Zinkl JG, Jain NC, eds.: Schalm’s veterinary hematology, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2000.
134. Hikasa, Y, Morita, T, Futaoka, Y, et al. Connective tissue-type mast cell leukemia in a dog. J Vet Med Sci. 2000;62:187–190.
135. Simpson, AM, Ludwig, LL, Newman, SJ, et al. Evaluation of surgical margins required for complete excision of cutaneous mast cell tumors in dogs. J Am Vet Med Assoc. 2004;224:236–240.
136. Fulcher, RP, Ludwig, LL, Bergman, PJ, et al. Evaluation of a two-centimeter lateral surgical margin for excision of grade I and grade II cutaneous mast cell tumors in dogs. J Am Vet Med Assoc. 2006;228:210–215.
137. Johnson, RE, Sigman, JD, Funk, GF, et al. Quantification of surgical margin shrinkage in the oral cavity. Head Neck. 1997;19:281–286.
138. Kerns, MJ, Darst, MA, Olsen, TG, et al. Shrinkage of cutaneous specimens: formalin or other factors involved? J Cutan Pathol. 2008;35:1093–1096.
139. Reimer, SB, Seguin, B, DeCock, HE, et al. Evaluation of the effect of routine histologic processing on the size of skin samples obtained from dogs. Am J Vet Res. 2005;66:500–505.
140. Allan, GS, Gilette, EL. Response of canine mast cell tumors to radiation. J Natl Cancer Inst. 1979;63:691–694.
141. Gillette, EL. Indications and selection of patients for radiation therapy. Vet Clin North Am Small Anim Pract. 1974;4:889–896.
142. Gillette, EL. Radiation therapy of canine and feline tumors. J Am Anim Hosp Assoc. 1976;12:359–362.
143. Gillette, EL. Veterinary radiotherapy. J Am Vet Med Assoc. 1976;157:1707–1712.
144. McClelland, RB. The treatment of mastocytomas in dogs. Cornell Vet. 1964;54:517–519.
145. Dobson, J, Cohen, S, Gould, S. Treatment of canine mast cell tumours with prednisolone and radiotherapy. Vet Comp Oncol. 2004;2:132–141.
146. al-Sarraf, R, Mauldin, GN, Patnaik, AK, et al. A prospective study of radiation therapy for the treatment of grade 2 mast cell tumors in 32 dogs. J Vet Intern Med. 1996;10:376–378.
147. Frimberger, AE, Moore, AS, LaRue, SM, et al. Radiotherapy of incompletely resected, moderately differentiated mast cell tumors in the dog: 37 cases (1989-1993). J Am Anim Hosp Assoc. 1997;33:320–324.
148. Poirier, VJ, Adams, WM, Forrest, LJ, et al. Radiation therapy for incompletely excised grade II canine mast cell tumors. J Am Anim Hosp Assoc. 2006;42:430–434.
149. Hahn, KA, King, GK, Carreras, JK. Efficacy of radiation therapy for incompletely resected grade-III mast cell tumors in dogs: 31 cases (1987-1998). J Am Vet Med Assoc. 2004;224:79–82.
150. Hosoya, K, Kisseberth, WC, Alvarez, FJ, et al. Adjuvant CCNU (lomustine) and prednisone chemotherapy for dogs with incompletely excised grade 2 mast cell tumors. J Am Anim Hosp Assoc. 2009;45:14–18.
151. Davies, DR, Wyatt, KM, Jardine, JE, et al. Vinblastine and prednisolone as adjunctive therapy for canine cutaneous mast cell tumors. J Am Anim Hosp Assoc. 2004;40:124–130.
152. Misdorp, W. Incomplete surgery, local immunostimulation, and recurrence of some tumour types in dogs and cats. Vet Q. 1987;9:279–286.
153. Lagoretta, RA, Denman, DL, Kelley, MC, et al. Use of hyperthermia and radiotherapy in treatment of a large mast cell sarcoma in a dog. J Am Vet Med Assoc. 1988;193:1545–1548.
154. Theon, AP, Madewell, BR, Castro, J. High dose-rate remote afterloading brachytherapy: Preliminary results in canine and feline cutaneous and subcutaneous tumors. Proc Annu Conf Vet Cancer Soc. 1993;23:109–110.
155. Northrup, NC, Roberts, RE, Harrell, TW, et al. Iridium-192 interstitial brachytherapy as adjunctive treatment for canine cutaneous mast cell tumors. J Am Anim Hosp Assoc. 2004;40:309–315.
156. Frimberger, AE, Moore, AS, Cincotta, L, et al. Photodynamic therapy of naturally occurring tumors in animals using a novel benzophenothiazine photosensitizer. Clin Cancer Res. 1998;4:2207–2218.
157. Tanabe, S, Yamaguchi, M, Iijima, M, et al. Fluorescence detection of a new photosensitizer, PAD-S31, in tumour tissues and its use as a photodynamic treatment for skin tumours in dogs and a cat: a preliminary report. Vet J. 2004;167:286–293.
158. Rogers, KS. Common questions about diagnosing and treating canine mast cell tumors. Vet Med. 1993;88:246–250.
159. Spugnini, EP, Vincenzi, B, Baldi, F, et al. Adjuvant electrochemotherapy for the treatment of incompletely resected canine mast cell tumors. Anticancer Res. 2006;26:4585–4589.
160. Spugnini, EP, Vincenzi, B, Citro, G, et al. Evaluation of cisplatin as an electrochemotherapy agent for the treatment of incompletely excised mast cell tumors in dogs. J Vet Intern Med. 2011;25:407–411.
161. Kodre, V, Cemazar, M, Pecar, J, et al. Electrochemotherapy compared to surgery for treatment of canine mast cell tumours. In Vivo. 2009;23:55–62.
162. Neyens, IJ, Kirpensteijn, J, Grinwis, GC, et al. Pilot study of intraregional deionised water adjunct therapy for mast cell tumours in dogs. Vet Rec. 2004;154:90–91.
163. Grier, RL, Di Guardo, G, Schaffer, CB, et al. Mast cell tumor destruction by deionized water. Am J Vet Res. 1990;51:1116–1120.
164. Grier, RL, DiGuardo, G, Myers, R, et al. Mast cell tumour destruction in dogs by hypotonic solution. J Small Anim Pract. 1995;36:385–388.
165. Jaffe, MH, Hosgood, G, Kerwin, SC, et al. The use of deionized water for the treatment of canine cutaneous mast cell tumors. Vet Cancer Soc Newsl. 1998;22:9–10.
166. Jaffe, MH, Hosgood, G, Kerwin, SC, et al. Deionised water as an adjunct to surgery for the treatment of canine cutaneous mast cell tumours. J Small Anim Pract. 2000;41:7–11.
167. Brocks, BA, Neyens, IJ, Teske, E, et al. Hypotonic water as adjuvant therapy for incompletely resected canine mast cell tumors: a randomized, double-blind, placebo-controlled study. Vet Surg. 2008;37:472–478.
168. Asboe-Hanson, G. The mast cell: Cortisone action on connective tissue. Proc Soc Exp Biol Med. 1952;80:677–679.
169. Bloom, F. Effect of cortisone on mast cell tumors (mastocytoma) of the dog. Proc Soc Exp Biol Med. 1952;80:651–654.
170. Brodey, RS, McGrath, JT, Martin, JE. Preliminary observations on the use of cortisone in canine mast cell sarcoma. J Am Vet Med Assoc. 1953;123:391–393.
171. Stanclift, RM, Gilson, SD. Evaluation of neoadjuvant prednisone administration and surgical excision in treatment of cutaneous mast cell tumors in dogs. J Am Vet Med Assoc. 2008;232:53–62.
172. McCaw, DL, Miller, MA, Ogilvie, GK, et al. Response of canine mast cell tumors to treatment with oral prednisone. J Vet Intern Med. 1994;8:406–408.
173. Takahashi, T, Kadosawa, T, Nagase, M, et al. Inhibitory effects of glucocorticoids on proliferation of canine mast cell tumor. J Vet Med Sci. 1997;59:995–1001.
174. Matsuda, A, Tanaka, A, Amagai, Y, et al. Glucocorticoid sensitivity depends on expression levels of glucocorticoid receptors in canine neoplastic mast cells. Vet Immunol Immunopathol. 2011;144:321–328.
175. Rassnick, KM, Al-Sarraf, R, Bailey, DB, et al. Phase II open-label study of single-agent hydroxyurea for treatment of mast cell tumours in dogs. Vet Comp Oncol. 2010;8:103–111.
175b. Henry, CJ, Downing, S, Rosenthal, RC, et al. Evaluation of a novel immunomodulator composed of human chorionic gonadotropin and bacillus Calmette-Guerin for treatment of canine mast cell tumors in clinically affected dogs. Am J Vet Res. 2007;68:1246–1251.
176. Valent, P, Arock, M, Akin, C, et al. The classification of systemic mastocytosis should include mast cell leukemia (MCL) and systemic mastocytosis with a clonal hematologic non-mast cell lineage disease (SM-AHNMD). Blood. 2010;116:850–851.
177. Cooper, M, Tsai, X, Bennett, P. Combination CCNU and vinblastine chemotherapy for canine mast cell tumours: 57 cases. Vet Comp Oncol. 2009;7:196–206.
178. Rassnick, KM, Moore, AS, Williams, LE, et al. Treatment of canine mast cell tumors with CCNU (lomustine). J Vet Intern Med. 1999;13:601–605.
179. McCaw, DL, Miller, MA, Bergman, PJ, et al. Vincristine therapy for mast cell tumors in dogs. J Vet Intern Med. 1997;11:375–378.
180. Grant, IA, Rodriguez, CO, Kent, MS, et al. A phase II clinical trial of vinorelbine in dogs with cutaneous mast cell tumors. J Vet Intern Med. 2008;22:388–393.
181. Taylor, F, Gear, R, Hoather, T, et al. Chlorambucil and prednisolone chemotherapy for dogs with inoperable mast cell tumours: 21 cases. J Small Anim Pract. 2009;50:284–289.
182. Rassnick, KM, Bailey, DB, Russell, DS, et al. A phase II study to evaluate the toxicity and efficacy of alternating CCNU and high-dose vinblastine and prednisone (CVP) for treatment of dogs with high-grade, metastatic or nonresectable mast cell tumours. Vet Comp Oncol. 2010;8:138–152.
183. Malone, EK, Rassnick, KM, Wakshlag, JJ, et al. Calcitriol (1, 25-dihydroxycholecalciferol) enhances mast cell tumour chemotherapy and receptor tyrosine kinase inhibitor activity in vitro and has single-agent activity against spontaneously occurring canine mast cell tumours. Vet Comp Oncol. 2010;8:209–220.
184. Hayes, A, Adams, V, Smith, K, et al. Vinblastine and prednisolone chemotherapy for surgically excised grade III canine cutaneous mast cell tumours. Vet Comp Oncol. 2007;5:168–176.
185. Rassnick, KM, Bailey, DB, Flory, AB, et al. Efficacy of vinblastine for treatment of canine mast cell tumors. J Vet Intern Med. 2008;22:1390–1396.
186. Vickery, KR, Wilson, H, Vail, DM, et al. Dose-escalating vinblastine for the treatment of canine mast cell tumour. Vet Comp Oncol. 2008;6:111–119.
187. Singh, J, Rana, JS, Sood, N, et al. Clinico-pathological studies on the effect of different anti-neoplastic chemotherapy regimens on transmissible venereal tumours in dogs. Vet Res Commun. 1996;20:71–81.
188. Ma, Y, Longley, BJ, Wang, X, et al. Clustering of activating mutations in c-KIT’s juxtamembrane coding region of canine mast cell neoplasms. J Invest Dermatol. 1999;112:165–170.
189. Liao, AT, Chien, MB, Shenoy, N, et al. Inhibition of constitutively active forms of mutant kit by multitargeted indolinone tyrosine kinase inhibitors. Blood. 2002;100:585–593.
190. Pryer, NK, Lee, LB, Zadovaskaya, R, et al. Proof of target for SU11654: inhibition of KIT phosphorylation in canine mast cell tumors. Clin Cancer Res. 2003;9:5729–5734.
191. London, CA, Malpas, PB, Wood-Follis, SL, et al. Multi-center, placebo-controlled, double-blind, randomized study of oral toceranib phosphate (SU11654), a receptor tyrosine kinase inhibitor, for the treatment of dogs with recurrent (either local or distant) mast cell tumor following surgical excision. Clin Cancer Res. 2009;15:3856–3865.
192. Carlsten, KS, London, CA, Haney, S, et al. Multicenter, prospective trial of hypofractionated radiation therapy plus toceranib for unresectable canine mast cell tumors. J Vet Intern Med. 2012;26:135–141.
193. London, C, Mathie, T, Stingle, N, et al. Preliminary evidence for biologic activity of toceranib phosphate (Palladia) in solid tumours. Vet Comp Oncol Epub ahead of print. 2011.
194. Hahn, KA, Ogilvie, G, Rusk, T, et al. Masitinib is safe and effective for the treatment of canine mast cell tumors. J Vet Intern Med. 2008;22:1301–1309.
195. Hahn, KA, Legendre, AM, Shaw, NG, et al. Evaluation of 12- and 24-month survival rates after treatment with masitinib in dogs with nonresectable mast cell tumors. Am J Vet Res. 2010;71:1354–1361.
196. Isotani, M, Ishida, N, Tominaga, M, et al. Effect of tyrosine kinase inhibition by imatinib mesylate on mast cell tumors in dogs. J Vet Intern Med. 2008;22(4):985–988.
197. Marconato, L, Bettini, G, Giacoboni, C, et al. Clinicopathological features and outcome for dogs with mast cell tumors and bone marrow involvement. J Vet Intern Med. 2008;22(4):1001–1007.
198. Yamada, O, Kobayashi, M, Sugisaki, O, et al. Imatinib elicited a favorable response in a dog with a mast cell tumor carrying a c-kit c.1523A>T mutation via suppression of constitutive KIT activation. Vet Immunol Immunopathol. 2011;142:101–106.
199. Robat, C, London, C, Bunting, L, et al. Safety evaluation of combination vinblastine and toceranib phosphate (Palladia) in dogs: a phase I dose-finding study. Vet Comp Oncol Epub ahead of print. 2011.
200. Kisseberth, WC, Murahari, S, London, CA, et al. Evaluation of the effects of histone deacetylase inhibitors on cells from canine cancer cell lines. Am J Vet Res. 2008;69:938–945.
201. Lin, TY, Fenger, J, Murahari, S, et al. AR-42, a novel HDAC inhibitor, exhibits biologic activity against malignant mast cell lines via down-regulation of constitutively activated Kit. Blood. 2010;115:4217–4225.
202. Nagamine, MK, Sanches, DS, Pinello, KC, et al. In vitro inhibitory effect of trichostatin A on canine grade 3 mast cell tumor. Vet Res Commun. 2011;35:391–399.
203. Lin, TY, Bear, M, Du, Z, et al. The novel HSP90 inhibitor STA-9090 exhibits activity against Kit-dependent and -independent malignant mast cell tumors. Exp Hematol. 2008;36:1266–1277.
204. London, CA, Bear, MD, McCleese, J, et al. Phase I evaluation of STA-1474, a Prodrug of the novel HSP90 inhibitor Ganetespib, in dogs with spontaneous cancer. PLoS One. 2011;6:e27018.
205. Pinello, KC, Nagamine, M, Silva, TC, et al. In vitro chemosensitivity of canine mast cell tumors grades II and III to all-trans-retinoic acid (ATRA). Vet Res Commun Epub ahead of print. 2009.
206. Ohashi, E, Miyajima, N, Nakagawa, T, et al. Retinoids induce growth inhibition and apoptosis in mast cell tumor cell lines. J Vet Med Sci. 2006;68:797–802.
207. Miyajima, N, Watanabe, M, Ohashi, E, et al. Relationship between retinoic acid receptor alpha gene expression and growth-inhibitory effect of all-trans retinoic acid on canine tumor cells. J Vet Intern Med. 2006;20:348–354.
208. Elders, RC, Baines, SJ, Catchpole, B. Susceptibility of the C2 canine mastocytoma cell line to the effects of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL). Vet Immunol Immunopathol. 2009;130:11–16.
209. Peter, B, Gleixner, KV, Cerny-Reiterer, S, et al. Polo-like kinase-1 as a novel target in neoplastic mast cells: demonstration of growth-inhibitory effects of small interfering RNA and the Polo-like kinase-1 targeting drug BI 2536. Haematologica. 2011;96:672–680.
210. Kenyon, AJ, Ramos, L, Michaels, EB. Histamine-induced suppressor macrophage inhibits fibroblast growth and wound healing. Am J Vet Res. 1983;44:2164–2166.
211. Huttunen, M, Hyttinen, M, Nilsson, G, et al. Inhibition of keratinocyte growth in cell culture and whole skin culture by mast cell mediators. Exp Dermatol. 2001;10:184–192.
212. Saar, C, Opitz, M, Lange, W, et al. Mastzellenreitkulose bei katzen. Berl Munch Tierarztl Wochenschr. 1969;82:438–444.
213. Hadzijusufovic, E, Peter, B, Rebuzzi, L, et al. Growth-inhibitory effects of four tyrosine kinase inhibitors on neoplastic feline mast cells exhibiting a Kit exon 8 ITD mutation. Vet Immunol Immunopathol. 2009;132:243–250.
214. Isotani, M, Tamura, K, Yagihara, H, et al. Identification of a c-kit exon 8 internal tandem duplication in a feline mast cell tumor case and its favorable response to the tyrosine kinase inhibitor imatinib mesylate. Vet Immunol Immunopathol. 2006;114:168–172.
215. Isotani, M, Yamada, O, Lachowicz, JL, et al. Mutations in the fifth immunoglobulin-like domain of kit are common and potentially sensitive to imatinib mesylate in feline mast cell tumours. Br J Haematol. 2009;148:144–153.
216. Mohr, FC, Dunston, SK. Culture and initial characterization of the secretory response of neoplastic cat mast cells. Am J Vet Res. 1992;53:820–828.
217. Antognoni, MT, Spaterna, A, Lepri, E, et al. Characteristic clinical, haematological and histopathological findings in feline mastocytoma. Vet Res Commun. 2003;27(suppl 1):727–730.
218. Feinmehl, R, Matus, R, Mauldin, GN, et al. Splenic mast cell tumors in 43 cats (1975-1992). Proc Annu Conf Vet Cancer Soc. 1992;12:50.
219. Macy, DW, Reynolds, HA. The incidence, characteristics, and clinical management of skin tumors of cats. J Am Anim Hosp Assoc. 1981;17:1026–1034.
220. Buerger, RG, Scott, DW. Cutaneous mast cell neoplasia in cats: 14 cases (1975-1985). J Am Vet Med Assoc. 1987;190:1440–1444.
221. Wilcock, BP, Yager, JA, Zink, MC. The morphology and behavior of feline cutaneous mastocytomas. Vet Pathol. 1986;23:320–324.
222. Chastain, CB, Turk, MA, O’Brien, D. Benign cutaneous mastocytomas in two litters of Siamese kittens. J Am Vet Med Assoc. 1988;193:959–960.
223. Holzinger, EA. Feline cutaneous mastocytomas. Cornell Vet. 1973;63:87–93.
224. Litster, AL, Sorenmo, KU. Characterisation of the signalment, clinical and survival characteristics of 41 cats with mast cell neoplasia. J Feline Med Surg. 2006;8:177–183.
225. Molander-McCrary, H, Henry, CJ, Potter, K, et al. Cutaneous mast cell tumors in cats: 32 cases (1991-1994). J Am Anim Hosp Assoc. 1998;34:281–284.
226. Johnson, TO, Schulman, FY, Lipscomb, TP, et al. Histopathology and biologic behavior of pleomorphic cutaneous mast cell tumors in fifteen cats. Vet Pathol. 2002;39:452–457.
227. Garrett, LD, Craig, CL, Szladovits, B, et al. Evaluation of buffy coat smears for circulating mast cells in healthy cats and ill cats without mast cell tumor-related disease. J Am Vet Med Assoc. 2007;231:1685–1687.
228. Skeldon, NC, Gerber, KL, Wilson, RJ, et al. Mastocytaemia in cats: prevalence, detection and quantification methods, haematological associations and potential implications in 30 cats with mast cell tumours. J Feline Med Surg. 2010;12:960–966.
229. Rodriguez-Carino, C, Fondevila, D, Segales, J, et al. Expression of KIT receptor in feline cutaneous mast cell tumors. Vet Pathol. 2009;46:878–883.
230. Fondevila, D, Rabanal, R, Ferrer, L. Immunoreactivity of canine and feline mast cell tumors. Schweiz Arch Tierheilk. 1990;132:409–484.
231. Buss, MS, Mollander, H, Potter, K, et al. Predicting survival and prognosis in cats with cutaneous mastocytomas of varying histological grade. Proc Annu Conf Vet Cancer Soc. 1996;16:56–57.
232. Sabattini, S, Bettini, G. Prognostic value of histologic and immunohistochemical features in feline cutaneous mast cell tumors. Vet Pathol. 2010;47:643–653.
233. Montgomery, KW, van der Woerdt, A, Aquino, SM, et al. Periocular cutaneous mast cell tumors in cats: evaluation of surgical excision (33 cases). Vet Ophthalmol. 2010;13:26–30.
234. Lepri, E, Ricci, G, Leonardi, L, et al. Diagnostic and prognostic features of feline cutaneous mast cell tumours: a retrospective analysis of 40 cases. Vet Res Commun. 2003;27(suppl 1):707–709.
235. Turrel, JM, Farrelly, J, Page, RL, et al. Evaluation of strontium 90 irradiation in treatment of cutaneous mast cell tumors in cats: 35 cases (1992-2002). J Am Vet Med Assoc. 2006;228:898–901.
236. Rassnick, KM, Gieger, TL, Williams, LE, et al. Phase I evaluation of CCNU (lomustine) in tumor-bearing cats. J Vet Intern Med. 2001;15:196–199.
237. Rassnick, KM, Williams, LE, Kristal, O, et al. Lomustine for treatment of mast cell tumors in cats: 38 cases (1999-2005). J Am Vet Med Assoc. 2008;232:1200–1205.
238. Lachowicz, JL, Post, GS, Brodsky, E. A phase I clinical trial evaluating imatinib mesylate (Gleevec) in tumor-bearing cats. J Vet Intern Med. 2005;19:860–864.
239. Bellamy, F, Bader, T, Moussy, A, et al. Pharmacokinetics of masitinib in cats. Vet Res Commun. 2009;33(8):831–837.
240. Daly, M, Sheppard, S, Cohen, N, et al. Safety of masitinib mesylate in healthy cats. J Vet Intern Med. 2011;25:297–302.
241. Spangler, WL, Culbertson, MR. Prevalence and type of splenic diseases in cats: 455 cases (1985-1991). J Am Vet Med Assoc. 1992;201:773–776.
242. Hanson, JA, Papageorges, M, Girard, E, et al. Ultrasonographic appearance of splenic disease in 101 cats. Vet Radiol Ultrasound. 2001;42:441–445.
243. Guerre, R, Millet, P, Groulade, P. Systemic mastocytosis in a cat: remission after splenectomy. J Small Anim Pract. 1979;20:769–772.
244. Liska, WD, MacEwen, EG, Zaki, FA, et al. Feline systemic mastocytosis: A review and results of splenectomy in seven cases. J Am Anim Hosp Assoc. 1979;15:589–597.
245. Schulman, A. Splenic mastocytosis in a cat. California Vet. 1987;17:17–18.
246. Gordon, SS, McClaran, JK, Bergman, PJ, et al. Outcome following splenectomy in cats. J Feline Med Surg. 2010;12:256–261.
247. Bortnowski, HB, Rosenthal, RC. Gastrointestinal mast cell tumors and eosinophilia in two cats. J Am Anim Hosp Assoc. 1992;28:271–275.
248. Halsey, CH, Powers, BE, Kamstock, DA. Feline intestinal sclerosing mast cell tumour: 50 cases (1997-2008). Vet Comp Oncol. 2010;8:72–79.
249. Arock, M, Valent, P. Pathogenesis, classification and treatment of mastocytosis: state of the art in 2010 and future perspectives. Exp Rev Hematol. 2010;3:497–516.
250. Bodemer, C, Hermine, O, Palmerini, F, et al. Pediatric mastocytosis is a clonal disease associated with D816V and other activating c-KIT mutations. J Invest Dermatol. 2010;130:804–815.
251. Horny, HP, Sotlar, K, Valent, P. Mastocytosis: state of the art. Pathobiology. 2007;74:121–132.
252. Valent, P, Akin, C, Escribano, L, et al. Standards and standardization in mastocytosis: consensus statements on diagnostics, treatment recommendations and response criteria. Eur J Clin Invest. 2007;37:435–453.
253. Ustun, C, Deremer, DL, Akin, C. Tyrosine kinase inhibitors in the treatment of systemic mastocytosis. Leuk Res. 2011;35(9):1143–1152.