CHAPTER 14 Parturition and Dystocia
The average gestation length in mares is approximately 340 days. There is considerable variation; gestation length may range from 315 to 400 days and is influenced by season, with pregnancies that terminate in winter longer than those that terminate in summer. When large variation occurs from the average there always should be some concern and the mare should be examined if indicated. The definition of eutocia is a “normal delivery” or as a safe easy delivery without significant injury to either the fetus or the mare.
MARE PREPARTUM CHANGES
Progesterone concentrations in the peripheral plasma are less than 1 ng/ml during the last half of gestation; thus, measurement of this hormone is useless for determining deficiencies or predicting the time of parturition.1 Other progestogens, 20α-hydroxy-5β-pregnan-3-one and 5β-pregnane-3α,20α-diol, decrease during the last 24 hours prior to parturition.2,3 Prepartum changes in the mare include enlargement of the udder 4 to 6 weeks prior to delivery. This time varies with the individual animal and is somewhat dependent on the number of previous pregnancies, if any. The udder becomes more rounded as it enlarges. Enlargement and edema of the udder and the abdominal wall immediately anterior to the udder are apparent 2 to 3 weeks prior to foaling. Waxing, or the appearance of a sebaceous-like secretion on the teat ends surrounding the sphincter, should occur as the mare approaches parturition. However, waxing has been observed to occur as early as 4 weeks prior to delivery and may not occur in some mares. Waxing generally occurs with regularity in the same animal at approximately the same time prior to parturition. The teats usually fill and distend 2 to 14 days prior to parturition, but this may not be observed. Some mares leak colostrum prior to parturition. This is undesirable because once the colostrum is lost from the udder it is not replaced. Colostrum should be collected and frozen or substitute colostrum should be made available for the foal following delivery.
Relaxation of the tailhead and pelvic ligaments occurs gradually over several weeks before delivery. During this same period the vulva relaxes and the opening elongates. At 1 to 3 weeks prior to foaling, relaxation becomes apparent in the flank area with the mare appearing somewhat “gaunt” in this area. Approximately 7 to 10 days later, the gluteal muscles and the muscles adjacent to the tailhead relax and appear less evident, with the bones in that area more pronounced. The ultrasonographic character of the fluids within the uterus also changes during the last 10 days of gestation, and echogenic particles appear. The vagina and vulva relax and there is an increase in mucus. The vaginal mucosa may appear reddened; this generally occurs within 24 hours of parturition. The cervix becomes completely relaxed and the uterine contractions increase in frequency and strength. Because some mares foal with only a few of these normal prepartum signs, prediction of the exact time of foaling is difficult without further diagnostic tests. Body temperature has been suggested as a possible method to determine the time of parturition before the onset of stage I of labor.4,5 Although it has been demonstrated that changes in body temperature measured at 6-hour intervals with an electronic rectal thermometer were not adequate to predict parturition, the use of telemetry with a computerized system to record core body temperatures at 15-minute intervals could be useful in parturition prediction.6,7
Several commercial aids are available for use in determining approximately when parturition will occur. These include the Sofchek Test strip, the Titrets Calcium Hardness Test Kit, and the Predict-a-Foal Predictor Kit. The Sofchek Test strips indicate there is a 79% probability of parturition within 24 hours when the hardness test strip exceeds 250 ppm. The Titret Calcium Hardness Test strip indicates a 53% probability of parturition within 24 hours when the hardness exceeds 250 ppm. The Predict-a-Foal Predictor Kit indicates a 59% probability of parturition within 24 hours if the color change is a 4 or greater. These tests are more predictive of indicating when the mare will not foal rather than when parturition will occur.
A number of methods commonly are used to monitor the actual parturition. The most frequently used and oldest method is to stay in the barn with the mare and personally observe. This method obviously has several disadvantages including inclement weather and loss of sleep. This system is not 100% effective, and many people have fallen asleep while supposedly observing the foaling or have gone to the house for a few minutes and have missed the birth. Others systems designed to improve the quality of life of the foaling attendant include video cameras, sound monitors, the Foal-alert system, the Birth Alert system, and other systems designed for the mare at parturition. Video cameras have progressed considerably from the days of the poor image quality requiring a great deal of light and hard wiring. The systems of today require minimal lighting and no wires. The cost of these systems also has been greatly reduced, making them affordable to most horse farms. They permit the person monitoring the mare to remain in a more comfortable environment than would otherwise be possible. The author has used several video monitoring systems over the past 22 years and has found them to be worth the cost. Sound monitors including baby monitors and intercoms are of limited value because many horse sounds may “wake” a horse owner and not be related to foaling. However, they do work in combination with other systems such as the monitors, which emit an audible signal at the time of parturition. The Foal-alert system is a monitoring device that includes the placement of a transmitter on the vulvar lips such that at the time of parturition the lips spread with passage of the fetus and the transmitter is activated. The receiver is activated and it produces an audible sound, which can be heard within the barn or transmitted by phone or pager to a distant point. An intercom system can also be used to transfer the alarm sound to a house or sleeping area of the foaling attendant. The Foal-alert system works excellently if any portion of the fetus or fetal membranes filled with fluids reaches the vulvar lips and causes activation of the transmitter. The Birth Alert system is another foaling monitoring system that utilizes a transmitter in the anterior vagina and is activated when the transmitter is expelled from the vagina and the temperature sensor signals the decrease in temperature to the receiver. The receiver transmits an audible signal.
Restlessness increases as the mare approaches parturition. Prior to this increase, mares may demonstrate decreased activity that could last for several weeks. Personality changes are obvious as the time of parturition approaches. This is especially true during the 24 hours before birth. Distractions of any kind should be kept to a minimum during this period. Changes in prepartum myometrial activity have been reported.8,9 Internally, during this period, the mare’s uterus begins more active contractions beginning at the end of the uterus near the ovary and progressing posteriorly toward the cervix.
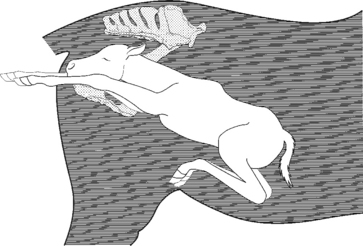
The fetus is in a variety of presentations until approximately the sixth month of gestation when it aligns itself in a cranial presentation (Fig. 14-1). Presentation may change after this stage, however, and therefore cannot beused reliably to determine the presentation of the fetus until parturition actually begins. The fetus assumes a variety of positions, including dorsosacral, for longer durations as term approaches. As parturition approaches, the head and forelimbs can be palpated in the pelvic canal of the mare and may at times be alongside the cervix with pressure on the vaginal wall.
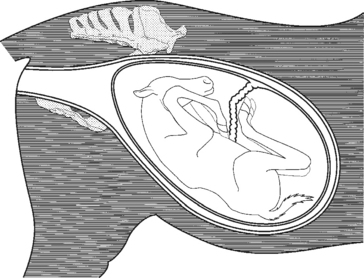
Fig. 14-1 Fetal presentation and posture 2 to 3 months before birth.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
There is no need to wrap the mare’s tail, wash the perineal area, or wash the udder before foaling. These procedures, although recommended by some, mostly serve to disrupt the mare and have no medical basis. However, cleaning the stall and maintaining reasonable cleanliness are especially important before and immediately post partum. This could include disinfecting stalls between mares but is not practical with most farm facilities. For disinfectants to be effective, all organic material must be removed. This is usually only feasible with a high-pressure sprayer and requires that relatively nonporous material be used in the construction of stalls, including the floor. Stalls should be at least 12 ft by 12 ft or larger and be bedded preferably with large quantities of straw. Other types of bedding material may promote bacterial growth or be too dusty for use with neonates or postpartum mares. If Caslick’s procedure has been performed to improve vulvar conformation, the vulva should be opened approximately 14 days prior to the due date or as determined by visual assessment of the mare’s preparation for foaling.
Stage I
Sweating initiated in the shoulder area combined with frequent observations of the flank area by the mare are indicators that stage I of labor is occurring. Kicking, biting of the flank, or other signs of mild colic frequently occur during this period. During this stage, final positioning and posturing of the fetus occur. The front feet and the nose make an excellent wedge to aid in cervical dilatation. This is also assisted by pressure of the fetal fluid on the cervical opening. The increase in pressure is first due to increased uterine activity. As the pressure increases and the cervix starts to dilate, oxytocin is released. Oxytocin increases the uterine contractions and indirectly stimulates the abdominal muscles to contract and further increase the uterine pressure. The beginning of stage I of parturition is difficult to determine because its onset is not marked by any single event or change in the mare and is rather vague and variable. As the normal mare approaches foaling, she may have a decrease in activity the day before the night of foaling. It has been reported that approximately 85% of mares foal between 7:00 PM and 9:00 AM, with most mares foaling between 11:00 PM and 4:00 AM.4 Within 2 hours prior to foaling, the mare may become restless and show signs of colic. She may paw the ground and stop eating for short periods of time as an indication of pain. Increased switching or movement of the tail is also usually observed as the mare approaches parturition. Milk may be seen squirting from the teats. This activity is associated with oxytocin release and apparent uterine pain. Signs of pain are not constant but intermittent and correspond with uterine contractions. These periods may last from 1 or 2 minutes to 20 minutes in length. These events may not be observed in older mares, even though the entire process may take several hours. This explains how mares are able to foal during the 30 minutes an observer may be absent. The mare should be observed but left undisturbed unless problems arise. The average range for this period is 1 to 4 hours. Any disturbances may delay the foaling and result in complications. The chorioallantoic membrane ruptures and the allantoic fluid escapes, marking the end of stage I.
The fetal heart rate prior to the onset of parturition is approximately 76 beats per minute, with elevations occurring with increased activity. Heart rate may increase by as much as 40 beats per minute and the accelerations may average one per minute. The activity of the fetus is most pronounced during the period of 5 to 72 hours prepartum. The fetal heart rate during the 24 hours prior to delivery is approximately 62 beats per minute and during stage I and stage II is between 54 and 60 beats per minute. The heart rate of the neonate averages over 100 beats per minute.
Stage II
Signs of the second stage of labor are more apparent. The mare lies down during most of this period; although she may sit up and lie down several times and is generally sweating. When in the recumbent position, all legs may be extended and the head stretched outward away from the body (Fig. 14-2). She may bite her flank area or chew on hay or straw. During stage II of labor, the mare frequently urinates and defecates because of the pressure applied by the contracting uterus and the abdominal wall and the presence of the fetus and fetal fluids. Some mares may roll in an apparent attempt to lessen the pain or position the fetus. The average time for stage II is 20 minutes, calculated from the time of chorioallantoic membrane rupture until delivery of the fetus. It is abnormal for mares to continue this stage of labor longer than 70 minutes, and prolonged second stage indicates problems are present and fetal death is likely. It is generally recommended that mares be given 20 minutes to complete the second stage before the foaling attendant becomes alarmed. Normal progression in the delivery process should occur during this period.

Fig. 14-2 Mare in stage II of parturition with severe abdominal contraction resulting in all limbs extended.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
During stage II, the amniotic membrane protrudes from the vulva (Fig. 14-3). The amniotic membrane should be visible at the vulvar lips within 5 to 10 minutes following rupture of the chorioallantoic membrane if the mare has not been disturbed during the delivery process. Once the amniotic membrane is visible, the fetus has entered the birth canal sufficiently to stimulate strong abdominal contractions. As the foal is pushed caudally by abdominal and uterine contractions, the feet are observed through the amniotic membrane. Rupture of the membrane does not usually occur until the fetus is at least midway or completely through the birth canal. Although most mares foal in lateral recumbency, it is possible for parturition to occur while the mare stands. The major concern in this situation is a ruptured umbilical cord close to the abdominal wall and blood loss. If the foal is delivered and the amniotic membrane remains intact as the foal struggles following delivery, the membrane should be incised and removed from the area of the fetal nose and mouth. The normal delivery posture of the fetus is one forelimb extending approximately 4 inches in front of the other and the soles of both feet directed ventrally (Fig. 14-4). This offsetting of the feet results in a slight angling of the shoulders and thereby reduces the width of this area as it passes through the mare’s pelvis. While the foal passes through the vulvar lips surrounded by the amnion, the observer can determine the offset position of the hooves and note that the soles are ventral. If the soles are not directed ventrally, immediate attention is indicated. The head should rest on the forelimbs in the area of the carpal joints. The head and neck are extended. If the nose of the fetus has not appeared by the time the carpal joints are observable immediate intervention is indicated. The vertebrae of the fetus are located near to the vertebrae of the mare; the position is close to a dorsosacral but slightly off toward the ileum. This position permits the fetus to take advantage of the greater pelvic diameter. As the fetus is expelled further, the rear limbs are extended so that the hooves are the last part of the fetus delivered. Any variation from this normal position, such as failure to observe one of the feet or the head and neck, indicates a postural abnormality and a difficult delivery. Because the mare’s delivery is so forceful, she may severely injure herself by pushing the fetus out and tearing her tissue as the fetus is expelled. Also, anything that slows the delivery process is detrimental because the placenta separates rapidly and eliminates the fetal supply of oxygen. This probably accounts for the poor survival rate of foals when the mare was in need of assistance and none was immediately available.
Stage III
The mare should be permitted to lie quietly in the stall for up to an hour following parturition; however, if she jumps up rapidly following delivery, it is not necessarily a reason to panic. Although it has been suspected, it has not been demonstrated that abdominal wall damage occurs to the fetus when this occurs. The determination of hemorrhage from the umbilicus, although not common, should be made. It was once believed that large volumes of fetal blood could be lost from the placenta and that care should be taken to assure the cord remained attached to the placenta. A more recent scientific study revealed that blood flow through the umbilical vessels ceases by the time the umbilical cord is visible at the vulvar area of the mare.10 Following delivery of the fetus and after the mare has accepted the foal and is resting, cleaning of the stall and observation of the mare and foal are the two most important managerial tasks. Stage III of parturition begins following expulsion of the foal and ends when expulsion of the placenta is complete. The fetal membranes should be expelled within 3 hours following delivery.
INDUCED PARTURITION
Parturition induction permits observation and professional assistance, if necessary, at the time of foaling. There are primarily two reasons for parturition induction. The first is for medical indications. It is of most value when used for mares that have a history of difficult deliveries or have had injuries or illnesses that could possibly endanger the life of the mare or the foal if not assisted immediately at the time of parturition. Among the clinical indications for induced parturition are ruptures of the prepubic tendon, rupture or weakening of the abdominal wall, following surgical correction of third-degree perineal lacerations or rectovaginal fistulas, previous fracture of the pelvis with narrowing of the birth canal, history of premature placental separation, prolonged gestation, near-term colic, and uterine inertia. Parturition induction also permits opening of Caslick’s vulvoplasty immediately prior to delivery and replacement immediately post partum, thereby reducing contamination of the reproductive tract. Furthermore, if an episiotomy is indicated to eliminate vulvar lacerations, it can be performed when indicated. Induced parturition in mares that have previously produced foals with neonatal isoerythrolysis can be easily managed by removal of the foal immediately following delivery.
The second reason for the induction of parturition is for convenience. Induction of parturition is becoming an acceptable method of permitting the owner, manager, or veterinarian to be present at the time of delivery in normal mares. The value of induced parturition in labor savings is brought about by the elimination of “foal watchers,” people hired to observe mares near term, or by the elimination of frequent observations throughout the night with the possibility of missing the foaling onset. The labor savings plus the guarantee that capable assistants will be present at the time of parturition easily offset the expenses incurred in parturition induction. The convenience factor also applies to certain research projects involving parturition and neonatal physiology and for the educational value of being able to provide a parturition demonstration. Induction has also been utilized to induce mares to deliver where the primary intention was to provide a nurse mare for a valuable foal. There is no association between induction and impaired future reproductive efficiency. Owners must be aware of the problems with dysmature or premature foals if delivery occurs prior to the time the foal is mature.
Some of the more general criteria to consider before induction of parturition include knowledge of the gestation length, which should exceed 320 days. The mare’s previous gestation lengths can be utilized to some extent to determine term but the effect of time of year should be considered. Mares foaling in the months of January, February, and March have longer gestations than mares foaling in April, May, and June. Prepartum changes such as perineal and cervical relaxation have been used as indicators for predicting parturition but may not be accurate enough to predict the time to induce parturition. Although relaxation of the pelvic ligaments can also be used as an indicator of approaching parturition, it is less noticeable than udder changes and more experience is necessary to detect subtle changes. Mares should be introduced into the foaling environment at least 3 to 4 weeks prior to induction if possible. This permits the mare to be exposed to the organisms in the new environment as well as become accustomed to her new surroundings. The mare should be placed in a clean stall bedded with straw in a quiet area of the barn. Rectal examination of the mare at this time usually permits evaluation of fetal presentation, position, and posture as well as viability of the fetus. Because this is an elective delivery and the time of delivery is predetermined, a tail wrap is applied to the mare and the perineal area is washed prior to administration of the induction agent.
Determination of fetal presentation, position, and posture plus a physical examination of the mare must be performed prior to induction. The fetus should be in cranial longitudinal presentation with slight dorsoileal position and the head and neck extended. Although the final delivery position and posture are determined as the mare enters stage I of parturition, the presentation will have already been predetermined. A caudal presentation would indicate the importance of assistance much earlier in the delivery process than a cranial presentation. If the head and feet are not in the proper posture, it is very probable that correction will occur before delivery without assistance. The author does not advise intervention once delivery has been induced unless it is apparent that the progress is slower than normal or is abnormal. Assistance that is too aggressive or premature may result in cervical lacerations or delay parturition.
Contraindications to parturition induction include conditions that indicate that expulsion of the fetus is not possible through a pelvic canal greatly reduced in size. Any abnormal condition affecting the mare prior to induction should be brought to the attention of the owner and a decision made as to whether to proceed. Conditions such as increased body temperature, abnormal vulvar discharges, and abnormal presentation of the fetus should influence the decision to induce because they may affect the outcome. Fetal extraction following cervical dilation without parturition induction may be indicated in certain instances to provide a better probability of fetal survival.
The most common agent used to induce parturition is oxytocin by intravenous or intramuscular administration.11 If the cervix is closed, administration of estradiol cypionate (4 to 6 mg) or diethylstilbestrol may be considered 12 to 24 hours in advance of oxytocin administration to aid in relaxation. Oxytocin also has the capability of inducing cervical relaxation in a mare with a closed or nearly closed cervix. The best results are obtained when it is administered as a 10-unit dose intravenously every 15 to 30 minutes by slow intravenous drip. Four to six repetitions of bolus administration may be required. If dilatation occurs without delivery, the dosage of oxytocin can be increased to 20 units. While determining the degree of cervical dilation, one can also determine the position and posture of the fetus by transrectal palpation because disruption of the mare has already occurred.
The dosage of oxytocin administered varies with the degree of cervical relaxation. If the internal diameter of the cervix is relaxed to at least 2 cm, it has been recommended by several authors to administer 40 to 60 units oxytocin as an intravenous bolus. Delivery of the fetus should occur within 90 minutes. In a pluriparous mare, the sequence may be more rapid, with stage II completed within 30 minutes after oxytocin administration. Many veterinarians have traditionally administered oxytocin intramuscularly.12 Much of the recent literature has reiterated the observation that the mare’s response (both in speed and violence) is proportional to the dose of oxytocin given. The higher the dose of oxytocin the faster the delivery of the fetus. Oxytocin has been reportedly used to induce parturition in six mares with all foals normal and healthy within approximately 34 minutes. None of the mares had a retained placenta and all lactated normally. The dose of oxytocin ranged from 40 to 60 units. The author prefers to administer 20 units of oxytocin intramuscularly to mares with a minimum of 2 cm cervical dilation and has not had any of the reported problems described later in this chapter.
In mares with at least 2 cm cervical dilation and other signs of preparedness for delivery, the administration of 20 units of oxytocin is followed in approximately 5 to 10 minutes with restlessness and slight colicky pains, which include tail movements and looking at the flank. Within 20 minutes, the mare will be walking, frequent defecation will be occurring, the tail will be held partially up for long periods of time, frequent urinations will occur, she may repeatedly move from the standing position to the recumbent position, and sweat will appear in the area of the shoulder. The movements will become more pronounced and the sweating will extend to other areas of the body. Rupture of the chorioallantoic membrane will occur approximately 30 minutes following oxytocin administration. Delivery of the fetus through the vulva will commence in approximately 30 to 60 minutes following administration and will take approximately 30 to 40 minutes. The fetal membranes should be passed within 3 hours or the mare should receive additional oxytocin as a treatment for the retained fetal membranes.
Reportedly, oxytocin is dangerous when used to induce parturition because it has the capability to induce delivery whether the fetus is mature or not. The response of the mare is to release larger quantities of prostaglandin than occurs during a natural parturition and is therefore a pharmacologic not a physiologic induction. Fetal membrane retention occurred as an undesirable effect in two of three mares when oxytocin was given by slow intravenous drip for longer than 3 hours. Four of five mares induced with oxytocin produced foals that were weaker than normal, and one had to be “destroyed.” Cases of malposition have been reported following induction with oxytocin. It is recommended to examine the fetus 20 minutes following oxytocin administration to determine the fetal position and to correct any malposture or malposition. The author believes that all these side effects could and do occur in natural deliveries and that some of the effects may be related to dose or route of administration.
Prostaglandin F2 alpha (PGF2α) reportedly failed to induce parturition in the mare.13 PGF2α can also cause very strong myometrial contractions and may decrease foal survival and increase fetal weakness and risk of death due to early placental separation.13,14
Fluprostenol is capable of inducing parturition in mares. Fluprostenol causes less myometrial stimulation than PGF2α and, therefore, has been successfully used for induction. Mares with a closed cervix can be induced with fluprostenol at a dose of 2.2 μg/kg. The time to delivery should be approximately 4 hours. Fluprostenol was administered to 17 ponies, horses, and donkeys to induce parturition. The prostaglandin F metabolites (PGFM) increased after injection in mares that delivered within 90 minutes following injection and peaked during the maximal expulsive efforts of parturition. If parturition required longer than 90 minutes, the PGFM increased at various times following injection and peaked before the maximal expulsive efforts.
Thirty-three mares were induced to foal with prostalene or fenprostalene based on presence of prefoaling mammary secretion. Twenty-three mares served as control subjects and were monitored but not induced. All mares given fenprostalene delivered within 3.9 hours following injection without complication. Seventy-five percent of mares receiving prostalene delivered within 3.7 hours and the remainder delivered within 30 to 56 hours following injection without difficulty. Tests were performed to determine the content of calcium carbonate or the total “hardness” of the colostral secretion. Mares were monitored beginning 10 days prior to the expected foaling date and the secretion checked daily for 3 days and then twice daily until parturition.
Combinations of fenprostalene followed by oxytocin in 5-unit doses at 20-minute intervals has been recommended as a means to reduce the approximate 4-hour time interval following the prostaglandin analogue administration until delivery. Oxytocin was administered 1 hour following the initial injection and the delivery time was more predictable.12
Glucocorticoids have reportedly failed to induce parturition in the mare. Dexamethasone, 100 mg at 24-hour intervals until parturition occurs, has been utilized but with less reliability than oxytocin. The average induction time of 4 ± 1.6 days was considered to be undesirable because qualified assistance probably would not be present when required. Because suppression of the immune response is a disadvantage of corticosteroid therapy, it is thought that the use of this substance to induce parturition may be undesirable.13 Combinations of PGF2α and flumethasone, a synthetic glucocorticoid, have been reported to successfully induce parturition.
Dystocia
Dystocia is defined as an abnormal or difficult delivery that may or may not require assistance. A dystocia may result in injury or death to the mare or the foal or both. Dystocia occurs in fewer than 1% of equine parturitions. Certain breeds or the crossbreeding of animals of extreme size difference when the mare is smaller may increase this percentage. Although mares have fewer problems with deliveries than other domestic species, when difficulties are present they are true emergencies. The reason for this is the rapid and very strenuous nature of the delivery process in this species.
Fetal causes of dystocia account for the majority of difficult deliveries. The primary reason is postural abnormalities of the long fetal extremities. Positional and presentational abnormalities can also occur but to a lesser degree. The fetus should be expelled from the uterus within 30 minutes with a maximum of 70 minutes following the rupture of the chorioallantoic membrane. Caution should be used when assisting in the extraction of a fetus to be certain the uterus, the cervix, the vagina, the vestibule, and the vulvar lips are not lacerated by traction applied too rapidly. Extraction of a fetus in an abnormal posture or position should not be attempted until the abnormality is corrected because of the increased probability of laceration. The round shape of the mare’s pelvis compared with that of the cow reduces dystocias caused by large fetuses. Other less frequently encountered fetal causes of dystocia include fetal anasarca, ascites, fetal tumor, hydrocephalic fetus, fetal monster, and mummified fetus. Maternal causes of dystocia include uterine torsion, abnormally small pelvis, uterine inertia, immaturity, constriction of the cervix or vagina, and other causes unrelated to the fetus.
The approach to a dystocia should not be hasty or heroic. A well-planned approach will be far more successful than one that overlooks major points of information critical to a successful delivery. Important aspects of this approach are a complete history and a rapid but complete physical examination. An obstetrician is often under real or perceived pressure from the owner upon arrival and may be tempted to rush the approach. The procedure will be far more successful if a reasonable time is taken for preliminary information and examination.
Notation should be made of the mare’s behavior, posture, character of her breathing, ability to rise and remain standing, response to stimulation, and degree and frequency of straining; the condition of the allantois-chorion; the presence of the amnion, visceral organs, or fetal extremities protruding from the vulva; and vulvar discharges and the appearance of the vulva. If possible prior to examination, the mare should be placed in a relatively dust-free, quiet area. The mare’s tail should be wrapped and secured to her neck with a cord.
Next, the reproductive tract and fetus should be examined. The author prefers to perform this procedure initially via transrectal palpation. This approach permits evaluation of the uterine body more anteriorly than may be possible via the vaginal canal, thus allowing assessment of the existence of uterine torsion, rupture of uterine arteries, or uterine rupture on the dorsal surface. Fetal viability can also be assessed using the transrectal approach. The perineal area is then washed and, with the use of a sleeve and sterile lubricant, the vaginal, cervical, and uterine walls are examined for possible lacerations. This procedure should always be performed before examination of the fetus to eliminate the possibility of missing a significant lesion.
Only after the determination of the absence of lacerations should the fetus be palpated through the vaginal canal to determine its presentation, position, posture, and viability. Several reflexes can be used to determine the viability of a fetus. Depression of the eyes should initiate either movement of the fetal head or, in a depressed fetus, only movement of the eye itself. A finger inserted deeply into the mouth should stimulate the sucking reflex. With a caudal presentation, a finger can be inserted into the fetal anus to detect movement of the entire fetus or simply contraction of the anal sphincter. The skin of the fetus can be pinched or a limb can be flexed or extended maximally to stimulate a response and thus indicate fetal viability. A stethoscope on ultrasonographic examination can also be performed for detection of fetal heart beat or blood flow. The relative size of the fetus and that of the pelvis and birth canal should be approximated during this examination and identification of any abnormalities of the fetus that could compromise the delivery should be made. Following the preceding examinations, the owner should be informed as to the prognosis for the mare and fetus and the cost of the recommended procedure before therapy is initiated.
All genital examinations and obstetric procedures should be performed as sanitarily as is feasible. Obstetric procedures are easiest with the mare in the standing position with epidural anesthesia unless the mare has been anesthetized and is in dorsal recumbency. Lateral recumbency is the most difficult position. Stocks are desirable to reduce side-to-side movement of the mare if one remembers that mares may suddenly go from the standing to the sternal or laterally recumbent position, making removal from stocks difficult. Anesthetized mares can be positioned with the rear quarters higher than the head on an incline or placed in dorsal recumbency with the rear feet elevated using a chain hoist (use caution following epidural). Elevation of the hindquarters permits the mare’s abdominal viscera to move away from the pelvic area. The uterus and fetus will also move cranially, permitting more space to manipulate the fetus.
Fetal presentation refers to the relationship of the spinal axis of the dam. Cranial longitudinal presentation is where the fetal head is presented first at the vulva. Caudal presentation occurs when the rear limbs or pelvis are presented first. Transverse and vertical presentations occur when the mid portion of the fetus is the first portion to contact the cervix. Position is defined as the relationship of the dorsum of the fetus to the quadrant of the maternal pelvis. The possibilities that exist in longitudinal presentation are dorsosacral, right dorsoileal, dorsopubic, and left dorsoileal. Posture refers to the relationship of the fetal extremities to the fetal trunk. A normal delivery is defined as cranial longitudinal presentation, dorsosacral position, with the fetal head, neck, and forelimbs extended.
Chemical restraint is often necessary to facilitate obstetric manipulations in the mare. Owing to their potent cardiovascular effects, sedatives (xylazine, detomidine) and tranquilizers (acepromazine) must be used with caution in compromised patients. Prior to administration of any sedative or tranquilizer drugs the cardiopulmonary status of the mare should be evaluated and doses adjusted accordingly. The potential for subsequent general anesthesia should always be considered when administering sedative/tranquilizer drugs to the equine dystocia patient.
Administering a combination of xylazine (0.66– 1.1 mg/kg IV) and acepromazine (0.04–0.06 mg/kg IV) generally provides a reasonable degree of patient cooperation and a reduction in the severity of uterine contractions. This combination should provide 20 to 40 minutes of relief and can be repeated. Butorphanol (0.01– 0.015 mg/kg IV) may be added to improve the efficacy of the preceding combination. In some cases general anesthesia may be required to facilitate fetal repositioning and removal. When available, inhalation anesthesia is always preferred for obstetric work.
Intravenous general anesthesia can be safely performed in the field setting. The practitioner should review a contemporary veterinary anesthesia text for a more thorough understanding of the procedures involved and the potential risks of equine field anesthesia. Sedation with xylazine (1.1 mg/kg IV) is followed by induction with a combination of diazepam (0.06–0.1 mg/kg IV) and ketamine (2.2 mg/kg IV). This combination should provide approximately 10 to 15 minutes of anesthesia when used alone. The duration of anesthesia can be extended with administration of “triple drip” (also called GKX), which is made by adding 1 mg/ml of ketamine and 0.5 mg/ml of xylazine to 5% guaifenesin solution. Triple drip is administered at a rate of 0.08 to 1.6 ml/kg/hour IV (or 1–2 drops/sec/450 kg). The 1 drop/sec rate will generally extend recumbency, but will often not cover significant surgical stimulation later in the procedure. The 2 drops/sec rate will generally extend complete surgical anesthesia for the duration of the procedure. An infusion rate of 3 drops/sec has been reportedly used without adverse effects. A more stable plane of anesthesia will result if triple drip administration is started immediately following anesthetic induction. If field anesthesia must be extended beyond 1 hour, the second bag of triple drip should be made using half the concentration of xylazine to minimize the accumulation of this drug. Recovery from triple drip is generally very smooth and usually takes 15 to 30 minutes following short anesthetic periods. Expect recovery time to increase as anesthetic duration is extended. α2-Adrenergic antagonists (yohimbine, tolazoline) may be used to reverse some of the xylazine sedation to shorten these longer recovery times. They should be administered in small increments (0.005 mg/kg for yohimbine and 0.5 mg/kg for tolazoline) and not until the horse has been in sternal recumbency for some time to minimize the risk of a rough recovery. It is very important to be patient when using smaller doses of reversal agents to produce a titrated response. For best results doses should be given at 3- to 5-minute intervals.
Repeated bolus administration of xylazine-ketamine can be used as an alternative to triple drip for extending the duration of equine field anesthesia. One third to one half of the initial dose of each drug is administered intravenously as a bolus when signs of a lightened plane of anesthesia are observed. Xylazine dose should be systemically reduced when numerous boluses are required. The anesthetic plane achieved using this approach is not an even plane and requires more attention than when using triple drip.15
One of the challenging aspects of treating animals in dystocia is that there are only a limited number of methods available for correction. The most difficult decision is to select the method that will achieve the objective of delivering a fetus alive with minimal trauma to the mare and the fetus. The second most important aspect of successful management of dystocia is to have access to the mare early in the delivery process. The possibilities for dystocia correction include mutation, forced extraction, fetotomy, laparotomy, and laparohysterotomy. Although euthanasia of the mare may be selected to terminate the case because of economics or the physical condition of the mare at the time of arrival, it is not included as a treatment for dystocia as it does not fulfill the definition of mare and foal survivability.
The amount of assistance necessary depends on the technique to be employed for correction. The minimal amount of assistance recommended for an obstetric procedure is two persons. One person is at the head of the mare for the entire procedure and one assists the obstetrician with equipment and with traction or fetotomy cuts when required. Generally three or four assistants make the procedure go more rapidly.
Obstetric equipment recommended by the author includes three obstetric chains (60 inch), three obstetric chain handles, fetatome (Utrecht or flat tube model), a Krey-Schottler hook, a wire introducer, two wire handles, a detorsion rod, a fetotomy finger knife, a rope snare, obstetric wire, a Kühn crutch, rubber sleeves, buckets, a stomach pump, a nasogastric tube, and lubricant. The lubricant of choice is polyethylene polymer (J-Lube*), ispolyethylene polymera which comes in powder form and is water soluble. It can be mixed at the site and delivered into the uterus with a stomach pump and tube. Although not all of this equipment is essential for every dystocia, its availability will improve the quality of the obstetric manipulation and reduce the work required to obtain desirable results.
Mutation
The most frequently used method of correction is mutation. Mutation is the procedure used to correct malposture, position, and presentation followed by delivery of the entire fetus. This method should be the least traumatic and should be employed prior to the use of forced extraction. Mutation may not always be possible or indicated, depending on the length of time the mare has been in labor, viability of the fetus, and the cause of the dystocia.
Mutation involves returning the fetus to a normal presentation, position, and posture by repulsion, rotation, version, and adjustment or extension of the fetal extremities. It is primarily indicated when the fetus is alive and the procedure can be performed in a relatively short period with a high probability of success. It has been found by the author that in the case of a dead fetus, fetotomy procedures to eliminate a postural abnormality are faster and less stressful to the mare and the obstetrician than attempts to mutate unless the dystocia has been of minimal duration and sufficient area exists within the uterus to permit manipulation. Repulsion of the fetus into the abdominal cavity away from the pelvis aids in creating more space in which to perform obstetric procedures. Lubrication is very important with all obstetric procedures, including mutation, and may make the difference between success and failure of the technique. Extension of a flexed limb is accomplished by repelling the proximal portion while the midportion of the limb (carpus or tarsus) is rotated laterally (Fig. 14-5). Following this, the foot is brought medially and extended into the pelvis. If correction is not possible in 15 to 20 minutes, another method of correction should be selected.
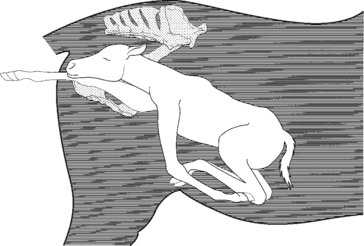
Fig. 14-5 Anterior presentation, dorsosacral position, with the head and right forelimb extended and left shoulder flexed.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
Lateral deviation of the head is a common cause of dystocia because of the relatively long neck of the fetus (Fig. 14-6). The fetus should never be delivered with this postural abnormality because of the potential for injury to the birth canal. The operator’s fingers can be inserted into the fetal mouth and traction applied to bring the head toward the brim of the pelvis. Much of the success of this technique depends on the amount of space within the pelvic area. In cases of prolonged labor, there may be no available space for the extension of the neck. The limb on the side opposite the deviation of the neck may need to be placed into carpal or shoulder flexion to permit sufficient space for extension of the head. Attachment of a rope snare to the fetlock area of this limb facilitates postural correction following extension of the neck. A repulsion rod can be used to repel the fetus by placing it in the area of the sternum and pushing gently. The muzzle can be brought into the pelvis by pushing the poll of the head to the opposite side of the pelvis while applying traction to the mouth or muzzle (Fig. 14-7). A rope snare can also be used to facilitate this technique. As traction is applied to the rope snare, the hand is used to guide the neck and head into the pelvic canal. A rope snare placed on the mandible can be used as a method of postural correction but should never be used as a point of traction because the mandible fractures easily and the incisors can be removed in such attempts. If the fetus is alive, anesthetizing the mare and placing her in dorsal recumbencywith the rear end elevated early in the correction process may be beneficial. If the fetus is dead, an immediate fetotomy may be the preferred method of correction.
Fig. 14-6 Left lateral deviation of head and neck with extended forelimbs and fetus in anterior longitudinal presentation with dorsosacral position (lateral view).
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
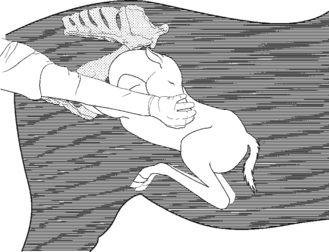
Fig. 14-7 Correction of head and neck lateral deviation by hand alone. Hand is placed around muzzle or fingers are placed in lateral commissure of mouth and a pulling pressure is applied.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
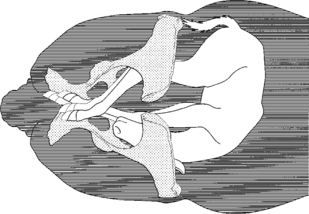
Cranial longitudinal presentation, dorsosacral position with head, neck, and forelimbs extended and with bilateral hip flexion can be diagnosed following failure of delivery of a fetus that appears to be in proper presentation, position, and posture (Fig. 14-8). Determination is made on vaginal examination that the fetal rear hooves are located in the mare’s pelvis near the elbows of the fetus. The first step in correcting this abnormal posture is to repel the rear hooves over the brim of the pelvis and into the abdominal cavity. This may not be possible owing to forced extraction applied before an accurate diagnosis was made or to the time elapsed waiting for delivery of the fetus in what appeared to be a normal presentation, position, and posture. A dead fetus may have to be transected in the lumbar area and, if possible, repelled or the pelvis bisected and removed. If the fetus is alive, it may be impossible to deliver a viable offspring even if the mare’s rear quarters are elevated or by cesarean section.
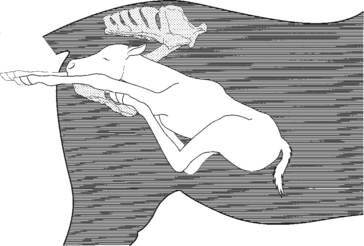
Fig. 14-8 Anterior presentation, dorsosacral position with head, front limbs, and rear limbs extended.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
Correction of carpal flexion (Fig. 14-9) by mutation in live fetuses is best accomplished by grasping the limb in the area of the metacarpus with the hand positioned so the thumb and fingers completely encircle the limb. The proximal portion of the limb is then repelled into the uterus. The limb is rotated with the carpus pushed laterally and the hoof moved medially under the neck of the fetus and then pulled cranially with respect to the fetus. Once the hoof can be brought into the pelvis, the limb is extended. If this technique is not possible with the hand alone, a rope snare can be attached to the wire introducer and placed around the flexed carpus and formed into a loop. The loop is moved distally on the limb until the snare is distal to the fetlock if possible. The rope is tightened and traction is applied as the proximal portion of the limb is repelled. The disadvantage of this technique is the loss of control of the direction of the hoof as it clears the brim of the pelvis. However, it is an acceptable and beneficial technique that has application in some dystocias with a live fetus.
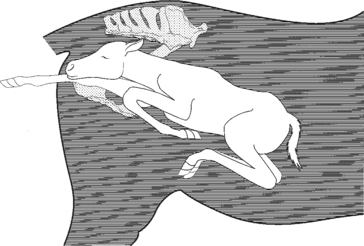
Fig. 14-9 Anterior presentation, left carpal flexion posture. The shoulder is converted to a carpal and elbow flexion.
(From Threlfall WR: Threlfall’s equine obstetrics. Powell, OH: Global Reproductive Services, 1996.)
Dorsoilial and dorsopubic positions should be corrected before delivery of the fetus to ensure minimal trauma to the birth canal during extraction. Although other methods to rotate the fetus have been described, such as the hand alone to push or pull the fetus in the desired direction, these techniques require more physical work and are not as successful as the use of a detorsion rod. Although techniques have been described using chains without a detorsion rod for correction, there is a higher probability of injury to the vagina of the mare and the limbs of the fetus with this technique.
After determining the viability of a fetus in transverse presentation (Fig. 14-10), the method of correction should be employed immediately. If the fetus is alive, the best possible choices would be to do a cesarean section or attempt to elevate the rear quarters of the mare to provide additional space for manipulation. If possible, an attempt should be made to deliver the fetus in caudal presentation; the reason for this is to eliminate the need to direct the fetal head, and this may make the delivery more rapid. If the fetus is dead, transection of the fetus should be attempted if sufficient space is available. A major problem associated with a transverse presentation is that affected mares have usually been in labor for a much longer period of time than believed by the owner, since there may be no cervical pressure to induce the more visible expulsive efforts of stage II labor.
Forced Extraction
Forced extraction is generally combined with mutation or fetotomy. Forced extraction is not intended to replace other techniques but to aid in the delivery process. If used unwisely, forced extraction results in injury to the fetus or the mare’s reproductive tract or both. Extractive force is used with uterine inertia, following corrective mutation, with inadequate cervical dilation, in caudal presentations and in combination with fetotomy. Extremetraction should never be applied in lieu of corrective mutation, a fetotomy or cesarean section because of the possibility of trauma to the mare or fetus. The position and posture of the foal should be as near to normal as possible before traction is applied. Traction placed on the fetus should be slightly dorsal and caudal until the forelimbs, head, and neck are at the vulvar lips. The direction of the traction is then directed more ventrally as more of the fetus is visible. Traction should be directed mostly ventral by the time the shoulders have passed through the vulvar lips.
When the operator is experienced and uses good judgment, forced extraction is relatively safe. It can cause various injuries, however, including damage to the head, limbs, and spinal cord of the fetus; damage to the uterus and cervix and adjacent structures; eversion of the uterus; and lacerations of the vagina, vulva, perineal body, and rectal floor. Aftercare following forced extraction may include uterine stimulants placed into the uterus or administered systemically. The use of antibiotics may be indicated to reduce the number of organisms that were introduced during the procedure. Broad-spectrum antibiotics are generally recommended for this purpose.
If it becomes apparent that forced extraction is not going to be successful, another technique for correction should be attempted. A common mistake made by obstetricians is to continue using a technique beyond a reasonable time in anticipation that eventually it will be successful. Determining the time to abandon one technique for another is gained through experience and is always a challenge.
Fetotomy
Fetotomy is indicated in many instances because the manipulative time and trauma to the mare can be reduced over that of mutation and forced extraction if the fetus is dead.16 Fetotomy is a reduction in fetal size by removal of the extremities or dissection of the body. Specific indications include the presence of a dead fetus in the absence of excessive uterine contracture; a fetus that is not overly emphysematous; abnormalities in fetal presentation, position, or posture; the presence of an oversized fetus in relationship to the maternal birth canal; the presence of fetal abnormalities such as ankylosis of joints; and incomplete cervical dilatation. The decision to perform a fetotomy also depends on the veterinarian’s opinion that there is sufficient space in the dam’s genital tract to perform the procedure and on the experience of the obstetrician. The advantages of a fetotomy include reduction of fetal size, elimination of need for a cesarean section, minimal assistance necessary, decreased trauma to the mare, less infertility than following cesarean section, less aftercare than with cesarean section, shorter recovery time than with cesarean section, greater practicality as a “field” technique than a cesarean section and greater monetary economy to both the owner and the veterinarian. A cesarean section is the preferred approach by many veterinarians over that of fetotomy in cases of a live or dead fetus that cannot be removed by mutation and forced extraction. Reasons given for not using fetotomy include overstretching of the cervix; more physical exertion by the veterinarian; lacerations of the uterus, cervix, vagina, and of the operator; and the procedure being “too hard on the mare.” A cesarean section, however, cannot generally be performed under farm situations where no technical assistance or facilities are available, whereas fetotomies can be performed under these conditions. Supposedly to reduce severe injury to the genital tract, it has not been recommended to perform fetotomies that require more than one or two cuts.17 However, the duration of the fetotomy, the damage to the reproductive tract prior to the initiation of the fetotomy, and the correctness of the cuts have a major influence on the success of the procedure. The other consideration on the farm is what other options are available that will save the life of the mare. Also, most equine dystocias are caused by simple postural anomalies, so only one or two cuts are necessary to permit delivery of the remainder of the fetus following fetotomy in most instances. Also, fetotomy procedures are generally less costly to the owner since aftercare is considerably less and future reproductive capability is better than following a nonelective cesarean section.
One of the primary determining factors in most but not all fetotomies is the quality and type of instrumentation available to the obstetrician and familiarity of the obstetrician with the procedures. Some veterinarians consider fetotomy as the last resort, and such thinking may result in failure. If performed properly, fetotomy requires less aftercare than a cesarean section and there is less probability of systemic infection, parametritis, perimetritis; higher reproductive capability; reduction in laminitis; and a shorter time to rebreeding.
Indications for total fetotomy should be recognized early so that cesarean section can be considered before a large amount of effort and time is expended on fetotomy. When performing a complete fetotomy on a fetus in cranial presentation, the following sequential cuts with some variations are recommended: amputation of the head; amputation of a forelimb; amputation of the opposite forelimb; transverse section through the third thoracic vertebra and removal of the remaining neck and the thorax cranial to the cut; transverse cut through approximately the third lumbar vertebra and longitudinal transection of the thorax; and finally a longitudinal cut through the pelvis. A partial fetotomy with one or more cuts, evisceration, and lubrication may enable simple mutation or forced extraction and delivery of the remainder of the fetus.
Dismembering a fetus in cranial presentation may be indicated for various reasons. Amputating a protruding fetal head in dystocias in which the forelimbs are retained provides more space for repositioning or removing the limbs. Owing to the rapid normal delivery of the fetus in the mare, partial placental separation and death of the fetus frequently occur by the time the obstetrician arrives at the dystocia. This situation plus the available assistance and surroundings may make fetotomy the only method possible to correct the dystocia and save the mare. An extended head is separated through the atlanto-occipital junction with the fetatome head resting against the caudal border of the ramus of the mandible. To do this, a loop of wire that has been threaded through the fetatome is placed around the fetal head and behind the ears in the area of the axis. After proper lubrication, it may be possible to deliver the remainder of the fetus by traction following head removal. The remaining portion of the fetus is within reach; it cannot drop further into the uterus because of pressure against the fetus. It is imperative that following placement of the obstetric wire, the position of the wire be checked one last time before any attempts to dissect the fetus are made. The hand of the obstetrician always covers the head of the fetatome during the amputation procedure. The person doing the sawing must fully understand that he or she is to start only when instructed to do so and to stop immediately when instructed to do so.
Probably the most common indication for amputating the fetal head and neck is lateral deviation. The forelimbs may have to be repelled if possible to provide more space in the birth canal for this fetotomy procedure. If the limbs cannot be repelled with little effort, the limb opposite the direction of the head deviation or opposite to the limb in flexure should be removed to provide additional working area for removal of the head. Neck amputation involves inserting the wire introducer with the obstetric wire attached around the fetal neck and then withdrawing it from the birth canal. The wire is threaded through the fetatome and the head of the fetatome is held tightly against the fetal neck at its greatest curvature. Following this cut, the head and attached portion of the neck of the fetus can be removed with the use of a Krey-Schottler hook.
Another common cause of dystocia in cranial presentation is a flexed forelimb. The limb is usually flexed at the shoulder and extends beneath the fetal body. A wire introducer with wire attached is passed dorsally over the shoulder and between the fetal trunk and the limb. The wire is then grasped ventrally and pulled outside of the genital tract. The fetatome is inserted into the uterus so that the head is approximately 5 cm dorsal and medial to the scapula’s spinous process. After the limb has been severed, it is removed. Following amputation of the limb, the area of the scapular attachment is examined for remnants of cartilage or bone fragments. If these are found, they can be removed with the fingers alone using blunt dissection or with the aid of the finger knife. The fetus can be removed if the flexed limb was the only cause for the dystocia, the opposite limb can be removed in the same manner, and the remaining cervical vertebral bodies used to secure the Krey-Schottler hook. In this instance the single point of traction is sufficient for delivery. If there exists a flexed carpal or, in the case of caudal presentation, tarsal joint, a cut distal to the joint may alleviate the dystocia with a dead fetus and save the mare further discomfort and injury that may occur with attempts to mutate the limb. The limb is amputated by placing obstetric wire around the limb with the wire introducer. The wire is then threaded through the fetatome and the cut is made distal to the joint. This permits the attachment of an obstetric chain to the remaining stump in order for this limb to be used as a point of traction.
A complete fetotomy performed in caudal presentation includes the following cuts: The first may involve either of the rear limbs depending on access. The second cut removes the opposite hind limb. The third cut removes the caudal aspect of the fetus including the remaining pelvis and the majority of the lumbar vertebra. The next cut is made through the area of thoracic vertebra immediately caudal to the scapula. Then the forelimbs can be removed one at a time. The neck and head with the remaining thorax could be removed together or separately. Other modified cuts may be necessary in cases such as hydrocephalus, when the head must be sectioned prior to removal, or in instances in which limbs may need to be sectioned, such as with a tarsal flexion, before delivery is possible.
With a true breech presentation only the tail is in the birth canal and may be observed protruding from the vulva. Both hind limbs are flexed and retained beneath the fetal body. A wire introducer is inserted dorsally over one hind limb between the trunk and the limb, and a hand is slipped under the limb to grasp the wire introducer ventrally and pull the end of the obstetric wire from the birth canal so that it can be threaded through the fetatome. The head of the fetatome is placed adjacent to the tailhead and a flexed hind limb is removed with a cut approximately through the coxofemoral joint. The amputated limb can then be removed. It usually is more rapid and less exhausting for the surgeon to remove the opposite retained limb in a similar manner rather than trying to mutate it. A Krey-Schottler hook can be inserted into the fetal pelvis to serve as a point of traction and deliver the remainder of the fetus after adequate lubrication.
In the case of an extended rear limb amputation, following placement of an obstetric chain on the rear limb with a loop above and another loop below the fetlock, the fetatome threaded with a loop of wire is placed as was described for removal of an extended forelimb. The loop of wire is fixed adjacent to the third phalanx alongside the chain. The head of the fetatome is moved slowly proximally toward the body of the fetus lateral to the limb until the head is 5 cm dorsal and cranial to the tuber coxae and is fixed in this position by attaching the chain to the fetatome. The wire is then moved alongside the medial surface of the limb while maintaining tension on the wire to prevent kinking or twisting. Immediately prior to dissection, the wire is checked to be certain of its placement. If indicated, the opposite rear limb can be removed in a similar manner. Once the limb or limbs have been removed, the fetal abdominal cavity should be incised and the abdominal contents removed to reduce the size of the abdomen. Removal of one or both rear limbs is a fairly common fetotomy procedure employed to permit the removal of an equine fetus due to abnormal posture of the rear limbs. If it is determined that the remainder of the fetus is still too large for forced extraction, a cut can be made through the area of the second lumbar vertebra to remove the pelvic portion of the fetus. If this problem was foreseen prior to removal of the second rear limb, the pelvis could be cut diagonally, thus allowing removal of the remaining rear limb and a portion of the pelvis with one cut. Fetotomy aftercare generally includes the administration of systemic uterine stimulants such as oxytocin and the infusion of antibiotics or antiseptics into the uterus.
Laparotomy is indicated primarily in those cases involving uterine torsion in which other methods of correction via the vagina were unsuccessful. The torsion may be evident months prior to the onset of labor as determined by prolonged colic-like signs that fail to respond to therapy for gastrointestinal pain. The diagnosis can be easily made by transrectal palpation of the uterus and broad ligaments. The finding of one broad ligament traversing the midline to the opposite side dorsal to the uterus with the other broad ligament nonpalpable is sufficient information to make the diagnosis. The correction of the uterine torsion via laparotomy can be achieved by one of several abdominal approaches with the mare standing or recumbent. The author prefers the standing flank approach on the side of torsion origin. For example, a counterclockwise torsion would be approached from the right flank. The author prefers this approach because the uterine horn can be pulled or pushed into normal position.
Laparohysterotomy
Laparohysterotomy is another option for the alleviation of dystocia. Cesarean section refers to delivery of a fetus through incisions in the abdominal wall and uterus of the dam. Cesarean section has its best advantage following repositioning of a uterine torsion or when preplanned and the time and facilities are immediately available to permit delivery of the fetus while alive. Indications for cesarean section include a previously fractured pelvis or other obstruction that reduces pelvic diameter; a small pelvis; an extremely large fetus; abdominal wall or prepubic tendon ruptures; uterine torsion that is not correctable by a vaginal approach or by rolling the mare; malpresentations that are not correctable by other methods; emphysematous fetuses; fetal anomalies; and a live fetus that cannot be delivered by any other way. One complication of cesarean section is rupture of the uterine artery during manipulation. The biggest problems encountered in regard to a cesarean section are mare and foal survival and future reproductive performance of the mare. An elective cesarean section gives the best prognosis for both.
The considerations involved in selecting a site for a cesarean section include the operative conditions and disposition of the animal. The surgeon’s previous experience with operative sites is another major consideration. The possible operative sites include right and left flank with the animal standing using sedation and local anesthesia. This approach, however, is seldom recommended owing to reduced exposure of the uterus, visible abdominal wall scarring, and possible movement of the mare during surgery. The flank approaches under general anesthesia are also options, but the reduced uterine exposure and visible scar following surgery are disadvantages. The primary advantage of the left flank over the right is that the cecum is less of a problem and thus does not obstruct access to the uterus. However, intestines may make the left flank approach difficult. Possible operative sites in a recumbent animal include low approaches through either flank, the paramedian area, or the abdominal midline. The ventral midline incision is most commonly used and has the advantage of providing excellent exposure of the uterus. There is very little hemorrhage when this site is used. There may be one or two large veins in this area that form an anastomosis from the right to left subcutaneous abdominal veins. These veins, if present, should be ligated prior to making the incision in the subcutaneous tissue.
After the fetus is removed through the incision, the placenta is removed if it is free within the uterine cavity. If the placenta is still adhered to the endometrium, it is left in the uterus and an antibiotic solution or boluses are placed into the lumen before closure. If hemorrhage occurs from the subendometrial veins, the veins are ligated independently or a ligature is placed in the area of the hemorrhage, including endometrium, subendometrium, and myometrium. Simple continuous, continuous interlocking, or similar suture patterns can also be used to control hemorrhage. A Cushing suture pattern can be used to infold the incision site. The suture should be placed so that very little if any suture material is apparent on the serosal surface following closure. This will reduce the adhesions that form between the uterine wall and abdominal viscera. The care of mares following a cesarean section should be provided on an individual basis because it is not feasible to treat all animals the same way and achieve good results. Repeated administration of oxytocin is advisable to enhance uterine involution.
Following the correction of dystocia by any method, the uterus should be examined to ensure that another fetus is not present. The tone of the uterine musculature should also be assessed. The birth canal should be palpated for evidence of lacerations.
1 Dorland’s illustrated medical dictionary, 22nd ed. WB Saunders, Philadelphia, 1957.
2 Holtan D, Houghton E, Silver M, et al. Plasma progesterone in the mare, fetus and newborn foal. J Reprod Fertil. 1991;44(Suppl.):517-528.
3 Haluska GJ, Currie WB. Variation in plasma concentrations of estradiol-17beta and their relationship to those of progesterone, 13,14-dihydro-15-ketoprostaglandin F2alpha and oxytocin across pregnancy and at parturition in pony mares. J Reprod Fertil. 1988;84:635-646.
4 Haluska GJ, Wilkins K. Predictive utility of prepartum temperature change in the mare. Equine Vet J. 1989;21:116-118.
5 Shaw E, Houpt K, Holmes D. Body temperature and behaviour of mares during the last weeks of pregnancy. Equine Vet J. 1988;20:199-202.
6 Ammons S, Threlfall W, Kline R. Equine body temperature and progesterone fluctuations during estrus and near parturition. Theriogenology. 1989;31:1007-1019.
7 Cross D, Threlfall W, Kline R. Telemetric monitoring of body temperature in the horse mare. Theriogenology. 1991;36:855-861.
8 Haluska G, Lowe J, Currie W. Electromyographic properties of the myometrium of the pony mare. J Reprod Fertil. 1987;81:471-478.
9 Haluska G, Lowe J, Currie W. Electromyographic properties of the myometrium correlated with the endocrinology of the prepartum and the postpartum periods and parturition in pony mares. J Reprod Fertil. 1987;35(Suppl.):553-564.
10 Doarn R, Threlfall W, Kline R. Umbilical blood flow and the effects of premature severance in the neonatal horse. Theriogenology. 1987;28:789-800.
11 Pashen RL. Oxytocin: The induction agent of choice in the mare? J Reprod Fertil. 1982;32(Suppl.):645.
12 Leadon D, Rossdale P, Jeffcott L, et al. A comparison of agents for inducing parturition in mares in the pre-viable and premature periods of gestation. J Reprod Fertil. 1982;32(Suppl.):597-602.
13 Alm C, Sullivan J, First N. The effect of a corticosteroid (dexamethasone), progesterone, oestrogen and prostaglandin F2 alpha on gestation length in normal and ovariectomized mares. J Reprod Fertil. 1975;23(Suppl.):637-640.
14 Townsend H, Tabel H, Bristol F. Induction of parturition in mares: effect on passive transfer of immunity to foals. J Am Vet Med Assoc. 1983;182:255-257.
15 Abrahamsen E, The Ohio State University: Personal communication, 2003.
16 Bierschwal CJ, deBois CHW. The technique of fetotomy in large animals. Bonner Springs: VM Publishing, 1972.
17 Blanchard T, Bierschwal C, Youngquist R, et al. Sequelae to percutaneous fetotomy in the mare. J Am Vet Med Assoc. 1983;182:1127.