22 SUSPECTED COPD
Chronic obstructive pulmonary disease (COPD): Disease characterised by the presence of airflow obstruction due to either chronic bronchitis or emphysema.
 Chronic bronchitis is defined clinically: A chronic productive cough on most days of the week for three months of the year in each of two successive years in a patient in whom other causes of chronic cough have been excluded.
Chronic bronchitis is defined clinically: A chronic productive cough on most days of the week for three months of the year in each of two successive years in a patient in whom other causes of chronic cough have been excluded. Emphysema is defined anatomically: Abnormal permanent enlargement of air spaces distal to the terminal bronchioles, accompanied by destruction of the alveolar walls but without obvious fibrosis.
Emphysema is defined anatomically: Abnormal permanent enlargement of air spaces distal to the terminal bronchioles, accompanied by destruction of the alveolar walls but without obvious fibrosis.
Table 22.1 Avoid terminological confusions1–3.
| Term | Includes/represents | Notes |
|---|---|---|
| Obstructive pulmonary disorders | Diseases that are characterised by a reduction in expiratory airflow | |
| COPD | ||
| Compensatory emphysema | Airspace dilatation (i.e. increased inflation) in response to loss of volume elsewhere in the lung |
CXR FINDINGS IN COPD
GENERAL
 COPD is usually suspected clinically. The diagnosis is confirmed by spirometry demonstrating airflow obstruction that is not fully reversible. The CXR has a limited role in diagnosis but can be useful:
COPD is usually suspected clinically. The diagnosis is confirmed by spirometry demonstrating airflow obstruction that is not fully reversible. The CXR has a limited role in diagnosis but can be useful:
 Even with extensive pathological changes (COPD) or severe clinical symptoms the CXR may appear normal—particularly if the dominant disease process is chronic bronchitis.
Even with extensive pathological changes (COPD) or severe clinical symptoms the CXR may appear normal—particularly if the dominant disease process is chronic bronchitis. Caution (1): large volume lungs are not necessarily indicative of over-inflation2. They can occur in:
Caution (1): large volume lungs are not necessarily indicative of over-inflation2. They can occur in:
 Caution (2): be careful about making a diagnosis of COPD on the CXR alone without supporting clinical evidence.
Caution (2): be careful about making a diagnosis of COPD on the CXR alone without supporting clinical evidence.CHRONIC BRONCHITIS
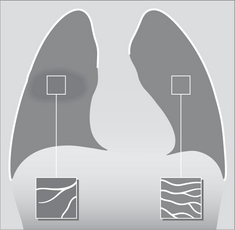
 The diagnosis of chronic bronchitis is made clinically on the basis of well-defined and internationally accepted features. The CXR appearance may be normal or there may be abnormalities which are very subtle or non-specific (Table 22.2).
The diagnosis of chronic bronchitis is made clinically on the basis of well-defined and internationally accepted features. The CXR appearance may be normal or there may be abnormalities which are very subtle or non-specific (Table 22.2). The principle role of the CXR is in helping to exclude diseases that can clinically mimic chronic bronchitis2. These include tuberculosis, carcinoma, bronchiectasis and lung abscess.
The principle role of the CXR is in helping to exclude diseases that can clinically mimic chronic bronchitis2. These include tuberculosis, carcinoma, bronchiectasis and lung abscess.
Table 22.2 CXR features in chronic bronchitis.
| Symptoms | CXR |
|---|---|
| Mild to moderate | Normal |
| Severe |
EMPHYSEMA
 A low diaphragm does not of itself indicate emphysema. Over-inflation of the lungs due to emphysema should only be assumed when a dome of the diaphragm is both low and flat (Fig. 22.5).
A low diaphragm does not of itself indicate emphysema. Over-inflation of the lungs due to emphysema should only be assumed when a dome of the diaphragm is both low and flat (Fig. 22.5).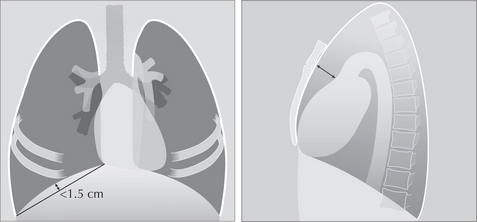
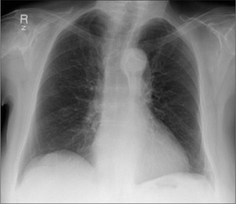
Figure 22.5 Over-inflated lungs. Low domes of the diaphragm are not necessarily abnormal. It should only be assumed to indicate COPD if the domes are both low and flat. On a PA CXR a flat dome is one in which its highest point is less than 1.5 cm above a line connecting the costophrenic and cardiophrenic angles2. On a lateral CXR a flat dome is one in which the diaphragmatic peak is less than 1.5 cm above a line joining the sternophrenic and posterior costophrenic angles2. Note the enlarged retrosternal air space—on the lateral CXR—a regular finding in COPD when over-inflation is present.
Table 22.3 CXR features in emphysema.
| Disease severity | CXR2–9 |
|---|---|
| Mild to moderate | |
| Severe |
 A low, flat dome of the diaphragm is very suggestive A low, flat dome of the diaphragm is very suggestive
 Flat: highest level of a dome is less than 1.5 cm above a line drawn between the costophrenic and the cardiophrenic sulci (Fig. 22.5) Flat: highest level of a dome is less than 1.5 cm above a line drawn between the costophrenic and the cardiophrenic sulci (Fig. 22.5) |
Vascular changes
Widespread emphysema may show the following abnormal appearances:
 A narrow, vertical, centrally situated heart. The explanation: over-inflation of the lungs causes the diaphragm to be low. Because the pericardium and the superior surface of the diaphragm are adherent, the heart is pulled inferiorly by the over-inflation. Consequently its transverse diameter appears narrow.
A narrow, vertical, centrally situated heart. The explanation: over-inflation of the lungs causes the diaphragm to be low. Because the pericardium and the superior surface of the diaphragm are adherent, the heart is pulled inferiorly by the over-inflation. Consequently its transverse diameter appears narrow. The hilar vessels are prominent10. This is because there is less cardiac shadow overlap, or because the vessel margins at the hilum are sharply defined by the hypertransradiant over-distended adjacent air spaces, or because the pulmonary arteries are actually enlarged due to secondary pulmonary arterial hypertension.
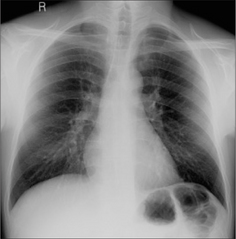
The hilar vessels are prominent10. This is because there is less cardiac shadow overlap, or because the vessel margins at the hilum are sharply defined by the hypertransradiant over-distended adjacent air spaces, or because the pulmonary arteries are actually enlarged due to secondary pulmonary arterial hypertension. The vessels extending outwards into the lungs appear thinner or have a smaller diameter than is usual. This peripheral narrowing is in marked contrast to the very prominent hilar vessels. There may also be fewer vessels in affected areas (Fig. 22.6).
The vessels extending outwards into the lungs appear thinner or have a smaller diameter than is usual. This peripheral narrowing is in marked contrast to the very prominent hilar vessels. There may also be fewer vessels in affected areas (Fig. 22.6).Bullae
Saber sheath trachea (UK: sabre sheath trachea)
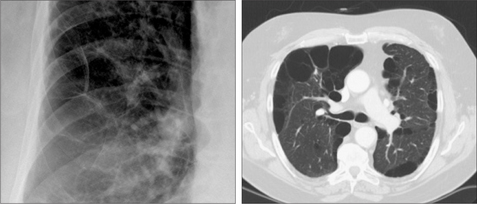
When a saber sheath appearance is present it is a reliable and sensitive sign of COPD. A saber sheath configuration is evident when the intrathoracic coronal diameter of the trachea is two-thirds of the saggital diameter or less, when measured 1 cm above the superior aspect of the aortic arch4. The precise mechanism causing this tracheal appearance remains speculative. This sign may appear in chronic bronchitis or emphysema (Figs 22.9 and 22.10).

Figure 22.9 Saber sheath trachea in COPD. The narrowing is limited to the intrathoracic part of the trachea. A saber sheath appearance exists when the coronal diameter of the trachea is two thirds of the sagittal diameter or less…measured 1 cm above the aortic arch4. Precise assessment requires a lateral as well as a PA CXR. Nevertheless, the tracheal narrowing is usually evident on the frontal CXR.
KNOWN COPD: INDICATIONS FOR A CXR
A CXR is only occasionally necessary during an acute exacerbation (Table 22.4).
Table 22.4 Indications for a CXR.
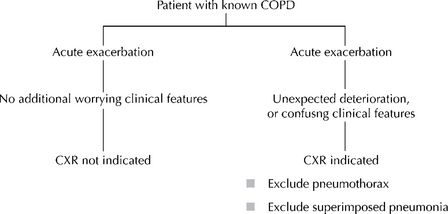 |
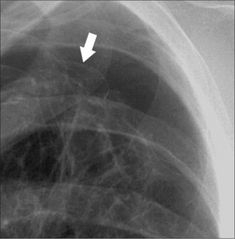
Figure 22.11 COPD. Unexpected clinical deterioration. A pneumo-thorax is present. The visceral pleura (arrow) is visible.

Figure 22.12 COPD. Acute exacerbation with confusing clinical features. The CXR reveals an extensive pneumonia in the left mid zone. (NB: this is the same patient as shown in Fig. 22.2)
 The differential diagnosis in a patient with clinical symptoms suggesting COPD will include asthma, bronchiectasis, cystic fibrosis, left heart failure, interstitial lung disease, and upper airway obstruction.
The differential diagnosis in a patient with clinical symptoms suggesting COPD will include asthma, bronchiectasis, cystic fibrosis, left heart failure, interstitial lung disease, and upper airway obstruction. Chronic bronchitis. The pathological changes: mucous gland enlargement, inflammation, and bronchial wall thickening. Airflow limitation results from the deformity of the bronchial walls and narrowing of the lumina.
Chronic bronchitis. The pathological changes: mucous gland enlargement, inflammation, and bronchial wall thickening. Airflow limitation results from the deformity of the bronchial walls and narrowing of the lumina. Recognised causes of emphysema are: cigarette smoking, alpha 1-antitrypsin deficiency, intravenous drug abuse (cocaine, heroin, methadone), immune deficiency syndromes (including HIV infection).
Recognised causes of emphysema are: cigarette smoking, alpha 1-antitrypsin deficiency, intravenous drug abuse (cocaine, heroin, methadone), immune deficiency syndromes (including HIV infection). Emphysema. Autopsy studies have shown that emphysema can involve as much as 30% of the lung tissue, and yet an individual may not have had any respiratory symptoms during life5.
Emphysema. Autopsy studies have shown that emphysema can involve as much as 30% of the lung tissue, and yet an individual may not have had any respiratory symptoms during life5.1. American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;152:77-121.
2. Takasugi JE, Godwin JD. Radiology of chronic obstructive pulmonary disease. Radiol Clin North Am. 1998;36:29-55.
3. Devereux G. ABC of chronic obstructive pulmonary disease. Definition, epidemiology, and risk factors. BMJ. 2006;332:1142-1144.
4. Greene R. “Saber-sheath” trachea: relation to chronic obstructive pulmonary disease. AJR. 1978;130:441-445.
5. Pratt PC. Role of conventional chest radiography in diagnosis and exclusion of emphysema. Am J Med. 1987;82:998-1006.
6. Thurlbeck WM, Muller NL. Emphysema: definition, imaging and quantification. AJR. 1994;163:1017-1025.
7. Collins J, Stern EJ. Chest Radiology: The Essentials. Philadelphia, PA: Lippincott Williams & Wilkins, 1999;200-201.
8. Foster WL, Gimenez EI, Robidoux MA, et al. The emphysemas: radiologic–pathologic correlations. Radiographics. 1993;13:311-328.
9. Klein JS, Gamsu G, Webb WR, et al. High-resolution CT diagnosis of emphysema in symptomatic patients with normal chest radiographs and isolated low diffusing capacity. Radiology. 1992;182:817-821.
10. Simon G. Principles of Chest X-ray Diagnosis, 2nd ed. London: Butterworths, 1962.