Chapter 161 Vasculitis Syndromes
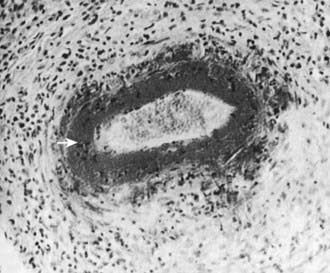
Childhood vasculitis encompasses a broad spectrum of diseases that share a common denominator, inflammation of the blood vessels. The pathogenesis of the vasculitides is generally idiopathic; some forms of vasculitis are associated with infectious agents and medications, and others may occur in the setting of preexisting autoimmune disease. The pattern of vessel injury provides insight into the form of vasculitis and serves as a framework to delineate the different vasculitic syndromes. The distribution of vascular injury includes small vessels (capillaries, arterioles, and postcapillary venules), medium vessels (renal arteries, mesenteric vasculature, and coronary arteries), and large vessels (the aorta and its proximal branches). Additionally, some forms of small vessel vasculitis are characterized by the presence of antineutrophil cytoplasmic antibodies (ANCAs), whereas others are associated with immune complex deposition in affected tissues. A combination of clinical features, histologic appearance of involved vessels, and laboratory data is utilized to classify vasculitis (Tables 161-1 to 161-3).
Table 161-1 CLASSIFICATION OF CHILDHOOD VASCULITIS
I. PREDOMINANTLY LARGE VESSEL VASCULITIS
II. PREDOMINANTLY MEDIUM VESSEL VASCULITIS
III. PREDOMINANTLY SMALL VESSEL VASCULITIS
IV. OTHER VASCULITIDES
* Associated with antineutrophil cytoplasmic antibody.
Adapted from Ozen S, Ruperto N, Dillon MJ, et al: EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides, Ann Rheum Dis 65:936–941, 2006.
Table 161-2 FEATURES THAT SUGGEST A VASCULITIC SYNDROME
CLINICAL FEATURES
LABORATORY FEATURES
From Cassidy JT, Petty RE: Textbook of pediatric rheumatology, ed 5, Philadelphia, 2005, Elsevier/Saunders.
Childhood vasculitis varies from a relatively benign and self-limited disease such as Henoch-Schönlein purpura to catastrophic disease with end-organ damage as seen in Wegener granulomatosis. Vasculitis generally manifests as a heterogeneous multisystem disease. Although some features, such as purpura, are easily identifiable, others, such as hypertension secondary to renal artery occlusion or glomerulonephritis, can be more subtle. Ultimately, the key to recognizing vasculitis relies heavily on pattern recognition. Demonstration of vessel injury and inflammation on biopsy or vascular imaging is required to confirm a diagnosis of vasculitis.
Bibliography
Dedeoglu F, Sundel RP: Vasculitis in children, Rheum Dis Clin North Am 33:555–583, 2007.
Jennette JC, Falk RJ, Andrassy K, et al: Nomenclature of systemic vasculitides: proposal of an international consensus conference, Arthritis Rheum 37:187–192, 1994.
Jones RB, Tervaert JWC, Hauser T, et al: Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis, N Engl J Med 363(3):211–226, 2010.
Ozen S, Ruperto N, Dillon MJ, et al: EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides, Ann Rheum Dis 65:936–941, 2006.
Wahezi DM, Gomes WA, Howite NT: Cranial nerve involvement with juvenile polyarteritis nodosa: clinical manifestations and treatment, Pediatrics 126(3):e719–e722, 2010.
161.1 Henoch-Schönlein Purpura
Henoch-Schönlein purpura (HSP) is the most common vasculitis of childhood and is characterized by leukocytoclastic vasculitis and immunoglobulin (Ig) A deposition in the small vessels in the skin, joints, gastrointestinal tract, and kidney.
Epidemiology
HSP occurs worldwide and affects all ethnic groups. The incidence of HSP is estimated at 14-20/100,000 children per year and affects males more than females, with a 1.2-1.8 : 1 male: female ratio. Approximately 90% of HSP cases occur in children, usually between the ages of 3 and 10 yr. HSP is distinctly less common in adults, in whom severe and chronic complications are often encountered. HSP is more common in the fall, winter, or spring and is unusual in summer months. Many cases of HSP follow a documented upper respiratory infection.
Pathology
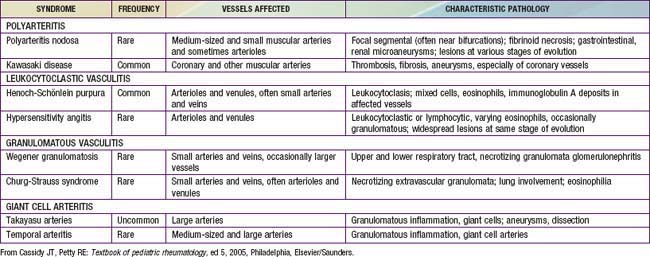
Skin biopsies demonstrate vasculitis of the dermal capillaries and postcapillary venules. The inflammatory infiltrate includes neutrophils and monocytes. Renal histopathology typically shows endocapillary proliferative glomerulonephritis, ranging from a focal segmental process to extensive crescentic involvement. In all tissues, immunofluorescence identifies IgA deposition in walls of small vessels (see Fig. 161-1), accompanied to a lesser extent by deposition of C3, fibrin, and IgM.
Pathogenesis
The exact pathogenesis of HSP remains unknown. Given the frequency of preceding upper respiratory infections, including group A streptococcal infections, an infectious trigger is suspected. The common finding of deposition of IgA, specifically IgA1, suggests that HSP is a disease mediated by IgA and IgA immune complexes. HSP occasionally clusters in families, suggesting a genetic component. HLA-B34 and HLA-DRB1*01 alleles have been linked to HSP nephritis.
Clinical Manifestations
The hallmark of HSP is its rash: palpable purpura starting as pink macules or wheals and developing into petechiae, raised purpura, or larger ecchymoses. Occasionally, bullae and ulcerations develop. The skin lesions are usually symmetric and occur in gravity-dependent areas (lower extremities) or on pressure points (buttocks) (Figs. 161-1 and 161-2). The skin lesions often evolve in groups, typically lasting 3-10 days, and may recur up to 4 mo after initial presentation. Subcutaneous edema localized to the dorsa of hands and feet, periorbital area, lips, scrotum, or scalp is also common.
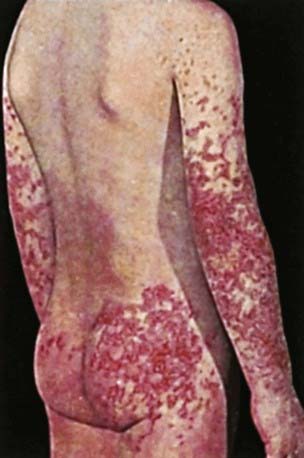
Figure 161-2 Henoch-Schönlein purpura.
(From Korting GW: Hautkrankheiten bei Kindern und Jungendlichen, ed 3, Stuttgart, 1982, FK Schattaur Verlag.)
Musculoskeletal involvement, including arthritis and arthralgias, is common, occurring in up to 75% of children with HSP. The arthritis tends to be self-limited and oligoarticular, with a predilection for the lower extremities, and does not lead to deformities. The arthritis usually resolves within 2 wk but can recur.
Gastrointestinal manifestations of HSP occur in up to 80% of children with HSP. They include abdominal pain, vomiting, diarrhea, paralytic ileus, melena, intussusception, and mesenteric ischemia or perforation. Endoscopic evaluation is usually not needed but may identify purpura of the intestinal tract.
Renal involvement occurs in up to 50% of children with HSP, manifesting as hematuria, proteinuria, hypertension, frank nephritis, nephrotic syndrome, and acute or chronic renal failure. Progression to end-stage renal disease is uncommon in children (1-2%) (see Chapter 509 for more detailed discussion of HSP renal disease).
Neurologic manifestations of HSP, due to hypertension or central nervous system (CNS) vasculitis, may also occur. They include intracerebral hemorrhage, seizures, headaches, and behavior changes. Other less common potential manifestations of HSP are orchitis, carditis, inflammatory eye disease, testicular torsion, and pulmonary hemorrhage.
Diagnosis
The diagnosis of HSP is a clinical one and is often straightforward when the typical rash is present. However, in at least 25% of cases, the rash appears after other manifestations, making early diagnosis challenging. Classification criteria for HSP are summarized in Table 161-4. The differential diagnosis for HSP depends on specific organ involvement but usually includes other small vessel vasculitides, infections, coagulopathies, and other acute intra-abdominal processes.
Table 161-4 CLASSIFICATION CRITERIA FOR HENOCH-SCHÖNLEIN PURPURA*
AMERICAN COLLEGE OF RHEUMATOLOGY CLASSIFICATION CRITERIA†
EUROPEAN LEAGUE AGAINST RHEUMATISM/PEDIATRIC RHEUMATOLOGY EUROPEAN SOCIETY CRITERIA‡
* Classification criteria are developed for use in research and not validated for clinical diagnosis.
† Developed for use in adult and pediatric populations. Adapted from Mills JA, Michel BA, Bloch DA, et al: The American College of Rheumatology 1990 criteria for classification of Henoch-Schonlein purpura, Arthritis Rheum 33:1114–1121, 1990.
‡ Developed for use in pediatric populations only.
Adapted from Ozen S, Ruperto N, Dillon MJ et al: EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides, Ann Rheum Dis 65:936–941, 2006.
Acute hemorrhagic edema (AHE), an isolated cutaneous leukocytoclastic vasculitis that affects infants <2 yr of age, resembles HSP clinically. AHE manifests as fever; tender edema of the face, scrotum, hands, and feet; and ecchymosis (usually larger than the purpura of HSP) on the face and extremities (Fig. 161-3). The trunk is spared, but petechiae may be seen in mucous membranes. The patient usually appears well except for the rash. The platelet count is normal or elevated, and the urinalysis results are normal. The younger age, the nature of the lesions, absence of other organ involvement, and a biopsy may help distinguish AHE from HSP.
Laboratory Findings
No laboratory finding is diagnostic of HSP. Common but nonspecific findings include leukocytosis, thrombocytosis, mild anemia, and elevations of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Occult blood is frequently found in stool specimens. Autoantibody testing is not useful diagnostically except to exclude other diseases. Serum IgA values are often elevated but are not routinely measured. Assessment of renal involvement with blood pressure, urinalysis, and serum creatinine is necessary.
Ultrasound is often used in the setting of gastrointestinal complaints to look for bowel wall edema or the rare occurrence of an associated intussusception. Barium enema can also be used to both diagnose and treat intussusception. Although often unnecessary in typical HSP, biopsies of skin and kidney can provide important diagnostic information, particularly in atypical or severe cases, and characteristically show IgA deposition in affected tissues.
Treatment
Treatment of HSP is supportive, with an emphasis on assuring adequate hydration, nutrition, and analgesia. Controversy continues concerning the appropriate use of glucocorticoids in the management of HSP, but steroids are most often used to treat significant gastrointestinal involvement or other life-threatening manifestations. Empiric use of prednisone (1 mg/kg/day for 1 to 2 wk, followed by taper) reduces abdominal and joint pain but does not alter overall prognosis nor prevent renal disease. Although few data are available to demonstrate efficacy, intravenous immune globulin and plasma exchange are sometimes used in the setting of severe disease. In some cases, chronic HSP renal disease is managed with a variety of immunosuppressants, including azathioprine, cyclophosphamide, and mycophenolate mofetil. End-stage renal disease develops in up to 8% of children with HSP nephritis.
Complications
Acutely, serious gastrointestinal involvement such as intestinal perforation imparts significant morbidity and mortality. Renal disease is the major long-term complication, occurring in 1-2% of children with HSP. Renal disease can develop up to 6 mo after diagnosis but rarely does so if the initial urinalyses findings are normal. It is recommended that children with HSP undergo serial monitoring of blood pressure and urinalyses for 6 mo after diagnosis, especially those who presented with hypertension or urinary abnormalities.
Prognosis
Overall, the prognosis for childhood HSP is excellent, and most children experience an acute, self-limited course. About 30% of children with HSP experience one or more recurrences, typically within 4-6 mo of diagnosis. With each relapse, symptoms are usually milder than at presentation. Children with a more severe initial course are at higher risk for relapse. Chronic renal disease develops in 1-2% of children with HSP, and approximately 8% of those with HSP nephritis go on to have end-stage renal disease.
Coppo R, Mazzucco G, Cagnoli L, et al. Long term prognosis of Henoch-Schonlein nephritis in adult and children. Italian Group of Renal Collaborative Study on Henoch-Schonlein purpura. Nephrol Dial Transplant. 1997;12:2277-2283.
Davin JC, Weening JJ. Henoch-Schönlein purpura nephritis: an update. Eur J Pediatr. 2001;160:689-695.
Donnithorne KJ, Atkinson P, Hinze CH, et al. Rituximab therapy for severe refractory chronic Henoch-Schönlein purpura. J Pediatr. 2009;155:136-139.
Hoffman GS. Therapeutic interventions for systemic vasculitis. JAMA. 2010;304(21):2413-2414.
Jauhola O, Ronkainen J, Koskimies O, et al. Clinical course of extrarenal symptoms in Henoch-Schönlein purpura: a 6-month prospective study. Arch Dis Child. 2010;95:871-876.
Jauhola O, Ronkainen J, Koskimies O, et al. Renal manifestations of Henoch-Schönlein purpura in a 6-month prospective study of 223 children. Arch Dis Child. 2010;95:877-882.
Mir S, Yavascan O, Mutlubas F, et al. Clinical outcome in children with Henoch-Schönlein nephritis. Pediatr Nephrol. 2007;22:64-70.
Peru H, Soylemezoglu O, Bakkaloglu SA, et al. Henoch Schönlein purpura in childhood: clinical analysis of 254 cases over a 3-year period. Clin Rheumatol. 2008;27:1087-1092.
Ronkainen J, Koskimies O, Ala-Houhala M, et al. Early prednisone therapy in Henoch-Schonlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247.
Tizard EJ, Hamilton-Ayres MJJ. Henoch-Schönlein purpura. Arch Dis Child Educ Pract Ed. 2008;93:1-8.
Weiss PF, Feinstein JA, Luan X, et al. Effects of corticosteroid on Henoch-Schönlein purpura: a systematic review. Pediatrics. 2007;120:1079-1087.
Weiss PF, Klink AJ, Hexem K, et al. Variation in inpatient therapy and diagnostic evaluation of children with Henoch-Schönlein purpura. J Pediatr. 2009;155:812-818.
161.2 Takayasu Arteritis
Takayasu arteritis (TA), also known as “pulseless disease,” is a chronic large vessel vasculitis of unknown etiology that predominantly involves the aorta and its major branches.
Epidemiology
Although TA occurs worldwide and can affect all ethnic groups, the disease is most common in Asians. Age of onset is typically between 10 and 40 yr. Up to 20% of individuals with TA are diagnosed prior to age 19 yr. Younger children may be affected but diagnosis in infancy is rare. TA preferentially affects females with a reported 2-4 : 1 female : male ratio in children and adolescents and a 9 : 1 ratio among adults. Occlusive complications are more common in the USA, Western Europe, and Japan, whereas aneurysms predominate in Southeast Asia and Africa.
Pathology
TA is characterized by inflammation of the vessel wall, starting in the vas vasorum. Involved vessels are infiltrated by T cells, natural killer cells, plasma cells, and macrophages. Giant cells and granulomatous inflammation develop in the media. Persistent inflammation damages the elastic lamina and muscular media, leading to blood vessel dilation and the formation of aneurysms. Progressive scarring and intimal proliferation can result in stenotic or occluded vessels. The subclavian, renal, and carotid arteries are the most commonly involved aortic branches; pulmonary, coronary, and vertebral arteries may also be affected.
Pathogenesis
The etiology of TA remains unknown. The presence of abundant T cells with a restricted repertoire of T-cell receptors in TA vascular lesions points to the importance of cellular immunity and suggests the existence of a specific but unknown aortic tissue antigen. Expression of interleukin-1 (IL)-1, IL-6, and tumor necrosis factor-α (TNF-α) is reported to be higher in patients with active TA than in patients with inactive TA and in healthy controls. In addition, some individuals with TA have elevated serum values of anti-endothelial antibodies. A link between TA and tuberculosis infection has been proposed but not proven. The increased prevalence of TA in certain ethnic populations and its occasional occurrence in monozygotic twins and families suggest a genetic predisposition to the disease.
Clinical Manifestations
The diagnosis of TA is challenging, because early disease manifestations are often nonspecific. As a result, diagnosis can be delayed for several months, and the time to diagnosis is usually longer in children than in adults. Fever, malaise, weight loss, headache, hypertension, myalgias, arthralgias, dizziness, and abdominal pain are common early complaints in the “pre-pulseless” phase of the disease. Among children, hypertension and headache are particularly common presenting manifestations and should prompt consideration of TA when present without alternative explanation. Some individuals with TA report no systemic symptoms and instead present with vascular complications. It is only after substantial vascular injury that evidence of hypoperfusion becomes clinically evident. Later manifestations of disease include diminished pulses, asymmetric blood pressures, claudication, Raynaud phenomenon, renal failure, and symptoms of pulmonary or cardiac ischemia. Inflammation can extend to the aortic valve, resulting in valvular insufficiency. Other findings may include pericardial effusion, pericarditis, pleuritis, splenomegaly, and arthritis.
Diagnosis
Specific pediatric criteria for TA have been proposed, as summarized in Tables 161-5 and 161-6. Radiographic demonstration of large vessel vasculitis is necessary. A thorough physical examination is required to detect an aortic murmur, diminished or asymmetric pulses, and vascular bruits. Four extremity blood pressures should be measured >10 mm Hg; asymmetry in systolic pressure is indicative of disease.
Table 161-5 PROPOSED CLASSIFICATION CRITERIA FOR PEDIATRIC-ONSET TAKAYASU ARTERITIS
Angiographic abnormalities (conventional, CT, or magnetic resonance angiography) of the aorta or its main branches and at least one of the following criteria:
Adapted from Ozen S, Ruperton N, Dillon MJ, et al: EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides, Ann Rheum Dis 65:936–941, 2006.
Table 161-6 PATTERNS OF ARTERIAL INVOLVEMENT IN TAKAYASU ARTERITIS
| TYPE | INVOLVED ARTERIES |
|---|---|
| I | |
| II | |
| III | Diffuse aortic involvement |
| IV | Diffuse aortic and pulmonary artery involvement |
Adapted from Hata A, Noda M, Moriwaki R, et al: Angiographic findings of Takayasu arteritis: new classification, Int J Cardiol 54(Suppl):S155–S163, 1996.
Differential Diagnosis
In the early phase of TA, when nonspecific symptoms predominate, the differential diagnosis includes a wide array of systemic infections, autoimmune conditions, and malignancies. Although giant cell arteritis, also known as “temporal arteritis,” is a common large vessel vasculitis in older adults, this entity is exceedingly rare in childhood. Non-inflammatory conditions that can cause large vessel compromise include fibromuscular dysplasia, Marfan syndrome, and Ehlers-Danlos syndrome.
Laboratory Findings
The laboratory findings in TA are nonspecific, and there is no specific diagnostic laboratory test. ESR and CRP value are typically elevated, and other nonspecific markers of chronic inflammation may include leukocytosis, thrombocytosis, anemia of chronic inflammation, and hypergammaglobulinemia. Autoantibodies are not useful in diagnosing TA except to help exclude other autoimmune diseases.
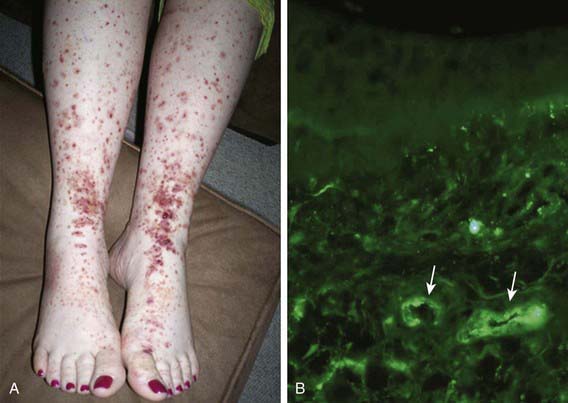
Radiographic assessment is essential to establish large vessel arterial involvement. The gold standard remains conventional arteriography of the aorta and major branches, including carotid, subclavian, pulmonary, renal, and mesenteric branches. Conventional arteriography can identify luminal defects, including dilation, aneurysms, and stenoses, even in smaller vessels such as the mesenteric arteries. Figure 161-4 shows a conventional arteriogram in a child with TA. Although not yet thoroughly validated in TA, magnetic resonance angiography (MRA) and CT angiography (CTA) are gaining acceptance and provide important information about vessel wall thickness and enhancement, although they may not image smaller vessels as well as conventional angiography. Positron emission tomography (PET) may detect vessel wall inflammation but has not been studied extensively. Ultrasound with duplex color-flow Doppler imaging also identifies vessel wall thickening and assesses arterial flow. Echocardiography is recommended to assess for aortic valvular involvement. Serial vascular imaging is usually necessary to assess response to treatment and to detect progressive vascular damage.
Treatment
Owing to the rarity of the disease, there is limited evidence to guide therapy. Glucocorticoids are the mainstay of therapy, typically starting with high doses (1 to 2 mg/kg/day of prednisone) followed by gradual dosage tapering. When TA progresses or recurs, steroid-sparing therapy is often required, usually involving methotrexate or azathioprine. Cyclophosphamide is reserved for severe or refractory disease. Results of small case series also suggest that mycophenolate mofetil and anti–TNF-α therapy may be beneficial in select patients. Antihypertensive medications are often necessary to control blood pressure due to renovascular disease.
Complications
Progressive vascular damage can result in arterial stenoses, aneurysms, and occlusions, which produce ischemic symptoms and can be organ- or life-threatening. Potential ischemic complications include stroke, renal impairment or failure, myocardial infarction, mesenteric ischemia, and limb-threatening arterial disease. When these complications occur or are imminent, intervention with surgical vascular grafting or catheter-based angioplasty and stent placement may be necessary to restore adequate blood flow. A high rate of recurrent stenosis has been reported following angioplasty and stent placement. Aortic valve replacement may be required if significant aortic insufficiency develops.
Prognosis
Although up to 20% of individuals with TA have a monophasic course and achieve sustained remission, most suffer relapses. Survival for individuals with TA has improved considerably over the decades, although higher mortality rates are reported in children and adolescents. The overall estimated survival for individuals with TA is 93% at 5 yr and 87% at 10 yr. However, morbidity from vascular complications remains high. Given the chronic endothelial insult and inflammation, children and adolescents with TA are probably at high risk for accelerated atherosclerosis. Early detection and treatment are critical to optimizing outcome in TA.
Cakar N, Yalcinkaya F, Duzova A, et al. Takayasu arteritis in children. J Rheumatol. 2008;35:913-919.
Filocamo G, Buoncompagni A, Viola S, et al. Treatment of Takayasu’s arteritis with tumor necrosis factor antagonists. J Pediatr. 2008;153:432-434.
Kalangos A, Christenson JT, Cikirikcioglu M, et al. Long-term outcome after surgical intervention and interventional procedures for the management of Takayasu’s arteritis in children. J Thorac Cardiovasc Surg. 2006;132:656-664.
Maksimowicz-McKinnon K, Clark TM, Hoffman GS. Limitations of therapy and a guarded prognosis in an American cohort of Takayasu arteritis patients. Arthritis Rheum. 2007;56:1000-1009.
Ozen S, Duzova A, Bakkaloglu A, et al. Takayasu arteritis in children: preliminary experience with cyclophosphamide induction and corticosteroids followed by methotrexate. J Pediatr. 2007;150:72-76.
Park MC, Lee SW, Park YB, et al. Clinical characteristics and outcomes of Takayasu’s arteritis: analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol. 2005;34:284-292.
Park MC, Lee SW, Park YB, et al. Serum cytokine profiles and their correlations with disease activity in Takayasu’s arteritis. Rheumatology. 2006;45:545-548. (Oxford)
161.3 Polyarteritis Nodosa and Cutaneous Polyarteritis Nodosa
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis affecting small and medium-sized arteries. Aneurysms and stenoses form at irregular intervals throughout affected arteries. Cutaneous PAN is limited to the skin.
Epidemiology
PAN is rare in childhood. Boys and girls are equally affected, and the mean age at presentation is 9 yr. The cause is unknown, but the development of PAN following infections, including group A streptococcus and chronic hepatitis B, suggests that PAN represents a postinfectious autoimmune response. Infections with other organisms, including Epstein-Barr virus, Mycobacterium tuberculosis, cytomegalovirus, parvovirus B19, and hepatitis C virus, have also been associated with PAN.
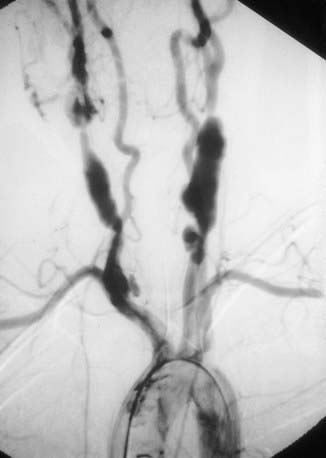
Pathology
Biopsies show necrotizing vasculitis with granulocytes and monocytes infiltrating the walls of small and medium-sized arteries (Fig. 161-5). Involvement is usually segmental and tends to occur at vessel bifurcations. Granulomatous inflammation is not present, and deposition of complement and immune complexes is rarely observed. Different stages of inflammation are found, ranging from mild inflammatory changes to panmural fibrinoid necrosis associated with aneurysm formation, thrombosis, and vascular occlusion.
Pathogenesis
Immune complexes are believed to be pathogenic, but the mechanism is poorly understood. There is no clear genetic association with PAN, and it is not known why PAN has a predilection for small- and medium-size blood vessels. The inflamed vessel wall becomes thickened and narrowed, impeding blood flow and contributing to end-organ damage characteristic of this disease.
Clinical Manifestations
The clinical presentation of PAN is variable but generally reflects the distribution of inflamed vessels. Constitutional symptoms are present in most children at disease onset. Weight loss and severe abdominal pain suggest mesenteric arterial inflammation and ischemia. Renovascular arteritis can cause hypertension, hematuria, or proteinuria, although glomerular involvement is not typical. Cutaneous manifestations include purpura, livedo reticularis, ulcerations, and painful nodules. Arteritis affecting the nervous system results in cerebrovascular accidents, transient ischemic attacks, psychosis, and ischemic peripheral neuropathy (mononeuritis multiplex). Myocarditis or coronary arteritis can lead to heart failure and myocardial ischemia; pericarditis and arrhythmias have also been reported. Arthralgias, arthritis, or myalgias are frequently present. Less common symptoms include testicular pain that mimics testicular torsion, bone pain, and vision loss due to retinal arteritis.
Diagnosis
The diagnosis of PAN requires demonstration of vessel involvement on biopsy or angiography. Biopsy of cutaneous lesions shows small or medium vessel vasculitis (see Fig. 161-5). Kidney biopsy in patients with renal manifestations may show necrotizing arteritis. Electromyography in children with peripheral neuropathy identifies affected nerves, and sural nerve biopsy may reveal vasculitis. Conventional arteriography is the gold standard diagnostic imaging study for PAN and reveals areas of aneurysmal dilatation and segmental stenosis, the classic “beads on a string” appearance (Fig. 161-6). MRA and CTA, less invasive imaging alternatives, are gaining acceptance but may not be as effective in identifying small vessel disease or in younger children.
Differential Diagnosis
Early skin lesions may resemble those of HSP, although the finding of nodular lesions and presence of systemic features help distinguish PAN. Pulmonary lesions suggest ANCA-associated vasculitis or Goodpasture disease. Other rheumatic diseases, including systemic lupus erythematosus, have characteristic target organ involvement and associated autoantibodies distinguishing them from PAN. Prolonged fever and weight loss should also prompt consideration of inflammatory bowel disease or malignancy.
Laboratory Findings
Nonspecific laboratory findings include elevations of ESR and CRP, anemia, leukocytosis, and hypergammaglobulinemia. Abnormal urine sediment, proteinuria, and hematuria indicate renal disease. Laboratory findings may be normal in cutaneous PAN or similar to those of systemic PAN. Elevated hepatic enzyme values may suggest hepatitis B or C infection. Serologic tests for hepatitis (hepatitis B surface antigen and hepatitis C antibody) should be performed in all patients.
Treatment
Oral (1-2 mg/kg/day) and intravenous pulse (30 mg/kg/day) corticosteroids are typically used, frequently in combination with oral or intravenous cyclophosphamide. If hepatitis B is identified, appropriate antiviral therapy should be initiated (Chapter 350). Most cases of cutaneous PAN can be treated with corticosteroids alone at doses of 1-2 mg/kg/day. If an infectious trigger for PAN is identified, antibiotic prophylaxis should be considered. Efficacy data are limited for the treatment of relapsing or refractory cutaneous disease, but dapsone, methotrexate, azathioprine, thalidomide, cyclosporine, and anti-TNF agents have been used successfully.
Complications
Cutaneous nodules may ulcerate and become infected. Hypertension and chronic renal disease may develop from renovascular involvement in PAN. Cardiac involvement may lead to decreased cardiac function or coronary artery disease. Mesenteric vasculitis can predispose to bowel infarction, rupture, and malabsorption. Stroke and rupture of hepatic arterial aneurysm are uncommon complications of this disorder.
Prognosis
The course of PAN varies from mild disease with few complications to a severe, multiorgan disease with high morbidity and mortality. Early and aggressive immunosuppressive therapy increases the likelihood of clinical remission. Compared with disease in adults, childhood PAN is associated with less mortality. Cutaneous PAN is unlikely to transition to systemic disease. Early recognition and treatment of the disease are important to minimizing potential long-term vascular complications.
Dedeoglu F, Sundel RP. Vasculitis in children. Rheum Dis Clin North Am. 2007;33:555-583.
Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic vasculitides: proposal of an international consensus conference. Arthritis Rheum. 1994;37:187-192.
Naumann-Bartsch N, Stachel D, Morhart P, et al. Childhood polyarteritis nodosa in autoimmune lymphoproliferative syndrome. Pediatrics. 2010;125:e169-e173.
Ozen S, Anton J, Arisoy N, et al. Juvenile polyarteritis: results of a multicenter survey of 110 children. J Pediatr. 2004;145:517-522.
Ozen S, Ruperto N, Dillon MJ, et al. EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Ann Rheum Dis. 2006;65:936-941.
Yalcinkaya F, Ozcakar B, Kasapcoupur O, et al. Prevalence of the MEFV gene mutations in childhood polyarteritis nodosa. J Pediatr. 2007;151:675-678.
161.4 ANCA-Associated Vasculitis
The ANCA-associated vasculitides are characterized by small vessel involvement, circulating antineutrophil cytoplasmic antibodies (ANCA), and pauci-immune complex deposition in affected tissues. ANCA-associated vasculitis is categorized into three distinct forms: Wegener granulomatosis (WG), microscopic polyangiitis (MPA), and Churg-Strauss syndrome (CSS).
Epidemiology
WG is a necrotizing granulomatous small vessel vasculitis that occurs at all ages and targets the respiratory tract and the kidneys. Although most cases of WG occur in adults, it does develop in children, with a mean age at diagnosis of 14 yr. There is a female predominance of 3-4 : 1, and pediatric WG is most prevalent in white persons.
MPA is a small vessel necrotizing vasculitis with clinical features similar to those of WG. CSS is a small vessel necrotizing granulomatous vasculitis associated with a history of refractory asthma and peripheral eosinophilia. MPA and CSS are rare in children, and there does not appear to be a gender predilection in either disease.
Pathology
Necrotizing vasculitis is the cardinal histologic feature in WG and MPA. Kidney biopsies typically demonstrate crescentic glomerulonephritis with little or no immune complex deposition (“pauci-immune”), in contrast to biopsies from patients with SLE. Although granulomatous inflammation is common in WG and CSS, it is typically not present in MPA. Biopsies showing perivascular eosinophilic infiltrates distinguish CSS syndrome from both MPA and WG (Table 161-7).
Pathogenesis
The etiology of ANCA-associated vasculitis remains unknown, although neutrophils, monocytes, and endothelial cells are involved in disease pathogenesis. Neutrophils and monocytes are activated by ANCAs, specifically by the ANCA-associated antigens proteinase-3 (PR3) and myeloperoxidase (MPO), and release proinflammatory cytokines such as TNF-α and IL-8. Localization of these inflammatory cells to the endothelium results in vascular damage characteristic of the ANCA vasculitides. Why the respiratory tract and kidneys are preferential targets in WG and MPA is unknown. Infectious agents and genetic factors have been implicated in disease susceptibility.
Clinical Manifestations
Early disease course is characterized by nonspecific constitutional symptoms, including fever, malaise, weight loss, myalgias, and arthralgias. In WG, upper airway involvement can manifest as sinusitis, nasal ulceration, epistaxis, otitis media, and hearing loss. Lower respiratory tract symptoms include cough, wheezing, dyspnea, and hemoptysis. Pulmonary hemorrhage can cause rapid respiratory failure. Compared with WG in adults, childhood WG is more frequently complicated by subglottic stenosis (see Fig. 161-5). Inflammation-induced damage to the nasal cartilage can produce a saddle nose deformity (Fig. 161-7). Ophthalmic involvement includes conjunctivitis, scleritis, uveitis, optic neuritis, and invasive orbital pseudotumor (causing proptosis). Perineural vasculitis or direct compression on nerves by granulomatous lesions can cause cranial and peripheral neuropathies. Hematuria, proteinuria, and hypertension signal renal disease. Cutaneous lesions include palpable purpura and ulcers. Venous thromboembolism is a rare but potentially fatal complication of WG. The frequencies of organ system involvement throughout the disease course in WG are: respiratory tract, 84%; kidneys, 88%; joints, 44%; eyes, 60%; skin, 48%; sinuses, 56%; and nervous system, 12%.
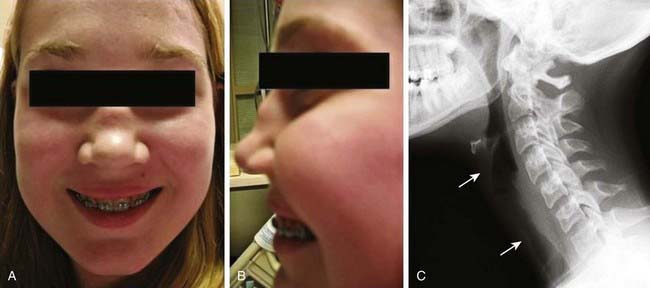
Figure 161-7 A and B, Anterior and lateral views of saddle nose deformity in an adolescent girl with Wegener granulomatosis. C, Segment of subglottic posterior tracheal irregularity (between arrows) on lateral neck radiograph in the same patient.
The clinical presentation of MPA closely resembles that of WG, although sinus disease is less common. Like WG, CSS frequently causes inflammation of the upper and lower respiratory tract, but cartilage destruction is rare. Unlike in WG, renal involvement in CSS is uncommon, and CSS tends to involve nerves, gastrointestinal tract, pericardium, and skin.
Diagnosis
WG should be considered in children who have recalcitrant sinusitis, pulmonary infiltrates, and evidence of nephritis. Chest radiography often fails to detect pulmonary lesions, and chest CT may show nodules, ground-glass opacities, mediastinal lymphadenopathy, and cavitary lesions (Fig. 161-8). The diagnosis is confirmed by the presence of anti–proteinase 3 (anti-PR3)–specific ANCAs (PR3-ANCAs) and the finding of necrotizing granulomatous vasculitis on pulmonary, sinus, or renal biopsy. The ANCA test result is positive in approximately 90% of children with WG, and the presence of anti-PR3 increases the specificity of the test.

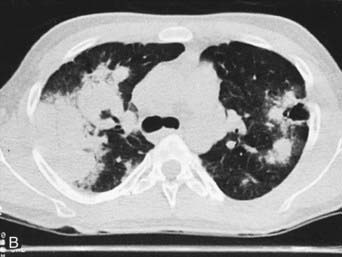
Figure 161-8 Radiographs of lower respiratory tract disease in Wegener granulomatosis. A, A chest radiograph of a 14 yr old girl with Wegener granulomatosis and pulmonary hemorrhage. Extensive bilateral, fluffy infiltrates are visualized. B, CT scan of the chest in a 17 yr old boy with Wegener granulomatosis. Air space consolidation, septal thickening, and a single cavitary lesion are present.
(From Kuhn JP, Slovis TL, Haller JO: Caffey’s pediatric diagnostic imaging, ed 10, vol 1, Philadelphia, 2004, Mosby.)
(From Cassidy JT, Petty RE: Granulomatous vasculitis, giant cell arteritis and sarcoidosis. In Textbook of pediatric rheumatology, ed 3, Philadelphia, 1995, WB Saunders.)
In MPA, ANCAs are also frequently present but have reactivity to myeloperoxidase (MPO-ANCAs). MPA can be distinguished from polyarteritis nodosa (PAN) by the presence of ANCAs and the tendency for small vessel involvement. The ANCA test result is positive in approximately 70% of cases of CSS, and MPO-ANCAs are more common than PR3-ANCAs. The presence of chronic asthma and peripheral eosinophilia suggests the diagnosis of CSS.
Differential Diagnosis
ANCAs are absent in other granulomatous diseases, such as sarcoidosis and tuberculosis. Goodpasture disease is characterized by antibodies to glomerular basement membrane. Medications such as propylthiouracil, hydralazine, and minocycline are associated with drug-induced ANCA vasculitis. Systemic lupus erythematosus can manifest as pulmonary hemorrhage and nephritis.
Laboratory Findings
Elevated ESR and CRP values, leukocytosis, and thrombocytosis are present in most patients with an ANCA-associated vasculitis but are nonspecific. Anemia may be due to chronic inflammation or pulmonary hemorrhage. ANCA antibodies show two distinct immunofluorescence patterns: perinuclear (p-ANCAs) and cytoplasmic (c-ANCAs). In addition, ANCAs can also be defined by their specificity for PR3 or MPO antigen. As summarized in Table 161-4, WG is strongly associated with c-ANCAs/anti-PR3 antibodies.
Treatment
When the lower respiratory tract or kidneys are significantly involved, initial therapy usually consists of corticosteroids (2 mg/kg/day oral or 30 mg/kg/day × 3 days given intravenously) in conjunction with daily oral cyclophosphamide (2 mg/kg/day). Patients are transitioned to a less toxic medication (usually methotrexate or azathioprine) within 3 to 6 mo once remission is achieved. Trimethoprim-sulfamethoxazole (one 180 mg/800 mg tablet 3 days/wk) is often prescribed both for prophylaxis against Pneumocystis carinii infection and to reduce upper respiratory bacterial colonization with Staphylococcus aureus, which may trigger disease activity. If disease is limited to the upper respiratory tract, corticosteroids (1-2 mg/kg/day) and methotrexate (0.5-1.0 mg/kg/wk) may be first-line treatment.
Complications
Upper respiratory tract lesions can invade the orbit and threaten the optic nerve, and lesions in the ear can cause permanent hearing loss. Respiratory complications include potentially life-threatening pulmonary hemorrhage and upper airway obstruction due to subglottic stenosis. Chronic lung disease secondary to granulomatous inflammation, cavitary lesions, and scarring can predispose to infectious complications. Chronic glomerulonephritis may progress to end-stage renal disease in a subset of patients with advanced or undertreated disease.
Prognosis
The course is variable but is accompanied by disease relapse in approximately 75% of patients. Mortality has been reduced with the introduction of cyclophosphamide and other immunosuppressive agents. Compared with adults, children with ANCA-associated vasculitis have fewer treatment-associated morbidities and malignancies.
Akikusa JD, Schneider R, Harvey EA, et al. Clinical features and outcome of pediatric Wegener’s granulomatosis. Arthritis Rheum. 2007;57:837-844.
Bosch X, Guilabert A, Espinosa G, et al. Treatment of antineutrophil cytoplasmic antibody-associated vasculitis. JAMA. 2007;298:655-668.
Finkielman JD, Merkel PA, Schroeder D, et al. Antiproteinase 3 antineutrophil cytoplasmic antibodies and disease activity in Wegener granulomatosis. Ann Intern Med. 2007;147:611-619.
Frosch M, Foell D. Wegener granulomatosis in childhood and adolescence. Eur J Pediatr. 2004;163:425-434.
Kallenberg CG. Pathogenesis of PR3-ANCA associated vasculitis. J Autoimmun. 2008;30:29-36.
Levine D, Akikusa J, Manson D, et al. Chest CT findings in pediatric Wegener’s granulomatosis. Pediatr Radiol. 2007;37:57-62.
Pagnoux C, Mahr A, Hamidou MA, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008;359:2790-2802.
Wung PK, Stone JH. Therapeutics of Wegener’s granulomatosis. Nat Clin Pract Rheumatol. 2006;2:192-200.
161.5 Other Vasculitis Syndromes
In addition to the more common vasculitides discussed earlier in this chapter, other vasculitic conditions can occur in childhood, the most common of which is Kawasaki disease (discussed in Chapter 160). Hypersensitivity vasculitis is a cutaneous vasculitis triggered by medication or toxin exposure. The rash consists of palpable purpura or other nonspecific rash. Skin biopsies reveal characteristic changes of leukocytoclastic vasculitis (small vessels with neutrophilic perivascular or extravascular neutrophilic infiltration). Hypocomplementemic urticarial vasculitis involves small vessels and manifests as recurrent urticaria that resolves over several days but leaves residual hyperpigmentation. This condition is associated with low levels of complement component C1q and systemic findings that include fever, gastrointestinal symptoms, arthritis, and glomerulonephritis. Cryoglobulinemic vasculitis can complicate mixed essential cryoglobulinemia and is a small vessel vasculitis affecting skin, joints, kidneys, and lungs. Primary angiitis of the central nervous system (PACNS) represents vasculitis confined to the CNS and requires exclusion of other systemic vasculitides. Benign angiitis of the central nervous system (BACNS), also known as transient CNS angiopathy, represents a self-limited variant. Cogan syndrome is rare in children; its potential clinical manifestations include constitutional symptoms, inflammatory eye disease, vestibuloauditory dysfunction, arthritis, and aortitis.
Identification of these vasculitis syndromes requires a comprehensive history and physical exam. Other diagnostic considerations are outlined in Table 161-8. Although treatment is tailored to disease severity, treatment generally includes prednisone (up to 2 mg/kg/day) plus steroid-sparing immunosuppressive medications if necessary. For hypersensitivity vasculitis, withdrawal of the triggering medication or toxin is indicated if possible.
Table 161-8 DIAGNOSTIC CONSIDERATIONS FOR OTHER VASCULITIS SYNDROMES
| VASCULITIS SYNDROME | APPROACH TO DIAGNOSIS |
|---|---|
| Hypersensitivity vasculitis | Skin biopsy demonstrating leukocytoclastic vasculitis |
| Hypocomplementemic urticarial vasculitis | |
| Cryoglobulinemic vasculitis | |
| Primary angiitis of the CNS | |
| Benign angiitis of the CNS | Conventional, CT, or MR angiographic evidence of CNS vasculitis |
| Cogan syndrome |
CNS, central nervous system; CT, computed tomography; MR, magnetic resonance.