Chapter 202 Botulism (Clostridium botulinum)
Three naturally occurring forms of human botulism are known: infant (intestinal toxemia) botulism (the most common in the USA), food-borne (classic) botulism, and wound botulism. Two other forms, both human-made, also occur: inhalational botulism from inhaling accidentally aerosolized toxin and iatrogenic botulism from overdosage of therapeutic or cosmetic use of botulinum toxin.
Etiology
Botulism is the acute, flaccid paralysis caused by the neurotoxin produced by Clostridium botulinum or, infrequently, an equivalent neurotoxin produced by rare strains of Clostridium butyricum and Clostridium baratii. C. botulinum is a gram-positive, spore-forming, obligate anaerobe whose natural habitat worldwide is soil, dust, and marine sediments. The organism is found in a wide variety of fresh and cooked agricultural products. Spores of some C. botulinum strains endure boiling for several hours, enabling the organism to survive efforts at food preservation. In contrast, botulinum toxin is heat labile and easily destroyed by heating at ≥85°C for 5 min. Neurotoxigenic C. butyricum has been isolated from a soybean food and from soils near Lake Weishan in China, the site of food-borne botulism outbreaks associated with this organism. Little is known about the ecology of neurotoxigenic C. baratii.
Botulinum toxin is a simple dichain protein consisting of a 100-kd heavy chain that contains the neuronal attachment sites and a 50-kd light chain that is taken into the cell after binding. Botulinum toxin is the most poisonous substance known, the parenteral human lethal dose being estimated at 10−6 mg/kg. The toxin blocks neuromuscular transmission and causes death through airway and respiratory muscle paralysis. Seven antigenic toxin types, designated by letters A-G, are distinguished by the inability of neutralizing antibody against 1 toxin type to protect against a different toxin type. Toxin types are further differentiated into subtypes by differences in the nucleotide sequences of their toxin genes. Like the gene for tetanus toxin, the gene for botulinum toxin for some toxin types and subtypes resides on a plasmid.
The 7 toxin types serve as convenient clinical and epidemiologic markers. Toxin types A, B, E, and F are well-established causes of human botulism, whereas types C and D cause illness in other animals. Neurotoxigenic C. butyricum strains produce a type E toxin, whereas neurotoxigenic C. baratii strains produce a type F toxin. Type G has not been established as a cause of either human or animal disease. The phenomenal potency of botulinum toxin occurs because its 7 light chains are zinc-endopeptidases whose substrates are 1 or 2 proteins of the docking complex by which synaptic vesicles fuse with the terminal neuronal cell membrane and release acetylcholine into the synaptic cleft.
Epidemiology
Infant botulism has been reported from all inhabited continents except Africa. Notably, the infant is the only family member who is ill. The most striking epidemiologic feature of infant botulism is its age distribution, in which in 95% of cases the infants are between 3 wk and 6 mo of age, with a broad peak from 2 to 4 mo of age. Cases have been recognized in infants as young as 1.5 days or as old as 382 days at onset. The male : female ratio of hospitalized cases is approximately 1 : 1, and cases have occurred in most racial and ethnic groups.
Infant botulism is an uncommon and often unrecognized illness. In the USA, about 80-100 hospitalized cases are diagnosed annually; more than 2,500 cases were reported from 1976 to 2010. The full clinical spectrum of infant botulism includes mild outpatient cases and fulminant sudden death cases. Approximately 40% of U.S. hospitalized cases have been reported from California. Consistent with the known asymmetric soil distribution of C. botulinum toxin types, most cases west of the Mississippi River have been caused by type A strains, whereas most cases east of the Mississippi River have been caused by type B strains. One case each in New Mexico, Washington, Ohio, California, Iowa, and Colorado has been caused by C. baratii and type F toxin. Four cases in Italy have resulted from C. butyricum and type E toxin. Identified risk factors for the illness include breast-feeding, the ingestion of honey, and a slow intestinal transit time (<1 stool/day). Breast-feeding may provide protection against fulminant sudden death from infant botulism. Under rare circumstances of altered intestinal anatomy, physiology, and microflora, older children and adults may contract infant-type botulism.
Food-borne botulism results from the ingestion of a food in which C. botulinum has multiplied and produced its toxin. Outbreaks in North America have been associated with baked potatoes, sautéed onions, and chopped garlic served in restaurants, revising the traditional view of food-borne botulism as resulting mainly from home-canned foods. Other outbreaks in the USA have occurred from commercial foods sealed in plastic pouches that relied solely on refrigeration to prevent outgrowth of C. botulinum spores. Uncanned foods responsible for food-borne botulism cases include peyote tea, the hazelnut flavoring added to yogurt, sweet cream cheese, sautéed onions in “patty melt” sandwiches, potato salad, and fresh and dried fish. A trend toward a single case per outbreak or of cases manifesting separately in different cities or hospitals portends that physicians cannot rely on the temporal and geographic clustering of cases to suggest the diagnosis.
Most types of preserved foods have been implicated in food-borne botulism, but the usual offenders in the USA are the “low-acid” (pH ≥ 6.0) home-canned foods such as jalapeño peppers, asparagus, olives, and beans. The potential for food-borne botulism exists throughout the world, but outbreaks occur most commonly in the temperate zones rather than the tropics, where preservation of fruits, vegetables, and other foods is less common.
Approximately 5-10 outbreaks and 20-25 cases of food-borne botulism have occurred annually in the USA. Most of the continental U.S. outbreaks resulted from proteolytic type A or type B strains, which produce a strongly putrefactive odor in the food that some people find necessary to verify by tasting. In contrast, in Alaska and Canada, most food-borne outbreaks have resulted from nonproteolytic type E strains in Native American foods, such as fermented salmon eggs and seal flippers, which do not exhibit signs of spoilage. A further hazard of type E strains is their ability to grow at the temperatures maintained by household refrigerators (5°C).
Wound botulism is an exceptionally rare disease, with <400 cases reported worldwide, but it is important to pediatrics because adolescents and children may be affected. Although many cases have occurred in young, physically active males at greatest risk for traumatic injury, wound botulism also occurs with crush injuries in which no break in the skin is evident. In the past 15 yr, wound botulism from injection has become increasingly common in adult heroin abusers in the western USA and in Europe, not always with evident abscess formation or cellulitis.
A single outbreak of inhalational botulism was reported in 1962 in which 3 laboratory workers in Germany were exposed unintentionally to aerosolized botulinum toxin. Some patients in the USA have been hospitalized by accidental overdose of therapeutic or cosmetic botulinum toxin.
Pathogenesis
All forms of botulism produce disease through a final common pathway. Botulinum toxin is carried by the bloodstream to peripheral cholinergic synapses, where it binds irreversibly, blocking acetylcholine release and causing impaired neuromuscular and autonomic transmission. Infant botulism is an infectious disease that results from ingesting the spores of any of the 3 botulinum toxin-producing clostridial strains, with subsequent spore germination, multiplication, and production of botulinum toxin in the large intestine. Food-borne botulism is an intoxication that results when preformed botulinum toxin contained in an improperly preserved or inadequately cooked food is swallowed. Wound botulism results from spore germination and colonization of traumatized tissue by C. botulinum; it is the analog of tetanus. Inhalational botulism occurs when aerosolized botulinum toxin is inhaled. A bioterrorist attack could result in large or small outbreaks of inhalational or food-borne botulism (Chapter 704).
Botulinum toxin is not a cytotoxin and does not causes overt macroscopic or microscopic pathology. Secondary pathologic changes (pneumonia, petechiae on intrathoracic organs) may be found at autopsy. No diagnostic technique is available to identify botulinum toxin bound at the neuromuscular junction. The healing process in botulism consists of sprouting of new terminal unmyelinated motor neurons. Movement resumes when these new twigs locate noncontracting muscle fibers and reinnervate them by inducing formation of a new motor end plate. In experimental animals, this process takes about 4 wk.
Clinical Manifestations
Botulinum toxin is distributed hematogenously. Because relative blood flow and density of innervation are greatest in the bulbar musculature, all forms of botulism manifest neurologically as a symmetric, descending, flaccid paralysis beginning with the cranial nerve musculature. It is not possible to have botulism without having multiple bulbar palsies, yet in infants, such symptoms as poor feeding, weak suck, feeble cry, drooling, and even obstructive apnea are often not recognized as bulbar in origin (Fig. 202-1). Patients with evolving illness may already have generalized weakness and hypotonia in addition to bulbar palsies when first examined. In contrast to botulism caused by C. botulinum, a majority of the rare cases caused by intestinal colonization with C. butyricum are associated with a Meckel diverticulum accompanying abdominal distention, often leading to misdiagnosis as an acute abdomen. The also rare C. baratii type F infant botulism cases have been characterized by very young age at onset, rapidity of onset, and greater severity of paralysis.
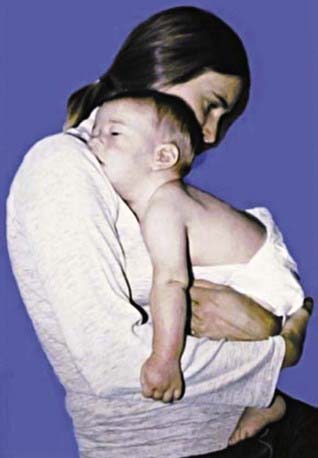
Figure 202-1 A 3 mo old infant with mild infant botulism showing signs of ptosis, an expressionless face, and hypotonia of the neck, trunk, and limbs. The additional bulbar palsies—ophthalmoplegia, weak cry, weak sucking, and dysphagia (drooling)—are not apparent in the photograph.
(From Arnon SS, Schechter R, Maslanka SE, et al: Human botulism immune globulin for the treatment of infant botulism, N Engl J Med 354:462–471, 2006.)
In older children with food-borne or wound botulism, the onset of neurologic symptoms follows a characteristic pattern of diplopia, blurred vision, ptosis, dry mouth, dysphagia, dysphonia, and dysarthria, with decreased gag and corneal reflexes. Importantly, because the toxin acts only on motor nerves, paresthesias are not seen in botulism, except when a patient hyperventilates from anxiety. The sensorium remains clear, but this fact may be difficult to ascertain because of the slurred speech.
Food-borne botulism begins with gastrointestinal symptoms of nausea, vomiting, or diarrhea in about 30% of cases. These symptoms are thought to result from metabolic by-products of growth of C. botulinum or from the presence of other toxic contaminants in the food because gastrointestinal distress is rarely observed in wound botulism. Constipation may occur in food-borne botulism once flaccid paralysis becomes evident. Illness usually begins 12-36 hr after ingestion of the contaminated food but can range from as little as 2 hr to as long as 8 days. The incubation period in wound botulism is 4-14 days. Fever may be present in wound botulism but is absent in food-borne botulism unless a secondary infection (often pneumonia) is present. All forms of botulism display a wide spectrum of clinical severity, from the very mild, with minimal ptosis, flattened facial expression, minor dysphagia, and dysphonia, to the fulminant, with rapid onset of extensive paralysis, frank apnea, and fixed, dilated pupils. Fatigability with repetitive muscle activity is the clinical hallmark of botulism.
Infant botulism differs in apparent initial symptoms of illness only because the infant cannot verbalize them. Usually, the 1st indication of illness is a decreased frequency or even absence of defecation, although this sign is frequently overlooked. Parents typically notice inability to feed, lethargy, weak cry, and diminished spontaneous movement. Dysphagia may be evident as secretions drooling from the mouth. Gag, suck, and corneal reflexes diminish as the paralysis advances. Oculomotor palsies may be evident only with sustained observation. Paradoxically, the pupillary light reflex may be unaffected until the child is severely paralyzed, or it may be initially sluggish. Loss of head control is typically a prominent sign. Respiratory arrest may occur suddenly from airway occlusion by unswallowed secretions or from obstructive flaccid pharyngeal musculature. Occasionally, the diagnosis of infant botulism is suggested by a respiratory arrest that occurs after the infant is curled into position for lumbar puncture.
In mild cases or in the early stages of illness, the physical signs of infant botulism may be subtle and easily missed. Eliciting cranial nerve palsies and fatigability of muscular function requires careful examination. Ptosis may not be seen unless the head of the child is kept erect.
Diagnosis
Clinical diagnosis of botulism is confirmed by specialized laboratory testing that requires hours to days to complete. Therefore, clinical diagnosis is the foundation for early recognition of and response to all forms of botulism. Routine laboratory studies, including those of the cerebrospinal fluid (CSF), are normal in botulism unless dehydration, undernourishment (metabolic acidosis and ketosis), or secondary infection is present.
The classic triad of botulism is the acute onset of a symmetric flaccid descending paralysis with clear sensorium, no fever, and no paresthesias. Suspected botulism represents a medical and public health emergency that is immediately reportable by telephone in most U.S. health jurisdictions. State health departments (1st call) and the U.S. Centers for Disease Control and Prevention (CDC; telephone 770-488-7100 at any time) can arrange for diagnostic testing, epidemiologic investigation, and provision of equine antitoxin.
The diagnosis of botulism is unequivocally established by demonstration of the presence of botulinum toxin in serum or of C. botulinum toxin or organisms in wound material, enema fluid, or feces. C. botulinum is not part of the normal resident intestinal flora of humans, and its presence in the setting of acute flaccid paralysis is diagnostic. An epidemiologic diagnosis of food-borne botulism can be established when C. botulinum organisms and toxin are found in food eaten by patients.
Electromyography (EMG) can sometimes distinguish between causes of acute flaccid paralysis, although results may be variable, including normal, in patients with botulism. The distinctive EMG finding in botulism is facilitation (potentiation) of the evoked muscle action potential at high-frequency (50-Hz) stimulation. In infant botulism, a characteristic pattern, known by the acronym BSAP (brief, small, abundant motor unit action potentials), is present only in clinically weak muscles. Nerve conduction velocity and sensory nerve function are normal in botulism.
Infant botulism requires a high index of suspicion for early diagnosis (Table 202-1). “Rule out sepsis” remains the most common admission diagnosis. If a previously healthy infant (commonly 2-4 mo of age) demonstrates weakness with difficulty in sucking, swallowing, crying, or breathing, infant botulism should be considered a likely diagnosis. A careful cranial nerve examination is then very helpful.
Table 202-1 DIAGNOSES CONSIDERED IN SUBSEQUENTLY LABORATORY-CONFIRMED CASES OF INFANT BOTULISM
| ADMISSION DIAGNOSIS | SUBSEQUENTLY CONSIDERED DIAGNOSES |
|---|---|
| Suspected sepsis, meningitis | Guillain-Barré syndrome |
| Pneumonia | Myasthenia gravis |
| Dehydration | Disorders of amino acid metabolism |
| Viral syndrome | Hypothyroidism |
| Hypotonia of unknown etiology | Drug ingestion Organophosphate poisoning |
| Constipation | Brainstem encephalitis |
| Failure to thrive | Heavy metal poisoning (Pb, Mg, As) |
| Spinal muscular atrophy (Werdnig-Hoffmann disease) | Poliomyelitis Viral polyneuritis Hirschsprung disease Metabolic encephalopathy Medium chain acetyl–CoA dehydrogenase (MCAD) deficiency |
Differential Diagnosis
Botulism is frequently misdiagnosed, most often as a polyradiculoneuropathy (Guillain-Barré or Miller Fisher syndrome), myasthenia gravis, or a disease of the central nervous system (Tables 202-1 and 202-2). In the USA, botulism is more likely than Guillain-Barré syndrome, intoxication, or poliomyelitis to cause a cluster of cases of acute flaccid paralysis. Botulism differs from other flaccid paralyses in its prominent cranial nerve palsies disproportionate to milder weakness and hypotonia below the neck, in its symmetry, and in its absence of sensory nerve damage. Spinal muscular atrophy may closely mimic infant botulism at presentation.
Additional diagnostic procedures may be useful in rapidly excluding botulism as the cause of paralysis. The CSF is unchanged in botulism but is abnormal in many central nervous system diseases. Although the CSF protein concentration is eventually elevated in Guillain-Barré syndrome, it may be normal early in illness. Imaging of the brain, spine, and chest may reveal hemorrhage, inflammation, or neoplasm. A test dose of edrophonium chloride briefly reverses paralytic symptoms in many patients with myasthenia gravis and, reportedly, in some with botulism. A close inspection of the skin, especially the scalp, may reveal an attached tick that is causing paralysis. Possible organophosphate intoxication should be pursued aggressively because specific antidotes (oximes) are available and because the patient may be part of a commonly exposed group, some of whom have yet to demonstrate illness. Other tests that require days for results include stool culture for Campylobacter jejuni as a precipitant of Guillain-Barré syndrome, spinal muscular atrophy and other genetic (including mitochondrial) disorders, and assays for the autoantibodies that cause myasthenia gravis, Lambert-Eaton syndrome, and Guillain-Barré syndrome.
Treatment
Human botulism immune globulin, given intravenously (BIG-IV), is licensed for the treatment of infant botulism caused by type A or B botulinum toxin. Treatment with BIG-IV consists of a single intravenous infusion of 50-100 mg/kg (see package insert) that should be given as soon as possible after infant botulism is suspected in order to immediately end the toxemia that is the cause of the illness. Treatment should not be delayed for laboratory confirmation. In the USA, BIG-IV may be obtained from the California Department of Health Services (24-hr telephone 510-231-7600; www.infantbotulism.org). The use of BIG-IV shortens mean hospital stay from ≈6 wks to 2 wks. Most of the decrease in length of hospital stay results from the reduced time that the patient requires ventilation and in intensive care. Hospital costs are reduced by >$100,000 per case (in 2004 dollars).
Older patients with suspected food, wound, or inhalational botulism may be treated with 1 vial of investigational equine heptavalent botulinum antitoxin (H-BAT), available in the USA through the CDC by way of state and local health departments.
Antibiotic therapy is not part of the treatment of uncomplicated infant or food-borne botulism, because the toxin is primarily an intracellular molecule that is released into the intestinal lumen with vegetative bacterial cell death and lysis. Antibiotics are reserved for the treatment of secondary infections, and in the absence of antitoxin therapy, a nonclostridiocidal antibiotic such as trimethoprim-sulfamethoxazole is preferred. Aminoglycoside antibiotics should be avoided because they may potentiate the blocking action of botulinum toxin at the neuromuscular junction. Wound botulism requires aggressive treatment with antibiotics and antitoxin in a manner analogous to that for tetanus (Chapter 203).
Supportive Care
Management of botulism rests on the following 3 principles: (1) fatigability with repetitive muscle activity is the clinical hallmark of the disease; (2) complications are best avoided by anticipating them; and (3) meticulous supportive care is a necessity. The 1st principle applies mainly to feeding and breathing. Correct positioning is imperative to protect the airway and improve respiratory mechanics. The patient is placed face up on a rigid-bottomed crib (or bed), the head of which is tilted at 30 degrees. A small cloth roll is placed under the cervical vertebrae to tilt the head back so that secretions drain to the posterior pharynx and away from the airway. In this tilted position, the abdominal viscera pull the diaphragm down, thereby improving respiratory mechanics. The patient’s head and torso should not be elevated by bending the middle of the bed; in such a position, the hypotonic thorax would slump into the abdomen and breathing would be compromised.
About half of patients with infant botulism require endotracheal intubation, which is best done prophylactically. The indications include diminished gag and cough reflexes and progressive airway obstruction by secretions. With meticulous management techniques (especially proper tube diameter), monitoring, and positioning, patients have tolerated months of intubation without subglottic stenosis or need for tracheostomy.
Feeding should be done by a nasogastric or nasojejunal tube until sufficient oropharyngeal strength and coordination enable feeding by breast or bottle. Expressed breast milk is the most desirable food for infants, in part because of its immunologic components (e.g., secretory immunoglobulin A [sIgA], lactoferrin, leukocytes). Tube feeding also assists in the restoration of peristalsis, a nonspecific but probably essential part of eliminating C. botulinum from the intestinal flora. Intravenous feeding (hyperalimentation) is discouraged because of the potential for infection and the advantages of tube feeding.
Because sensation remains intact, providing auditory, tactile, and visual stimuli is beneficial. Maintaining strong central respiratory drive is essential, so sedatives and central nervous system depressants are best avoided. Full hydration and stool softeners such as lactulose may mitigate the protracted constipation. Cathartics are not recommended. Patients with food-borne and infant botulism excrete C. botulinum toxin and organisms in their feces, often for weeks, and care should be taken in handling their excreta. When bladder palsy occurs in severe cases, gentle suprapubic pressure with the patient in the sitting position with the head supported may help attain complete voiding and reduce the risk for urinary tract infection. Families of affected patients may require emotional and financial support, especially when the paralysis of botulism is prolonged.
Complications
Almost all of the complications of botulism are nosocomial, and a few are iatrogenic (Table 202-3). Some critically ill, pharmacologically paralyzed patients who must spend weeks or months on ventilators in intensive care units inevitably experience some of these complications. Suspected “relapses” of infant botulism usually reflect premature hospital discharge or an inapparent underlying complication such as pneumonia, urinary tract infection, or otitis media.
Prognosis
When the regenerating nerve endings have induced formation of a new motor end plate, neuromuscular transmission is restored. In the absence of complications, particularly those related to hypoxia, the prognosis in infant botulism is for full and complete recovery. Hospital stay in untreated infant botulism averages 5.7 wk but differs significantly by toxin type, with patients with untreated type B disease being hospitalized a mean of 4.2 wk and those with untreated type A disease 6.7 wk.
In the USA, the case fatality ratio for hospitalized cases of infant botulism is <1%. Patients with untreated infant botulism appear after recovery to have an increased incidence of strabismus that requires timely screening and treatment.
The case fatality ratio in food-borne and wound botulism varies by age, with younger patients having the best prognosis. Some adults with botulism have reported chronic weakness and fatigue for more than 1 yr as sequelae.
Prevention
Food-borne botulism is best prevented by adherence to safe methods of home canning (pressure cooker and acidification), by avoiding suspicious foods, and by heating all home canned foods to 85°C for ≥5 min. Wound botulism is best prevented by not using illicit drugs and by treatment of contaminated wounds with thorough cleansing, surgical debridement, and provision of appropriate antibiotics.
Most patients with infant botulism probably inhaled and then swallowed airborne clostridial spores; these cases cannot be prevented. The one identified, avoidable source of botulinum spores for infants is honey. Honey is an unsafe food for any child younger than 1 yr. Corn syrups were once thought to be a possible source of botulinum spores, but evidence indicates otherwise. Breast-feeding appears to slow the onset of infant botulism and to diminish the risk for sudden death in infants in whom the disease develops.
Arnon SS, Schechter R, Maslanka SE, et al. Human botulism immune globulin for the treatment of infant botulism. N Engl J Med. 2006;354:462-471.
Barash JR, Hsia JK, Arnon SS. Presence of soil-dwelling clostridia in commercial powdered infant formulas. J Pediatr. 2010;156:402-408.
Chertow DS, Tan ET, Maslanka SE, et al. Botulism in 4 adults following cosmetic injections with an unlicensed, highly concentrated botulinum preparation. JAMA. 2006;296:2476-2479.
Fernicia L, Anniballi F, Aurelia P. Intestinal toxemia botulism in Italy, 1984–2005. Eur J Clin Microbiol Infect Dis. 2007;26:385-394.
Francisco AMO, Arnon SS. Clinical mimics of infant botulism. Pediatrics. 2007;119:826-828.
Gottlieb SL, Kretsinger K, Tarkhashvili N, et al. Long-term outcomes of 217 botulism cases in the Republic of Georgia. Clin Infect Dis. 2007;45:174-180.
Koepke R, Sobel J, Arnon SS. Global occurrence of infant botulism, 1976–2006. Pediatrics. 2008;122:e73-e82.
Long SS. Infant botulism and treatment with BIG-IV (BabyBIG). Pediatr Infect Dis J. 2007;26:261-262.
Mitchell WG, Tseng-Ong L. Catastrophic presentation of infant botulism may obscure or delay diagnosis. Pediatrics. 2005;116:e436-e438.
Nevas M, Lindstrom M, Virtanen A, et al. Infant botulism acquired from household dust presenting as sudden infant death syndrome. J Clin Microbiol. 2005;43:511-513.
Sobel J. Botulism. Clin Infect Dis. 2005;41:1167-1173.
Underwood K, Rubin S, Deakers T, et al. Infant botulism: a 30-year experience spanning the introduction of botulism immune globulin intravenous in the intensive care unit at Children’s Hospital Los Angeles. Pediatrics. 2007;120:e1380-e1385.