Chapter 238 Measles
Measles is highly contagious and was once an inevitable experience during childhood. Owing to widespread vaccination, endemic transmission has been interrupted in the USA; indigenous or imported cases (in children or adults) have occasionally resulted in epidemics in the USA in unimmunized or partially immunized American or foreign-born children. In some areas of the world, measles remains a serious threat to children.
Etiology
Measles virus is a single-stranded, lipid-enveloped RNA virus in the family Paramyxoviridae and genus Morbillivirus. Other members of the genus Morbillivirus affect a variety of mammals, such as rinderpest virus in cattle and distemper virus in dogs, but humans are the only host of measles virus. Of the 6 major structural proteins of measles virus, the 2 most important in terms of induction of immunity are the hemagglutinin (H) protein and the fusion (F) protein. The neutralizing antibodies are directed against the H protein, and antibodies to the F protein limit proliferation of the virus during infection. Small variations in genetic composition have also been identified that result in no effect on protective immunity but provide molecular markers that can distinguish between viral types. These markers have been useful in the evaluation of endemic spread of measles.
Epidemiology
The measles vaccine has changed the epidemiology of measles dramatically. Once worldwide in distribution, endemic transmission of measles has been interrupted in many countries where there is widespread vaccine coverage. Historically, measles caused universal infection in childhood in the USA, with 90% of children acquiring the infection before 15 yr of age. Morbidity and mortality associated with measles decreased prior to the introduction of the vaccine as a result of improvements in health care and nutrition. However, the incidence declined dramatically following the introduction of the measles vaccine in 1963. The attack rate fell from 313 cases/100,000 population in 1956-1960 to 1.3 cases/100,000 in 1982-1988.
A nationwide indigenous measles outbreak occurred in 1989-1991, resulting in >55,000 cases, 11,000 hospitalizations, and 123 deaths, demonstrating that the infection had not yet been conquered. This resurgence was attributed to vaccine failure in a small number of school-aged children, low coverage of preschool-aged children, and more rapid waning of maternal antibodies in infants born to mothers who had never experienced wild-type measles infection. Implementation of the 2-dose vaccine policy and more intensive immunization strategies resulted in interruption of endemic transmission in the USA in 1993. The current rate is <1 case/1,000,000 population.
Measles continues to be imported into the USA from abroad; therefore, continued maintenance of >90% immunity through vaccination is necessary to prevent widespread outbreaks from occurring (Fig. 238-1).
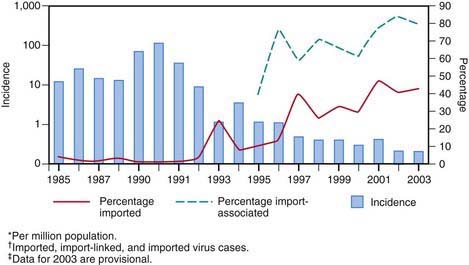
Figure 238-1 Incidence* and percentage of import-associated† measles cases, by year in the USA, 1985–2003‡.
(From the Centers for Disease Control and Prevention: Epidemiology of measles—United States, 2001–2003, MMWR Morb Mortal Wkly Rep 53:713–716, 2004.)
In 2008, 131 cases of measles were reported to the U.S. Centers for Disease Control and Prevention (CDC) in the first 7 months of the year, the highest year-to-date number of cases since 1996. Seven outbreaks accounted for 106 (81%) of the cases. Of the total, 17 patients (13%) had acquired the infection abroad and 99 cases (76%) were linked epidemiologically with the importations. These importation-associated cases occurred primarily among unvaccinated school-aged children whose parents had religious or philosophical objections to vaccination. Measles continues to be imported from abroad, and outbreaks will continue to occur in communities with low vaccination rates.
Transmission
The portal of entry of measles virus is through the respiratory tract or conjunctivae following contact with large droplets or small-droplet aerosols in which the virus is suspended. Patients are infectious from 3 days before to up to 4-6 days after the onset of rash. Approximately 90% of exposed susceptible individuals experience measles. Face-to-face contact is not necessary, because viable virus may be suspended in air for as long as 1 hr after the patient with the source case leaves a room. Secondary cases due to spread of aerosolized virus have been reported in physicians’ offices and in hospitals.
Pathology
Measles infection causes necrosis of the respiratory tract epithelium and an accompanying lymphocytic infiltrate. Measles produces a small vessel vasculitis on the skin and on the oral mucous membranes. Histology of the rash and exanthem reveals intracellular edema and dyskeratosis associated with formation of epidermal syncytial giant cells with up to 26 nuclei. Viral particles have been identified within these giant cells. In lymphoreticular tissue, lymphoid hyperplasia is prominent. Fusion of infected cells results in multinucleated giant cells, the Warthin-Finkeldey giant cells that are pathognomonic for measles, with up to 100 nuclei and intracytoplasmic and intranuclear inclusions.
Pathogenesis
Measles consists of 4 phases: incubation period, prodromal illness, exanthematous phase, and recovery. During incubation, measles virus migrates to regional lymph nodes. A primary viremia ensues that disseminates the virus to the reticuloendothelial system. A secondary viremia spreads virus to body surfaces. The prodromal illness begins after the secondary viremia and is associated with epithelial necrosis and giant cell formation in body tissues. Cells are killed by cell-to-cell plasma membrane fusion associated with viral replication that occurs in many body tissues, including cells of the central nervous system (CNS). Virus shedding begins in the prodromal phase. With onset of the rash, antibody production begins, and viral replication and symptoms begin to subside. Measles virus also infects CD4+ T cells, resulting in suppression of the Th1 immune response and a multitude of other immunosuppressive effects.
Clinical Manifestations
Measles is a serious infection characterized by high fever, an enanthem, cough, coryza, conjunctivitis, and a prominent exanthem. After an incubation period of 8-12 days, the prodromal phase begins with a mild fever followed by the onset of conjunctivitis with photophobia, coryza, a prominent cough, and increasing fever. Koplik spots represent the enanthem and are the pathognomonic sign of measles, appearing 1 to 4 days prior to the onset of the rash (Fig. 238-2). They first appear as discrete red lesions with bluish white spots in the center on the inner aspects of the cheeks at the level of the premolars. They may spread to involve the lips, hard palate, and gingiva. They also may occur in conjunctival folds and in the vaginal mucosa. Koplik spots have been reported in 50-70% of measles cases but probably occur in the great majority.

Figure 238-2 Koplik spots on the buccal mucosa during the 3rd day of rash.
(From Centers for Disease Control and Prevention: Public health image library, image #4500 [website]. http://phil.cdc.gov/phil/details.asp.)
Symptoms increase in intensity for 2-4 days until the 1st day of the rash. The rash begins on the forehead (around the hairline), behind the ears, and on the upper neck as a red maculopapular eruption. It then spreads downward to the torso and extremities, reaching the palms and soles in up to 50% of cases. The exanthem frequently becomes confluent on the face and upper trunk (Fig. 238-3).

Figure 238-3 A child with measles displaying the characteristic red blotchy pattern on his face and body.
(From Kremer JR, Muller CP: Measles in Europe—there is room for improvement, Lancet 373:356–358, 2009.)
With the onset of the rash, symptoms begin to subside. The rash fades over about 7 days in the same progression as it evolved, often leaving a fine desquamation of skin in its wake. Of the major symptoms of measles, the cough lasts the longest, often up to 10 days. In more severe cases, generalized lymphadenopathy may be present, with cervical and occipital lymph nodes especially prominent.
Inapparent Measles Infection
In individuals with passively acquired antibody, such as infants and recipients of blood products, a subclinical form of measles may occur. The rash may be indistinct, brief, or, rarely, entirely absent. Likewise, some individuals who have received vaccine, when exposed to measles, may have a rash but few other symptoms. Persons with inapparent or subclinical measles do not shed measles virus and do not transmit infection to household contacts.
Children who had received the original formalin-inactivated measles vaccine at times demonstrated a more severe form of disease called atypical measles. Such patients had onset of high fever and headache followed by the appearance of a maculopapular rash on the extremities that become petechial and purpuric and progressed in a centripetal direction. The illness was frequently complicated by pneumonia and pleural effusions. It is thought that atypical measles was caused by development of circulating immune complexes that formed as a result of an abnormal immune response to the vaccine.
Laboratory Findings
The diagnosis of measles is almost always based on clinical and epidemiologic findings. Laboratory findings in the acute phase include reduction in the total white blood cell count, with lymphocytes decreased more than neutrophils. Absolute neutropenia has been known to occur, however. In measles not complicated by bacterial infection, the erythrocyte sedimentation rate and C-reactive protein level are normal.
Diagnosis
In the absence of a recognized measles outbreak, confirmation of the clinical diagnosis is often recommended. Serologic confirmation is most conveniently made by identification of immunoglobulin M (IgM) antibody in serum. IgM antibody appears 1-2 days after the onset of the rash and remains detectable for about 1 mo. If a serum specimen is collected <72 hr after onset of rash and is negative for measles antibody, a second specimen should be obtained. Serologic confirmation may also be made by demonstration of a fourfold rise in IgG antibodies in acute and convalescent specimens collected 2-4 wk later. Viral isolation from blood, urine, or respiratory secretions can be accomplished by culture at the CDC or local or state laboratories. Molecular detection by polymerase chain reaction (PCR) is possible but is a research tool.
Differential Diagnosis
Typical measles is unlikely to be confused with other illnesses, especially if Koplik spots are observed. Measles in the later stages or inapparent or subclinical infections may be confused with a number of other exanthematous immune-mediated illnesses and infections, including rubella, adenoviruses, enteroviruses, and Epstein-Barr virus. Exanthem subitum (in infants) and erythema infectiosum (in older children) may also be confused with measles. Mycoplasma pneumoniae and group A streptococcus may also produce rashes similar to that of measles. Kawasaki syndrome can cause many of the same findings as measles but lacks discrete intraoral lesions (Koplik spots) and a severe prodromal cough, and typically leads to elevations of neutrophils and acute-phase reactants. In addition, the characteristic thrombocytosis of Kawasaki syndrome is absent in measles (Chapter 160). Drug eruptions may occasionally be mistaken for measles.
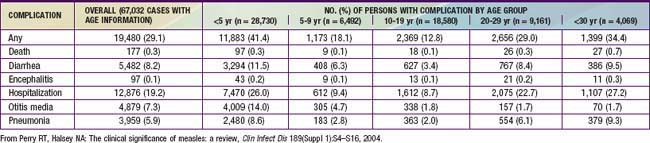
Complications
Complications of measles are largely attributable to the pathogenic effects of the virus on the respiratory tract and immune system (Table 238-1). Several factors make complications more likely. Morbidity and mortality from measles are greatest in patients <5 yr of age (especially <1 yr of age) and >20 yr of age. In developing countries, higher case fatality rates have been associated with crowding, which are possibly attributable to larger inoculum doses after household exposure. Severe malnutrition in children results in suboptimal immune response and higher morbidity and mortality with measles infection. Low serum retinol levels in children with measles have been shown to be associated with higher measles morbidity and mortality in developing countries and in the USA. Measles infection lowers serum retinol concentrations, so subclinical cases of hyporetinolemia may be made symptomatic during measles. Measles infection in immunocompromised persons is associated with increased morbidity and mortality. Among patients with malignancy in whom measles develops, pneumonitis occurs in 58% and encephalitis in 20%.
Pneumonia is the most common cause of death in measles. It may manifest as giant cell pneumonia caused directly by the viral infection or as superimposed bacterial infection. The most common bacterial pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. Following severe measles pneumonia, the final common pathway to a fatal outcome is often the development of bronchiolitis obliterans.
Croup, tracheitis, and bronchiolitis are common complications in infants and toddlers with measles. The clinical severity of these complications frequently requires intubation and ventilatory support until the infection resolves.
Acute otitis media is the most common complication of measles and was of particularly high incidence during the epidemic of the late 1980s and early 1990s because of the relatively young age of affected children. Sinusitis and mastoiditis also occur as complications. Viral and/or bacterial tracheitis is seen and can be life threatening. Retropharyngeal abscess has also been reported.
Measles infection is known to suppress skin test responsiveness to purified tuberculin antigen. There may be a higher rate of activation of pulmonary tuberculoses in populations of individuals infected with Mycobacterium tuberculosis who are then exposed to measles.
Diarrhea and vomiting are common symptoms associated with acute measles, and diffuse giant cell formation is found in the epithelium the gastrointestinal tract. Dehydration is a common consequence, especially in young infants and children. Appendicitis may occur from obstruction of the appendiceal lumen by lymphoid hyperplasia.
Febrile seizures occur in <3% of children with measles. Encephalitis following measles has been a long-associated complication, often with an unfavorable outcome. Rates of 1-3/1,000 cases of measles have been reported, with greater numbers occurring in adolescents and adults than in preschool or school-aged children. Encephalitis is a postinfectious, immunologically mediated process and is not due to a direct effect by the virus. Clinical onset begins during the exanthem and manifests as seizures (56%), lethargy (46%), coma (28%), and irritability (26%). Findings in cerebrospinal fluid (CSF) include lymphocytic pleocytosis in 85% of cases and elevated protein concentration. Approximately 15% of patients with measles encephalitis die, and 20-40% suffer long-term sequelae, including mental retardation, motor disabilities, and deafness.
Measles encephalitis in immunocompromised patients results from direct damage to the brain by the virus. Subacute measles encephalitis manifests 1-10 mo after measles in immunocompromised patients, particularly those with AIDS, lymphoreticular malignancies, and immunosuppression. Signs and symptoms include seizures, myoclonus, stupor, and coma. In addition to intracellular inclusions, abundant viral nucleocapsids and viral antigen are seen in brain tissue. Progressive disease and death almost always occur.
A severe form of measles rarely seen now is hemorrhagic measles or “black measles.” It manifested as a hemorrhagic skin eruption and was often fatal. Keratitis, appearing as multiple punctate epithelial foci, resolved with recovery from the infection. Thrombocytopenia sometimes occurred following measles.
Myocarditis is a rare complication of measles. Miscellaneous bacterial infections have been reported, including bacteremia, cellulitis, and toxic shock syndrome. Measles during pregnancy has been associated with high maternal morbidity, fetal wastage and stillbirths, and congenital malformations in 3% of live born infants.
Subacute Sclerosing Panencephalitis
Subacute sclerosing panencephalitis (SSPE) is a chronic complication of measles with a delayed onset and an outcome that is nearly always fatal. It appears to result from a persistent infection with an altered measles virus that is harbored intracellularly in the CNS for several yr. After 7-10 yr the virus apparently regains virulence and attacks the cells in the CNS that offered the virus protection. This “slow virus infection” results in inflammation and cell death, leading to an inexorable neurodegenerative process.
SSPE is a rare disease and generally follows the prevalence of measles in a population. The incidence rate in the USA in 1960 was 0.61 cases/million persons younger than 20 yr. By 1980 the rate had fallen to 0.06 cases/ million. Between 1956 and 1982 a total of 634 cases had been reported to the national SSPE registry. After 1982 about 5 cases/ yr were reported annually in the USA, and only 2-3 cases/ yr in the early 1990s. However, between 1995 and 2000, reported cases in the USA increased and 13 cases were reported in 2000. Nine of the 13 cases occurred in foreign-born individuals. This “resurgence” may be the result of an increased incidence of measles between 1989 and 1991. Although the age of onset ranges from <1 to <30 yr, the illness is primarily one of children and adolescents. Measles at an early age favors the development of SSPE: 50% of patients with SSPE had primary measles before 2 yr of age, and 75% before 4 yr of age. Males are affected twice as often as females, and there appear to be more cases reported from rural rather than urban populations. Recent observations from the registry indicate a higher prevalence among children of Hispanic origin.
The pathogenesis of SSPE remains enigmatic. Factors that seem to be involved include defective measles virus and interaction with a defective or immature immune system. The virus isolated from brain tissue of patients with SSPE is missing 1 of the 6 structural proteins, the matrix or M protein. This protein is responsible for assembly, orientation, and alignment of the virus in preparation for budding during viral replication. Immature virus may be able to reside, and possibly propagate, within neuronal cells for long periods. The fact that most patients with SSPE were exposed at a young age suggests that immune immaturity is involved in pathogenesis. In addition, the intracellular location of the virus sequesters it from the immune system, especially from humoral immunity.
Clinical manifestations of SSPE begin insidiously 7-13 yr after primary measles infection. Subtle changes in behavior or school performance appear, including irritability, reduced attention span, and temper outbursts. This initial phase (stage I) may at times be missed because of brevity or mildness of the symptoms. Fever, headache, and other signs of encephalitis are absent. The hallmark of the second stage is massive myoclonus, which coincides with extension of the inflammatory process site to deeper structures in the brain, including the basal ganglia. Involuntary movements and repetitive myoclonic jerks begin in single muscle groups but give way to massive spasms and jerks involving both axial and appendicular muscles. Consciousness is maintained. In the third stage, involuntary movements disappear and are replaced by choreoathetosis, immobility, dystonia, and lead pipe rigidity that result from destruction of deeper centers in the basal ganglia. Sensorium deteriorates into dementia, stupor, and then coma. The fourth stage is characterized by loss of critical centers that support breathing, heart rate, and blood pressure. Death soon ensues. Progression through the clinical stages may follow courses characterized as acute, subacute, or chronic progressive.
The diagnosis of SSPE can be established through documentation of a compatible clinical course and at least 1 of the following supporting findings: (1) measles antibody detected in CSF, (2) characteristic electroencephalographic findings, and (3) typical histologic findings in and/or isolation of virus or viral antigen from brain tissue obtained by biopsy or postmortem examination.
CSF analysis reveals normal cells but elevated IgG and IgM antibody titers in dilutions >1:8. Electroencephalographic patterns are normal in stage I, but in the myoclonic phase, suppression-burst episodes are seen that are characteristic of but not pathognomonic for SSPE. Brain biopsy is no longer routinely indicated for diagnosis of SSPE.
Management of SSPE is primarily supportive and similar to care provided to patients with other neurodegenerative diseases. A large randomized clinical trial compared the use of oral inosine pranobex (isoprinosine) alone to oral inosine pranobex and intraventricular interferon-α2b. The treatment courses for both groups were 6 months. Although there were no differences in the rates of stabilization or improvement at 6 months (34% vs 35%), the investigators concluded that these rates were substantially better than historically reported spontaneous improvement rates, which are 5-10%.
Virtually all patients eventually succumb to SSPE. Most die within 1-3 yr of onset from infection or loss of autonomic control mechanisms. Prevention of SSPE depends on prevention of primary measles infection through vaccination. SSPE has been described in patients who have no history of measles infection and only exposure to the vaccine virus. However, wild-type virus, not vaccine virus, has been found in brain tissue of at least some of these patients, suggesting that they had had subclinical measles previously.
Treatment
Management of measles is supportive. Antiviral therapy is not effective in the treatment of measles in otherwise normal patients. Maintenance of hydration, oxygenation, and comfort are goals of therapy. Antipyretics for comfort and fever control are useful. For patients with respiratory tract involvement, airway humidification and supplemental oxygen may be of benefit. Respiratory failure due to croup or pneumonia may require ventilatory support. Oral rehydration is effective in most cases, but severe dehydration may require intravenous therapy. Prophylactic antimicrobial therapy to prevent bacterial infection is not indicated.
Measles infection in immunocompromised patients is highly lethal. Ribavirin is active in vitro against measles virus. Anecdotal reports of ribavirin therapy with or without intravenous gamma globulin suggest some benefit in individual patients. However, no controlled trials have been performed, and ribavirin is not licensed in the USA for treatment of measles.
Vitamin A
Vitamin A deficiency in children in developing countries has long been known to be associated with increased mortality from a variety of infectious diseases, including measles. In the USA, studies in the early 1990s documented that 22-72% of children with measles had low retinol levels. In addition, one study demonstrated an inverse correlation between the level of retinol and severity of illness. Several randomized controlled trials of vitamin A therapy in the developing world and the USA have demonstrated reduced morbidity and mortality from measles. The American Academy of Pediatrics suggests vitamin A therapy for selected patients with measles (Table 238-2).
Table 238-2 RECOMMENDATIONS FOR VITAMIN A TREATMENT OF CHILDREN WITH MEASLES
INDICATIONS
Children 6 mo-2 yr of age hospitalized with measles and its complications (e.g., croup, pneumonia, and diarrhea). (Limited data are available about the safety of and need for vitamin A supplementation for infants <6 mo of age).
Children >6 mo of age with measles who are not already receiving vitamin A supplementation and who have any of the following risk factors:
REGIMEN
Parenteral and oral formulations of vitamin A are available in the USA. The recommended dosage, administered as a capsule, is:
The dose should be repeated the next day and again 4 wk later for children with ophthalmologic evidence of vitamin A deficiency
Data from the American Academy of Pediatrics: Red book: 2009 report of the Committee on Infectious Diseases, ed 28, Elk Grove Village, IL, 2009, American Academy of Pediatrics, p 446.
Prognosis
In the early 20th century, deaths due to measles varied between 2,000 and 10,000, or about 10 deaths per 1,000 cases of measles. With improvements in health care and antimicrobial therapy, better nutrition, and decreased crowding, the death-to-case ratio fell to 1/1,000 cases. Between 1982 and 2002, the CDC estimated that there were 259 deaths caused by measles in the USA, with a death-to-case ratio of 2.5-2.8/1,000 cases of measles. Pneumonia and encephalitis were complications in most of the fatal cases, and immunodeficiency conditions were identified in 14-16% of deaths.
Prevention
Patients shed measles virus from 7 days after exposure to 4-6 days after the onset of rash. Exposure of susceptible individuals to patients with measles should be avoided during this period. In hospitals, standard and airborne precautions should be observed for this period. Immunocompromised patients with measles will shed virus for the duration of the illness, so isolation should be maintained throughout the disease.
Vaccine
Measles vaccine in the USA is available as a monovalent preparation or combined with the rubella (MR) or measles-mumps-rubella (MMR) vaccine, the last of which is the recommended form in most circumstances (Table 238-3). Following the measles resurgence of 1989-1991, a second dose of measles vaccine was added to the schedule. The current recommendations include a first dose at 12-15 mo followed by a second dose at 4-6 yr of age. Seroconversion is slightly lower in children who receive the first dose before or at 12 mo of age (87% at 9 mo, 95% at 12 mo, and 98% at 15 mo) because of persisting maternal antibody. For children who have not received 2 doses by 11-12 yr of age, a second dose should be provided. Infants who receive a dose before 12 mo of age should be given 2 additional doses at 12-15 mo and 4-6 yr of age.
Table 238-3 RECOMMENDATIONS FOR MEASLES IMMUNIZATION
| CATEGORY | RECOMMENDATIONS |
|---|---|
| Unimmunized, no history of measles (12-15 mo of age) | A 2-dose schedule (with MMR) is recommended The first dose is recommended at 12-15 mo of age; the 2nd is recommended at 4-6 yr of age |
| Children 6-11 mo of age in epidemic situations or prior to international travel | Immunize (with monovalent measles vaccine, or if not available, MMR); reimmunization (with MMR) at 12-15 mo of age is necessary, and a 3rd dose is indicated at 4-6 yr of age |
| Children 4-12 yr of age who have received 1 dose of measles vaccine at ≥12 mo of age | Reimmunize (1 dose) |
| Students in college and other post–high school institutions who have received 1 dose of measles vaccine at ≥12 mo of age | Reimmunize (1 dose) |
| History of immunization before the 1st birthday | Consider susceptible and immunize (2 doses) |
| History of receipt of inactivated measles vaccine or unknown type of vaccine, 1963-1967 | Consider susceptible and immunize (2 doses) |
| Further attenuated or unknown vaccine given with IG | Consider susceptible and immunize (2 doses) |
| Allergy to eggs | Immunize; no reactions likely |
| Neomycin allergy, nonanaphylactic | Immunize; no reactions likely |
| Severe hypersensitivity (anaphylaxis) to neomycin or gelatin | Avoid immunization |
| Tuberculosis | Immunize; if patient has untreated tuberculosis disease, start antituberculosis therapy before immunizing |
| Measles exposure | Immunize and/or give IG, depending on circumstances |
| HIV-infected | Immunize (2 doses) unless severely immunocompromised |
| Personal or family history of seizures | Immunize; advise parents of slightly increased risk of seizures |
| IG or blood recipient | Immunize at the appropriate interval (see Table 238-4) |
IG, immunoglobulin; MMR, measles-mumps-rubella vaccine.
From American Academy of Pediatrics: Red book: 2009 report of the Committee on Infectious Diseases, ed 28, Elk Grove Village, IL, 2009, American Academy of Pediatrics, p 450.
Adverse events from the MMR vaccine include fever (usually 6-12 days following vaccination), rash in about 5% of vaccines, and, rarely, transient thrombocytopenia. Children prone to febrile seizures may experience an event following vaccination, so the risks and benefits of vaccination should be discussed with parents. Encephalopathy and autism have not been shown to be causally associated with the MMR vaccine nor vaccine constituents.
A review of the effect of measles vaccination on the epidemiology of SSPE has demonstrated that measles vaccination protects against SSPE and does not accelerate the course of SSPE or trigger the disease in those already infected with wild measles virus.
Passively administered immune globulin may inhibit the immune response to live measles vaccine, and administration should be delayed for variable amounts of time based on the dose of immune globulin (Table 238-4).
Live vaccines should not be administered to pregnant women or to immunodeficient or immunosuppressed patients. However, patients with HIV who are not severely immunocompromised should be immunized. Because measles virus may suppress the cutaneous response to tuberculous antigen, skin testing for tuberculosis should be performed before or at the same time as administration of the vaccine. Individuals infected with M. tuberculosis should be receiving appropriate treatment at the time of administration of measles vaccine.
Postexposure Prophylaxis
Susceptible individuals exposed to measles may be protected from infection by either vaccine administration or immunization with immune globulin. The vaccine is effective in prevention or modification of measles if given within 72 hr of exposure. Immune globulin may be given up to 6 days after exposure to prevent or modify infection. Immunocompetent children should receive 0.25 mL/kg intramuscularly, and immunocompromised children should receive 0.5 mL/kg (maximum dose in both cases is 15 mL/kg). Immune globulin is indicated for susceptible household contacts of measles patients, especially infants <6 mo of age, pregnant women, and immunocompromised persons.
American Academy of Pediatrics, Committee on Infectious Diseases. Vitamin A treatment of measles. Pediatrics. 1993;91:1014-1015.
Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333:890-895.
Campbell H, Andrews N, Brown KE, et al. Review of the effect of measles vaccination on the epidemiology of SSPE. Int J Epidemiol. 2007;36:1334-1348.
Caulfield LE, deOvis M, Blössner M, et al. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria and measles. Am J Clin Nutr. 2004;80:193-198.
Centers for Disease Control and Prevention. Global measles mortality, 200–2008. MMWR Morb Mortal Wkly Rep. 2009;58:1321-1326.
Centers for Disease Control and Prevention. Measles—United States, January 1–April 25, 2008. Morb Mortal Wkly Rep. 2008;57:494-498.
Centers for Disease Control and Prevention. Out break of measles—San Diego, California, January–February 2008. Morb Mortal Wkly Rep. 2008;57:203-206.
Centers for Disease Control and Prevention. Multistate measles outbreak associated with an international youth sporting event—Pennsylvania, Michigan, and Texas, August–September 2007. MMWR Morb Mortal Wkly Rep. 2008;57:169-172.
Centers for Disease Control and Prevention. Import-associated measles outbreak—Indiana, May–June 2005. Morb Mortal Wkly Rep. 2005;54:1073-1075.
Centers for Disease Control and Prevention. Update: Measles—United States, January–July 2008. Morb Mortal Wkly Rep. 2008;57:893-896.
Demicheli V, Jefferson T, Rivetti A, et al: Vaccines for measles, mumps, and rubella in children (review), Cochrane Database Syst Rev (4):CD004407, 2005.
Dyken PR. Nonprogressive disease of post-infectious origin: a review of resurging subacute sclerosing parencephalitis (SSPE). Ment Retard Dev Disabil Res Rev. 2001;7:217-225.
Elliman D, Bedford H. Achieving the goal for global measles mortality. Lancet. 2007;369:165-166.
Halsey NA. Measles in developing countries. BMJ. 2006;333:1234.
Katz SL. Has the measles-mumps-rubella vaccine been fully exonerated? Pediatrics. 2006;118:1744-1745.
Kremer JR, Muller CP. Measles in Europe—there is room for improvement? Lancet. 2009;373:356-358.
Meissner HC, Strebel PM, Orenstein WA. Measles vaccine and the potential for worldwide eradication of measles. Pediatrics. 2004;114:1065-1069.
Otten M, Kezaala R, Fall A, et al. Public-health impact of accelerated measles control in the WHO African region 2000–03. Lancet. 2005;366:832-838.
Parker AA, Staggs W, Dayan GH, et al. Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355:447-454.
Perry RT, Halsey NA. The clinical significance of measles: a review. Clin Infect Dis. 2004;189(Suppl 1):S4-S16.
Rosales FJ. Vitamin A supplementation of vitamin deficient measles patients lowers risk of measles-related pneumonia in Zambian children. J Nutr. 2002;132:3700-3703.
Redd SC, King GE, Heath JL, et al. Comparison of vaccination with measles-mumps-rubella vaccine at 9, 12, and 15 months of age. J Infect Dis. 2004;189(Suppl 1):S116-S122.
Remington PL, Hall WN, Davis IH, et al. Airborne transmission of measles in a physician’s office. JAMA. 1985;253:1574-1577.
Rivera ME, Mason WH, Ross LA, et al. Nosocomial measles infection in a pediatric hospital during a community-wide epidemic. J Pediatr. 1991;119:183-186.
Sugerman DE, Barskey AE, Delea MG, et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally under vaccinated. Pediatrics. 2010;125:747-755.
Suringa DWR, Bank LJ, Ackerman AB. Role of measles virus in skin lesions and Koplik’s spots. N Engl J Med. 1970;283:1139-1142.