Chapter 251 Parainfluenza Viruses
Parainfluenza viruses (PIVs) are common causes of respiratory illness in infants and children and are second only to respiratory syncytial virus as an important viral cause of lower respiratory tract infections in young children and immunocompromised patients. These viruses cause a spectrum of upper and lower respiratory tract illnesses but are particularly associated with croup (laryngotracheitis or laryngotracheobronchitis), bronchiolitis, and pneumonia.
Etiology
The PIVs are members of the Paramyxoviridae family. Four PIVs cause illness in humans, classified as types 1-4, with diverse manifestations of infection. Type 4 is divided into 2 antigenic subgroups, A and B. PIVs have a nonsegmented, single-stranded RNA genome with a lipid-containing envelope derived from budding through the cell membrane. The major antigenic moieties are the HN and F envelope spike glycoproteins, which exhibit hemagglutinin-neuraminidase and fusion functions, respectively.
Epidemiology
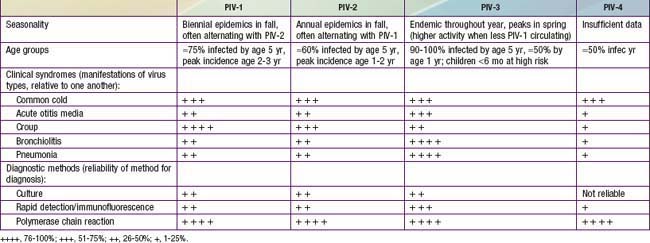
By 5 yr of age, most children have experienced primary infection with PIV types 1, 2, and 3 (Table 251-1). PIV-3 infections often occur in the first 6 mo of life, whereas PIV-1 and PIV-2 are more common after infancy. In the USA and temperate climates, PIV-1 and PIV-2 have biennial epidemics in the fall, usually alternating years in which their serotype is most prevalent. PIV-3 is endemic throughout the year but typically peaks in late spring. In years with less PIV-1 activity, the PIV-3 season may extend longer or have a second peak in the fall. The epidemiology of PIV-4 is less well defined, because it is difficult to grow in tissue culture and was often excluded from early studies.
PIVs are spread primarily from the respiratory tract by inhalation of large respiratory droplets or contact with infected secretions. PIVs are notable for causing outbreaks of respiratory infections in hospital wards, clinics, neonatal nurseries, and other institutional settings. The incubation period from exposure to symptom onset is 2-6 days. Children are likely to excrete virus from the oropharynx for 2-3 wk, but excretion can be more prolonged even in immunocompetent children; in immunocompromised patients, excretion may persist for months. Primary infection does not confer permanent immunity, and re-infections are common throughout life. Re-infections are generally mild and self limited.
Pathogenesis
PIVs replicate in the respiratory epithelium. The propensity to cause illness in the upper large airways is presumably related to preferential replication in the larynx, trachea, and bronchi in comparison with other viruses. Some PIVs induce cell-to-cell fusion. During the budding process, cell membrane integrity is lost, and viruses can induce cell death through the process of apoptosis. In children, the most severe illness coincides with the time of maximal viral shedding. However, disease severity is likely related to the inflammatory response as much as to direct cytopathic effects of the virus.
Virus-specific immunoglobulin (Ig) A antibody levels correlate with protection from PIV infection. Circulating serum antibody is also likely to play a role in protection against PIV acquisition and progression to severe infection. Patients with compromised cellular immunity have severe, prolonged disease, suggesting that T cells are critical to controlling and terminating PIV infection.
Clinical Manifestations
Most PIV infections manifest themselves primarily in the upper respiratory tract (see Table 251-1). The most common types of illness consist of some combination of low-grade fever, rhinorrhea, cough, pharyngitis, and hoarseness and may be associated with vomiting or diarrhea. Rarely, PIV infection has been associated with parotitis. The illnesses usually last 4-5 days. The generally mild illness pattern is belied by a spectrum of rarer but more serious illnesses that result in hospitalization. PIVs account for 50% of hospitalizations for croup and at least 15% of cases of bronchiolitis and pneumonia. PIV-1 and to a lesser extent PIV-2 cause more cases of croup, whereas PIV-3 is more likely to infect the small air passages and cause pneumonia, bronchiolitis, or bronchitis. Any PIV can cause lower respiratory tract disease, particularly during primary infection or in immunosuppressed patients.
Laboratory Findings
Conventional laboratory diagnosis of infection is accomplished by PIV isolation in tissue culture. Direct immunofluorescent (IF) staining is available in some centers for rapid identification of virus antigen in respiratory secretions. Many laboratories perform polymerase chain reaction (PCR) viral genomic testing, which greatly increases sensitivity of PIV detection (see Table 251-1). For viral culture or IF, a nasal wash or aspirate provides the best sample, but for PCR, nasal swabs are also appropriate.
Diagnosis and Differential Diagnosis
The diagnosis of PIV infection in children is often based only on clinical and epidemiologic criteria. Croup is a clinical diagnosis and must be distinguished from foreign body aspiration, epiglottitis, pharyngeal abscess, and subglottic hemangioma. Although the radiographic “steeple sign,” consisting of progressive narrowing of the subglottic region, is characteristic of croup, differential considerations include acute epiglottitis, thermal injury, angioedema, and bacterial tracheitis. Manifestation of PIV lower respiratory tract disease may be similar to that of a number of other respiratory viral infections; therefore, identification of virus should be specifically sought by the most sensitive diagnostic means available for certain severe illnesses, such as pneumonia in immunocompromised children.
Treatment
There are no approved treatments for PIV infections with the exception of croup. For croup, the possibility of rapid respiratory compromise should influence the acuity of care given (Chapter 377). Humidified air has not been shown to be effective. Generally a single dose of oral, intramuscular, or intravenous dexamethasone (0.6 mg/kg) should be part of the management of croup in the office or emergency room setting. This dose may be repeated, but there are no guidelines to compare outcomes of single- and multiple-dose treatment schedules. Nebulized epinephrine (either racemic epinephrine 2.25%, 0.5 mL in 2.5 mL of saline, or L-epinephrine, 1:1000 dilution in 5 mL of saline) may also provide temporary symptomatic improvement. Children should be observed for at least 2 hr after receiving epinephrine treatment for return of obstructive symptoms. Repeated treatments may obviate the need for intubation. Oxygen should be administered for hypoxia, and supportive care with analgesics and antipyretics is reasonable for fever and discomfort associated with PIV infections. The indications for antibiotics are limited to well-documented secondary bacterial infections of the middle ear(s) or lower respiratory tract.
Ribavirin has some antiviral activity against PIVs in vitro and in animal models. Inhaled ribavirin should be considered for severely immunocompromised children with PIV pneumonia. Promising strategies for drug development include hemagglutinin-neuraminidase inhibitors and synthetic small interfering RNAs.
Complications
Eustachian tube obstruction can lead to secondary bacterial invasion of the middle ear space and acute otitis media in 30-50% of PIV infections. Similarly, obstruction of the paranasal sinuses can lead to sinusitis. The destruction of cells in the upper airways can lead to secondary bacterial invasion and resultant bacterial tracheitis, and antecedent PIV infection of lower airways may predispose to bacterial pneumonia. Non-respiratory complications of PIV are rare but include aseptic meningitis, encephalitis, acute disseminated encephalomyelitis, rhabdomyolysis, myocarditis, and pericarditis.
Prognosis
The prognosis for full recovery from PIV infection in the normal child is excellent, with no long-term pulmonary sequelae.
Prevention
Vaccine development is focused on live intranasal PIV-3 vaccines. The candidates include a cold-adapted virus of human origin, an attenuated bovine PIV-3, and a newer construct using the bovine PIV-3 vaccine with insertion of human PIV-3 HN and F genes and the F protein of respiratory syncytial virus. The measure of protection afforded by vaccines will be difficult to assess, because symptomatic re-infection is seen and the frequency of serious infection in the general population is low. Nonetheless, it is clear that prevention of acute respiratory illness caused by PIVs, particularly lower respiratory tract infections among infants and young children, is a worthwhile goal.
Cherry JD. Clinical practice: croup. N Engl J Med. 2008;358:384-391.
Chonmaitree T, Revai K, Grady JJ, et al. Viral upper respiratory tract infection and otitis media complication in young children. Clin Infect Dis. 2008;46:815-823.
Fry AM, Curns AT, Harbour K, et al. Seasonal trends of human parainfluenza viral infections: United States, 1990–2004. Clin Infect Dis. 2006;43:1016-1022.
Henrickson KJ. Parainfluenza viruses. Clin Microbiol Rev. 2003;16:242-264.
Lau SK, To WK, Tse PW, et al. Human parainfluenza virus 4 outbreak and the role of diagnostic tests. J Clin Microbiol. 2005;43:4515-4521.
Loughlin GM, Moscona A. The cell biology of acute childhood respiratory disease: therapeutic implications. Pediatr Clin North Am. 2006;53:929-959.
Nichols WG, Peck Campbell AJ, Boeckh M. Respiratory viruses other than influenza virus: impact and therapeutic advances. Clin Microbiol Rev. 2008;21:274-290.
Reed G, Jewett PH, Thompson J, et al. Epidemiology and clinical impact of parainfluenza virus infections in otherwise healthy infants and young children <5 years old. J Infect Dis. 1997;175:807-813.
Sato M, Wright PF. Current status of vaccines for parainfluenza virus infections. Pediatr Infec Dis J. 2008;27:S123-S125.
Weinberg GA, Hall CB, Iwane MK, et al. Parainfluenza virus infection of young children: estimates of the population-based burden of hospitalization. J Pediatr. 2009;154:694-699.