Chapter 450 Other Microcytic Anemias
Sideroblastic anemias result from acquired and hereditary disorders of heme synthesis. The anemias are characterized by hypochromic microcytic red blood cells (RBCs) mixed with normal RBCs, thus giving an overall picture of a dimorphic population of erythrocytes, and the complete blood cell count indicates an extremely high RBC distribution width (RDW). The serum iron concentration usually is elevated, and the transferrin saturation of iron is increased. In all cases of sideroblastic anemia, regardless of the specific cause, impaired heme synthesis leads to retention of iron within the mitochondria. Morphologically, this is seen in marrow nucleated RBCs with iron granules (aggregates of iron in mitochondria) that have a perinuclear distribution. These unusual cells, known as ringed sideroblasts (see ![]() Fig. 450-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com), are found only in pathologic states and are distinct from the sideroblasts (RBC precursors that contain diffuse cytoplasmic ferritin granules) in the marrow of normal subjects. Sideroblastic anemias most commonly occur in adulthood, and these acquired disorders can be idiopathic or secondary to drugs, alcohol, or myelodysplastic disorders. A few sideroblastic anemias are seen in children.
Fig. 450-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com), are found only in pathologic states and are distinct from the sideroblasts (RBC precursors that contain diffuse cytoplasmic ferritin granules) in the marrow of normal subjects. Sideroblastic anemias most commonly occur in adulthood, and these acquired disorders can be idiopathic or secondary to drugs, alcohol, or myelodysplastic disorders. A few sideroblastic anemias are seen in children.
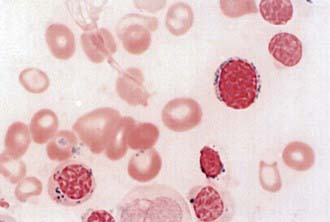
Figure 450-1 Ring sideroblast in myelodysplastic syndrome (refractory anemia with ring sideroblasts)—iron stain.
(From Ryan DH, Cohen HJ: Bone marrow examination. In Hoffman R, Benz EJ Jr, Shattil SJ, et al, editors: Hematology, ed 4, Philadelphia, 2005, Churchill Livingstone.)
Congenital Sideroblastic Anemia
Congenital sideroblastic anemia is rare and conforms to an X-linked pattern of inheritance. It usually occurs in males, although skewed lyonization has resulted in affected females. Autosomal dominant and sporadic cases also occur. Hereditary sideroblastic anemias result from abnormalities of the erythrocytic isozyme for 5-aminolevulinic acid synthetase (ALAS), the rate-limiting enzyme reaction in heme synthesis. An important cofactor for ALAS is pyridoxal phosphate. The gene for the erythrocyte-specific ALAS (ALAS2) is located on the X chromosome, and >25 different missense mutations have been identified. Several of these mutations occur near the binding site for pyridoxal phosphate.
Severe anemias are recognized in infancy or early childhood, whereas milder cases might not become apparent until early adulthood or later. Clinical findings include pallor, icterus, and moderate splenomegaly and/or hepatomegaly. The severity of the anemia varies such that some patients require no therapy and others need regular RBC transfusions. A subset of patients with hereditary sideroblastic anemia manifests a hematologic response to pharmacologic doses of pyridoxine. Iron overload as manifested by elevated serum ferritin, elevated serum iron, and increased transferrin saturation is a major complication of this disorder. Clinical evidence of iron overload (e.g., diabetes mellitus, liver dysfunction) may be found in some patients who have little or no anemia. Stem cell transplantation has been used to treat affected children who were dependent on RBC transfusions.
A unique variant of congenital sideroblastic anemia is Pearson syndrome, characterized by the early onset of transfusion-dependent anemia, neutropenia, and thrombocytopenia. In addition to the usual marrow abnormalities of sideroblastic anemia, children with this syndrome also have vacuolization of RBC and myeloid precursors. In contrast to other sideroblastic anemias, which are microcytic, this is a macrocytic anemia and consequently it sometimes is confused with Diamond-Blackfan anemia (Chapter 442).
Rare Types of Hypochromic Microcytic Anemia
Isolated cases of hypochromic microcytic anemia with other abnormalities of iron metabolism are known; some patients have had defects in iron mobilization or reutilization. Congenital absence of iron-binding protein (atransferrinemia) is a very rare disorder associated with severe hypochromic anemia despite iron overload and requires infusions of apo-transferrin and iron chelation therapy, although the latter may be avoided if the transferrin infusions are started early. Iron is absorbed normally and is deposited in the visceral organs rather than in bone marrow.
Several patients have had refractory hypochromic anemia associated with lymphatic tumors or lymphoid hyperplasia. Correction of the anemia followed removal of the abnormal lymphatic tissue in these patients (Chapters 483 and 500).
Hereditary pyropoikilocytosis and copper deficiency are other rare microcytic anemias. The former is a severe hemolytic anemia in which marked red cell fragmentation is noted on smear. Copper deficiency may be associated with a mild microcytic anemia.
Alcindor T, Bridges KR. Sideroblastic anaemias. Br J Haematol. 2002;116:733-743.
Ayas M, Al-Jefri A, Mustafa MM, et al. Congenital sideroblastic anaemia successfully treated using allogeneic stem cell transplantation. Br J Haematol. 2001;113:938.
Chalco JP, Huicho L, Alamo C, et al. Accuracy of clinical pallor in the diagnosis of anemia in children: a meta-analysis. BMC Pediatrics. 2005;5:46.
Fleming MD. The genetics of inherited sideroblastic anemias. Semin Hematol. 2002;39:270-281.
Guernsey DL, Jiang H, Campagna DR, et al. Mutations in mitochondrial carrier family gene SLC25A38 cause nonsyndromic autosomal recessive congenital sideroblastic anemia. Nat Genet. 2009;41:651-656.
Moy RJ. Prevalence, consequences and prevention of childhood nutritional iron deficiency: a child public health perspective. Clin Lab Haematol. 2006;28:291-298.
Panagiotou JP, Douros K. Clinicolaboratory findings and treatment of iron-deficiency anemia in childhood. Pediatr Hematol Oncol. 2004;21:521-534.
Sandoval C, Jayabose S, Eden AN. Trends in diagnosis and management of iron deficiency during infancy and early childhood. Hematol Oncol Clin North Am. 2004;18:1423-1438. x
Walter T. Effect of iron-deficiency anemia on cognitive skills and neuromaturation in infancy and childhood. Food Nutr Bull. 2003;24(4 Suppl):S104-S110.