Chapter 511 Goodpasture Disease
Goodpasture disease is characterized by pulmonary hemorrhage and glomerulonephritis. The disease results from the attack of these normal organs by antibodies directed against specific epitopes of type IV collagen within the alveolar basement membrane in the lung and glomerular basement membrane (GBM) in the kidney. The etiology of these antibodies is unknown.
Pathology
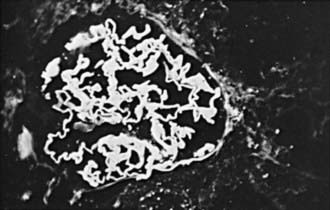
Kidney biopsy shows crescentic glomerulonephritis in most patients. Immunofluorescence microscopy demonstrates continuous linear deposition of immunoglobulin G along the GBM (Fig. 511-1).
Clinical Manifestations
Goodpasture disease is rare in childhood. Patients usually present with hemoptysis from pulmonary hemorrhage that can be life-threatening. Concomitant renal manifestations include acute nephritic syndrome with hematuria, proteinuria, and hypertension, which usually follows a rapidly progressive course. Renal failure commonly develops within days to weeks of clinical presentation. Uncommonly, patients can have anti-GBM nephritis manifesting as isolated, rapidly progressive glomerulonephritis without pulmonary hemorrhage. In essentially all cases, serum anti-GBM antibody is present and complement C3 level is normal.
Diagnosis and Differential Diagnosis
The diagnosis is made by a combination of the clinical presentation of pulmonary hemorrhage with acute glomerulonephritis, the presence of serum antibodies directed against GBM (anti–type IV collagen in GBM), and characteristic renal biopsy findings. Other diseases that can cause a pulmonary-renal syndrome need to be considered and include systemic lupus erythematosus, Henoch-Schönlein purpura, Wegener granulomatosis, and microscopic polyangiitis. These diseases are ruled out by the absence of other characteristic clinical features, kidney biopsy findings, and negative serologic studies for antibodies against nuclear (ANA), DNA (A-DNase), and neutrophil cytoplasmic components (ANCA).
Prognosis and Treatment
Untreated, the prognosis of Goodpasture disease is poor. The combination of high-dose intravenous methylprednisolone, cyclophosphamide, and plasmapheresis appears to improve the possibility of survival. Nevertheless, patients who survive the pulmonary hemorrhage often progress to end-stage renal failure despite ongoing immunosuppressive therapy.
Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: diagnosing it and finding the cause. Cleve Clin J Med. 2008;75:258-280.
Levy JB, Turner N, Rees AJ, et al. Long-term outcome of anti-glomerular basement membrane antibody disease treated with plasma exchange and immunosuppression. Ann Intern Med. 2001;134:1033-1042.
Nagata M. Immune-mediated glomerular injury. In: Avner ED, Harmon WE, Niaudet P, et al, editors. Pediatric nephrology. ed 6. Heidelburg, Germany: Springer-Verlag; 2009:703-742.
Ooi JD, Holdsworth SR, Kitching AR. Advances in the pathogenesis of Goodpasture’s disease: from epitopes to autoantibodies to effector T cells. J Autoimmun. 2008;31:295-300.