Chapter 535 Anomalies of the Bladder
Bladder Exstrophy
Classic exstrophy of the urinary bladder occurs in about 1/35,000-40,000 births. The male:female ratio is 2 : 1. The severity ranges from simple epispadias (in boys) to complete exstrophy of the cloaca involving exposure of the entire hindgut and the bladder (termed cloacal exstrophy).
Clinical Manifestations
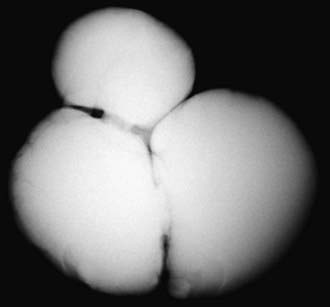
Anomalies of the bladder are hypothesized to result when the mesoderm fails to invade the cephalad extension of the cloacal membrane; the extent of this failure determines the degree of the anomaly. In classic bladder exstrophy (Fig. 535-1), the bladder protrudes from the abdominal wall and its mucosa is exposed. The umbilicus is displaced downward, the pubic rami are widely separated in the midline, and the rectus muscles are separated. In boys, there is complete epispadias with dorsal chordee, and the overall penile length is approximately half that of unaffected boys. The scrotum typically is separated slightly from the penis and is wide and shallow. Undescended testes and inguinal hernias are common. Girls also have epispadias, with separation of the two halves of the clitoris and wide separation of the labia. The anus is displaced anteriorly in both sexes, and there may be rectal prolapse. The pubic rami are widely separated. Persons with exstrophy tend to be shorter than normal.

Figure 535-1 Classic bladder exstrophy in a newborn boy. The bladder is exposed in the midline, the umbilical cord is displaced caudad, the penis is epispadiac, and the scrotum is broad.
The consequences of untreated bladder exstrophy are total urinary incontinence and an increased incidence of bladder cancer, usually adenocarcinoma. The genital deformities can produce sexual disability in both sexes, particularly in males. The wide separation of the pubic rami causes a characteristic broad-based gait but no significant disability. In classic bladder exstrophy, the upper urinary tracts usually are normal.
Treatment
Management of bladder exstrophy should start at birth. The bladder should be covered with plastic wrap to keep the bladder mucosa moist. Application of gauze or petroleum-gauze to the bladder mucosa should be avoided, because significant inflammation will result. The infant should be transferred promptly to a center with pediatric urologic and anesthetic support for the treatment of such anomalies. These children are prone to latex allergy, so latex precautions should be practiced in their care.
There are 2 surgical approaches: staged reconstruction and total single-stage reconstruction. In a staged reconstruction, the initial stage is bladder closure, the second (in boys) is epispadias repair, and the final stage is bladder neck reconstruction. The single stage reconstruction attempts to reconstruct the entire malformation in a single procedure. When this operation is performed in the newborn, there is an increased risk of intraoperative penile injury and postoperative hydronephrosis, compared with the staged reconstruction. The complication rate is high with both approaches and there is no consensus on which is better.
Prompt closure of the exstrophic bladder in the newborn is preferred. During this procedure the abdominal wall is mobilized and the pubic rami are brought together in the midline. In most cases the pelvic bones must be broken (pelvic osteotomy) to allow the pubic rami to be brought together and create a pubic symphysis to support the bladder closure. Early bladder closure can be performed in almost all neonates with classic bladder exstrophy. Treatment should be deferred in selected situations when surgical therapy would be excessively risky or complex, such as in a premature baby or when it would have to be performed by inexperienced surgeons. In the staged approach, in boys, epispadias repair usually is performed at 1-2 yr of age. At this point the child has total urinary incontinence because there is no functional external urinary sphincter. At 3-6 yr, if the bladder is sufficiently large, bladder neck reconstruction is performed to try to create a functional sphincter.
Total single-stage reconstruction includes closure of the bladder, closure of the abdominal wall, and, in boys, correction of epispadias using a technique of penile disassembly, in which the 2 corpora cavernosa and the midline urethra are mobilized separately into 3 parts. Postoperatively, the infant’s upper urinary tract is monitored closely for the possible development of hydronephrosis and infection. Most infants with bladder exstrophy have vesicoureteral reflux and should receive antibiotic prophylaxis. The final stage of reconstruction involves creation of a sphincter muscle for bladder control and correction of the vesicoureteral reflux. At this point the child is 3-6 yr old, the bladder capacity should be at least 80-90 mL, and the child must have gained rectal control. Typically, bladder capacity is monitored every 12-24 mo using cystoscopy under anesthesia.
At puberty, often the pubic hair is distributed to the sides of the external genitals. A monsplasty can performed to provide a normal escutcheon.
Long-Term Prognosis
This plan of treatment has yielded a continence rate of 60-70% in a few centers, with <15% deterioration of the upper urinary tract. This continence rate reflects not only the successful reconstruction but also the quality and size of the bladder. The reconstructed bladder neck does not relax during voiding as in a normal child; instead the patient must void by Valsalva. Children who undergo reconstructive surgery as newborns have a greater chance of obtaining a normally functioning bladder.
Children who remain incontinent for more than 1 yr after bladder neck reconstruction or those who are not eligible for bladder neck reconstruction because of a small bladder capacity are candidates for an alternative reconstructive procedure to achieve dryness. In selected cases, cystoscopic injection of dextranomer or polydimethylsiloxane microspheres into the bladder neck can provide sufficient bladder neck coaptation to establish continence. Alternatively, if the child is not a candidate for endoscopic therapy, options include:
Ureterosigmoidostomy carries a significant risk of chronic pyelonephritis, upper urinary tract damage, metabolic acidosis resulting from absorption of hydrogen ion and chloride in the intestine, and at least a 15% long-term risk of colon carcinoma. Patients from less-developed countries often undergo the Mainz II procedure because the continence rate is high and pyelonephritis and upper tract changes are uncommon.
Late follow-up has shown that although men with exstrophy have a penis that is half normal length, they usually experience satisfactory sexual function. Fertility has been low, possibly because of iatrogenic injury to the secondary sexual organs during reconstruction. With artificial reproductive technology, nearly all men can be fertile. In women, fertility is not affected, but uterine prolapse during pregnancy is a problem. In women who have undergone a continent urinary diversion, delivery by cesarean section may be necessary.
Other Exstrophy Anomalies
Children with more complex cases of cloacal exstrophy, which has an incidence of 1/400,000, have an omphalocele and severe abnormalities of the colon and the rectum and often have short bowel syndrome, the most devastating anomaly managed by pediatric urologists. Approximately 50% of patients have an upper urinary tract anomaly, and 50% have spina bifida. Children with cloacal exstrophy do not achieve normal urine or stool continence. Reconstructive techniques result in a satisfactory outcome in most patients with permanent urinary diversion (either ileal conduit or continent urinary diversion) and a colostomy. Because the penis in boys with cloacal exstrophy usually is diminutive, genital reconstruction in boys with cloacal exstrophy has been unsatisfactory. Previously, most specialists recommended assigning a female gender to such infants, but currently there is debate whether these children, who have a 46,XY karyotype and androgen imprinting in utero, can have a satisfactory female gender identity. Many assume male gender characteristics by adolescence. Decisions regarding gender assignment should be made jointly by the physicians caring for the infant (surgical team, pediatric endocrinologist, child psychiatrist, and ethicist) and family.
Epispadias is in the spectrum of exstrophy anomalies, affecting approximately 1/117,000 boys and 1/480,000 girls. In boys, the diagnosis is obvious because the prepuce is distributed primarily on the ventral aspect of the penile shaft and the urethral meatus is on the dorsum of the penis. Distal epispadias in boys usually is associated with normal urinary control and normal upper urinary tracts and should be repaired by 6-12 mo of age. In girls, the clitoris is bifid and the urethra is split dorsally (Fig. 535-2). In more severely affected boys and in all girls with epispadias, there is total urinary incontinence because the sphincter is incompletely formed, and there is wide separation of the pubic rami. These children require surgical reconstruction of the bladder neck, similar to the final management stage in children with classic bladder exstrophy.
Bladder Diverticula
Bladder diverticula develop as herniations of bladder mucosa between defects of bladder smooth muscle fibers. Primary bladder diverticula usually develop at the ureterovesical junction and may be associated with vesicoureteral reflux, because the diverticulum interferes with the normal flap-valve attachment between the ureter and bladder. In rare circumstances the diverticulum is so large that it interferes with normal micturition by obstructing the bladder neck. Bladder diverticula also commonly are associated with distal urethral obstruction such as posterior urethral valves or neurogenic bladder dysfunction. They occur commonly in children with connective tissue disorders including Williams syndrome, Ehlers-Danlos syndrome, and Menkes syndrome (Fig. 535-3). Small diverticula require no treatment other than that of the primary disease, whereas large diverticula can contribute to inefficient voiding, residual urine, urinary stasis, and urinary tract infections and should be excised.
Urachal Anomalies
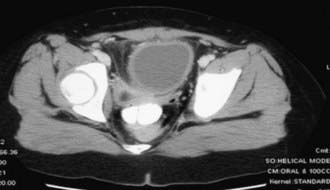
The urachus is an embryologic canal connecting the dome of the fetal bladder with the allantois, a structure that contributes to the formation of the umbilical cord. The lumen of the urachus is normally obliterated during embryonic development, transforming the urachus into a solid cord. Urachal abnormalities are more common in boys than in girls. A patent urachus can occur as an isolated anomaly; it may be associated with prune-belly syndrome or posterior urethral valves (Chapter 534). In this condition there is continuous urinary drainage from the umbilicus. The tract should be excised. Another urachal anomaly is the urachal cyst, which can become infected. Typical symptoms and physical findings include suprapubic pain, fever, irritative voiding symptoms, and an infraumbilical mass, which can be erythematous. Diagnosis is made by ultrasonography or CT (Fig. 535-4). Treatment is intravenous antibiotic therapy and drainage and excision. Other urachal anomalies include the vesicourachal diverticulum, which is a diverticulum of the bladder dome, and umbilical-urachal sinus, which is a blind external sinus that opens at the umbilicus. These lesions should be excised.
Ashley RA, Inman BA, Routh JC. Urachal anomalies: a longitudinal study of urachal remnants in children and adults. J Urol. 2007;178:1615-1618.
Frimberger D, Kropp BP. Bladder anomalies in children. In: Wein AJ, Kavoussi LR, Novick AC, et al, editors. Campbell-Walsh urology. ed 9. Philadelphia: Elsevier; 2007:3573-3582.
Galati V, Donovan B, Ramji F, et al. Management of urachal remnants in early childhood. J Urol. 2008;180:1824-1826.
Gambhir L, Höller T, Müller M, et al. Epidemiological survey of 214 families with bladder exstrophy–epispadias complex. J Urol. 2008;179:1539-1543.
Gargollo PC, Borer JG, Diamond DA, et al. Prospective followup in patients after complete primary repair of bladder exstrophy. J Urol. 2008;180:1665-1670.
Gearhart JP, Mathews R. Exstrophy-epispadias complex. In: Wein AJ, Kavoussi LR, Novick AC, et al, editors. Campbell-Walsh urology. ed 9. Philadelphia: Elsevier; 2007:3497-3553.
Jarzebowski AC, McMullin ND, Grover SR, et al. The Kelly technique of bladder exstrophy repair: continence, cosmesis and pelvic organ prolapse outcomes. J Urol. 2009;182:1802-1806.
Mednick L, Gargollo P, Oliva M, et al. Stress and coping of parents of young children diagnosed with bladder exstrophy. J Urol. 2009;181:1312-1316.
Schaeffer AJ, Purvers JT, King JA, et al. Complications of primary closure of classic bladder exstrophy. J Urol. 2008;180:1671-1674.
Wood HM, Babineau D, Gearhart JP. In vitro fertilization and the cloacal/bladder exstrophy–epispadias complex: a continuing association. J Pediatr Urol. 2007;3:305-310.