Chapter 570 Congenital Adrenal Hyperplasia and Related Disorders
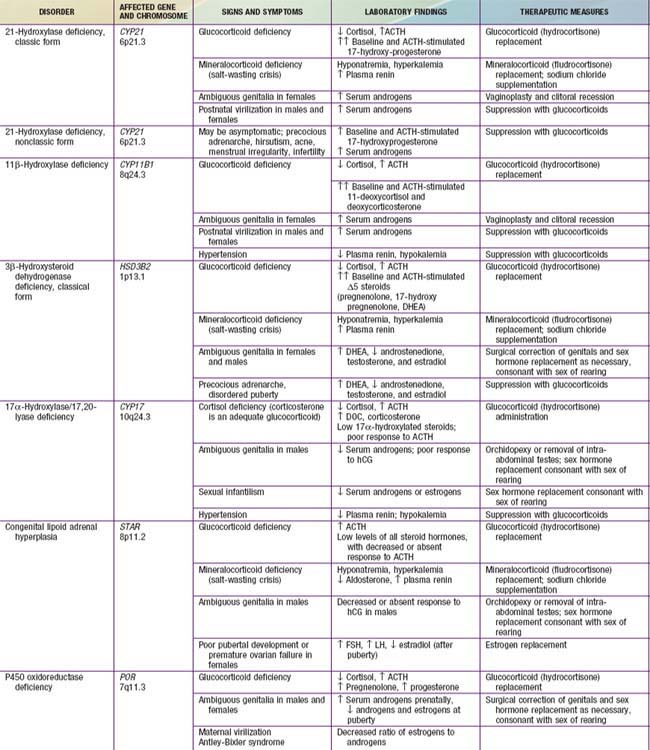
Congenital adrenal hyperplasia (CAH) is a family of autosomal recessive disorders of cortisol biosynthesis (normal adrenal steroidogenesis is discussed in Chapter 568). Cortisol deficiency increases secretion of corticotropin (ACTH), which in turn leads to adrenocortical hyperplasia and overproduction of intermediate metabolites. Depending on the enzymatic step that is deficient, there may be signs, symptoms, and laboratory findings of mineralocorticoid deficiency or excess; incomplete virilization or premature puberty in affected males; and virilization or sexual infantilism in affected females (Figs. 570-1 and 570-2 and Table 570-1).

Figure 570-1 A, A 6-yr-old girl with congenital virilizing adrenal hyperplasia. The height age was 8.5 yr, and the bone age was 13 yr. B, Notice the clitoral enlargement and labial fusion. C, Her 5-yr-old brother was not considered to be abnormal by the parents. The height age was 8 yr, and the bone age was 12.5 yr.
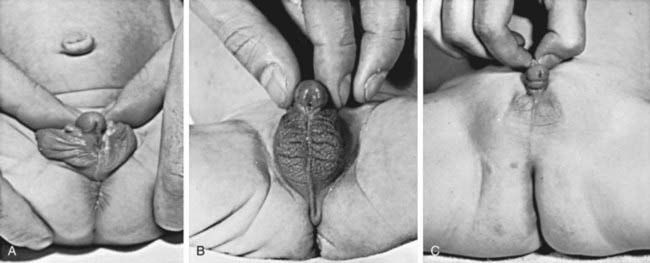
Figure 570-2 Three virilized females with untreated congenital adrenal hyperplasia. All were erroneously assigned male sex at birth, and each had a normal female sex-chromosome complement. Infants A and B had the salt-wasting form and received the diagnosis early in infancy. Infant C was referred at 1 yr of age because of bilateral cryptorchidism. Notice the completely penile urethra; such complete masculinization in females with adrenal hyperplasia is rare; most of these infants have the salt-wasting form.
570.1 Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency
Etiology
More than 90% of congenital adrenal hyperplasia (CAH) cases are caused by 21-hydroxylase deficiency. This P450 enzyme (CYP21, P450c21) hydroxylates progesterone and 17-hydroxyprogesterone (17-OHP) to yield 11-deoxycorticosterone (DOC) and 11-deoxycortisol, respectively (see Fig. 568-1). These conversions are required for synthesis of aldosterone and cortisol, respectively. Both hormones are deficient in the most severe, “salt-wasting” form of the disease. Slightly less severely affected patients are able to synthesize adequate amounts of aldosterone but have elevated levels of androgens of adrenal origin; this is termed simple virilizing disease. These 2 forms are collectively termed classical 21-hydroxylase deficiency. Patients with nonclassical disease have relatively mildly elevated levels of androgens and may have signs of androgen excess after birth.
Epidemiology
Classical 21-hydroxylase deficiency occurs in about 1 in 15,000-20,000 births in most populations. Approximately 70% of affected infants have the salt-losing form, whereas 30% have the simple virilizing form of the disorder. In the USA, CAH is less common in African-Americans compared with white children (1 : 42,000 vs 1 : 15,500). Nonclassical disease has a prevalence of about 1 in 1,000 in the general population but occurs more frequently in specific ethnic groups such as Ashkenazi Jews and Hispanics.
Genetics
There are 2 steroid 21-hydroxylase genes—CYP21P (CYP21A1P, CYP21A) and CYP21 (CYP21A2, CYP21B)—which alternate in tandem with 2 genes for the 4th component of complement (C4A and C4B) in the human leukocyte antigen (HLA) major histocompatibility complex on chromosome 6p21.3 between the HLA-B and HLA-DR loci. Many other genes are located in this cluster. CYP21 is the active gene; CYP21P is 98% identical in DNA sequence to CYP21 but is a pseudogene due to 9 different mutations. More than 90% of mutations causing 21-hydroxylase deficiency are recombinations between CYP21 and CYP21P. Approximately 20% are deletions generated by unequal meiotic crossing-over between CYP21 and CYP21P, whereas the remainder is nonreciprocal transfers of deleterious mutations from CYP21P to CYP21, a phenomenon termed gene conversion.
The deleterious mutations in CYP21P have different effects on enzymatic activity when transferred to CYP21. Several mutations completely prevent synthesis of a functional protein, whereas others are missense mutations (they result in amino acid substitutions) that yield enzymes with 1-50% of normal activity. Disease severity correlates well with the mutations carried by an affected individual; for example, patients with salt-wasting disease usually carry mutations on both alleles that completely destroy enzymatic activity. Patients are frequently compound heterozygotes for different types of mutations (i.e., 1 allele is less severely affected than the other), in which case the severity of disease expression is largely determined by the activity of the less severely affected of the 2 alleles.
Pathogenesis and Clinical Manifestations
Aldosterone and Cortisol Deficiency
Because both cortisol and aldosterone require 21-hydroxylation for their synthesis, both hormones are deficient in the most severe, salt-wasting form of the disease. This form constitutes about 70% of cases of classical 21-hydroxylase deficiency. The signs and symptoms of cortisol and aldosterone deficiency, and the pathophysiology underlying them, are essentially those described in Chapter 569. These include progressive weight loss, anorexia, vomiting, dehydration, weakness, hypotension, hypoglycemia, hyponatremia, and hyperkalemia. These problems typically 1st develop in affected infants at approximately 10-14 days of age. Without treatment, shock, cardiac arrhythmias, and death may occur within days or weeks.
CAH differs from other causes of primary adrenal insufficiency in that precursor steroids accumulate proximal to the blocked enzymatic conversion. Because cortisol is not synthesized efficiently, ACTH levels are high, leading to hyperplasia of the adrenal cortex and levels of precursor steroids that may be hundreds of times normal. In the case of 21-hydroxylase deficiency, these precursors include 17-hydroxyprogesterone and progesterone. Progesterone and perhaps other metabolites act as antagonists of the mineralocorticoid receptor and thus may exacerbate the effects of aldosterone deficiency in untreated patients.
Prenatal Androgen Excess
The most important problem caused by accumulation of steroid precursors is that 17-hydroxyprogesterone is shunted into the pathway for androgen biosynthesis, leading to high levels of androstenedione that are converted outside the adrenal gland to testosterone. This problem begins in affected fetuses by 8-10 wk of gestation and leads to abnormal genital development in females (see Figs. 570-1 and 570-2).
The external genitals of males and females normally appear identical early in gestation (Chapter 576). Affected females, who are exposed in utero to high levels of androgens of adrenal origin, have masculinized external genitalia (see Figs. 570-1 and 570-2). This is manifested by enlargement of the clitoris and by partial or complete labial fusion. The vagina usually has a common opening with the urethra (urogenital sinus). The clitoris may be so enlarged that it resembles a penis; because the urethra opens below this organ, some affected females may be mistakenly presumed to be males with hypospadias and cryptorchidism. The severity of virilization is usually greatest in females with the salt-losing form of 21-hydroxylase deficiency. The internal genital organs are normal, because affected females have normal ovaries and not testes and thus do not secrete antimüllerian hormone.
Prenatal exposure of the brain to high levels of androgens may influence subsequent sexually dimorphic behaviors in affected females. Girls tend to be interested in masculine toys such as cars and trucks and often show decreased interest in playing with dolls and demonstrate aggressive play behavior. Women may have decreased interest in maternal roles. There is an increased frequency of homosexuality in affected females. Nonetheless, most function heterosexually and do not have gender identity confusion or dysphoria. It is unusual for affected females to assign themselves a male role.
Male infants appear normal at birth. Thus, the diagnosis may not be made in boys until signs of adrenal insufficiency develop. Because patients with this condition can deteriorate quickly, infant boys are more likely to die than infant girls. For this reason, many states and countries have instituted newborn screening for this condition (see Newborn Screening, later).
Postnatal Androgen Excess
Untreated or inadequately treated children of both sexes develop additional signs of androgen excess after birth. Boys with the simple virilizing form of 21-hydroxylase deficiency often have delayed diagnosis because they appear normal and rarely develop adrenal insufficiency.
Signs of androgen excess include rapid somatic growth and accelerated skeletal maturation. Thus, affected patients are tall in childhood but premature closure of the epiphyses causes growth to stop relatively early, and adult stature is stunted (see Fig. 570-1). Muscular development may be excessive. Pubic and axillary hair may appear; and acne and a deep voice may develop. The penis, scrotum, and prostate may become enlarged in affected boys; however, the testes are usually prepubertal in size so that they appear relatively small in contrast to the enlarged penis. Occasionally, ectopic adrenocortical cells in the testes of patients become hyperplastic similarly to the adrenal glands, producing testicular adrenal rest tumors (Chapter 578). The clitoris may become further enlarged in affected females (see Fig. 570-1). Although the internal genital structures are female, breast development and menstruation may not occur unless the excessive production of androgens is suppressed by adequate treatment.
Similar but usually milder signs of androgen excess may occur in nonclassical 21-hydroxylase deficiency. In this attenuated form, cortisol and aldosterone levels are normal and affected females have normal genitals at birth. Males and females may present with precocious pubarche and early development of pubic and axillary hair. Hirsutism, acne, menstrual disorders, and infertility may develop later in life. However, many females and males are completely asymptomatic.
Adrenomedullary Dysfunction
Development of the adrenal medulla requires exposure to the extremely high cortisol levels normally present within the adrenal gland. Thus patients with classic CAH have abnormal adrenomedullary function, as evidenced by blunted epinephrine responses, decreased blood glucose and lower heart rates with exercise. Ability to exercise is unimpaired and the clinical significance of these findings is uncertain. Adrenomedullary dysfunction may exacerbate the cardiovascular effects of cortisol deficiency in untreated or undertreated patients.
Laboratory Findings (See Table 570-1)
Patients with salt-losing disease have typical laboratory findings associated with cortisol and aldosterone deficiency, including hyponatremia, hyperkalemia, metabolic acidosis, and often hypoglycemia, but these abnormalities can take 10-14 days or longer to develop after birth. Blood levels of 17-hydroxyprogesterone are markedly elevated. However, levels of this hormone are high during the 1st 2-3 days of life, even in unaffected infants and especially if they are sick or premature. After infancy, once the circadian rhythm of cortisol is established, 17-hydroxyprogesterone levels vary in the same circadian pattern, being highest in the morning and lowest at night. Blood levels of cortisol are usually low in patients with the salt-losing type of disease. They are often normal in patients with simple virilizing disease but inappropriately low in relation to the ACTH and 17-hydroxyprogesterone levels. In addition to 17-hydroxyprogesterone, levels of androstenedione and testosterone are elevated in affected females; testosterone is not elevated in affected males because normal infant males have high testosterone levels compared with those seen later in childhood. Levels of urinary 17-ketosteroids and pregnanetriol are elevated but are now rarely used clinically because blood samples are easier to obtain than 24-hr urine collections. ACTH levels are elevated but have no diagnostic utility over 17-hydroxyprogesterone levels. Plasma levels of renin are elevated, and serum aldosterone is inappropriately low for the renin level. However, renin levels are high in normal infants in the 1st few weeks of life.
Diagnosis of 21-hydroxylase deficiency is most reliably established by measuring 17-hydroxyprogesterone before and 30 or 60 min after an intravenous bolus of 0.125-0.25 mg of cosyntropin (ACTH 1-24). Nomograms exist that readily distinguish normals and patients with nonclassical and classical 21-hydroxylase deficiency. Heterozygous carriers of this autosomal recessive disorder tend to have higher ACTH-stimulated 17-hydroxyprogesterone levels than genetically unaffected individuals, but there is significant overlap between subjects in these 2 categories. However, in infants with frank electrolyte abnormalities or circulatory instability, it may not be possible or necessary to delay treatment to perform this test, as levels of precursors will be sufficiently elevated on a random blood sample to make the diagnosis.
Differential Diagnosis
Intersex conditions are discussed more generally in Chapter 582. The initial step in evaluating an infant with ambiguous genitals is a thorough physical examination to define the anatomy of the genitals, locate the urethral meatus, palpate the scrotum or labia and the inguinal regions for testes (palpable gonads almost always indicate the presence of testicular tissue and thus that the infant is a genetic male), and look for any other anatomic abnormalities. Ultrasonography is helpful in demonstrating the presence or absence of a uterus and can often locate the gonads. A rapid karyotype (such as fluorescence in situ hybridization of interphase nuclei for X and Y chromosomes) can quickly determine the genetic sex of the infant. These results are all likely to be available before the results of hormonal testing and together allow the clinical team to advise the parents as to the genetic sex of the infant and the anatomy of internal reproductive structures. Injection of contrast medium into the urogenital sinus of female pseudohermaphrodites demonstrates a vagina and uterus, and most surgeons utilize this information to formulate a plan for surgical management.
Prenatal Diagnosis
Prenatal diagnosis of 21-hydroxylase is possible late in the 1st trimester by analysis of DNA obtained by chorionic villus sampling or during the 2nd trimester by amniocentesis. This is usually done because the parents already have an affected child. Most often, the CYP21 gene is analyzed for frequently occurring mutations; more rare mutations may be detected by DNA sequencing.
Newborn Screening
Because 21-hydroxylase deficiency is often undiagnosed in affected males until they have severe adrenal insufficiency, all states in the USA and many other countries have instituted newborn screening programs. These programs analyze 17-hydroxyprogesterone levels in dried blood obtained by heel-stick and absorbed on filter paper cards; the same cards are screened in parallel for other congenital conditions such as hypothyroidism and phenylketonuria. Potentially affected infants are typically quickly recalled for additional testing (electrolytes and repeat 17-hydroxyprogesterone determination) at approximately 2 wk of age. Infants with salt-wasting disease often have abnormal electrolytes by this age but are usually not severely ill. Thus, screening programs are effective in preventing many cases of adrenal crisis in affected males. The nonclassical form of the disease is not reliably detected by newborn screening, but this is of little clinical significance because adrenal insufficiency does not occur in this type of 21-hydroxylase deficiency.
The main difficulty with current newborn screening programs is that to reliably detect all affected infants, the cutoff 17-hydroxyprogesterone levels for recalls are set so low that there is a very high frequency of false-positive results (i.e., the test has a low positive predictive value of approximately 1%). This problem is worst in premature infants. Positive predictive value can be improved by using cutoff levels based on gestational age, and by utilizing more specific 2nd-tier screening methods such as liquid chromatography followed by tandem mass spectrometry (LC-MS/MS).
Treatment
Glucocorticoid Replacement
Cortisol deficiency is treated with glucocorticoids. Treatment also suppresses excessive production of androgens by the adrenal cortex and thus minimizes problems such as excessive growth and skeletal maturation and virilization. This often requires larger glucocorticoid doses than are needed in other forms of adrenal insufficiency, typically 15-20 mg/m2/24 hr of hydrocortisone daily administered orally in 3 divided doses. Affected infants usually require dosing at the high end of this range. Double or triple doses are indicated during periods of stress, such as infection or surgery. Glucocorticoid treatment must be continued indefinitely in all patients with classical 21-hydroxylase deficiency but may not be necessary in patients with nonclassical disease unless signs of androgen excess are present. Therapy must be individualized. It is desirable to maintain linear growth along percentile lines; crossing to higher height percentiles may suggest undertreatment, whereas loss of height percentiles often indicates overtreatment with glucocorticoids. Overtreatment is also suggested by excessive weight gain. Pubertal development should be monitored by periodic examination, and skeletal maturation is evaluated by serial radiographs of the hand and wrist for bone age. Hormone levels, particularly 17-hydroxyprogesterone and androstenedione, should be measured early in the morning, before taking the morning medications, or at a consistent time in relation to medication dosing. In general, desirable 17-hydroxyprogesterone levels are in the high-normal range or several times normal; low-normal levels can usually be achieved only with excessive glucocorticoid doses.
Menarche occurs at the appropriate age in most girls in whom good control has been achieved; it may be delayed in girls with suboptimal control.
Children with simple virilizing disease, particularly males, are frequently not diagnosed until 3-7 yr of age, at which time skeletal maturation may be 5 yr or more in advance of chronological age. In some children, especially if the bone age is 12 yr or more, spontaneous gonadotropin-dependent puberty may occur when treatment is instituted, because therapy with hydrocortisone has suppressed production of adrenal androgens and stimulated release of pituitary gonadotropins if the appropriate level of hypothalamic maturation is present. This form of superimposed true precocious puberty may be treated with a gonadotropin hormone-releasing hormone analog such as leuprolide.
Males with 21-hydroxylase deficiency who have had inadequate corticosteroid therapy may develop adrenal rest testicular tumors, which usually regress with increased steroid dosage. Testicular MRI, ultrasonography, and color flow Doppler examination help define the character and extent of disease. Testis-sparing surgery for steroid-unresponsive tumors has been reported.
Mineralocorticoid Replacement
Patients with salt-wasting disease (i.e., aldosterone deficiency) require mineralocorticoid replacement with fludrocortisone. Infants may have very high mineralocorticoid requirements in the 1st few mo of life, usually 0.1-0.3 mg daily in 2 divided doses but occasionally up to 0.4 mg daily, and often require sodium supplementation (sodium chloride, 8 mmol/kg) in addition to the mineralocorticoid. Older infants and children are usually maintained with 0.05-0.1 mg daily of fludrocortisone. In some patients, simple virilizing disease may be easier to control with a low dose of fludrocortisone in addition to hydrocortisone even when these patients have normal aldosterone levels in the absence of mineralocorticoid replacement. Therapy is evaluated by monitoring of vital signs; tachycardia and hypertension are signs of overtreatment with mineralocorticoids. Serum electrolytes should be measured frequently in early infancy as therapy is adjusted. Plasma renin activity is a useful way to determine adequacy of therapy; it should be maintained in or near the normal range but not suppressed.
Additional approaches to improve outcome have been proposed but have not yet become the standard of care. These include an antiandrogen such as flutamide to block the effects of excessive androgen levels, and/or an aromatase inhibitor such as anastrozole, which blocks conversion of androgens to estrogen and thus retards skeletal maturation, a process that is sensitive to estrogens in both boys and girls. Aromatase inhibitors generally should not be used in pubertal girls because they will obviously retard normal puberty and may expose the ovaries to excessive levels of gonadotropins. Growth hormone, with or without LHRH agonists to retard skeletal maturation, has been suggested to improve adult height.
Surgical Management of Ambiguous Genitals
Significantly virilized females usually undergo surgery between 2-6 mo of age. If there is severe clitoromegaly, the clitoris is reduced in size, with partial excision of the corporal bodies and preservation of the neurovascular bundle; however, moderate clitoromegaly may become much less noticeable even without surgery as the patient grows. Vaginoplasty and correction of the urogenital sinus usually are performed at the time of clitoral surgery; revision in adolescence is often necessary.
Risks and benefits of surgery should be fully discussed with parents of affected females. There is limited long-term follow-up of functional outcomes in patients who have undergone modern surgical procedures, although it appears that there is frequent sexual dysfunction that increases in frequency and severity with the initial degree of genital virilization. Sex assignment of infants with disorders of sexual differentiation (including CAH) is usually based on expected sexual functioning and fertility in adulthood with early surgical correction of the external genitals to conform with the sex assignment. Confused psychosexual identity is not common with CAH. Lay and medical opponents of this practice for other intersex conditions state that it ignores any prenatally biased gender role predisposition and precludes the patient from having any decision as to his or her own preferred sexual identity and what surgical correction of the genitals should be performed. These individuals and groups say treatment should be aimed primarily at educating patient, family, and others about the medical condition, its treatment, and how to deal with the intersex condition. They propose that surgery should be delayed until the patient decides on what, if any, correction should be performed.
In adolescent and adult females with poorly controlled 21-hydroxylase deficiency (hirsutism, obesity, amenorrhea) bilateral laparoscopic adrenalectomy (with hormone replacement) may be an alternative to standard medical hormone replacement therapy, but patients treated in this way may be more susceptible to acute adrenal insufficiency if treatment is interrupted because the adrenal glands have been removed. Moreover, they may exhibit signs of elevated ACTH levels such as abnormal pigmentation.
Prenatal Treatment
Besides genetic counseling, the main goal of prenatal diagnosis is to facilitate appropriate prenatal treatment of affected females. Mothers with pregnancies at risk are given dexamethasone, a steroid that readily crosses the placenta, in an amount of 20 µg/kg prepregnancy maternal weight daily in 2 or 3 divided doses. This suppresses secretion of steroids by the fetal adrenal, including secretion of adrenal androgens. If started by 6 wk of gestation, it ameliorates virilization of the external genitals in affected females. Chorionic villus biopsy is then performed to determine the sex and genotype of the fetus; therapy is continued only if the fetus is an affected female. DNA analysis of fetal cells isolated from maternal plasma for sex determination and CYP21 gene analysis may permit earlier identification of the affected female fetus. Children exposed to this therapy have slightly lower birthweights. Effects on personality or cognition, such as increased shyness, have been suggested but not consistently observed. At present there is insufficient information to determine whether there are any long-term risks, particularly in the males and unaffected females who derive no direct benefit from the treatment. Maternal side effects of prenatal treatment have included edema, excessive weight gain, hypertension, glucose intolerance, cushingoid facial features, and severe striae. Prenatal treatment is therefore carried out only under institutional protocols in some locales, but it is offered as an option outside the research setting by high-risk obstetricians in other communities.
Berenbaum SA, Korman BK, Duck SC, et al. Psychological adjustment in children and adults with congenital adrenal hyperplasia. J Pediatr. 2004;144:741-746.
Bonfig W, Bechtold S, Schmidt H, et al. Reduced final height outcome in congenital adrenal hyperplasia under prednisone treatment: deceleration of growth velocity during puberty. J Clin Endocrinol Metab. 2007;92:1635-1639.
Crouch NS, Liao LM, Woodhouse CR, et al. Sexual function and genital sensitivity following feminizing genitoplasty for congenital adrenal hyperplasia. J Urol. 2008;179:634-638.
Green-Golan L, Yates C, Drinkard B, et al. Patients with classic congenital adrenal hyperplasia have decreased epinephrine reserve and defective glycemic control during prolonged moderate-intensity exercise. J Clin Endocrinol Metab. 2007;92:3019-3024.
Hagenfeldt K, Janson PO, Holmdahl G, et al. Fertility and pregnancy outcome in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Reprod. 2008;23:1607-1613.
Lajic S, Nordenstrom A, Hirvikoski T. Long-term outcome of prenatal treatment of congenital adrenal hyperplasia. Endocr Dev. 2008;13:82-98.
Merke DP, Bornstein SR. Congenital adrenal hyperplasia. Lancet. 2005;365:2125-2136.
Meyer-Bahlburg HF, Dolezal C, Baker SW, et al. Sexual orientation in women with classical or non-classical congenital adrenal hyperplasia as a function of degree of prenatal androgen excess. Arch Sex Behav. 2008;37:85-99.
Nimkarn S, New MI. Prenatal diagnosis and treatment of congenital adrenal hyperplasia owing to 21-hydroxylase deficiency. Nat Clin Pract Endocrinol Metab. 2007;3:405-413.
Speiser PW, Azziz R, Baskin LS, et al. Congenital adrenal hyperplasia due to steroid 21-hydooxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:4133-4160.
Speiser PW, White PC. Congenital adrenal hyperplasia. N Engl J Med. 2003;349:776-788.
White PC: Newborn screening for congenital adrenal hyperplasia owing to steroid 21-hydroxylase deficiency, Nat Clin Pract Endocrinol Metab in press
570.2 Congenital Adrenal Hyperplasia Due to 11β-Hydroxylase Deficiency
Etiology
Deficiency of 11β-hydroxylase is due to a mutation in the CYP11B1 gene located on chromosome 8q24. CYP11B1 mediates 11-hydroxylation of 11-deoxycortisol to cortisol. Because 11-deoxycortisol is not converted to cortisol, levels of corticotropin are high. In consequence, precursors—particularly 11-deoxycortisol and deoxycorticosterone—accumulate and are shunted into androgen biosynthesis in the same manner as occurs in 21-hydroxylase deficiency. The adjacent CYP11B2 gene encoding aldosterone synthase is generally unaffected in this disorder, so patients are able to synthesize aldosterone normally.
Epidemiology
11β-Hydroxylase deficiency accounts for approximately 5% of cases of adrenal hyperplasia; its incidence has been estimated as 1/250,000 to 1/100,000. More than 30 different mutations in CYP11B1 have been identified. The disorder occurs relatively frequently in Israeli Jews of North African origin (1 in 15,000-17,000 live births); in this ethnic group almost all alleles carry an Arg448 to His (R448H) mutation. This disorder presents in a classical, severe form and very rarely in a nonclassical, milder form.
Clinical Manifestations
Although cortisol is not synthesized efficiently, aldosterone synthetic capacity is normal, and some corticosterone is synthesized from progesterone by the intact aldosterone synthase enzyme. Thus, it is unusual for patients to manifest signs of adrenal insufficiency such as hypotension, hypoglycemia, hyponatremia, and hyperkalemia. Approximately 65% of patients become hypertensive, although this can take several years to develop. Hypertension is probably a consequence of elevated levels of deoxycorticosterone, which has mineralocorticoid activity. Infants may transiently develop signs of mineralocorticoid deficiency after treatment with hydrocortisone is instituted. This is presumably due to sudden suppression of deoxycorticosterone secretion in a patient with atrophy of the zona glomerulosa caused by chronic suppression of renin activity.
All signs and symptoms of androgen excess that are found in 21-hydroxylase deficiency may also occur in 11-hydroxylase deficiency.
Laboratory Findings
Plasma levels of 11-deoxycortisol and deoxycorticosterone are elevated. Because deoxycorticosterone and metabolites have mineralocorticoid activity, plasma renin activity is suppressed. Consequently, aldosterone levels are low even though the ability to synthesize aldosterone is intact. Hypokalemic alkalosis occasionally occurs.
Treatment
Patients are treated with hydrocortisone in doses similar to those used for 21-hydroxylase deficiency. Mineralocorticoid replacement is sometimes transiently required in infancy but is rarely necessary otherwise. Hypertension often resolves with glucocorticoid treatment but may require additional therapy if it is of long standing. Calcium channel blockers may be beneficial under these circumstances.
Peter M. Congenital adrenal hyperplasia: 11beta-hydroxylase deficiency. Semin Reprod Med. 2002;20:249-254.
White PC. Steroid 11 beta-hydroxylase deficiency and related disorders. Endocrinol Metab Clin North Am. 2001;30:61-79.
Zhao LQ, Han S, Tian HM. Progress in molecular-genetic studies on congenital adrenal hyperplasia due to 11beta-hydroxylase deficiency. World J Pediatr. 2008;4:85-90.
570.3 Congenital Adrenal Hyperplasia Due to 3β-Hydroxysteroid Dehydrogenase Deficiency
Etiology
Deficiency of 3β-hydroxysteroid dehydrogenase (3β-HSD) occurs in fewer than 2% of patients with adrenal hyperplasia. This enzyme is required for conversion of Δ5 steroids (pregnenolone, 17-hydroxypregnenolone, dehydroepiandrosterone [DHEA]) to Δ4 steroids (progesterone, 17-hydroxyprogesterone, and androstenedione). Thus, deficiency of the enzyme results in decreased synthesis of cortisol, aldosterone, and androstenedione but increased secretion of DHEA (see Fig. 568-1). The 3β-HSD enzyme expressed in the adrenal cortex and gonad is encoded by the HSD3B2 gene located on chromosome 1p13.1. Over 30 mutations in the HSD3B2 gene have been described in patients with 3β-HSD deficiency.
Clinical Manifestations
Because cortisol and aldosterone are not synthesized in patients with the classical form of the disease, infants are prone to salt-wasting crises. Because androstenedione and testosterone are not synthesized, boys are incompletely virilized. Varying degrees of hypospadias may occur, with or without bifid scrotum or cryptorchidism. Because DHEA levels are elevated and this hormone is a weak androgen, girls are mildly virilized, with slight to moderate clitoral enlargement. Postnatally, continued excessive DHEA secretion can cause precocious adrenarche. During adolescence and adulthood, hirsutism, irregular menses, and polycystic ovarian disease occur in females. Males manifest variable degrees of hypogonadism, although appropriate male secondary sexual development may occur. A persistent defect of testicular 3β-HSD is demonstrated, however, by the high Δ5 to Δ4 steroid ratio in testicular effluent.
Laboratory Findings
The hallmark of this disorder is the marked elevation of the Δ5 steroids (such as 17-hydroxypregnenolone and DHEA) preceding the enzymatic block. Patients may also have elevated levels of 17-hydroxyprogesterone because of the extra-adrenal 3β-HSD activity that occurs in peripheral tissues; these patients may be mistaken for patients with 21-hydroxylase deficiency. The ratio of 17-hydroxypregnenolone to 17-hydroxyprogesterone is markedly elevated in 3β-HSD deficiency, in contrast to the decreased ratio in 21-hydroxylase deficiency. Plasma renin activity is elevated in the salt-wasting form.
Differential Diagnosis
It is not unusual for children with premature adrenarche, or women with signs of androgen excess, to have mild to moderate elevations in DHEA levels. It has been suggested that such individuals have “nonclassical 3β-HSD deficiency.” Mutations in the HSD3B2 gene are usually not found in such individuals, and a nonclassical form of this deficiency must actually be quite rare. The activity of 3β-HSD in the adrenal zonae fasciculata and reticularis, relative to CYP17 (17-hydroxylase/17,20-lyase) activity, normally decreases during adrenarche to facilitate DHEA synthesis, and so modest elevations in DHEA in preteenage children or women usually represent a normal variant.
Treatment
Patients require glucocorticoid and mineralocorticoid replacement with hydrocortisone and fludrocortisone, respectively, as in 21-hydroxylase deficiency. Incompletely virilized genetic males in whom a male sex of rearing is contemplated may benefit from several injections of a depot form of testosterone early in infancy to increase the size of the phallus. They may also require testosterone replacement at puberty.
Simard J, Moisan AM, Morel Y. Congenital adrenal hyperplasia due to 3beta-hydroxysteroid dehydrogenase/delta(5)-delta(4) isomerase deficiency. Semin Reprod Med. 2002;20:255-276.
Simard J, Ricketts ML, Gingras S, et al. Molecular biology of the 3beta-hydroxysteroid dehydrogenase/delta5-delta4 isomerase gene family. Endocr Rev. 2005;26:525-582.
570.4 Congenital Adrenal Hyperplasia Due to 17-Hydroxylase Deficiency
Etiology
Less than 1% of CAH cases are caused by 17-hydroxylase deficiency. A single polypeptide, CYP17, catalyzes 2 distinct reactions: 17-hydroxylation of pregnenolone and progesterone to 17-hydroxypregnenolone and 17-hydroxyprogesterone, respectively, and the 17,20-lyase reaction mediating conversion of 17-hydroxypregnenolone to DHEA and, to a lesser extent, 17-hydroxyprogesterone to Δ4-androstenedione. DHEA and androstenedione are steroid precursors of testosterone and estrogen (see Fig. 568-1). The enzyme is expressed in both the adrenal cortex and the gonads and is encoded by a gene on chromosome 10q24.3. Most mutations affect both the hydroxylase and lyase activities, but rare mutations can affect either activity alone.
Clinical Manifestations and Laboratory Findings
Patients with 17-hydroxylase deficiency cannot synthesize cortisol, but their ability to synthesize corticosterone is intact. Because corticosterone is an active glucocorticoid, patients do not develop adrenal insufficiency. Deoxycorticosterone, the immediate precursor of corticosterone, is synthesized in excess. This can cause hypertension, hypokalemia, and suppression of renin and aldosterone secretion, as occurs in 11-hydroxylase deficiency. In contrast to 11-hydroxylase deficiency, patients with 17-hydroxylase deficiency are unable to synthesize sex hormones. Affected males are incompletely virilized and present as phenotypic females (but gonads are usually palpable in the inguinal region or the labia) or with sexual ambiguity (male pseudohermaphroditism). Affected females usually present with failure of sexual development at the expected time of puberty. 17-Hydroxylase deficiency in females must be considered in the differential diagnosis of primary hypogonadism (Chapter 580). In addition to the increased DOC, suppressed renin and aldosterone, and decreased 17-hydroxylated steroids, cortisol, and sex steroids are unresponsive to stimulation with ACTH and human chorionic gonadotropin, respectively.
Treatment
Patients with 17-hydroxylase deficiency require cortisol replacement to suppress secretion of deoxycorticosterone and thus control hypertension. Additional antihypertensive medication may be required. Females require estrogen replacement at puberty. Genetic males may require either estrogen or androgen supplementation depending on the sex of rearing. Because of the possibility of malignant transformation of abdominal testes with androgen insensitivity syndrome (Chapter 577), genetic males with severe 17-hydroxylase deficiency being reared as females require gonadectomy at or before adolescence.
570.5 Lipoid Adrenal Hyperplasia
Etiology
Lipoid adrenal hyperplasia is a rare disorder, reported in fewer than 100 patients, the majority of whom are Japanese. In this disorder there is marked accumulation of cholesterol and lipids in the adrenal cortex and gonads, associated with severe impairment of all steroidogenesis. Lipoid adrenal hyperplasia is usually caused by mutations in the gene for steroidogenic acute regulatory protein (StAR), a mitochondrial protein that promotes the movement of cholesterol from the outer to the inner mitochondrial membrane. Mutations in the CYP11A1 gene have been reported in 2 patients with lipoid adrenal hyperplasia.
Some cholesterol is able to enter mitochondria even in the absence of StAR, so it might be supposed that this disorder would not completely impair steroid biosynthesis. The accumulation of cholesterol in the cytoplasm is cytotoxic, eventually leading to death of all steroidogenic cells in which StAR is normally expressed. This occurs prenatally in the adrenals and testes. The ovaries do not normally synthesize steroids until puberty, so cholesterol does not accumulate and the ovaries can retain the capacity to synthesize estrogens until adolescence.
Although estrogens synthesized by the placenta are required to maintain pregnancy, the placenta does not require StAR for steroid biosynthesis. Thus, mutations of StAR are not prenatally lethal.
Clinical Manifestations
Patients with lipoid adrenal hyperplasia are usually unable to synthesize any adrenal steroids. Thus, affected infants are likely to be confused with those with adrenal hypoplasia. Salt-losing manifestations are usual, and many infants die in early infancy. Genetic males are unable to synthesize androgens and thus are phenotypically female but with gonads. Genetic females appear normal at birth and may undergo feminization at puberty with menstrual bleeding. They too, progress to hypergonadotropic hypogonadism when accumulated cholesterol kills granulosa (i.e., steroid synthesizing) cells in the ovary.
Laboratory Findings
Adrenal and gonadal steroid hormone levels are low in lipoid adrenal hyperplasia, with a decreased or absent response to stimulation (ACTH, human chorionic gonadotropin). Plasma renin levels are increased.
Imaging studies of the adrenal gland demonstrating massive adrenal enlargement in the newborn help establish the diagnosis of lipoid adrenal hyperplasia.
Treatment
Patients require glucocorticoid and mineralocorticoid replacement. Genetic males are usually assigned a female sex of rearing; thus both genetic males and females require estrogen replacement at the expected age of puberty.
Hiort O, Holterhus PM, Werner R, et al. Homozygous disruption of P450 side-chain cleavage (CYP11A1) is associated with prematurity, complete 46,XY sex reversal, and severe adrenal failure. J Clin Endocrinol Metab. 2005;90:538-541.
Miller WL. StAR search—what we know about how the steroidogenic acute regulatory protein mediates mitochondrial cholesterol import. Mol Endocrinol. 2007;21:589-601.
Stocco DM. Clinical disorders associated with abnormal cholesterol transport: mutations in the steroidogenic acute regulatory protein. Mol Cell Endocrinol. 2002;191:19-25.
570.6 Deficiency of P450 Oxidoreductase (Antley-Bixler Syndrome)
Etiology, Pathogenesis, and Clinical Manifestations
P450 oxidoreductase (POR, gene located on chromosome 7q11.3) is required for the activity of all microsomal cytochrome P450 enzymes (Chapter 568) including the adrenal enzymes CYP17 and CYP21. Thus, complete POR deficiency abolishes all microsomal P450 activity. This is embryonically lethal in mice and presumably in humans as well. Patients with mutations that decrease but do not abolish POR activity have partial deficiencies of 17-hydroxylase and 21-hydroxylase activities in the adrenals. Deficiency of 17-hydroxylase leads to incomplete masculinization in males; 21-hydroxylase deficiency may lead to virilization in females. Additionally, aromatase (CYP19) activity in the placenta is decreased, leading to unopposed action of androgens produced by the fetal adrenal. This exacerbates virilization of female fetuses and may virilize the mother of an affected fetus as well. Although it is puzzling that affected females could be virilized despite a partial deficiency in CYP17 (which is required for androgen biosynthesis), an alternative biosynthetic pathway may be utilized in which 17-hydroxyprogesterone is converted to 5α-pregnane-3α,17α-diol-20-one, a metabolite that is a much better substrate for the 17,20-lyase activity of CYP17 than the usual substrate, 17-hydroxypregnenolone (Chapter 568). The metabolite is then converted in several enzymatic steps to dihydrotestosterone, a potent androgen.
Because many other P450 enzymes are affected, patients often (but not invariably) have other congenital anomalies collectively referred to as Antley-Bixler syndrome. These include craniosynostosis; brachycephaly; frontal bossing; severe midface hypoplasia with proptosis and choanal stenosis or atresia; humeroradial synostosis; medial bowing of ulnas; long, slender fingers with camptodactyly; narrow iliac wings; anterior bowing of femurs; and malformations of the heart and kidneys. Studies of mutant mice suggest that the metabolic defects responsible for these anomalies include defective metabolism of retinoic acid, leading to elevated levels of this teratogenic compound, and deficient biosynthesis of cholesterol.
Epidemiology
The prevalence is not known with certainty. It must be rare compared with 21-hydroxylase deficiency but might occur at similar frequencies to the other forms of CAH.
Laboratory Findings
Serum steroids that are not 17- or 21-hydroxylated are most increased, including pregnenolone and progesterone. 17-Hydroxy, 21-deoxy-steroids are also increased, including 17-hydroxypregnenolone, 17-hydroxyprogesterone, and 21-deoxycortisol. Urinary steroid metabolites may be determined by quantitative mass spectrometry. Metabolites excreted at increased levels include pregnanediol, pregnanetriol, pregnanetriolone, and corticosterone metabolites. Urinary cortisol metabolites are decreased. Genetic analysis demonstrates mutations in the POR gene.
Differential Diagnosis
This disorder must be distinguished from other forms of congenital adrenal hyperplasia, particularly 21-hydroxylase deficiency in females, which is far more common and has similar laboratory findings. Suspicion for POR deficiency may be raised if the mother is virilized or if the associated abnormalities of Antley-Bixler syndrome are present. Conversely, virilization of both the mother and her daughter can result from a luteoma of pregnancy, but in this case postnatal abnormalities of corticosteroid biosynthesis should not be observed. Antley-Bixler syndrome may also occur without abnormalities of steroid hormone biosynthesis, resulting from mutations in the fibroblast growth factor receptor, FGFR2.
Fluck CE, Pandey AV, Huang N, et al. P450 oxidoreductase deficiency—a new form of congenital adrenal hyperplasia. Endocr Dev. 2008;13:67-81.
Huang N, Pandey AV, Agrawal V, et al. Diversity and function of mutations in p450 oxidoreductase in patients with Antley-Bixler syndrome and disordered steroidogenesis. Am J Hum Genet. 2005;76:729-749.
Schmidt K, Hughes C, Chudek JA, et al. Cholesterol metabolism: the main pathway acting downstream of cytochrome P450 oxidoreductase in skeletal development of the limb. Mol Cell Biol. 2009;29:2716-2729.
570.7 Aldosterone Synthase Deficiency
Etiology
This is a rare autosomal recessive disorder in which conversion of corticosterone to aldosterone is impaired; a group of Iranian Jewish patients has been the most thoroughly studied. The majority of cases result from mutations in the CYP11B2 gene coding for aldosterone synthase; however, linkage to CYP11B2 has been excluded in other kindreds. When not due to CYP11B2 mutations, the disorder has been termed familial hyperreninemic hypoaldosteronism type 2; the causative gene or genes have not yet been identified.
Aldosterone synthase mediates the 3 final steps in the synthesis of aldosterone from deoxycorticosterone (11-hydroxylation, 18-hydroxylation, and 18-oxidation). Although 11-hydroxylation is required to convert deoxycorticosterone to corticosterone, this conversion can also be catalyzed by the related enzyme, CYP11B1, located in the fasciculata, which is unaffected in this disorder. For the same reason, these patients have normal cortisol biosynthesis.
The disease has previously been classified into 2 types, termed corticosterone methyloxidase deficiency types I and II. They differ only in levels of the immediate precursor of aldosterone, 18-hydroxycorticosterone; levels are low in type I deficiency and elevated in type II deficiency. These differences do not correspond in a simple way to particular mutations and are of limited clinical importance.
Clinical Manifestations
Infants with aldosterone synthase deficiency may have severe electrolyte abnormalities with hyponatremia, hyperkalemia, and metabolic acidosis. Because cortisol synthesis is unaffected, infants rarely become as ill as untreated infants with salt-losing forms of congenital adrenal hyperplasia such as 21-hydroxylase deficiency. Thus, some infants escape diagnosis. Later in infancy or in early childhood they may exhibit failure to thrive and poor growth. Adults often are asymptomatic, although they may develop electrolyte abnormalities when depleted of sodium through procedures such as bowel preparation for a barium enema.
Laboratory Findings
Infants have elevated plasma renin activity. Aldosterone levels are decreased; they may be at the lower end of the normal range but are always inappropriately low for the degree of hyperkalemia or hyperreninemia. Corticosterone levels are often elevated.
Some but not all patients have marked elevation of 18-hydroxycorticosterone, but low levels of this steroid do not exclude the diagnosis. In those kindreds that 18-hydroxycorticosterone levels are elevated in affected individuals, this biochemical abnormality persists in adults even when they have no electrolyte abnormalities.
Differential Diagnosis
It is important to distinguish aldosterone synthase deficiency from primary adrenal insufficiency in which both cortisol and aldosterone are affected (including salt-wasting forms of congenital adrenal hyperplasia) because the latter condition is usually associated with a much greater risk of shock and hyponatremia. This becomes apparent after the appropriate laboratory studies. Pseudohypoaldosteronism (Chapter 52) may have similar electrolyte abnormalities and hyperreninemia, but aldosterone levels are high, and this condition usually does not respond to fludrocortisone treatment.
570.8 Glucocorticoid-Suppressible Hyperaldosteronism
Etiology
Glucocorticoid-suppressible aldosteronism (glucocorticoid-remediable aldosteronism, familial hyperaldosteronism type I) is an autosomal dominant form of low-renin hypertension in which hyperaldosteronism is rapidly suppressed by glucocorticoid administration. This unusual effect of glucocorticoids suggests that this disorder is regulated by ACTH aldosterone secretion instead of by the renin-angiotensin system. In addition to abnormally regulated secretion of aldosterone, there is marked overproduction of 18-hydroxycortisol and 18-oxocortisol. The synthesis of these steroids requires both 17-hydroxylase (CYP17) activity, which is expressed only in the zona fasciculata, and aldosterone synthase (CYP11B2) activity, which is normally expressed only in the zona glomerulosa. Together, these features imply that aldosterone synthase is being expressed in a manner similar to the closely related enzyme steroid 11-hydroxylase (CYP11B1). The disorder is caused by unequal meiotic crossing over events between the CYP11B1 and CYP11B2 genes, which are closely linked on chromosome 8q24. An additional “hybrid” gene is produced, having regulatory sequences of CYP11B1 juxtaposed with coding sequences of CYP11B2. This results in the inappropriate expression of a CYP11B2-like enzyme with aldosterone synthase activity in the adrenal fasciculata.
Clinical Manifestations
Some affected children have no symptoms, the diagnosis being established after incidental discovery of moderate hypertension, typically about 30 mm Hg higher than unaffected family members of the same age. Others have more symptomatic hypertension with headache, dizziness, and visual disturbances. A strong family history of early-onset hypertension or early strokes may alert the clinician to the diagnosis. Some patients have chronic hypokalemia, but this is not a consistent finding and is usually mild.
Laboratory Findings
Patients have elevated plasma and urine levels of aldosterone and suppressed plasma renin activity. Hypokalemia is not consistently present. Urinary and plasma levels of 18-oxocortisol and 18-hydroxycortisol are markedly increased. The hybrid CYP11B1/CYP11B2 gene can be readily detected by molecular genetic methods; these assays are not routinely available.
Differential Diagnosis
This condition should be distinguished from primary aldosteronism due to bilateral hyperplasia or an aldosterone-producing adenoma (Chapter 572). Most cases of primary aldosteronism are sporadic although rare affected kindreds have been reported. Patients with primary aldosteronism may also have elevated levels of 18-hydroxycortisol and 18-oxocortisol, and these biochemical tests should be used cautiously to distinguish primary and glucocorticoid-suppressible aldosteronism. A therapeutic trial of dexamethasone may be helpful if aldosterone secretion is suppressed, and genetic testing should identify the hybrid gene of glucocorticoid-suppressible hyperaldosteronism if it is present.
Treatment
Glucocorticoid-suppressible hyperaldosteronism is managed by daily administration of a glucocorticoid, usually dexamethasone, 25 µg/kg/day in divided doses. If necessary, effects of aldosterone can be blocked with a potassium-sparing diuretic such as spironolactone, eplerenone, or amiloride. Hypertension resolves in patients in whom the hypertension is not severe or of long standing. If hypertension is long standing, additional antihypertensive medication may be required, such as a calcium channel blocker.