Chapter 673 The Upper Limb
Shoulder
The shoulder is a ball-and-socket joint that is similar to the hip; however, the shoulder has a greater range of motion than the hip. This is due to the size of the humeral head relative to the glenoid, as well as to the presence of scapulothoracic motion. The shoulder positions the hand along the surface of a theoretical sphere in space, with its center at the glenohumeral joint.
Brachial Plexus Birth Palsy
Injuries to the brachial plexus can occur in the peripartum time, usually as a result of a stretching mechanism. This palsy is often associated with large fetal size and shoulder dystocia. The incidence is 1-3/1,000 live births. The injury can range in severity from neurapraxia to complete rupture of the nerve root or avulsion of the nerve root from the spinal cord. More often, the upper roots (C5 and C6) are affected rather than a complete brachial plexus palsy. Rarely, in isolation, a lower plexus injury (C8 and T1) is observed. The clinical appearance of a C5-6 brachial plexus birth palsy is the waiter’s tip position. The arm is held in a position of shoulder adduction and internal rotation, elbow extension, and wrist flexion. This is the classic Erb’s palsy.
Treatment
Occupational therapy for brachial plexus injuries should be instituted quickly to maintain passive range of motion of the limb and encourage use of the arm. If the biceps muscle does not demonstrate any recovery by 3 mo of age or shows persistent weakness at 5 mo of age, rupture or avulsion of the nerve roots is suspected. Surgical exploration and nerve grafting of the brachial plexus are then indicated. MRI and electrodiagnostic testing are not consistently reliable in this setting.
Shoulder dysplasia and dislocation (analogous to developmental dysplasia of the hip) can occur as a result of muscle imbalances in infants and older children and can require arthroscopic or open reduction and muscle balancing. Older children with residual weakness in shoulder abduction and external rotation can benefit from muscle transfers. Osteotomies are reserved for children with severely deformed glenohumeral joints and functional impairment from persistent shoulder internal rotation contracture.
Sprengel’s Deformity
Sprengel’s deformity, or congenital elevation of the scapula, is a disorder of development that involves a high scapula and limited scapulothoracic motion. The scapula originates in early embryogenesis at a level posterior to the 4th cervical vertebra, but it descends during development to below the 7th cervical vertebra. Failure of this descent, either unilateral or bilateral, is the Sprengel deformity. The severity of the deformity depends on the location of the scapula and associated anomalies. The scapula in mild cases is simply rotated, with a palpable or visible bump corresponding to the superomedial corner of the scapula in the region of the trapezius muscle. Function is generally good. In moderate cases, the scapula is higher on the neck and connected to the spine with an abnormal omovertebral ligament or even bone. Shoulder motion, particularly abduction, is limited. In severe cases, the scapula is small and positioned on the posterior neck, and the neck may be webbed. The majority of patients have associated anomalies of the musculoskeletal system, especially in the spine, making spinal evaluation important.
Treatment
In mild cases, treatment is generally unnecessary, although a prominent and unsightly superomedial corner of the scapula can be excised. In more severe cases, surgical repositioning of the scapula with rebalancing of parascapular muscles can significantly improve both function and appearance.
Elbow
The elbow is the most congruent joint in the body. The stability of the elbow is imparted via this bony congruity as well as through the medial and radial collateral ligaments. Where the shoulder positions the hand along the surface of a theoretical sphere, the elbow positions the hand within that sphere. The elbow allows extension and flexion through the ulnohumeral articulation and pronation and supination through the radiocapitellar articulation.
Panner’s Disease
Panner’s disease is a disruption of the blood flow to the articular cartilage and subchondral bone to the capitellum (Fig. 673-1). It typically occurs in boys between the ages of 5 and 13 yr. Presenting symptoms include lateral elbow pain, loss of motion, and, in advanced cases, mechanical symptoms of the elbow.
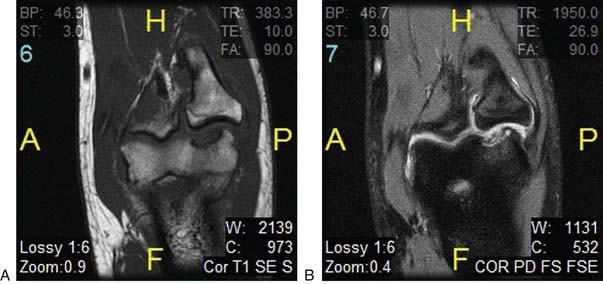
Figure 673-1 T1 (A) and T2 (B) coronal MRI images of the elbow depicting Panner disease of the elbow.
The mechanism of injury can be impaction or overloading of the joint, as seen with sports such as gymnastics and baseball. It can also be idiopathic. Radiographs of the elbow may be normal, but they can also show a small lucency within the capitellum. MRI is the study of choice to evaluate a suspected capitellar lesion. It can demonstrate the extent of the lesion as well as the integrity of the articular surface better than plain radiographs.
Radial Longitudinal Deficiency
Radial longitudinal deficiency of the forearm comprises a spectrum of conditions and diseases that have resulted in hypoplasia or absence of the radius (Table 673-1). This process was formerly referred to as radial club hand, but the name has been changed to radial longitudinal deficiency, which better characterizes the condition. Clinical characteristics consist of a small, shortened limb with the hand and wrist in excessive radial deviation.
Table 673-1 SYNDROMES COMMONLY ASSOCIATED WITH RADIAL DEFICIENCY
| SYNDROME | CHARACTERISTICS |
|---|---|
| Holt-Oram syndomre | Heart defects, most commonly atrial septal defects |
| Thrombocytopenia absent radius | Thrombocytopenia present at birth but improves over time |
| VACTERL association | Vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula, esophageal atresia, renal defects, radial dysplasia, lower limb abnormalities |
| Fanconi anemia | Aplastic anemia not present at birth, develops about 6 yr of age; fatal without bone marrow transplant; chromosomal breakage challenge test available for early diagnosis |
From Trumble T, Budoff J, Cornwall R, editors: Core knowledge in orthopedics: hand, elbow, shoulder, Philadelphia, 2005, Elsevier, p 425.
Radial longitudinal deficiency can range in severity from mild to severe and has been classified into four types according to Bayne and Klug (Table 673-2). Radial longitudinal deficiency can be associated with other syndromes such as Holt-Oram and Fanconi’s anemia.
Table 673-2 CLASSIFICATION OF RADIAL LONGITUDINAL DEFICIENCY
| TYPE | CHARACTERISTICS |
|---|---|
| I | Short radius Minor radial deviation of the hand |
| II | Hypoplastic radius with abnormal growth at proximal and distal ends Moderate radial deviation of the hand |
| III | Partial absence of the radius Severe radial deviation of the hand |
| IV | Complete absence of the radius The most common type |
Adapted from Bayne LG, Klug MS: Long-term review of the surgical treatment of radial deficiencies, J Hand Surg Am 12(2):169–179, 1987.
Treatment
The goals for the treatment of radial longitudinal deficiency include centralizing the hand and wrist on the forearm, balancing the wrist, and maintaining appropriate thumb and digital motion. Shortly after birth, parents are encouraged to passively stretch the wrist and hand to elongate the contracted radial soft tissues. Serial casting and splinting are ineffective at this time, due to the small size of the arm.
For surgical treatment, the preoperative plan begins with careful examination of the patient; considerations in regard to thumb and elbow function must be made before surgery. The surgery typically occurs when the child is 1 yr of age. Correction of the radial deviation as well as centralization of the wrist can be accomplished with a variety of different surgical techniques. These techniques include open release, capsular reefing, and tendon rebalancing. External fixation techniques have also been described.
Nursemaid Elbow
Nursemaid elbow is a subluxation of a ligament rather than a subluxation or dislocation of the radial head. The proximal end of the radius, or radial head, is anchored to the proximal ulna by the annular ligament, which wraps like a leash from the ulna, around the radial head, and back to the ulna. If the radius is pulled distally, the annular ligament can slip proximally off the radial head and into the joint between the radial head and the humerus (Fig. 673-2). The injury is typically produced when a longitudinal traction force is applied to the arm, such as when a falling child is caught by the hand, or when a child is pulled by the hand. The injury usually occurs in toddlers and rarely occurs in children >5 yr of age. Subluxation of the annular ligament produces immediate pain and limitation of supination. Flexion and extension of the elbow are not limited, and swelling is generally absent. The diagnosis is made by history and physical examination, as radiographs are typically normal.

Figure 673-2 The pathology of nursemaid, or pulled, elbow. The annular ligament is partially torn when the arm is pulled. The radial head moves distally, and when traction is discontinued, the ligament is carried into the joint.
(From Rang M: Children’s fractures, ed 2, Philadelphia, 1983, JB Lippincott, p 193.)
Treatment
The annular ligament is reduced by rotating the forearm into supination while holding pressure over the radial head. A palpable click or clunk can be felt. The child recovers active supination immediately and usually has immediate relief of discomfort. Immobilization is not required, but recurrent annular ligament subluxations can occur, and the parents should avoid activities that apply traction to the elbows. Parents can learn reduction maneuvers for recurrent episodes to avoid trips to the emergency department or pediatrician’s office. Recurrent subluxation beyond 5 yr of age is rare. Irreducible subluxations tend to resolve spontaneously, with gradual resolution of symptoms over days to weeks; surgery is rarely indicated.
Wrist
The wrist is composed of the two forearm bones as well as the eight carpal bones. The wrist allows flexion, extension, and radial and ulnar deviation through the radiocarpal and midcarpal articulations. Pronation and supination occur, at the wrist, through the distal radial ulnar joint (DRUJ). The wrist is a complex joint with numerous ligamentous and soft tissue attachments. It has complex kinematics that allow its generous range of motion, but when these kinematics are altered they can cause significant dysfunction.
Madelung’s Deformity
Madelung’s deformity is a deformity of the wrist that is characterized as radial and palmar angulations of the distal aspect of the radius. Growth arrest of the palmar and ulnar aspect of the distal radial physis is the underlying cause of this deformity. Bony physeal lesions and an abnormal radiolunate ligament (Vicker ligament) have been implicated. The deformity can be bilateral and affects girls more than boys.
Treatment
Treatment of Madelung’s deformity is typically observation. Mild deformities can be observed until skeletal maturity. Moderate to severe deformities that either are painful or limit function may be candidates for surgical intervention. Surgical treatment for Madelung’s deformity is motivated by appearance. Patients and their families are often concerned about the palmar angulation of the wrist as well as the resulting prominent distal ulna.
There are a multitude of surgical options for treating Madelung’s deformity. For the skeletally immature patient, resection of the tethering soft tissue (Vicker ligament) and physiolysis (fat grafting of any bony lesion seen within the physis) is often the first option. When Madelung’s deformity is encountered in skeletally mature patients, an osteotomy is often the treatment of choice. Dorsal closing wedge, dome, and ulnar shortening osteotomies may be used alone or in combination to achieve the desired result.
Long-term considerations of Madelung’s deformity concern the incongruity of the DRUJ and resulting premature DRUJ arthritis.
Ganglion
As a synovial joint, the wrist articulation is lubricated with synovial fluid, which is produced by the synovial lining of the joint and maintained within the joint by the joint capsule. A defect in the capsule can allow fluid to leak from the joint into the soft tissues, resulting in a ganglion. The term cyst is a misnomer, because this extra-articular collection of fluid does not have its own true lining. The defect in the capsule can occur as a traumatic event, although trauma is rarely a feature of the presenting history. The fluid usually exits the joint in the interval between the scaphoid and lunate, resulting in a ganglion located at the dorsoradial aspect of the wrist. Ganglia can occur at other locations, such as the volar aspect of the wrist, or in the palm as a result of leakage of fluid from the flexor tendon sheaths. Pain is not commonly associated with ganglia in children, and when it is, it is unclear whether the cyst is the cause of the pain. The diagnosis is usually evident on physical examination, especially if the lesion transilluminates. Extensor tenosynovitis and anomalous muscles can mimic ganglion cysts, but radiography or MRI is not routinely required. Ultrasonography is an effective, noninvasive tool to support the diagnosis and reassure the patient and family.
Treatment
Up to 80% of ganglia in children <10 yr of age resolve spontaneously within 1 yr of being noticed. If the ganglion is painful or bothersome and the child is >10 yr of age, treatment may be warranted. Simple aspiration of the fluid has a high recurrence rate and is painful for children given the large-bore needle required to aspirate the gelatinous fluid. Surgical excision, including excision of the stalk connecting the ganglion to its joint of origin, has a high success rate, although the ganglion can recur.
Hand
The hand and fingers allow complex and fine manipulations. An intricate balance among extrinsic flexors, extensors, and intrinsic muscles allow these complex motions to occur. Congenital anomalies of the hand and upper extremity rank just behind cardiac anomalies in incidence, and like cardiac anomalies, if they are not properly identified and remedied, they can have long-term consequences.
Camptodactyly
Camptodactyly is a nontraumatic flexion contracture of the proximal interphalangeal joint that is often progressive. The small and ring fingers are most often affected. Bilateralism is observed two thirds of the time. The etiology of camptodactyly is varied. Several different hypotheses have been offered as to the cause of this condition. Camptodactyly can be divided into three different types (Table 673-3).
Table 673-3 CLASSIFICATION OF CAMPTODACTYLY
| TYPE | CHARACTERISTICS |
|---|---|
| I | Congenital no sex bias, small finger only |
| II | Acquired between 7-11 yr, typically progressive |
| III | Severe, significant contracture, bilateral and associated with other musculoskeletal syndromes |
Adapted from Kozin SH: Pediatric hand surgery. In Beredjiklian PK, Bozentka DJ, editors: Review of hand surgery, Philadelphia, 2004, WB Saunders, pp 223–245.
Treatment
Nonsurgical treatment is the primary treatment of camptodactyly. Mild contractures of less than 30 degrees are usually well tolerated and do not need treatment. Serial casting and static and dynamic splinting are the treatments of choice for preventing progression of contractures. This should be performed until the child is skeletally mature.
Surgical treatment is limited to the treatment of severe contractures. At the time of surgery, all contracted and anomalous structures are released. Results of contracture release for camptodactyly are mixed; often a loss of flexion results from an attempt to improve extension.
Clinodactyly
Angular deformity of the digit in the coronal plane, distal to the metacarpophalangeal joint is clinodactyly. The most commonly observed finding is a mild radial deviation of the small finger at the level of the distal interphalangeal joint. This is often due to a triangular or trapezoidal middle phalanx. In some cases, a disruption of the physis at the middle phalanx produces a longitudinal epiphysial bracket. This bracket is thought to be the underlying cause for the formation the “delta phalanx” that is often observed in clinodactyly. Clinodactyly has been observed in other fingers, including the thumb (Fig. 673-3) and ring finger.
Treatment
Often the treatment for clinodactyly is observation and not surgery. For severe deformities and for those affecting the thumb, surgery is often indicated. Surgery is technically demanding. Bracket resections, corrective osteotomies, and growth plate ablations are the most common procedures performed to correct the observed angular deformities. Results are good and recurrences are few when an appropriate procedure is performed.
Polydactyly
Polydactyly or duplication of a digit can occur either as a preaxial deformity (involving the thumb) or as a post axial deformity (involving the small finger) (Table 673-4). Each has an inherited and genetic component. Duplication of the thumb occurs more in white children and is often unilateral, whereas duplication of the small finger occurs mainly in African-Americans and may be bilateral. Transmission is typically in an autosomal dominant pattern and has been linked to defects in genes localized to chromosome 2.
Duplication of the thumb was extensively studied by Wassel. Wassel subdivided thumb duplication on the basis of the degree of duplication. The seven types according to Wassel are listed in Table 673-5. Small finger duplication has been further subdivided into two types. Type A is a well-formed digit. Type B is a small, often underdeveloped supernumerary digit.
Table 673-5 WASSEL CLASSIFICATION OF THUMB DUPLICATION
| TYPE | CHARACTERISTICS |
|---|---|
| I | Bifid distal phalanx |
| II | Duplicate distal phalanx |
| III | Bifid proximal phalanx |
| IV | Duplicate proximal phalanx |
| V | Bifid metacarpal |
| VI | Duplicate metacarpal |
| VII | Triphalangeal component |
Adapted from Wassel, HD: The results of surgery for polydactyly of the thumb. A review, Clin Orthop 125:175–193, 1969.
Treatment
Thumb and small finger duplication is typically treated with ablation of the supernumerary digit. Treatment options vary based on the degree of involvement. Less well formed digits can be treated with suture ligation. Well-formed digits require reconstructive procedures that preserve important structures such as the collateral ligaments and nail folds.
Thumb Hypoplasia
Hypoplasia of the thumb is a challenging condition for both the patient and the doctor. The thumb represents ∼40% of hand function. A less-than-optimal thumb can severely limit a patient’s function as he or she grows and develops. Hypoplasia of the thumb can range from being mild with slight shortening and underdeveloped musculature to complete absence of the thumb (Fig. 673-4). Radiographs are useful to help determine osseous abnormalities. The most important finding on physical exam is the presence or absence of a stable carpometacarpal (CMC) joint. This finding helps guide surgical treatment.
Treatment
If the thumb has a stable CMC joint, reconstruction is advised. Key elements of thumb reconstruction include rebuilding the ulnar collateral ligament of the metacarpophalangeal joint, tendon transfers to aid in abduction, and procedures to deepen the web space.
If a stable CMC joint is not present or the thumb is completely absent, pollicization (surgical construction of a thumb from a finger) is the definitive treatment. Pollicization is a complex procedure rotating the index finger along its neurovascular pedicle to form a thumb. This procedure is typically performed at around 1 yr of age and may be followed by subsequent procedures to deepen the web space or augment abduction (Fig. 673-5).
Syndactyly
Failure of the individual digits to separate during development produces syndactyly. Syndactyly is one of the more common anomalies observed in the upper limb (Table 673-6). It is seen in 0.5 of 1,000 live births. Syndactyly can be classified as simple (skin attachments only), complicated (bone and tendon attachments), complete (fusion to the tips, including the nail), or incomplete (simple webbing).
Treatment
Division of the conjoined digits should be considered before the 2nd year of life. Border digits should be divided earlier (3-6 mo) because of concern over tethering effects of digits of unequal length. Digits of similar size, such as the ring and middle, may wait until the 12-18 mo age range. Reconstruction of the web space and nail folds as well as appropriate skin-grafting techniques must be used to ensure the best possible functional and cosmetic result.
Fingertip Injuries
Young children are fascinated with door-jambs or car doors and other tight spaces, making crush injuries to the fingertips quite common. Injury can range from a simple subungual hematoma to complete amputation of part or the entire fingertip. Radiographs are important to rule out fractures. Physeal fractures associated with nailbed injuries are open fractures with a high risk of osteomyelitis, growth arrest, and deformity if not treated promptly with formal surgical debridement and reduction. Tuft fractures involving the very distal portion of the distal phalanx are common and require little specific treatment other than that for the soft-tissue injury.
The treatment of the soft-tissue injury depends on the type of injury. For suture repairs, only absorbable sutures should be used, because suture removal from a young child’s fingertip can require sedation or general anesthesia. If a subungual hematoma exists but the nail is normal and no displaced fracture exists, the nail need not be removed for nailbed repair. If the nail is torn or avulsed, the nail should be removed, the nail bed and skin should be repaired with absorbable sutures, and the nail (or a piece of foil if the nail is absent) should be replaced under the eponychial fold to prevent scar adhesion of the eponychial fold to the nail bed that can prevent nail regrowth.
If the fingertip is completely amputated, treatment depends on the level of amputation and the age of the child. Distal amputations of skin and fat in children <2 yr of age can be replaced as a composite graft with a reasonable chance of surviving. Similar amputations in older children can heal without replacing the skin as long as no bone is exposed and the amputated area is small. A variety of coverage procedures exist for amputations through the mid-portion of the nail. Amputations at or proximal to the proximal edge of the fingernail should be referred emergently to a replant center for consideration for microvascular replantation. When referring, all amputated parts should be saved, wrapped in saline-soaked gauze, placed in a watertight bag, and then placed in ice water. Ice should never directly contact the part, because it can cause severe osmotic and thermal injury.
Trigger Thumb and Fingers
The flexor tendons for the thumb and fingers pass through fibrous tunnels made up of a series of pulleys on the volar surface of the digits. These tunnels, for reasons that are not well understood, can become tight at the most proximal or 1st annular pulley. Swelling of the underlying tendon occurs, and the tendon no longer glides under the pulley. In children, the most common digit involved is the thumb. It has classically been thought to be a congenital problem, but prospective screening studies of large numbers of neonates have failed to find a single case in a newborn child. Trauma is rarely a feature of the history, and the condition is often painless. Overall function is rarely impaired. A trigger thumb typically manifests with the inability to fully extend the thumb interphalangeal joint. A palpable nodule can be felt in the flexor pollicis longus tendon at the base of the thumb. Other conditions can mimic trigger thumb, including the thumb-in-palm deformity of cerebral palsy. Similar findings in the fingers are much less common and can be associated with inflammatory conditions such as juvenile rheumatoid arthritis.
Treatment
Trigger thumbs spontaneously resolve in up to 30% of children in whom they are diagnosed before 1 yr of age. Spontaneous resolution beyond that age is not common. Corticosteroid injections are effective in adults but are not effective in children and risk injury to the nearby digital nerves. Surgical release of the 1st annular pulley is curative and is generally performed between 1 and 3 yr of age. Treatment of trigger fingers other than the thumb in children involves evaluation and treatment of any underlying inflammatory process and in some cases surgical decompression of the flexor sheath.
Ali M, Jackson T, Rayan GM. Closing wedge osteotomy of abnormal middle phalanx for clinodactyly. Hand Surg Am. 2009;34(5):914-918.
Altergott C, Garcia FJ, Nager AL. Pediatric fingertip injuries. Pediatr Emerg Med. 2008;24:148-152.
Kenniston JA, Beredjiklian PK, Bozentka DJ. Osteochondritis dissecans of the capitellum in fraternal twins: case report. J Hand Surg Am. 2008;33:1380-1383.
Lahiri A, Lester R. Hand anomalies in Russell Silver syndrome. J Plast Reconstr Aesthet Surg. 2009;62(4):462-465.
Manske PR, Goldfarb CA. Congenital failure of formation of the upper limb. Hand Clin. 2009;25(2):157-170.
Pill SG, Ganley TJ, Flynn JM, et al. Osteochondritis dissecans of the capitellum: arthroscopic-assisted treatment of large, full-thickness defects in young patients. Arthroscopy. 2003;19(2):222-225.
Ty JM, James MA. Failure of differentiation: part II (arthrogryposis, camptodactyly, clinodactyly, madelung deformity, trigger finger, and trigger thumb). Hand Clin. 2009;25(2):195-213.
Wafa AM. Hourglass dorsal metacarpal island flap: a new design for syndactylized web reconstruction. J Hand Surg Am. 2008;33(6):905-908.
Zebala LP, Manske PR, Goldfarb CA. Madelung’s deformity: a spectrum of presentation. J Hand Surg Am. 2007;32(9):1393-1401.


