Ethics Applied to Nursing: Personal Versus Professional Ethics
On completing this chapter, you will be able to do the following:
- 1. List four current ethical issues of concern in twenty-first-century health care.
- 2. Explain the differences among ethics, morals, and values.
- 3. Differentiate between personal and professional ethics.
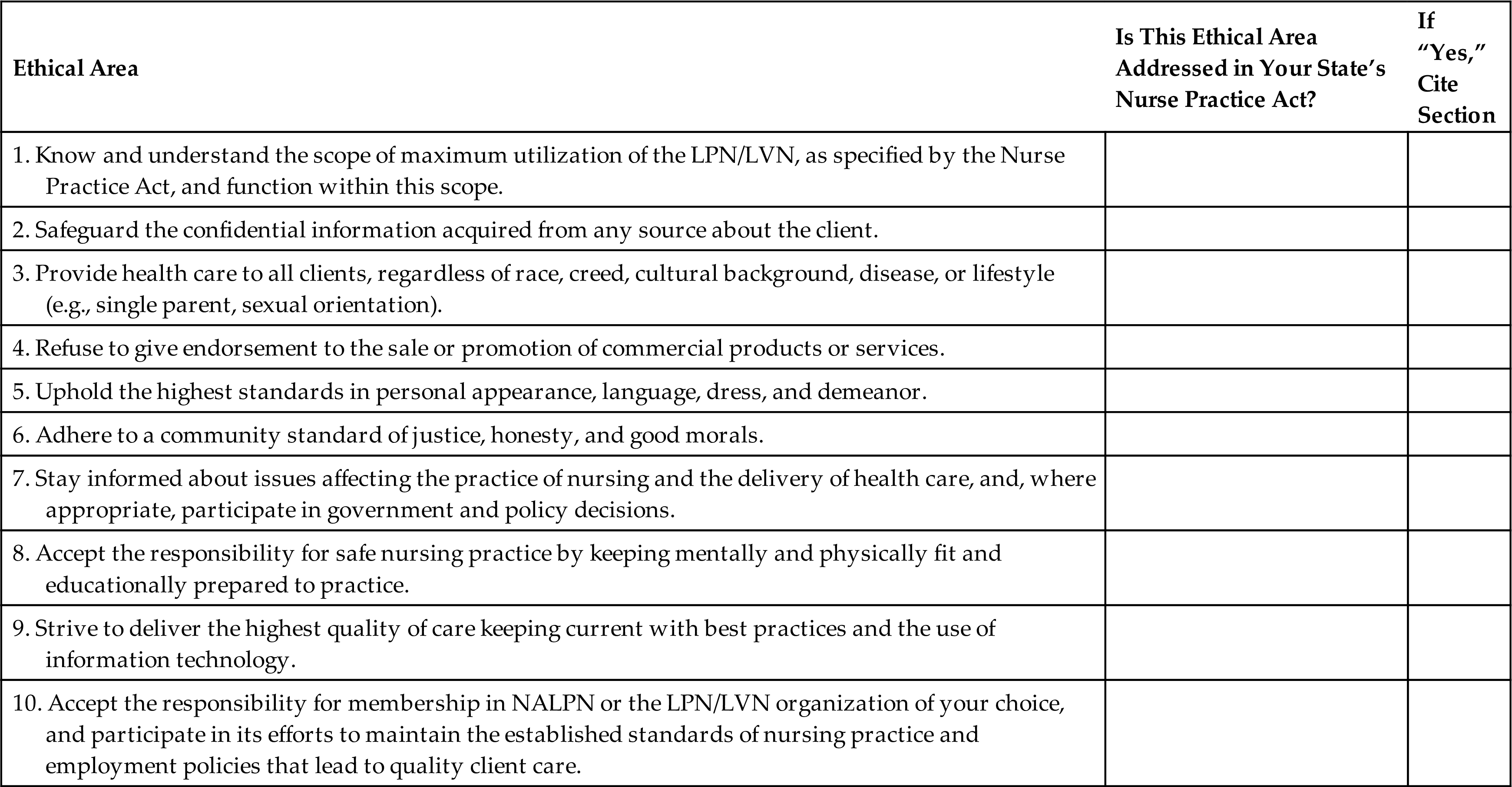
- 4. Identify ethical elements in your state/territory or country’s Nurse Practice Act.
- 5. Describe how the role of nursing has changed since the introduction of the nursing process and critical thinking into nursing curricula.
- 6. Discuss how nonmaleficence is more complex than the definition of “do no harm.”
- 7. Differentiate between beneficence and paternal beneficence.
- 8. Explain the steps for an autonomous decision.
- 9. Describe how fidelity affects nursing care.
- 10. Discuss how a nurse applies the principle of justice to nursing.
- 11. Differentiate between ethical and legal responsibilities in nursing.
Key Terms
beneficence (bĕ-NĔF-ĭ-sĕns)
beneficent paternalism (bĕ-NĔF-ĭ-sĕnt-pă-TŬR-nă-lĭz-ŭm)
ethics (ĕ-THIKS)
fidelity (fĭ-DĔL-ĭ-t ē)
justice (JŬS-tĭs)
morals (MŎR-ăls)
nonmaleficence (nŏn-mă-LĔF-ĭ-sĕns)
nursing ethics (NŬR-sĭng-ĕ-THIKS)
personal ethics (PĔR-sŭn-ăl-ĕ-THIKS)
privacy (PRĪ-vă-sē)
values (VĂL-ūs)
Two student nurses share with their clinical instructor a concern regarding a conversation they overheard while caring for a resident at the nursing home earlier in the week. The resident’s son, accompanied by their friend, had arrived to visit. The son was trying to convince their client to sign a new will. The resident was asking questions, and the son stated, “Just sign right on the line, Mom, everything will be okay. Trust me.” The students stated that the resident seemed very uncomfortable but did sign the will. They had not said anything to the staff, as they thought they were respecting the resident’s autonomy. Thus they did not think it was their concern. However, after completing their reading for their ethics class today, they believe they may have made a mistake and should have reported this event. Their instructor indicates that this is an important issue, and will notify the nursing home. The instructor thanks the students for reporting their concern and directs them to report any ethical issues immediately in the future.
As you read this chapter, think about all of the ethical issues that can face a nurse on a daily basis.
The twenty-first century presents numerous ethical issues in health care, as reflected in agency policies and medical procedures that create life, prolong life, cure chronic diseases, ensure a peaceful death, and end life. Additional ethical issues will arise as scientific research continues to explore possibilities, the procedures are discussed, and if procedures are legalized, people press for their right to make autonomous decisions. Students in practical/vocational nursing classes identified the following current ethical issues in health care: in vitro fertilization, artificial insemination, surrogate motherhood, cloning, organ donation (including cadaver donations), child organ donors, procedures that use fetal tissues (stem cells) or organs from aborted fetuses, conceiving a child to produce tissue for a sibling, abortion, experiments that destroy a human embryo, euthanasia, assisted suicide, advance directives (including living wills and durable power of attorney), and insertion and/or withdrawal of feeding tubes.
A clinical example of an ethical issue follows: a client has verbalized to the health care provider the wish to avoid further heroic means to stay alive. Two adult children have arrived and insist that all means be used to maintain life, but the three children already at the bedside do not agree. The client lacks a living will and durable power of attorney and is unconscious at this point.
You will encounter similar scenarios as a student participating in a clinical assignment. These learning experiences are instrumental to provide time for self-discovery, self-reflection, and self-analysis. Understanding your own ethics is a first step in providing unbiased ethical care to your clients.
Description and Scope of Ethics
Ethics is a system of standards or moral principles that direct actions as being right or wrong. Ethics is concerned with the meaning of words such as right, wrong, good, bad, ought, and duty. Ethics is concerned with the ways people, either individually or as a group, decide the following:
This basic definition is somewhat of an over simplification. Ethics sounds like the words morals and values, but there are differences among them.
Morals and Values
Morals are concerned with dealing with right or wrong behavior (conduct) and character. The terms ethics and morals are difficult to define separately. Morals comes from a Latin root, and ethics comes from a Greek root. Both words mean “customs” or “habits” and refer to the general area of rights and wrongs. The words are often substituted for each other. Ethics and morals are used in the same way in this chapter.
Values involve the worth you assign to an idea or an action. Values are freely chosen and are affected by age, experience, and maturity. A child usually embraces family values during childhood. The teen years are a time of trying out family values and either incorporating them or rejecting and replacing them with new values. Values continue to be modified throughout your lifetime as you acquire new knowledge and experience. Based on changes in values, one’s code of ethics/morals can shift (e.g., organ transplants after you have learned about or cared for a client who receives a transplant).
Law is thought of as a minimum ethic that is written and enforced. As a licensed practical nurse/licensed vocational nurse (LPN/LVN), the Nurse Practice Act in your state is your final authority on what you are legally obligated to do as a nurse regardless of where you are employed (see Chapter 7 for more about nursing and the law). It is essential to have a thorough knowledge of the Nurse Practice Act in the state in which you are employed.
Comparison of Legal Aspects of Nursing and Ethics
Nursing ethics are similar to, but also different from, the legal aspects that regulate your nursing practice. Table 6.1 presents a comparison of legal aspects and nursing ethics.
Table 6.1

NAPNES, National Association for Practical Nurse Education and Service; NALPN, National Association of Licensed Practical Nurses; PN, practical nurse.
Nursing Ethics
According to the Miller-Keane Encyclopedia & Dictionary of Medicine, Nursing & Allied Health, nursing ethics is described as “the values and ethical principles governing nursing practice, conduct, and relationships.” Nursing ethics deals with the relationship of a nurse to the client, the client’s family, associates and fellow nurses, and society at large. Nursing ethics attempts to look for underlying patterns or order in a large number of ethical decisions and practices of nurses, individually or as a group. Codes provide a guideline for what the LPN/LVN ought to do. However, codes do not carry the weight of law.
It is interesting to note how many ethical items are actually found in the law, such as your Nurse Practice Act. When ethical items are included in a legal document, it places emphasis on the importance of these items. It also gives the LPN/LVN a source to fall back on to defend the choices in behavior they make in regard to clients and families; it is then a matter of law. Mosby Medical Dictionary (2017) describes ethics as “the science or study of moral values or principles, including the ideals of autonomy, beneficence, and justice.” A discussion of all of these terms follows.
Ethical Codes of the National Association for Practical Nurse Education and Service and National Association of Licensed Practical Nurses
Ethics that are adopted by nursing groups are in their codes of behavior. Both the National Association for Practical Nurse Education and Service (NAPNES) and the National Association of Licensed Practical Nurses (NALPN) have ethical codes for LPN/LVNs.
Your Personal Code of Ethics
Practical/vocational nursing students and LPNs/LVNs also have personal ethics that provide personal guidelines for living. You ultimately choose what your personal code of ethics includes. Your personal code of ethics will influence your nursing ethics. Sometimes personal ethics conflict with the law (state’s Nurse Practice Act). When this occurs, you have an obligation to follow the law.
If you object to a medical procedure on religious or moral grounds, discuss this concern during the interview process. This objection may be incompatible with the job description and the mission and beliefs of the institution. In this case, you are not the right “fit” for the job. However, if an institution initiates a new procedure/service during your employment period that challenges your religious or moral beliefs, discuss and submit in writing your objections. Present the statement to your employer, including a possible solution to the issue. For example, you may be ethically opposed to abortion. Abortion in the United States is permitted under certain circumstances. You may ethically wish to refuse to assist with the abortion procedure.
Proactively creating a plan may prevent an ethical dilemma for you. However, you cannot refuse to give nursing care if needed. Abandonment is a legal matter, and maintaining your license may be at risk. The best strategy is to seek employment in a health agency that does not participate in procedures or nursing care of which you do not ethically approve.
Some nurses have tried to opt out of caring for clients who have an illness that may be related to a lifestyle of which they do not approve. A nurse needs to separate personal ethics from nursing ethics. You are legally expected to care for a client regardless of his or her lifestyle. For example, when caring for a client with acquired immune deficiency syndrome (AIDS), use proper techniques during care as you would with any client with an infectious disease. You may not refuse to care for this client. Ethically and legally this client must receive the same level of care, with dignity and respect that other clients do. Nursing is not about giving care selectively to those clients you approve of and refusing care to others that have different beliefs or a different lifestyle.
Roots of Nursing Ethics
Years ago, nurses saw themselves as doers, not thinkers. Nurses worked only to serve the health care providers’ wishes. Before the nursing process and critical thinking were added to nursing curricula, those in the nursing profession did not see themselves as having something separate to contribute to client care (in addition to the nurses’ dependent role to health care providers). Nursing ethics was primarily a modification of medical ethics and ethics of other professions at that time.
What Changed?
Nursing education was initially disease oriented. Nursing textbooks focused on the disease process, including cause, signs, symptoms, treatment, prognosis, and nursing care related to the treatment. Health care providers did the medical assessment and wrote orders for the nurse to carry out. The nurse reported on client progress, based on health care providers’ orders. Nursing assessments did not exist. Additional concerns the client might have had (e.g., spiritual, cultural, emotional, sexual) were not routinely assessed and addressed. Clients were expected to follow health care providers’ orders without question. The nurse’s job was to see that the orders were carried out. The early nursing role was limited to the dependent relationship with the health care provider.
As nursing theories emerged, so did the nursing process and critical thinking, and nursing textbooks began to include these topics. Nurses discovered that in addition to their dependent role to health care providers, they had something special to contribute to the client. Finally, it was understood that the client was a person, not just a disease. With the help of the nursing process, nurses had a way to identify additional needs that could be responded to through nursing care. Rather than expecting clients to blindly follow orders because “we know what is wrong with you and we can fix it” (benevolent paternalism), clients were encouraged to be an active part in planning and implementing their own nursing care plan (support of client autonomy). Today, the availability of evidence-based resources on the Internet has contributed to client autonomy.
Despite what we observe today, changes in nursing did not happen easily. Many nurses were entrenched in their dependent role to health care providers, and they believed that nursing was being ruined by the changes that were taking place. Nursing textbooks and curricula, however, both had to change to reflect the nursing process, critical thinking, and a focus on the total client (not just the physically diseased or injured portion of the client). Adding the nursing process and critical thinking changed the nursing role and nursing philosophy. Nurses, both LPNs/LVNs and registered nurses (RNs), are not just “doers” but also “thinkers.” The nursing process and critical thinking empowered nurses. This in turn influenced a change in nursing ethics.
Ethical principles in this chapter are about application of nursing ethics to nursing decisions and action. You are encouraged to look at both sides of an ethical principle. Recognize that no principle applies in the same way to all clients and their unique situation. No principle is absolute.
Critical thinking (see Chapter 5) plays a major role in sorting out ethical choices and legal responsibilities in regard to the client. The client’s knowledge of choices regarding care also affects ethical decision-making.
Ethical Decisions in Health Care
Ethics Committees
Health agencies such as hospitals, hospice units, and long-term care settings have an ethics committee. This multidisciplinary team (e.g., nurses, health care providers, clergy, social worker, and other allied health members) assists with difficult ethical decisions. Usually the discussions relate to new or unusual ethical questions. The recommendations of the ethics committee are expected to be given serious consideration by all stakeholders. In a faith-based organization, the principles of the faith can be anticipated to impact the decision-making of this committee. However, if you think the ethics committee makes all the medical ethical decisions, you are only partially right. Clients arrive with their culture-based and/or religion-based ethics, which were often established long before they were born. What the person can and cannot do in regard to health care has already been established by the culture of which they are a part. See Chapters 10 and 11 for a discussion of cultural and spiritual needs, spiritual caring, and religious differences.
Western Secular Belief System
In the Western secular belief system, the emphasis is shifted from duties to the rights of the individual. This system has the following characteristics:
- 1. Individual autonomy means “self-rule.” Individuals have the capacity to think, and based on these thoughts, to make the decision freely whether or not to seek health care (the freedom to choose).
- 2. Individual rights mean the ability to assert one’s rights. The extent to which a client can exert his or her rights is restricted (i.e., their rights cannot restrict the rights of others). For example, the client’s right to refuse treatment can be at odds with the health professional’s perceived duty to always act in a way that will benefit the client (do good and prevent harm). The individual’s right has become a central theme of health care:
Numerous bills of rights have been written, and fierce debates have taken place at both state and national levels. The question of individual autonomy and individual rights is far from being settled. Recently, some laws based on individual autonomy and rights have been passed (e.g., Health Care Reform; death with dignity laws). However, attempts to rescind laws that have been passed continue. The question is: To what extent do one’s individual moral decisions (rights) get in the way of another’s moral autonomy?
Ethical Responsibilities of Nurses
As the nurse’s role has evolved from being simply a “doer” to being also a “thinker,” it is logical that the number of ethical issues has also increased. Adding the nursing process and critical thinking to nursing curricula changed the nursing focus to the whole client. Although the interdependent role to the health care team remains, responsibilities that are unique to nursing were added. The following responsibilities, both ethical and legal, emerged:
- 1. Client advocacy: Client advocacy is a key role of all nurses. Clients are often in a vulnerable state when they are in need of nursing care; vulnerable because of the symptoms of the illness and because of the complexity of health care delivery. As a result, their need for advocacy often increases.
- Knowledge is power. Thus informing the client of the plan of care is essential. This needs to be done at least every shift, and more often if indicated by the client’s condition. Information, as simple as explaining the steps of a procedure, will empower clients. You also need to include a brief overview of the role of all the members of the health care team in the plan of care.
- At times, you may need to advocate ensuring the plan of care is not altered inappropriately because of an error or misjudgment. Advocacy is usually done in collaboration with the RN. Fully understand your advocacy role. In most states, the LPN/LVN’s role is to support teaching done by the RN, health care provider, or other members of the health care team. If the client has questions, and you are unsure about whether you should provide an answer, discuss with the RN your next steps.
- When the client does make a decision, be supportive even though you might not agree with the decision. It is your job to ensure that the client has enough knowledge and resources (evidence) to make an informed decision. If not, seek out the resources needed and provide them to the client.
- 2. Accountability: The word accountability means that you are answerable to yourself, to your assigned client and their family, to your supervisor, the health care team, and to your instructor who evaluates your work. As an LPN/LVN, accountability to the instructor is replaced by accountability to the employing agency. You are held accountable for all the nursing actions that you perform or are assigned to perform. The measures of accountability are the nursing standards of practice; that is, what a prudent nurse with your education and experience would do in a similar situation.
- 3. Client safety reporting: Report peers, supervisors, or any team members for behaviors that are potentially harmful to clients (e.g., impaired at work because of alcohol and/or other drug use, stealing client’s medication, substituting water or normal saline for injectable narcotics, leaving unstable clients unattended in the shower, sleeping while on duty, and verbal or physical abuse).
- 4. System-based issues: Identifying system-based issues is essential to providing safe high-quality care (e.g., if new procedures are implemented without appropriate education and training on all shifts, you need to notify administration and suggest a plan to ensure safe practice).
Principles of Ethics
As a nurse of the twenty-first century, you recognize there is something unique that a nurse has to offer clients beyond the dependent role to health care providers. This realization places greater responsibility on student practical nurses/student vocational nurses (SPNs/SVNs) to learn all they can during the nursing program of study. For example, now you can add knowledge of basic ethics to critical thinking as you assist the RN with the nursing process. The data you collect will have an added dimension of ethics. It will make a difference in developing a quality care plan that considers the client as a whole person and not just the part of his or her body that is sick.
At this level, you incorporate a basic understanding of how SPNs/SVNs and LPNs/LVNs practice nursing according to nursing codes. Learning about ethics is more than being able to recite the definition to pass a test; it means being able to help make ethical decisions when ethical dilemmas arise.
The following ethical principles are discussed in this chapter:
Nonmaleficence (do No Harm)
In her book Leadership and Management According to Florence Nightingale, Nightingale said the following:
“It may seem a strange principle to enunciate as the very first requirement in a hospital that it should do the sick no harm. It is quite necessary nevertheless to lay down such a principle.”
Nightingale is referring to the ethical principle nonmaleficence, which comes from the Latin primum non nocere, meaning “first do no harm.” Nonmaleficence is the basis of many of the “rules” promoted by your instructors, such as the following:
- • Six rights for giving medications.
- • Use of SBAR (Situation Background Assessment Recommendation) in collaboration with the RN for interdisciplinary communication.
- • Checking the temperature of bath or shower water.
- • Checking the temperature of formula before feeding the infant or child.
- • Returning the bed to its lowest position after completing a treatment or preparing to leave the room.
- • Raising side rails after nursing care if it is in the plan of care.
- • Providing care for your clients when their ethical principles conflict with yours.
- • Performing only necessary procedures on clients, instead of unnecessary procedures just to gain additional experience.
- • Protecting those who cannot protect themselves; for example, clients who have a cognitive disability, or who are unconscious, weak, or debilitated.
If the principle of nonmaleficence is taken to the extreme, however, SPNs/SVNs and LPNs/LVNs would not be able to perform many nursing duties. Few beneficial treatments are entirely without harm, including the following:
- • Puncture the client’s skin with a needle, there is some tissue damage, a risk of infection, and the possibility of an untoward reaction to a solution if administered.
- • Administration of medications can cause side effects: rare, serious, and not so serious.
- • Insertion of a tube into a bodily opening (e.g., catheterization, irrigating a colostomy), there is some trauma to surrounding tissue. There is the possibility of introducing infection and penetrating the tissue wall.
- • Performance of a procedure can hurt the client physically (e.g., positioning a client properly after surgery, cleansing the mouth of an elderly client who has not had proper mouth care for a period, irrigating a pressure ulcer, moving a client with osteoporosis from bed to chair to toilet and back).
- • Administration of a vaccine carries the risk of the client experiencing a side effect, but the overall effect for most people is the prevention of serious diseases.
- • Administration of a solution through an intra venous (IV) line can cause harm. One thing to continually monitor is that the solution and additive, if any, are infusing, as compared with what the health care provider ordered. A common additive is KCl (potassium chloride). KCl within a narrow blood level range is necessary for proper heart functioning. If too little or too much is administered, it can result in heart dysfunction, sometimes resulting in death. (Jack Kevorkian, a health care provider who participated in several assisted suicides, used KCl.) KCl can save lives, but it can also kill.
- • Performing range of motion after a stroke can elicit some discomfort because of stiff and slightly contracted muscles.
Each of the preceding procedures has the potential for doing good and doing harm. The question always is how to do the least amount of harm when doing something that is expected to result in good. The obvious answer is to never knowingly participate in any action that will deliberately harm the client. The client must also have agreed to the procedure verbally or in writing, depending on the procedure (autonomy). This is a reason for practicing procedures in the nursing lab; preparing for nursing care; reviewing your nursing care plan with the instructor; and reviewing action, side effects, and dosage with the instructor before giving a medication.
The following are negative examples of nursing actions that were meant to do no harm but resulted in injury:
- • Putting down a client’s side rail without first checking that the client’s arm is not hanging between the rail and the bed. The client who immediately comes to mind is an 80-year-old client whose arm was fractured and who received several skin tears and bruises. The staff person who put the rail down was irritated because of “a bad night shift” and was hurrying to get off duty.
- • Rapidly feeding large spoonfuls of food to a client who has a dry mouth as a side effect of medication. Because of the lack of liquid before beginning to eat, large spoonfuls of food, lack of adequate time to chew, and lack of additional liquid before the next bite, the client aspirated some of the food that accumulated in their mouth. The client survived but refused future attempts to eat when they saw the same nurse come in with their food tray.
- • Applying an external (Texas) catheter (condom-like catheter applied to male’s penis) incorrectly, causing constriction of circulation resulting in gangrene of the penis. The client’s penis required amputation.
- • Leaving the bed in the high position and the client subsequently falls.
Beneficence (do Good)
Beneficence means to “do good” with your nursing actions and is the basis of trust in nursing. It also involves preventing harm and removing harm. You have read how nonmaleficence and beneficence are often difficult to separate and may go hand in hand. The following major nursing duties to the client are associated with beneficence:
- 1. Put the client’s interests first; for example:
- • You do not go off duty until you hand over the care of the client to equally skilled nursing staff to continue the nursing care. You are obligated to report to the nurse taking over the next shift what has transpired during the time you have been responsible for nursing care.
- • If you give the wrong medication, report it as soon as you recognize the error. Your ethical concern is to “do good” and “prevent harm.” Beneficence is a greater good than concern for self in regard to the error. In addition, your individual error may be related to a system error. Prompt reporting and investigation can minimize a similar event from occurring in the future. Unsafe staffing levels can be a root cause of many errors and need to be reported.
- • You go to work even though you are tempted to call in sick because you want to go out of town for the weekend.
- 2. Place the good of clients before your needs. This is where interpretation of duty gets more complex. Does this mean that duty to the client means utmost sacrifice? No, it does not, but it does mean that you sacrifice something. Key points follow:
- • Client needs are above organizational needs. You may have administrative responsibility (perhaps as a charge nurse) that must be completed by the end of the day or meetings you are expected to attend that day. If a client needs your skill and expertise, as in an emergency situation, your first duty is to the client.
- • Placing the good of clients before your needs does not mean that you behave as though no one in the world can assume the nursing care you give to a client. Do not stay past your scheduled hours when there is someone ready to assume responsibility for nursing care. This also means that you do not call the client from home, accept calls in your home from the client, or visit the client after hours. If you are doing any of this, you have just entered an unhealthy codependent relationship with the client. These behaviors are usually prohibited by your employer.
- • Situations can be difficult. For example, you receive an emergency phone call regarding a sick child and leave abruptly. This would be viewed as client abandonment. You must always ensure that the client receives adequate nursing care in your absence. Reporting off to a colleague who is capable/competent of receiving the assignment is essential.
Autonomy (free to Choose)
Potter, Perry, and Stockert (2017) describe autonomy as respecting a client’s independence and right to determine a course of action. However, autonomy does not mean that clients can do whatever they want. Autonomy means the following:
Yoder-Wise (2019) describes autonomy as follows:
“The principal of autonomy addresses personal freedom and self-determination, the right to choose what will happen to oneself as well as the accountability for making individual choices.”
We expect people to respect our rights, and we respect their rights as long as their rights do not interfere with someone else’s rights.
For clients to make an autonomous decision, they must have all the facts without leaving out information to influence the decision in a particular way. For example, the nurse may unintentionally (sometimes intentionally) influence the client’s decision by repeating what the health care provider has suggested is best for the client (“The health care provider would not have suggested the treatment if they did not think it best for you”).
There is also a fine line between autonomy and abandonment. Excessive control means interfering too much in a client’s life. Not interfering enough results in neglect of the client. Here are some examples:
More information is needed in both situations to determine if more or less interference is recommended.
Role of Privacy in Autonomy
Privacy is both an ethical and a legal issue. Autonomy includes a client’s right to privacy. This is the reason your instructor asks a client directly for permission to allow SPNs/SVNs to observe a particular treatment or to do a procedure. Similarly, the instructor checks with the client before assigning a student to give nursing care. In some cases clients can sign on admission a consent to have students from all disciplines participate in their care. The client has the right to refuse care from any practitioner, including the student nurse. Privacy includes the right to choose care based on personal beliefs, feelings, or attitudes. It includes the client’s right to decide what is done to their body (accepting or rejecting treatment or exposure of the body). As an SPN/SVN, you respect the client’s decision. When giving care, avoid exposing the client needlessly in the course of care. This is an invasion of privacy.
Role of Culture, Religion, and Personal Values in Autonomy
Culture or a religion-based belief system may be contrary to the accepted medical ethics. Examples of decisions based on religion and culture include the following:
- • The client, a Jehovah’s Witness, could benefit from a blood transfusion for severe blood loss. The adult client has refused because a blood transfusion is prohibited by his religion (religion based).
- • If the client is an underage child, the parents may forbid the blood transfusion on religious grounds. The health care provider can decide to go to court to ask the court to overrule the parents’ decision. An underage child is too young to understand all the facts to make a decision required for informed consent. Parents can authorize treatment for what is appropriate for their children up to a certain age. In this case the health care provider has decided that the value of beneficence is greater than the value of respect for the parents’ autonomy. The court is the greater authority and will decide if the health care provider can transfuse the child.
- • The client, a young woman, is diagnosed with breast cancer. Her husband has received a complete explanation from the health care provider about her illness, alternatives for each treatment, anticipated effects, possible side effects, and prognosis with each treatment. Her husband will not permit any treatment to take place (culture based).
The client’s personal values may also be opposed to accepted medical ethics. The following is an example of a personal value-based decision: - • A client in their late sixties is diagnosed with advanced cancer of the colon. They have has refused omit treatment, even though he understands that although not curative, the surgery could result in less discomfort for a period and more time to live (personal value based).
Fidelity (be True)
Fidelity challenges each practical/vocational nurse to be faithful to the charge of acting in the client’s best interest when the capacity to make free choice is no longer available to the client. This does not include rescuing behaviors and becoming paternalistic in making decisions for vulnerable clients (legal competency will be described in Chapter 7). As a nurse, you must differentiate between your feelings and choices regarding an issue and the feelings and wishes of the client. These points are foremost in making a decision. Charting the client’s feelings and wishes as expressed, without your personal interpretation, provides information for the health care provider when important decisions need to be considered. Examples of breaching fidelity include the following:
- • Discussing a client in a public area such as the cafeteria, an elevator, at home, or when you are out with friends. Never mention a client by name or discuss any specific client characteristics or a detailed plan of care. These activities could allow individuals to conclude who you are speaking about due to the unique characteristics shared. In doing so, fidelity and confidentiality (a legal term) would both be compromised, as would the client’s dignity. The action says the client has limited worth in the eyes of the nurse and chips away at the client’s dignity.
- • You overhear LPNs/LVNs speaking disrespectfully about an obese client and complaining about how difficult it is to move them. What will you do in response to this discussion? Explain why you will take the action you have chosen. Is it an ethical response?
- • A student practical nurse shared a personal experience that sharpened their awareness of the meaning of fidelity. During the first day of the mental health rotation, they saw their neighbor, now a client, in the day room. The SPN’s spouse worked with the client. One day the neighbor did not come to work. The boss offered no information about what happened. Being a close-knit neighborhood, the SPN’s spouse, other workers, and neighbors speculated with great concern about the missing worker. Seeing the neighbor on the psychiatric unit was a shock, and the SPN did not know how to approach them.
- • The SPN asked the instructor for assistance. The instructor suggested that the SPN approach the client and let the neighbor know that they recognized them but reassure them that the SPN would not tell anyone about them being hospitalized. The SPN was also to tell the client that not telling anyone outside of the hospital was part of their nursing education and duty. As a SPN they must abide by the Health Insurance Portability and Accountability Act (HIPAA) guidelines. That took care of the discomfort for both the SPN and the client regarding their hospitalization.
- • The class after the clinical day was about fidelity and confidentiality (a legal concern). The SPN was sure they would never breach their promise not to talk about clients, except to the health care team and the instructor. That evening at dinner with their spouse, the SPN decided their spouse should know because of their concern for their coworker. The SPN made the spouse promise not to tell anyone about the client, and the spouse agreed.
- • Later that evening, while they were grocery shopping, the SPN was in another aisle, and heard their spouse tell someone, that their spouse was a SPN and that their neighbor was a client at the psych hospital and asked them not to tell anyone. The SPN breached confidentiality, an ethical and legal matter. They also started a chain reaction of “I’ll tell you, but you can’t tell anyone.” This constituted both an ethical and legal breach of confidentiality. The client’s best interest (fidelity) was not served.
You alone make the decisions regarding what you do when you are away from the clinical area and the immediate support and supervision of the instructor. In a sense, fidelity sits on your shoulder, to ignore or to embrace. To ignore creates an ethical dilemma and a potential legal consequence. Dismissal from school or termination from a job can be the end result.
Justice (fair to All)
Justice means that SPNs/SVNs and LPNs/LVNs must deliver fair and equal treatment to all clients, recognizing and avoiding personal bias. For example, each client with the same diagnosis should receive the same level of care. Being fair does not mean giving every client the same things. It means treating them all the same (i.e., with dignity and respect). As a nurse, you make daily decisions to provide the highest quality of care possible.
Personal bias can cloud our vision as nurses. Identifying hidden bias can assist the LPN/LVN in providing justice to all clients. For example, if the clients on your floor in the hospital represent different levels of wealth, social status, culture, religion, and moral and value systems, but all of them are acutely ill.
Consider the client who has Kaposi sarcoma, a defining component of AIDS. Do you classify AIDS as a life-threatening illness or as a retribution for behaviors you consider immoral? If your personal ethics interfere with the care you give, you may find yourself giving this client more time than needed and doing less than needed for other acutely ill clients or providing minimal care for the client and lavishing attention on those who “deserve the care.”
Consider a young, single mother who has five children and just found out she is pregnant. How you proceed can be impacted by a personal bias, assuming that she should have prevented this pregnancy. All clients must be treated equally. This is your ethical duty.
It is within your power to make decisions about daily issues related to justice. Be careful to hear hidden bias within yourself: “They are so young; so much living left to do”; “They had a full life already”; “They are an alcoholic; never took care of their kids”; and so on. Identifying a bias will assist you in providing “just” care. Visit the following website to identify your hidden biases: https://implicit.harvard.edu/implicit/
As an SPN/SVN, you report clients’ comments regarding ethical matters to the RN. Final ethical decisions are not within the LPN/LVN scope of nursing practice. Recall also that ethics is what you ought to do; law is what you have to do.
Role of Beneficent Paternalism
We are including beneficent paternalism because it continues to be confused with the ethic of beneficence (do no harm). Beneficent paternalism is a disrespectful attitude toward the client and what the client has to contribute to personal care and recovery. It is an “I know what’s best for you” attitude that discounts the client’s knowledge of self. The following are examples of beneficent paternalism:
- • You conclude that this client fits into a “specific category,” discounting what the client wants you to know. Many medication errors could have been avoided if the nurse listened to the client when they stated, “That pill looks different to me.” The error may occur in part because of beneficent paternalism. When assisting to collect data, really hear what the client is trying to tell you.
- • You assist in developing the care plan without client input reflecting the nurse’s needs, not the client’s. Later on, you complain that the client is non-compliant and will not cooperate with the plan of care. Ask yourself: “Did the client know what the alternatives were for treatment?” and “Did the client have the opportunity to offer input into the plan and agree to what the care plan would be?” It is difficult for clients to cooperate when they are not empowered.
- • If the client has agreed to the plan of care, then encouraging the client to do what has been agreed upon is beneficence. However, if you are influencing the client into choosing one alternative treatment over another, it is paternalistic beneficence. If you find yourself saying, “I overheard the health care provider saying they think you should choose this treatment” or “My husband chose the treatment and he is doing great,” you are actively influencing the client’s decision (paternalism).
- • If the client asks your opinion for the choice, and you respond with your choice (“Well, if I were you, I would . . .”) instead of saying, “The health care provider explained the alternatives for treatment and the possible side effects of each, and it is for you to decide what is best for you.”
Beneficent paternalism is justified only in extreme circumstances and is most often a medical decision (e.g., a health care provider approaching the court to be allowed to do a potentially lifesaving procedure when parents have refused to sign an authorized treatment form for the child).
To avoid paternalism with new mothers, a lactation counselor at a public health nursing, seminar, knowing the evidence (i.e., Baby-friendly Hospital Initiative), may present the following method (WHO, 2015): “I wish all women would breastfeed their babies. The value to both mother and child is based in evidence. I present the facts and respond to their questions, but the final decision belongs to the mother. I respectfully support their decision.” As an LPN/LVN, evidence should always guide your decision-making and education strategies with clients and the community, while respecting individual autonomy and avoiding paternalism.
Paternalism and Women’s Health
The issue of paternalism toward women in medical research and receiving health care is slowly changing through the efforts of women themselves and the advocacy of nurses. The term paternalism is derived from a Latin word that means “father” (i.e., father knows best). In the health care system, it can be interpreted as “the health care provider knows best because of their superior knowledge.” Because the word is derived from the Latin word pater, some may believe that men know better than women.
Health care providers define what is considered ill health for women. Anything that is normally different from men is considered an illness and requires the health care provider’s intervention. Because women are different from men biologically, medicine has defined what is normal for women as being abnormal. For example, menstruation, pregnancy, and menopause have been defined in the past as ill health instead of normal, healthy processes.
Although this trend still can exist, great strides have been made in women’s health care. Many factors have contributed, including the increase in female health care providers and empowerment of nurses and females in general in the United States. Accomplishments have been realized; however, clear signs remain as women continue to average 82% of the total income of their male counterparts for similar jobs. This represents an almost flat trend since 2004 (BLS, 2017).
Advocacy for women remains an important responsibility. As a nurse, speak up when you see decisions being made based on incomplete information (e.g., the health care provider or other health care worker not really listening to a female client). Review Chapter 9 regarding assertiveness and your responsibility. It reminds you that an aggressive, rude approach does not gain you anything except a bad reputation among your peers and clients. Practice assertiveness and remember that change will occur slowly. Many female clients are already experiencing a change and assertively stating their needs. Nurses who advocate for their female clients assist in this process of reducing a paternalistic attitude toward women, one client at a time, as the need arises.