Cultural Uniqueness, Sensitivity, and Competence
On completing this chapter, you will be able to do the following:
- 1. Define in your own words the following terms: culture; cultural competence; cultural diversity; cultural uniqueness; ethnocentrism; cultural bias; cultural sensitivity; stereotype.
- 2. Explain in your own words nine basic daily needs of all persons.
- 3. Describe your culture in the areas of family; religion; communication; educational background; economic level; wellness, illness, birth, and death beliefs and practices.
- 4. Identify how all persons are unique and similar using Giger and Davidhizar’s Transcultural Model (2002).
- 5. Explain in your own words the philosophy of individual worth as it applies to health care.
- 6. Explain the importance of awareness, knowledge, sensitivity, humility, and listening in providing client-centered care.
Key Terms
assimilation (ă-SĬM-ă-LĀ-shŭn)
complementary and alternative medicine (CAM) (KŎM-plĕ-MĔN-tĕ-rē, ăl-TŬR-nă-tĭv)
cultural competence (KŎM-pĭ-tĕns)
cultural diversity (dĭ-VŬR-sĭ-tē)
cultural sensitivity (SĔN-sĭ-TĬV-ĭ-tē)
customs (ĕn-KŬL-chŭr-Ā-shŭn)
discrimination (ĕn-KŬL-chŭr-Ā-shŭn)
enculturation (ĕn-KŬL-chŭr-Ā-shŭn)
ethnocentrism (ĔTH-nō-SĔN-TRĬZ-ĕm)
nonjudgmental (NŎN-jŭj-MĔN-tăl)
worldview
You have chosen a career that will give you an opportunity to meet people who are different from you.
- • Some of these people will be your clients.
- • Some will be your peers at school.
- • Some will be your coworkers.
- • Some will be a different age than you.
- • Some will belong to a different social class.
- • Some will have disabilities.
- • Some will have different health care beliefs about what causes them to get sick.
- • Some will have different values.
- • Because of ethnic group status, some of your clients and coworkers will have different cultural backgrounds.
- • Regardless of cultural background, some differences will be the result of a growing diversity in individual and family lifestyles.
You will discover that people think, feel, believe, act, and see the world differently from you and your family and friends. Log on to www.minoritynurse.com/about/index.html to check out featured articles about issues facing nurses.
Review the standards of the National Association for Practical Nurse Education and Service, Inc. (NAPNES) at www.napnes.org, and the National Association of Licensed Practical Nurses (NALPN) at www.nalpn.org. You will note that both organizations have embraced statements that describe the need of the licensed practical nurse/licensed vocational nurse (LPN/LVN) to provide health care to all clients regardless of race, creed, cultural background, disease, or lifestyle. This is an ethical expectation.
Review your state’s Nurse Practice Act (NPA). You will find that failing or refusing to render nursing services to a client because of the client’s race, color, sex, age, beliefs, national origin, disability, or sexual orientation is listed as unprofessional conduct. The ethical expectation now becomes a legal mandate. Nurses could risk legal suits because of their ignorance of the culture of the client and resulting poor nursing judgment.
Not only do LPNs/LVNs need to provide care for all persons, but they also need to provide culturally competent care. Cultural competence is the continuous attempt of LPNs/LVNs to gain the knowledge and skills that will allow them to effectively provide care for clients of different cultures. Cultural competence is not gained by reading a chapter in a textbook or by looking up a culture in a reference book. It is developing an awareness of different cultures (cultural sensitivity) and continually learning about people who are different from you. Giger (2017) describes cultural competence as “a dynamic, fluid, continuous process whereby an individual, system, or health care agency finds meaning and useful care delivery strategies based on knowledge of the cultural heritage, beliefs, attitudes, and behaviors of those to whom they render care” (p. 7).
When differences are identified in a health care situation, the LPN/LVN needs to suggest adaptations to the plan of care so the plan recognizes these differences. In doing so, the client will be encouraged to follow suggestions, avoid treatment failures, and return to health as quickly as possible. Practical/vocational nurses will then be able to say that they have truly met the client’s needs. The U.S. Department of Health and Human Services, Office of Minority Health (2019) provides a free E-learning program, Culturally Competent Nursing Care: A Cornerstone of Caring, grounded in the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care. These standards aim to advance health equity. Improve quality and help eliminate disparities (U.S. Department of Health and Human Services, 2019). Visit https://ccnm.thinkculturalhealth.hhs.gov/ to access this training.
Definition Of Culture
Culture is a way of life. It is the total of the ever-changing knowledge, ideas, thoughts, beliefs, values, communication, actions, attitudes, traditions, customs, and objects that a group of people possess and the ways they have of doing things. Culture also includes standards of behavior and sets of rules to live by. Customs are the generally accepted ways of doing things that are common to people who share the same culture.
Characteristics Of Culture
An important point about culture is that it is learned behavior. The culture of a group is passed on from generation to generation. From the moment you were born, you began to learn about the culture of the group into which you were born. The process of learning your culture (the way your group does things) is called enculturation. A result of enculturation is a worldview that is generally shared by persons with the same cultural background. The worldview, or similar ways of seeing and understanding the world, becomes the reality of the group. This reality fills every aspect of life. It is a cultural bias (a mental leaning) that is never proved or questioned by the individual. The worth of everything, either within or outside the group, depends on whether or not it fits the worldview of the cultural group. One’s worldview can lead to ethnocentrism, prejudice, and discrimination, unless modified by knowledge and experience.
Socialization is the process by which a person of one culture learns how to function in a larger culture. Right now you are being socialized into the career of practical/vocational nursing. You are learning how to think and act like an LPN/LVN.
Danger: Ethnocentrism, Prejudice, And Discrimination
People who belong to the same cultural group may develop the attitude, through their worldview, that their way of doing things is superior, right, or better than that of groups with different cultures (ethnocentrism). The group uses its culture as the norm against which to measure and evaluate the customs and ways of others. The group can be uncomfortable with people who display customs and behaviors that differ from their cultural group. Ethnocentrism is common to all cultural groups. When intolerance of another cultural group occurs, prejudice results. When rights and privileges are withheld from those of another cultural group, this is called discrimination.
Avoiding False Assumptions
Nursing students sometimes think that somewhere there is a manual that will tell them how to care for people who are different from themselves. This type of approach can lead to false assumptions, which are called stereotypes. A stereotype is an assumption used to describe all members of a specific group without exception. It is an expectation that all individuals in a group will act exactly the same in a situation just because they are members of that group. Stereotypes ignore the individual differences that occur within every cultural group. Members of any culture may have modified the degree to which they observe the values and practices of the culture.
Think Like An Anthropologist!
Anthropologists are scientists who study physical, social, and cultural characteristics of human groups. It is helpful to understand how these scientists conduct their studies:
- • Anthropologists start the study of cultural groups by identifying common trends in a cultural group.
- • These common trends found in the group are called “generalizations.”
- • Then anthropologists gather data to determine if the common trends (generalizations) apply to all individuals within that cultural group.
Automatically generalizing cultural information about a group’s health practices to one person in that group might be drawing a wrong conclusion. Does the individual follow the traditional practice of the group? Has the individual rejected the practice? Does the individual use the practice only in certain situations? If so, what situations? Is the person an immigrant? How recently?
When people immigrate to a new country, culturally different groups do adopt some of the culture of the new country. The process of giving up parts of their own culture and adopting parts of the culture of the dominant group is called assimilation. Complete assimilation, however, rarely occurs. Members of the generations that follow the original immigrants may retain some elements of their original culture in addition to assimilating parts of the new culture. For these reasons, generalizations help explain observed behavior, but they do not predict behavior.
Each Culture And Person Is Unique
Remember that each individual is unique and a product of their experiences, cultural norms, and beliefs (Giger, 2013). Giger and Davidhizar’s Transcultural Model (1991) provides a framework for caring for clients in a variety of settings focused on their unique personal identity. Giger and Davidhizar (1990, 2002, 2017) describe six cultural phenomena that are critical to the assessment of clients in providing data necessary for decision making in providing culturally competent care. See Fig. 10.1 for details. These six phenomena include communication, space, social organization, time, environmental control, and biological variations. A brief discussion follows.
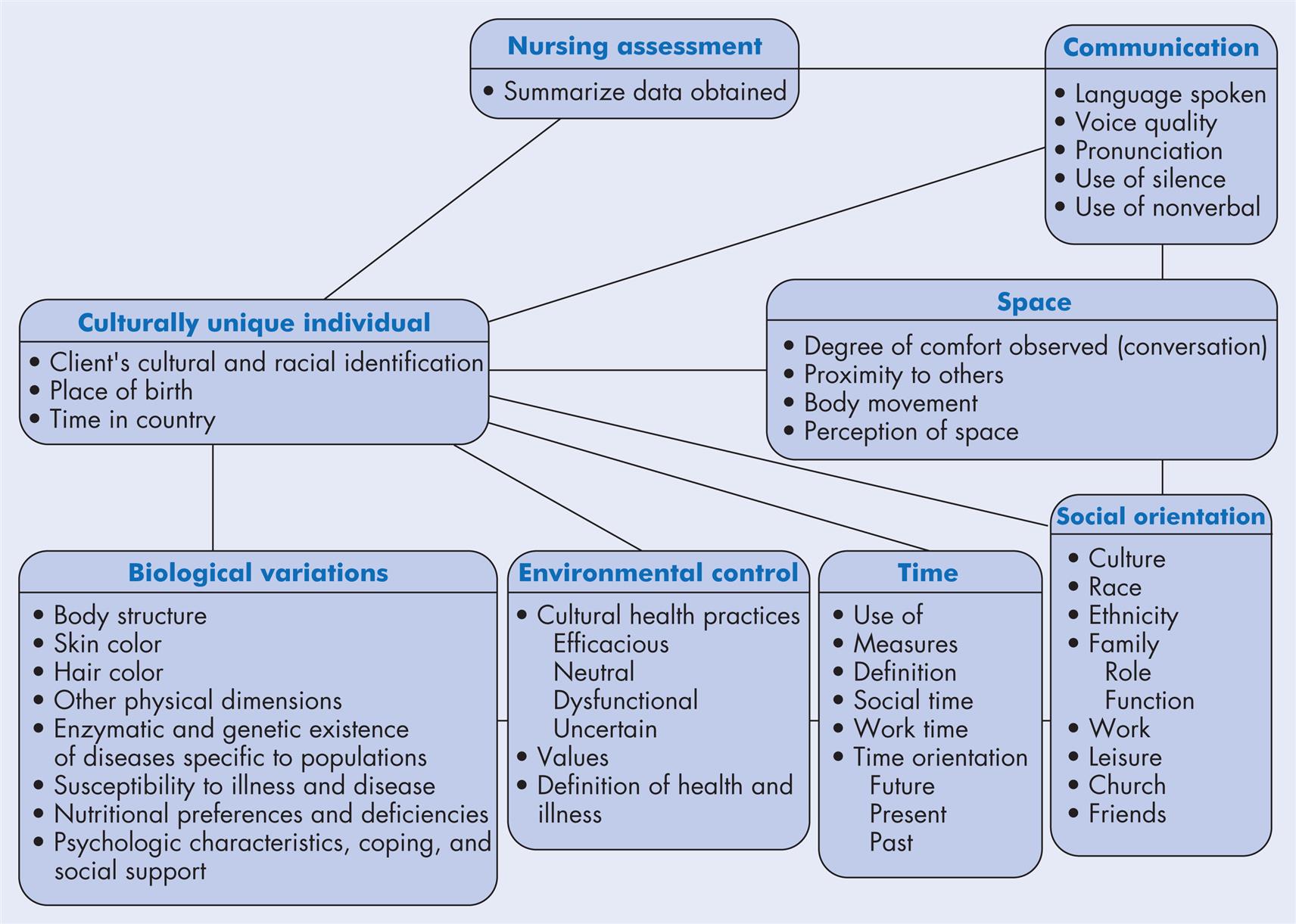
Communication
Communication differences include language spoken, verbal behaviors (i.e., voice quality and pronunciation), nonverbal behaviors (e.g., direct eye contact, touching), and the use of silence. Communication is a cornerstone to effective client care. Thus, research supports the critical need for an interpreter, when a nurse and client speak a different language. Communication and language assistance is listed as one of the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care (U.S. Department of Health and Human Services, 2019). The purpose of CLAS is to “provide effective, equitable, understandable, and respectful quality care and services that are responsive to diverse cultural health beliefs and practices, preferred languages, health literacy, and other communication needs” (U.S. Department of Health and Human Services, 2019). The standards highlight the need to ensure the competence of an interpreter among other initiatives.
Potential Health Insurance Portability and Accountability Act (HIPAA) violations should be considered if asking family to assist. In most cases, children should not be used as interpreters because of the subject matter; women may also not be acceptable because of the cultural view of women in some cultures (Cherry and Jacob, 2019). Your local community may offer interpreter services. In addition, entities such as language line exist to meet this need (www.languageline.com). The LPN/VPN should review institutional policy and procedure for process and resources and implement accordingly.
Space
Space refers to the degree of comfort when speaking or interacting with people around us in a two person or a group setting. For example, most nurses generally feel comfortable with a small space zone of 0 to 18 inches (Cherry and Jacob, 2019). This can be necessary for the delivery of care to a client. This can vary significantly in some cultures. Nurses need to assess this aspect of culturally sensitive care when establishing a relationship with a client.
Social Organization
Social organization refers to the family unit, the client’s affiliated religious or ethnic groups, and their political views. Family can be interpreted differently across cultures. For example, you may have heard a person of another culture call someone their sister, even though they may not be related by blood but instead by friendship or experience.
Time
Time orientation differs across cultures. People and cultures can be described as present, past, or future oriented. People who live in the present live in the “moment.” They move on to the next task when the time is right (Cherry and Jacob, 2019). This can contrast greatly with someone who lives in the past or future. People living in the past often look to their ancestors for wisdom and guidance and value previous experiences. Punctuality is often not a priority for those who have a past oriented time reference. Lastly, those who live in the future are generally punctual and strong planners. Long-term health care goals are important.
Environmental Controls
Environmental controls refer to whether the person has an internal (power is within them) or external locus of control (fate plays a large role in outcomes). The person’s belief or lack of belief in supernatural forces can also vary across cultures.
Biological Variations
Biological variations across cultures can be visible or invisible. Genetic tendencies related to body build and body structure, hair type, eye shape, and skin characteristics can be easily visible. In contrast, nutritional variations and incidence of specific diseases can be invisible. For example, rates of cardiac disease can differ across cultures.
These six cultural phenomena should be an important component of a health care team’s assessment of all clients, given our diverse society. Box 10.1 provides a detailed assessment model (Giger and Davidhizar, 1991) for the LPN/VPN to use. This will assist in providing data needed by the health care team to develop a culturally competent plan of care.
Knowing Yourself
According to the Standards of Practice for Culturally Competent Nursing Care (Douglas et al., 2011), critical reflection is defined in the following way: “Nurses shall engage in critical reflection of their own values, beliefs, and cultural heritage to have an awareness of how these qualities and issues can affect culturally congruent nursing care” (p. 318). Thus knowing yourself is a critical step in providing culturally competent care.
What Makes You Unique?
To become aware of different cultures, you need to be aware of yourself as a person. Several activities are included in this chapter to help you with cultural self-awareness. The exercises also help you develop an awareness of cultural differences with peers.
How Many Hats Do You Wear?
Most people have several roles in life. People speak of “wearing many hats” or “having a full plate.” Some of these roles are played out individually, one at a time, and others are performed simultaneously. Identify the various roles you play in your life: home, work, family, friends, culture, etc.
What We Share In Common
Because of our genes, each of us is different from every other person in the world. (The only exception is identical twins.) Before you start to think about the differences among people, it is a good idea to think about what people have in common.
Knowing Others: Cultural Diversity
In the nineteenth century, waves of immigrants from all over the world came to the United States. The United States was eventually called a melting pot, meaning that these immigrants had given up their native cultures and adopted the culture of the American people.
The 2010 U.S. Census included the categories of Hispanic/Latino/Spanish origin (if so, indicate if Mexican, Mexican American, Chicano, Puerto Rican, Cuban, Argentinean, Colombian, Dominican, Nicaraguan, Salvadoran, Spaniard, and so on), white, black, African American or Negro, American Indian or Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian (Hmong, Laotian, Thai, Pakistani, Cambodian, and so on), Native Hawaiian, Guamanian or Chamorro, Samoan, other Pacific Islander, or other race. Effective July 2019, data.census.gov will be the primary way to access Census Bureau data including Census 2020. If current trends continue, the U.S. Census Bureau predicts that minorities will make up 57% of the U.S. population by 2060 (United States Census Bureau, 2012).
In 2017, the Census Bureau’s American Community Survey reported the following distribution: 61% of the U.S. population is white, 12% black, 18% Hispanic, 6% Asian, 1% American Indian/Alaska Native, and, 1% Native Hawaiian/other Pacific Islander and 3% two or more races (Keiser Family Foundation [KFF], 2019). The concept of the melting pot has been replaced by the concept of cultural diversity, which refers to the many differences in the elements of culture in groups of people in American and Canadian society.
Cultural diversity goes beyond racial and ethnic groups. As an LPN/LVN, you need to define this concept more broadly so culturally diverse groups can also mean single parents, people who live in poverty, homosexuals, bisexuals, the wealthy, the poor, the homeless, the elderly, and people with disabilities.
The concept of race as a means of categorizing people by biologic traits has come under attack by social scientists. These scientists suggest using ethnicity as a more accurate means of capturing the great diversity found in over 7.753 billion people in the world (World Bank, 2021). Members of ethnic groups are a special type of cultural group, composed of people who are members of the same race, religion, or nation, or who speak the same language. They derive part of their identity through membership of the ethnic group. Examples of ethnic groups in the United States include Italian Americans, African Americans, American Indians, Asian Americans, German Americans, Mexican Americans, Jewish Americans, Arab Americans, Greek Americans, Finnish Americans, and many more.
Importance Of Cultural Diversity
Health care today and into the future needs to be able to accommodate clients of many different cultural backgrounds. Failure to develop sensitivity to and competence in handling this diversity could lead to misunderstandings between you and the client, resulting in stress for both. The plan of treatment for the client could fail. You could make false assumptions based on generalizations. You might label clients as difficult or uncooperative when their lack of cooperation with the plan of care could be related to a conflict with their personal health belief system. Clients may experience less-than-adequate care when cultural diversity and the differences it represents are overlooked or misinterpreted.
Philosophy of Individual Worth
The philosophy of individual worth is a belief shared by all members of the health care team. The philosophy includes the uniqueness and value of each human being who comes for care, regardless of differences that may be observed or perceived in that individual. LPNs/LVNs need to realize that each individual has the right to live according to their personal beliefs and values, as long as they do not interfere with the rights of others. Each individual deserves respect as a human being.
LPNs/LVNs need to guard against making judgments about people who are culturally different. This does not mean you must adopt differences as part of your behavior. It means being open-minded and nonjudgmental. It means taking the difference at face value, accepting people as they are, and giving high-quality care. Be aware of your own attitudes, beliefs, and values and hidden biases as they affect your ability to give care. If you do identify biases, see them for what they are. Become sensitive to cultural differences, and acknowledge that they exist. Gather knowledge about them so you can work on trying to modify your biases and provide more culturally competent care.
Learning About Cultural Diversity
How to Begin
You have been given exercises that help you to discover your own uniqueness and that of others, as well as similarities. Unless you understand your own culture, it will be difficult to understand the culture of others. You need to look inside yourself to learn about your own cultural beliefs, values, and worldview and the influence they have on how you think and act. Some elements of your culture are obvious, such as your language, celebrated holidays, and how and what you eat. However, other aspects of your culture are hidden. Elements such as aspects of communication, beliefs, attitudes, values, sex roles, use of space, concept of time, structure of the family, and family dynamics may be more difficult to recognize and discuss. Some areas of cultural diversity may be taken for granted in client situations. Examples include food preferences, religion, educational background, economic level, wellness and illness beliefs and practices, the birth experience, and terminal illness and death beliefs and practices.
The first step to developing knowledge about client differences in these areas is to become aware of and explore your cultural patterns in these areas. Read the general information about each area below. Develop an awareness of your own cultural patterns in these areas by answering the group of statements or questions included with each area. Sharing this information with peers will highlight the cultural diversity that exists in your nursing class, regardless of cultural background. The questions also provide examples of areas to be discussed with clients when collecting data about their personal beliefs and health practices.
Areas Of Cultural Diversity
Family Structure
No matter what culture is being discussed, the family is the basic unit of society. The role of the family is to have children, if desired or as they come, and to raise them to be contributing members of the group. Actual child-rearing practices vary from culture to culture. Families generally socialize the young to the culture of the group. They meet the physical and psychological needs of the young in culturally specific ways. Some cultures expect only the nuclear family (mother, father, and children) to live in the same house. Others may expect the extended family (the nuclear family plus the grandparents and other relatives) to do so.
The single-parent family continues to challenge the traditional nuclear family as the typical family structure. A parent may become a single parent on the death of a spouse, by electing not to marry at the time of pregnancy, or by divorce. The blended family and same sex parent families represent a growing trend in our society. Health care workers who have not been in the same situation may be unaware of, and insensitive to, the way of life of these various types of family.
Food Preferences
All cultures use food to provide needed nutrients. However, what they eat, when they eat, and how they eat differ vastly by cultural group. Knowledge of nutrition as a science differs by culture. It is interesting that the soil of some cultures (e.g., Mexico) encouraged the growth of two complementary foods that together make up a basic protein source (corn and beans) and became a staple of that culture’s diet. Specific foods in different cultures have different meanings. All cultures use food during celebrations. Through generations of experience, different cultures have learned to use different foods to promote health and cure disease.
Religious Beliefs
Religious beliefs are personal to the individual. Religion is an important aspect of culture. Religion can have different meanings in people’s lives. For some, religion is a brief, momentary, and sporadic part of daily life. For another person, it may influence every aspect of life and have a profound effect on personal outlook and on how one lives his or her life. For others, religion may not play a part in their lives at all. Chapter 11 deals with spirituality and religious differences. There is a close relationship between religious beliefs and the concept of wellness and illness in some groups. LPNs/LVNs need to be aware of their own religious beliefs, obligations, and attitudes. They need to know whether or not these beliefs and attitudes influence the care that is given to clients.
Concept of Time
Some people follow clock time. An hour has a beginning and an end (after 60 minutes). People who follow clock time eat, sleep, work, and engage in recreational activities at definite times each day. Other people live on linear time. For them, time is a straight line with no beginning and no end. People who follow linear time eat when they are hungry and sleep when they are tired.
Communication
Chapter 8 introduced you to the types of communication and potential barriers to the communication process. As mentioned earlier in this chapter, a major barrier to communication in health care is when the client or nurse speaks a different language. A person’s language gives a view of reality that may differ from yours. For example, in English, the clock “runs,” but in Spanish, it “walks.” This illustrates the different concept of time between the two cultures. For a person who speaks English as a first language, time could move quickly, and there may be a rush to get things done. For some who speak Spanish as a first language, time may move more slowly. The following is a list of areas of communication that may vary for people who are culturally different.
Forms of hellos and good-byes
- • You may greet your client and want to get right down to business.
- • The client might expect some light conversation before getting to the matter at hand.
- • In some cultural groups, people take an hour to say good-bye, whereas people from other cultures may get up and leave without saying anything.
Appropriateness of the situation
Confidentiality
- • All information the client gives the nurse is considered confidential.
- • Some clients do not want their spouse questioned or informed about their problems of the reproductive organs. They fear the spouse may think they are less desirable sexually.
- • See Chapter 7 for HIPAA-related content.
Emotions and feelings and their expression
- • Emotions are universal, but the cues to those emotions vary considerably. A lack of awareness of this fact can cause unnecessary stress between the client and the nurse.
- • In some cultural groups, people cannot display affection in public, show disapproval or frustration, or vent anger.
- • You may show dissatisfaction with other members of the health care team by approaching them directly, whereas some team members may show dissatisfaction with you by being polite to your face but then complaining about you to the rest of the staff. The same applies to your peers.
Pain expression
- • Pain has two parts: sensation and response. All individuals experience the same sensation of pain.
- • One’s culture influences the definition of pain and the response to the sensation.
- • Pain is whatever the person says it is. It exists whenever the person says it does.
- • One’s culture provides guidelines for approved ways of expressing one’s response to the pain sensation and ways to relieve the pain.
- • Some cultures teach individuals that it is acceptable to cry, moan, and exhibit other behavior that calls attention to the pain. These behaviors may be considered a cure for pain in their culture.
- • Other cultures encourage uncomplaining acceptance of pain and passive behavior when pain is experienced (stoic behavior).
Tempo of conversation
Meaning of silence
- • Silence can mean anything from disapproval to warmth, but generally it does not indicate tension or lack of rapport.
- • Silence can be difficult for some nurses to tolerate. Resist the temptation to jump in at a pause in the conversation by forcing yourself to concentrate on listening and reflecting on the discussion.
Educational Background
The 2003 National Assessment of Adult Literacy assessed the English health literacy of adults in the United States and found that 14% do not have basic health literacy skills (able to understand a simple health pamphlet), whereas 22% have these skills (able to understand a more complex health pamphlet). Differences in educational background and literacy need to be taken into consideration when teaching clients. According to the U.S. Department of Education (2019), one in five U.S. adults has difficulty when completing tasks that require comparing and contrasting and making low-level inferences. This equates to 43 million Americans. Of this 43 million, 8.4 million are considered English illiterate. When in the clinical area, be sure to assess the client’s level of understanding and adapt explanations accordingly.
Economic Level
Economic level is often related to educational background. Sociologists use these two factors to determine the social class of individuals. You will meet clients who are very wealthy and clients who are at or near the poverty level. Others have midlevel incomes. Clients’ annual incomes can impact the type of house they live in, the neighborhood where they live, the availability of food, and the ability to participate in certain types of preventive health care. LPNs/LVNs need to take economic level into consideration while reinforcing client teaching and should adapt their approach accordingly when needed.
Wellness and Illness Beliefs and Practices
Wellness and illness can have different meanings for persons who are culturally different. Wellness and illness are relative terms. What is good health to one person can be sickness to another. Wellness may not be a high-priority matter to some clients.
Preventing illness. Some clients believe that illness can be prevented; they practice elaborate rituals and engage special persons to carry out those rituals in an attempt to prevent disease. Other clients look at prevention as an attempt to control the future; they may consider this an impossible feat in the way they view their lives. They may wonder about the necessity of making a trip to a health care provider for preventive care, such as immunizations or cancer screening. Others may think prevention is tempting fate and following through with prevention is risky.
Curing illness. When disease does strike, some people blame pathogens (germs), some blame spirits, and others blame an imbalance in the body. Some cultural groups have folk medicine practices, such as rituals, special procedures (e.g., rubbing the skin with the edge of a coin to release the toxins causing illness), and special persons in the group to cure disease (e.g., health care provider, herbalist, shaman). Some groups believe that special foods or food combinations (e.g., “cold” foods for “hot” illness) and herbs (e.g., Echinacea and Feverfew) can prevent or cure illnesses. Others see no relationship between diet and health.
Complementary and alternative medicine. The dominant health system in the United States is biomedicine (Western medicine). Biomedicine focuses on symptoms, with the goal of finding the cause of a disease and then eliminating or relieving the problem. Over 50% of Americans seek methods that avoid side effects from medications and treatments and/or that focus on the whole body and not just symptoms when treating disease. They are spending billions of dollars a year, mostly out of pocket, on complementary (used in conjunction with biomedical treatments) and alternative (a substitute for conventional medicine) medicines.
Complementary and alternative medicine (CAM) focuses on assisting the body’s own healing powers and restoring body balance. The diversity of non-Western health care practices among the many cultural groups in the United States has helped increase the interest and use of CAM. Common examples include massage therapy, acupuncture, or the use of herbs. The National Center for Complementary and Alternative Medicine (NCCAM), renamed by Congress the National Center for Complementary and Integrative Health (NCCIH), is part of the National Institutes of Health. NCCIH conducts research and evaluates the effectiveness and safety of CAM. NCCIH’s website (https://nccih.nih.gov/) provides information about CAM.
Modesty. Individuals in some cultures are embarrassed when they have to discuss bodily functions or allow certain body parts to be examined. Hygiene practices vary according to beliefs, living conditions, personal resources, and physical characteristics.
Mental illness. Some cultural groups attach a stigma to mental illness and psychiatrists but are accepting of impairments to physical health. Other groups believe that the mental symptoms manifested are a healthy reaction to an emotional crisis. Yet others believe that the mind and body are united and are not separate entities. These cultures may have traditional healers who are experts at healing both the mind and the body. Some people may seek out traditional healers to heal the mind, while at the same time consult Western medicine to heal the body.
Pregnancy and Birth Beliefs and Practices
Different cultures welcome a new member into the world in different ways. The Try This: Cultural Patterns: Pregnancy and Birth Beliefs and Practices box helps you to identify your own beliefs about pregnancy and birth.
Terminal Illness and Death Beliefs and Practices
Generally, death and terminal illness bring out strong emotions in most people. Be aware that some cultures have special taboos and prohibitions when a death occurs. Roles that family and friends carry out at the time of death may vary. There are many differences in the way different cultures handle terminal illness for a member. When death does occur, the rituals practiced are numerous and varied. It is important to listen to your clients and family to learn of their needs during terminal illness and death.
Increasing Your Knowledge Of Culturally Diverse Groups
No one can be an expert on every culture in the world. Even those who are experts on a particular culture do not like being labeled as such. These people are aware of the ever-changing nature of cultures and of the important individual variations that occur within any cultural group. Experts are always cautious about stereotyping persons in any particular cultural group.
Diversity Profiles Of Predominant Cultural Groups In The United States
At the beginning of the twentieth century, the majority of immigrants to the United States were of European ancestry. This trend has changed and is impacting the overall trend of the U.S. population. According to the 2017 Census Bureau’s American Community Survey 61% of the U.S. population is white, 12% black, 18% Hispanic, 6% Asian, 1% American Indian/Alaska Native, and ,1% Native Hawaiian/other Pacific Islander, and 3% two or more races (Keiser Family Foundation [KFF], 2017).
Developing Cultural Competence In Health Care Situations
You have started the long road to becoming an LPN/LVN who gives culturally competent care. Up to this point, participating in this chapter has given you the opportunity to do the following:
- • Identify your culture and its strengths and limitations.
- • Recognize how your culture affects your thinking and behavior.
- • Discover how persons are similar despite their cultural group.
- • Discover how persons are unique despite their cultural group.
- • Gain knowledge of the three major health belief systems to increase your awareness of different worldviews about the cause, treatment, and prevention of disease.
- • Gain awareness of ethnocentrism that can help you respect the health beliefs and practices of others when they are different from your own.
- • Learn to be flexible when your values and assumptions differ from those of your clients.
Your next step to cultural competence is to develop a knowledge base for a few cultures that are different from yours.
Identify Your Agency’s Cultural Groups
Identify the cultural groups in your community that are served by local health care agencies. Use the following blank lines to list the groups. It is necessary to be knowledgeable about the cultural groups that you frequently come across in your community.
Modify Your Work Setting
The health care environment can be made more “welcoming” to culturally diverse clients. Many of these changes require little cost or time to implement, but the results can promote better health and compliance among culturally diverse clients. Box 10.2 presents suggestions for modifying the workplace environment for the practical/vocational nurse working in health care agencies with culturally diverse clients.
Care Planning For Culturally Diverse Clients In Your Service Area
Imagine this scenario: a 60-year-old client requires an urgent surgical procedure. The health care provider is frustrated as the consent form still is not signed and surgery is imminent. This client speaks limited English. You are struggling to determine why the consent is still not signed. Through discussion the husband explains the decision-making role of the elders important to their family’s cultural lifestyle and research, using the Dimensions of Culture website (www.dimensionsofculture.com), you conclude that people often need extra time to sign consent forms, as discussion with elders and the family (clan) needs to occur. Given this information, you assist the client in contacting their elders, the health care provider obtains consent, and surgery occurs as planned.
Each client of a different culture needs to have data gathered regarding activities of daily living (ADLs) and personal health beliefs and practices. Develop a fact sheet for collecting data for a client.
Use websites such as https://www.thinkculturalhealth.hhs.gov/ to access general information about caring for different cultural groups. This information is helpful when you are dealing with a client from a culture with which you are not familiar because they offer general information about, for example, wellness and illness beliefs and practices, nutritional preferences, and communication issues. These quick sources of generalities of various cultural groups are a starting point for learning which topics to include when collecting data (assessing) that must be clarified and validated with the individual client. Remember that general group behavior sometimes explains observed behavior but it is not predictive of individual behavior. Assumptions based on generalizations should not be made. When using this information, avoid stereotyping your client. Use Box 10.3 as a guide to help you avoid falling into the stereotype trap.
Suspect cultural differences when a client is not following the plan of care, refuses treatment, labeled by some erroneously as a “problem” client and so on. Question the client about their ADLs and wellness and illness beliefs.
Adapting Plans Of Care For Culturally Diverse Clients
Jackson (1993) offers suggestions for finding out about clients’ health beliefs, along with guidelines for developing plans of care that incorporate those beliefs through a process with the client. Jackson points out that discovering specific health beliefs is easier if the nurse is familiar with a specific culture, but this is not absolutely necessary. Jackson suggests ways of co-creating a treatment plan with culturally diverse clients. The LPN/LVN can collaborate with the professional nurse to incorporate these beliefs into the client’s plan of care:
- 1. Discover the health beliefs of the individual. Be respectful and open minded when you question the client about the cause of the health problem, when it started, its severity, its course, the problems it has caused in the client’s life, and the treatment the client thinks will cure the disease. Avoid assuming anything. When you are unsure of anything, ask! In situations of cultural diversity, our clients are the teachers and we are the students.
- 2. Co-create treatment plans with the client. Avoid trying to change clients’ beliefs. Cultural health practices that can be deeply respected. Tradition means more than your word does, even though you are a representative of a health profession. Instead, involve the client in making decisions about his or her own care. Do so in a way that does not threaten the client’s beliefs and practices or conflict with them. Explain from the biomedical point of view the cause of the disease, how the disease alters the body, the role of treatment, and the expected outcome. Then compare the client’s belief system with that of biomedicine. All clients need to have this information to help ensure their cooperation with the plan of care.
- 3. Preserve the beliefs and practices that are helpful to the client. Starting in 1993, the Office of Alternative Medicine of the National Institutes of Health began to identify, study, and bring together the best healing practices of other cultures with those of Western medicine. In 1998, the National Center for Complimentary and Integrative Health was established to focus on determining the usefulness and safety of complementary and integrative health interventions and their roles in improving health and health care. Many of the beliefs and practices of non-Western systems of health beliefs have proved beneficial. Acupuncture and acupressure are now a common practice in the United States and many more alternative treatment modalities continue to emerge.
Collaborate with your professional nurse about clients’ practices that have not yet been researched or found effective. If the practices seem to help the client and do no harm, include them in the plan of care, regardless of your ability to see the benefit of the practice. These practices have special significance and meaning to some individuals, despite the fact that you may be unable to see how or whether they help. Box 10.4 provides an example of preserving the beliefs and practices that are helpful to the client. - 4. Repattern harmful practices. Harmful practices that are prevalent in Western society include smoking, diets high in fat, refined grains, and refined sugar, and lack of exercise which can cause high blood pressure and heart disease. Extreme dietary restrictions during pregnancy can lead to maternal toxemia and poor fetal development. Explain your reasons for opposing a harmful practice, and offer alternatives.
When LPNs/LVNs listen and learn with sensitivity and humility to all people they are on the road to delivering exceptional client-centered care.