Nursing Care of Women with Complications After Birth
http://evolve.elsevier.com/Leifer.
- 1. Define each key term listed.
- 2. Describe signs and symptoms for each postpartum complication.
- 3. Identify factors that increase a woman’s risk for developing each complication.
- 4. Explain nursing measures that reduce a woman’s risk for developing specific postpartum complications.
- 5. Describe the medical and nursing management of postpartum complications.
- 6. Explain general and specific nursing care for each complication.
- 7. Compare and contrast mood disorders in the postpartum period.
Key Terms
curettage (KYŪ-rĕ-tăhzh, p. 255)
endometritis (ĕn-dō-mē-TRĪ-tĭs, p. 257)
hematoma (hē-mă-TŌ-mă, p. 255)
hypovolemic shock (hī-pō-vō-LĒ-mĭk shŏk, p. 251)
involution (ĭn-vō-LŪ-shŭn, p. 256)
puerperal sepsis (pū-ĔR-pŭr-ăl SĔP-sĭs, p. 257)
subinvolution (sŭb-ĭn-vō-LŪ-shŭn, p. 256)
Most women who give birth recover from pregnancy and childbirth uneventfully. However, some experience complications after birth that slow their recoveries and may interfere with their ability to assume their new role. A woman can have any medical problem after a birth, but most complications related to childbirth fall into one of six categories:
The maternal mortality rate is defined as deaths from women while pregnant or within 42 days of being pregnant from any cause related to or aggravated by pregnancy or its management. The maternal mortality rate in the United States was 20.1 deaths per 100,000 births in 2019, with the leading causes including the following (Hovert, 2021):
These rates are 7.7 times higher among women over 40 years of age as opposed to those under 25 years of age.
Shock
Shock is defined as a condition in which the cardiovascular system fails to provide essential oxygen and nutrients to the cells. Postpartum shock related to childbearing includes the following:
The inherent danger of obstetric shock is that body compensation can mask the signs until the condition becomes life-threatening. The vigilance of the nurse can enable detection of early signs and then prompt intervention.
Hemorrhage
Postpartum hemorrhage is traditionally defined as blood loss greater than 500 mL after vaginal birth or 1000 mL after cesarean birth, resulting in signs or symptoms of hypovolemia. Because the average-sized woman has 1 to 2 L of added blood volume from pregnancy, she can tolerate up to these amounts of blood loss better than would otherwise be expected.
Most cases of hemorrhage occur immediately after birth, but some are delayed up to several weeks. Early (primary) postpartum hemorrhage occurs within 24 hours of birth. Late postpartum hemorrhage occurs after 24 hours and within 6 weeks after birth.
The major risk of hemorrhage is hypovolemic (low-volume) shock, which interrupts blood flow to body cells. This prevents normal oxygenation, nutrient delivery, and waste removal at the cellular level. Although a less dramatic problem, anemia is likely to occur after hemorrhage. Postpartum hemorrhage is a leading cause of postpartum death around the world.
Hypovolemic Shock
Hypovolemic shock occurs when the volume of blood is depleted and cannot fill the circulatory system. The woman can die if blood loss does not stop and if the blood volume is not corrected.
Body’s Response to Hypovolemia
The body initially responds to a reduction in blood volume with increased heart and respiratory rates. These reactions increase the oxygen content of each erythrocyte (red blood cell) and cause faster circulation of the remaining blood. Tachycardia (a rapid heart rate) is usually the first sign of inadequate blood volume (hypovolemia). The first blood pressure change is a narrow pulse pressure (a falling systolic pressure and a rising diastolic pressure). The blood pressure continues falling and eventually cannot be detected.
Blood flow to nonessential organs gradually stops, to make more blood available for vital organs, specifically the heart and brain. This change causes the woman’s skin and mucous membranes to become pale, cold, and clammy (moist). As blood loss continues, flow to the brain decreases, resulting in mental changes, such as anxiety, confusion, restlessness, and lethargy. As blood flow to the kidneys decreases, they respond by conserving fluid. Urine output decreases and eventually stops.
Medical Management
Medical management of hypovolemic shock resulting from hemorrhage may include any of the following actions:
- • Stopping the blood loss
- • Giving intravenous (IV) fluids to maintain the circulating volume and to replace fluids
- • Giving blood transfusions to replace lost erythrocytes
- • Giving oxygen to increase the saturation of remaining blood cells; a pulse oximeter is used to assess oxygen saturation of the blood
- • Placing an indwelling (Foley) catheter to assess urine output, which reflects kidney function
- • Uterine massage and administration of drugs to contract the uterus (e.g., oxytocin)
Nursing Care
Routine postpartum care involves assessing vital signs every 15 minutes until stable so that the signs of postpartum hemorrhage are identified as early as possible. The woman should be observed closely for early signs of shock, such as tachycardia, pallor, cold and clammy hands, and decreased urine output. Decreased blood pressure may be a late sign of hypovolemic shock.
Routine frequent assessment of lochia in the fourth stage of labor helps identify early postpartum hemorrhage. When the amount and character of the lochia are normal and the uterus is firm, but signs of hypovolemia are still evident, the cause may be a large hematoma. Excessive bright red bleeding despite a firm fundus may indicate a cervical or vaginal laceration. The occurrence of petechiae, bleeding from venipuncture sites, or oliguria may indicate a blood clotting problem. In the first hours postpartum, the perineal pad should be weighed to determine the output amount: 1 g equals 1 mL (see Chapter 9). Intake and output should be recorded and IV therapy monitored. Oxygen saturation levels are also monitored in early postpartum hemorrhage.
Careful explanations to the mother and family are essential, and providing emotional support and maintaining the integrity of the woman’s support system are key nursing roles. Even if the mother is separated from her infant, information concerning the infant’s condition should be readily accessible. Rooming-in should be established as soon as the woman’s condition permits.
Intensive care may be required to allow invasive hemodynamic monitoring of the woman’s circulatory status. Nursing Care Plan 10.1 specifies interventions for the woman at high risk for altered tissue perfusion related to hemorrhage.
Early (Primary) Postpartum Hemorrhage
Early postpartum hemorrhage results from one of three causes:
Table 10.1 summarizes the types of early postpartum hemorrhage.
Table 10.1
| Uterine atony | Lacerations | Hematoma |
|---|---|---|
| Characteristics | ||
| Contributing Factors | ||
Uterine Atony
Atony describes a lack of normal muscle tone. The postpartum uterus is a large, hollow organ with three layers of muscle. The middle layer includes interlacing figure-eight fibers. The uterine blood supply passes through this network of muscle fibers to supply the placenta.
After the placenta detaches, the uterus normally contracts and the muscle fibers compress bleeding vessels. If the uterus is atonic, however, these muscle fibers are flaccid and do not compress the vessels. Uterine atony allows the blood vessels at the placenta site to bleed freely and usually massively. Uterine overdistention, retained placental fragments, prolonged labor, or the use of drugs during labor that relax the uterus may cause atony.
Normal Postpartum Changes
After a full-term birth, the uterus should easily be felt through the abdominal wall as a firm mass about the size of a grapefruit. After the placenta is expelled, the fundus of the uterus is at the umbilicus level and then begins descending at a rate of about 1 finger’s width (1 cm) each day.
Lochia rubra should be dark red. The amount of lochia during the first few hours should be no more than one saturated perineal pad per hour. A few small clots may appear in the drainage, but large clots are not normal.
Characteristics of Uterine Atony
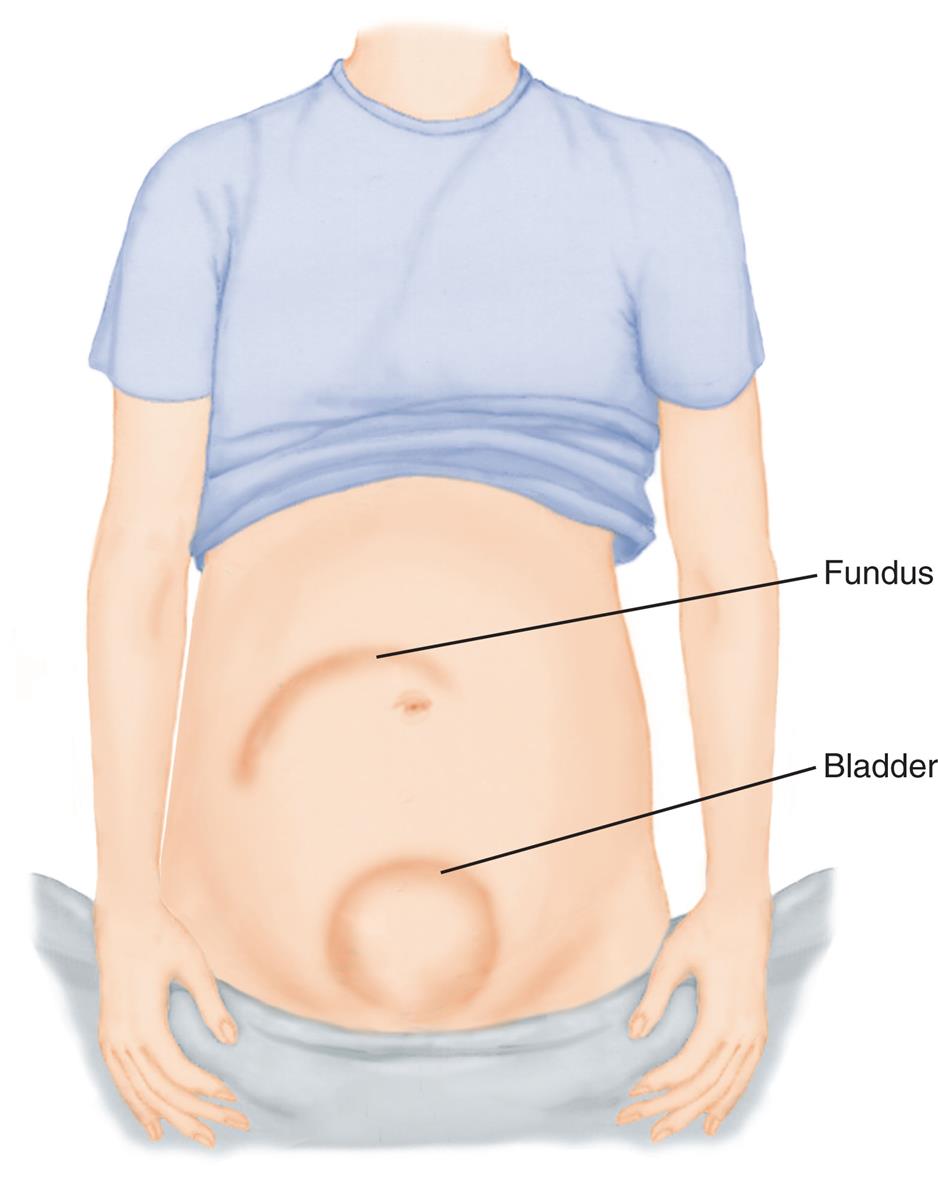
When uterine atony occurs, the woman’s uterus is difficult to feel and, when found, feels boggy (soft). The fundal height is high, often above the umbilicus. If the bladder is full, the uterus is higher and pushed to one side rather than located in the midline of the abdomen (Fig. 10.1). The uterus may or may not be soft if the bladder is full. A full bladder interferes with the ability of the uterus to contract and, if not corrected, eventually leads to uterine atony.
Lochia is increased and may contain large clots. The bleeding may be dramatic but may also simply be slightly above normal for a long time. Some lochia will be retained in the relaxed uterus because the cavity is enlarged; thus the true amount of blood loss may not be immediately apparent. Collection of blood in the uterus further interferes with contraction and worsens uterine atony and postpartum hemorrhage. A woman who has risk factors for postpartum hemorrhage (see Table 10.1) should have more frequent postpartum assessments of the uterus, lochia, and vital signs.
Medical Management and Nursing Care
Care of the woman with uterine atony combines nursing and medical measures. When the uterus is boggy, it should be massaged until firm (see Chapter 9), but it should not be overly massaged. Because the uterus is a muscle, excessive stimulation to contract it will tire it and can actually worsen uterine atony. If the uterus is firmly contracted, it should be left alone.
Bladder distention is an easily corrected cause of uterine atony. The nurse should catheterize the woman if she cannot urinate on the toilet or in a bedpan. Pressing toward the vagina should expel any clots or blood pooled in the vagina after the uterus is firm. Most health care providers include an order for catheterization to prevent delaying this corrective measure. First the uterus is massaged to firmness, and then the bladder is emptied to keep the uterus firm.
The infant suckling at the breast stimulates the woman’s posterior pituitary gland to secrete oxytocin, which causes uterine contraction. A dilute oxytocin (Pitocin) IV infusion is the most common drug ordered to control uterine atony. Other drugs to increase uterine tone include methylergonovine (Methergine) and prostaglandins (e.g., Hemabate or Cytotec). Methylergonovine increases blood pressure and should not be given to a woman with hypertension. Excessive bleeding may also be managed by providing a uterine tamponade (packing), using an intrauterine balloon, selective arterial embolization, or surgical ligation of the artery. Intravenous calcium gluconate may be used to counteract a tocolytic drug that may have been administered to relax the uterus during labor.
The health care provider may examine the woman in the delivery or operating room to determine the source of her bleeding and to correct it. Rarely, a hysterectomy is needed to remove the bleeding uterus that does not respond to any other measures. The woman should have nothing by mouth (NPO) until her bleeding is controlled.
Lacerations of the Reproductive Tract
Lacerations of the perineum, vagina, cervix, or area around the urethra (periurethral lacerations) can cause postpartum bleeding. The vascular beds are engorged during pregnancy, and bleeding can be profuse. Trauma is more likely to occur if the woman has a rapid labor or if forceps or a vacuum extractor is used. Blood lost in lacerations is usually a brighter red than lochia and flows in a continuous trickle. Typically, the uterus is firm.
Treatment
The health care provider should be notified if the woman has signs of a laceration, such as bleeding with a firmly contracted uterus. The injury is usually sutured in the delivery or operating room.
Nursing Care
Signs and symptoms of a bleeding laceration should be reported. A continuous trickle of blood can result in as much or more blood loss than the dramatic bleeding associated with uterine atony. The woman should be kept on NPO status until further orders are received, because she may need a general anesthetic for repair of the laceration. Genital trauma can cause long-term effects, such as cystocele, a prolapsed uterus, or urinary incontinence (Cooper & Gosnell, 2019).
Hematomas of the Reproductive Tract
A hematoma is a collection of blood within the tissues. Hematomas resulting from birth trauma are usually on the vulva or inside the vagina. They may be easily seen as a bulging bluish or purplish mass. Hematomas deep within the vagina are not visible from the outside.
Discomfort after childbirth is normally minimal and easily relieved with mild analgesics. The woman with a hematoma usually has severe, unrelenting pain that analgesics do not relieve. Depending on the amount of blood in the tissues, she also may describe pressure in the vulva, pelvis, or rectum. She may be unable to urinate because of the pressure.
The woman does not have unusual amounts of lochia, but she may develop signs of concealed blood loss if the hematoma is large. Her pulse and respiratory rates rise, and her blood pressure falls. She may develop other signs of hypovolemic shock if blood loss into the tissues is substantial. See Table 10.1 for risk factors for the development of a hematoma.
Treatment
Small hematomas usually resolve without treatment. Larger ones may require incision and drainage of the clots. The bleeding vessel is ligated or the area packed with a hemostatic material to stop the bleeding.
Nursing Care
An ice pack to the perineum is sufficient for most small perineal hematomas and requires no physician prescription. The nurse should observe for and report the classic symptom—excessive, poorly relieved pain. Signs of concealed blood loss accompanied by maternal complaints of severe pain, perineal or vaginal pressure, or inability to void should be reported. The woman is kept NPO until the health care provider examines her and prescribes treatment.
Medication to Support Clot Formation
In addition to the specific interventions for specific causes of postpartum hemorrhage, the medication tranexamic acid can be used to inhibit the breakup of clots that form; this supports the developing blood clot that is necessary to control hemorrhage. However, the drug must be administered within 3 hours of delivery (Francois and Foley, 2020).
Late Postpartum Hemorrhage
Late postpartum hemorrhage (bleeding that occurs 24 hours to 6 weeks after childbirth) usually occurs after discharge from the hospital and usually results from the following:
Placental fragments are more likely to be retained if the placenta does not separate cleanly from its implantation site after birth or if there is disruption of the placental scab. Clots form around these retained fragments and slough several days later, sometimes carrying the retained fragments with them. Retention of placental fragments is more likely to occur if the placenta is manually removed (removed by hand rather than being pushed away from the uterine wall spontaneously as the uterus contracts). These placental fragments are also more likely to exist if the placenta grows more deeply into the uterine muscle than is normal.
Treatment
Treatment consists of the administration of drugs such as oxytocin, methylergonovine, or prostaglandins (e.g., carboprost) to contract the uterus. Firm uterine contraction often expels the retained fragments, and no other treatment is needed. Ultrasonography may be used to identify remaining fragments. If bleeding continues, curettage (scraping or vacuuming of the inner surface of the uterus) is performed to remove small blood clots and placental fragments. This procedure is known as dilation and curettage (D&C) or dilation and evacuation (D&E). Antibiotics are prescribed if infection is suspected.
Nursing Care
The nurse should teach each postpartum woman what to expect about changes in the lochia (see Chapter 9). The woman should be instructed to report the following signs of late postpartum hemorrhage to her health care provider:
If a late postpartum hemorrhage occurs, the nurse assists in implementing pharmacological and surgical treatment.
Subinvolution of the Uterus
Involution is the return of the uterus to its nonpregnant condition after birth. The muscles of the uterus contract and constrict the blood vessels at the placental site, stopping the bleeding. Normally the uterus descends at the rate of 1 cm (one finger’s width) per day and is no longer palpable by 12 days postpartum. The placental site heals by 6 weeks postpartum. Subinvolution is a slower than expected return of the uterus to its nonpregnant condition. Infection and retained fragments of the placenta are the most common causes. Typical signs of subinvolution include the following:
Treatment
Medical treatment is selected to correct the cause of the subinvolution. It may include the following:
Nursing Care
The mother will almost always have been discharged when subinvolution of the uterus occurs. All new mothers should be taught about the normal changes to expect so they can recognize a departure from the normal pattern. Women should report fever, persistent pain, persistent red lochia (or return of bleeding after it has changed), or foul-smelling vaginal discharge. The woman should be taught how to palpate the fundus and what normal changes to expect.
The woman may be admitted to the hospital on the gynecology unit. Nursing care involves assisting with medical therapy and providing analgesics and other comfort measures. Specific nursing care depends on whether the subinvolution results from infection or another cause.
Thromboembolic Disorders
A venous thrombosis is a blood clot within a vein. It occurs in 1 in 1500 pregnancies (Merriam and Pettker, 2020). The size of the clot can increase as circulating blood passes over it and deposits more platelets, fibrin, and cells. It often causes an inflammation of the vessel wall. The pregnant woman is at increased risk for venous thrombosis because of the venous stasis that can occur from compression of the blood vessels by the heavy uterus or by pressure behind the knees when the legs are placed in stirrup leg supports for episiotomy repair. Blood vessel injury during cesarean section can also cause a thrombus.
The levels of fibrinogen and other clotting factors normally increase during pregnancy, whereas levels of clot-dissolving factors (e.g., plasminogen activator and antithrombin III) are normally decreased, resulting in a state of hypercoagulability (an increased susceptibility to developing blood clots). If the woman has varicose veins or remains on bed rest, her state of hypercoagulability places her at increased risk for thrombus formation.
Preventive measures include the use of pneumatic compression devices on the lower extremities or prophylactic heparin for women undergoing cesarean sections or who are on prolonged bed rest (Merriam and Pettker, 2020).
There are three types of thromboembolic disorders:
- 1. Superficial venous thrombosis (SVT) involves the saphenous vein of the lower leg and is characterized by a painful, hard, reddened, warm vein that is easily seen.
- 2. Deep venous thrombosis (DVT) can involve veins from the feet to the femoral area and is characterized by pain, calf tenderness, leg edema, color changes, pain when walking, and sometimes a positive Homans’ sign (pain when the foot is dorsiflexed), although the Homans’ sign is not always reliable during the postpartum period because it is not specific to blood clots postpartum. An increase in leg circumference greater than 2 cm accompanied by redness, tenderness, and edema should be promptly reported. The diagnosis is confirmed by ultrasound, with or without Doppler assistance (Merriam and Pettker, 2020).
- 3. Pulmonary embolism (PE) occurs when the pulmonary artery is obstructed by a blood clot that breaks off (embolizes) and lodges in the lungs. It may have dramatic signs and symptoms, such as sudden chest pain, cough, dyspnea (difficulty breathing), a decreased level of consciousness, and signs of heart failure. A small PE may have nonspecific signs and symptoms, such as shortness of breath, palpitations, hemoptysis (bloody sputum), faintness, and a low-grade fever.
Treatment
SVT is treated with administration of analgesics, local application of heat, and elevation of the legs to promote venous drainage. DVT is treated similarly, with the addition of subcutaneous or IV anticoagulation drugs, such as heparin. Low-molecular-weight heparin (LMWH), such as Lovenox, may be used, because it is long acting and requires less frequent doses and lab testing. LMWH anticoagulants are contraindicated with regional anesthesia.
Nursing Care
The woman should be observed before and after birth for signs and symptoms that suggest venous thrombosis. Dyspnea, coughing, and chest pain suggest PE and must be reported immediately.
Prevention of thrombi is most important. Pregnant women should not cross their legs because this impedes venous blood flow. When the legs are elevated, there should not be sharp flexion at the groin or pressure in the popliteal space behind the knee, which would restrict venous flow. Measures to promote venous flow should be continued during and after birth because levels of clotting factors remain high for several weeks.
Early ambulation or range-of-motion exercises are valuable aids to preventing thrombus formation in the postpartum woman. Antiembolic stockings may be used if varicose veins are present. The nurse should teach the woman how to put on the stockings properly because rolling or kinking of the stocking can further impede blood flow. If stirrups are used during birth or episiotomy repair, they should be padded to prevent pressure at the popliteal angle.
The woman who will be undergoing anticoagulant therapy at home should be taught how to give herself the drug and about signs of excess anticoagulation (prolonged bleeding from minor injuries, bleeding gums, nosebleeds, unexplained bruising). She should use a soft toothbrush and avoid minor trauma that can cause prolonged bleeding or a large hematoma. Home nursing visits are often prescribed to obtain blood for laboratory clotting studies and to help the woman cope with therapy.
Infections
Puerperal Sepsis
Puerperal sepsis is an infection or septicemia after childbirth and is one of the five leading causes of maternal mortality in the United States (Hovert, 2021). Tissue trauma during labor, the open wound of the placental insertion site, surgical incisions, cracks in the nipples of the breasts, and the increased pH of the vagina after birth are all risk factors for the postpartum woman.
The fever is most often caused by endometritis, an inflammation of the inner lining of the uterus. Blockage of the lochial flow because of retained placenta or clots increases susceptibility to infection.
The danger of postpartum infection is that a localized infection of the perineum, vagina, or cervix can ascend the reproductive tract and spread to the uterus, fallopian tubes, and peritoneum, causing peritonitis, which is a life-threatening condition. Table 10.2 lists characteristics, medical treatment, and nursing care for these infections. Regardless of their location or the causative organism, postpartum infections have several common features.
Table 10.2
| Wound Infections | Endometritis (Uterus) | Urinary Tract Infections | Mastitis (Breast) |
|---|---|---|---|
| Characteristics | |||
| Medical Management | |||
| Nursing Care | |||
Manifestations
Puerperal (postpartum) fever is defined as a temperature of 38°C (100.4 °F) or higher after the first 24 hours and for at least 2 days during the first 10 days after birth. Slight temperature elevations with no other signs of infection often occur during the first 24 hours because of dehydration. The nurse should look for other signs of infection if the woman’s temperature is elevated, regardless of the time since delivery. A pulse rate that is higher than expected and an elevated temperature often occur when the woman has an infection. Other signs and symptoms of infection may be localized (in a small area of the body) or systemic (throughout the body).
The assessment of any cesarean section wound or episiotomy wound using the REEDA criteria (redness, edema, ecchymosis, discharge, approximation), or hardening of the operative area, should be promptly reported and documented. Fever, pain, a foul odor, or abnormal findings on routine postpartum assessment must be reported to the health care provider.
White blood cells (leukocytes) are normally elevated during the early postpartum period to about 20,000 to 30,000 cells/mm3, which limits the usefulness of the blood count to identify infection. Leukocyte counts in the upper limits are more likely to be associated with infection than lower counts.
Treatment
The goals of medical treatment are to limit the spread of infection, to prevent it from reaching the blood and other organs, and to eliminate the infection. A culture and sensitivity sample from the suspected site of infection is taken to determine the antibiotics that will be most effective. IV antibiotics may be ordered, and the woman may be placed on bed rest.
Nursing Care
Nursing care objectives focus on preventing infection and, if an infection occurs, on facilitating medical treatment. To achieve these goals, the nurse should do the following:
- • Use and teach hygienic measures to reduce the number of organisms that can cause infection (e.g., hand hygiene, perineal care).
- • Promote adequate rest and nutrition for healing.
- • Observe for signs of infection.
- • Teach signs of infection that the woman should report after discharge.
- • Teach the woman to take all of the antibiotics prescribed rather than stopping them after her symptoms are eliminated.
- • Teach the woman how to apply perineal pads (front to back).
Women should be taught to wash their hands before and after performing self-care that may involve contact with secretions. The nurse should explore ways to help the woman get enough rest.
Ultimately, a woman’s own body must overcome infection and heal any wound. Nutrition is an essential component of her body’s defenses. The nurse, and sometimes a dietitian, should teach her about foods that are high in protein (meats, cheese, milk, legumes) and vitamin C (citrus fruits and juices, strawberries, cantaloupe), because these nutrients are especially important for healing. Foods high in iron, to correct anemia, include meats, enriched cereals and breads, and dark green, leafy vegetables.
Mastitis and Breastfeeding
Mastitis is an infection of the breast. It usually occurs about 2 or 3 weeks after giving birth (Fig. 10.2). Mastitis occurs when organisms from the skin or the infant’s mouth enter small cracks in the nipples or areolae. These cracks may be microscopic. Breast engorgement and inadequate emptying of milk are associated with mastitis. Mastitis often involves only one breast.

Signs and symptoms of mastitis include the following:
The woman usually has fever, chills, and other systemic signs and symptoms. If not treated, the infected area becomes encapsulated (walled off) and an abscess forms. The infection is usually outside the ducts of the breast, and the milk is not contaminated.
Treatment
Antibiotics and the continued removal of milk from the breast are the primary treatments for mastitis. Mild analgesics make the woman more comfortable. The woman may need an incision and drainage of the infected area and IV antibiotics if an abscess forms. The mother can usually continue to breastfeed. If she should stop nursing for any reason, she should pump her breasts. She should not wean her infant when she has mastitis because weaning leads to engorgement and stasis of milk, which worsens the mastitis.
Nursing Care
The nursing mother should be taught proper breastfeeding techniques to reduce the risk for mastitis (see Chapter 9). Nursing care for mastitis centers on relieving pain and on maintaining lactation. Heat promotes blood flow to the area, comfort, and complete emptying of the breast. Moist heat can be applied with chemical packs. Placing a warm, wet cloth in a plastic bag and applying it to the breasts can create an inexpensive warm pack. A warm shower taken just before nursing provides warmth and cleanliness and stimulates the flow of milk.
Both breasts should be emptied regularly to reduce milk stasis, which increases the risk for abscess formation. If the affected breast is too painful for the mother to breastfeed, she can use a breast pump to empty it. She can massage the area of inflammation to improve milk flow and reduce stasis. Nursing first on the unaffected side starts the milk flow in both breasts and can improve emptying with less pain. Other nursing measures include the following:
Mood Disorders
A mood is a pervasive and sustained emotion that can color one’s view of life. “Postpartum blues” or “baby blues” is common after birth. The woman has periods when she feels let down, but overall she finds pleasure in life and in her new role as a mother. Her rollercoaster emotions are usually self-limiting as she adapts to the changes in her life.
A psychosis involves serious impairment of one’s perception of reality. Postpartum depression and postpartum psychosis are disorders that are more serious than “postpartum blues.” Postpartum blues, also known as an adjustment reaction, occurs in about 70% of women, appearing on day 5 and disappearing by day 10 (Isley, 2020). After childbirth, estrogen and progesterone levels decrease rapidly, which leads to increased brain levels of monoamine oxidase-A (MAO-A), which is related to the onset of postpartum depression. The presence of a thyroid disorder often presents with symptoms of postpartum dysphoria, and referral for follow-up care is indicated. Research has shown that it is possible a nutritional supplement of tryptophan, tyrosine, and blueberry juice counters the effects of increased MAO-A levels and may prevent the development of postpartum depression (Dawlati et al., 2017). Research is ongoing.
Postpartum Depression
According to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V), which is published by the American Psychiatric Association, there are three types of postpartum depression:
Postpartum depression is a depressive illness that is usually manifested within 2 to 4 weeks after delivery. The onset of depression during this time may interfere with the mother’s ability to respond to her infant’s cues and interferes with the developing maternal-infant bonding. Formal postpartum screening for depression is not standard practice in the United States, which places the responsibility on the nurse to detect and refer problems to prevent progression to chronic depression. The nurse can promote the behaviors that improve mental health. Risk factors for postpartum depression include inadequate social support, a poor relationship with the partner, life and childcare stress, low self-esteem, and an unplanned pregnancy. Those having close contact with the woman notice the depression. Signs and symptoms may include the following:
- • Lack of enjoyment in life
- • Disinterest in others; loss of normal give-and-take in relationships
- • Intense feelings of inadequacy, unworthiness, guilt, inability to cope
- • Loss of mental concentration; inability to make decisions
- • Disturbed sleep or appetite
- • Constant fatigue and feelings of ill health
Postpartum depression strains the coping mechanisms of the entire family at a time when all are adapting to the birth of a child. As a result of the strained relationships, communication is often impaired, and the depressed woman may withdraw further, which distances her even further from her support system. The woman usually remains in touch with reality. The nurse should observe for signs and symptoms during clinic visits.
Treatment
A combination of psychotherapy and antidepressants is often the course of therapy, either in an outpatient or inpatient setting. Screening tools are available. The nurse provides support and observation of behavior and is alert to the possibility of self-harm by the woman. Light therapy (phototherapy) and exercise are complementary and alternative medicine (CAM) treatment strategies that may help in the management of postpartum depression (see Chapter 34 for other types of CAM therapy). The influence of hormones on mood changes before, during, and after menstruation supports the theory that fluctuating hormone levels postpartum may also have an effect on the woman’s mood. Referral for follow-up to available community mental health support services and facilities is a nursing responsibility, to assure ongoing care and support. Counseling should include the woman’s partner and family.
Postpartum Psychosis
Women experiencing a postpartum psychosis have an impaired sense of reality. Psychosis is much less common than postpartum depression. A woman may have any psychiatric disorder, but two are most often encountered:
- • Bipolar disorder: a disorder characterized by episodes of mania (hyperactivity, excitability, euphoria, and a feeling of being invulnerable) and depression
- • Major depression: a disorder characterized by deep feelings of worthlessness and guilt, serious sleep and appetite disturbances, and sometimes delusions about the infant being dead
Postpartum psychosis can be fatal for both mother and infant. The mother may endanger herself and her infant during manic episodes because she uses poor judgment and has a sense of being invulnerable. Suicide and infanticide are possible, especially during depressive episodes.
In some cases, social workers within the community may refer the woman for counseling. In other cases, an inpatient psychiatric treatment center is the appropriate environment for treatment.
The Homeless Mother and Newborn
Homelessness is defined as a lack of a permanent home and is not limited to women who must live on the street. Some women live in single-room hotels, and others stay with friends or extended family. Homeless women often have difficulty accessing care, receive care from different health care providers at different sites, and have incomplete medical records. Follow-up is difficult. Before a mother is discharged with her newborn infant, it is essential to determine that she has a place to go and has a way of accessing help for herself or her newborn. The nurse can be a key link in facilitating referrals to outreach programs, support services, counseling, shelters, and follow-up medical care.
Get Ready for the Next-Generation NCLEX® Examination!
Key Points
- • The nurse must be aware of women who are at higher risk for postpartum hemorrhage and assess them more often.
- • A constant small trickle of blood can result in significant blood loss, as can a larger one-time hemorrhage.
- • Pain that is persistent and more severe than expected is characteristic of a hematoma in the reproductive tract.
- • It is essential to identify and limit a local infection before it spreads to the blood or other organs.
- • The nurse should teach new mothers about normal postpartum changes and indications of problems that should be reported.
- • Early ambulation can prevent thrombosis formation.
- • Types of obstetric shock include cardiogenic (from anemia or cardiac disorders), hypovolemic (from hemorrhage), anaphylactic (from a drug response), and septic (caused by puerperal infection).
- • Careful listening and observation can help the nurse identify a new mother who is suffering from postpartum depression.
- • Postpartum psychoses are serious disorders that are potentially life-threatening to the woman and others, including her infant.
Additional Learning Resources
![]() Go to your Study Guide for additional learning activities to help you master this chapter content.
Go to your Study Guide for additional learning activities to help you master this chapter content.
Go to your Evolve website (http://evolve.elsevier.com/Leifer) for the following learning resources:
- • Animations
- • Answer Guidelines for Critical Thinking Questions
- • Answers and Rationales for Review Questions for the NCLEX® Examination
- • Glossary with English and Spanish pronunciations
- • Interactive Review Questions for the NCLEX® Examination
- • Patient Teaching Plans in English and Spanish
- • Skills Performance Checklists
- • Video clips and more!
 Online Resources
Online Resources
- • Association of Women’s Health, Obstetric, and Neonatal Nurses: https://www.awhonn.org
- • Behavioral health care: https://www.nabh.org
- • Child passenger safety: https://www.saferoads.org/issues/child-passenger-safety/
Clinical Judgment and Next-Generation NCLEX® Examination-Style Questions
- 1. During the postpartum period the white blood cell (leukocyte) count is normally:
- 2. A woman delivered her newborn several hours previously, and her uterus remains soft and boggy. Which of the following should the nurse anticipate that the health care provider would prescribe to increase uterine tone and firm the uterus? (Select all that apply.)
- 3. Identify the possible postpartum complications that may be indicated by the nursing observations listed.
Observation Complication 1. Blood loss of 800 mL after vaginal birth Hypovolemic shock 2. Tachycardia and narrow pulse pressure Subinvolution of the uterus 3. Persistence of lochia rubra at 4 weeks postpartum Puerperal sepsis 4. Sudden chest pain and dyspnea Hemorrhage 5. Foul-smelling lochia and fever Mood disorders 6. Prolonged bouts of crying and refusal to hold the baby Thromboembolic disorders - 4. Place an X in the appropriate column to identify the following characteristics as evidence of either uterine atony, laceration, or hematoma.
Characteristic Uterine Atony Laceration Hematoma Heavy lochia with large clots Purplish mass on vulva Pain and pressure in rectum Continuous trickle of bright blood Bladder distention Soft, high fundus - 5. A postpartum mother who is breastfeeding has developed mastitis. She states that she does not think it is good for her infant to drink milk from her infected breast. Which of the following would be appropriate responses from the nurse? (Select all that apply.)
- 1. Apply a tight breast binder to the infected breast until the infection subsides.
- 2. Instruct her to nurse the infant from only the unaffected breast until the infection clears up.
- 3. Apply a warm pack to the affected breast.
- 4. Suggest that she discontinue breastfeeding and start infant on formula until infection subsides.
- 5. Advise the woman to wear a supportive bra.
- 6. Encourage the infant to empty the breast at each feeding
- 7. Message the area as newborn nurses.
- 6. Complete the nursing actions from the choices below to fill in each blank in the following sentence.
- A 29-year-old multipara has vaginally delivered her second child 60 minutes ago. Breastfeeding was initiated in delivery room. The placenta was delivered spontaneously and intact. At 60 minutes postdelivery, the patient’s uterus is palpated at one fingerbreadth below the umbilicus and is “boggy.” Pad saturation was estimated to be between 10 to 15 mL of bloody lochia. Vital signs all within normal limits. The diagnosis of uterine atony is made by the attending obstetrician.
- Considering the diagnosis and patient condition, the nurse should expect the prioritizing of ___________ and then ___________.
- Nursing actions
- Uterine massage
- Breastfeeding
- Facilitating patient urination
- Administering methylergonovine
