Principles of Tooth Preparation
Abstract
How to perform restorative treatment that includes fixed prostheses is not a short-term, simple decision. The biological, esthetic, and restorative/tooth interface considerations define three categories of principles that all must be considered before performing any irreversible procedures. These principles offer a framework for clinical decision making. Indications and contraindications for restorative interventions are discussed and related to research-based rationales to help make optimal decisions for the delivery of care.
Keywords
Tooth preparation; Biologic Considerations; Esthetic Considerations; Tooth-Restoration interface; Iatrogenic damage; Pulp size; Clinical crown heights; Conservation; Prognosis; Margin Geometry and Placement; Retention form; Resistance Form; Diagnostic waxing; Operator positioning
Demineralized tooth structure can be remineralized. Instead of diamond-cutting instruments to prepare diseased teeth, the use of fluorides and optimization of oral environments have become a cornerstone of clinical dental care.1 Although extremely helpful to arrest disease in progress and from a preventive perspective, at a macroscopic level, however, teeth cannot regenerate missing anatomical parts. Today, more than ever before, clinicians face the dilemma to choose between remineralization of a carious lesion or embarking on restorative intervention. Caries monitoring can prove to have high risks if a patient is non-compliant or the disease process is refractory. Restorative intervention, however, results in removal of not only diseased tooth structure but some healthy tooth structure as well. The dentist needs to educate the patient in the decision process because it is not solely solved by preparing a tooth. The health of a tooth is dependent on a lifelong balance between demineralization with remineralization of enamel, dentin, and cementum along with maintenance of any subsequent restoration.
Once enamel and dentin are lost as a result of caries, trauma, erosion, wear, congenital factors, or iatrogenically, restorative materials are all that are currently available to reestablish form and function. With rare exceptions, teeth require preparation to receive restorations, and these preparations must be based on fundamental principles from which basic criteria can be developed to help predict the success of prosthodontic treatment. Careful attention to every detail is imperative during tooth preparation. Tooth preparations can receive direct or indirect restorations. Direct restorations are created intraorally with plastic materials such as composite resin, glass ionomer, or dental amalgam. Indirect restorations are fabricated extraorally. This chapter focuses on tooth preparations for indirect restorations. A good preparation for an indirect restoration facilitates subsequent techniques (e.g., interim restoration fabrication, soft tissue management, digital scans, impression making, along with virtual or analog fabrication of dies and casts, waxing) while ensuring the best possible prognosis.
Indications and Contraindications for Indirect Restorations
The following are common indications and contraindications for the various treatment options:
- Indications for indirect restorations:
- • Missing cusp(s)
- • Gross caries causing an unsupported cusp
- • Protection of posterior endodontically treated teeth2,3
- • Caries associated with a preexisting indirect restoration causing weakened cusps
- • Worn teeth with moderate to severe dentin exposure
- • Cracked teeth (to encircle the tooth)
- • Complete crowns are indicated on teeth with five affected surfaces
- Contraindications for indirect restorations:
- • Patients with uncontrolled high caries risk
- • To remove sound tooth structure that could be preserved with a direct restoration or be remineralized
- • Patients with temporomandibular disorder (TMD) symptoms (e.g., pain) should first have such concerns addressed prior to tooth preparation
- • Teeth with a poor or guarded prognosis (e.g., if the loss of a tooth is anticipated within five or so years due to periodontal disease)
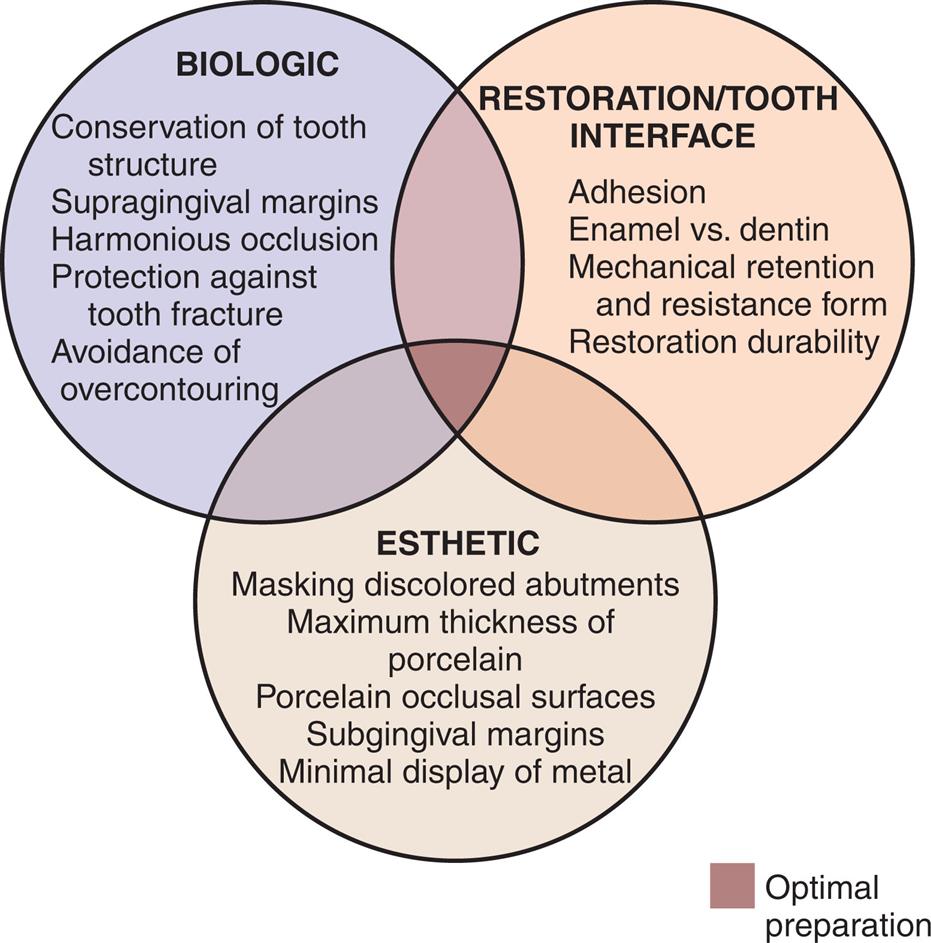
Once the decision has been made to intervene restoratively, the next question is if the restoration will be adhesively or cohesively retained. Through adhesive dentistry, prosthetic reconstructions can be performed with conservative techniques using porcelain laminate veneers, and partial-coverage restorations bonded to enamel. With cohesive dentistry, partial-coverage restorations, inlays, and complete crowns can also be performed conservatively but those rely on opposing axial walls of certain geometric shapes within the tooth preparation to deliver mechanical retention. The dentist needs to select the best approach suitable for the specific tooth and situation. To aid in the decision process, the principles of tooth preparation may be divided into three broad categories that encompass both methods:
- 1. Biologic considerations, which affect the health of the oral tissues
- 2. Restoration/tooth interface considerations, how the prosthetic materials are connected to living hard tissues affecting the integrity and durability of the restoration (mechanical retention vs. adhesion)
- 3. Esthetic considerations, which affect the appearance of the patient
Successful tooth preparation and subsequent restoration depend on simultaneous consideration of all these factors. Improvement in one area often adversely affects another area, and striving for perfection in one may lead to failure in another. For example, consider two restorative options for an endodontically treated maxillary central incisor with gross proximal caries and severe intrinsic staining. A complete crown or a porcelain laminate veneer supplemented with a composite restoration to restore the endodontic access hole could be treatment planned. In the tooth preparation for a porcelain laminate veneer (see Chapter 11), sufficient thickness of ceramic is necessary to mask the discolored tooth. However, if too much tooth structure is removed, less enamel will be available for bonding and the ceramic will have to rely on less predictable dentin bonding (restoration/tooth interface). In contrast, if such stained enamel is preserved for bonding but the ceramic is made thicker to mask the discolored tooth structure, an overcontoured veneer may not promote periodontal health (biological considerations). Furthermore, if the stained enamel is preserved and the veneer is not overcontoured, the ceramist is forced to use more opaque ceramic which could limit the lifelike appearance of the restoration (esthetic consideration).
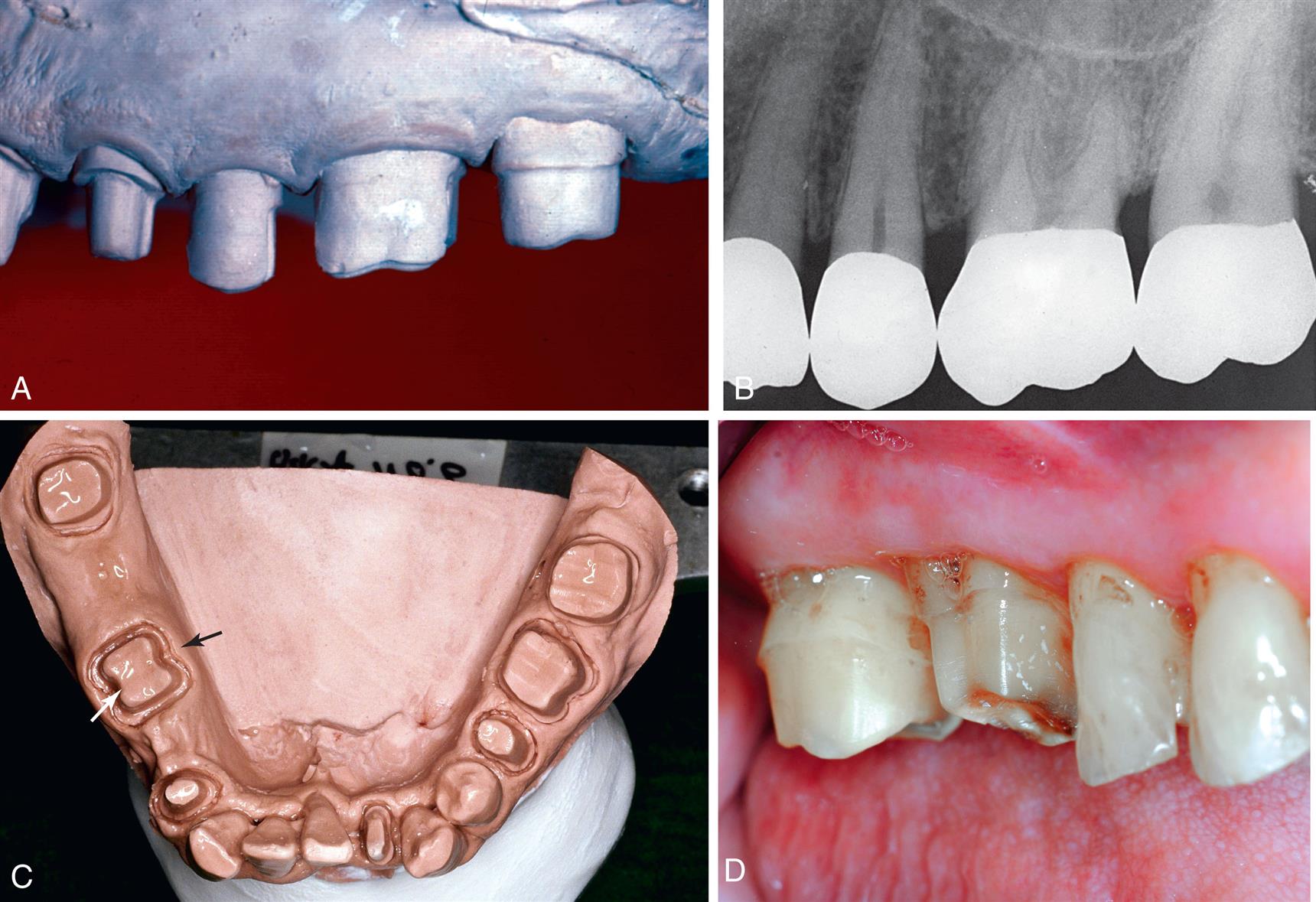
If a metal-ceramic crown is planned (see Chapter 24), the metal coping will mask discolored tooth structure (esthetic consideration). However, sufficient thickness of porcelain is necessary for a lifelike appearance. Furthermore, if too much tooth structure is removed to accommodate a greater thickness of porcelain for esthetic reasons, the pulp may be encroached upon (biological consideration) and the tooth unduly weakened (restoration-tooth interface and biological considerations). In-depth knowledge and understanding of the various criteria are prerequisite to the development of a treatment plan, communication with a dental patient, and satisfactory tooth preparation skills. Accomplishment of optimum tooth preparation (Fig. 7.1) invariably challenges the dentist to find the best combination of compromises among applicable biologic, restoration/tooth interface, and esthetic considerations.
Biologic Considerations
Surgical procedures involving living tissues must be performed carefully to avoid unnecessary damage. The adjacent teeth, soft tissues, and the pulp of the tooth being prepared are easily damaged during tooth preparation. If poor preparation leads to inadequate marginal fit or deficient crown contour, plaque control around fixed restorations becomes more difficult. This, in turn, impedes the long-term maintenance of dental health.
Prevention of Damage During Tooth Preparation
Adjacent Teeth
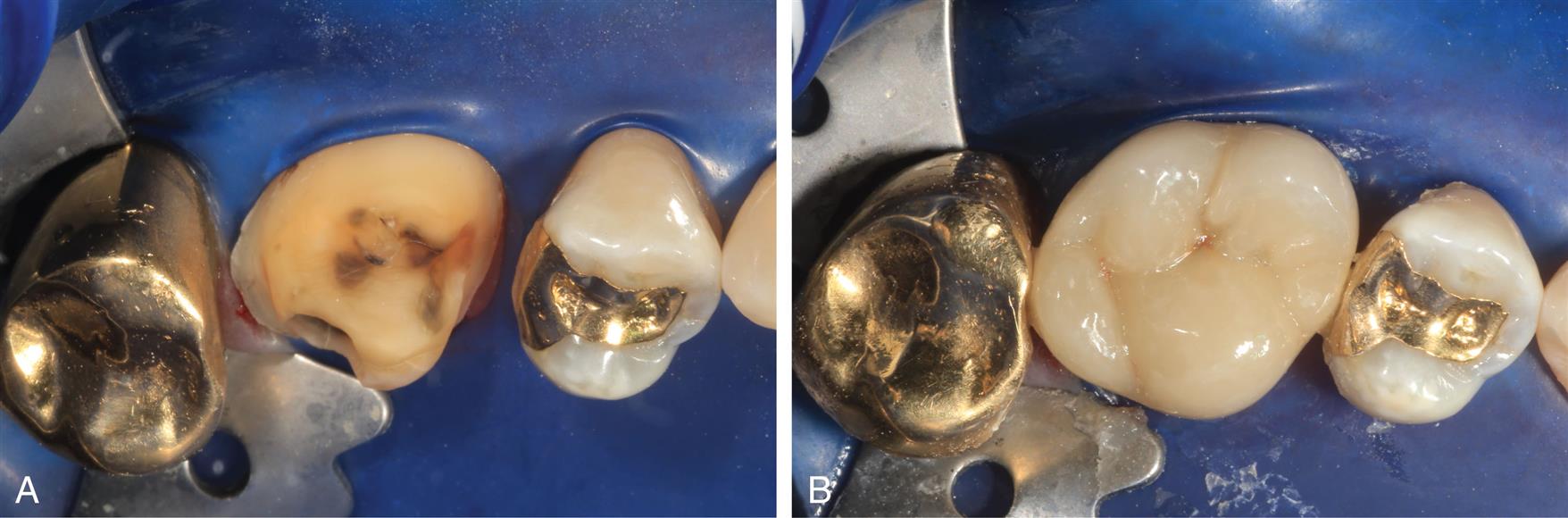
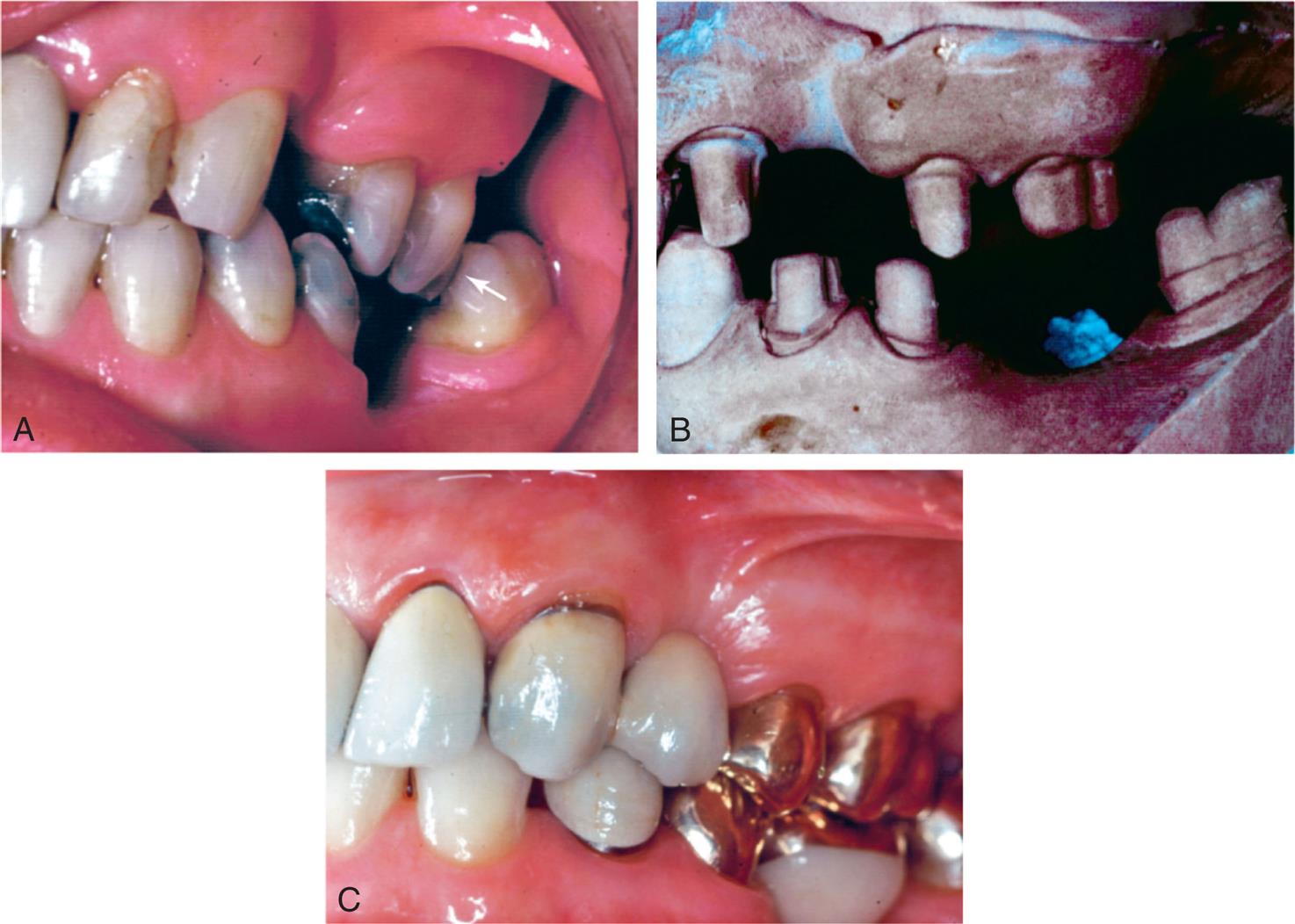
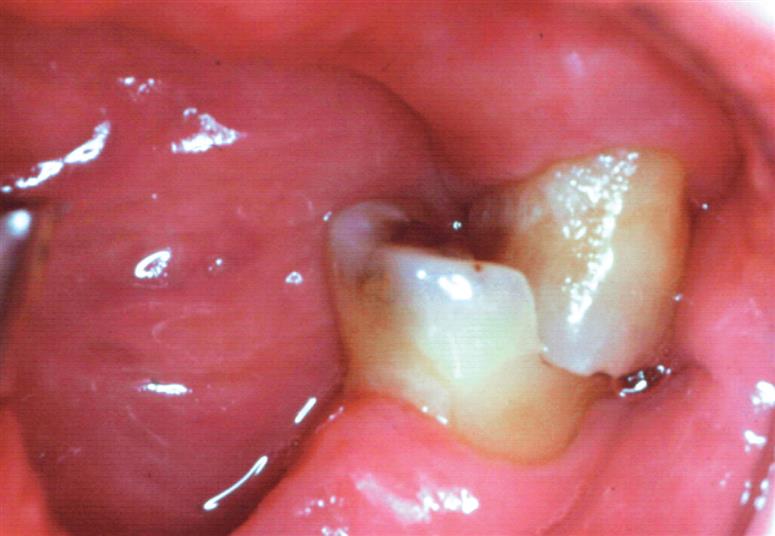
Iatrogenic damage to an adjacent tooth is a common error in dentistry. Even if a damaged proximal contact area is carefully reshaped and polished, it remains more susceptible to dental caries than the original undamaged tooth surface (Fig. 7.2), presumably because the original surface enamel contains higher fluoride concentrations and the polished layer is more prone to plaque retention.4 Sound tooth preparation technique avoids and prevents damage to adjacent proximal surfaces.
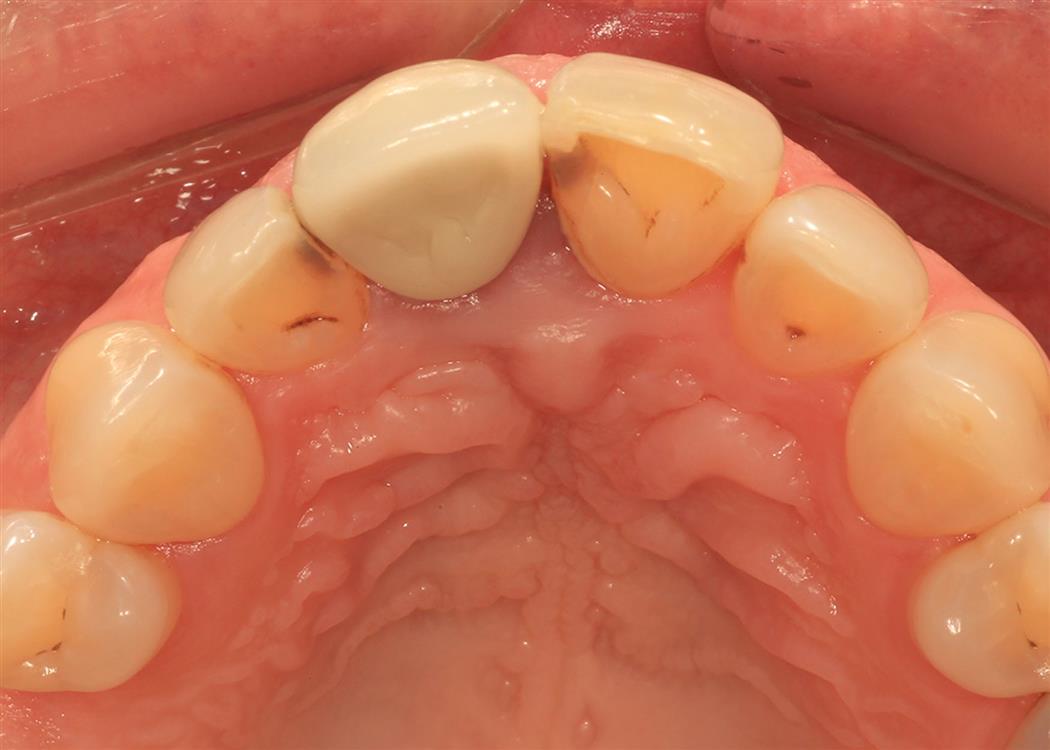
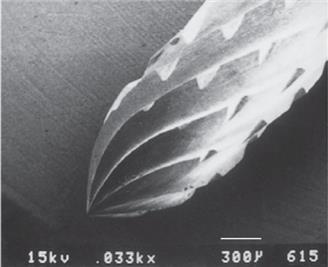
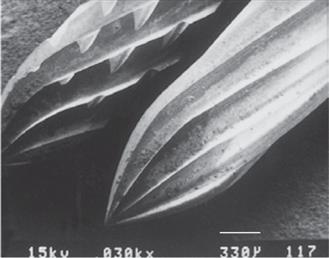
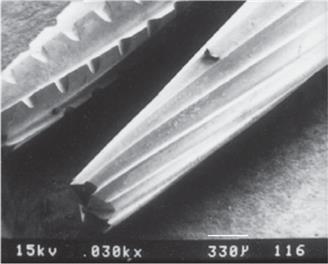
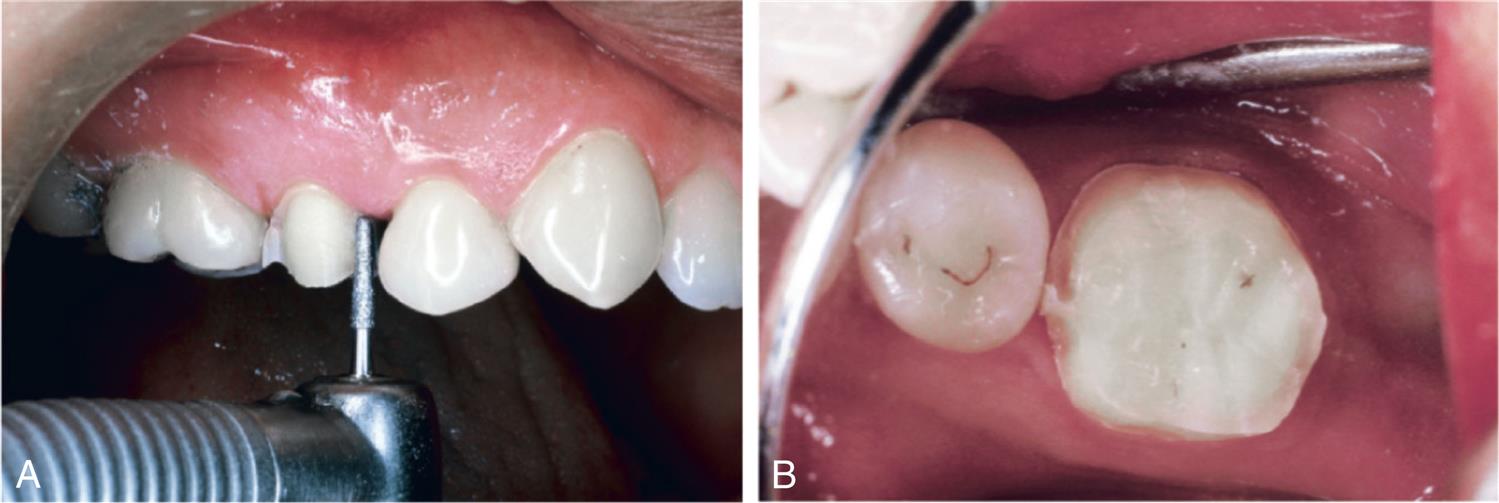
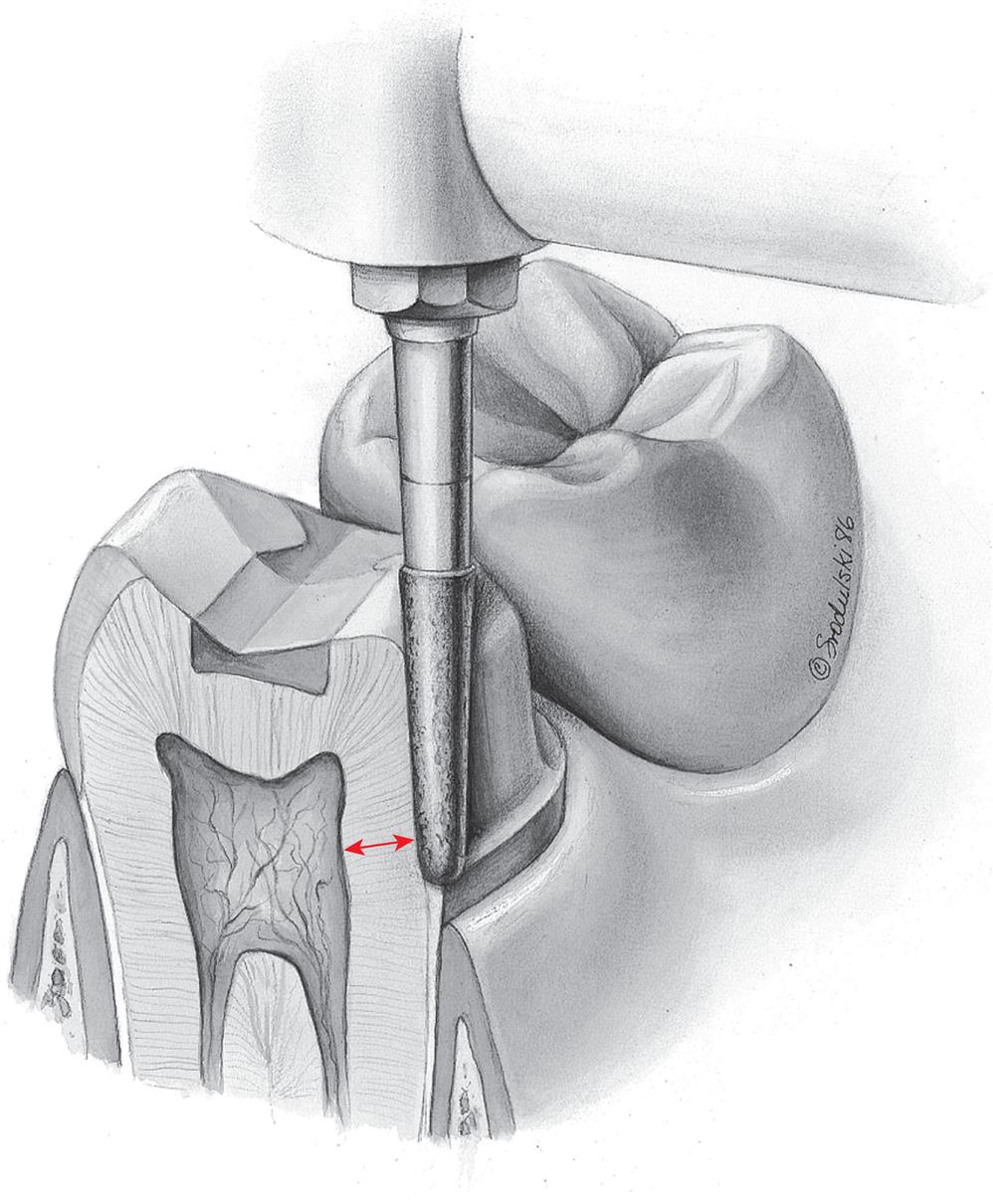
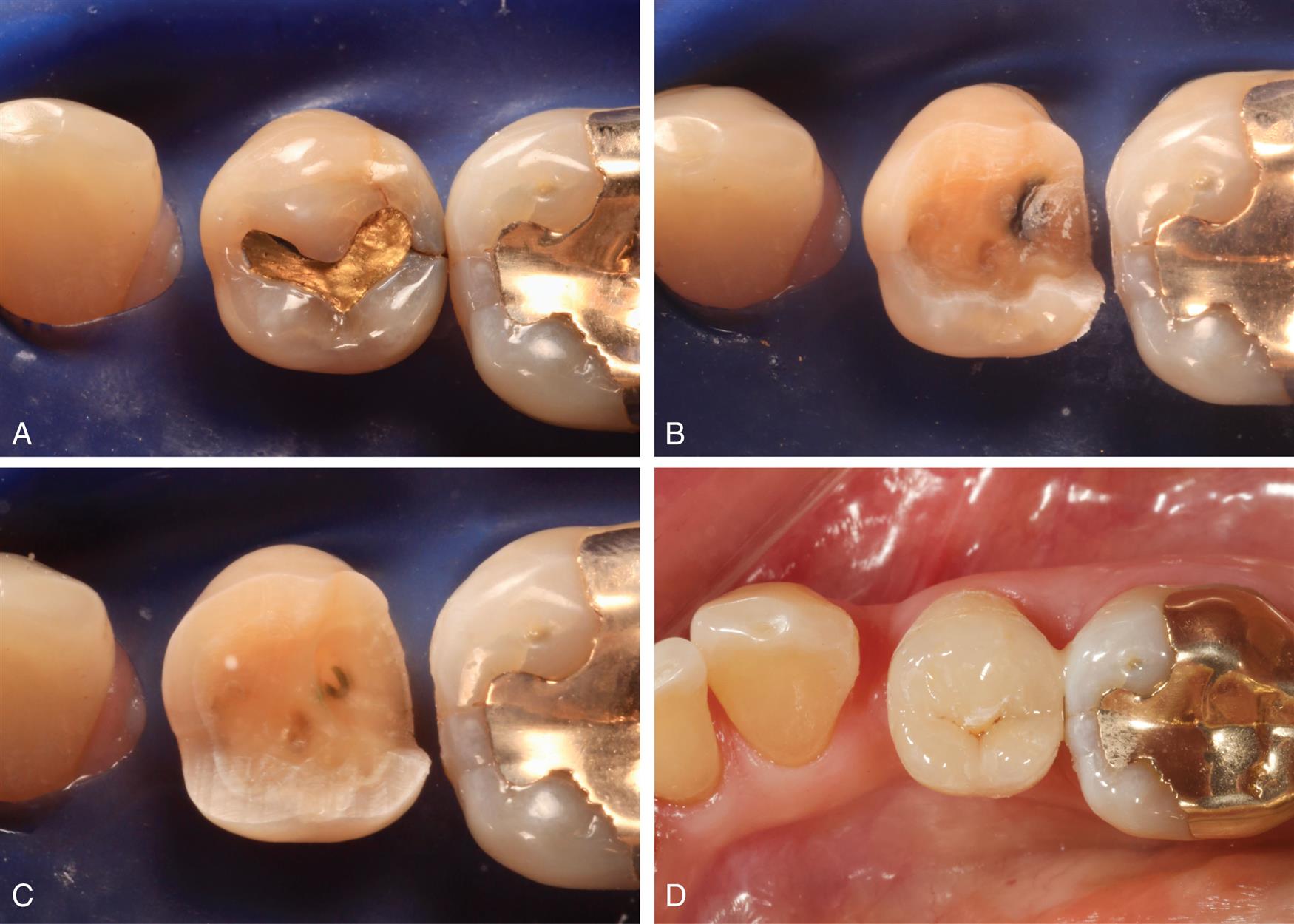
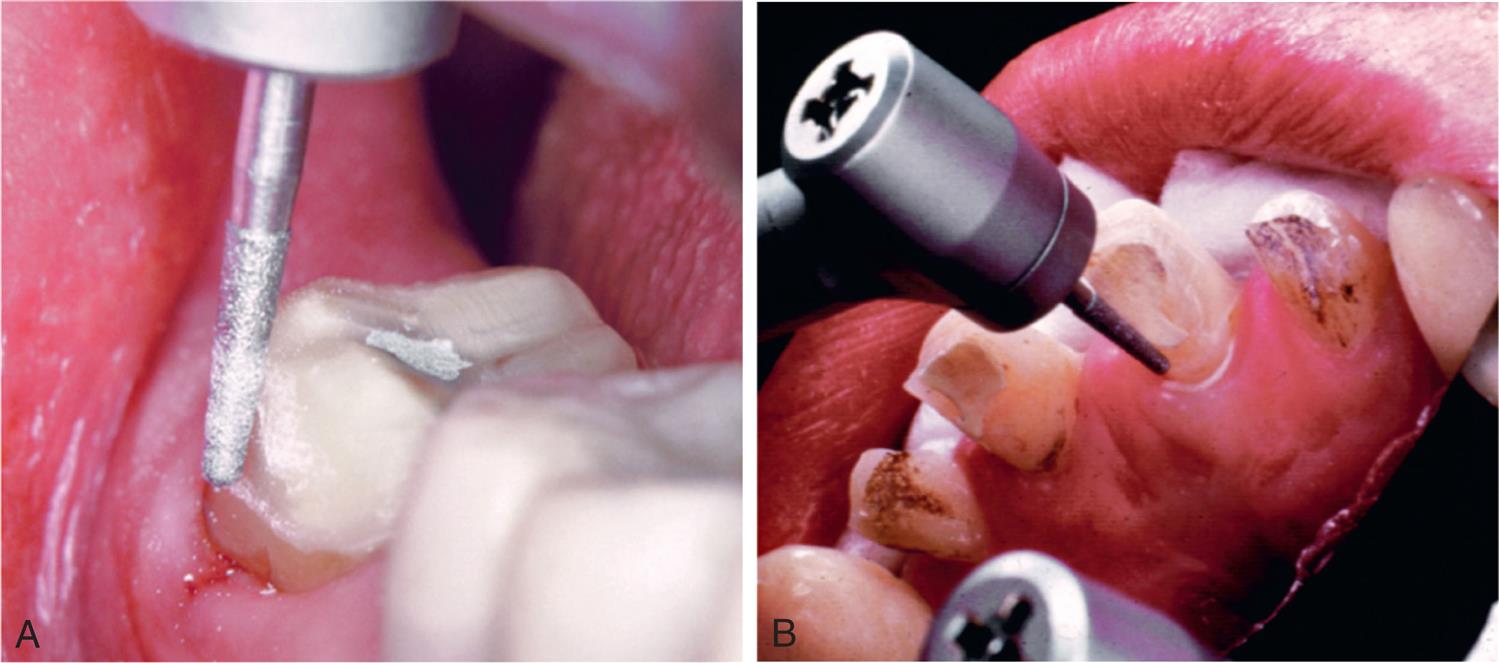
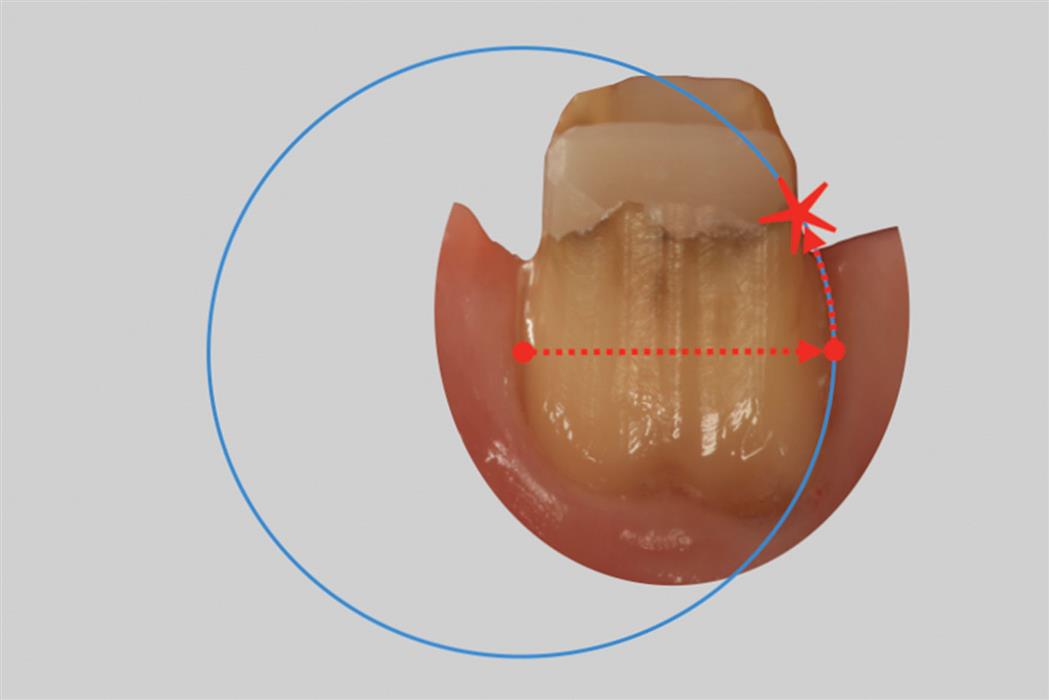
A metal matrix band placed around the adjacent tooth for protection may be helpful; however, the thin band can be perforated and the underlying enamel still damaged. The preferred method is to use the proximal enamel of the tooth that is being prepared for protection of the adjacent structures. Teeth are 1.5 to 2 mm wider at the contact area than at the cementoenamel junction. Therefore, a thin, tapered diamond or tungsten carbide rotary instrument can be passed through the proximal contact area (Fig. 7.3) while leaving a slight “lip” or “fin” of enamel without resulting in excessive tooth reduction or necessitating undesirable angulation of the rotary instrument. The latter situation, tipping the diamond unnecessarily away from the adjacent proximal surface, is a common clinical error.
Soft Tissues
Placing preparation finish lines subgingivally takes great planning and care lest the periodontal soft tissues becomes red, inflamed, or recede (see Chapter 5). Naturally, a poor periodontal response at the gingival margin of a crown can adversely impact the esthetic result.
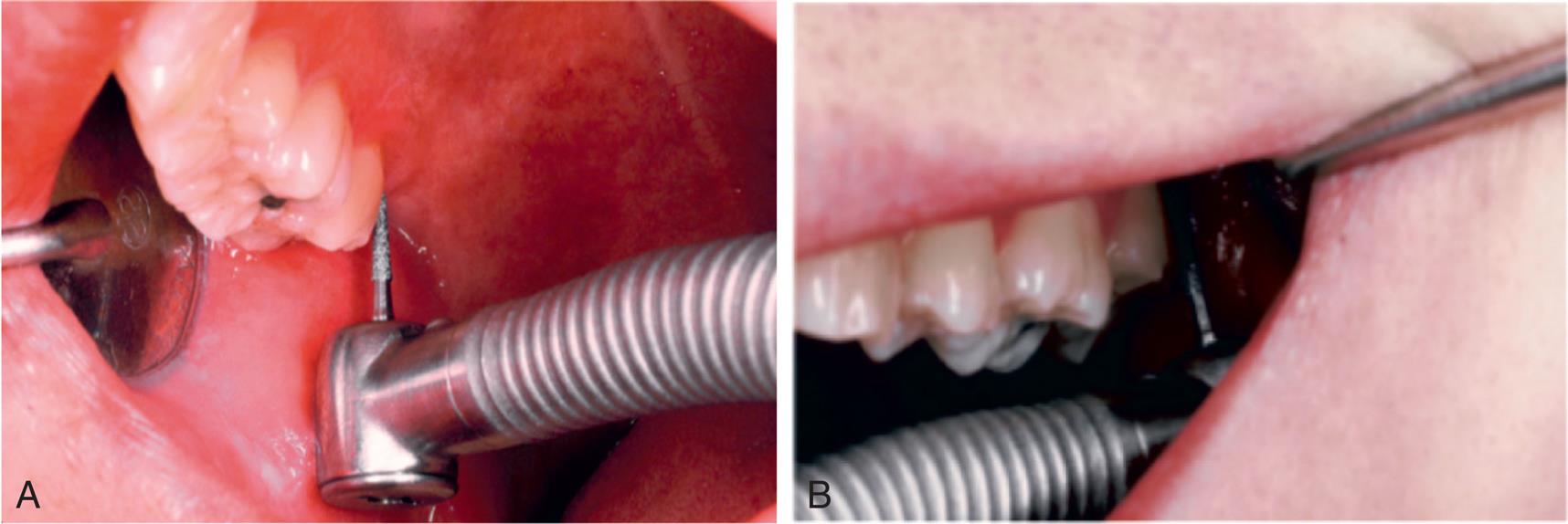
Damage to the soft tissues of the tongue and cheeks can be prevented by careful retraction with an aspirator tip, mouth mirror (Fig. 7.4), or flanged saliva ejector. Great care is needed to protect the tongue when the lingual surfaces of mandibular molars are being prepared.
Pulp
Great care is also needed to prevent pulpal injuries during fixed prosthodontic procedures, especially when significant amounts of tooth structure are being removed. Pulpal degeneration that occurs many years after tooth preparation has been documented.5 Extreme temperatures, chemical irritation, or microorganisms can cause an irreversible pulpitis,6 particularly when they occur on freshly sectioned dentinal tubules. Prevention of pulpal damage necessitates selection of techniques and materials that reduce the risk of injury while teeth are prepared.7
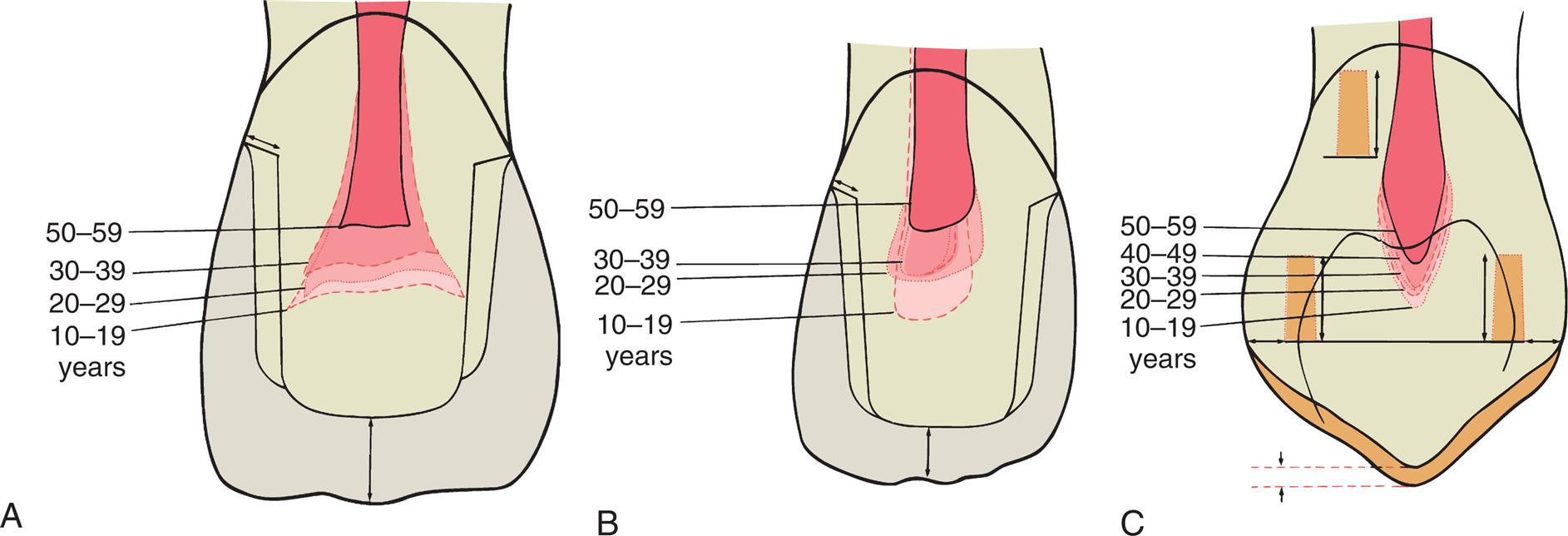
Tooth preparations must account for the geometry of the pulp chamber. Pulp size can be evaluated on a radiograph and decreases with age. Up to about age 50, it decreases more so occlusocervically than faciolingually. Average pulp dimensions have been related to coronal contour8 and are presented in Table 7.1 and Fig. 7.5. Literature reports 5.7% to 33.8% of teeth prepared for a compete crown or fixed partial denture (FPD) retainers succumb to pulpal degeneration and require endodontics.9–12 Vital pulp survival in teeth restored with single metal-ceramic crowns was more favorable than teeth prepared for FPD retainers.12 Pulp tissue in maxillary anterior teeth prepared for metal-ceramic FPD has a higher risk of necrosis than for any other tooth type.12 This is not a contradiction for crowns or FPDs but illustrates the importance of careful case selection, meticulous delivery of patient care, and constant improvement of one’s clinical skills.
Table 7.1
| Age Range (Years) | Length (Millimeters) | |||||
|---|---|---|---|---|---|---|
| Coronal | Incisal to PH | Mesial Surface to PH | Distal Surface to PH | Labial Surface to PH | Palatal Surface to PH | |
| Maxillary Canine | ||||||
| 10–19 | 10.7 | 4.4 | 3.4 | 4.0 | 2.7 | 2.3 |
| 20–29 | 10.6 | 4.6 | 3.3 | 3.7 | 3.1 | 2.6 |
| 30–39 | 10.5 | 4.8 | 3.0 | 4.0 | 2.9 | 2.5 |
| 40–49 | 9.5 | 4.8 | 3.0 | 3.6 | 2.8 | 2.8 |
| 50–59 | 9.5 | 5.4 | 2.8 | 3.4 | 2.9 | 3.0 |
| Mean ± SD | 10.23 ± 0.26 | 4.8 ± 0.20 | 3.1 ± 0.13 | 3.7 ± 0.12 | 2.9 ± 0.11 | 2.6 ± 0.15 |
| Range | 8.29–12.7 | 3.8–7.2 | 2.3–3.6 | 2.9–4.8 | 2.5–3.5 | 1.9–3.7 |
DPH, Distal pulp horn; MPH, mesial pulp horn; PH, pulp horn; —, data unavailable.
From Ohashi Y. Research related to anterior abutment teeth of fixed partial denture. Shikagakuho. 1968;68:726.
Causes of Injury
Temperature
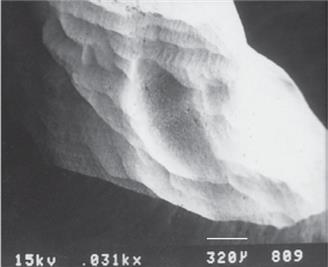
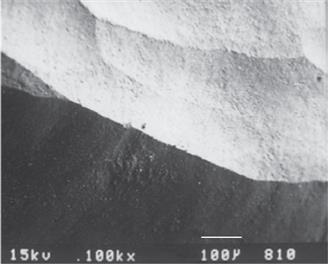
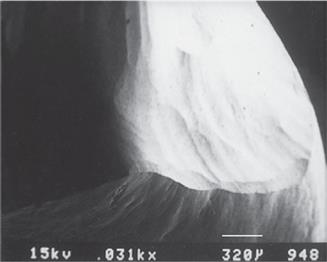
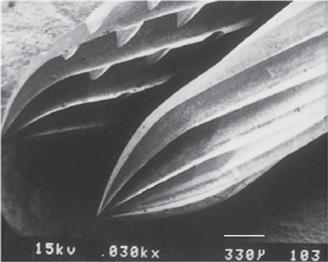
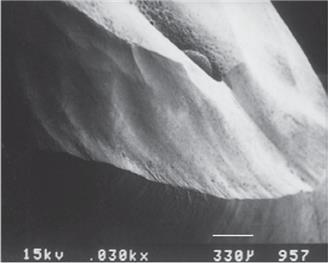
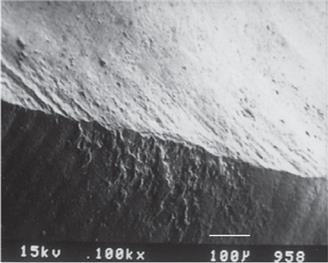
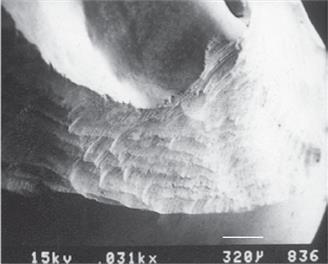
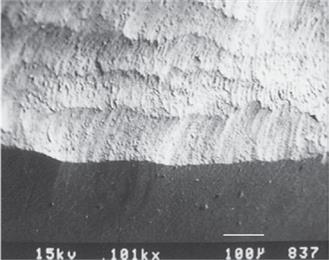
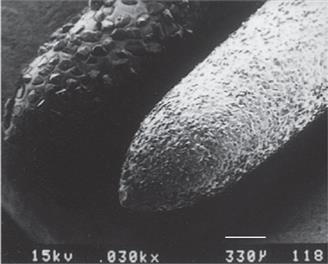
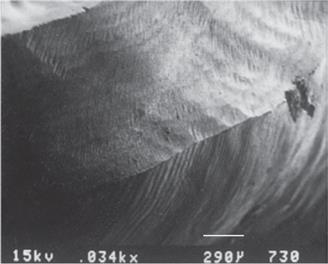
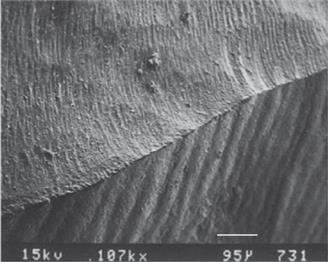
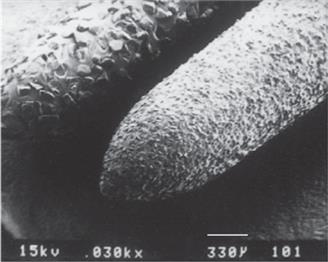
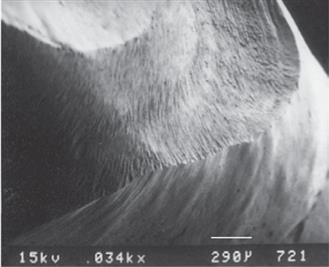
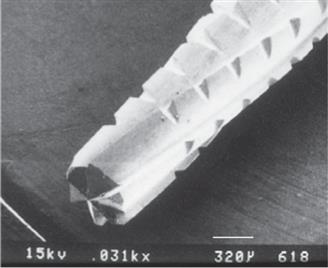
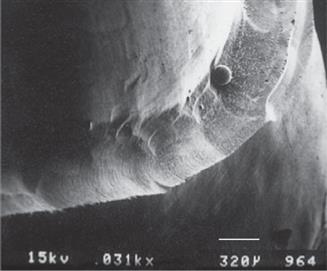
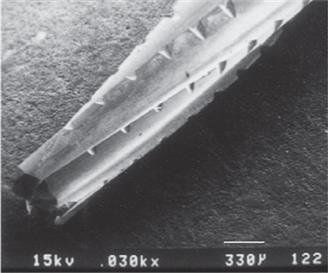
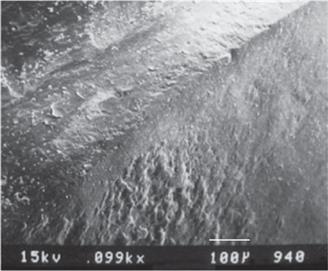
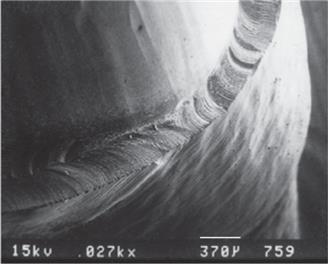
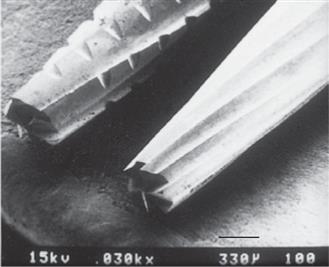
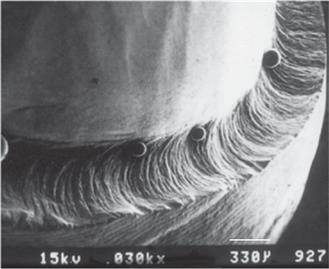
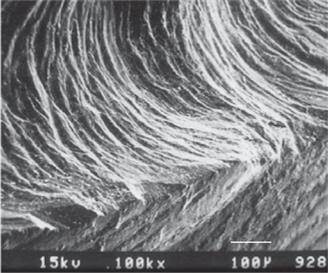
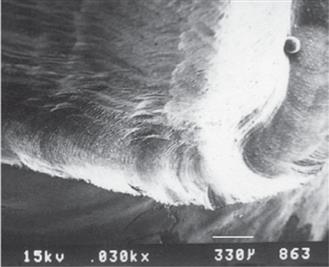
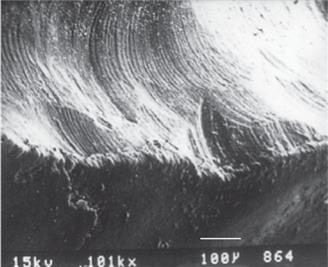
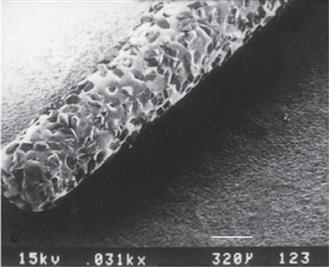
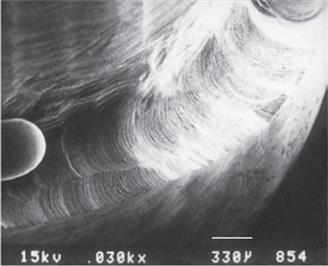
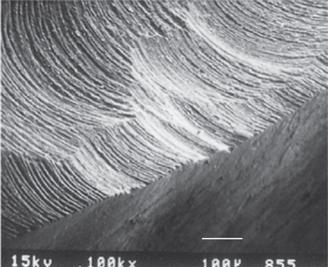
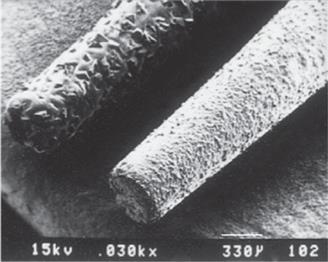
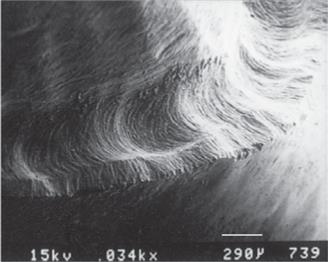
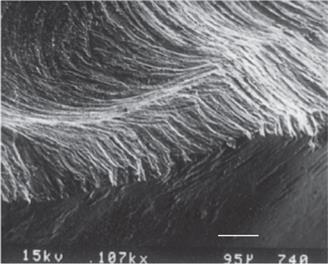
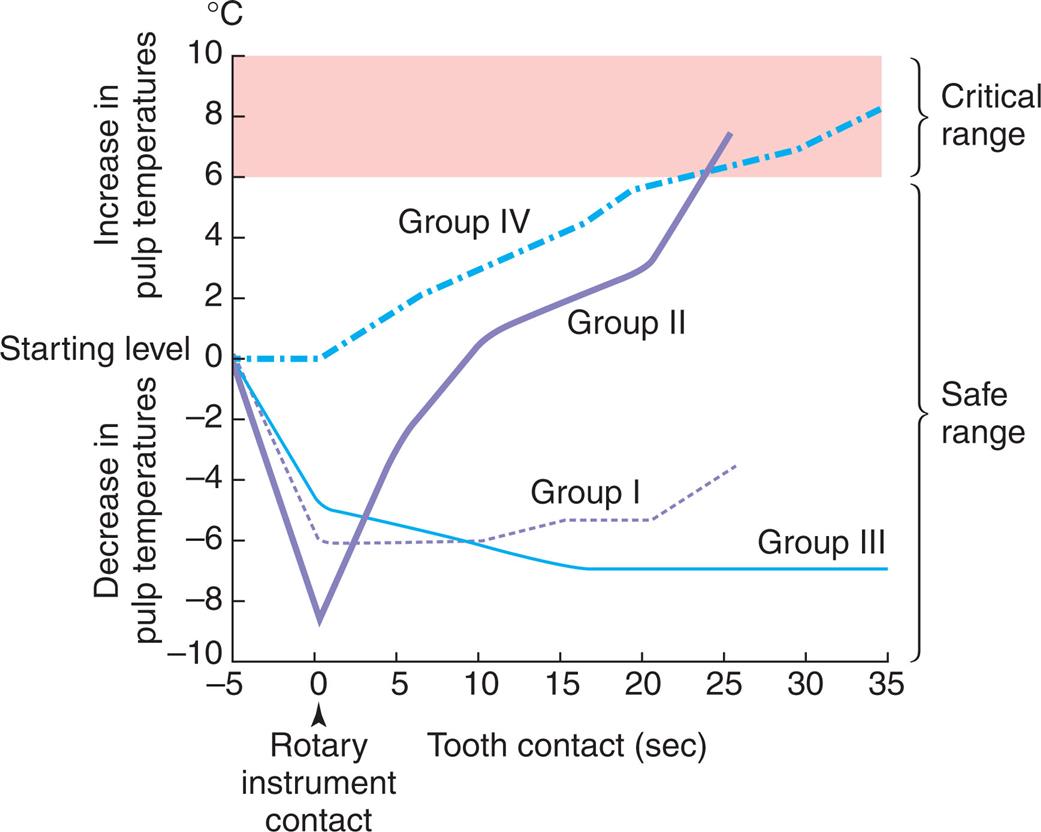
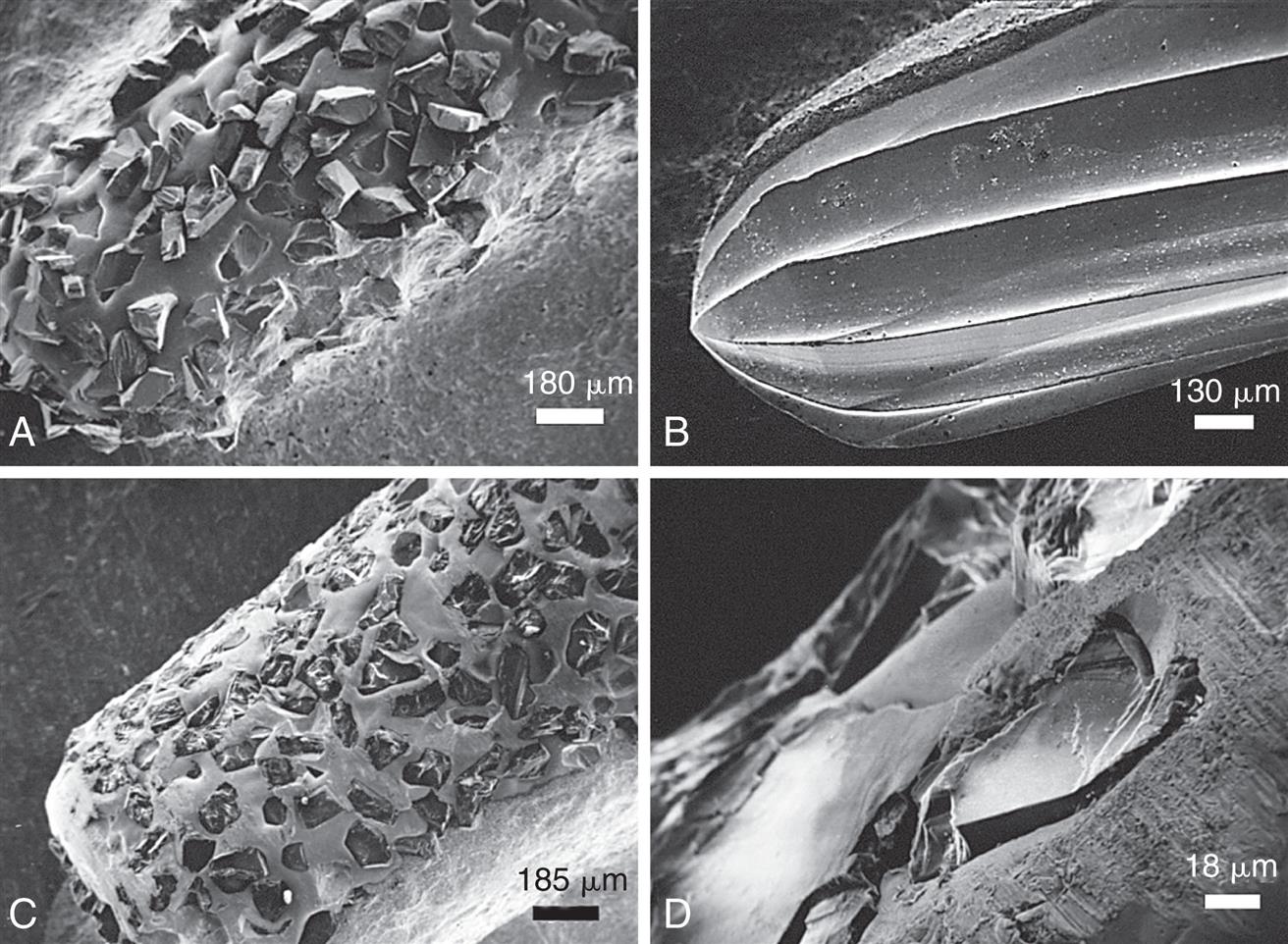
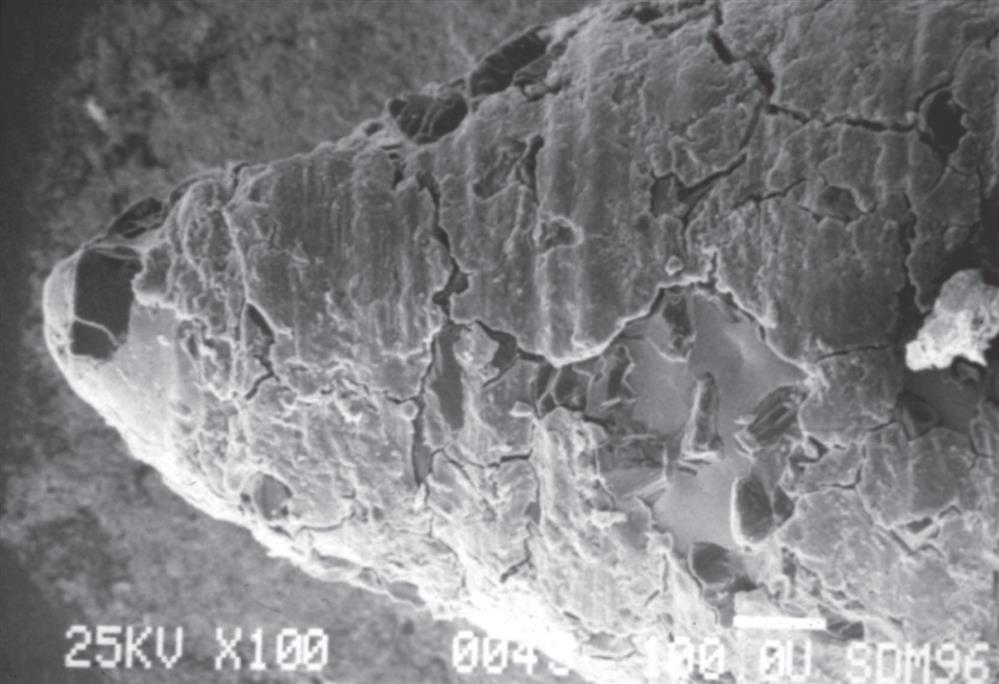
Considerable heat is generated by friction between a rotary instrument and the surface being prepared (Fig. 7.6). Excessive pressure, higher rotational speeds, temperature and flow rate of water coolant13 along with the type, shape, and condition of the cutting instrument (Fig. 7.7) may all increase the generated heat.13,14 When using a high-speed handpiece, a feather-light, intermittent touch (approximately 100 g) allows efficient removal of tooth material with minimal heat generation.15 Nevertheless, even with the lightest touch, the tooth overheats unless a water spray is used. The spray must be accurately directed at the area of contact between tooth and rotary instrument. It also washes away debris, which is important because rotary instrument clogging reduces cutting efficiency (Fig. 7.8).16 Irrigation also prevents dentin desiccation (which may cause severe pulpal irritation).5,17 Debris accumulation has been shown to vary with rotary instrument shape. Shoulder- and chamfer-shaped diamonds may accumulate less debris. Debris is not readily removed after 5 minutes of ultrasonic cleaning.18 During tooth preparation, rotary instrument performance is largely dependent on the dentist’s execution of the specific clinical procedure and less on handpiece design and characteristics.19
Electric handpieces have adjustable rpms. Generally, gross tooth reduction and shaping is done with 200,000 rpm using water coolant. If the spray prevents adequate visibility, as may be the case when a margin is being finished, rotations can be reduced to 17,000 rpm with reduced water spray. Alternatively, hand instrumentation can be used as the safest option. Relying on air cooling alone with a high-speed handpiece is hazardous because a tooth can easily overheat and the pulp is easily damaged.20
Particular care is needed when preparing grooves or pinholes because coolant cannot reach the cutting edge of the rotary instrument. To prevent heat buildup, these retention features should ideally be prepared at low rotational speed or with a high-speed handpiece with a feather-light intermittent touch.
Chemical action
Biomaterials in tissue engineering
The chemical action of certain dental materials (bases, restorative resins, solvents, and luting agents) can cause pulpal damage,21 particularly when applied to freshly cut dentin. Resin-based sealers increase crown retention when luted with resin, modified-resin, and resin-modified glass-ionomer cements.22,23 However, adhesive systems can be cytotoxic and affect the viability of odontoblastic cells.24,25 Compounds may be released from dental adhesive cements that are known carcinogens.24,25
Matrix metalloproteinases (MMPs) are known to exist within the dentin collagen hybrid bond layer.26 MMPs are a group of enzymes that modulate biological cellular mechanisms through multiple signaling pathways in normal physiological processes as well as cancer invasion, metastasis, and inflammatory diseases.27,28 MMPs degrade physical barriers as in extracellular matrix proteins such as the collagen in the dentin-resin hybrid layer. When dentin is etched, MMPs are released by pulpal odontoblast cells to the dentinal tubules.26 Since it is difficult for an adhesive to infiltrate the full depth of the conditioned dentin, deep collagen is not protected from MMPs.29 In the laboratory through transmission electron microscopy, it has been observed that the number of dentin collagen fibrils within the hybrid layer of the resin-dentin bonded interface significantly decreases within 44 months of water storage.30 Hydrolytic degradation of the hybrid layer is symptomatic by water tree propagation, also known as nanoleakage.31
Dental agents applied to etched dentin are capable of inhibiting MMP.32 Treating prepared dentin with 5% glutaraldehyde has been used successfully to decrease dentinal hypersensitivity. It has no effect on the retention of crowns.33 However, it is capable of preserving resin-dentin bond by cross-linking collagen in the hybrid layer and MMPs.34 By itself, glutaraldehyde is not harmful to odontoblast-like cells. However, when mixed with hydroxyethylmetacrylate (HEMA), the compound material is cytotoxic.34 Chlorhexidine, carbodiimine, and proanthocyanidin when applied to acid-etched dentin have also been successfully used to significantly reduce MMP activity.32
MMP inhibitor research looks promising in that the dentin treatments will improve the long-term durability of the hybrid layer by making it less prone to degradation. Future clinical research is indicated to evaluate MMP inhibitor challenges with nanoleakage, recurrent caries, postoperative sensitivity, cytotoxicity, cell vitality, and integrity of the prosthesis.
Bacterial action
Vital dentin seems to resist infection.35 However, pulpal damage under restorations has been attributed36,37 to bacteria that either were left behind or gained access to the dentin because of microleakage.38 Bacteria have been detected in the interface between clinically acceptable crowns and failed root canals.39 This indicates that the fitting surface of a crown to a tooth is a potential pathway for bacterial leading to endodontic complications.40
The colonization and adhesion of bacteria in oral biofilms have been associated with secondary caries41,42 and gingival inflammation.43 The roughness of a crown cement margin has also been suggested to influence plaque accumulation.44 It has been demonstrated that monolithic ceramics with a glazed surface have a greater roughness than a polished one and will tend to accumulate more biofilm.45 When oral biofilmes attach to a resin-dentin margin, the acidity of the bacteria can weaken the bonded interface.46 When an adhesive resin cement is used, it is recommended to polish the margin area after curing.44
Many dental materials, including glass ionomers, zirconia-reinforced glass-ionomer, and zinc phosphate cement, have an antibacterial effect.47,48 Many dentists use an antimicrobial agent, such as chlorhexidine gluconate disinfecting solution after tooth preparation and before cementation to clean the abutment, although clinical trials do not show an improvement in postoperative sensitivity,49 retention, or failure rates when used for direct composite resin restorations.50,51
A general clinical recommendation in fixed prosthodontics is that all carious dentin be removed before placement of a restoration that will serve as a foundation for a comprehensive reconstruction. In general, for teeth that will subsequently receive indirect restorations, direct pulp caps are contraindicated because subsequent failure of the pulp cap is likely to jeopardize costly prosthodontic treatment.
Conservation of Tooth Structure
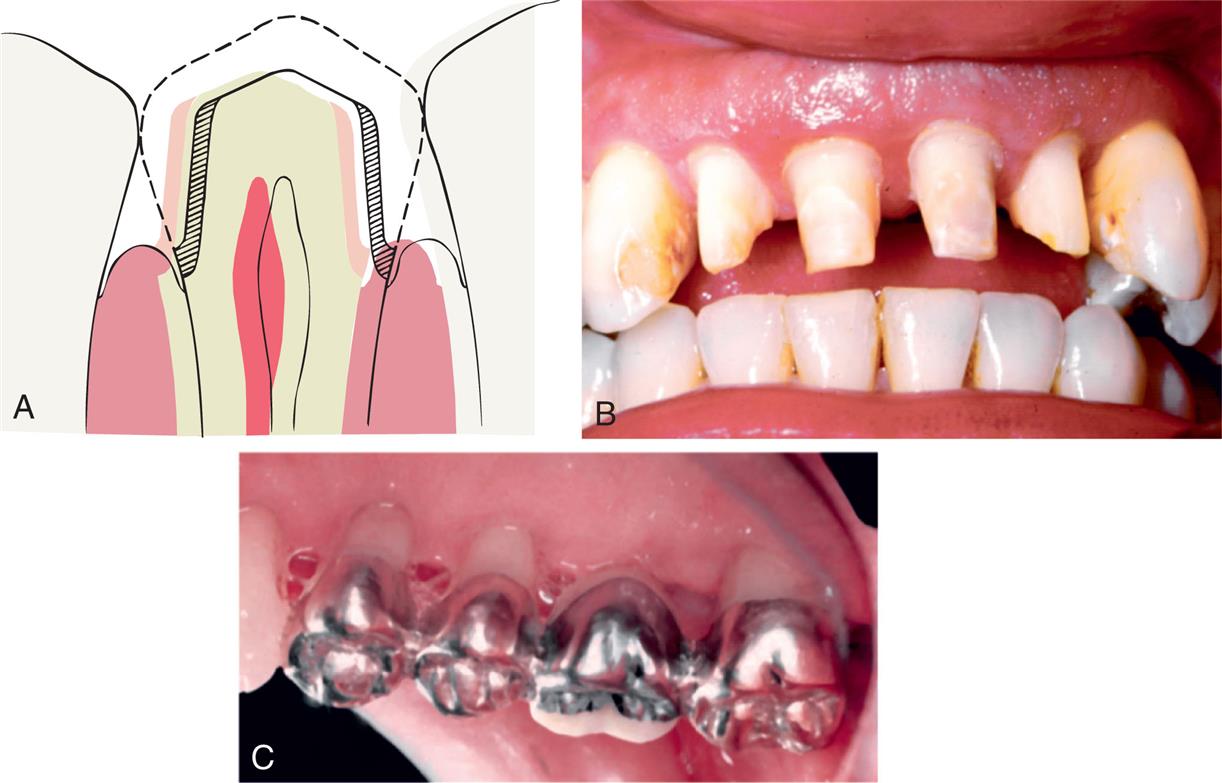
One of the basic tenets of restorative dentistry is to conserve as much tooth structure as possible while preparation design remains consistent with the adhesive or mechanical principles and coupled to esthetic and outcomes in tooth preparation. Tissue preservation reduces the harmful pulpal effects of the various procedures and materials used. Remaining dentin thickness has been shown52 to be inversely proportional to pulpal response, and tooth preparation in close proximity to the pulp should be avoided. Dowden53 argued that any damage to the odontoblastic processes would adversely affect the cell nucleus at the dentin-pulp interface, no matter how far from the nucleus it occurred. Thus, in assessing a possible adverse pulpal response, the amount of residual dentin must be taken into consideration; particular care must be exercised when vital teeth are prepared for complete-coverage restorations (Fig. 7.9).
Tooth structure is conserved through adherence to the following guidelines:
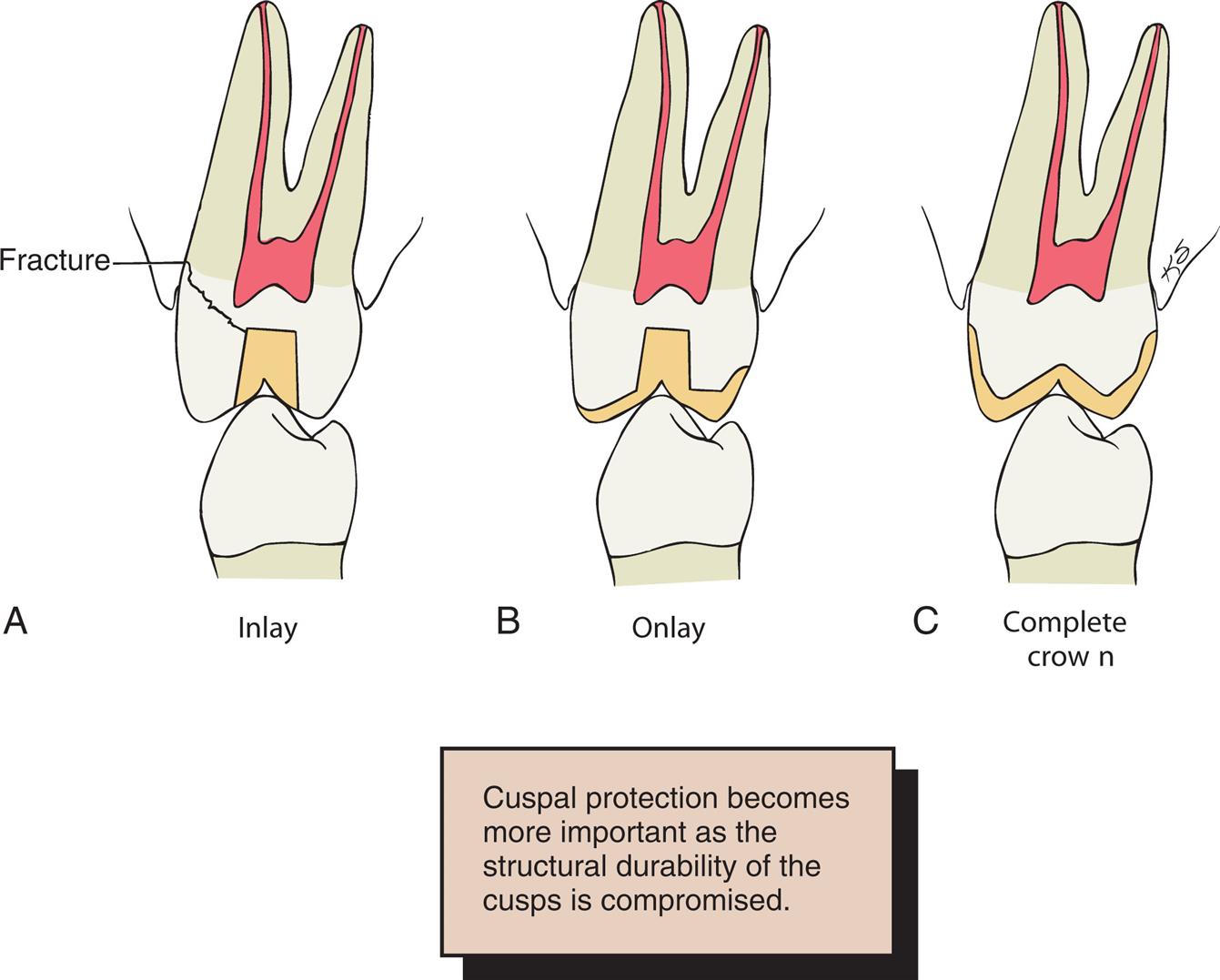
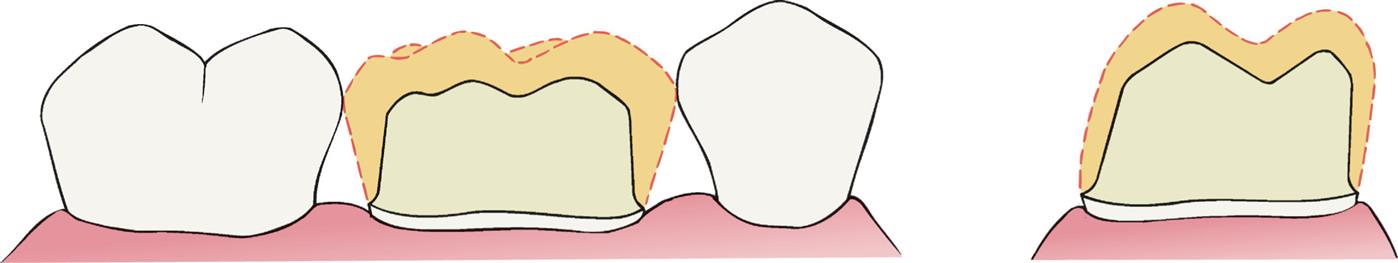
- 1. Use of partial-coverage rather than complete-coverage restorations (Fig. 7.10)54
- 2. Use adhesive bonding techniques to preserve enamel for bonding instead of preparing multiple axial walls (Fig. 7.11)
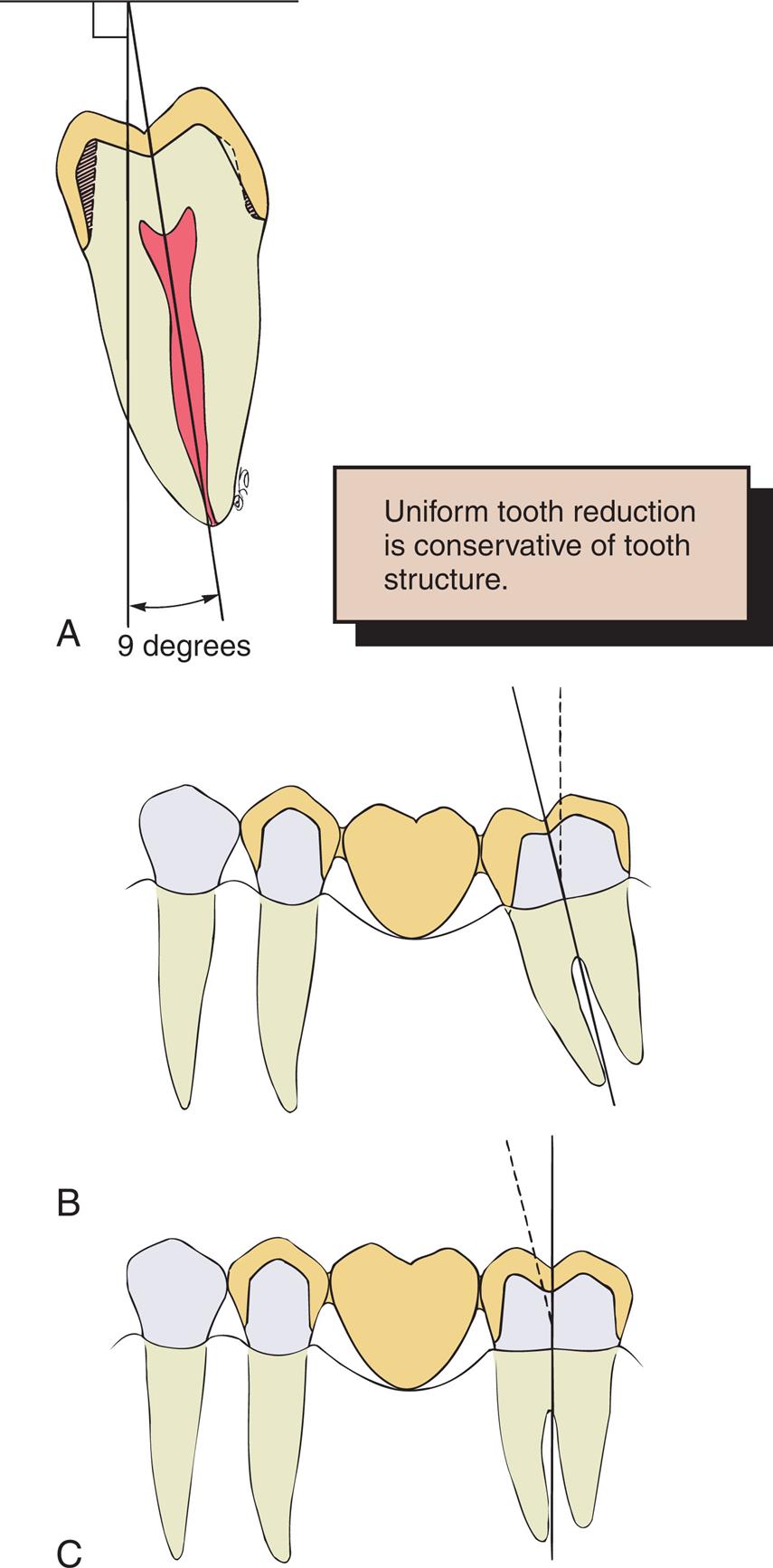
- 3. Preparation of the occlusal surface so that reduction follows the anatomic planes and produces uniform thickness in the restoration (Fig. 7.12)
- 4. Selection of a margin geometry that is conservative and yet compatible with the other principles of tooth preparation (Figs. 7.13 and 7.14)
- 5. Avoidance of unnecessary apical extension of the preparation (Fig. 7.15), which would result in loss of additional tooth structure
- 6. When a complete crown is indicated: Preparation of teeth with the minimum practical convergence angle (taper) between axial walls (Fig. 7.16)
- 7. When a complete crown is indicated: Preparation of the axial surfaces so that a maximal thickness of residual tooth structure surrounding pulpal tissues is retained; if feasible, teeth may be orthodontically repositioned (Fig. 7.17; see Figs. 3.8 and 3.9), allowing less axial convergence than necessary when tooth alignment is less than optimal to accommodate preparations for fixed dental prosthetic retainers

Considerations Affecting Future Dental Health
Current techniques in tooth preparation and materials used for fixed reconstructions are compatible with healthy periodontium when patients are educated and motivated in self-performed oral hygiene.55,56 The primary etiological factor for periodontitis is bacterial biofilm. However, improper tooth preparation may have adverse effects on long-term dental health. For example, insufficient axial reduction inevitably results in overcontoured restorations that hamper plaque control. This may cause periodontal disease57 or dental caries in patients without good oral hygiene and a pathogenic oral biofilm. Alternatively, inadequate occlusal reduction may result in poor form and subsequent occlusal dysfunction. Poor choice of margin location, such as in the area of occlusal contact, may lead to chipping of ceramic, or enamel.58
Axial Reduction
Crown contours have been long debated with little scientific evidence. Gingival inflammation is commonly associated with crowns and fixed dental prosthetic abutments that have excessive axial contours, probably because it is more difficult for the patient to maintain plaque control around the gingival margin (Fig. 7.18).59 Successful preparations provide a balance between sufficient space for the development of anatomically correct axial contours and conservation of tooth structure to preserve a durable abutment. The junction between the restoration and the tooth must be smooth and free of any ledges or abrupt changes in direction.

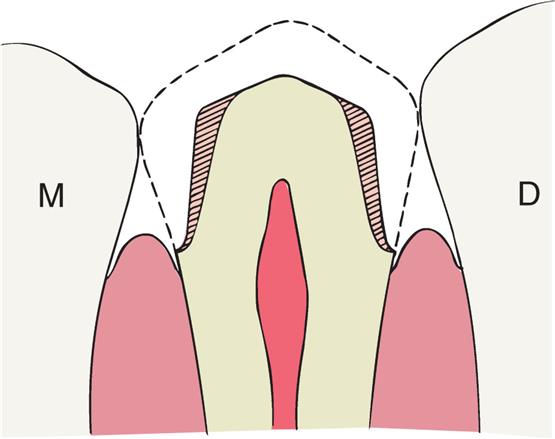
In most circumstances, a crown should duplicate the profile of the original natural tooth that it is restoring.60,61 Natural anterior teeth have facial mean subgingival emergence angles of 9.93 ± 5.68 degrees to the long axis of the tooth and 14.34 ± 8.44 degrees at the lingual.62 As the contours migrate supragingivally, they slightly increase on the facial and lingual 11.13 ± 7.92 degrees and 15.58 ± 9.16 degrees respectively.62 If an error is made, a slightly undercontoured, flat restoration is better because it is easier to keep free of plaque; however, increasing proximal contour on anterior crowns to maintain the interproximal papilla63 (see Chapter 5) may be beneficial from an esthetic perspective. A general guideline is to match the contours of the contralateral tooth. Following this guideline, one would need to impress the complete arch so that these contours are communicated to the laboratory. Sufficient tooth structure must be removed to allow the development of correctly formed axial contours (Fig. 7.19), particularly in the interproximal and furcation areas of posterior teeth, where periodontal disease often progresses with serious consequences.
Margin Placement
Whenever possible, the margin of the preparation should be supragingival. Restorative margins placed within the periodontal sulcus are known as subgingival margins. Subgingival margins of indirect restorations have been identified as a factor in gingival inflammation, bleeding on probing, and recession of the periodontium (see Chapter 5).64–70 Supragingival margins are easier to prepare accurately without trauma to the soft tissues and facilitate impression making or optical capture. They can usually also be situated on hard enamel, whereas subgingival margins are often on dentin or cementum.
Advantages of supragingival margins include the following:
- 1. Improved bonding with no crevicular seepage
- 2. Preservation of cervical tooth structure maintains structural integrity of the abutment
- 3. A dental dam could be used if indicated
- 4. They can be easily finished without associated soft tissue trauma.
- 5. They are more easily kept plaque free.
- 6. Impressions are more easily made, with less potential for soft tissue damage.
- 7. Restorations can be easily evaluated at the time of placement and at recall appointments.
- 8. Elevation of the restorative margin eliminates potential risks of chronic periodontal complications contributed by restorative dentistry.
Subgingival margins (Fig. 7.20), however, are indicated if any of the following conditions are present:
- 1. Dental caries, cervical erosion, or restorations extend subgingivally, and a crown-lengthening procedure (see Chapter 6) is contraindicated.
- 2. The proximal contact area extends apically to the level of the gingival crest.
- 3. Additional retention, resistance, or both are needed (see Restoration/Tooth Interface Considerations section later in the chapter).
- 4. The margin of an esthetic restoration is to be hidden behind the labiogingival crest.
- 5. Root sensitivity cannot be controlled by more conservative procedures, such as the application of dentin bonding agents or connective tissue grafts to cover exposed root structure.

Axial contour modification is indicated: for example, to provide an undercut to provide retention for a removable partial denture clasp (see Chapter 21). To start the emergence profile of a crown more apical to close gingival black triangles Average dimensions for clinical crown height and sulcus depth in young healthy adults are provided in Fig. 7.21.

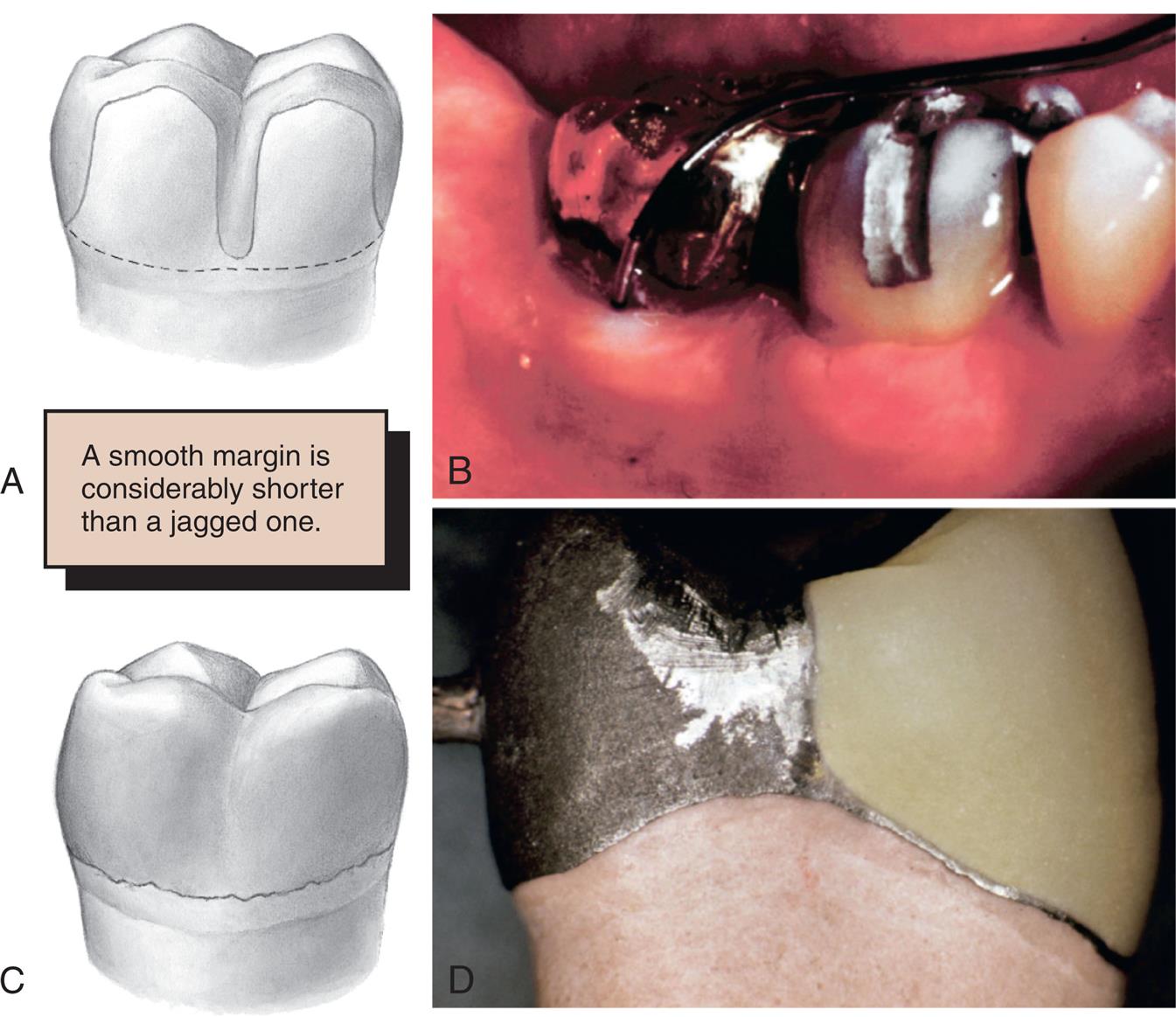
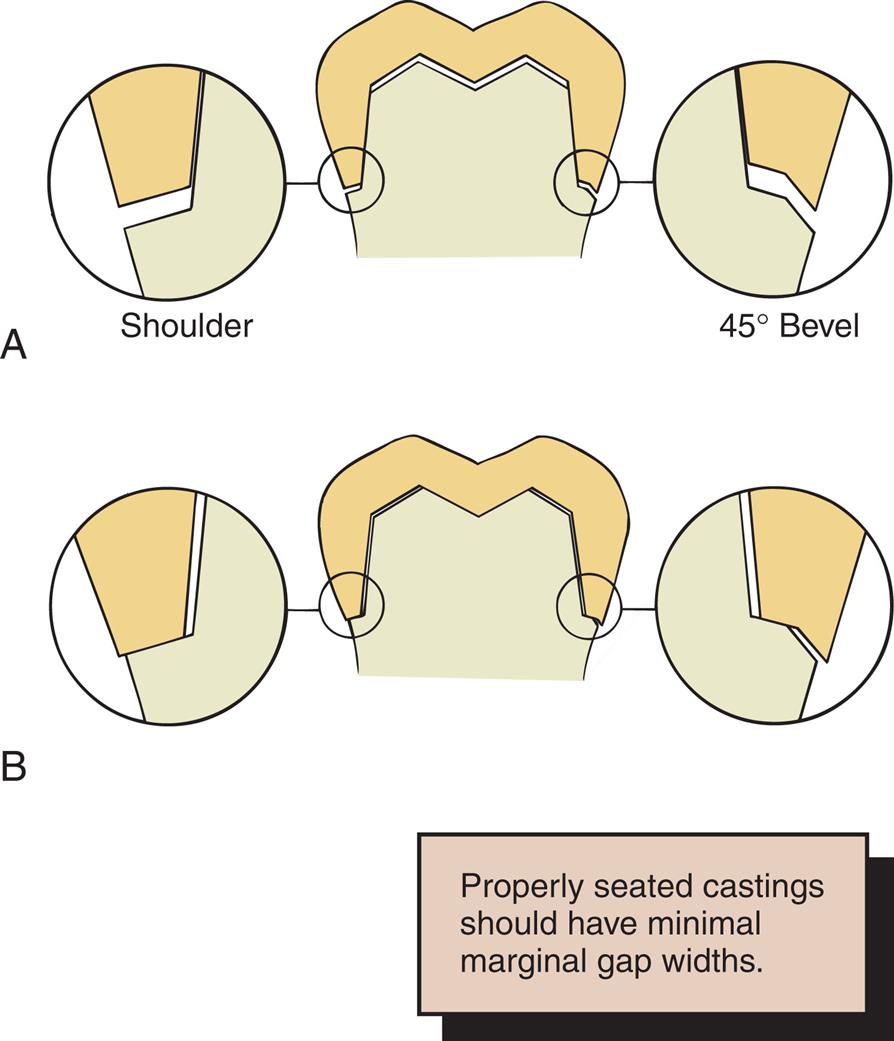
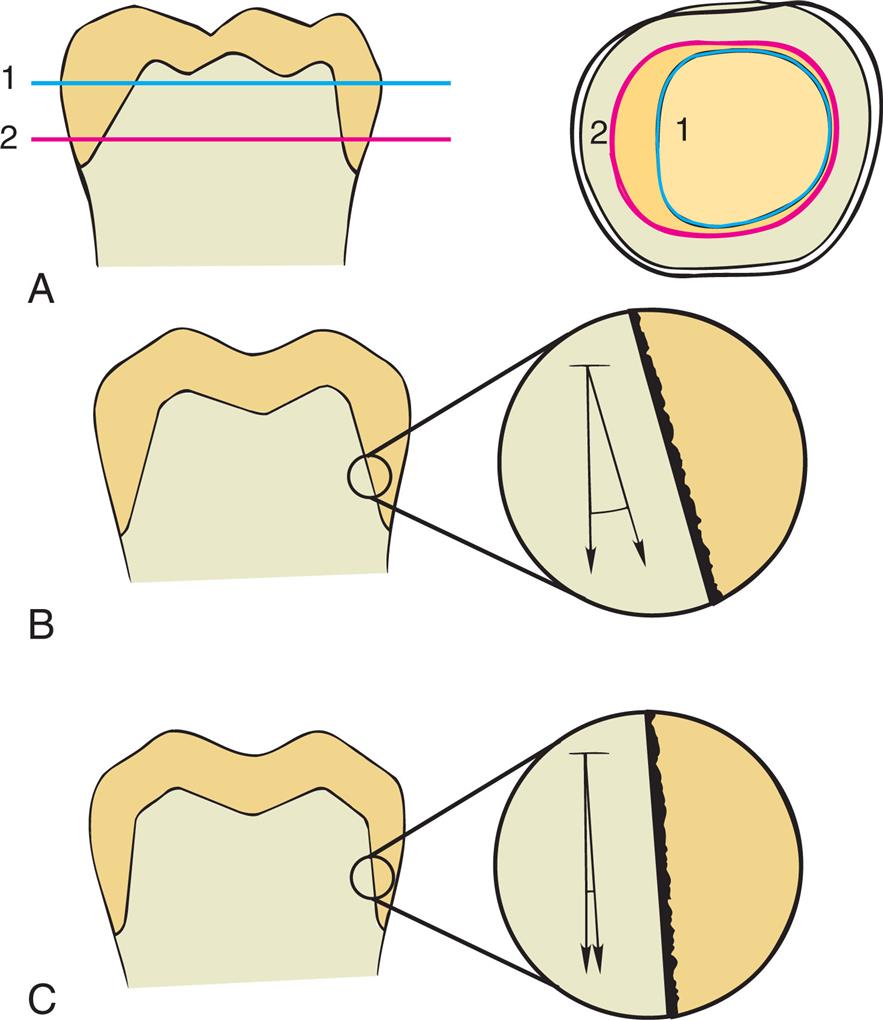
Margin Adaptation
The interface between a restoration and the tooth is always a potential site for recurrent caries because of dissolution of the luting agent and inherent surface roughness. The more precisely the restoration is adapted to the tooth, the lower is the risk for recurrent caries or periodontal disease.71 Although a precise number for acceptable marginal gap width is not known, opinion papers have established a range from 40 to 120 μm.72 A skilled technician can routinely make castings that fit to within 10 μm73 and porcelain margins that fit to within 50 μm,74 provided that the tooth was properly prepared. A well-designed preparation has a smooth and even margin. Rough, irregular, or “stepped” junctions between tooth and restoration greatly increase overall margin length and substantially reduce the adaptation accuracy of the restoration (Fig. 7.22).75,76 The clinical significance of preparing smooth margins cannot be overemphasized. Time spent obtaining smooth margins makes the subsequent steps of tissue displacement, impression making, laboratory communication, die formation, waxing, and finishing much easier and ultimately results in longer-lasting restorations. Smooth, accurately placed preparation finish lines are particularly important when restorations are fabricated with a computer-aided design and computer-aided manufacturing (CAD-CAM) process.77 Preparations need to consider the shape and diameter of the burs that mill the ceramic restorations. Preparations with sharp line angles result in restorations with over-milled intaglio surfaces. Over milling naturally leads to large internal cement gaps.
Margin Geometry
The cross-sectional configuration of the margin has been the subject of much analysis and debate.78–85 Different shapes have been described and advocated (Table 7.2).86,87 For evaluation, the following guidelines for margin design should be considered:
- 1. Ease of preparation without overextension or unsupported enamel at the cavosurface line angle
- 2. Ease of identification in the optical scan or impression and on the (virtual) die
- 3. A distinct boundary to which the virtual design or wax pattern can be terminated and finished
- 4. Sufficient bulk of material (to enable restoration strength at all phases of fabrication and durability for patient service)
- 5. Conservation of tooth structure (assuming the above criteria are met)
Table 7.2
Courtesy Dr. H. Lin.
Proposed margin designs are presented in Table 7.3.
Table 7.3
The feather edge margin design creates a vertical sleeve effect between the tooth and restorations with no horizontal shelf (Fig. 7.23A). Although extremely conservative to tooth structure, feather edge margins have been limited in clinical use because of their challenges with either providing adequate material bulk or creating an overcontoured emergence profile in the restored tooth. These margin designs were frequently used before the development of elastomeric impression materials. Historically, their main advantage was that they facilitated impression making with rigid modeling compounds in copper bands (a technique rarely used today). They were useful for that purpose because there was no ledge on which a band could catch. Restorations with feather margins are difficult from a laboratory technician viewpoint as well. Overcontoured restorations often result because conservative axial reduction may lead to insufficient space to make restorations of adequate thickness within the confines of correct anatomic form. When a cast restoration is planned, the technician can handle the wax pattern without distortion only by increasing its bulk beyond the original contours. For milled restorations, in most esthetic materials, minimal thickness requirements approaching 1 mm apply. However, margins of current mechanically improved ceramics like zirconia and lithium disilicate are durable at 0.5 mm thickness when luted with resin cements.88–90 A 4-year randomized clinical trial on single monolithic zirconia crowns evaluated feather edge and chamfer finish lines. In the trial, the two geometric finish lines had no significant difference in clinical survival and success rates.91 However, zirconia crowns with feather margins had a higher probability of bleeding on probing than the chamfer design. A 9-year retrospective study looked at lithium disilicate single crowns also with feather margins. The 9-year data showed a low clinical failure rate of 1.8%.92 A variation of the feather edge, the biologically oriented preparation technique, is a geometric shape that prepares the tooth in a convergent form without a finish line (modified feather margin).93 Randomized clinical trial found posterior 3-unit zirconia FPDs on biologically oriented tooth preparations have high survival rates and low gingival index after 5 years.94 A variation of the feather edge, the chisel edge margin (see Fig. 7.23B), is formed when the angle between the axial surfaces and the unprepared tooth structure is larger. Unfortunately, this margin is frequently associated with preparations with excessive angles of convergence (taper) and preparations in which the orientation of the axial reduction is not correctly aligned with the long axis of the tooth.
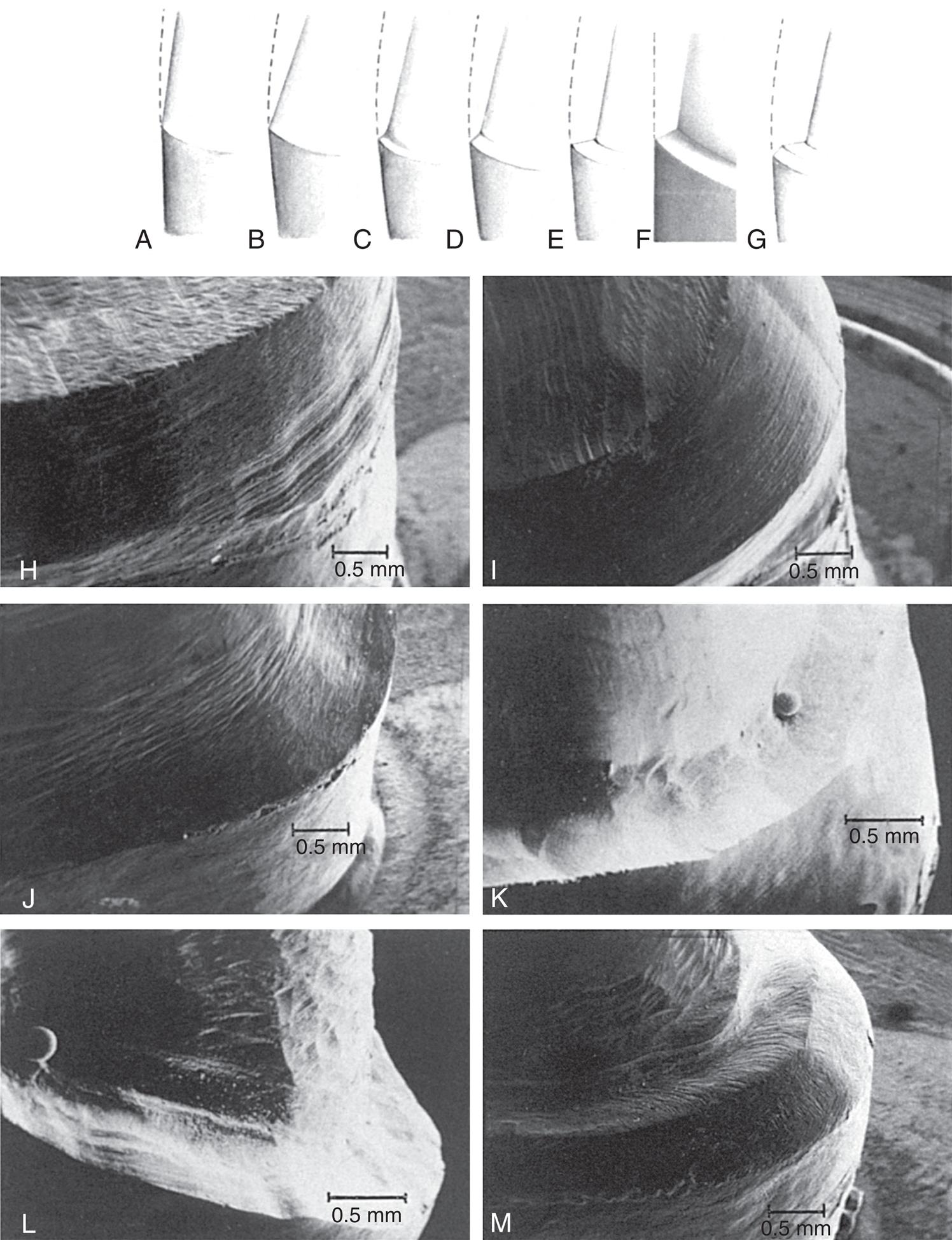
Feather edge preparations may be the best option for porcelain laminate veneer preparations (see Chapter 8), inasmuch as maintaining enamel for the bonded restoration is important for the longevity of the bond. Bulk of the ceramic at the margin can be reduced after bonding (see Chapter 25), and because laminate veneer margins are accessible to the patient, plaque control around veneers is rarely a problem, in contrast to complete crowns.
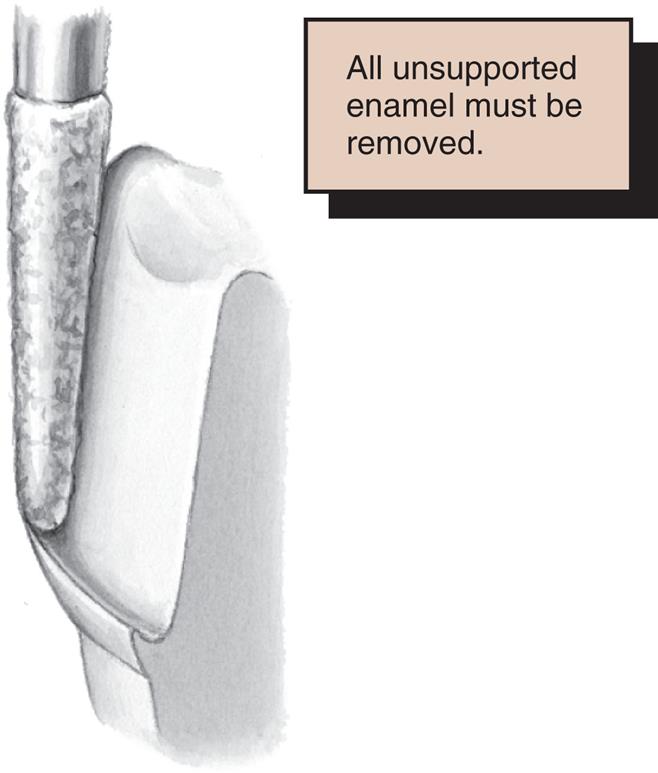
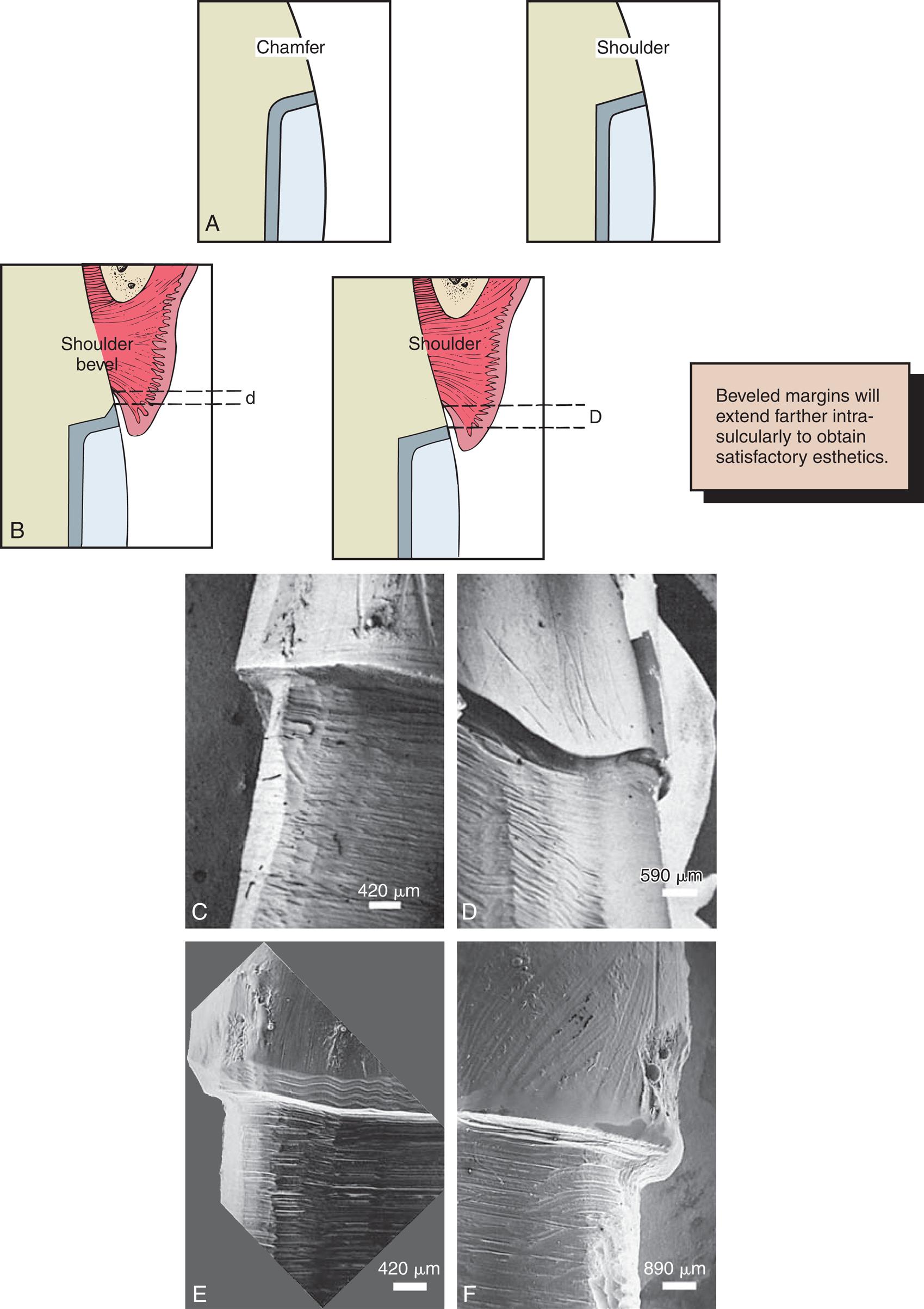
A chamfer margin (see Fig. 7.23C) is particularly suitable for high-strength ceramic, cast metal crowns, and the metal-only portion of metal-ceramic crowns (Fig. 7.24). It is distinct and easily identified, and it provides room for adequate bulk of material and the development of anatomically correct axial contours. Chamfer margins can be placed expediently and with precision, although care is needed to avoid leaving a lip of unsupported enamel (Fig. 7.25).
The most suitable instrument for making a chamfer margin is probably a torpedo shaped diamond with a rounded tip; the resulting margin is the exact profile of the instrument (Fig. 7.26). Marginal accuracy depends on having a high-quality diamond and a true-running handpiece. The gingival margin is prepared with the diamond held precisely in the intended path of placement of the restoration (Fig. 7.27).

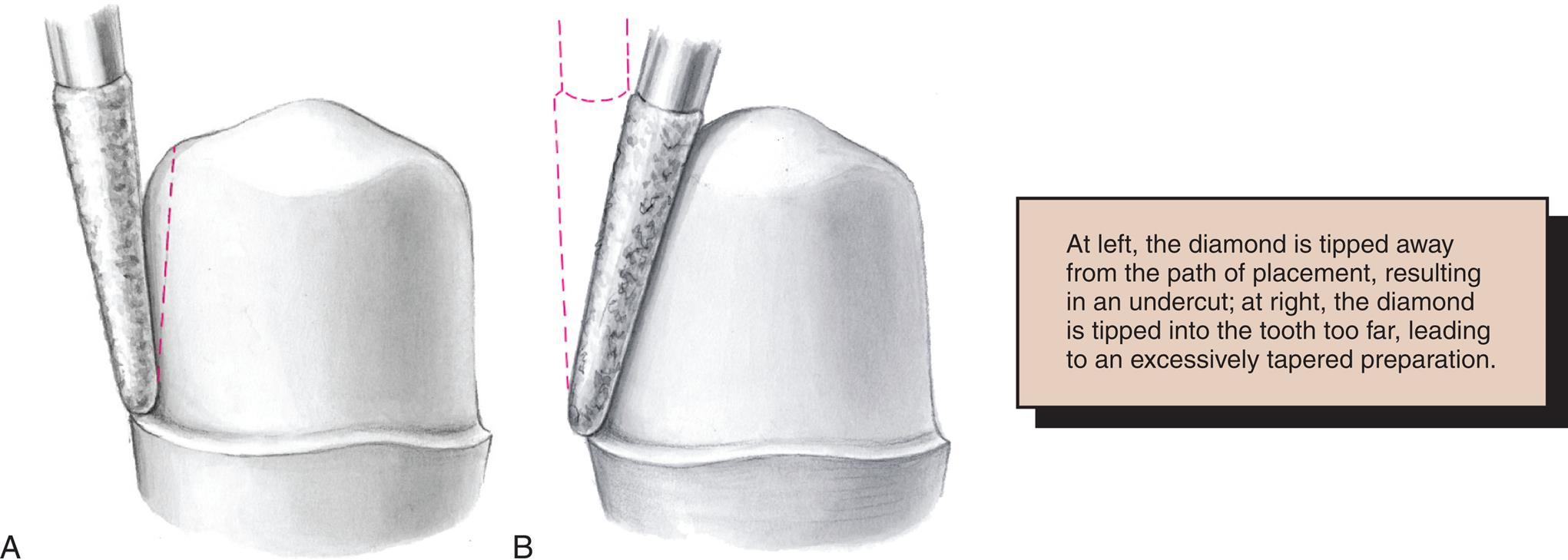
Tilting it away from the tooth produces an undercut, whereas angling it toward the tooth leads to excessive convergence and reduction and loss of retention. The chamfer margin should never be prepared wider than half the tip of the diamond; otherwise, an unsupported lip of enamel may result (see Fig. 7.25). Some authorities have recommended the use of a diamond with a noncutting guide tip to aid accurate chamfer margin placement.95 However, such guides have been shown to damage tooth structure beyond the intended preparation margin.96
In some circumstances, a beveled margin (see Fig. 7.23D) is more suitable for cast restorations, particularly if a ledge or shoulder margin already exists, possibly as a result of dental caries, cervical erosion, or a previous restoration. The objective in beveling is threefold: (1) to allow the cast metal margin to be bent or burnished against the prepared tooth structure; (2) to minimize the marginal discrepancy78 caused by a complete crown that fails to seat completely (however, Pascoe83 showed that when an oversized crown is considered, the discrepancy is increased rather than decreased; Fig. 7.28); and (3) to protect the unprepared tooth structure from chipping (e.g., by removing unsupported enamel). Of note is that when access for burnishing is limited, there is little advantage in beveling. This applies particularly to a gingival margin, in which beveling would lead to subgingival extension of the preparation or placement of the margin on dentin rather than on enamel.
Because a shoulder margin (see Fig. 7.23C) allows room for porcelain and an alloy, it is recommended for the facial part of metal-ceramic crowns, especially when the porcelain margin technique is used. It should form a 90-degree angle with the unprepared tooth surface. An acute angle is likely to chip (Fig. 7.29A). In practice, dentists tend to underprepare the facial shoulder margin,97,98 leading to restorations with inferior esthetics or poor (excessive) axial contour.
Some authorities87 have recommended a heavy chamfer margin rather than a shoulder margin, and some find a chamfer margin easier to prepare with precision. Earlier workers81,82 found less distortion of the metal framework during porcelain application with a shoulder margin, although with modern alloys, these results could not be replicated.99–102
A 120-degree sloped shoulder margin (see Fig. 7.23F) is sometimes used as an alternative to the 90-degree shoulder margin for the facial margin of metal-ceramic crowns. The sloped shoulder margin reduces the possibility of leaving unsupported enamel but leaves sufficient bulk to allow thinning of the metal framework to a knife edge for acceptable esthetics.
A beveled shoulder margin (see Fig. 7.23G) has been recommended by some authorities for the facial surface of a metal-ceramic restoration if a metal collar is planned (as opposed to a porcelain labial margin). The beveling removes unsupported enamel and may allow some finishing of the metal. It is particularly useful for restoring structurally compromised anterior teeth that have preexisting large shoulder finish lines and minimal ferrule effect. The existing shoulder is incorporated into the preparation, but a bevel is placed subgingivally onto the root surface to increase the ferrule effect. The shoulder bevel margin design is a more conservative option for retreating previously restored teeth with existing shoulder margins and slender roots instead of extending the shoulder subgingivally to lengthen axial walls and gain retention. However, when the tooth structure is available, a shoulder or sloped shoulder margin is preferred for esthetic reasons. This allows improved esthetics because the metal coping of the crown can be thinned to a knife edge margin and hidden in the sulcus without the need for positioning the margin closer to the epithelial attachment (see Fig. 7.29B). Table 7.2 illustrates chamfer and shoulder margin preparations obtained with selected instruments.
A comprehensive literature review of current scientific knowledge on complete-coverage tooth preparations suggests that margin design should be selected on the basis of the type of crown, applicable esthetic requirements, ease of formation, and operator experience. Research has not validated the expectation of enhanced fit being associated with the selection of certain types of finish line geometry.103
Occlusal Considerations
A satisfactory tooth preparation allows sufficient space to develop a functional occlusal scheme in the finished restoration. To deliver successful functional occlusion, the clinician has to evaluate the occlusion before occlusal reduction is performed and determine if the patient’s occlusion will be maintained or altered. Typically, the goal of a single crown is to maintain the current occlusal relationship in maximal intercuspation. When the patient’s occlusion is changed, it is customary to involve multiple restorations and to have a diagnostic set up before tooth preparation. The diagnostic setup is discussed later in the chapter. At the assessment of the occlusion, it is important to distinguish between occlusal reduction and interocclusal clearance. The glossary of prosthodontic terms defines occlusal reduction as the quantity of tooth structure that is removed to establish adequate space for a restorative material between the occlusal aspect of the tooth preparation and the opposing dentition.104 In contrast, interocclusal clearance is defined as the amount of reduction achieved during tooth preparation to provide for an adequate thickness of restorative material.104
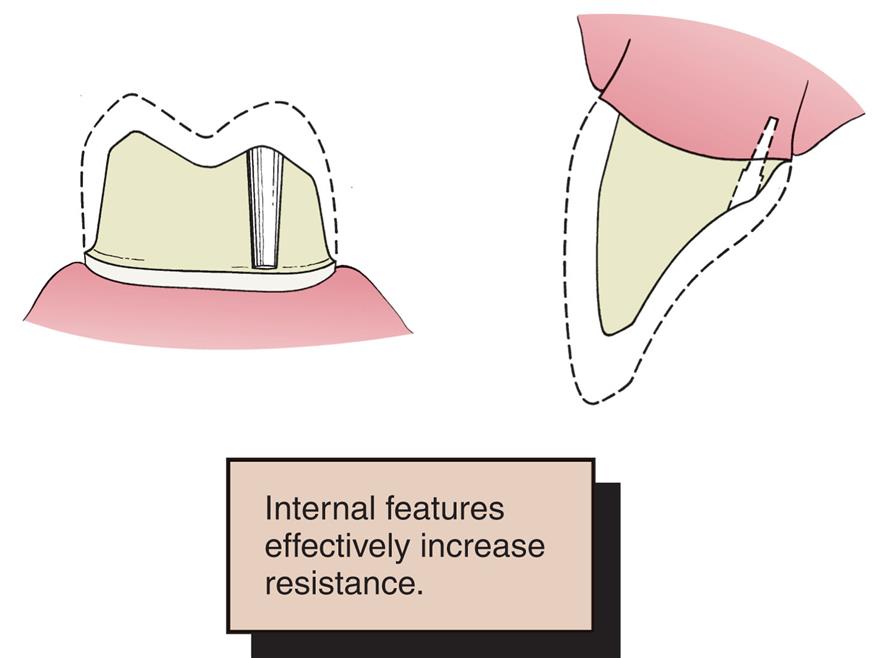
To summarize, the amount of tooth occlusal tooth structure removed is to achieve the appropriate amount of prosthetic space for a specific type of crown so that it can maintain or deliver a successful occlusal scheme for that specific patient. Sometimes, the patient’s occlusion is disrupted by supra-erupted or tilted teeth (Fig. 7.30; see Fig. 3.8B and C). When such teeth are prepared for crowns, the eventual occlusal plane must be carefully analyzed and the teeth reduced accordingly. Considerable reduction is often needed to compensate for the supra-eruption of abutments. In turn, this may shorten tooth preparation axial wall height to the extent that mechanical properties such as retention and resistance are compromised (see the later section on Restoration/Tooth Interface Considerations), which may necessitate the preparation to rely on an adhesive preparation and cementation protocol or perform clinical crown lengthening. In mechanically compromised situations where the residual tooth structure is not adequate for bonding and periodontal crown lengthening is not indicated, it is advised to supplement preparations with secondary retentive features. Secondary retention consists of grooves, boxes, and cast pin retention. It must be noted that internal features like boxes and groves are classically considered for cast alloy restorations and not for ceramics. However, one fatigue study showed that zirconia-based crowns with a mesial and distal groove of 1 mm wide and 1 mm deep, .5 mm coronal of the finish line, halted crack progression at the crowns cameo surface and preparations without grooves did not.105 In addition, a finite element analysis study identified retentive grooves reduced stress concentrations in both the tooth and lithium disilicate glass-ceramic endocrowns.106 Caution must be used with extrapolating clinical results from laboratory studies; however, the data offered looks promising for teeth with questionable mechanical retentive forms.
Sometimes even endodontic treatment is necessary to make enough inter-arch space. However, in these circumstances, compromising the principle of conservation of tooth structure is preferable to the potential harm that might result from a restoration that incorporates a traumatic occlusal scheme. Careful judgment is obviously needed. Diagnostic tooth preparations and diagnostic waxing procedures are essential to help determine the exact amount of reduction necessary to develop an optimum occlusion (see Chapter 4).
Preventing Tooth Fracture
No tooth is unbreakable (Fig. 7.31). If teeth are suddenly smashed together (as in an automobile accident, sports injury, or biting unexpectedly on a hard object), a cusp may break. Cuspal fracture can also result from parafunctional habits such as bruxism.

The likelihood that a restored tooth will fracture can be lessened if the tooth preparation is designed to minimize potentially destructive stresses (Fig. 7.32). For example, an intracoronal cast restoration (inlay) has a greater potential for fracture because when occlusal forces are applied to the restoration, it tends to serve as a wedge between opposing walls of the preparation. This wedging must be resisted by the remaining tooth structure; if the remaining tooth structure is thin (as with a wide preparation isthmus), the tooth may fracture during function. As a result, wide inlay preparations with cohesively cemented gold restorations result in less cuspal stress when the preparation is extended to wrap over the cusps (onlay).107 Teeth with missing vital anatomical parts like marginal ridges and dentin above the pulp chamber are structurally weak in comparison to fully intact teeth.108 In contrast, an in vitro study showed that when indirect composite restorations were adhesively bonded to tooth structure, the restored teeth had similar fracture strength and fracture modes independent of isthmus width and cuspal coverage.109 Another in vitro study concluded that bonded ceramic inlays with isthmus widths and depths of 2 and 3 mm respectively restored the fracture load of teeth to a comparable level to intact teeth.110 However, a different in vitro study investigated large mesio-occluso-distal (MOD) inlay preps with the isthmus depth of 4 and 3 mm wide at the pulpal floor. The faciolingual dimensions of the proximal boxes were prepared to 6 mm wide. The data showed that bonding ceramic to large inlay preparations with week cusps did not strengthen the tooth. It was determined that the MOD preparations weakened the tooth by approximately 59%.111 In situations where the residual cusps are thin and marginal ridges are missing, it may be advisable to perform occlusal reduction to cover the weak cusps with a restoration.
Restoration/Tooth Interface Considerations
Traditional Mechanical Geometric Shapes for Tooth Preparation
Traditional tooth preparation design for fixed prosthodontics was developed before adhesive dentistry and still has relevance today. With badly broken-down teeth and questionable substrates for bonding, an in-depth understanding of certain mechanical principles are valuable; otherwise, the restoration may dislodge, distort, or fracture during service. These principles have evolved from theoretical and clinical observations and are supported by experimental studies. The monolithic zirconia complete crown and FPDs are examples of contemporary restorations that is steeped in traditional tooth preparation design.
Mechanical considerations can be divided into three categories:
Retention and resistance form coexist and work together to develop a geometric form of preparation to prevent a restoration from dislodging.104 For theoretical purposes only, retention and resistance will be discussed separately; however, clinically, it is not possible to have one without the other.
Retention Form and Vertical Forces
Vertical forces (e.g., when the jaws are moved apart after biting on very sticky food) act on a cemented restoration in the same direction as the path of placement. The quality of a preparation that prevents the restoration from becoming dislodged by such forces parallel to the path of placement is known as its retention form. Retention form has to consist of two opposing walls. An axial wall without an opposing axial wall has no mechanical benefit to the geometric space of a tooth preparation. With a complete crown preparation, the tooth is prepared 360 degrees around the tooth to deliver circumferential opposing axial walls at every point. As a result of a complete crown preparation, when the crown is seated on the preparation along its path of placement the axial walls deliver circumferential retention to a crown that will counteract vertical forces of removal. The opposing axial walls of a crown preparation create the primary retention of a crown. Only dental caries and porcelain failure cause more failure of crowns and fixed dental prostheses than does lack of retention.112,113
The dentist must consider the following factors when deciding whether retention is adequate for a given fixed restoration:
Magnitude of the Dislodging (Vertical) Forces
Forces that tend to remove a cemented restoration along its path of placement are small in comparison with those that tend to seat or tilt it. An FPD or splint can be subjected to such forces by pulling with floss under the connectors; however, the greatest removal forces generally arise when exceptionally sticky food (e.g., caramel) is eaten. The magnitude of the dislodging forces exerted by the elevator muscles depends on the stickiness of the food and on the amount of surface area of the preparation. The surface area is affected by the height of axial walls and the diameter of a tooth. Each tooth type has a different inherent risk dependent on its perimeter and height to resist vertical forces generated in the mouth.
Geometry of the Tooth Preparation
Many fixed dental prostheses depend on the geometric form of the preparation and then are supplemented with adhesion. To understand the theory of mechanical retentive forms, it is helpful for one to first understand traditional luting agents. Zinc phosphate, a traditional luting agent, is nonadhesive (i.e., they act by increasing the frictional resistance between tooth and restoration). Interestingly, zinc phosphate is also water soluble. The grains of the luting agent prevent two surfaces from sliding, although they do not prevent one surface from being lifted from another. This is analogous to the effect of particles of sand or dust within machinery: They do not adhere specifically to metal, but they increase the friction between sliding metal parts. If sand or dust gets into a mechanical camera or watch, the increase in friction can effectively jam the mechanism. To demonstrate the success of mechanical retention, zinc phosphate, and the highest level of clinical precision of cast gold restorations, a retrospective clinical evaluation of 1314 cast gold restorations by Dr. R. V. Tucker was performed. Over a period of service that ranged from 1 to 52 years, data showed an overall failure rate of 4.6% with a survival rate of 95.4% (Fig. 7.33).114

Traditional luting agents are effective only if the restoration has a limited number of paths of placement (i.e., the tooth is shaped to restrain the free movement of the restoration). The relationship between a nut and a bolt is an example of restrained movement (Fig. 7.34): The nut is not free to move in just any direction; it can move only along the precisely determined helical path of the threads on the bolt.

The relationship between two bodies, one (in this case, a tooth preparation) restraining movement of the other (a luted restoration), has been studied mathematically and is known in analytical mechanics as a closed lower pair of kinematic elements.115 In fixed prosthodontics, a sliding pair is the only pair that has relevance. It is formed by two cylindricala surfaces constrained to slide along one another. The elements are constrained if the curve that defines the cylinder is closed or shaped to prevent movement at right angles to the axis of the cylinder (Fig. 7.35).
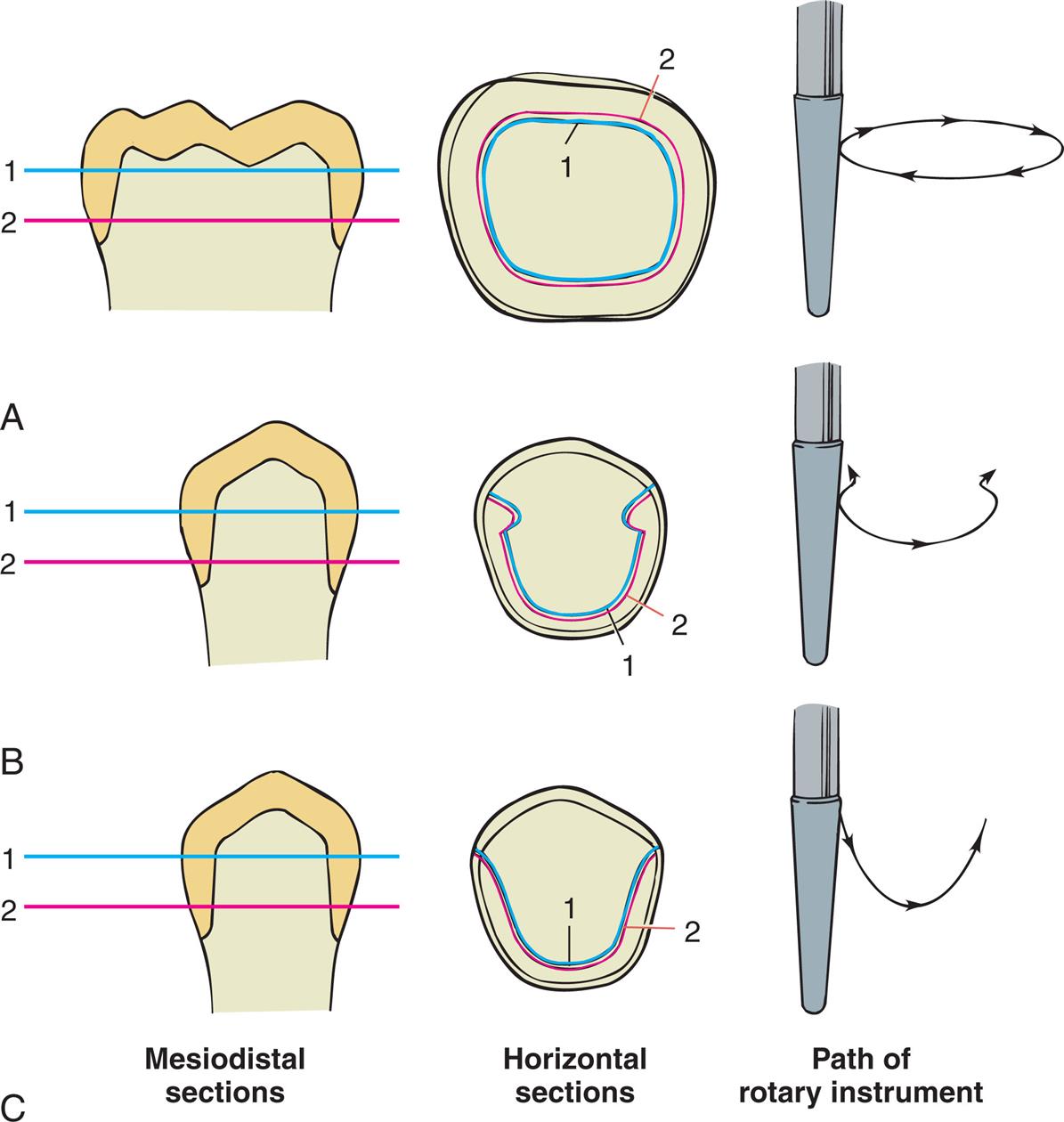
A tooth preparation is cylindrical if the axial surfaces are prepared by a cylindrical rotary instrument held at a constant angle. The fixed curve of the mathematical definition is the gingival margin of the preparation, and the occlusoaxial line angle of the tooth preparation should be a replica of the gingival margin geometry. The curve of a complete crown preparation is closed, whereas the grooves of a partial crown preparation prevent movement at right angles to the long axis of the cylinder. However, if one wall of the complete crown preparation is overtapered, it is no longer cylindrical, and the cemented restoration is not constrained by the preparation because the restoration will have an increased number of pathways for withdrawal. Under these circumstances, the cement particles tend to lift away from rather than slide along the preparation, and the only retention is a result of the cement’s limited adhesion (Fig. 7.36).
Taper
Taper is defined as the convergence of two opposite-facing external walls of a crown preparation as viewed in a given plane (e.g., taper between a mesial wall and a distal wall, or between a buccal wall and a lingual wall of a crown preparation). The extension of those planes forms an angle described as the angle of convergence. Theoretically, maximum retention is obtained if a tooth preparation has parallel walls. However, it is neither desirable nor practical to prepare a tooth this way with current techniques and instrumentation because (1) some convergence is desirable to allow escape of excess luting agent during seating of the crown and (2) slight undercuts are often present in preparations that are too cylindrical and prevent the restoration from seating.
An undercut on a complete crown preparation is defined as any irregularity in the wall of a prepared tooth that prevents the withdrawal or seating of a wax pattern or crown. Such is the case when divergence is inadvertently created between opposite-facing external axial walls, or wall segments, in a cervico-occlusal direction (Fig. 7.37A). In other words, if the cervical diameter of a tooth preparation at the margin is narrower than at the occlusoaxial junction (reverse taper), it is impossible to seat a complete crown of similar geometry (see Fig. 7.37A and B). Undercuts can be present whenever two axial walls face opposite directions (see Fig. 7.37C). Thus, the mesial wall of a complete crown preparation can be undercut in relation to the distal wall, or the buccal wall can be undercut in relation to the lingual wall, and the mesiobuccal wall can be undercut in relation to the distolingual wall. In a partial veneer preparation, in accordance with the same principle, the lingual wall of a proximal groove can be undercut in relation to the lingual wall of the preparation, but the buccal wall of the same groove cannot be undercut in relation to the lingual axial preparation wall; either of these walls may, however, restrict the number of directions in which a restoration can be placed on the preparation in relation to the other.
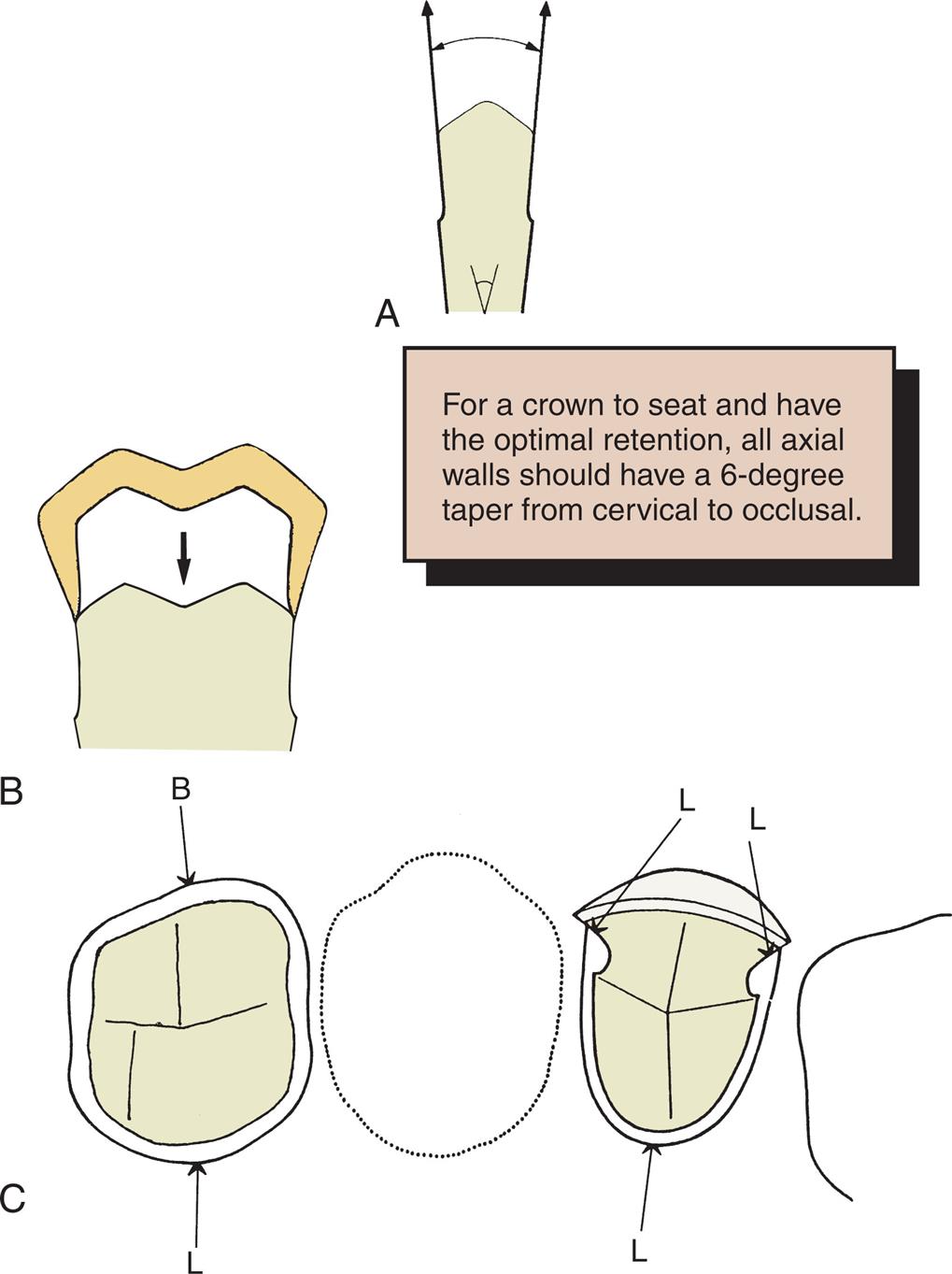
A slight convergence, or taper, is clinically desirable in complete crown preparations. As long as this taper is small, the movement of the luted restoration will be effectively restrained by the preparation and will have what is known as a limited path of placement. As taper increases, so does the number of paths of placement. An increase in the number of paths of placement decreases the tooth preparations retention form.
The relationship between the degree of axial wall taper and the magnitude of retention was first demonstrated experimentally by Jørgensen116 in 1955. He cemented brass caps on Galalith cones of different tapers and measured retention with a tensile-testing machine. The relationship was found to be hyperbolic, with retention rapidly becoming less as taper increased (Fig. 7.38), although the relationship was no longer hyperbolic when the internal surfaces of the caps were roughened. The retention of a cap with 10 degrees of taperb was approximately half that of a cap with 5 degrees. Similar results have been reported by other workers.117–119

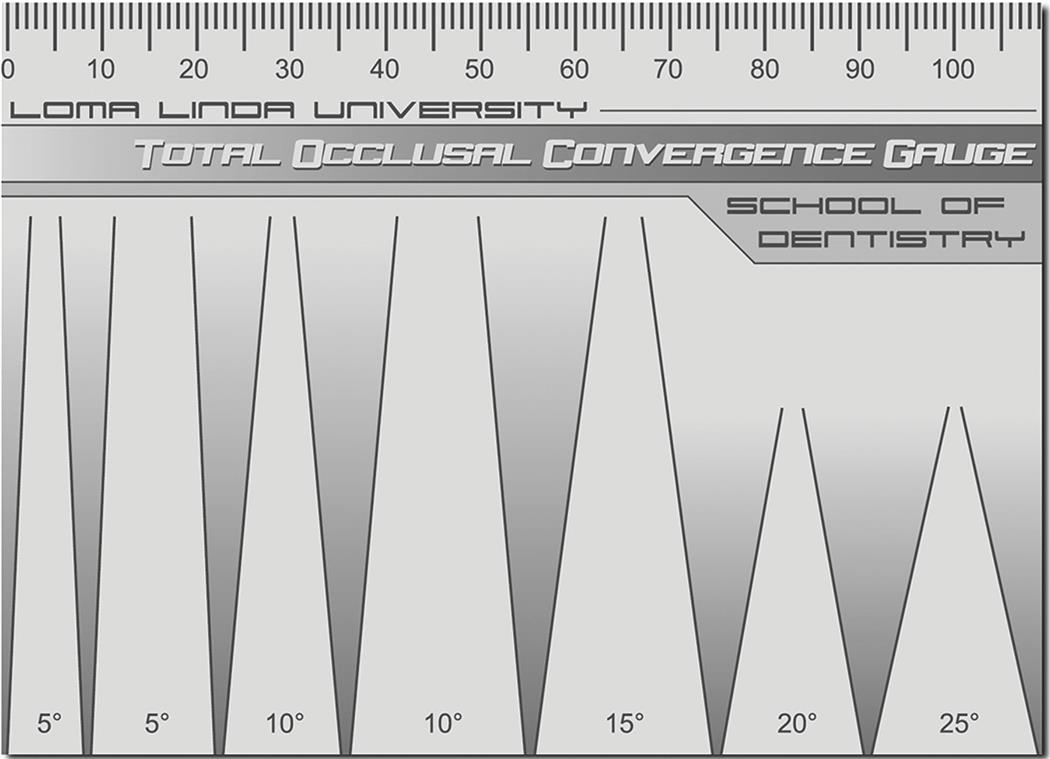
Selection of the appropriate degree of taper for tooth preparation involves compromise. Too small a taper may lead to unwanted undercuts; too large leads to a lack of retention. The traditionally recommended convergence between opposing walls has been 6 degrees. The 6 degrees of convergence was developed between two opposing axial walls of 3 degrees of convergence to a path of removal chosen by a clinician. However, to give perspective, the traditional 6-degree convergence form was recommended to optimize retention for zinc phosphate cement.120 Being able to recognize this angle is important (Fig. 7.39). It is necessary to be able to quickly quantify the approximate angle of convergence between preparation walls. To evaluate the angle from an occlusal perspective, it is recommended to close one eye to judge the relative convergence of all involved axial walls.121 When both eyes are used to evaluate taper, axial walls that are divergent (undercut) up to 10 degrees cannot be detected from a typical viewing distance of 25 to 45 cm (10 to 20 inches).121 Since most individuals are quite skilled at discerning subtle differences in height and width, but less effective in terms of our depth perception, evaluating preparation convergence from the buccal or lingual is often straightforward. Since adjacent teeth can partially obstruct the view of the preparation silhouette from mesial or distal, most will evaluate convergence from as many different directions as conveniently feasible.

It is not necessary to deliberately tilt a rotary cutting instrument to create a taper because this invariably leads to overpreparation. Rather, teeth are easily prepared with a rotary instrument of the desired taper held at a constant orientation. The tapered rotary instrument is moved through a cylindrical path as the tooth is prepared, and the taper of the instrument should produce the desired axial wall taper on the completed preparation. In practice, many dentists experience difficulty consistently avoiding excessively tapered preparations, particularly when preparing posterior teeth with limited access.122–124 Comprehensive review of the dental literature suggests that clinically acceptable taper for a complete crown preparation may range from 10 up to 20 degrees.111 It should be noted, however, that angles of convergence in excess of 10 degrees will result in reduced dentin thickness between the pulpal tissues and the axial walls of the prepared tooth.
Clinicians have a tendency to overtaper preparations. Abutments for fixed dental prostheses tend to be prepared with greater taper than do single crown preparations.121 The visual quantification skill is low enough that some may need additional training.125 One technique that is useful intraorally is the use of a dental bur of known taper to survey the tooth preparation. Another technique is a total occlusal convergence template of known angles to overlay on to tooth preparations to evaluate the amount of taper (Fig. 7.40).
Some authorities recommend the routine use of secondary retention features like grooves, boxes, or even pin holes to supplement the primary retention of crown preparations. Theoretically, they can reduce the incidence of restoration displacement. But it is unclear, however, whether accurate alignment of secondary retentive features is achieved more easily than restricted axial wall convergence. Skillfully prepared axial walls at a minimal convergence are mechanically desirable for primary retention while having a very conservative tooth structure. Furthermore, one research article evaluated the dentin thickness with different amounts of axial taper. In regard to maxillary first premolar, when the axial reduction was preformed with a margin width of 1.2 mm and the axial walls converged at 20 degrees, the proximity to the pulp ranged from 0.3 to 1.8 mm of dentin thickness.126 Dentin is a porous material that delivers protection to the dental pulp. An axial wall of 0.3 mm in thickness raises a clinical concern of creating irreversible pulpitis. Twenty degrees of axial wall convergence may be acceptable for a large molar but is a questionable practice on teeth with smaller diameters. Secondary retentive features may be useful to supplement the primary retention form when retreating teeth that have previously been prepared and over tapered. In the case of a maxillary first premolar with 20 degrees, there may not be enough dentin thickness for a groove without getting a pulp exposure. Since 1955, adhesive resin cements have been developed that have increased the retention of crowns. For some restorations, research suggests that the selection of a resin cement over a water-based luting agent may have more clinical relevance to enhance crown retention than does preparation taper.127,128
Surface area
If the restoration has a restricted taper, and thus a limited path of placement, its retention depends on the length of this path or, more precisely, on the surface area that is in sliding contact. Therefore, crowns with tall axial walls are more retentive than those with short axial walls,129 and molar crowns are more retentive than premolar crowns of similar taper because of the greater diameter of molar teeth. Surfaces from which the crown is essentially being pulled away (rather than sliding along the tooth), such as the occlusal surface, do not add significantly to total mechanical retention.
Stress concentration
When a retentive failure occurs, the luting agent often adheres to both the tooth preparation and the fitting surface of the restoration. In these cases, cohesive failure occurs through the cement layer because the strength of the luting agent is less than that of the induced stresses. A computerized analysis of these stresses130,131 reveals that they are not uniform throughout the luting agent but are concentrated around the junction of the axial and occlusal surfaces. Sharp occlusoaxial line angles should be rounded to minimize these stresses, which can precipitate retentive failure.130,131 Changes in preparation geometry may thus indirectly increase the retention of the restoration.
Type of preparation
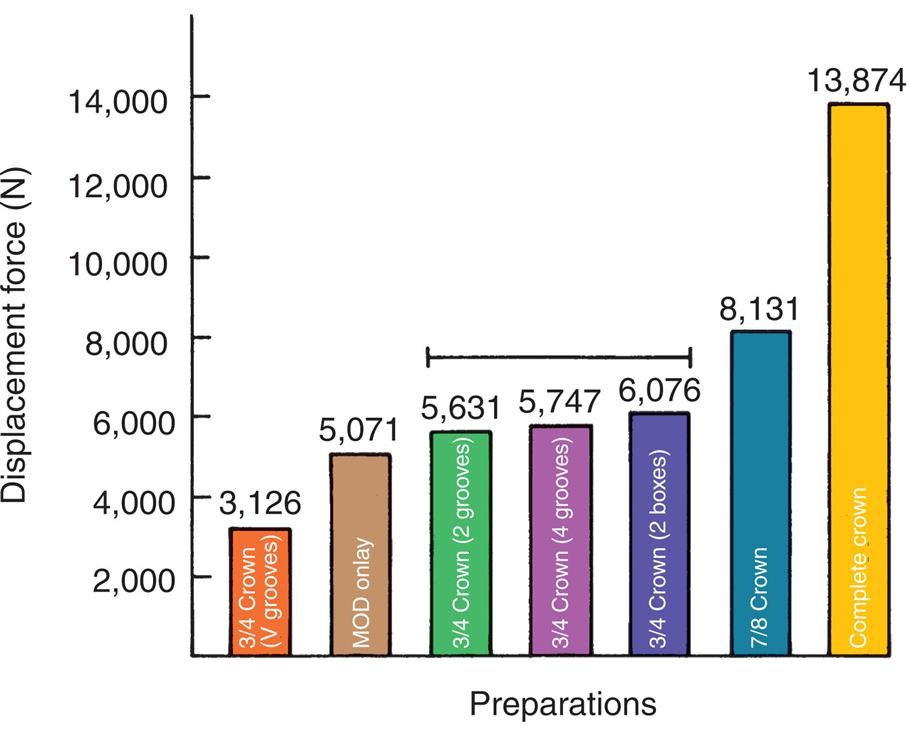
Different types of preparation have different retentive values that correspond fairly closely to the total surface area of the axial walls with restricted taper, as long as other factors (e.g., preparation height) are kept constant. Thus, the retention of a complete crown is more than double that of partial-coverage restorations (Fig. 7.41).132
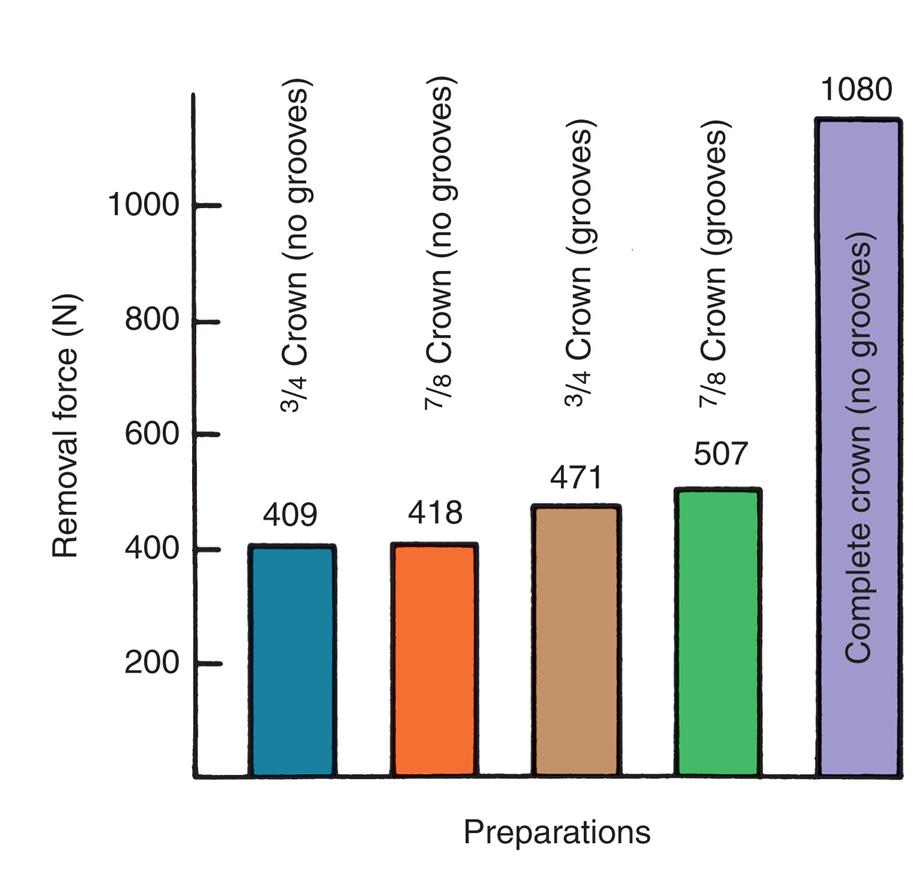
Adding grooves or boxes (Fig. 7.42) to a preparation with a limited path of placement does not markedly affect its retention because the surface area is not increased significantly. However, where the addition of a groove limits the paths of placement, retention is increased.133,134
Roughness of the Surfaces Being Cemented
When the internal surface of a restoration is very smooth, retentive failure occurs not through the cement but at the interface between the luting agent and the restoration. Under these circumstances, retention is increased if the restoration is roughened or grooved.135–137 Metal castings are most effectively prepared by airborne-particle abrading the fitting surface with 50 μm of alumina. This should be done carefully to avoid abrading the polished surfaces or margins. Airborne-particle abrasion has been shown138 to increase in vitro retention by 64%. Similarly, acid etching of the fitting surface of restorations can improve retention with certain luting agents.
Failure rarely occurs at the interface between the luting agent and the tooth. Therefore, deliberately roughening the tooth preparation hardly influences retention and is not recommended because roughness adds to the difficulty of subsequent technical steps in crown fabrication such as imaging, impression making, milling, and waxing (see Chapters 14 and 18).
Materials Being Cemented
Retention is affected by both the type of casting alloy and any core or buildup material that is present on the axial walls of the crown preparation. The clinical significance of laboratory testing results has yet to be confirmed by longer-term clinical studies, but it appears that the more reactive the alloy is, the better adhesion there is with selected luting agents. Therefore, base metal alloys are better retained than are less reactive metals with high gold content.139 The effect of adhesion to different core materials also has been tested, with conflicting results. In one laboratory study,140 researchers examining adhesion between luting agents and core materials found that the luting agent adhered better to amalgam than to composite resin or cast gold. However, when other researchers141 tested crowns for retention, they found higher values with the composite resin cores than with amalgam cores. The differences may have resulted from dimensional changes of the core materials, although the clinical implications of this finding are not clear.
Luting Agent
Type
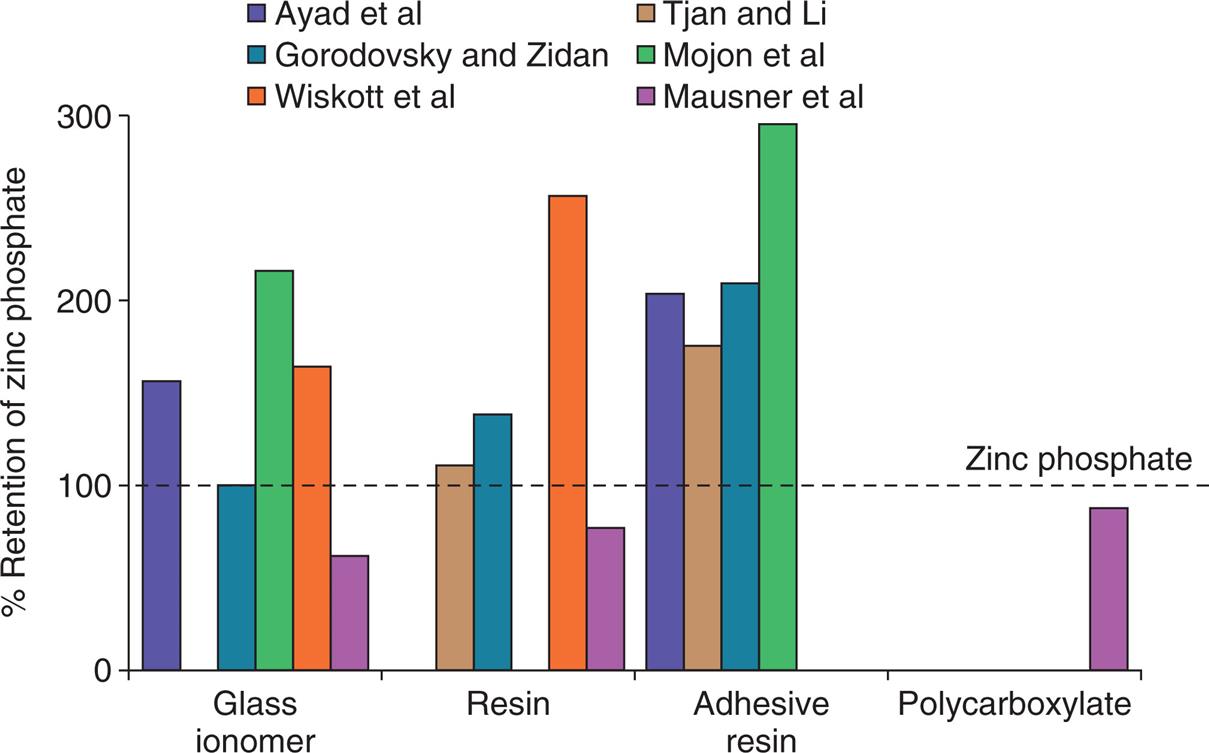
The type of luting agent chosen affects the retention of a cemented restoration.142–144 However, the decision regarding which agent to use is also based on other factors. In general, the data suggest that adhesive resin cements are the most retentive (Fig. 7.43).127,145,146 Of concern is that long-term in vitro studies have shown deterioration of the resin-dentin bond in association with so-called nanoleakage (ability of small ions or molecules to permeate the hybrid layer).147,148
Film thickness
There is conflicting evidence149–152 about the effect of increased thickness of the cement film on retention of a restoration. This may be important if a slightly oversized restoration is made (as when the die-spacer technique is used; see Chapter 18), or when milled crowns are fabricated (see Chapter 25). The factors that influence the retention of a cemented restoration are summarized in Table 7.4.
Resistance Form and Horizontal Forces
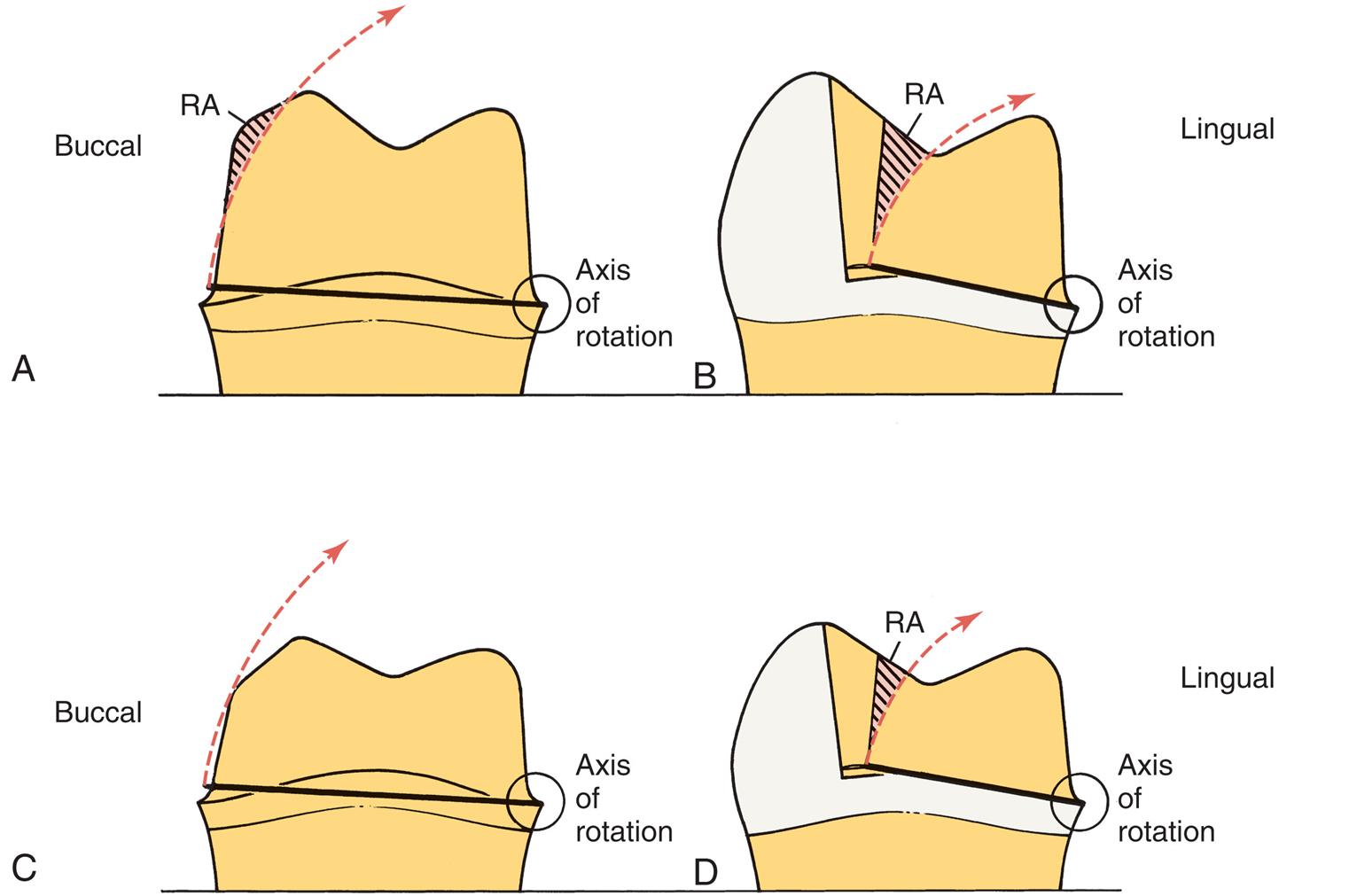
Certain features must be present in the preparation to prevent dislodgment of a cemented restoration in a horizontal plane. Mastication and parafunctional activity may subject a prosthesis to substantial horizontal or oblique forces. These forces are normally much greater than the ones overcome by retention, especially if the restoration is loaded during eccentric contact between posterior teeth. Lateral forces tend to displace the restoration by causing rotation around the gingival margin, effectively tipping the crown off its preparation. Rotation is prevented by any areas of the tooth preparation that are placed in compression, called resistance areas (Fig. 7.44). Multiple resistance areas cumulatively make up the resistance form of a tooth preparation, which is defined as the features of a tooth preparation that enhances the stability of a restoration and resist dislodgment along any axis other than the path of placement.

Adequate resistance depends on the following:
Magnitude and Direction of the Dislodging Forces
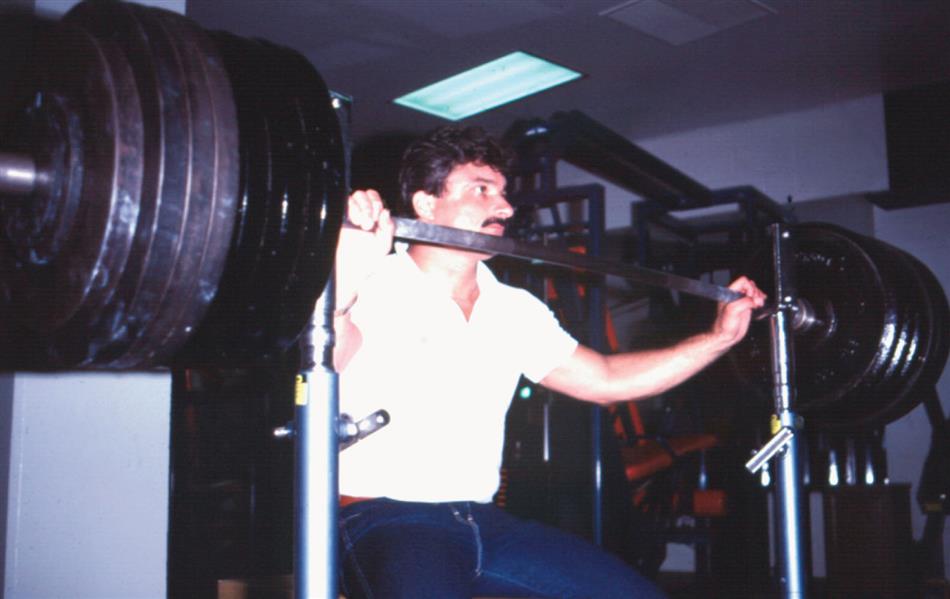
Some patients can develop enormous biting forces. Gibbs and colleagues153 described one individual (Fig. 7.45) who had a biting force of 4340 N (443 kg).c Although this is considered extraordinary, historically, restoration designs attempted to withstand forces approaching such magnitude. In one laboratory study,130 a complete crown cemented on a nickel-chromium test die was found to be capable of withstanding more than 13,500 N (1400 kg)—a far greater force than would occur in the mouth—before becoming displaced (Fig. 7.46).
In a normal occlusion, biting force is distributed over all the teeth; most of it is axially directed. If an FPD is carefully made with a properly designed occlusion, the load should be well distributed and favorably directed (see Chapter 4). However, if a patient has a biting habit such as vaping or parafunctional movements, it may be difficult to prevent fairly large oblique forces from being applied to a restoration. Consequently, the successful tooth preparation and restoration must be able to withstand considerable oblique forces, as well as the normal axial ones, and it has been argued that from a clinical durability perspective, adequate resistance form may be more crucial than overall preparation retentiveness.154,155
Geometry of the Tooth Preparation
As with retention, preparation geometry plays a key role in attaining desirable resistance form. The tooth preparation must be shaped so that specific areas of the axial wall prevent rotation of the crown. A good way to determine whether tooth preparation geometry provides adequate resistance form is to answer a specific question: “How much tooth structure needs to break off in order for this crown to be displaced by tipping off the tooth?”
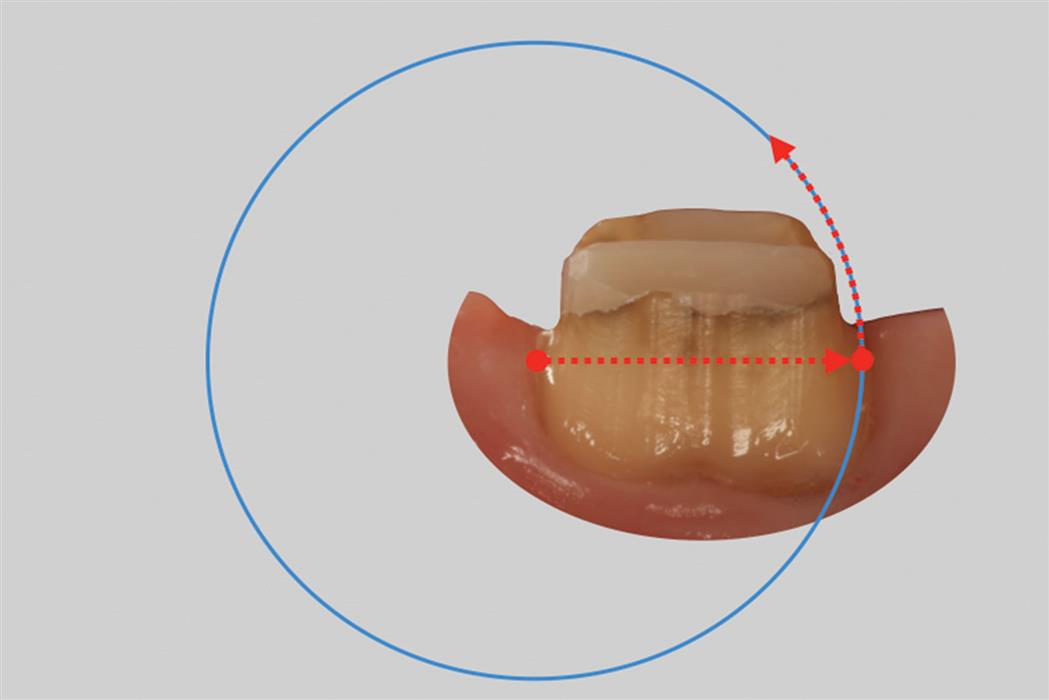
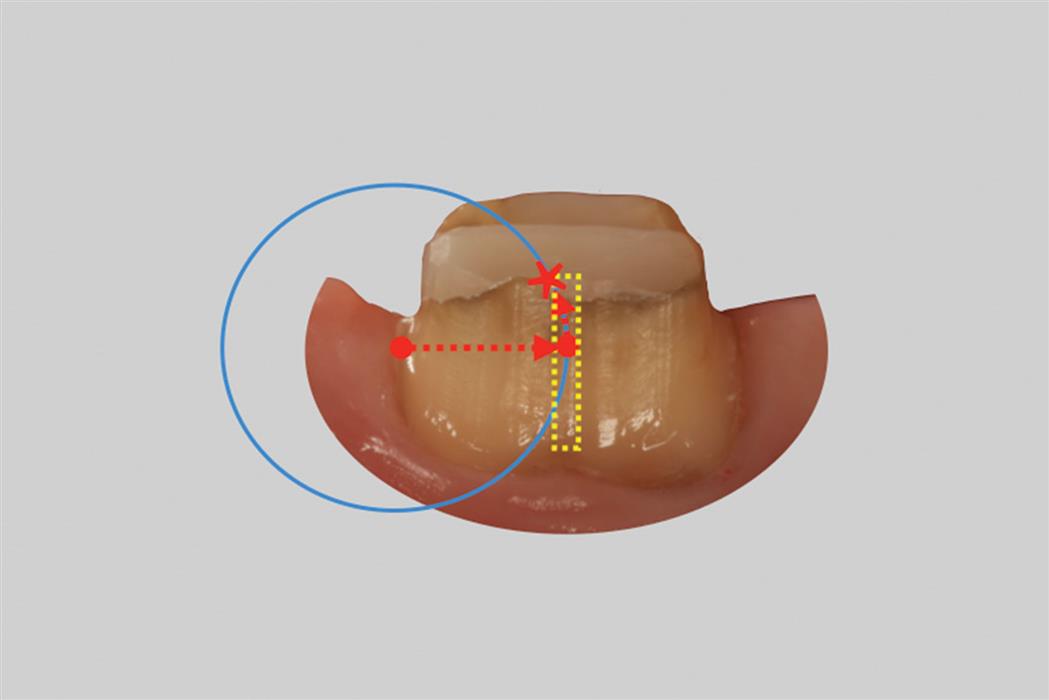
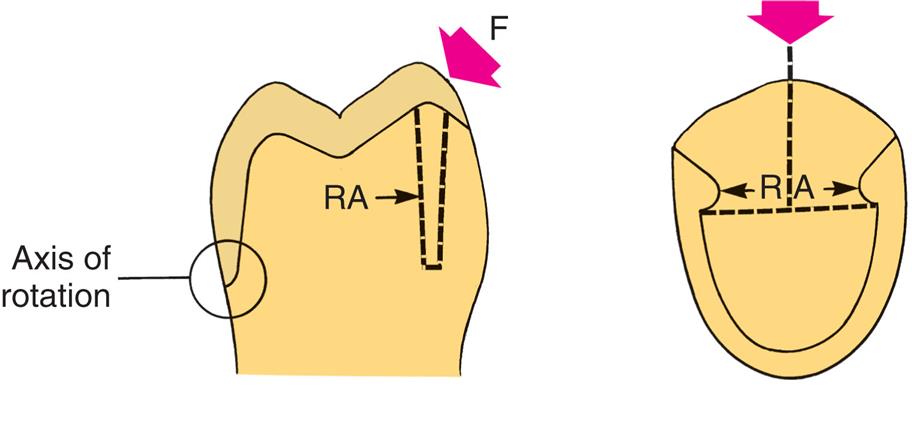
Resistance is a function of the relationship between axial wall taper, preparation diameter, and preparation height. Consider the diameter of a tooth as a radius of an imaginary circle. The radius represents a pathway a crown would theoretically pivot off of a tooth. If the arch of the radius interfered with the axial wall of its tooth preparation, the crown would have resistance (Fig. 7.47). If the arch of the radius did not interfere with the axial wall of its tooth preparation, the crown would not have resistance and rotate off the preparation (Fig. 7.48). Resistance decreases as taper or diameter increases or as preparation height is reduced.156 The relationship between preparation height, or diameter, and resistance to displacement is approximately linear.157
Preparation taper of 5 to 22 degrees has been suggested as being within a clinically acceptable range.158,159 However, at the higher end of this range, the tipping resistance of both cemented and uncemented cast restorations is inadequate but increases significantly as taper is reduced.158,160
Short tooth preparations with large diameters were found to have very little resistance form.161 In general, molar teeth require more parallel preparation than do premolar or anterior teeth to achieve adequate resistance form.161 A 3-mm preparation height provides adequate resistance if taper is restricted to 10 degrees or less,160 but additional height is necessary as tooth diameter increases. On molar crown preparations in which many more preparations are observed that lack resistance,162 minimal preparation wall height should thus be in the range of 3.5 to 4 mm. A fairly simple way to quantify this at chairside is to evaluate whether the height-to-width ratio of a preparation is 4:10 or greater. If so, resistance is probably adequate.
Hegdahl and Silness162 analyzed how the areas that provide resistance form change as the geometry of the tooth preparation is modified. They demonstrated that increasing preparation taper and rounding of axial angles tend to reduce resistance; pyramidal preparations thus have greater resistance than do conical ones. Secondary retentive grooves or boxes placed in healthy tooth structure are particularly effective in enhancing the resistance form of crown preparations because these shorten the theoretical radius of rotation which results in a greater chance of interfering with rotational movement (tipping) of the crown and thereby subject additional areas of the luting agent to compression (Fig. 7.49). Therefore, the resistance form of an excessively tapered preparation can be improved by adding such grooves or boxes. As an alternative, pinholes can be prepared to achieve the same effect by making use of dentin that surrounds the pin.
Preparation modifications appear not to be used as often157 as clinical failure data suggest they should be.155
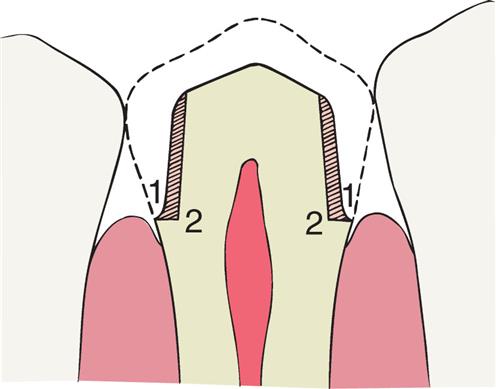
A partial-coverage restoration may have less resistance (Fig. 7.50) than a complete crown because it has no buccal resistance areas. In this case, resistance is provided by proximal boxes or grooves (Fig. 7.51) and is greatest if the groove, box walls, or both are perpendicular to the direction of the applied force. Thus, U-shaped grooves or flared boxes provide more resistance than do V-shaped ones.132 On short preparations, the reverse scenario can apply: Short complete crown preparations may lack resistance, where proximal grooves, in comparison, will then result in better resistance on a partial veneer crown. In general, ideal grooves and boxes should be prepared so that their walls are located in a healthy tooth structure. Placing proximal grooves as close as possible to the location of the original proximal contact offers the opportunity to maintain as much dentin as possible because this is where the tooth has its greatest mesiodistal dimension. However, the proximal axial walls are typically shorter in the occlusogingival dimension than the buccal and lingual axial walls because of the scalloped shape of the periodontium. As a result, buccal and or lingual retentive grooves are generally longer than mesiodistal grooves. An in vitro study reported that mesial-distal grooves delivered better resistance to dislodgment than buccal-lingual grooves.160 However, the study only looked at forces applied in a buccal direction. Whereas it is reasonable to assume that most loads resulting in crown dislodgment are applied from either a buccal and lingual direction since some bracing of the restoration occurs as a function of stabilizing proximal contacts, it is not possible to declare an absolute optimal location for retentive grooves. Each tooth has to be individually assessed for its resistance form in all horizontal directions. The weakest area of the tooth preparation will have the longest radius of rotation for a crown to pivot off. Once the longest radius has been identified, a retentive groove can be placed in the axial wall that will shorten the radius of the specific rotation (see Figs. 7.48 and 7.49).
Similarly, in order to more effectively enhance resistance, grooves that are placed in excessively inclined preparation walls should be prepared to greater depth in their cervical aspect than in their occlusal aspect. Taper restriction in the cervical aspect of an excessively tapered crown preparation has been shown to enhance resistance more effectively than do grooves that are prepared flush into excessively inclined preparation walls because the number of paths of removal is reduced.163
Physical Properties of the Luting Agent (Cohesive Versus Adhesive Cements)
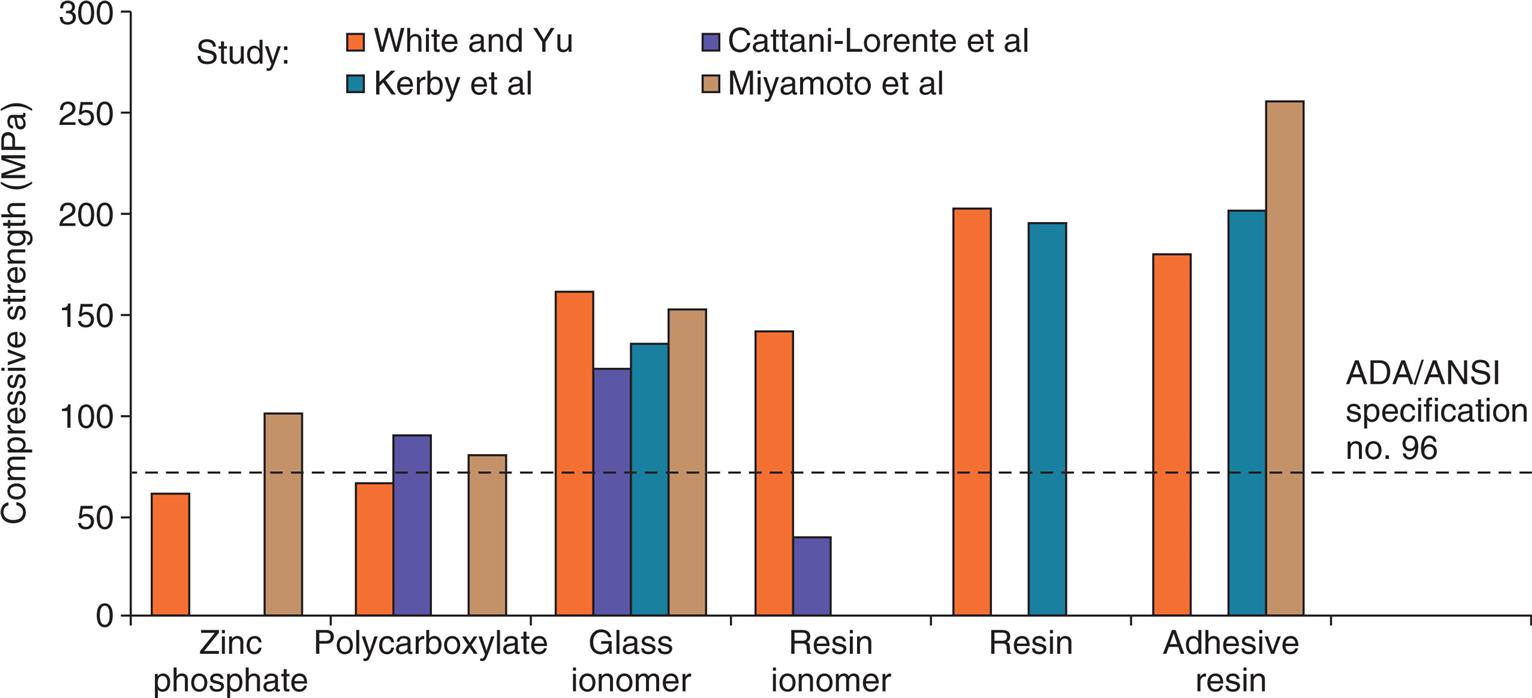
Resistance to deformation is affected by physical properties of the luting agent, such as compressive strength and modulus of elasticity.164 To satisfy American Dental Association/American National Standards Institute specification no. 96 (International Standards Organization specification no. 9917), the compressive strength of zinc phosphate cement must exceed 70 MPad at 24 hours (Fig. 7.52).165–168 Glass ionomer cements and most resins have higher compressive strength, whereas polycarboxylates have values similar to those of zinc phosphate.164
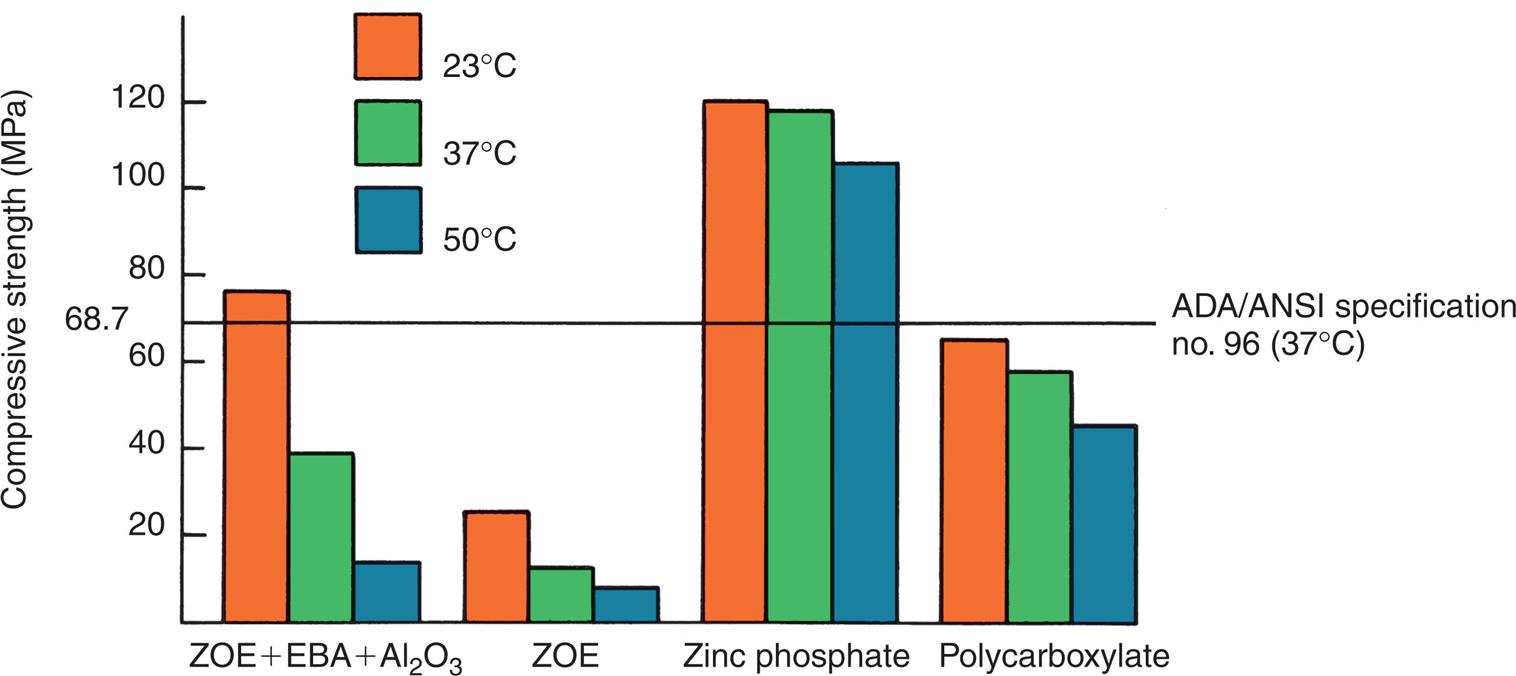
Increasing temperature has a dramatic effect on the compressive strength of luting agents, particularly weakening reinforced zinc oxide–eugenol cement (Fig. 7.53). An increase from room temperature (23°C) to body temperature (37°C) halves the compressive strength of reinforced zinc oxide–eugenol cements, and a rise in temperature to 50°C (equivalent to hot food) reduces the compressive strength by more than 80%.169 Equivalence testing of more modern luting agents has not been reported.
Zinc phosphate cements have a higher modulus of elasticity than do polycarboxylate cements, which exhibit relatively large plastic deformation.170 This may account for the observation that the retentive ability of polycarboxylate cement is more dependent on the taper of the preparation than is the retention with zinc phosphate cement.171
In the selection process of choosing a durable luting agent, clinicians have a choice in how the dental cement is delivered and mixed. Cements come in a liquid-powder or dual paste form and can be hand mixed, auto-mixed through convenient dispensing tips, or triturated in prepackaged capsules (see Chapter 30). Although the decision process of luting agent selection may be driven by factors such as mixing ease and cleanup time, the method of luting agent mixing and delivery can affect resulting physical properties as well. One thermocycle study investigated the long-term aging effect of monolithic zirconia crowns cemented on natural teeth with powder-liquid and paste-paste forms of the same resin-modified glass ionomer. Interestingly, the retention of the zirconia crowns luted with the dual paste method required less than half of the removal force than the crowns cemented with the same commercial resin-modified glass ionomer cement that was a powder-liquid mix.172
The factors that affect the resistance to displacement of a cemented restoration are summarized in Table 7.5.
Preventing Deformation
A restoration must have sufficient strength to prevent permanent deformation during function (Fig. 7.54); otherwise, it will fail (typically at the restoration-cement interface or at the metal-porcelain interface). This may be a result of unsuccessful bonding, poor tooth preparation, inappropriate alloy selection, or poor metal-ceramic framework design (see Chapter 19).

Bonding
Composite luting agents shrink upon polymerization and deliver a pre-compressive force to bonded ceramics.173 On thermal loading, the luting composite also expands and generates tensile forces within ceramic restorations.174 When bonded feldspathic ceramic restorations fit well (i.e., a gap width of approximately 100 μm) the luting composite tends to protect the ceramic against thermal expansion.174 Lithium disilicate and zirconia restorations have also been shown to mechanically benefit from adhesive luting.175,176 Laboratory research reports that for posterior ceramic occlusal veneers, there is no significant difference in fracture resistance between 1 mm and 2 mm of lithium disilicate ceramic when bonded to tooth structure (Fig. 7.55).177
Adequate Tooth Reduction
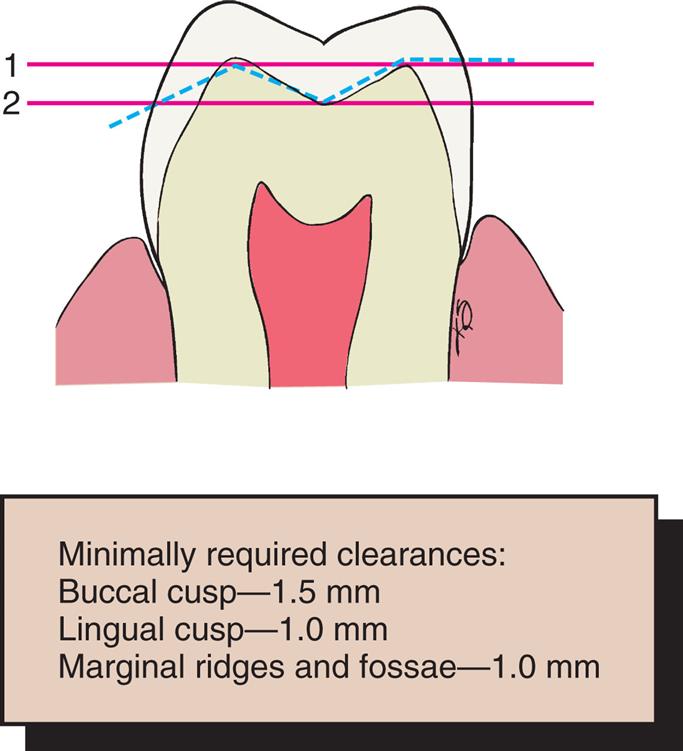
Largely according to empirical data, metal restorations require a minimum alloy thickness of about 1.5 mm over functional cusps (buccal in the mandible, lingual in the maxilla). The less stressed nonfunctional cusps can be protected with less metal (1 mm is adequate in most circumstances) for a strong and long-lasting restoration. Occlusal reduction should be as uniform as possible, following the cuspal planes of the teeth; this ensures that sufficient occlusal clearance is combined with the preservation of as much tooth structure as possible. In addition, an anatomically prepared occlusal surface (Fig. 7.56) gives rigidity to the crown because of the “corrugated effect”178 of the planes.
When teeth are misaligned or overerupted, the occlusal surface needs to be prepared with the thickness requirements of the eventual restoration in mind. For example, a supra-erupted tooth may need considerably more than 1.5 mm of reduction to establish adequate clearance so that optimal occlusal form and the appropriate plane can be reestablished and adequate restoration thickness ensured (Fig. 7.57). Diagnostic tooth preparation and waxing are helpful in determining the correct tooth reduction. A practical approach is to reshape the supra-erupted tooth on the diagnostic cast to the desired occlusal plane that is anticipated. Diagnostically, the opposing teeth and, if necessary, the target tooth itself can be waxed to final form. An external matrix is then fabricated over the diagnostic endpoint from a suitable elastomeric putty. After sectioning, this can be used intraorally as a reduction guide to ensure that optimal, yet conservative tooth reduction is achieved (Fig. 7.58).

Margin Design
To prevent distortion of the restoration margin occlusally, the dentist should design the preparation outline form so that occlusal contact is avoided in this area. Keeping preparation margins approximately 1 to 1.5 mm away from occlusal contact locations satisfies this requirement.
Ideally, cervical enamel should be conserved to maintain structural integrity of the tooth and for bonding. When finish lines need to be extended apically, tooth reduction must provide sufficient room for the bulk of restorative material at the margin to prevent distortion. For example, as discussed before, one disadvantage of the feather edge margin preparation is that the resulting thin layer of gold is not as strong as the comparatively thicker restoration of a chamfer margin preparation. When teeth have been prepared with increased taper, however, it is advisable to reduce margin width in order to maintain adequate dentin thickness between the axial preparation wall and the pulpal tissues.179
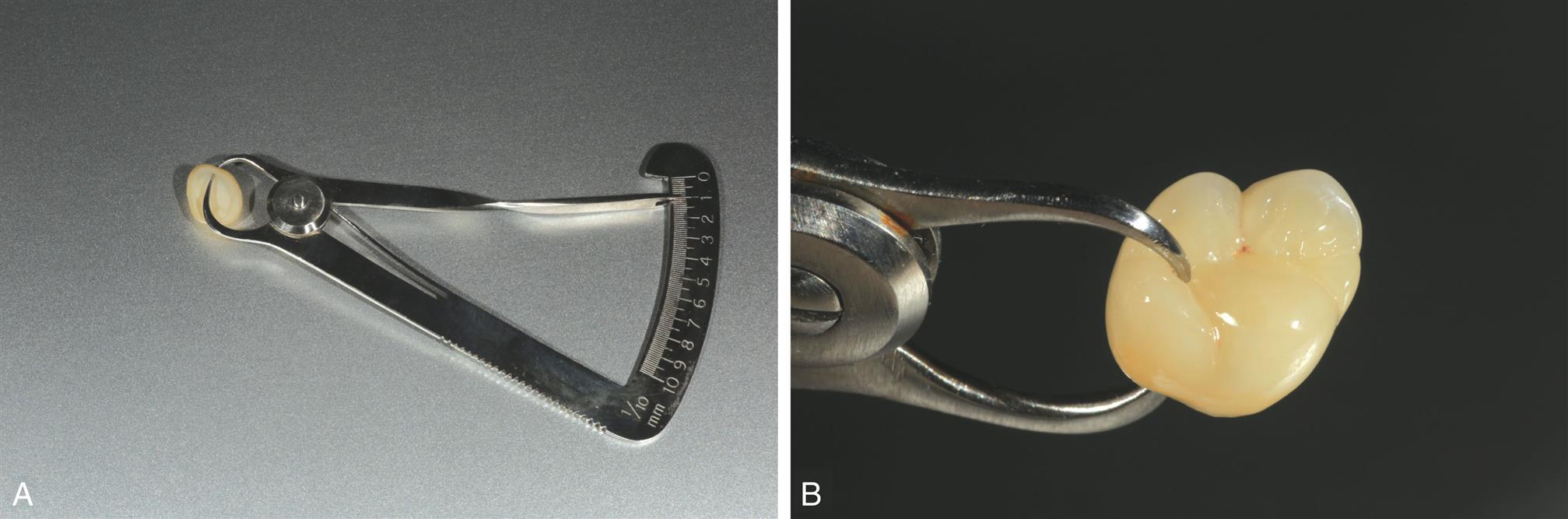
Quantitatively, the amount of reduction in the cervical part of a preparation is a function of the restorative material selected. For gold castings or high-strength anatomic contour zirconia and bonded lithium disilicate, 0.3 to 0.5 mm is adequate; for bilayered ceramic and metal-ceramic crowns, 1 to 1.2 mm of facial shoulder or chamfer margin width is desirable but not easily achieved on small teeth or teeth with large pulps. Lower strength ceramic crowns can be fabricated successfully on shoulder margin preparations with a margin width of 0.8 to 1.0 mm, although minimum dimensions may increase for certain materials and fabrication techniques.180 With the advent of CAD-CAM restorations, the limitations of the milling systems used may influence specific reduction requirements. Not all milling machines are equal. The selection of CAD-CAM laboratory equipment or a laboratory that uses CAD-CAM technology should be weighed carefully against the biological criteria discussed at the beginning of this chapter.
The grooves and ledges incorporated in a partial-coverage preparation provide essential strengthening for such castings that yet remain inherently weaker than their complete-coverage counterparts; in particular, the classic anterior pinledge retainer benefited from the beamlike reinforcement that resulted from the incorporation of ledges in the tooth preparation design (Fig. 7.59).

Alloy Selection
Although type I and type II gold alloys (see Chapter 22) are satisfactory for intracoronal cast restorations, they are too soft for crowns and fixed dental prostheses, for which type III or type IV gold alloys (or an appropriate low-gold alternative) are chosen. These are harder, and their strength and hardness can be further increased by heat treatment.
Metal-ceramic alloys with high noble metal content have a hardness equivalent to that of type IV gold alloys, whereas nickel-chromium or cobalt-chromium alloys are considerably harder yet. These may be indicated when large forces are anticipated, as with a long-span FPD, although their use presents certain challenges (see Chapter 19). Even the stronger alloys need sufficient bulk if they are to withstand occlusal forces.
Esthetic Considerations
The restorative dentist should develop skill in understanding the esthetic expectations of the patient. Most patients prefer their dental restorations to look as natural as possible. However, esthetic considerations should not be pursued at the expense of the prognosis of the patient’s long-term oral health or function.
At the initial examination, the dentist fully assesses the appearance of each patient, noting which areas of which teeth show during speech, smiling, and laughing (Fig. 7.60). The patient’s esthetic expectations must be discussed in relation to oral hygiene needs and to the potential for development of future disease. Simply asking the question “Are you happy with the way your teeth look?” and observing the patient while carefully listening to the response is important and helpful. The final decision regarding an appropriate restoration can then be made with the full cooperation and informed consent of the patient.

Options for esthetic restorations include partial veneer crowns which maintain an intact labial or buccal surface in original tooth structure; metal-ceramic restorations, which consist of a metal cast substructure that in visible areas has an esthetic porcelain veneer; and ceramic restorations (Fig. 7.61).
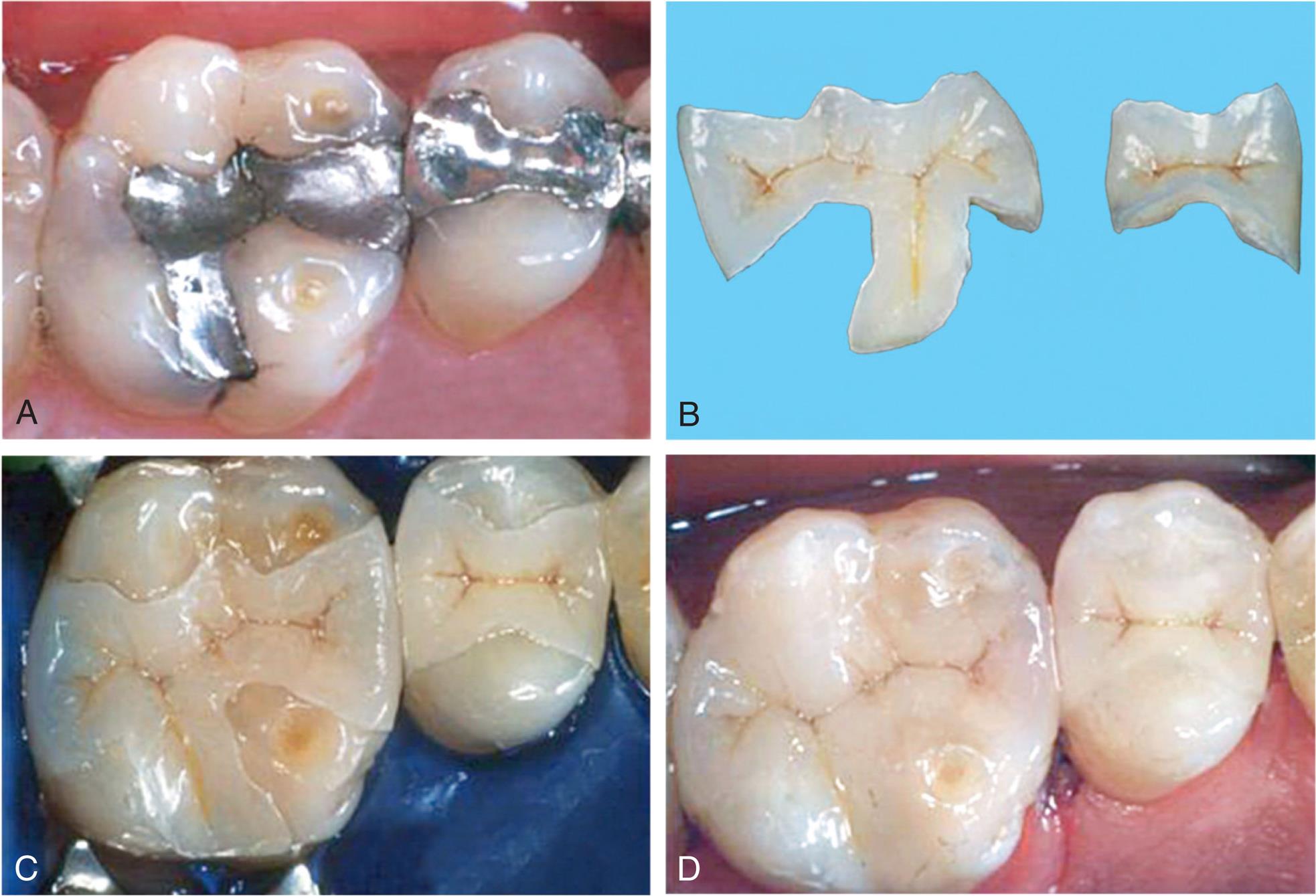
Ceramic Restorations
Some of the most conservative and pleasing esthetic restorations are ceramic inlays, onlays, veneers, and crowns (see Chapters 25 and 26). They can mimic original tooth color better than the other restorative options. Although ceramic restorations are at somewhat greater risk of brittle fracture than are other restorations, the newest materials have improved physical properties and can be strengthened through the use of resin-bonded luting agents.
Metal-Ceramic Restorations
The appearance of some metal-ceramic restorations (see Chapters 19, and 24) is often compromised by insufficient porcelain thickness. However, adequate porcelain thickness is sometimes obtained at the expense of proper axial contour (such overcontoured restorations almost invariably lead to periodontal disease). In addition, the labial margin of a metal-ceramic crown is not always accurately placed. To correct all these deficiencies, certain principles are recommended during tooth preparation that ensures sufficient room for porcelain and accurate placement of the margins. Otherwise, good appearance would be achievable only at the expense of periodontal health.
Facial Tooth Reduction
If there is to be sufficient bulk of porcelain for appearance and metal thickness for strength, adequate reduction of the facial surface is essential. The exact amount of reduction depends to some extent on the physical properties of the alloy used for the substructure, as well as on the manufacturer and the shade of the porcelain. A good color match for some restorations in older individuals typically requires a slightly greater porcelain thickness than is needed in younger patients. A minimum reduction of 1.5 mm is typically required for optimal appearance. Adequate thickness of porcelain (Fig. 7.62) is needed to create a sense of color depth and translucency. Shade problems are frequently encountered in maxillary incisor crowns at the incisal and cervical thirds of the restoration, where direct light reflection from the opaque layer can make the restoration very noticeable. Because opaque porcelains generally have a shade different from that of body porcelains, they often need to be modified with special stains in these areas (see Chapter 24).181
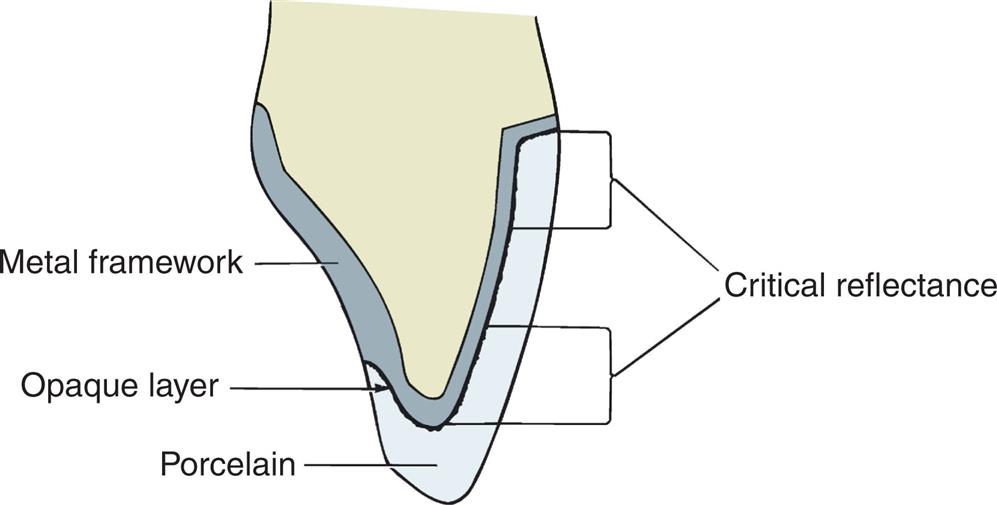
With very thin teeth (e.g., mandibular incisors), it may be impossible to achieve adequate tooth reduction without exposing the pulp or leaving the tooth preparation severely weakened. Under these circumstances, a less-than-ideal appearance may have to be accepted.
The labial surfaces of anterior teeth should be prepared for metal-ceramic restorations in two distinct planes (Fig. 7.63). If they are prepared in a single plane, the reduction in either the cervical or the incisal area of the preparation is insufficient.
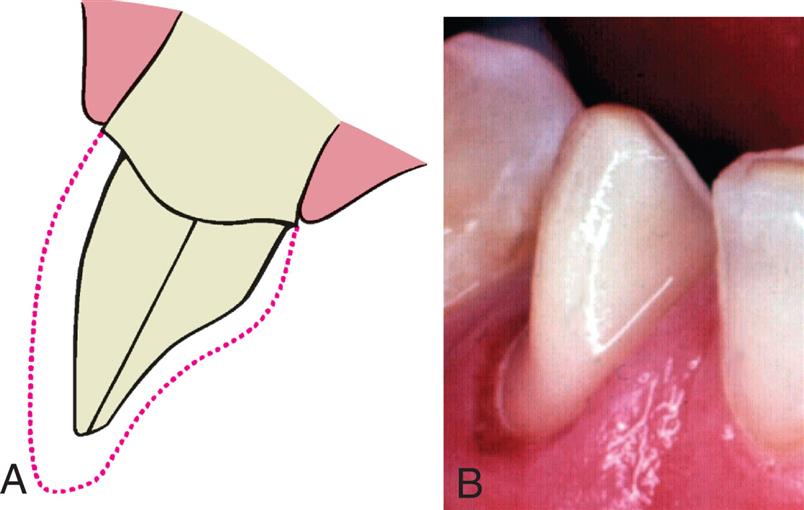
Incisal Reduction
The incisal edge of a metal-ceramic restoration has no metal backing and can be made with a translucency similar to that of natural tooth structure. An incisal reduction of 2 mm is recommended to enable the ceramist to achieve good esthetics. Excessive incisal reduction must be avoided because it reduces the resistance and retention form of the preparation.
Proximal Reduction
The extent of proximal reduction is contingent on the exact predetermination of the location of the metal-ceramic junction in the completed restoration. The proximal surfaces of anterior teeth look most natural if they are restored at the incisal edges, without metal backing. This allows some light to pass through the restoration in a manner similar to what occurs on a natural tooth (Fig. 7.64). Obviously, if the restoration is part of an FPD, the need for connectors makes this impossible.

Labial Margin Placement
Supragingival margin placement has many biological and adhesive interface advantages. The restorations are easier to prepare properly and easier to keep clean. Nevertheless, margin placement at the free gingival crest or subgingival margins may be indicated for esthetic reasons, particularly when ceramic restorations need to mask cervical tooth colors.
The patient’s smile is observed as part of the initial examination (see Chapter 1). It is important to record which teeth and which parts of each tooth are exposed. Patients with a high lip line, which exposes considerable gingival tissue, present the greatest problem if complete crowns are needed. Where the root surface is not discolored, appearance can be restored with a metal-ceramic restoration with a supragingival porcelain labial margin (see Chapter 24). If the patient has a low lip line, a supragingival margin may be placed because the restorative interface is not seen during normal function
However, it cannot be assumed that the patient will be happy with a supragingival margin just because it is not visible during normal function. Some patients have reservations about exposed restorative interfaces, and the advantages of such supragingival margins must be carefully explained before treatment.
Metal collars can be hidden below the gingival crest, although there is some discoloration if the gingival tissue is thin. Successful margin placement within the gingival sulcus requires care to ensure that inflammation and recession, with resulting metal exposure, are avoided or minimized. The periodontium must be healthy before the tooth is prepared. If periodontal surgery is needed, the sulcular space should not be eliminated completely; rather, a postsurgical depth of about 2 mm should be the objective. Sufficient time should be allowed after surgery for the periodontal tissues to stabilize. Wise182 found that the gingival crest does not stabilize until 20 weeks after surgery (see Chapter 5).
Margins should not be placed so far apically that they encroach on the attachment; extension to within 1.5 mm of the alveolar crest leads to bone resorption.183 Subgingivally placed margins should follow the scalloped contour of the free gingival margin, being further apical in the middle of the tooth and further incisal interproximally. A common error (Fig. 7.65) is to prepare the tooth so that the margin lies almost in one plane, with exposure of the collar labially and irreversible loss of bone and papilla proximally.

Partial-Coverage Restorations
Whenever possible, an esthetically acceptable result without the use of complete crowns is preferred because tooth structure is conserved: no restorative material can approach the appearance of intact tooth enamel. Esthetic partial-coverage restorations (see Chapter 11) depend on accurate placement of the potentially visible facial and proximal margins. A visible display of metal is not esthetic and is thus unacceptable to many patients. If a partial-coverage restoration is poorly prepared, the patient may demand that it be replaced by a metal-ceramic crown, and the result is unnecessary loss of tooth structure and a greater potential for tissue damage.
Proximal Margin
Precise placement of the proximal margins (particularly the mesial, generally more visible, margin) is crucial for the esthetic result of a partial-coverage restoration. The rule is to place the margin just buccal to the proximal contact area, where metal is hidden by the distal line angle of the neighboring tooth and yet provides adequate access to the tooth-restoration interface for plaque control. Tooth preparation angulation is critical and should normally follow the long axes of posterior teeth and the incisal two-thirds of the facial surface of anterior teeth. If a buccal or lingual tilt is given to the tooth preparation, the likelihood that metal will be visible increases significantly (Fig. 7.66).
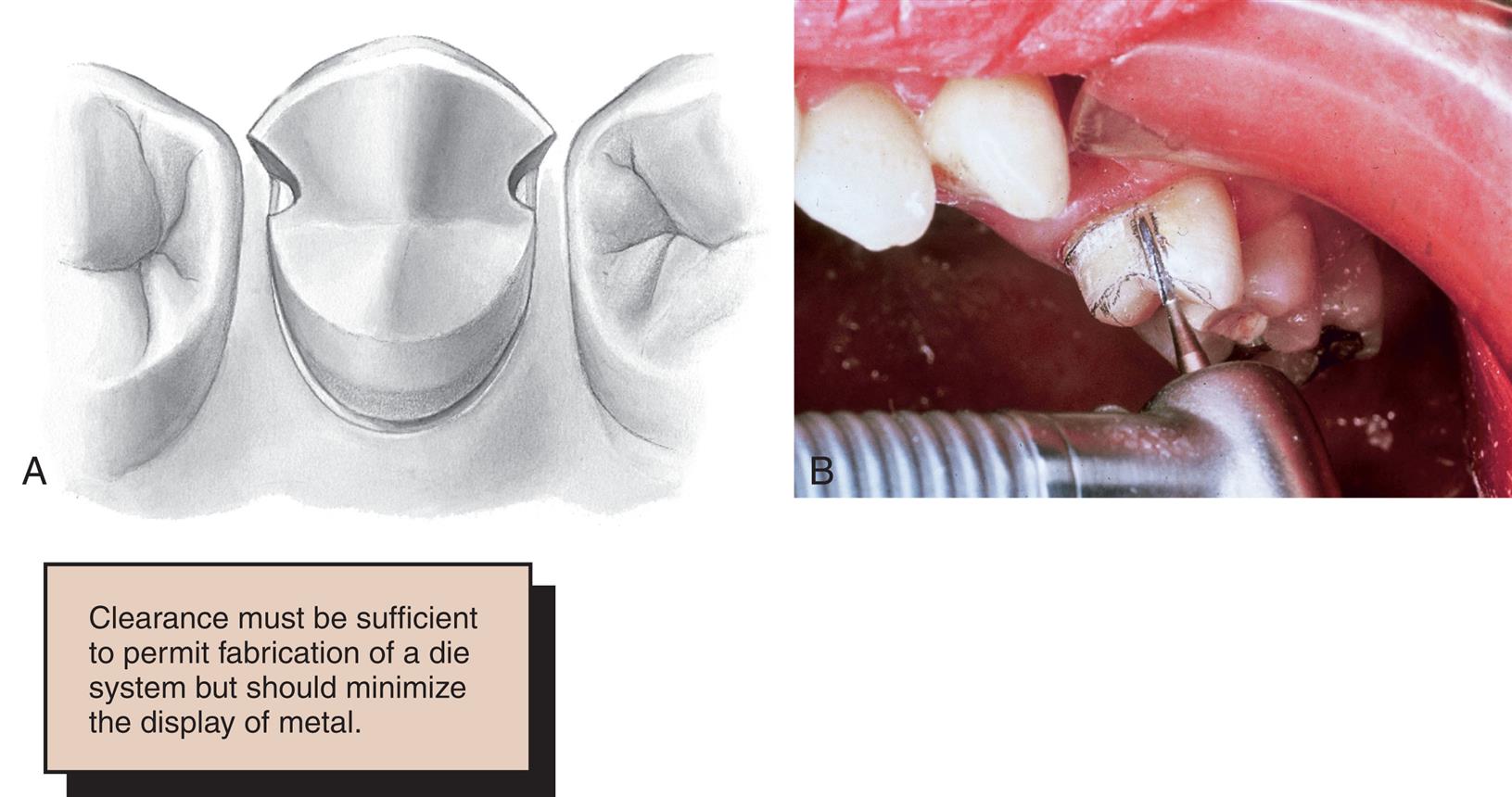
The distal margin of posterior partial-coverage restorations is less visible than the mesial margin. In this area, it is often advantageous to extend the preparation farther beyond the contact point for easier preparation and finishing of the restoration and to facilitate access for oral hygiene.
Facial Margin
The facial margin of a maxillary partial-coverage restoration should be extended just beyond the occlusofacial line angle. A short bevel is needed to prevent enamel chipping. A chamfer margin can be placed in areas where appearance is less important (e.g., on molars) because this provides greater bulk of metal for strength.
If the facial margin of metal is correctly shaped (Fig. 7.67), it does not reflect light to an observer. As a result, the tooth appears to be merely a little shorter than normal and not as though its buccal cusp is outlined in metal. If the buccal margin is skillfully placed so as to follow the original cuspal contour, the appearance of the final restoration is acceptable.
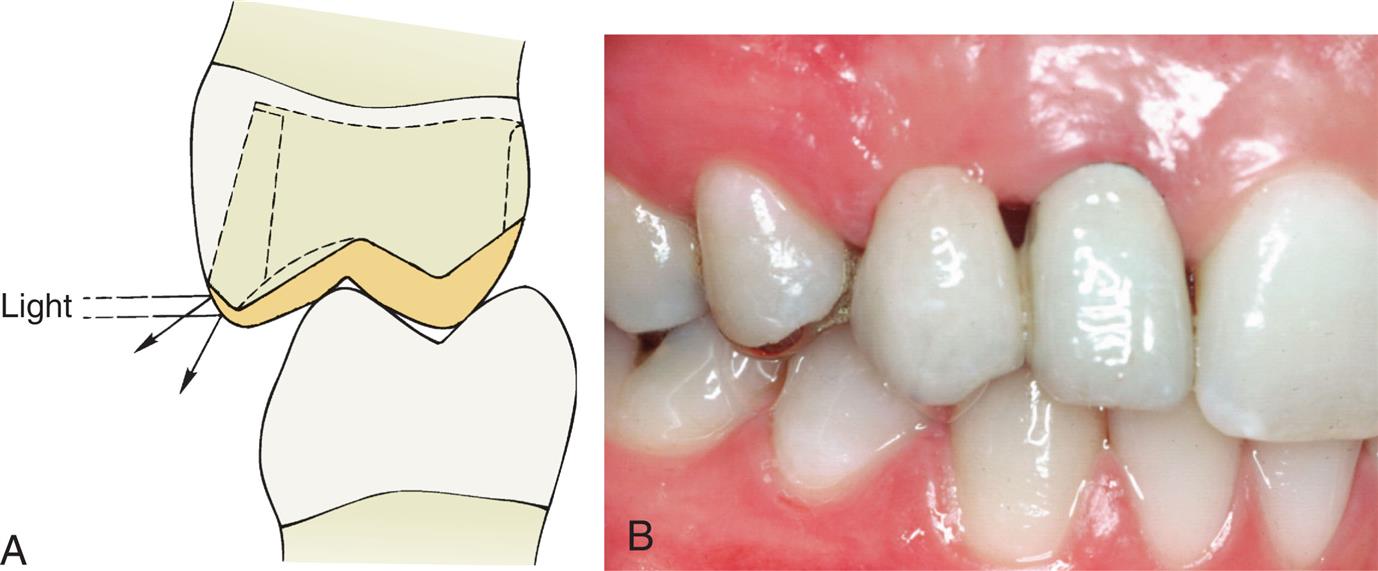
When mandibular partial cast crowns are made, metal display is unavoidable because the occlusal surface of mandibular teeth can be seen during speech. A chamfer margin, rather than a beveled margin, is recommended for the buccal margin because it provides a greater bulk of metal around the highly stressed functional cusp (Fig. 7.68). If the appearance of metal is unacceptable to the patient, a metal-ceramic restoration with porcelain coverage on the occlusal surface can be made.
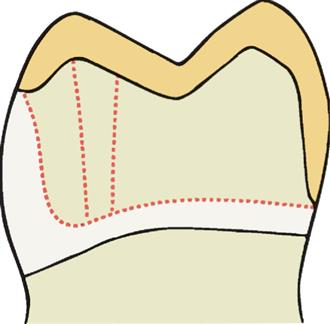
Anterior partial-coverage restorations can be fabricated to show no metal (Fig. 7.69), but their preparation requires considerable care. The facial margin is extended just beyond the highest contour of the incisal edge but not quite to the incisolabial line angle. In this case, the metal protects the tooth from chipping but is not visible.
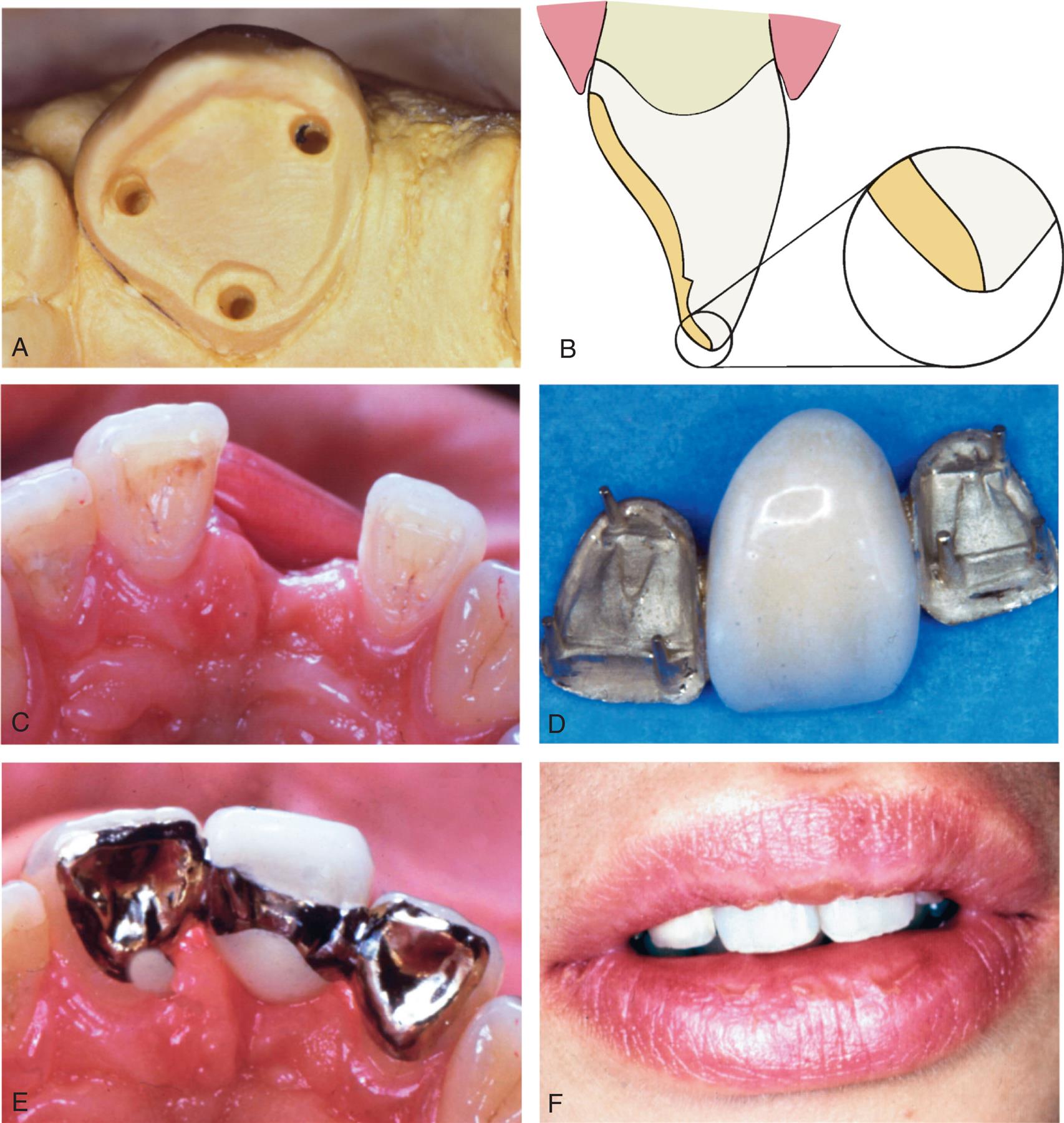
Planning and Evaluating Tooth Preparations
Tooth preparation is a precise, technically complicated, and irreversible procedure. Thus, it is the practitioner’s responsibility to carry it out properly, every time. Mistakes are often difficult, if not impossible, to correct. Rehearsing the planned preparations on diagnostic casts invariably proves helpful in achieving a better quality preparation.
Diagnostic Tooth Preparations
Diagnostic tooth preparations are performed on articulated casts before the actual clinical preparation. They yield information about the following:
- • Selecting the appropriate path of placement for an FPD, particularly for abutment teeth that are tilted, are rotated, or have an atypical coronal contour (Figs. 7.70 and 7.71).
- • Deciding on the amount of tooth reduction necessary to accomplish a planned change in the occlusion.
- • Determining the best location for the facial and proximal margins of a partial-coverage restoration so that the metal is not visible.
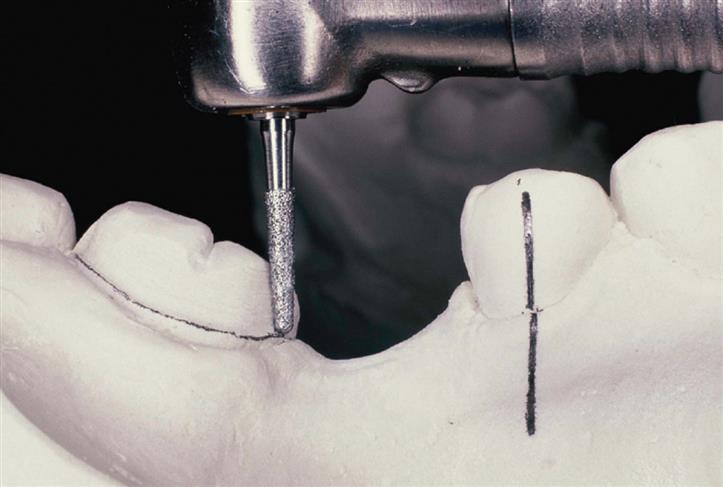
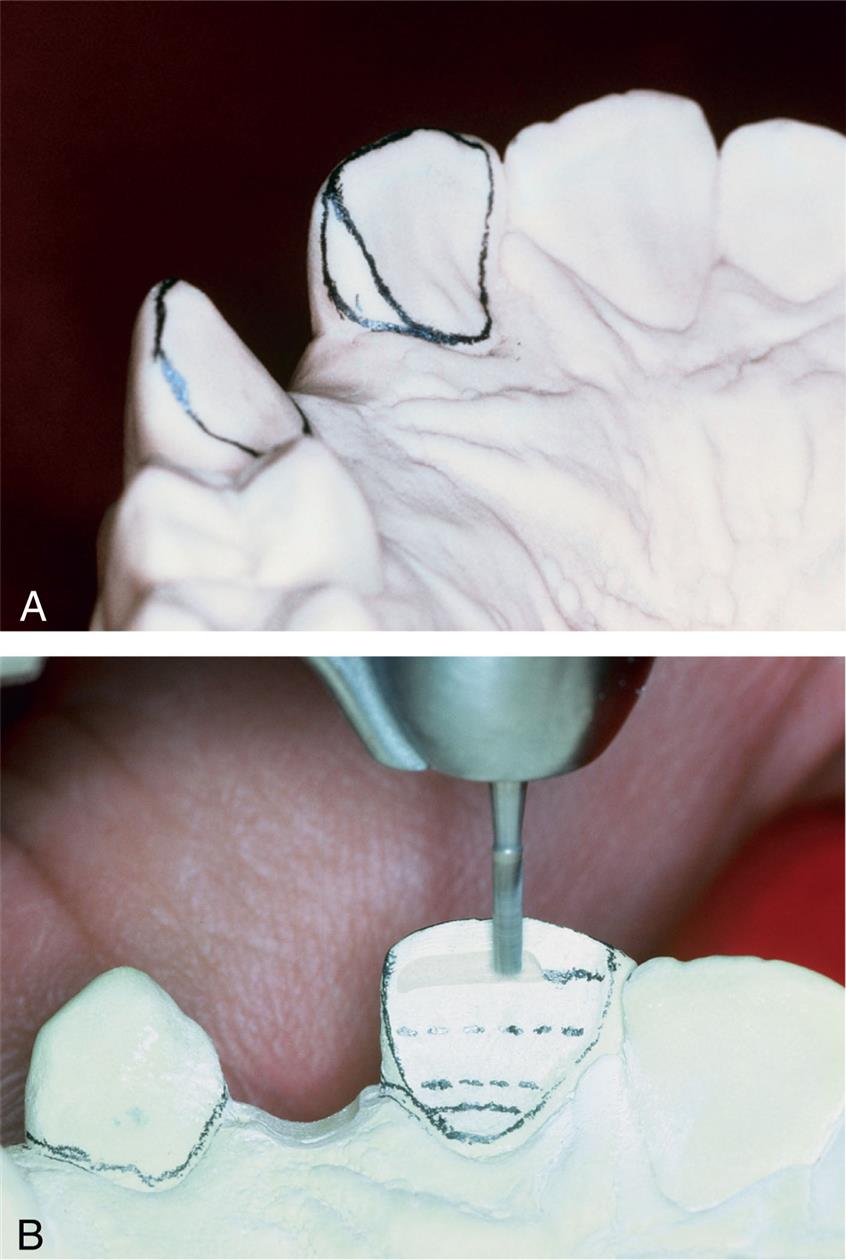
An important advantage of diagnostic tooth preparations is that the operator can practice each step of the intended restoration. Mistakes are not permanently destructive. Also, diagnostic preparations can be used in the prefabrication of interim restorations, significantly reducing the appointment time duration after the clinical tooth preparation has been completed (the indirect/direct interim restoration fabrication technique is described in Chapter 15).
Diagnostic Waxing Procedures
For all but the most straightforward prosthodontic treatment plans, a diagnostic waxing procedure (Fig. 7.72) should be performed. This is done on diagnostic casts and helps determine optimal contour and occlusion of the eventual prosthesis. The procedure is of particular benefit if the patient’s occlusal scheme or anterior (incisal) guidance requires alteration (Fig. 7.73). Once the teeth are prepared consistent with the needs identified during the diagnostic waxing, interim restorations can be created from the waxing. At a subsequent appointment before making a definitive impression, the interim restorations are removed and the thickness of the restorations and interim cements are evaluated to verify that there is appropriate prosthetic space for the specific definitive restoration(s) (Fig. 7.74).
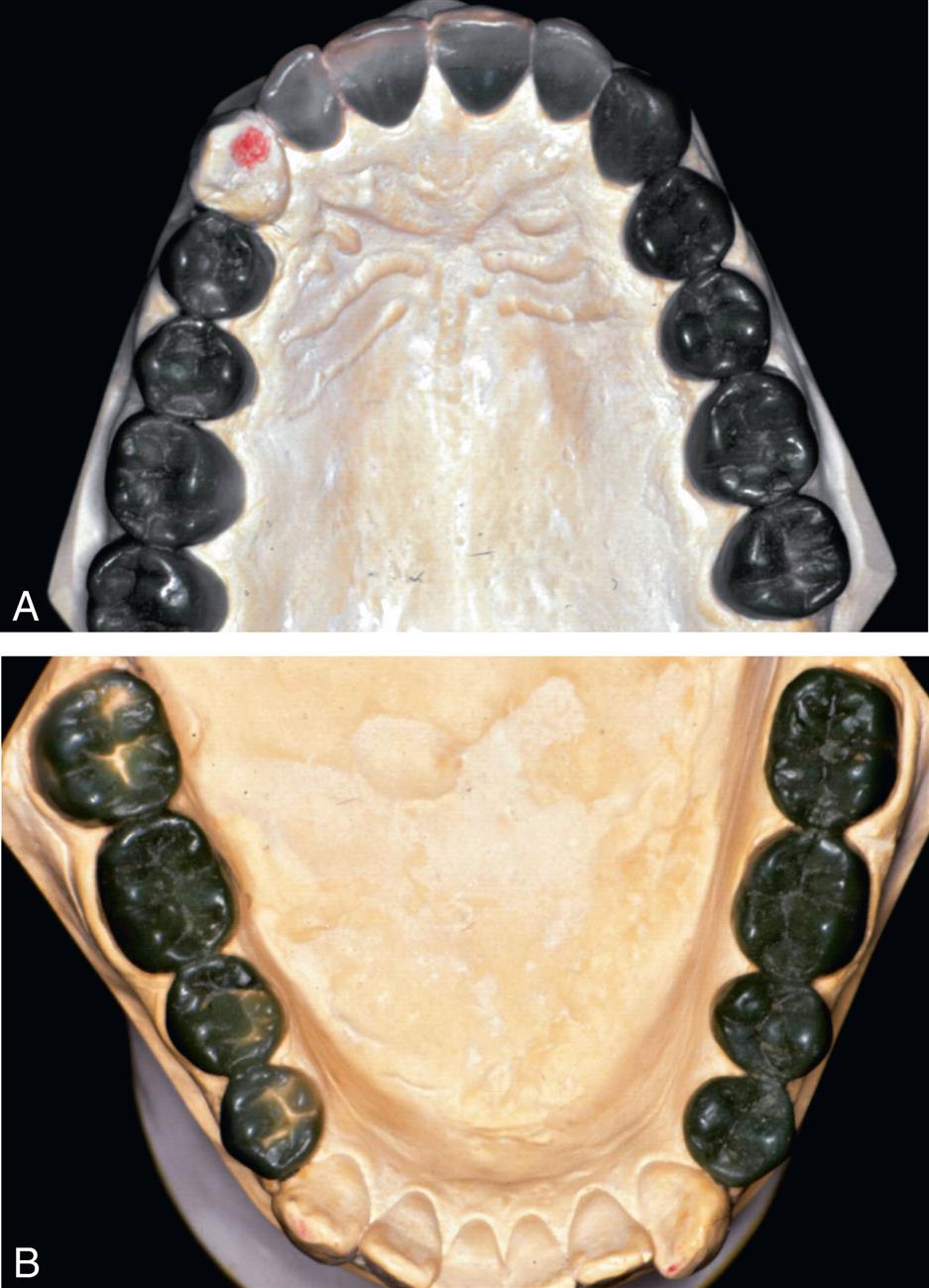
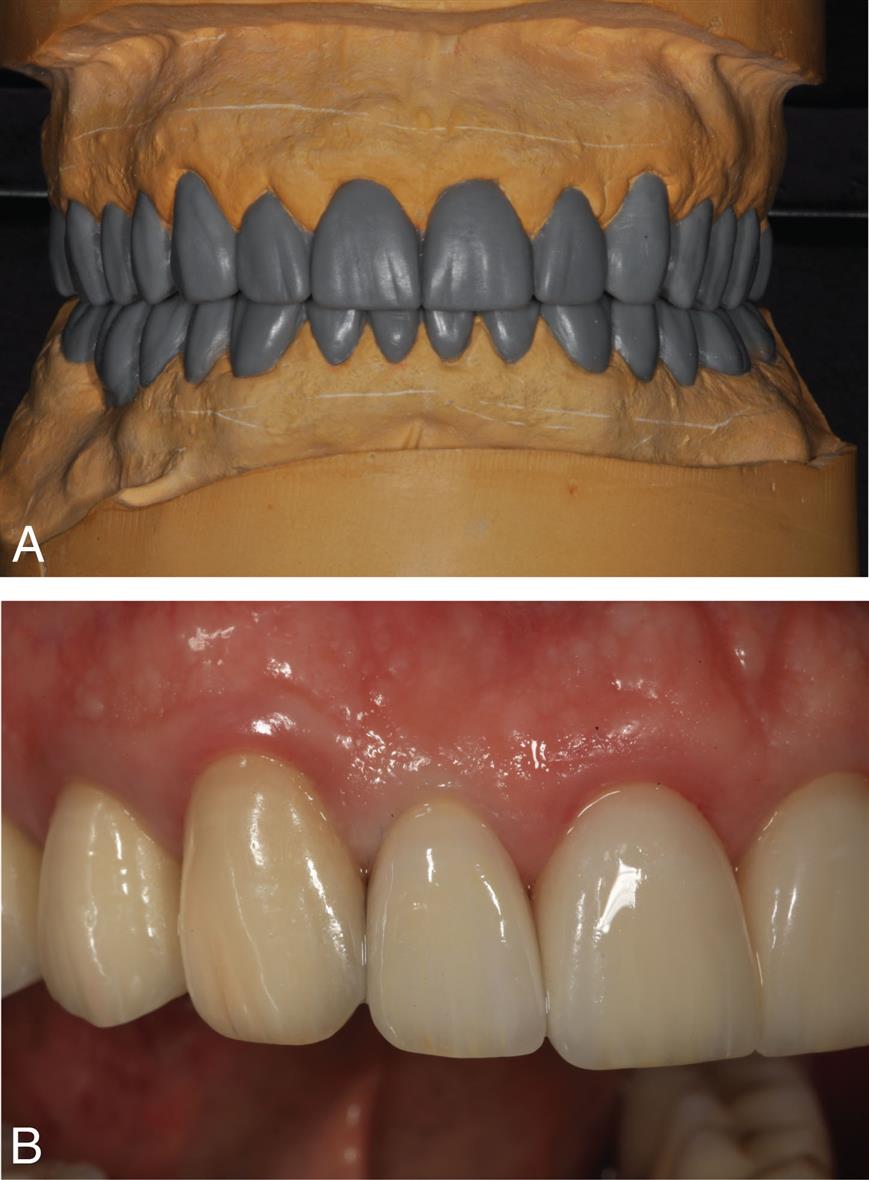
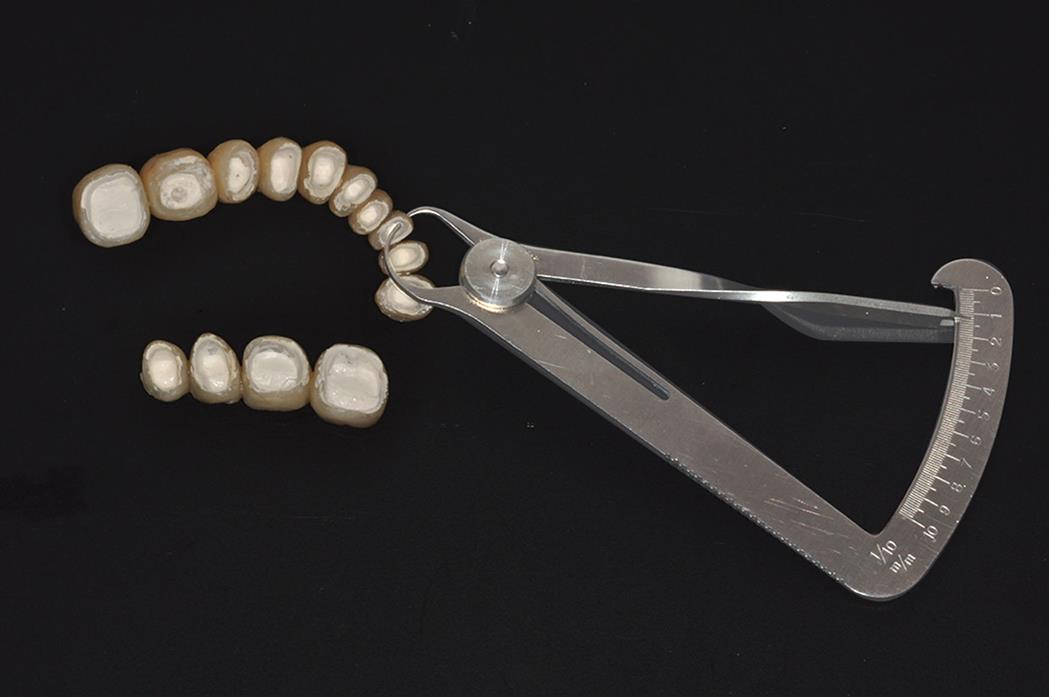
Evaluative Procedures During Tooth Preparation
Each step of a tooth preparation should be carefully evaluated with direct vision or indirectly with a dental mirror. Alignment of multiple abutment teeth can be problematic, and use of the mirror helps superimpose the image of adjacent abutment teeth. To evaluate complex preparations, the dentist should make an alginate impression and pour it in fast-setting stone. A dental surveyor (Fig. 7.75) can then be used to precisely measure the axial inclinations of the tooth preparation. Making such an impression may appear to take unnecessary time; however, the information obtained often saves time in subsequent procedures by identifying problems that can then be addressed immediately. For tooth preparation, the contra-angle handpiece can be used for both measuring and cutting. This is done by concentrating on the top surface of the turbine head, which is perpendicular to the shank of the rotary instrument. If the top surface is kept parallel to the occlusal surface of the tooth being prepared, the rotary instrument is automatically in the correct orientation (Fig. 7.76). To prevent undercuts or excessive convergence during axial reduction, the handpiece must be maintained at the same angulation. The correct taper is imparted by the diamond instrument. Keeping the turbine head at its correct angulation initially is often most effectively done by supporting it with a finger of the opposite hand.

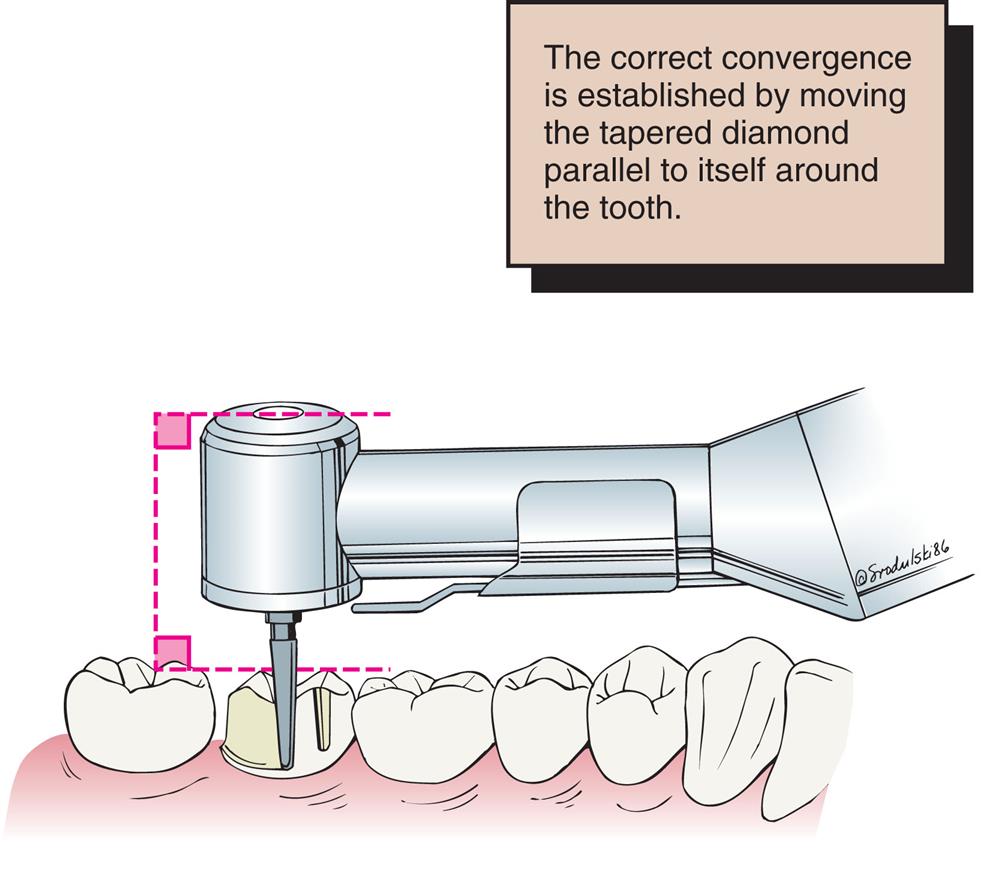
Patient and Operator Positioning
Learning the proper patient and operator positions is as beneficial as learning the proper preparation steps. Of particular importance are the advantages of obtaining a direct view of the preparation, which is always preferred to an indirect or mirror view. However, certain areas (e.g., the distal surfaces of maxillary molars) cannot be seen directly.
Inexperience, coupled with a hesitation to move the patient’s head into a more favorable position, can unnecessarily complicate tooth preparation. For instance, having the patient rotate the head to the left or right side can considerably improve the visibility of molar teeth that are being prepared. In most instances, a direct view can be obtained by subtly changing the operator’s or the patient’s position. Having the patient open maximally does not necessarily provide the best view. If the jaws are only partially open, the cheek may be retracted more easily (Fig. 7.77), and if the patient is encouraged to make a lateral excursion, the distobuccal line angle, together with the buccal third of the distal wall, may be seen directly. In practice, the mirror is essential only for visualizing a small portion of the distal surface. When a complete crown is prepared, the parts of the tooth most easily seen should be prepared first; the other areas can be prepared with the help of the mirror in a final stage.
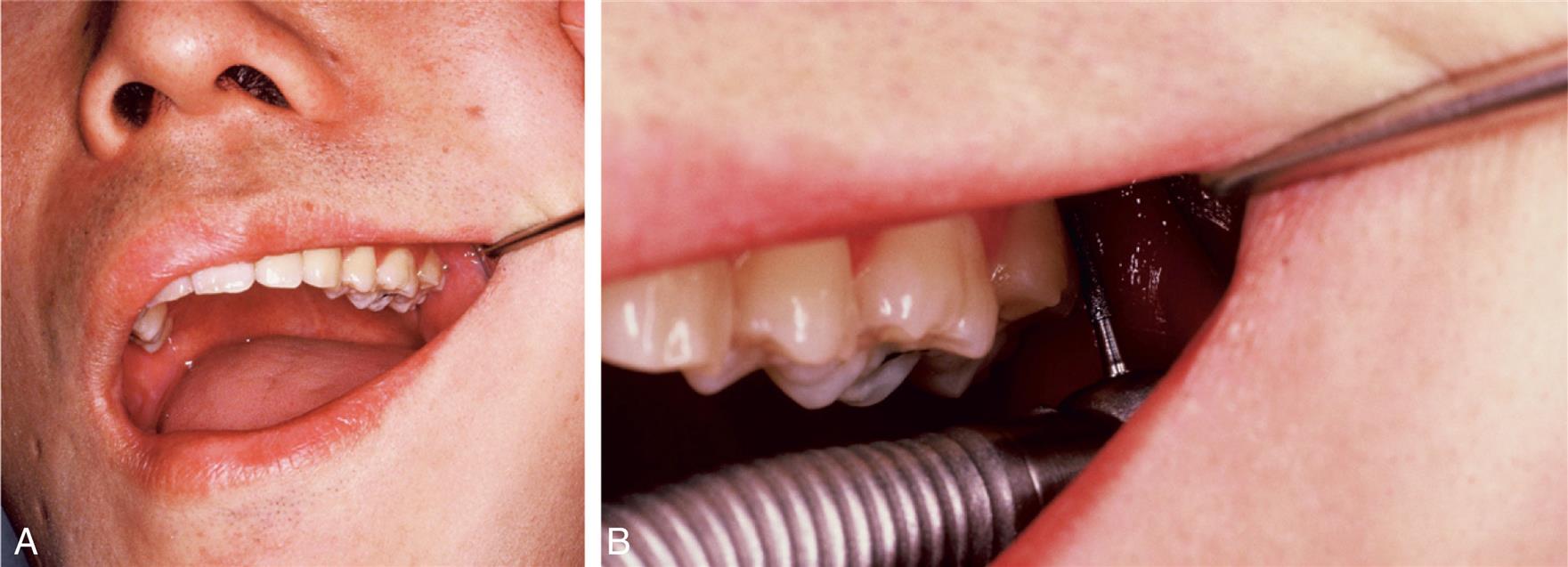
Fig. 7.78 shows positioning of the patient and a right-handed dentist for tooth preparation of the less accessible maxillary posterior teeth.

It can be fatiguing for the patient to have the mouth opened for longer periods of time, which is not only uncomfortable during the appointment but can also cause some discomfort after the appointment. It is helpful to use a bite block on the opposite side of the arch. This allows the patient to relax by closing down onto the block and maintaining slight positive pressure, which eliminates or minimizes the concern.
Summary
The principles of tooth preparation can be categorized into biological, esthetic, and restoration/tooth interface considerations. Often, these principles conflict, and the dentist must decide how the restoration should be designed to best fit the clinical situation. One area may be given too much emphasis, and the long-term prognosis may be limited by a lack of consideration of other factors.
Experience helps in determining whether preparations are “complete.” Each tooth preparation must be measured by clearly defined criteria, which can be used to identify and correct problems. Diagnostic tooth preparations and the evaluation of impressions are often very helpful. The types of preparation described in the following chapters are explained in a step-by-step format. Although detailed techniques are provided, the rationale and goals to be attained in fixed prosthodontic procedures are of greater importance than the technique itself. Understanding the pertinent theories underlying each step is crucial. Successful preparation can be obtained most easily by systematically following the steps. It is crucial to refrain from “jumping ahead” before the previous step has been evaluated and, if necessary, corrected. If the clinician proceeds too rapidly, precious chair time will be lost, and the quality of the preparation will probably suffer.
Study Questions
- 1. Discuss how the manipulation and condition of the armamentarium being used can contribute to injury.
- 2. Discuss optimal occlusocervical margin placement. What are some reasons for deviating from the ideal? Why?
- 3. Discuss the difference between retention and resistance. What can be done to enhance retention, and what can be done to improve the resistance form of a tooth preparation?
- 4. Discuss six different margin configurations. Discuss their advantages, disadvantages, indications, and contraindications as applicable.
- 5. What is an undercut? How is an undercut eliminated? Can a buccal and lingual wall be undercut in relation to each other? Why or why not?
- 6. What are the differences in retention and resistance form between a partial veneer crown preparation and a complete cast crown preparation on the same tooth? How do clinical crown length and tooth size influence either? Why?
- 7. List six different means of conserving tooth structure during tooth preparation design, and explain why they achieve the objective.
- 8. What is the purpose of diagnostic waxing? Give four indications for a diagnostic waxing procedure.