Pontic Design
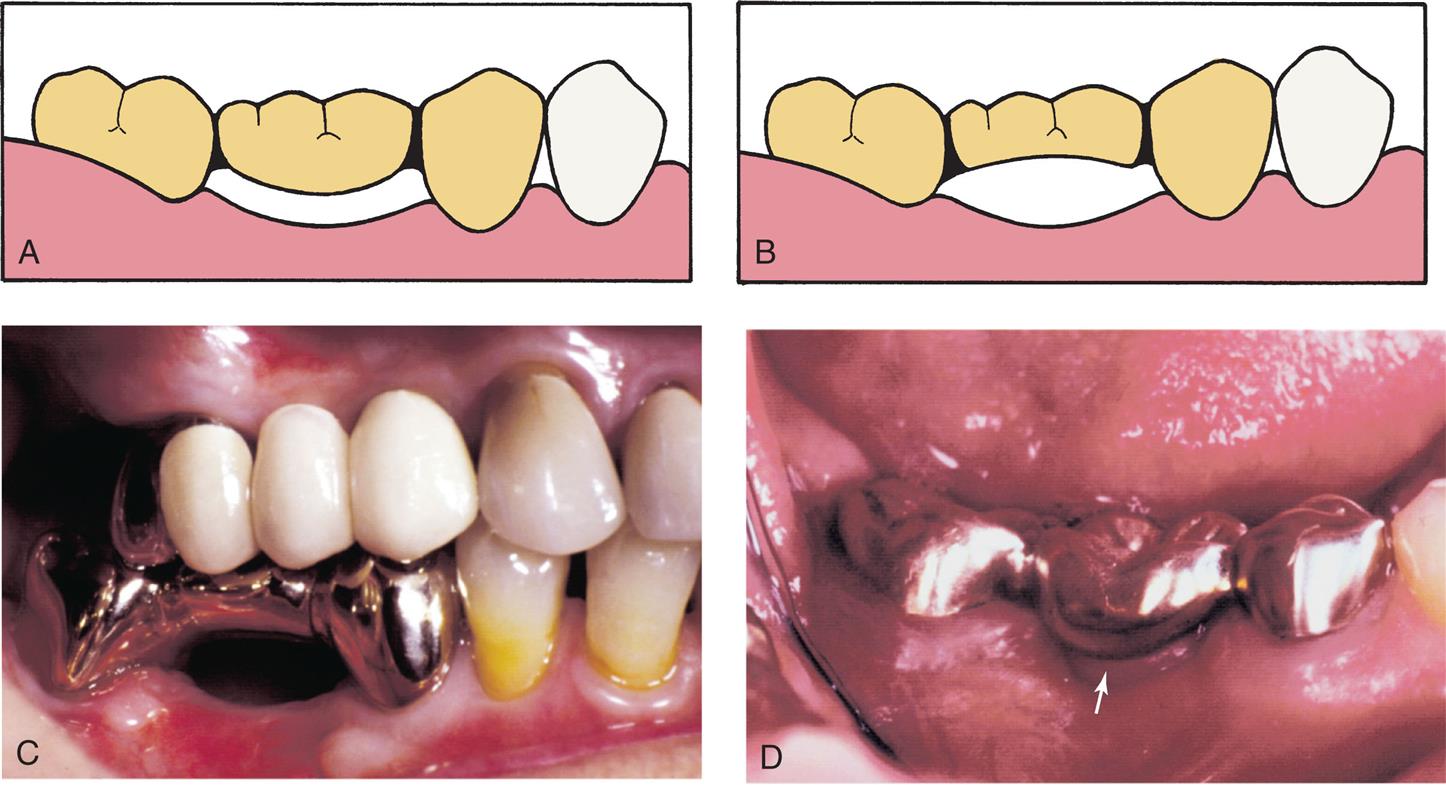
Pontics are the artificial teeth of a fixed partial denture (FPD) that replace missing natural teeth, restoring function and appearance (Fig. 20.1). They must enable continued oral health and comfort. The edentulous areas where a fixed prosthesis is to be provided may be overlooked during the treatment-planning phase. Unfortunately, any deficiency or potential problem that may arise during the fabrication of a pontic is often identified only after the teeth have been prepared or even when the definitive cast is ready to be sent to the dental laboratory technician. Proper preparation includes a careful analysis of the definitive dimensions of the edentulous areas: mesiodistal width, occlusocervical distance, buccolingual dimension, and location of the residual ridge. To design a pontic that meets hygienic requirements and prevents irritation of the residual ridge, particular attention must be given to the form and shape of the gingival surface. Merely replicating the form of the missing tooth or teeth is not enough. The pontic must be carefully designed and fabricated not only to facilitate plaque control of the tissue surface and around the adjacent abutment teeth, but also to adjust to the existing occlusal conditions. In addition to these biologic considerations, pontic design must incorporate mechanical principles for strength and longevity, as well as esthetic principles for satisfactory appearance of the replacement teeth (Fig. 20.2).
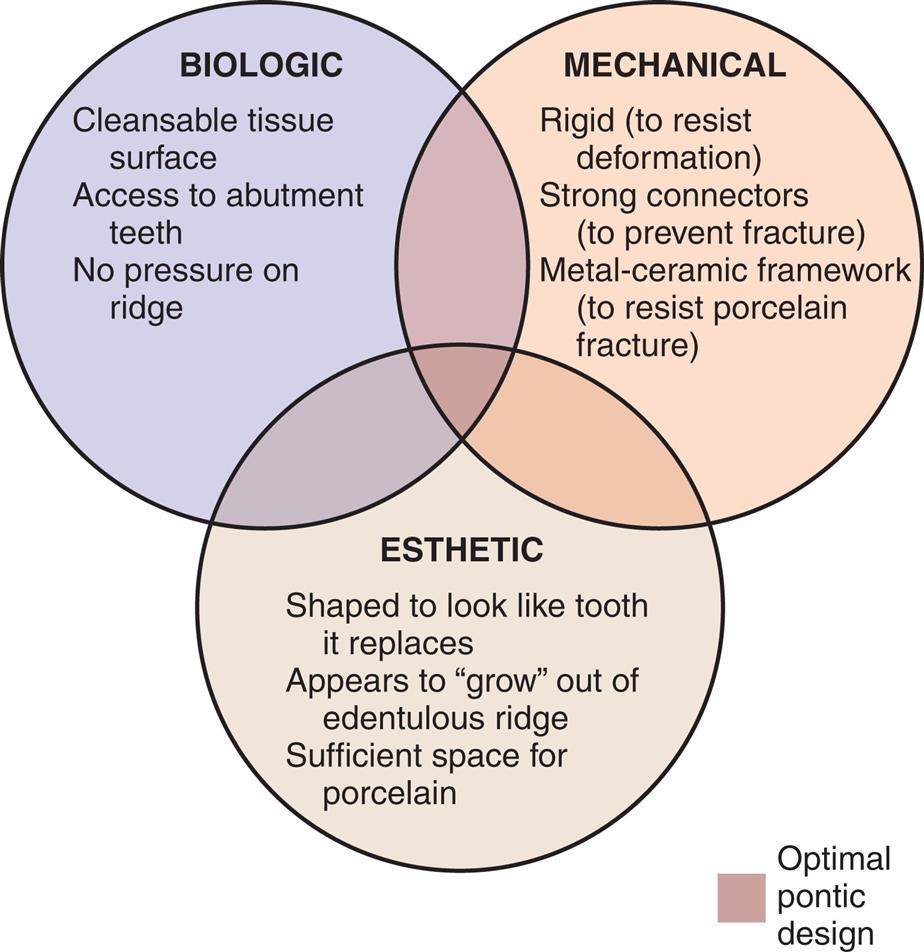
Because the pontic mechanically unifies the abutment teeth and covers a portion of the residual ridge, it assumes a dynamic role as a component of the prosthesis and cannot be considered a lifeless insert of gold, porcelain, acrylic resin, or zirconia.1
Pretreatment Assessment
Certain procedures enhance the success of an FPD. In the treatment-planning phase, diagnostic casts and waxing procedures may prove especially valuable for determining optimal pontic design (see Chapters 3 and 18).
Pontic Space
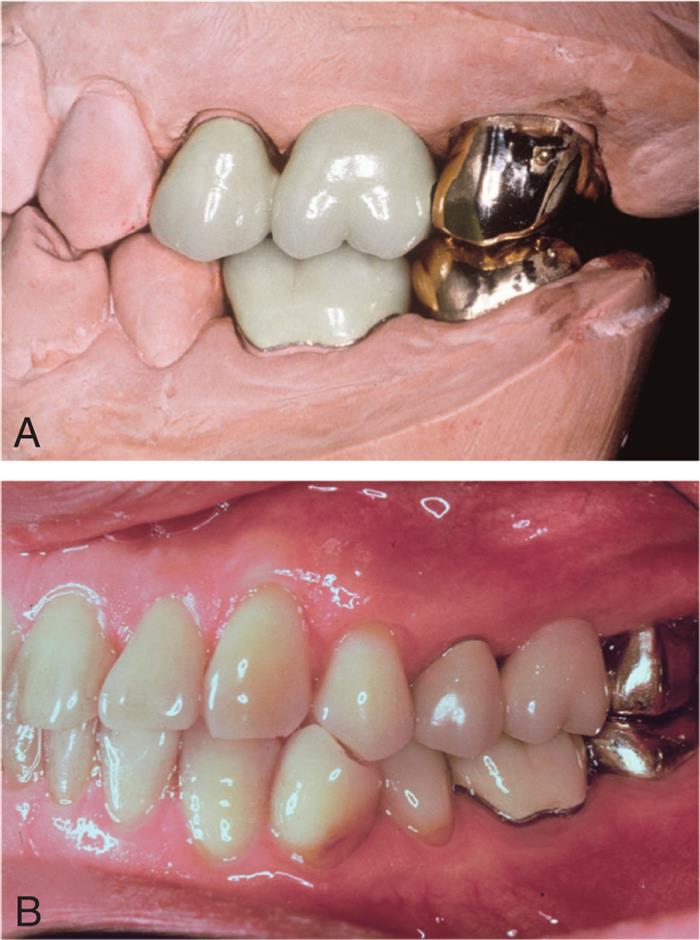
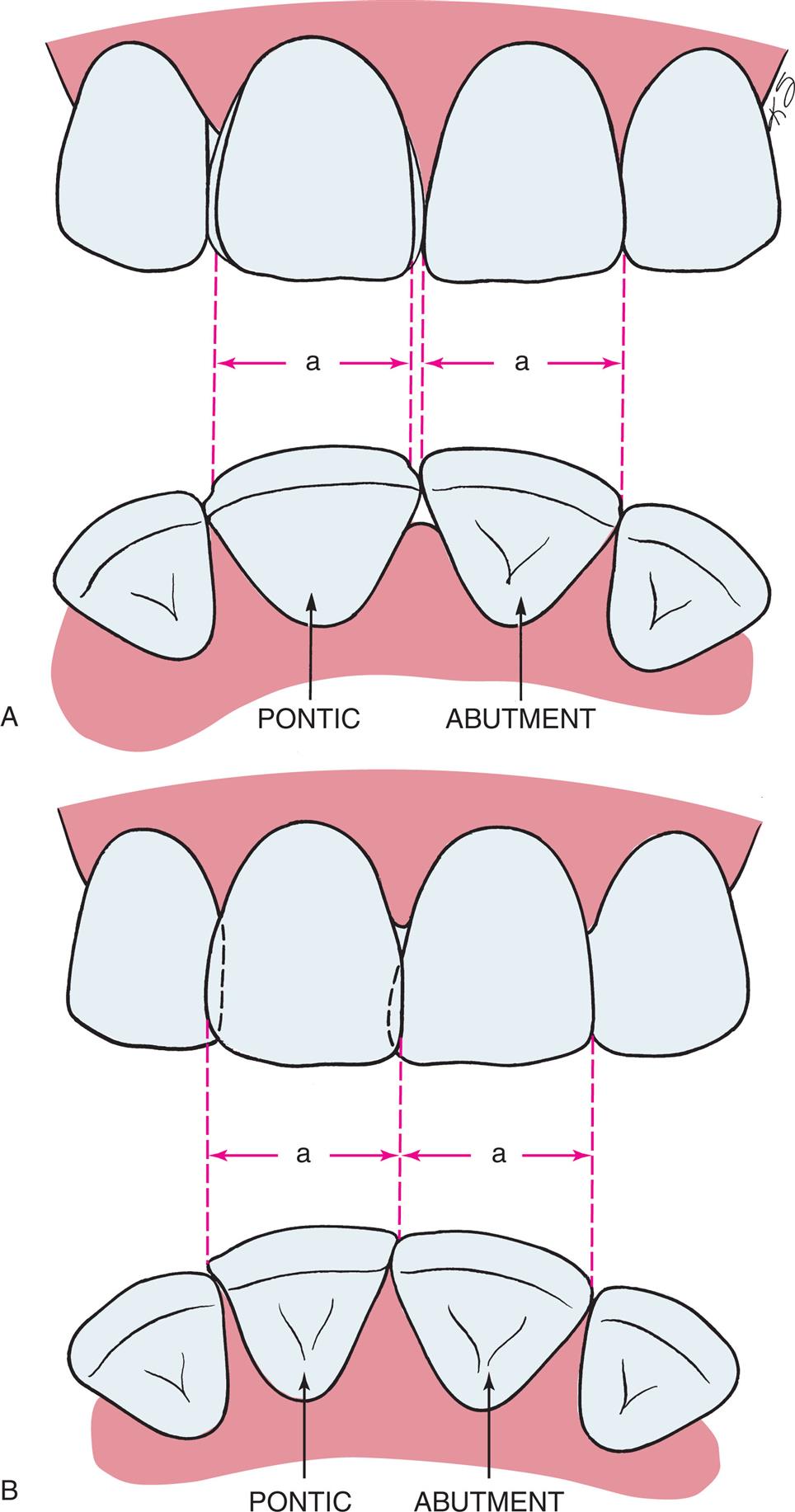
One function of an FPD is to prevent tilting or drifting of the adjacent teeth into the edentulous space. If such movement has already occurred, the space available for the pontic may be reduced and its fabrication may be complicated. In such circumstances, creating an acceptable appearance without orthodontic repositioning of the abutment teeth is often impossible, particularly if esthetic appearance is important. (Modification of abutments with complete-coverage retainers is sometimes feasible.) Careful diagnostic waxing procedures help determine the most appropriate treatment (see Chapters 2). Even with a lesser esthetic requirement, as for posterior teeth, overly small pontics are unacceptable because they trap food and are difficult to clean. When orthodontic repositioning is not possible, increasing the proximal contours of adjacent teeth may be better than making an FPD with undersized pontics (Fig. 20.3). If there is no functional or esthetic deficit, the space can be maintained without prosthodontic intervention.
Residual Ridge Contour
The edentulous ridge's contour and topography should be carefully evaluated during the treatment-planning phase. An ideally shaped ridge has a smooth, regular surface of attached gingiva, which facilitates maintenance of a plaque-free environment. Its height and width should allow placement of a pontic that appears to emerge from the ridge and mimics the appearance of neighboring teeth. Facially, it must be free of frenum attachment and be of adequate facial height to sustain the appearance of interdental papillae.
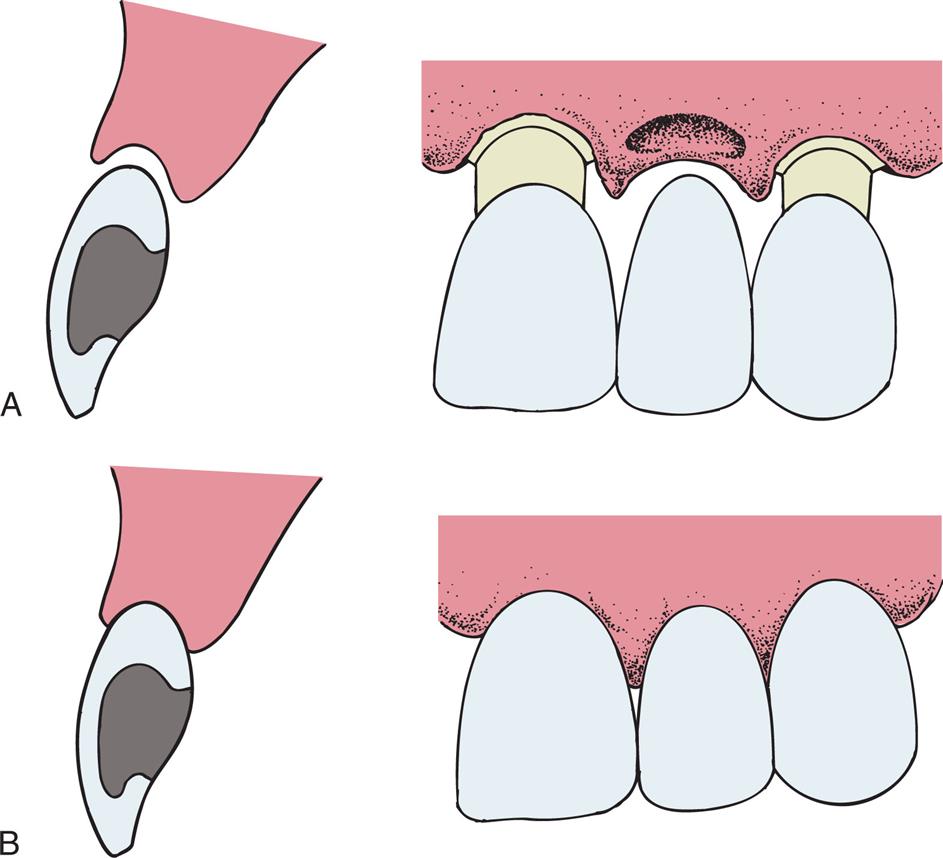
Loss of residual ridge contour may lead to unesthetic open gingival embrasures (“black triangles”; Fig. 20.4A), food impaction (see Fig. 20.4B), and percolation of saliva during speech. Siebert2 classified residual ridge deformities into three categories (Table 20.1; Fig. 20.5):
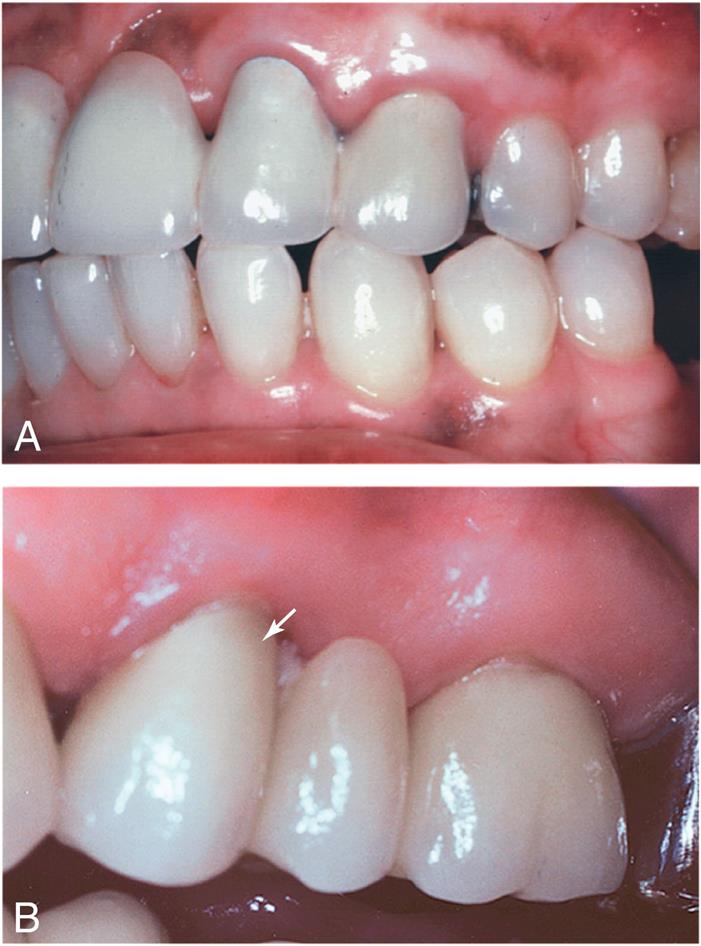
Table 20.1
| Class | INCIDENCE (%) | ||
|---|---|---|---|
| Description | Abrams et al.3 | Siebert2 | |
| 0 | No defect | 12 | 0 |
| I | Horizontal loss | 36 | 13 |
| II | Vertical loss | 0 | 40 |
| III | Horizontal and vertical loss | 52 | 47 |
Adapted from Edelhoff D, Spiekermann H, Yildirim M. A review of esthetic pontic design options. Quintessence Int. 2002;33:736.
The incidence of residual ridge deformity after anterior tooth loss is high at 91%3. In the majority of these patients, the deformities are class III defects. Many patients with class II and class III defects are dissatisfied with the esthetics of their FPDs.4 Pre-prosthetic surgery to augment such residual ridges should be carefully considered.
Surgical Modification
Although residual ridge width may be augmented with hard tissue grafts, this is usually not indicated unless the edentulous site is to receive an implant (see Chapter 13).
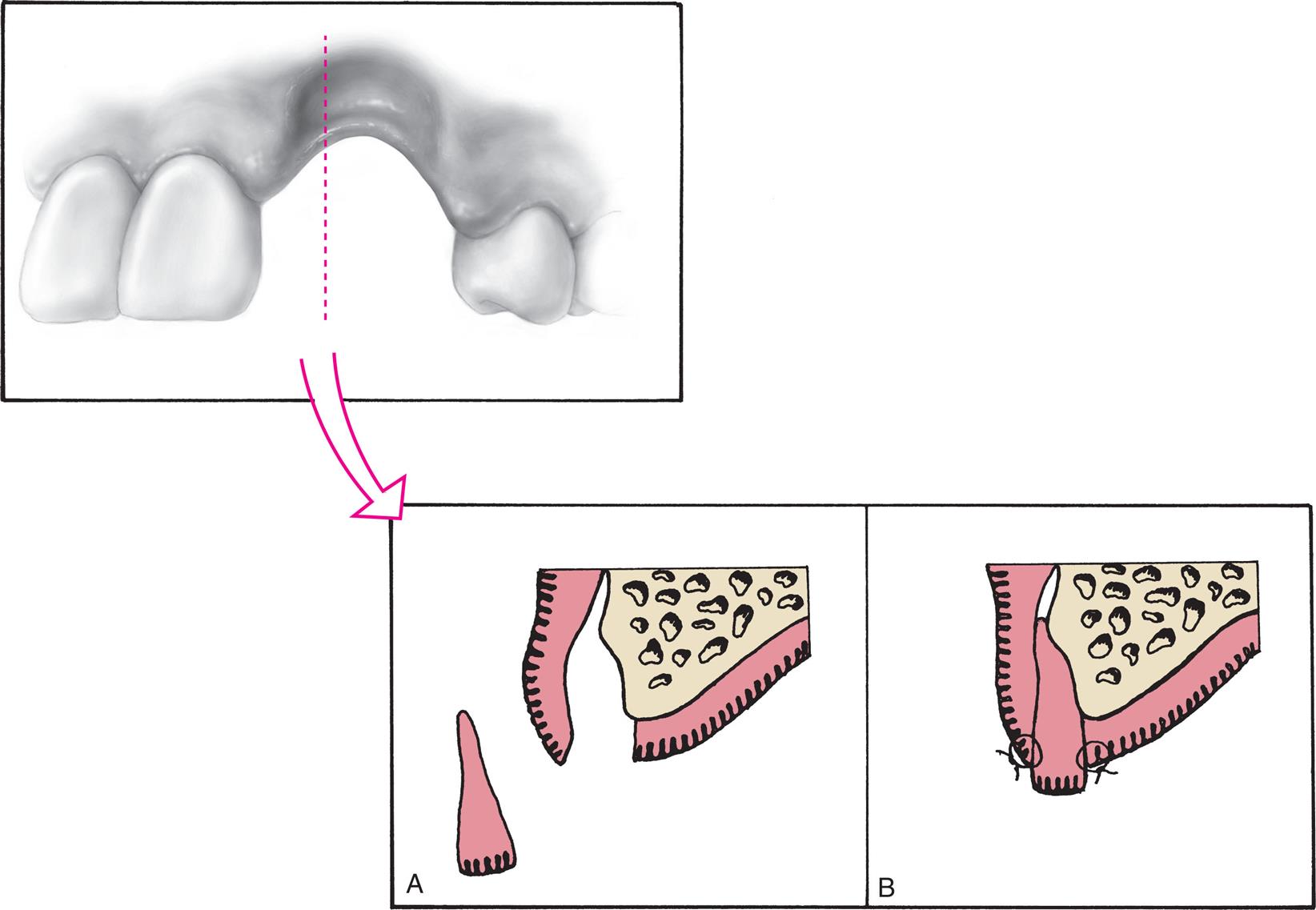
Class I Defects
Soft tissue procedures have been advocated for improving the width of a class I defect. However, because class I defects are infrequent and are not esthetically challenging, surgical augmentation of ridge width is uncommon. By paying careful attention to interim pontic contour, the operator can identify patients who would benefit from surgery. In the roll5 technique, soft tissue from the lingual side of the edentulous site is used. The epithelium is removed, and the tissue is thinned and rolled back upon itself, thereby thickening the facial aspect of the residual ridge (Fig. 20.6). Pouches may also be prepared in the facial aspect of the residual ridge6 into which subepithelial7,8 or submucosal9 grafts harvested from the palate or tuberosity may be inserted (Fig. 20.7).
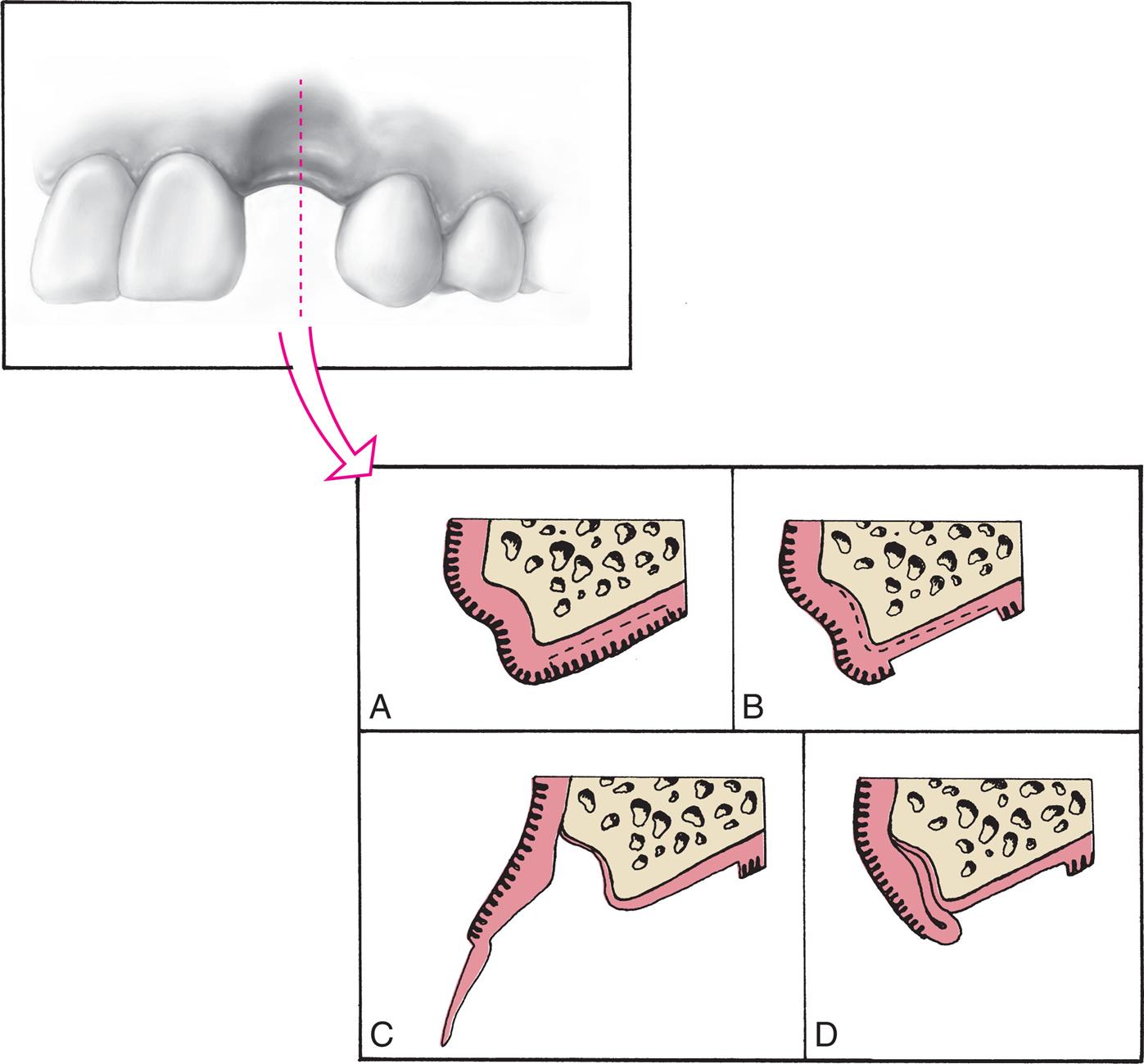
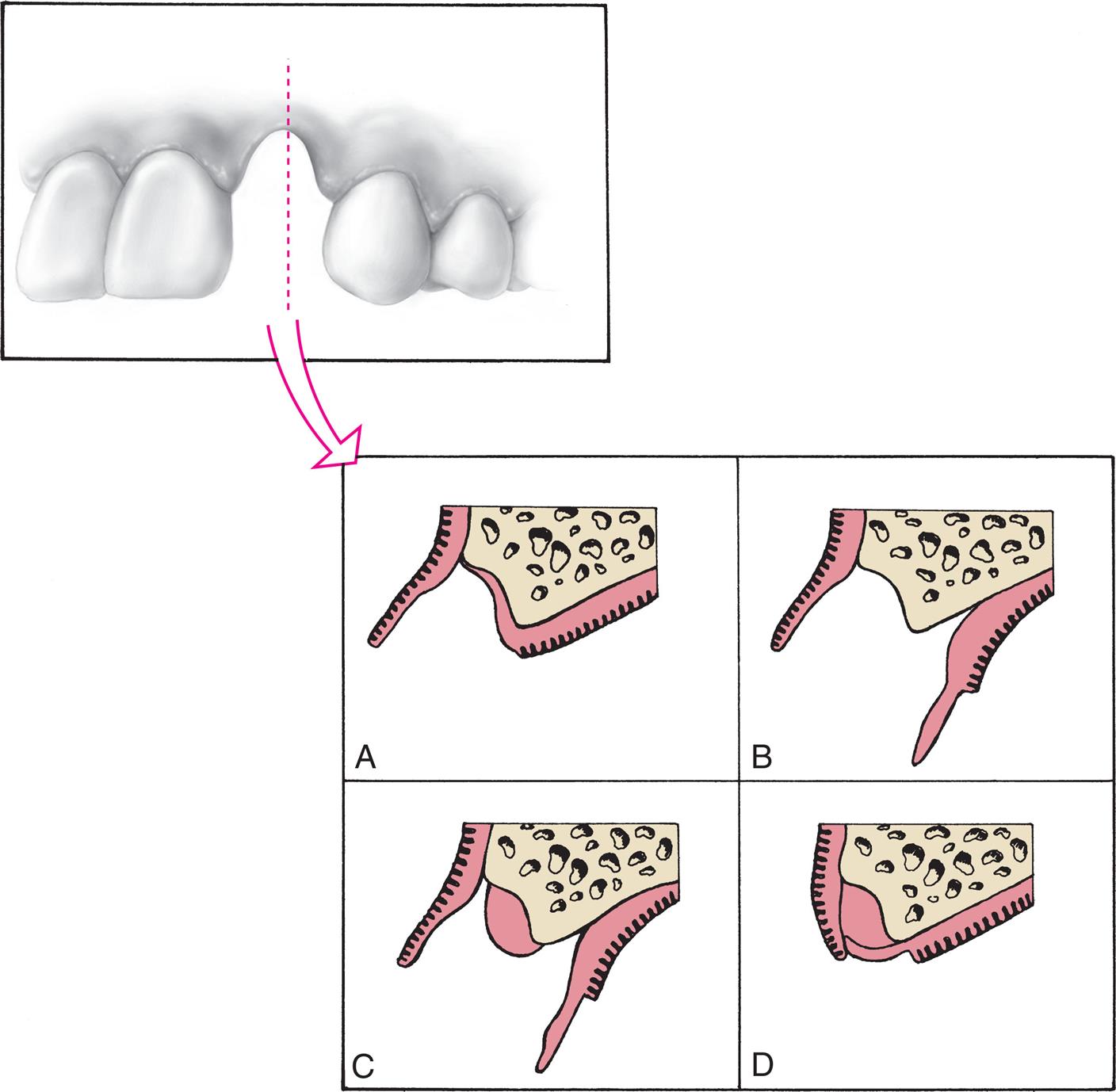
Class II and Class III Defects
Unfortunately, few soft tissue surgical techniques can increase the height of a residual ridge with predictability. The interpositional graft2,10 is a variation of the pouch technique in which a wedge-shaped, connective tissue graft is inserted into a pouch preparation on the facial aspect of the residual ridge. The epithelial portion of the wedge may be positioned coronally to the surrounding epithelium if an increase of ridge height is desired (Fig. 20.8). The onlay graft is designed to increase ridge height,2,11 but also contributes to ridge width, which makes it useful for treating class III ridge defects (Fig. 20.9). It is a thick “free gingival graft,” harvested from partial- or full-thickness palatal donor sites. Because the amount of height augmentation can be only as thick as the graft, the procedure may have to be repeated several times to reestablish normal residual ridge height. Although the onlay graft has greater potential for increasing ridge height than the interpositional graft, its survival is greatly dependent on revascularization, which requires meticulous preparation of the recipient site. Therefore, the onlay graft is more technique-sensitive than the interpositional graft. In fact, connective tissue grafts have been demonstrated to achieve approximately a 50% increase in ridge-volume 3.5 months after surgery than free gingival grafts in single-tooth residual ridge defects.12
Gingival Architecture Preservation
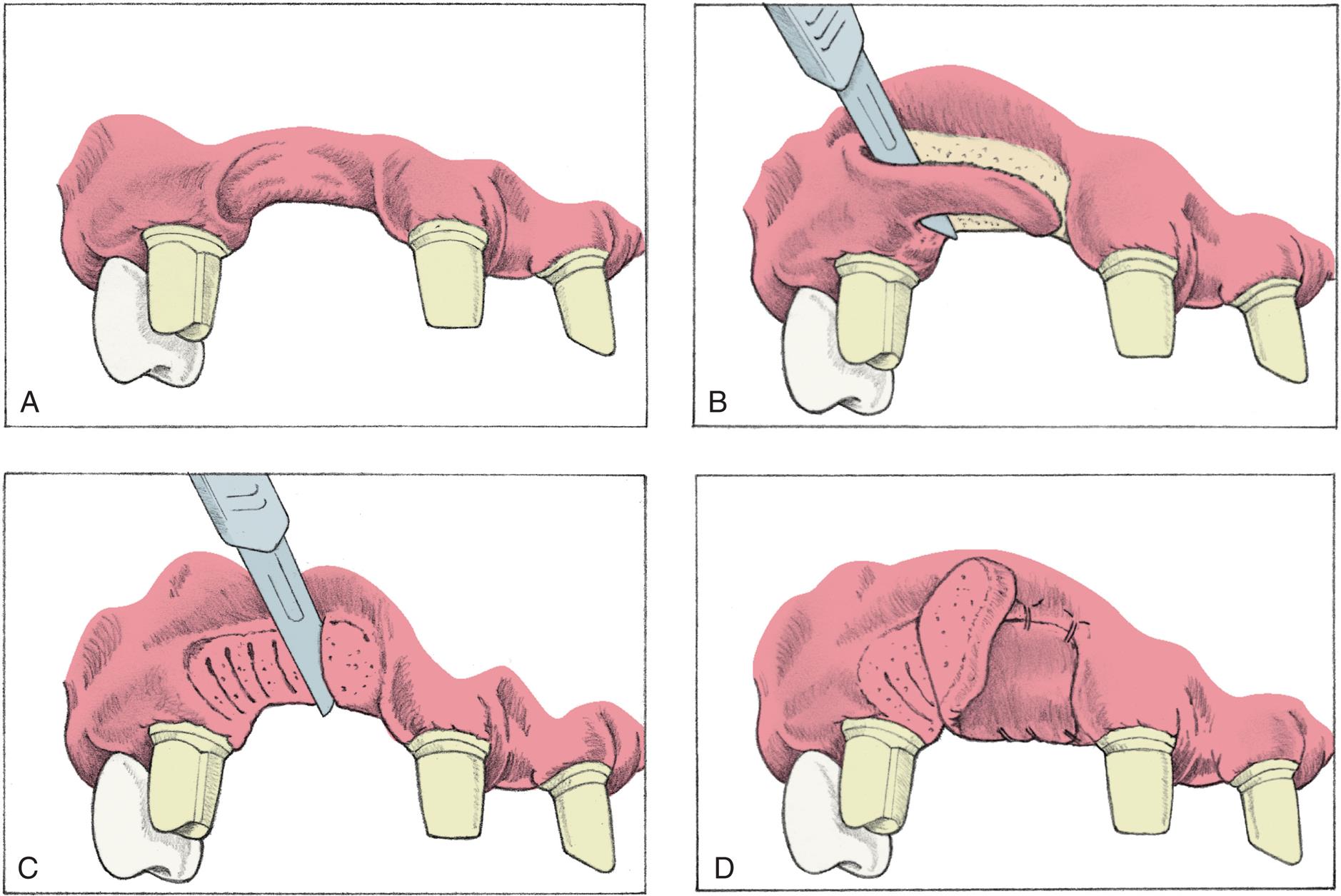
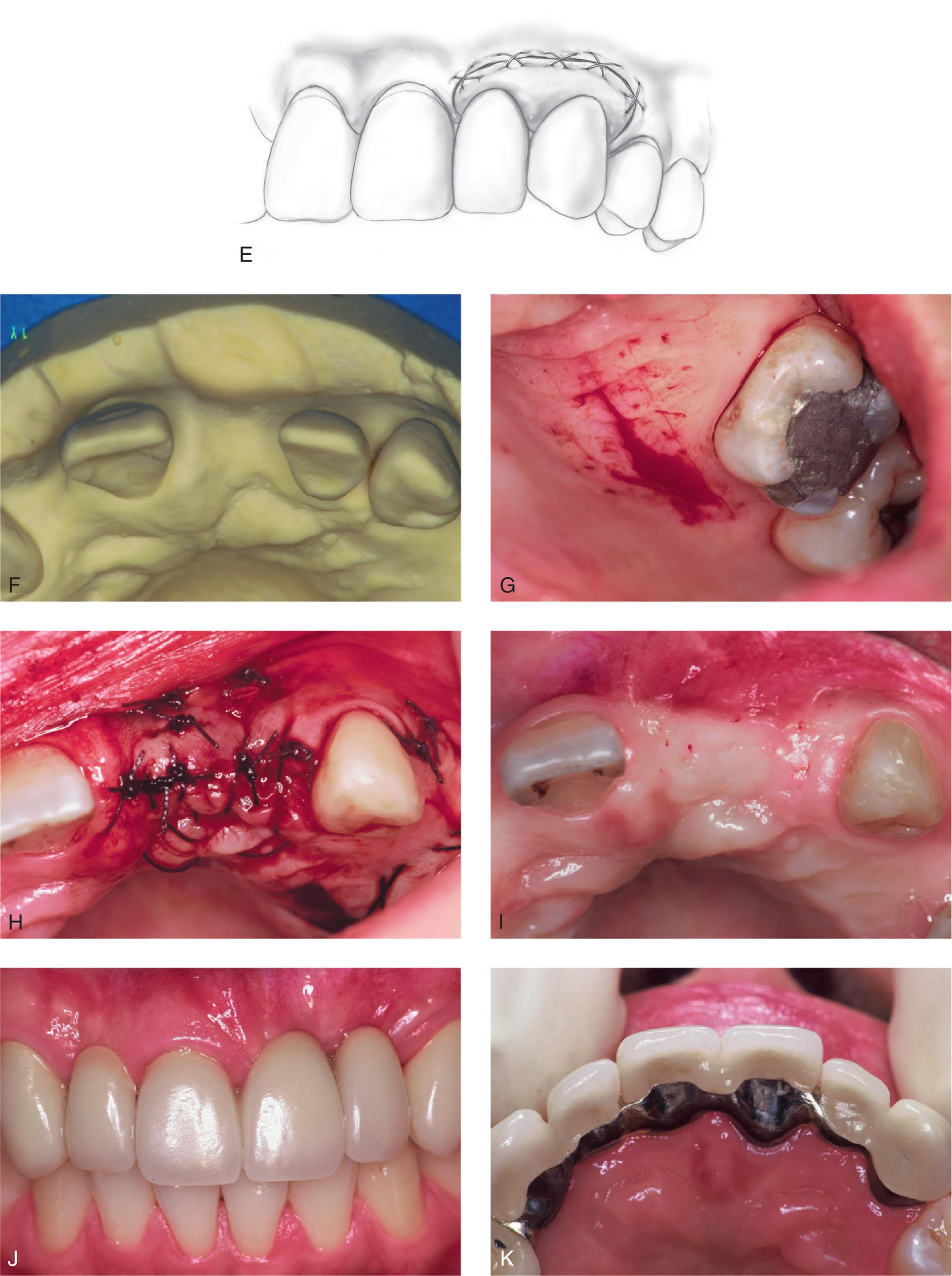
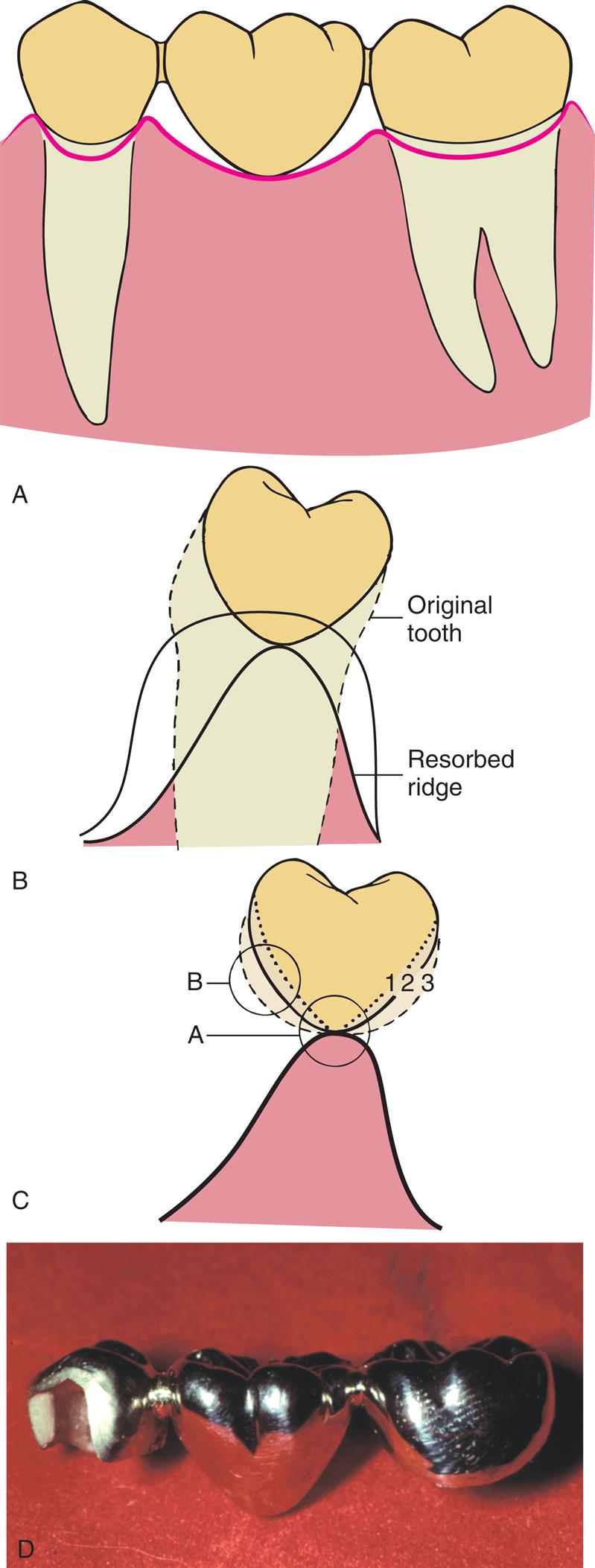
Resorption of the alveolar ridge, after tooth extraction, occurs primarily at the buccal plate, typically resulting in a horizontal defect. Bone loss averages 3 to 5 mm at 6 months after extraction; 50% of the width of the alveolar ridge is lost at 12 months.13,14 Although the degree of residual ridge resorption after tooth extraction is unpredictable, resulting deformities are not inevitable. The alveolar process can be preserved through immediate restorative and periodontal intervention at the time of tooth removal. By conditioning the extraction site and providing a matrix for healing, the dentist can preserve the pre-extraction gingival architecture or “socket.”
Preparing the abutment teeth before the extraction is the preferred technique. An interim FPD can be fabricated indirectly, ready for immediate insertion. Because socket preservation is dependent on underlying bone contour, the extraction of the tooth to be replaced should be atraumatic, with the aim of preserving the facial plate of bone. The scalloped architecture of interproximal bone forming the extraction site is essential for proper papilla form, as are facial bone levels in the prevention of alveolar collapse. If bone levels are compromised before or during extraction, the sockets can be grafted with an allograft material (hydroxyapatite, tricalcium phosphate, or freeze-dried bone).13,15,16
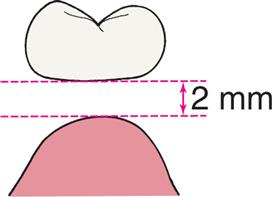
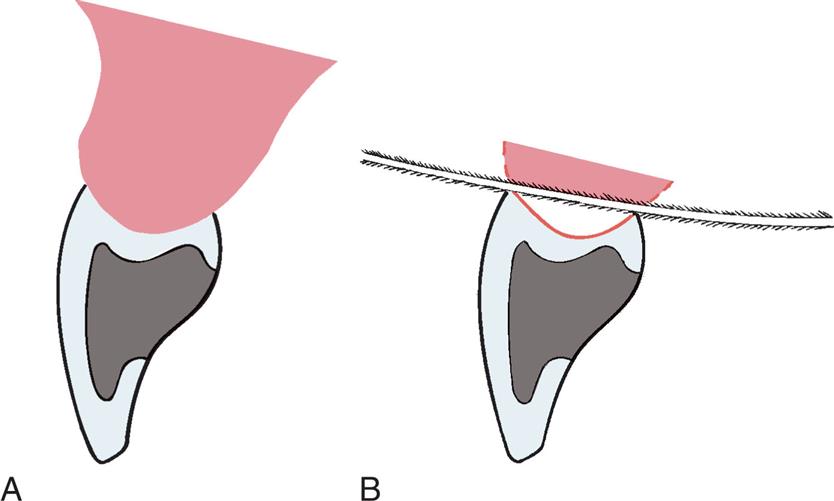
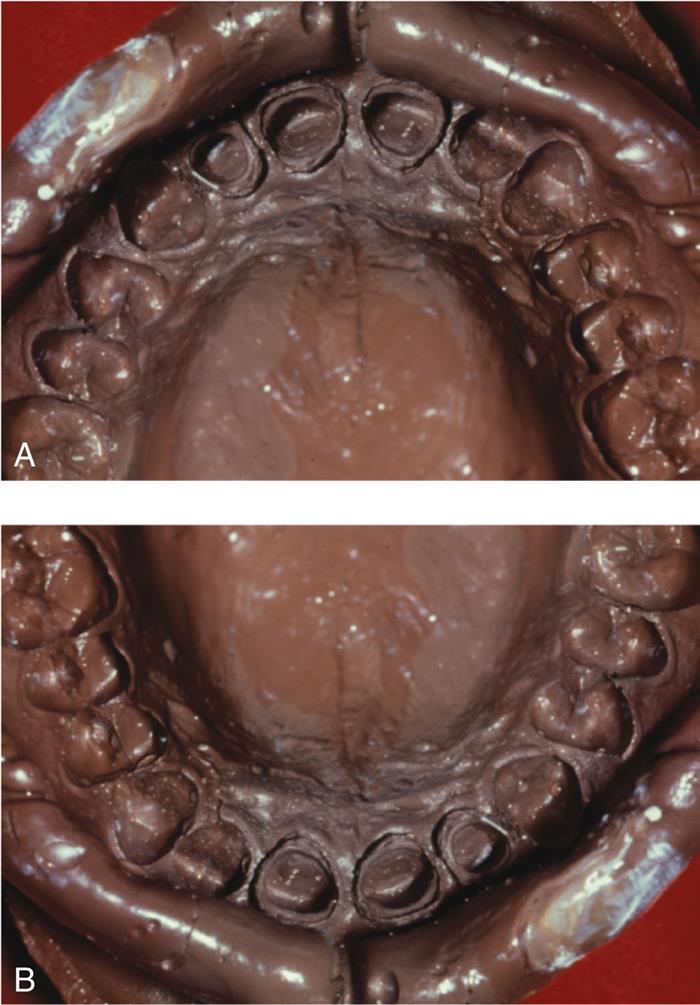
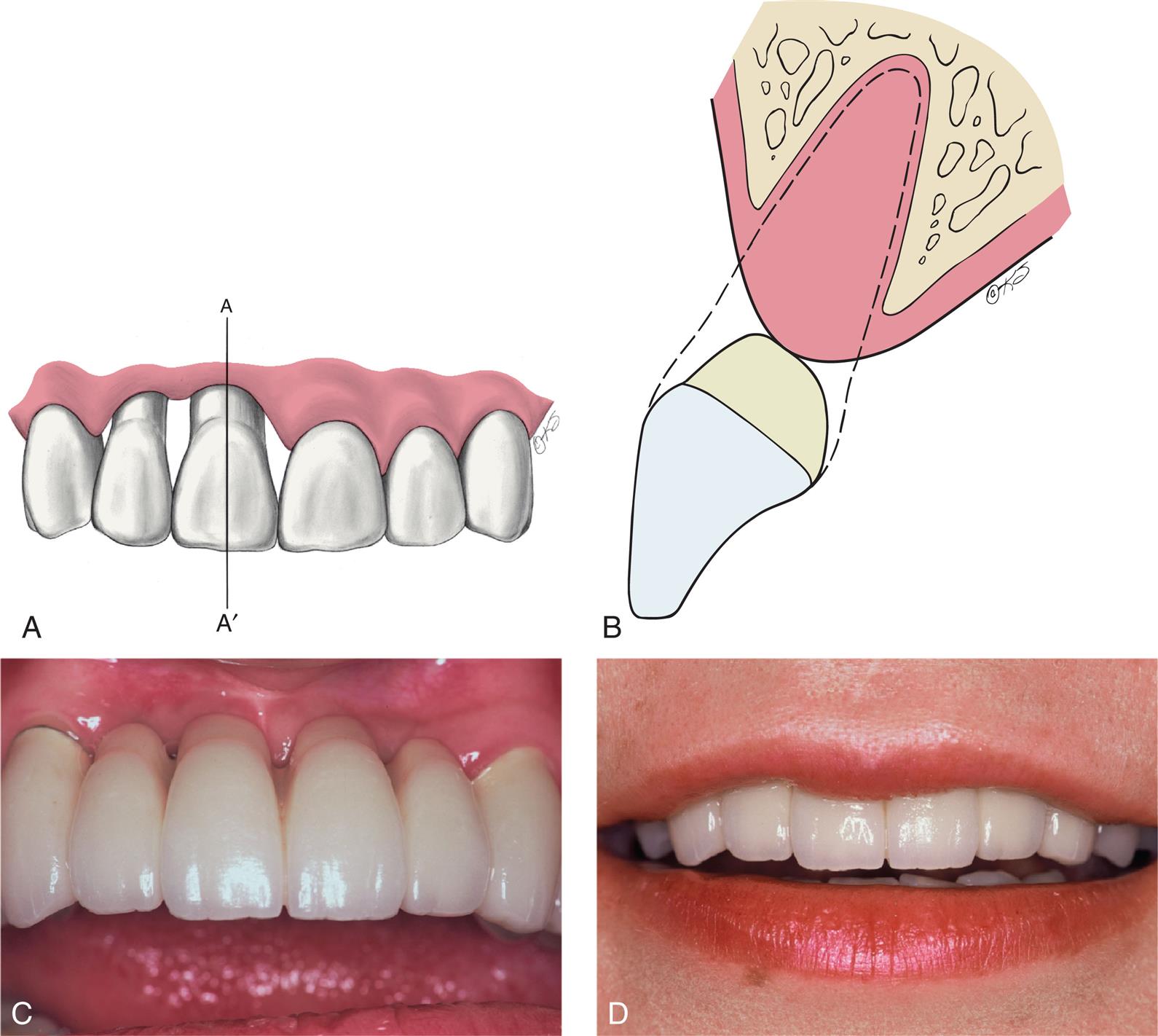
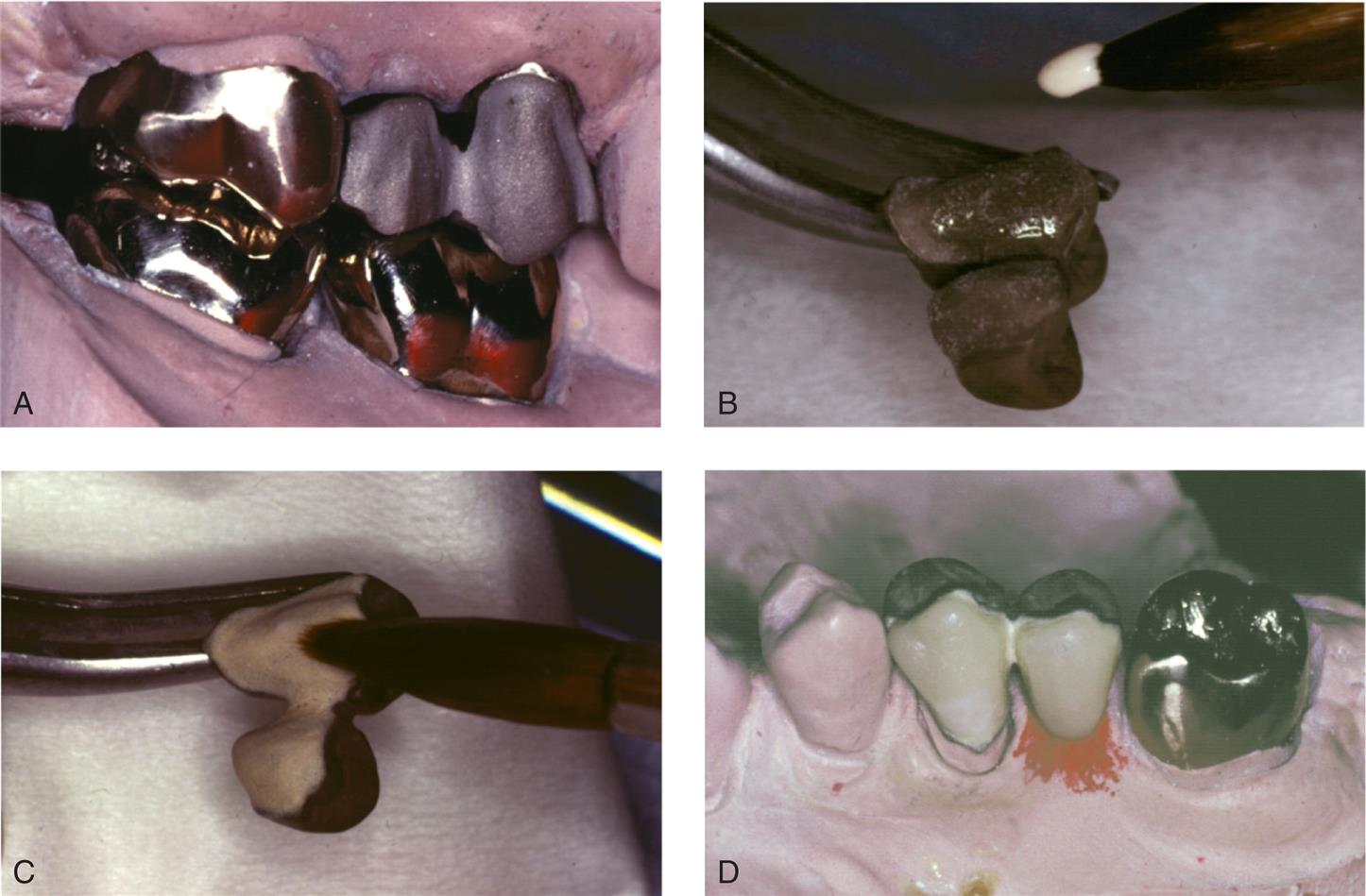
Immediately after preparation of the extraction site, a carefully shaped interim FPD is placed (Fig. 20.10A and B). The tissue side of the pontic should be an ovate form, and, according to Spear,17 it should extend approximately 2.5 mm apical to the facial free gingival margin of the extraction socket (see Fig. 20.10C and D). Because the soft tissues of the socket begin to collapse immediately after the tooth extraction, the pontic causes tissue blanching as it supports the papillae and facial/palatal gingiva. The contour of the ovate tissue side of the pontic is critical and must conform to within 1 mm of the interproximal and facial bone contour to act as a template for healing. Oral hygiene in this area is difficult during the initial healing period, so the interim restoration should be highly polished to minimize plaque retention. After approximately 1 month of healing, oral hygiene access is improved by recontouring the pontic to provide 1 to 1.5 mm of relief from the tissue. When the gingival levels are stable (approximately 6 to 12 months) the definitive restoration can be fabricated (see Fig. 20.10E).

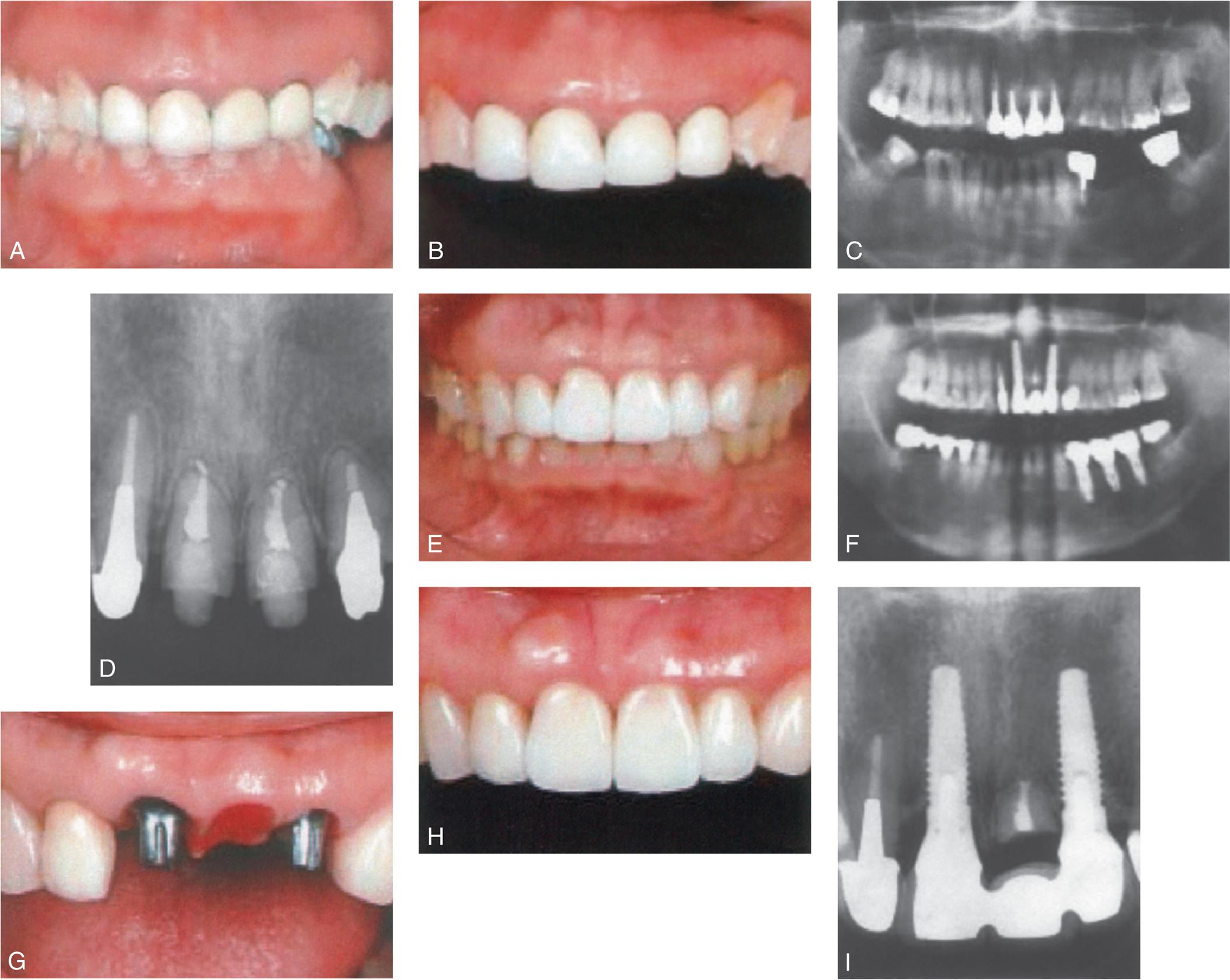
Techniques involving orthodontic extrusions have also been employed to preserve ridge form before extraction. In these proactive methods, light forces are used to extrude the teeth destined to be extracted. As the teeth are extruded, apposition of bone occurs at the root apex, thereby filling the socket with bone as the tooth is slowly extracted orthodontically. First employed to avoid ridge augmentation and to increase vertical ridge height before immediate implant placement,18 the orthodontic extrusion technique has been used successfully to maintain ridge contour before treatment with conventional FPDs (Fig. 20.11). In addition to the additional time and expense of orthodontic treatment, endodontic treatment is necessary beforehand because the teeth to be extracted must continuously be adjusted as they are extruded.

Although maintenance of the residual ridge after extraction is desirable, socket-preservation techniques are technically challenging, require frequent patient monitoring, and necessitate conscientious hygiene by the patient. Even when the procedure is performed meticulously, success is unpredictable because of the variability in patients' healing responses. Rarely can socket preservation completely preserve the alveolar ridge frame.19 Additional surgical augmentation of the ridge may still be necessary for some patients.
As an alternative to socket preservation and ridge augmentation surgery, root submergence techniques have been recommended to preserve alveolar bone heights. Originally documented in the 1970s, root submergence technique involves the resection of the tooth crown and the subsequent covering of the remaining root with a gingival flap. This technique has been successfully employed to preserve ridge height for patients with complete dentures.20 The technique has been performed with vital and nonvital roots. Root submergence can also be used to preserve the alveolar ridge for anterior pontic sites between natural tooth abutments21 and implant abutments (Fig. 20.12).22
Pontic Classification
Pontic designs are classified into two general groups: those that contact the oral mucosa and those that do not (Box 20.1). Several subclassifications exist within these groups that are based on the shape of the gingival side of the pontic. Pontic selection depends primarily on esthetics and oral hygiene. In the anterior region, where esthetic appearance is a concern, the pontic should be well adapted to the tissue to make it appear as if it emerges from the gingiva. Conversely, in the posterior regions (mandibular premolar and molar areas), contours can be modified in the interest of designs that are less esthetic but amenable to oral hygiene. The advantages and disadvantages of the various pontic designs are summarized in Table 20.2.
Table 20.2
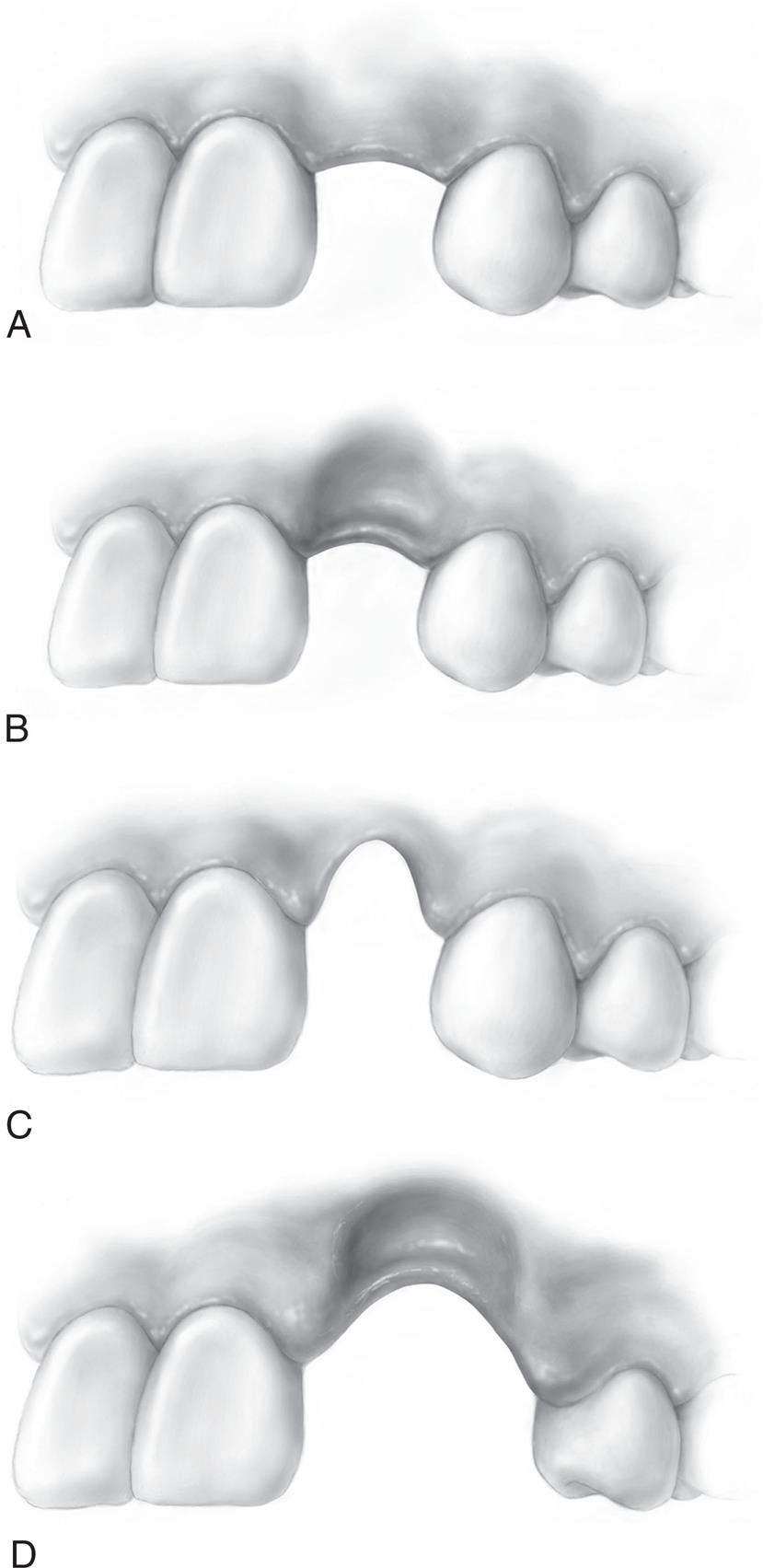
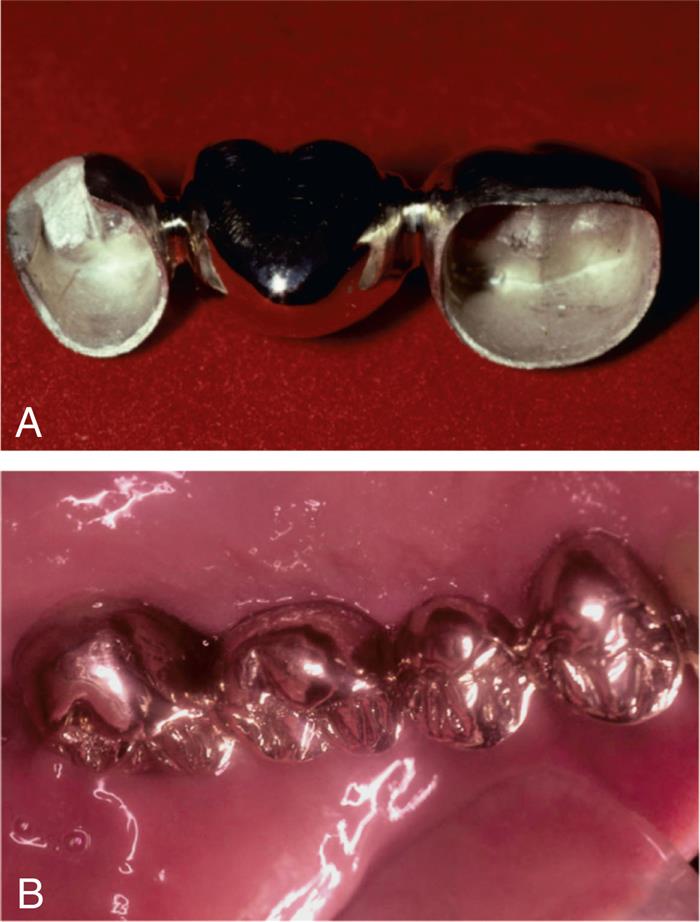
Sanitary or Hygienic Pontic
As its name implies, the primary design feature of the sanitary pontic allows easy cleaning because its tissue surface remains clear of the residual ridge (Fig. 20.13A). This hygienic design enables easier plaque control by allowing gauze strips and other cleaning devices to be passed under the pontic and seesawed in a shoeshine manner. Disadvantages include entrapment of food particles, which may lead to tongue habits that annoy the patient. The hygienic pontic is the least tooth-like design and is therefore reserved for teeth seldom displayed during function (i.e., the mandibular molars).
A modified version of the sanitary pontic has been developed (see Fig. 20.13B and C).23 Its gingival portion is shaped like an archway between the retainers. This geometry allows for an increase in connector size and a decrease in the stress concentrated in the pontic and connectors.24 It is also less susceptible to tissue proliferation that can occur when a pontic is too close to the residual ridge (see Fig. 20.13D).
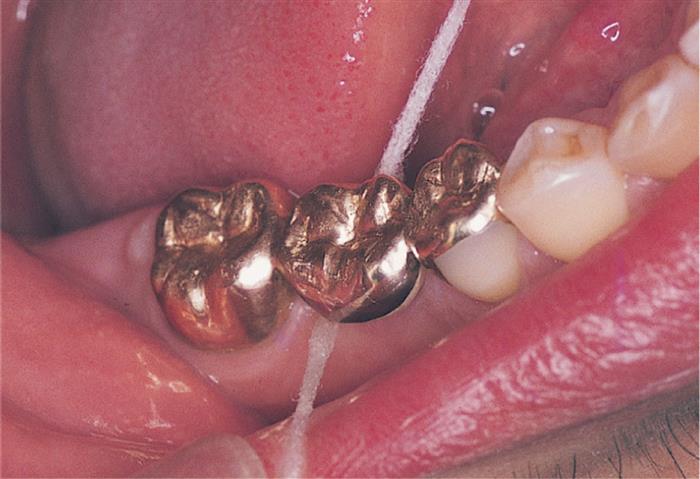
Saddle and Ridge-Lap Pontics
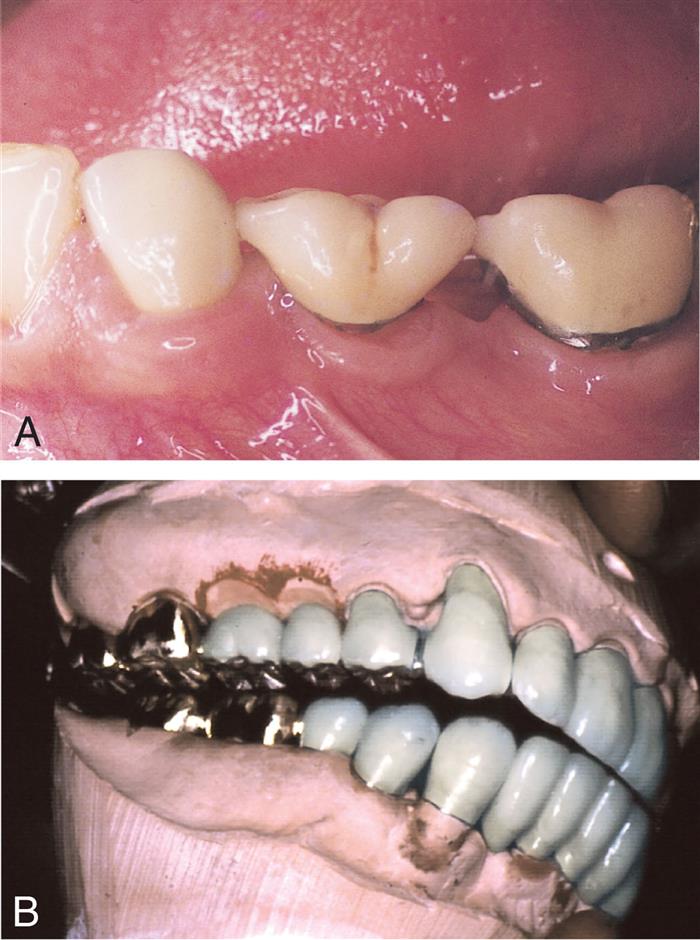
The saddle pontic has a concave fitting surface that overlaps the residual ridge buccolingually, simulating the contours and emergence profile of the missing tooth on both sides of the residual ridge. However, saddle or ridge-lap designs should be avoided because the concave gingival surface of the pontic is not accessible to cleaning with dental floss, which leads to plaque accumulation (Fig. 20.14). This design deficiency has been shown to result in tissue inflammation (Fig. 20.15).1

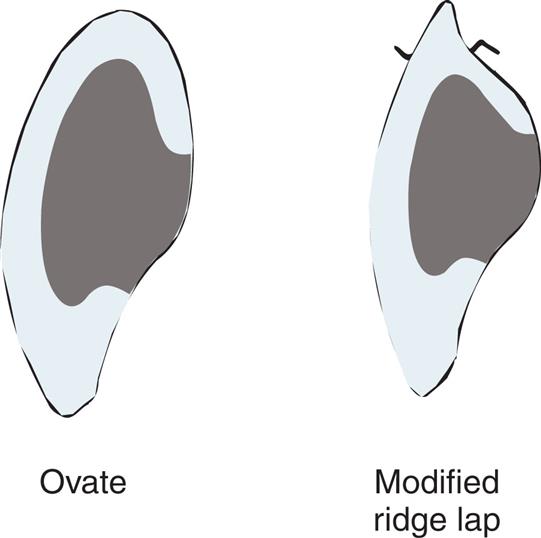
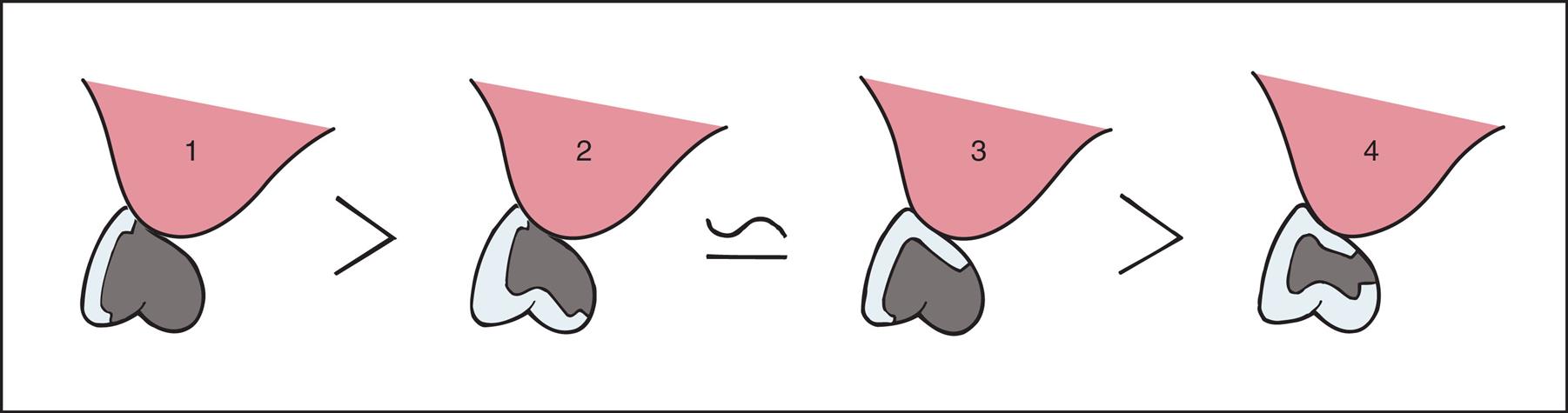
Modified Ridge-Lap Pontic
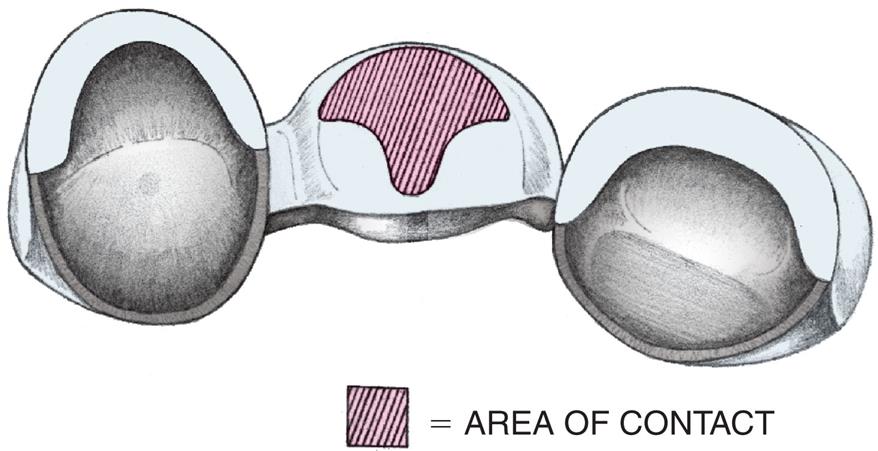
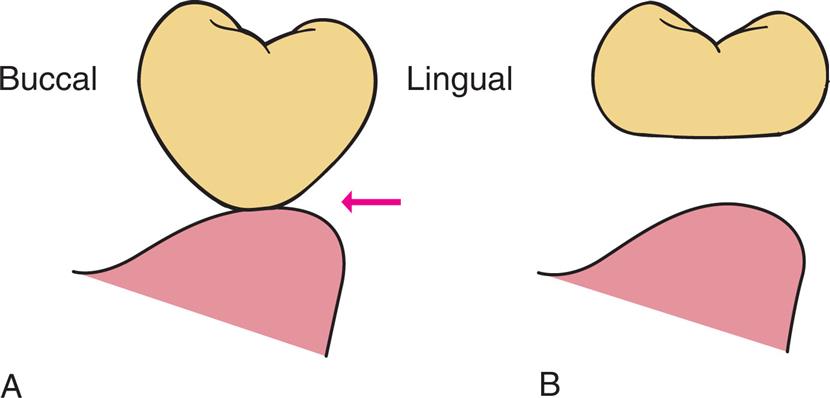
The modified ridge-lap pontic combines the best features of the hygienic and saddle pontic designs, combining esthetics with easy cleaning. Demonstrated by Figs. 20.16 and 20.17, the modified ridge-lap pontic overlaps the residual ridge on the facial side (to achieve the appearance of a tooth emerging from the gingiva), but remains clear of the ridge on the lingual side. To enable optimal plaque control, the gingival surface must have no depression or hollow; rather, it should be as convex as possible from mesial to distal aspects (the greater the convexity, the easier the oral hygiene). Tissue contact should resemble a letter T (Fig. 20.18) whose vertical arm ends at the crest of the ridge. Facial ridge adaptation is essential for a natural appearance. Although this design was historically referred to as ridge-lap design,25,26 the term ridge-lap is now used synonymously with saddle design. The modified ridge-lap design is the most common pontic form used in areas of the mouth that are visible during function (maxillary and mandibular anterior teeth, maxillary premolars, and first molars).
Conical Pontic
Often called egg-shaped, bullet-shaped, or heart-shaped, the conical pontic (Fig. 20.19) is straightforward for the patient to keep clean. It should be made as convex as possible and should have only one point of contact: at the center of the residual ridge. This design is recommended for the replacement of mandibular posterior teeth, for which esthetic appearance is a lesser concern. The facial and lingual contours are dependent on the width of the residual ridge; a knife-edged residual ridge necessitates flatter contours with a narrow tissue contact area. This type of design may be unsuitable for broad residual ridges because the emergence profile associated with the small tissue contact point may create areas of food entrapment (Fig. 20.20). The sanitary or hygienic pontic is the design of choice in these clinical situations.
Ovate Pontic
The ovate pontic is the pontic design that is most esthetically appealing. Its convex tissue surface resides in a soft tissue depression or hollow in the residual ridge, which makes it appear that a tooth is literally emerging from the gingiva (Fig. 20.21). Careful treatment planning is necessary for successful results. Socket-preservation techniques should be performed at the time of extraction to create the tissue recess from which the ovate pontic form will appear to emerge. For a preexisting residual ridge, surgical augmentation of the soft tissue is typically required. When an adequate volume of ridge tissue is established, a socket depression is sculpted into the ridge with surgical diamonds, electrosurgery, or a dental laser. With every option, meticulous attention to the contour of the pontic of the interim restoration is essential when the residual ridge that will receive the definitive prosthesis is conditioned and shaped.
The advantages of an ovate pontic include its pleasing appearance and its strength. When it is used successfully with ridge augmentation, its emergence from the ridge appears identical to that of a natural tooth. In addition, its recessed form is not susceptible to food impaction. The broad convex geometry is stronger than that of the modified ridge-lap pontic because the porcelain at the gingivofacial extent of a pontic is supported (Fig. 20.22). Because the tissue surface of the pontic is convex in all dimensions, it is accessible to dental floss; however, meticulous oral hygiene is necessary to prevent tissue inflammation resulting from the large area of tissue contact. Other disadvantages include the need for surgical tissue management and the associated cost. Furthermore, an additional evaluation appointment is typically necessary to achieve an esthetic result. The socket depression, with its pseudopapillae, requires the support of the interim ovate pontic and will collapse when the interim restoration is removed before an impression is made. To compensate for this three-dimensional change in the socket that occurs during the impression making, it is necessary to scrape the cast in this area to ensure positive contact and support of the pseudopapillae with the definitive pontic. Alternatively, special impression techniques can be used, such as the one described by de Vasconcellos et al.27 Because these adjustments are made somewhat arbitrarily, it may also be necessary to make revisions to the tissue surface of the pontic (reshaping or porcelain additions) at the evaluation phase.
Modified Ovate Pontic
Liu28 described a modified version of the ovate pontic that expands the clinical indications for the ovate pontic. The modified ovate pontic possesses an ovate form with the apex positioned more facially on the residual ridge, rather than at the crest of the ridge. This alteration allows the use of the pontic in clinical scenarios in which horizontal ridge width is not sufficient for a conventional ovate pontic. Cleansing of this pontic is also purported to be easiest of all pontic types.
Biologic Considerations
The biologic principles of pontic design pertain to the maintenance and preservation of the residual ridge, abutments, opposing teeth, and healthy supporting mucosa on the alveolar ridge at the pontic site. Factors of specific influence are pontic-ridge contact, amenability to oral hygiene, and the direction of occlusal forces.
Alveolar Ridge Mucosal Lesions
Mucosa overlying the edentulous ridge is often not protected adequately after extraction with a removable or a fixed prosthesis. White lesions of the oral cavity are a common presentation and can have a variety of etiologies, both benign and malignant.29 Parafunctional habits such rubbing, chewing, or sucking on external objects, that is, ice chips, pencil, or any constant insult, can result in keratosis of the alveolar ridge mucosa. Woo and Lin evaluated histopathological findings of 584 patients with leukoplakia and reported that the most common age group to exhibit frictional keratosis were in the fifth and sixth decade.30 Edentulous ridges and retromolar pads frequently exhibit benign keratosis as they are susceptible to both masticatory forces, occlusal trauma, ill-fitting removable denture, or other dental prosthesis. Most traumatized gingiva along the alveolar ridge show clinical signs of erythema, ulceration, edema, or other reactive lesions such as pyogenic granuloma.31,32 A thorough evaluation of pontic site alveolar ridge tissue for any such white lesion, such as frictional keratosis and proliferative verrucous leukoplakia (PVL), should not be overlooked. PVL has shown to be associated with high recurrence and malignant transformation rates.33,34 Once the fixed prosthesis is cemented the pontic can obstruct the occlusal view of the alveolar ridge, risking the chance of unnoticed progression of these lesions. Careful and vigilant evaluation and following the necessary protocols in evaluating the suspicious tissue, typically with a biopsy, is highly recommended. These special circumstances help to modify the design and selection of pontic types to aid in rigorous soft tissue monitoring.
Ridge Contact
Pressure-free contact between the pontic and the underlying tissues prevent ulceration and inflammation of the soft tissues.1,35 If any blanching of the soft tissues is observed at evaluation, the pressure area should be identified with a disclosing medium (e.g., pressure-indicating paste) and the pontic should be recontoured until tissue contact is entirely passive. This passive contact should occur exclusively on keratinized attached tissue. When a pontic rests on mucosa, some ulceration may appear as a result of the normal movement of the mucosa in contact with the pontic (Fig. 20.23). Positive ridge pressure (hyperpressure) may be caused by excessive scraping of the ridge area on the definitive cast (Fig. 20.24). This was once promoted as a way to improve the appearance of the pontic-ridge relationship. However, because of the ulceration that inevitably results when flossing is not meticulously performed, the concept is not recommended1,36,37 unless followed as previously described for an ovate pontic.35,38 Although ovate pontics maintain positive tissue contact to support the pseudopapillae, healthy mucosa can be maintained if the contact to the mucosa is tight but noncompressive, and the gingival portion of the pontic is regularly cleaned.39


Oral Hygiene Considerations
The chief cause of ridge irritation is the toxins released from microbial plaque, which accumulate between the gingival surface of the pontic and the residual ridge, causing tissue inflammation and calculus formation.
Unlike removable partial dentures, FPDs cannot be taken out of the mouth for daily cleaning. Patients must be taught efficient oral hygiene techniques, with particular emphasis on cleaning the gingival surface of the pontic. The shape of the gingival surface, its relation to the ridge, and the materials used in its fabrication influence ultimate success.
Normally, where tissue contact occurs, the gingival surface of a pontic is inaccessible to the bristles of a toothbrush. Therefore, the patient must develop excellent hygiene habits. Devices such as proxy brushes, pipe cleaners, Oral-B Super Floss (Oral-B, Procter & Gamble), and dental floss with a threader are highly recommended (Fig. 20.25). Gingival embrasures around the pontic should be wide enough to allow oral hygiene aids. However, to prevent food entrapment, they should not be opened excessively. To enable passage of floss over the entire tissue surface, tissue contact between the residual ridge and pontic must be passive.
If the pontic has a depression or concavity in its gingival surface, plaque accumulates because the floss cannot clean this area and tissue irritation40 follows. This is usually reversible; when the surface is subsequently modified to eliminate the concavity, inflammation disappears (see Fig. 20.15). Therefore, an accurate description of pontic design should be submitted to the laboratory and the prosthesis should be checked and corrected if necessary before cementation. Prevention is the best solution for controlling tissue irritation.
Pontic Material
Any material chosen to fabricate the pontic should provide good esthetic results where needed; biocompatibility, rigidity, and strength to withstand occlusal forces; and longevity. FPDs should be made as rigid as possible because any flexure during mastication or parafunction may cause pressure on the gingiva and cause fractures of the veneering material. Occlusal contacts should not fall on the junction between metal and porcelain during centric or eccentric tooth contacts, nor should a metal-ceramic junction be in contact with the residual ridge on the gingival surface of the pontic.
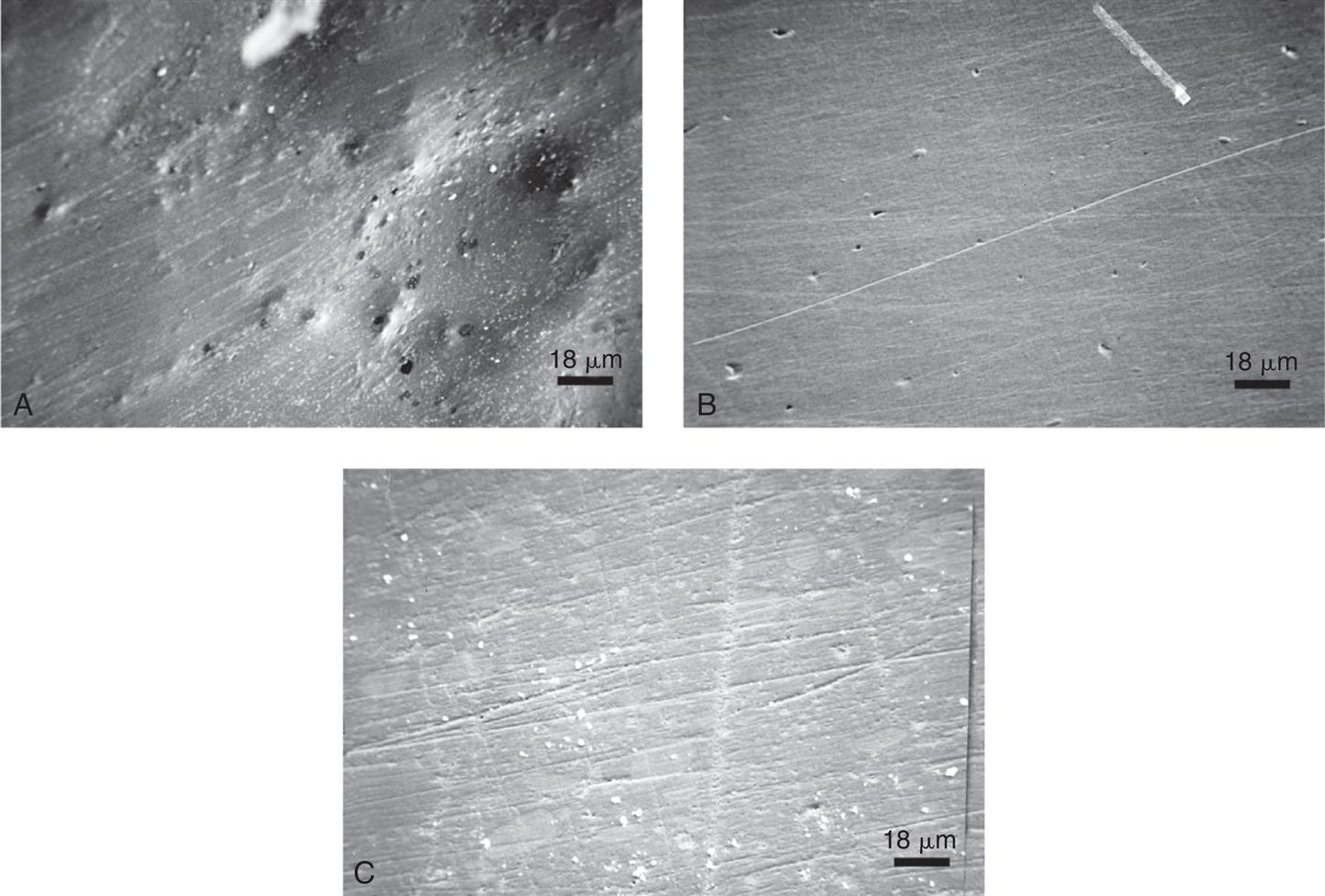
Investigations into the biocompatibility of materials used to fabricate pontics have centered on two factors: (1) the effect of the materials and (2) the effects of surface adherence. Glazed porcelain is generally considered the most biocompatible of the available pontic materials,41–43 and clinical data36,44 tends to support this opinion, although the crucial factor seems to be the material's ability to resist plaque accumulation45 (rather than the material itself). Well-polished gold is smoother, less prone to corrosion, and less retentive of plaque than unpolished or porous casting.46 However, even highly polished surfaces accumulate plaque if oral hygiene measures are ignored.47,48
Glazed porcelain looks very smooth, but when viewed under a microscope, its surface shows many voids and is rougher than that of either polished gold or acrylic resin (Fig. 20.26).49 Nevertheless, highly glazed porcelain is easier to clean than are other materials. For easier plaque removal and biocompatibility, the tissue surface of the pontic should be made in glazed porcelain. However, ceramic tissue contact may be contraindicated in edentulous areas where there is minimal distance between the residual ridge and the occlusal surface. In these instances, placing ceramic on the tissue side of the pontic may weaken the design of the metal substructure, particularly with porcelain occlusal surface (Fig. 20.27). If metal is placed in tissue contact, it should be highly polished. Zirconia has been shown to be a biocompatible material. The soft tissue response to this material is superior to other porous materials because of its low bacterial colonization potential.50 The absence of plaque produces clinically insignificant inflammatory responses to oral tissues.51 Regardless of the choice of pontic material, patients can prevent inflammation around the pontic with meticulous oral hygiene.52
Occlusal Forces
Reducing the buccolingual width of the pontic by as much as 30% has been suggested53,54 as a way to lessen occlusal forces on, and thus the loading of, abutment teeth. This practice continues today, although it has little scientific basis. Critical analysis55 has revealed that forces are lessened only when food of uniform consistency is chewed and that a mere 12% increase in chewing efficiency can be expected from a one-third reduction of pontic width. Potentially harmful forces are more likely to be encountered if an FPD is loaded by the accidental biting on a hard object or by parafunctional activities such as bruxism, rather than by chewing foods of uniform consistency. Narrowing the occlusal surface does not reduce these forces.
In fact, narrowing the occlusal surface may actually impede or even preclude the development of a harmonious and stable occlusal relationship. Like a malposed tooth, it may cause difficulties in plaque control and may not provide proper cheek support. For these reasons, pontics with normal occlusal widths (at least in the occlusal third) are generally recommended. One exception is the situation in which the residual alveolar ridge has collapsed buccolingually. Reducing pontic width may then be desired and would thereby lessen the lingual contour and facilitate plaque-control measures.
Mechanical Considerations
The prognosis of FPD pontics is compromised if mechanical principles are not followed closely. Mechanical problems may be caused by improper choice of materials, poor framework design, poor tooth preparation, or poor occlusion. These factors can lead to fracture of the prosthesis or displacement of the retainers. Long-span posterior FPDs are particularly susceptible to mechanical problems. Inevitably, significant flexing occurs as a result of high occlusal forces and because the displacement effects increase with the cube of the span length (see Chapter 3). Therefore, evaluating the likely forces on a pontic and designing accordingly are important. For example, a strong metal or zirconia pontic, rather than a metal-ceramic pontic (Fig. 20.28), may be needed in high-stress situations, in which it would be more susceptible to fracture. When metal-ceramic pontics are chosen, extending porcelain onto the occlusal surfaces to achieve better esthetics should also be carefully evaluated. In addition to its potential for fracture, porcelain may abrade the opposing dentition if the occlusal contacts are on enamel or metal.

Available Pontic Materials
Some FPDs are fabricated entirely of metal, lithium disilicate, acrylic resin, or zirconia, but most consist of a combination of metal and porcelain. The acceptance of acrylic resin–veneered pontics has been limited because of their reduced durability (wear and discoloration). The newer indirect composite resins, which are based on high inorganic content–filled resins and fiber-reinforced materials (see Chapter 15), have revived some interest in composite resin and resin-veneered pontics. Composite resin and resin-veneered pontics are seldom used as newer materials such as zirconia have better physical properties.
Zirconia Pontics
Zirconia has become a popular material for fixed implants and natural teeth restorations. Use of zirconia dictates the need to utilize computer-aided design and computer-aided manufacture (CAD-CAM) technology. Zirconia restorations can be milled from fully sintered, semi-sintered, or unsintered zirconia blanks.56 Fully sintered zirconia is very high in strength and can wear out the milling equipment rapidly. Most restorations are milled in the non-sintered or green stage. At this stage, the restorations are about 20% to 30% larger to accommodate for the shrinkage of the material during the sintering process. The CAD technology determines and calculates this value during the planning and designing stage.
A unique property of yttrium-stabilized tetragonal zirconia polycrystal (Y-TZP) is, ‘transformation toughening’ by which it prevents crack propagation by increasing the localized fracture resistance (see Chapter 25). The high fracture resistance makes it suitable to be used for long-span, fixed restorations with multiple pontics and abutments provided adequate connector dimension can be achieved.
Esthetics can be improved with zirconia pontics as it is a tooth colored material. With advancements, multiple shades of zirconia are now available to best color match with the adjacent teeth. A thin layer of porcelain can be added on the facial surface to improve the esthetics (porcelain fused to zirconia). One of the disadvantages of this material is the large connector size required between pontics and abutments,57 for adequate strength, which can compromise the gingival and occlusal/incisal embrasures (see Chapter 27). Large connectors can diminish the natural appearance of the restoration and compromise the ability for oral hygiene maintenance under zirconia pontics.
Metal-Ceramic Pontics
Most pontics are fabricated by the metal-ceramic technique. If properly used, this technique is helpful in solving commonly encountered clinical problems. A well-fabricated, metal-ceramic pontic is strong, easy to keep clean, and natural-looking. However, mechanical failure (Fig. 20.29) can occur and is often attributable to inadequate framework design. The principles of framework design are discussed in Chapter 19, but the following points are emphasized in this chapter:
- • The framework must provide a uniform veneer of porcelain (approximately 1.2 mm). Excessive thickness of porcelain contributes to inadequate support and predisposes to eventual fracture (Fig. 20.30). This is often true in the cervical portion of an anterior pontic. A reliable technique for ensuring uniform thickness of porcelain is to wax the fixed prosthesis to complete anatomic contour and then accurately cut back the wax to a predetermined depth (Fig. 20.31).
- • The metal surfaces to be veneered must be smooth and free of pits. Surface irregularities cause incomplete wetting by the porcelain slurry, which leads to voids at the porcelain-metal interface that reduce bond strength and increase the possibility of mechanical failure.
- • Sharp angles on the veneering area should be rounded. They produce increased stress concentrations that can cause mechanical failure.
- • The location and design of the external metal-porcelain junction require particular attention. Any deformation of the metal framework at the junction can lead to chipping of the porcelain (Fig. 20.32). For this reason, occlusal centric contacts must be placed at least 1.5 mm away from the junction. Excursive, eccentric contacts that might deform the metal-ceramic interface must be evaluated carefully.


Esthetic Considerations
No matter how well biologic and mechanical principles have been followed during fabrication, the patient evaluates the result by how it looks, especially when anterior teeth have been replaced. Many esthetic considerations that pertain to single crowns also apply to pontics (see Chapter 23). Several problems unique to pontics may be encountered in the attempt to achieve a natural appearance.
The Gingival Interface
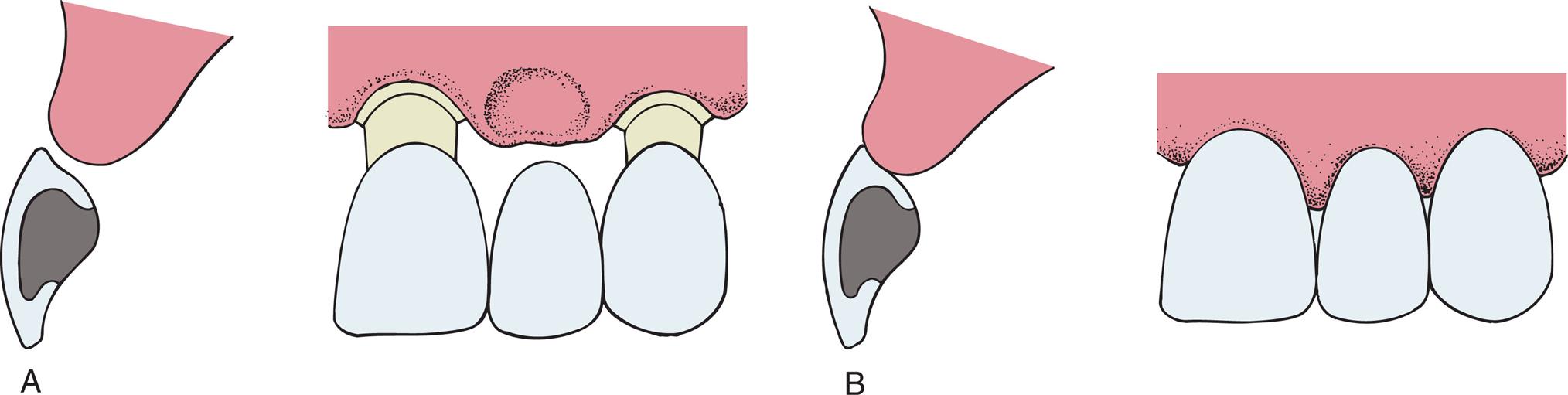
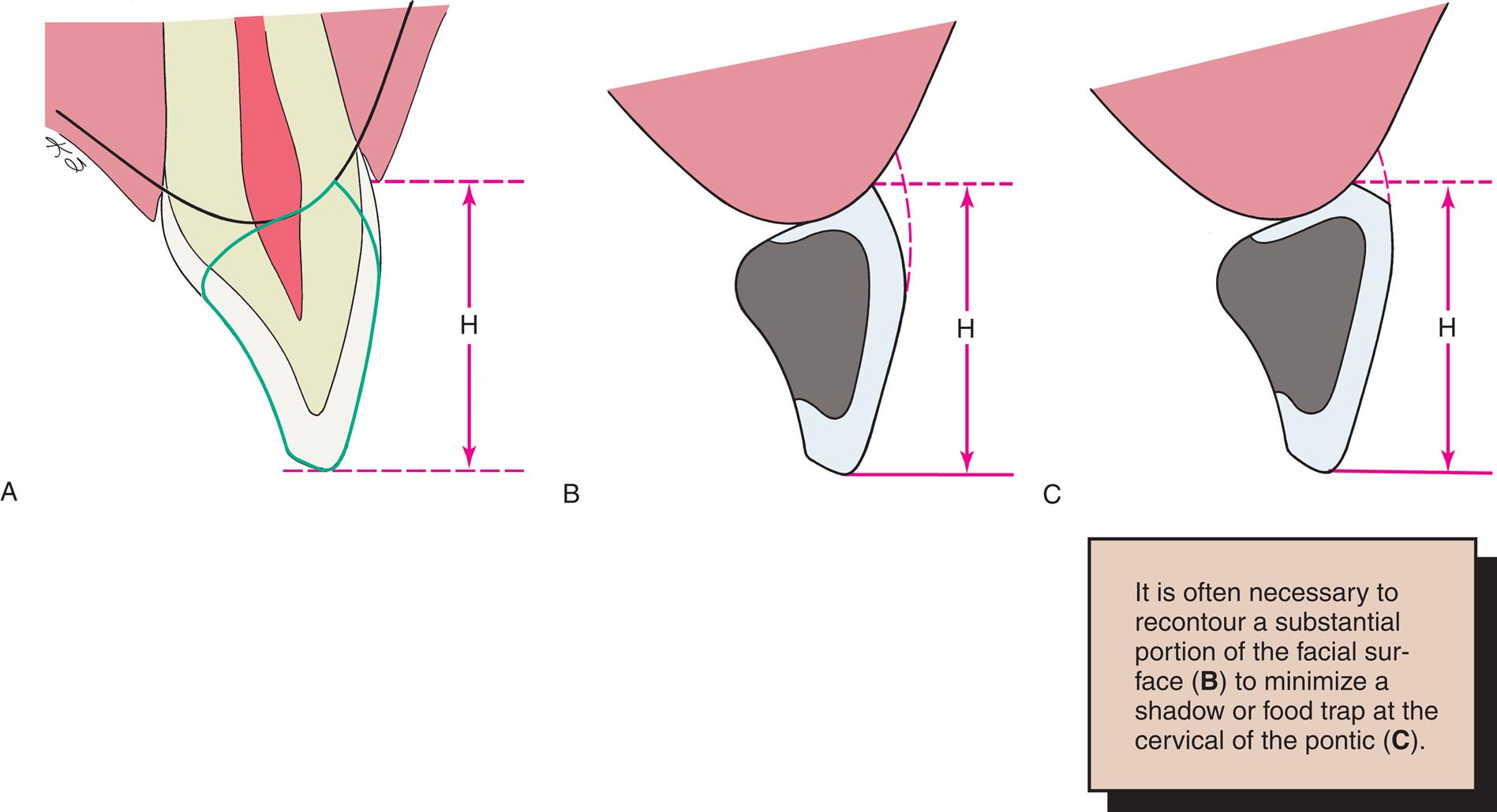
An esthetically successful pontic replicates the form, contours, incisal edge, gingival and incisal embrasures, and color of adjacent teeth. The pontic's simulation of a natural tooth is most often betrayed at the tissue-pontic junction. The greatest challenge in this situation is to compensate for anatomic changes that occur after extraction. To achieve a “natural” appearance, special attention should be paid to the contour of the labial surface as it approaches the tissue-pontic junction. This cannot be accomplished by mere duplication of the facial contour of the missing tooth; after a tooth is removed, the alveolar bone undergoes resorption, remodeling, or both. If the original tooth contour were followed, the pontic would look unnaturally long incisogingivally (Fig. 20.33). For an esthetic pontic to achieve the illusion of a natural tooth, observers must think that they are seeing a natural tooth.

The modified ridge-lap pontic is recommended for most anterior situations; it compensates for lost buccolingual width in the residual ridge by overlapping what remains. Rather than emerging from the crest of the ridge as a natural tooth would, the cervical aspect of the pontic sits in front of the ridge, covering any abnormal ridge structure that results from tooth loss. Fortunately, because most teeth are viewed from only two dimensions, this relationship remains undetected. A properly designed, modified ridge-lap pontic provides the required convexity on the tissue side with smooth and open embrasures on the lingual side for ease of cleaning. This is difficult to accomplish. Clinically, many pontics have suboptimal contour, resulting in an unnatural appearance. This can be avoided with careful preparation at the diagnostic waxing stage (see Chapter 3). Sometimes the ridge tissue must be surgically reshaped to enhance the result.
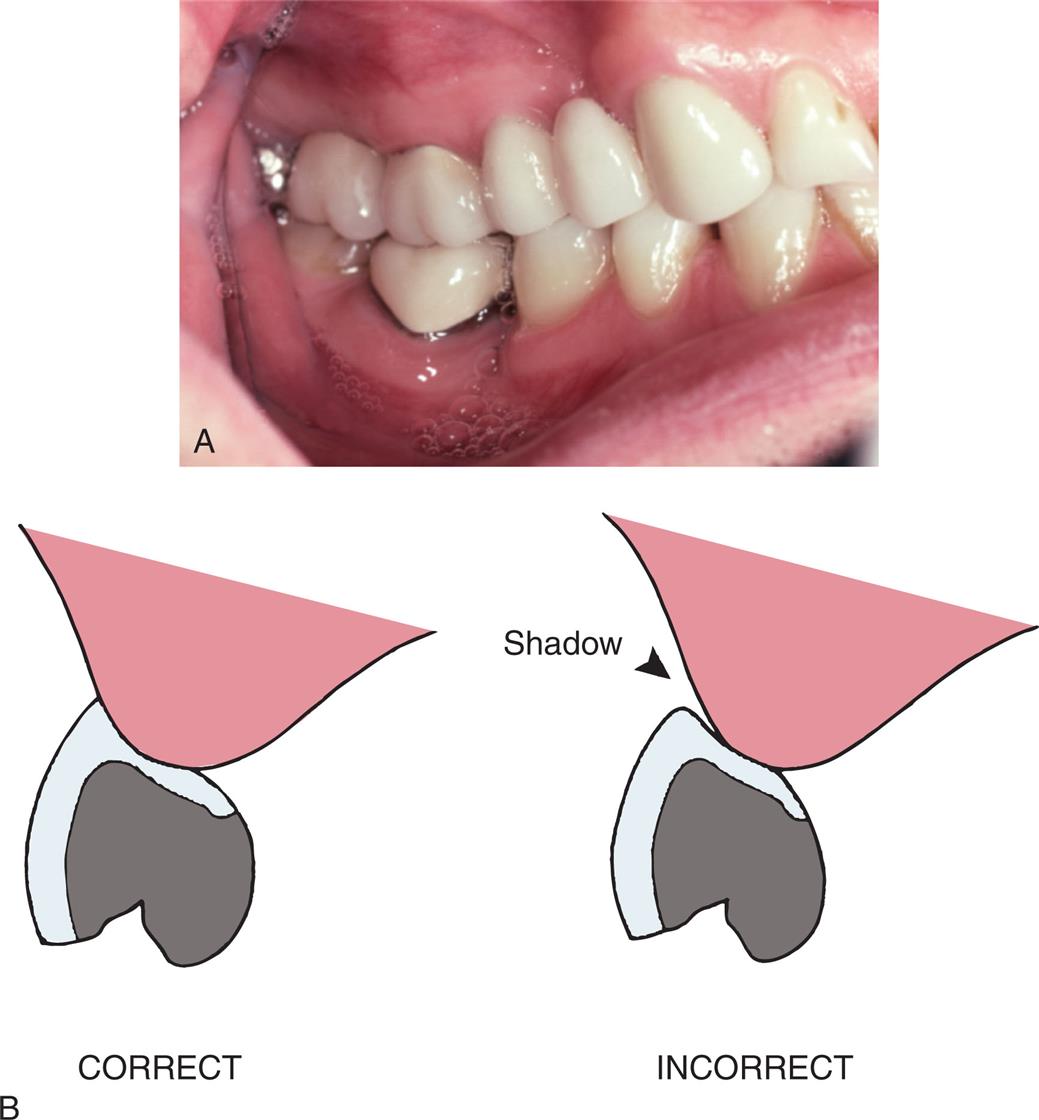
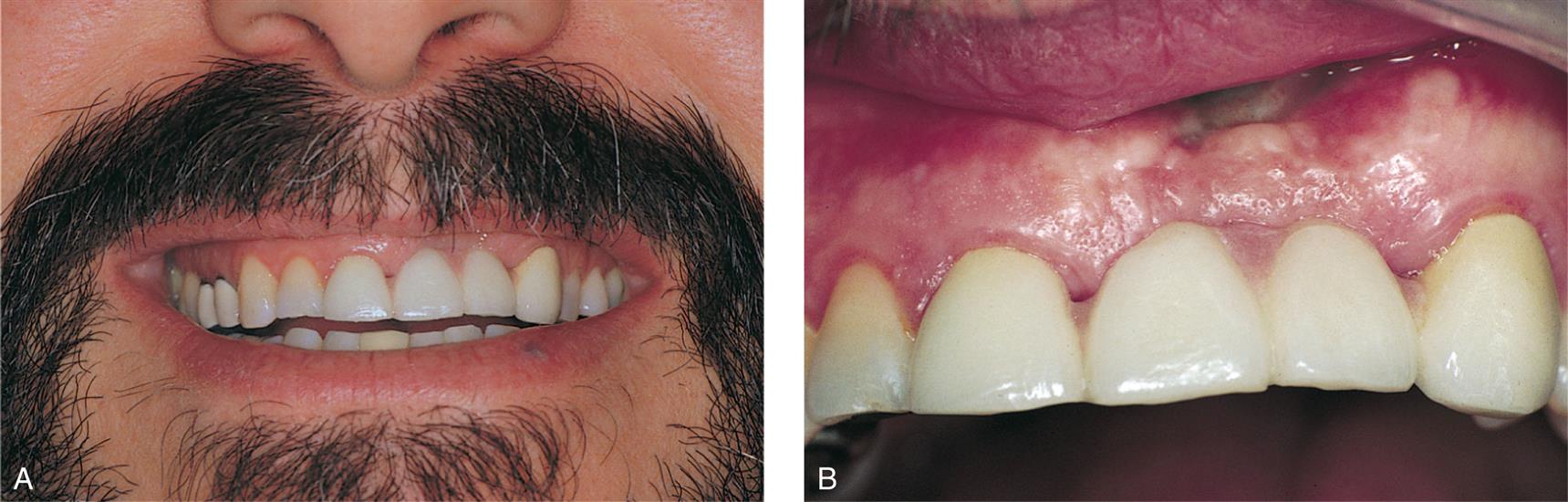
In normal situations light falls from above and an object's shadow is below it. Unexpected lighting or positioned shadows (Fig. 20.34) can be confusing to the brain. Because of past experience, the brain “knows” that a tooth grows out of the gingiva and it therefore “sees” a pontic as a tooth unless telltale shadows suggest otherwise. The dentist must carefully study where shadows fall around natural teeth, particularly around the gingival margin. If a pontic is poorly adapted to the residual ridge, an unnatural and odd-looking shadow exists in the cervical area and spoils the illusion of a natural tooth (Fig. 20.35). In addition, recesses at the pontic-gingival interface collect food debris, further ruining the illusion of a natural tooth.
When appearance is of utmost concern, the ovate pontic, used in conjunction with alveolar preservation or soft tissue ridge augmentation, can provide an appearance at the gingival interface that is virtually indistinguishable from that of a natural tooth. Because it emerges from a soft tissue recess, this pontic is not susceptible to many of the esthetic pitfalls applicable to the modified ridge-lap pontic. However, in most circumstances, the patient must be willing to undergo the additional surgical procedures that are necessary for placement of an ovate pontic.
Incisogingival Length
Correctly sizing a pontic simply by duplicating the original tooth is not possible. Ridge resorption makes such a pontic look too long in the cervical region. The height of a tooth is immediately obvious when the patient smiles and shows the gingival margin (Fig. 20.36). An abnormal labiolingual position or cervical contour is not immediately obvious. This fact can be used to produce a pontic of good appearance by recontouring the gingival half of the labial surface (see Fig. 20.35). The observer sees a normal tooth length but is unaware of the abnormal labial contour, meaning the illusion is successful.
Even with moderately severe bone resorption, obtaining a natural appearance by exaggerated contouring of the pontics may still be possible. In areas where tooth loss is accompanied by excessive loss of alveolar bone, however, a pontic of normal length would not touch the ridge at all.
One solution is to shape the pontic to simulate a normal crown and root with emphasis on the cementoenamel junction. The root can be stained to simulate exposed dentin (Fig. 20.37). Another approach is to use pink porcelain to simulate the gingival tissues (Fig. 20.38). However, such pontics then have considerably increased tissue contact and require scrupulous plaque control to achieve long-term success. Ridge augmentation procedures have been successful in correcting areas of limited resorption. When bone loss is severe, the esthetic result obtained with a removable partial denture is often better than that obtained with an FPD.
Mesiodistal Width
Frequently, the space available for a pontic is greater or smaller than the width of the contralateral tooth. This is usually because of uncontrolled tooth movement that occurred when a tooth was removed and not replaced.
If possible, such a discrepancy should be corrected by orthodontic treatment. If this is not possible, an acceptable appearance may be obtained by incorporating visual perception principles into the pontic design. In the same way that the brain can be confused into misinterpreting the relative sizes of shapes or lines because of an erroneous interpretation of perspective (Fig. 20.39), a pontic of abnormal size may be designed to give the illusion of being a more natural size. The width of an anterior tooth is usually identified by the relative positions of the mesiofacial and distofacial line angles, the overall shape by the detailed pattern of surface contour, and light reflection between these line angles. The features of the contralateral tooth (Fig. 20.40) should be duplicated as precisely as possible in the pontic and the space discrepancy can be compensated by alteration in the shape of the proximal areas. The retainers and the pontics can be proportioned to minimize the discrepancy. (This is another situation where a diagnostic waxing procedure helps solve a challenging restorative problem.)
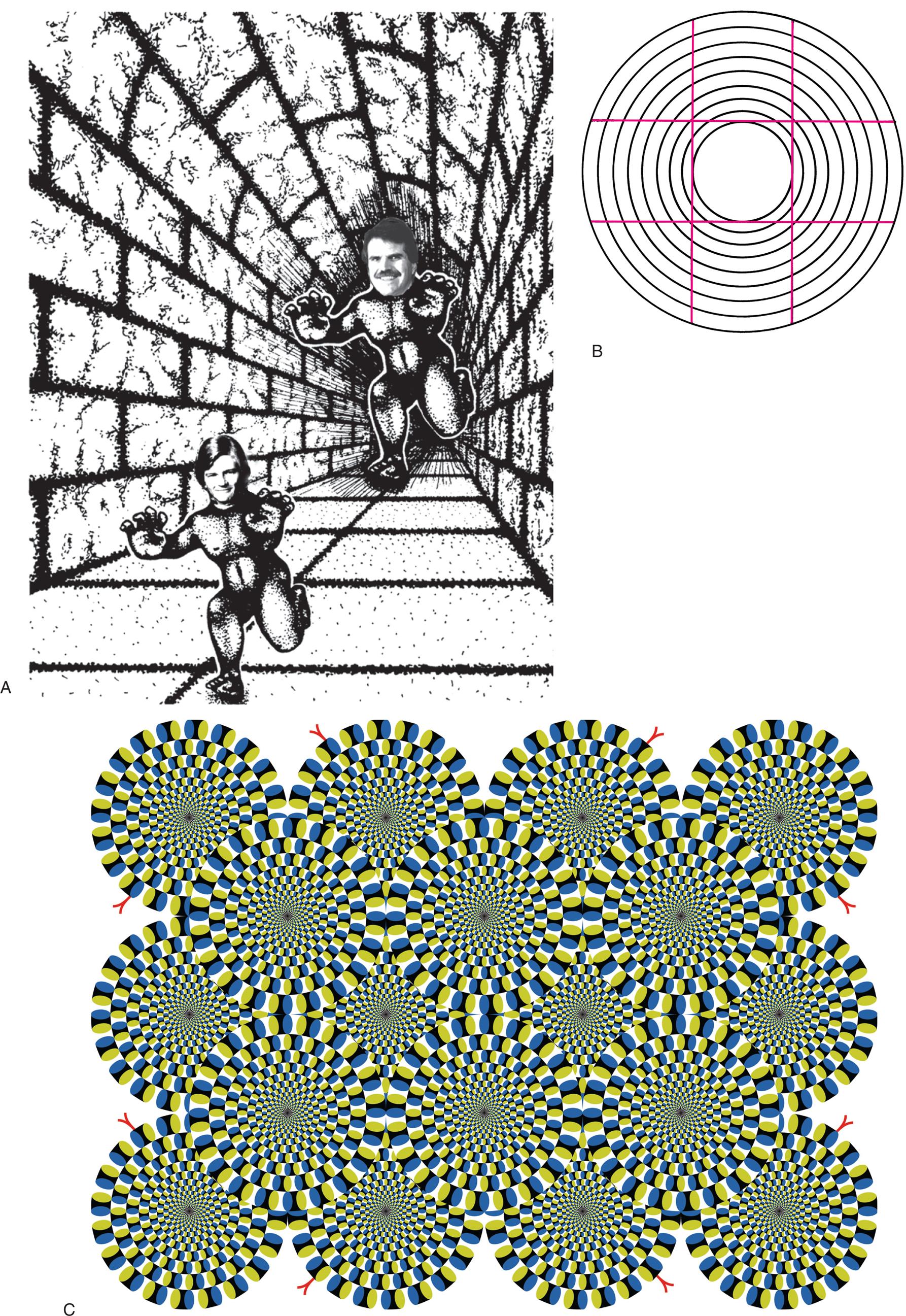
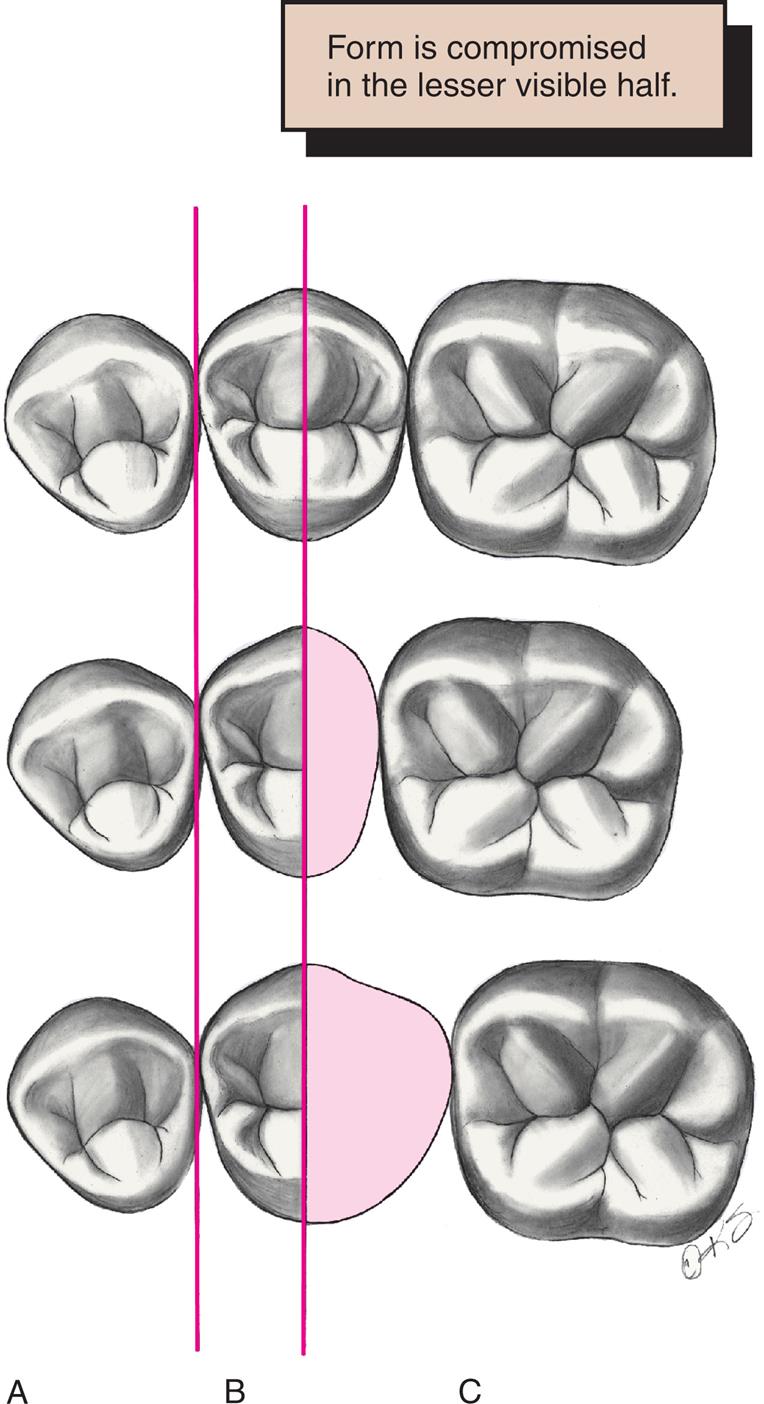
Space discrepancy presents less of a problem when posterior teeth are being replaced (Fig. 20.41) because their distal halves are not normally visible from the front. A discrepancy here can be managed by duplicating the visible mesial half of the tooth and adjusting the size of the distal half.
Pontic Fabrication
Available Materials
Over time, several techniques for pontic fabrication have evolved. Prefabricated porcelain facings were traditionally very popular for use with conventional gold alloys. As use of the metal-ceramic technique increased during the 1970s, prefabricated facings lost their popularity and essentially disappeared. Although custom-made, metal-ceramic facings were an acceptable substitute, they never gained widespread acceptance. The various techniques are summarized in Table 20.3 (Fig. 20.42).
Table 20.3
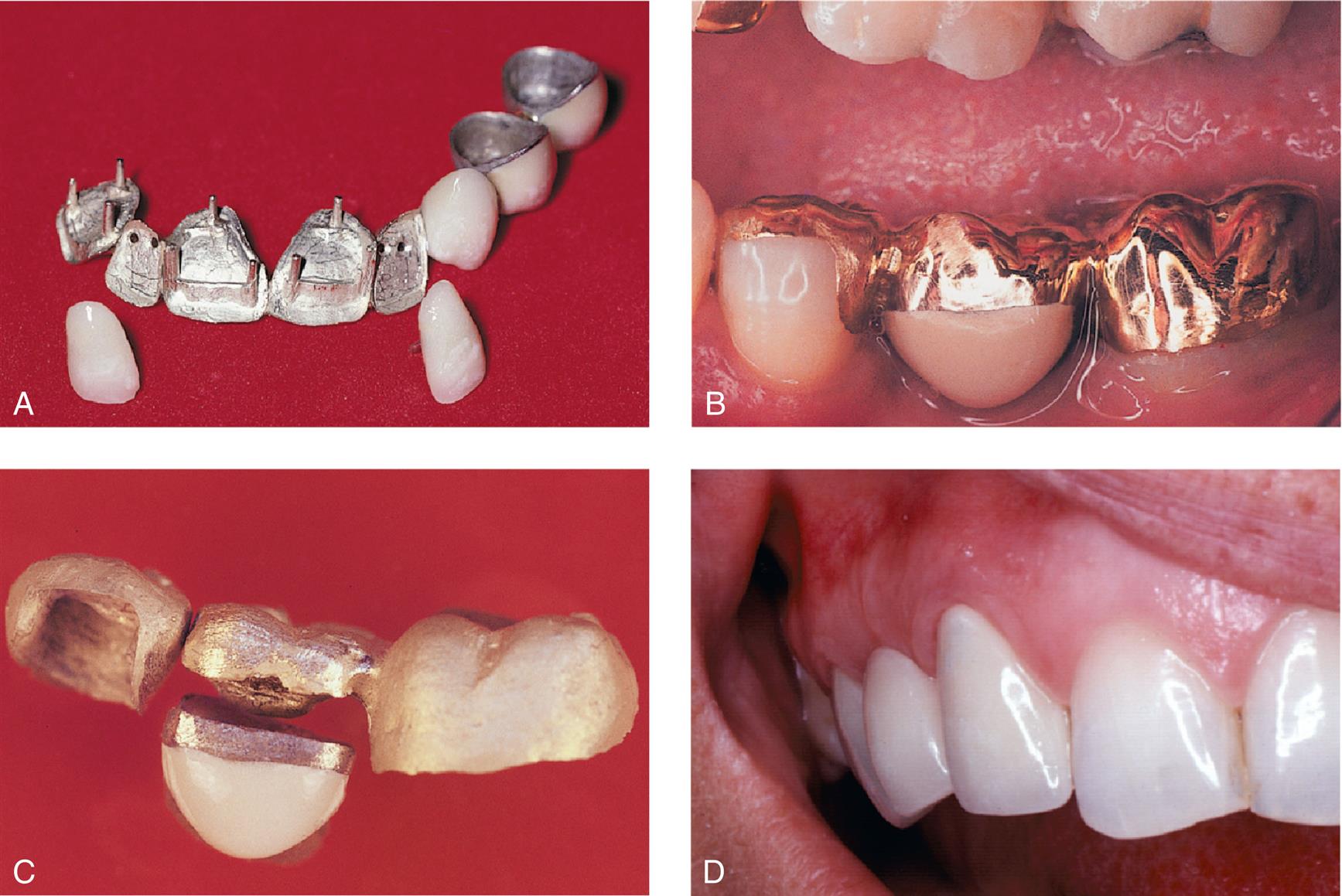
Most pontics are now made with metal-ceramic or zirconia, which provides the best solution to the biologic, mechanical, and esthetic challenges encountered in pontic design. Their fabrication, however, differs slightly from the fabrication of individual crowns. These differences are emphasized in the following paragraphs.
Metal-Ceramic Pontics
A well-designed, metal-ceramic pontic allows for easy plaque removal and has good strength, wear resistance, and esthetics (see Fig. 20.42D). Its fabrication is relatively simple if at least one retainer is also metal-ceramic. The metal framework for the pontic and one or both of its retainers is then cast in one piece. This facilitates pontic manipulation during the successive laboratory and clinical phases. In the following discussion, it is assumed that either one or both of the retainers are metal-ceramic, complete crowns. When this is not the case, an alternative approach is necessary.
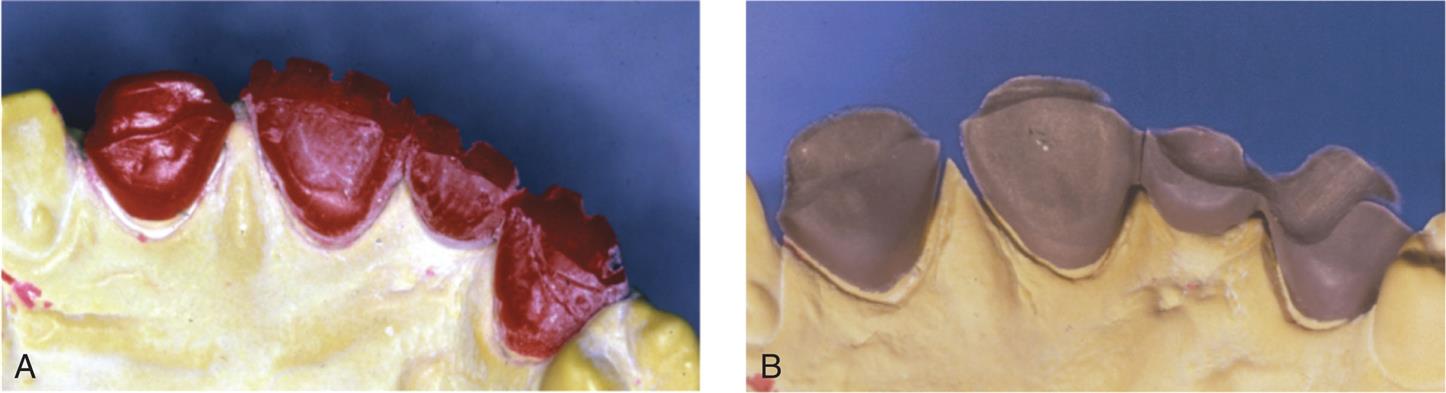
Anatomic Contour Waxing
For strength and esthetics, the thickness of porcelain must be controlled accurately in the finished restoration. To ensure this, a wax pattern is made to the final anatomic contour. This also enables the dentist to assess connector design adequacy and the relationship between the connectors and the proposed configuration of the ceramic veneer (see Chapter 27).
Armamentarium
The following equipment is needed (Fig. 20.43):

Step-by-step procedure
- 1. Wax the internal, proximal, and axial surfaces of the retainers as described in Chapter 18.
- 2. Soften the inlay wax, mold it to the approximate desired pontic shape, and adapt it to the ridge. This is the starting point for subsequent modification. An alternative (and perhaps preferable) method is to make an impression of the diagnostic waxing or interim restoration. Molten wax can then be poured into this to form the initial pontic shape. Prefabricated pontic shapes are also available (Fig. 20.44).
- 3. If a posterior tooth is being replaced, leave the occlusal surface flat because the occlusion is best developed with the wax addition technique outlined in Chapter 18.
- 4. Lute the pontic to the retainers and for additional stability, connect its cervical aspect directly to the definitive cast with sticky wax. Then wax the pontic to proper axial and occlusal (or incisal) contour (Fig. 20.45).
- 5. Complete the retainers and contour the proximal and tissue surfaces of the pontic for the desired tissue contact. The pontic is now ready for evaluation before cutback.

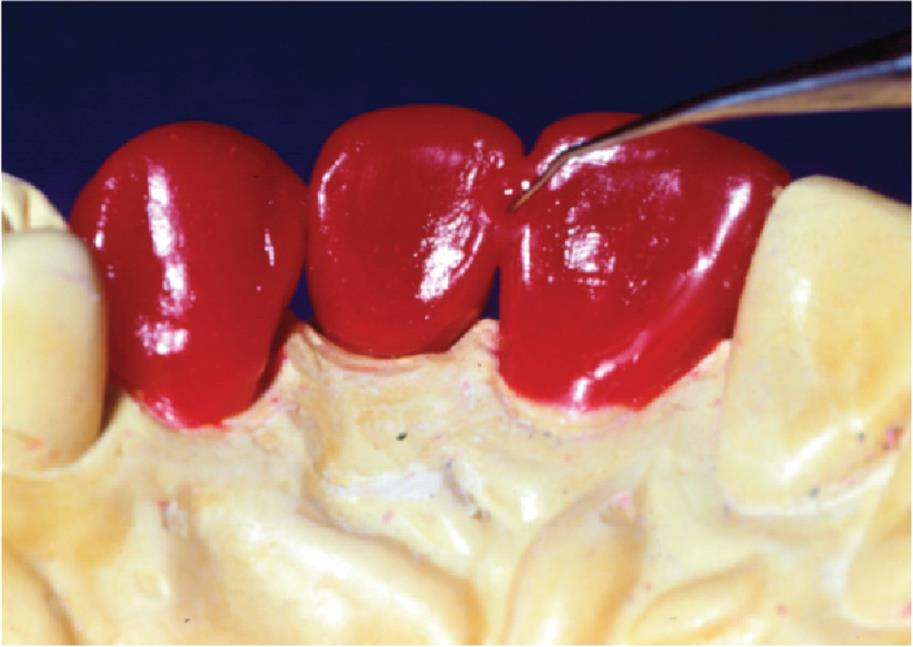
Evaluation
The form of the wax pattern is evaluated (Fig. 20.46), and any deficiencies are corrected. Particular attention is given to the connectors, which should have the correct shape and size. The connectors provide firm attachment for the pontic so that it does not separate from the retainers during the subsequent cutback procedure.

Cutback
Armamentarium
Step-by-step procedure
- 1. Use a sharp explorer to outline the area that will be veneered with porcelain (Fig. 20.47A). The porcelain-metal junction must be placed sufficiently lingually to ensure good esthetics.
- 2. Make depth cuts or grooves in the wax pattern (see Chapter 19 and Fig. 20.47B).
- 3. Complete the cutback as far as access allows with the units connected and on the definitive cast.
- 4. Section one wax connector with a thin ribbon saw (sewing thread is a suitable alternative) and remove the isolated retainer from the definitive cast (see Fig. 20.47C).
- 5. Finish the cutback of this retainer. Ensure there is a distinct 90-degree, porcelain-metal junction.
- 6. Reflow and finalize the margins. The pontic is held in position by the other retainer during this procedure.
- 7. Refine the pontic cutback where access is improved by removal of the first retainer.
- 8. Reseat the first retainer, reattach it to the pontic, section the other connector, and repeat the process.
- 9. Sprue the units and do any final reshaping as needed.
- 10. Invest and cast in the manner described in Chapter 22.
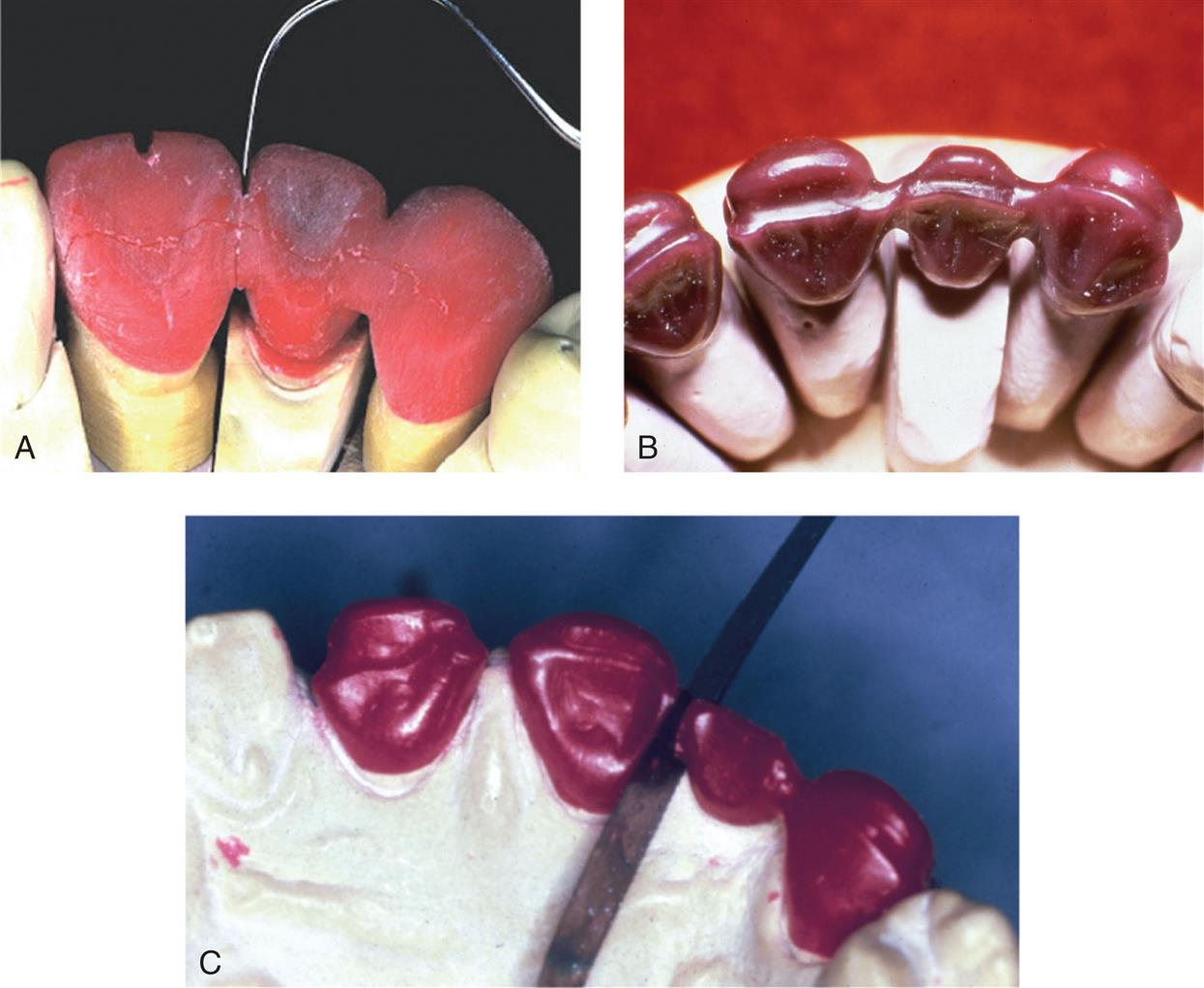
When one connector of a three-unit FPD is to be cast and the other soldered, the cast connector should be sectioned first when the foregoing procedure is followed. The gingival surface of the pontic should be cut back in the metal rather than in the wax because the tissue contact helps stabilize the pontic. Access is difficult and it is easy to break the fragile wax connector.
Metal Preparation
Armamentarium
Step-by-step procedure
- 1. Recover the castings from the investment and prepare the surfaces to be veneered as described in Chapter 19 (Fig. 20.48).
- 2. Finish the gingival surface of the pontic. Do not over reduce this area.

Evaluation
Less than 1 mm of porcelain thickness is needed on the gingival surface because once it is cemented the restoration is seen from the facial side, rather than from the gingival side. Excessive gingival porcelain is a common fault in pontic framework design and may lead to fracture and poor appearance (see Fig. 20.30).
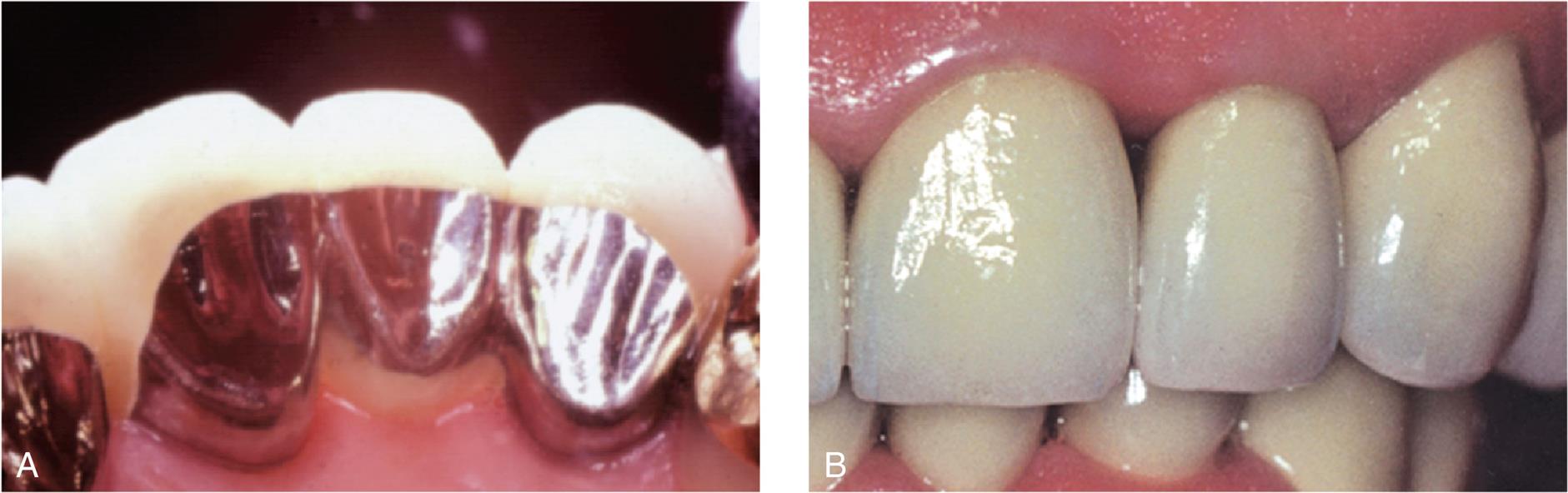
To facilitate plaque control, the metal-ceramic junction should be located lingually. Then tissue contact is on the porcelain and not on metal, which retains plaque more tenaciously.58
Porcelain Application
Many of the steps for porcelain application are identical to those in individual crown fabrication (see Chapter 24). There are some features peculiar to pontic fabrication, however, and these are emphasized.
Armamentarium
The following equipment is needed (Fig. 20.49):
- • Paper napkin
- • Glass slab
- • Tissues or gauze squares
- • Distilled water
- • Glass spatula
- • Serrated instrument
- • Porcelain tweezers or hemostat
- • Ceramist's brushes (No. 2, 4, or 6)
- • Whipping brush
- • Razor blade
- • Cyanoacrylate resin
- • Colored pencil
- • Articulating tape
- • Ceramic-bound stones
- • Diamond stones
- • Diamond disk

Step-by-step procedure
- 1. Prepare the metal and apply opaque as described in Chapter 24 (Fig. 20.50).
- 2. Apply cervical porcelain to the gingival surface of the pontic and seat the castings on the definitive cast. A small piece of tissue paper adapted to the residual ridge on the cast, moistened with a brush, prevents porcelain powder from sticking to the stone. (Cyanoacrylate resin or special separating agents can be used for the same purpose.)
- 3. Build up the porcelain (as described in Chapter 24) with the appropriate distribution of cervical, body, and incisal shades. The tissue paper acts as a matrix for the gingival surface of the pontic.
- 4. When the porcelain has been condensed, section between the units with a thin razor blade. This prevents the porcelain from pulling away from the framework as a result of firing shrinkage. A second application of porcelain is needed to correct any deficiencies caused by firing shrinkage. Such additions usually are needed proximally and gingivally on the pontic.
- 5. Apply a porcelain separating liquid (e.g., VITA Modisol, Vita Zahnfabrik 5; VITA North America, Yorba Linda, CA) to the stone ridge so that the additional gingival porcelain can be lifted directly from the cast as in the fabrication of a porcelain labial margin (see Chapter 24).
- 6. Mark the desired tissue contact and contour the gingival surface to create as convex a surface as possible. The pontic is now ready for clinical evaluation, soldering procedures, characterization, glazing, finishing, and polishing (see Chapters 27–29).
Evaluation
The porcelain on the tissue surface of the pontic should be as smooth as possible (Fig. 20.51). Pits and defects hamper plaque control and promote calculus formation. The metal framework must be highly polished with special care directed to the gingival embrasures (where access for plaque removal is more difficult).

Metal Pontics
Pontics made from metal (Fig. 20.52) require fewer laboratory steps and are therefore sometimes used for posterior FPDs. However, they have some disadvantages (e.g., their appearance). In addition, investing and casting must be done carefully because the mass of metal in the pontic is prone to porosity as the bulk increases. A porous pontic retains plaque and tarnishes and corrodes rapidly.
Zirconia Pontics
The number of materials available for fabrication of FPD has increased in the recent years.59 CAD-CAM technology has gained popularity due to the lower cost of materials and faster processing times, increasing the overall efficiency.60,61 Zirconia is one such material that is now being utilized for single and multi-unit FPDs on natural teeth and on dental implants. Although in the anterior zone, the zirconia FPDs may need to be veneered with feldspathic porcelain for superior esthetic results and to color match with the adjacent teeth. The fracture (chipping) of the porcelain layer in zirconia-porcelain restorations is one of the most commonly observed clinical complication,62,63 although improved laboratory processing with slow cooling has greatly reduced this complication.64
Zirconia pontics are digitally planned and designed. All traditional principles of pontic design should be strictly adhered to maintain adequate hygiene and strength. The restorations can be milled after capturing the tooth preparations with an intraoral scanner. The teeth preparations can also be recorded with an elastomeric impression material, which is then digitized with a laboratory scanner.
Armamentarium
Step-by-step procedure
- 1. Once you have an intra oral scan of the preparations, follow the steps on the software for designing the prosthesis.
- 2. Mark the finish lines on the screen. Most software auto-generate a proposed prosthesis design.
- 3. Verify the pontic design: the shape, size, width, and tissue contact. All the surfaces can be adjusted as per your preference.
- 4. Verify the occlusal contacts and increase or decrease the contact area.
- 5. Follow the consecutive steps on the design software. Once designing is complete, the software will send the file to the milling unit.
- 6. Screw in the block of zirconia in the milling unit and start the milling process.
- 7. Once the zirconia prosthesis is milled, it is still in the pre-sintered stage and appears much larger than the actual FPD.
- 8. Remove the FPD and grind the sprue with the help of a round tungsten carbide bur (No. 6 or 8).
- 9. Place the FPD in the furnace and let it sinter as per manufacturer’s instructions.
- 10. Once the sintering process is completed and the FPD has cooled, it is ready for insertion.
Pontics in Fixed Implant Restorations
Pontics for implant restorations is similar to natural teeth restorations and should serve four important purposes: function, esthetics, mechanical, and hygiene maintenance.6 The pontic design depends on many factors including the residual alveolar ridge anatomy with or without grafting. Developing adequate soft tissue contours under pontic spaces is somewhat challenging in resorbed or atrophic residual ridges and could lead to mechanical, esthetic, functional, and phonetic challenges. This may require addition of pink porcelain in severe situations to camouflage defects. Gingival tissue molding or manipulation around the pontic area would require at least 2 to 3 mm of attached gingiva thickness for compressibility.38 If the gingival thickness is less than 1 mm, alveolar bone ridge reduction will be necessary to gain space, and also to preserve the residual alveolar ridge anatomy and interproximal papilla after extraction. Typically, esthetic implant restorations are restored immediately with interim restorations. The architecture of the pontic provides support and shapes the soft tissue during the healing process. It also prevents loss of interproximal papilla, leading to a dark interproximal space appearance called ‘black triangle.’
Intimate contact between the pontic and the gingival tissue has to be evaluated before definitive insertion of the prosthesis. The pontic will exert some amount of pressure on the tissues but the ischemia (blanching) should disappear in 3 to 5 minutes. If the tissues continue to be blanched and displaced for prolonged periods of time, the prosthesis should be removed and adjusted for tissue contact under the pontic. Low viscosity elastomeric disclosing agents can be useful for accessing tissue contact, displacement, and patient comfort.
A thin layer of the disclosing agent is placed on the undersurface of the pontic. The prosthesis is seated intraorally and the screws are tightened until there is resistance. Patient discomfort may prevent the complete seating of the prosthesis. After the material has set, it is evaluated for any areas that have completely been wiped. Those heavy contact areas are adjusted with a diamond rotary instrument until the soft tissue ischemia is reduced and the prosthesis is seated completely.
Summary
Designs that allow easy plaque control are especially important to the long-term success of a pontic. Minimizing tissue contact by maximizing the convexity of the pontic's gingival surface is essential. Special consideration is also needed to create a design that combines easy maintenance, natural appearance, and adequate mechanical strength. When the appropriate design has been selected, it must be accurately conveyed to the dental technician.
There are subtle differences between metal-ceramic pontic fabrication and the fabrication of other types of pontics. Under most circumstances, the metal-ceramic technique is used because it is straightforward and practical. However, it requires careful execution for maximum strength, esthetic appearance, and effective plaque control. Alternative procedures are sometimes helpful, particularly when gold alloys are used for the retainers. Resin-veneered pontics should be restricted to use as longer-term interim restorations and metal pontics may be the restoration of choice in non-esthetic situations, particularly those in which forces are high. Zirconia pontics can be used in esthetic and non-esthetic areas because of their high strength and esthetic properties. Every material has some limitations and the decision of the choice of pontic material should be based on each individual clinical scenario.
Study Questions
- 1. Outline and discuss a logical classification of pontics.
- 2. How does pontic design change as a function of location in the dental arch?
- 3. What are the materials available for pontic fabrication? What are their respective advantages, disadvantages, indications, and contraindications?
- 4. Discuss the factors that govern the shaping of the facial and lingual surfaces of a modified ridge-lap pontic.
- 5. What common clinical problems might be encountered if a pontic is improperly shaped or fabricated?
- 6. Discuss the various techniques for soft tissue augmentation and the residual ridge defects that these techniques are designed to resolve.
- 7. What factors should be considered in the selection of the pontic material that will be in contact with the residual ridge?