Mental Health Assessment Skills
http://evolve.elsevier.com/Morrison-Valfre/
Upon completion of this chapter, the student will be able to:
- 1. Identify two purposes of the mental health treatment plan.
- 2. List and define each step of the nursing process.
- 3. Describe three methods of data collection.
- 4. List six parts of a holistic nursing assessment.
- 5. Identify four guidelines for conducting effective psychiatric interviews.
- 6. Explain the importance of performing physical assessments of clients with psychiatric diagnoses.
- 7. Explain the purpose of the mental status examination.
- 8. List the five general categories of the mental status examination.
- 9. Describe the process for conducting a mental status examination.
Key Terms
affect (ĀF-ĕkt) (p. 98)
assessment (ă-SĔS-mĕnt) (p. 94)
calculation (KĂL-kyū-LĀ-shŭn) (p. 100)
clinical judgment model (p. 94)
data collection (DĀ-tă kă-lĕc-shŭn) (p. 94)
depersonalization (p. 99)
insight (p. 100)
interview (ĬN-tәr-vyū) (p. 94)
judgment (JŬDJ-mĕnt) (p. 100)
memory (MĔM-ŏr-ē) (p. 100)
mood (p. 98)
nursing (therapeutic) process (NŬR-sĭng PRŎ-sĕs) (p. 93)
perceptions (pĕr-CĔP-shŭns) (p. 98)
risk factor assessment (p. 95)
sensorium (sĕn-SŌ-rē-ŭm) (p. 99)
thought content (p. 99)
thought processes (p. 99)
Good assessment skills are critical to quality health care. The ability to effectively obtain and use information about clients is a vital part of the multidisciplinary treatment plan and the foundation of the nursing (therapeutic) process. Caregivers must first learn about the person before they can provide personalized care or judge the effectiveness of any therapeutic action. Uncovering clients’ problems requires critical thinking abilities and exceptional assessment skills. Therapeutic communications, interactions, and assessment skills help care providers learn about all aspects of their clients. This chapter provides the starting point for making thorough mental health assessments.
Mental Health Treatment Plan
People enter the health care system because they are distressed, disabled, or suffering. The diagnosis and treatment of people with mental health problems is challenging because diagnoses of mental illness are not as easily identified and defined as physical disorders. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), “no definition adequately specifies precise boundaries for the concept of mental disorder” (American Psychiatric Association, 2013). The relationship between the physical and psychological self is such that the two are difficult to separate. It is important to remember, however, that every psychological problem has physical effects, and each physical illness has psychological effects. The wise care provider is aware of both.
When individuals first enter the mental health care system, ideally they undergo a comprehensive assessment. Clients are interviewed by several members of the multidisciplinary health care team. Physical and psychological diagnostic testing is performed, and data (information) are gathered from as many sources as possible. The physician provides information regarding the client’s physical state and need for medications. The social worker assesses the client’s family, work, and social interactions. The dietitian learns about the client’s nutritional status. The psychiatrist and psychologist explore the client’s emotional and cognitive (intellectual) functioning. The nurse assesses how the illness or disability affects the client’s activities of daily living. Other care providers contribute information through their observations and interactions with the client.
Team members then meet to compare data, identify problems, and develop treatment approaches. When the team and the client agree on the treatment goals, a course of action is planned. Usually medical treatments (medications) are combined with psychotherapies, behavioral therapies, and other therapeutic actions. The overall treatment plan is then developed for the individual client. Therapeutic actions are implemented, and the client’s progress toward each goal is evaluated.
The mental health treatment plan serves several purposes. First, it is a guide for planning and implementing client care. Nurses are guided by the treatment plan when they develop specific nursing care plans. Psychologists, social workers, and other therapists use the treatment plan as a framework for implementing their specialized therapeutic actions.
Second, the plan serves as a vehicle for monitoring the client’s progress and the effectiveness of therapeutic interventions. Clients meet often with treatment team members to discuss problems and attempts to meet their goals. Therapeutic interventions are evaluated, and the treatment plan is revised to include new information.
Third, the mental health treatment plan serves as a means for communicating and coordinating client care. The plan prevents costly duplication of services and provides a focus for all therapeutic activities, regardless of specialty. This increases the effectiveness of each team member’s efforts. Developing the mental health treatment plan is not a complex process, but it is a dynamic, changing as the client progresses. Using the treatment plan allows clients and care providers the opportunity to work together to meet client goals.
DSM-5 Diagnosis
Therapists who work with mentally or emotionally troubled individuals often use the fifth edition of the DSM, DSM-5, to aid in diagnosis and help guide clinical practice. One of the tools used in the DSM-5 is the World Health Organization’s Disability Assessment Tool (WHODAS 2.0; Table 9.1). The diagnosis of mental health problems remains the responsibility of the physician, but nurses and other care providers should be familiar with the multiaxial system of psychiatric assessment. Several tools are available for assessing mental status. One example of a mental health assessment tool is seen in Appendix A.
Table 9.1
Nursing (Therapeutic) Process
Each step of the nursing (therapeutic) process is designed to support goal-directed care for clients (Stuart, 2014). The process is an organizational framework for effective care and consists of five steps: assessment, diagnosis, planning, intervention, and evaluation. Using this process encourages us to focus on the client and develop appropriate and effective care.
The first step, assessment, is the data collection step. Bits of information relating to the client are collected from every possible source. Medical records are reviewed, a history is obtained, and observations are made; discussions with family members or friends add to the database. Soon a picture of the client begins to emerge. Using the mass of collected information as a database, care providers plan care based on the needs, abilities, preferences, and concerns of the client.
Next, data are organized into related areas, and problems are identified. Each problem is then examined in detail, and problem statements and nursing diagnoses are developed. (Medical diagnoses and interventions relate to the client’s physical or mental dysfunctions; nursing diagnoses and interventions focus on how the client’s problems affect his or her ability to carry out the activities of daily living.) Client needs are also considered when problem statements are being developed.
During the planning phase, specific short-term and long-term goals are developed. The outcome of each problem is projected by identifying behaviors that would indicate the problem is solved. These “expected outcomes” are then used to monitor the client’s progress. Therapeutic actions (interventions) are planned using goals and expected outcomes. Then a written care plan is developed.
The intervention phase includes the actual delivery of the planned actions. Therapeutic interventions, carried out by all mental health care team members, guide clients toward their goals. Client responses to each intervention are monitored. Work to keep an open mind when observing the client’s responses to care, and remember that many reactions are culturally determined.
The final phase of the process, evaluation, determines the effectiveness of care. By comparing expected outcomes with actual results, care providers are able to note which actions met the goals and which did not. Those actions that did not meet their goals are reassessed, and the process is begun again.
The clinical judgment model is another way of establishing and supporting goal-directed care. It includes critical thinking and reasoning skills. The use of the clinical judgment model involves these skills: processing information allows the nurse to identify important cues about the client’s condition. Thinking critically helps the nurse recognize relevant data, prioritize concerns, and choose the best course of action. Using problem-solving skills and applying relevant knowledge encourage the nurse to reflect on the situation and evaluate the evidence for planning safe and effective care.
To develop good clinical judgment, a nurse uses six skills. To recognize cues, the nurse determines which data are of immediate concern and what is relevant or irrelevant. To analyze cues, the client’s history and situation are considered in relation to the assessed information. All possible issues relating to the client are determined when the nurse prioritizes hypotheses. The desired outcomes of care are identified and specific actions are planned in the generate solutions phase. During the take action phase, the nurse delivers care, provides health education, and works with other health care providers to improve the client’s condition. Last, the evaluate outcomes phase compares the client’s actual outcomes with expected outcomes of care. If the client’s condition does not change, or it declines, the nurse must decide which nursing actions are ineffective or made no difference and repeat the process.
Clients are involved as partners in care. Although some individuals are unable or too discouraged to make decisions, most are capable of participating in some part of their care. Caregivers help clients problem-solve by involving them in the care planning process. Evaluation of both clients’ and caregivers’ actions allows for adjustments in the dynamic process known as “treatment.” Use of the nursing (therapeutic) process and clinical judgment model requires knowledge, experience, and the practice of good judgment. Experience grows with each application of the process, and sound judgment is gained by looking at every possible side of a problem before arriving at a decision. The nursing (therapeutic) process serves as a tool for defining and solving client problems, but the tool is only as effective as the practitioner. The art of choosing the best course of action must be carefully practiced. Let the “do no harm” principle guide you as you grow.
About Assessment
Assessment includes the “gathering, verifying and communicating of information relative to the client” (Mosby’s Dictionary, 2016). Clients are dynamic (changing) individuals affected by more than an illness or disorder. For this reason, the holistic assessment includes gathering information about the physical, intellectual, emotional, social, cultural, and spiritual aspects of each client. The more complete the picture, the more effective the treatment approaches will be.
The process of assessing clients is ongoing. It begins with the client’s admission to the facility or service and ends only after his or her relationship with the health care system is over. To gain an understanding of clients, become observant and alert for any information that may have an effect on care.
Data Collection
Data (information) relating to clients are grouped into objective and subjective categories. Objective data are information that can be measured and shared, and they are gathered through the senses of sight, smell, touch, and hearing. Blood pressure readings, pulse rates, and laboratory reports that are compared with “normal” results are examples of objective data. When working with mental health clients, care providers obtain objective data through physical examinations, daily assessments, diagnostic testing results, and repeated observations of behaviors (Potter and Perry, 2017).
Subjective data relate to clients’ perceptions. They include information that is abstract and difficult to measure or share. For example, the experiences of pain, nausea, and anxiety cannot be measured by anyone but the individual experiencing them. Emotions and mental states are all subjective and difficult to measure. As a result, it is extremely important to document subjective information as descriptively and accurately as possible. Do not include interpretive statements (judgments). Document client reactions and behaviors in exact terms. To say that the client is angry (unless he states that he is angry) is an interpretive statement or judgment; it is better to state that the client was pacing about the room while slamming his fist into the wall and swearing. When documenting subjective data, quote the client as much as possible. Subjective information is collected during the initial health history interview and during every interaction with the client. The simple question “How do you feel?” can elicit much subjective information.
The term data collection refers to a variety of activities designed to gather information about a certain subject. Data-collecting methods for care providers include interviews, observational techniques, and rating scales and inventories. An interview is a meeting of people with the purpose of obtaining or exchanging information (Keltner and Steele, 2019). Interviews can be formal and highly structured, or informal and casual. Information gathered from formal interviews is usually documented on a standardized form. The interview is an excellent method for obtaining information and it serves as the starting point for building the therapeutic relationship. Informal interviews usually occur casually and provide great opportunities to learn more about clients and their families. Caregivers use informal interview techniques when they investigate client problems or explore certain topics.
Data-gathering through observational techniques is commonly used. Observation is the process of purposeful looking. When using observation as a data-gathering technique, caregivers must take care to be objective; personal bias or attitudes can alter one’s perceptions and affect the objectivity of the observations. The use of observation is an excellent method for gathering information when the caregiver can remain impartial and does not pass judgment.
Physical assessment skills are important to the data-gathering process. They are used to gather data, investigate changes in physical conditions, and evaluate the effectiveness of therapeutic interventions. Physical examination skills are special methods for obtaining information about the body’s functioning. The technique of observation is called inspection, which means a purposeful examination of the body. The skills of auscultation and percussion use the examiner’s sense of hearing to detect sounds within the body. Finally, the technique of palpation requires the sense of touch to draw out information about temperature, texture, and pulsations of the body.
Social workers, psychologists, and other therapists frequently use rating scales and inventories. These are data-gathering tools specifically designed to bring out certain kinds of information. The results are then compared with standardized measurements. Rating scales and inventories can be very useful for focusing on specific aspects of client problems.
Assessment Process
Holistic Assessment
The physical, social, cultural, intellectual, emotional, and spiritual areas of an individual’s life each have an effect on their health. Without knowledge of these six aspects, health care providers become narrowed and limited in their effectiveness. The holistic assessment for those who work with mentally or emotionally troubled clients is the same as that used by caregivers in any setting. In psychiatric treatment situations, however, the emphasis is on mental-emotional functioning. The psychiatric assessment tool focuses on obtaining data about the problems, coping behaviors, and resources of clients (Table 9.2). Information collected from assessment activities serves as part of the database from which medical, nursing, and other treatment decisions are made. An additional risk factor assessment is required for clients who may pose a risk for violence toward themselves or others.
Table 9.2
Modified from Stuart GW: Principles and practice of psychiatric nursing, ed 10, St Louis, 2013, Elsevier.
Risk Factor Assessment
A risk factor assessment helps “formulate a nursing diagnosis based on the identification of risk factors that potentially present an immediate threat to the patient” (Stuart, 2014) or others in the vicinity. With this assessment tool, five areas of potential risk for harm are identified (Box 9.1). Positive findings lead to more specific assessments and appropriate safety precautions. A registered nurse completes the risk factor assessment, but other health care providers assist by gathering important information and making objective observations.
The Health History
Each client is interviewed on admission to the health care service. The purpose of the history interview is to obtain data about the unique individual who is the client. It offers care providers an opportunity to introduce themselves and serves as a starting point for establishing the therapeutic relationship. During the interview, insight into client concerns, worries, and expectations is gained and there is the opportunity to obtain clues that may require further investigation. When used appropriately, the interview is a powerful method for gathering important information and establishing the therapeutic relationship.
Effective Interviews
The success of any client interview rests on the caregiver’s ability to listen objectively and respond appropriately. To enhance your interviewing skills, follow these guidelines:
- • Remember that personal values must not cloud professional judgments. Reacting to a client’s personal appearance or behaviors can stereotype him or her and have a negative impact on the effectiveness of the therapeutic relationship.
- • Do not make assumptions about how you think the client feels. Discover what each event means to the client and how he or she views the situation. The experience of losing a loved one, for example, depends on how an individual interprets or perceives an event.
- • Always consider the client’s cultural and religious values and beliefs. With mental health clients, this point cannot be emphasized enough. Caregivers must learn about their clients’ cultures if they are to understand their points of view. With clients from unfamiliar cultures, it is wise to research information about the culture and its religious practices before conducting the interview.
- • Pay particular attention to nonverbal communications. Much can be learned if one is observant. Note which subjects are avoided or quickly passed over during the interview. These behaviors can be clues that indicate a need for further investigation. Observing methods of self-expression helps the caregiver to focus on the client’s unspoken signals and the messages they communicate.
- • Have clearly set goals. Know the purpose of the interview. Is this an initial assessment interview or an investigation of a specific condition? The assessment interview is not a random discussion; it is a purposefully planned interaction with the client.
- • Monitor your own reactions during the interview. Use self-awareness to signal when you are becoming too emotionally involved; a caregiver may identify with certain clients who have similar interests or situations. Self-awareness allows one to understand the emotional responses generated by certain clients. Interviewing skills are used throughout the nursing (therapeutic) process. Work to develop and refine your interviewing skills because they are important tools.
Sociocultural Assessment
The health history includes information about both the physical and psychological functions of an individual. The sociocultural assessment focuses on the cultural, social, and spiritual aspects of an individual. During the history interview, the care provider obtains information about a client’s background and observes his or her appearance, behaviors, and attitudes (these are also included in the mental status examination).
The sociocultural assessment focuses on six areas; clients are asked questions about their age, ethnicity (culture), gender, education, income, and belief system. Risk factors and stressors are also defined during the sociocultural assessment (National Depressive and Manic-Depressive Association, 2014). This information helps care providers develop accurate and appropriate plans of care.
Review of Systems
The holistic assessment also includes a review of each body system and its functioning. Clients are first questioned about their general health care, past illnesses and hospitalizations, and family health history. Questions then focus on the function of each body system. Last, the lifestyle and activities of daily living are assessed. Box 9.2 lists the topics covered by the health history for clients with mental health problems. Data obtained from the health history, physical assessments, and various diagnostic examinations all help complete the picture of each individual client.
Physical Assessment
Clients receive a physical examination on admission to a psychiatric service. The purpose of the examination is to discover physical problems that can be treated medically. Many alterations in behavior are often traced to a physical cause. For example, low blood sugar levels can result in confused and uncooperative behavior. Hormone imbalances, exposure to toxic substances, and severe pain can also affect behavior.
A complete physical examination is performed by a physician or nurse practitioner. The client’s current health status is explored, and then each system is examined. Nurses have an obligation to assess each client’s health status on a routine basis. A complete physical assessment is not needed every day, but nurses must be alert to changes in their clients’ conditions. Most nurses use a systems approach or head-to-toe assessment. Both take less than 5 minutes and can be performed whenever information about physical functions is needed.
Diagnostic studies for clients with mental-emotional problems include standard blood and urine tests, evaluation of electrolytes, and hormone function examinations. Many clients are screened for tuberculosis, HIV, and sexually transmitted diseases. Studies such as x-ray examinations, electrocardiograms (ECGs), electroencephalograms (EEGs), and brain imaging studies (computed tomography [CT], magnetic resonance imaging [MRI], positron emission tomography [PET] scans) may be ordered. To complete the picture, the client’s current mental and emotional state is assessed via a mental status examination.
Mental Status Assessment
The mental status examination allows care providers to observe and describe a client’s behavior in an objective, nonjudgmental way. It is a tool for assessing mental health dysfunctions and identifying the causes of clients’ problems. Understanding each part of the examination enables care providers to plan and deliver the most appropriate care for each client.
The mental status examination explores five areas: general description, emotional state, experiences, thinking, and sensorium and cognition (Table 9.3).
Table 9.3
From Stuart GW: Handbook of psychiatric nursing, ed 7, St Louis, 2012, Elsevier.
General Description
Under the category of general description, the client’s general appearance, speech, motor activity, and behavior during the interaction are assessed. This category includes everything that can be readily observed about a client, such as physical characteristics, dress, facial expressions, motor activity, speech, and reactions. To assess a client’s physical characteristics, observe each part of the client’s body, noting anything unusual. Describe the person’s build, skin coloring, cleanliness, and manner of dress. Does the person appear neat and tidy or careless and unkempt? Note any body odors. If cosmetics are used, are they appropriately applied? Does the client’s appearance match his or her gender, age, and situation? People with depression, for example, may look unkempt and neglected and it is not uncommon for manic clients to dress in colorful but bizarre clothing and wear a lot of cosmetics and jewelry. Document all findings. Note the client’s facial expressions and use of eye contact; do the facial expressions match his or her emotions and actions? Is eye contact avoided or held for long periods? Also note the size of the client’s pupils; large, dilated pupils are seen in people with certain drug intoxications, whereas small pupils are associated with narcotic use.
Describe the rate, volume, and characteristics of the client’s speech. Note any abnormal speech patterns (see Chapter 10).
Next, turn your attention to the client’s motor activity, gestures, and posture. Observe the client’s physical movements for the level and type of activity, and note any unusual movements or mannerisms. Is the client agitated, tense, restless, lethargic, or relaxed? Are there any tics, grimaces, repeated facial expressions, or tremors? Excessive body movements are seen in individuals with anxiety or mania; they can also result from the use of stimulants or other drugs. Repeated movements or behaviors are seen in clients with obsessive-compulsive disorders, and picking at one’s clothing is often seen in clients with delirium or toxic reactions.
To complete the general description, assess the client’s behavior during the interaction. How did the client relate to you? Was he or she cooperative, hostile, or overly friendly? Did the client appear to trust you? Note whether the verbal messages matched the behaviors. Clients who use unconnected gestures, for example, may be hallucinating.
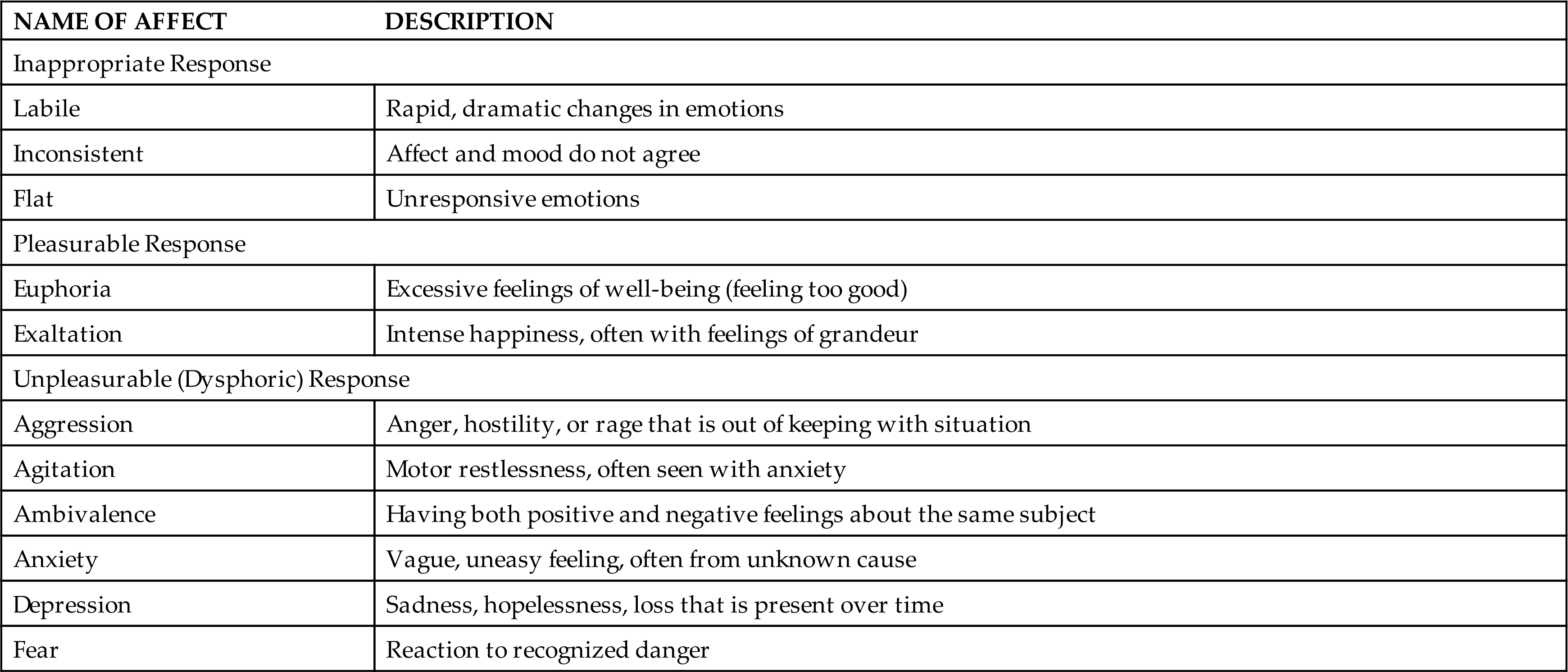
Emotional State
To assess the client’s emotional state, the care provider considers the client’s mood and affect. Mood is defined as an individual’s overall feelings; it is a subjective factor that can be explained only by the person experiencing it. Usually, people will have a basic mood, although it may change during the day. To illustrate: a basically relaxed and happy person may feel disappointed by an incident during the day but soon forgets and returns to his or her usual happy mood. A person’s mood can range from overwhelming sadness to great elation and joy. These variations are referred to as one’s range of emotion. Affect is the client’s emotional display of the mood being experienced. Table 9.4 explains several kinds of affect. Affect can be categorized as appropriate, inappropriate, pleasurable, or unpleasurable. To assess a client’s affect, ask what he or she is feeling and then observe the reactions. Do the responses to your questions match the subjects being discussed? Is the client overreacting, not reacting at all, or responding inappropriately? Document objective descriptions of the client’s behaviors. Descriptions communicate much more information than does a single medical term.
Table 9.4
Experiences
The category of experiences explores the client’s perceptions, the ways in which he or she experiences the world. An individual’s perceptions are often called one’s frame of reference. In short, a person’s perceptions help determine his or her sense of reality.
People who are having mental health problems may have difficulty in perceiving the same reality as the rest of society. Hallucinations are perceptions that have no external stimulus. The client may hear voices or see things that are not perceived by other people. Hallucinations involving taste, touch, or smell may indicate a physical problem. Visual and auditory hallucinations are associated with schizophrenia, the acute stage of alcohol or drug withdrawal, and organic brain disorders. Alterations in perceptions that have a basis in reality are called illusions. External stimuli are present, but the client perceives them differently, for example, a client who perceives the person walking down the hall as a wolf. If a client is having illusions or hallucinations, ask him or her to describe the experience. Box 9.3 lists several questions that can help explain the client’s experience.
Remember that hallucinations or illusions are very real to the person experiencing them. Caregivers cannot “talk them out of it” or tell them to ignore what they perceive. However, because they are so real, clients usually are willing to describe them when asked.
Thinking
The “thinking” section of the mental status examination focuses on thought content and processes. Thought content relates to what an individual is thinking. Clients may be experiencing delusions, obsessions, phobias, preoccupations, amnesia, or confabulations.
Disturbances in thought processes relate to how a person thinks—how he or she analyzes the world, connects and organizes information. Disorders of thought processes include blocking, flight of ideas, loose associations, and perseveration. Several disorders of thought processes are listed in Table 9.5.
Table 9.5

Another problem of thinking is depersonalization, a feeling of unreality or detachment from oneself or one’s environment. The unreal feelings produce a dreamlike atmosphere that overtakes the individual’s consciousness. One’s body does not feel like one’s own. Events that are dramatic or important are seen with a detached calmness, as if the person were watching instead of participating in reality. Feelings of depersonalization can normally occur when one is anxious, stressed, or very tired. Depersonalization disorders are often seen in clients with severe depression and in some forms of schizophrenia.
Assessment of the client’s thought content and process occurs throughout the entire mental status examination. Are the client’s thoughts based in reality? Are his or her ideas communicated clearly? Do the client’s thoughts follow a logical order? Are any unusual thoughts, preoccupations, or beliefs present? Does the client have any suicidal, violent, or destructive thoughts (American Psychiatric Association, 2018)? Are there any persistent dreams? Does the client believe that someone is intent on harming him or her (feelings of persecution)? Observe the client closely, and listen intently. Much information will be revealed during the course of the interaction.
Sensorium and Cognition
The sensorium is that part of consciousness that perceives, sorts, and combines information. People with a clear sensorium are oriented to time, place, and person. They are able to use their memories to recall recent and remote information. Levels of consciousness and memory recall help assess a person’s sensorium.
Level of consciousness can be determined by observing the amount of stimuli needed to arouse the client (Table 9.6). If the client cannot be awakened by verbal stimuli, notify your supervisor immediately. If the client is awake, note his or her responses to your questions, the degree of interaction, and the amount of eye contact that is being made.
Table 9.6
Memory is the ability to recall past events, experiences, and perceptions. For the purpose of testing, memory is divided into three categories: immediate, recent, and remote memory. Immediate memory is also referred to as recall. To assess it, ask the client to remember three things (e.g., a color, an address, an object). Later in the conversation (after at least 15 minutes have elapsed), ask the client to repeat the three items. Recall can also be tested by having the client repeat a series of numbers within a 10-second period.
Recent memory includes events within the past 2 weeks. Caregivers test recent memory by asking the client to recall the events of the past 24 hours. Loss of recent memory is seen in people with Alzheimer’s disease, anxiety, and depression.
Assessing remote memory involves asking the client questions about his or her place of birth, background, schools attended, and ages of family members. This part of the mental status examination can easily be done during the nursing health history interview. It is sometimes difficult to tell whether the client has accurate memories. Long-term memory loss is seen in clients with organic (physical) problems, conversion disorders, and dissociative disorders.
The level of concentration focuses on the client’s ability to pay attention during the conversation. Calculation tests the ability to do simple math problems. Have the person count rapidly from 1 to 20; perform simple addition, multiplication, and division problems; and subtract 7 from 100, then 7 from 93, and so on. Then ask practical questions such as the number of dimes in $1.90. Note how easily the client becomes distracted during these tasks. People with mental-emotional problems commonly have difficulty with concentration and calculations. These difficulties also occur in people with physical disorders, such as brain tumors, so it is important to assess the client’s ability to concentrate and do simple calculations.
During this phase of the mental status examination, the client’s education level, general knowledge, ability to read, use of vocabulary, and ability to think abstractly are also assessed. General knowledge can be tested by asking the person to name the past five presidents or five large cities. Ask the client about the last grade completed in school.
To determine reading ability, print a command, such as “Close your eyes,” on a piece of paper. Ask the client to read it and follow the directions. During the conversation, also note the client’s choice of words and their use.
Assess the client’s ability to think abstractly by having him or her explain the meaning of several well-known proverbs, such as “a stitch in time saves nine”; “a rolling stone gathers no moss”; “when it rains, it pours”; or “people in glass houses shouldn’t throw stones.” Many people with mental health problems give concrete answers such as, “Moss only grows on the north sides of stones,” or “People who live in glass houses shouldn’t throw stones because it breaks the glass.”
Judgment refers to the ability to evaluate choices and make appropriate decisions. During the health history interview, observe how the client explains personal relationships, his or her job, and economic responsibilities. Assess the client’s judgment by asking questions such as, “What would you do if you …
Judgment is often impaired in people with chemical dependence, intoxication, schizophrenia, intellectual disability, and organic mental disorders. Document the client’s responses using the client’s own words whenever possible.
Insight refers to the client’s understanding of the situation. What is the client’s understanding of the disorder? Questions that help the caregiver assess insight include, “Have you noticed a change in yourself recently?” and, “What do you think is the cause of your anxiety (discomfort)?” Expect clients to have different degrees of insight. For example, a person with an alcohol problem may realize that he or she drinks too much but does not think that it is interfering with family life. Again, be sure to document the client’s statements rather than your opinions.
Although the mental status examination may appear to be a lengthy process, much of it can be performed during the history interview. Checklists that address each area of the examination are available (see Box 9.4 and Appendix A for a copy of the Mental Status Assessment at a Glance).
Care providers often use parts of the mental status examination to assess clients whose mental state changes frequently. For example, the caregiver assesses the hallucinating client for thought content and process at intervals throughout the day.
Work to develop your powers of observation. Do not pass judgment or let your opinions interfere with data-gathering. Remember, the results of the mental status examination can be affected by attitudes and beliefs. Learn to use assessment tools. Develop your observation and assessment skills because they will serve you well in all practice settings.