Introduction to Radiologic and Imaging Sciences
Arlene M. Adler, MEd, R.T.(R), FAEIRS, Richard R. Carlton, MS, R.T.(R)(CV), FAEIRS, Kori L. Stewart, PhD, R.T.(R)(CT), CIIP
During World War I, the demand for x-ray technicians in military hospitals was so great that a shortage of technical workers became acute at home. The value of the well-trained technician was emphasized, and the radiologist was no longer satisfied with someone who knew only how to throw the switch and develop films.
Margaret HoingThe First Lady of Radiologic TechnologyA History of the American Society of X-Ray Technicians, 1952
Objectives
- • Explain the use of radiation in medicine.
- • Provide an overview of the history of medicine.
- • Describe the discovery of x-rays.
- • Define terms related to radiologic technology and the other radiologic and imaging sciences.
- • Explain the career opportunities within the professions of radiologic and imaging sciences.
- • Identify the various specialties within radiologic and imaging sciences departments.
- • Describe the typical responsibilities of the members of the radiologic and imaging sciences team.
- • Explain the career-ladder opportunities within radiologic and imaging sciences.
- • Discuss the roles of other members of the healthcare team.
Key Terms
Bone Densitometry (BD) Measurement of bone density using dual-energy x-ray absorptiometry (DEXA or DXA) to detect osteoporosis
Cardiac Interventional Radiography (CI) Radiologic procedures for the diagnosis and treatment of diseases of the cardiovascular system
Computed Tomography (CT) Recording of a predetermined plane in the body using an x-ray beam that is measured, recorded, and then processed by a computer for display on a monitor
Diagnostic Medical Sonography Visualization of deep structures of the body by recording the reflections of pulses of ultrasonic waves directed into the tissue
Echocardiography Ultrasonographic imaging of the heart and associated vasculature
Energy Capacity to operate or work
Ionization Any process by which a neutral atom gains or loses an electron, thus acquiring a net charge
Magnetic Resonance Imaging (MRI) Process of using a magnetic field and radiofrequencies to create sectional images of the body
Mammography Radiography of the breast
Nuclear Medicine Technology Branch of radiology that involves the introduction of radioactive substances into the body for both diagnostic and therapeutic purposes
Positron Emission Tomography (PET) The creation of sectional images of the body that demonstrate the physiologic function of various organs and systems
Radiation Energy transmitted by waves through space or through a medium
Radiation Therapy Branch of radiology involved in the treatment of disease by means of x-rays or radioactive substances
Radiography Making of records (radiographs) of internal structures of the body by passing x-rays or gamma rays through the body to act on specially sensitized film or an imaging plate or system
Radiologic Technologist (R.T.) General term applied to an individual who performs radiography, radiation therapy, or nuclear medicine technology
Radiologist Physician who specializes in the use of x-rays and other forms of both ionizing and nonionizing radiation in the diagnosis and treatment of disease
Radiologist Assistant (R.A.) An advanced-level radiographer who extends the capacity of the radiologist in the diagnostic imaging environment, thereby enhancing patient care
Radiology Branch of the health sciences dealing with radioactive substances and radiant energy and with the diagnosis and treatment of disease by means of both ionizing (e.g., roentgen rays) and nonionizing (e.g., ultrasound) radiation
Roentgen Ray Synonym for x-ray
Vascular Interventional Radiography (VI) Radiologic procedures for the diagnosis and treatment of diseases of the vascular system.
X-ray Electromagnetic radiation of short wavelength that is produced when electrons moving at high velocity are suddenly stopped
RADIOLOGIC AND IMAGING SCIENCES
When the term radiation is used, it generally evokes concern and a sense of danger. This circumstance is unfortunate because radiation not only is helpful but also is essential to life. Radiation is energy that is transmitted by waves through space or through a medium (matter); it has permeated the universe since the beginning of time and is a natural part of all of our lives. For example, the sun radiates light energy, and a stove radiates heat energy.
Energy is the capacity to operate or work. The many different forms of energy include mechanical, electrical, heat, nuclear, and electromagnetic energy. Many forms of energy are used in medicine to create images of anatomic structures or physiologic actions. These images are essential for the proper diagnosis of disease and treatment of the patient. All of these energy forms can be described as radiation because they can be, and in many instances must be, transmitted through matter.
Some higher energy forms, including x-rays, have the ability to ionize atoms in matter. Ionization is any process by which a neutral atom gains or loses an electron, thus acquiring a net charge. This process has the ability to disrupt the composition of the matter and, as a result, is capable of disrupting life processes. Special protection should be provided to prevent excessive exposure to ionizing radiation.
Sound is a form of mechanical energy. It is transmitted through matter, and images of the returning sound waves can be created. Diagnostic medical sonography is the field of study that creates anatomic images by recording reflected sound waves. Sound waves are a form of nonionizing radiation.
Electrocardiography and electroencephalography are methods of imaging the electrical activities of the heart and of the brain, respectively. The graphs they produce provide useful information about the physiologic activities of these organs.
The body’s naturally emitted heat energy can also produce images for diagnostic purposes. These images are called thermograms, and they can be useful in demonstrating conditions such as changes in the body’s circulation.
Nuclear energy is emitted by the nucleus of an atom. Nuclear medicine technology uses this type of energy to create images of both anatomic structures and physiologic actions. It involves the introduction of a radioactive substance into the body for diagnostic and therapeutic purposes. These substances emit gamma radiation from their nuclei. Gamma radiation is a form of electromagnetic energy that has the ability to ionize atoms. As a result, proper radiation protection is important in the nuclear medicine department.
Electromagnetic energy has many forms (Fig. 1.1). Many of these forms are used in medicine to deliver high-quality patient care. For example, light is an essential energy form in many of the scopes used by physicians to view inside the body. In addition, x-rays are a human-made form of electromagnetic energy. They are created when electrons moving at high speed are suddenly stopped. X-rays, also called roentgen rays, named after their discoverer, Wilhelm Conrad Röntgen, allow physicians to visualize many of the anatomic structures that were once visible only at surgery.
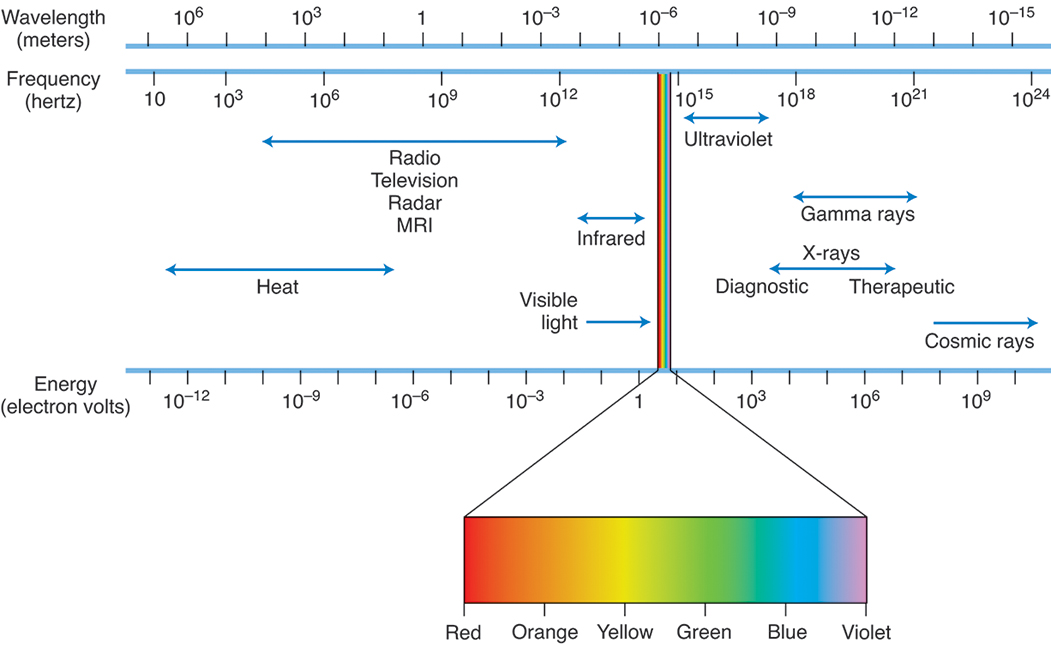
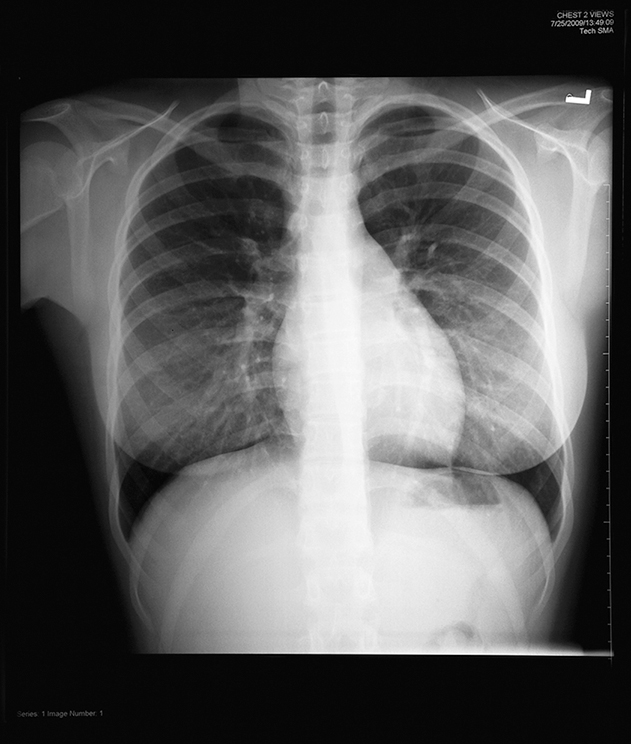
Radiography is the making of records, known as radiographs, of internal structures of the body by passage of x-rays or gamma rays through the body to act on, historically, specially sensitized film or, most commonly, on a digital imaging plate or detector. In the diagnostic radiography department, images are created using x-rays that pass through the body (Fig. 1.2). In addition, very-high-energy x-rays are used in the radiation therapy department for the treatment of many forms of cancer. In both of these departments, proper radiation protection is essential.
Radio waves are another form of electromagnetic radiation. They are a nonionizing form of radiation and are important in magnetic resonance imaging (MRI) (Fig. 1.3).

The radiologic and imaging sciences involves the study of the use of radiation throughout medicine. The fact that many forms of radiation are used in all branches of medicine should be apparent. Because many laypeople assume that the terms radiation and ionizing radiation are used interchangeably, the term imaging sciences has been preferred to the term radiation or radiologic sciences in areas that use a nonionizing form of radiation such as diagnostic medical sonography and MRI. Furthermore, because radiation therapy is primarily involved in treatment and not imaging, the term imaging sciences alone is not encompassing enough. As a result, many feel that our profession is best described by both terms, imaging and radiation or radiologic sciences. With regard to the profession, the term radiologic technology is used by the American Registry of Radiologic Technologists (ARRT) to encompass all of their individual disciplines.
OVERVIEW OF THE HISTORY OF MEDICINE
Humankind’s attempt to treat and cure diseases can be dated back almost 5,000 years to Egypt and Mesopotamia, where evidence exists that medicine was being practiced in combination with religious beliefs. Prehistoric skulls found in Europe and South America also demonstrate that early humans deliberately removed bone from the skull successfully. Whether this action was performed as a surgical treatment or as a religious attempt to release evil spirits is unknown. In addition, evidence exists that many potent drugs still in use today, such as castor oil and opium, were used in ancient Egypt for medicinal purposes. However, the Egyptians demonstrated little knowledge of anatomy, despite their sophisticated embalming skills.
The understanding of human anatomy and physiology by the early Greek philosophers was of such high quality that it was not equaled for hundreds of years. Hippocrates (c. 460–370 BC) was a Greek physician who is considered the father of Western medicine. Little is really known about him, but the fact that he was a contemporary of Socrates and was one of the most famous physicians and teachers of medicine of his time is generally accepted. More than 60 medical treatises, called the Hippocratic Corpus, traditionally have been attributed to him; however, Hippocrates did not write most of them himself. The writings are similar in that they emphasize rational and natural explanations for the treatment of disease and reject sorcery and magic. Hippocrates emphasized the importance of carefully observing the patient. He believed in the powers of nature to heal over time and taught the prevention of disease through a regimen of diet and exercise. He is also attributed with developing a high standard of ethical conduct, as incorporated in the Hippocratic Oath, which provided guidelines for physician–patient relationships, for the rights of patients to privacy, and for the use of treatment for curative purposes only. The Hippocratic Oath still governs the ethical conduct of physicians today.
The Romans recognized the importance of proper sanitation for good public health, evidenced by their construction of aqueducts, baths, sewers, and hospitals. Unfortunately, during the Middle Ages the destruction or neglect of the Roman sanitary facilities resulted in many local epidemics that eventually led to the great plague, known as the Black Death, during the 14th century. Medicine was strongly controlled by religious groups during this period, and it was not until the early 1500s that a physician in England had to be licensed to practice.
By the 17th century, medicine began to develop an increasingly scientific experimental approach. William Harvey (1578–1657), an English physician, is considered by many scholars to have laid the foundation of modern medicine. Harvey was first to demonstrate the function of the heart and the circulation of the blood. This feat is especially remarkable because it was accomplished without the aid of a microscope. By the end of the 17th century, bacteria had been described by Anton Van Leeuwenhoek (1632–1723), a Dutch zoologist, who isolated the microorganism with a microscope he made. With the development of improved microscopes, the discovery of the capillary system of the blood helped complete Harvey’s explanation of blood circulation.
During the 18th century a significant number of developments in medicine occurred. Surgery was becoming an experimental science, a large number of reforms were taking place in the area of mental health, and the heart drug digitalis was introduced. In 1796, Edward Jenner (1749–1823), an English physician, introduced a vaccine to prevent smallpox when he inoculated an 8-year-old boy, which proved that cowpox provided immunity against smallpox. This discovery served as the foundation for the field of immunology.
In the 19th century the theory that germs cause disease was established. Louis Pasteur (1822–1895), a French chemist, worked with bacteria to prove the germ theory of infection. Through his work, the process of pasteurization was developed. Robert Koch (1843–1910), a German bacteriologist, established the bacterial cause for many infections, such as anthrax, tuberculosis, and cholera. In 1905 Koch received a Nobel Prize for his work in developing tuberculin as a test for tuberculosis. During the mid-1800s Florence Nightingale (1820–1910), an English nurse, developed the foundations for modern nursing. In 1895, Wilhelm Röntgen discovered x-rays, and the radiologic and imaging sciences had their start.
The 20th century saw development of the use of the scientific method throughout medicine. The early part of the century welcomed the discovery of the first antibiotics. Sir Alexander Fleming (1881–1955), a Scottish bacteriologist, discovered penicillin in 1928 (it was isolated for mass production by Howard Florey working at the start of WWII from a cantaloupe brought to his lab in Peoria, IL). Further medical advances included the increased use of chemotherapy and a better understanding of the immune system, which resulted in the increased prophylactic use of vaccines such as the Salk vaccine, discovered by Jonas Salk (1914–1995), which helped to control and prevent poliomyelitis. Increased knowledge of the endocrine system has helped to treat diseases resulting from hormone imbalance, including the use of insulin to treat diabetes.
In 1953, at Cambridge University in England, Francis Crick (1916–2004), an English scientist, and James Watson (b. 1928), an American biologist, announced that they had discovered the secret of life. Through their work, they identified the molecular structure of deoxyribonucleic acid (DNA), a key to heredity and genetics. Currently, much research is being devoted to the field of genetics. Completed in 2003, the Human Genome Project (HGP) was a 13-year international scientific research project coordinated by the US Department of Energy and the National Institutes of Health. During the early years of the HGP, the Wellcome Trust (United Kingdom) became a major partner; additional partners came from Japan, France, Germany, China, and others. The project goals were to:
- • Identify all of the approximately 20,000 to 25,000 genes in human DNA
- • Determine the sequences of the 3 billion chemical base pairs that make up human DNA
- • Store this information in databases
- • Improve tools for data analysis
- • Transfer related technologies to the private sector
- • Address the ethical, legal, and social issues that may arise from the project
Although the HGP is finished, analyses of the data will continue for many years. The replacement of faulty genes through gene therapy offers promises of cures for a variety of hereditary diseases, and, through genetic engineering, important pharmaceuticals have been developed.
HISTORY OF RADIOLOGIC TECHNOLOGY
The field of radiologic technology began on November 8, 1895, when Wilhelm Röntgen, a German physicist, was working in his laboratory at the University of Wurzburg. Röntgen had been experimenting with cathode rays and was exploring their properties outside glass tubes. He had covered the glass tube to prevent any visible light from escaping. During this work, Röntgen observed that a screen that had been painted with barium platinocyanide was emitting light (fluorescing). This effect had to be caused by invisible rays being emitted from the tube. During the next several weeks, Röntgen investigated these invisible rays. During his investigation, he saw the very first radiographic image—his own skeleton. Röntgen became the first radiographer when he produced a series of photographs of radiographic images, most notably the image of his wife’s hand (Fig. 1.4). He termed these invisible rays x-rays because x is the symbol for an unknown variable.

Wilhelm Röntgen was born in Lennep, Germany, on March 27, 1845. In 1872, he married Anna Bertha Ludwig (1839–1919), and they had one adopted daughter. In 1888, Röntgen began working at the University of Wurzburg in the physics department. During the 1870s and 1880s, many physics departments were experimenting with cathode rays, electrons emanating from the negative (cathode) terminal of a tube. During his discovery, Röntgen worked with a Crookes tube. Sir William Crookes (1832–1919) used a large, partially evacuated glass tube that encompassed a cathode and an anode attached to an electrical supply. His tube was the early version of the modern fluorescent light. Crookes actually produced x-rays during his experimentation in the 1870s but failed to grasp the significance of his finding. He often found that photographic plates stored near his worktable were fogged. He even returned fogged photographic plates to the manufacturer, claiming they were defective. Many physicists created x-rays during the course of their work with cathode rays, but Röntgen was the first to appreciate the significance of the penetrating rays.
The actual day that the significance of Röntgen’s finding became clear to him is the subject of much debate. However, Friday, November 8, 1895, is believed by historians to be the day that Röntgen created the famous image of his wife’s hand (see Fig. 1.4). On Saturday, December 28, 1895, Röntgen submitted his first report, titled On a New Kind of Rays, to the Wurzburg Physico-Medical Society. Through his investigative methods, Röntgen identified the properties of x-rays. His methods were so thorough that no significant additions have been made to his work.
For his efforts, Röntgen was honored in 1901 with the first Nobel Prize in physics. He refused to patent any part of his discovery and rejected many commercial company offers. As a result, he saw little financial reward for his work. He died on February 10, 1923, of colon cancer.
Throughout the 20th century, the use of x-rays advanced significantly to include the imaging of almost all aspects of the human body and the treatment of diseases with radiation therapy. In addition, radioactive substances came into use for both imaging (nuclear medicine) and treatment. By the 1970s, imaging had further advanced to include diagnostic medical sonography, computed tomography (CT), and MRI. Today, through the use of hybrid scanners that combine nuclear medicine imaging with either CT or MRI, both anatomic and physiologic function can be assessed in a single examination.
OPPORTUNITIES IN THE RADIOLOGIC AND IMAGING SCIENCES PROFESSION
Radiologic technology is the technical science that deals with the use of x-rays or radioactive substances for diagnostic or therapeutic purposes in medicine. Radiologic technologist (R.T.) is a general term applied to persons qualified to use x-rays (radiography) or radioactive substances (nuclear medicine) to produce images of the internal parts of the body for interpretation by a physician known as a radiologist. Radiologic technology also involves the use of x-rays or radioactive substances in the treatment of disease (radiation therapy).
In addition to using x-rays and radioactive substances, R.T.s are also involved in using magnetic fields and radio waves (MRI) to create images of the internal anatomy of the body.
The ARRT is the credentialing organization for medical imaging, interventional procedures, and radiation therapy. The organization supports the following 15 credentials: bone densitometry (BD), breast sonography (BS), cardiac interventional radiography (CI), cardiovascular interventional radiography (CV), computed tomography (CT), magnetic resonance imaging (MR), mammography (M), nuclear medicine technology (N), quality management (QM), radiation therapy (T), radiography (R), registered radiologist assistant (R.R.A.), sonography (S), vascular interventional radiography (VI) and vascular sonography (VS). From this list, credentials in Quality Management (QM) and Cardiovascular Interventional Radiography (CV) are no longer being issued but indivduals who hold these credentials can maintain them if they continue to meet the ARRT requirements for doing so. Individuals can earn an ARRT credential through either a primary or post-primary pathway. A primary pathway requires an earned associate’s degree or higher and the completion of an ARRT-approved educational program. Primary pathway disciplines include magnetic resonance imaging, nuclear medicine technology, radiation therapy, radiography, sonography, and vascular sonography. Post-primary pathways are for those currently certified by the ARRT, the American Registry for Diagnostic Medical Sonography (ARDMS) or the Nuclear Medicine Technology Certification Board (NMTCB). Individuals can earn the MRI or VS credential either through a primary or post-primary pathway. From this list, one can see how all-encompassing the profession of radiologic technology truly is.
Radiography
An R.T. specializing in the use of x-rays to create images of the body is known as a radiographer (Fig. 1.5). Radiographers perform a wide variety of diagnostic x-ray procedures, including examinations of the skeletal system, the chest, and the abdomen. They administer contrast media to permit visualization of the gastrointestinal (GI) tract and the genitourinary system. They also assist the radiologist during more specialized contrast media procedures, such as those used to visualize the spinal cord (myelography) and the joint spaces (arthrography).

To become a registered radiographer, one must complete an ARRT-recognized radiography program. Programs are most commonly sponsored by hospitals, community colleges, and universities. There are approximately 740 ARRT-recognized radiography programs, primarily in the United States but in Canada and Australia as well. On successful completion of a recognized program, individuals are awarded a certificate, an associate degree, or a baccalaureate degree and are eligible to take the national examination in radiography offered by the ARRT. All candidates must have earned an academic degree to qualify for this certification. A registered radiographer uses the initials R.T.(R)(ARRT) after their name. This abbreviation means registered technologist (radiography).
Appendix A contains Clinical Practice Standards for Radiography, developed by the American Society of Radiologic Technologists. These practice standards help to define the role of the radiographer and establish criteria used to judge performance.
Cardiac and Vascular Interventional Radiography.
Radiographers can specialize in performing radiologic examinations of the cardiovascular system. There are two disciplines for this specialty called cardiac interventional radiography (CI) and vascular interventional radiography (VI) (Fig. 1.6). These procedures involve the injection of iodinated contrast media for diagnosing diseases of the heart and blood vessels. Angiography is the term for radiologic examination of the blood vessels after injection of a contrast medium. Most often, the contrast material is injected through a catheter, which can be directed to a variety of major arteries or veins for visualization of these structures. By way of a catheter, injecting contrast media into structures such as the carotid arteries leading to the brain, the renal arteries leading to the kidneys, the femoral artery of the leg, and many other sites is relatively easy.

Placing a catheter into one of the chambers of the heart is termed cardiac catheterization. This catheter then can be directed into one or both of the two main arteries that supply blood to the heart itself. These arteries are called the coronary arteries.
Coronary arteriography is an extremely valuable tool in diagnosing atherosclerosis, which can block the coronary arteries and cause a heart attack (myocardial infarction). By way of a special catheter with a balloon tip, effective treatment of atherosclerosis is possible. This treatment of a blocked blood vessel is termed angioplasty. Angioplasty is used to treat patients without having to use invasive open heart surgery. In addition to angioplasty, blocked vessels are also typically treated by placing a stent in the vessel to physically keep it open.
These procedures involve the use of highly specialized equipment and complex procedures. This specialization of equipment and supplies has resulted in a need for radiographers to be specially prepared in this advanced technology. Most of this advanced education occurs through continuing education classes and on-the-job clinical experience. In 1991, the ARRT began offering a postprimary examination in CV. This examination is no longer offered but has been split into two separate examinations, one for cardiac interventional (CI) technology and another for vascular interventional (VI) technology. To qualify for this examination, individuals must be ARRT certified in radiography and meet clinical requirements. An ARRT-certified individuals use the initials R.T.(CI)(ARRT) and/or R.T.(VI)(ARRT) after their name.
Mammography.
Radiographers can specialize in performing radiologic examination of the breast, a procedure called mammography. Mammography is a valuable diagnostic tool for the early detection of breast disease, especially breast cancer. Current statistics indicate that one of every eight or nine women in the United States will develop breast cancer. Men are not excluded from this disease; approximately 1% of breast cancers are found in men. Early detection of breast cancer is important to successful treatment and cure. As a result, the American Cancer Society (ACS) has recommended regular mammography screening for all women. The current ACS guidelines for women of average risk state that women between 40 and 44 years should have the option to start screening with an annual mammogram, women between 45 and 54 years should have annual mammograms, and women 55 years and older can switch to mammograms every other year or continue yearly mammograms.
This emphasis on screening mammography has resulted in an increase in the number of mammographic examinations being performed across the country. Special breast imaging centers have been built to accommodate the demand for these procedures. Equipment and supplies, such as a specially designed x-ray tube and high-resolution digital imaging detectors, are used to create high-quality breast images. Many facilities now routinely perform breast tomosynthesis also known as three-dimensional (3-D) mammography. These systems use low-dose x-rays and computer reconstruction to create 3-D images of the breast. This specialization of equipment and supplies has resulted in a need for radiographers to be specially prepared in this advanced technology. Most of this advanced education occurs through continuing education classes and on-the-job clinical experience. In 1992 the ARRT began offering a post-primary examination in mammography. To qualify to take the examination, individuals must be ARRT certified in radiography and meet educational and clinical requirements. An ARRT-certified individual uses the initials R.T.(M)(ARRT) after their name.
Radiologist Assistant.
A radiologist assistant (R.A.) is an advanced-level radiographer who extends the capacity of the radiologist in the diagnostic imaging environment, thereby enhancing patient care. The R.R.A. is an ARRT-certified radiographer who has completed an advanced academic program encompassing a nationally recognized R.R.A. curriculum and a radiologist-directed clinical preceptorship. R.R.A.s perform a wide variety of patient care procedures under the direction of the radiologist. These procedures include fluoroscopic examinations such as GI studies, myelograms, arthrograms, and central venous line placements, along with contrast media and general medication administration. R.R.A.s also evaluate images for completeness and diagnostic quality and report clinical observations to the radiologist.
The concept of the R.R.A. has moved in and out of popularity in the United States. Pilot programs at the University of Kentucky and Duke University were launched in the mid-1970s to educate technologists to carry out certain tasks traditionally performed by radiologists. The programs produced a small number of graduates before they were forced to close when federal funding was cut in the late 1970s. The American College of Radiology was not in support of the concept, and the programs slowly died over the next 20 years. A new era of R.R.A. programs began in 1995, when Weber State University in Utah started a 2-year educational program for registered R.T.s who had at least 5 years of experience and wanted to work in an advanced clinical role. Although this program has also been somewhat controversial, it was joined in 2003 by a Bachelor of Science program at Loma Linda University in California and in 2004 by several other undergraduate programs around the country. In 2005 the ARRT began offering a post-primary examination for R.R.A.s. To qualify to take the examination, individuals must be ARRT certified in radiography, earn a bachelor’s degree, have at least 1 year of acceptable clinical experience in radiography, complete an ARRT-approved R.R.A. education program, and meet the educational, ethics, and examination standards established by the ARRT. Currently, seven ARRT-recognized R.R.A. educational programs are listed on the ARRT website at http://www.arrt.org. In addition to R.R.A.s, there are R.T.s who have also completed a physician assistant program and who work with radiologists much as the R.R.A. does. An ARRT-certified individual uses the initials R.R.A. (ARRT) after their name.
Nuclear Medicine
The branch of radiologic technology that involves procedures that require the use of radioactive materials for diagnostic or therapeutic purposes is nuclear medicine technology (Fig. 1.7). Nuclear medicine procedures usually involve the imaging of a patient’s organs—such as the liver, heart, or brain—after the introduction of a radioactive material known as a radiopharmaceutical. Radiopharmaceuticals are usually administered intravenously but can be administered orally or by inhalation. Procedures can also be performed on specimens such as blood or urine. Samples from a patient can be combined with a radioactive substance to measure various constituents in the sample. Radiopharmaceuticals are also used to perform positron emission tomography (PET) procedures. After the injection of a positron-emitting radioisotope, PET scans create sectional images of the body that demonstrate the physiologic function of various organs and systems. Today many PET scanners are combined with CT or MR to acquire both the functional images that PET can provide with the anatomic references that CT and MR accomplish. These hybrid imaging techniques have advantages over either system performed separately.

To become a registered nuclear medicine technologist, completing an accredited nuclear medicine technology program is necessary. There are approximately 115 ARRT-recognized programs, primarily in the United States. Most commonly sponsored by hospitals, community colleges, or universities, these programs vary in length from 1-year programs to 4-year baccalaureate programs. One-year programs are usually designed for persons who already hold credentials in radiography, medical technology, or nursing or who possess a baccalaureate degree in one of the basic sciences. All candidates must have earned an academic degree to qualify for ARRT certification. Graduates of an accredited program are eligible to take the national examination in nuclear medicine technology offered by either the ARRT or the Nuclear Medicine Technology Certification Board (NMTCB). Successful completion of one of these two examinations is usually required for employment. An ARRT-certified person uses the initials R.T.(N) (ARRT) after their name, meaning registered technologist (nuclear medicine technology). An NMTCB-certified individual uses the initials CNMT after their name, signifying certified nuclear medicine technologist.
Radiation Therapy
A radiation therapy technologist, or radiation therapist, is a person who administers radiation treatments to patients according to the prescription and instructions of a physician, known as a radiation oncologist (Fig. 1.8). Radiation oncology involves the use of high-energy ionizing radiation to treat primarily malignant tumors (cancer). Therapists are responsible for administering a planned course of prescribed radiation treatments using high-technology therapeutic equipment and accessories. They provide specialized patient care and observe the clinical progress of their patients. Radiation therapists can specialize in the area of medical dosimetry. Medical dosimetrists are involved in treatment planning and dose calculations. This specialized area usually requires advanced education and certification.

To become a registered radiation therapist, it is necessary to complete an ARRT-recognized radiation therapy program. There are approximately 110 educational programs, primarily in the United States. Programs are most commonly sponsored by hospitals, community colleges, or universities and vary in length from 1-year programs to 4-year baccalaureate programs. One-year programs are usually designed for persons who already have credentials in radiography or who can demonstrate competence in the areas identified in the essentials for a radiation therapy program. All candidates must have earned an academic degree to qualify for certification. Graduates of an ARRT-recognized program are eligible to take the national examination in radiation therapy offered by the ARRT. An ARRT-certified individual uses the initials R.T.(T)(ARRT) after their name. This abbreviation means registered technologist (radiation therapy).
Bone Densitometry
Bone densitometry (BD) is most often used to diagnose osteoporosis, a condition that is often recognized in menopausal women but can also occur in men. Osteoporosis involves a gradual loss of calcium, causing the bones to become thin, fragile, and prone to fractures. Routine x-ray examinations can diagnose bone fractures but are not the best way to assess bone density. To detect osteoporosis accurately, dual-energy x-ray absorptiometry (DEXA or DXA) is used. DEXA BD is the current standard for measuring bone mineral density. Measurement of the lower spine and hips is most often performed. The International Society for Clinical Densitometry has offered the Certified Bone Densitometry Technologist credential since 1993. In 2001 the ARRT began offering a post-primary examination in BD. To qualify to take the examination, individuals must be ARRT certified in radiography, nuclear medicine technology (or NMTCB certified), or radiation therapy and meet clinical requirements. An ARRT-certified individual uses the initials R.T.(BD)(ARRT) after their name.
Computed Tomography
Computed tomography (CT) is the recording of a predetermined plane in the body using an x-ray beam that is measured, recorded, and then processed by a computer for display on a monitor (Fig. 1.9). This technology allows physicians to visualize patient anatomy in various sectional planes.

CT involves the use of highly specialized equipment and complex procedures, which has resulted in a need for radiographers to be specially prepared in this advanced technology. Most of this advanced education occurs through continuing education courses and on-the-job clinical experience. In 1995 the ARRT began offering a post-primary examination in CT. To qualify to take the examination, individuals must be ARRT certified in radiography, nuclear medicine technology (or NMTCB certified), or radiation therapy technology and meet clinical requirements. An ARRT-certified individual uses the initials R.T.(CT)(ARRT) after their name.
Diagnostic Medical Sonography
Diagnostic medical sonography is the visualization of structures of the body by recording the reflections of pulses of high-frequency sound (ultrasound) waves directed into the tissue. A person who specializes in this field is known as a diagnostic medical sonographer (Fig. 1.10).

Sonographers may have previous experience as radiographers, but this experience is not required. To become a sonographer, the candidate can either complete a diagnostic medical sonography program or, less commonly, be prepared on the job. On-the-job clinical experience is typically provided only to persons who have previous experience in another health specialty, such as radiography. Individuals are eligible to take a national examination offered by the American Registry for Diagnostic Medical Sonography (ARDMS) through a variety of pathways. A registered diagnostic medical sonographer uses the initials RDMS after their name. A registered vascular technologist uses the initials RVT after their name. A registered diagnostic cardiac sonographer uses the initials RDCS after their name with differentiations for Adult Echocardiography (AE), Fetal Echocardiography (FE), and Pediatric Echocardiography (PE). In addition, a cardiovascular credentialing international organization provides cardiac sonographers with a credential that allows them to use the initials CCI after their names. There is also a credential available in Musculoskeletal Sonography (MSKS).
In 1999 the ARRT began offering a post-primary examination in sonography. To qualify to take the examination, individuals must be ARRT certified in radiography, nuclear medicine technology (or NMTCB certified), radiation therapy, or MRI (or ARDMS certified) and meet clinical requirements. Candidates can also become eligible to take the examination by completing a formal ARRT-recognized educational program in sonography. There are approximately 210 ARRT-recognized sonography programs, primarily in the United States. Effective January 1, 2015, all candidates must have earned an academic degree to qualify for ARRT certification. An ARRT-certified individual uses the initials R.T.(S)(ARRT) after their name.
Magnetic Resonance Imaging
MRI uses a strong magnetic field and radio waves along with a computer to generate sectional images of patient anatomy (Fig. 1.11). Like CT, this advanced technology uses highly specialized equipment and requires specialized education. Although many MRI technologists have obtained their education through continuing education courses and on-the-job clinical experience, formal educational programs now exist with baccalaureate, associate, or certificate credentials. For the most part, MRI technologists have credentials in radiography and many are also experienced CT technologists. In 1995 the ARRT began offering a post-primary pathway for the certification examination in MRI. To qualify to take the examination, individuals must be ARRT certified in radiography, nuclear medicine technology (or NMTCB certified), radiation therapy, or sonography (or ARDMS certified) and meet clinical requirements. Candidates can also become eligible to take the primary magnetic resonance examination by completing a formal educational program in MRI approved by the ARRT. There are approximately 65 ARRT-recognized educational programs in MRI. Effective January 1, 2015, all candidates must have earned an academic degree to qualify for this certification. An ARRT-certified individual uses the initials R.T.(MR) after their name.

Additional Opportunities
Regardless of the area in which an individual chooses to specialize within the profession of radiologic technology, additional opportunities exist in education, management, and commercial firms.
Education.
Individuals who have an interest in teaching any of the specific disciplines can find opportunities in hospitals, colleges, and universities. Careers include clinical instructor, didactic faculty member, clinical coordinator, and program director.
A clinical instructor teaches students primarily on a one-on-one basis in the clinical setting. A didactic faculty member teaches students typically through classroom lectures and laboratory activities. A clinical coordinator has teaching responsibilities along with administrative duties in overseeing clinical education, most often in programs using many clinical education centers. A program director has teaching responsibilities, as well as overall administrative responsibility for the entire educational program. Advanced coursework in education is desirable for these positions. Program directors are required to have a master’s degree.
Administration.
Persons who have an interest in the management of the radiology services in a given facility can specialize in a wide spectrum of supervisory and administrative positions. Many departments have supervisory positions in areas such as CT, MRI, interventional, mammography, or sonography.
Along with experience, advanced coursework in management is often expected for these positions. The Association for Medical Imaging Management (AHRA) supports the credentialing of radiology administrators. The Radiology Administration Certification Commission (RACC) offers an examination for administrators and upon successful completion, the Certified Radiology Administrator (CRA) credential is awarded.
Commercial Firms.
Opportunities for R.T.s exist in a variety of areas within commercial companies involved in the selling of x-ray equipment, image receptor systems, and related x-ray supplies. These companies need sales representatives with technical knowledge of the radiologic procedures and equipment, as well as the ability to sell. In addition, companies hire application specialists who are not directly involved in sales but who are involved with the education and training of the staff at the sites where the equipment is installed. Sales representatives and technical specialists generally have some travel requirements as part of their responsibilities.
HEALTHCARE TEAM
A wide array of specialists make up the healthcare team. Although not all of the various disciplines can be detailed here, some healthcare services that an R.T. encounters on a regular basis are highlighted. These services include medicine and osteopathy, nursing, and the healthcare careers that encompass many of the diagnostic, therapeutic, and health information services. Persons employed in healthcare find opportunities in all kinds of environments, such as hospitals, clinics, doctors’ offices, long-term care facilities, schools, and industry.
Many healthcare workers share the titles of technologist, technician, and therapist. Technologist is a general term that applies to an individual skilled in a practical art. This healthcare provider applies knowledge to practical and theoretic problems in the field. Technician is a term that applies to a person who performs procedures that require attention to technical detail. Technicians work under the direction of another healthcare provider. The terms technologist and technician are often used interchangeably, which can create problems in disciplines in which the terms are used to denote differing levels of education. In the clinical laboratory sciences, a medical technologist (MT) has earned a 4-year degree and a medical laboratory technician (MLT) has completed a 2-year program. In general, technologists are involved in higher level problem-solving situations and have more extensive educational preparation than do technicians. Technologists and technicians work throughout all areas of healthcare; many provide direct patient care, whereas others serve in support roles.
Therapists specialize in carrying out treatments designed to correct or improve the function of a particular body part or system. Therapists possess varied levels of educational experiences ranging from 2-year to 4-year to graduate college degrees.
Medicine and Osteopathy
Physicians are primary care providers who promote the optimal health of their patients and who provide for patients’ care during an illness. Two principal types of physicians are the medical doctor (MD) and the doctor of osteopathy (DO). MDs generally complete a baccalaureate degree program with a science major such as biology or chemistry and then complete 4 years of medical school. DOs have educations similar to those of MDs. The philosophy of osteopathic medicine differs from that of traditional medicine. In addition to learning the important concepts of medicine, DOs are taught to do manipulations of muscles and bones as a part of the healing process. Both MDs and DOs must be state licensed to practice.
After medical school, most MDs and DOs complete additional clinical experience, known as a residency, in an area of specialization. Residencies are usually 3 or 4 years and may include the following branches of medicine:
- • Anesthesiology: Study of the use of medication to cause loss of sensation during surgery
- • Cardiology: Study of diseases of the cardiovascular system
- • Emergency medicine: Study of illnesses and injuries requiring immediate medical attention
- • Family medicine: Study of diseases in patients of all ages
- • Geriatrics: Study of diseases of older adults
- • Gynecology: Study of diseases of the female reproductive system
- • Internal medicine: Study of diseases of the internal organs of the chest and abdomen
- • Neurology: Study of diseases of the brain and nervous system
- • Obstetrics: Study of pregnancy and childbirth
- • Oncology: Study of the treatment of tumors
- • Orthopedics: Study of diseases of muscles and bones
- • Pediatrics: Study of diseases in children
- • Psychiatry: Study and treatment of mental illnesses
- • Radiology: Study of the use of x-rays and radioactive substances to diagnose and treat diseases
- • Surgery: Study of the use of operative procedures to treat diseases
- • Urology: Study of diseases of the urinary system
In addition, many physicians choose a subspecialty—for example, the primary duties of a pediatric cardiovascular surgeon include performing surgery on the heart and blood vessels of children.
Nursing
A nurse provides direct patient care, typically under the direction of physicians. Nurses are classified as nursing assistants, licensed practical nurses (LPNs), or registered nurses (RNs). RNs have a variety of duties, depending on their area of expertise. Nurses often choose to work exclusively in one specialty area (e.g., pediatrics, orthopedics, intensive care, the emergency department). To become an RN, the candidate must pass a state licensing examination after completion of a 2-, 3-, or 4-year program of study.
Advanced education for the nurse can lead to work as a nurse practitioner (NP), a nurse midwife, or a nurse anesthetist. An NP performs physical examinations, orders and interprets some tests, and, in some states, prescribes medications. A nurse midwife provides perinatal care and can deliver infants under the supervision of an obstetrician. A nurse anesthetist provides anesthesia under the supervision of an anesthesiologist.
Nursing assistants and LPNs generally work under the direction of an RN or a physician to provide basic care to patients. Nursing assistants generally have limited training, most of which is done on the job. LPNs generally complete a 1-year program and therefore have a broader scope of practice.
Diagnostic Services
Healthcare workers in diagnostic service areas perform tests or evaluations that aid the physician in determining the presence or absence of a disease or condition. Many healthcare specialists perform diagnostic procedures. For example, cardiovascular technologists operate equipment that records the electrical impulses of the heart, and electroneurodiagnostic technologists operate equipment to record the electrical impulses of the brain as a part of their responsibilities.
The clinical laboratory sciences involve a wide variety of careers in healthcare. An MT works in the laboratory performing tests and analyzing results. Several areas of specialization exist in the laboratory, including hematology, microbiology, clinical chemistry, immunology, and blood banking. MLTs generally work under the supervision of an MT or a physician to perform basic laboratory tests in all the various departments of the laboratory. Other laboratory personnel include the cytotechnologist, who specializes in the preparation and screening of cells, and the histologic technologist, who specializes in the preparation of tissues.
Radiology is predominantly a diagnostic service. These careers have already been detailed. Educational requirements for careers in the diagnostic services vary considerably across the disciplines, but most positions require 2 to 4 years of education beyond high school.
Therapeutic Services
Therapists provide services designed to help patients overcome some form of physical or psychological disability. Examples include occupational therapists, who teach useful skills to patients with physical or emotional illnesses; physical therapists, who help to restore muscle strength and coordination through exercise and the use of special devices such as braces or crutches; radiation therapists, who treat cancer patients using high-energy x-rays and gamma rays; and respiratory therapists, who help to treat patients with breathing difficulties. Educational requirements vary considerably across the disciplines, but most positions require 2 to 6 years of education beyond high school.
Health Information Services
Health information services involve careers that are responsible for the management of health information, such as that contained in the patient’s health record. These careers do not involve direct patient contact but are essential to the efficient operation of any healthcare facility. For example, health information professionals are involved in the coding of patient conditions, and these codes are used to determine the amount of money a facility is reimbursed for providing care to a patient. Educational requirements for careers in health information management vary considerably across disciplines, but most positions require 2 to 4 years of education beyond high school.
Other Health Services
A vast number of other careers exist within the healthcare environment. Other health services include such disciplines as communication sciences, counseling, dental health, dietetics, and psychology.
SUMMARY
- • Radiation is energy transmitted by waves through space or through a medium (matter). It is both helpful and essential for life. Energy is the capacity to operate or work. One form of energy is electromagnetic energy, which includes radio waves, light, and x-rays. Many forms of energy are used in medicine to help diagnose and treat patients. Some higher energy forms, such as x-rays, are capable of causing ionization. This process is capable of causing biologic damage, and caution should be exercised to prevent unnecessary exposure to ionizing radiation.
- • X-rays were discovered by Wilhelm Conrad Röntgen on November 8, 1895. For his discovery, Röntgen was awarded the first Nobel Prize in physics in 1901.
- • Radiologic technology is the technical science that deals with the use of x-rays or radioactive substances for diagnostic or therapeutic purposes in medicine. Radiologic technologist is a general term applied to an individual qualified to use x-rays (radiography) or radioactive substances (nuclear medicine) to produce images of the internal parts of the body for interpretation by a physician known as a radiologist. R.T.s also use x-rays or radioactive substances in the treatment of disease (radiation therapy).
- • In addition to using x-rays and radioactive substances, radiologic and imaging science professionals have become involved in using high-frequency sound waves (diagnostic medical sonography) and magnetic fields and radio waves (MRI) to create images of the internal anatomy of the body. Additional opportunities also exist for R.T.s in education, management, and commercial firms.
- • The healthcare team comprises a wide array of specialists. R.T.s work as a part of the healthcare team and interact with many of the other healthcare members on a regular basis. These other members are employed in such health services as medicine and osteopathy, nursing, and the other health careers that encompass many of the diagnostic therapeutic, and health information services.
- • Individuals employed in healthcare find opportunities in all kinds of environments, such as hospitals, clinics, doctors’ offices, long-term care facilities, schools, and industry.
BIBLIOGRAPHY
American Registry of Diagnostic Medical Sonographers website, ardms.org.
American Registry of Radiologic Technologists website, arrt.org.
Callaway WJ: Introduction to radiologic technology, ed 7, St. Louis, 2019, Mosby.
Carlton R, Adler AM, Balac, V: Principles of radiographic imaging: an art and a science, ed 7, Albany, NY, 2020, Cengage Learning.
Eisenberg RL: Radiology: an illustrated history, St. Louis, 1995, Mosby.
Gerdin JA: Health careers today, ed 7, St. Louis, 2022, Mosby.
Grigg ERN: The trail of the invisible light, Springfield, IL, 1965, Charles C Thomas.
Papp J: Quality management in the imaging sciences, ed 6, St. Louis, 2018, Mosby.
Röntgen WC: On a new kind of rays, Nature 53:1369, 1896.
Simmers LM, Simmers-Narker K, Simmers-Kobelak S: Simmers DHO: Health Science, ed 8, Albany, NY, 2018, Cengage Learning.