Gait Analysis of Running and the Management of Common Injuries
Kim Hébert-Losier and Komsak Sinsurin
Running is a popular form of physical activity and is associated with health-enhancing benefits, including a 27% reduction in the risk of all causes of mortality (Pedisic et al., 2019). Despite these benefits, the risk of sustaining a running-related injury is relatively high, with reported injury incidence rates ranging from 26.0% to 92.4% (Van Gheluwe and Madsen, 1997) and from 7.7 to 17.8 injuries per 1000 hours of running (Videbæk et al., 2015). Typically, 40% to 50% of runners experience an injury each year (Kakouris et al., 2021), with 75% these of injuries occurring at or below the knee and primarily due to overuse. Clinicians and researchers alike are still searching for the main risk factors associated with running-related injuries (van der Worp et al., 2015; Dillon et al., 2021), with the cause of running-related injuries being undoubtedly multifactorial (Esculier et al., 2020). However, risk factors have been linked to training errors and loads such as doing ‘too much, too soon’ (Soligard et al., 2016), and there is some evidence that suggests sudden changes in training loads increase the risk of running-related injuries (Damsted et al., 2019). The majority of clinicians and researchers agree that running biomechanics is part of the puzzle and an important aspect to consider, assess and train or retrain in the context of prevention, management and rehabilitation of injuries, as well as performance (Harrast, 2019). This chapter provides a brief overview of running biomechanics, clinical assessment of running mechanics, as well as potential risk factors and key management strategies of common running-related injuries.
Running Biomechanics
Key Differences to Walking
Running is a form of bipedal gait, and adults typically transition from walking to running at a speed of approximately 2 m/s which is triggered by a number of factors, notably those related to mechanical efficiency and load (Kung et al., 2018). Several of the concepts and terminology used in walking gait covered in the previous chapters apply to running, including the usual delineation of a gait cycle (or running stride) from footstrike to footstrike of the same foot. The aim of this section is not to address all facets of running biomechanics in detail, but rather to highlight a few key distinguishing features of running compared to walking.
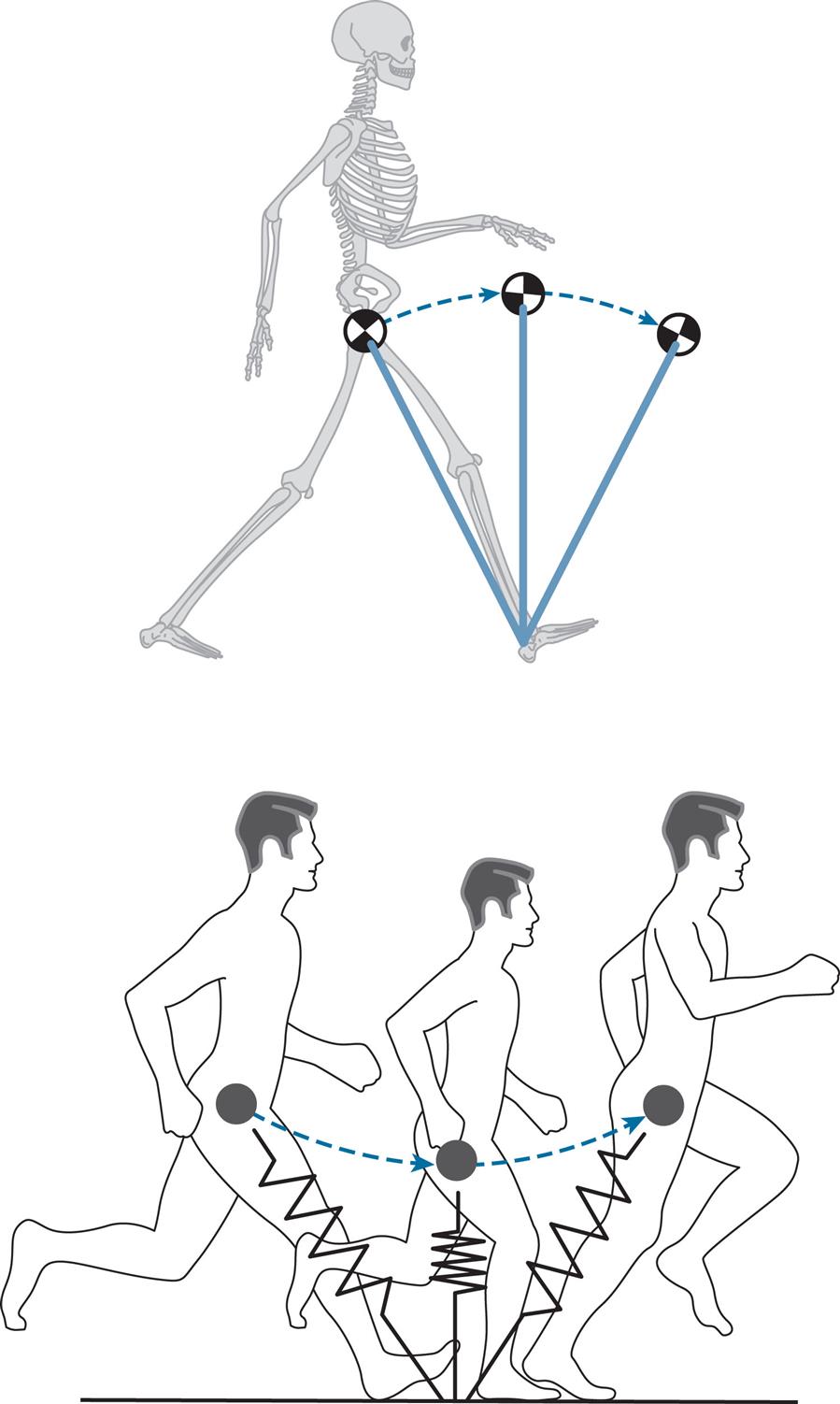
Walking has a double support phase where both limbs are in contact with the ground. An inverted pendulum is often used to model walking gait (Cavagna et al., 1977). In contrast, running has a float or flight phase where no limbs are in contact with the ground, and is modelled using a spring-mass model (McMahon et al., 1987) (Fig. 8.1). In both walking and running models, the centre of mass motion follows an arch trajectory from footstrike to toe off. These models are of course oversimplifications of the complexities of human locomotion. Nonetheless, these models provide a conceptual mechanical framework and apt pictorial representation of these cyclical locomotive tasks. The centre of mass during walking is lowest close to footstrike and highest near mid-stance, when the limb is relatively extended; in running the centre of mass is highest during flight and lowest at mid-stance, when the limb is flexed.
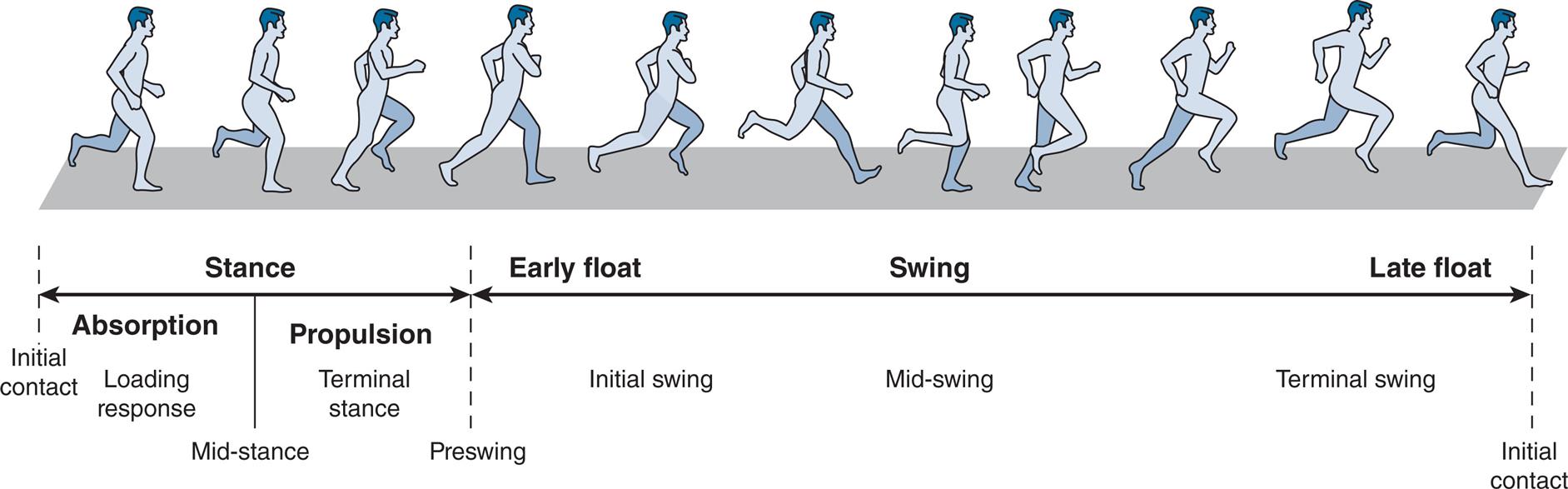
The stance and swing phases of the walking cycle represent about 60% and 40%, respectively, which can be further subdivided into seven periods (see Chapter 2, Normal Gait). On the other hand, the stance and swing phases of the running cycle represent about 35% and 65% respectively, which can be subdivided into five key periods: stance phase absorption, stance phase propulsion, early float (or swing phase generation), swing (or swing phase reversal) and late float (or swing phase reversal), as shown in Fig. 8.2.
To increase running speed, both stride frequency (also known as cadence) and stride length can increase. Whereas endurance running mainly relies on increases in stride length to increase speed (Bramble and Lieberman, 2004), increases in sprinting speed are primarily through increasing cadence, although it is worth noting that certain elite sprinters rely more on increases in stride length whilst others increase cadence to achieve top-end running speeds (Salo et al., 2011). At sprinting speeds, the proportion of time spent in stance can decrease to 20%. Concurrently with increases in speed from walking to running, peak vertical ground reaction forces increase from approximately 1.2 to 2.5, and reach up to 4.0 times body weight in elite sprinters (Čoh et al., 2018). Joint ranges of motion (ROMs) of the lower extremity, predominantly in the sagittal plane, increase as speed increases; additionally, the pelvis becomes more anteriorly tilted and the trunk becomes more flexed. The major muscle groups involved during walking, including the gluteus maximus, iliopsoas, hamstrings, quadriceps, triceps surae and tibialis anterior, all become more active in running, and joint moments and powers at the hip, knee, ankle and foot increase. Predictably, the mechanical and energetic demands of running are overall greater than walking.
Running Gait Analysis
The two main goals of addressing running biomechanics are injury management (prevention, rehabilitation, retraining) and performance enhancement. This chapter predominantly addresses the former aspect. The methods of running gait analysis parallel those presented in Chapter 4, Methods of Gait Analysis, but typically involve higher sampling frequencies. A minimum of 120 Hz or higher is recommended when conducting objective biomechanical assessment of running kinematics using two- or three-dimensional motion analysis methods (Souza, 2016). Visual running gait analysis is still common in clinical practice; however, even experts cannot accurately identify runners with an economical running gait using observations alone (Cochrum et al., 2020). This challenge might be due to the absence of an ‘ideal’ running style. Indeed, several running patterns can result in similar running economy outcomes.
The use of rating scales can assist in assessing runners’ global running patterns along a continuum using visual observations (Lussiana et al., 2017), but when possible and for monitoring purposes, the use of objective measures to quantify running gait is recommended. Most commonly, biomechanical metrics of interest are grouped as spatiotemporal (e.g., speed, step/stride length, step/stride frequency or cadence, contact times, flight times, duty factor, etc.), kinematic (e.g., joint angles, angular velocities, angular accelerations, etc.) and kinetic (e.g., peak ground reaction forces, vertical loading rates, impulses, etc.). The duty factor reflects the proportion of the stride period during which time each foot is in contact with the ground. This measure is suggested to represent a more global biomechanical behaviour than the footstrike pattern, as it considers the duration of force production in relation to stride duration. External forces are lower in recreational runners who run with a higher duty factor (Bonnaerens et al., 2021), which could have implications for injury prevention. A higher duty factor reflects a runner who spends a proportionally longer time in contact with the ground when running and can be calculated as follows:

Most clinicians conduct running assessments on a treadmill. In this situation, treadmill speed is used to calculate some of the spatiotemporal parameters. For example, right step length (m) can be measured by multiplying the treadmill speed (m/s) by the time (s) taken from left footstrike to right footstrike. Conducting a running assessment on a treadmill has several advantages (Table 8.1), notably that it allows analysis of numerous cycles, permits standardisation of running conditions and requires limited space. In contrast, it necessitates financial investment, requires familiarisation of runners and is less ecologically valid. Reviews on the differences between overground and treadmill running highlight that spatiotemporal, kinematic, kinetic, muscle activity and muscle-tendon measures are largely comparable between the two modes of running (Van Hooren et al., 2019), with the exception of vertical displacement, knee flexion ROM and foot-ground angles at footstrike which are greater when running overground. Noteworthy, though, is that the mechanical properties of commercial-grade treadmills can markedly differ from one another as well as from outdoor running surfaces (Colino et al., 2020). Treadmills typically demonstrate higher shock absorption, greater vertical deformation and lower energy restitution than outdoor running surfaces. Since treadmill construction itself can significantly affect biomechanics, metabolic cost and perception of effort (Miller et al., 2019), clinicians undertaking treadmill analysis should attempt to select a treadmill that mimics the overground running conditions of their target population. A stiffer treadmill is recommended for running assessment given that most runners run on concrete or asphalt where vertical deformation and shock absorption are minimal, and energy restitution is high. In research, using an instrumented treadmill is ideal as this provides a stiff running platform in addition to ground reaction force data.
TABLE 8.1
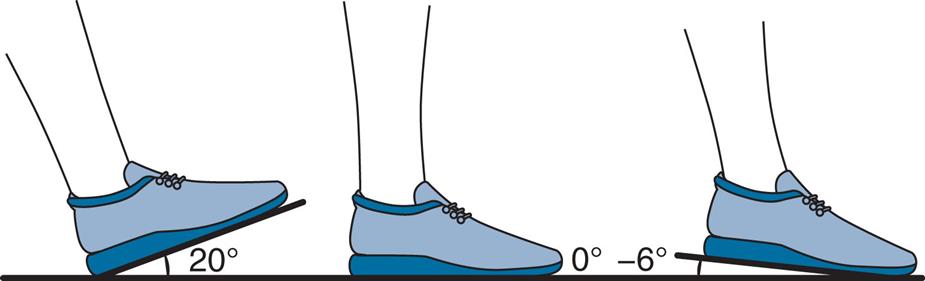
The foot normally contacts the ground with the heel or rear part of the foot during walking. In running, the footstrike pattern is typically classified in one of three discrete categories based on which part of the foot makes initial contact with the ground. Footstrike patterns are categorised as rearfoot when the first contact is with the heel or rear third of the sole; midfoot when the first contact is with the midfoot or entire sole; or forefoot when the first contact is with the forefoot or front half of the sole (Fig. 8.3). A foot-ground angle from two-dimensional videos is often also calculated as the line that joins the sole of the shoe from the point of first contact and the horizontal plane of the running surface, where positive angles represent more pronounced rearfoot striking and negative angles represent more pronounced forefoot striking (Fig. 8.3). The foot-ground angle when using three-dimensional motion analysis can be calculated as the angle between the anteroposterior laboratory axis and a vector formed between a heel marker and another placed on the second metatarsal head. Using this method, the foot-ground angle in stance is subtracted from that during running, so a 0-degree value reflects a flat foot. This foot-ground angle can be used to categorise footstrike patterns; with rearfoot being greater than 8 degrees, midfoot from 8 to –1.6 degrees, and forefoot when less than –1.6 degrees (Altman and Davis, 2012).
There is controversy regarding which footstrike pattern is more or less injurious and more or less economical, and whether it even matters. Given their distinct structural and mechanical loading patterns, it is likely that certain types of injuries are more common in rearfoot strikers, such as patellofemoral pain syndrome and medial tibial stress syndrome, whereas others are more frequent in forefoot strikers, such as Achilles tendinopathies and metatarsal stress fractures. To date, however, there is limited evidence to support a causal relationship of footstrike pattern with injury risk in running (Anderson et al., 2020).
Kinematic Measures
In clinical settings, sagittal and frontal planes are most commonly examined (see Table 8.2). It is important to emphasise that humans are dynamic systems and move in a ‘global’ manner, so changes in one area are likely to lead to changes elsewhere. For instance, increasing cadence at a given running speed is typically linked with shorter stride lengths, lower vertical oscillations, an initial ground contact with the foot closer to the centre of mass, a smaller foot-ground angle and a more vertical tibia.
Table 8.2
| Event | Sagittal | Frontal |
|---|---|---|
| Initial contact | Footstrike pattern | |
| Foot-ground angle | ||
| Foot-to-centre of mass distance | ||
| Tibial inclination | ||
| Knee flexion angle | ||
| Midstance | Knee flexion angle | Foot placement (or step width) |
| Ankle dorsiflexion angle | Foot-to-centre of mass alignment | |
| Antero-posterior pelvic tilt | Pronation/supinationa | |
| Trunk flexion | Knee separation | |
| Dynamic knee valgusb | ||
| Pelvis lateral inclination | ||
| Trunk lateral flexion | ||
| Toe-off | Knee flexion | |
| Hip extension | ||
| Gait cycle | Vertical displacement of the centre of mass |
aPronation: rearfoot inwardly rotates about the subtalar joint. Supination: rearfoot outwardly rotates about the subtalar joint. In running gait, pronation is commonly considered a combined movement of eversion, dorsiflexion and forefoot abduction, whereas supination combines inversion, plantarflexion and forefoot adduction.
bCombination of hip adduction, hip internal rotation and knee abduction.
Kinetic Measures
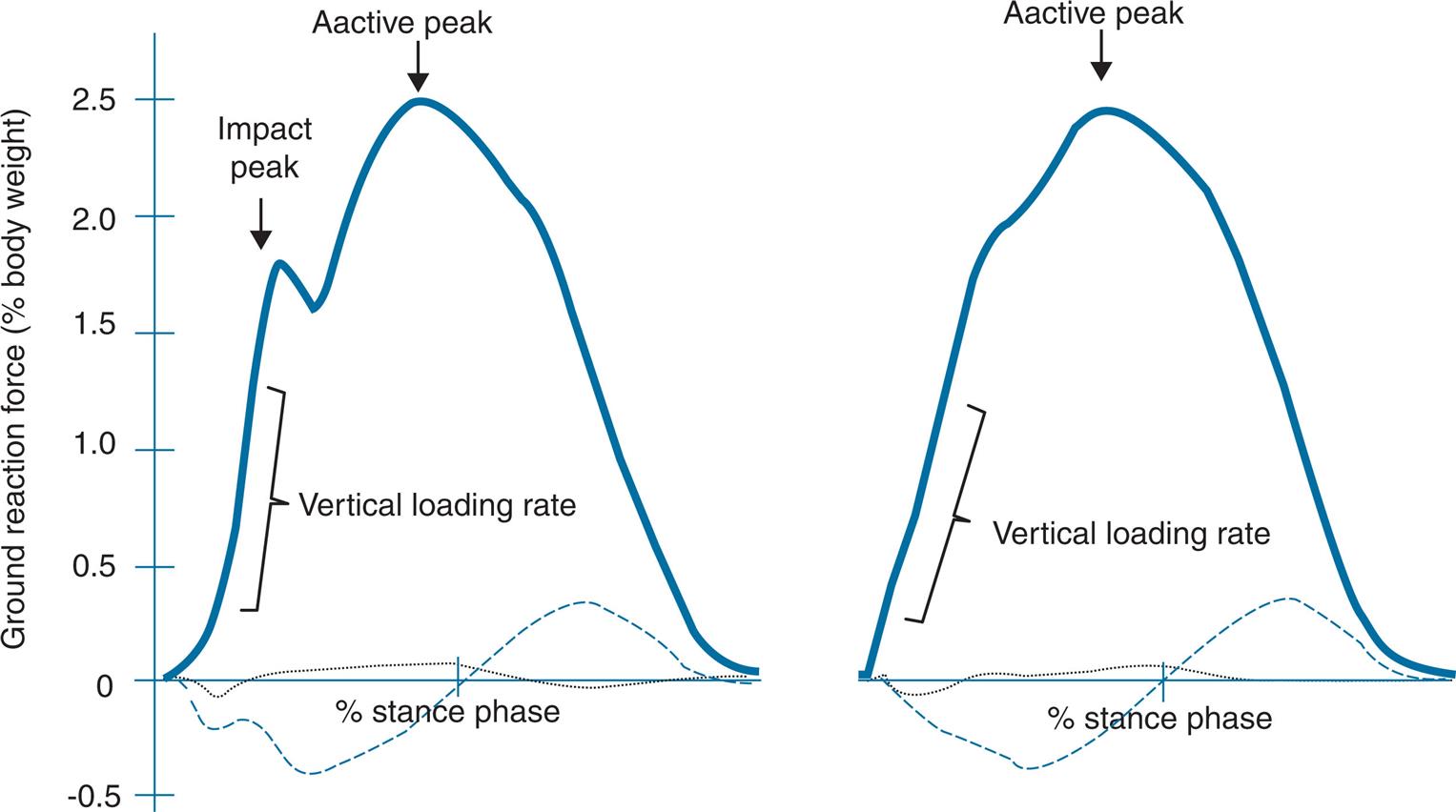
The ground reaction forces during running are usually examined in research using instrumented treadmills or forceplates embedded into the ground. The vertical component of the ground reaction force is the most studied and typically presents one of two distinct shapes based on footstrike pattern (Fig. 8.4). Rearfoot strikers typically present an impact peak resulting from a sharp increase in the ground reaction force after the initial ground contact. In forefoot strikers, this impact peak is not always present. The peak vertical ground reaction force occurs at mid-stance in both instances, is commonly referred to as the active peak and generally reaches 2.5 to 3.0 times body weight at endurance running speeds. In habitual rearfoot strikers, the active peak is generally slightly higher than nonrearfoot strikers. The vertical loading rate reflects how quickly the vertical ground reaction force is applied (body weights per second). Peak and average vertical loading rates are approximately two times lower in forefoot than rearfoot strikers. The precise vertical loading rate values depend on assessment and computational methods, but range from 30 to 90 body weights per second; however, vertical loading rates can be up to 460 body weights per second when running barefoot with a rearfoot strike pattern (Lieberman et al., 2010). The anteroposterior ground reaction forces reflect propulsion and braking forces, and are much smaller in magnitude than the vertical force. Peak anteroposterior force values during running range from 0.25 to 0.5 times body weight. Relatively little is known regarding the mediolateral forces and their impact on running gait, with peak values ranging from 0.10 to 0.20 times body weight and demonstrating numerous zero crossings.
There is again conflicting evidence regarding the role of kinetic parameters in running-related injury incidence, which might be due to the few prospective studies available. Currently, vertical loading rates and braking forces are the two variables that demonstrate potential links with certain running-related injuries, in particular in female recreational runners (Davis et al., 2016; Napier et al., 2018).
Note on Wearable Sensors
There is growing interest and promise in the use of wearable sensors to quantify and analyse running gait, predominantly in the use of inertial measurement units (IMUs), but also in pressure-sensing insoles and flexible textiles. There are currently a number of considerations in using such wearable sensors, including their sampling frequency, anatomical calibration method, fixation method, sensor capacity, durability, and validity and reliability of the derived metrics (Hughes et al., 2021). On the latter topic, the accuracy of metrics from wearable devices compared to laboratory-based methods is acceptable for spatiotemporal parameters (Horsley et al., 2021), but these are heterogeneous across studies and still suboptimal for numerous measures (Blazey et al., 2021), warranting further research before they are widely implemented within clinical practice.
Common Running-Related Injuries and Clinical Considerations
As highlighted in this chapter’s introduction, the risk of sustaining a running-related injury is considerable. Understanding the aetiology of injury is essential to implement successful injury prevention programmes. From a basic biomechanical standpoint, injuries happen when the mechanical load placed on a structure exceeds its load tolerance (McIntosh, 2005).
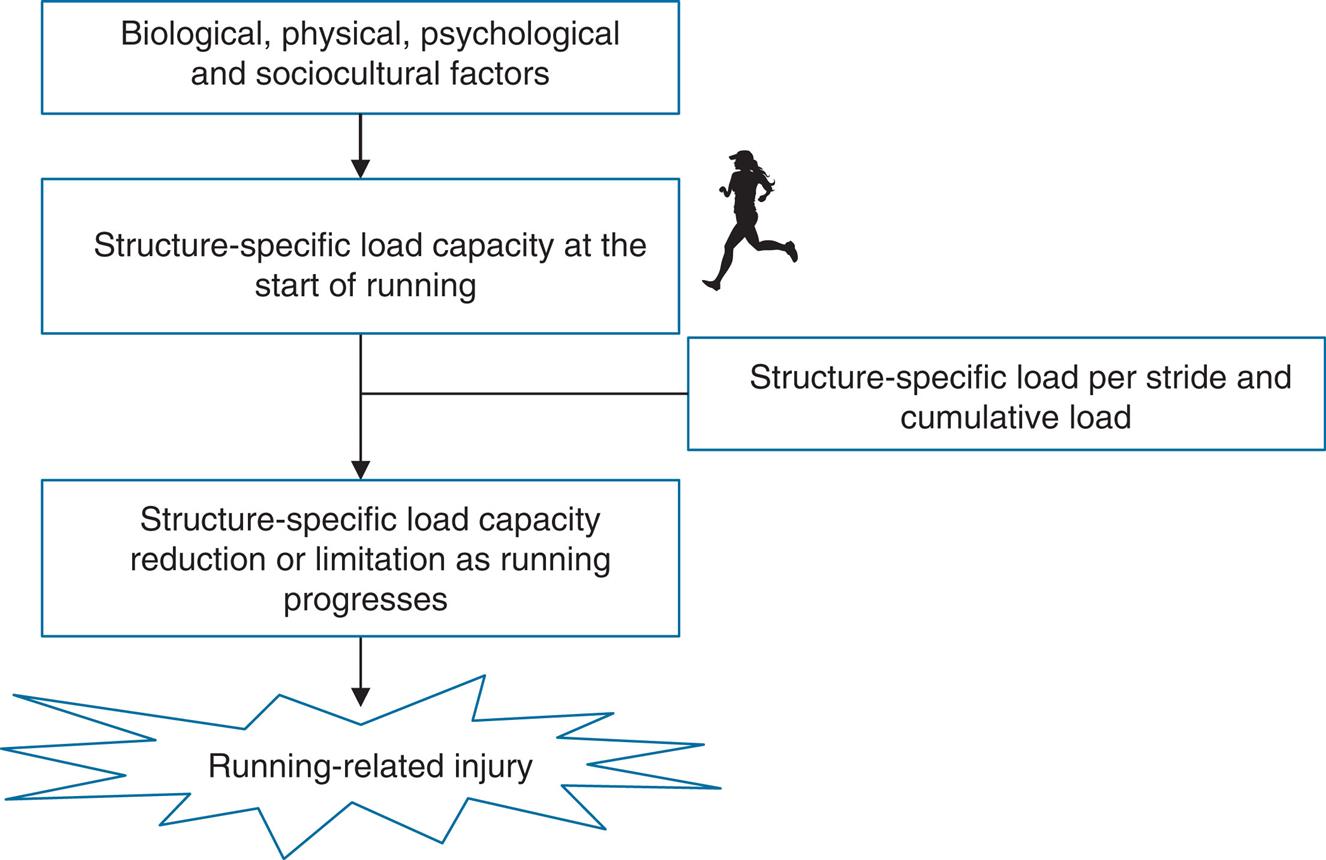
There are numerous sport-related injury aetiologies (McIntosh, 2005) and prevention (Finch, 2006) models. While it is beyond the scope of this chapter to address each one of these models, it is worth emphasising that all of them acknowledge the multifactorial nature of sport-related injuries, with more recent frameworks highlighting their complex and dynamic nature, and involvement of biological, physical, psychological and sociocultural factors (Wiese-Bjornstal, 2010). A framework specific to the aetiology of running-related injuries was proposed in 2017 (Bertelsen et al., 2017) which focused on their causal mechanisms. This framework considered the structure-specific load capacity at the start of a running session and the reduction in this capacity throughout the session as a product of the magnitude, distribution and number of load cycles (Fig. 8.5).
There have been numerous reviews on running-related injuries, which overall indicate that injuries to the lower extremities are the most common. Two of the most recent reviews identified the knee (28% to 31%), ankle-foot (26% to 28%), lower leg (16% to 20%) and hip-thigh (14%) regions accounting for the highest proportion of injuries in adult runners (Francis et al., 2019; Kakouris et al., 2021). The specific pathologies accounting for the highest proportion of overall injuries were patellofemoral pain syndrome (17%), Achilles tendinopathy (7% to 10%), medial tibial stress syndrome (8% to 9%), plantar fasciitis (7% to 8%) and iliotibial band syndrome (6% to 8%) (Francis et al., 2019; Kakouris et al., 2021), with stress fractures accounting for 4% to 6% of running-related injuries.
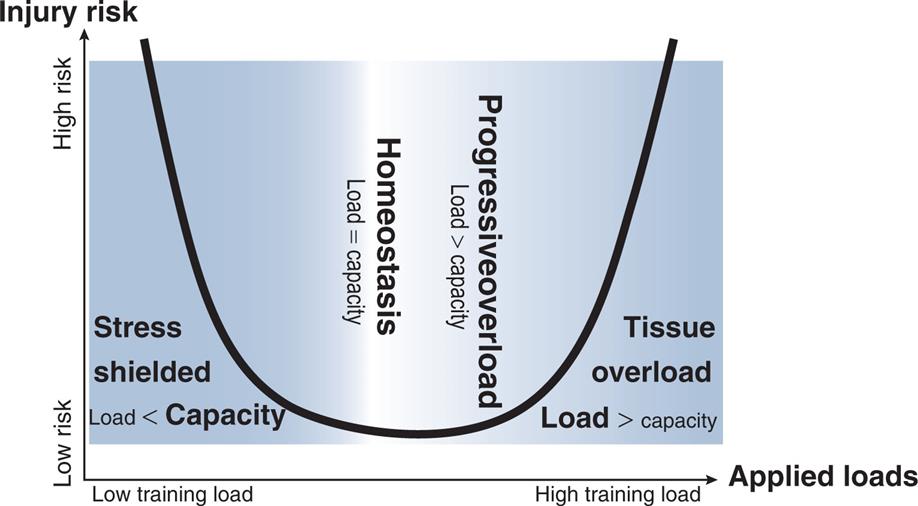
A key component in the management of running-related injuries is a comprehensive subjective assessment and history. One of the more consistently reported risk factors associated with running-related injuries is a previous injury (van der Worp et al., 2015). Another important clinical factor is training load and history, which should consider more than weekly distance (Paquette et al., 2020). Both too little and too much running have been associated with running-related injuries, with either insufficient or excessive loads impeding the biological adaptations needed for injury-free running. Some important external (mechanical) load metrics include volume, intensity, surface and terrain; internal (physiological) load metrics include perception of effort and heart rate (Paquette et al., 2020). It is well known that footwear and change in footwear can substantially affect running biomechanics and load distribution, which needs to be considered as a tool in the management of injuries. More often than not, something has changed and led to the development of a running-related injury where the load exceeded the capacity of the tissue. However, addressing purely the physical components of running-related injuries might be insufficient in certain cases, requiring a more holistic or interdisciplinary approach and involvement of other healthcare professionals.
There are numerous cross-sectional studies indicating the presence of certain movement patterns once an injury is present; but few prospective studies exist linking given movement patterns with the incidence of running-related injuries. For instance, runners with common running-related injuries have been shown to run with greater peak contralateral pelvic drop and forward trunk lean at midstance, and more extended knee and ankle dorsiflexion at initial contact compared to uninjured runners (Bramah et al., 2018). While insightful, these movements can often represent a consequence rather than a cause of injury. In fact, hierarchical cluster analysis on three-dimensional kinematic data performed on injured and healthy runners identified distinct subgroups of runners with similar running patterns; but these distinct running patterns were not related to injury location or injury status (Jauhiainen et al., 2020). These findings support the notion that there might be no ‘ideal’ or ‘protective’ running pattern. That is not to say that biomechanics does not play a role in the management of running-related injuries. Indeed, running gait retraining has been successfully used in the prevention (Chan et al., 2018) and treatment (Davis et al., 2020) of running-related injuries. The following sections address some of the most common running-related injuries and clinical considerations.
Patellofemoral Pain
Clinical Presentations
Patellofemoral pain (PFP) is the most common running injury, representing around 17% of injuries in runners (Francis et al., 2019; Kakouris et al., 2021). Runners with PFP typically present with pain around or behind the patella that is worsened in weight-bearing and dynamic knee flexion activities, such as stair climbing, squatting, running and jump-landing (Crossley et al., 2016). No ‘gold standard’ PFP diagnosis exists, although this clinical diagnosis should be considered in the presence of retro- or peri-patellar pain and in pain reproduction during activities loading the patellofemoral joint in a flexed posture or dynamic movements when tibiofemoral pathologies have been excluded (Willy et al., 2019). In runners with PFP, a number of kinematic, kinetic, muscle activity and muscle strength presentations have been reported. Runners with PFP typically present with one or more of the following:
- • knee pain during running;
- • weakness of lower limb muscles, notably knee extensors, hip abductors, hip external rotators and hip extensors (Duffey et al., 2000);
- • increased peak hip adduction and internal rotation during the stance phase of running (Wirtz et al., 2012);
- • increased contralateral pelvic drop during the stance phase of running (Bramah et al., 2018);
- • increased rearfoot eversion in heel strikers (Duffey et al., 2000; Kulmala et al., 2013);
- • greater peak lateral forces at the patellofemoral joint (Chen and Powers, 2014); or
- • dynamic knee valgus during the stance phase of running (Petersen et al., 2014) (Fig. 8.6).
Key Management Strategies
Patient education in terms of load management and activity modification plays a central role in managing PFP and is a key feature in best-practice guidelines for the conservative management of PFP (Collins et al., 2018; Willy et al., 2019). Runners have been shown to successfully self-manage rehabilitation of PFP by reducing their running distance and speed, increasing their running frequency and managing their training within acceptable clinical thresholds, such as by keeping pain levels less than 2 out of 10 with no worsening of symptoms (Esculier et al., 2017). Hence, it is important that clinicians educate patients regarding self-management strategies, the benefits of active rehabilitation and anticipated recovery and return-to-running times.
A holistic approach to the treatment of PFP is encouraged and should consider biological, physical, psychological and sociocultural factors (Fig. 8.5). Graded exercise and return to activity are one facet, but psychological stressors and lifestyle factors can also contribute to injury or slow rehabilitation. It is important for clinicians to help patients with PFP understand these potential contributing factors and assist them in accessing appropriate and suitable intervention options.
Running gait retraining should be considered as a viable intervention, especially in the presence of altered running gait mechanics. Several gait retraining approaches exist and have been successfully used in the rehabilitation of runners with PFP. These approaches include the use of visual, tactile and auditory feedback aimed at increasing cadence, running more ‘softly’, reducing tibial acceleration or vertical impact peaks, reducing dynamic knee valgus or promoting a less rearfoot strike pattern to reduce patellofemoral joint stress. To date, there is no conclusive evidence with regards to what type of feedback and approach is best suited for an individual and condition; thus, clinicians need to work with their patients to identify the most cost-effective and implementable approach on a case-by-case basis.
Physical examinations should be performed for PFP cases to aid in individualised prescription (Table 8.3). Based on the clinical examination, clinical presentation and individual responses, numerous adjunct interventions can be integrated in the management of runners with PFP. These interventions can include hip and knee strengthening exercises, taping, foot orthoses and mobility/flexibility exercises. Running in minimal footwear has also been shown to reduce patellofemoral joint stress and may be beneficial in the treatment of runners with PFP.
Table 8.3
| PFP presentation | Intervention |
Above patellofemoral pain (PFP) presentations and intervention guidelines based on Willy et al. (2019).
Achilles Tendinopathy
Clinical Presentations
Achilles tendinopathy reflects 7% to 10% of running-related injuries (Francis et al., 2019; Kakouris et al., 2021). Achilles tendinopathy is characterised by localised pain and swelling of the Achilles tendon, as well as loss of function. Symptoms can be reproduced during running, single-leg hopping or functional activities. Achilles tendinopathy is considered an overuse injury resulting from excessive mechanical loading of the tendon with impaired healing. Runners presenting with Achilles tendinopathy typically present with a recent increase in training volume, intensity or frequency, or a rapid change to more minimal footwear. Other clinical findings can include local tissue thickening (Maffulli et al., 2003), dorsiflexion ROM limitation and plantar flexor muscle weakness (Martin et al., 2018), stiffness and pain in the morning or after a prolonged rest, pain at the start of an activity that decreases as activity progresses, and reduced running performance (Janssen et al., 2018). There are few running kinematic differences in runners with compared to without Achilles tendinopathy (Mousavi et al., 2019), except for increased rearfoot eversion at ground contact. Changes in neuromuscular control have been reported, such as earlier soleus offset relative to lateral gastrocnemius during running (Wyndow et al., 2013). Other risk factors associated with Achilles tendinopathy of relevance to runners include previous lower limb tendinopathy or fracture, use of ofloxacin antibiotics, training in cold weather, use of compressive socks and use of a training schedule (Lagas et al., 2020).
Key Management Strategies
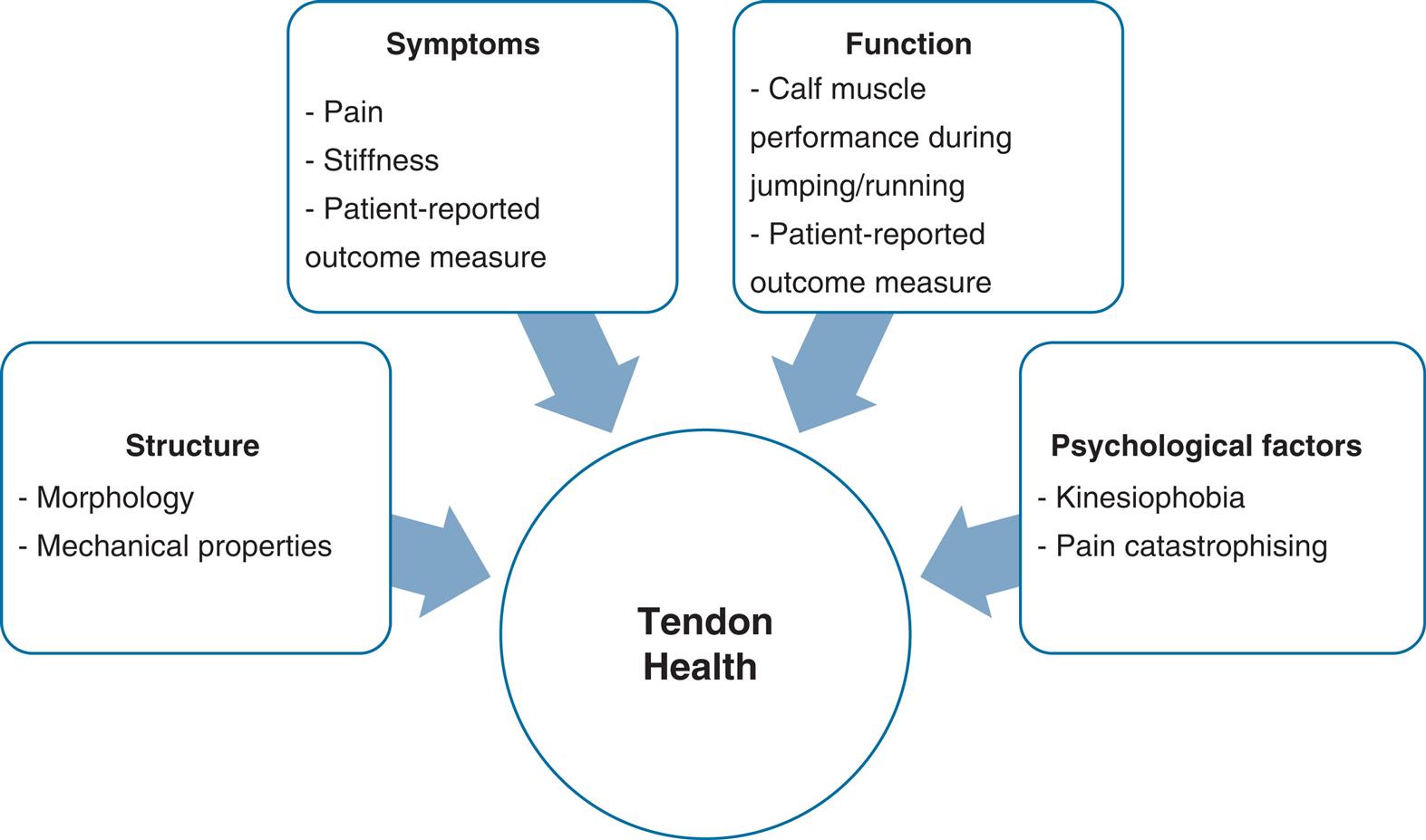
Early detection and intervention can help to prevent worsening or persistence of Achilles tendinopathies. Active treatments are more effective than the wait-and-see approach for Achilles tendinopathy (van der Vlist et al., 2021). Various domains can affect tendon health (Fig. 8.7), which should be considered in the planning and provision of interventions (Silbernagel et al., 2020; Vicenzino, B., et al., 2020). A holistic approach to treatment can contribute to restoring function and preventing recurrence.
There is emerging evidence that subgroups of Achilles tendinopathies exist which may require tailored approaches to rehabilitation (Hanlon et al., 2021). These subgroups can be categorised by activity, psychosocial and body structure considerations. The activity-dominant subgroup is the largest and contains patients with higher physical activity levels, functional abilities and quality-of-life scores than the other subgroups; moderate symptoms; and generally younger age. Rehabilitation methods for this subgroup should consider load management, progressive rehabilitation and gradual return-to-running scenarios to optimise recovery. The majority of runners who sustain an Achilles tendinopathy would fall under an activity-dominant subgroup; however, it remains important to consider all subgroups as potential causes of Achilles tendinopathy.
There is strong evidence for the effectiveness of exercise therapy for the treatment of Achilles tendinopathy, either alone or in conjunction with adjunct therapies. The Victorian Institute of Sport Assessment-Achilles questionnaire (VISA-A) along with a battery of tests, including the calf raise test for endurance, are recommended to assess and monitor individuals with Achilles tendinopathy. The number of calf raises an individual is expected to complete ranges from 20 to 50 repetitions based on age, physical activity levels, gender and body mass index (Hébert-Losier et al., 2017). The rehabilitation phase is important in the treatment of Achilles tendinopathy. It requires time and an individually progressed loading programme to allow the tendon to adapt and prevent injury recurrence (Magnusson and Kjaer, 2019). Early in the rehabilitation of runners, high-speed and uphill running should be avoided due to the load on the Achilles tendon; furthermore, the use of minimal shoes and forefoot striking in the acute phases of an Achilles tendinopathy might exasperate symptoms and should be considered later in the rehabilitation process or in chronic stages to promote adaptation and remodelling. Gait retraining aimed at increasing cadence should also be considered given that increasing step frequency lowers peak Achilles tendon stress and strain (Lyght et al., 2016).
Medial Tibial Stress Syndrome
Clinical Presentations
Medial tibial stress syndrome (MTSS) is a common (8% to 9%) running-related injury (Francis et al., 2019; Kakouris et al., 2021) and typically presents as localised pain at the two-thirds distal portion of the posteromedial aspect of the tibia, but can also be located at the anterolateral aspect. MTSS is commonly referred to as shin splints and is categorised as an exercise-induced lower leg pain (Raissi et al., 2009). MTSS is often considered as part of a continuum, spanning irritation of the periosteum to stress fractures. MTSS is treated based on its clinical presentation due to lack of strong evidence regarding its aetiology (Winters, 2018), although bone stress as a result of tibial bending has been suggested as a cause of MTSS. Typically, runners with MTSS present with pain during or after running which improves with rest. The reproduction of pain upon palpation over a 5-cm or more area along the posteromedial tibia is used for clinical diagnosis (Winters, 2020). Prior use of orthotics, fewer years of running experience, previous history of MTSS, increased navicular drop, increased body mass index, increased plantarflexion and hip external rotation ROMs and female gender are identified risk factors for MTSS in runners (Newman et al., 2013). These risk factors can inform the management strategies. Runners who develop MTSS have been reported to show greater rearfoot eversion, contralateral pelvic drop and pressure on the medial aspect of the foot during running (Becker et al., 2018). Case studies have also reported the incidence of MTSS when transitioning to shoes with more cushioning and a broader base of support (Hannigan and Pollard, 2021), warranting footwear considerations.
Key Management Strategies
Various modalities have been used to treat MTSS, including cryotherapy, shockwave therapy, massage, orthotics, pneumatic leg bracing, gait retraining and avoidance of high loading activities. However, there is yet to be strong evidence regarding the effectiveness of these interventions (Winters et al., 2013). For runners, education regarding load management and graded return to running is central to managing MTSS. Progressing running distance less than 30% from week to week has been suggested as appropriate to avoid running-related injuries (Damsted et al., 2019). In the presence of MTSS, a slower progression is advised, and should be symptom based.
A randomised control trial in runners with MTSS was conducted in 2012. All runners followed a graded return-to-running programme that allowed no more than 4 or more on a 10-point visual analogue scale. The addition of calf muscle stretching and strengthening exercises, or wearing sports compression stockings during running, did not speed up the return-to-run time, with the average time to return to 18 minutes of running at a difficult speed being approximately 3.5 months (Moen et al., 2012).
Gait retraining can also be considered in MTSS patients. A 6-week gait retraining programme aimed at adopting a forefoot strike pattern has been successfully used to treat exercise-induced lower leg pain in runners (Helmhout et al., 2015). Providing two to six running gait retraining sessions promoting landing more on the forefoot and a higher cadence has also been linked with positive MTSS results in military populations (Zimmermann et al., 2019a, 2019b), with a successful return taking approximately 5 months.
Plantar Heel Pain
Clinical Presentations
Plantar heel pain represents 7% to 8% of running-related injuries (Francis et al., 2019; Kakouris et al., 2021). Other commonly used terms to reference plantar heel pain include plantar fasciitis, plantar fasciopathy and plantar fasciosis (McNeill and Silvester, 2017). Plantar heel pain is a common condition in active populations and normally has a gradual onset (Hill et al., 2008). Typically, patients with plantar heel pain report a high intensity of pain in the first few steps of walking after sleeping or long resting (Buchbinder, 2004), and a worsening of symptoms when standing or walking for a long time or towards the end of the day (Petraglia et al., 2017). Common clinical presentations include one or more of the following:
- • localised pain at the anteromedial aspect of the heel, especially at the origin of the plantar fascia (Buchbinder, 2004);
- • increased ankle plantar flexion ROM (Hamstra-Wright et al., 2021);
- • weak foot muscles (Osborne et al., 2019);
- • less femoral internal rotation (Harutaichun et al., 2019);
- • poor movement quality in the lateral step-down test (Harutaichun et al., 2019); or
- • increased body mass index and body mass (Hamstra-Wright et al., 2021).
Key Management Strategies
There are three strategies reflecting the core approach to treating plantar heel pain in the first 4 to 6 weeks of care: individualised education, plantar fascia stretching and low dye taping (Morrissey et al., 2021). Education should be individualised and address load management, pain education, health-related conditions and footwear considerations. Psychosocial variables, such as depression, anxiety and job satisfaction, may increase levels of pain and loss of function in patients with plantar heel pain (Drake et al., 2018); hence, this aspect should be integrated within patient education, and referrals should be sought when needed. In the case of no or limited improvement, shockwave therapy and orthoses can be added as adjunct therapies.
Body weight is an important factor to address in the management and prevention of plantar heel pain. This consideration might be of relevance to runners who have taken a rest or who are getting back to training. A gradual increase in running load, intensity and volume can assist in tissue adaptation and improve load capacity (Hamstra-Wright et al., 2021). Combining calf muscle strengthening and shoe inserts showed superior outcomes in terms of pain and foot function at 3 months compared to combining plantar-specific stretching and shoe inserts (Rathleff et al., 2015). Given that individuals with plantar heel pain present with reduced foot muscle strength and volume, intrinsic foot muscle strengthening exercises can also be recommended (Osborne et al., 2019).
Running uphill or at high speeds can increase the strain on the plantar fascia and should be avoided during early rehabilitation. There are few studies on runners with plantar heel pain; hence, in terms of gait retraining and footwear, similar principles to those presented in the Achilles tendinopathy section are proposed until evidence specific to plantar heel pain is available.
Iliotibial Band Syndrome
Clinical Presentations
Iliotibial band syndrome (ITBS) represents 6% to 8% of running-related injuries (Francis et al., 2019; Kakouris et al., 2021) and is the second most common overuse injury in runners (Taunton et al., 2002). Tissue compression or impingement of the iliotibial band on the lateral femoral epicondyle is thought to be responsible for ITBS and associated lateral knee pain. Lateral knee pain is typically worse at 20 degrees to 30 degrees of knee flexion (Hamill et al., 2008). Usually, runners with ITBS report lateral knee pain onset a few kilometres into running. Training errors are common in the subjective history of patients, such as a sudden increase in running volume and downhill running. Such training errors can lead to a disruption in tissue homeostasis (Dye, 2005; Gabbett, 2016) and tissue overload (Fig. 8.8).
There are limited prospective studies on ITBS (Aderem and Louw, 2015), and no clear biomechanical causes of ITBS have been identified in runners (Louw and Deary, 2014). Runners with ITBS can clinically present with decreased hip abductor muscle strength and the following running gait kinematics (Aderem and Louw, 2015; Foch et al., 2015), particularly when fatigued:
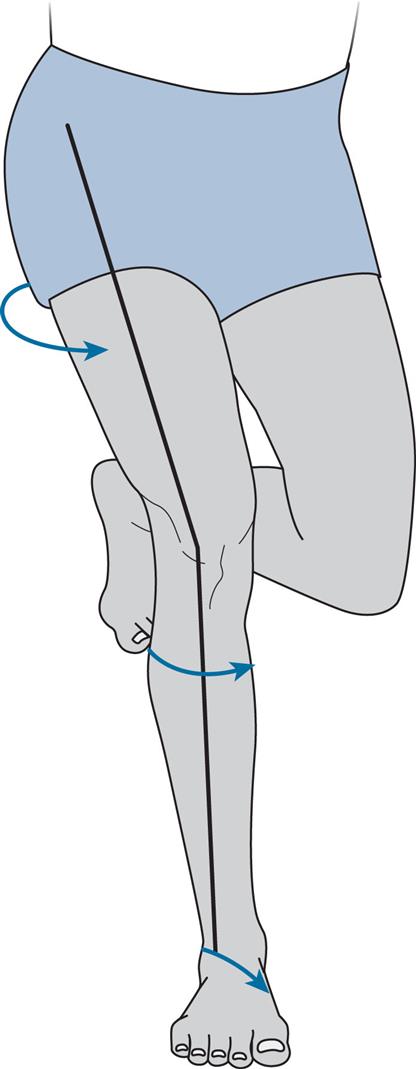
Running with excessive hip adduction and knee internal rotation in stance may increase the tensile and torsional strains in the iliotibial band. This running pattern can maintain compression of the iliotibial band onto the lateral femoral epicondyle (Fairclough et al., 2006) and induce high strain rates on the iliotibial band (Hamill et al., 2008). Gait retraining methods that reduce these movement patterns may be beneficial in the treatment of ITBS, such as increasing cadence.
Key Management Strategies
ITBS symptoms in athletes can be effectively reduced using conservative management strategies (Bolia et al., 2020), despite the quality of available evidence being relatively low. Generally, pain management is a primary focus in the acute phases. Exercise or training while managing load should nonetheless be encouraged during this phase. After the pain-dominant phase, clinicians should progress running programmes and exercises to increase load tolerance. Lateral knee pain or irritation the following day should not exceed 2 on a 10-point visual analogue scale during the pain-dominant phase.
Running gait retraining is one strategy that can be used to address hip and knee coordination and running patterns (van der Worp et al., 2012) and can reduce knee loads while running. The gait retraining approaches highlighted in the earlier discussion of patellofemoral pain can be considered for ITBS. Incorporating running retraining using verbal and visual feedback into an 8-week conditioning programme was shown to be more effective than no feedback when attempting to influence some of the proposed risk factors to running-related injury, including average and instantaneous vertical loading rates, peak hip adduction, peak knee internal rotation and peak rearfoot invertor moments (Letafatkar et al., 2020). In this particular study, the feedback provided included running more softly, avoiding a rearfoot strike landing, and running with the knees apart and kneecaps pointing forwards. At the 1-year follow-up, the running gait retraining with feedback group had a lower injury incidence of 66.7% ITBS, 57% PFP, and 66.7% plantar fasciitis (Letafatkar et al., 2020).
Strengthening should also be considered in individuals with ITBS. Progressive hip exercises performed over 8 weeks have demonstrated superior outcomes in terms of pain, function and strength than stretching and conventional exercises (McKay et al., 2020). Complementing interventions with mobilisation and education regarding running surfaces (e.g., avoiding concrete surfaces and downhill running, and incorporating various running surfaces) can also contribute to positive treatment outcomes (van der Worp et al., 2012). Clinicians should prescribe intervention programmes individually, and consider including strengthening, especially the hip abductors; joint mobilisation; orthoses and the management of soft tissues (van der Worp et al., 2012; McKay et al., 2020).
Key Points
- • About one in every two runners experiences a running-related injury each year, with 75% of injuries occurring at or below the knee.
- • Running-related injuries are multifactorial in nature. The most consistently reported risk factors include a previous injury and recent changes in running training.
- • Numerous cross-sectional studies indicate the presence of certain movement patterns once an injury is present, but few prospective studies link specific movement patterns to injury incidence. Changes in movement patterns are often a consequence rather than a cause of injury.
- • The key management strategies in treating the most common running-related injuries include patient education on load management, activity modification and footwear; gait retraining; and graded exercise and return-to-running programmes.
- • Addressing purely the physical components of running-related injuries might be insufficient in certain cases, requiring a more holistic or interdisciplinary approach and referrals to other healthcare professionals when needed.