Transobturator Slings
Subsequent to the development of TVT it was recognized that transobturator tape (TOT) was a viable method for correction of SUI. Since Ulmsten’s initial article in 1996 there has been extensive acceptance of the various midurethral sling technologies. In Europe, as of 2005, approximately 83.9% of all procedures are midurethral-type synthetic slings, of which 26.9% are with TOT (de Tayrac and Medelenat, 2004). Since the initial description of the TOT approach, numerous other similar TOT approaches have been noted.
The goal of the minimally invasive surgical procedure should be to provide acceptable long-term efficacy comparable to that of more standard methods as well as a relatively low incidence of long-term complications, again compared with these “gold standard” procedures. Retropubic midurethral slings have demonstrated robust outcomes in both primary and recurrent SUI as well as in women with MUI and in those with ISD. Delorme (2001) initially described the placement of synthetic polypropylene mesh using the TOT approach. The technique was described as being relatively facile and associated with fewer complications than retropubic approaches. It was also thought that the procedure did not require cystoscopy.
Much of the understanding of the function of the TOT slings arises from that which has evolved from TVT-type procedures. Perineal ultrasonography has been used to assess the function of the TVT in patients who undergo successful incontinence procedures. In those individuals, a functional kinking of the urethra during stress events is noted to occur when the tape is placed at the midurethra (Lo et al, 2004). In relatively long-term follow-up (3 years), 92% of patients had ultrasonic demonstration of tape at the midurethra and evidence of urethra kinking that caused the “urethral knee angle.” Of these patients, 92% were continent. Of the patients who had tape location either at the posterior urethra or bladder neck, only three of five (60%) were continent, presumably because of lack of a fulcrum-like effect at the midurethra. These ultrasound studies appear to underscore the importance of the midurethral location and also the ability of the TOT to accomplish this localization (Lo et al, 2001, 2004).
Similarly, Minaglia and colleagues (2004), using a variant of the TOT (ObTape), showed no difference in resting urethral angulation after tape insertion. These authors, however, did notice that there was a statically significant difference preoperatively and postoperatively in urethral angle with straining. They also noted that most women had persistent urethral hypermobility after the procedure, and they concluded that correction of hypermobility was not necessary to achieve continence. Their results documented that 90.4% of patients with documented hypermobility were continent, whereas only 50% of the patients without hypermobility were continent. They concluded that a persistently positive Q-tip test was predictive of a successful outcome. They found that concomitant prolapse surgery or previous incontinence surgery had no effect on outcome.
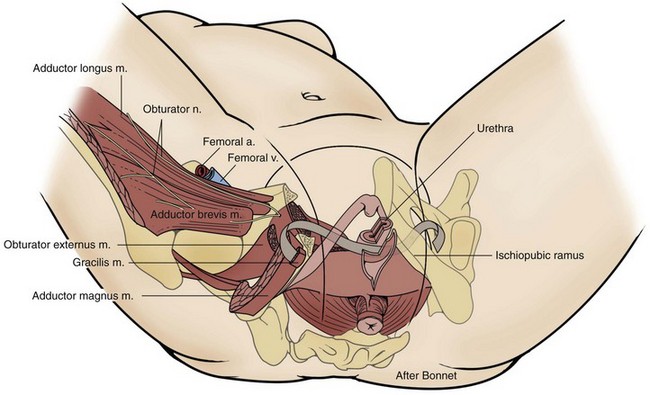
Surgical Anatomy
For successful implantation of the TOT, an understanding of the surgical anatomy of the pelvic floor, including the surrounding neurovascular structures, pelvic and perineal anatomy, and the obturator foramen, is crucial to provide surgical success and minimize morbidity. Three reviews have demonstrated with cadaveric dissection the importance of landmarks and implantation technique for the success of the TOT procedure.
Bonnet and colleagues (2005) performed the “inside-out” TOT technique as described by de Leval (2003) in 13 cadavers to determine tape path and proximity to surrounding structures. Cadaveric dissection was extended from the femoral triangle medially through the obturator externus muscle and adductor longus to the inferior pubic ramus. The perineal space was then entered, and the pubic bone was sectioned to evaluate the relationship of the tape to various structures. Finally, the subfascial anterior perineum and pelvis were dissected to analyze the tape path fully. These authors demonstrated several significant points in their cadaveric dissection. They noted that the tape never penetrated the adductor longus muscle, thus being a safe distance from neurovascular structures. In approximately 70% of studied cases the implanted material did traverse the adductor magnus, adductor brevis, and gracilis muscles during its path into the pelvis.
At the level of the obturator foramen the tape was noted to traverse both the obturator externus and internus muscles as well as the obturator membrane. The relationship between the inserted tape and the obturator nerve showed that the closest proximity of the two was 22 mm with a distance as great as 30 mm (mean 26.2 ± 2 mm) at the level of the obturator foramen. The authors emphasized that an individual’s thighs in hyperflexion and the rotational trajectory of the helical passer associated with this positioning ensured the separation of the insertion tool from the nerve during the actual implantation of the material. They also noted that regional vascular anatomy (anterior branch of the obturator) was protected from injury by the bony architecture of the inferior pubic ramus.
More medially, the tape entered the anterior compartment of the ischiorectal fascia, in the area of the levator ani membrane and obturator internus muscle. The tape remained outside the pelvic space and did not penetrate the levator ani muscular group. The tape remained above the perineal membrane at all times. The dorsal nerve of the clitoris was found to be consistently caudal to the perineal membrane and thus protected from injury during needle passage. These relationships were found to be consistently confirmed in each cadaveric specimen, and thus Bonnet and colleagues believed that these observations represented highly reproducible anatomic positioning and therefore concluded that the TOT technique is safe.
Delmas and associates (2003) utilized the “outside-in” approach on 10 female cadavers, again detailing the relevant pelvic anatomy in relationship to the tape insertion path. In this study, dissection demonstrated that the tape always consistently passed 4 cm opposite and caudal to the obturator canal, again confirming the relative safety of neurovascular structures. They also demonstrated that the tape traverses a plane between the perineal and levator antimusculature but above the neurovascular pedicle of the pudendum. They also noted that in the pelvic component of their dissections, the tape courses medial to the obturator plexus. They concluded that tunneling passage anteriorly risks injury to the bladder and passage in the posterior dissection demonstrated a risk of vaginal perforation.
A third study by Whiteside and Walters (2004) further evaluated the obturator anatomy in relationship to tape insertion in six female cadavers. These authors found that the mesh, on average, passed 2.4 cm inferior and medial to the obturator canal and that both divisions of the obturator (anterior and posterior) were 3.4 and 2.8 cm, respectively, separated from the path of the insertion tool. They also noted that the insertion tool passed within, on average, 1.1 cm proximity to the medial branch of the obturator vessels. These authors concluded that a risk of injury does exist and that appropriate caution should be exercised.
Operative Technique
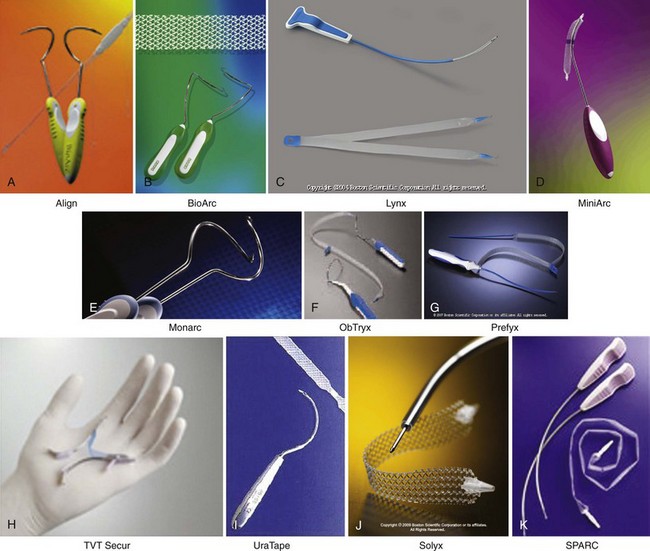
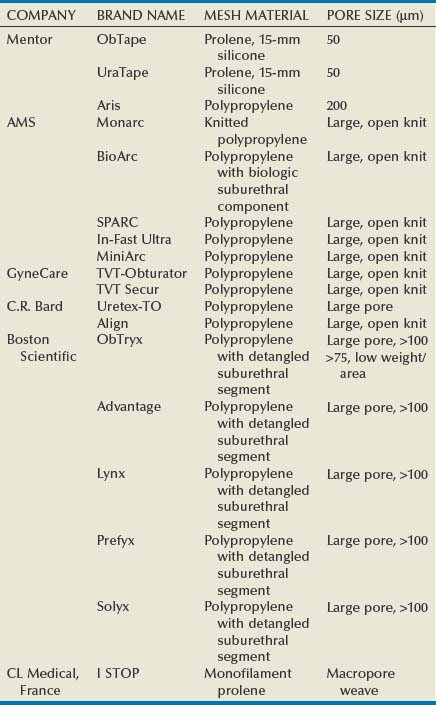
Operative technique varies with insertion method. Various procedures using similar insertion methods represent relatively similar technique (Fig. 73–12). Not only does implantation technique affect overall success of the sling, but also the type of mesh or tape implanted has a substantive effect on overall results. Mesh properties have been shown to have a significant effect on local inflammatory response and ingrowth of local fibrous tissues (collagen, neovascularity) and subsequent integration of these tapes into host tissues. These differences in properties are believed to affect the risk of erosion and subsequent infection and other vaginal and local complications. There are intrinsic differences between the various meshes that have been used for the TOT approach. The ObTape and UraTape meshes are polypropylene material but are small pore, knitted, and thermally bonded with an approximately 15-mm silicone component that is immediately suburethral in location after implantation. A second-generation obturator tape developed by the Mentor Corporation is known as the Aris TOT; it has a larger 200-µm pore size that allows improved tissue ingrowth with less encapsulation. The ObTryx, TVT-O, Monarc, I STOP, and Urotex-TO are large-pore open knit polypropylene meshes. A unique obturator mesh is the BioArc, which, like the suprapubic variety, has a biologic graft material that is sutured on either end to the polypropylene tape. The biologic material actually occupies a suburethral position (de Leval, 2003; Delorme et al, 2003) (Table 73–17; Fig. 73–13).
Table 73–17 Devices and Descriptions (see Fig. 73–13)
Transobturator Outside-In
The patient is placed in the dorsal lithotomy position with legs in hyperflexion (120 degrees). A small vertical vaginal incision is created as with the TVT procedure over the midurethra, and dissection is carried out laterally to the ischiopubic ramus. A puncture incision is made in the obturator foramen at the level of the clitoris in the leg using the tunneler; the obturator membrane is perforated, at which point resistance is noted by the operative surgeon. Using the nondominant index finger and identifying the landmarks of ramus and the obturator internus muscle, the surgeon turns the tunneler in a medial orientation and advances it on the tip of the index finger and brings it out through the vaginal incision. Inspection is carried out at this point to exclude inadvertent penetration of the vaginal fornix or associated urinary structures. The synthetic material is then attached to the tunneler and brought out through the inner thigh stab wound. The procedure is then repeated on the contralateral side. Tension is set on the tape by passing a clamp between the tape and urethra such that a surgical clamp can be passed easily between these two structures. Excess material is then cut at the skin puncture site, and the incisions are closed according to the surgeon’s preference.
This approach is used for the following devices: ObTape, UraTape, Aris TOT, Monarc, BioArc TO, Uretex-TO, ObTryx, I STOP.
Transobturator Inside-Out
The vaginal component of the procedure is essentially the same as in the outside-in technique. Stab incisions are created approximately 2 cm superior to the horizontal line level with the urethra and 2 cm lateral to the labial folds, which will be the exit point for the helical passer. Once the device is inserted through the urethra and the upper part of the ischiopubic ramus is reached with the device, the obturator membrane is perforated sharply with scissors. The introducer is then passed at a 45-degree angle relative to the midline sagittal plane until it reaches and perforates the obturator membrane. The open side of the introducer is passed out facing the surgeon. The more distal end of the tubing is then mounted on the spiral segment of the helical passer and slipped along the open gutter of the introducer. The passer is aligned parallel to the sagittal axis and rotated so that the tip of the tubing exits the inner thigh stab incision. The tubing is then removed from the passer until the first few centimeters of the tape become externalized, and the procedure is repeated on the contralateral side. All plastic covering sheaths are then removed simultaneously from the tape while maintaining no tension on the sling itself using the technique previously described.
Results
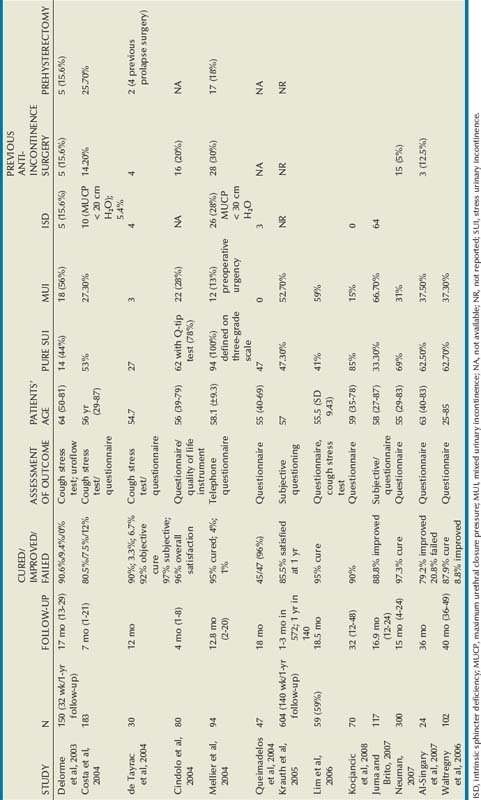
Since the initial description by Delorme in 2001, continence rates have been reproducibly satisfactory although follow-up has, in general, been short (Table 73–18). Reported continence rates range from 80.5% to 96% on the basis of a variety of subjective (questionnaire and quality of life single-item assessment) and objective (cough stress test, uroflowmetry, physical examination) measures.
Efficacy
Efficacy analyses have included heterogeneous groups of patients, including those in whom prior procedures failed, those who had concomitant prolapse, and those with MUI. Delorme (2001) noted that 15.6% of his patients had ISD, and Mellier and colleagues (2004) diagnosed 28% of their patients with ISD. Despite these diverse populations of patients, relatively similar results were obtained. O’Connor was the first group to examine the early outcomes of the transobturator approach for SUI in women with a variable VLPP. Patients were divided into high (>60 cm H2O) or low (<60 cm H2O) VLPP groups. The odds of continued SUI after TVT-O were 12 times greater for women with VLPP less than 60 cm H2O compared with those with VLPP greater than 60 cm H2O (O’Connor et al, 2006). However, no preoperative predictors of outcomes using either clinical or urodynamic parameters were established to determine overall results of these procedures. Therefore, the effect of MUI and concomitant prolapse on surgical outcomes for this intervention are unknown. Prospective studies are needed to answer these questions.
Two nonrandomized studies have compared TOT with TVT procedures and have found no significant difference in postoperative voiding dysfunction, complications, or overall continence. There was a tendency toward more bladder injuries (10% vs. 0%) and hemorrhage (10% vs. 2%) with the suprapubic as compared with the TOT approach, but this did not reach statistical significance (de Tayrac et al, 2004; Mellier et al, 2004). Five prospective randomized studies have compared TOT with TVT procedures, ranging in follow-up from 6 to 31 months (Lee et al, 2007b; Porena et al; 2007; Zullo et al, 2007; Rinne et al, 2008; Schierlitz et al, 2008; Rechberger et al, 2009). Among two groups there were a significantly greater number of bladder perforations in patients with the retropubic approach over the TOT approach: 6.5% vs. 0% (Rechberger et al, 2009) and 7.3% vs. 0% (Schierlitz et al, 2008). Both of these groups also found the TVT to be more effective than the TOT in patients with ISD. Schierlitz and colleagues (2008) observed that at 6-month follow-up, 13% of the TOT procedure patients with ISD required further surgery whereas 0% of the TVT patients with ISD required reoperation for SUI (Schierlitz et al, 2008). Porena and associates noted that storage symptoms were significantly improved in the TOT group (still present in 24%) while persisting in 44% of the TVT group (Porena et al, 2007). A few key points are consistent between these studies: these techniques were safe, there were no long-term complications in either group, cure rates were equal (with exception of ISD group), and patients were equally satisfied.
Complications of the Transobturator Approach
Despite the minimally invasive nature of these procedures, perioperative and postoperative complications have been reported with a variety of techniques.
Bladder Injury
The anatomic variation between the inside-out (TVT-O) and outside-in (TOT) approaches has been compared, especially in regard to their association with adverse outcomes. Cadaver dissections after a TVT-O procedure noted the mean distance from the vaginal incision to the obturator membrane is 4.0 cm, and from the vaginal incision to the obturator neurovascular bundle is 6.75 cm. At the obturator membrane the closest point of the passer is only a mean distance of 2 cm from the obturator neurovascular bundle. This is the reason the curved passer is directed away from these structures and advanced. Also, an anterior branch of the obturator artery coursed medially along the exterior edge of the obturator foreman in 60% of the cadavers. They believed that this artery was protected by the exterior bony rim of the obturator foramen during an inside-out pass but could be potentially injured in an outside-in approach (Rogers et al, 2005).
Conflicting results have been reported by Zahn and associates (2007), who found that the inside-out method was significantly closer to the obturator canal. The greater proximity and distance from the ischiopubic ramus of the inside-out method was noted in all of their cadaveric dissections. Additional dissections revealed the deep external pudendal vascular structures coursing from superolateral to inferomedial over the obturator foramen, putting it at risk during the exit of an inside-out approach. No clinical correlations exist to date, suggesting that one approach is associated with a higher incidence of tunneler-related complications.
Bladder perforation appears to be the most common complication associated with any midurethral sling, with a 2% to 11% risk with the suprapubic approach. Although initial reports described the risk with the TOT approach as being negligible, the risk of bladder injury is now identified as associated with this sling insertion technique (Table 73–19) (Olsson and Kroon, 1999; Kobashi and Govier, 2003b; de Tayrac et al, 2004).
Table 73–19 Complications Associated with Transobturator Tape Techniques
| STUDY | NO. PATIENTS | ADVERSE EVENTS |
|---|---|---|
| Delorme et al, 2003 | 32 | None reported |
| de Leval, 2003 | 107 | One superficial vein thrombosis with abscess; ?(27/107) 15.9% transient thigh pain |
| Domingo et al, 2005 | 65 | Nine vaginal mesh erosion |
| Costa et al, 2004 | 183 | Three vaginal erosion; two urethral erosion; one bladder perforation; one vaginal perforation; two urethral perforation |
| de Tayrac et al, 2004 | 30 | Six uncomplicated UTI; one obturator hematoma |
| Cindolo et al, 2004 | 80 | One vaginal erosion with inguinal abscess |
| Mellier et al, 2004 | 94 | 2% intraoperative hemorrhage (300 mL); one urethral perforation |
| Queimadelos et al, 2004 | 47 | None reported |
| Krauth et al, 2005 | 604 (140 with 1-yr follow-up) | 0.3% vaginal erosion; 2.5%UTI; 0.5% bladder perforation; 0.33% vaginal perforation; 2.3% perineal pain |
| Giberti et al, 2007 | 118 | 6.4% vaginal erosion; one vaginal hematoma |
| Juma and Brito, 2007 | 117 | 3.84% vaginal erosion; 1.52% bladder perforation |
| Neuman, 2007 | 300 | 0.7% vaginal erosion; 1.3% dyspareunia |
| Al-Singary et al, 2007 | 24 | 1% perforated vaginal fornix; 12.5% vaginal erosion |
| Waltregny et al, 2008 | 102 | 1 vaginal laceration |
| Rechberger et al, 2009 | 197 | 2.5% vaginal erosion; 5.5% UTI; 5% urinary retention |
| Lee et al, 2009 | 105 | 4% dyspareunia |
UTI, urinary tract infection.
Minaglia and colleagues (2004) reported three cases of intraoperative bladder injury while performing the TOT insertion method. They identified all injuries intraoperatively because of their utilization of cystoscopy as an adjunct to all insertion procedures. All injuries were managed with catheter placement for 1 week postoperatively, and these authors noted no complications after sling removal and reinsertion at that same setting. Parekh and associates (2006) reported a case of intravesical mesh erosion after TOT placement and cystocele repair. The patient did not have cystoscopy intraoperatively. She initially presented with mesh on the left side of the bladder and then 6 months later with sling material in the right side of the bladder. She had a successful transurethral, transvaginal, and suprapubic mesh resection.
A single case of bladder laceration was reported by Cindolo and Costa that was also managed intraoperatively (Cindolo et al, 2004; Costa et al, 2004). This apparently was a more extensive injury than just trocar perforation. The tunneler passage of the outside-in obturator approach has been shown to be associated with lower urinary tract injury. To date, no case of bladder injury when performing the TOT procedure by the inside-out approach has been reported using the TVT-O (Hermieu et al, 2003; Whiteside and Walters, 2004).
Erosions, Extrusions, and Infectious Complications
Domingo and coworkers (2005) reported a relatively high incidence of vaginal erosion in their series using either the ObTape or UraTape. They attributed their erosion rate to the characteristics of the particular mesh that they utilized, with the reduced pore size and other mechanical properties of that particular material. They noted a slightly increased risk of erosion with the ObTape (15-mm silicone-coated portion)—19% versus 12% compared with the UraTape—and they believed that this was most likely due to reduction in pore size and higher degree of encapsulation. They also concluded that synthetic mesh with larger pore sizes facilitates vascular and tissue ingrowth, optimizing mesh incorporation. Tape erosion was usually managed by removal by the transvaginal approach alone or combined with the transobturator approach. They noted continence rates of 78% (despite tape removal in their series) (Domingo et al, 2005). Vaginal extrusions and erosions of up to 15% have been reported, often accompanied by obturator and ischiorectal abscesses, sinus formation, and voiding difficulty using the ObTape or UraTape (Babalola et al, 2005; Domingo et al, 2005; Deval et al, 2006; Robert et al, 2006; Al-Singary et al, 2007; Dobson et al, 2007; Giberti et al, 2007; Juma and Brito, 2007; Karsenty et al, 2007). Abscess and adductor myositis have been reported, manifesting as leg pain, difficulty ambulating, and cellulitis (Goldman, 2006; DeSouza et al, 2007; Karsenty et al, 2007; Leanza et al, 2008; Zumbé et al, 2008). Gamé and colleagues (2004) reported an infected obturator hematoma also requiring exploration and drainage. Tamussino and associates (2007) published data from the Austrian database, including 2543 transobturator cases, using 11 different tape systems. They reported greater number of complications than reported earlier in their TVT database. This included 120 intraoperative complications (4.7%), 85 cases of bleeding (3.3%), 10 vaginal perforations (0.4%), 10 bladder perforations (0.4%), and 2 urethral perforations. Bladder perforations occurred more frequently with the outside-in tape systems than the inside-out tape systems in their database. The ObTape is no longer available for construction due to the high erosion rates.
Newer, knitted polypropylene slings and many of the reports using the inside-out approach have lower incidence of erosions, extrusions, and infectious complications (Neuman, 2007; Waltregny et al, 2008; Lee et al, 2009; Rechberger et al, 2009). Neuman (2007) reported two patients with vaginal extrusion, which were repaired by covering the exposed mesh with surrounding vaginal mucosa successfully. Of the 197 women who had multifilament transobturator slings by Rechberger and associates (2009), 2.5% developed vaginal extrusions. These were all managed successfully with sling excision and closure of the vagina. Two groups reported no evidence of extrusion or erosion at 1 year (Lee et al, 2009) and 3-year (Waltregny et al, 2008) follow-up. Waltregny and associates (2008) experienced one intraoperative vaginal sulcus laceration, which was closed uneventfully. Lee and colleagues (2009) presents a modified canal TOT approach, creating a suburethral tunnel between two oblique lateral incisions in the anterior vaginal wall to decrease the incidence of vaginal extrusion through the classic single midline incision. The value of this needs to confirmed by a randomized control trial.
Voiding Dysfunction
Postoperative voiding dysfunction has been noted to occur in 0% to 20.6% of patients after a TVT procedure (Pesschers et al, 2000). The incidence after TOT procedures varies between 2.1% and 6.7%. Although clinically there seems greater voiding dysfunction associated with a TVT than the TOT there is no significant difference in postoperative voiding dysfunction between the TVT and TOT in nonrandomized studies (Mansoor et al, 2003; de Tayrac et al, 2004). Urinary retention also appears to not be significantly different. The rate of obstructive symptoms after the TOT midurethral sling varies between 1.5% and 15.6% of patients. Tsivian and colleagues (2009) assessed the effect of concomitant vagina surgery on the outcomes of TOT placement. The group without concurrent vaginal surgery had no voiding dysfunction postoperatively, whereas 7 (11%) of the group who had additional pelvic surgery experienced voiding dysfunction. Three went on to require sling lysis for obstruction. After lysis, the continence rates were similar: 82.86% and 85.2%. Yang and associates (2009) identified morphologic features associated with functional impairment after a transobturator procedure. Among 98 women at a median follow-up of 22 months, 11 women had recurrent SUI, 22 had voiding dysfunction, and 12 had worsening or de novo urgency. A resting tape distance of less than 12 mm and urethral encroachment at rest were the variables predictive of postoperative voiding dysfunction. Bladder neck funneling was associated with postoperative urgency symptoms.
Urinary obstruction is usually transient and managed with short-term intermittent catheterization, although occasionally symptoms mandate tape release. Long-term retention after TVT is a rare complication (0.6% to 3.8%) and can be expected in the TOT population as well (deTayrac et al, 2004). Removal of the tape, in most cases, improves the patient’s symptoms. There has been some anecdotal experience with downward displacement of the tape under local anesthesia to provide symptomatic relief in patients with persistent voiding dysfunction (Ozel et al, 2004). Nonetheless, the overall risk of postoperative voiding dysfunction after the TOT is relatively low.
Management of MUI by a TOT sling has been discussed by three groups (Botros et al, 2007; Paick et al, 2008; Tahseen and Reed, 2009). Botros and coworkers (2007) compared the resolution of DO, UUI, and de novo urgency between the Monarc (125), TVT (99), and SPARC (52) procedures. De novo urgency was significantly lower in the Monarc group (8% vs. 33% TVT and 17% SPARC, P = .04), yet rates of resolution of DO, UUI, and de novo DO did not differ between the three groups. Paick and associates (2008) performed 72 TVT, 22 SPARC, and 50 TOT procedures in women with MUI. There were no significant differences in SUI cure rates or general urinary incontinence cure rates between the three slings. The presence of DO during preoperative UDS was associated with a high treatment failure of UUI in all three groups. Tahseen and associates (2009) performed a TOT procedure in 58 women and found a 77% SUI cure rate and 19% SUI improvement rate. UUI was additionally cured in 43% and improved in 36% of women suffering from MUI. Twenty-one percent had persistent UUI.
Pain
Another bothersome complication, unique to the TOT approach, is that of postoperative leg pain. de Leval (2003) described 15.9% of patients with temporary groin pain that resolved after the second postoperative day. Similarly, Krauth and associates (2005) reported 14 cases (2.3%) of patients with postoperative perineal groin pain. They also noted it to be transient and responding to nonsteroidal anti-inflammatory agents in all but 1 case. They hypothesized that the cause of the pain was either subclinical hematoma or a transient neuropathic phenomenon. They recommended that persistent leg pain that does not respond to conservative measures should prompt an investigation to exclude the possibility of erosion. Roth (2007) managed three women with persistent groin pain 3 months postoperatively in a similar fashion. Combined corticosteroids and local anesthetic was effective for pain relief, and no side effects were noted from the treatment. One case of failed sling and vaginal extrusion was reported by Mahajan and associates (2006). This patient additionally reported severe groin pain, fevers, and chills 10 days postoperatively. The tape was easily removed through the vaginal erosion, and mesh cultures were positive for Bacteroides fragilis. Complete symptom resolution occurred within 1 week of tape removal. Wolter and colleagues published a case report on recalcitrant medial thigh pain after TOT midurethral sling placement; the patient ultimately required medial thigh/TOT exploration by orthopedic surgery and sling excision (Wolter et al, 2008).
Key Points: Transobturator Midurethral Slings
Secondary or Salvage Procedure
There are limited data regarding the efficacy of midurethral slings as secondary surgery in women with recurrent incontinence. Five small studies with relatively short follow-up could be found addressing the issue (Azam et al, 2001; Rezapour and Ulmsten, 2001; Kuuva and Nilsson, 2002, 2003; Lo et al, 2002a; Rardin et al, 2002). Comparison of the studies is hampered by differences in the definitions used for cure, improved, and failed. The population of patients may be considered skewed by the inclusion of women in whom bulking agents failed. It is debatable whether women in whom bulking agents fail are the same as those in whom a surgical anti-incontinence procedure has failed. The methods of evaluating outcomes (objective, subjective, or both) also differ between studies. Despite these limitations between studies, cure rates of a midurethral sling after prior failed anti-incontinence surgery vary from 81% to 89.6%. Failure rates vary from 4.2% to 13%. In a review of these articles, several trends emerge: the procedure can be performed in the same way as it is performed for primary genuine SUI. The complication rate is similar to that of TVT done for primary SUI, but risk of bladder perforation appears to be higher in women who have had one or more prior retropubic suspensions. The failure rate is higher in women with immobile urethras, as is the case in primary surgery.
The longest follow-up of women who underwent TVT for recurrent incontinence is 4 years in a study by Rezapour and Ulmsten (2001). The 34 women studied had undergone 64 different anti-incontinence surgeries. Any patient with significant prolapse, DO, or ISD defined as a MUCP of less than 20 cm H2O was excluded. By physical examination, 24 women had a hypermobile urethra. Ten had a less mobile urethra, but none had a fixed urethra. The procedure was performed using the standard TVT technique, and only one bladder perforation occurred in a patient with a prior Marshall-Marchetti-Krantz urethroplasty. No significant complications were encountered. Twenty-eight (82%) were cured by objective and subjective parameters, 3 (9%) were improved based on failure to achieve more than 90% improvement in quality of life, and in 3 the procedure failed. Postoperative voiding dysfunction was negligible with no change in postvoid residual urine volume after 8 weeks. Long-term catheterization was not necessary in any patient. These results were durable up to 5 years.
The mechanism of failure in midurethral slings is typically misplacement of the suburethral tape or inadequate tension on the tape. There are a few reports of small numbers concerning recurrent incontinence after a midurethral sling in patients being treated with a repeat midurethral sling (Riachi et al, 2002; Villet et al, 2002; Lee et al, 2007a; Tsivian et al, 2007; Biggs et al, 2009). Reported cure rates of a midurethral sling after prior failed anti-incontinence surgery vary from 62.5% to 92.3%. Cure rates are higher for retropubic slings than for the TOT approach for recurrent SUI. Tsivian and associates (2007) found that in 12 patients with repeat midurethral sling the only procedure that failed was the TOT. Similarly, Lee and colleagues (2007a) found that the cure rate for the repeat TOT approach was 62.5% as compared with 92.3% for the repeat retropubic sling procedure. A possible explanation for this difference is the angle of the tape; specifically the retropubic sling has a U shape, which may be more supportive and obstructive than the TOT. Additionally, the outside-in approach to the TOT procedure may need wider dissection of the periurethral area, leading to future migration of the tape. Salvage procedures are performed on a portion of women who failed the initial midurethral sling due to underlying ISD or now have a fixed urethra from the initial surgery. This is consistent with the evidence of high success in retropubic slings for patients with a component of ISD.
New Technology: Single-Incision Transvaginal Slings
Surgical treatment of SUI has expanded to include a single-incision sling (TVT-S). This technology was first approved (Gynecare, TVT Secur) by the U.S. Food and Drug Administration in 2006 and has since included the AMS and MiniArc. There are little data available regarding the safety and efficacy of this new generation of slings. The ideal midurethral sling requires a short hospital stay, has rare and mild complications, provides a quick return to active life, and has high success rates.
Procedure
The device consists of a short 8 × 1.1-cm polypropylene laser-cut tape, the same material as a standard TVT, which is coated on both ends with an absorbable fleece material (Ethisorb). The absorbable material is made of polyglactin and polydioxanone. It is usually absorbable within 90 days, with polypropylene remaining intact to provide long-term fixation. A curved stainless steel inserter instrument and “release wire” is attached on both ends of the mesh. The implant may be placed under the midurethra and can be fixed in the “hammock” position (Fig. 73–14A) into the obturator internus muscle or in the U-shaped position (see Fig. 73–14B) into the connective tissue of the urogenital diaphragm behind the pubic bone (Meschia et al, 2009).
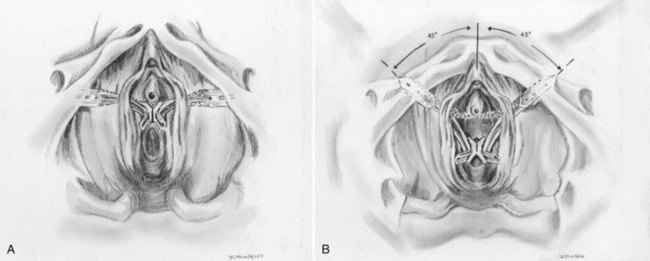
Figure 73–14 Midurethral sling as placed with single-incision approach. A, “Hammock.” B, “U” position.
The procedure is performed with the patient in the dorsal lithotomy position (with sequential compression devices in place) with a significant degree of flexion (70 degrees or more) of the thighs. A Foley catheter is placed before the repair to ensure the bladder is fully decompressed before passage of the device. As heretofore described, the patient has received parenteral sedation, and approximately 5 mL of 0.9% normal saline is used to hydrodistend the anterior vagina. After the vaginal incision is created, minimal dissection is performed using Metzenbaum scissors under the vaginal flaps on either side to elevate the vaginal epithelium from the underlying periurethral tissue to the level of the pubocervical fascia, which is not perforated. One inserter of the device is placed in the right dissection tunnel immediately beneath the vaginal epithelium and advanced up to the ischiopubic bone and into the internal obturator muscle, where the tape edges are anchored by the needle holder. The left side is introduced in the same way, creating a hammock-shaped sling. The definitive sling tension is achieved when the tip of a hemostat is easily passed between the urethra and the sling. Before engaging the sling by pulling the release wire, the patient is given indigo carmine and undergoes cystoscopy with a 30-degree rigid cystoscope. This step is essential to avoid the future morbidity of repeat surgery for intravesical or urethral mesh. Efflux of both ureteral orifices is confirmed. At this point the release wires are pulled with an empty needle driver and the inserters are removed on each side with a twisting motion of the hand. The authors’ experience suggests that the tension of the mini-slings should be tighter than in the classic TVT or TVT-O procedures to achieve the same result.
Anatomic Considerations
Like the TVT procedure, early attempts are being made at describing the anatomic localization and function of the TVT-S with cadaveric dissection and through ultrasound. Using 14 embalmed and 5 fresh frozen female bodies, Hubka and colleagues (2009) placed TVT-S inserters bilaterally. After dissection, they measured the distances from the obturator bundle (obturator nerve and vessels) and found that the mean distance of the TVT-S from the obturator bundle was 3.05 to 3.07 cm. Perforation of the fascia of obturator internus muscle occurred in 4.4% and they believed that injury to variable vessels could occur. The position of the TVT-S was not found to change with repositioning the legs. Ultrasound studies attempt to identify the dynamics behind the curative effects of the TVT-S. Martan and associates (2009) analyzed 85 patients after a TVT-S with perineal ultrasonography. Efficacy of the TVT-S was evaluated with cough test and validated questionnaire. Objectively, 62% had a negative cough test and 38% had persistent leakage. The TVT-S was noted to restrict urethral mobility, with a higher degree of obstruction associated with a higher likelihood of cure. This restrictive effect was noted to weaken within the first 3 months after surgery.
Results
There are nine prospective, often multi-institutional trials with minimum of 1-year follow-up reviewing the results of TVT-S and MiniArc slings. Dmochowski and colleagues (2009) report on the largest ongoing registry at 29 sites in eight countries. Effectiveness was measured by standing cough test and Incontinence Quality of Life (I-QOL) instrument. Six hundred forty-two women were studied, with 64.5% having a hammock placement and 35.5% having the U placement of the TVT-S. Of these women, 65.3% had pure SUI and 34.7% had MUI, with predominately stress symptoms. Intraoperative complications noted included one bladder perforation (0.2%) and 3 cases of bleeding more than 200 mL (0.5%). Postoperatively, there was one reported case of retention (0.2%), 10 UTIs (1.6%), 6 cases of voiding dysfunction (0.9%), and 15 cases of de novo urgency (2.3%). There were 5 cases of mesh erosion (0.8%). Improvements in quality of life at 3 months were sustained at 12 months. Objective incontinence with cough test was 11% at 6 months and 12.5% at 12 months, giving an objective cure rate of 87.5%.
Pickens and colleagues (2009) presented their initial experience with 120 MiniArc cases at 13 month follow-up. Success was defined as using no pads, with subjective outcomes assessed with the IIQ-7 and UDI-6 questionnaires. Thirty-five percent had concurrent UUI. At 13 months, 94% had complete resolution of SUI whereas 6 patients reported significant improvement and 1 patient experienced a treatment failure. Twenty-four percent reported resolution of their UUI. Three patients (0.4%) had intraoperative bladder perforations. Two patients experienced retention postoperatively: in 1 it resolved, and the other patient had a urethrolysis due to persistent retention.
Krofta and coworkers (2009) analyzed the efficacy and complications among 73 women using a cough stress test and validated questionnaires. There were no major perioperative complications or cases of urinary retention reported. Two patients had UTIs (2.9%) and 4 had wound infections (5.8%) within the first week after surgery. Mesh erosion occurred in 4 patients (6%). Subjective outcomes were cure of 58.2%, 23.9% improvement, and 17.9% failure. Objective cure rate was 51.5%. A second anti-incontinence procedure was performed in 8 patients (six TVT procedures, two Burch colposuspensions). These authors believe that the TVT-S was less effective than the TVT or TVT-O.
In a prospective, multicenter study of 154 women with TVT-S, Debodinance and associates (2009) reported cure rates of 70.3%, improvement in 11%, and failure in 18.7% at 1 year follow-up. MUI occurred in 31.8%. Perioperative complications included five hemorrhages, one bladder injury, one vaginal wound, 21 cases of elevated postvoid residual urine volume, and 1 woman with persistent groin pain. Two patients returned with vaginal extrusion of mesh and 1 with a granuloma. Cure of urgency was reported by 61.1%, whereas 12.3% reported de novo urgency. The overall cure rate did not change between 2 months and 1 year.
Neuman and associates (2008) performed a prospective observational study of 100 consecutive women with “hammock-style” TVT-S. The perioperative and 12-month postoperative data were compared between the first 50 patients and the last 50 patients. The objective failure rate went down from 20% to 8% between the two groups with the tape being placed closer to the urethra. Four (8%) patients in the first group had vaginal perforation with the inserter. This was avoided in the second group by widening the submucosal tunnel. The tape extrusion rate decreased from 12% to 8% by making deeper submucosal tunnels. There was one case of a paravesical self-remitting hematoma. Otherwise, the authors reported no cases of bladder or urethral perforation, UTI, wound infection, or intraoperative bleeding. At 12-month follow-up the objective cure rates between the two groups were 88.6% and 93.5%. Oliveira and colleagues (2009) provide 15-month follow-up of 107 patients with TVT-S. Fifteen percent had MUI, with predominant SUI symptoms. Seventy-one percent reported being dry, and 14% improved. Six (5.6%) patients presented with de novo urgency, and one case of vaginal mesh extrusion was reported. There were no cases of bowel injury, bladder perforation, hematuria, excessive bleeding, or hematoma formation. Meschia and coworkers (2009) used multiple validated questionnaires and cough test to assess 91 women after placement of TVT-S at 1-year follow-up. Fifty-five patients had a TVT-S in the hammock position, and 40 patients had it in the U position. These researchers reported subjective and objective cure rates of 78% and 81%, respectively. No bladder perforations were encountered. Two patients had intraoperative hemorrhage greater than 500 mL. Postoperative complications included 7 women with voiding difficulty (8%), 9 with recurrent UTIs (10%), 9 with de novo urgency (10%), and 2 with vaginal extrusions. Among the 20 with failed procedures, 8 patients went on to have a second anti-incontinence procedure (5 with retropubic TVT surgery, 2 with transobturator slings, 1 with a Reemex implant). Tartaglia and colleagues (2009) provide up to 18-month follow-up on 32 hammock-shaped TVT-S tapes. There were no surgical complications or reports of postoperative pain. One case of vaginal extrusion occurred. All 32 patients achieved continence based on quality of life assessment and physical examination. Jimenez and associates (2008) reported on their experience with both TVT-S and MiniArc slings in 41 patients with 1-year follow-up. The median follow-up in the TVT-S group was longer than the MiniArc group (328 days vs. 101 days). Only one bladder perforation was experienced in the TVT-S group. The reported cure rates were 80.4% in the TVT-S group and 90.2% in the MiniArc group. Ninety percent of the patients reported being satisfied at 3 months.
Four studies have compared mini-slings to standard midurethral slings (TVT or TVT-O). Using the TVT-WORLD observational registry, Tincello and colleagues (2009) compared 12-month outcomes of the TVT, TVT-O, and TVT-S procedures. The primary outcome measures are cough stress test and incontinence quality of life. The baseline characteristics, including proportions of MUI, were similar. TVT-S procedure patients returned to normal activities quicker than those who received either the TVT or TVT-O. Satisfaction rates were similar between the three groups. Objective cure rates were as follows: 90.6% TVT-S, 87.7% TVT, and 97.2% TVT-O. In regard to complications, all three techniques were similar.
Basu and Duckett (2009) performed a prospective, randomized control trial of the TVT versus the MiniArc in 70 women with 6-month follow-up. The MiniArc group had statistically lower subjective cure rates and urodynamic SUI cure rates than the TVT group: 63.3% vs. 100% and 45% vs. 93%, respectively. At 6-month follow-up, 50% of the MiniArc population had urodynamic SUI versus 7% of the TVT group. Two groups reported on randomized control trials of the TVT-O versus the TVT-S (Hinoul et al, 2009; Jarmi-Di et al, 2009). Jarmy-Di and associates (2009) observed the early postoperative results at 30 days. Two patients in the TVT-S group had temporary urinary retention, and 1 patient in the TVT-O group had leg pain. There were no UTIs or evidence of de novo urgency within this month period. No early mesh erosions were reported. Hinoul and associates (2009) performed a 12-month study of 135 randomized women (70 TVT-O and 65 TVT-S). Quality of life and subjective outcomes were reported using validated questionnaires. One bladder perforation occurred in the TVT-O group. The self-reported cure rates for the TVT-O were significantly higher than for the TVT-S (91.5% vs. 78.5%, P = .02), yet the TVT-S procedure was associated with less pain in the first week postoperatively. This pain difference disappeared within 2 weeks. Based on short-term follow-up, the single incision slings are a valuable addition, providing short hospital stays, quicker return to active life, and success rates equal to the TVT and TVT-O procedures. Their appeal is the single incision, avoidance of the retropubic space, and prevention of thigh pain. Most importantly, patients thus far appear to have reduced discomfort in the postoperative period. Long-term, comparative data collection is necessary to establish the efficacy and durability of these procedures.
Abouassaly R, Steinberg J, Lemieux M, et al. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004;94:110-113.
Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:2143-2155.
Anger JT, Weinberg AE, Albo ME, et al. Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. J Urol. 2009;74(2):283-287.
Blaivas JG, Sandhu J. Urethral reconstruction after erosion of slings in women. Curr Opin Urol. 2004;14:335-338.
Campeau L, Tu LM, Lemieux MC, et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn. 2007;26:990-994.
Chaikin DC, Rosenthal J, Blaivas JG. Pubovaginal fascial sling for all types of stress urinary incontinence: long-term analysis. J Urol. 1998:1312-1316.
Chou EC, Flisser AJ, Panagopoulos G, Blaivas JG. Effective treatment for mixed urinary incontinence with a pubovaginal sling. J Urol. 2003;170:494-497.
deTayrac R, Deffieux X, Droupy S, et al. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190:602-608.
Doo CK, Hong B, Chung BJ, et al. Five-year outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence. Eur Urol. 2006;50:333-338.
Klutke C, Siegel S, Carlin B, et al. Urinary retention after tension-free vaginal tape procedure: incidence and treatment. Urology. 2001;58:697-701.
Kulseng-Hanssen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:391-396.
Kuuva N, Nilsson C. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 2002;81:72-77.
Kuuva N, Nilsson C. Tension-free vaginal tape procedure: an effective minimally invasive operation for the treatment of recurrent stress urinary incontinence? Gynecol Obstet Invest. 2003;56:93-98.
Laurikainen E, Killholma P. A nationwide analysis of transvaginal tape release for urinary retention after tension-free vaginal tape procedure. Int Urogynecol J. 2006;17:111-119.
Leach G, Dmochowski R, Appell R, et al. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. J Urol. 1997;158:875-880.
Lee KS, Han DH, Choi YS, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year follow-up. J Urol. 2007;177:214-218.
Lemack GE, Krauss S, Litman H, et al. Normal postoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. J Urol. 2008;180:2076-2080.
Mansoor A, Vedrine N, Darcq C. Surgery of female urinary incontinence using trans-obturator tape (TOT): a prospective randomized comparative study with TVT. Neurourol Urodyn. 2003;22:488-489.
Meltomaa S, Backman T, Haarala M. Concomitant vaginal surgery did not affect outcome of the tension-free vaginal tape operation during a prospective 3-year follow up study. J Urol. 2004;172:222-226.
Neuman M. TVT-obturator: short-term data on the operative procedure for the cure of female stress urinary incontinence performed on 300 patients. Eur Urol. 2007;51:1083-1088.
Nilsson C, Falconer C, Rezapour M. Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004;104:1259-1262.
Petros P, Ulmsten U. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993;153:1-93.
Porena M, Constantini E, Frea B, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomized trial. Eur Urol. 2007;52:1481-1491.
Sokol A, Jelovsek J, Walters M, et al. Incidence and predictors of prolonged urinary retention after TVT with and without concurrent prolapse surgery. Am J Obstet Gynecol. 2005;192:1537-1543.
Tamussino K, Hanzal E, Kölle D, et al. Tension-free vaginal tape operation: results of the Austrian registry. Obstet Gynecol. 2001;98:732-736.
Waltregny D, Gaspar Y, Reul O, et al. TVT-O for the treatment of female stress urinary incontinence: results of prospective study after a 3-year minimum follow-up. Eur Urol. 2008;53:401-410.
Ward K, Hilton P. Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow-up. Br J Obstet Gynaecol. 2008;115:226-233.
Woodruff AJ, Cole EE, Dmochowski RR, et al. Histologic comparison of pubovaginal sling graft materials: a comparative study. Urology. 2008;72(1):85-89.
Abdel-Fattah M, Barrington JW, Arunkalaivanan AS. Pelvicol versus tension-free vaginal tape for treatment of urodynamic stress incontinence: a prospective randomized three-year follow-up study. Eur Urol. 2004;46:629-635.
Abouassaly R, Steinberg J, Lemieux M, et al. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004;94:110-113.
Adamiak A, Milart P, Skorupski P, et al. The efficacy and safety of the tension-free vaginal tape procedure do not depend on the method of analgesia. Eur Urol. 2002;42:29-33.
Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:2143-2155.
Aldridge AH. Transplantation of fascia for relief of urinary stress incontinence. Am J Obstet Gynecol. 1942;44:398.
Allahdin S, McKinley C, Mahmood T. Tension free vaginal tape: a procedure for all ages. Acta Obstet Gynecol Scand. 2004;83:937-940.
Almeida SHM, Gregorio E, Grando JPS, et al. Pubovaginal sling using cadaveric allograft fascia for the treatment of female urinary incontinence. Transplant Proc. 2004;36:995-996.
Al-Singary W, Shergill IS, Allen SE, et al. Trans-obturator tape for incontinence: a 3-year follow-up. Urol Int. 2007;78:198-201.
Al-Wadi K, Al-Badr A. Martius graft for the management of tension-free vaginal tape vaginal erosion. Obstet Gynecol. 2009;114:489-491.
American Urological Association Female Stress Urinary Incontinence Clinical Guidelines Panel. Report on the surgical management of female stress urinary incontinence. April 1997.
Amid PK. Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia. 1997;1:15-21.
Amid PK, Shulman AG, Lichtenstein IL. Selecting synthetic mesh for the repair of groin hernia. Postgrad Gen Surg. 1992;4:1505.
Amundsen C, Flynn B, Webster G. Urethral erosion after synthetic and nonsynthetic pubovaginal slings: differences in management and continence outcome. J Urol. 2003;170:134-137.
Amundsen CL, Guralnick ML, Webster GD. Variations in strategy for the treatment of urethral obstruction after a pubovaginal sling procedure. J Urol. 2000;164:434-437.
Amundsen CL, Visco AG, Ruiz H, et al. Outcome in 104 pubovaginal slings using freeze-dried allograft fascia lata from a single tissue bank. Urology. 2000;56(Suppl. 6A):2-8.
Andonian S, Chen T, St-Denis B, Corcos J. Randomized clinical trial comparing suprapubic arch sling (SPARC) and tension-free vaginal tape (TVT): one-year results. Eur Urol. 2005;47:537-541.
Anger JT, Litwin MS, Wang Q, et al. Complications of sling surgery among female Medicare beneficiaries. Obstet Gynecol. 2007;109:707-714.
Anger JT, Litwin MS, Wang Q, et al. Variations in stress incontinence and prolapsed management by surgeon specialty. J Urol. 2007;178:1411-1417.
Anger JT, Litwin MS, Wang Q, et al. The effect of concomitant prolapse repair on sling outcomes. J Urol. 2008;180:1003-1006.
Anger JT, Weinberg AE, Albo ME, et al. Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. J Urol. 2009;74(2):283-287.
Appell RA. In situ vaginal wall sling. Urology. 2000;56:499-503.
Arunkalaivanan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol implant) vs. tension-free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire-based study. Int Urogynecol J. 2003;14:17-23.
Arya LA, Myers DL, Jackson ND. Office screening test for intrinsic urethral sphincter deficiency: pediatric Foley catheter test. Obstet Gynecol. 2001;97:885-889.
Asmussen M, Ulmsten U. On the physiology of continence and pathophysiology of stress incontinence in the female. Contrib Gynecol Obstet. 1983;10:32-50.
Athanasiou S, Grigoriadis T, Kalamara E, et al. Mixed urodynamic incontinence: TVT or TVT-O? Int Urogynecol J. 20, 2009. 34th annual IUGA meeting, abstract 173 (S218)
Atherton M, Staton S. TVT and colposuspension: comparisons and contrasts of possible mechanism. Neurourol Urodyn. 2000;19:396-398.
Austin PF, Westney OL, Leng WW, et al. Advantages of rectus fascial slings for urinary incontinence in children with neuropathic bladders. J Urol. 2001;165:2369-2371.
Azam U, Frazier M, Kozman E, et al. The tension-free vaginal tape procedure in women with previous failed stress incontinence surgery. J Urol. 2001;166:554-556.
Babalola EO, Famuyide AO, McGuire LJ, et al. Vaginal erosion, sinus formation and ischiorectal abscess following transobturator tape: ObTape implantation. Int Urogynecol J Pelvic Floor Dysfunction. 2005;17:418-421.
Bafghi A, Valerio L, Trastour C, et al. Evaluation of the TVT technique according to age. J Gynecol Obstet Biol Reprod (Paris). 2005;34:47-52.
Bai SW, Sohn WH, Chung DJ, et al. Comparison of the efficacy of Burch colposuspension, pubovaginal sling and tension-free vaginal tape for stress urinary incontinence. Int J Gynaecol Obstet. 2005;91:246-251.
Balakrishnan S, Lim YN, Barry C, et al. Sling distress: a subanalysis fo the IVS tapes from the SUSPEND trial. Aust NZ J Obstet Gynecol. 2007;47:496-498.
Ballert KN, Biggs GY, Isenalumhe AJr, et al. Managing the urethra at transvaginal pelvic organ prolapse repair: a urodynamic approach. J Urol. 2009;181:679-684.
Ballert KN, Kanofsky JA, Nitti VW. Effect of tension-free vaginal tape and TVT-obturator on lower urinary tract symptoms other than stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:335-340.
Baracat F, Mitre AI, Kanashiro H, Montellato NI. Endoscopic treatment of vesical and urethral perforations after tension-free vaginal tape (TVT) procedure for female stress urinary incontinence. Clinics (São Paulo). 2005;60:397-400.
Barnes NM, Dmochowski RR, Park R, Nitti VW. Pubovaginal sling and pelvic prolapse repair in women with occult stress urinary incontinence: effect on postoperative emptying and voidng symptoms. Urology. 2002;59(6):856-860.
Basu M, Duckett J. Tension-free vaginal tape for stress incontinence in women with detrusor overactivity. Int Urogynecol J. 2007;18:1097-1099.
Basu M, Duckett J. A randomized trial of the surgical treatment of urodynamics stress incontinence—the TVT versus MiniArc. Int Urogynecol J. 2009;20:S74. abstract 003
Beck RP, McCormick S, Nordstrom L. The fascia lata sling procedure for treating recurrent genuine stress incontinence of urine. Obstet Gynecol. 1988;72:699-703.
Bent AE, Ostergard DR, Zwick-Zaffuto MT. Tissue reaction to expanded polytetrafluoroethylene suburethral sling for urinary incontinence: clinical and histologic study. Am J Obstet Gynecol. 1993;169:1198-1204.
Bidmead J, Cardozo L. Sling techniques in the treatment of genuine stress incontinence. Br J Obstet Gynecol. 2000;107:147-156.
Biggs GY, Baller KN, Rosenblum N, Nitti V. Patient-reported outcomes for tension-free vaignal tape-obturator in women treated with a previous anti-incontinence procedure. Int Urogynecol J. 2009;20:331-335.
Blaivas JG. Pubovaginal slings. In: Kursh ED, McGuire EJ, editors. Female urology. Philadelphia: JB Lippincott; 1994:235.
Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn. 2000;19:553-564.
Blaivas JG, Heritz DM. Vaginal flap reconstruction of the urethra and vesical neck in women: a report of 49 cases. J Urol. 1996;155:1014-1017.
Blaivas JG, Jacobs BZ. Pubovaginal fascial sling for the treatment of complicated stress urinary incontinence. J Urol. 1991;145:1214-1218.
Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. J Urol. 1988;139:727-731.
Blaivas JG, Sandhu J. Urethral reconstruction after erosion of slings in women. Curr Opin Urol. 2004;14:335-338.
Bobyn JD, Wilson GJ, MacGregor DC, et al. Effect of pore size on the peel strength of attachement of fibrous tissue to porous-surfaced implants. J Biomed Mater Res. 1982:571-584.
Bodelsson G, Henriksson L, Osser S, et al. Short term complications of the tension-free vaginal tape operation for stress urinary incontinence in women. Br J Obstet Gynaecol. 2002;109:566-569.
Bonnet P, Waltregny D, Reul O, et al. Transobturator vaginal tape inside out for the surgical treatment of female stress urinary incontinence: anatomical considerations. J Urol. 2005;173:1223-1228.
Botros SM, Miller JJ, Goldberg RP, et al. Detrusor overactivity and urge urinary incontinence following transobturator versus midurethral slings. Neurourol Urodyn. 2007;26:42-45.
Bradley CS, Morgan MA, Arya LA, Rovner ES. Vaginal erosion after pubovaginal sling procedures using dermal allografts. J Urol. 2003;169:286-287.
Brown SL, Govier FE. Cadaveric versus autologous fascia lata for the pubovaginal sling: surgical outcome and patient satisfaction. J Urol. 2000;164:1633-1637.
Campeau L, Tu LM, Lemieux MC, et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn. 2007;26:990-994.
Carbone JM, Kavaler E, Hu JC, Raz S. Pubovaginal sling using cadaveric fascia and bone anchors: disappointing early results. J Urol. 2001;165:1605-1611.
Carey J, Leach GE. Transvaginal surgery in the octogenarian using cadaveric fascia for pelvic prolapsed and stress incontinence: minimal one-year results compared to younger patients. Urology. 2004;63:665-670.
Carr LK, Webster GD. Voiding dysfunction following incontinence surgery: diagnosis and treatment with retropubic or vaginal urethrolysis. J Urol. 1997;157:821-823.
Centers for Disease Control and Prevention (CDC). Hepatitis C virus transmission from an antibody-negative organ and tissue donor—United States, 2000-2002. MMWR Morb Mortal Wkly Rep. 2003;52:273-274.
Chaikin DC, Blaivas JG. Weakened cadaveric fascial sling: an unexpected cause of failure. J Urol. 1998;160:2151.
Chaikin DC, Rosenthal J, Blaivas JG. Pubovaginal fascial sling for all types of stress urinary incontinence: long-term analysis. J Urol. 1998:1312-1316.
Chaliha C, Stanton SL. Complications of surgery for genuine stress incontinence. Br J Obstet Gynaecol. 1999;106:1238-1245.
Chancellor MB, Erhard MJ, Kiilholma PJ, et al. Functional urethral closure with pubovaginal sling for destroyed female urethra after long-term urethral catheterization. Urology. 1994;43:499-505.
Chen HY, Ho M, Hung YC, Huang LC. Analysis of risk factors associated with vaginal erosion after synthetic sling procedures for stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:117-121.
Chen Z, Chen Y, Du GH, et al. Comparison of three kinds of mid-urethral slings for surgical treatment of female stress urinary incontinence. Urologia. 2010;77(1):37-41.
Chene G, Cotte B, Tardieu A, et al. Clinical and ultrasonographic correlations following three surgical anti-incontinence procedures (TOT, TVT and TVT-O). Int Urogynecol J. 2008;19:1125-1131.
Chilaka V, Amu O, Mayne C. Factors affecting outcome of colposuspension. J Obstet Gynaecol. 2002;22:72-74.
Choe JM, Bell T. Genetic material is present in cadaveric dermis and cadaveric fascia lata. J Urol. 2001;166:122-124.
Chou EC, Flisser AJ, Panagopoulos G, Blaivas JG. Effective treatment for mixed urinary incontinence with a pubovaginal sling. J Urol. 2003;170:494-497.
Cindolo L, Salzano L, Rota G, et al. Tension-free transobturator approach for female stress urinary incontinence. Minerva Urol Nefrol. 2004;56:89-98.
Clemens JL, La Sala CA. The tension-free vaginal tape in women with a nonhypermobile urethra and low maximum urethral closure pressure. Int Urogynecol J Pelvic Floor Dysfunction. 2007;18:727-732.
Clemens JQ, DeLancey JO, Faerber GJ, et al. Urinary tract erosions after synthetic pubovaginal slings: diagnosis and management strategy. Urology. 2000;56:589-595.
Connolly TP. Necrotizing surgical site infection after tension-free vaginal tape. Obstet Gynecol. 2004;104:1275-1276.
Costa P, Grise P, Droupy S, et al. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T.O.T.) UraTape: short term results of a prospective multicentric study. Eur Urol. 2004;46:102-107.
Couillard D, Deckard-Janatpour KA, Stone AR. The vaginal wall sling: a compressive suspension procedure for recurrent incontinence in elderly patients. Urology. 1994;43:203-208.
Crivellaro S, Smith JJ, Kocjancic E, Bresette JF. Transvaginal sling using acellular human dermal allograft: safety and efficacy in 253 patients. J Urol. 2004;172:1374-1378.
Cross CA, Cespedes RD, English SF, et al. Transvaginal urethrolysis for urethral obstruction after anti-incontinence surgery. J Urol. 1998;159:1199-1201.
Cross CA, Cespedes RD, McGuire EJ. Treatment results using pubovaginal slings in patients with large cystoceles and stress incontinence. J Urol. 1997;158:431-434.
Cundiff GW, Harris RL, Coates KW, Bump RC. Clinical predictors of urinary incontinence in women. Am J Obstet Gynecol. 1997;177:262-266.
Daneshgari F, Kong W, Swartz M. Complications of midurethral slings: important outcomes for future clinical trials. J Urol. 2008;180:1890-1897.
Darai E, Jeffry L, Deval B, et al. Results of tension-free vaginal tape in patients with or without vaginal hysterectomy. Eur J Obstet Gynecol Reprod Biol. 2002;103:163-167.
de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44:724-730.
de Tayrac R, Deffieux X, Droupy S, et al. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190:602-608.
de Tayrac R, Madelenat P. Evolution of surgical routes in female stress urinary incontinence. Gynecol Obstet Fertil. 2004;32:1031-1038.
Dean N, Herbison P, Ellis G, Wilson D. Laparoscopic colposuspension and tension-free vaginal tape: a systematic review. Br J Obstet Gynaecol. 2006;112:1345-1353.
Debodinance P, Amblard J, Lucot JP, et al. TVT Secur: prospective study and follow up at 1 year about 154 patients. J Gynecol Obstet Biol Reprod (Paris). 2009;38:299-303.
Defreitas G, Herschorn S. Unilateral pubovaginal sling release: a minimally invasive transvaginal approach. J Urol. 2000;163(Suppl.):74.
DeLancey JO. Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol. 1994;170:1713-1723.
Dell J, O’Kelley K. TVT erosion secondary to a twist in tape. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:168-169.
Delmas V, Hermieu J, Dompeyre P, et al. The UraTape transobturator sling in the treatment of female stress urinary incontinence: mechanism of action. Eur Urol. 196, 2003.
Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306-1313.
Delorme E, Droupy S, de Tayrac R, et al. Transobturator tape (UraTape): a new minimally invasive method in the treatment of urinary incontinence in women. Prog Urol. 2003;13:656-659.
Demirkesen O, Onal B, Tunc B, et al. Does vaginal anti-incontinence surgery affect sexual satisfaction? A comparison of TVT and Burch-colposuspension. Int Braz J Urol. 2008;34:214-219.
Descurtins M, Buchmann P. Bovine pericardium—a new graft material for hernial repair (author’s transl). Res Exp Med (Berl). 1982;180:11-14.
DeSouza R, Shapiro A, Westney OL. Adductor brevis myositis following transobturator tape procedure: a case report and review of the literature. Int Urogynecol J Pelvic Floor Dysfunction. 2007;18:817-820.
Deval B, Ferchaux J, Berry R, et al. Objective and subjective cure rates after trans-obturator tape (ObTape) treatment of female urinary incontinence. Eur Urol. 2006;49:373-377.
Dietz HP, Vancaille P, Svehla M, et al. Mechanical properties of implant materials used in incontinence surgery. International Continence Society 31st Annual Meeting proceedings, Seoul, Korea, September 18-21, 2001.
Dietz HP, Vancaillie P, Svehla M, et al. Mechanical properties of urogynecologic implant materials. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:239-243.
Dietz HP, Wilson PD. The “iris effect”: how two-dimensional and three-dimensional ultrasound can help us understand anti-incontinence procedure. Ultrasound Obstet Gynecol. 2004;23:267.
Digesu GA, Hendricken C, Fernando R, Khullar V. Do women with pure stress urinary incontinence need urodynamics? Urology. 2009;74(2):278-281.
Dmochowski RR, Grier D, Franco N. One year results from a world-wide registry of TVT-Secur in women with stress urinary incotninence [annual meeting abstract]. J Urol. 2009;181:544. abstract 1520
Dobson A, Robert M, Swaby C, et al. Trans-obturator surgery for stress urinary incontinence: 1-year follow-up of a cohort of 52 women. Int Urogynecol J Pelvic Floor Dysfunction. 2007;18:27-32.
Domingo S, Alama P, Ruiz N, et al. Diagnosis, management and prognosis of vaginal erosion after transobturator suburethral tape procedure using a nonwoven thermally bonded polypropylene mesh. J Urol. 2005;173:1627-1630.
Doo CK, Hong B, Chung BJ, et al. Five-year outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence. Eur Urol. 2006;50:333-338.
Dora CD, Dimarco DS, Zobitz ME, et al. Time dependent variations in biomechanical properties of cadaveric fascia, porcine dermis, porcine small intestine submucosa, polypropylene mesh, and autologous fascia in the rabbit model. J Urol. 2004;171:1970-1973.
Duckett J, Aggarwal I, Patil A, Vella M. Effect of tension-free vaginal tape position on the resolution of irritative bladder symptoms in women with mixed incontinence. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:237-239.
Duckett J, Basu M. The predictive value of preoperative pressure-flow studies in the resolution of detrusor overactivity and overactive bladder after tension-free vaginal tape insertion. BJU Int. 2007;99:1439-1442.
Duckett J, Constantine G. Complications of silicone insertion for stress urinary incontinenence. J Urol. 2000;163:1835-1837.
Duckett JR, Jain S. Groin pain after a tension-free vaginal tape or similar suburethral sling: management strategies. BJU Int. 2005;95:95-97.
Dwyer NT, Kreder KJ. Fascia lata sling. In: Raz S, Rodriguez LV, editors. Female urology. 3rd ed. Philadelphia: Saunders Elsevier; 2008:409-410.
El-Barky E, El-Shazly A, El-Wahab OA, et al. Tension free vaginal tape versus Burch colposuspension for treatment of female stress urinary incontinence. Int Urology Nephrol. 2005;37:277-281.
Faerber GJ. Urethral diverticulectomy and pubovaginal sling for simultaneous treatment of urethral diverticulum and intrinsic sphincter deficiency. Tech Urol. 1998;4:192-197.
FitzGerald MP, Mollenhauer J, Bitterman P, et al. Functional failure of fascia lata allografts. Am J Obstet Gynecol. 1999;181(6):1339-1344.
FitzGerald MP, Brubaker L. The etiology of urinary retention after surgery for genuine stress incontinence. Neurourol Urodyn. 2001;20:13.
FitzGerald MP, Mollenhauer J, Brubaker L. The fate of rectus fascia suburethral slings. Am J Obstet Gynecol. 2000;183:964-966.
Flisser AJ, Blaivas JG. Outcome of urethral reconstruction surgery in series of 74 women. J Urol. 2003;169:2246-2249.
Flock F, Reich A, Muche R, et al. Hemorrhagic complications associated with tension-free vaginal tape procedure. Obstet Gynecol. 2004;104:989-994.
Flynn BJ, Yap WT. Pubovaginal sling using allograft fascia lata versus autograft fascia for all types of stress urinary incontinence: 2-year minimum follow-up. J Urol. 2002;167:608-612.
Forse RA, Karam B, MacLean LD, et al. Antibiotic prophylaxis for surgery in morbidly obese patients. Surgery. 1989;106:750-756.
Foster HE, McGuire EJ. Management of urethral obstruction with transvaginal urethrolysis. J Urol. 1993;150:1448-1451.
Frangenheim P. Zur operative Behaundlung der Inkontinenz der Mannlichen Harnohre. Verh Dtsch Ges Chir. 1914;43:149.
Frederick RW, Leach GE. Cadaveric prolapsed repair with sling: intermediate outcomes with 6 months to 5 years of followup. J Urol. 2005;173:1229-1233.
Fritel X, Fauconnier A, Pigne A. Circumstances of leakage related to low urethral closure pressure. J Urol. 2008;180:223-226.
Fritel X, Zabak K, Pigne A, et al. Predictive value of urethral mobility before suburethral tape procedure for urinary stress incontinence in women. J Urol. 2002;168:2472-2475.
Fulford SCV, Flynn R, Barrington J, et al. An assessment of the surgical outcome and urodynamic effects of the pubovaginal sling for stress incontinence and the associated urge syndrome. J Urol. 1999;162:135-137.
Gallantine ML, Cespedes RD. Review of cadaveric allografts in urology. Urology. 2002;59:318.
Gallup DG, Freedman MA, Meguiar RV, et al. Necrotizing fasciitis in gynecologic and obstetric patients: a surgical emergency. Am J Obstet Gynecol. 2002;187:305-310.
Gamble TL, Botros SM, Beaumont JL, et al. Predictors of persistent detrusor overactivity after transvaginal sling procedures. Am J Obstet Gynecol. 2008;199:696.
Gamé X, Mouzin M, Vaessen C, et al. Obturator infected hematoma and urethral erosion following transobturator tape implantation. J Urol. 2004;171:1629.
Gamé X, Soulié M, Malavaud B, et al. Treatment of bladder outlet obstruction secondary to suburethral tape by section of the tape. Prog Urol. 2006;16:67-71.
Gateau T, Faramarzi-Roques R, Le Normand L, et al. Clinical and urodynamic repercussions after TVT procedure and how to diminish patient complaints. Eur Urol. 2003;44:372-376.
Ghezzi F, Serati M, Cromi A, et al. Tension-free vaginal tape for the treatment of urodynamic stress incontinence with intrinsic sphincteric deficiency. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):335-339.
Ghoniem GM. Modified pubovaginal sling for treatment of complicated stress urinary incontinence in females. AUA Today. 1991;4:5.
Ghoniem GH, Elgamasy A. Simplified surgical approach to bladder outlet obstruction following pubovaginal sling. J Urol. 1995;154:181-183.
Ghoniem GH, Hassouna ME. Bladder neck prop using vaginal wall island for intrinsic sphincteric deficiency in elderly patients: a new technique. Urology. 1998;52:668-671.
Giberti C, Gallo F, Cortese P, Schenone M. Transobturator tape for treatment of female stress urinary incontinence: objective and subjective results after a mean follow-up of two years. Urology. 2007;69:703-707.
Gillon G, Stanton SL. Long-term follow up of surgery for urinary incontinence in elderly women. Br J Urol. 1984;56:478-481.
Giri SK, Drumm J, Flood HD. Endoscopic holmium laser excision of intravesical tension-free vaginal tape and polypropylene suture after anti-incontinence procedures. J Urol. 2005;174(4 Pt. 1):1306-1307.
Giri SK, Hickey JP, Sil D, et al. The long-term results of pubovaginal sling surgery using acellular cross-linked porcine dermis in the treatment of urodynamic stress incontinence. J Urol. 2006;175:1788-1793.
Giri SK, Sil D, Narasimhulu G, et al. Management of vaginal extrusion after tension-free vaginal tape procedure for urodynamics stress incontinence. Urology. 2007;69:1077-1080.
Glavind K, Glavind E. Treatment of prolonged voiding dysfunction after tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2007;86:357-360.
Glavind K, Sander P. Erosion, defective healing and extrusion after tension-free urethropexy for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:179-182.
Goebell R. Zur operativen Beseitgung der angeborenen Incontinentia Vesicae. Dtsch Gynakol Urol. 1910;2:187-191.
Goldman HB. Simple sling incision for the treatment of iatrogenic urethral obstruction. Urology. 2003;62:713-718.
Goldman HB. Large thigh abscess after placement of synthetic transobturator sling. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(3):295-296.
Goldman HB, Rackley RR, Appell RA. The efficacy of urethrolysis without re-suspension for iatrogenic urethral obstruction. J Urol. 1999;161:1268-1271.
Golomb J, Groutz A, Mor Y, et al. Management of urethral erosion caused by a pubovaginal fascial sling. Urology. 2001;57:159-160.
Gomelsky A, Scarpero HM, Dmochowski RR. Sling surgery for stress urinary incontinence in the female: what surgery, which material?, vol 22. American Urological Association, Houston, TX, 2003. 267–75 AUA Update Series, lesson 34
Gordon D, Gold R, Pauzner D, et al. Tension-free vaginal tape in the elderly: is it a safe procedure? Urology. 2005;65:479-482.
Gormley EA, Bloom DA, McGuire EJ, et al. Pubovaginal slings for management of urinary incontinence in female adolescents. J Urol. 1994;152:822-825.
Govier FE, Gibbons RP, Correa RJ, et al. Pubovaginal slings using fascia lata for the treatment of intrinsic sphincter deficiency. J Urol. 1997;157:117-121.
Griffiths D, Kondo A, Bauer S, et al. Dynamic testing. In: Abrams P, Cardozo L, Khouri S, et al, editors. Incontinence: volume 1: basics and evaluation. Plymouth, UK: Health Publication Ltd.; 2005:587-674.
Groutz A, Blaivas JG, Hyman MJ, Chaikin DC. Pubovaginal sling surgery for simple stress urinary incontinence: analysis by an outcome score. J Urol. 2001;165:1597-1600.
Groutz A, Gold R, Pauzner D, et al. Tension-free vaginal tape (TVT) for the treatment of occult stress urinary incontinence in women undergoing prolapse repair: a prospective study of 100 consecutive cases. Neurourol Urodyn. 2004;23:632-635.
Gutierrez Banos JL, Martin Garcia B, Portillo Martin JA, et al. [Usefulness of abdominal leak point pressure determination in the diagnosis of female urinary incontinence in the TVT era]. Actas Urol Esp. 2004;28:506-512. in Spanish
Haab F, Trockman BA, Zimmern PE, Leach GE. Results of pubovaginal sling for the treatment of intrinsic sphincter deficiency determined by questionnaire analysis. J Urol. 1997:1738-1741.
Haferkamp A, Steiner G, Muller S, et al. Urethral erosion of tension-free vaginal tape. J Urol. 2002;167:250.
Hammad FT, Kennedy-Smith A, Robinson RG. Erosions and urinary retention following polypropylene synthetic sling: Australasian Survey. Eur Urol. 2005;47:641-647.
Handa V, Jensen JK, Germain MM, Ostergard DR. Banked human fascia lata for suburethral sling procedure: a preliminary report. Obstet Gynecol. 1996;88:1045-1049.
Handa VL, Stone A. Erosion of a fascial sling into the urethra. Urology. 1999;54(5):923.
Hassouna ME, Ghoniem GM. Long-term outcome and quality of life after modified pubovaginal sling for intrinsic sphincteric defiency. Urology. 1999;53:287-291.
Hassouna VL, Stone A. Erosion of a fascial sling into the urethra. Urology. 1999;54:923.
Hathaway JK, Choe JM. Intact genetic material is present in commercially processed cadaveric allografts used for pubovaginal slings. J Urol. 2002;168:1040-1043.
Hellberg D, Holmgren C, Lanner L, Nilsson S. The very obese women and the very old women: tension-free vaginal tape for the treatment of stress urinary incontinence. Int Urogynecol J. 2007;18:423-429.
Hermieu JF, Messas A, Delmas V, et al. [Bladder injury after TVT transobturator]. Prog Urol. 2003;13:115-117. in French
Hinoul P, Vervest HA, Venema P, et al. TVT obturator system versus TVT Secur: a randomized controlled trail, short term results. Int Urogynecol J. 2009;20:S213. abstract 166
Hinton R, Jinnah RH, Johnson C, et al. A biomechanical analysis of solvent-dehydrated and freeze dried human fascia lata allograft: a preliminary report. Am J Sports Med. 1992;20:607-612.
Ho K-LV, Witte M, Bird ET. 8-Ply small intestinal submucosa tension-free sling: spectrum of postoperative inflammation. J Urol. 2004;171:268-271.
Hodroff M, Portis A, Siegel S. Endoscopic removal of intravesical polypropylene sling with the holmium laser. J Urol. 2004;172:1361-1362.
Holmgren C, Nilsson S, Lanner L, et al. Long term results with tension-free vaginal tape on mixed and stress urinary incontinence. Obstet Gynecol. 2005;106:38-43.
Hong B, Park S, Kim HS, et al. Factors predictive of urinary retention after a tension-free vaginal tape procedure for female stress urinary incontinence. J Urol. 2003;170:852-856.
Hosker G. Is it possible to diagnose intrinsic sphincter deficiency in women? Curr Opin Urol. 2009;19:342-346.
Howden NS, Zyczynski HM, Moalli PA, et al. Comparison of autologous rectus fascia and cadaveric fascia in pubovaginal sling continence outcomes. Am J Obstet Gynecol. 2006;194:1444-1449.
Hsu TH, Rackley RR, Appell RA. The supine stress test: a simple method to detect intrinsic sphincter deficiency. J Urol. 1999;162:460-463.
Huang K, Kung F, Liang H, et al. Concomitant surgery with tension-free vaginal tape. Acta Obstet Gynecol Scand. 2003;82:948-953.
Huang K, Kung F, Liang H, et al. Management of polypropylene mesh erosion after intravaginal midurethral sling operation for female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(6):437-440.
Huang WC, Yang JM. Bladder neck funneling on ultrasound cystourethrography in primary stress urinary incontinence: a sign associated with urethral hypermobility and intrinsic sphincter deficiency. Urology. 2003;61:936-941.
Huang Y, Lin ATL, Chen K, et al. High failure rate using allograft fascia lata in pubovaginal sling surgery for female stress urinary incontinence. Urology. 2001;58:943-946.
Hubka P, Masata J, Nanka O, et al. Anatomical relationship and fixation of tension-free vaginal tape Secur. Int Urogynecol J Pelvic Floor Dysfunction. 2009;20:681-688.
Huwyler M, Springer J, Kessler TM, Burkhard FC. A safe and simple solution for intravesical tension-free vaginal tape erosion: removal by standard transurethral resection. BJU Int. 2008;102:582-585.
Ingelman-Sundberg A. [Urinary incontinence in women.]. Nord Med. 1953;50(34):1149-1152.
Iosif CS. Porcine corium sling in the treatment of urinary stress incontinence. Arch Gynecol. 1987;240:131-136.
Irer B, Aslan G, Cimen S, et al. Development of vesical calculi following tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunction. 2005;16:245-246.
Jarmi-Di BZ, Bianchi AM, Castro RA, et al. Randomised trial of TVT-O and TVT-S for the treatment of stress urinary incontinence: preliminary study. Int Urogynecol J. 2009;20:S176. [abstract 117]
Jarvis GJ. Surgery for genuine stress incontinence. Br J Obstet Gynecol. 1994;101:371-374.
Jeffcoate T. The results of the Aldridge sling operation for stress incontinence. J Obstet Gynaecol Br Emp. 1953;63:36.
Jeffry L, Deval B, Birsan A, et al. Objective and subjective cure rates after tension-free vaginal tape for treatment of urinary incontinence. J Urol. 2002;58:702-706.
Jha S, Jones G, Radley S, Farkas A. Factors influencing outcome following the tension-free vaginal tape (TVT). Eur J Obstet Gynecol Reprod Biol. 2009;144:85-87.
Jimenez CJ, Hualde AA, Raigoso OO, et al. [Our experience with mini tapes (TVT Secur and MiniArc) in the surgery for stress urinary incontinence.]. Actas Urol Esp. 2008;32(10):1013-1018. [in Spanish]
John TT, Aggarwl N, Singla AK, Santucci RA. Intense inflammatory reaction with porcine small intestine submucosa pubovaginal sling or tape for stress urinary incontinence. Urology. 2008;72:1036-1039.
Jomaa M. Combined tension-free vaginal tape and prolapse repair under local anaesthesia in patients with symptoms of both urinary incontinence and prolapse. Gynecol Obstet Invest. 2001;51:184-186.
Jorion J. Endoscopic treatment of bladder perforation after tension-free vaginal tape procedure. J Urol. 2002;168:197.
Juma S, Brito CG. Transobturator tape (TOT): two years follow-up. Neurourol Urodyn. 2007;26:37-41.
Kalota SJ. Small intestinal submucosa tension-free sling: postoperative inflammatory reactions and additional data. J Urol. 2004;172:1349-1350.
Karram M, Bhatia N. Patch procedure: modified transvaginal fascia lata sling for recurrent or severe stress urinary incontinence. Obstet Gynecol. 1990;75:461-463.
Karram M, Segal J, Vassallo BJ, et al. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929-932.
Karsenty G, Boman J, Elzayat E, et al. Severe soft tissue infection of the thigh after vaginal erosion of transobturator tape for stress urinary incontinence. Int Urogynecol J. 2007;18:207-212.
Kawashima H, Hirai K, Okada N, et al. The importance of studying pressure-flow for predicting postoperative voiding difficulties in women with stress urinary incontinence: a preliminary study that correlates low Pdet × Qave with postoperative residual urine. Urol Res. 2004;32:84-88.
Killingsworth LB, Wheeler TL2nd, Burgio KL, et al. One-year outcomes of tension-free vaginal tape (TVT) mid-urethral sling in overweight and obese women. Int Urogynecol J. 2009;20(9):1103-1108.
Klutke C, Siegel S, Carlin B, et al. Urinary retention after tension-free vaginal tape procedure: iIncidence and treatment. Urology. 2001;58:697-701.
Kobashi K, Dmochowski R, Mee SL, et al. Erosion of woven polyester pubovaginal sling. J Urol. 1999;162:2070-2072.
Kobashi K, Govier F. Management of vaginal erosion of polypropylene mesh slings. J Urol. 2003;169:2242-2243.
Kobashi KC, Govier F. Perioperative complications: the first 140 polypropylene pubovaginal slings. J Urol. 2003;170:1918-1921.
Kobashi KC, Hsiao KC, Govier FE. Suitability of different sling materials for the treatment of female stress urinary incontinence. Nat Clin Pract. 2005;2:84-91.
Kobashi KC, Mee SL, Leach GE. A new technique for cystocele repair and transvaginal sling: the cadaveric prolapsed reapir and sling (CaPS). Urology. 2000;56(Suppl. 6A):9-14.
Kociszewski J, Rautenberg O, Perucchini D, et al. Tape functionality: sonographic tape characteristics and outcome after TVT incontinence surgery. Neurourol Urodyn. 2008;27:485-490.
Kocjancic E, Crivellaro S, Oyama IA, et al. Transobturator tape in the management of female stress incontinence: clinical outcomes at medium term follow-up. Urol Int. 2008;80:275-278.
Kolle D, Tamussino K, Hanzal E, et alAustrian Urogynecology Working Group. Bleeding complications with the tension-free vaginal tape operation. Am J Obstet Gynecol. 2005;193:2045-2049.
Konig JE, Pannek J, Martin W, et al. [Severe postoperative inflammation following implantation of a Sratatsis sling]. Urologe A. 2004;43:1541-1543. [in German]
Kraatz H. Use of nylon sling in urinary incontinence. Zentralbl Gynakol. 1953;75:1486-1487.
Krauth JS, Rasoamiaramanana H, Barletta H, et al. Sub-urethral tape treatment of female urinary incontinence: morbidity assessment of the trans-obturator route and a new tape (I-STOP): a multi-centre experiment involving 604 cases. Eur Urol. 2005;47:102-107.
Krofta L, Feyereisl J, Krcmár M, et al. One year prospective follow-up of the TVT-S procedure for treatment of stress urinary incontinence. Int Urogynecol J. 2009;20:S125. [abstract 058]
Kubricht WS, Williams J, Eastham JA, et al. Tensile strength of cadaveric fascia lata compared to small intestinal submucosa using suture pull through analysis. J Urol. 2001;165:486-490.
Kuhn A, Burkhard F, Eggemann C, Mueller MD. Sexual function after suburethral sling removal for dyspareunia. Surg Endosc. 2009;23:765-768.
Kuhn A, Eggeman C, Burkhard F, Mueller MD. Correction of erosion after suburethral sling insertion for stress incontinence: results and related sexual function. Eur Urol. 2009;5:371-377.
Kulseng-Hanssen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:391-396.
Kusuda L. Simple release of pubovaginal sling. Urology. 2001;57:358-359.
Kuuva N, Nilsson C. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 2002;81:72-77.
Kuuva N, Nilsson C. Tension-free vaginal tape procedure: an effective minimally invasive operation for the treatment of recurrent stress urinary incontinence? Gynecol Obstet Invest. 2003;56:93-98.
Lane B, Singh D, Meraney A, Streem S. Novel endourologic applications for holmium laser. Urology. 2005;65:991-993.
Lapouge O, Bram R, Hocke C, Ballanger P. Management of erosive complications after tension-free vaginal tape procedure. Prog Urol. 2009;19:193-2001.
Latini JM, Lux MM, Kreder KJ. Efficacy and morbidity of autologous fascia lata sling cystourethropexy. J Urol. 2004;171:1180-1184.
Laurikainen E, Killholma P. The tension-free vaginal tape procedure for female urinary incontinence without preoperative urodynamic evaluation. J Am Coll Surg. 2003;196:579-583.
Laurikainen E, Killholma P. A nationwide analysis of transvaginal tape release for urinary retention after tension-free vaginal tape procedure. Int Urogynecol J. 2006;17:111-119.
Leach G, Dmochowski R, Appell R, et al. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. J Urol. 1997;158:875-880.
Leanza V, Garozzo V, Accardi M, et al. A late complication of transobturator tape: abscess and myositis. Minerva Ginecol. 2008;60(1):91-94.
Lee JH, Yoon JH, Lee SJ, et al. Modified transobturator tape (canal transobturator tape) surgery for female stress urinary incontinence. J Urol. 2009;181:2616-2621.
Lee K, Chin KD, Deok HH, et al. Outcomes following repeat midurethral synthetic sling after failure of the initial sling procedure: rediscovery of the tension-free vaginal tape procedure. J Urol. 2007;178:1370-1374.
Lee KS, Han DH, Choi YS, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year followup. J Urol. 2007;177:214-218.
Lemack GE, Krauss S, Litman H, et al. Normal postoperative urodynamic testing does not predict voiding dysfunction after burch colposuspension versus pubovaginal sling. J Urol. 2008;180:2076-2080.
Lemer ML, Chaikin DC, Blaivas JG. Tissue strength analysis of autologous and cadaveric allografts for the pubovaginal sling. Neurourol Urodyn. 1999;18:497-503.
Leng WW, McGuire EJ. Management of female urethral diverticula: a new classification. J Urol. 1998;160:1297-1300.
Leron E, Steiner N, Peri Z, Mazor M. Long term follow-up and prevalence of persistent, de novo and improvement of overactive bladder symptoms after tension free vaginal tape, 34th Annual IUGA meeting. Int Urogynecol J, 2009;20. abstract 132 (S186–7)
Levin I, Groutz A, Gold R, et al. Surgical complications and medium-term outcome results of tension-free vaginal tape: a prospective study of 313 consecutive patients. Neurourol Urodyn. 2004;23:7-9.
Liapis A, Bakas P, Creatsas G. Long-term efficacy of tension-free vaginal tape in the management of stress urinary incontinence in women: efficacy at 5- and 7-year follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(11):1509-1512.
Liapis A, Bakas P, Christopoulos P, et al. Tension-free vaginal tape for elderly women with stress urinary incontinence. Int J Gynaecol Obstet. 2006;92:48-51.
Lieb J, Das A. Urethral erosion of tension-free vaginal tape. Scand J Urol Nephrol. 2003;37:184-185.
Lim JL, Cornish A, Carey MP. Clinical and quality of life outcomes in women treated by the TVT-O procedure. Br J Obstet Gynaecol. 2006;113:1315-1320.
Lim YN, Muller R, Corstiaans A, et al. Suburethral slingplasty evaluation study in North Queensland, Australia: the SUSPEND trial. Aust N Z J Obstet Gynaecol. 2005;45:52-59.
Lin LY, Sheu BC, Lin HH. Sequential assessment of urodynamic findings before and after tension-free vaginal tape (TVT) operation for female genuine stress incontinence. Eur Urol. 2004;45:362-366.
Lo T, Chang TC, Chao AS, et al. Tension-free vaginal tape procedure on genuine stress incontinent women with coexisting genital prolapse. Acta Obstet Gynecol Scand. 2003;82(11):1049-1053.
Lo T, Horng S, Chang C, et al. Tension-free vaginal tape procedure after previous failure in incontinence surgery. Urology. 2002;60:57-61.
Lo T, Horng S, Liang C, et al. Ultrasound assessment of mid-urethra tape at three-year follow up after tension free vaginal tape procedure. Urology. 2004;63:671-675.
Lo T, Huang H, Chang C, et al. Use of intravenous anesthesia for tension-free vaginal tape therapy in elderly women with genuine stress incontinence. Urology. 2002;59:349-353.
Lo T, Wang A, Horng S, et al. Ultrasonographic and urodynamic evaluation after tension free vagina tape procedure (TVT). Acta Obstet Gynecol Scand. 2001;80:65-70.
Lobel RW, Sand PK. The empty supine stress test as a predictor of intrinsic urethral sphincter deficiency: pediatric Foley catheter test. Obstet Gynecol. 1996;88:128-132.
Long C, Hsu C, Wu M, et al. Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol. 2009;21:342-347.
Long C, Lo T, Liu CM, et al. Lateral excision of tension-free vaginal tape for the treatment of iatrogenic urethral obstruction. Obstet Gynecol. 2004;104:1270-1274.
Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367-376.
Loughlin KR. Epithelial inclusion cyst formation after free vaginal wall swing sling procedure for stress urinary incontinence. J Urol. 1998;159:208.
Lovatsis D, Gupta C, Dean E, et al. Tension-free vaginal tape procedure is an ideal treatment for obese patients. Am J Obstet Gynecol. 2003;189:1601-1605.
Madjar S, Tchetgen M, Van Antwerp A, et al. Urethral erosion of tension-free vaginal tape. Urology. 2002;59:601.
Mahajan ST, Kenton K, Bova DA, et al. Transobturator tape erosion associated with leg pain. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:66-68.
Maher C, Baessler K, Glazener CM, et al. Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn. 2008;27:3-12.
Mahmoud M, Wadie BS. Bladder erosion of tension-free vaginal tape presented as vesical stone; management and review of literature. Int Urol Nephrol. 2007;39:453-455.
Manca A, Sculpher MJ, Ward K, Hilton P. A cost-utility analysis of tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence. Br J Obstet Gynaecol. 2003;110:255-262.
Mansoor A, Vedrine N, Darcq C. Surgery of female urinary incontinence using trans-obturator tape (TOT): a prospective randomized comparative study with TVT. Neurourol Urodyn. 2003;22:488-489.
Marszalek M, Roehlich M, Racz U, et al. Sexual function after tension-free vaginal tape procedure. Urol Int. 2007;78:126-129.
Martan A, Svabik K, Masata J, et al. Correlation between changes in ultrasound measurements and clinical curative effect of tension-free vaginal tape-SECUR procedure. Int Urogynecol J Pelvic Floor Dysfunction. 2009. Feb 14. [Epub ahead of print]
Masata J, Martan A, Svabik K, et al. Ultrasound imaging of the lower urinary tract after successful tension-free vaginal tape (TVT) procedure. Ultrasound Obstet Gyncol. 2006;28:221.
Mason RC, Roach M. Modified pubovaginal sling for treatment of intrinsic sphincteric deficiency. J Urol. 1996;156:1991-1994.
Mazouni C, Karsenty G, Bretelle F, et al. Urinary complications and sexual function after the tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2004;83:955-961.
McGuire EJ. Urodynamic findings in patient after failure of stress incontinence operations. Prog Clin Biol Res. 1981;78:351-360.
McGuire EJ, Bennett CJ, Konnak JA, et al. Experience with pubovaginal slings for urinary incontinence at the University of Michigan. J Urol. 1987;138:525-526.
McGuire EJ, Fitzpatrick CC, Wan J, et al. Clinical assessment of urethral sphincter function. J Urol. 1993;150:1452-1454.
McGuire EJ, Lytton B. Pubovaginal sling procedure for stress incontinence. J Urol. 1978;119:82-84.
McGuire EJ, O’Connell HE. Surgical treatment of intrinsic urethral dysfunction: slings. Urol Clin North Am. 1995;22:657-664.
McLennan M. Transurethral resection of transvaginal tape. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:360-362.
McLennan MT, Bent AE. Sling incision with associated vaginal wall interposition for obstructed voiding secondary to suburethral sling procedure. Int Urogynecol J Pelvic Floor Dysfunction. 1997;8:168-172.
McLennan MT, Melick CF, Bent AE. Clinical and urodynamic predictors of delayed voiding after fascia lata suburethral sling. Obstet Gynecol. 1998;92:608.
Mellier G, Benayed B, Bretones S, et al. Suburethral tape via the obturator route: Is the TOT a simplification of the TVT? Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:227-232.
Meltomaa S, Backman T, Haarala M. Concomitant vaginal surgery did not affect outcome of the tension-free vaginal tape operation during a prospective 3-year follow up study. J Urol. 2004;172:222-226.
Meschia M, Barbacini P, Ambrogi V, et al. TVT-Secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence: one-year data from a multi-centre prospective trial. Int Urogynecol J. 2009;20:313-317.
Meschia M, Pifarotti P, Bernasconi F, et al. Tension-free vaginal tape: analysis of outcomes and complications in 404 stress incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl. 2):S24-S27.
Meschia M, Pifarotti P, Bernasconi F, et al. Tension-free vaginal tape (TVT) and intravaginal slingplasty (IVS) for stress urinary incontinence: a multicenter randomized trial. Am J Obstet Gynecol. 2006;195(5):1338-1342.
Meschia M, Pifarotti P, Gattei U, Bertozzi R. Tension-free vaginal tape: analysis of risk factors for failure. Int Urogynecol J. 2007;18:419-422.
Mesens T, Aich A, Bhal PS. Late erosions of mid-urethral tapes for stress urinary incontinence— need for long-term follow-up? Int Urogynecol J. 2007;18:1113-1114.
Miller EA, Amundsen CL, Toh KL, et al. Preoperative urodynamic evaluation may predict voiding dysfunction in women undergoing pubovaginal sling. J Urol. 2003;169:2234.
Millin T, Read CD. Stress urinary incontinence of urine in the female. Postgrad Med. 1948;24:51-56.
Minaglia S, Ozel B, Klutke C, et al. Bladder injury during transobturator sling. Urology. 2004;64:376-377.
Mishra VC, Mishra N, Karim OM, et al. Voiding dysfunction after tension-free vaginal tape: a conservative approach is often successful. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:210-214.
Mitsui T, Tanaka H, Moriya K, et al. Clinical and urodynamic outcomes of pubovaginal sling procedure with autologous rectus fascia for stress urinary incontinence. Int J Urol. 2007;14:1076-1079.
Morgan TO, Westney OL, McGuire EJ. Pubovaginal sling: 4-year outcome and quality of life assessment. J Urol. 2000;163:1845-1848.
Mukherjee K, Constantine G. Urinary stress incontinence in obese women: tension-free vaginal tape is the answer. BJU Int. 2001;88:881-883.
Muller M, Koebele A, Deval B. Determinants of success and recurrence after suburethral free tape procedure for female incontinence. J Gynecol Obstet Biol Reprod (Paris). 2007;36:19-29.
Mustafa M, Wadie BS. Bladder erosion of tension-free vaginal tape presented as vesical stone; management and review of literature. Int Urol Nephrol. 2007;39(2):453-455.
Myers DL, LaSala CA. Conservative surgical management of Mersilene mesh suburethral sling erosion. Am J Obstet Gynecol. 1998;179:1424-1429.
Nazemi TM, Rapp DE, Govier FE, Kobashi KC. Cadaveric fascial sling with bone anchors: minimum of 24 months of follow-up. Urology. 2008;71:834-838.
Negoro H, Kawakita M, Imai Y. Intravesical tape erosion following the tension-free vaginal tape procedure for stress urinary incontinence. Int J Urol. 2005;12:696-698.
Neuman M. TVT-Obturator: short-term data on the operative procedure for the cure of female stress urinary incontinence performed on 300 patients. Eur Urol. 2007;51:1083-1088.
Neuman M. Perioperative complications and early follow-up with 100 TVT-SECUR procedures. J Minim Invasive Gynecol. 2008;15:480-484.
Nguyen JN. Tape mobilization for urinary retention after tension-free vaginal tape procedures. J Urol. 2005;66:523-526.
Niknejad K, Plzak LS, Staskin DR, Loughlin KR. Autologous and synthetic urethral slings for female incontinence. Urol Clin North Am. 2002;29:597-611.
Nilsson C, Falconer C, Rezapour M. Seven-year follow up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004;104:1259-1262.
Nilsson C, Kuuva N, Falconer C, et al. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl. 2):S5-S8.
Nilsson CG, Kuuva N. The tension-free vaginal tape procedure is successful in the majority of women with indications for surgical treatment of urinary stress incontinence. Br J Obstet Gynaecol. 2001;108:414-419.
Nilsson CG, Palva K, Rezapour M, et al. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1043-1047.
Nitti VW, Carlson KV, Blaivas JG, Dmochowski RR. Early results of pubovaginal sling lysis by midline sling incision. Urology. 2002;59:47-51.
Nitti VW, Raz S. Obstruction following anti-incontinence procedures: diagnosis and treatment with transvaginal urethrolysis. J Urol. 1994;152:93-98.
Nordling J, Meyhoff H, Andersen JT, et al. Urinary incontinence in the female: the value of detrusor reflex activation procedures. Br J Urol. 1979;51:110-113.
Novara G, Ficarra V, Boscolo-Berto R, et al. Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007;52(3):663-678.
Novara G, Galfano A, Boscolo-Berto R, et al. Complication rates of tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials comparing tension-free mid-urethral tapes to other surgical procedures and different devices. Eur Urol. 2008;53:288-309.
O’Connor RC, Nanigian DK, Lyon MB, et al. Early outcomes of mid-urethral slings for female stress urinary incontinence stratified by Valsalva leak point pressure. Neurourol Urodyn. 2006;25:685-688.
O’Reilly KJ, Govier FE. Intermediate term failure of pubovaginal slings using cadaveric fascia lata: a case series. J Urol. 2002;167:1356-1358.
Oh T, Ryu D. Transurethral resection of intravesical mesh after midurethral sling procedures. J Endourol. 2009;23:1-5.
Oliveira E, Bezerra LR, de Araujo MP, et al. Uroflowmetry and flow pressure study parameters in urogynecology patients. Rev Assoc Med Bras. 2008;54:139-141.
Oliveira FR, Ramos JG, Martins-Costa S. Translabial ultrasonography in the assessment of urethral diameter and intrinsic sphincter deficiency. J Ultrasound Med. 2006;25:1153-1158.
Oliveira R, Silva A, Pinto R, et al. Short-term assessment of a tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2009;104:225-228.
Olsson I, Kroon U. A three-year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest. 1999;48:267-269.
Onur R, Singla A. Solvent-dehydrated cadaveric dermis: a new allograft for pubovaginal sling surgery. Int J Urol. 2005;12:801-805.
Onur R, Singla A, Kobashi KC. Comparison of solvent-dehydrated allograft dermis and autograft rectus fascia for pubovaginal sling: questionnaire-based analysis. Int Urol Nephrol. 2008;40:45-49.
Ordorica R, Rodriguez AR, Coste-Delvecchio F, et al. Disabling complications with slings for managing female stress urinary incontinence. BJU Int. 2008;102:333-336.
Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU Int. 2003;92:964-968.
Owens DC, Winters JC. Pubovaginal sling using Duraderm graft: intermiediate follow-up and patient satisfaction. Neurourol Urodyn. 2004;23:115-118.
Ozel B, Minaglia S, Hurtado E, et al. Treatment of voiding dysfunction after transobturator tape procedure. Urology. 2004;64:1030.
Padmanabhan P, Nitti VW. Female stress urinary incontinence: how do patient and physician perspectives correlate in assessment of outcomes? Curr Opin Urol. 2006;16:212-218.
Paick JS, Ku JAH, Shin JW, et al. Tension-free vaginal tape procedure for urinary incontinence with low Valsalva leak point pressure. J Urol. 2004;172:1370-1373.
Paick JS, Oh SJ, Kim SW, Ku JH. Tension-free vaginal tape, suprapubic arc sling and transobturator tape in the treatment of mixed urinary incontinence in women. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:123-129.
Panayi DC, Duckett J, Digesu GA, et al. Pre-operative opening detrusor pressure is predictive of detrusor overactivity following TVT in patients with pre-operative mixed urinary incontinence. Neurourol Urodyn. 2009;28:82-85.
Paraiso M, Walters M, Karram M, et al. Laparoscopic Burch colposuspension versus tension-free vaginal tape: a randomized trial. Obstet Gynecol. 2004;104:1249-1258.
Parekh MH, Minassian VA, Poplawsky D. Bilateral bladder erosion of a transobturator tape mesh. Obstet Gynecol. 2006;108:713-715.
Partoll L. Efficacy of tension-free vaginal tape with other pelvic reconstructive surgery. Am J Obstet Gynecol. 2002;186:1292-1298.
Persson J, Teleman P, Eten-Bergqvist C, et al. Cost-analyses based on a prospective, randomized study comparing laparoscopic colposuspension with tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2002;81:1066-1073.
Pesschers UM, Tunn R, Buczkowski M, et al. Tension-free vaginal tape for the treatment of stress urinary incontinence. Clin Obstet Gynecol. 2000;43:670-675.
Petros P, Ulmsten U. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993;153:1-93.
Petrou SP, Brown JA, Blaivas JG. Suprameatal transvaginal urethrolysis. J Urol. 1999;161:1268-1271.
Petrou SP, Frank I. Complications and initial continence rates after a repeat pubovaginal sling procedure for recurrent stress urinary incontinence. J Urol. 2001;165:1979-1981.
Petrou SP, Young PR. Rate of recurrent SUI after retropubic urethrolysis. J Urol. 2002;167(2 Pt 1):613-615.
Pianezza ML, Joffe R, Chugh T, Radomski SB. Long-term patient satisfaction following cadaveric pubovaginal sling incontinence surgery using the UDI and IIQ-7 questionnaires. Neurourol Urodyn. 2007;26:185-189.
Pickens RB, White WM, Klein FA, et al. Initial experience with the MiniArc single incision sling system for the treatment of stress urinary incontinence. J Urol. 2009;181:544. [abstract 1521] Annual Meeting
Pit M. Rare complications of tension-free vaginal tape procedure: late intraurethral displacement and early misplacement of tape. J Urol. 2002;167:647.
Porena M, Constantini E, Frea B, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol. 2007;52:1481-1491.
Powers K, Lazarou G, Greston WM. Delayed urethral erosion after tension-free vaginal tape. Int Urogynecol J. 2006;17:422-425.
Pugsley H, Barbrook C, Mayne CJ, Tincello DG. Morbidity of incontinence surgery in women over 70 years old: a retrospective cohort study. Br J Obstet Gynaecol. 2005;112:786-790.
Queimadelos MA, Cimadevilla GA, Lema GJ, et al. Monarc transobturator suburethral sling: eighteen months’ experience. Paris: ICS/IUGA; 2004. abstract 559
Rafii A, Darai E, Haab F, et al. Body mass index and outcome of tension-free vaginal tape. Eur Urol. 2003;43:288-292.
Rardin C, Kohli N, Rosenblatt PL, et al. Tension-free vaginal tape: outcomes among women with primary versus recurrent stress urinary incontinence. Obstet Gynecol. 2002;100:893-897.
Raz S, Siegel AL, Short JL, et al. Vaginal wall sling. J Urol. 1989;141:143-146.
Rechberger T, Futyma K, Jankiewicz K, et al. The clinical effectiveness of retropubic (IVS-02) and transobturator (IVS-04) midurethral slings: randomized trial. Eur Urol. 2009;56:24-30.
Rehman J, Chugtai B, Sukkarieh T, Khan SA. Extraperitoneal laparoscopic removal of eroded midurethral sling: a new technique. J Endourol. 2008;22:365-368.
Rezapour M, Falconer C, Ulmsten U. Tension free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD): a long term follow up. Int Urogynecol J Pubic Floor Dysfunct. 2001;12(Suppl. 2):512-514.
Rezapour M, Ulmsten U. Tension-free vaginal tape (TVT) in women with recurrent stress urinary incontinence—a long-term follow up. Int Urogynecol J. 2001:S9-S11.
Riachi L, Kohli N, Miklos J. Repeat tension-free transvaginal tape (TVT) sling for the treatment of recurrent stress urinary incontinence. Int Urogynecol J. 2002;13:133-135.
Richter HE, Burgio KL, Holley RL, et al. Cadaveric fascia lata sling for stress urinary incontinence: a prospective quality-of-life analysis. Am J Obstet Gynecol. 2003;189:1590-1596.
Richter HE, Varner E, Sanders E, et al. Effects of pubovaginal sling procedure on patients with urethral hypermobility and intrinsic sphincteric deficiency: would they do it again? Am J Obstet Gynecol. 2001;184:14-19.
Rinne K, Laurikainen E, Arre K, et al. A randomized trial comparing TVT with TVT-O: 12-month results. Int Urogynecol J. 2008;19:1049-1054.
Robert M, Murphy M, Birch C, et al. Five cases of tape erosion after transobturator surgery for urinary incontinence. Obstet Gynecol. 2006;107:472-474.
Rodriguez LV, de Almeida F, Dorey F, et al. Does Valsalva leak point pressure predict outcome alter the distal urethral polypropylene sling? Role of urodynamics in the sling era. J Urol. 2004;172:210-214.
Rogers R, Lucente V, Raders J. Anatomic considerations for the TVT-obturator approach for the correction of female stress urinary incontinence. Abstract, ICS, 2005.
Roth TM. Management of persistent groin pain after transobturator slings. Int Urogynecol J. 2007;18:1371-1373.
Rovner ES, Wein AJ. Diagnosis and reconstruction of the dorsal or circumferential urethral diverticulum. J Urol. 2003;170:82-86.
Rutman MP, Blaivas JG. Urodynamics: what to do and when is it clinically necessary? Curr Urol Rep. 2007;8:263-268.
Rutner AB, Levine SR, Schmaelzle JF. Processed porcine small intestine submucosa as a graft material for pubovaginal sling: durability and results. Urology. 2003;62:805-809.
Sand PK, Bowen LW, Panganiban R, Ostergard DR. The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol. 1987;69:399-402.
Sander P, Moller LM, Rudnicki PM, et al. Does the tension-free vaginal tape procedure affect the voiding phase? Pressure-flow studies before and 1 year after surgery. BJU Int. 2002;89:694-698.
Scarpero HM, Dmochowski RR, Nitti VW. Repeat urethrolysis after failed urethrolysis for iatrogenic obstruction. J Urol. 2003;169:1013-1016.
Schierlitz L, Dwyer PL, Rosamilia A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol. 2008;112:1253-1261.
Schmidbauer C, Chiang H, Raz S. Surgical treatment for female geriatric incontinence. Clin Geriatr Med. 1986;2:759-776.
Schrepferman CG, Griebling TL, Nygaard IE, Kreder KJ. Resolution of urge symptoms following sling cystourethropexy. J Urol. 2000;164:1628-1631.
Segal J, Vassallo B, Kleeman S, et al. Prevalence of persistent de novo overactive bladder symptoms after the tension-free vaginal tape. Obstet Gynecol. 2004;104:1263-1269.
Serels SR, Rackley RR, Appell RA. In situ slings with concurrent cystocele repair. Tech Urol. 1999;5:129-132.
Serels SR, Rackley RR, Appell RA. Surgical treatment for stress urinary incontinence associated with Valsalva induced detrusor instability. J Urol. 2000;163:884-887.
Seung-June Oh, Stoffel JT, McGuire EJ. Pubovaginal sling. In Wein AJ, Kavoussi LR, Novick AC, et al, editors: Campbell-Walsh urology, 9th ed, Philadelphia: Elsevier, 2007.
Sevestre S, Ciofu C, Deval B, et al. Results of the tension-free vaginal tape technique in the elderly. Eur Urol. 2003;44:128-131.
Sharma B, Oligbo N. Delayed vaginal erosion of the tape—a rare complication with TVT. J Obstet Gynaecol. 2004;24:96-98.
Shenassa B, Novak T, Ghoniem GM. Management of obstructing sling with transvaginal urethrolysis and vaginal patch interposition. J Urol. 2000;163:74.
Shrotri KN, Shervington JP, Shrotri NC. Laser excision of encrusted intra-vesical tension-free vaginal tape (TVT). Int Urogynecol J Pelvic Floor Dysfunct. 2010;21(3):375-377.
Shukla A, Paul SK, Nishta A, Bibby J. Factors predictive of voiding problems following insertion of tension-free vaginal tape. Int J Gynaecol Obstet. 2007;96:122-126.
Shutkin NM. Homologous-serum hepatitis following the use of refrigerated bone-bank bone. J Bone Joint Surg Am. 1954;35:160-162.
Siddighi S, Karram MM. Surgical and nonsurgical approaches to treat voiding dysfunction following anti-incontinence surgery. Curr Opin Obstet Gynecol. 2007;19:490-495.
Sinha D, Blackwell A, Moran PA. Outcome measures after TVT for mixed urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunction. 2008;19:927-931.
Siow A, Morris AR, Lam A. Laparoscopic treatment of tension free vaginal tape erosion. Aust N Z J Obstet Gynecol. 2005;45:333-336.
Siracusano S, Bertolotto M, Silvestre G, et al. The feasibility of urethral color ultrasound imaging in the diagnosis of female intrinsic sphincter deficiency: preliminary results. Spinal Cord. 2002;40:192-195.
Skriapas K, Poulakis V, Dillenburg W, et al. Tension-free vaginal tape (TVT) in morbidly obese patients with severe urodynamics stress incontinence as last option treatment. Eur Urol. 2006;49:544-550.
Slack M, Sandhu J, Staskin D, et al. In vivo comparison of suburethral sling materials. Int Urogynecol J Pelvic Floor Dysfunct. 2005;17:106-110.
Smith PP, Appell RA. Does uroflow predict ISD? Neurourol Urodyn. 2008;27:40-44.
Sokol A, Jelovsek J, Walters M, et al. Incidence and predictors of prolonged urinary retention after TVT with and without concurrent prolapse surgery. Am J Obstet Gynecol. 2005;192:1537-1543.
Sokol ER, Urban R. Novel repair of tension-free midurethral sling erosion into the urethra. J Minim Invasive Gynecol. 2008;15:755-757.
Song PH, Kim YD, Kim HT, et al. The 7-year outcome of the tension-free vaginal tape procedure for treating female stress urinary incontinence. BJU Int. 2009;104(8):1113-1117.
Stanton SL, Ozsoy C, Hilton P. Voiding difficulties in the female: prevalence, clinical and urodynamic review. Obstet Gynecol. 1983;61:144-147.
Starkman JS, Christopher WE, Scarpero HM, et al. Management of refractory urinary urge incontinence following urogynecological surgery with sacral neuromodulation. Neurourol Urodyn. 2007;26:29-35.
Starkman JS, Duffy JW3rd, Wolter CE, et al. Refractory overactive bladder after urethrolysis for bladder outlet obstruction: management with sacral neuromodulation. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:277.
Starkman JS, Duffy JW3rd, Wolter CE, et al. The evolution of obstruction induced overactive bladder symptoms following urethrolysis for female bladder outlet obstruction. J Urol. 2008;179:1018-1023.
Starkman JS, Wolter C, Gomelsky A, et al. Voiding dysfunction following removal of eroded synthetic mid-urethral slings. J Urol. 2006;176:1040-1044.
Stephenson TP, Mundy AT. The urge syndrome. In: Mundy AT, Stephenson TP, Wien AJ, editors. Urodynamics: principles, practice and application. 2nd ed. New York: Churchill Livingstone; 1994:263-276.
Stoffel JT, Smith JJ, Crivellaro S, Bresette JF. Mixed incontinence: does preoperative urodynamic detrusor overactivity affect postoperative quality of life after pubovaginal sling? Int Braz J Urol. 2008;34:765-771.
Summit RL, Bent AE, Ostergard DR, Harris TA. Suburethral sling procedure for genuine stress incontinence and low urethral closure pressure: a continued experience. Int Urogynecol J. 1992;3:18-21.
Sweat S, Itano N, Clemens J, et al. Polypropylene mesh tape for stress urinary incontinence: complications of urethral erosion and outlet obstruction. J Urol. 2002;168:144-146.
Swiertzewski SJ, McGuire EJ. Pubovaginal sling for treatment of female stress urinary incontinence complicated by urethral diverticulum. J Urol. 1993;149:1012-1014.
Tahseen S, Reid P. Effect of transobturator tape on overactive bladders symptoms and urge urinary incontinence in women with mixed urinary incontinence. Obstet Gynecol. 2009;113:617-623.
Takacs P, Medina CA. Tension-free vaginal tape: poor intraoperative cough test as a predictor of postoperative urinary retention. Int Urogynecol J Pelvic Floor Dysfunction. 2007;18:1445-1447.
Tamussino K, Hanzal E, Kölle D, et al. Tension-free vaginal tape operation: results of the Austrian registry. Obstet Gynecol. 2001;98:732-736.
Tamussino K, Hanzal E, Kölle D, et al. Transobturator tapes for stress urinary incontinence: results of the Austrian registry. Am J Obstet Gynecol. 2007;197(6):634. e1–5
Tartaglia E, Delicato G, Baffigo G, et al. Third-generation tension-free tape for female stress urinary incontinence. J Urol. 2009;182:612-615.
Thiel DD, Pettit PD, McClellan WT, Petrou SP. Long-term urinary continence rates after simple sling incision for relief of urinary retention following fascia lata pubovaginal slings. J Urol. 2005;174:1878-1881.
Thiel M, Rodrigues Palma PC, Riccetto CL, et al. A stereological analysis of fibrosis and inflammatory reaction induced by four different synthetic slings. Br J Urol Int. 2005;95:833-837.
Tincello D, Lucente V, Khandwala S, et al. Twelve-month objective and subjective outcomes from a worldwide registry of tension-free vaginal tapes in women with stress urinary incontinence. Int Urogynecol J. 20(Suppl. 2), 2009. abstract 063
Touloupidis S, Papatsoris AG, Thanopoulos C, et al. Tension-free vaginal tape for the treatment of stress urinary incontinence in geriatric patients. Gerontology. 2007;53:125-127.
Tseng LH, Wang AC, Lin YH, et al. Randomized comparison of the suprapubic arch sling procedure vs tension-free vaginal tape for stress incontinent women. Int Urogynecol J Pelvic Floor Dysfunction. 2005;16:230-235.
Tsivian A, Benjamin S, Tsivian M, et al. Transobturator tape procedure with and without concomitant vaginal surgery. J Urol. 2009;182(3):1068-1071.
Tsivian A, Kessler O, Mogutin B, et al. Tape related complications of the tension-free vaginal tape procedure. J Urol. 2004;171:762-764.
Tsivian A, Menahem N, Yulish E, et al. Redo midurethral synthetic sling for female stress urinary incontinence. Int Urogynecol J. 2007;18:23-26.
Ulmsten U, Ekman G, Giertz G, et al. Different biochemical composition of connective tissue in continent and stress incontinent women. Acta Obstet Gynecol Scand. 1987;66:455-457.
Ulmsten U, Falconer C, Johnson P, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J. 1998;9:210-213.
Ulmsten U, Henriksson L, Johnson P, et al. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J. 1996;7:81-86.
Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999;106:345-350.
Ustun Y, Engin-Ustun Y, Gungor M, Tezcan S. Tension-free vaginal tape compared with laparoscopic Burch urethropexy. J Am Assoc Gynecol Laparosc. 2003;10:386-389.
Valpas A, Kivelä A, Penttinen J, et al. Tension-free vaginal tape and laparoscopic mesh colposuspension for stress urinary incontinence. Obstet Gynecol. 2004;104:42-48.
Vangsness CT, Wagner PP, Moore TM, Roberts MR. Overview of safety issues concerning the preparation and processing of soft-tissue allografts. Arthroscopy. 2006;22:1351-1358.
Vasavada SP, Rackley R. Pubovaginal sling. emedicine.medscape.com/article/447951-overview. updated April 25, 2011 [accessed 09.06.11]
Vassallo B, Kleeman S, Segal J, et al. Urethral erosion of a tension-free vaginal tape. Obstet Gynecol. 2003;101:1055-1058.
Velemir L, Amblard J, Jacquetin B, Fatton B. Urethral erosion after suburethral synthetic slings: risk factors, diagnosis, and functional outcome after surgical management. Int Urogynecol J. 2008;19:999-1006.
Vervest HA, Bisseling TM, Heintz AP, Schraffordt Koops SE. The prevalence of voiding difficulty after TVT, its impact on quality of life, and related risk factors. Int Urogynecol J Pelvic Floor Dysfunction. 2007;18:173-182.
Villet R, Ercoli A, Atallah D, et al. Second tension-free vaginal tape procedure and mesh retensioning: two possibilities of treatment of recurrent-persistent genuine stress urinary incontinence after a primary tension-free vaginal tape procedure. Int Urogynecol J. 2002;13:377-379.
Volkmer BG, Nesslauer T, Rinnab L, et al. Surgical intervention for complications of tension-free vaginal tape procedure. J Urol. 2003;169:570-574.
Wadie BS, Edwan A, Nabeeh AM. Autologous fascial sling vs. polypropylene tape at short-term follow-up: a prospective randomized study. J Urol. 2005;174:990-993.
Wai C, Atnip S, Williams K, et al. Urethral erosion of tension-free vaginal tape presenting as recurrent stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:353-355.
Walsh IK, Nambirajan T, Donellan SM, et al. Cadaveric fascia lata pubovaginal slings: early results on safety, efficacy and patient satisfaction. BJU Int. 2002;90:415-419.
Walsh K, Generao S, White M, et al. The influence of age on quality of life outcome in women following a tension-free vaginal tape procedure. J Urol. 2004;171:1185-1188.
Waltregny D, Gaspar Y, Reul O, et al. TVT-O for the treatment of female stress urinary incontinence: results of prospective study after a 3-year minimum follow-up. Eur Urol. 2008;53:401-410.
Waltregny D, Reul O, Mathantu B, et al. Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum followup. J Urol. 2006;175(6):2191-2195.
Wang AC. An assessment of the early surgical outcome and urodynamic effects of the tension-free vaginal tape (TVT). Int Urogynecol J Pelvic Floor Dysfunct. 2000;11:282-284.
Wang AC, Chen MC. Randomized comparison of local versus epidural anesthesia for tension-free vaginal tape operation. J Urol. 2001;165:1177-1180.
Wang AC, Chen MC. Comparison of tension-free vaginal taping versus modified Burch colposuspension on urethral obstruction: a randomized controlled trial. Neurourol Urodyn. 2003;22:185-190.
Wang AC, Chen MC. The correlation between preoperative voiding mechanism and surgical outcome of the tension-free vaginal tape procedure, with reference to quality of life. BJU Int. 2003;91:502-506.
Wang W, Zhu L, Lang J. Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet. 2009;104:113-116.
Ward K, Hilton P. Prospective multicentre randomized trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ. 2002;325:1-7.
Ward K, Hilton P. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary stress incontinence: two-year follow-up. Am J Obstet Gynecol. 2004;190:324-331.
Ward K, Hilton P. Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow-up. Br J Obstet Gynaecol. 2008;115:226-233.
Webster TM, Gerridzen RG. Gone in 24 hours: the feasibility of performing pubovaginal sling surgery with an overnight hospital stay. Can J Urol. 2003;10:1905-1909.
Wei J, Nygaard I, Richter H, et alPelvic Floor Disorders Network. Outcomes following vaginal prolapsed repair and mid urethral sling (OPUS) trial—design and methods. Clin Trials. 2009;6:162-171.
Weinberger MW, Ostergard DR. Long-term clinical and urodynamic outcomes of polytetrafluoroethylene suburethral sling for treatment of genuine stress incontinence. Obstet Gynecol. 1995;86:92-96.
Westby M, Asmussen M, Ulmsten U. Location of maximal intraurethral pressure related to urogenital diaphragm in the female subject as studied by simultaneous urethrocystometry and voiding urethrocystography. Am J Obstet Gynecol. 1982;144:408-412.
Wheatcroft SM, Vardy SJ, Tyers AG. Complications of fascia lata harvesting for ptosis surgery. Br J Ophthalmol. 1997;81:581-583.
White RA. The effect of porosity and biomaterial on the healing and long-term mechanical properties of vascular prostheses. ASAIO Trans. 1988;11:95-100.
White RA, Hirose FM, Sproat RW, et al. Histopathology observations after short-term implantation of two porous elastomers in dogs. Biomaterials. 1981;2:171-176.
Whiteside JL, Walters MD. Anatomy of the obturator region: relations to a trans-obturator sling. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:223-226.
Wiedemann A, Otto M. Small intestinal submucosa for pubourethral sling suspension for the treatment of stress incontinence: first histopathological results in humans. J Urol. 2004;172:215-218.
Wijffels SA, Elzevier HW, Lycklama a Nijeholt AAB. Transurethral mesh resection after urethral erosion of tension-free vaginal tape: report of three cases and review of literature. Int Urogynecol J. 2009;20:261-263.
Wilson CM, Williams BJ, Bilello S, Gomelsky A. Bovine dermis: a novel biologic substitute for autologous tissue in sling surgery. Int Urogynecol J. 2008;19:1671-1676.
Wolter CE, Starkman JS, Scarpero HM, et al. Removal of transobturator midurethral sling for refractory thigh pain. Urology. 2008;72(2):461.e1-461.e3.
Woodruff AJ, Cole EE, Dmochowski RR, et al. Histologic comparison of pubovaginal sling graft materials: a comparative study. Urology. 2008;72(1):85-89.
Wright EJ, Iselin CE, Carr LK, Webster GD. Pubovaginal sling using cadaveric allograft fascia for the treatment of intrinsic sphincter deficiency. J Urol. 1998;160:759-762.
Wyczolkowski M, Klima W, Piasecki Z. Reoperation after complicated tension-free vaginal tape procedures. J Urol. 2001;166:1004-1005.
Yang J, Yang S, Huang W. Correlation of morphological alterations and functional impairment of the tension-free vaginal tape obturator procedure. J Urol. 2009;181:211-218.
Yuan Z, Dai Y, Chen Y, Wei Q. [Clinical study on concomitant surgery for stress urinary incontinence and pelvic organ prolapse.]. Zhonghua Wai Ke Za Zhi. 2008;46(20):1533-1535. [in Chinese]
Zaccharin R. The anatomic supports of the female urethra. Obstet Gynecol. 1968;21:754-759.
Zahn CM, Siddique S, Hernandez S, Lockrow EG. Anatomic comparison of two transobturator tape procedures. Obstet Gynecol. 2007;109:701-706.
Zaragoza MR. Expanded indications for the pubovaginal sling: treatment of type 2 or 3 stress incontinence. J Urol. 1996;156:1620-1622.
Zimmern PE, Hadley HR, Leach GE, Raz S. Female urethral obstruction after Marshall-Marchetti-Krantz operation. J Urol. 1987;138:517.
Zubke W, Becker S, Kramer B, et al. Persistent urinary retention after tension-free vaginal tape: a new surgical solution. Eur J Obstet Gynecol Reprod Biol. 2004;115:95-98.
Zullo MA, Plotti F, Calcagno M, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol. 2007;51(5):1376-1382. discussion 1383–4
Zumbé J, Porres D, Degiorgis PL, Wyler S. Obturator and thigh abscess after transobturator tape implantation for stress urinary incontinence. Urol Int. 2008;81:483-485.