Complications
Many of the complications of progressive BPH are rare, and much of the knowledge comes from studies of men presenting with such complications for treatment (i.e., cases) rather than observing cohorts of men for the development of complications.
Mortality
Between 1950 and 1954, 17 of 24 countries reported mortality rates of greater than 10 per 100,000, whereas between 1985 and 1989 data were available for 61 countries, only one reporting a greater than 10/100,000 mortality rate (Boyle et al, 1996). If the mortality rates from 1950 were applied to 1990, 13,681 fewer deaths occurred in the United States alone than expected, a major but unheralded health care achievement.
Bladder Stones
In a large autopsy study the prevalence of bladder stones was 8 times higher in men with a histologic diagnosis of BPH (3.4%) compared with controls (0.4%) but no increased incidence of ureteral or kidney stones was found (Grosse, 1990). In a study comparing watchful waiting and TURP in men with moderate symptoms, only 1 of 276 patients assigned to watchful waiting developed a bladder stone in 3 years of follow-up (Wasson et al, 1995). The self-reported rate of a bladder stone in a cross-sectional study in 2002 Spanish men was 0.7% (Hunter et al, 1996).
In clinical practice the risk of bladder stone development is small and screening only indicated if clinical circumstances warrant it (e.g., hematuria, stuttering of urination).
Urinary Tract Infections
In older surgical series UTIs constitute the main indication for surgical intervention in about 12% (Holtgrewe et al, 1989; Mebust et al, 1989). Although one might intuitively assume that increased amounts of residual urine would predispose to the development of UTIs, clear evidence is lacking. Hunter and colleagues (1996) quoted a rate of 5.2% self-reported episodes of UTI in a cross-sectional survey of 2002 men in Madrid, Spain. The best data to date come from the MTOPS study, in which the incidence of UTIs in the placebo-treated patients was only 0.1/100 patient-years (McConnell et al, 2003).
Bladder Decompensation
Urologists search for a progression from a normal mucosa to advancing trabeculation, development of cellules, and diverticula with ultimate detrusor muscle failure in mind when evaluating the bladder in men with BPH endoscopically. However, when the process starts, whether it really is related to BPH and obstruction, and when an intervention is necessary to prevent decompensation with resultant inability to void is unclear.
Biopsy samples from trabeculated, obstructed bladders show dense connective tissue deposition, a finding similar to that seen in animals experimentally obstructed (Gosling and Dixon, 1980; Levin et al, 1990, 2000; Chapple et al, 1991). However, bladder fibrosis is seen in both sexes with advancing age and may be a normal consequence of aging (Lepor et al, 1992a).
The critical question is whether delayed intervention might lead to progressive irreversible loss of bladder function and misses a window for cure. There is no direct evidence for this from longitudinal population or clinic patient studies. However, in the Veterans Affairs cooperative study comparing watchful waiting with TURP, those patients who crossed over from the conservative arm to TURP later in the trial had not as significant an improvement in symptoms and flow rate compared with those who underwent TURP at the beginning after randomization (Flanigan et al, 1998).
Urinary Incontinence
Incontinence is one of the most feared complications from surgical intervention for BPH. Although it may be the result of BPH secondary to overdistention of the bladder (overflow incontinence) or to detrusor instability estimated to affect up to one half or more of all obstructed patients (urge incontinence) (McConnell et al, 1994), it also is associated with aging; and in a community study an incidence of incontinence of 24% and 49% of incontinence in men and women older than 50 years was reported (Roberts et al, 1998). In the Veterans Affairs cooperative study a 4% incidence of incontinence in both the surgical and conservative treatment arms was reported (Wasson et al, 1995). The self-reported rate of incontinence in a cross-sectional study in 2002 Spanish men was 6.1% (Hunter et al, 1996). In MTOPS the rate of socially unacceptable incontinence was 0.3/100 patient-years (McConnell et al, 2003).
Upper Urinary Tract Deterioration and Azotemia
The Agency for Health Care Policy and Research BPH guidelines reported a mean of 13.6% (range 0.3% to 30%) of patients presenting for TURP with evidence of renal failure based on predominantly older studies (McConnell et al, 1994). Patients in renal failure have an increased risk for complication after TURP compared with patients with normal renal function (25% vs. 17%) (Holtgrewe et al, 1989; Mebust et al, 1989) whereas the mortality increases up to 6-fold (Holtgrewe and Valk, 1962; Melchior et al, 1974a, 1974b). In the large database of patients who had upper tract imaging before surgery, 7.6% of 6102 patients in 25 series had evidence of hydronephrosis, of whom one third had renal insufficiency (McConnell et al, 1994).
The term silent obstruction or silent prostatism has been used to describe the constellation of asymptomatic patients who eventually develop renal failure resulting from bladder outlet obstruction, a case both rare and important (Mukamel et al, 1979). In the Veterans Affairs cooperative study, only 3 of 280 surgically treated patients and 1 or 276 patients in the watchful waiting arm developed renal azotemia, defined as a doubling of the serum creatinine concentration from baseline (Wasson et al, 1995). In none of the cohort or population-based studies have cases of renal failure been reported clearly attributable to BPH. However, the self-reported rate of an episode of renal failure in a cross-sectional study in 2002 Spanish men was 2.4% (Hunter et al, 1996).
In MTOPS there was not a single case of renal insufficiency due to BPH in over 3000 men observed for more than 4 years (McConnell et al, 2003). One has to be, however, careful not to overinterpret these findings. Participants in MTOPS were screened at baseline, and one might argue that some at higher risk for developing renal failure were excluded from participation.
Hematuria
It has always been recognized that patients with BPH might develop gross hematuria and form clots with no other cause being identifiable. Recent evidence suggests that in those patients predisposed to hematuria the microvessel density is higher compared with controls. Some renewed interest in the issue of BPH-related hematuria stems from the observation that finasteride appears to be a reasonable first-line therapy apparently influencing the expression of vascular endothelial growth factor (DiPaola et al, 2001). The self-reported rate of hematuria in a cross-sectional study in 2002 Spanish men was 2.5% (Hunter et al, 1996). Precise population estimates and incidence rates are not available, and the clinical management is dictated by the circumstances.
Acute Urinary Retention
AUR is for several reasons one of the most significant complications or long-term outcomes resulting from BPH. It has in the past represented an immediate indication for surgery. Between 25% and 30% of men who underwent TURP had AUR as their main indication in older series (Holtgrewe et al, 1989; Mebust et al, 1989), and today most patients failing to void after an attempt of catheter removal still undergo surgery. For this reason alone, AUR is both from an economic viewpoint as well as from the viewpoint of the patient an important and feared event. For the patient it presents as the inability to urinate with increasing pain, eventually a visit to the emergency department, catheterization, follow-up visits to the physicians, an attempt at catheter removal, and either recovery of spontaneous voiding or surgery, both painful and time-consuming processes. In older literature the risk of recurrent AUR was cited as being 56% to 64% within 1 week of the first episode and as occurring in 76% to 83% in men with diagnosed BPH (Breum et al, 1982; Klarskov et al, 1987; Hastie et al, 1990).
The etiology of AUR is poorly understood and obstructive, myogenic, and neurogenic causes all may play a role (Kaplan et al, 2008). Prostate infection, bladder overdistention (Powell et al, 1980), excessive fluid intake, alcohol consumption, sexual activity, debility, and bed rest have all been mentioned (Stimson and Fihn, 1990). Prostatic infarction has been suggested as being an underlying event causing AUR (Graversen et al, 1989). Spiro and associates (1976) found evidence for infarction in 85% of prostates removed for AUR versus 3% in prostates of men having surgery for symptoms only. In contrast, there was no evidence of infarction in six prostatectomy specimens removed from men who had surgery for AUR (Jacobsen et al, 1997). Anjum and associates (1998) found fundamentally similar rates of infarction in 35 men each in AUR versus no AUR (1.9% vs. 3.0%).
From a clinical and prognostic point of view, spontaneous AUR should be separated from precipitated AUR, although this is by no means consistently done in the literature. Precipitated AUR refers to the inability to urinate after a triggering event such as non–prostate-related surgery, catheterization, anesthesia, ingestion of medications with sympathomimetic or anticholinergic effects or antihistamines, or others. All other AUR episodes are classified as spontaneous (Roehrborn et al, 2000a). The importance of differentiating the two types of AUR becomes clear when evaluating the ultimate outcomes of patients. After spontaneous AUR, 15% of patients had another episode of spontaneous AUR and a total of 75% underwent surgery, whereas after precipitated AUR only 9% had an episode of spontaneous AUR, and 26% underwent surgery (Roehrborn et al, 2000a).
Descriptive Epidemiology
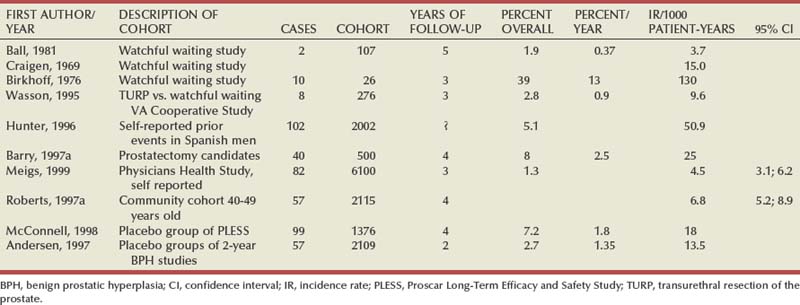
Older estimates of occurrence of AUR range from 4 to 15 to as high as 130 per 1000 patient-years (calculated by Jacobsen et al, 1997, based on studies by Craigen et al, 1969; Birkhoff et al, 1976; Ball et al, 1981), which leads to 10-year cumulative incidence rates ranging from 4% to 73% (Table 91–15). The self-reported rate of AUR in a cross-sectional study in 2002 Spanish men was 5.1% (Hunter et al, 1996).
More recent data from carefully controlled studies in better defined population shed additional light on the incidence rates in community-dwelling men and clinical BPH populations. AUR occurred in the Veterans Affairs cooperative study over 3 years in 1 man after TURP and in 8 of 276 men in the watchful waiting arm for an incidence rate of 9.6/1000 patient-years (Wasson et al, 1995). Barry and associates (1997a) reported outcomes of 500 men diagnosed by urologists with BPH who were candidates for prostatectomy by established criteria but elected to be followed conservatively. In 1574 patient-years 40 episodes of AUR occurred at a constant rate throughout the 4 years of follow-up for an incidence rate of 25/1000 patient-years.
During 15,851 patient-years of follow-up in the Physicians Health Study 82 men reported an episode of AUR for an incidence rate of 4.5/1000 patient-years (95% CI 3.1 to 6.2) (Meigs et al, 1999). Of the 2115 men aged 40 to 79 years in the Olmsted County study, 57 had a first episode of AUR during 8344 patient-years of follow-up (incidence 6.8/1000 patient-years, 95% CI 5.2, 8.9) (Jacobsen et al, 1997).
The first excellent data from men diagnosed with BPH stem from PLESS (McConnell et al, 1998). In PLESS, 1,376 placebo-treated men with enlarged prostates and moderate symptoms had complete follow-up over 4 years, of which 99 experienced an episode of AUR for a calculated incidence rate of 1.8/100 patient-years. The placebo treatment groups from three 2-year studies with a similar patient population were meta-analyzed by Boyle and associates (1998). Of 2109 patients, 57 experienced AUR over the 2 years with a constant hazard for an incidence rate of 14/1000 patient-years. In the MTOPS placebo group the incidence rate was 0.6/100 patient-years for a cumulative incidence of 2%.
Analytical Epidemiology
Age
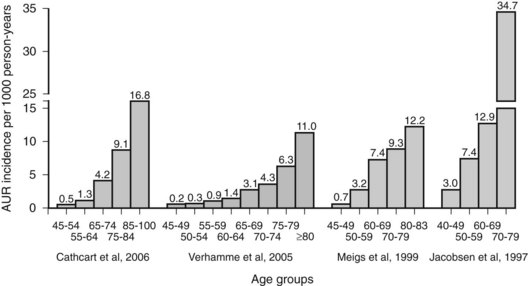
Several well-controlled studies provided considerable insights into the risk factors for AUR. Perhaps the most significant of these risk factors is age. Studies from European countries and the United States demonstrate a nearly linear increase in the age-specific incidence of AUR for men ranging in age from 40 to older than 80 years (Jacobsen et al, 1997; Meigs et al, 1999; Verhamme et al, 2005; Cathcart et al, 2006) (Fig. 91–22).
LUTS
Increased symptom severity is associated with increased risk of AUR in several large population-based or cohort studies (Table 91–16). In the Physician’s Health Study in men with mild symptoms the incidence of AUR increased from 0.4/1000 patient-years for those 45 to 49 years old to 7.9/1000 patient-years for those 70 to 83 years old. In men with an AUASI score of 8 to 35, rates increased from 3.3/1000 patient-years for those 45 to 49 years old to 11.3/1000 patient-years for those 70 to 83 years old. Men with a clinical diagnosis of BPH and an AUASI score of 8 or greater had the highest rates (age-adjusted incidence 13.7/1000 patient-years). All seven LUTS comprising the AUASI individually predicted AUR. The sensation of incomplete bladder emptying, having to void again after less than 2 hours, and a weak urinary stream were the best independent symptom predictors. Use of medications with adrenergic or anticholinergic side effects also predicted AUR (Meigs et al, 1999).
Table 91–16 Incidence of AUR by Patient Age and AUASI Score in Two Population-Based Studies
| AGE GROUP | No. AUR Events/1000 Men-Years (95% CI) | |
|---|---|---|
| Health Professionals Follow-up Study* | Olmsted County Study of Urinary Symptoms and Health Status among Men† | |
| AUASI ≤7: | ||
| 40-49 | 2.6 (0.8-6.0) | |
| 45-49 | 0.4 (0.02-1.8) | |
| 50-59 | 1.2 (0.4-2.6) | 1.7 (0.3-4.8) |
| 60-69 | 3.6 (1.9-6.1) | 5.4 (2.0-11.6) |
| 70-79 | 9.3 (3.4-20.3) | |
| 70-83 | 7.9 (4.1-13.5) | |
| AUASI >7: | ||
| 40-49 | 3.0 (0.4-10.8) | |
| 45-49 | 3.3 (0.2-14.4) | |
| 50-59 | 10.0 (5.4-16.8) | 7.4 (2.7-16.1) |
| 60-69 | 14.1 (9.4-20.2) | 12.9 (6.2-23.8) |
| 70-79 | 34.7 (20.2-55.5) | |
| 70-83 | 11.3 (6.4-18.3) | |
AUASI, American Urological Association Symptom Index; AUR, acute urinary retention; CI, confidence interval.
* Total of 82 AUR episodes in 6100 men with a crude incidence of 5.2/1000 patient-years (95% CI 4.1-6.4) in 15,851 patient-years of follow-up.
† Total of 57 AUR episodes in 2115 men with an overall incidence of 6.8/1000 patient-years (95% CI 5.2-8.9) in 8344 patient-years of follow-up.
From Kaplan SA, Wein AJ, et al. Urinary retention and post-void residual urine in men: separating truth from tradition. J Urol 2008;180(1):47–54.
The Olmsted County study focused on age, symptom severity, maximum flow rate, and prostate volume (Jacobsen et al, 1997). Incidence rates per 1000 patient-years increased from 2.6 to 9.3 for men in their 40s to their 70s if they had mild symptoms and from 3.0 to 34.7 if they had more than mild symptoms (see Table 91–16).
Urodynamic Parameters
The relative risk increased for older men, men with moderate to severe symptoms (3.2×), those with a flow rate under 12 mL/sec (3.9 times) and those with a prostate volume greater than 30 mL by TRUS (3.0 times), all compared with a baseline risk of 1.0 time for the corresponding groups (Fig. 91–23). The highest relative risk by proportional hazard models exists for 60- to 69-year-old men with more than mild symptoms and a flow rate of less than 12 mL/sec (10.3 times), and for 70- to 79-year-old men except if they had mild symptoms and a flow rate over 12 mL/sec. All other stratification of men older than age 70 years had a relative risk ranging from 12.9 to 14.8 times (all compared with men 40 to 49 years old with mild symptoms and a flow rate over 12 mL/sec for which the base risk is 1.0 time).
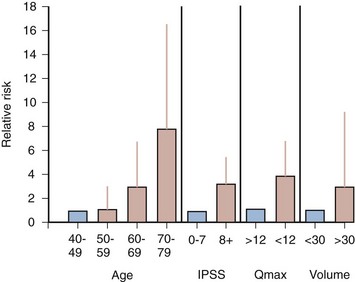
Figure 91–23 Relative risk of acute urinary retention in Olmsted County Study of Urinary Symptoms and Health Status Among Men by age, symptom severity, peak flow rate, and prostate volume. The shaded column represents the baseline and a relative risk of 1.0; the vertical line represents the 95% confidence interval. IPSS, International Prostate Symptom Score.
(Data from Jacobsen SJ, Jacobson DJ, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol 1997;158[2]:481–7.)
Prostate Volume and Serum PSA
Although age in community-dwelling men is an important risk factor, in the BPH trial population of men who already are diagnosed with BPH, other factors can be analyzed. In the placebo groups of three 2-year studies (Marberger et al, 2000) and a 4-year study (PLESS) (McConnell et al, 1998; Kaplan et al, 2000; Roehrborn et al, 2000a), prostate volume, serum PSA, and symptom severity all were predictors of AUR episodes.
The incidence increased from 5.6% to 7.7% in men with a serum PSA of less than 1.4 ng/mL from mild to severe symptoms and from 7.8% to 10.2% for those with a serum PSA of more than 1.4 ng/mL over 4 years in PLESS (Kaplan et al, 2000). In the 2-year studies the rate of AUR was 8-fold higher in those with a serum PSA of over 1.4 ng/mL (0.4% vs. 3.9%) and threefold higher if the prostate volume was over 40 mL (1.6% vs. 4.2%) (Marberger et al, 2000; Roehrborn et al, 2001). A detailed analysis showed a near linear increase in risk for AUR with increasing thresholds of serum PSA (Fig. 91–24) in PLESS, an observation that applies to both spontaneous and precipitated AUR (Roehrborn et al, 1999d). The risk for both types of AUR increases with increasing serum PSA as well as prostate volume stratified by tertiles (Fig. 91–25). Similar observations were made in MTOPS, in which the risk for AUR increased with increasing prostate volume as well as increasing baseline serum PSA (Fig. 91–26), as well as in the 2-year phase III studies comparing dutasteride with placebo (Roehrborn et al, 2002). An analysis of over 100 possible outcome predictors alone or in combination revealed a combination of serum PSA, urinating more than every 2 hours, symptom problem index, maximum urinary flow rate, and hesitancy as being only slightly superior to PSA alone in predicting AUR episodes (Roehrborn et al, 2001).
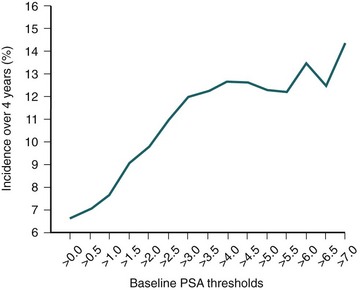
Figure 91–24 Incidence of spontaneous or precipitated acute urinary retention in the Proscar Long-Term Efficacy and Safety Study over 4 years stratified by increasing thresholds of serum prostate-specific antigen (PSA) at baseline.
(From Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology 1999;53[3]:473–80.)
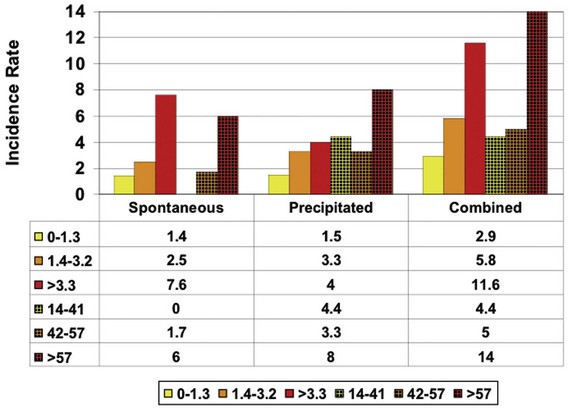
Figure 91–25 Spontaneous, precipitated, or combined acute urinary retention incidence over 4 years in the Proscar Long-Term Efficacy and Safety Study stratified by tertiles of serum prostate-specific antigen or prostate volume at baseline.
(From Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology 1999;53[3]:473–80.)
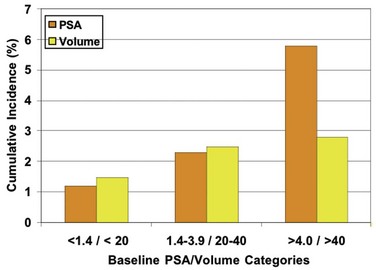
Figure 91–26 Cumulative incidence of acute urinary retention in placebo-treated patients in the Medical Therapy of Prostatic Symptoms study stratified by baseline prostate volume (yellow) and baseline serum prostate-specific antigen (PSA) (orange).
(From Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology 1999;53[3]:473–80.)
Surgery for Benign Prostatic Hyperplasia
Both surgery and AUR represent distinct end points in the disease progression of BPH. There are, however, distinct differences. AUR is an outcome mandating management, and surgery is one of the commonly employed management styles. AUR is probably one of the clearer indications for surgery, leaving the treating physician little choice in a patient who failed a trial without catheterization. However, most patients undergo surgery not for AUR but for symptoms (Holtgrewe et al, 1989). Depending on local practice pattern, AUR accounts for 5% to over 30% of the indications for surgery. AUR can be compared with a bone fracture. It is impossible for the physician in his or her interaction with the patient to increase or decrease the probability for that outcome to occur. Furthermore, once it has occurred, no interaction or consultation can undo it. In contrast, it is easy to see how patients can be influenced in their decision to undergo surgery by the consultation with the physician. The interaction style, the quoted probabilities of beneficial and harmful outcomes to occur, and many other factors cause considerable variability in the incidence rates of prostate-related surgery, an observation that caused the Agency for Health Care Policy and Research to develop guidelines for the treatment of BPH (Wennberg et al, 1988). This situation is similar to myocardial infarction and coronary artery bypass grafting (CABG). The analytical epidemiology of myocardial infarctions is well understood, and risk factors are characterized. Not all myocardial infarctions result in CABG, and, in fact, CABG is frequently performed for other indications than a recent infarction. Consequently, there is abundant literature focusing on the geographic variation in the usage of CABG. From this brief discussion it becomes clear that surgery for BPH is a softer end point from an epidemiologic point of view than AUR, and data on rates of prostatectomy need to be interpreted in light of variation in its use, from provider to provider, region to region, health care plan to health care plan, and over time.
Of all prostate surgeries, TURP and laser ablation of the prostate are still clearly the most common procedures and the best studied. Cross-sectional descriptive data on incidence rates are available from the Medicare database. While in 1962 TURP constituted over 50% of all major surgeries performed by American urologists, this number had dropped to 38% by 1986 (Holtgrewe et al, 1989; Mebust et al, 1989). Although the number of TURPs performed on Medicare patients declined from an all time peak of 258,000 in 1987 to 168,000 in 1993—a reduction by 34%—it remains second only to cataract surgery on the list of Medicare’s most costly surgical procedures. A 20% sample of Medicare beneficiaries was examined to further specify rates of TURP in the United States. In 1990 the rates of TURP (including all indications) were approximately 25, 19, and 13 per 1000 for men older than the age of 75, 70 to 74, and 65 to 69, respectively. The 30-day mortality after TURP for the treatment of BPH decreased from 1.20% in 1984 to 0.77% in 1990 (Lu-Yao et al, 1994). Compared with the period 1984 to 1990, age-adjusted rates of TURP for BPH during 1991 to 1997 declined further by approximately 50% for white (14.6 to 6.72/1000) and 40% for black (11.8 to 6.58/1000) men (Wasson et al, 2000). Medicare databases are only relevant to those men older than age 65 years enrolled in Medicare and therefore are less interesting from a longitudinal epidemiologic point of view.
Older series of the natural history of BPH such as the one reported by Craigen and coworkers (1969) projected somewhat unrealistic estimates of 35% incidence of prostatectomy at 1 year and 45% at 7 years. Diokno and colleagues (1992) reported an annual incidence rate of 2.6% and 3.3% for years 1 and 2 in their cohort of men followed longitudinally (1992). Frequency, hesitancy, straining, and an interrupted stream were all associated with an increased risk.
The first study of substantial quality reporting on incidence rates and risk factors of prostate surgery was the Baltimore Longitudinal Study of Aging (BLSA) (Arrighi et al, 1990, 1991; Guess et al, 1990). Over 1000 men were observed for 30 years with yearly symptom assessments, questionnaires, and examinations. Age, incomplete emptying, change in size, and force of stream were all independently associated with the risk of prostate surgery, as was a reportedly enlarged prostate by DRE. Of 464 men without risk factors, only 3% required surgery during follow-up. For men with one risk factor the cumulative incidence was 9%, with two risk factors 16%, and with three risk factors even 37%. In a similar study, namely, the Veterans Affairs Normative Aging Study, nocturia and hesitancy emerged as independent predictors of surgery in 1868 men aged 49 to 68 observed for more than 20 years (Hindley et al, 2001). Age and five LUTS (dysuria, incontinence, trouble initiating flow, nocturia, and slow stream) were associated with the risk of surgery in 16,219 men over 40 years enrolled in the Kaiser Permanente Health Plan in California, of whom 1027 men underwent prostatectomy over 12 years of follow-up (Sidney et al, 1991a, 1991b).
In the Veterans Affairs cooperative trial comparing surgery with watchful waiting, 65 of 276 (24%) patients assigned to watchful waiting crossed over to surgery within 3 years of follow-up, of which 20 met predefined end points (azotemia, high residual urine volumes, incontinence, or high AUASI scores). High baseline bother score was a strong predictor of requiring surgery (Wasson et al, 1995).
The probability of undergoing surgery over 4 years increased from 10% in those men diagnosed with BPH who had mild symptoms to 24% in those with moderate and 39% in those with severe symptoms at baseline as reported in a natural history and observation study by Barry and colleagues (1997a).
The Olmsted County study and the placebo-treated patients from PLESS provide additional insights into the risk factors for undergoing prostate surgery in either community-dwelling men or men enrolled in a BPH treatment trial.
In the Olmsted County study during more than 10,000 patient-years of follow-up 167 men were treated, yielding an overall incidence of 16.0/1000 patient-years. There was a strong age-related increase in risk of any treatment from 3.3/1000 patient-years for men 40 to 49 years old to more than 30/1000 patient-years for those 70 years old or older. Men with moderate to severe symptoms, depressed peak urinary flow rates (<12 mL/sec), enlarged prostate (>30 mL), or elevated serum PSA (≥1.4 ng/mL) had about four times the risk of BPH treatment than those who did not. After adjustment for all measures simultaneously an enlarged prostate (hazard ratio 2.3, 95% CI 1.1 to 4.7), depressed peak flow rate (hazard ratio 2.7, 95% CI 1.4 to 5.3), and moderate to severe symptoms (hazard ratio 5.3, 95% CI 2.5 to 11.1) at baseline each independently predicted subsequent treatment. Overall nearly 1 in 4 men received treatment in the eighth decade of life. These data suggest that men with moderate to severe LUTS, impaired flow rates, or enlarged prostates are more likely to undergo treatment, with increases in risk of similar magnitude to those associated with adverse outcomes, such as AUR (Jacobsen et al, 1999).
Over 1500 patients with moderate LUTS and enlarged prostate glands were followed in PLESS on placebo for 4 years. Of these, 10% or 2.5% per year underwent surgery for BPH (McConnell et al, 1998). Whereas the hazard of undergoing surgery was linear, that is, it remained constant throughout the duration of the study, it was different when patients were stratified by either prostate volume or serum PSA in tertiles at the beginning of the study (Fig. 91–27). Similar to the incidence of AUR, the rates of surgery increased from 6.2% to 14.6% for patients in the lowest to the highest PSA tertile and from 6.7% to 14.0% from the lowest to the highest prostate volume tertile. In MTOPS the incidence of invasive therapy for BPH in the placebo group increased equally nearly linearly when stratifying by baseline serum PSA or prostate volume (Fig. 91–28) (McConnell et al, 2003).
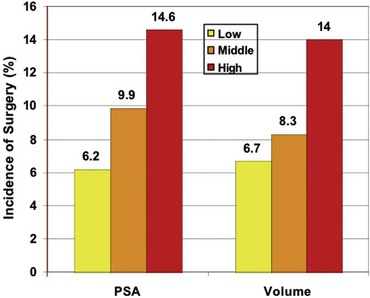
Figure 91–27 Incidence of surgery stratified by tertiles of serum prostate-specific antigen (PSA) and prostate volume in placebo-treated patients in the Proscar Long-Term Efficacy and Safety Study.
(From Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology 1999;53[3]:473–80.)
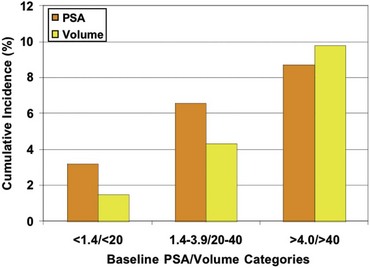
Figure 91–28 Cumulative incidence of invasive therapy (surgery) for benign prostatic hyperplasia in placebo-treated patients in the Medical Therapy of Prostatic Symptoms study stratified by baseline prostate volume (yellow) and baseline serum prostate-specific antigen (PSA) (orange).
(From Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology 1999;53[3]:473–80.)
Key Points: Epidemiology and Natural History
Abrams P. Objective evaluation of bladder outlet obstruction [review]. Br J Urol. 1995;76(Suppl. 1):11-15.
Abrams P, Cardozo L, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37-49.
Abrams PH, Farrar DJ, et al. The results of prostatectomy: a symptomatic and urodynamic analysis of 152 patients. J Urol. 1979;121(5):640-642.
American Urological Association Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia. Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003;170(2 Pt. 1):530-547.
Andriole G, Bruchovsky N, et al. Dihydrotestosterone and the prostate: the scientific rationale for 5alpha-reductase inhibitors in the treatment of benign prostatic hyperplasia. J Urol. 2004;172(4 Pt. 1):1399-1403.
Arrighi HM, Guess HA, et al. Symptoms and signs of prostatism as risk factors for prostatectomy. Prostate. 1990;16:253-261.
Arrighi HM, Metter EJ, et al. Natural history of benign prostatic hyperplasia and risk of prostatectomy. Urology. 1991;38(1):4-8.
Barry MJ, Cockett AT, Holtgrewe HL, et al. Relationship of symptoms of prostatism to commonly used physiological and anatomical measures of the severity of benign prostatic hyperplasia. J Urol. 1993;150:351-358.
Barry MJ, Fowler FJJr, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549-1557. discussion 1564
Barry MJ, Williford WO, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? [see comments]. J Urol. 1995;154(5):1770-1774.
Berry SJ, Coffey DS, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474-479.
Berry SJ, Coffey DS, et al. Effect of age, castration, and testosterone replacement on the development and restoration of canine benign prostatic hyperplasia. Prostate. 1986;9:295-302.
Berry SJ, Coffey DS, et al. Effects of aging on prostate growth in beagles. Am J Physiol. 1986;250:R1039-R1046.
Boyle P, Maisonneuve P, et al. Decrease in mortality from benign prostatic hyperplasia: a major unheralded health triumph [see comments]. J Urol. 1996;155(1):176-180.
Boyle P, Robertson C, et al. The association between lower urinary tract symptoms and erectile dysfunction in four centres: the UrEpik study. BJU Int. 2003;92(7):719-725.
Bruskewitz RC, Iversen P, et al. Value of postvoid residual urine determination in evaluation of prostatism. Urology. 1982;20:602-604.
Chapple CR, Wein AJ, et al. Lower urinary tract symptoms revisited: a broader clinical perspective. Eur Urol. 2008;54(3):563-569.
Cunha GR. Role of mesenchymal-epithelial interactions in normal and abnormal development of the mammary gland and prostate [review]. Cancer. 1994;74(3):1030-1044.
Cunha GR, Chung LW, Shannon JM, et al. Hormone-induced morphogenesis and growth: role of mesenchymal-epithelial interactions. Recent Prog Horm Res. 1983;39:559.
Flanigan RC, Reda DJ, et al. 5-Year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998;160(1):12-16. discussion 16–17
Garraway WM, Armstrong C, et al. Follow-up of a cohort of men with untreated benign prostatic hyperplasia. Eur Urol. 1993;24(3):313-318.
Girman CJ. Natural history and epidemiology of benign prostatic hyperplasia: relationship among urologic measures. Urology. 1998;51(Suppl.):8-12.
Girman CJ, Epstein RS, et al. Natural history of prostatism: impact of urinary symptoms on quality of life in 2115 randomly selected community men. Urology. 1994;44(6):825-831.
Girman CJ, Jacobsen SJ, et al. Natural history of prostatism: relationship among symptoms, prostate volume and peak urinary flow rate. J Urol. 1995;153(5):1510-1515.
Girman CJ, Jacobsen SJ, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998;51(3):428-436.
Glynn RJ, Campion EW, et al. The development of benign prostatic hyperplasia among volunteers in the normative aging study. Am J Epidemiol. 1985;121(1):78-90.
Gormley GJ, Stoner E, et al. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group [see comments]. N Engl J Med. 1992;327(17):1185-1191.
Gosling JA, Dixon JS. Structure of trabeculated detrusor smooth muscle in cases of prostatic hypertrophy. Urol Int. 1980;35(5):351-355.
Gosling JA, Gilpin SA, et al. Decrease in the autonomic innervation of human detrusor muscle in outflow obstruction. J Urol. 1986;136:501.
Holtgrewe HL, Mebust WK, et al. Transurethral prostatectomy: practice aspects of the dominant operation in American urology. J Urol. 1989;141(2):248-253.
Irwin DE, Milsom I, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306-1314. discussion 1314–15
Isaacs JT. Prostate stem cells and benign prostatic hyperplasia. Prostate. 2008;68(9):1025-1034.
Jacobsen SJ, Jacobson DJ, et al. Frequency of sexual activity and prostatic health: fact or fairy tale? Urology. 2003;61(2):348-353.
Kaplan SA, Wein AJ, et al. Urinary retention and post-void residual urine in men: separating truth from tradition. J Urol. 2008;180(1):47-54.
Kramer G, Mitteregger D, et al. Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol. 2007;51(5):1202-1216.
Kyprianou N, Tu H, et al. Apoptotic versus proliferative activities in human benign prostatic hyperplasia. Hum Pathol. 1996;27(7):668-675.
Lepor H, Tang R, Meretyk S, Shapiro E. The alpha-adrenoceptor subtype mediating the tension of human prostatic smooth muscle. Prostate. 1993;22:301-307.
Lu-Yao GL, Barry MJ, et al. Transurethral resection of the prostate among Medicare beneficiaries in the United States: time trends and outcomes. Prostate Patient Outcomes Research Team (PORT). Urology. 1994;44(5):692-698. discussion 698–9
Marberger M, Roehrborn CG, et al. Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. J Clin Endocrinol Metab. 2006;91(4):1323-1328.
McConnell JD, Barry MJ, et al. Benign prostatic hyperplasia: diagnosis and treatment. Clinical practice guideline no. 8. Rockville, MD: U.S. Department of Health and Human Services, Agency for Health Care Policy and Research, Public Health Service; 1994. p. 1–17
McConnell JD, Bruskewitz R, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride Long-Term Efficacy and Safety Study Group. N Engl J Med. 1998;338(9):557-563.
McConnell JD, Roehrborn C, et al. The long-term effects of doxazosin, finasteride and the combination on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349(25):2385-2396.
McNeal J. Pathology of benign prostatic hyperplasia: insight into etiology [review]. Urol Clin North Am. 1990;17:477-486.
McVary KT. Erectile dysfunction and lower urinary tract symptoms secondary to BPH. Eur Urol. 2005;47(6):838-845.
Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications: a cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243-247.
Nordling J. The aging bladder—a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol. 2002;37(8–9):991-999.
Oishi K, Boyle P, et al. Epidemiology and natural history of benign prostatic hyperplasia. In: 4th International consultation on benign prostatic hyperplasia. Plymouth (UK): Plymbridge Distributors Ltd; 1989:23-59.
Parsons JK. Modifiable risk factors for benign prostatic hyperplasia and lower urinary tract symptoms: new approaches to old problems. J Urol. 2007;178(2):395-401.
Partin AW, Oesterling JE, et al. Influence of age and endocrine factors on the volume of benign prostatic hyperplasia. J Urol. 1991;145(2):405-409.
Partin AW, Page WF, et al. Concordance rates for benign prostatic disease among twins suggest hereditary influence. Urology. 1994;44(5):646-650.
Roehrborn CG, Boyle P, et al. Serum prostate-specific antigen and prostate volume predict long-term changes in symptoms and flow rate: results of a four-year, randomized trial comparing finasteride versus placebo. PLESS Study Group. Urology. 1999;54(4):662-669.
Roehrborn CG, Boyle P, et al. Serum prostate-specific antigen as a predictor of prostate volume in men with benign prostatic hyperplasia. Urology. 1999;53(3):581-589.
Roehrborn CG, Bruskewitz R, et al. Urinary retention in patients with BPH treated with finasteride or placebo over 4 years: characterization of patients and ultimate outcomes. The PLESS Study Group. Eur Urol. 2000;37(5):528-536.
Roehrborn CG, Lange JL, et al. Changes in amount and intracellular distribution of androgen receptor in human foreskin as a function of age. J Clin Invest. 1987;79(1):44-47.
Roehrborn CG, McConnell JD, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology. 1999;53(3):473-480.
Roehrborn CG, Schwinn DA. Alpha1-adrenergic receptors and their inhibitors in lower urinary tract symptoms and benign prostatic hyperplasia. J Urol. 2004;171(3):1029-1035.
Rosen R, Altwein J, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol. 2003;44(6):637-649.
Rosen RC, Coyne KS, et al. Beyond the cluster: methodological and clinical implications in the Boston Area Community Health survey and EPIC studies. BJU Int. 2008;101(10):1274-1278.
Russell DW, Wilson JD. Steroid 5alpha-reductase: two genes/two enzymes. Annu Rev Biochem. 1994;63:25.
Sagnier PP, Girman CJ, et al. International comparison of the community prevalence of symptoms of prostatism in four countries. Eur Urol. 1996;29(1):15-20.
Sech SM, Montoya JD, et al. The so-called “placebo effect” in benign prostatic hyperplasia treatment trials represents partially a conditional regression to the mean induced by censoring. Urology. 1998;51(2):242-250.
Sherwood JB, McConnell JD, et al. Heterogeneity of 5 alpha-reductase gene expression in benign prostatic hyperplasia. J Urol. 2003;169(2):575-579.
Steers WD, Ciambotti J, Erdman S, de Groat WC. Morphological plasticity in efferent pathways to the urinary bladder of the rat following urethral obstruction. J Neurosci. 1990;19:1943.
Walsh PC, Hutchins GM, Ewing LL. Tissue content of dihydrotestosterone in human prostatic hyperplasia is not supernormal. J Clin Invest. 1983;72:1772-1777.
Walsh PC, Wilson JD. The induction of prostatic hypertrophy in the dog with androstanediol. J Clin Invest. 1976;57:1093.
Wang W, Bergh A, et al. Chronic inflammation in benign prostate hyperplasia is associated with focal upregulation of cyclooxygenase-2, Bcl-2, and cell proliferation in the glandular epithelium. Prostate. 2004;61(1):60-72.
Wang Z, Tufts R, et al. Genes regulated by androgen in the rat ventral prostate. Proc Natl Acad Sci U S A. 1997;94(24):12999-13004.
Wasson JH, Bubolz TA, et al. Transurethral resection of the prostate among medicare beneficiaries: 1984 to 1997. For the Patient Outcomes Research Team for Prostatic Diseases. J Urol. 2000;164(4):1212-1215.
Wasson JH, Reda DJ, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995;332(2):75-79.
Wein AJ, Coyne KS, et al. The impact of lower urinary tract symptoms on male sexual health: EpiLUTS. BJU Int. 2009;103(Suppl. 3):33-41.
Wennberg JE, Mulley AGJr, et al. An assessment of prostatectomy for benign urinary tract obstruction: geographic variations and the evaluation of medical care outcomes. JAMA. 1988;259(20):3027-3030.
Yang G, Timme TL, et al. Transforming growth factor beta 1 transduced mouse prostate reconstitutions: II. Induction of apoptosis by doxazosin. Prostate. 1997;33(3):157-163.
Zucchetto A, Tavani A, et al. History of weight and obesity through life and risk of benign prostatic hyperplasia. Int J Obes Relat Metab Disord. 2005;29(7):798-803.
Abbou CC, Colombel M, et al. The efficacy of microwave induced hyperthermia in the treatment of BPH: the Paris public hospitals’ experience. In: Kurth KH, Newling DWW, editors. Benign prostatic hyperplasia: recent progress in clinical research and practice. New York: Wiley-Liss; 1994:449-454.
Abrams P. Objective evaluation of bladder outlet obstruction [review]. Br J Urol. 1995;76(Suppl. 1):11-15.
Abrams P, Cardozo L, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37-49.
Abrams PH, Farrar DJ, et al. The results of prostatectomy: a symptomatic and urodynamic analysis of 152 patients. J Urol. 1979;121(5):640-642.
Alarid ET, et al. Keratinocyte growth factor functions in epithelial induction during seminal vesicle development. Proc Nat Acad Sci U S A. 1994;91:1074-1078.
Altwein JE, Keuler FU. Benign prostatic hyperplasia and erectile dysfunction: a review. Urol Int. 1992;48(1):53-57.
American Urological Association Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia. Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003;170(2 Pt. 1):530-547.
Andersen JT, Nickel JC, et al. Finasteride significantly reduces acute urinary retention and need for surgery in patients with symptomatic benign prostatic hyperplasia. Urology. 1997;49:839-845.
Andriole G, Bruchovsky N, et al. Dihydrotestosterone and the prostate: the scientific rationale for 5alpha-reductase inhibitors in the treatment of benign prostatic hyperplasia. J Urol. 2004;172(4 Pt. 1):1399-1403.
Anglin IE, Glassman DT, et al. Induction of prostate apoptosis by alpha1-adrenoceptor antagonists: mechanistic significance of the quinazoline component. Prostate Cancer Prostatic Dis. 2002;5(2):88-95.
Anjum I, Ahmed M, et al. Prostatic infarction/infection in acute urinary retention secondary to benign prostatic hyperplasia. J Urol. 1998;160(3 Pt. 1):792-793.
Araki H, Watanabe H, et al. High-risk group for benign prostatic hypertrophy. Prostate. 1983;4(3):253-264.
Arrighi HM, Guess HA, et al. Symptoms and signs of prostatism as risk factors for prostatectomy. Prostate. 1990;16:253-261.
Arrighi HM, Metter EJ, et al. Natural history of benign prostatic hyperplasia and risk of prostatectomy. Urology. 1991;38(1):4-8.
Azadzoi KM. Effect of chronic ischemia on bladder structure and function. Adv Exp Med Biol. 2003;539(Pt. A):271-280.
Azadzoi KM, Babayan RK, et al. Chronic ischemia increases prostatic smooth muscle contraction in the rabbit. J Urol. 2003;170(2 Pt. 1):659-663.
Azadzoi KM, Radisavljevic ZM, et al. Effects of ischemia on tachykinin-containing nerves and neurokinin receptors in the rabbit bladder. Urology. 2008;71(5):979-983.
Azadzoi KM, Tarcan T, et al. Overactivity and structural changes in the chronically ischemic bladder. J Urol. 1999;162(5):1768-1778.
Badia X, Rodriguez F, et al. Influence of sociodemographic and health status variables on the American Urological Association symptom scores in patients with lower urinary tract symptoms. Urology. 2001;57(1):71-77.
Ball AJ, Feneley RC, et al. The natural history of untreated “prostatism. Br J Urol. 1981;53(6):613-616.
Barnboym E, Ahrens A, et al. Effect of scrambling on the short-term reliability of the American Urological Association Symptom Index. Urology. 1999;53(3):568-573.
Barrack ER, Bujnovszky P, et al. Subcellular distribution of androgen receptors in human normal, benign hyperplastic, and malignant prostatic tissues: characterization of nuclear salt-resistant receptors. Cancer Res. 1983;43(3):1107-1116.
Barrack ER, Berry SJ. DNA synthesis in the canine prostate: effects of androgen induction and estrogen treatment. Prostate. 1987;10:45-56.
Barry MJ. Epidemiology and natural history of benign prostatic hyperplasia. Urol Clin North Am. 1990;17:495-507.
Barry MJ. Medical outcomes research and benign prostatic hyperplasia. Prostate [Suppl.]. 1990;3:61-74.
Barry MJ, Cockett AT, Holtgrewe HL, et al. Relationship of symptoms of prostatism to commonly used physiological and anatomical measures of the severity of benign prostatic hyperplasia. J Urol. 1993;150:351-358.
Barry MJ, Fowler FJJr, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549-1557. discussion 1564
Barry MJ, Fowler FJJr, et al. Correlation of the American Urological Association symptom index with self-administered versions of the Madsen-Iversen, Boyarsky and Maine Medical Assessment Program symptom indexes. Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1558-1563. discussion 1564
Barry MJ, Fowler FJJr, et al. The American Urological Association symptom index: does mode of administration affect its psychometric properties? J Urol. 1995;154(3):1056-1059.
Barry MJ, Fowler FJJr, et al. Measuring disease-specific health status in men with benign prostatic hyperplasia. Measurement Committee of the American Urological Association. Med Care. 1995;33(4):AS145-AS155.
Barry MJ, Fowler FJJr, et al. The natural history of patients with benign prostatic hyperplasia as diagnosed by North American urologists. J Urol. 1997;157:10-15.
Barry MJ, Fowler FJJr, et al. A nationwide survey of practicing urologists: current management of benign prostatic hyperplasia and clinically localized prostate cancer. J Urol. 1997;158(2):488-491. discussion 492
Barry MJ, Girman CJ, et al. Using repeated measures of symptom score, uroflowmetry and prostate specific antigen in the clinical management of prostate disease. Benign Prostatic Hyperplasia Treatment Outcomes Study Group. J Urol. 1995;153(1):99-103.
Barry MJ, Williford WO, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? [see comments]. J Urol. 1995;154(5):1770-1774.
Bautista O, Kusek J, et al. Study design of the Medical Therapy of Prostatic Symptoms (MTOPS) trial. Controlled Clin Trials. 2003;24:224-243.
Bdesha AS, Bunce CJ, et al. A sham controlled trial of transurethral microwave therapy with subsequent treatment of the control group. J Urol. 1994;152:453-458.
Beck AD, Gaudin HJ. The measurement and significance of the urinary flow rate. Aust N Z J Surg. 1969;39(1):99-102.
Bedford MT, van Helden PD. Hypomethylation of DNA in pathological conditions of the human prostate. Cancer Res. 1987;47(20):5274-5276.
Begun FP, Story MT, et al. Regional concentration of basic fibroblast growth factor in normal and benign hyperplastic human prostates. J Urol. 1995;153(3 Pt. 1):839-843.
Benaim EA, Montoya JD, et al. Characterization of prostate size, PSA and endocrine profiles in patients with spinal cord injuries. Prostate Cancer Prostatic Dis. 1998;1(5):250-255.
Bennett H, Baggenstoss A, et al. The testis, breast, and prostate of men who die of cirrhosis of the liver. Am J Clin Pathol. 1950;20:814.
Berry SJ, Coffey DS, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474-479.
Berry SJ, Coffey DS, et al. Effect of age, castration, and testosterone replacement on the development and restoration of canine benign prostatic hyperplasia. Prostate. 1986;9:295-302.
Berry SJ, Coffey DS, et al. Effects of aging on prostate growth in beagles. Am J Physiol. 1986;250:R1039-R1046.
Birkhoff JD, Wiederhorn AR, et al. Natural history of benign prostatic hypertrophy and acute urinary retention. Urology. 1976;7(1):48-52.
Blotnik S, et al. T lymphocytes synthesize and export heparin-binding epidermal growth factor–like growth factor and basic fibroblast growth factor, mitogens for vascular cells and fibroblasts: differential production and release by CD4+ and CD8+ T cells. Proc Natl Acad Sci U S A. 1994;91:2890-2894.
Blute ML, Tomera KM, et al. Transurethral microwave thermotherapy for management of benign prostatic hyperplasia: results of the United States Prostatron Cooperative Study [see comments]. J Urol. 1993;150(5):1591-1596.
Bosch JL, Hop WC, et al. Parameters of prostate volume and shape in a community based population of men 55 to 74 years old. J Urol. 1994;152(5):1501-1505.
Bosch JL, Hop WC, et al. The International Prostate Symptom Score in a community-based sample of men between 55 and 74 years of age: prevalence and correlation of symptoms with age, prostate volume, flow rate and residual urine volume. Br J Urol. 1995;75(5):622-630.
Bosch JL, Hop WC, et al. Natural history of benign prostatic hyperplasia: appropriate case definition and estimation of its prevalence in the community. Urology. 1995;46(3):34-40.
Bosch JL, Kranse R, et al. Reasons for the weak correlation between prostate volume and urethral resistance parameters in patients with prostatism. J Urol. 1995;153(3):689-693.
Bousema JT, Bussemakers MJ, et al. Polymorphisms in the vitamin D receptor gene and the androgen receptor gene and the risk of benign prostatic hyperplasia. Eur Urol. 2000;37(2):234-238.
Boyle P. Some remarks on the epidemiology of acute urinary retention. Arch Ital Urol Androl. 1998;70(2):77-82.
Boyle P, Maisonneuve P, et al. Decrease in mortality from benign prostatic hyperplasia: a major unheralded health triumph [see comments]. J Urol. 1996;155(1):176-180.
Boyle P, Napalkov P. The epidemiology of benign prostatic hyperplasia and observations on concomitant hypertension. Scand J Urol Nephrol Suppl. 1995;168:7-12.
Boyle P, Robertson C, et al. The association between lower urinary tract symptoms and erectile dysfunction in four centres: the UrEpik study. BJU Int. 2003;92(7):719-725.
Breum L, Klarskov P, et al. Significance of acute urinary retention due to infravesical obstruction. Scand J Urol Nephrol. 1982;16:21-24.
Bruskewitz R, Girman CJ, et al. Effect of finasteride on bother and other health-related quality of life aspects associated with benign prostatic hyperplasia. PLESS Study Group. Proscar Long-term Efficacy and Safety Study. Urology. 1999;54(4):670-678.
Bruskewitz RC, Iversen P, et al. Value of postvoid residual urine determination in evaluation of prostatism. Urology. 1982;20:602-604.
Burchardt M, Burchardt T, et al. Vascular endothelial growth factor-α expression in the rat ventral prostate gland and the early effects of castration. Prostate. 2000;43(3):184-194.
Buttyan R, Ghafar MA, et al. The effects of androgen deprivation on the prostate gland: cell death mediated by vascular regression [review]. Curr Opin Urol. 2000;10(5):415-420.
Caine M, Schuger L. The “capsule” in benign prostatic hypertrophy. Publication No. 87–2881. Bethesda (MD): U.S. Department of Health and Human Services; 1987. p. 221
Canto EI, Singh H, et al. Serum BPSA outperforms both total PSA and free PSA as a predictor of prostatic enlargement in men without prostate cancer. Urology. 2004;63(5):905-910. discussion 910–11
Carson C3rd, Rittmaster R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology. 2003;61(4 Suppl. 1):2-7.
Carter HB, Coffey DS. The prostate: an increasing medical problem. Prostate. 1990;16(1):39-48.
Castro P, Giri D, et al. Cellular senescence in the pathogenesis of benign prostatic hyperplasia. Prostate. 2003;55(1):30-38.
Castro P, Xia C, et al. Interleukin-8 expression is increased in senescent prostatic epithelial cells and promotes the development of benign prostatic hyperplasia. Prostate. 2004;60(2):153-159.
Cathcart P, van der Meulen J, et al. Incidence of primary and recurrent acute urinary retention between 1998 and 2003 in England. J Urol. 2006;176(1):200-204. discussion 204
Chai TC, Andersson KE, et al. Altered neural control of micturition in the aged f344 rat. Urol Res. 2000;28(5):348-354.
Chapple CR, Crowe R, et al. The innervation of the human prostate gland—the changes associated with benign enlargement. J Urol. 1991;146(6):1637-1644.
Chapple CR, Wein AJ, et al. Lower urinary tract symptoms revisited: a broader clinical perspective. Eur Urol. 2008;54(3):563-569.
Chatterjee B. The role of the androgen receptor in the development of prostatic hyperplasia and prostate cancer. Mol Cell Biochem. 2003;253(1–2):89-101.
Cher ML, Abernathy BB, et al. Smooth-muscle myosin heavy-chain isoform expression in bladder-outlet obstruction. World J Urol. 1996;14(5):295-300.
Chicharro-Molero JA, Burgos-Rodriguez R, et al. Prevalence of benign prostatic hyperplasia in Spanish men 40 years old or older. J Urol. 1998;159(3):878-882.
Choi J, Shendrik I, et al. Expression of senescence-associated beta-galactosidase in enlarged prostates from men with benign prostatic hyperplasia. Urology. 2000;56(1):160-166.
Chopra IJ, Tulchinsky D, et al. Estrogen-androgen imbalance in hepatic cirrhosis: studies in 13 male patients. Ann Intern Med. 1973;79(2):198-203.
Christ GJ, Liebert M. Proceedings of the Baltimore smooth muscle meeting: identifying research frontiers and priorities for the lower urinary tract. J Urol. 2005;173(4):1406-1409.
Chung W, Nehra A, et al. Epidemiologic evidence evaluating lower urinary tract symptoms (LUTS) and sexual dysfunction in the Olmsted County Study of Urinary Tract Symptoms and Health Status Among Men. J Urol. 2003;169(4):323A.
Chute CG, Panser LA, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993;150(1):85-89.
Chyou PH, Nomura AM, et al. A prospective study of alcohol, diet, and other lifestyle factors in relation to obstructive uropathy. Prostate. 1993;22(3):253-264.
Clarke R. The prostate and the endocrines, 1919.
Clemow DB, Steers WD, et al. Altered regulation of bladder nerve growth factor and neurally mediated hyperactive voiding. Am J Physiol. 1998;275(4 Pt. 2):R1279-R1286.
Clemow DB, Steers WD, et al. Stretch-activated signaling of nerve growth factor secretion in bladder and vascular smooth muscle cells from hypertensive and hyperactive rats. J Cell Physiol. 2000;183(3):289-300.
Cohen P, Nunn SE, et al. Transforming growth factor-beta induces growth inhibition and IGF-binding protein-3 production in prostatic stromal cells: abnormalities in cells cultured from benign prostatic hyperplasia tissues. J Endocrinol. 2000;164(2):215-223.
Colombel M, Vacherot F, et al. Zonal variation of apoptosis and proliferation in the normal prostate and in benign prostatic hyperplasia. Br J Urol. 1998;82(3):380-385.
Corica FA, Jacobsen SJ, et al. Prostatic central zone volume, lower urinary tract symptom severity and peak urinary flow rates in community dwelling men. J Urol. 1999;161:831-834.
Coyne KS, Kaplan SA, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int. 2009;103(Suppl. 3):24-32.
Craigen AA, Hickling JB, et al. Natural history of prostatic obstruction. J R Coll Gen Pract. 1969;18:226-232.
Cross NA, Reid SV, et al. Opposing actions of TGFbeta1 and FGF2 on growth, differentiation and extracellular matrix accumulation in prostatic stromal cells. Growth Factors. 2006;24(4):233-241.
Cunha GR. Role of mesenchymal-epithelial interactions in normal and abnormal development of the mammary gland and prostate [review]. Cancer. 1994;74(3):1030-1044.
Cunha GR. Stromal-epithelial interactions during development of the male urogenital system. In: 1996 International Symposium on Biology of Prostate Growth, Washington, DC, March 1996.
Cunha GR, Chung LW, et al. Stromal-epithelial interactions in sex differentiation. Biol Reprod. 1980;22:19-42.
Cunha GR, Chung LW, Shannon JM, et al. Hormone-induced morphogenesis and growth: role of mesenchymal-epithelial interactions. Recent Prog Horm Res. 1983;39:559-598.
Cunha GR, Donjacour A. Stromal-epithelial interactions in normal and abnormal prostatic development. Prog Clin Biol Res. 1987;239:251-272.
Cunha GR, Hayward SW, et al. Role of the stromal microenvironment in carcinogenesis of the prostate. Int J Cancer. 2003;107(1):1-10.
d’Ancona FC, Francisca EA, et al. The predictive value of baseline variables in the treatment of benign prostatic hyperplasia using high-energy transurethral microwave thermotherapy. Br J Urol. 1998;82(6):808-813.
Dahle SE, Chokkalingam AP, et al. Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol. 2002;168(2):599-604.
Dalton FS, et al. Nonadrogenic role of testis in enhancing ventral prostate growth in rats. Prostate. 1990;16:225.
Daniell HW. Larger prostatic adenomas in obese men with no associated increase in obstructive uropathy [see comments]. J Urol. 1993;149(2):315-317.
Daniell HW. More stage A prostatic cancers, less surgery for benign hypertrophy in smokers. J Urol. 1993;149(1):68-72.
de la Rosette JJ, et al. Transurethral microwave thermotherapy (TUMT) in benign prostatic hyperplasia: placebo versus TUMT. Urology. 1994;44:58-63.
de la Rosette JJ, Witjes WP, et al. Relationships between lower urinary tract symptoms and bladder outlet obstruction: results from the ICS-”BPH” study. Neurourol Urodyn. 1998;17(2):99-108.
Dhanasekaran SM, Dash A, et al. Molecular profiling of human prostate tissues: insights into gene expression patterns of prostate development during puberty. FASEB J. 2005;19(2):243-245.
Dinh DT, Frauman AG, et al. Identification, distribution, and expression of angiotensin II receptors in the normal human prostate and benign prostatic hyperplasia. Endocrinology. 2001;142(3):1349-1356.
Dinh DT, Frauman AG, et al. Evidence for activation of the renin-angiotensin system in the human prostate: increased angiotensin II and reduced AT (1) receptor expression in benign prostatic hyperplasia. J Pathol. 2002;196(2):213-219.
Diokno AC, Brown MB, Goldstein N, Herzog AR. Epidemiology of bladder emptying symptoms in elderly men. J Urol. 1992;148(6):1817-1821.
DiPaola RS, Kumar P, et al. State-of-the-art prostate cancer treatment and research. A report from the Cancer Institute of New Jersey. N J Med. 2001;98(2):23-33.
Djavan B, Fong YK, et al. Longitudinal study of men with mild symptoms of bladder outlet obstruction treated with watchful waiting for four years. Urology. 2004;64:1144-1148.
Dong G, Rajah R, et al. Decreased expression of Wilms’ tumor gene WT-1 and elevated expression of insulin growth factor-II (IGF-II) and type 1 IGF receptor genes in prostatic stromal cells from patients with benign prostatic hyperplasia. J Clin Endocrinol Metab. 1997;82(7):2198-2203.
Donovan JL, Abrams P, et al. The ICS-’BPH’ Study: the psychometric validity and reliability of the ICSmale questionnaire. Br J Urol. 1996;77(4):554-562.
DeKlerk DP, Coffey DS, Ewing LL, et al. Comparison of spontaneous and experimentally induced canine prsptatic hyperplasia. J Clin Invest. 1979;64:842-849.
Drach GW, Steinbronn DV. Clinical evaluation of patients with prostatic obstruction: correlation of flow rates with voided, residual or total bladder volume. J Urol. 1986;135(4):737-740.
Eddy DM. Clinical decision making: from theory to practice. comparing benefits and harms: the balance sheet. JAMA. 1990;263:2493-2505.
Eddy DM. Applying cost-effectiveness analysis: the inside story. JAMA. 1992;268:2575-2582.
Eddy DM, Hasselblad V. FAST*PRO. Software for meta-analysis by the Confidence Profile Method. San Diego, CA: Academic Press; 1992.
Ekman P. BPH epidemiology and risk factors. Prostate [Suppl.]. 1989;2:23-31.
Eldrup E, Lindholm J, et al. Plasma sex hormones and ischemic heart disease. Clin Biochem. 1987;20(2):105-112.
Epstein RS, Deverka PA, et al. Validation of a new quality of life questionnaire for benign prostatic hyperplasia. J Clin Epidemiol. 1992;45(12):1431-1445.
Ezz el Din K, Kiemeney LA, et al. Correlation between uroflowmetry, prostate volume, postvoid residue, and lower urinary tract symptoms as measured by the International Prostate Symptom Score. Urology. 1996;48(3):393-397.
Fabiani ME, Sourial M, et al. Angiotensin II enhances noradrenaline release from sympathetic nerves of the rat prostate via a novel angiotensin receptor: implications for the pathophysiology of benign prostatic hyperplasia. J Endocrinol. 2001;171(1):97-108.
Farnsworth WE. Roles of estrogen and SHBG in prostate physiology [review]. Prostate. 1996;28(1):17-23.
Farnsworth WE. Estrogen in the etiopathogenesis of BPH [review]. Prostate. 1999;41(4):263-274.
Flanigan RC, Reda DJ, et al. 5-Year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998;160(1):12-16. discussion 16–17
Franks LM. Benign nodular hyperplasia of the prostate: a review. Ann R Coll Surg Engl (Lond). 1954;14:92-106.
Franks LM. Benign prostatic hypertrophy: gross and microscopic anatomy. NIH publication No. 76–1113–63. Bethesda, MD: U.S. Department of Health, Education, and Welfare; 1976.
Frea B, Annoscia S, et al. Correlation between liver cirrhosis and benign prostatic hyperplasia: a morphological study. Urol Res. 1987;15(5):311-314.
Freeman MR, et al. Peripheral blood T lymphocytes and T cells infiltrating human cancers express vascular endothelial growth factor: a potential role for T cells in angiogenesis. Cancer Res. 1995;55:4140-4145.
Fromont G, Chene L, et al. Molecular profiling of benign prostatic hyperplasia using a large scale real-time reverse transcriptase-polymerase chain reaction approach. J Urol. 2004;172(4 Pt. 1):1382-1385.
Garraway WM, Armstrong C, et al. Follow-up of a cohort of men with untreated benign prostatic hyperplasia. Eur Urol. 1993;24(3):313-318.
Garraway WM, et al. High prevalence of benign prostatic hypertrophy in the community. Lancet. 1991;338(8765):469-471.
Garraway WM, Russell EB, et al. Impact of previously unrecognized benign prostatic hyperplasia on the daily activities of middle-aged and elderly men. Br J Gen Pract. 1993;43:318-321.
Giovannucci E, Platz EA, et al. The CAG repeat within the androgen receptor gene and benign prostatic hyperplasia. Urology. 1999;53(1):121-125.
Giovannucci E, Rimm EB, et al. Obesity and benign prostatic hyperplasia. Am J Epidemiol. 1994;140:989-1002.
Giovannucci E, Stampfer MJ, et al. CAG repeat within the androgen receptor gene and incidence of surgery for benign prostatic hyperplasia in U.S. physicians. Prostate. 1999;39(2):130-134.
Giri D, Ittmann M. Interleukin-1alpha is a paracrine inducer of FGF7, a key epithelial growth factor in benign prostatic hyperplasia. Am J Pathol. 2000;157(1):249-255.
Girman CJ. Natural history and epidemiology of benign prostatic hyperplasia: relationship among urologic measures. Urology. 1998;51(4A Suppl.):8-12.
Girman CJ, Epstein RS, et al. Natural history of prostatism: impact of urinary symptoms on quality of life in 2115 randomly selected community men. Urology. 1994;44(6):825-831.
Girman CJ, Jacobsen SJ, et al. Natural history of prostatism: relationship among symptoms, prostate volume and peak urinary flow rate. J Urol. 1995;153(5):1510-1515.
Girman CJ, Jacobsen SJ, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998;51(3):428-436.
Girman CJ, Jacobsen SJ, et al. Association of health-related quality of life and benign prostatic enlargement. Eur Urol. 1999;35(4):277-284.
Girman CJ, Panser LA, et al. Natural history of prostatism: urinary flow rates in a community-based study. J Urol. 1993;150(3):887-892.
Giubilei G, Ponchietti R, et al. Accuracy of prostate volume measurements using transrectal multiplanar three-dimensional sonography. Int J Urol. 2005;12(10):936-938.
Glynn RJ, Campion EW, et al. The development of benign prostatic hyperplasia among volunteers in the normative aging study. Am J Epidemiol. 1985;121(1):78-90.
Golomb J, Lindner A, et al. Variability and circadian changes in home uroflowmetry in patients with benign prostatic hyperplasia compared to normal controls. J Urol. 1992;147:1044-1047.
Gong G, et al. Testosterone regulation of renal alpha-2B-adrenergic receptor mRNA levels. Hypertension. 1995;25:350-355.
Gormley GJ, Stoner E, et al. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group [see comments]. N Engl J Med. 1992;327(17):1185-1191.
Gosling JA, Dixon JS. Structure of trabeculated detrusor smooth muscle in cases of prostatic hypertrophy. Urol Int. 1980;35(5):351-355.
Gosling JA, Gilpin SA, et al. Decrease in the autonomic innervation of human detrusor muscle in outflow obstruction. J Urol. 1986;136:501.
Graversen PH, Gasser TC, et al. Controversies about indications for transurethral resection of the prostate [review]. J Urol. 1989;141(3):475-481.
Grayhack JT, Kozlowski JM, et al. The pathogenesis of benign prostatic hyperplasia: a proposed hypothesis and critical evaluation. J Urol. 1998;160(6 Pt. 2):2375-2380.
Grosse H. Frequency, localization and associated disorders in urinary calculi: analysis of 1671 autopsies in urolithiasis. Z Urol Nephrol. 1990;83:469-474.
Gu FL, Xia TL, et al. Preliminary study of the frequency of benign prostatic hyperplasia and prostatic cancer in China. Urology. 1994;44(5):688-691.
Guess HA. Epidemiology and natural history of benign prostatic hyperplasia [review]. Urol Clin North Am. 1995;22(2):247-261.
Guess HA, Arrighi HM, et al. Cumulative prevalence of prostatism matches the autopsy prevalence of benign prostatic hyperplasia. Prostate. 1990;17:241-246.
Guess HA, Chute CG, et al. Similar levels of urologic symptoms have similar impact on Scottish and American men—though Scots report less symptoms. J Urol. 1993;150:1701.
Gupta A, Aragaki C, et al. Relationship between prostate specific antigen and indexes of prostate volume in Japanese men. J Urol. 2005;173(2):503-506.
Gupta A, Gupta S, et al. Anthropometric and metabolic factors and risk of benign prostatic hyperplasia: a prospective cohort study of Air Force veterans. Urology. 2006;68(6):1198-1205.
Habuchi T, Suzuki T, et al. Association of vitamin D receptor gene polymorphism with prostate cancer and benign prostatic hyperplasia in a Japanese population. Cancer Res. 2000;60(2):305-308.
Haffner S, Taegtmeyer H. Epidemic obesity and the metabolic syndrome. Circulation. 2003;108(13):1541-1545.
Hall SA, Link CL, et al. Urological symptom clusters and health-related quality-of-life: results from the Boston Area Community Health Survey. BJU Int. 2009;103:1502-1508.
Hammarsten J, Hogstedt B. Clinical, anthropometric, metabolic and insulin profile of men with fast annual growth rates of benign prostatic hyperplasia. Blood Press. 1999;8(1):29-36.
Hammarsten J, Hogstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001;39(2):151-158.
Hammarsten J, Hogstedt B, et al. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998;1(3):157-162.
Hansen BJ, Flyger H, et al. Validation of the self-administered Danish Prostatic Symptom Score (DAN-PSS-1) system for use in benign prostatic hyperplasia. Br J Urol. 1995;76(4):451-458.
Harbitz TB, Haugen OA. Histology of the prostate in elderly men: a study in an autopsy series. Acta Pathol Microbiol Scand [A]. 1972;80(6):756-768.
Hastie KJ, Dickinson AJ, et al. Acute retention of urine: is trial without catheter justified? J R Coll Surg Edinb. 1990;35(4):225-227.
Haugen OA, Harbitz TB. Prostatic weight in elderly men: an analysis in an autopsy series. Acta Pathol Microbiol Scand [A] Pathol. 1972;80(6):769-777.
Hayek OR, Shabsigh A, et al. Castration induces acute vasoconstriction of blood vessels in the rat prostate concomitant with a reduction of prostatic nitric oxide synthase activity. J Urol. 1999;162(4):1527-1531.
Haylen BT, Ashby D, et al. Maximum and average urine flow rates in normal male and female populations—the Liverpool nomograms. Br J Urol. 1998;64:30-38.
Hedelin H, Johansson N, et al. Relationship between benign prostatic hyperplasia and lower urinary tract symptoms and correlation between prostate volume and serum prostate-specific antigen in clinical routine. Scand J Urol Nephrol. 2005;39(2):154-159.
Hieble JP, et al. International Union of Pharmacology X recommendation for nomenclature of alpha1-adrenoreceptors: consensus update. Pharm Rev. 1995;47:267-270.
Hindley RG, Mostafid AH, et al. The 2-year symptomatic and urodynamic results of a prospective randomized trial of interstitial radiofrequency therapy vs transurethral resection of the prostate. BJU Int. 2001;88(3):217-220.
Hochberg DA, Armenakas NA, et al. Relationship of prostate-specific antigen and prostate volume in patients with biopsy proven benign prostatic hyperplasia. Prostate. 2000;45(4):315-319.
Hoke GP, McWilliams GW. Epidemiology of benign prostatic hyperplasia and comorbidities in racial and ethnic minority populations. Am J Med. 2008;121(8 Suppl. 2):S3-10.
Holtgrewe HL, Mebust WK, et al. Transurethral prostatectomy: practice aspects of the dominant operation in American urology. J Urol. 1989;141(2):248-253.
Holtgrewe HL, Valk WL. Factors influencing the mortality and morbidity of transurethral prostatectomy: a study of 2015 cases. J Urol. 1962;87:450-459.
Holund B. Latent prostatic cancer in a consecutive autopsy series. Scand J Urol Nephrol. 1980;14(1):29-35.
Homma Y, Gotoh M, et al. Predictability of conventional tests for the assessment of bladder outlet obstruction in benign prostatic hyperplasia. Int J Urol. 1998;5(1):61-66.
Homma Y, Kawabe K, et al. Epidemiologic survey of lower urinary tract symptoms in Asia and Australia using the international prostate symptom score. Int J Urol. 1997;4(1):40-46.
Hunter DJ, Berra-Unamuno A, et al. Prevalence of urinary symptoms and other urological conditions in Spanish men 50 years old or older [see comments]. J Urol. 1996;155(6):1965-1970.
Hunter DJ, McKee CM, et al. Urinary symptoms: prevalence and severity in British men aged 55 and over. J Epidemiol Community Health. 1994;48(6):569-575.
Hunter DJ, McKee CM, et al. Health status and quality of life of British men with lower urinary tract symptoms: results from the SF-36. Urology. 1995;45(6):962-971.
Imajo C, Walden PD, et al. Evaluation of the effect of endothelin-1 and characterization of the selective endothelin a receptor antagonist pd155080 in the prostate. J Urol. 1997;158(1):253-257.
Irwin DE, Milsom I, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306-1314. discussion 1314–15
Isaacs JT. Antagonistic effect of androgen on prostatic cell death. Prostate. 1984;5:545-557.
Isaacs JT. Prostate stem cells and benign prostatic hyperplasia. Prostate. 2008;68(9):1025-1034.
Isaacs JT, Coffey DS. Etiology and disease process of benign prostatic hyperplasia. Prostate Suppl. 1987;2:33-50.
Jacobsen SJ, Girman CJ, et al. Natural history of prostatism: four-year change in urinary symptom frequency and bother. J Urol. 1995;153:300A.
Jacobsen SJ, Girman CJ, et al. New diagnostic and treatment guidelines for benign prostatic hyperplasia: potential impact in the United States. Arch Intern Med. 1995;155(5):477-481.
Jacobsen SJ, Girman CJ, et al. Natural history of prostatism: longitudinal changes in voiding symptoms in community dwelling men. J Urol. 1996;155(2):595-600.
Jacobsen SJ, Jacobson DJ, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997;158(2):481-487.
Jacobsen SJ, Jacobson DJ, et al. Treatment for benign prostatic hyperplasia among community dwelling men: the Olmsted County study of urinary symptoms and health status. J Urol. 1999;162(4):1301-1306.
Jacobsen SJ, Jacobson DJ, et al. Frequency of sexual activity and prostatic health: fact or fairy tale? Urology. 2003;61(2):348-353.
Jakobsen H, Torp-Pedersen S, et al. Ultrasonic evaluation of age-related human prostatic growth and development of benign prostatic hyperplasia. Scand J Urol Nephrol (Suppl). 1988;107:26-31.
Jolleys JV, Donovan JL, et al. Urinary symptoms in the community: how bothersome are they? Br J Urol. 1994;74(5):551-555.
Juniewicz PE, Berry SJ, et al. The requirement of the testis in establishing the sensitivity of the canine prostate to develop benign prostatic hyperplasia. J Urol. 1994;152(3):996-1001.
Kadow C, Feneley RC, et al. Prostatectomy or conservative management in the treatment of benign prostatic hypertrophy? Br J Urol. 1988;61(5):432-434.
Kakehi Y, Segawa T, et al. Down-regulation of macrophage inhibitory cytokine-1/prostate derived factor in benign prostatic hyperplasia. Prostate. 2004;59(4):351-356.
Kaplan S, Garvin D, et al. Impact of baseline symptom severity on future risk of benign prostatic hyperplasia-related outcomes and long-term response to finasteride. Urology. 2000;56(4):610-616.
Kaplan SA, Roehrborn CG, et al. Implications of recent epidemiology studies for the clinical management of lower urinary tract symptoms. BJU Int. 2009;103(Suppl. 3):48-57.
Kaplan SA, Te AE, et al. Transition zone index (TZI) as a method of assessing benign prostatic hyperplasia: correlation with symptoms, uroflow and detrusor pressure. J Urol. 1995;154:1764-1769.
Kaplan SA, Wein AJ, et al. Urinary retention and post-void residual urine in men: separating truth from tradition. J Urol. 2008;180(1):47-54.
Kariya KI, et al. Transcriptional enhancer factor-1 in cardiac myocytes interacts with an alpha1-adrenergic- and beta-protein kinase C-inducible element in the rat beta-myosin heavy chain promoter. J Biol Chem. 1993;268:26658-26662.
Karube K. Study of latent carcinoma of the prostate in the Japanese based on necropsy material. Tohodu J Exp Med. 1961;74:265-285.
Kasturi S, Russell S, et al. Metabolic syndrome and lower urinary tract symptoms secondary to benign prostatic hyperplasia. Curr Urol Rep. 2006;7(4):288-292.
Kerr JF, Searle SJ. Deletion of cells by apoptosis during castration induced involution in the rat prostate. Virchows Arch B Cell Pathol. 1973;13:87-102.
Kitsberg DI, Leder P. Keratinocyte growth factor induces mammary and prostatic hyperplasia and mammary adenocarcinoma in transgenic mice. Oncogene. 1996;13(12):2507-2515.
Klarskov P, Andersen JT, et al. Acute urinary retention in women: a prospective study of 18 consecutive cases. Scand J Urol Nephrol. 1987;21(1):29-31.
Kobayashi S, Tang R, et al. Binding and functional properties of endothelin receptor subtypes in the human prostate. Mol Pharmacol. 1994;45(2):306-311.
Kobayashi S, Tang R, et al. Localization of endothelin receptors in the human prostate. J Urol. 1994;151(3):763-766.
Konig JE, Senge T, et al. Analysis of the inflammatory network in benign prostate hyperplasia and prostate cancer. Prostate. 2004;58(2):121-129.
Konishi N, Hiasa Y, et al. Genetic variations in human benign prostatic hyperplasia detected by restriction landmark genomic scanning. J Urol. 1997;157(4):1499-1503.
Konno-Takahashi N, Takeuchi T, et al. Engineered IGF-I expression induces glandular enlargement in the murine prostate. J Endocrinol. 2003;177(3):389-398.
Konno-Takahashi N, Takeuchi T, et al. Engineered FGF-2 expression induces glandular epithelial hyperplasia in the murine prostatic dorsal lobe. Eur Urol. 2004;46(1):126-132.
Kramer G, Mitteregger D, et al. Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol. 2007;51(5):1202-1216.
Kramer G, Steiner GE, et al. Increased expression of lymphocyte-derived cytokines in benign hyperplastic prostate tissue, identification of the producing cell types, and effect of differentially expressed cytokines on stromal cell proliferation. Prostate. 2002;52(1):43-58.
Krege JH, Hodgin JB, et al. Generation and reproductive phenotypes of mice lacking estrogen receptor beta. Proc Natl Acad Sci U S A. 1998;95(26):15677-15682.
Kristal AR, Arnold KB, et al. Dietary patterns, supplement use, and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. Am J Epidemiol. 2008;167(8):925-934.
Kundu SD, Kim IY, et al. Absence of proximal duct apoptosis in the ventral prostate of transgenic mice carrying the c3 (1)-TGF-beta type II dominant negative receptor. Prostate. 2008;43(2):118-124.
Kuo HC. Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology. 1999;54(1):90-96.
Kupeli B, Soygur T, et al. The role of cigarette smoking in prostatic enlargement. Br J Urol. 1997;80(2):201-204.
Kyprianou N, Isaacs JT. Expression of transforming growth factor-beta in the rat ventral prostate during castration-induced programmed cell death. Mol Endocrinol. 1989;3:1515-1522.
Kyprianou N, Tu H, et al. Apoptotic versus proliferative activities in human benign prostatic hyperplasia. Hum Pathol. 1996;27(7):668-675.
Lee AJ, Russell EB, et al. Three-year follow-up of a community-based cohort of men with untreated benign prostatic hyperplasia. Eur Urol. 1996;30(1):11-17.
Lee C. Physiology of castration-induced regression in rat prostate. In: The prostatic cell: structure and function. New York: Alan R. Liss; 1981:145-159.
Lee C, et al. Prostatic ductal system in rats: regional variation in morphological and functional activities. Biol Reprod. 1990;43:1079-1086.
Lee KL, Peehl DM. Molecular and cellular pathogenesis of benign prostatic hyperplasia. J Urol. 2004;172(5 Pt. 1):1784-1791.
Lepor H, Sunaryadi I, et al. Quantitative morphometry of the adult human bladder. J Urol. 1992;148(2 Pt. 1):414-417.
Lepor H, Sypherd D, et al. Randomized double-blind study comparing the effectiveness of balloon dilation of the prostate and cystoscopy for the treatment of symptomatic benign prostatic hyperplasia. J Urol. 1992;147(3):639-642. discussion 642–4
Lepor H, Tang R, et al. Alpha1 adrenoceptor subtypes in the human prostate. J Urol. 1993;149:640-642.
Lepor H, Tang R, Meretyk S, Shapiro E. The alpha-adrenoceptor subtype mediating the tension of human prostatic smooth muscle. Prostate. 1993;22:301-307.
Levin RM, et al. Genetic and cellular characteristics of bladder outlet obstruction. Urol Clin North Am. 1995;22:262-283.
Levin RM, Haugaard N, et al. Obstructive response of human bladder to BPH vs. rabbit bladder response to partial outlet obstruction: a direct comparison. Neurourol Urodyn. 2000;19(5):609-629.
Levin RM, Longhurst PA, et al. Effect of bladder outlet obstruction on the morphology, physiology, and pharmacology of the bladder. Prostate [Suppl]. 1990;3:9-26.
Li Z, Habuchi T, et al. Increased risk of prostate cancer and benign prostatic hyperplasia associated with transforming growth factor-beta 1 gene polymorphism at codon 10. Carcinogenesis. 2004;25(2):237-240.
Lin VK, McConnell JD. Effects of obstruction on bladder contractile proteins [review]. Prog Clin Biol Res. 1994;386:263-269.
Lin VK, Wang D, et al. Myosin heavy chain gene expression in normal and hyperplastic human prostate tissue. Prostate. 2000;44(3):193-203.
Lin VK, Wang SY, et al. Alpha (2) macroglobulin, a PSA binding protein, is expressed in human prostate stroma. Prostate. 2005;63(3):299-308.
Lu-Yao GL, Barry MJ, et al. Transurethral resection of the prostate among Medicare beneficiaries in the United States: time trends and outcomes. Prostate Patient Outcomes Research Team (PORT). Urology. 1994;44(5):692-698. discussion 698–9
Lu W, Luo Y, et al. Fibroblast growth factor-10: a second candidate stromal to epithelial cell andromedin in prostate [published erratum appears in J Biol Chem 1999;274(39):28058]. J Biol Chem. 1999;274(18):12827-12834.
Lukacs B, Leplege A, et al. Construction and validation of a BPH specific health related quality of life scale including evaluation of sexuality. J Urol. 1995;153:320A.
Lytton B, Emery JM, et al. The incidence of benign prostatic obstruction. J Urol. 1968;99:639-645.
Mannikarottu AS, Changolkar AK, et al. Over expression of smooth muscle thin filament associated proteins in the bladder wall of diabetics. J Urol. 2005;174(1):360-364.
Mannikarottu AS, Disanto ME, et al. Altered expression of thin filament-associated proteins in hypertrophied urinary bladder smooth muscle. Neurourol Urodyn. 2006;25(1):78-88.
Mannikarottu AS, Hypolite JA, et al. Regional alterations in the expression of smooth muscle myosin isoforms in response to partial bladder outlet obstruction. J Urol. 2005;173(1):302-308.
Marberger M, Roehrborn CG, et al. Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. J Clin Endocrinol Metab. 2006;91(4):1323-1328.
Marberger MJ, Andersen JT, et al. Prostate volume and serum prostate-specific antigen as predictors of acute urinary retention: combined experience from three large multinational placebo-controlled trials. Eur Urol. 2000;38(5):563-568.
Marcelli M, Cunningham GR. Hormonal signaling in prostatic hyperplasia and neoplasia [review]. J Clin Endocrinol Metab. 1999;84(10):3463-3468.
Martikainen P, et al. Effect of transforming growth factor-beta on proliferation and death of rat prostatic cells. Endocrinology. 1990;127:2963-2968.
Matsui H, et al. Modulation of adrenergic receptors during regression of cardiac hypertrophy. J Hyper. 1994;12:1353-1357.
McConnell JD. The pathophysiology of benign prostatic hyperplasia. J Androl. 1991;12:356-363.
McConnell JD. Prostatic growth: new insights into hormonal regulation [review]. Br J Urol. 1995;76(Suppl. 1):5-10.
McConnell JD, Barry MJ, et al. Benign prostatic hyperplasia: diagnosis and treatment. Clinical practice guideline no. 8. Rockville, MD: U.S. Department of Health and Human Services, Agency for Health Care Policy and Research, Public Health Service; 1994. p. 1–17
McConnell JD, Bruskewitz R, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride Long-Term Efficacy and Safety Study Group. N Engl J Med. 1998;338(9):557-563.
McConnell JD, Roehrborn C, et al. The long-term effects of doxazosin, finasteride and the combination on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349(25):2385-2396.
McKeehan WL, Adams PS, et al. Direct mitogenic effects of insulin, epidermal growth factor, glucocorticoid, cholera toxin, unknown pituitary factors and possibly prolactin, but not androgen, on normal rat prostate epithelial cells in serum-free, primary cell culture. Cancer Res. 1984;44:1998.
McKeehan WL, Adams PS. Heparin-binding growth factor/prostatropin attenuates inhibition of rat prostate tumor epithelial cell growth by transforming growth factor type beta. In Vitro Cell Dev Biol. 1988;24(3):243-246.
McNeal JE. Origin and evolution of benign prostatic enlargement. Invest Urol. 1978;15:340.
McNeal JE. Pathology of benign prostatic hyperplasia: insight into etiology [review]. Urol Clin North Am. 1990;17:477-486.
McVary KT. Erectile dysfunction and lower urinary tract symptoms secondary to BPH. Eur Urol. 2005;47(6):838-845.
McVary KT, Monnig W, et al. Sildenafil citrate improves erectile function and urinary symptoms in men with erectile dysfunction and lower urinary tract symptoms associated with benign prostatic hyperplasia: a randomized, double-blind trial. J Urol. 2007;177(3):1071-1077.
McVary KT, Rademaker A, et al. Autonomic nervous system overactivity in men with lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2005;174(4 Pt. 1):1327-1433.
McVary KT, Razzaq A, et al. Growth of the prostate gland is facilitated by the autonomic system. Biol Reprod. 1994;51:99-107.
Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications: a cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243-247.
Meigs JB, Barry MJ, et al. Incidence rates and risk factors for acute urinary retention: the health professionals followup study. J Urol. 1999;162(2):376-382.
Meigs JB, Mohr B, et al. Risk factors for clinical benign prostatic hyperplasia in a community-based population of healthy aging men. J Clin Epidemiol. 2001;54(9):935-944.
Meikle AW, Bansal A, et al. Heritability of the symptoms of benign prostatic hyperplasia and the roles of age and zonal prostate volumes in twins. Urology. 1999;53(4):701-706.
Meikle AW, Stephenson RA, et al. Age, genetic, and nongenetic factors influencing variation in serum sex steroids and zonal volumes of the prostate and benign prostatic hyperplasia in twins. Prostate. 1997;33(2):105-111.
Melchior J, Valk WL, et al. Transurethral prostatectomy in the azotemic patient. J Urol. 1974;112:643-647.
Melchior J, Valk WL, et al. Transurethral prostatectomy: computerized analysis of 2,223 consecutive cases. J Urol. 1974;112:634.
Minnery CH, Getzenberg RH. Benign prostatic hyperplasia cell line viability and modulation of jm-27 by doxazosin and ibuprofen. J Urol. 2005;174(1):375-379.
Mononen N, Ikonen T, et al. Androgen receptor CAG polymorphism and prostate cancer risk. Hum Genet. 2002;111(2):166-171.
Monti S, Di Silverio F, et al. Regional variations of insulin-like growth factor I (IGF-I), IGF-II, and receptor type I in benign prostatic hyperplasia tissue and their correlation with intraprostatic androgens. J Clin Endocrinol Metab. 2001;86(4):1700-1706.
Montpetit ML, et al. Androgen repressed messages in the rat ventral prostate. Prostate. 1986;8:25-26.
Moon H, Moon W, et al. High prevalence of prostatism and benign prostatic hyperplasia in Korean men. J Urol. 1995;155(Suppl.):631A.
Moon TD, Brannan W, et al. Effect of age, educational status, ethnicity and geographic location on prostate symptom scores. J Urol. 1994;152(5):1498-1500.
Moore R. Benign hypertrophy of the prostate. J Urol. 1943;50:689-690.
Moore RJ, et al. Concentration of dihydrotestosterone and 3beta-androstanediol in naturally occurring and androgen induced prostatic hyperplasia in the dog. J Clin Invest. 1979;64:1003.
Mora GR, Olivier KR, et al. Regulation of expression of the early growth response gene-1 (EGR-1) in malignant and benign cells of the prostate. Prostate. 2005;63(2):198-207.
Morote J, Encabo G, et al. Prediction of prostate volume based on total and free serum prostate-specific antigen: is it reliable? Eur Urol. 2000;38(1):91-95.
Morrison AS. Prostatic hypertrophy in greater Boston. J Chron Dis. 1978;31(5):357-362.
Morrison AS. Risk factors for surgery for prostatic hypertrophy. Am J Epidemiol. 1992;135(9):974-980.
Mukamel E, et al. Occult progressive renal damage in the elderly male due to benign prostatic hyperplasia. J Am Geriatr Soc. 1979;27:403-406.
Nacey JN, Morum P, et al. Analysis of the prevalence of voiding symptoms in Maori, Pacific Island, and Caucasian New Zealand men. Urology. 1995;46(4):506-511.
Nakano K, Fukabori Y, et al. Androgen-stimulated human prostate epithelial growth mediated by stromal-derived fibroblast growth factor-10. Endocrine J. 1999;46(3):405-413.
Naslund JF, Coffey DS. The differential effects of neonatal androgen, estrogen, and progesterone on adult prostate growth. J Urol. 1986;136:1136-1140.
Nielsen KK, Nordling J, et al. Critical review of the diagnosis of prostatic obstruction [review]. Neurourol Urodyn. 1994;13(3):201-217.
Nordling J. The aging bladder—a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol. 2002;37(8–9):991-999.
Norman RW, Nickel JC, et al. “Prostate-related symptoms” in Canadian men 50 years of age or older: prevalence and relationships among symptoms. Br J Urol. 1994;74(5):542-550.
O’Leary MP, Barry MJ, et al. Hard measures of subjective outcomes: validating symptom indexes in urology. J Urol. 1992;148(5):1546-1548. discussion 1564
O’Leary MP, Fowler FJ, et al. A brief male sexual function inventory. Urology. 1995;46:697-706.
Oesterling JE, Jacobsen SJ, et al. Serum prostate-specific antigen in a community-based population of healthy men: establishment of age-specific reference ranges [see comments]. JAMA. 1993;270(7):860-864.
Ogden CW, Reddy P, et al. Sham versus TUMT: a randomized study with cross over. J Urol. 1993;149:250A.
Ogden CW, Reddy P, et al. Sham versus transurethral microwave thermotherapy in patients with symptoms of benign prostatic bladder outflow obstruction. Lancet. 1993;341(8836):14-17.
Oishi K, Boyle P, et al. Epidemiology and natural history of benign prostatic hyperplasia. In: 4th International consultation on benign prostatic hyperplasia. Plymouth (UK): Plymbridge Distributors Ltd.; 1989:23-59.
Orlandi A, Ropraz P, Gabbiani G. Proliferative activity and alpha-smooth muscle actin expression in cultured rat aortic smooth muscle cells are differently modulated by transforming growth factor beta-1 and heparin. Exp Cell Res. 1994;214:528-536.
Overland G, Vatten L, et al. Lower urinary tract symptoms, prostate volume and uroflow in Norwegian community men. Eur Urol. 2001;39(1):36-41.
Padley R, Olson P, et al. Education and socio-economic status influence patterns of response to therapy with the alpha adrenergic receptor blocker terazosin and placebo in men with clinical benign prostatic hyperplasia (BPH). J Urol. 1997;157:312A.
Parsons JK. Modifiable risk factors for benign prostatic hyperplasia and lower urinary tract symptoms: new approaches to old problems. J Urol. 2007;178(2):395-401.
Parsons JK, Bergstrom J, et al. Lipids, lipoproteins and the risk of benign prostatic hyperplasia in community-dwelling men. BJU Int. 2008;101(3):313-318.
Parsons JK, Carter HB, et al. Metabolic factors associated with benign prostatic hyperplasia. J Clin Endocrinol Metab. 2006;91(7):2562-2568.
Parsons JK, Kashefi C. Physical activity, benign prostatic hyperplasia, and lower urinary tract symptoms. Eur Urol. 2008;53(6):1228-1235.
Partin AW, Getzenberg RH, et al. Nuclear matrix protein patterns in human benign prostatic hyperplasia and prostate cancer. Cancer Res. 1993;53(4):744-746.
Partin AW, Oesterling JE, et al. Influence of age and endocrine factors on the volume of benign prostatic hyperplasia. J Urol. 1991;145(2):405-409.
Partin AW, Page WF, et al. Concordance rates for benign prostatic disease among twins suggest hereditary influence. Urology. 1994;44(5):646-650.
Pearson JD, Lei HH, et al. Familial aggregation of bothersome benign prostatic hyperplasia symptoms. Urology. 2003;61(4):781-785.
Peehl DM, Cohen P, et al. The insulin-like growth factor system in the prostate [review]. World J Urol. 1995;13(5):306-311.
Peehl DM, Sellers RG. Basic FGF, EGF, and PDGF modify TGFbeta-induction of smooth muscle cell phenotype in human prostatic stromal cells. Prostate. 1998;35(2):125-134.
Peters CA, Walsh PC. The effect of nafarelin acetate, a luteinizing-hormone-releasing hormone agonist, on benign prostatic hyperplasia. N Engl J Med. 1987;317(10):599-604.
Pinsky PF, Kramer BS, et al. Prostate volume and prostate-specific antigen levels in men enrolled in a large screening trial. Urology. 2006;68(2):352-356.
Polnaszek N, Kwabi-Addo B, et al. FGF17 is an autocrine prostatic epithelial growth factor and is upregulated in benign prostatic hyperplasia. Prostate. 2004;60(1):18-24.
Powell PH, Smith PJ, et al. The identification of patients at risk from acute retention. Br J Urol. 1980;52(6):520-522.
Pradhan BK, Chandra K. Morphogenesis of nodular hyperplasia—prostate. J Urol. 1975;113(2):210-213.
Prakash K, Pirozzi G, et al. Symptomatic and asymptomatic benign prostatic hyperplasia: molecular differentiation by using microarrays. Proc Natl Acad Sci U S A. 2002;99(11):7598-7603.
Pressler L, Santarosa R, et al. The incidence of hypertension (HTN) in a population of men with benign prostatic hyperplasia (BPH): analysis based on the AUA symptom score and race. J Urol. 1997;157:371A.
Price DT, Schwinn DA, et al. Identification, quantification, and localization of mRNA for three distinct alpha 1 adrenergic receptor subtypes in human prostate. J Urol. 1993;150(2):546-551.
Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008;73(3):233-244.
Prins GS, Marmer M, et al. Estrogen receptor-beta messenger ribonucleic acid ontogeny in the prostate of normal and neonatally estrogenized rats. Endocrinology. 1998;139(3):874-883.
Randall A. Surgical pathology of prostatic obstruction. Baltimore: Williams and Wilkins; 1931.
Rennie PS, Bruchovsky N, et al. Relationship of androgen receptors to the growth and regression of the prostate. Am J Clin Oncol. 1988;11(Suppl. 2):S13-S17.
Reynard JM, Lim C, et al. The significance of terminal dribbling in men with lower urinary tract symptoms. Br J Urol. 1996;77(5):705-710.
Rhodes T, Girman CJ, et al. Longitudinal measures of prostate volume in a community-based sample: 3.5 year followup in the Olmsted County Study of Urinary Symptoms and Health Status Among Men. J Urol. 1995;153:301A.
Rhodes T, Girman CJ, et al. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999;161(4):1174-1179.
Rhodes T, Girman CJ, et al. Longitudinal prostate volume in a community-based sample: 7-year followup in the Olmsted County Study of Urinary Symptoms and Health Status among Men. J Urol. 2000;163(4):249.
Roberts AB, Sporn MB. Physiological actions and clinical applications of transforming growth factor-beta (TGF-beta). Growth Factors. 1993;8:1-9.
Roberts RO, Bergstralh EJ, et al. Polymorphisms in the 5alpha reductase type 2 gene and urologic measures of BPH. Prostate. 2005;62(4):380-387.
Roberts RO, Jacobsen SJ, et al. Cigarette smoking and prostatism: a biphasic association? Urology. 1994;43(6):797-801.
Roberts RO, Jacobsen SJ, et al. Urinary incontinence in a community-based cohort: prevalence and healthcare-seeking. J Am Geriatr Soc. 1998;46(4):467-472.
Roberts RO, Jacobsen SJ, et al. Longitudinal changes in peak urinary flow rates in a community based cohort. J Urol. 2000;163(1):107-113.
Roberts RO, Jacobson DJ, et al. Insulin-like growth factor I, insulin-like growth factor binding protein 3, and urologic measures of benign prostatic hyperplasia. Am J Epidemiol. 2003;157(9):784-791.
Roberts RO, Jacobson DJ, et al. Serum sex hormones and measures of benign prostatic hyperplasia. Prostate. 2004;61(2):124-131.
Roberts RO, Rhodes T, et al. Natural history of prostatism: worry and embarrassment from urinary symptoms and health care-seeking behavior. Urology. 1994;43(5):621-628.
Roberts RO, Rhodes T, et al. Association between family history of benign prostatic hyperplasia and urinary symptoms: results of a population-based study. Am J Epidemiol. 1995;142(9):965-973.
Roberts RO, Rhodes T, et al. The decision to seek care: factors associated with the propensity to seek care in a community-based cohort of men. Arch Fam Med. 1997;6(3):218-222.
Roberts RO, Tsukamoto T, et al. Association between cigarette smoking and prostatism in a Japanese community. Prostate. 1997;30(3):154-159.
Robson MC. Cirrhosis and prostatic neoplasms. Geriatrics. 1966;21(12):150-154.
Roehrborn CG. Pathology of benign prostatic hyperplasia. Int J Impot Res. 2008;20(Suppl. 3):S11-S18.
Roehrborn CG, Boyle P, et al. Serum prostate-specific antigen and prostate volume predict long-term changes in symptoms and flow rate: results of a four-year, randomized trial comparing finasteride versus placebo. PLESS Study Group. Urology. 1999;54(4):662-669.
Roehrborn CG, Boyle P, et al. Serum prostate-specific antigen as a predictor of prostate volume in men with benign prostatic hyperplasia. Urology. 1999;53(3):581-589.
Roehrborn CG, Boyle P, et al. Serum prostate specific antigen (PSA) is a reliable surrogate for prostate volume. Urology. 1999;53:581-589.
Roehrborn CG, Boyle P, et al. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60(3):434-441.
Roehrborn CG, Bruskewitz R, et al. Urinary retention in patients with BPH treated with finasteride or placebo over 4 years: characterization of patients and ultimate outcomes. The PLESS Study Group. Eur Urol. 2000;37(5):528-536.
Roehrborn CG, Fuh V, et al. The relationship between total and free PSA, prostate volume and age in men age 40–60 with no clinical diagnosis of benign prostatic hyperplasia necessitating therapy. J Urol. 2000;163(Suppl.):252A.
Roehrborn CG, Girman CJ, et al. Correlation between prostate size estimated by digital rectal examination and measured by transrectal ultrasound. Urology. 1997;49(4):548-557.
Roehrborn CG, Lange JL, et al. Changes in amount and intracellular distribution of androgen receptor in human foreskin as a function of age. J Clin Invest. 1987;79(1):44-47.
Roehrborn CG, Malice M, et al. Clinical predictors of spontaneous acute urinary retention in men with LUTS and clinical BPH: a comprehensive analysis of the pooled placebo groups of several large clinical trials. Urology. 2001;58(2):210-216.
Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology. 1999;53(3):473-480.
Roehrborn CG, McVary KT, et al. Tadalafil administered once daily for lower urinary tract symptoms secondary to benign prostatic hyperplasia: a dose finding study. J Urol. 2008;180(4):1228-1234.
Roehrborn CG, Oesterling JE, et al. The Hytrin Community Assessment Trial study: a one-year study of terazosin versus placebo in the treatment of men with symptomatic benign prostatic hyperplasia. HYCAT Investigator Group. Urology. 1996;47(2):159-168.
Roehrborn CG, Schwinn DA. Alpha1-adrenergic receptors and their inhibitors in lower urinary tract symptoms and benign prostatic hyperplasia. J Urol. 2004;171(3):1029-1035.
Rohrmann S, Smit E, et al. Association between markers of the metabolic syndrome and lower urinary tract symptoms in the Third National Health and Nutrition Examination Survey (NHANES III). Int J Obes (Lond). 2005;29(3):310-316.
Ropiquet F, Giri D, et al. FGF7 and FGF2 are increased in benign prostatic hyperplasia and are associated with increased proliferation. J Urol. 1999;162(2):595-599.
Rosen R, Altwein J, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol. 2003;44(6):637-649.
Rosen RC, Coyne KS, et al. Beyond the cluster: methodological and clinical implications in the Boston Area Community Health survey and EPIC studies. BJU Int. 2008;101(10):1274-1278.
Rule AD, Jacobson DJ, et al. The association between benign prostatic hyperplasia and chronic kidney disease in community-dwelling men. Kidney Int. 2005;67(6):2376-2382.
Russell DW, Wilson JD. Steroid 5alpha-reductase: two genes/two enzymes. Annu Rev Biochem. 1994;63:25.
Sagnier PP, Girman CJ, et al. International comparison of the community prevalence of symptoms of prostatism in four countries. Eur Urol. 1996;29(1):15-20.
Sakamoto S, Yokoyama M, et al. Development of quantitative detection assays for CYR61 as a new marker for benign prostatic hyperplasia. J Biomol Screen. 2003;8(6):701-711.
Sakamoto S, Yokoyama M, et al. Induction and function of CYR61 (CCN1) in prostatic stromal and epithelial cells: CYR61 is required for prostatic cell proliferation. Prostate. 2004;61(4):305-317.
Sakamoto S, Yokoyama M, et al. Increased expression of CYR61, an extracellular matrix signaling protein, in human benign prostatic hyperplasia and its regulation by lysophosphatidic acid. Endocrinology. 2004;145(6):2929-2940.
Salam MT, Ursin G, et al. Associations between polymorphisms in the steroid 5-alpha reductase type II (SRD5A2) gene and benign prostatic hyperplasia and prostate cancer. Urol Oncol. 2005;23(4):246-253.
Salm SN, Koikawa Y, et al. Transforming growth factor-beta is an autocrine mitogen for a novel androgen-responsive murine prostatic smooth muscle cell line, psmc1. J Cell Physiol. 2000;185(3):416-424.
Sanda MG, Beaty TH, et al. Genetic susceptibility of benign prostatic hyperplasia. J Urol. 1994;152(1):115-119.
Sanda MG, Doehring CB, et al. Clinical and biological characterization of familial benign prostatic hyperplasia. J Urol. 1997;157(3):876-879.
Sarma AV, Wei JT, et al. Comparison of lower urinary tract symptom severity and associated bother between community-dwelling black and white men: the Olmsted County Study of Urinary Symptoms and Health Status and the Flint Men’s Health Study. Urology. 2003;61(6):1086-1091.
Sciarra F, Toscano V. Role of estrogens in human benign prostatic hyperplasia [review]. Arch Androl. 2000;44(3):213-220.
Scott R, McIlhaney JS. Voiding rates in normal adults. J Urol. 1961;85:980-982.
Sech SM, Montoya JD, et al. The so-called “placebo effect” in benign prostatic hyperplasia treatment trials represents partially a conditional regression to the mean induced by censoring. Urology. 1998;51(2):242-250.
Sech S, Montoya J, et al. Interexaminer reliability of transrectal ultrasound for estimating prostate volume. J Urol. 2001;166(1):125-129.
Seitter WR, Barrett-Connor E. Cigarette smoking, obesity, and benign prostatic hypertrophy: a prospective population-based study. Am J Epidemiol. 1992;135(5):500-503.
Shah US, Arlotti J, et al. Androgen regulation of JM-27 is associated with the diseased prostate. J Androl. 2004;25(4):618-624.
Shapiro E, Becich MJ, et al. The relative proportion of stromal and epithelial hyperplasia is related to the development of symptomatic benign prostate hyperplasia. J Urol. 1992;147:1293-1297.
Sherwood JB, McConnell JD, et al. Heterogeneity of 5 alpha-reductase gene expression in benign prostatic hyperplasia. J Urol. 2003;169(2):575-579.
Shirakawa T, Okada H, et al. Messenger RNA levels and enzyme activities of 5 alpha-reductase types 1 and 2 in human benign prostatic hyperplasia (BPH) tissue. Prostate. 2004;58(1):33-40.
Sidney S. Vasectomy and the risk of prostatic cancer and benign prostatic hypertrophy. J Urol. 1987;138(4):795-797.
Sidney S, Quesenberry CJr, et al. Incidence of surgically treated benign prostatic hypertrophy and of prostate cancer among black and white multiphasic examinees in a prepaid health care plan. Am J Epidemiol. 1991;134:825.
Sidney S, Quesenberry CJr, et al. Risk factors for surgically treated benign prostatic hyperplasia in a prepaid health care plan. Urology. 1991;38(1 Suppl.):13-19.
Silver RI, Wiley EL, et al. Expression and regulation of steroid 5 alpha-reductase 2 in prostate disease. J Urol. 1994;152(2):433-437.
Siroky MB, Olsson CA, et al. The flow rate nomogram: I. development. J Urol. 1979;122:665-668.
Siroky MB, Olsson CA, et al. The flow rate nomogram: II. clinical correlation. J Urol. 1980;123:208-210.
Smith P, Rhodes NP, et al. Modulating effect of estrogen and testosterone on prostatic stromal cell phenotype differentiation induced by noradrenaline and doxazosin. Prostate. 2000;44(2):111-117.
Smith P, Rhodes NP, et al. Upregulation of estrogen and androgen receptors modulate expression of FGF-2 and FGF-7 in human, cultured, prostatic stromal cells exposed to high concentrations of estradiol. Prostate Cancer Prostatic Dis. 2002;5(2):105-110.
Soygur T, Kupeli B, et al. Effect of obesity on prostatic hyperplasia: its relation to sex steroid levels. Int Urol Nephrol. 1996;28(1):55-59.
Spiro LH, Labay G, et al. Prostatic infarction: role in acute urinary retention. Urology. 1976;3(3):345-347.
Sporn MB, Roberts AB. TGF-beta: problems and prospects. Cell Regul. 1990;5:3-7.
Sporn MB, Roberts AB. Interactions of retinoids and transforming growth factor-beta in regulation of cell differentiation and proliferation. Mol Endocrinol. 1991;5:3-7.
Srinivasan D, Kosaka AH, et al. Pharmacological and functional characterization of bradykinin B2 receptor in human prostate. Eur J Pharmacol. 2004;504(3):155-167.
Steele GS, Sullivan MP, et al. Combination of symptom score, flow rate and prostate volume for predicting bladder outflow obstruction in men with lower urinary tract symptoms. J Urol. 2000;164(2):344-348.
Steers WD, Ciambotti J, Erdman S, de Groat WC. Morphological plasticity in efferent pathways to the urinary bladder of the rat following urethral obstruction. J Neurosci. 1990;19:1943.
Steers WD, Clemow DB, et al. The spontaneously hypertensive rat: insight into the pathogenesis of irritative symptoms in benign prostatic hyperplasia and young anxious males [review]. Exp Physiol. 1999;84(1):137-147.
Steiner GE, Newman ME, et al. Expression and function of pro-inflammatory interleukin IL-17 and IL-17 receptor in normal, benign hyperplastic, and malignant prostate. Prostate. 2003;56(3):171-182.
Steiner GE, Stix U, et al. Cytokine expression pattern in benign prostatic hyperplasia infiltrating T cells and impact of lymphocytic infiltration on cytokine mRNA profile in prostatic tissue. Lab Invest. 2003;83(8):1131-1146.
Steiner MS. Review of peptide growth factors in benign prostatic hyperplasia and urological malignancy [review]. J Urol. 1995;153(4):1085-1096.
Stief CG, Porst H, et al. A randomised, placebo-controlled study to assess the efficacy of twice-daily vardenafil in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Eur Urol. 2008;53(6):1236-1244.
Stimson JB, Fihn SD. Benign prostatic hyperplasia and its treatment [review]. J Gen Intern Med. 1990;5(2):153-165.
Story MT, Hopp KA, et al. Influence of transforming growth factor beta 1 and other growth factors on basic fibroblast growth factor level and proliferation of cultured human prostate-derived fibroblasts. Prostate. 1993;22(3):183-197.
Story MT, Livingston B, et al. Cultured human prostate-derived fibroblasts produce a factor that stimulates their growth with properties indistinguishable from basic fibroblast growth factor. Prostate. 1989;15(4):355-365.
Stumpf H, Wilens S. Inhibitory effects of portal cirrhosis of the liver on prostatic enlargement. Arch Intern Med. 1953;91:304.
Su L, Guess HA, et al. Adverse effects of medications on urinary symptoms and flow rate: a community-based study. J Clin Epidemiol. 1996;49:483-487.
Susset JG, Picker P, et al. Critical evaluation of uroflowmeters and analysis of normal curves. J Urol. 1973;109:874-878.
Sutkowski DM, et al. Effect of spermatocele fluid on growth of human prostatic cells in culture. J Androl. 1993;14:233.
Swyer G. Postnatal growth changes in the human prostate. J Anat. 1944;78:130-136.
Takane KK, Husmann DA, et al. Androgen receptor levels in the rat penis are controlled differently in distinctive cell types. Endocrinology. 1991;128:2234-2238.
Takane KK, Wilson JD, et al. Decreased levels of the androgen receptor in the mature rat phallus are associated with decreased levels of androgen receptor mRNA. Endocrinology. 1991;129:1093-1100.
Taoka R, Tsukuda F, et al. Association of prostatic inflammation with down-regulation of macrophage inhibitory cytokine-1 gene in symptomatic benign prostatic hyperplasia. J Urol. 2004;171(6 Pt. 1):2330-2335.
Tarcan T, Azadzoi KM, et al. Age-related erectile and voiding dysfunction: the role of arterial insufficiency. Br J Urol. 1998;82(Suppl. 1):26-33.
Tay KP, Chin CM, et al. Prostate screening—the Singapore experience. Int J Urol. 1996;3(2):102-107.
Tenniswood M. Role of epithelial-stromal interactions in the control of gene expression in the prostate: an hypothesis. Lab Invest. 1992;66:96-107.
Theyer G, Kramer G, et al. Phenotypic characterization of infiltrating leukocytes in benign prostatic hyperplasia. Lab Invest. 1992;66(1):96-107.
Thigpen AE, Silver RI, et al. Tissue distribution and ontogeny of steroid 5 alpha-reductase isozyme expression. J Clin Invest. 1993;92(2):903-910.
Thomas LN, Douglas RC, et al. 5alpha-Reductase type 1 immunostaining is enhanced in some prostate cancers compared with benign prostatic hyperplasia epithelium. J Urol. 2003;170(5):2019-2025.
Thomas LN, Douglas RC, et al. Type 1 and type 2 5alpha-reductase expression in the development and progression of prostate cancer. Eur Urol. 2008;53(2):244-252.
Torp-Pedersen S, Juul N, et al. Transrectal prostatic ultrasonography: equipment, normal findings, benign hyperplasia and cancer. Scand J Urol Nephrol (Suppl). 1988;107:19-25.
Tsang KK, Garraway WM. Impact of benign prostatic hyperplasia on general well-being of men. Prostate. 1993;23(1):1-7.
Tsukamoto T, Kumamoto Y, et al. Prevalence of prostatism in Japanese men in a community-based study with comparison to a similar American study [see comments]. J Urol. 1995;154(2 Pt. 1):391-395.
Tutrone RF, et al. Benign prostatic hyperplasia in a transgenic mouse: a new hormonally sensitive investgatory model. J Urol. 1993;149:633-639.
Uckert S, Kuthe A, et al. Phosphodiesterase isoenzymes as pharmacological targets in the treatment of male erectile dysfunction. World J Urol. 2001;19(1):14-22.
Uckert S, Sigl K, et al. [Significance of phosphodiesterase isoenzymes in the control of human detrusor smooth muscle function: an immunohistochemical and functional study]. Urologe A. 2009;48(7):764-769. [in German]
Uckert S, Sormes M, et al. Effects of phosphodiesterase inhibitors on tension induced by norepinephrine and accumulation of cyclic nucleotides in isolated human prostatic tissue. Urology. 2008;71(3):526-530.
Untergasser G, Madersbacher S, et al. Benign prostatic hyperplasia: age-related tissue-remodeling. Exp Gerontol. 2005;40(3):121-128.
Verhamme KM, Dieleman JP, et al. Low incidence of acute urinary retention in the general male population: the triumph project. Eur Urol. 2005;47(4):494-498.
Von Garrelts B. Analysis of micturition: a new method of recording the voiding of the bladder. Acta Chir Scand. 1956;112:326-340.
Von Garrelts B. Micturition in the normal male. Acta Chir Scand. 1957;114:197-210.
Von Garrelts B. Micturition in disorders of the prostate and posterior urethra. Acta Chir Scand. 1958;115:227-241.
Walden PD, Ittmann M, et al. Endothelin-1 production and agonist activities in cultured prostate-derived cells: implications for regulation of endothelin bioactivity and bioavailability in prostatic hyperplasia. Prostate. 1998;34(4):241-250.
Walden PD, Lefkowitz GK, et al. Mitogenic activation of human prostate-derived fibromuscular stromal cells by bradykinin. Br J Pharmacol. 1999;127(1):220-226.
Walsh K, Sriprasad S, et al. Distribution of vascular endothelial growth factor (VEGF) in prostate disease. Prostate Cancer Prostatic Dis. 2002;5(2):119-122.
Walsh PC, Hutchins GM, Ewing LL. Tissue content of dihydrotestosterone in human prostatic hyperplasia is not supernormal. J Clin Invest. 1983;72:1772-1777.
Walsh PC, Wilson JD. The induction of prostatic hypertrophy in the dog with androstanediol. J Clin Invest. 1976;57:1093.
Wang W, Bergh A, et al. Chronic inflammation in benign prostate hyperplasia is associated with focal upregulation of cyclooxygenase-2, Bcl-2, and cell proliferation in the glandular epithelium. Prostate. 2004;61(1):60-72.
Wang Z, Tufts R, et al. Genes regulated by androgen in the rat ventral prostate. Proc Natl Acad Sci U S A. 1997;94(24):12999-13004.
Wasson JH, Bubolz TA, et al. Transurethral resection of the prostate among medicare beneficiaries: 1984 to 1997. For the Patient Outcomes Research Team for Prostatic Diseases. J Urol. 2000;164(4):1212-1215.
Wasson JH, Reda DJ, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995;332(2):75-79.
Wein AJ, Coyne KS, et al. The impact of lower urinary tract symptoms on male sexual health: EpiLUTS. BJU Int. 2009;103(Suppl. 3):33-41.
Wennberg JE, Mulley AGJr, et al. An assessment of prostatectomy for benign urinary tract obstruction: geographic variations and the evaluation of medical care outcomes. JAMA. 1988;259(20):3027-3030.
Wennbo H, Kindblom J, et al. Transgenic mice overexpressing the prolactin gene develop dramatic enlargement of the prostate gland. Endocrinology. 1997;138(10):4410-4415.
Werely CJ, Heyns CF, et al. DNA fingerprint detection of somatic mutations in benign prostatic hyperplasia and prostatic adenocarcinoma. Genes Chromosomes Cancer. 1996;17(1):31-36.
White JJ, et al. DNA alterations in prostatic adenocarcinoma and benign prostatic hyperplasia: detection by DNA fingerprint analysis. Mutat Res. 1990;237:37.
Wilding G, Zugmeier G, et al. Differential effects of transforming growth factor beta on human prostate cancer cells in vitro. Mol Cell Endocrinol. 1989;62(1):79-87.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA. 1995;273(1):59-65.
Witjes WP, Aarnink RG, et al. The correlation between prostate volume, transition zone volume, transition zone index and clinical and urodynamic investigations in patients with lower urinary tract symptoms. Br J Urol. 1997;80(1):84-90.
Wu S. Anatomic changes in the prostate of patients with cirrhosis of the liver. Arch Pathol. 1942;34:735.
Yalla SV, et al. Correlation of American Urological Association Symptom Index with obstructive and nonobstructive prostatism. J Urol. 1995;153:674-680.
Yan G, et al. Heparin-binding keratinocyte growth factor is a candidate stromal to epithelial cell andromedin. Mol Endocrinol. 1992;6:2123.
Yang G, Timme TL, et al. Transforming growth factor beta 1 transduced mouse prostate reconstitutions: II. Induction of apoptosis by doxazosin. Prostate. 1997;33(3):157-163.
Zucchetto A, Tavani A, et al. History of weight and obesity through life and risk of benign prostatic hyperplasia. Int J Obes Relat Metab Disord. 2005;29(7):798-803.