Transurethral Vaporization of the Prostate
Whereas TURP removes tissue by resection of prostatic tissue and causes hemostasis by fulguration, transurethral vaporization of the prostate (TUVP) is brought about by combining the concepts of vaporization and desiccation. Desiccation is the drawing out of water from tissue, by drying out, rather than vaporizing the cells. This concept was introduced by Mebust and coworkers (1972, 1977) using a transurethral probe with direct-vision capabilities to heat and desiccate the prostate. TUVP was first described by Kaplan and Te (1995a, 1995b).
Mechanism of Action
With TUVP, two electrosurgical effects are combined: vaporization and desiccation. Vaporization steams tissue away using high heat, and coagulation uses lower heat to dry out tissue. Other factors are also involved that modify the delivery of electrical energy. These include the voltage production by the generator, the current density of the surface area of contact of the electrode, and the electrical resistance of the tissue being treated (Kaplan et al, 1998).
In the case of TUVP the electrode’s leading edge is the point at which maximal efficiency for vaporization occurs, as well as that of current density delivery. At the point of the trailing edge of the electrode there is a decrease in the delivery of current, lowering the power and permitting tissue desiccation to occur. Therefore vaporization occurs at the leading edge and desiccation occurs at the trailing edge (Kaplan et al, 1998).
The power of the generator determines whether vaporization occurs at the leading edge of the electrode. The electricity that is transmitted to the cell is converted to heat, resulting in the cell exploding or drying out. This is dependent on the conduction of electricity by the cell or the tissue resistance encountered by the current. In simple terms, the well-hydrated cell conducts electricity well, whereas the drier the tissue, the greater the electrical resistance. Clearly, a higher power is required to overcome this resistance, which may lead to poor vaporization if the power cannot be varied.
The type of generator used is also important in deciding the effectiveness of the vaporization. Older machines do not have a method of modulating delivery of power to the tissues depending on the degree of resistance encountered. Usually, therefore, the power is switched high to overcome this problem. The balance then is in some cases controlled by the limitation of the amount of current required to maintain a constant power. This safety feature prevents the delivery of an ever-increasing voltage that would compensate for the increase in resistance associated with the drying out of tissue that would occur with vaporization. This could potentially lead to unwanted damage both to the local tissues and to other areas such as the urethra. For this reason, modern generators specifically designed for TUVP can vary the delivery of power by reading tissue resistance. In addition, the safety feature described earlier whereby power can be limited is set at a higher level, thus making TUVP more efficient.
For TUVP, the cutting current power should be set to a maximum of 75% higher power than for a standard TURP, but the power used need not always be as high as this. In fact, it has been estimated that a minimal power delivery of 150 W is required for TUVP (van Swol et al, 1999).
Electrode Design
The rollerball, which is traditionally used for fulgurating the base of superficial bladder tumors, can be used for TUVP. However, it should not be used for prostates that are particularly large. In the study by Juma (1996), it was most effective in patients with glands whose mean volume as estimated by TRUS was 31.9 mL. The effectiveness in larger glands is probably limited by the shape of the rollerball, where the most satisfactory vaporization takes place at the middle part of the leading edge, assuming an equal distribution of contact pressure.
A grooved rollerbar has been widely used and consists of a bar that is 3 mm wide and 3 mm in diameter, which is composed of nickel-silver and insulated with Teflon (Vapor Trode, Circon-ACMI, Stamford, CT). The design is superior to the standard rollerball because the grooved design increases the number of leading edges at which electrovaporization takes place, and this allows increased efficiency of vaporization to a wide contact area and thus to a larger volume of tissue (Narayan et al, 1996; Reis et al, 1999). A similar grooved electrode has also been produced (Richard Wolf, Germany), known as the EVAP.
New second-generation vaporizing electrodes have been manufactured and evaluated. They have the aim of both vaporizing and resecting prostatic tissue simultaneously and have been termed vaporizing loops by some. The technique has been given several possible names in the literature, all amounting to the same thing: transurethral vaporization-resection of the prostate (TUVRP), thick-loop TURP, vapor-cut electrovaporization-resection (Cabelin et al, 2000).
Some examples of these are testament to the inventiveness of many of the instrument companies in relation to design. The Vapor Tome (Circon-ACMI, Stamford, CT) is a thick loop with grooves, giving a thin leading edge for vaporization and a thick trailing edge for desiccation. The Wedge (Microvasive, Natick, MA) is a smooth loop with the same edge configuration, made of stainless steel, tungsten, and chromium. The Wing EVAP (Richard Wolf, Germany) is a semicircular gold-plated wide loop that is wider and thicker than the standard TURP loop (Cabelin et al, 2000). Other modifications are under investigation, in which not only new electrodes but also specific electrosurgical generators are being developed, the aim of which is to reduce side effects while maintaining efficacy and also decreasing the potential risks of high-voltage power to the tissues surrounding the prostate.
Clinical Experience with Electrovaporization
The first report of TUVP was from Kaplan and Te (1995a), using the Vapor Trode. They reported on 25 men with moderate LUTS with a mean prostatic size of 57.6 mL. There was an improvement in AUASI from 17.8 to 4.2 at 3 months and in PFR from 7.4 to 17.3 mL/sec at the same time. The most encouraging findings were that all of the patients had their catheters removed within 24 hours (mean, 14.6), but by 3 months 1 patient had developed a distal urethral stricture. In the study by Juma (1996) using the standard rollerball in a study of 20 patients for 3 months, the results were similar, although 1 patient developed a bladder neck stenosis and 1 required repeated TURP.
Other pilot studies also suggested that a comparative trial would be appropriate because of the efficacy and safety that had been demonstrated. Galluci and his colleagues (1996) treated 35 patients with the Vapor Trode and found that improvements at 28 days were as encouraging as those at 3 months in other studies (PFR, 9.8 to 20.74 mL/sec; AUASI score, 18.2 to 10.4), but of note was that the standard deviation of the mean in both cases was very wide. Stewart and colleagues (1995) with the same electrode treated 34 patients, 20 of whom were in urinary retention; 33 of 34 were voiding satisfactorily. In a study of 22 patients subjected to pressure-flow analysis at 6 months, the mean Pdet at PFR decreased from 108 to 39 cm H2O (Okada et al, 1998). Similar results related to relief of obstruction in 91 patients were reported by Matos Ferreira and Varregoso (1997).
Comparative Studies
All of the pilot studies were short term, none longer than 6 months, but comparative studies were indicated, and several of these compare TUVP with TURP. Patel and colleagues (2000) have carefully reviewed five of these in which different types of electrode were used (Galluci et al, 1996; Patel et al, 1997; Shokeir et al, 1997; Hammadeh et al, 1998; McAllister et al, 1998). A total of 270 patients had TURP, whereas 262 patients had TUVP. A comparison of complications shows that postoperative irritative symptoms, urinary infection, 1-year reoperation rate, and urethral stricture were the same in both groups. However, catheter duration postoperatively, hematuria, transfusion rate, and retrograde ejaculation were lower in the TUVP group, as was hospital stay. Operating time, postoperative urinary retention, impotence, and urinary incontinence were higher in the TUVP group. Again, these were all short-term studies, with follow-up to a maximum of 1 year. In some cases, the numbers of patients who had actually reached 1-year follow-up were not stated. In addition, the range on either side of the mean was quite wide. All of the studies showed significant improvements in symptom score and PFR, which were maintained to the time of maximal follow-up in the study reported.
In most studies the size of the prostate gland operated on was 60 mL or less as measured by TRUS. The follow-up period for these studies needs to be much longer than 1 year so that the comment “TUVP is an acceptable alternative to TURP” can be sustained. In addition, the complication rates in some studies are rather high; for example, the study by De Sautel and colleagues (1998) shows that in a relatively small number of cases TUVP is as effective as TURP in relieving urodynamically proven outflow obstruction, but the overall complication rate for TUVP was 17.5%.
There has been a somewhat longer randomized trial comparing TUVP with TURP (McAllister et al, 2003). In this study, 235 patients with symptomatic BPH were randomly assigned to the two treatment options and it was a multicenter trial from four study centers in the United Kingdom. Forty-five of the 235 presented with acute urinary retention, and for the remainder a reduction in IPSS of 5 or more points was defined as success; statistically, and using this definition of success, 220 patients were required in the study to be able to detect a 15% difference in treatment outcome with 80% power at the 5% level. The mean reduction in prostate volume was the same in both groups, as were the operating time, hospital stay, and the improvement in symptom score, PFR, and postvoid residual volume. The transfusion rate was higher in the TURP group. At 6 months, 9% of the TURP group had become impotent, compared with 17% in the TUVP group, but this difference was not statistically significant.
A meta-analysis was performed comparing the efficacy and safety of TUVP and TURP for symptomatic BOO secondary to BPH. From a total of 25 randomized controlled trials, 20 met the predefined inclusion criteria and were subjected to a formal analysis. A total of 1489 patients were randomly assigned to TUVP (708) or TURP (781). There was a considerable variation in the follow-up, but the median was 12 months. The meta-analysis found a considerable limitation to most of the studies, particularly pertaining to the justification of sample size, randomization, the procedure for concealing treatment allocation, and the appropriate handling of study withdrawals to maintain the principle of intention-to-treat analysis. None of the studies estimated the sample size before starting the study as part of their calculation of statistical power, and only two described how the random allocation sequence was generated. There was also a considerable variation in the method of reporting the outcomes of the individual studies. Once again, this meta-analysis, as others related to other minimally invasive treatments have shown, demonstrates a poor database for drawing meaningful conclusions. However, it did suggest that TURP and TUVP provide comparable improvements in AUASI score and PFR for up to 1 year of follow-up (Poulakis et al, 2004).
Vaporization-Resection
A number of relatively short-term pilot studies using the Wing, Wedge, and Vapor Cut electrodes have been published and have been summarized by Cabelin and colleagues (2000). They have shown that the efficacy and complication rates are the same as with the standard Vapor Trode. The number of patients treated varied from 31 to 91, and the size of the gland ranged from 39 to 59.6 mL. The operating time was long (49.3 to 56.7 minutes), but the AUASI score decreased from 24.3 to 4.1 with the Wing and from 19.0 to 7.2 with the Vapor Cut. The PFR improved from 5.2 and 8.9 to 16.0 and 18.4 mL/sec, respectively (Perlmutter and Schulsinger, 1998; Küpeli et al, 1999; Perlmutter and Vallencien, 1999; Talic, 1999).
A comparative study between TUVRP and TURP has been reported by Talic and coworkers (2000). The Wing resection electrode was used in the TUVRP group. All patients were observed for about 9 months, with a range of 6 to 15 months. At 6 months the TUVRP group had improvements in AUASI score (24.9 to 4 ± 3.4) and PFR (7.5 to 19 ± 6.5 mL/sec); the TURP group had comparable improvements in symptom score (20.1 to 5.6 ± 3.1) and PFR (9.1 to 15.2 ± 10 mL/sec). Of particular note is the very wide range on either side of the mean values.
Summary
TUVP and TUVRP are technologic innovations based on an idea that has been present for some years. Modifications are being made in the equipment that will make this even safer and that will prevent some of the potential problems associated with the delivery of high power to tissues. Efficacy appears similar to that of TURP, but the studies are short-term evaluations and the glands operated on are relatively small. The short-term complication profile appears to be better than with TURP, but further studies are required to prove this because there is a certain variability in the rate of occurrence of some of them. In general, although the catheterization time is shorter than with TURP, the operating time is longer. Before this can be accepted as a technique that will replace TURP, long-term multicenter randomized trials are required. However, the technologic improvements and the consistently similar short-term improvements in AUASI score and PFR are encouraging.
Transurethral Incision of the Prostate
If a poll were to be taken among urologists as to how many would favor a transurethral incision of the prostate (TUIP) as treatment for symptomatic BPH, it is likely that the number would be very small. However, TUIP has been available since the 19th century. Edwards and colleagues (1985) credit Bottini with describing the technique in 1887, but Hedlund and Ek (1985) credit Guthrie in 1834. Guthrie’s technique was to disrupt the bladder neck, whereas Bottini used diathermy to divide it. However, in 1973, Orandi published the first significant series on TUIP. The procedure seemed to be most useful in those who had a small prostate and who had obstructive bladder outflow symptoms. Classically, the patient was a younger man when compared with those having TURP (Orandi, 1973).
Technique
The surgical technique is relatively simple. With a Collings knife, an incision is made at the 5- and 7-o’clock positions or on one side of the midline only. It starts just distal to the ureteral orifice and ends just proximal to the verumontanum (Fig. 93–16). The incision depth should be to the point at which fine filaments of the external capsule are seen. Care must be taken not to incise too deeply because extravasation of irrigation fluid or rectal injury may occur. With completion of the incisions and with the scope in the more distal urethra there should be no visible obstruction to the bladder outflow.
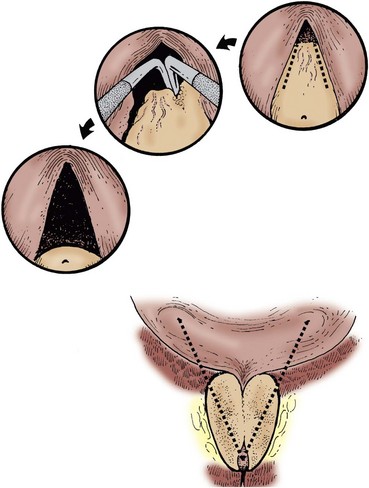
Figure 93–16 Transurethral incision of the prostate. The incision is started at the ureteral orifice and carried through the bladder neck up to the verumontanum. This procedure is done bilaterally.
(From Mebust WK. A review of TURP complications and the National Cooperative Study, lesson 24, volume VIII. 1989. p. 189–90.)
Complications
The advantage of TUIP is that it is quick, technically easier, and associated with less morbidity and a decrease in retrograde ejaculation compared with TURP. The incidence of retrograde ejaculation after TURP ranges from 50% to 95%; but after TUIP it has been reported as occurring in 0% to 37% of cases. Turner-Warwick (1979) noted that with one incision the incidence of retrograde ejaculation was less than 5% but with two incisions it was 15%. Hedlund and Ek (1985) reported no difference between this incidence with one and with two incisions.
Clinical Efficacy
The procedure has been assessed by some open studies using strict urodynamic criteria for evaluation. Edwards and Powell (1982) found a significant reduction in voiding pressure after TUIP. Kelly and colleagues (1989) used pressure-flow curves and showed a significant fall in voiding pressure, with shift of the Pdet at PFR from the obstructive to the equivocal range on the Abrams-Griffiths nomogram. They found it to be less effective than TURP in relieving obstruction. Katz and colleagues (1990) noted a satisfaction rating of up to 94% with a significant improvement in symptoms and PFR after TUIP.
Sirls and colleagues (1993) reviewed 41 men (mean age, 63.4 years) for a mean follow-up of 53 months. The Boyarsky symptom score decreased from 12.5 to 6.9, and the PFR improved from 10.3 to 15.3 mL/sec. The postvoid residual urine volume decreased from 179.8 to 99.4. The Pdet at PFR decreased from 84.5 to 44.5 cm H2O, all of which indicated an excellent response to TUIP, particularly if the prostate gland weighed 30 g or less.
In the largest series, Orandi (1985) reported on 646 patients whom he had observed from 3 months to 15 years, finding a reoperation rate of 9.6%.
Comparative Studies
Orandi (1973), in a prospective study over a 2-year period of 132 patients managed with TURP or TUIP, found that the results and complications did favor TUIP but there was no statistically significant difference between the two treatments. The only apparent difference was the higher incidence of bladder neck contraction after TURP.
Miller and associates (1992) reported on 108 patients who underwent a bladder neck incision and compared them with a similar group undergoing TURP. They believed that bladder neck incision was better than TURP in terms of a shorter operative time and shorter duration of catheterization. No other perioperative differences were found. For the 10-year follow-up there was no difference in reoperation rates between the two groups, with an equally high approval by patients after both procedures. In another comparative study, Soonawalla and Pardanini (1992) found that the PFR increased from 8 to 19 mL/sec after TUIP and from 8 to 21 mL/sec after TURP.
Dorflinger and coworkers (1992) randomly assigned 60 patients to either TURP or TUIP. They found that both operations significantly improved AUASI score and PFR, but the improvement in PFR was better for the TURP group. Neither operation caused any significant change in sexual activity or erectile function postoperatively. Retrograde ejaculation was a more common occurrence in patients treated by TURP. Riehmann and colleagues (1995) randomly assigned 56 patients to TURP and 61 to TUIP, and there was a mean follow-up of 34 months. Differences in PFR improvement were significant statistically at 3 months and 24 months only and not at any other time. Retrograde ejaculation was twice as common in the TURP group. Reoperation was required in slightly more patients in the TUIP group, but the difference was not statistically significant. The AHCPR BPH Guideline Panel (McConnell et al, 1994) performed a meta-analysis of the various studies, and the results are noted in Table 93–5. There is a slightly better chance of improvement of symptoms of patients treated by TURP, as there is in the degree of that improvement.
Table 93–5 Treatment Outcomes Balance Sheet
| OUTCOME | TUIP | TURP |
|---|---|---|
| Chance of symptom improvement | 78%-83% (80) | 75%-96% (88) |
| Degree of symptom improvement | 73% | 85% |
| Morbidity (20% significant) | 2.2%-33% (14) | 5.2%-30.7% (16) |
| Mortality (30-90 days) | 0.2%-1.5% | 0.53%-3.31% |
| Incontinence (total) | 0.061%-1.1% | 0.68%-1.4% |
| Operative treatment for surgical complications | 1.34%-2.65% | 0.68%-10% |
| Impotence | 3.9%-24.5% | 3.3%-34.8% |
| Retrograde ejaculation | 6%-55% | 25%-99% |
TUIP, transurethral incision of the prostate; TURP, transurethral resection of the prostate.
From Barry MJ, Fowler FJ Jr, O’Leary MP, et al. The American Urological Association’s symptom index for benign prostatic hyperplasia. J Urol 1992;148:1549–57.
Summary
TUIP is effective in treating patients with LUTS caused by BOO. It has been shown to have an important role in the management of younger patients, especially if the prostate is smaller than 30 g. The efficacy is comparable in such patients with TURP, and the results are maintained in the long term. The technique is simple, and the morbidity is low.
Other Technologies
There are some other approaches that have not been previously mentioned in this chapter but they are included only to complete the picture. There is no significant evidence available to support any of these as having a future in the treatment of symptomatic BPH. The literature mainly consists of open studies, which in many cases would correspond to phase 1 trials or very small phase 2 trials.
Water-Induced Thermotherapy
Water-induced thermotherapy is another treatment introduced to treat LUTS and to reduce BOO secondary to BPH. An early article (Corica et al, 2000) assessed its effect on prostatic tissue, using it in both benign and malignant prostates, in 27 patients. The patients were awake, with local anesthetic gel inserted urethrally. The discomfort experienced by patients was recorded as mild. Pathologic examination of the removed prostate consistently showed periurethral hemorrhagic necrosis extending up to 11 mm from the urethra, focal or extensive urothelial denudation, and mild inflammation.
The same group of authors subsequently developed a novel rapid high-temperature, liquid-filled, flexible balloon thermotherapy system (Corica et al, 2003). The same anesthesia as previously was used in 17 patients, and a full histologic study was performed. Again, consistent findings were recorded, including periurethral hemorrhagic necrosis, extensive denudation, and varying degrees of inflammation. The mean depth of necrosis was 0.9 cm, involving a mean of 16% of the prostatic adenoma. In the prostates examined later, the necrotic tissue had been replaced by scar tissue (fibrosis and hyalinization) with a mean depth of 0.13 cm.
In a small open study, two slightly different temperatures were used in two groups of patients (Breda and Isgro, 2002). Because of the small numbers the results are somewhat difficult in that the temperature did not matter and that previously catheter-dependent patients were able to void with a PFR of 10.7 to 11.5 mL/sec in 73% to 88% of patients.
There has been a prospective multicenter trial performed involving 125 patients (Muschter et al, 2000). Improvement was noted at 3 months, extending to 12 months. The IPSS at 12 months had improved by a median of 12.5 symptom units and the PFR improved by 6.4 mL/sec over baseline. This was not a comparative study. Side effects were minimal. The authors concluded that the treatment held promise as a useful and cost-effective option for management of BPH. In a later review of the topic, the failure rate and rate of subsequent TURP were reported as 5.6% after 12 months, 9.6% after 24 months, and 11.2% after 36 months (Muschter, 2003).
Transurethral Ethanol Ablation of the Prostate
This technique has not been subjected to a great deal of in-depth study. It was initially introduced as a transperineal injection, with phenol being the agent injected (Talwar and Pande, 1966; Angell, 1969). There was clear evidence from several early studies that the agent injected leaked extraprostatically, with consequently a relatively high incidence of significant adverse events. The development of a transurethral method of injecting ethanol has been seen as a safer approach (Goya et al, 1999; Ditrolio et al, 2002). A detailed description of the injection technique is to be found in these articles and in the study presented by Plante and colleagues (2003), who also describe the histologic findings observed in the canine prostate. They found a considerable lobular volume of necrosis (mean of 42.6%); and although the findings were not absolutely consistent, they found that the prostate capsule always acted as a relative barrier to ethanol diffusion after transurethral injection.
A European multicenter study has been performed in 115 symptomatic BPH patients using transurethral ethanol ablation of the prostate (Grise et al, 2004), and 94 of these patients were observed for 12 months. An average reduction in prostate volume of 16% was found, with a small adverse event rate and a requirement for TURP in 7% of patients in that time period. Relatively modest improvements in IPSS and PFR were reported, with 98% of patients voiding spontaneously 4 days after treatment.
Rotoresection of the Prostate
This technique has not been widely reported, but early studies, both experimental and clinical, have been published. It has been designed for conventional transurethral application, with an axially adjustable actively rotating crank with a milling-head spiked electrode fitting into a specifically designed working element instead of a loop electrode. It is driven by a micromotor, which transmits rotation to the electrode by an angled drill handle. The first use of this system was reported by Michel and coworkers in 1996. In an experimental porcine model these researchers found a rate of time ablation comparable to that of a standard resection loop (5.5 to 6.0 g/min) and more than twice that of electrovaporization (1.7 to 2.0 g/min). The rate of bleeding was significantly better than for either, and the depth of tissue coagulation was 1.5 mm, compared with 0.4 mm with TURP.
There have been three clinical studies. Michel and coworkers (2003) used the rotoresect system in 84 patients and evaluated them for up to 4 years. They found no change in hemoglobin or serum sodium values. The mean duration of catheterization was 1.4 days. There was an early significant improvement in IPSS and PFR, which lasted to the 4-year evaluation.
A prospective study was carried out, and results at 12 months (Wadie et al, 2003) and 24 months (Wadie et al, 2005) have been published. In the latter report the results of 23 of the original 24 patients have been evaluable. The AUASI score decreased from 20.5 ± 3.8 to 1.12 ± 1.56, and the PFR rose from 8.7 ± 2.1 to 21.8 ± 8.5 mL/sec, results comparable to those reported earlier. Again, the complication rate was found to be low.
Summary
Since the previous edition of this book there is very little new apart from the explosion of interest in the newer types of laser therapy. Many of the recent papers on thermotherapy describe newer techniques but once again fail to get to the “meat” of the subject, which is to answer the question as to the exact position of thermotherapy in the management of BPH. Even in the case of the laser therapies, the authors do not tell the reader if they consider that they will actually overtake TURP and supplant it in the future. In addition, the standard of trials has not improved greatly, with many still being open label studies with no comparator group; some of the comparative studies have group sizes that do not give the impression of having been powered statistically to show either equivalence or a specifically stated difference. There have been several new meta-analyses or systematic literature reviews, which may help the reader to make a more balanced, evidence-based decision.
There has been much discussion as to which of these therapies is better than TURP. At present, it would seem that TURP is either equivalent to the best of the minimally invasive therapies or better than most in terms of improvement of subjective and objective indices. As was stated in the introduction, however, it is not only the efficacy of the treatment that must be compared with TURP. The adverse event profile, the requirement for intravenous sedation, length of hospitalization, and cost also are all very important.
The vast majority of trials that have been reported compare a treatment with TURP only against efficacy, whereas it would be of benefit to the urologist if trials could view the comparison of the other factors in a prospective way, perhaps even excluding efficacy. This has been done by some authors, but a major multicenter approach would give the best information. In this way, it would be clear which is the best way to treat BPH.
However, the view could be taken that it is not necessary to find a minimally invasive treatment that is better than TURP. For example, none of the drug treatments has even come close to the efficacy of TURP, but they have been demonstrated to be of lasting value in management and have found a very specific place in the treatment armamentarium of BPH. In that case, the questions just posed would need to be answered very carefully.
It might be considered controversial to state that perhaps patients should be allowed to have sequential treatments. It is known that some patients do not respond well to specific minimally invasive treatments, so perhaps they might have a second treatment with the same modality, even a relatively short time after the first. There may be cost implications that would have the hospital managers shaking their heads, but it would certainly lower hospital bed requirements if it proved successful. In the same way, if a treatment proved efficacious for a 3-year period and then the symptoms returned, it is conceivable that a further treatment might return the patient to symptomatic well-being, even if a further full evaluation was required.
What is definitely necessary is that the exact place for each treatment modality should be found. Some may well have a small but well-defined role in the management of BPH, and, in the case of others, this role may be larger. One of the problems with extracorporeal shockwave lithotripsy was that it took a long time to find exactly how it should be used to treat, for example, staghorn renal calculi; no comparative trial was performed. In the same way, TURP was introduced without a comparative trial; and although it is recognized now as the gold standard, it took several decades before this happened. Minimally invasive treatments are in most cases pitted against TURP, but with many of them this has been a wasted exercise because in the preliminary open studies they could have clearly been seen not to be as efficacious. Commercial necessity requires comparison against a recognized treatment, but often this is not in the patients’ best interests. It may be that the treatment has a lesser, but equally important, role to play.
At the International Consultation on BPH, held in July 2000, the committee that discussed “International Therapy for Benign Prostatic Hyperplasia” prepared a report (Debruyne et al, 2001). In it was outlined final recommendations on the use of such treatments, which were defined as acceptable, acceptable with restriction, investigational, or unacceptable. This decision was based on several meetings between the members of the panel and is rather a suggestion than an instruction to urologists.
The panel found that a number of treatments for BPH were unacceptable: balloon dilatation, hyperthermia, and high-intensity focused ultrasonography. It is widely accepted that this is so, and these treatments have not been dealt with in this discussion because it is unlikely that they will have a role in the future in their present form. Prostatic stents are deemed acceptable with restriction, which once again is not controversial because that restriction has been clearly described in the large number of original and review articles related to them.
Rather more interesting is the list of treatments described as being acceptable, presumably without restriction in the minds of the panel: TUMT, transurethral needle ablation, interstitial laser coagulation, laser-vaporization, and transurethral electrovaporization (naturally, TURP and open prostatectomy are also included). It may be that these newer treatments are acceptable, but it is absolutely necessary to define in what way and to remember that, in most of these treatments, the results are short term. In some cases, they may be considered as possible replacements for TURP, but, in that case, a large amount of further information is required related to the points previously discussed and to long-term efficacy. In the case of those being considered as alternative treatments for BPH not necessarily as good as TURP, their exact role needs to be defined.
It is very likely that some day TURP will be replaced as the ideal interventional treatment for BPH. It took a considerable amount of time for TURP to achieve its exalted position, but it could happen soon that some other treatment will occupy that position.
Key Points
Boyle P, Robertson C, Vaughan ED, Fitzpatrick JM. A meta-analysis of trials of transurethral needle ablation for treating symptomatic benign prostatic hyperplasia. BJU Int. 2004;94:83-88.
Emberton M, Neal DE, Black N, et al. The National Prostatectomy Audit: the clinical management of patients during hospital admission. Br J Urol. 1995;75:301-316.
Hoffman RM, MacDonald R, Wilt TJ. Laser prostatectomy for benign prostatic obstruction. Cochrane Database Syst Rev 2004;(1):CD001987.
McAllister WJ, Absalom MJ, Mir K, et al. Does endoscopic laser ablation of the prostate stand the test of time? Five-year results from a multicentre randomised controlled trial of endoscopic laser ablation against transurethral resection of the prostate. BJU Int. 2000;85:437-439.
Mebust WK, Holtgrewe HL, Cockett ATK, et al. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of thirteen participating institutions evaluating 3,885 patients. J Urol. 1989;141:243-247.
Roehrborn CG, Preminger G, Newhall P, et al. Microwave thermotherapy for benign prostatic hyperplasia with the Dormier Urowave: results of a randomized, double blind, multicenter, sham-controlled study. Urology. 1998;51:19-28.
Tan AH, Gilling PJ, Kennett KM, et al. Long-term results of high-power holmium laser vaporization (ablations) of the prostate. BJU Int. 2003;92:707-709.
Te AE, Malloy TR, Stein BS, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicentre prospective trial. J Urol. 2004;172:1404-1408.
Wheelahan J, Scott NA, Cartmill R, et al. Minimally invasive non-laser thermal techniques for prostatectomy: a systematic review. BJU Int. 2000;86:977-988.
Anson KM, Barnes DJ, Briggs TP, et al. Temporary prostatic stenting and androgen suppression: a new minimally invasive approach to malignant prostatic retention. J R Soc Med. 1993;86:634-638.
Bajoria S, Agarwal SA, White R, et al. Experience with the second generation UroLume prostatic stent. Br J Urol. 1995;75:325-327.
Barnes DJ, Butterworth P, Flynn JT. Combined endoscopic laser ablation of the prostate (ELAP) and temporary stenting. Min Invas Ther Allied Technol. 1996;5:333-335.
Braf Z, Chen J, Sofer M, et al. Intraprostatic stents (Prosta Kath and Urospiral): more than six years’ clinical experience with 110 patients. J Endourol. 1996;10:555-558.
Chancellor MB, Bennett C, Simoneau AR, et al. Sphincteric stent versus external sphincterotomy in spinal cord injured men: prospective randomized multicenter trial. J Urol. 1999;161:1893-1898.
Chapple CR, Milroy EJG, Rickards D. Permanently implanted urethral stent for prostatic obstruction in the unfit patient: preliminary report. Br J Urol. 1990;66:58-64.
Chartier-Kastler EJ, Thomas L, Bussel B, et al. A urethral stent for the treatment of detrusor-striated sphincter dyssynergia. BJU Int. 2000;86:52-57.
Clayman RV. In vitro results with special plastics for biodegradable endoureteral stents. J Urol. 2000;163:1620-1621.
Corica AP, Larson BT, Sagaz A, et al. A novel temporary prostatic stent for the relief of prostatic urethral obstruction. BJU Int. 2004;93:346-348.
Dahlstrand C, Grundtman S, Pettersson S. High energy transurethral microwave thermotherapy for large severely obstructing prostates and the use of biodegradable stents to avoid catheterization after treatment. Br J Urol. 1997;79:907-909.
Devonec M, Dahlstrand C. Temporary urethral stenting after high-energy transurethral microwave thermotherapy of the prostate. World J Urol. 1998;16:120-125.
Djavan B, Fakhari M, Shariat S, et al. A novel intraurethral prostatic bridge-catheter for prevention of temporary prostatic obstruction following high-energy transurethral microwave thermotherapy in patients with benign prostatic hyperplasia. J Urol. 1999;161:144-151.
Dotter CT. Transluminally placed coilspring endarterial tube grafts: long-term patency in canine popliteal artery. Invest Radiol. 1969;4:329-332.
Dotter CT, Buschmann RW, McKinney MK, et al. Transluminal expandable nitinol coil stent grafting: preliminary report. Radiology. 1983;147:259-260.
Fabian KM. Der Intraprostatische “Partielle Katheter” (Urologische Spirale). Urologe [A]. 1980;19:236-238.
Furui S, Sawoda S, Irie T, et al. Hepatic IVC obstruction: treatment of two types with Gianturco expandable metallic stents. Radiology. 1990;176:620-621.
Gajewski JB, Chancellor MB, Ackman CF, et al. Removal of UroLume endoprosthesis: experience of the North American Study Group for detrusor-sphincter dyssynergia application. J Urol. 2000;163:773-776.
Gesenberg A, Sintermann R. Management of benign prostatic hyperplasia in high risk patients: long-term experience with the Memotherm stent. J Urol. 1998;160:72-76.
Guazzoni G, Pansadoro V, Montorsi F, et al. A modified prostatic UroLume wallstent for healthy patients with benign prostatic hyperplasia: a European multicenter study. Urology. 1994;44:364-370.
Harrison NW, De Souza JV. Prostatic stenting for outflow obstruction. Br J Urol. 1990;65:192-196.
Hurwitz JJ. Teflon tubes for stenting and bypassing the lacrimal drainage pathway. Ophthalmic Surg. 1989;20:855-859.
Kaplan SA, Chiou RK, Morton WJ. Long-term experience utilising a new balloon expandable prostatic endoprosthesis: the Titan Stent. North American Titan Stent Study Group. Urology. 1995;45:224-234.
Karaoglau U, Alkibay T, Tokucoglu H, et al. Urospiral in benign prostatic hyperplasia. J Endourol. 1992;6:455-461.
Kemppainen E, Talja M, Riihela M, et al. A bioresorbable urethral stent: an experimental study. Urol Res. 1993;21:235-238.
Kirby RS, Heard BR, Miller P, et al. Use of the ASI titanium stent in the management of bladder outlet obstruction due to benign prostatic hyperplasia. J Urol. 1992;48:1195-1197.
Knutson T, Pettersson S, Dahlstrand C. The use of biodegradable PGA stents to judge the risk of post-TURP incontinence in patients with combined bladder outlet obstruction and overactive bladder. Eur Urol. 2003;42:262-267.
Konety BR, Phelan MW, O’Donnell WF, et al. UroLume stent placement for the treatment of postbrachytherapy bladder outlet obstruction. Urology. 2000;55:721-724.
Laaksovirta S, Isotalo T, Talja M, et al. Interstitial laser coagulation and biodegradable self-expandable, self-reinforced poly-L-lactic and poly-L-glycolic copolymer spiral stent in the treatment of benign prostatic enlargement. J Endourol. 2002;16:311-315.
Luesley DM, Redman CW, Buxton EJ, et al. Prevention of postcone biopsy cervical stenosis using a temporary cervical stent. Br J Obstet Gynaecol. 1990;97:334-337.
Lumiaho J, Heino A, Tunninen V, et al. New bioabsorbable polylactide ureteral stent in the treatment of ureteral lesions: an experimental study. J Endourol. 1999;13:107-112.
Maass D, Kropf L, Gloff L, et al. Transluminal implantation of intravascular “double helix” spiral prosthesis: technical and biological considerations. Proc Eur Soc Artif Organs. 1982;9:252-257.
Mair EA, Parsons DS, Lally PK, et al. Treatment of severe bronchomalacia with expanding endobronchial stents. Arch Otolaryngol Head Neck Surg. 1990;116:1087-1090.
Masood S, Djaladat H, Kouriefs C, et al. The 12-year outcome analysis of an endourethral Wallstent for treating benign prostatic hyperplasia. BJU Int. 2004;94:1271-1274.
McLoughlin J, Jager R, Abel PD, et al. The use of prostatic stents in patients with urinary retention who are unfit for surgery. Br J Urol. 1990;66:66-70.
Meulen T, Zambon JV, Janknegt RA. Treatment of anastomotic strictures and urinary incontinence after radical prostatectomy with UroLume Wallstent and AMS 800 artificial sphincter. J Endourol. 1991;13:517-520.
Nissenkorn I. Prostatic stents. J Endourol. 1991;5:79-82.
Nissenkorn I, Slutzker D, Shalev M. Use of an intraurethral catheter instead of a Foley catheter after laser treatment of benign prostatic hyperplasia. Eur Urol. 1996;29:341-344.
Nordling J. Temporary stents. In: Kirby R, McConnell J, Fitzpatrick J, et al, editors. Textbook of benign prostatic hyperplasia. Oxford (UK): Isis Medical Media; 1996:443-452.
Nordling J, Holm HH, Klarskov P. The intraprostatic spiral: a new device for insertion with the patient under local anesthesia and with ultrasonic guidance with 3 months follow-up. J Urol. 1989;142:756-762.
Oesterling JE, Kaplan SA, Epstein HB, et al. The North American experience with the UroLume endoprosthesis as a treatment for benign prostatic hyperplasia: long-term results. The North American UroLume Study Group. Urology. 1994;44:353-362.
Oosterlinck W, Talja M. Endoscopic urethroplasty with a free graft on a biodegradable polyglycolic acid spiral stent: a new technique. Eur Urol. 2000;37:112-115.
Ozgur GK, Sivrikaya A, Bilen R, et al. The use of intraurethral prostatic spiral in high risk patients for surgery with benign prostatic hyperplasia. Int Urol Nephrol. 1993;25:65-71.
Palmaz JD, Kapp DT, Hayoski H, et al. Normal and stenotic renal arteries: experimental balloon-expandable intraluminal stenting. Radiology. 1987;164:705-708.
Perry MJ, Roodhouse AJ, Gidlow AB, et al. Thermo-expandable intraprostatic stents in bladder outlet obstruction: an 8-year study. BJU Int. 2002;90:216-223.
Petas A, Talja M, Tammela TL, et al. The biodegradable self-reinforced poly-DL-lactic acid spiral stent compared with a suprapubic catheter in the treatment of postoperative urinary retention after visual laser ablation of the prostate. Br J Urol. 1997;80:439-443.
Petas A, Talja M, Tammela T, et al. A randomised study to compare biodegradable self-reinforced polyglycolic acid spiral stents to suprapubic and indwelling catheters after visual laser ablation of the prostate. J Urol. 1997;157:173-176.
Petas A, Vuopio-Varkila J, Siitonen A, et al. Bacterial adherence to self-reinforced polyglycolic acid and self-reinforced polylactic acid 96 urological spiral stents in vitro. Biomaterials. 1998;19:677-681.
Poulsen AL, Shou J, Oveson H, et al. Memokath: a second generation of intraprostatic spirals. Br J Urol. 1993;72:331-337.
Sassine AM, Schulman CC. Intra-urethral catheter in high-risk patients with urinary retention: 3 years of experience. Eur Urol. 1994;25:131-134.
Schlick RW, Planz K. In vitro results with special plastics for biodegradable endourethral stents. J Endourol. 1998;12:451-455.
Skapshay SM, Beamis JF, Dumon JF. Total cervical tracheal stenosis: treatment by laser, dilatation, and stenting. Am J Otol Laryngol Rhinol. 1989;8:890-895.
Talja M, Tammela T, Petas A, et al. Biodegradable self-reinforced polyglycolic acid spiral stents in prevention of postoperative urinary retention after visual laser ablation of the prostate-laser prostatectomy. J Urol. 1995;154:2089-2092.
Tamai H, Igaki K, Kyo E, et al. Initial and 6-month results of biodegradable poly-L-lactic acid coronary stents in humans. Circulation. 2000;102:399-404.
Thomas PJ, Britton JP, Harrison NW. The Prosta Kath stent: 4 years’ experience. Br J Urol. 1993;71:430-432.
Tillem SM, Press SM, Badlani GH. Use of multiple UroLume endourethral prosthesis in complex bulbar urethral strictures. J Urol. 1997;157:1665-1668.
Vaajanen A, Nuutinen JP, Isotalo T, et al. Expansion and fixation properties of a new braided biodegradable urethral stent: an experimental study in the rabbit. J Urol. 2003;169:1171-1174.
Williams G, Coulange C, Milroy E, et al. The nonoperative treatment for bladder outflow obstruction. J Urol. 1993;156:69-75.
Williams G, White R. Experience with the Memotherm permanently implanted prostatic stent. Br J Urol. 1995;76:337-340.
Wright KC, Wallace S, Chamsanguej C, et al. Percutaneous endovascular stents: an experimental evaluation. Radiology. 1985;156:69-72.
Yachia D, Beyar M, Aridogan IA. A new large calibre self expanding and self retaining temporary intraprostatic stent (Prostacoil) in the treatment of prostatic obstruction. Br J Urol. 1994;74:47-52.
Transurethral Needle Ablation of the Prostate
Boyle P, Robertson C, Vaughan ED, Fitzpatrick JM. A meta-analysis of trials of transurethral needle ablation for treating symptomatic benign prostatic hyperplasia. BJU Int. 2004;94:83-88.
Bruskewitz R, Issa M, Roehrborn CG, et al. A prospective, randomised, 1-year clinical trial comparing transurethral needle ablation (TUNA) to transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia. J Urol. 1998;159:1588-1594.
Calkins H, Langberg J, Sousa J, et al. Radiofrequency catheter ablation of accessory atrioventricular connections in 250 patients: abbreviated therapeutic approach to Wolff-Parkinson-White syndrome. Circulation. 1992;85:1337-1346.
Campo B, Bergamasghi F, Corrada P, et al. Transurethral needle ablation (TUNA) of the prostate: a clinical and urodynamic evaluation. Urology. 1997;49:847-850.
Giannakopoulos X, Grammeniatis E, Gartzios A, et al. Transurethral needle ablation (TUNA) of the prostate: preliminary results using the new generation TUNA III catheter on patients with symptomatic BPH controlled by a series of 50 patients using the TUNA II device. Eur Urol. 1996;30(Suppl.):A986.
Goldwasser B, Ramon J, Engelberg S, et al. Transurethral needle ablation (TUNA) of the prostate using low-level radiofrequency energy: an animal experimental study. Eur Urol. 1993;24:400-405.
Hill B, Belville W, Bruskewitz R, et al. Transurethral needle ablation versus transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia: 5-year results of a prospective, randomized, multicenter clinical trial. J Urol. 2004;171:2336-2340.
Issa MM, Oesterling JE. Radiofrequency thermal therapy for benign prostatic hyperplasia by transurethral needle ablation of the prostate. In: Narayan P, editor. Benign prostatic hyperplasia. London: Churchill Livingstone; 2000:269-280.
Issa MM, Wojno KJ, Oesterling JE, et al. Histopathological and biochemical study of the prostate following transurethral needle ablation (TUNA): insight into the mechanism of improvement in BPH symptoms. J Endourol. 1996;10:109.
Lord SM, Barnsley L, Wahis BJ, et al. Percutaneous radiofrequency neurotomy for chronic cervical zygapophyseal joint pain. N Engl J Med. 1996;336:1721-1726.
Millard RJ, Harewood LM, Tamaddon K. A study of the efficacy and safety of transurethral needle ablation (TUNA) for benign prostatic hyperplasia. Neurourol Urodyn. 1996;15:916-929.
Minardi D, Garofalo F, Yehia M, et al. Pressure-flow studies in men with benign prostatic hypertrophy before and after treatment with transurethral needle ablation. Urol Int. 2001;66:89-93.
Naslund MJ. A cost comparison of TUNA vs TURP. J Urol. 1997;157:155.
Naslund MJ, Carlson AM, Williams MJ. A cost comparison of medical management and transurethral needle ablation for treatment of benign prostatic hyperplasia during a 5-year period. J Urol. 2005;173:2090-2093.
Organ LW. Electrophysiological principles of radiofrequency lesion making. International Symposium on Radiofrequency Lesion Making Procedures, Chicago, Illinois, 1976. Appl Neurophysiol. 1976;39:69-76.
Perlmutter AP, Verdi J, Watson GM. Prostatic heat treatments for urinary outflow obstruction. J Urol. 1993;150:1603-1606.
Ramon J, Goldwasser B, Shenfeld O, et al. Needle ablation using radiofrequency current as a treatment for benign prostatic hyperplasia: experimental results in ex vivo human prostate. Eur Urol. 1993;24:406-410.
Ramon J, Lynch TH, Eardley I, et al. Transurethral needle ablation of the prostate for the treatment of benign prostatic hyperplasia: a collaborative multicenter study. Br J Urol. 1997;80:128-135.
Rasor JS, Zlotta AR, Edwards SD, et al. Transurethral needle ablation (TUNA): thermal gradient mapping and comparison of lesion size in a tissue model and in patients with benign prostatic hyperplasia. Eur Urol. 1993;24:411-414.
Roehrborn CG, Issa MM, Bruskewitz R, et al. Transurethral needle ablation (TUNA) for benign prostatic hyperplasia: 12-month results of a prospective multicenter study. Urology. 1998;51:415-421.
Rosario DJ, Woo H, Potts KL, et al. Safety and efficacy of transurethral needle ablation of the prostate for symptomatic outlet obstruction. Br J Urol. 1997;80:579-586.
Rossi S, Di Stasi M, Buscharini E, et al. Percutaneous radiofrequency interstitial thermal ablation in the treatment of small hepatocellular carcinoma. Cancer J Sci Am. 1995;1:73-81.
Schulman CC, Zlotta AR. Transurethral needle ablation of the prostate for treatment of benign prostatic hyperplasia: early clinical experience. Urology. 1995;45:28-33.
Schulman CC, Zlotta AR, Rasor JS, et al. Transurethral needle ablation (TUNA): safety, feasibility and tolerance of a new office procedure for treatment of benign prostatic hyperplasia. Eur Urol. 1993;24:415-423.
Steele GS, Sleep DJ. Transurethral needle ablation of the prostate: a urodynamic-based study with two-year follow-up. J Urol. 1997;158:1834-1838.
Zlotta AR, Giannakopoulos X, Maehlum O, et al. Long-term evaluation of transurethral needle ablation of the prostate (TUNA) for treatment of symptomatic benign prostatic hyperplasia: clinical outcome up to five years from three centers. Eur Urol. 2003;44:89-93.
Zlotta AR, Kiss R, De Decker R, et al. MXT mammary tumor treatment with a high temperature radiofrequency ablation device. Int J Oncol. 1995;7:863-869.
Zlotta AR, Raviv G, Peny MO, et al. Possible mechanisms of action of transurethral needle ablation of the prostate on benign prostatic hyperplasia symptoms: a neurohistochemical study. J Urol. 1997;157:894-899.
Transurethral Microwave Therapy
Ahmed M, Bell T, Lawrence WT, et al. Transurethral microwave therapy (Prostatron version 2.5) compared with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: a randomised, controlled, parallel study. Br J Urol. 1997;79:181-185.
Alivizatos G, Ferakis N, Mitropoulos D, et al. Feedback microwave thermotherapy with the ProstaLund Compact Device for obstructive benign prostatic hyperplasia: 12-month response rates and complications. J Endourol. 2005;19:72-78.
Astrahan M, Ameye F, Oyen R, et al. Interstitial temperature measurements during transurethral microwave hyperthermia. J Urol. 1991;145:305.
Baba S, Nakamura K, Tachibana M, et al. Transurethral microwave thermotherapy for management of benign prostatic hyperplasia: durability of response. Urology. 1996;47:664-671.
Bdesha AS, Schachter M, Sever P, et al. Radioligand-binding analysis of human prostatic alpha-1 adrenoreceptor density following transurethral microwave therapy. Br J Urol. 1996;78:886-892.
Berger A, Niescher M, Spranger R, et al. Transurethral microwave thermotherapy (TUMT) with the Targis System: a single-centre study on 78 patients with acute urinary retention and poor general health. Eur Urol. 2003;43:176-180.
Blomqvist P, Ekbom A, Carlsson P, et al. Benign prostatic hyperplasia in Sweden 1987 to 1994: changing patterns of treatment, changing patterns of cost. Urology. 1997;50:214-220.
Blute ML, Patterson DE, Segura JW, et al. Transurethral microwave thermotherapy versus sham treatment: a double-blind randomised study. J Endourol. 1996;10:565-573.
Blute ML, Tomera KM, Hellerstein DK, et al. Transurethral microwave thermotherapy for management of benign prostatic hyperplasia: results of the United States Prostatron Cooperative Study. J Urol. 1993;150:1591-1596.
Bolmsjo M, Wagrell L, Hallin A, et al. The heat is on—but how? A comparison of TUMT devices. Br J Urol. 1996;78:564-572.
Brehmer M. Morphological changes in prostatic adenomas after transurethral microwave thermotherapy. Br J Urol. 1997;80:123-127.
Brehmer M, Hilliges M, Kinn AC. Denervation of periurethral prostatic tissue by transurethral microwave thermotherapy. Scand J Urol Nephrol. 2000;34:42-45.
Brehmer M, Svensson I. Heat-induced apoptosis in human prostatic stromal cells. BJU Int. 2000;85:535-541.
Brehmer M, Wiksell H, Kinn AC. Sham treatment compared with 30 or 60 minutes of thermotherapy in benign prostatic hyperplasia: a randomised study. Br J Urol. 1999;84:292-296.
Carter S, Patel A, Reddy P, et al. Single-session transurethral microwave thermotherapy for the treatment of benign prostatic obstruction. J Endourol. 1991;5:137-144.
Dahlstrand C, Geirsson G, Fall M, et al. Transurethral microwave thermotherapy versus transurethral resection for symptomatic benign prostatic hyperplasia: preliminary results of a randomised study. Eur Urol. 1993;23:292-298.
Dahlstrand C, Walden M, Geirsson G, et al. Transurethral microwave thermotherapy versus transurethral resection for symptomatic benign prostatic obstruction: results of a prospective randomised study with 2 year follow-up. J Urol. 1997;158:120-125.
D’Ancona FC, Albers YH, Kiemeney LA, et al. Can histopathology predict outcome following high-energy transurethral microwave thermotherapy of the prostate? Results of a biopsy study. Prostate. 1999;40:28-36.
D’Ancona FC, Francisca EA, Witjes WP, et al. High-energy thermotherapy versus transurethral resection in the treatment of benign prostatic hyperplasia: results of a prospective randomised study with 1 year of follow-up. J Urol. 1997;158:120-125.
D’Ancona FC, Francisca EA, Witjes WP, et al. Transurethral resection of the prostate versus high-energy thermotherapy of the prostate in patients with benign prostatic hyperplasia: long-term results. Br J Urol. 1998;81:259-264.
David RD, Grunberger I, Shore N, Swierzewski SJ. Multicenter initial US experience with CoreTherm-monitored feedback transurethral microwave thermotherapy for individualized treatment of patients with symptomatic benign prostatic hyperplasia: a systematic review. J Endourol. 2004;18:682-685.
De La Rosette J, De Wildt M, Alvizatos G, et al. Transurethral microwave thermotherapy (TUMT) in benign prostatic hyperplasia: placebo versus TUMT. Urology. 1994;44:58-63.
De La Rosette J, De Wildt M, Höfner K, et al. High-energy thermotherapy in the treatment of benign prostatic hyperplasia: results of the European Benign Prostatic Hyperplasia Study Group. J Urol. 1996;156:97-102.
De La Rosette J, Francisca E, Kortmann B, et al. Clinical efficacy of a new 30-min algorithm for transurethral microwave therapy: initial results. BJU Int. 2000;86:47-51.
De La Rosette J, Tubaro A, Trucchi A, et al. Changes in pressure-flow parameters in patients treated with transurethral microwave thermotherapy. J Urol. 1995;154:1382-1385.
Devonec M, Berger N, Fendler JP, et al. Thermoregulation during transurethral microwave thermotherapy: experimental and clinical fundamentals. Eur Urol. 1993;23(Suppl.):63-68.
Devonec M, Berger N, Perrin P. Transurethral microwave heating of the prostate—or from hyperthermia to thermotherapy. J Endourol. 1991;5:129-135.
De Wildt M, Debruyne F, De La Rosette J. High-energy transurethral microwave thermotherapy: a thermoablative treatment for benign prostatic obstruction. Urology. 1996;48:416-423.
De Wildt M, Hubregtse M, Ogden C, et al. A 12-month study of the placebo effect in transurethral microwave thermotherapy. Br J Urol. 1996;77:221-227.
Djavan B, Seitz C, Ghawidel K, et al. High-energy transurethral microwave thermotherapy in patients with acute urinary retention due to benign prostatic hyperplasia. Urology. 1999;54:18-22.
Djavan B, Shariat S, Fakhari M, et al. Neoadjuvant and adjuvant alpha-blockade improves early results of high-energy transurethral microwave thermotherapy for lower urinary tract symptoms of benign prostatic hyperplasia: a randomized, prospective clinical trial. Urology. 1999;53:111-117.
Francisca EA, D’Ancona FC, Hendriks JC, et al. A randomised study comparing high-energy TUMT to TURP: quality-of-life results. Eur Urol. 2000;38:569-575.
Francisca EA, Keijzers GB, D’Ancona FC, et al. Lower energy thermotherapy in the treatment of benign prostatic hyperplasia: long-term follow-up results of a multicenter international study. World J Urol. 1999;17:279-284.
Francisca EA, Kortmann BB, Floratos DL, et al. Tolerability of 3.5 versus 2.5 high-energy transurethral microwave thermotherapy. Eur Urol. 2000;38:59-63.
Floratos DL, Sonke GS, Francisca EA, et al. High-energy microwave thermotherapy for the treatment of patients in urinary retention. J Urol. 2000;163:1457-1460.
Hallin A, Berlin T. Transurethral microwave thermotherapy for benign prostatic hyperplasia: clinical outcome after 4 years. J Urol. 1998;159:459-464.
Harada T, Etori K, Kumazaki T, et al. Microwave surgical treatment of diseases of the prostate. Urology. 1985;26:572-576.
Hoffman RM, MacDonald R, Monga M, Wilt TJ. Transurethral microwave thermotherapy vs transurethral resection for treating benign prostatic hyperplasia: a systematic review. BJU Int. 2004;94:1031-1036.
Höfner K, Tan H-K, Kramer A, et al. Changes in outflow obstruction in patients with benign prostatic hypertrophy (BPH) after transurethral microwave therapy (TUMT). Neurourol Urodyn. 1993;12:376.
Homma Y, Aso Y. Transurethral microwave thermotherapy for benign prostatic hyperplasia: a 2-year follow-up study. J Endourol. 1993;7:261-265.
Javlé P, Blair M, Palmer M, et al. The role of an advanced thermotherapy device in prostatic voiding dysfunction. Br J Urol. 1996;78:391-397.
Kaplan SA, Shabsigh R, Soldo K, et al. Prostatic and periprostatic interstitial temperature measurements in patients treated with transrectal thermal therapy (local intracavitary microwave hyperthermia). J Urol. 1992;147:1562-1565.
Keijzers GB, Francisca EA, D’Ancona FC, et al. Long-term results of lower energy transurethral microwave thermotherapy. J Urol. 1998;159:1966-1972.
Kellner DS, Armenakas NA, Brodherson M, et al. Efficacy of high-energy transurethral microwave therapy in alleviating medically refractory urinary retention due to benign prostatic hyperplasia. Urology. 2004;64:703-706.
Larson TR, Blute ML, Tri JL, et al. Contrasting heating patterns and efficacy of the Prostatron and Targis microwave antennae for thermal treatment of benign prostatic hyperplasia. Urology. 1998;51:908-915.
Larson TR, Bostwick DG, Corica A. Temperature-correlated histopathologic changes following microwave thermoablation of obstructive tissue in patients with benign prostatic hyperplasia. Urology. 1996;47:463-469.
Larson TR, Collins JM. An accurate technique for detailed prostatic interstitial temperature-mapping in patients receiving microwave thermal treatment. J Endourol. 1995;9:339-347.
Larson TR, Collins JM. Increased prostatic blood flow in response to microwave thermal treatment: Preliminary findings in two patients with benign prostatic hyperplasia. Urology. 1995;46:584-590.
Larson TR, Collins JM, Corica A. Detailed interstitial temperature mapping during treatment with a novel transurethral microwave thermoablation system in patients with benign prostatic hyperplasia. J Urol. 1998;159:258-264.
Leib Z, Rothern A, Lev A, et al. Histopathological observations in the canine prostate treated by local hyperthermia. Prostate. 1986;8:93-102.
Magin RL, Fridd CW, Bonfiglio TA, et al. Thermal destruction of the canine prostate by high intensity microwaves. J Surg Res. 1980;29:265-275.
Miller PD, Kastner C, Ramsey EW, Parsons K. Cooled thermotherapy for the treatment of benign prostatic hyperplasia: durability of results obtained with the Targis System. Urology. 2003;61:1160-1165.
Mulvin D, Creagh T, Kelly D, et al. Transurethral microwave therapy versus transurethral catheter therapy for benign prostatic hyperplasia. Eur Urol. 1994;26:6-9.
Nawrocki JD, Bell TJ, Lawrence WT, et al. A randomised controlled trial of transurethral microwave therapy. Br J Urol. 1997;79:389-393.
Nordenstam G, Aspelin P, Isberg B, et al. Effect of transurethral microwave thermotherapy: an evaluation with MR imaging. Acta Radiol. 1996;37:933-936.
Ogden CW, Reddy P, Johnson H, et al. Sham versus transurethral microwave thermotherapy in patients with symptoms of benign prostatic bladder outflow obstruction. Lancet. 1993;341:14-17.
Ohigashi T, Baba S, Ohki T, et al. Long-term effects of transurethral microwave thermotherapy. Int J Urol. 2002;9:141-145.
Osman YM, Larson TR, El-Diasty T, Ghoneim MA. Correlation between central zone perfusion defects on gadolinium-enhanced MRI and intraprostatic temperatures during transurethral microwave thermotherapy. J Endourol. 2000;14:761-766.
Perachino M, Bozzo W, Puppo P, et al. Does transurethral thermotherapy induce a long-term alpha blockade? Eur Urol. 1993;23:299-301.
Roehrborn C, Mynderse L, Partin A, et al. Intermediate results of a multi-center trial of a new generation cooled TUMT for BPH. Program and abstracts of the American Urological Association Annual Meeting; May 21–6, 2005; San Antonio, Texas. Abstract 1553.
Roehrborn CG, Krongrad A, McConnell JD. Temperature mapping in the canine prostate during transurethrally applied local microwave hyperthermia. Prostate. 1992;20:97.
Roehrborn CG, Preminger G, Newhall P, et al. Microwave thermotherapy for benign prostatic hyperplasia with the Dormier Urowave: results of a randomized, double blind, multicenter, sham-controlled study. Urology. 1998;51:19-28.
Servadio C, Leib Z, Lev A. Diseases of prostate treated by local microwave hyperthermia. Urology. 1987;30:97-99.
Thalmann GN, Mattei A, Treuthardt C, et al. Transurethral microwave therapy in 200 patients with a minimum follow-up of 2 years: urodynamic and clinical results. J Urol. 2002;167:2496-2501.
Trock BJ, Brotzman M, Utz WJ, et al. Long-term pooled analysis of multicenter studies of cooled thermotherapy for benign prostatic hyperplasia: results of three months through four years. Urology. 2004;63:716-721.
Tubaro A, Carter S, De La Rosette J, et al. The prediction of clinical outcome from transurethral microwave thermotherapy by pressure-flow analysis: a European multicenter study. J Urol. 1995;153:1526-1530.
Wheelahan J, Scott NA, Cartmill R, et al. Minimally invasive non-laser thermal techniques for prostatectomy: a systematic review. BJU Int. 2000;86:977-988.
Yerushalmi A, Fishelovitz Y, Singer D, et al. Localised deep microwave hyperthermia in the treatment of poor operative risk patients with benign prostatic hyperplasia. J Urol. 1985;133:873-876.
Zerbib M, Steg A, Conquy S, et al. Localised hyperthermia versus the sham procedure in obstructive benign hyperplasia of the prostate: a prospective randomised study. J Urol. 1992;147:1048-1052.
Aho TF, Gilling PJ, Kennett KM, et al. Holmium laser bladder neck incision versus holmium enucleation of the prostate as outpatient procedures for prostates less than 40 grams: a randomized trial. J Urol. 2005;174:210-214.
Anson K, Nawrocki J, Buckley J, et al. A multicenter randomised prospective study of endoscopic laser ablation versus transurethral resection of the prostate. Urology. 1995;43:305-310.
Arai Y, Aoki Y, Okubo K, et al. Impact of interventional therapy for benign prostatic hyperplasia on quality of life and sexual function: a prospective study. J Urol. 2000;164:1206-1211.
Arai Y, Ishitoya H, Okubo K, et al. Transurethral interstitial laser coagulation for BPH: treatment outcome and quality of life. Br J Urol. 1996;78:93-98.
Bartsch G, Janetschek G, Watson G, et al. The development of an endoscope and of contact probes for transurethral laser surgery of the prostate. J Urol. 1994;151:333A.
Carter A, Sells H, Speakman M, et al. A prospective randomised controlled trial of hybrid laser treatment or transurethral resection of the prostate, with a 1-year follow-up. BJU Int. 1999;83:254-259.
Chatzopoulos C, Lorge FJ, Opsomer RJ, et al. Transurethral ultrasound-guided laser-induced prostatectomy: a critical evaluation. J Endourol. 1996;10:463-467.
Conn RL, Kursh ED, Williams JC, et al. One year outcomes of interstitial laser coagulation of the prostate in 100 men: a multicenter experience. J Urol. 1999;161:1513A.
Corvin S, Schneede P, Slakavara E, et al. Interstitial laser coagulation combined with minimal transurethral resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol. 2002;16:387-390.
Costello AJ, Bowsher WG, Bolton DM, et al. Laser ablation of the prostate in patients with benign prostatic hypertrophy. Br J Urol. 1992;69:603-608.
Costello AJ, Crowe MR. A single institution experience of reflecting laser fiber over 4 years. J Urol. 1994;152:229A.
Costello AJ, Shaffer BS, Crowe MR. Second generation delivery options for laser prostatic ablation. Urology. 1994;43:262-266.
Cowles RS, Kabalin JN, Childs S, et al. A prospective randomised comparison of transurethral resection to visual laser ablation of the prostate for the treatment of benign prostatic hyperplasia. Urology. 1995;46:155-158.
Cummings J, Parra RO, Bouiller JA, et al. Evaluation of fluid absorption during laser prostatectomy by breath ethanol techniques. J Urol. 1995;154:2080-2082.
Dennstedt JD, Razvi HA, Sales JC, et al. Preliminary experience with holmium:YAG laser in urology. J Endourol. 1995;9:255-258.
De La Rosette, Huschter R, Lopez M, et al. Interstitial laser coagulation in the treatment of benign prostatic hyperplasia using a diode-laser system with temperature feedback. Br J Urol. 1997;80:433-438.
Fitzpatrick JM. A critical evaluation of technological innovations in the treatment of symptomatic benign prostatic hyperplasia. Br J Urol. 1998;81(Suppl. 1):56-63.
Fitzpatrick JM. Will laser replace TURP for the treatment of benign prostatic hyperplasia? Lancet. 2000;356:357-358.
Fournier GRJr, Tewari A, Induhara R, et al. Nd:YAG laser transurethral evaporation of the prostate (TUEP) for urinary retention. Lasers Surg Med. 1996;19:480-486.
Gilling P, Cass C, Cresswell M, et al. The use of the holmium laser in the treatment of benign prostatic hyperplasia. J Endourol. 1996;10:459-461.
Gilling P, Cass C, Malcolm A, et al. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995;9:151-153.
Gilling P, Mackey M, Cresswell M, et al. Holmium laser versus transurethral resection of the prostate: a randomised prospective trial with 1-year followup. J Urol. 1999;162:1640-1644.
Hai MA, Malek RS. Photoselective vaporization of the prostate: initial experience with a new 80w KTP laser for the treatment of benign prostatic hyperplasia. J Endourol. 2003;17:93-96.
Hoffman RM, MacDonald R, Wilt TJ. Laser prostatectomy for benign prostatic obstruction. Cochrane Database Syst Rev 2004;(1):CD001987.
Horninger W, Janetschek G, Watson G, et al. Are contact laser, interstitial laser, and transurethral ultrasound-guided laser-induced prostatectomy superior to transurethral prostatectomy? Prostate. 1997;31:255-263.
Issa M, Townsend M, Jiminez V, et al. A new technique of intraprostatic fibre placement to minimize thermal injury to prostatic urothelium during indigo interstitial thermal therapy. Urology. 1998;51:105-110.
James MJ, Harriss DR, Ceccherini A, et al. A urodynamic study of laser ablation of the prostate and a comparison of techniques. Br J Urol. 1995;76:179-183.
Johnson DE, Cromeens DM, Price RE. Transurethral incision of the prostate using the holmium:YAG laser. Lasers Surg Med. 1992;12:364-369.
Jung P, Mattelaer P, Wolff JM, et al. Visual laser ablation of the prostate: efficacy evaluated by urodynamics and compared to TURP. Eur Urol. 1996;30:418-423.
Kabalin J. Laser prostatectomy performed with a right angle firing neodymium:YAG laser fibre at 40 watts power setting. J Urol. 1993;150:95-99.
Kabalin J. Holmium:YAG laser prostatectomy: results of a US pilot study. J Endourol. 1996;10:453-457.
Kabalin J, Gill H, Bite G, et al. Comparative study of laser versus electrocautery prostatic resection: 18-month followup with complex urodynamic assessment. J Urol. 1995;153:94-98.
Keoghane S, Lawrence K, Gray A, et al. A double-blind randomised controlled trial and economic evaluation of transurethral resection vs contact laser vaporisation for benign prostatic enlargement: a 3-year follow-up. BJU Int. 2000;85:74-78.
Keoghane SR, Cranston DW, Lawrence KC, et al. The Oxford Laser Prostate Trial: a double-blind randomised controlled trial of contact vaporisation of the prostate against transurethral resection: preliminary results. Br J Urol. 1996;77:382-385.
Kingston TE, Nonnenmacher AK, Crowe H, et al. Further evaluation of transurethral laser ablation of the prostate in patients treated with anticoagulant therapy. Aust N Z J Surg. 1995;65:40-43.
Kumar SM. Photoselective vaporization of the prostate: a volume reduction analysis in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia and carcinoma of the prostate. J Urol. 2005;173:511-513.
Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electronically resection of the prostate: a randomized prospective trial in 200 patients. J Urol. 2004;172:1012-1016.
Kuntz RM, Lehrich K, Ahyai S. Transurethral holmium laser enucleation of the prostate compared with transvesical open prostatectomy: 18-month follow-up of a randomized trial. J Endourol. 2004;18:189-191.
Kuo RL, Kim SC, Lingeman JE, et al. Holmium laser enucleation of prostate (HoLEP): the Methodist Hospital experience with greater than 75 gram enucleations. J Urol. 2003;170:149-152.
Kursh ED, Concepcion R, Chan S, et al. Interstitial laser coagulation versus transurethral prostate resection for treating benign prostatic obstruction: a randomized trial with 2-year follow-up. Urology. 2003;61:573-578.
Larner TR, Agarwal D, Costello AJ. Day-case holmium laser enucleation of the prostate for gland volume of <60 mL: early experience. BJU Int. 2003;91:61-64.
Liedberg F, Adell L, Hagberg G, Palmqvist IB. Interstitial laser coagulation versus transurethral resection of the prostate for benign prostatic enlargement—a prospective randomized study. Scand J Urol Nephrol. 2003;37:494-497.
Mackey MJ, Chilton CP, Gilling PJ, et al. The results of holmium laser resection of the prostate. Br J Urol. 1998;81:518-519.
Matlaga BR, Kim SC, Kuo RL, et al. Holmium laser enucleation of the prostate for prostates of >125 mL. BJU Int. 2006;97:81-84.
McAllister WJ, Absalom MJ, Mir K, et al. Does endoscopic laser ablation of the prostate stand the test of time? Five-year results from a multicentre randomised controlled trial of endoscopic laser ablation against transurethral resection of the prostate. BJU Int. 2000;85:437-439.
McCullough DL. Transurethral ultrasound-guided laser-induced prostatectomy (TULIP) for the treatment of BPH. Semin Urol. 1994;26:193-196.
McCullough DL, Roth RA, Babayan RK, et al. Transurethral ultrasound-guided laser-induced prostatectomy: National Human Cooperative Study results. J Urol. 1993;150:1607-1611.
McNicholas TA, Hines J. Contact and interstitial laser treatment methods. In: Narayan P, editor. Benign prostatic hyperplasia. London: Churchill Livingstone; 2000:249-256.
McNicholas TA, Singh S. The use of lasers in benign prostatic enlargement. Curr Urol Rep. 2000;1:124-131.
McNicholas TA, Steger A, Bown S. Interstitial laser coagulation of the prostate: an experimental study. Br J Urol. 1993;71:439-444.
Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-centre, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004;172:1926-1929.
Muschter R, Hofstetter A. Interstitial laser therapy outcomes in benign prostatic hyperplasia. J Endourol. 1995;9:129-135.
Muschter R. Interstitial laser therapy of benign prostatic hyperplasia. In: Graham SD, Glenn JS, editors. Glenn’s urologic surgery. Philadelphia: Lippincott-Raven; 1999:1111-1118.
Narayan P, Tewari A, Aboseif S, et al. A randomised study comparing visual laser ablation and transurethral evaporation of prostate in the management of benign prostatic hyperplasia. J Urol. 1995;154:2083-2088.
Nau WHJr, Milam DF, Roseli RJ, et al. Principles of laser therapy. In: Narayan P, editor. Benign prostatic hyperplasia. London: Churchill Livingstone; 2000:221-229.
Nishizawa K, Kobayashi T, Watanabe J, Ogura K. Interstitial laser coagulation of the prostate for management of acute urinary retention. J Urol. 2003;170:879-882.
Norby B, Nielsen HV, Frimodt-Moller PC. Transurethral interstitial laser coagulation of the prostate and transurethral microwave thermotherapy vs transurethral resection or incision of the prostate: results of a randomized, controlled study in patients with symptomatic benign prostatic hyperplasia. BJU Int. 2002;90:853-862.
Norris JP, Norris DM, Lee RD, et al. Visual laser ablation of the prostate: clinical experience in 108 patients. J Urol. 1993;150:1612-1614.
Orovan W, Whelan J. Neodymium:YAG laser treatment of BPH using interstitial thermotherapy: a transurethral approach. J Urol. 1994;151:230A.
Pearcy R, Carter A, Sells H, et al. Long-term follow-up of hybrid KTP/Nd:YAG laser treatment of the prostate versus TURP: a prospective randomised trial, 18 month results. J Urol. 1999;161:1541A.
Press SM, Smith AD. Endoscope modifications for laser prostatectomy. J Endourol. 1995;9:101-106.
Reich O, Bachmann A, Schneede P, et al. Experimental comparison of high power (80w) potassium titanyl phosphate laser vaporization and transurethral resection of the prostate. J Urol. 2004;171:2502-2504.
Reich O, Bachmann A, Siebels M, et al. High power (80w) potassium-titanyl-phosphate laser vaporization of the prostate in 66 high risk patients. J Urol. 2005;173:158-160.
Sandhu JS, Ng C, Vanderbrink BA, et al. High-power potassium-titanyl-phosphate photoselective laser vaporization of prostate for treatment of benign prostatic hyperplasia in men with large prostates. Urology. 2004;64:1155-1159.
Schulze H, Martin W, Hoch P, et al. Transurethral ultrasound-guided laser-induced prostatectomy: clinical outcome and data analysis. Urology. 1995;45:241-247.
Sengor F, Kose O, Yocebas E, et al. A comparative study of laser ablation and transurethral electroresection for benign prostatic hyperplasia: results of a 6-month follow-up. Br J Urol. 1996;78:398-400.
Stein BS, Narayan P. Laser therapy: rationale, technique and results of vaporization. In: Narayan P, editor. Benign prostatic hyperplasia. London: Churchill Livingstone; 2000:231-238.
Sulser T, Reich D, Wyler S, et al. Photoselective KTP laser vaporization of the prostate: first experiences with 65 procedures. J Endourol. 2004;18:976-981.
Tan AH, Gilling PJ, Kennett KM, et al. Long-term results of high-power holmium laser vaporization (ablations) of the prostate. BJU Int. 2003;92:707-709.
Tan AH, Gilling PJ, Kennett KM, et al. A randomized trial comparing holmium laser enucleation of the prostate with transurethral resection of the prostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams). J Urol. 2003;170:1270-1274.
Te AE, Malloy TR, Stein BS, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicentre prospective trial. J Urol. 2004;172:1404-1408.
Terada N, Arai Y, Okubo K, et al. Interstitial laser coagulation for management of benign prostatic hyperplasia: long-term follow-up. Int J Urol. 2004;11:978-982.
Te Slaa E, De Wildt M, Rosier P, et al. Urodynamic assessment in the laser treatment of benign prostatic enlargement. Br J Urol. 1995;76:604-610.
Tooher R, Sutherland P, Costello A, et al. A systematic review of holmium laser prostatectomy for benign prostatic hyperplasia. J Urol. 2004;171:1773-1781.
Tuhkanen K, Heino A, Ala-Opas M. Contact laser prostatectomy compared to TURP in prostatic hyperplasia smaller than 4.0 ml: 6-month follow-up with complex urodynamic assessment. Scand J Urol Nephrol. 1999;33:31-34.
Watson G, Anson K, Janetschek G, et al. An in depth evaluation of contact laser vaporization of the prostate. J Urol. 1994;151:231A.
Webb DR, Kockelburgh R, Johnson WF. The Versapulse holmium surgical laser in clinical urology: a pilot study. Min Inv Ther. 1993;2:23-25.
Westenberg A, Gilling P, Kennett K, et al. Holmium laser resection of the prostate versus transurethral resection of the prostate: results of a randomized trial with 4-year minimum long-term follow-up. J Urol. 2004;172:616-619.
Wheelahan J, Scott NA, Cartmill R, et al. Minimally invasive laser techniques for prostatectomy: a systematic review. BJU Int. 2000;86:805-815.
Transurethral Resection of the Prostate
Ala-Opas MY, Aitola PT, Metsola TEJ. Evaluation of immediate and late results of transurethral resection of the prostate. Scand J Urol Nephrol. 1993;27:235-239.
Arrighi HM, Metter EJ, Guess HA, et al. Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. Urology. 1991;38(1 Suppl.):4-8.
Ball AJ, Feneley RCL, Abrams PH. The natural history of untreated prostatism. Br J Urol. 1981;53:613-616.
Ball AJ, Smith PJB. The long-term effects of prostatectomy: a uroflowmetric analysis. J Urol. 1982;128:538-540.
Barry MJ, Fowler FJJr, O’Leary MP, et al. The American Urological Association’s symptom index for benign prostatic hyperplasia. J Urol. 1992;148:1549-1557.
Barry MJ, Fowler FJJr, O’Leary MP, et al. Measuring disease-specific health states in men with benign prostatic hyperplasia. Med Care. 1995;33(Suppl):AS145-AS155.
Birch BR, Gelister JS, Parker CJ, et al. Transurethral resection of the prostate under sedation and local anaesthesia (sedoanalgesia): experience in 100 patients. Urology. 1991;38:113-118.
Botto H, Lebret T, Barre P, et al. Electrovaporization of the prostate with the Gyrus device. J Endourol. 2001;15:313-316.
Boyarsky S, Jones G, Paulson DF, et al. A new look at bladder neck obstruction by the Food and Drug Administration: guidelines for investigation of benign prostatic hypertrophy. Trans Am Assoc Genitourin Surg. 1977;68:28-32.
Bruskewitz RC, Iversen P, Madsen PO. Value of post-void residual urine determination in evaluation of prostatism. Urology. 1982;20:602-604.
Bruskewitz RC, Larsen EH, Madsen PO, et al. 3-Year follow up of urinary symptoms after transurethral resection of the prostate. J Urol. 1986;136:613-615.
Chute CG, Stephenson WP, Guess HA, et al. Benign prostatic hyperplasia: a population-based study. Eur Urol. 1991;20(Suppl. 2):11-17.
Concato J, Horwitz RI, Feinstein AR, et al. Problems of co-morbidity in mortality after prostatectomy. JAMA. 1992;267:1077-1086.
Dunsmuir WD, McFarlane JP, Tan A, et al. Gyrus bipolar electrovaporization vs transurethral resection of the prostate: a randomized prospective single-blind trial with 1 y follow-up. Prostate Cancer Prostatic Dis. 2003;6:182-186.
Emberton M, Neal DE, Black N, et al. The National Prostatectomy Audit: the clinical management of patients during hospital admission. Br J Urol. 1995;75:301-316.
Emberton M, Neal DE, Black N, et al. The effect of prostatectomy on symptom severity and quality of life. Br J Urol. 1996;77:233-247.
Estey EP, Mador DR, McPhee MS, et al. A review of 1486 transurethral resections of the prostate in a teaching hospital. Can J Surg. 1993;36:37-40.
Fitzpatrick JM, Mebust WK. Minimally invasive and endoscopic management of benign prostatic hyperplasia. In: Walsh PC, Retik AB, Vaughan EDJr, Wein AJ, editors. Campbell’s urology. 8th ed. Philadelphia: WB Saunders; 2002:1379-1422.
Fuglsig S, Aagaard J, Jonler M, et al. Survival after transurethral resection of the prostate: a 10-year follow-up. J Urol. 1994;151:637-639.
Glynn RJ, Campion EW, Bouchard GR, et al. The development of benign prostatic hyperplasia among volunteers in the Normative Aging Study. Am J Epidemiol. 1985;121:78-90.
Hagstrom RS. Studies on fluid absorption during transurethral prostatic resection. J Urol. 1955;73:852-859.
Hargreave TB, Heynes CF, Kendrick SW, et al. Mortality after transurethral and open prostatectomy in Scotland. Br J Urol. 1996;77:547-553.
Harrison RH, Boren JS, Robinson JR. Dilutional hyponatraemic shock: another concept of the transurethral prostatic resection reaction. J Urol. 1956;75:95-110.
Holman CD, Wisniewski ZS, Semmens JB, et al. Mortality and prostate cancer risk in 19,598 men after surgery for benign prostatic hyperplasia. BJU Int. 1999;84:37-42.
Holtgrewe HL, Valk WL. Factors influencing mortality and morbidity of transurethral prostatectomy: a study of 2,015 cases. J Urol. 1962;87:450-459.
Hopkins HH. Optical principles of the endoscope. In: Berci G, editor. Endoscopy. New York: Appleton-Century-Crofts; 1976:3-26.
Lee M, Cannon B, Sharifi R. Chart for preparation of dilutions of alpha-adrenergic agonists for intracavernous use in treatment of priapism. J Urol. 1995;153:1182-1183.
Lytton B, Emery JM, Harvard BM. The incidence of benign prostatic obstruction. J Urol. 1968;99:639-645.
Madsen PO, Iversen P. A point system for selecting operative candidates. In: Hinman FJr, editor. Benign prostatic hypertrophy. New York: Springer-Verlag; 1983:763-765.
Madsen PO, Naber KG. The importance of the pressure in the prostatic fossa and absorption of irrigating fluid during transurethral resection of the prostate. J Urol. 1973;109:446-452.
Malenka DJ, Roos N, Fisher ES, et al. Further study of the increased mortality following transurethral prostatectomy: a chart-based analysis. J Urol. 1990;144:224-227. discussion 228
Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. Eur Urol. 2009;56(5):798-809.
Matani Y, Mottrie AM, Stöckle M, et al. Transurethral prostatectomy: a long-term follow-up study of 106 patients over 80 years of age. Eur Urol. 1996;30:414-417.
McConnell JD, Barry MJ, et al. Benign prostatic hyperplasia: diagnosis and treatment. Clinical practice guideline no. 8. Rockville (MD): U.S. Department of Health and Human Services, Agency for Health Care Policy and Research, Public Health Service; 1994. p. 1–17
McGowan SW, Smith GFN. Anaesthesia for transurethral prostatectomy: a comparison of spinal intradural anaesthesia with two methods of general anaesthesia. Anaesthesia. 1980;35:847-853.
Mebust WK, Holtgrewe HL, Cockett ATK, et al. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of thirteen participating institutions evaluating 3,885 patients. J Urol. 1989;141:243-247.
Mebust WK, Roizo R, Schroeder F, et al. Correlations between pathology, clinical symptoms and the course of the disease. The International Consultation on Benign Prostatic Hyperplasia—Proceedings. Paris, 1991, p. 51–62.
Melchior J, Valk WL, Foret JD, et al. Transurethral resection of the prostate via perineal urethrostomy: complete analysis of 7 years of experience. J Urol. 1974;111:640-643.
Meyhoff HH, Nordling J. Long term results of transurethral and transvesical prostatectomy: a randomised study. Scand J Urol Nephrol. 1986;20:27-33.
Montorsi F, Guazzoni G, Bergamaschi F, et al. Long-term clinical reliability of transurethral and open prostatectomy for benign prostatic obstruction: a term of comparison for nonsurgical procedures. Eur Urol. 1993;23:262-266.
Naspro R, Bachmann A, Gilling P, et al. A review of the recent evidence (2006–2008) for 532-nm photoselective laser vaporisation and holmium laser enucleation of the prostate. Eur Urol. 2009;55:1345-1357.
Neal DE. The National Prostatectomy Audit. Br J Urol. 1997;79(Suppl. 2):69-75.
Nesbit RM. A history of transurethral prostatectomy. Rev Mex Urol. 1975;35:349-362.
Nielsen OS, Maigaard S, Frimodt-Moller N, et al. Prophylactic antibiotics in transurethral prostatectomy. J Urol. 1981;126:60-62.
Oester A, Madsen PO. Determination of absorption of irrigating fluid during transurethral resection of the prostate by means of radioisotopes. J Urol. 1969;102:714-719.
Patel A, Adshead JM. First clinical experience with new transurethral bipolar prostate electrosurgery resection system: controlled tissue ablation (coblation technology). J Endourol. 2004;18:959-964.
Perrin P, Barnes R, Hadley H, et al. Forty years of transurethral prostatic resections. J Urol. 1976;116:757-758.
Plentka L, Loghem JV, Hahn E, et al. Comorbidities and perioperative complications among patients with surgically treated benign prostatic hyperplasia. Urology. 1991;38(Suppl. 1):43-48.
Roos NP, Wennberg JE, Malenka DJ, et al. Mortality and reoperation after open and transurethral resection of the prostate for benign prostatic hyperplasia. N Engl J Med. 1989;320:1120-1123.
Singh H, Desai MR, Shrivastav P, Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. J Endourol. 2005;19:333-338.
Sinha B, Haikel G, Lange PH, et al. Transurethral resection of the prostate with local anaesthesia in 100 patients. J Urol. 1986;135:719-721.
Stalberg HP, Hahn RG, Jones AW. Ethanol monitoring of transurethral prostatic resection during inhaled anesthesia. Anesth Analg. 1992;75:983-988.
Wasson JH, Reda DJ, Bruskewitz RC, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. N Engl J Med. 1995;332:75-79.
Transurethral Vaporization of the Prostate
Cabelin M, Te AE, Kaplan SA. Transurethral vaporization of the prostate: current techniques. Curr Urol Rep. 2000;1:116-123.
De Sautel MG, Burney TL, Diaz PA, et al. Outcome of VaporTrode transurethral vaporization of the prostate using pressure-flow urodynamic criteria. Urology. 1998;51:1013-1017.
Galluci M, Puppo P, Fortunato P, et al. Transurethral electrovaporization of the prostate with the VaporTrode VE-B: preliminary results. Eur Urol. 1996;29:450-455.
Hammadeh MY, Fowlis GA, Singh M, et al. Transurethral electrovaporization of the prostate—a possible alternative to transurethral resection: a one-year follow-up of a prospective randomised trial. Br J Urol. 1998;81:721-725.
Juma S. Transurethral fulguration of the prostate with the roller ball. Urology. 1996;47:53-58.
Kaplan SA, Laor E, Fatal M, Te AE. Transurethral resection of the prostate versus transurethral electrovaporization of the prostate: a blinded, prospective comparative study with 1-year followup. J Urol. 1998;159:454-458.
Kaplan SA, Te AE. Transurethral electrovaporization of the prostate (TVP): a novel method for treating men with benign prostatic hyperplasia. Urology. 1995;45:566-573.
Kaplan SA, Te AE. A comparative study of transurethral resection of the prostate using a modified electro-vaporising loop and transurethral laser vaporization of the prostate. J Urol. 1995;154:1785-1790.
Küpeli S, Soygür T, Yilmaz E, Budak M. Combined transurethral resection and vaporization of the prostate using newly designed electrode: a promising treatment alternative for benign prostatic hyperplasia. J Endourol. 1999;13:225-228.
Matos Ferreira A, Varregoso J. Electrovaporization of the prostate in patients with benign prostatic enlargement. Br J Urol. 1997;80:575-578.
McAllister WJ, Karim O, Plail RD, et al. A prospective randomised multicentre trial of transurethral electrovaporization of the prostate against TURP: preliminary results. Br J Urol. 1998;81(Suppl. 4):22.
McAllister WJ, Karim O, Plail RD, et al. Transurethral electrovaporisation of the prostate: is it any better than conventional transurethral resection of the prostate? BJU Int. 2003;91:211-214.
Mebust WK, Damico C. Prostatic desiccation: a preliminary report of laboratory and clinical experience. J Urol. 1972;108:601-603.
Mebust WK, White TG. Immune reactions following desiccation surgery of the canine prostate. Invest Urol. 1977;14:427-430.
Narayan P, Tewari A, Crocker B, et al. Factors affecting size and configuration of electrovaporization lesions in the prostate. Urology. 1996;47:679-688.
Okada T, Terai A, Terachi T, et al. Transurethral electrovaporization of the prostate: preliminary clinical results with pressure-flow analysis. Int J Urol. 1998;5:55-59.
Patel A, Fuchs GJ, Gutierrez-Aceves J, et al. Prostate heating patterns comparing electrosurgical transurethral resection and vaporization: a prospective randomised study. J Urol. 1997;157:169-172.
Patel A, Fuchs GJ, Gutierrez-Aceves J, et al. Transurethral electrovaporization and vapour-resection of the prostate: an appraisal of possible electrosurgical alternatives to regular loop resection. BJU Int. 2000;85:202-210.
Permutter AP, Schulsinger DA. The “Wedge” resection device for electrosurgical transurethral prostatectomy. J Endourol. 1998;12:75-79.
Perlmutter AP, Vallencien G. Thick loop transurethral resection of the prostate. Eur Urol. 1999;35:161-165.
Poulakis V, Dahm P, Witzsch U, et al. Transurethral electrovaporization vs transurethral resection for symptomatic prostatic obstruction: a meta-analysis. BJU Int. 2004;94:89-95.
Reis RB, Te AE, Cologna AJ, et al. Interstitial thermometry in men undergoing electrovaporization of the prostate. J Endourol. 1999;13:53-56.
Shokeir AA, Al Sisi H, Farage YM, et al. Transurethral prostatectomy: a prospective randomised study of conventional resection and electrovaporization in benign prostatic hyperplasia. Br J Urol. 1997;80:570-574.
Stewart SC, Benjamin D, Ruckle H, et al. Electrovaporization of the prostate: new technique for treatment of symptomatic benign prostatic hyperplasia. J Endourol. 1995;9:413-416.
Talic RF. Transurethral electrovaporization-resection of the prostate using the “wing” cutting electrode: preliminary results of safety and efficacy in the treatment of men with prostatic outflow obstruction. Urology. 1999;53:106-110.
Talic RF, El Tiraifi A, El Faqih SR, et al. Prospective randomised study of transurethral vaporization resection of the prostate using the thick loop and transurethral prostatectomy. Urology. 2000;55:886-890.
Van Swol CF, Van Vliet RJ, Verdaasdonk RM, et al. Electrovaporization as a treatment modality for transurethral resection of the prostate: influence of generator type. Urology. 1999;53:317-321.
Transurethral Incision of the Prostate
Debruyne FMJ, Djavan B, De la Rosette J, et al. Interventional therapy of benign prostatic hyperplasia. In: Chatelain C, Denis L, Foo KT, et al, editors. Fifth international consultation on benign prostatic hyperplasia. Plymouth, UK: Health Publications; 2001:399-421.
Dorflinger T, Jensen FS, Krarup T, et al. Transurethral prostatectomy compared with incision of the prostate in the treatment of prostatism caused by small benign glands. Scand J Urol Nephrol. 1992;26:333-338.
Edwards LE, Bucknall TE, Pittam MR, et al. Transurethral resection of the prostate and bladder neck incision: c review of 700 cases. Br J Urol. 1985;57:168-171.
Edwards LE, Powell C. An objective comparison of transurethral resection and bladder neck incision in the treatment of prostatic hypertrophy. J Urol. 1982;128:325-327.
Hedlund H, Ek A. Ejaculation and sexual function after endoscopic bladder neck incision. Br J Urol. 1985;57:164-167.
Katz PG, Greenstein A, Ratliff JE, et al. Transurethral incision of the bladder neck and prostate. J Urol. 1990;144:694-696.
Kelly MJ, Roskamp D, Leach GE. Transurethral incision of the prostate: a preoperative and postoperative analysis of symptoms and urodynamic findings. J Urol. 1989;142:1507-1509.
McConnell JD, Barry MJ, et al. Benign prostatic hyperplasia: diagnosis and treatment. Clinical practice guideline no. 8. Rockville (MD): U.S. Department of Health and Human Services, Agency for Health Care Policy and Research, Public Health Service; 1994. p. 1–17
Miller J, Edyvane KA, Sinclair GR, et al. A comparison of bladder neck incision and transurethral prostatic resection. Aust N Z J Surg. 1992;62:116-122.
Orandi A. Transurethral incision of the prostate. J Urol. 1973;110:229-231.
Orandi A. Transurethral incision of prostate (TUIP): 646 cases in 15 years—a chronological appraisal. Br J Urol. 1985;57:703-707.
Riehman M, Knes JM, Heisey D, et al. Transurethral resection versus incision of the prostate: a randomised, prospective study. Urology. 1995;45:768-775.
Sirls LT, Ganabathi K, Zimmern PE, et al. Transurethral incision versus transurethral resection of the prostate: an objective and subjective evaluation of long-term efficacy. J Urol. 1993;150:1615-1621.
Soonawalla PF, Pardanini DS. Transurethral incision versus transurethral resection of the prostate. a subjective and objective analysis. Br J Urol. 1992;79:174-177.
Turner-Warwick R. A urodynamic review of bladder outlet obstruction in the male and its clinical implications. Urol Clin North Am. 1979;6:171-192.
Angell JC. Treatment of benign prostatic hyperplasia by phenol injection. Br J Urol. 1969;41:735-738.
Breda G, Isgro A. Treatment of benign prostatic hyperplasia with water-induced thermotherapy: experience of a single institution. J Endourol. 2002;16:123-126.
Corica AG, Qian J, Ma J, et al. Fast liquid ablation system for prostatic hyperplasia: a new minimally invasive thermal treatment. J Urol. 2003;170:874-878.
Corica FA, Cheng L, Ramnani D, et al. Transurethral hot-water balloon thermoablation for benign prostatic hyperplasia: patient tolerance and pathologic findings. Urology. 2000;56:76-80.
Ditrolio J, Patel P, Watson RA, Irwin RJ. Chemo-ablation of the prostate with dehydrated alcohol for the treatment of prostatic obstruction. J Urol. 2002;167:2100-2103.
Goya N, Ishikawa N, Ito F, et al. Ethanol injection therapy of the prostate for benign prostatic hyperplasia: preliminary report on application of a new technique. J Urol. 1999;162:383-386.
Grise P, Plante M, Palmer J, et al. Evaluation of the transurethral ethanol ablation of the prostate (TEAP) for symptomatic benign prostatic hyperplasia (BPH): a European multi-center evaluation. Eur Urol. 2004;46:496-501.
Michel MS, Köhrman KU, Weber A, et al. Rotoresect: a new technique for resection of the prostate. Experimental phase. J Endourol. 1996;10:473-478.
Michel MS, Knoll T, Trojan L, et al. Rotoresect for bloodless transurethral resection of the prostate: a 4-year follow-up. BJU Int. 2003;91:65-68.
Muschter R. Conductive heat: hot water-induced thermotherapy for ablation of prostatic tissue. J Endourol. 2003;17:609-616.
Muschter R, Schorsch I, Danielli L, et al. Transurethral water-induced thermotherapy for the treatment of benign prostatic hyperplasia: a prospective multicenter trial. J Endourol. 2000;164:1565-1569.
Plante MK, Gross AL, Kliment J, et al. Intraprostatic ethanol chemoablation via transurethral and transperineal injection. BJU Int. 2003;91:94-98.
Talwar GL, Pande SK. Injection treatment of enlarged prostate. Br J Surg. 1966;53:421-427.
Wadie BS, Shehab El-Dein AB, Mohamed AM, et al. Short-term results of rotoresection: a prospective study on safety and efficacy. BJU Int. 2003;92:710-712.
Wadie BS, Shehab El-Dein AB, Mosbah A, et al. A 2-year follow-up after rotoresection of the prostate: a prospective study. BJU Int. 2005;96:828-830.