CHAPTER 64 SUPPLEMENT A Periodontal Microsurgery
Microsurgery is defined as surgery performed under magnification of 10× or more which is only possible using a surgical microscope.6 The hallmarks of microsurgery are increased visual acuity and improved manual dexterity.18 When visibility is increased tenfold, motor movement precision is increased from 1 mm to 10 µm.3 This is the approximate size of an epithelial cell.12 Large incisions for visibility are therefore not necessary. Small surgical instruments are used to advantage in the reduced surgical field (Supplement A Figure 64-1). This minimally invasive philosophy results in less injury, diminished morbidity, and rapid healing.10,13 Central to this approach are sharp microsurgical blades to create incisions at a virtual cellular level (Supplement A Figure 64-2). These incisions are closed with meticulous apposition to eliminate wound edge gaps and dislocations, allowing healing by primary intention to begin within hours of microsurgical closure. This circumvents the need for an extensive secondary mitotic stage of wound healing to bridge wound gaps and fill surgical voids.
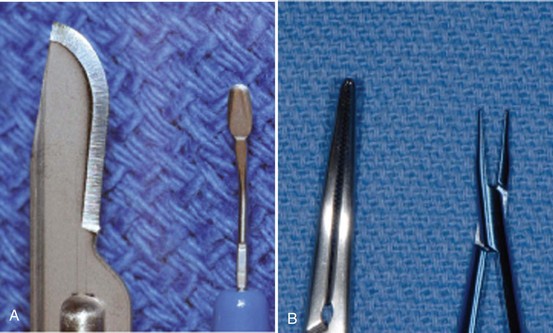
Supplement A Figure 64-1 Side-by-side dimensional comparison of commonly used conventional versus microsurgical instruments. A, #15 blade versus ophthalmic blade. B, Working tip of conventional needleholder versus McGregor microsuturing forceps.
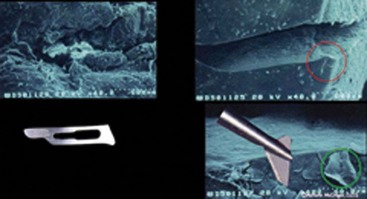
Supplement A Figure 64-2 Scanning electron microscopy (SEM) comparison of incisions made with a #15 blade (upper left image) and an ophthalmic microsurgical “feather” blade (upper and lower right images). The red circle in the top right image shows the area magnified in the bottom right image. The green circle shows the disruption of only one epithelial cell.
(SEM photographs courtesy Masana Susuki, DDS, Tokyo, Japan.)
The Surgical Microscope
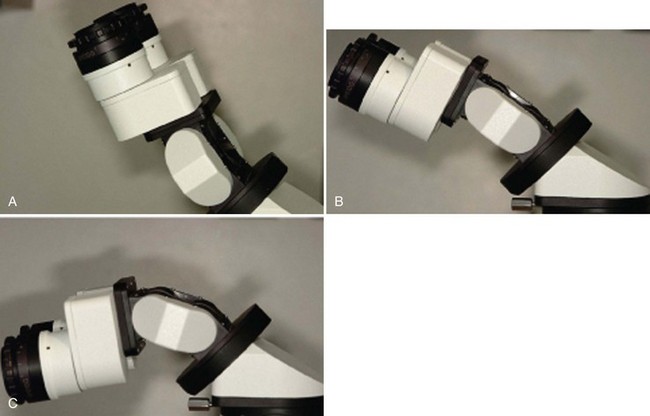
The surgical microscope offers greater versatility than dental loupes, by providing a range of magnification with superior optical performance. A surgical microscope can last an entire career, making its long-term expense practical. Proficient use of the microscope requires training and practice. Surgical microscopes designed for dentistry employ Galilean optics, which have binocular eyepieces joined by offset prisms, to establish a parallel optical axis and permit stereoscopic vision without eye convergence or eyestrain. An additional binocular eyepiece can aid the microsurgical assistant (Supplement A Figure 64-3).

Supplement A Figure 64-3 Accessory binocular module allows the assistant to better support the operator during the procedure.
Surgical microscopes have coated achromatic lenses and high optical resolution, as well as a rotating magnification element that allows the microsurgeon to easily change magnification to a value appropriate for the surgical task at hand (Supplement A Figure 64-4). Because the optical elements of surgical microscopes are more advanced than those in loupes, depth-of-focus and field-of-view characteristics are greatly enhanced. Surgical microscopes have objective lenses with various working distances. A useful range in dentistry is 250 to 350 mm. For practical use, a surgical microscope must have both maneuverability and stability. Mountings are available for the ceiling, wall, or floor. Adjustable inclining eyepieces enhance postural flexibility for various procedures (Supplement A Figure 64-5). This maneuverability provides visual access to every area of the mouth and is an important factor in choosing to use a surgical microscope.

Supplement A Figure 64-4 Rotating magnification element with field of view ranging from full mouth to approximately 3 cm when using a 250-mm objective lens.
Illumination of the microsurgical field is also an important consideration. Dentists are accustomed to working with lateral illumination from side-mounted dental lights or headlamps. Fiberoptic coaxial illumination is a major advantage because it focuses light parallel to the microscope’s optical axis, which eliminates shadows. Surgeons can visualize the deepest reaches of the oral cavity, including subgingival pockets and angular bony defects. Definitive visualization of root surface to detect deposits and irregularities is possible. Surgeons can view anatomy to make clinical decisions based on accurate assessment of pathology rather than blind, educated guesses.
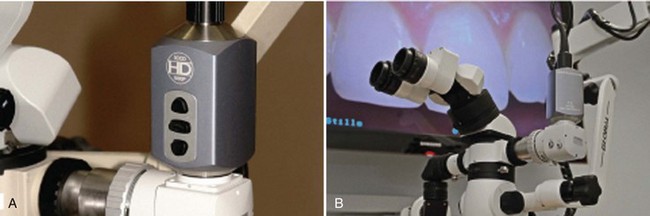
Documentation is important for patient and professional education and for dental-legal reasons. The surgical operating microscope is an ideal platform for documenting periodontal pathology and clinical procedures. Digital images can be captured using a beam splitter and camera attachment. A foot-control switch permits a surgeon to record, as the procedure unfolds, without interrupting surgery. These images represent the surgical field exactly as the surgeon sees it, as opposed to a camera view over the surgeon’s shoulder. High-definition (HD) video cameras capture both still and video images simultaneously to permit documentation of periodontal procedures for educational purposes (Supplement A Figure 64-6).
Philosophy of Periodontal Microsurgery
Microsurgery is a philosophy that embraces three core values. The first is enhanced motor skill for better surgical performance. This is accomplished through improved visual acuity and the use of a precise hand grip to increase accuracy and reduce tremor (Supplement A Figure 64-7). The second is minimal tissue trauma, which is accomplished through smaller incisions and reduced surgical fields (Supplement A Figure 64-8). The third value is primary passive wound closure.19 This is accomplished by microsuturing to eliminate gaps and dead spaces at the wound edge (Supplement A Figure 64-9). Advanced periodontics has an increasing need for clinical procedures that require intricate surgical skills. Regenerative procedures, periodontal plastic surgery, and dental implants are but a few of the surgical prodecures that demand clinical performance that frequently challenge the skills of periodontal surgeons beyond the range of possiblity with ordinary vision. Microsurgery establishes a minimal invasive surgical approach to periodontics exemplified by fewer vertical incisions and smaller surgical sites. Every field of microsurgery has noted the extent to which reduced incision size and less retraction directly relates to reduced postoperative morbidity and rapid healing2 (Supplement A Figure 64-10).
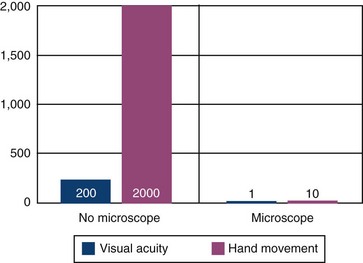
Supplement A Figure 64-7 Chart showing the correlation between enhanced visual acuity through magnification and dramatic reduction in minimal hand movement.17
Advantages of Microsurgery
Periodontal microsurgery raises the treatment bar in many ways. Surgical decision making is enhanced because the quality and quantity of visual data reaching the cerebral cortex is increased by a square of the magnification level. Ergonomic and body posture advantages also occur when using the surgical microscope1 (Supplement A Figure 64-11). Issues, such as neuromuscular fatigue and occupational skeletal pathology, are reduced. Sitting comfort, good body posture, arm support, and controlled breathing are inherent to proper microscope use. Motor skills are enhanced through instruments designed for a precision grip of the hand. Titanium instruments are used for strength and lightness and are made with round handles to permit precise rotation (Supplement A Figure 64-12). This reduces hand fatigue and tremor for precise surgical movement. Ergonomic benefit may be one of the most significant aspects of microscope use in periodontics.

Supplement A Figure 64-11 Muscle strain and potential career-ending injuries can be prevented through a more ergonomic position facilitated by the proper use of a microscope.
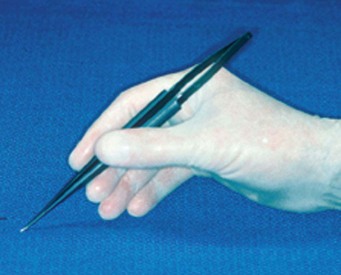
Supplement A Figure 64-12 Rounded, titanium microsurgical instruments, ideally 9 mm in diameter, reduce muscle fatigue and facilitate precise, rotational hand movements.
An important aspect of periodontal microsurgery is technical improvement in surgical performance. Higher skill levels have been shown in many surgical disciplines and can be fully appreciated when a surgeon tries his or her hand under the microscope. Viewing surgery under the microscope impresses a surgeon with the coarseness of conventional surgical manipulation (Supplement A Figure 64-13). What appears to the unaided eye as gentle surgery is revealed, under the microscope, as gross crushing and tearing of delicate tissues. Periodontics has long advocated atraumatic surgery, but the limits of normal vision have made this goal unattainable.
Supplement A Figure 64-13 The coarseness of conventional periodontal surgery is readily apparent under microscopic magnification.
Proprioceptive guidance is of little value at the microsurgical level. Visual guidance is used for midcourse correction of scalpels and instruments to achieve the finest level of skill and dexterity.5,10 Incisions can be accurately mapped, flaps elevated with minimal damage, and wounds closed accurately without tension (Supplement A Figure 64-14). Periodontal microsurgery is a natural progression from conventional surgical principles to a surgical ethic in which the surgical microscope is employed for the most accurate and atraumatic handling of tissue (Supplement A Figure 64-15).

Supplement A Figure 64-14 Tension-free wound closure is one of the goals of a microsurgical approach.

Supplement A Figure 64-15 Atraumatic microsurgical tissue manipulation during a microsurgical crown-lengthening procedure.
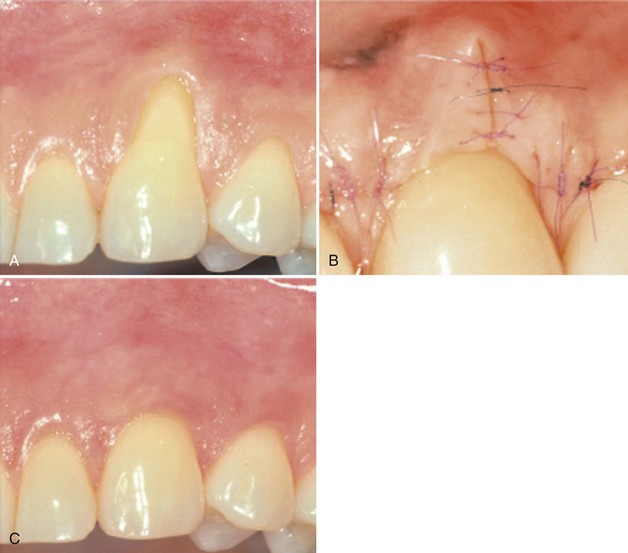
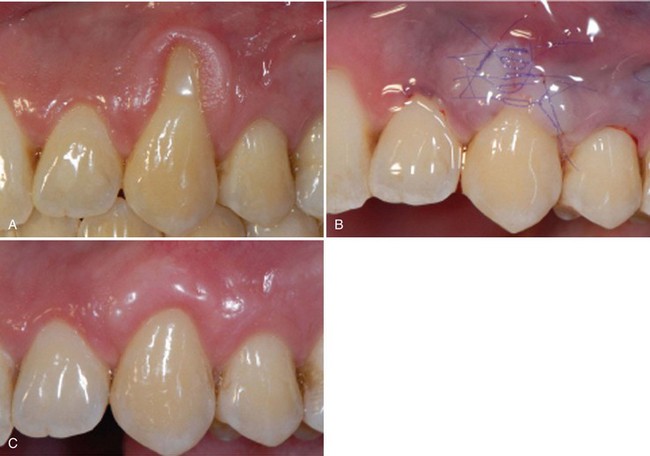
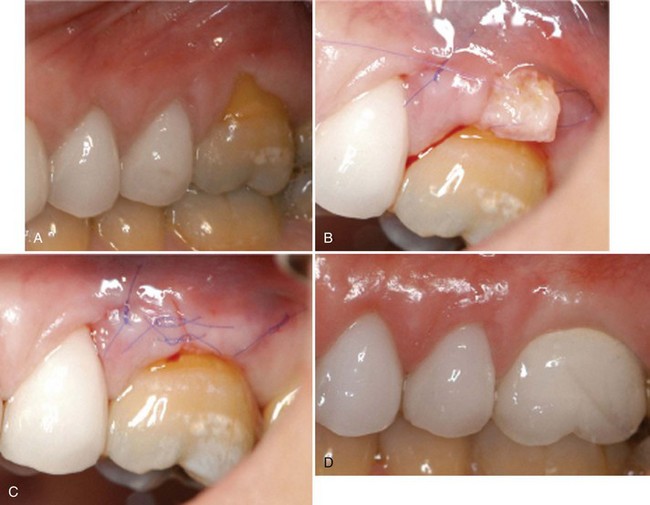
The end-point appearance of microsurgery is superior to that of conventional surgery. The difference is self-evident and often startling (Supplement A Figures 64-16 to 64-18). As much as judgment and knowledge play a role in surgery, in the end, surgery is a craft. Surgeons appreciate this, especially when microsurgery raises their work to levels of artistic expression. Personal gratification in performing better surgery leads to acceptance of periodontal microsurgery by surgeons motivated to improve the quality of their work. With training, the average periodontal microsurgeon can consistently produce better-crafted work than the most talented conventional surgeon (Supplement A Figure 64-19).

Supplement A Figure 64-16 A, Suppurating gingival fenestration. B, After careful root planing, a connective tissue graft (CTG) was carefully sutured under the envelope flap. C, Three weeks postoperative healing. D, One-year postoperative follow-up.

Supplement A Figure 64-17 Microsurgical correction of macrosurgical unsatisfactory outcome. A, Improper placement caused unesthetic result. B, Microsurgical grafting procedure. C, Final surgical result after new crowns fabrication.
Microsurgical Sutures
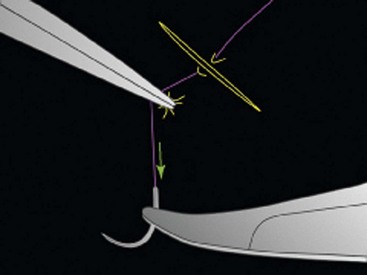
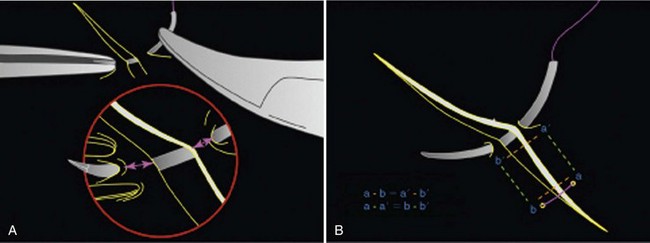
To achieve ideal microsurgical wound closure, a surgeon depends on how the incisions were planned and executed, how the surgery was performed, and the suturing technique. Selection of proper suture needles and materials is essential for successful microsurgical wound closure. The choice of suture and needle size is critical for atraumatic tissue passage. Suture material must maintain wound closure until healing is sufficiently advanced to withstand functional stress.
Sutures are classified according to structure as monofilament or braided, according to surface as coated or uncoated, and according to biologic properties as absorbable or nonabsorbable.2 The suture of choice in microsurgery is a monofilament suture material such as polypropylene or polydioxanone. These materials are bacteriostatic and noninflammatory, hold a knot extremely well, and are easily removed. The purpose of sutures is to provide initial wound support. They are chosen to appropriate wounds based on the fragility of the tissue. The smallest suture capable of supporting the wound produces the least tissue trauma and the least interruption of the blood supply.
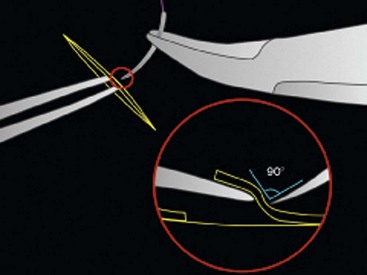
In periodontal microsurgery the suture size ranges from 6-0 (diameter of a human hair) to 9-0 (Supplement A Figure 64-20). The size and shape of the needle used is essential for the atraumatic passage of the suture. The needle diameter is ideally slightly larger than the suture size. Sutures used in microsurgery are swaged, making the needle and the suture continuous1 (Supplement A Figure 64-21). Penetration and passage of the needle depends on the angle of entry of needle point. Cutting needles pass through gingival tissue easily but can tear tissue. Tapered needles are less traumatic and less likely to tear tissue.
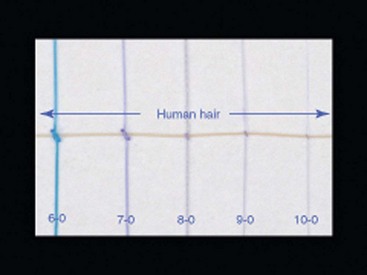
Supplement A Figure 64-20 Size comparison of microsutures in relation to the dimension of a human hair.
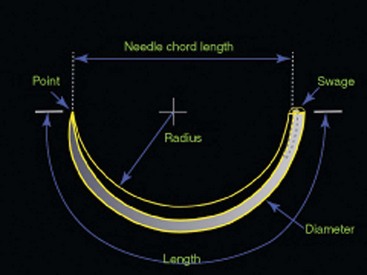
Supplement A Figure 64-21 Anatomy of a needle. Microsutures are hand-inserted into the laser-drilled swaged end of the needle, forming a seamless, contiguous unit.
An important component to needle design is the chord distance (see Supplement A Figure 64-21). The chord of a needle is the length of a line drawn between the cutting point and the swaged end.1 The radius of a needle is the arc of its circumference. A one-half ( ) round needle has an arc of 180 degrees. The chord determines the ease in passing a suture between adjacent teeth. The arc determines the bite size and angle of entry taken by the needle. These needle dimensions are important when selecting sutures for periodontal microsurgery.5
) round needle has an arc of 180 degrees. The chord determines the ease in passing a suture between adjacent teeth. The arc determines the bite size and angle of entry taken by the needle. These needle dimensions are important when selecting sutures for periodontal microsurgery.5
Esthetic Periodontal Microsurgery
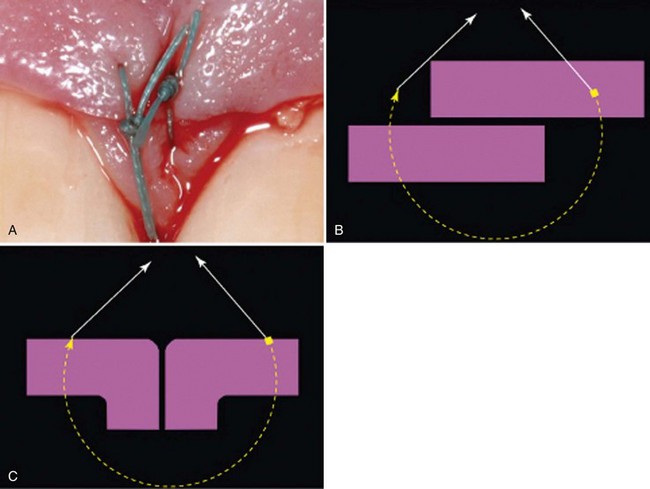
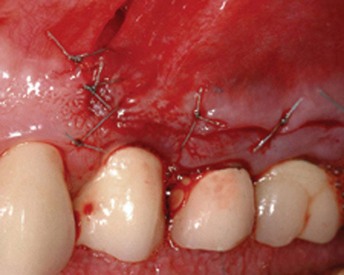
Esthetic periodontal microsurgery to reconstruct gingival tissue over denuded roots is routine and predictable utilizing subepithelial connective tissue grafting (Supplement A Figure 64-22). The color match, esthetic appearance, and lack of scarring of these grafts are ideal. Microsurgical closure of the palatal donor site allows healing by primary intention without a painful period of open granulation (Supplement A Figure 64-23). This greatly reduces postoperative pain.
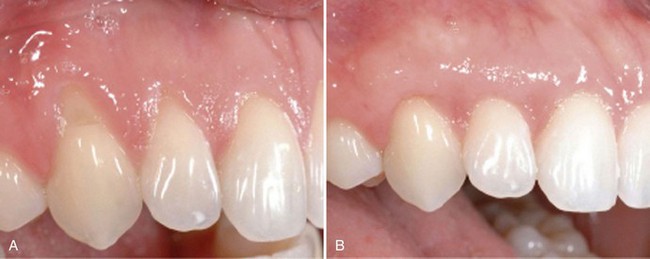
Supplement A Figure 64-22 Preoperative and postoperative view of recession area treated microsurgically with connective tissue graft.
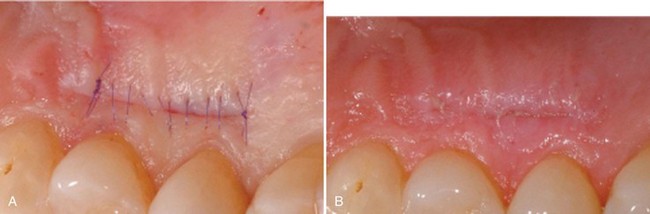
Supplement A Figure 64-23 A, Microsuturing of palatal donor site after harvesting connective tissue graft (CTG). B, One week postoperative healing of donor site.
To achieve optimal wound healing, three basic microsurgical principles are needed: (1) precision tailoring, (2) delicate tissue manipulation, and (3) passive primary wound closure.9
Precise Tailoring
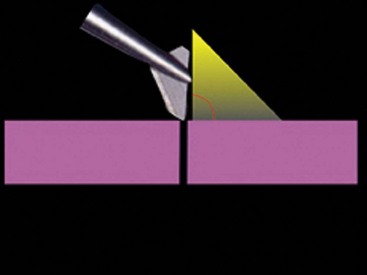
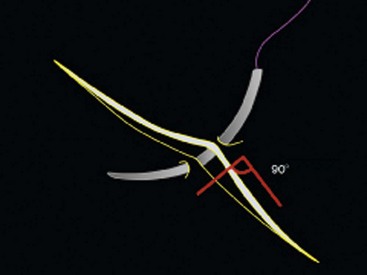
An important feature of microsurgery is the ability to create clean incisions. Design of incisions has significant impact on how the wound edges fit together. A fundamental principle of microsurgery is making incisions perpendicular to the tissue surface, creating “butt joint” edges that easily approximate for wound edge stability and maintain blood supply patency (Supplement A Figure 64-24).
Delicate Tissue Manipulation
The microsurgical philosophy is based on minimal invasiveness and minimal traumma. This premise extends to the manipulation gingival tissues during surgery.11 Gentle handling is necessary to reduce cellular injury and subsequent necrosis and inflammation. It is also necessary to maintain tissue hydration and color to maximize healing.8
Passive Primary Wound Closure
After precision tailoring and gentle tissue manipulation, the final and critical element of microsurgery is achieving passive primary wound closure. There is a specific geometry of the suturing required, with the following six well-defined components14:
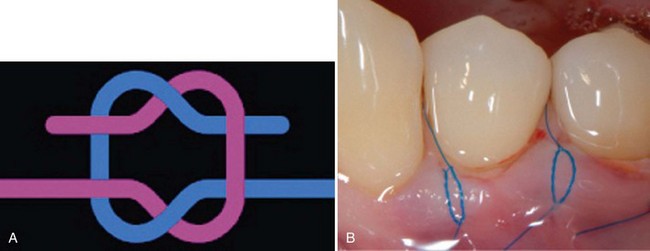
Microsurgical Knots
Two basic knots are employed in microsurgery. The square knot, or reef knot, is composed of two single loops thrown in opposite directions. The reef knot has more internal stability than any other knot. For this reason, it has been employed for centuries in nautical applications. It lies flat when tied well and is ideal for passive wound closure. As postsurgical edema occurs, the reef knot opens sightly then becomes self-locking. It maintains wound edge support without ligation caused by excessive tension (Supplement A Figure 64-32). If, in tying a knot, both loops are thrown in opposite directions, it becomes the granny knot and unties easily. The English surgeon’s knot is composed of two double loops thrown in opposite directions. The first double throw is less likely to loosen when performing the second throw, making it is easier to control tissue apposition. The English surgeon’s knot requires, however, a larger bite size. Both knots are tied with instruments.
Conclusion
As medicine and dentistry continue the pursuit of minimally invasive treatment, periodontal microsurgery and its principles will emerge as the methodology to meet both professional and public demand.15 The microscope provides a tremendous platform from which the microsurgical clinician can gather and observe detailed and precise amounts of information for the diagnosis and treatment of patients with skill and accuracy.7 Microsurgery leads to improved esthetics, rapid healing, reduced morbidity, and enhanced patient acceptance.4,16,17
1 Acland R. Practice manual for microvascular surgery. St Louis: Mosby; 1989.
2 Banowsky LH. Basic microvascular techniques and principles. Urology. 1985;23:495-503.
3 Barraquer JI. The history of microsurgery in ocular surgery. J Microsurg. 1980:1292.
4 Bunke H. The manual of microvascular surgery. San Francisco: Ralph K. Davies Medical Center Microsurgical Unit; 1975.
5 Chang T. Principles, techniques and applications in microsurgery. Hackensack, NJ: World Scientific; 1986.
6 Daniel RK. Through the looking glass: a history of microsurgery. N Engl J Med. 1979;300:1251-1258.
7 Leknius C, Geissberger M. The effect of magnification on the performance of fixed prosthodontic procedures. J Calif Dent Assoc. 1995;23(12):66-70.
8 McGregor M. Scientific session. Society of Microscope Enhanced Dentistry; 2008.
9 Olszewski W. Handbook of microsurgery. Boca Raton, FL: CRC Press; 1984.
10 Pecora G, et al. Operating microscope in endodontic surgery. Oral Surg, Oral Med Oral Pathol. 1993;75:751-759.
11 Riediger D, Ehrenfeld M, Microsurgical tissue transplantation, Quintessence, 1989
12 Serafin D. Microsurgery: past, present and future. Plast Reconstr Surg. 1980;66:781.
13 Shanelec D, Tibbetts LS. Periodontal microsurgery. Periodontal Insights. May 1994.
14 Shanelec DA, Watson N. The geometry of suturing. Microsurgery Training Institute Workshop; February, 1995.
15 Shanelec D, Tibbetts LS: Periodontal microsurgery: Continuing Education Course, American Academy of Periodontology Seventy-Eighth Annual Meeting, Nov.19, 1992, Orlando, FL.
16 Shanelec D, Tibbetts LS. Current status of periodontal microsurgery. Periodontics 2000. 1996;2:88-92.
17 Shanelec DA. Periodontal microsurgery. J Esthet Rest Dent. 2003;15(7):402-407.
18 Society of Microsurgical Specialists: Training curriculum position paper, 1999.
19 Urbaniak J. Microsurgical skills development. Chicago: American Academy of Orthopaedic Surgeons; 1985.