CHAPTER 50 SUPPLEMENT A Pathologic Tooth Migration
A Case Report*
Introduction
Pathologic tooth migration (PTM) is a common complication of moderate-to-severe periodontitis.1,2 The prevalence of PTM among periodontal patients has been reported to range from 30.03% to 55.8%. It occurs most frequently in the anterior region, but posterior teeth can also be affected. There are many types of pathologic tooth migration: diastema, extrusion, rotation, facial flaring, and drifting into edentulous spaces. Some of the important factors are poor periodontal support as the result of periodontal disease and the eventual loss of teeth, which changes the forces exerted on the remaining dentition. Later, if the missing teeth are not replaced, especially the first molars, the maxillary incisors are forced labially and laterally, which leads to the extrusion of the anterior teeth and the resulting diastema. Teeth mobility increases, and the second and third molars tilt mesially, which results in a reduced vertical dimension. This can also lead to an anterior overbite, and the mandibular incisors occlude near or on the palatal gingival margin of the maxillary anterior dentition.
PTM is caused by several factors, and one or more teeth can be involved. The treatment of most cases may require a multidisciplinary approach. In addition to periodontal therapy, orthodontic tooth movement can be beneficial. Replacing missing teeth with implants can stabilize the occlusion and reduce the trauma on the anterior dentition
Case Report
The following is a case that involves the multidisciplinary approach. A 56-year-old female patient was referred for periodontal treatment. The general dentist had diagnosed periodontal involvement with deep pocket formation and increased tooth mobility. He was willing to place a bridge to replace the missing teeth #29 and 30 and asked an assessment of the prognosis of tooth #31.
The patient’s complaints were as follows:
The patient has no reported medical problems. She does not use medications or drugs and is a nonsmoker.
The patient visited the dentist once a year for routine recall therapy. The most recent oral prophylaxis was performed 10 days before the first periodontal visit. The oral hygiene regimen included toothbrushing with a manual toothbrush, once a day. The patient was not using any other hygiene instruments or mouthwashes. She had a negative history of previous periodontal or orthodontic treatment.
Her overall oral hygiene status was poor with abundant bacterial plaque present, especially around the distal and lingual surfaces. There were no visible supragingival calculus deposits because the patient had a dental appointment a few days earlier. However, subgingival calculus was present throughout. The patient did not present any pathologic lesions and was not aware of oral malodor.
There were numerous restorations on the maxillary arch, but no areas of abrasions or erosions presented. The majority of the teeth were sensitive to thermal changes.
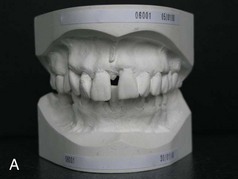
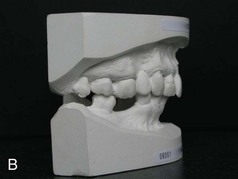
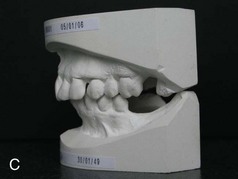
There were symptoms of PTM in the anterior region (Supplement A Figure 50-1). Diastemas were present between the maxillary incisors, as well as the mandibular dentition. The patient confirmed that in the past the position of her anterior teeth was normal and that her teeth “were all touching.” The maxillary and mandibular incisors displayed extrusion, rotation, and facial flaring. There was a pronounced anterior overbite.






Supplement A Figure 50-1 Different views of the oral cavity and the teeth. Note the different signs of pathologic tooth migration in the anterior region: diastemas, extrusion, tooth rotation, and flaring. A, Facial view. Note diastema between teeth #8 and 9. B, Lips retracted to display diastema. C, Palatal view of maxillary arch. D, Incisal view of mandibular arch. E, Right lateral view. Note overbite. F, Left lateral view.
In the posterior region, several teeth had been missing for many years. The most prominent missing teeth were the mandibular first molars. Only teeth #5 and 13 were replaced. The patient was able to function bilaterally even though the first molars were missing.
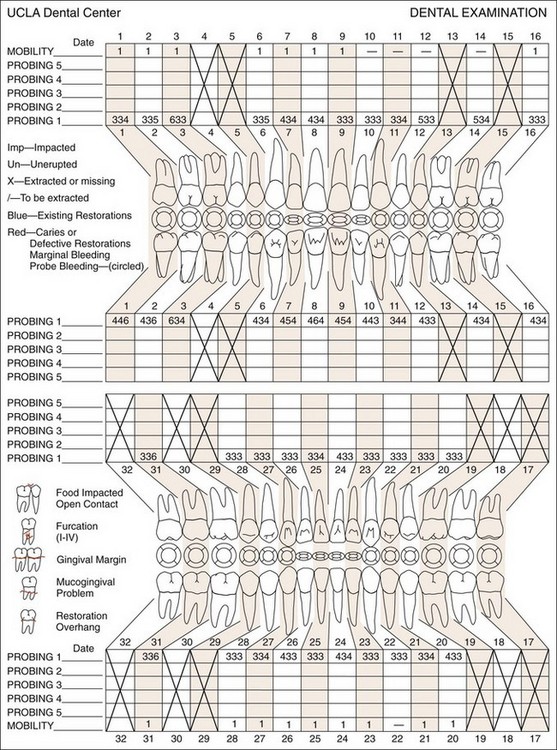
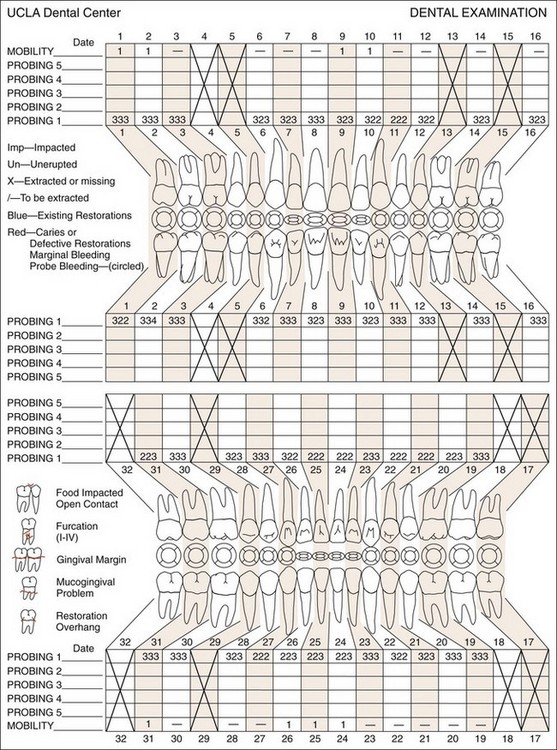
To assess the extent of the periodontal disease, a full periodontal examination was accomplished. The examination included pocket probing and evaluation of gingival recession and tooth mobility. Supplement A Figure 50-2 indicates the extensive periodontal involvement of the maxillary arch. Periodontal pockets that involved the interdental and lingual areas ranged from 4 to 6 mm. The majority of the anterior teeth presented recession that measured 2 mm. Increased mobility was noted for most teeth, especially tooth #31. Most of the furcations were Class I.
The panoramic radiograph (Supplement A Figure 50-3) presented generalized horizontal bone loss. Tooth #31 presented mesial angular bone defect and early furcation involvement. Several areas presented subgingival calculus.
A diagnostic model was indicated to evaluate the occlusal problem of the anterior area (Supplement A Figure 50-4). A diagnostic model can help to better assess the occlusion, tooth malposition, and inclination and to visualize the entire dentition and jaw.
The generalized bone loss and periodontal pockets are due to chronic periodontitis. The poor oral hygiene and the lack of maintenance therapy has been a major contribution to the periodontal involvement.
The failure to replace the missing teeth, especially the mandibular first molars, has also created an occlusal problem. Only one crown was used to replace both teeth #5 and 4 (Supplement A Figure 50-1, C), seriously reducing the occlusal surface in width. There were few stable occlusal contacts for many years. On the right side, only tooth #31 had occlusal contact, while only teeth #21 and 20 were contacting on the left side. Other occlusal contacts were sliding contacts, which are considered unstable.
The combination of chronic periodontitis and trauma from occlusion resulted in the pathologic migration in the anterior region. The reduced occlusal support caused by the missing mandibular first molars played an important role in the prognosis.
The prognosis of each tooth was determined individually, taking into account the patient’s age, disease severity, plaque control compliance, and cooperation, as well as the periodontal and occlusal factors.
In addition to tooth #31, all teeth displaying PTM were considered to be susceptible to further periodontal breakdown in the future with inadequate treatment. The prognosis of these teeth was determined as poor. The prognosis of the remaining teeth was considered fair because of the reduced influence of trauma from occlusion.
The orthodontist was asked to assess the possibility of orthodontic treatment in the anterior region to restore a normal occlusal plane and thus reestablish the contacts.
The patient received detailed explanation about periodontitis and the etiologic factors. She was initially surprised but became aware of the severity of the problem and the negative effects of this disease in the future.
The initial therapy was the treatment of the periodontal disease to reduce the inflammation. It was also realized that neglecting the occlusal problem would not help improve the prognosis of these teeth. The orthodontist concurred on the need for orthodontic therapy in the anterior region. The patient also insisted on saving teeth #1 and 16 despite the supereruption.
The following treatment plan was proposed after considering the patient’s complaints, wishes, and social situation:
Treatment
Periodontal Therapy
The nonsurgical phase of therapy consisted of scaling and root planing combined with the use of chlorhexidine rinses twice a day for 4 weeks. The patient’s compliance was excellent after the initial 4 weeks of therapy. The patient was instructed to brush at least twice a day, using a manual toothbrush in combination with interdental brushes and dental floss.
The patient was seen 3 months later for reevaluation, plaque control, and professional prophylaxis.
Reevaluation
The results of the nonsurgical phase were evaluated 6 months after the start of the initial therapy and resulted in a new periodontal status (Supplement A Figure 50-5). The patient’s motivation remained stable and consistent during the entire 6-month period.
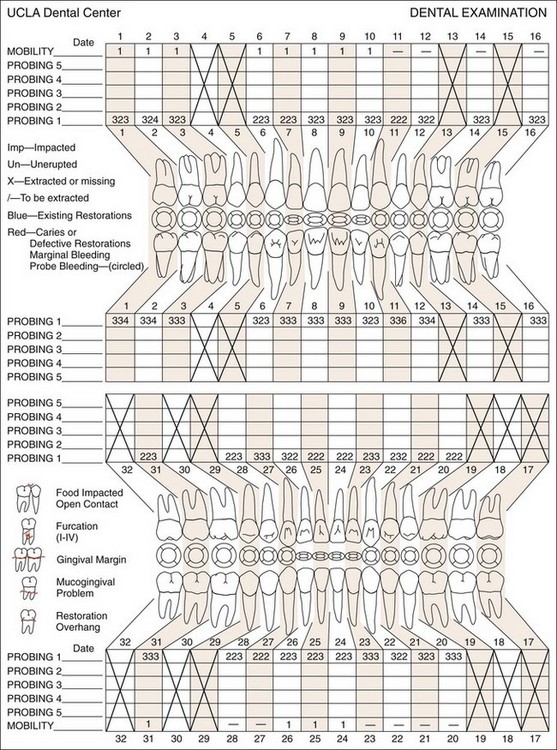
Supplement A Figure 50-5 A new chart obtained 6 months after the initial therapy reveals an important reduction in probing pocket depth. Changes in the recessions in the anterior region were noted.
There was significant generalized reduction of pocket depth. The remaining periodontal pockets around teeth #1, 2, and, 11 did not display bleeding on probing, as well as the other remaining sites. This favorable response to the nonsurgical phase permitted the initiation of orthodontic therapy.
Orthodontic Therapy
The orthodontic treatment plan was to correct the overbite, intrude the maxillary anterior teeth, and move these teeth back to their previous position. They will also be splinted from canine to canine. Full-arch fixed orthodontic appliances were placed in both the maxillary and the mandibular arches (Supplement A Figure 50-6). The total duration of the orthodontic therapy was 1 year and 3 months. Only light orthodontic forces were applied.






Supplement A Figure 50-6 Different views of the orthodontic appliance and implants placed in the mandibular and maxillary arches. Implants were placed at sites 19 and 30 a few months after the orthodontic treatment.
During the orthodontic therapy phase, the patient was seen every 3 months for periodontal evaluation by the periodontist. This was essential to maintain periodontal health, to monitor progress, and to diagnose any periodontal changes caused by orthodontic tooth movement. The orthodontist also reinforced oral hygiene at each orthodontic visit.
After the removal of the appliances, an orthodontic retention wire was placed from canine to canine in the maxilla and from tooth #21 to tooth #28 in the mandible (see Supplement A Figure 50-7, D).
Implant Therapy
Two implants were placed 4 months after the start of the orthodontic therapy to replace teeth #19 and 30. It was possible to start the implant therapy at this stage because the orthodontist had confirmed that teeth #20 and 28 would not be displaced. There was also a possibility of using the implants for orthodontic anchorage at a later stage if needed.
Restorative Phase
After removal of the orthodontic appliances, the dentist initiated the final restorations on the implants. The addition of two crowns at the first molar sites was very important to stabilize the occlusion. Consequently, tooth #31was stabilized mesially (Supplement A Figure 50-7).






Supplement A Figure 50-7 Different views after completion of the orthodontic and restorative therapy. A, The diastemas were closed, and the maxillary incisors were intruded, significantly improving the esthetic appearance. B, Note the resolution of most of the recessions, especially at teeth #8 and 9. C and D, A normal curve could be obtained after aligning all teeth from canine to canine. E and F, The overbite, the facial flaring, and rotation of some teeth were either reduced or resolved.
A panoramic radiograph was taken to determine the effect of the treatment on the jaw bone and the roots (Supplement A Figure 50-8).
Periodontal Maintenance
The periodontal maintenance consisted of 3-month recall visits that included hygiene control, probing, and prophylaxis. Regular maintenance care is essential in cases that utilize combined therapy to assure case stability.
One year after the termination of orthodontic treatment, a new periodontal recording and panoramic radiographs were obtained (Supplement A Figure 50-9 and Supplement A Figure 50-10) to evaluate the periodontal status. The result of these examinations presented a stable and healthy periodontal status.
Results and Discussion
The final result was considered satisfactory not only for the clinician but also for the patient (see Supplement A Movie 1). The patient was especially pleased with the esthetic outcome. The main goal of periodontal therapy was the preservation of the dentition and treatment of periodontal disease. This was achieved without surgical therapy. The cooperation of the patient played an important role in the outcome of treatment. The patient reported a significant improvement in mastication compared to her situation before the treatment. Sensitivity to thermal changes remained unchanged.
Supplement A Video 50-1: A slide presentation showing the results of the rehabilitation.
Periodontal therapy alone was not sufficient for the preservation of her dentition in the anterior region. The excessive PTM in this area could not be neglected. To improve the long-term stability of the dentition, both periodontal and orthodontic therapy was necessary. The facially flared teeth could be successfully aligned into a better position, which allowed for the splinting of the anterior dentition. Replacing the missing mandibular first molars was necessary to assure occlusal stability. Moreover, the periodontal maintenance during the orthodontic treatment was necessary to avoid any further bone loss.
Besides improving the prognosis of the anterior teeth, an esthetic improvement was noted at the gingival level. The recessions on the buccal side of the maxillary incisors were reduced significantly, and in some areas, it was completely eliminated. The closure of the diastema between teeth #8 and 9 allowed for the regeneration of the interdental papillae.