CHAPTER 22 Restoration of the Endodontically Treated Tooth
Special Features of Endodontically Treated Teeth
Endodontically treated teeth are structurally different from vital teeth; major changes include altered tissue physical characteristics, loss of tooth structure, and possibly also discoloration. Tissue modifications must therefore be analyzed at different levels, including tooth composition, dentin microstructure and tooth macrostructrure. It is fundamental to understand the implication of such features on tooth biomechanics, since they will largely influence restorative approach and means (Table 22-1). Numerous in vitro studies dealing with the complexity of the nonvital tooth substrate are reported in the literature; ultimately, in vivo trials describe the global effect of tissue qualitative and quantitative changes on restoration, long-term behavior, and survival.
TABLE 22-1 Specific Tissue Modifications and Possible Clinical Implications Following Loss of Vitality or Endodontic Treatment
| Alteration Level | Specific Changes | Possible Clinical Implication |
|---|---|---|
| Composition | ||
| Dentin structure | Increased tooth fragility | |
| Tooth macrostructure |
Compositional Changes in Nonvital Teeth and Influence of Endodontic Therapy
The loss of pulpal vitality is accompanied by a slight change in tooth moisture content. This loss of moisture (9%) is attributed to a change in free water but not in bonded water.69,73 This alteration was associated with a slight change in values for the Young modulus and proportional limit.79 However, no decrease in compressive and tensile strength values was associated with this change in water content.79 Only one study showed no difference in moisture content between vital and nonvital teeth.129 No difference in collagen cross-linkage was found between vital and nonvital dentin.147 There is no other evidence of chemical alteration due to the removal of pulpal tissue.
Sodium hypochlorite and chelators such as ethylenediamine tetra-acetic acid (EDTA), cyclohexane-1,2-diaminetetra-acetic acid (CDTA), ethylene glycol-bis-(β-amino-ethyl ether) N,N,N′,N′-tetra-acetic acid (EGTA), and calcium hydroxide (Ca[OH]2) commonly used for canal irrigation and disinfection interact with root dentin, either with mineral content (chelators) or organic substrate (sodium hypochlorite).82,115,122 Chelators mainly deplete calcium by complex formation and also affect noncollagenous proteins (NCP), leading to dentin erosion and softening.82,88,151 Sodium hypochlorite supposedly demonstrates a proteolytic action by extensive fragmentation of long peptide chains such as collagen.72 These alterations are likely to fragilize dentin and root structure and reduce adhesion to this substrate.
Dentin Structure and Properties in Nonvital and Endodontically Treated Teeth
It is important to know about the normal variations in dentin physical properties, which must be differentiated from alterations related to loss of vitality or endodontic treatment. For instance, dentin microhardness and elasticity actually varies between peritubular and intertubular dentin and depends on tooth location. Peritubular dentin presents an elasticity modulus of 29.8 GPa, whereas intertubular dentin ranges from 17.7 GPa (close to pulp) to 21.1 GPa (close to root surface).74,91,107 Most if not all the decrease in hardness on approaching the pulp can be attributed to changes in hardness of the intertubular dentin.90,91 Overall dentin elasticity modulus is considered to be in the range of 16.5 to 18.5 GPa16,33,52 even though variations can be observed due to the measuring methods.92,127,145
The changes in mineral density due to the variation in the number and diameter of tubules within the tooth may also explain variations in the properties of dentin. It was shown that dentin hardness values are inversely related to dentin tubule density.130 Ultra microindentation measurements also demonstrated significantly higher values for hardness and elasticity modulus when forces were parallel to the tubules rather than perpendicular.139 Differences in maximum strength and compressive strength were also found to vary according to tubule orientation.127 The ultimate tensile strength (UTS) of human dentin is lowest when the tensile force is parallel to tubule orientation, showing the influence of dentin microstructure and anisotropy of the tissue.99 No difference was found in the Young modulus of aged, transparent dentin (also called sclerotic) and normal dentin,20,93,175 but the mineral concentration significantly increases and crystallite size is slightly smaller in transparent dentin, in relation with closure of the tubule lumens. Transparent dentin, unlike normal dentin, exhibits almost no yielding before failure. Its fracture toughness is also lowered by about 20% while the fatigue lifetime is deleteriously affected.93
However, no or only minor differences in microhardness values were found between vital and nonvital dentin of contralateral teeth after periods varying from 0.2 to 10 years.100,161 The literature does not support a widely held belief that attributes particular weakness or brittleness to nonvital dentin. It is also believed that the age-related reduction of pulp volume, progressively replaced by secondary or tertiary dentin, could account for a reduced fracture resistance of aged, nonvital teeth; this assumption is evaluated in the literature. The only impact of age-related tissue changes are the aforementioned reduction in fracture toughness and fatigue lifetime attributed to dentin sclerosis.93
The chemicals used for canal irrigation and disinfection, as already mentioned, interact with mineral and organic contents and then reduce dentin elasticity and flexural strength to a significant extent,68,164 as well as microhardness.34,81,153 On the contrary, disinfectants like eugenol and formocresol increase dentin tensile strength by way of protein coagulation and chelation with hydroxyapatite (eugenol). Dentin hardness, however, did not prove to be influenced by the latter products.118
In conclusion, possible decrease in tooth strength can be attributed to dentin aging and to a smaller extent to dentin alteration by endodontic irrigants.
Fracture Resistance and Tooth Stiffness of Nonvital and Endodontically Treated Teeth
The major changes in tooth biomechanics are attributed to the loss of tissue following decay, fracture, or cavity preparation, including the access cavity prior to endodontic therapy.
The loss of tooth structure following a conservative access cavity preparation affects tooth stiffness by only 5%.177 The influence of subsequent canal instrumentation and obturation lead only to a slight reduction in the resistance to fracture177 and ultimately have little effect on tooth biomechanics.144,177 Practically, one can expect alteration of tooth biomechanics only in cases of nonconservative canal preparation or through the chemical or structural alteration triggered by endodontic irrigants, as previously mentioned.
In fact, the largest reduction in tooth stiffness results from additional preparation, especially the loss of marginal ridges. The literature reports 20% to 63% and 14% to 44% reduction in tooth stiffness following occlusal and MOD cavity preparations, respectively.45,98,144 It was shown that an endodontic access cavity combined with an MOD preparation results in maximum tooth fragilization. The cavity depth, isthmus width, and configuration are therefore highly critical to the reduction in tooth stiffness and risk of fracture (Fig. 22-1).78,89,102,128

FIG. 22-1 The negative impact of poor initial biomechanical status on restoration success. A-B, Preoperative radiographic views following the removal of the old metallic foundation. C, A new amalgam core, using post and self-anchorage into mesial root structure, was performed. D, Prosthetic restorations on working model. E, Full arch view after 3 years. F, The tooth is symptomatic due to furcation involvement and periapical lesion. G, This untreatable tooth was finally extracted and replaced by an implant. H, Eight-year postoperative radiograph showing a stable situation. Other teeth with less extensive biomechanical damage overcame functional stresses.
The presence of residual tissue in the cervical area (which comprises the ferrule for restorations) and a larger amount of residual tissue in general increase tooth resistance to fracture. It actually allows the axial walls of the crown to encircle the tooth, providing restoration retention and stabilization and reducing cervical tensile stresses.7,24,169 Crown preparations with as little as 1 mm coronal extension of dentin above the margin doubles the fracture resistance of preparations, compared to those where the core terminates on a flat surface immediately above the margin109,169; therefore, a minimal 1-mm ferrule is considered necessary to stabilize the restoration.169 However, the widths of preparation shoulder and crown margin do not appear to influence fracture strength.2
It is critical to understand that the most important part of the restored tooth is the tooth itself, and no restorative material or combination of materials will perfectly substitute for tooth structure.
Esthetic Changes in Nonvital and Endodontically Treated Teeth
Color change and darkening of nonvital teeth is a common clinical observation (Fig. 22-2), and improper endodontic techniques can contribute to discoloration. For instance, inadequate cleaning and shaping can leave necrotic tissue in coronal pulp horns, resulting in tooth darkening. As well, root canal filling materials (gutta-percha and root canal cements) retained in the coronal aspect of anterior teeth can detract from the esthetic appearance. Opaque substances also adversely affect the color and translucency of most uncrowned teeth. Biochemically altered dentin modifies tooth color and appearance. It is generally accepted that organic substances present in dentin (e.g., hemoglobin) might play an important role in this color change and also food and drink pigment penetration triggered by the absence of pulpal pressure. However, the respective contribution of these two phenomena and precise physicochemical mechanisms leading to discoloration are poorly understood or described in the literature.35,71,137

FIG. 22-2 Severe discoloration can significantly disturb esthetics, even in the lateral area of the smile. When not treatable with bleaching agents or veneers, this condition might justify tooth preparation for a full crown.
Thin gingival tissue or in general, thin biotype is considered a negative factor for esthetic outcome of restorative and prosthetic treatment of discolored teeth.116,117,124
Endodontic treatment and subsequent restoration of teeth in the esthetic zone require careful control of procedures and materials to retain a translucent, natural appearance. It is therefore strongly recommended to avoid the use of potentially staining endodontic cements and to clean all material residues in the pulpal chamber and access cavity.
Restorative Materials and Options
Endodontic treatment can result in significant loss and weakening of tooth structure. Tooth structure lost during endodontic treatment increases the risk of crown fracture, with fatigue mechanisms mediating the fracture of roots over time. Restorations of endodontically treated teeth are designed to (1) protect the remaining tooth from fracture, (2) prevent reinfection of the root canal system, and (3) replace the missing tooth structure.
According to the amount of tissue to be replaced, restorations of endodontically treated teeth will rely on different materials and clinical procedures. As a general rule, most structurally damaged teeth should be restored with an artificial crown.
Although the use of a crown built on post and core is a traditional approach, others have advocated the use of direct composite resins for restoring small defects in endodontically treated teeth. More recently, indirect restorations such as overlays or endocrowns made of composite resins or ceramics have also been used. The selection of appropriate restorative materials and techniques is dictated by the amount of remaining tooth structure. This is far more relevant to the long-term prognosis of endodontically treated teeth than any properties of post, core, or crown materials.
Direct Composite Restorations
When a minimal amount of coronal tooth structure has been lost after endodontic therapy, a direct resin composite restoration may be indicated. Composite resins are a mixture of a polymerized resin network reinforced by inorganic fillers. Contemporary composites have compressive strengths of about 280 MPa, and the Young modulus of composite resins is generally about 10 to 16 GPa, which is close to that of dentin.140
When properly cured, resin composites are highly esthetic, exhibit high mechanical properties, and can reinforce the remaining tooth structure through bonding mechanisms. Typically, 500 to 800 mW/cm2 of blue light for 30 to 40 seconds is necessary to polymerize an increment of composite which must be 1 to 3 mm thick. Unfortunately, the shrinkage that accompanies polymerization of contemporary composite resins remains a significant problem to the long-term success of these restorations. The use of an incremental filling technique, which helps to reduce shrinkage stresses during polymerization, is highly recommended. The amount of shrinkage will also depend on the shape of the cavity preparation and the ratio of bonded to unbonded (or free) surfaces.37,55 This so-called C-factor is a clinically relevant predictor of the risk of debonding and leakage; restorations with high C-factors (>3.0) are at greatest risk for debonding.183 In other words, a direct composite restoration may be indicated when only one proximal surface of the tooth has been lost; using an incremental filling technique is mandatory.
Classically, direct composite restorations have been placed in anterior teeth that have not lost tooth structure beyond the endodontic access preparation. In such cases, the placement of a direct composite restoration offers an immediate sealing of the tooth, which prevents coronal leakage and recontamination of the root canal system with bacteria. In vitro studies have demonstrated that the fracture resistance of small bonded restorations is nearly as great as that of intact teeth.61,142
Although direct composite resins may also be used for small restorations in posterior teeth, they are contraindicated when more than a third of coronal tissue has been lost. In one study,142 it was reported that the resistance to fracture of endodontically treated teeth is reduced by 69% in cases where MOD cavities are present.143 Under such conditions, a direct composite restoration may not be appropriate to prevent the tooth structure from fracture and reinfection. Furthermore, resin composite materials may require the use of reinforcing in vitro fibers to increase their mechanical resistance. Although most studies on the clinical performance of direct composite restorations were conducted on vital teeth, a recent clinical report indicates that direct in vitro fiber-reinforced composite restorations may represent a valuable alternative to conventional restorations of endodontically treated teeth.38 On the contrary, inserting an in vitro fiber post in the root canal of an endodontically treated tooth before bonding a direct MOD restoration significantly reduces its fracture resistance compared to the same composite restoration without a post.167
Indirect Restorations: Composite or Ceramic Onlays and Overlays
Ceramic or resin composite onlays and endocrowns can also be used to restore endodontically treated teeth. Whereas overlays incorporate a cusp or cusps by covering the missing tissue, endocrowns combine the post in the canal, the core, and the crown in one component.94 Both onlays and endocrowns allow for conservation of remaining tooth structure, whereas the alternative would be to completely eliminate cusps and perimeter walls for restoration with a full crown.62 Onlays and overlays are generally constructed in the laboratory from either hybrid resin composite or ceramics.
Ceramics are a material of choice for long-term esthetic indirect restorations because their translucency and light transmission mimic enamel. Whereas traditional feldspathic porcelains were sintered from a slurry, new ceramic materials may be cast, machined, pressed, or slip-cast in addition to being sintered. New materials are either variations of feldspathic porcelains (e.g., In-Ceram, Cerec, IPS Empress) or may be fabricated from other ceramic systems, including alumina, zirconia, or silica.3,39 Among these newer compositions is lithium disilicate, which offers high strength, high fracture toughness, and a high degree of translucency. Physical properties of these materials have improved to the point where they can survive high stress-bearing situations such as posterior restorations in endodontically treated teeth.46,77 Researchers have examined 140 partial Cerec restorations (Vita MKII, feldspathic porcelain) adhesively cemented to endodontically treated teeth and found this treatment approach satisfactory after an observation period of 55 months.10 Their results indicate that survival rates are higher for molars than for premolars.
Onlays, overlays, and endocrowns can also be fabricated from resin composites processed in the laboratory. Using various combinations of light, pressure, and vacuum, these fabrication techniques are claimed to increase the conversion rate of the polymer and consequently the mechanical properties of the restorative material. Other investigations have described the application of glass fiber–reinforced composite endocrowns on premolars and molars as single restorations or as abutment for fixed partial dentures.62,63 A recent in vitro study by another research team indicates that composite inlays can partially restore the resistance to fracture of endodontically treated molars and prevent catastrophic fractures after loading.29 Other investigators reported that composite resin MZ100 increased the fatigue resistance of overlay-type restorations in endodontically treated molars when compared to porcelain MKII.103 Another recent study used three-dimensional finite element analysis to estimate bone resorption around endocrowns made up of high- (alumina) or low-elastic modulus materials (resin composites). They concluded that the higher resilience of resin composite restorations acts positively against the risk of periodontal bone resorption by reducing the amount of force transferred to root dentin.4
Full Crowns
When a significant amount of coronal tooth structure has been lost by caries, restorative procedures, and endodontics, a full crown may be the restoration of choice. In a few cases, the crown can be directly built on the remaining coronal structure which has been prepared accordingly (see Core Materials heading). More frequently, the cementation of a post inside the root canal is necessary to provide retention for the core material and the crown.172 The core is anchored to the tooth by extension into the root canal through the post and replaces missing coronal structure. The crown covers the core and restores the esthetics and function of the tooth.
An additional role of the post and core is to protect the crown margins from deformation under function and thereby to prevent coronal leakage. Because most endodontic sealers do not completely seal the root canal space, the coronal seal provided by the placement of a post and core will positively influence the outcome of the endodontic treatment.155 The post’s ability to anchor the core is also an important factor for successful reconstruction, since the core and the post are usually fabricated of different materials. Finally, the luting material used to cement the post, the core, and the crown to the tooth will also influence the longevity of the restoration. The post, the core, and their luting or bonding agents together form a foundation restoration to support the future crown.112
The Foundation Restoration: General Considerations
Although there are many materials and techniques to fabricate a foundation restoration, no combination of materials can substitute for tooth structure. As a general rule, the more tooth structure that remains, the better the long-term prognosis of the restoration. The coronal tooth structure located above the gingival level will help to create a ferrule.6,85,106,134 The ferrule is formed by the walls and margins of the crown, encasing at least 2 to 3 mm of sound tooth structure. A properly executed ferrule significantly reduces the incidence of fracture in endodontically treated teeth by reinforcing the tooth at its external surface and dissipating forces that concentrate at the narrowest circumference of the tooth.101,181 A longer ferrule increases fracture resistance significantly.86 The ferrule also resists lateral forces from posts and leverage from the crown in function and increases the retention and resistance of the restoration. To be successful, the crown and crown preparation together must meet five requirements:
Root anatomy can also have significant influence over post placement and selection. Root curvature, furcations, developmental depressions, and root concavities observed at the external surface of the root are all likely to be reproduced inside the root canal. Within the same root, the shape of the canal will vary between the cervical level and the apical foramen.66 As a result, severe alteration of the natural shape of the canal is often necessary to adapt a circular post inside the root. This increases the risk of root perforation, especially in mesial roots of maxillary and mandibular molars which exhibit deep concavities on the furcal surface of their mesial root.17,95 The tooth is also weakened if root dentin is sacrificed to place a larger-diameter post. A study using three-dimensional electronic speckle-pattern interferometry (ESPI) evaluated the effects of root canal preparation and post placement on the rigidity of human roots.99 ESPI has the major advantage of being able to assess tooth deformation in real time and can be used repeatedly on the same root because of the nondestructive nature of the test. Study results indicate that root deformability is significantly increased after the preparation of a post space. Thus, preservation of root structure is also a guiding principle in the decision to use a post, the selection of the post, and the preparation of the post space. This is a reason why not every endodontically treated tooth needs a post and why more conservative approaches that do not rely on the use of a post are currently being developed.
However, a post may be used in the root of a structurally damaged tooth in which additional retention is needed for the core and coronal restoration. Posts should provide as many of the following clinical features as possible:
From a mechanical point of view, an endodontic post should not break, should not break the root, and should not distort or allow movement of the core and crown. An ideal post would have an optimal combination of resilience, stiffness, flexibility, and strength. Resilience is the ability to deflect elastically under force without permanent damage. It is a valuable quality in endodontic posts, but too much flexibility in a narrow post compromises its ability to retain the core and crown under functional forces. Stiffness describes a material’s ability to resist deformation when stressed. The stiffness of a material is an inherent physical property of that material, regardless of size. However, the actual flexibility of a post depends both on the diameter of a specific post and on the modulus of elasticity of the post’s material. Posts with a lower modulus of elasticity are more flexible than posts of the same diameter with a higher modulus of elasticity. Posts made of non-stiff materials (low modulus of elasticity) are more resilient, absorb more impact force, and transmit less force to the root than stiff posts, but low-modulus posts fail at lower levels of force than high-modulus posts.105,126,150
Excessive flexing of the post and micromovement of the core are particular risks in teeth with minimal remaining tooth structure, because these teeth lack their own cervical stiffness as a result of the missing dentin. Post flexion can also distort and open crown margins. Open margins can result in potentially devastating caries or endodontic leakage and apical reinfection. Extensive caries extending into the root can be as irreparable as root fracture. Because rigid posts flex and bend less than nonrigid posts, they can limit movement of the core and possible disruption of the crown margins and cement seal. However, the force must go somewhere. Force from a stiff post is transmitted to the root, next to the apex of the post. An attempt to strengthen a weak root by adding a stiff post can instead make the root weaker as a result of the force concentration of a stiff rod in a more flexible material. Stress concentration in the post/root complex can lead to the self-destructive process of cracking and fracturing. Root fracture is particularly a risk in teeth with minimal remaining tooth structure to support a ferrule.
Roots also flex under force, which is a function of both the modulus of elasticity of dentin and the diameter of the root. Dentin is relatively flexible, and posts can be flexible or stiff. Although no material can behave exactly like dentin, a post with functional behavior similar to that of dentin is beneficial when the post must be placed next to dentin. Posts have been developed with a modulus of elasticity closer to dentin than that offered by traditional metal posts. But posts are significantly narrower than roots, and the actual deflection of a post within dentin is a function of both the modulus of elasticity and the diameter. The modulus of elasticity of various posts, compared with that of dentin, represents only one aspect of flexion.
In summary, an ideal post would be resilient enough to cushion an impact by stretching elastically, thereby reducing the resulting stress to the root. It would then return to normal without permanent distortion. At the same time, this ideal post would be stiff enough not to distort, permanently bend, or structurally fail under mastication forces. Finally, the perfect post would combine the ideal level of flexibility and strength in a narrow-diameter structure, which is dictated by root canal morphology. Current post systems are designed to provide the best compromise between the desired properties and inherent limitations of available materials.
Why Roots Fracture
Structures subjected to low but repeated forces can appear to fracture suddenly for no apparent reason. This phenomenon, also known as fatigue failure, occurs when a material or a tissue is subjected to cyclic loading. Fatigue may be characterized as a progressive failure phenomenon that proceeds by the initiation and propagation of cracks; many failures of teeth or materials observed in the mouth are fatigue-related. Because teeth are subjected to fluctuating cycles of loading and unloading during mastication, fatigue failure of dentin, posts, cores, crown margins, or adhesive components are all likely to occur.160 Mechanical loading will favor the propagation of microcracks that will progress from the coronal to the apical region of the tooth.
Initial failure of crown margins from fatigue loading is clinically undetectable. However, when measured in vitro, early failure resulted in significant leakage of crown margins, extending between the tooth, restoration, and post space.48 Particularly in teeth with minimal remaining tooth structure, fatigue can cause endodontic posts to bend permanently or break, or it can cause a fiber-matrix complex to disintegrate.
Fatigue failure of nonvital teeth restored with a post is more catastrophic because it may result in a complete fracture of the root. A post placed into a dentin root will function physically like any structural rod anchored in another material. This means that the forces applied on the post are transmitted to the root dentin with characteristic patterns depending on the modulus of elasticity of both the post and the dentin. If the post has a higher modulus than the dentin, the stress concentration is adjacent to the bottom of the post (Fig. 22-3). This is evident in clinical cases of root fracture originating at the apex of a rigid post.
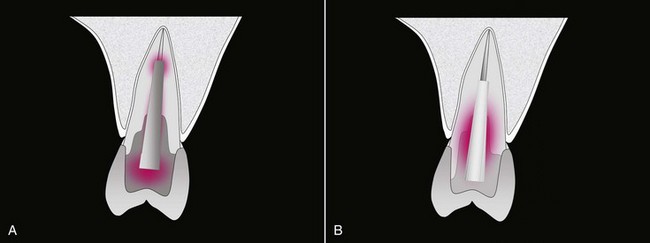
FIG. 22-3 A, Stress distribution within a metallic post and core foundation and residual tooth structure, according to photoelastic and FEM studies. The post is cemented and usually penetrates the apical portion of the root. Functional stresses accumulate inside the foundation, slightly around the post and further inside the canal, around the apex of the post; there is less stress buildup in the cervical area compared to that with a fiber post (as shown in Fig. 22-3, B). This configuration more ideally protects the coronocervical structures but when failing, results in severe untreatable root fractures. B, Stress distribution within a fiber post/composite foundation and residual tooth structure, according to photoelastic and FEM studies. The post is bonded to the canal walls and penetrates the canal less apically. Functional stresses mainly accumulate around the post in the cervical area. This configuration protects the cervical area less efficiently but tends to prevent untreatable root fractures. The presence of a ferrule is mandatory.
(Adapted from Dietschi D, Duc O, Krejci I, Sadan A: Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature—Part 1. Composition and micro- and macrostructure alterations. Quintessence Int 38:733–743, 2007.)
When the stiffness of the endodontic post is similar to that of dentin, stresses are not concentrated in the dentin adjacent to the apex of the post but rather dissipated by both the coronal and the root dentin (see Fig. 22-3). A resilient post can also prevent a sudden blow by stretching elastically, which reduces the transient forces against the tooth, but a post that is too elastic becomes too flexible for retaining a core and a crown when the tooth cannot do so on its own. A resilient post that is overloaded fails with less force than a stiffer post. This limits the amount of resilience that can be designed into a post.
Direct Foundation Restorations
In general, the evolution of foundation restorations has been to diminish invasiveness and eliminate some components in selected cases. When a sufficient amount of tissue is present at the periphery of the prepared tooth, a direct foundation restoration is indicated. In the direct technique, a prefabricated post is cemented inside the root canal, and the core is built directly on the prepared tooth. For other clinical situations, an indirect custom-cast post and core may be indicated.
Various materials can be used to fabricate a direct foundation restoration. Although there is growing interest in using resin-based materials such as resin composites or fiber-reinforced resin posts, more traditional materials such as amalgam are still used for that purpose.28 For clarity, the components used for fabricating a direct foundation restoration (e.g., the endodontic post and core material) are described individually.
Posts
The large number of post designs and materials available on the market reflects the absence of consensus in that field. Based on what manufacturers or clinicians consider the most important properties, posts can be fabricated from metal (gold, titanium, stainless steel), ceramic, or fiber-reinforced resins. As a general rule, a post needs retention and resistance. Whereas post retention refers to the ability of a post to resist vertical forces, resistance refers to the ability of the tooth/post combination to withstand lateral and rotational forces. Resistance is influenced by the presence of a ferrule, the post’s length and rigidity, and the presence of antirotational features. A restoration lacking resistance form is not likely to be a long-term success, regardless of the retentiveness of the post.
Prefabricated Metallic Posts
Prefabricated metallic posts are frequently used for the fabrication of a direct foundation restoration. These posts are classified several ways, including by alloy composition, retention mode, and shape. Materials used to fabricate metallic posts include gold alloys, stainless steel, or titanium alloys. Metallic posts are very strong, and with the exception of the titanium alloys, very rigid.96 A recent study indicates that the flexural strength of stainless steel posts is about 1430 MPa and that flexural modulus approximates 110 GPa.136 On the other hand, titanium posts are less rigid (66 GPa) but exhibit a flexural strength (1280 MPa) similar to stainless steel.
The retention of prefabricated posts inside the root canal is also essential for successful restorations. Two basic concepts have been used to promote the retention of endodontic posts: active posts and passive posts. Active posts derive their primary retention directly from the root dentin by the use of threads. Most active posts are threaded and are intended to be screwed into the walls of the root canal. A major concern about threaded posts has been the potential for vertical root fracture during placement. As the post is screwed into place, it introduces great stresses within the root, causing a wedging effect.171 Therefore, it is generally accepted that the use of threaded posts should be avoided. Furthermore, the improved retention once offered by threaded posts can now be achieved with adhesive luting cements (see later).123 Passive posts are passively placed in close contact to the dentin walls, and their retention primarily relies on the luting cement used for cementation. The shape of a passive post may be either tapered or parallel.146 A parallel post is more retentive than a tapered post but also requires removal of more root dentin during the preparation of the post space. Parallel posts are reported to be less likely to cause root fractures than tapered posts, although they are less conforming to the original shape of the root.83,158,170 Unfortunately, modern techniques for root canal preparation use tapered nickel-titanium (NiTi) rotary shaping files, which results in a very wide tapered and unretentive canal exhibiting a significant divergence from apical to coronal.152 Longer posts are often necessary to accommodate this problem and offer adequate retention; adequate length in the root canal is considered to be greater than 6 mm. When teeth are protected by crowns with an adequate ferrule, longer posts do not further increase fracture resistance.84 Posts designed with mechanical locking features in the heads and roughened surface texture can show better retention of the core.30
Fiber Posts
A fiber post consists of reinforcing fibers embedded in a resin polymerized matrix. Monomers used to form the resin matrix are typically bifunctional methacrylates (Bis-GMA, UDMA, TEGDMA), but epoxies have also been used. Common fibers in today’s fiber posts are made of carbon, glass, silica, or quartz but the type, volume content, and uniformity of the fibers and the matrix are proprietary and vary among fiber post systems. These differences in the manufacturing process may reflect the large variations observed among different types of fiber posts subjected to a fatigue resistance test.67 Fibers are commonly 7 to 20 µm in diameter and are used in a number of different configurations, including braided, woven, and longitudinal. The original fiber posts consisted of carbon fibers embedded in epoxy resin, but quartz-fiber posts are currently preferred for their favorable mechanical properties, esthetic qualities, and their ability to chemically bond to the polymer matrix.51 A recent study indicates that the flexural strength of glass-, silica-, or quartz-fiber posts approximates 1000 MPa and that flexural modulus is about 23 GPa.36 Current fiber posts are radiopaque and may also conduct the light for polymerization of resin-based luting cements. A light-transmitting post results in better polymerization of resin composites in the apical area of simulated root canals, as measured by hardness values.148,182 To enhance bonding at the post/core/cement interfaces, several physicochemical pretreatments such as silanization or sand blasting of the post surface have been described. Recent research indicates that silanization, hydrofluoric etching, and sandblasting (with 30 to 50 µm Al2O3) do not modify the mechanical properties of different glass-, silica-, or quartz-fiber posts.5
It is generally accepted that bonding fiber posts to root canal dentin can improve the distribution of forces applied along the root, thereby decreasing the risk of root fracture and contributing to the reinforcement of the remaining tooth structure.13,19,58 A well-adapted adhesively cemented fiber post is considered the most retentive with the least stress generated on the canal walls. In a retrospective study which evaluated three types of bonded fiber posts, investigators reported 3.2% failure of 1306 fiber posts in recalls of 1 to 6 years.57 More recently, another study reported survival rates of 98.6% and 96.8% for parallel-sided and tapered fiber posts, respectively, placed in anterior teeth covered with full-ceramic crowns after a mean observation period of 5.3 years.163
Zirconia Posts
Zirconia posts are composed of zirconium dioxide (ZrO2) partially stabilized with yttrium oxide and exhibit a high flexural strength. Zirconia posts are esthetic, partially adhesive, very rigid, but also brittle. Zirconia posts cannot be etched, and available literature suggests that bonding resins to these materials is less predictable and requires substantially different bonding methods than conventional ceramics.12 When a composite core is built on a zirconia post, core retention may also be a problem. Controversies exist about the efficiency of airborne particle abrasion at establishing a durable resin bond to zirconia posts treated or not treated with a coupling agent.1,133 Overall, there are concerns about the rigidity of zirconia posts, which tends to make those posts too brittle. Other reports indicate that the rigidity of zirconia posts negatively affects the quality of the interface between the resin core material and dentin when subjected to fatigue testing.41,44
Core Materials
The core replaces carious, fractured, or missing coronal structure and helps to retain the final restoration. Desirable physical characteristics of a core include (1) high compressive and flexural strength, (2) dimensional stability, (3) ease of manipulation, (4) short setting time, and (5) the ability to bond to both tooth and post. Core materials include composite resin, cast metal or ceramic, amalgam, and sometimes glass ionomer materials. The core is anchored to the tooth by extension into the coronal aspect of the canal or through the endodontic post. The importance of retention between the post, the core, and the tooth increases as remaining tooth structure decreases.
Composite Resin Core
Composite core materials take a number of strategies to enhance their strength and resistance; metal may be added, filler levels may be greater, or faster-setting ionomers may be used.140 Composite core materials have been shown to exhibit slightly better mechanical values than conventional materials, but improvements are negligible.184 However, they appear to be superior to silver-glass-ionomer cement and amalgam.31 The advantages of composite core resins are adhesive bonding to tooth structure and many posts, ease of manipulation, rapid setting, and translucent or highly opaque formulations. Composite cores have been shown to protect the strength of all-ceramic crowns equally to amalgam cores. Bond strength of composite cores to dentin depends on a complete curing of the resin materials, so dentin bonding agents must be chemically compatible with composite core materials. Self-cure composite resins require self-cure adhesives and are mostly incompatible with light-cure adhesives.27 However, no adhesive has been shown to completely eliminate microleakage at the margins of the restoration.18 A degradation of the resin core or the marginal integrity of the crown can result in invasion of oral fluids. Therefore, as with all buildup materials for decimated teeth, more than 2 mm of sound tooth structure should remain at the margin for optimal composite resin core function.
Composite core materials can be used in association with metallic, fiber, or zirconia posts. This is frequently observed in the presence of structurally compromised teeth. They may provide some protection from root fracture in teeth restored with metal posts compared with amalgam or gold cores. Loosening of the post, core, and crown with composite core can occur, but composite cores have been shown to fail more favorably than amalgam or gold.135 A recent retrospective study of the clinical performance of fiber posts indicates that fiber posts and cores have a failure rate ranging between 7% and 11% after a service period of 7 to 11 years and that post loosening may also occur.56 Composite core materials are typically two-paste, self-cured composites, but light-curing materials are also available. The use of light-curing composite core materials generally eliminates the risk of chemical incompatibility between adhesives and self-curing resin core materials. Bonding light-cured resin composites to the irregular structure of the pulp chamber and canal orifices might eliminate the need for a post when sufficient tooth structure remains. Research indicates that bonding to the dentin walls of the pulp chamber is easier and superior to resin dentin bonds made on dentin canal walls.8
Amalgam Core
Dental amalgam is a traditional core buildup material with a long history of clinical success. Although there are many variations in the alloy’s composition, more recent formulations have high compressive strength (400 MPa after 24 hours), high tensile strength, and a high modulus of elasticity. High-copper alloys tend to be stiffer (60 GPa) than low-copper alloys.
Amalgam can be used with or without a post. Thirty years ago, investigators described the amalcore.119 With the amalcore technique, amalgam is compacted into the pulp chamber and 2 to 3 mm coronally of each canal. The following criteria were considered for the application of this technique: the remaining pulp chamber should be of sufficient width and depth to provide adequate bulk and retention of the amalgam restoration, and an adequate dentin thickness around the pulp chamber was required for the tooth-restoration continuum rigidity and strength. The fracture resistance of the amalgam coronal-radicular restoration with four or more millimeters of chamber wall was shown to be adequate, although the extension into the root canal space had little influence.87
Amalgam can also be used in combination with a prefabricated metallic post when the retention offered by the remaining coronal tissue needs to be increased. Amalgam cores are highly retentive when used with a preformed metal post in posterior teeth; they require more force to dislodge than cast posts and cores.108 Others have suggested the use of adhesive resins to bond amalgam to coronal tissue.162
Significant disadvantages of amalgam cores are the “nonadhesive nature” of the material, the potential for corrosion, and subsequent discoloration of the gingiva or dentin. Amalgam use is declining worldwide because of legislative, safety, and environmental issues.
Glass Ionomer Core and Modified Glass Ionomer Core
Glass ionomer and resin-modified glass ionomer cements are adhesive materials useful for small buildups or to fill undercuts in prepared teeth. The rationale for using glass ionomer materials is based on their cariostatic effect resulting from fluoride release. However, their low strength and fracture toughness result in brittleness, which contraindicates the use of glass ionomer buildups in thin anterior teeth or to replace unsupported cusps. They may be indicated in posterior teeth in which (1) a bulk of core material is possible, (2) significant sound dentin remains, and (3) caries control is indicated.180
Resin-modified glass ionomer materials are a combination of glass ionomer and composite resin technologies and have properties of both materials. Resin-modified glass ionomers have moderate strength, greater than glass ionomers but less than composite resins. As a core material, they are adequate for moderate-sized buildups, but hygroscopic expansion can cause fracture of ceramic crowns and fragilized roots.165 The bond to dentin is close to that of dentin-bonded composite resin and significantly higher than traditional glass ionomers. Today, resin composites have replaced glass ionomer materials for core fabrication.
Indirect Foundation Restorations: Cast Post and Core
For many years, the cast metal post and core has been the traditional method for fabricating the foundation restoration of a prosthetic crown. Classically, smooth-sided, tapered posts conforming to the taper of the root canal are fabricated from high noble alloys, although noble and base-metal classes of dental alloys have also been used. Noble alloys used for post and core fabrication have high stiffness (approximately 80 to 100 GPa), strength (1500 MPa), hardness, and excellent resistance to corrosion.32
One advantage of the cast post/core system is that the core is an integral extension of the post, and that the core does not depend on mechanical means for retention on the post. This construction prevents dislodgment of the core from the post and root when minimal tooth structure remains. However, the cast post/core system also has several disadvantages. Valuable tooth structure must be removed to create a path of insertion or withdrawal. Second, the procedure is expensive because two appointments are needed, and laboratory costs may be significant. The laboratory phase is technique sensitive. Metal casting of a pattern with a large core and a small-diameter post can result in porosity in the gold at the post/core interface. Fracture of the metal at this interface under function results in failure of the restoration. Most important, the cast post/core system has a higher clinical rate of root fracture than preformed posts.47,166
Studies on cast post retention have shown that the post must fit the prepared root canal as closely as possible to be perfectly retained. When a ferrule is present, custom cast posts and cores exhibit a higher fracture resistance compared to composite cores built on prefabricated metallic posts or carbon posts.104 Cast posts are also known to exhibit the least amount of retention and are associated with a higher failure rate compared to prefabricated parallel-sided posts. In a classic retrospective study (1 to 20 years) of 1273 endodontically treated teeth in general practice, 245 (19.2%) were restored with tapered cast posts and cores. Among these, 12.7% were deemed failures. This failure rate was higher than that for the other passive post systems used. Of particular concern was the fact that 39% of the failures led to unrestorable teeth requiring extraction. Thirty-six percent of the failures were due to loss of retention, and 58% were due to the fracture of the root. It has been suggested that tapered smooth-sided posts have a “wedging” effect under functional loading, and it is this that leads to increased risk of root fracture.168
One 6-year retrospective study reported a success rate higher than 90% using a cast post and core as a foundation restoration.9 The lower failure rate and fewer root fractures were attributed to the presence of an adequate ferrule and careful tooth preparation. Attention has also been drawn to the fact that the higher failure rate may be due to the fact that nearly half of the posts were shorter than recommended from the literature. A venting groove for the cement along the axis of the post results in less stress on residual tissues.
Luting Cements
A variety of cements have been used to cement endodontic posts and include traditional cements, glass ionomer cements, and resin-based luting cements.
Traditional Cements
Zinc phosphate cements or polycarboxylate cements are still used for cementation of posts and crowns. They are generally supplied as a powder and a liquid and their physical properties are highly influenced by the mixing ratio of the components. Their compressive strength is about 100 MPa, and elastic moduli are lower than that of dentin (5 to 12 GPa). Zinc phosphate cement is mostly used for cementing metal restorations and posts; film thickness of the zinc phosphate cement is less than 25 µm. These cements provide retention through mechanical means and have no chemical bond to the post or to dentin but provide clinically sufficient retention for posts in teeth with adequate tooth structure.
Glass Ionomer Luting Cements
Glass ionomer cements are a mixture of glass particles and polyacids, but resin monomers may also be added. Depending on the resin content, glass ionomer cements can be classified as either conventional or resin-modified glass ionomer cements. Conventional glass ionomer cements have compressive strengths ranging between 100 and 200 MPa; the Young modulus is generally about 5 GPa. They are mechanically more resistant than zinc phosphate cements, and they can bond to dentin with values ranging between 3 and 5 MPa. Some authors still recommend the use of glass ionomer cements for the cementation of metallic posts. Major advantages of conventional glass ionomer cements are their ease of manipulation, chemical setting, and ability to bond to both tooth and post.
On the contrary, resin-modified glass ionomer cements are not indicated for post cementation, because these cements exhibit hygroscopic expansion that can promote fracture of the root.
Resin-Based Luting Cements
Today there is a trend toward the use adhesive cements for bonding endodontic posts during the restoration of nonvital teeth. The rationale for using adhesive cements is based on the premise that bonding posts to root canal dentin will reinforce the tooth and help retain the post and the restoration.50 Contemporary resin-based luting cements have been shown to exhibit compressive strengths around 200 MPa and elastic moduli between 4 and 10 GPa.25 These materials may be polymerized through a chemical reaction, a photopolymerization process, or a combination of both mechanisms. Photopolymerization of these resin-based materials is often necessary to maximize strength and rigidity.
Most luting cements require a pretreatment of the root canal dentin with either etch-and-rinse or self-etching adhesives. Both types of adhesives have been shown to form hybrid layers along the walls of the post spaces.11 However, bonding to root canal dentin may be compromised by the use of endodontic irrigants such as sodium hypochlorite, hydrogen peroxide, or their combination.121 Because these chemicals are strong oxidizing agents, they leave behind an oxygen-rich layer on the dentin surface that inhibits the polymerization of the resin.159 Previous research has shown that the bond strength of C&B Metabond to root canal dentin was reduced by half when the dentin was previously treated with 5% sodium hypochlorite (NaOCl) or 15% EDTA/10% urea peroxide (RC Prep, Premier Dental, Plymath Meeting, PA).113 Other reports indicate that the contamination of the dentin walls by eugenol diffusing from endodontic sealers may also affect the retention of bonded posts.70,176 Further, it is difficult to control the amount of moisture left in a root canal after acid etching, making impregnation of collagen fibers with etch-and-rinse adhesives problematic. The use of self-etching adhesives has been proposed as an alternative for the cementation of endodontic posts, because self-etching adhesives are generally used on dry dentin and do not require rinsing of the etchant. However, their efficiency at infiltrating thick smear layers like those produced during post space preparation remains controversial.110,179 More recently, dual-curing adhesives have been developed to ensure a better polymerization of the resin deep inside the root canal. Dual-cured adhesives contain ternary catalysts to offset the acid-base reaction between the acidic monomers and the basic amines along the composite/adhesive interface.111
Although both self-curing and light-curing luting cements can be used for cementation of prefabricated endodontic posts, most resin cements have a dual-curing process that requires light exposure to initiate the polymerization reaction. Dual-curing cements are preferred because there are concerns as to whether light-curing materials are properly cured, especially in areas of difficult light access such as the apical portion of the root canal. However, it has been reported that photocured composites generate more shrinkage stress and exhibit less flow than chemically cured composites.54 Contraction stresses induced by polymerization also depend on the geometry of the post space and the thickness of the resin film. Previous research indicates that the restriction of flow of resin cements by the configuration of the root canal can significantly increase the contraction stress at the adhesive interface.53,174
In recent years, a number of techniques have been used to measure the adhesion of resin-based luting cements to root canal dentin. These methods include the pull-out tests, the microtensile bond strength tests and the push-out tests.49,65 Although laboratory tests confirmed that bond strengths ranging between 10 and 15 MPa can be obtained with modern resin-based luting cement, there is also evidence that frictional retention is a factor contributing to post retention.15 It is generally accepted that bonding to dentin of the pulp chamber is more reliable than to root canal dentin, especially at the apical level.132 The lowered bond strength values recorded at the apical third of the root canal are likely to be related to the reduced number of dentinal tubules available for dentin hybridization. Shorter posts may be used when successful bonding occurs between fiber-reinforced posts and root dentin, because current adhesive luting cements can assist in the retention of posts in the root canal space.138
Another factor that may influence the performance of resin-based luting cements is the thickness of the cement layer. The cementation of endodontic fiber posts with thicker cement layers might be required when posts do not perfectly fit inside the root canal. Although a slight increase in cement thickness (up to 150 microns) does not significantly affect the performance of adhesive luting cements applied to root canal dentin, thicker layers may be detrimental to bond quality.80,157
A recent study indicates that bond strength to radicular dentin might be maximized by adopting procedures that compensate for polymerization stresses.14 The bonding procedures are realized in two separate steps. The initial step allows optimal resin film formation and polymerization along the root canal walls, leading to more ideal resin-dentin hybridization without stresses imposed by the placement of the post. A second step bonds the post to the cured resin film. The polymerization shrinkage that occurs during the initial adhesive coating step will reduce the effects of stress imposed when the resin-coated post polymerizes, thereby preserving the bond integrity.
Although the bonding performance of resin-based luting cements is well documented, there are other reports indicating that resin-dentin bonds degrade over time.23,60 The loss of bond strength and seal are attributed to the degradation of the hybrid layer created at the dentin-adhesive interface. This is particularly true for etch-and-rinse adhesives, because the gelatinization of collagen fibers caused by phosphoric acids may restrict the diffusion of the resin within the interfibrillar spaces and may leave unprotected fibers available for degradation. Removing organic components from the demineralized dentin prior to bonding procedures was recently suggested. The use of dilute NaOCl (0.5%) after acid etching or the conditioning of dentin smear layers with EDTA (0.1 M, pH 7.4) have been shown to produce more durable resin-dentin bonds made with single-step etch-and-rinse adhesives.156
Other research indicates that the degradation of denuded collagen fibrils exposed in incompletely infiltrated hybrid layers is driven by an endogenous proteolytic mechanism involving the activity of matrix metalloproteinases (MMPs).22,131 The release of MMPs such as collagenases has been evidenced in both coronal and root dentin of fully developed teeth of young patients.154 Researchers suggest that conditioning root canal dentin with a broad-spectrum protease inhibitor such as chlorhexidine (2 wt% chlorhexidine digluconate solution) might be useful for the preservation of dentin bond strength over time.21
Interestingly, these dentin-conditioning procedures, which may improve the resistance of the resin-dentin bond to chemical degradation, also act as antibacterial agents; this might be of interest in the endodontic context.
Self-Adhesive Cements
More recently, self-adhesive resin cements have been introduced as an alternative to conventional resin-based luting cements. Self-adhesive luting cements contain multifunctional phosphoric acid methacrylates that react with hydroxyapatite and simultaneously demineralize and infiltrate dental hard tissue.114 They do not require any pretreatment of the tooth substrates, and their clinical application is accomplished in a single step. Therefore, the self-etching capability of these new cements reduces the risk for incomplete impregnation of the conditioned tissue by the resins and reduces technique sensitivity. The elastic moduli of chemically cured self-adhesive resin cements are relatively low (4 to 8 GPa) but generally increase when a dual-curing process is used. It is therefore recommended that all dual-cured resin cements receive maximal light to achieve superior material properties wherever clinically possible.141 Adhesion performance to dentin was found comparable to multistep luting cements, but bonding to enamel without prior phosphoric acid etching is not recommended.76 However, their long-term clinical performances need to be assessed before making a general recommendation for their use.
Pretreatment Evaluation and Treatment Strategy
Before any therapy is initiated, the tooth must be thoroughly evaluated to ensure treatment success. Each tooth must be examined individually and in the context of its contribution to the overall treatment plan and rehabilitation. This assessment includes endodontic, periodontal, biomechanical, and esthetic evaluations. Planning of the restoration for endodontically treated teeth brings together all aforementioned biomechanical and clinical factors, as well as the various materials and procedures designed to address them.
Pretreatment Evaluation
Endodontic Evaluation
The prerestorative examination should include an inspection of the quality of existing endodontic treatment. New restorations, particularly complex restorations, should not be placed on abutment teeth with a questionable endodontic prognosis. Endodontic retreatment is indicated for teeth showing radiographic signs of apical periodontitis or clinical symptoms of inflammation. Restorations that require a post need a post space, which is prepared by removal of gutta-percha from the canal. Canals obturated with a silver cone or other inappropriate filling material should be endodontically retreated before starting any restorative therapy. Because the probability for periapical tissue to heal after endodontic retreatment is reasonably high, the chances to retain a well-restored tooth in asymptomatic function over time are excellent.125
Periodontal Evaluation
Maintenance of periodontal health is also critical to the long-term success of endodontically treated teeth. The periodontal condition of the tooth must therefore be determined before the start of endodontic therapy and restorative phase. The following conditions are to be considered as critical for treatment success:
If one or more of the aforementioned conditions are not met owing to preexisting pathology or structural defects, treatment success or even feasibility can be compromised, sometimes suggesting extraction of weak teeth and replacement with dental implants rather than conventional therapy.
Biomechanical Evaluation
All previous events, from initial decay or trauma to final root canal therapy, influence the biomechanical status of the tooth and the selection of restorative materials and procedures. The biomechanical status can even justify the decision to extract extremely mutilated teeth that do not deserve extensive treatments that carry a limited probability of success. Important clinical factors include the following:
Teeth with minimal remaining tooth structure are at increased risk for the following clinical complications120,173,178 (see Fig. 22-1; Fig. 22-4):
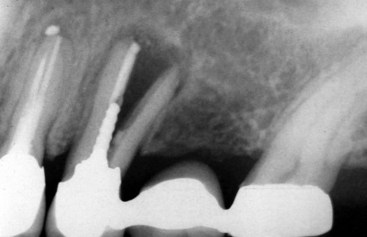
FIG. 22-4 Failure of prosthetic foundations can have dramatic consequences on both overlying restorations and surrounding tissues. A better understanding of compositional and structural changes that affect tooth resistance to repeated functional forces is mandatory to improve treatment success in endodontically treated teeth.
The amount and quality of remaining tooth substrate are far more important to the long-term prognosis of the restored tooth than any restorative material properties. One must consider that no restorative material can truly substitute for dentin or enamel and that a minimal amount of intact structure is mandatory to justify tooth maintenance and its strategic importance to the overall treatment plan. The presence of healthy adjacent teeth available as abutments or the option of dental implants are additional factors to be analyzed when justifying the restoration of endodontically treated teeth.
Tooth Position, Occlusal Forces, and Parafunctions
Teeth are subjected to cyclic axial and nonaxial forces. The teeth and associated restorations must resist these forces to limit potential damages such as wear or fracture. The degree and direction of forces depend on the location of the tooth in the arch, the occlusal scheme, and the patient’s functional status.
In most occlusal schemes, anterior teeth protect posterior teeth from lateral forces through anterolateral guidance. In the context of very steep anterior guidance and deep vertical overbite, maxillary anterior teeth are sustaining higher protrusive and lateral forces from the mandibular anterior teeth. Restorations of damaged anterior teeth with heavy function should therefore be designed to resist flexion. Restorative components should be stronger than would be required for teeth with an edge-to-edge relationship and therefore vertical forces.
Posterior teeth normally carry more vertical forces, especially when canine and anterior guidance are maintained; they also sustain greater occlusal loads than anterior teeth, and restorations must be planned to protect posterior teeth against fracture. In the case of parafunctions, protection by anterior contacts are likely to be reduced or lost and posterior teeth then submitted to more lateral stresses, generating higher demand for restorative materials.
The literature reports average biting forces varying between 25 and 75 N in the anterior region and between 40 and 125 N for the posterior region of the mouth, depending on food type, dental status (dentate or edentulous), and patient anatomy and functional habits.59,75 Those forces can easily reach 1000 N or above in case of parafunctions, showing how potentially destructive they can be for intact teeth and even more so for nonvital, fragilized teeth. Parafunctional habits (clenching and bruxism) are major causes of fatigue or traumatic injury to teeth, including wear, cracks, and fractures. Teeth that show extensive wear or sequelae from parafunctions, especially heavy lateral function, require components with the highest physical properties to protect restored teeth against fracture.
In general, modern strategy focuses on tissue preservation and also on the use of adhesion to achieve stabilization of the restoration for improved short- and long-term service. However, in certain conditions like reduced tooth support, conventional materials are not obsolete.
Esthetic Evaluation and Requirements
Anterior teeth, premolars, and often the maxillary first molar, along with the surrounding gingiva, compose the esthetic zone of the mouth. Changes in the color or translucency of the visible tooth structure, along with thin soft tissues or biotype, diminish the chance for a successful esthetic treatment outcome.
Potential esthetic complications should be investigated before endodontic therapy is initiated. For instance, metal or dark carbon fiber posts or amalgam placed in the pulpal chamber can result in unacceptable esthetic results, such as a grayish appearance of the overlying prosthetic restoration (especially with modern, more translucent full-ceramic crowns) or gingival discoloration from the underlying cervical area or root (see Fig. 22-1). All teeth located in the esthetic zone also require critical control of endodontic filling materials in the coronal third of the canal and the pulp chamber to avoid or reduce the risk of discoloration. Careful selection of restorative materials, careful handling of tissues, and timely endodontic intervention are important to preserving the natural appearance of nonvital teeth and gingiva.
Treatment Strategy
General Principles and Guidelines
The post, the core, and their luting or bonding agents form together the foundation restoration to support the coronal restoration of endodontically treated teeth. The recent evolution of foundation restorations has been to diminish invasiveness, to use adhesion rather than macromechanical anchorage, and to eliminate intraradicular components in selected cases. These changing clinical concepts derive from both an improved understanding of tooth biomechanics and advances in restorative materials.
The foundation and its different constituents are then aimed at providing the best protection against leakage-related caries, fracture, or restoration dislodgment. Therefore, all aforementioned local and general parameters are to be systematically analyzed in order to select the best treatment approach and restorative materials. Prosthetic requirements are also to be taken into consideration to complete each case analysis. In general, abutments for fixed or removable partial dentures clearly dictate more extensive protective and retentive features than do single crowns, owing to greater transverse and torquing forces. This modern biomechanical treatment strategy is summarized in Fig. 22-5.
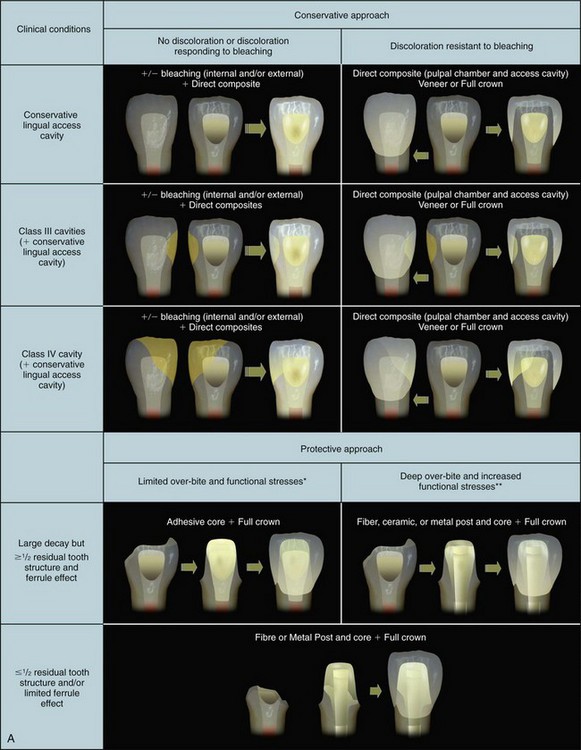
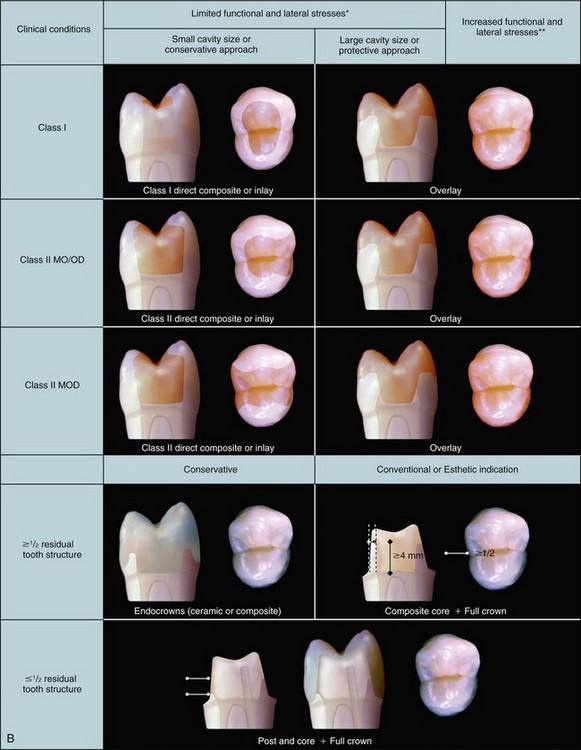
FIG. 22-5 A, Current recommendations for the treatment of nonvital anterior teeth. *Normal function and anterior guidance; **moderate to severe parafunctions and abnormal occlusion/anterior guidance. B, Current recommendations for the treatment of nonvital posterior teeth. *Relatively flat anatomy and canine guidance, normal function; **group guidance, steep occlusal anatomy, parafunctions.
Structurally Sound Anterior Teeth
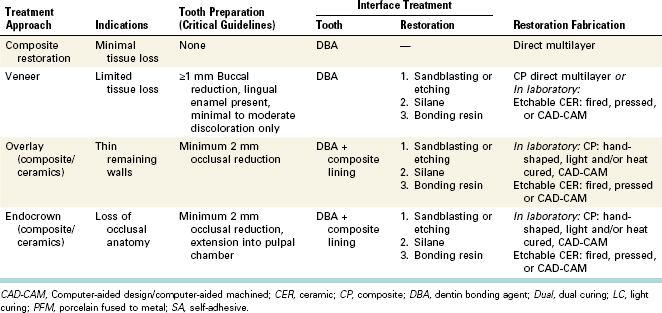
Anterior teeth can lose vitality as a result of a trauma with no or minimal structural damage. They generally do not require a crown, core, or post; restorative treatment is limited to sealing the access cavity and direct composite fillings. Discoloration, whenever present, is addressed by nonvital bleaching, or for untreatable or relapsing ones, with conservative restorative approaches such as direct or indirect veneers (Table 22-2).
Nonvital Posterior Teeth With Minimal/Reduced Tissue Loss
The loss of vitality in posterior teeth resulting from trauma, decay, or restorative procedure does not necessarily lead to extreme biomechanical involvement and therefore allow in certain conditions for conservative restorations.
Occlusal cavities or mesio/disto-occlusal cavities can be restored with either direct- or indirect-adhesive intracoronal restorations, providing residual walls are thick enough (proximal ridges and buccolingual walls more then 1.5 mm thickness). The three additional clinical factors which must be analyzed to ensure optimal treatment success are the configuration factor (C-factor), cavity volume, and dentin quality. For instance, a large class I cavity with contaminated and sclerotic dentin would clearly be a contraindication to the direct approach, despite the fact it apparently falls within the indications of direct techniques. Conservative options must, however, always be analyzed under the light of functional and occlusal environment. They can only be considered in the absence of parafunctions and with anterior guidance, which limits overall functional loading and lateral or flexural forces. In less favorable biomechanical conditions (group guidance, steep occlusal anatomy, bruxism, clenching, etc.), a protective approach with full occlusal coverage (onlay or overlay) is mandated to minimize the risk of fatigue failures (see Table 22-2).
Structurally Compromised Teeth
The decision for placing a post as well as the selection of a post system (rigid or nonrigid) depends once again on the amount and quality of remaining tooth structure and the anticipated forces sustained by this tooth (Table 22-3).
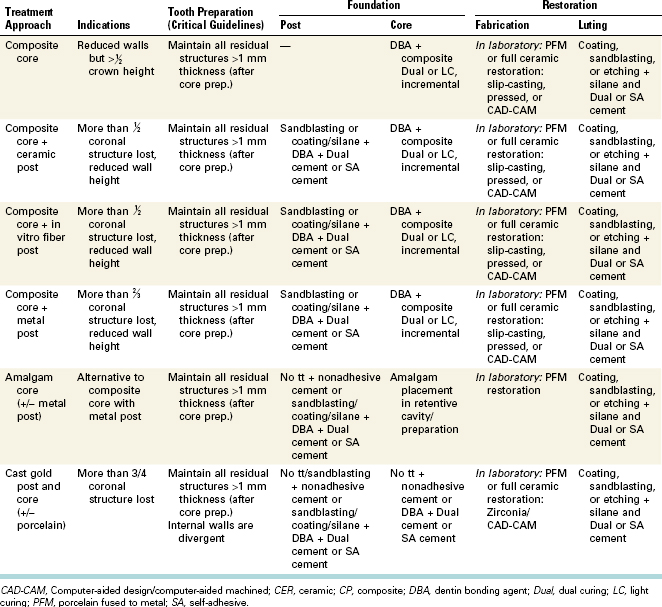
TABLE 22-3 Clinical Protocols for Restoring Nonvital Teeth With Full Prosthetic Restorations (Most Likely Procedures)
In general, rigid posts made of stiff materials (metal and ceramics) are indicated for teeth with minimal tooth structure which rely on the post to hold the core and crown. Because rigid posts flex and bend less than other types of posts, they are supposed to limit movement of the core and possible disruption of the crown margins and cement seal. But one must remember that stiff posts transmit more stresses to the root, next to the post apex, when conventionally cemented. An attempt to strengthen a weak root by adding a stiff post can instead make the root weaker as a result of the force concentration behavior of a stiff rod in a more flexible material. Adhesion therefore plays a crucial role, since a well-bonded post can help absorb stresses more evenly throughout the remaining tooth structure. Benefit and increased risk of fissure and fracture must then be appropriately weighed against adhesion potential inside the root and post type, composition, and surface treatment.
In structurally sound teeth, nonrigid posts flex with the tooth under functional forces, reducing the transfer of force to the root and reducing the risk of root fracture. Flexion is of course related to post diameter. In structurally compromised teeth, which lack cervical stiffness from dentin and ferrule effect, excessive post flexion can be detrimental to the marginal seal and prosthesis longevity, so fiber posts are generally contraindicated.
White or translucent fiber posts are generally preferred underneath full-ceramic restorations, whereas stronger black carbon fiber posts, which can reflect through gingiva, tooth structure, or ceramic restorations, are usually used in teeth to be restored with gold or porcelain fused to metal crowns, as well as in zirconia-based restorations. The literature has largely overemphasized the impact of post color on restoration esthetics. Metal or carbon post color can be masked with resin opaquer and gold post and core ceramized to enhance esthetic integration. Such procedures can help to approach a more ideal restoration biomechanical behavior through the fabrication of rigid but more esthetic foundations. Upper lateral and lower incisors, together with extremely thin biotype, are probably the only real esthetic contraindication for metal or carbon fiber posts.
In cases of extreme tooth fragility secondary to caries, fracture, previous overenlargement of the root canal system, or immaturity, residual root structure can be unified and reinforced with adhesive bonding and composite before placing a normal-diameter post, forming altogether a cohesive unit, as previously described.
In conclusion, in a damaged tooth that is to be restored with a nonrigid post, 2 to 3 mm of cervical tooth structure must ideally remain to allow creation of a restoration as a whole that is resistant to flexion. Teeth with minimal tooth structure and limited ferrule effect need additional cervical stiffness from a more rigid post to resist distortion. In this situation, adhesive cementation is preferred to conventional cementation.
Structurally Compromised Anterior Teeth
Restoration of endodontically treated teeth becomes more complex as teeth or supporting structures become increasingly affected. A nonvital anterior tooth that has lost significant tooth structure requires restoration with a crown, supported and retained by a core and possibly a post as well.
When less than half the core height is present, or when remaining walls are extremely thin (less than 1 mm on more than three-fourths of the tooth circumference), a post is needed to increase retention and stabilize and reinforce the foundation. Many post options are available nowadays, including titanium, fiber-reinforced resin, and ceramics. Adhesion is now the preferred mode of post cementation unless a long-term contamination of root dentin is obvious (e.g., with eugenol), making adhesion highly questionable.
In the latter situation or in the presence of flared canals (possibly as well when a limited ferrule effect is present), cast gold post and core are still considered a feasible option. Actually, in this extremely unfavorable biomechanical environment, this traditional treatment approach provides a higher rigidity in the cervical area, which is mandatory for restoration stability. Here, a fiber-reinforced composite foundation having higher flexibility might present less favorable biomechanical behavior, such as suggested by FEM studies43 (see Fig. 22-3 and Table 22-2). Tooth extraction and implant placement or bonded bridge (particularly for lateral incisors) are also to be considered in this situation.
In the esthetic zone, the post should not detract from the esthetics of the coronal tooth structure, ceramic crown, or gingiva. Current restorative procedures allow fabrication of highly esthetic ceramic coronal restorations that have no metal substructure. When such restorations with remarkable lifelike color and vitality are selected, it usually implies the use of nonmetal esthetic posts, either ceramic or resin fiber-reinforced ones.
Structurally Compromised Posterior Teeth
Slightly decayed posterior teeth in the context of parafunctions or significantly fragilized premolars and molars require cuspal protection afforded by onlay restoration, endocrown, or a full crown. The need for a post and core depends on the amount of remaining tooth structure. When remaining walls (buccal and lingual) provide more than 3 to 4 mm height (from pulpal chamber floor) and 1.5 to 2 mm thickness, core and restoration stability are granted through macromechanical retention and/or adhesion; then, posts are not needed (see Fig. 22-5). With current treatment strategy, the post has become the exception rather than the rule for the restoration of nonvital posterior teeth.
Additional Procedures
Periodontal crown lengthening surgery or orthodontic extrusion can expose additional root structure to allow restoration of a severely damaged tooth. In the smile frame, crown lengthening might however be limited by esthetic adverse consequences (proximal attachment reduction); basically, buccal crown lengthening only can be considered as a potential indication for this procedure. In the posterior region, crown lengthening is limited by tooth and furcation anatomy or by loss of bone structure, which complicates future implant placement. As regards to orthodontic extrusion, root length and anatomy are the limiting factors of this procedure; short roots or conical anatomy are contraindications to orthodontic extrusion. Once again, when a long-lasting, functional restoration cannot be predictably created, tooth extraction might be better than to pursue heroic efforts to restore extremely weak teeth, using complex, expensive, and unpredictable procedures.
Clinical Procedures
The restoration of a nonvital tooth may include several restorative components such as the post, the core, and the overlying restoration. Within the same tooth, several interfaces such as post to radicular dentin, core to coronal dentin, core to post, and core to overlying restoration will be created. According to the biomechanical status, some or all restorative components and interfaces will be present and need to be addressed.
General clinical guidelines for restoring endodontically treated teeth with either partial or full crown restorations are presented in Table 22-2, with specific procedures for tooth preparation and treatment of the different interfaces involved. Clinical steps for all recommended treatment options are presented in Figs. 22-6 through 22-14.
Tooth Preparation
The most important part of the restored tooth is the tooth itself. As described earlier, thickness and height of remaining dentin walls or cusps along with functional occlusal conditions are the determining factors in choosing the most appropriate restorative solution.
For partial intracoronal restorations, maximal tissue conservation is the only consideration for the clinician. In other situations, the selected restorative approach will usually necessitate some tooth preparation to comply with restoration design and thickness. Onlays, overlays, and endocrowns require about 1.5 to 2 mm occlusal space to guarantee restoration resistance to functional loads. For full crowns, a ferrule is needed to encircle the vertical walls of sound tooth structure above the restoration margin (1.5 to 3 mm), thus preventing a coincidence between core and restoration limits. Other preparation requirements presented in this chapter are to be respected to ensure treatment success. This means that a 4- to 5-mm height and 1-mm thickness of sound, suprabony tooth structure should be available to accommodate both the periodontal biologic width and the restorative ferrule.
Post Placement
The post is an extension of the foundation into the root of structurally damaged teeth, needed for the core and coronal restoration stability and retention. The post is cemented or bonded into the root, according to tissue quality and post and core choice. The post performs both a mechanical and biologic function by protecting the apical seal from bacterial contamination in case of coronal leakage. These functions should not be attained at the expense of tooth strength; post space preparation should be as conservative as possible to avoid an increased risk of root fracture. It is important to point out again that a post does not strengthen or reinforce a tooth. This elusive goal would only be achieved in a case of perfect cohesion between post and tooth substrate, nowadays only partially achievable. Therefore, the clinician must keep in mind that inherent strength of the tooth and its resistance to root fracture comes mostly from the remaining tooth structure and the surrounding alveolar bone. The tooth is weakened if dentin is sacrificed to place a larger-diameter post.
The post should be long enough to meet aforementioned biomechanical demands without jeopardizing root integrity. The standard parameters for post placement in a tooth with normal periodontal support are:
The first step for all types of post and core restorations is removal of gutta-percha and endodontic cement from the future post space. This procedure generally is best accomplished by the clinician providing the endodontic service, because that person has a clear knowledge of the size and form of the canal system. The initial post space preparation procedure is similar for most standardized post and core systems. The space, cleared of gutta-percha, has the form of the canal after cleaning and shaping. Proprietary systems are supplied with a series of drills to prepare the internal surface of the canal. The goal of post space formation is to remove little or no dentin from the root canal.
Adhesive Procedures
In general, both self-etch and etch-and-rinse adhesive systems can be used successfully on root dentin, both systems having a well-documented proof of efficacy. However, the use of etch-and-rinse adhesive systems may be advantageous in the presence of highly sclerotic or contaminated dentin, because phosphoric acids will etch dentin more deeply than self-etching primers. When treating the canal in the perspective of post cementation, a dual-curing adhesive system is preferably used to optimize polymerization. Self-adhesive cements have also demonstrated satisfactory performance for post cementation.
Partial Restorations
In the case of limited to moderate coronal substance loss, the restorative strategy for endodontically treated front teeth varies, from direct composite restoration using the same layering or application techniques as for vital teeth (possibly with the contribution of intracoronal or extracoronal bleaching) to full veneers, when discoloration is not fully treatable or tends to relapse. From a restorative standpoint, it is only necessary to mention that a 1- to 2-week delay is mandatory prior to adhesively restoring a bleached tooth. For more extensive restoration, it is even advised to wait up to 6 weeks or more (depending on the extent and duration of bleaching treatment) to allow for tooth final color stabilization and to proceed with shade selection.40 Figs. 22-6 and 22-7 describe the clinical steps involved in the restoration of moderately decayed front teeth using direct composite and bleaching or veneers.

FIG. 22-6 Direct composite restorations on front teeth (following bleaching). Nonvital anterior tooth with sufficient amount of residual tissue and intact, healthy neighboring teeth, usually in rather young patients. A, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha were removed from the cavity to expose a clean dentin substrate. Opaque cement can be used to mark the entrance of the roots to facilitate eventual retreatment or for the later placement of a post. B, Bleaching procedures. Two sessions of internal bleaching were needed to adapt the color of both traumatized anterior teeth (tooth #11), using a mixture of 3% hydrogen peroxide and sodium perborate powder. Each bleaching session extended over a 10-day period. Between sessions and until the given delay to proceed with final restoration (1 to 2 weeks up to 6 to 8 weeks), access cavity is closed with either a temporary filling material or flowable resin composite. C-D, Restorative procedures. A layer of adhesive is applied over all cavity surfaces. An etch-and-rinse system is frequently preferred when the dentinal tissue is highly sclerotic or was contaminated (e.g., by eugenol). A hard cement such as glass ionomer (not a resin-modified glass ionomer because of water uptake and further expansion) was used for dentin replacement, before adding enamel composite to close the lingual cavity. A full resin composite restoration can also be considered to fill in the lingual cavity (dentin + enamel masses) in consideration of the material’s hydrophobic nature, which could presumably prevent or limit penetration of water-soluble pigments from the oral cavity. Two or three layers are usually used to replace the missing tissue, preferably following the “natural layering concept,” which aims to build up the restoration with two basic masses, namely dentin and enamel, with help of a silicone index. E-F, Postoperative views. The two conservative restorations are shown after finishing and polishing, with rubber dam still in place (E) and after several weeks (F). Note that esthetic integration can not be evaluated before full rehydration has occurred (4 to 6 hours at least).

FIG. 22-7 Direct composite restoration on posterior tooth. Nonvital posterior tooth with sufficient amount of residual tissue and mostly intact, rather healthy neighboring teeth. No significant discoloration of buccal tooth substrate and absence of severe parafunctions and/or group guidance or other unfavorable occluso-functional condition. A, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. Opaque cement can be used to mark the entrance of the roots to facilitate eventual retreatment or for a later placement of a post. B, Adhesive procedure. An etch-and-rinse adhesive system was used here owing to the presence of sclerotic and contaminated dentin. C-E, Restoration base and layering technique. Resins or glass ionomer cements can be used for dentin replacement, before adding enamel composite to close the lingual cavity. A full resin composite restoration can also be considered to fill in the lingual cavity (dentin + enamel masses) in consideration of the material’s hydrophobic nature, which could presumably prevent or limit penetration of water-soluble pigments from the oral cavity. A dentin composite mass is used to replace missing dentinal tissue, and enamel composite is used to build up proximal walls and the occlusal anatomy. F, Postoperative view. The postoperative view demonstrates the advantage of this conservative approach in the context of teeth with appropriate biomechanical status.
In posterior teeth exhibiting limited to moderate tissue loss, direct to indirect partial or full occlusal restorations are proposed. Their benefit is to take advantage of residual tooth structure to stabilize the restoration and minimize the potential impact of a prosthetic rehabilitation on periodontal tissues. For instance, second molars definitely profit from a conservative approach using adhesively luted intracoronal and full occlusal coverage restorations. Endocrown is a modification of the aforementioned concept, with extension of the restoration into the pulpal chamber as additional retentive and stabilization structure. Figs. 22-8, 22-9, and 22-10 describe the clinical steps involved in the restoration of moderately decayed posterior teeth using onlays, overlays, and endocrowns.

FIG. 22-8 Veneer. Nonvital anterior tooth with sufficient amount of residual tissue and rather healthy neighboring teeth. Discoloration resisted bleaching or relapsed, despite several retreatments. Preferably thick biotype to limit the risk of gingival recession and loss of esthetic integration. A, Closing the lingual cavity. A hard cement such as glass ionomer (not resin-modified glass ionomer because of water uptake and possible expansion) can be used for dentin replacement, before adding enamel composite to close the lingual cavity. A full resin composite restoration can also be considered to fill in the lingual cavity (dentin + enamel masses) in consideration of the material’s hydrophobic nature, which could presumably prevent or limit penetration of water-soluble pigments from the oral cavity. B, Preparation. A sufficient amount of buccal tooth structure must be removed to allow for a good esthetic result (preparation depth is dictated by the discoloration severity). Cervical margins closely follow gingival contours, preventing soft-tissue impingement, but they assume complete coverage of discolored tooth structure. C-D, Adhesive procedure. Hydrophobic bonding systems are preferred to wet-etched enamel when no dentin is exposed. An etch-and-rinse adhesive system is preferred when dentin is exposed (here, in the presence of significant areas of sclerotic dentin). Restoration. Ceramic is etched and silanated. Just before cementation, a last layer of bonding resin is applied but not light-cured until placement. E, Luting technique. A light-curing, highly filled, translucent and fluorescent restorative material is preferably used for cementation. This allows better control of restoration placement and minimal wear and fatigue of the cement layer. F, Postoperative view. The postoperative view demonstrates satisfactory esthetics. This approach is sometimes suitable to meet patient’s high esthetic demands.
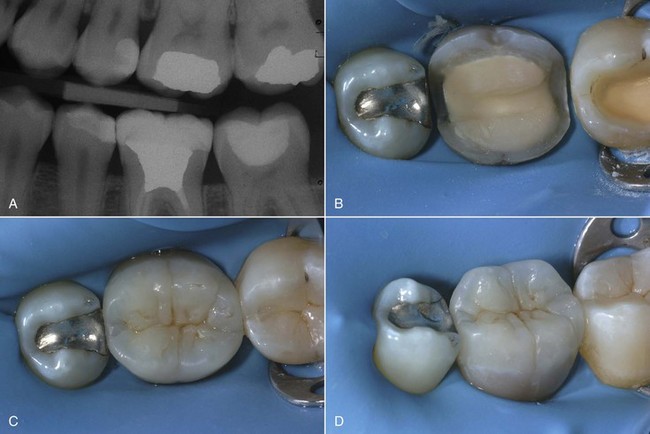
FIG. 22-9 Onlay/Overlay. Nonvital posterior tooth with sufficient amount of residual tissue to justify partial restoration. Preparation involves both proximal surfaces or only two surfaces, but in a less favorable occluso-functional environment (thin walls). No significant discoloration of visible buccal tooth substrate. Option is favorable for short clinical crowns. A-B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. Opaque cement can be used to mark the entrance of the roots to facilitate eventual retreatment or for the later placement of a post. Thin and weak occlusal walls are removed until reaching sufficient thickness for the restoration (1.5 to 2 mm in occlusal-free and occlusal areas, respectively). Adhesive procedure: an etch-and-rinse adhesive system is preferably used here owing to the presence of sclerotic and contaminated dentin (a self-etch adhesive system can also be used). A resin composite base is made with a restorative composite or preferably with flowable composite (for limited volume and thickness) to smooth internal angles, fill undercuts, and when needed, to relocate cervical margins occlusally. C-D, After impression and model fabrication, the restoration is generated in the laboratory to optimize restoration anatomy, function, and esthetics. The restoration can be made of different tooth-colored materials: ceramics (fired, pressed, or CAD-CAM generated) or resin composite. This treatment option provides optimal tissue conservation, function, and esthetics and is a good alternative to full crowns.

FIG. 22-10 Endocrown. Nonvital posterior tooth with reduced amount of residual cervical tissue but sufficient to provide supragingival restoration margins and good stabilization within former pulpal chamber. No or limited discoloration in visible buccal tooth substrate. Favorable option for short clinical crowns. A-B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. Opaque cement can be used to mark the entrance of the roots to facilitate eventual retreatment or for the later placement of a post. Thin and weak walls are removed until reaching sufficient thickness (1.5 mm minimum); as much residual cervical structure as possible is then maintained to avoid restoration interference with periodontal tissues. C, Prosthetic restoration on working model. D, Restoration base. Adhesive procedures: An etch-and-rinse adhesive system is preferably used here owing to the presence of sclerotic and contaminated dentin (a self-etch adhesive system can also be used). Restoration base: A resin composite base is made with a restorative composite or preferably with flowable composite (for limited volume and thickness) to smooth internal angles, fill undercuts, and when needed, to relocate cervical margins occlusally. E, Impression and restoration fabrication. After impression and model fabrication, the restoration is generated in the laboratory to optimize restoration anatomy, function, and esthetics. The restoration can be made of different tooth-colored materials: ceramics (fired, pressed, or CAD-CAM generated) or resin composite. F, Postoperative result. Despite their relatively rare application, endocrowns combine biomechanical advantages with facilitation of clinical procedures and minimal if any involvement of biologic width. It is an interesting alternative to full crowns.
(From Rocca GT, Bouillaguet S: Alternative treatments for the restoration of nonvital teeth. Rev Odont Stomat 37:259–272, 2008.)
Foundation Restoration Underneath Full Crowns
If significant coronal substance loss justifies a full-tooth coverage, the strategy for foundation fabrication varies from:
Amalgam Core
A coronal-radicular amalgam foundation may be realized with or without post (Figs. 22-11 through 22-14). The amalgam coronal-radicular core without post is indicated for posterior teeth that have a large pulp chamber and lateral walls at least 4 mm high. This restoration extends slightly into the coronal portion of the canals (1 to 1.5 mm). The core is then retained by a combination of the divergence of the canals and natural undercuts in the pulp chamber. A single, homogenous material is used for the entire restoration, rather than the dual phases of a conventional preformed post and core.

FIG. 22-11 Amalgam core. Nonvital posterior teeth with reduced tooth structure and wall height. Amalgam core stability is granted by extension of the restoration into the coronal portion of the canal (curved roots) and post (only if straight root anatomy) and remaining pulpal chamber undercuts. Today, this option is considered obsolete or historical because of the intrinsic staining of amalgam, the nonadhesive technique, and the less-than-ideal biomechanical behavior of amalgam. A-B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. Thin and weak walls are removed until reaching sufficient thickness (1.5 to 2 mm); existing retentions are used to stabilize the amalgam core, together with a post. The metal post (with passive and anatomic design, preferably made of titanium) extends into the root for about the same length as its coronal extension. C-E, Restoration fabrication. After placing a matrix or cupper ring to envelop the preparation, amalgam is compacted into the cavity, superior root canal portion and around the post, until restoring the appropriate coronal volume. Preparation of cores is made to manage optimal space for PFM crowns. F, Posttreatment result. This treatment approach is feasible for teeth already restored with amalgam cores and when PFM restorations are mandated. Satisfactory esthetics can be attained with intrasulcular restoration margins.
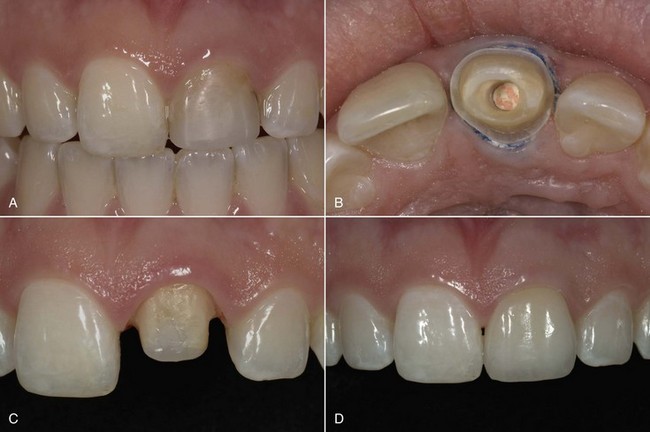
FIG. 22-12 Composite core (without post). Nonvital tooth with more than half the coronal structure left and sufficient wall thickness. Core stability is granted by adhesion, remaining pulpal chamber, and residual wall height. A-B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. The tooth is prepared to evaluate precisely the height and thickness of residual tooth structure. Half of the abutment height and more than 1.5 mm wall thickness must be present to restore the tooth without post. If aforementioned conditions are met, a thin layer of hard cement (calcium hydroxide, zinc phosphate, or glass ionomer; not resin-modified glass ionomer) is applied at the entrance of the root canal to enable possible retreatment in the future. C, Adhesive procedures and core fabrication. All walls are covered with the adhesive system (etch-and-rinse or self-etch) before applying in layers a direct light-curing restorative composite or a self-curing material, in case of limited restoration volume. D, Postoperative view. The advantage of this approach is the ease of application and excellent esthetics. It is considered a good restorative solution for highly esthetic ceramic crowns placed on teeth with limited tissue loss and discoloration.

FIG. 22-13 Composite core with white post (resin reinforced fiber or zirconia post). Nonvital tooth with less than half the coronal structure left and/or insufficient wall thickness. Core stability is improved through adhesion and a tooth-colored post (resin reinforced fiber or ceramic posts). A, Preoperative view. B-C, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose a clean dentin substrate. The tooth is prepared to evaluate precisely the height and thickness of residual tooth structure. If less than half of the abutment height or 1.5 mm wall thickness remain, the abutment requires a post to increase core retention and foundation stability. D-E, Post-and-core fabrication. Post placement: The post space is prepared with ad hoc instruments until reaching a length equivalent to core height or slightly less depending on remaining wall height. Increased length is not needed, since retention is predominantly achieved through adhesion. Any tooth-colored post can be used, but fiber posts are usually preferred to limit stress buildup into the root structure, even though they provide less rigidity to the foundation. Post cementation: A self-curing adhesive system is applied on all cavity walls and into post preparation before luting the post with a dual-cured composite cement or, as a simple alternative, a self-adhesive cement (then, no adhesive is used). Core fabrication: The remaining core volume is built up in layers, using a direct light-curing restorative composite or with a single increment of a self-curing material when only limited volume is to be completed. F, Postoperative view. The primary advantage of this approach is the excellent esthetic outcome. It is considered a good restorative solution for highly esthetic ceramic crowns placed on teeth with more tissue loss but moderate discoloration.

FIG. 22-14 Composite core with prefabricated metal post. Nonvital tooth with reduced coronal structure and ferrule effect and/or insufficient wall thickness. Core stability is improved through adhesion and a metal (opacified) post (titanium posts are usually preferred). A, Preoperative view. B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose remaining tooth structure and a clean dentin substrate. The absence of coronal tissue and ferrule effect mandates the use of a more rigid post (ceramic posts are considered too rigid and contraindicated in this situation). C-F, Post and core fabrication. Post space preparation: The post space is prepared with ad hoc instruments until reaching a length equivalent to about core height. More length is not needed, since retention is predominantly achieved through adhesion. Post preparation: The metal post (titanium here) is sandblasted (silicoating can be used to increase adhesion; i.e., Rocatec or CoJet systems, 3M), followed by silane application. An opaque resin or flowable composite can be used to mask metal dark color and improve esthetics. Post cementation: A self-curing adhesive system is applied on all cavity walls and into post preparation before luting the post with a dual-cured composite cement or, as a simple alternative, a self-adhesive cement (then, no adhesive is used). Core fabrication: The remaining core volume is built up in layers, using a direct light-curing restorative composite or a single increment of a self-curing material when only limited volume is to be completed.
When shorter lateral walls are present, a post is mandatory to improve core stability and retention. The preferred roots for post placement for molars are the palatinal root in the upper jaw and the distal root in the lower jaw. Other roots, thinner and presenting more pronounced curvatures, are normally not indicated for post placement. Coronal-radicular amalgam foundations are not indicated for premolars owing to their smaller dimensions; adhesive foundations or cast gold post and core are preferred.
Cast Gold Post and Core
Cast gold post and core restorations can be fabricated with either direct or indirect techniques.
Direct Technique
In the direct technique, a castable post and core pattern is fabricated in the mouth on the prepared tooth. A preformed plastic post pattern is seated in the post space. To gain a path of withdrawal, undercuts are blocked out with resin composite rather than by removing healthy dentin structure. Acrylic resin is added to create a core directly attached to the post pattern. The finished pattern is removed from the tooth and cast in the laboratory.
Indirect Technique
With the indirect technique, a final impression of the prepared tooth and post space is made (Fig. 22-15). As with the direct technique, the path of withdrawal is made by undercut blockout, not by dentin removal. The castable final post and core pattern are fabricated on a die from this impression. The crown margins need not be accurately reproduced at this stage. Proprietary systems provide matched drills, impression posts, and laboratory casting patterns of various diameters. An impression post (preferably a repositionable one) is fitted to the post space, and a final impression is made that captures the form of the remaining coronal tooth structure and picks up the impression post. In the laboratory, a die reproduces the post space and the residual coronal tooth structure for fabrication of the post and core pattern.

FIG. 22-15 Nonvital teeth with limited coronal structure and/or numerous abutments. Indirect post and core fabrication helps to achieve proper parallelism and core anatomy. Core retention is assumed by a conventional or adhesive cement. Today, this solution is considered mostly for extended metal-ceramic restorations or sometimes for multiple full-ceramic restorations. A, Preoperative view. B, Preparation. Existing restorative material and all remnants of endodontic sealer and gutta-percha are removed from the cavity to expose remaining tooth structure and a clean dentin substrate. Despite the indirect approach, all healthy coronal structures must be maintained to improve foundation stability. Access cavity and coronal walls are prepared with minimal convergence (6 to 10 degrees) to allow for easy insertion. C-D, Cast gold post and core fabrication and luting. Post space preparation: The post space is prepared with ad hoc instruments until reaching a length equivalent to about core height or more. More length is needed here, since retention cannot always be achieved through adhesion (endodontic retreatment or highly sclerotic contaminated dentin). Then a conventional glass ionomer or zinc phosphate cement is used.
Post and core preparation: The gold post is sandblasted (or eventually sandblasted and coated if adhesive procedures are possible) using Rocatec or CoJet systems, 3M + silane. Post cementation: The post and core is luted with the aforementioned conventional cements or adhesive technique. Next, a self-curing adhesive system is applied on all cavity walls and into post preparation (before the insertion of the post and core) and covered with a dual-cured composite cement or, as a simple alternative, a self-adhesive cement (then, no adhesive is used). E-F, Restoration fabrication and placement. A second impression is needed for the final prosthetic work to optimize restoration precision and quality. Lab-made PFM or full ceramic crowns are made with optimal foundation design and alignment.
With both techniques, the fabrication of a temporary crown with intraradicular retention is needed. This provisional restoration must stay only for a limited time in the mouth to prevent decementation or canal reinfection. This is why this approach is less popular today and replaced by direct techniques in most cases.
The cast post and core is cemented at the second appointment. The cementation process must be passive in nature and an evacuation groove made on post side to facilitate cement expulsion and limit seating pressure. Rapid seating, excessive cement, and heavy seating pressure (e.g., occlusal force) can produce high hydraulic pressures inside the root that may be great enough to crack the root.
Crown Preparation and Temporary Restoration
When a coronal restoration is indicated, the amount of tooth structure remaining after final preparation is the most important determinant of the design of the post and core. In addition, the underlying sound tooth structure provides greater resistance to fracture than any post and core type, design, or material. Natural tooth structure should always be carefully preserved during all phases of post space and crown preparation. Otherwise, preparation of endodontically treated teeth is not different from vital teeth, with the exception of severely discolored teeth, which require a slightly deeper chamfer to hide discoloration with the prosthetic structure and intrasulcular margins to reduce the visibility of dark cervical tooth structure.
Provisional crowns for endodontically treated teeth must be used only for short periods of time because the loss of cement seal—which is of course symptom free—can lead to leakage, canal reinfection, and even serious carious invasion, thereby jeopardizing the success of endodontic treatment and even result in tooth loss.
Summary
Endodontically treated teeth represent a singular situation because of the attendant qualitative and quantitative alterations of the dental substrate. Current literature indicates that treatment success relies on an effective coronal seal that will prevent canal reinfection and an adequate restoration that will resist functional stresses applied to the remaining tooth structure. The purpose of this chapter is to help the clinician make decisions about the restorative options available to restore endodontically treated teeth with predictable clinical results.
1. Akgungor G, Sen D, Aydin M. Influence of different surface treatments on the short-term bond strength and durability between a zirconia post and a composite resin core material. J Prosthet Dent. 2008;99:388-399.
2. Al-Wahadni A, Gutteridge DL. An in vitro investigation into the effects of retained coronal dentine on the strength of a tooth restored with a cemented post and partial core restoration. Int Endod J. 2002;35:913-918.
3. Anusavice KJ, editor. Phillips’ science of dental materials, 11th ed, St. Louis: Saunders, 2003.
4. Aversa R, Apicella D, Perillo L, et al. Non-linear elastic three-dimensional finite element analysis on the effect of endocrown material rigidity on alveolar bone remodeling process. Dent Mater. 2009;25:678-690.
5. Balbosh A, Kern M. Effect of surface treatment on retention of glass-fiber endodontic posts. J Prosthet Dent. 2006;95:218-223.
6. Barkhodar RA, Radke R, Abbasi J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent. 1989;61:676.
7. Barkhodar RA, Radke R, Abbasi J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent. 1989;61:676.
8. Belli S, Zhang Y, Pereira PN, Ozer F, Pashley DH. Regional bond strengths of adhesive resins to pulp chamber dentin. J Endod. 2001;27:527-532.
9. Bergman B, Lundquist P, Sjögren U, Sundquist G. Restorative and endodontic results after treatment with cast posts and cores. J Prosthet Dent. 1989;61:10-15.
10. Bindl A, Richter B, Mormann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int J Prosthodont. 2005;18:219-224.
11. Bitter K, Paris S, Mueller J, Neumann K, Kielbassa AM. Correlation of scanning electron and confocal laser scanning microscopic analyses for visualization of dentin/adhesive interfaces in the root canal. J Adhes Dent. 2009;11:7-14.
12. Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003;89:268-274.
13. Boschian Pest L, Cavalli G, Bertani P, Gagliani M. Adhesive post-endodontic restorations with fiber posts: push-out tests and SEM observations. Dent Mater. 2002;18:596-602.
14. Bouillaguet S, Bertossa B, Krejci I, Wataha JC, Tay FR, Pashley DH. Alternative adhesive strategies to optimize bonding to radicular dentin. J Endod. 2007;33:1227-1230.
15. Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003;19:199-205.
16. Bowen RL, Rodriguez MS. Tensile strength and modulus of elasticity of tooth structure and several restorative material. J Am Dent Assoc. 1962;64:378-387.
17. Bower RC. Furcation morphology relative to periodontal treatment. J Periodontol. 1979;50:366-374.
18. Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24:90-101.
19. Butz F, Lennon AM, Heydecke G, Strub JR. Survival rate and fracture strength of endodontically treated maxillary incisors with moderate defects restored with different post-and-core systems: an in vitro study. Int J Prosthodont. 2001;14:58-64.
20. Carrigan PG, Morse DR, Furst L, Sinai JH. A scanning electron microscopic evaluation of human dentinal tubules according to age and location. J Endod. 1984;10:359-363.
21. Carrilho MR, Carvalho RM, de Goes MF, et al. Chlorhexidine preserves dentin bond in vitro. J Dent Res. 2007;86:90-94.
22. Carrilho MR, Tay FR, Donnelly AM, et al. Host-derived loss of dentin matrix stiffness associated with solubilization of collagen. J Biomed Mater Res B Appl Biomater. 2008 Dec 17. [Epub ahead of print.]
23. Carrilho MR, Tay FR, Pashley DH, Tjäderhane L, Carvalho RM. Mechanical stability of resin-dentin bond components. Dent Mater. 2005;21:232-241.
24. Cathro PR, Chandler NP, Hood JA. Impact resistance of crowned endodontically treated central incisors with internal composite cores. Endod Dent Traumatol. 1996;12:124-128.
25. Ceballos L, Garrido MA, Fuentes V, Rodríguez J. Mechanical characterization of resin cements used for luting fiber posts by nanoindentation. Dent Mater. 2007;23:100-105.
26. Chiba M, Itoh K, Wakumoto S. Effect of dentin cleansers on the bonding efficacy of dentin adhesive. Dent Mater. 1989;8:76-85.
27. Christensen G. Core buildup and adhesive incompatibility. Clin Res Assoc Newsl. 2000;24:6.
28. Christensen G. Posts: a shift away from metal? Clin Res Assoc Newsl. 2004;28:1.
29. Cobankara FK, Unlu N, Cetin AR, Ozkan HB. The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper Dent. 2008;33:526-533.
30. Cohen BI, Pagnillo MK, Newman I, Musikant BL, Deutsch AS. Retention of a core material supported by three post head designs. J Prosthet Dent. 2000;83:624-628.
31. Combe EC, Shaglouf AM, Watts DC, Wilson NH. Mechanical properties of direct core build-up materials. Dent Mater. 1999;15:158-165.
32. Council on Dental Materials, Instruments, and Equipment, American Dental Association. Classification system for cast alloys. J Am Dent Assoc. 1984;109:766.
33. Craig RG, Peyton FA. Elastic and mechanical properties of human dentin. J Dent Res. 1958;52:710-718.
34. Cruz-Filho AM, Souza-Neto MD, Saquy PC, Pecora JD. Evaluation of the effect of EDTAC, CDTA and EGTA on radicular dentin microhardness. J Endod. 2001;27:183-184.
35. Dahl JE, Pallesen U. Tooth bleaching—a critical review of the biological aspects. Crit Rev Oral Biol Med. 2003;14:292-304.
36. D’Arcangelo C, D’Amario M, Vadini M, De Angelis F, Caputi S. Influence of surface treatments on the flexural properties of fiber posts. J Endod. 2007;33:864-867.
37. Davidson CL, Feilzer AJ. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J Dent. 1997;25:435-440.
38. Deliperi S, Bardwell DN. Reconstruction of nonvital teeth using direct fiber-reinforced composite resins: a pilot clinical study. J Adhes Dent. 2009;11:71-78.
39. Denry IL. Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med. 1996;7:134-143.
40. Dietschi D, Ardu S, Krejci I. A new shading concept based on natural tooth color applied to direct composite restorations. Quintessence Int. 2006;37:91-102.
41. Dietschi D, Ardu S, Rossier-Gerber A, Krejci I. Adaptation of adhesive post and cores to dentin after in vitro occlusal loading: evaluation of post material influence. J Adhes Dent. 2006;8:409-419.
42. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth:a systematic review of the literature–Part 1—Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38:733-743.
43. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II—Evaluation of fatigue behavior, interfaces, and in vivo studies. Quintessence Int. 2008;39:117-129.
44. Dietschi D, Romelli M, Goretti A. Adaptation of adhesive posts and cores to dentin after fatigue testing. Int J Prosthodont. 1997;10:498-507.
45. Douglas WH. Methods to improve fracture resistance of teeth. In: Vanherle G, Smith DC, editors. Proceedings of the international symposium on posterior composite resin dental restorative materials. Peter Szulc Publishing; 1985:433-441.
46. Drummond JL, King TJ, Bapna MS, Koperski RD. Mechanical property evaluation of pressable restorative ceramics. Dent Mater. 2000;16:226-233.
47. Drummond JL, Toepke TR, King TJ. Thermal and cyclic loading of endodontic posts. Eur J Oral Sci. 1999;107:220.
49. Drummond JL. In vitro evaluation of endodontic posts. Am J Dent. 2000;13:5B-8B.
50. Duncan JP, Pameijer CH. Retention of parallel-sided titanium posts cemented with six luting agents: an in vitro study. J Prosthet Dent. 1998;80:423-428.
51. Duret B, Reynaud M, Duret F. New concept of coronoradicular reconstruction: the Composipost (1). Chir Dent Fr. 1990;60:131-141.
52. Duret B, Reynaud M, Duret F. Un nouveau concept de reconstitution corono-radiculaire: le composipost (1). Chir Dent Fr. 1990;540:131-141.
53. Feilzer A, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res. 1987;66:1636-1639.
54. Feilzer A, De Gee AJ, Davidson CL. Setting stresses in composite for two different curing modes. Dent Mater. 1993;9:2-5.
56. Ferrari M, Cagidiaco MC, Goracci C, et al. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007;20:287-291.
57. Ferrari M, Vichi A, Mannocci F, Mason PN. Retrospective study of the clinical performance of fiber posts. Am J Dent. 2000;13(Spec No):9B-13B.
59. Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79:1519-1524.
60. García-Godoy F, Tay FR, Pashley DH, Feilzer A, Tjäderhane L, Pashley EL. Degradation of resin-bonded human dentin after 3 years of storage. Am J Dent. 2007;20:109-113.
61. Gelb MN, Barouch E, Simonsen RJ. Resistance to cusp fracture in Class II prepared and restored premolars. J Prosthet Dent. 1986;55:184-185.
62. Göhring TN, Peters OA. Restoration of endodontically treated teeth without posts. Am J Dent. 2003;16:313-317.
63. Gohring TN, Roos M. Inlay-fixed partial dentures adhesively retained and reinforced by glass fibers: clinical and scanning electron microscopy analysis after five years. Eur J Oral Sci. 2005;113:60-69.
64. Goodacre CJ, Spolnik KJ. The prosthodontic management of endodontically treated teeth: a literature review. II. Maintaining the apical seal. J Prosthodont. 1995;4:51.
65. Goracci C, Tavares AU, Fabianelli A, et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112:353-361.
66. Grandini S, Goracci C, Monticelli F, Borracchini A, Ferrari M. SEM evaluation of the cement layer thickness after luting two different posts. J Adhes Dent. 2005;7:235-240.
67. Grandini S, Goracci C, Monticelli F, Tay FR, Ferrari M. Fatigue resistance and structural characteristics of fiber posts: three-point bending test and SEM evaluation. Dent Mater. 2005;21:75-82.
68. Grigoratos D, Knowles J, Ng YL, Gulabivala K. Effect of exposing dentin to sodium hypochlorite on itsd flexural strength and elasticity modulus. Int J Endod J. 2001;34:113-119.
69. Gutmann JL. The dentin root complex: anatomic and biologic considerations in restoring endotontically treated teeth. J Prosthet Dent. 1992;67:458-467.
70. Hagge MS, Wong RD, Lindemuth JS. Retention strengths of five luting cements on prefabricated dowels after root canal obturation with a zinc oxide/eugenol sealer: 1. Dowel space preparation / cementation at one week after obturation. Prosthodont. 2002;11:168-175.
71. Hattab FN, Qudeimat MA, al-Rimawi HS. Dental discoloration: an overview. J Esthet Dent.. 1999;11:291-310.
72. Hawkins CL, Davies MJ. Hypochlorite-induced damage to proteins: formation of nitrogen-centred radicals from lysine residues and their role in protein fragmentation. Biochem J. 1998;332:617-625.
73. Helfer AR, Melnick S, Shilder H. Determination of the moisture content of vital and pulpless teeth. Oral Surg Oral Med Oral Pathol. 1972;34:661-670.
74. Herr P, Ciucchi B, Holz J. Méthode de positionnement de répliques destinée au contrôle clinique des matériaux d’obturation. J Biol Buccale. 1981;9:17-26.
75. Hidaka O, Iwasaki M, Saito M, Morimoto T. Influence of clenching intensity on bite force balance, occlusal contact area, and average bite pressure. J Dent Res. 1999;78:1336-1344.
76. Hikita K, Van Meerbeek B, De Munck J, et al. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23:71-80.
77. Holand W, Rheinberger V, Apel E, et al. Clinical applications of glass-ceramics in dentistry. J Mater Sci Mater Med. 2006;17:1037-1042.
78. Hood JAA. Methods to improve fracture resistance of teeth. In: Vanherle G, Smith DC, editors. Proceedings of the international symposium on posterior composite resin dental restorative materials. Utrecht, Netherlands: Peter Szulc Publishing; 1985:443-450.
79. Huang TJ, Shilder H, Nathanson D. Effect of moisture content and endodontic treatment on some mechanical properties of human dentin. J Endod. 1992;18:209-215.
80. Huber L, Cattani-Lorente M, Shaw L, Krejci I, Bouillaguet S. Push-out bond strengths of endodontic posts bonded with different resin-based luting cements. Am J Dent. 2007;20:167-172.
81. Hulsmann M, Heckendorf M, Shafers F. Comparative in-vitro evaluation of three chelators pastes. Int Endod J. 2002;35:668-679.
82. Hulsmann M, Heckendorff M, Lennon A. Chelating agents in root canal treatment: mode of action and indications for their use. Int Endod J. 2003;36:810-830.
83. Isidor F, Brondum K. Intermittent loading of teeth with tapered, individually cast or prefabricated, parallel-sided posts. Int J Prosthodont. 1992;5:257-261.
84. Isidor F, Brøndum K, Ravnholt G. The influence of post length and crown ferrule length on the resistance to cyclic loading of bovine teeth with prefabricated titanium posts. Int J Prosthodont. 1999;12:78-82.
87. Kane JJ, Burgess JO, Summitt JB. Fracture resistance of amalgam coronal-radicular restorations. J Prosthet Dent. 1990;63:607-613.
88. Kawasaki K, Ruben J, Stokroos I, Takagi O, Arends J. The remineralization of EDTA-treated human dentine. Caries Res. 1999;33:275-280.
89. Khera SC, Goel VK, Chen RCS, Gurusami SA. Parameters of MOD cavity preparations: a 3D FEM study. Oper Dent. 1991;16:42-54.
90. Kinney JH, Balooch M, Marshall SJ, Marshall GW, Weihs TP. Atomic forces microscope measurements of the hardness and elasticity of peritubular and intertubular human dentin. J Biomech Eng. 1996;118:133-135.
91. Kinney JH, Balooch M, Marshall SJ, Marshall GW, Weihs TP. Hardness and Young’s modulus of human peritubular and intertubular dentine. Arch Oral Biol. 1996;41:9-13.
92. Kinney JH, Marshall SJ, Marshall GW. The mechanical properties: a critical review and re-evaluation of the dental literature. Crit Rev Oral Biol Med. 2003;14:13-29.
93. Kinney JH, Nallab RK, Poplec JA, Breunigd TM, Ritchie RO. Age-related transparent root dentin: mineral concentration, crystallite size, and mechanical properties. Biomaterials. 2005;26:3363-3376.
94. Krejci I, Lutz F, Füllemann J. Tooth-colored inlays/overlays. Tooth-colored adhesive inlays and overlays: materials, principles and classification. Schweiz Monatsschr Zahnmed. 1992;102:72-83.
95. Kuttler S, Mclean A, Dorn S, Fischzang A. The impact of post space preparation with Gates-Glidden drills on residual dentin thickness in distal roots of mandibular molars. J Am Dent Assoc. 2004;135:903.
96. Lambjerg-Hansen H, Asmussen E. Mechanical properties of endodontic posts. J Oral Rehabil. 1997;24:882-887.
97. Lang H, Korkmaz Y, Schneider K, Raab WH. Impact of endodontic treatments on the rigidity of the root. J Dent Res. 2006;85:364-368.
98. Larsen TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6:2.5.
99. Lertchirakarn V, Palamara JE, Messer HH. Anisotropy of tensile strength of root dentin. J Dent Res. 2001;80:453-456.
100. Lewinstein I, Grajower R. Root dentin hardness of endodontically treated teeth. J Endod. 1981;7:421-422.
101. Libman WJ, Nicholls JI. Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont. 1995;8:155.
102. Linn J, Messer HH. Effect of restorative procedures on the strength of endodonticallly treated molars. J Endod. 1994;20:479-485.
103. Magne P, Knezevic A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence Int.. 2009;40:125-133.
104. Marchi GM, Mitsui FH, Cavalcanti AN. Effect of remaining dentine structure and thermal-mechanical aging on the fracture resistance of bovine roots with different post and core systems. Int Endod J. 2008;41:969-976.
105. Martinez-Insua A, da Silva L, Rilo B, Santana U. Comparison of the fracture resistances of pulpless teeth restored with a cast post and core or carbon fiber post with a composite core. J Prosthet Dent. 1998;80:527.
106. McLean A. Criteria for the predictably restorable endodontically treated tooth. J Can Dent Assoc. 1998;64:652.
107. Meredith N, Sheriff M, Stechell DJ, Swanson SA. Measurements of the microhardness and Young’s modulus of human enamel and dentine using an indentation technique. Arch Oral Biol. 1996;41:539-545.
108. Millstein PL, Ho J, Nathanson D. Retention between a serrated steel dowel and different core materials. J Prosthet Dent. 1991;65:480.
109. Milot P, Stein RS. Root fracture in endodontically treated teeth related to post selection and crown design. J Prosthet Dent. 1992;68:428.
110. Miyasaka K, Nakabayashi N. Combination of EDTA conditioner and Phenyl-P/HEMA self-etching primer for bonding to dentin. Dent Mater. 1999;15:153-157.
111. Monticelli F, Ferrari M, Toledano M. Cement system and surface treatment selection for fiber post luting. Med Oral Patol Oral Cir Bucal. 2008;13:E214-E221.
112. Morgano SM, Brackett SE. Foundation restorations in fixed prosthodontics: current knowledge and future needs. J Prosthet Dent. 1999;82:643.
113. Morris MD, Lee KW, Agee KA, Bouillaguet S, Pashley DH. Effect of sodium hypochlorite and RC-Prep on bond strengths of resin cement to endodontic surfaces. J Endod. 2001;27:753-757.
114. Moszner N, Salz U, Zimmermann J. Chemical aspects of self-etching enamel-dentin adhesives: a systematic review. Dent Mater. 2005;21:895-910.
115. Mountouris G, Silikas N, Eliades G. Effect of sodium hypochlorite treatment on the molecular composition and morphology of human coronal dentin. J Adhes Dent. 2004;6:175-182.
116. Muller HP, Eger T. Gingival phenotypes in young male adults. J Clin Periodontol. 1997;24:65-71.
117. Muller HP, Eger T. Masticatory mucosa and periodontal phenotype: a review. Int J Periodontics Restorative Dent. 2002;22:172-183.
118. Nakano F, Takahashi H, Nishimura F. Reinforcement mechanism of dentin mechanical properties by intracanal medicaments. Dent Mater J. 1999;18:304-313.
119. Nayyar A, Zalton RE, Leonard LA. An amalgam coronal-radicular dowel and core technique for endodontically treated posterior teeth. J Prosthet Dent. 1980;43:511-515.
120. Nicopoulou-Karayianni K, Bragger U, Lang NP. Patterns of periodontal destruction associated with incomplete root fractures. Dentomaxillofac Radiol. 1997;26:321.
121. Nikaido T, Takano Y, Sasafuchi Y, Burrow MF, Tagami J. Bond strengths to endodontically-treated teeth. Am J Dent. 1999;12:177-180.
122. Nikiforuk G, Sreebny L. Demineralization of hard tissues by organic chelating agents at neutral PH. J Dent Res. 1953;32:859-867.
123. Nissan J, Dmitry Y, Assif D. The use of reinforced composite resin cement as compensation for reduced post length. J Prosthet Dent. 2001;86:304-308.
124. Olsson M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisors. J Clin Periodontol. 1991;18:78-82.
125. Orstavik D, Pitt Ford T, editors. Essential endodontology: prevention and treatment of apical periodontitis, 2nd ed, Munsksgaard Blackwell Ltd, 2008.
126. Ottl P, Hahn L, Lauer HCH, Lau YH. Fracture characteristics of carbon fibre, ceramic and non-palladium endodontic post systems at monotonously increasing loads. J Oral Rehabil. 2002;29:175.
127. Palamara JE, Wilson PR, Thomas CD, Messer HH. A new imaging technique for measuring the surface strains applied to dentine. J Dent. 2000;28:141-146.
128. Panitvisai P, Messer HH. Cuspidal deflection in molars in relation to endodontic and restorative procedures. J Endod. 1995;21:57-61.
129. Papa J, Cain C, Messer HH. Moisture content of vital vs endodontically treated teeth. Endod Dent Traumatol. 1994;10:91-93.
130. Pashley D, Okabe A, Parham P. The relationship between dentin microhardness and tubule density. Endod Dent Traumatol. 1985;1:176-179.
131. Pashley DH, Tay FR, Yiu C, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216-221.
132. Perdigão J, Lopes MM, Gomes G. Interfacial adaptation of adhesive materials to root canal dentin. J Endod. 2007;33:259-263.
133. Phark JH, Duarte SJr, Blatz M, Sadan A. An in vitro evaluation of the long-term resin bond to a new densely sintered high-purity zirconium-oxide ceramic surface. J Prosthet Dent. 2009;101:29-38.
134. Pierrisnard L, Hohin F, Renault P, Barquins M. Coronoradicular reconstruction of pulpless teeth: a mechanical study using finite element analysis. J Prosthet Dent. 2002;88:442.
135. Pilo R, Cardash HS, Levin E, Assif D. Effect of core stiffness on the in vitro fracture of crowned, endodontically treated teeth. J Prosthet Dent. 2002;88:302-306.
136. Plotino G, Grande NM, Bedini R, Pameijer CH, Somma F. Flexural properties of endodontic posts and human root dentin. Dent Mater. 2007;23:1129-1135.
137. Plotino G, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008;34:394-407.
138. Pontius O, Hutter JW. Survival rate and fracture strength of incisors restored with different post and core systems and endodontically treated incisors without coronoradicular reinforcement. J Endod. 2002;28:710-715.
139. Poolthong S, Mori T, Swain MV. Determination of elastic modulus of dentin by small spherical diamond indenters. Dent Mater. 2001;20:227-236.
140. Powers JM, Sakaguchi RL. Craig’s Restorative Dental Materials, ed 12. St. Louis: Mosby; 2006.
141. Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: a literature review. J Adhes Dent. 2008;10:251-258.
142. Reeh ES, Douglas WH, Messer HH. Stiffness of endodontically treated teeth related to restoration technique. J Dent Res. 1989;68:540-544.
143. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512-516.
144. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512-516.
145. Rees JS, Jacobsen PH, Hickman J. The elastic modulus of dentine determined by static and dynamic methods. Clin Mater. 1994;17:11-15.
146. Ricketts DN, Tait CM, Higgins AJ. Post and core systems, refinements to tooth preparation and cementation. Br Dent J. 2005;198:533-541. Review
147. Rivera EM, Yamauchi M. Site comparisons of dentine collagen cross-links from extracted human teeth. Arch Oral Biol. 1993;38:541-546.
148. Roberts HW, Leonard DL, Vandewalle KS, Cohen ME, Charlton DG. The effect of a translucent post on resin composite depth of cure. Dent Mater. 2004;20:617-622.
149. Rocca GT, Bouillaguet S. Alternative treatments for the restoration of non-vital teeth. Rev Odont Stomat. 2008;37:259-272.
150. Rosentritt M, Furer C, Behr M, Lang R, Handel G. Comparison of in vitro fracture strength of metallic and tooth-coloured posts and cores. J Oral Rehabil. 2000;27:595.
151. Rosentritt M, Plein T, Kolbeck C, Behr M, Handel G. In vitro fracture force and marginal adaptation of ceramic crowns fixed on natural and artificial teeth. Int J Prosthodont. 2000;13:387-391.
152. Ruddle CJ. Nickel-titanium rotary instruments: current concepts for preparing the root canal system. Aust Endod J. 2003;29:87-98.
153. Saleh AA, Ettman WM. Effect of endodontic irrigation solutions on microhardness of root canal dentin. J Dent. 1999;27:43-46.
154. Santos J, Carrilho M, Tervahartiala T, et al. Determination of matrix metalloproteinases in human radicular dentin. J Endod. 2009;35:686-689.
155. Saunders WP, Saunders EM. Coronal leakage as a cause of failure in root-canal therapy: a review. Endod Dent Traumatol. 1994;10:105-108.
156. Sauro S, Mannocci F, Toledano M, Osorio R, Pashley DH, Watson TF. EDTA or H3PO4/NaOCl dentine treatments may increase hybrid layers’ resistance to degradation: a microtensile bond strength and confocal-micropermeability study. J Dent. 2009;37:279-288.
157. Schmage P, Pfeiffer P, Pinto E, Platzer U, Nergiz I. Influence of oversized dowel space preparation on the bond strengths of FRC posts. Oper Dent. 2009;34:93-101.
158. Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30:289-301.
159. Schwartz RS. Adhesive dentistry and endodontics. Part 2: bonding in the root canal system-the promise and the problems: a review. J Endod. 2006;32:1125-1134.
160. Scotti R, Malferrari S, Monaco C: Clarification on fiber posts: prosthetic core restoration, pre-restorative endodontics, Proceedings from the 6th International Symposium on Adhesive and Restorative Dentistry, pp 7–13, 2002.
161. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18:332-335.
162. Setcos JC, Staninec M, Wilson NH. Bonding of amalgam restorations: existing knowledge and future prospects. Oper Dent. 2000;25:121-129. Review
163. Signore A, Benedicenti S, Kaitsas V, Barone M, Angiero F, Ravera G. Long-term survival of endodontically treated, maxillary anterior teeth restored with either tapered or parallel-sided glass-fiber posts and full-ceramic crown coverage. J Dent. 2009;37:115-121.
164. Sim TP, Knowles JC, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. 2001;33:120-132.
165. Sindel J, Frandenberger R, Kramer N, Petschelt A. Crack formation in all-ceramic crowns dependent on different core build-up and luting materials. J Dent. 1999;27:175.
166. Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with six post-and-core systems. J Prosthet Dent. 1999;81:262.
167. Soares CJ, Soares PV, de Freitas Santos-Filho PC, Castro CG, Magalhaes D, Versluis A. The influence of cavity design and glass fiber posts on biomechanical behavior of endodontically treated premolars. J Endod.. 2008;34:1015-1019.
168. Sorensen JA, Martinoff MD. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent. 1984;51:780-784.
169. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63:529-536.
170. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63:529-536.
171. Standlee JP, Caputto AA, Holcomb JP. The Dentatus screw: comparative stress analysis with other endodontic dowel designs. J Oral Rehabil. 1982;9:23-33.
172. Summit JB, Robbins JW, Schwart RS. Fundamentals of Operative Dentistry—A Contemporary Approach, ed 3. Illinois: Quintessence; 2006.
173. Tamse A, Fuss Z, Lustig J. An evaluation of endodontically treated vertically fractured teeth. J Endod. 1999;25:506.
174. Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod. 2005;31:584-589.
175. Tidmarsch BG, Arrowsmith MG. Dentinal tubules at the root ends of apisected teeth: a scanning electron microscopy study. Int Endod J. 1989;22:184-189.
176. Tjan AH, Nemetz H. Effect of eugenol-containing endodontic sealer on retention of prefabricated posts luted with adhesive composite resin cement. Quintessence Int. 1992;23:839-844.
177. Trope M, Ray HL. Resistance to fracture of endodontically treated roots. Oral Surg Oral Med Oral Pathol. 1992;73:99-102.
178. Vire DE. Failure of endodontically treated teeth: classification and evaluation. J Endod. 1991;17:338.
179. Watanabe I, Saimi Y, Nakabayashi N. Effect of smear layer on bonding to ground dentin—relationship between grinding conditions and tensile bond strength. Shika Zairyo Kikai. 1994;13:101-108.
180. Wiegand A, Buchalla W, Attin T. Review on fluoride-releasing restorative materials—fluoride release and uptake characteristics, antibacterial activity and influence on caries formation. Dent Mater. 2007;23:343-362.
181. Wu MK, Pehlivan Y, Kontakiotis EG, Wesselink PR. Microleakage along apical root fillings and cemented posts. J Prosthet Dent. 1998;79:264.
182. Yoldas O, Alaçam T. Microhardness of composites in simulated root canals cured with light transmitting posts and glass-fiber reinforced composite posts. J Endod. 2005;31:104-106.
183. Yoshikawa T, Sano H, Burrow MF, Tagami J, Pashley DH. Effects of dentin depth and cavity configuration on bond strength. J Dent Res. 1999;78:898-905.
184. Yüzügüllü B, Ciftçi Y, Saygili G, Canay S. Diametral tensile and compressive strengths of several types of core materials. J Prosthodont. 2008;17:102-107.