Sedation and monitoring
Sedation
Sedation is the use of a drug or drugs to produce a state of depression of the central nervous system that enables interventional procedures or treatment to be carried out. Sedative drugs may be combined with drugs used for pain relief (analgesia). Sedation is only part of a ‘package’ of care comprising pre-assessment, properly informed consent, adequate facilities, good techniques and risk avoidance.1
Over recent years the number and complexity of diagnostic imaging and image-guided interventional procedures in radiology departments has increased; often these patients are frail, medically unfit, unable to cooperate or lie still. The relief of anxiety, discomfort and pain allows patients to tolerate these procedures. Some drugs, such as benzodiazepines, have purely sedative effects but others, such as opioids, have combined sedative and analgesic effects. Although sedative and analgesic agents are generally safe, catastrophic complications related to their use can occur, often as a result of incorrect drug administration or inadequate patient monitoring.2 The incidence of adverse outcomes is reduced by improved understanding of the pharmacology of drugs used, appropriate monitoring of sedated patients and by recognizing those at increased risk of adverse event.
There is a continuum between the main types of sedation (Fig. 18.1) defined as:
1. Anxiolysis: the patient is alert and calm
2. Conscious sedation: a state of depression of the central nervous system that enables diagnostic and therapeutic procedures to be carried out, but during which the patient remains conscious, retains protective reflexes and is able to understand and respond to verbal commands
3. Deep sedation: in which these criteria are not fulfilled and airway or ventilation intervention may be required. Deep sedation requires the presence of an anaesthetist
The joint Royal College of Radiologists/Royal College of Anaesthetists Working Party on Sedation and Anaesthesia in Radiology recommended establishment of local guidelines for sedation in radiology.3 These should include:
1. Each patient must have a pre-procedure evaluation to assess their suitability for sedation
2. The operator must not supervise the sedation
3. Nurses and technicians should not administer drugs without medical supervision
4. All staff carrying out sedation should have undertaken training in sedation and resuscitation, and should have knowledge and experience of the sedative drugs, monitoring and resuscitation equipment
5. There should be periodic retraining and assessment of staff
6. There should be an appropriate recovery area
7. Resuscitation equipment and appropriate reversal drugs must be immediately available.
Preparation
Sympathetic patient management with an explanation of the procedure may reduce anxiety and remove the need for any medication. Sedation should be explained and consent obtained. Patients who are to be given intravenous (i.v.) sedation should undergo a period of fasting before the procedure; 6 h fasting for solid food and 2 h for clear liquids.
Resuscitation and monitoring equipment and oxygen delivery devices should be checked and venous access established.
Drugs
As part of a sedation protocol the following may be used:
1. Combination of a sedative drug and an analgesic drug (e.g. i.v. midazolam and i.v. opiate). Intravenous analgesic and sedative drugs have a synergistic sedative effect and the dose of each drug must be reduced by up to 70% when administered together. It is best to give the i.v. analgesic first and then titrate the dose of i.v. sedative
Analgesic drugs
Analgesic drugs are used for pain control and improve patient comfort. For some procedures local anaesthesia or oral analgesia (using paracetamol 1 g or ibuprofen 400 mg taken 1–2 h before the procedure) will be appropriate. For more invasive interventional radiology procedures the use of intravenous analgesia may be required.
Local anaesthesia
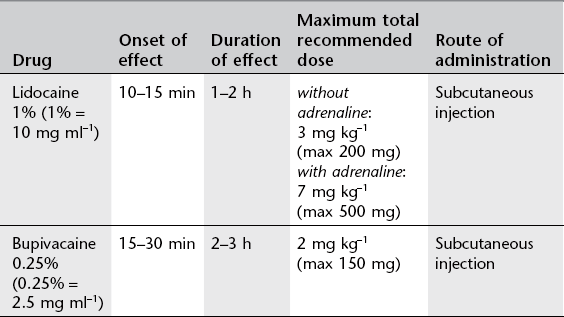
For recommended doses see Table 18.1.
Commonly used local anaesthetics for subcutaneous infiltration are:
1. Lidocaine 1%. Lidocaine may be used in combination with adrenaline (epinephrine) and is supplied in pre-mixed ampoules for this purpose. Adrenaline causes local vasoconstriction, decreases drug absorption and will increase the intensity and duration of action of lidocaine. Lidocaine is also available as a 2% solution.
2. Bupivacaine 0.25%. Has slower onset but longer duration of action than lidocaine. The effect of adrenaline is much less pronounced in combination with bupivacaine. Bupivacaine is also available as a 0.5% solution.
Inhalational analgesia
A mixture of 50% nitrous oxide and 50% oxygen (Entonox®) may be used. This has both analgesic and sedative properties.
Intravenous analgesia
These drugs are used for pain control but also have a dose-dependent sedative effect. Most commonly used are the opioid drugs morphine, pethidine and fentanyl. These drugs must be given in small, divided doses and dose-titrated to the patient's need. It is extremely important to titrate the dosage to effect rather than assume a fixed dose based on body weight. The maximum recommended dose must not be exceeded because of the risk of adverse events, particularly respiratory depression. For recommended dosage see Table 18.2.
Table 18.2
Recommended doses of intravenous analgesic drugs
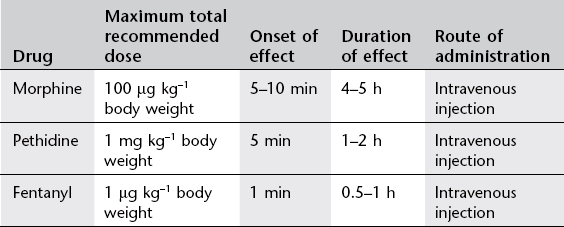
These drugs should be used in divided doses and the maximum total dose must not be exceeded. It is always important to titrate the dosage of medication to effect rather than assume a fixed dose based on body weight.
Effects of opioids can be reversed by the competitive antagonist naloxone (dose 0.4–2 mg). Naloxone should be administered intravenously in a solution containing 0.4 mg in 10 ml and given in 1 ml increments. It has peak effect at 1–2 min with duration of 20–60 min. As a result of the relatively short duration of action, repeated doses of naloxone may be necessary.
Sedative drugs
For conscious sedation in the radiology department, the water-soluble benzodiazepine midazolam is the drug of choice. Midazolam has superseded diazepam because the latter has active metabolites and longer duration of effect. Midazolam produces:
Midazolam is given i.v. It has a rapid onset of effect, within 1–5 min, and a variable duration of effect of 1–4 h. The sedative dose is 70 µg kg−1 body weight (for average adult approx. 4–5 mg) and the sleep dose is 100–200 µg kg−1 (>7 mg). Typically, 2–2.5 mg is administered i.v. over 30–120 s with further 0.5-mg doses titrated as required. Rarely are total doses of more than 5 mg required. Smaller doses of 1–3 mg must be used in the elderly.
The effects of midazolam can be reversed by the competitive antagonist flumazenil; onset of flumazenil is within 1–3 min with a half-life of 7–15 min. The dose of flumazenil should be titrated every 1–2 min starting with 200 µg up to a maximum of 1 mg. The clinical effect depends on the dose of flumazenil and sedative given. Note: the half-life of flumazenil is shorter than that of midazolam, therefore re-sedation effects can occur.
Remifentanil is a potent ultra-short-acting synthetic opioid analgesic drug, the sedative dose range by intravenous infusion is 0.025–0.1 µg kg−1 min−1, at higher doses it can cause marked respiratory depression. Dexmedetomidine is an agonist of α2-adrenergic receptors; it can provide sedation, analgesia and anxiolysis without respiratory depression when given as an intravenous infusion at 0.2–1 µg kg−1 h−1. The use of i.v. anaesthetic agents, such as ketamine and propofol, can result in the patient moving quickly from a state of sedation to anaesthesia with concomitant risks. These drugs should only be used by those who have undergone appropriate specialist training.
Sedation of children
Each child should be individually assessed. In most circumstances parents should stay with the child, and with patience and encouragement the need for sedation may be avoided in some cases. Short procedures such as CT can often be achieved in neonates by keeping them awake and then feeding the child and swaddling just prior to the procedure. Often, children over the age of 4–5 years will not need sedation and will cooperate. If venous access is required, local anaesthetic cream, e.g. Ametop, can be applied to a suitable vein prior to insertion of a cannula. Oral sedation does not work well in children over the age of 4 and older children who are unable to co-operate will usually require general anaesthetic.
It is important to ensure that all monitoring and resuscitation equipment is suitable for paediatric use. A nurse, experienced in the care of sedated children, should be present throughout. When drugs are given which are likely to result in loss of consciousness, the primary care of the patient should be under the direct supervision of an anaesthetist.
For many years chloral hydrate has been the mainstay for sedation of young children for a variety of procedures. Triclofos, which is an active metabolite of chloral hydrate, causes less gastric irritation and vomiting. Alimemazine (Vallergan) is a sedating antihistamine, with anticholinergic effects and can be used in combination with triclofos. The recommendations in Table 18.3 are made as being suitable for the majority of patients, in respect of both safety and efficacy. It is recognized that, for certain patients, deviation from these guidelines will be appropriate on clinical or weight grounds (Table 18.3).
Table 18.3
Sedation recommendations made as being suitable for the majority of child patients. These doses are used to achieve deep sedation: a nurse should be present throughout
| Age/weight | Sedation | Dose |
| <1 month old | Feed only or Triclofos | 30 mg kg−1 |
| >1 month old but <5 kg | Triclofos | 50–70 mg kg−1 |
| 5–10 kg | Triclofos | 100 mg kg−1 |
| >10 kg up to 4 years | Triclofos + Alimemazine |
100 mg kg−1 (maximum 2 g) 1 mg kg−1 (maximum 30 mg) |
| Over 4 years | Consider oral sedation (as above) or general anaesthetic |
Vomiting is not uncommon after oral sedation is given. If the child vomits within 10 min of administration the dose can be repeated. After 10 min a reduced dose of 50–70% of the Triclofos + Alimemazine dose can be repeated. The dose should not be repeated after 20 min as significant absorption may have occurred.
On the night before the procedure or scan parents should be asked to try to keep the child awake for as long as possible. The child should be woken early on the relevant day and no ‘naps’ allowed on the journey to the hospital. This will ensure that the child is already tired prior to administration of the sedation. The sedative medication usually takes about 45 min to take effect.
Children should have nothing to eat or drink prior to sedation as follows:
1. Breast fed only: Last feed 2 hours before sedation
2. Under 1 year or on formula, or weaning onto a soft diet: Last feed/milk 4 h before sedation, but can have clear fluids up to 2 h before
3. Over 1 year: Light meal, such as fruit juice, milk, toast or cereal 4 h before sedation, clear fluids up to 2 h before sedation.
Complications of sedation
Early recognition and treatment of complications is essential to reduce morbidity and mortality from sedation in all patients.
Major complications are rare, but include:
Sedation causes a reduction in muscle tone of the oropharynx and at deeper levels of sedation the glottic reflexes may fail. Major complications of sedation are most often due to airway obstruction and respiratory depression. The following patient groups are at high risk:
1. Elderly patients. Old age is an independent risk factor for sedation. The effects of sedative drugs are more pronounced and prolonged in the elderly. Small incremental doses of sedatives are required.
2. Chronic obstructive pulmonary disease. These patients have a blunted ventilator drive. Supine position impairs chest wall function and oxygenation. Patients may need supplemental oxygen and bronchodilators. Local anaesthesia should be used for pain whenever possible and sedative drugs should be used sparingly.
3. Coronary artery disease. Under-sedation will increase cardiac oxygen demand but over-sedation can cause hypotension, hypoxaemia and decrease myocardial oxygen delivery leading to myocardial ischaemia. Patients should be given supplemental oxygen.
4. Hepatic dysfunction or renal failure. Altered drug metabolism in renal and liver disease increases the risk of overdose when using opioids and benzodiazepines. These drugs should be used in reduced doses. In children, similarly, Triclofos should be avoided in those with end-stage liver failure and used with caution in cholestasis. In renal impairment dose reduction should be considered.
5. Drug addicts. These patients may exhibit unpredictable requirements and drug-seeking behaviour. Local anaesthetics and short-acting benzodiazepines are preferred; reversal agents should be avoided.
References
1. Royal College of Radiologists, Safe Sedation, Analgesia and Anaesthesia within the Radiology Department. The Royal College of Radiologists, London, 2003. http://www. rcr. ac. uk/publications. aspx?PageID=310&PublicationID=186
2. Martin, ML, Lennox, PH. Sedation and analgesia in the interventional radiology department. J Vasc Interv Radiol. 2003; 14(9 Pt 1):1119–1128.
3. Royal Radiologists/Royal College of College of Anaesthetists joint publication. Sedation and Anaesthesia in Radiology. London: The Royal College of Radiologists; 1992.
American College of Radiology. ACR-SIR Practice guideline for sedation/analgesia. www. acr. org, 2010.
Patatas, K, Koukkoulli, A. The use of sedation in the radiology department. Clin Radiol. 2009; 64:655–663.
2010. NICE clinical guideline 112. Sedation for diagnostic and therapeutic procedures in children and young people. www. nice. org. uk/guidance/CG112, 2010.
Monitoring
The purpose is to observe and assess response of the patient to any psychological or physiological stress imposed by the procedure or sedative agents administered and allow appropriate therapeutic action to be taken.
Equipment
1. Pulse oximetry. Pulse oximetry is the most sensitive monitoring method to detect hypoxaemia. It is the minimum requirement for safe monitoring and may suffice as the sole monitoring device in the young and fit. It accurately measures the oxygen saturation of blood and provides information on pulse rate and adequacy of the circulation. The oxygen saturation should be maintained at or above 95%. Most pulse oximeters have a short lag time in demonstrating desaturation. Due to the nature of the oxygen dissociation curve, patients may rapidly desaturate from 90% to 70%. Oxygen saturation of 90% is an emergency and corrective action should be taken immediately. The pulse oximeter signal may be affected by interference from nail polish, light, movement and cold extremities.
2. Electrocardiograph. A continuous electrocardiography monitor will provide information on pulse rate and rhythm, presence of arrhythmia and signs of ischaemia, but does not monitor circulation or cardiac output.
3. Automated blood pressure monitor. Minimum acceptable mean arterial pressure is 60 mmHg, but patients with cardiac disease or hypertension require higher pressures. Falsely high arterial pressure readings are obtained with cuffs which are too small. Manual blood pressure measurements are inconvenient and inconsistent. The blood pressure monitor may impede function of the pulse oximeter so should not be on the same arm. The monitor should be set to 5-min recording intervals; nerve damage has been reported with prolonged use.
Monitor alarms may be the first signal of an adverse event and should not be silenced. If there is any doubt repeat measurement should be performed.
Technique
Monitoring should include assessment of:
1. The patient's level of consciousness
3. Adequacy of respiratory function – respiratory rate and pattern
4. Adequacy of cardiac function – pulse and skin colour
The patient should be monitored by a trained professional who should have no other role at the time of the procedure than to continuously monitor these parameters. The radiologist performing the procedure should not monitor the patient.
Vital signs (pulse, blood pressure and respiratory rate) should be regularly measured. Any adverse events must be fully recorded in the patient's notes. Monitoring should continue into the recovery period.
Sedation and monitoring for magnetic resonance imaging
Sedation should be given in a quiet area close to the scanner and there should be an appropriate recovery area available.
The MRI scan room is a challenging environment in which to monitor the patient. The scanner is noisy, potentially claustrophobic and any patient inside the scanner is relatively inaccessible.
All equipment used for monitoring and all anaesthetic equipment must be MR-compatible, e.g. MR-compatible pulse oximeters with fibre-optic cabling. Potential problems include effects from the gradient field and radiofrequency fields. Heat induction in conducting loops formed by ECG leads can cause superficial burns and induced current in monitoring equipment may produce unreliable readings or malfunction of syringe drivers resulting in incorrect drug-dose delivery (see Chapter 1). Responsibility for safe use of MRI monitoring equipment should be allocated to a small number of experienced and appropriately trained staff.
Recovery and discharge criteria
The effects of most agents used for sedation and analgesia last longer than the duration of the procedure; therefore, monitoring of the patient must continue into the recovery period. Once the patient is alert and orientated and vital signs have returned to their baseline values or acceptable levels, the patient can be considered fit to be moved from the radiology department. The overall responsibility for the patient's care until discharge is with the consultant radiologist or main operator and every unit should have written guidelines for discharge criteria.
Sedation and Monitoring for Magnetic Resonance Imaging
American Society of Anesthesiologists Task force on anesthetic care for magnetic resonance imaging. Practice advisory on anesthetic care for magnetic resonance imaging: A report by the American Society of Anesthesiologists Task force on anesthetic care for magnetic resonance imaging. Anesthesiology. 2009; 110:459–479.