Radiography Education
From Classroom to Clinic
On completion of this chapter, you should be able to:
• Describe the essentials for patient–radiologic technologist interaction.
• List and describe the basic courses essential to the education of radiologic technologists.
• Explain the relationship between clinical education and the theory component of the radiologic technology curriculum.
• Explain what is meant by clinical competency evaluation.
• List and describe the competencies evaluated in clinical education.
Few professions are as diverse as radiologic technology. Daily tasks range from communications and psychologic to artistic expression in the production of the radiographic image to the application of physics, anatomy, physiology, and chemistry.
To the novice, the work performed by a well-educated registered technologist may seem methodic, repetitious, and lacking challenge. However, on close examination it becomes apparent that the technologist must possess complex knowledge and apply it to the radiologic examination of patients.
The reason a particular occupation or task appears easy is that the person performing the job has learned the many intricacies involved. This statement is particularly true with radiologic technology. The educated technologist provides every patient with optimal patient care, which includes interaction with the patient, positioning procedures, and the selection of exposure factors that produce the best diagnostic radiologic examination. Therefore the performance of various tasks might appear easy to the patients and others outside the profession.
This chapter introduces the student to the work of the radiologic technologist, provides the minimum core curriculum necessary for entry-level performance, and evaluates the student during the learning process.
The patient as our guest
The key individual in the health care setting is the patient. This means that we must think of the patient as our guest. Examining this phrase and understanding how the patient is a guest is very important. The patient is the recipient of the many services provided in medical facilities. On admission to the hospital, clinic, or physician’s office, the patient is abruptly introduced to an unusual environment filled with wondrous, unnamed machines and a variety of people, all waiting for the guest—the patient.
When a qualified physician requests a radiographic examination, it becomes the radiologic technologist’s responsibility to:
Essentially, this treatment should be respectful without being familiar, empathetic without being maudlin (tearful, emotional), considerate without being solicitous (fearful, overly concerned), and professional without being cold and clinical.
This all sounds like a tall order, especially when the workload is heavy, the hour grows late, and more things are yet to be done; but you only need to put yourself in the place of the patient to understand the importance of a health care professional’s responsibility (Fig. 6-1).
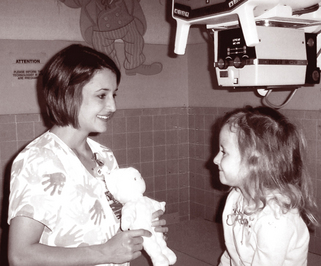
FIGURE 6-1 Technologist interacting with a young patient. (Courtesy of University of Mississippi Medical Center, Amy Justice-Hill and Ansley Hill.)
When caring for the very young or the very old, the terminally ill, or the handicapped, this responsibility may be difficult to handle. These patients do not, however, change the importance of these responsibilities. This responsibility is the basis of being in a helping profession. Above all, every patient who comes to radiology is a guest!
Your responsibilities in health care
No substitute exists for the knowledge necessary to perform the tasks of a radiologic technologist with confidence, effectiveness, and efficiency.
This confidence is a direct result of being prepared. Students are confronted with quizzes, competency tests, and finally, the certifying examination. Yet the greatest tests will come with every radiologic examination you perform. Educators in radiologic technology are aware of the need for well-prepared radiologic technologists.
The field of radiology is continually changing in the wake of technology and has recently accelerated with the space age. However, learning the basic principles of the production of x-radiation and how to make these principles work is imperative for the student radiologic technologist.
What does the radiologic technologist need to know to perform the responsibilities of radiologic technology? To answer this question, you need to look at the course recommendations for approved programs in radiologic technology, as well as the unique goals and needs of the sponsoring institutions and clinical affiliates.
Essentially, the courses listed here are considered basic. The titles and brief descriptions of topics are based on the curriculum guide published by the American Society of Radiologic Technologists (ASRT). More complete information is available from ASRT.
Radiologic Technology Basic Curriculum
The radiologic technology curriculum is composed of several courses taught over 2 consecutive calendar years. The courses listed are not inclusive and each is under continual study and review by the professional organizations responsible for recommending the basic curriculum.
Introduction to Radiography
This course is designed to introduce the student to the basic aspects of the department of imaging, radiologic technology, and the health care system in general. The basic principles of radiation protection are introduced. The student should gain a better understanding of the structure and function of agencies through which medical services are delivered.
Medical Ethics and Law
What are the moral, legal, and professional responsibilities of the radiologic technologist? This course helps the student understand how to deal with confidential information and the interpersonal relationships, or interaction, with patients and other health care team members. In addition, attention is given to medicolegal considerations, as well as to professional guidelines and codes of ethics.
Principles of Diagnostic Imaging
This course introduces the student to various methods of recording images. These images result from the fluoroscopic and radiographic application of the principles of image production. The student is expected to comprehend and apply the principles to the various imaging systems. Some special techniques, such as magnetic resonance imaging (MRI), digital radiography, and ultrasonography, are discussed.
Imaging Equipment
This course describes the process of radiographic image production and the specific equipment needed to produce the radiographic image.
Radiographic Processing
The design, structure, function, and application of the various rooms and equipment needed to obtain a radiograph are presented. Darkrooms, processing and materials, and radiographic film, including its storage, handling, characteristics, and possible artifacts, are discussed.
Human Structure and Function
This course refers to the anatomy and physiology of the human body. For the radiologic technologist to conduct radiologic procedures on various anatomic parts, knowing the location and function of all body parts is necessary.
Medical Terminology
The written and spoken language of medicine incorporates many uncommon words, meanings, and symbols. For the radiologic technologist to work effectively in radiology, understanding the language of medicine is also necessary.
Principles of Radiographic Exposure
What are the technical factors required to produce high-quality diagnostic radiographs? What kinds of accessory equipment is used? This course involves the use of the mathematic principles used in producing a radiograph.
Radiographic Procedures
Every radiology department has a routine for performing procedures specific to that particular department. These procedures range from simple radiographic imaging to more complex tasks requiring contrast media, special radiographic equipment, and accessory materials.
Principles of Radiation Protection
The technologist must know how to use ionizing radiation in a safe and prudent manner. Patients, as well as radiologic technologists and co-workers, must be protected from radiation as much as possible. Therefore radiologic technologists must know how exposure factors affect radiation doses, what the maximum permissible dose is, and the methods for monitoring exposure. The objective is to practice the as low as reasonably achievable (ALARA) concept in diagnostic radiography.
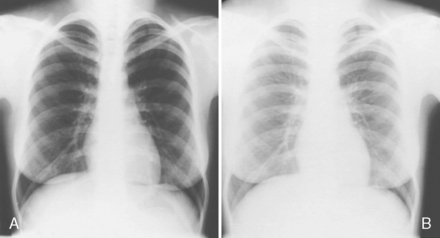
Radiographic Image Evaluation
What is the difference between an optimal quality radiograph and a nondiagnostic one (Fig. 6-2)? This course integrates all of the material previously learned. Although radiologic technologists do not interpret radiographs, they evaluate them for diagnostic quality, which includes the consideration of pathologic conditions.
Pathologic Conditions
The student needs to be acquainted with the various disease conditions that may affect the resulting radiographic image. In addition, knowledge of disease entities is helpful in working with patients.
Methods of Patient Care
Through information presented in this course, the radiologic technologist prepares to work with patients, regardless of their health conditions, in a manner that does not cause them additional injury or discomfort or hinder their recovery.
Quality Assurance
Optimal quality radiographs achieve many important benefits. They (1) minimize the patient’s exposure to radiation, (2) provide the physician with the best possible image for diagnosis, and (3) contain health care costs. Students must know the regulations that govern quality assurance, as well as the techniques, equipment, and procedures for attaining it.
Radiation Physics
To help the student understand how radiation works, as well as be familiar with the interaction of radiation with matter, this course concentrates on basic information about the physical properties of radiation—how it is produced, how it is measured, and how it is used in the medical environment. In addition, information about electrostatics, electric safety, x-ray tubes and transformers, and x-ray circuits and equipment is also included.
Radiobiology
The hazardous effects of ionizing radiation on living tissue have long been known. The student must be thoroughly familiar with the reactions that occur when a single living cell or an entire organism is irradiated.
Introduction to Computer Science
Many of the technical innovations that are constantly changing the nature of radiology rely on computers. The capacity of computer storage and image manipulation is basic to many of the newer imaging systems, such as computed tomography, digital imaging, and MRI. This course introduces the student to basic computer applications (Fig. 6-3).
From the classroom to the clinical setting
During classroom preparation the student may practice taking radiographs using phantom material. In x-ray imaging phantoms are solid or liquid materials whose x-ray attenuation and scattering properties are similar to those of body tissues. This helps the student to learn proper anatomic positioning and exposure techniques (Fig. 6-4).

FIGURE 6-4 Phantoms are used for instructing students in radiography. (Courtesy of Professor Tom H. Wolfe and student, Twii Dean; Southwest Tennessee Community College.)
After classroom preparation, clinical experience offers the opportunity for the student radiologic technologist to determine whether all things learned about the production of x-rays are true.
However, there is more to the clinical experience than proving that widely held theories are indeed true. Patients with differing health problems are encountered, hundreds of procedures are experienced, and rules of behavior and ethics by which to abide are learned. In the clinical experience situation, students have the opportunity to prove their understanding of the classroom material by competently performing various radiologic procedures (Fig. 6-5).

FIGURE 6-5 After classroom instruction, clinical education provides the student with the opportunity to practice what has been learned. (Courtesy of Courtney Hensley and Laura Veltri-Smith and Methodist University Hospital; Joseph Martin, photographer.)
A basic guideline for evaluating the competency skills of a student radiologic technologist in the clinical setting has been developed and approved by the ASRT and is entitled, Clinical Competency Evaluation. Although other methods of clinical competency evaluation may be available and in use, the information in this document is the focus of our discussion because it has been accepted by ASRT, which is the profession’s official organization.
Clinical competency evaluation
Simply defined, clinical competency evaluation is a method of standardizing the evaluation of a student radiologic technologist’s performance in the clinical setting. The student must fully appreciate and understand the importance of a standard evaluation concept and its methodology. Three specific aspects of learning are provided in this evaluation of performance: cognitive, affective, and psychomotor.
Cognitive learning refers to classroom lectures and demonstrations of theories, as well as to the facts and background information necessary to understand a specific body of knowledge. Once this fundamental information has been learned, the student has the opportunity to participate in the clinical setting where each student has the opportunity to apply the knowledge gained from the classroom setting.
Affective learning involves attitudes, values, and feelings. The clinical environment provides the opportunity to develop pride in your work, as well as feelings of self-worth, skills in interpersonal relationships, and personal, moral, and ethical beliefs for daily practice.
Psychomotor learning is the actual hands-on phase—the application of previously learned material. Didactic information is put to actual use in the clinical situation.
Clinical participation
Clinical participation is the integration of the cognitive, affective, and psychomotor aspects of radiologic technology education. The student participates as follows:
1. Assists the practicing radiologic technologist and observes each detail of the radiographic procedure. This involvement is considered passive participation because the student is observing.
2. Performs various assigned tasks associated with procedures after becoming familiar with them. The performance of any task depends on the student’s ability to understand the responsibilities involved with the assigned tasks and to perform these tasks correctly.
3. Progresses into the independent clinical performance phase. This involvement means that the student will perform all aspects of the procedure with remote supervision of a radiologic technologist.
During this time, the student’s learning ability and performance are evaluated. The student now has the opportunity to demonstrate knowledge of the subject material and how well each task can be accomplished.
This evaluation is designed to be a positive experience. It is an opportunity for the student to gain confidence by becoming thoroughly familiar with each detail of the assigned tasks.
As the student makes the transition from a classroom environment to one that combines both classroom and clinical experience, the learning process becomes integrated and more complex. The student is expected to be more aware of the responsibilities in learning. This means he must answer the following questions:
3. How well have I learned the basic material?
4. Can I apply the classroom information in the clinical setting?
During this phase of radiologic technology education, the student also learns the importance of meeting the objectives of the educational process. Because competency levels vary from individual to individual, these objectives are self-paced. However, a great deal of coordination exists between classroom learning and clinical application. This coordination is facilitated by the program director, as well as the clinical supervisors and coordinators. These individuals plan the course work and clinical participation that provide an optimal learning environment for the student (see Box 6-1).
Competency Evaluations
Examinations vary in emphasis, depending on the teaching institution. However, the final objective is always that each student be able to perform all examinations successfully, regardless of specific emphasis, because routines for procedures vary from institution to institution. Student radiologic technologists must have a well-rounded preparatory education in the professional program to enable them to practice radiologic technology in any type of medical facility.
The American Registry of Radiologic Technologists (ARRT), the organization certifying radiologic technologists, published, Radiography Didactic and Clinical Competency Requirements. This document lists the rules and regulations for meeting certification. A significant rule is that your program director or designated faculty member must verify that the didactic and clinical skills have been satisfied. Therefore, you may expect frequent testing and evaluation throughout your course of study.
Criteria for Performance Evaluation
To provide a basis for minimal performance evaluation criteria, ASRT has developed a general, comprehensive list to help make performance evaluation as objective as possible for a wide variety of programs. The remainder of this chapter is taken directly from the Clinical Competency Evaluation document (with permission from ASRT) to ensure that the integrity of this process, as defined by ASRT, is maintained.
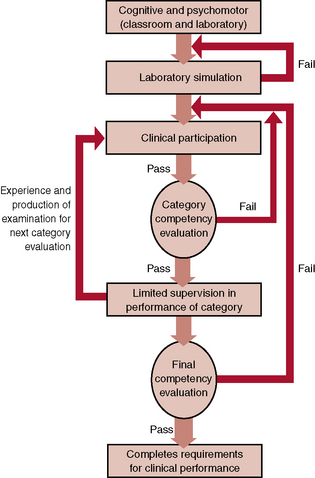
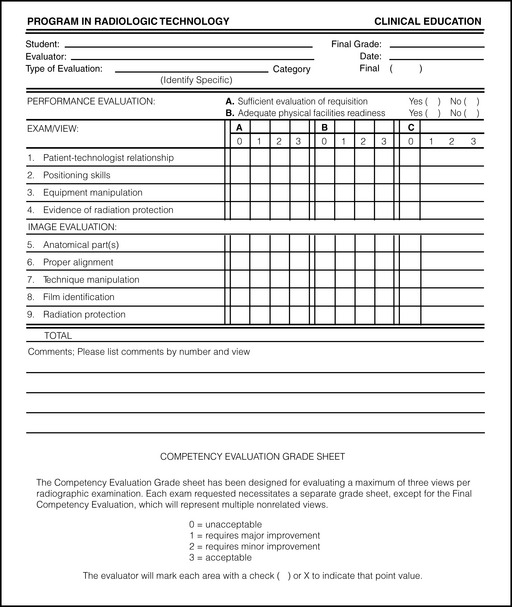
The entire evaluation process is outlined (Fig. 6-6), and a model competency evaluation grade sheet is provided (Fig. 6-7). These criteria for performance evaluation might be more demanding at some teaching institutions. The criteria are listed in the following categories.
Physical Facilities Readiness
Patient-Technologist Relationship
Positioning Skills
Position the patient correctly on the table (head at the appropriate end, prone or supine).
Align center of the anatomic part to be demonstrated to the center of the image receptor.
Position the central ray to the center of the image receptor.
Correctly guide the patient into the oblique angle, if required.
Angle the central ray to the center of the image receptor.
Restrict the size of the radiation field (collimation, cones, shields) and be certain that nonpertinent anatomic parts are not in the radiographic exposure area.
Equipment Manipulation
Turn the tube from a horizontal to a vertical (and vice versa) angle.
Move the Bucky tray and locks.
Insert and remove cassettes from the Bucky tray and spot-film device.
Select factors at the control panel.
Identify the image with right (R) and left (L) markers and other appropriate identifications (e.g., time, tube angle, name, date).
Fill syringes using the aseptic technique.
Operate controls for the mobile unit.
Select the proper cassette size.
Adapt for the technique changes in source-to-image receptor distance (SID) or focal-film distance (FFD), grid ratio, and collimation, among others.
Standard Radiographic Exposure—Image Evaluation
Continuing education
In 1997, ARRT began requiring continuing education for all ARRT registrants. Each ARRT registrant must obtain either 24 continuing education credits acceptable to ARRT or pass an examination in an additional discipline.
It is imperative that each student consider his or her education in radiologic technology as a continuing process. These courses are an indication of the basic responsibilities of every radiologic technologist. This material must be learned and understood before you can correctly and safely operate the complicated equipment. You need to know not only how the equipment works but also why it works as it does. You must also be able to provide the physician with the best diagnostic radiographic study possible, regardless of the patient’s condition.
Look closely at each task as it is encountered, and study not only the work involved but also the concepts behind the tasks. You should not be surprised to learn that radiologic technology education must be an ongoing process.
Conclusion
Educators in radiologic technology are aware that, for the student radiologic technologist, the transition from classroom to clinic can be not only demanding but also, at times, confusing. In approved programs, every effort is made to ensure that students are better prepared to accept and deal with this transition. In addition, educators work to ensure that each student is evaluated on a fair and objective basis according to acceptable standards and institutional requirements for the completion of the program.
From time to time, changes are made in the current procedures as new ideas and developments occur in radiologic technology. These changes are incorporated into the curriculum to ensure that students are familiar with new concepts and procedures.
No substitute exists for being well-prepared to practice your chosen profession. For the student, this time must be spent preparing for the challenges presented with each radiologic procedure. Each radiologic procedure is, after all, a test of your ability to perform the assigned tasks in an efficient, cheerful, and professional manner.
Bibliography
American Registry of Radiologic Technologists. Radiography didactic and clinical competency requirements. St Paul: The Registry, 2005.
JRCERT. Essentials and guidelines of an accredited educational program for the radiographer. Albuquerque: The Society, 1994.
American Society of Radiologic Technologists. Radiography clinical competency requirements. Albuquerque: The Society, 1999.
Ballinger, P. Merrill’s atlas of radiographic positions and radiologic procedures, ed 10. St Louis: Mosby, 2003.
Bontrager, K.L. Textbook of radiographic positioning and related anatomy, ed 5. St Louis: Mosby, 2001.
Joint Review Committee on Education in Radiologic Technology. Standards for an accredited program in radiologic sciences. Chicago: The Committee, 2002.