Stress and Coping
• Describe the three stages of the general adaptation syndrome.
• Differentiate acute stress disorder and posttraumatic stress disorder.
• Discuss the integration of stress theory with nursing theories.
• Describe stress management techniques beneficial for coping with stress.
• Discuss the process of crisis intervention.
• Develop a care plan for patients who are experiencing stress.
http://evolve.elsevier.com/Potter/fundamentals/
Health care professionals need to know about stress so they are able to recognize it in patients and families and intervene effectively. Caregiver stress frequently affects family members of patients and must be considered in patient care. Equally important, health care professionals also experience stressful events that occur in the course of clinical practice and in their own lives. Nurses need to recognize the signs and symptoms of stress and understand stress management techniques to aid personal coping and design stress management interventions for their patients and families.
People use the term stress in many ways. It is an experience to which a person is exposed through a stimulus or stressor. Stressors are tension-producing stimuli operating within or on any system (Neuman and Fawcett, 2011). It is also the appraisal, or perception, of a stressor. Appraisal is how people interpret the impact of the stressor on themselves or on what is happening and what they are able to do about it (Lazarus, 2007). Finally stress is a physical, emotional, or psychological demand that often leads to growth or overwhelms a person and leads to illness (Varcarolis and Halter, 2010). Stress refers to the consequences of the stressor and the person’s appraisal of it.
People experience stress as a consequence of daily life events and experiences. It stimulates thinking processes and helps people stay alert to their environment. It results in personal growth and facilitates development. How people react to stress depends on how they view and evaluate the impact of the stressor, its effect on their situation and support at the time of the stress, and their usual coping mechanisms. When stress overwhelms existing coping mechanisms, patients lose emotional balance, and a crisis results. If symptoms of stress persist beyond the duration of the stressor, a person has experienced a trauma.
Scientific Knowledge Base
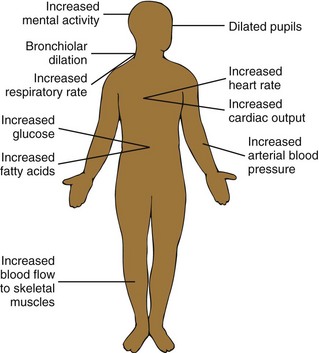
The fight-or-flight response to stress, which is arousal of the sympathetic nervous system, prepares a person for action (Fig. 37-1). Neurophysiological responses to stress function through negative feedback. The process of negative feedback senses an abnormal state such as lowered body temperature and makes an adaptive response such as initiating shivering to generate body heat. Three structures, the medulla oblongata, the reticular formation, and the pituitary gland, control the response of the body to a stressor.
Medulla Oblongata
The medulla oblongata, located in the lower portion of the brainstem, controls heart rate, blood pressure, and respirations. Impulses traveling to and from the medulla oblongata increase or decrease these vital functions. For example, sympathetic or parasympathetic nervous system impulses traveling from the medulla oblongata to the heart control regulation of the heartbeat. The heart rate increases in response to impulses from sympathetic fibers and decreases with impulses from parasympathetic fibers.
Reticular Formation
The reticular formation, a small cluster of neurons in the brainstem and spinal cord, continuously monitors the physiological status of the body through connections with sensory and motor tracts. For example, certain cells within the reticular formation cause a sleeping person to regain consciousness or increase the level of consciousness when a need arises.
Pituitary Gland
The pituitary gland is a small gland immediately beneath the hypothalamus. It produces hormones necessary for adaptation to stress such as adrenocorticotropic hormone, which in turn produces cortisol. In addition, the pituitary gland regulates the secretion of thyroid, gonadal, and parathyroid hormones. A feedback mechanism continuously monitors hormone levels in the blood and regulates hormone secretion. When hormone levels drop, the pituitary gland receives a message to increase hormone secretion. When they rise, it decreases hormone production.
General Adaptation Syndrome
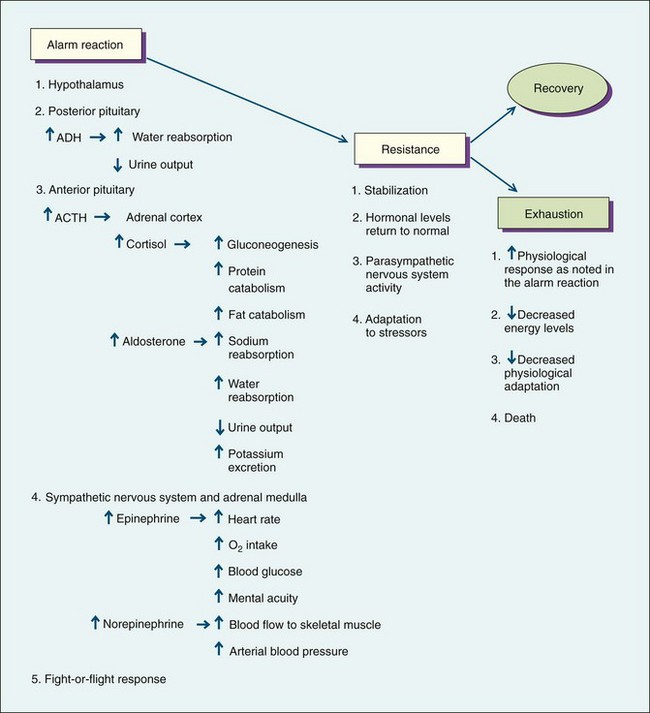
The general adaptation syndrome (GAS), a three-stage reaction to stress, describes how the body responds to stressors through the alarm reaction, the resistance stage, and the exhaustion stage. The GAS is triggered either directly by a physical event or indirectly by a psychological event. It involves several body systems, especially the autonomic nervous and endocrine systems, and responds immediately to stress (Fig. 37-2). When the body encounters a physical demand such as an injury, the pituitary gland initiates the GAS.
During the alarm reaction rising hormone levels result in increased blood volume, blood glucose levels, epinephrine and norepinephrine amounts, heart rate, blood flow to muscles, oxygen intake, and mental alertness. In addition, the pupils of the eyes dilate to produce a greater visual field. If the stressor poses an extreme threat to life or remains for a long time, the person progresses to the second stage, resistance.
During the resistance stage the body stabilizes and responds in a manner opposite to that of the alarm reaction. Hormone levels, heart rate, blood pressure, and cardiac output return to normal; and the body repairs any damage that has occurred. However, if the stress response is chronically activated, a state of allostasis occurs. This chronic arousal with the presence of powerful hormones causes excessive wear and tear on the person and is called allostatic load. An increased allostatic load leads to chronic illness (Diamond, 2009/2010). A persistent allopathic load can cause long-term physiological problems such as chronic hypertension, depression, sleep deprivation, chronic fatigue syndrome, and autoimmune disorders (McEwen, 2005).
The exhaustion stage occurs when the body is no longer able to resist the effects of the stressor and has depleted the energy necessary to maintain adaptation. The physiological response has intensified; but with a compromised energy level, the person’s adaptation to the stressor diminishes.
Reaction to Psychological Stress
The GAS is activated indirectly for psychological threats, which are different for each person and produce differing reactions. The intensity and duration of the psychological threat and the number of other stressors that occur at the same time affect the person’s response to the threat. In addition, whether or not the person anticipated the stressor influences its effect. It is often more difficult to cope with an unexpected stressor. Personal characteristics that influence the response to a stressor include the level of personal control, presence of a social support system, and feelings of competence.
A person experiences stress only if the event or circumstance is personally significant. Evaluating an event for its personal meaning is primary appraisal. Appraisal of an event or circumstance is an ongoing perceptual process. If primary appraisal results in the person identifying the event or circumstance as a harm, loss, threat, or challenge, the person experiences stress. If stress is present, secondary appraisal focuses on possible coping strategies. Balancing factors contribute to restoring equilibrium. According to crisis theory, feedback cues lead to reappraisals of the original perception. Therefore coping behaviors constantly change as individuals perceive new information.
Coping is the person’s effort to manage psychological stress. Effectiveness of coping strategies depends on the individual’s needs. A person’s age and cultural background influence these needs. For this reason no single coping strategy works for everyone or for every stressor. The same person may cope differently from one time to another. In stressful situations most people use a combination of problem- and emotion-focused coping strategies. In other words, when under stress a person obtains information, takes action to change the situation, and regulates emotions tied to the stress. In some cases people avoid thinking about the situation or change the way they think about it without changing the actual situation itself. The type of stress, people’s goals, their beliefs about themselves and the world, and personal resources determine how people cope with stress. Resources include intelligence, money, social skills, supportive family and friends, physical attractiveness, health and energy, and ways of thinking such as optimism (Lazarus, 2007).
Coping mechanisms include psychological adaptive behaviors. Such behaviors are often task oriented, involving the use of direct problem-solving techniques to cope with threats. Ego-defense mechanisms regulate emotional distress and thus give a person protection from anxiety and stress. Ego-defense mechanisms help a person cope with stress indirectly and offer psychological protection from a stressful event. Everyone uses them unconsciously to protect against feelings of worthlessness and anxiety. Occasionally a defense mechanism becomes distorted and no longer helps the person adapt to a stressor. However, people generally find them very helpful in coping and use them spontaneously (Box 37-1). Frequently short-term stressors activate ego-defense mechanisms. These usually do not result in psychiatric disorders.
Types of Stress
Stress includes work, family, chronic, and acute stress; daily hassles; trauma; and crisis. One person looks at a stimulus and sees it as a challenge, leading to mastery and growth. Another sees the same stimulus as a threat, leading to stagnation and loss. The individual with family responsibilities and a full-time job outside the home can experience chronic stress. It occurs in stable conditions and from stressful roles. Living with a long-term illness produces chronic stress. Conversely, time-limited events that threaten a person for a relatively brief period provoke acute stress. Recurrent daily hassles such as commuting to work, maintaining a house, dealing with difficult people, and managing money further complicate chronic or acute stress.
Posttraumatic stress disorder (PTSD) begins when a person experiences, witnesses, or is confronted with a traumatic event and responds with intense fear or helplessness. Some examples of traumatic events that lead to PTSD include motor vehicle crashes, natural disasters, violent personal assault, and military combat. Anxiety associated with PTSD is sometimes manifested by nightmares and emotional detachment. Some people with PTSD experience flashbacks, or recurrent and intrusive recollections of the event. Responses may also include self-destructive behaviors such as suicide attempts and substance abuse.
A crisis implies that a person is facing a turning point in life. This means that previous ways of coping are not effective and the person must change. There are three types of crises: (a) maturational or developmental crises, (b) situational crises, and (c) disasters or adventitious crises (Varcarolis and Halter, 2010). A new developmental stage such as marriage, birth of a child, or retirement requires new coping styles. Developmental crises occur as a person moves through the stages of life. External sources such as a job change, a motor vehicle crash, a death, or severe illness provoke situational crises. A major natural disaster, man-made disaster, or crime of violence often creates an adventitious crisis.
Patient-centered care provides an important context for crisis intervention. The view of the person experiencing a crisis is the frame of reference for the crisis. The vital questions for a person in crisis are, “What does this mean to you; how is it going to affect your life?” What causes extreme stress for one person is not always stressful to another. The perception of the event, situational supports, and coping mechanisms all influence return of equilibrium or homeostasis. A person either advances or regresses as a result of a crisis, depending on how he or she manages the crisis (Lazarus, 2007).
Nursing Knowledge Base
Nurses have proposed theories related to stress and coping. Because stress plays a central role in vulnerability to disease, symptoms of stress often require nursing intervention.
Nursing Theory and the Role of Stress
The Neuman Systems Model is based on the concepts of stress and reaction to it. Nurses are responsible for developing interventions to prevent or reduce stressors on the patient or make them more bearable him or her (Neuman and Fawcett, 2011). This model views the person, family, or community as constantly changing in response to the environment and stressors and helps explain individual, family, and community responses to stressors. All systems experience multiple stressors, each of which potentially disturbs the person’s, family’s, or community’s balance. Examples of stress include intrapersonal stressors such as an illness or injury, interpersonal stressors such as an argument or misunderstanding between two people, or extrapersonal stressors such as financial concerns. Every person develops a set of responses to stress that constitute the “normal line of defense” (Neuman and Fawcett, 2011). This line of defense helps to maintain health and wellness. However, when physiological, psychological, sociocultural, developmental, or spiritual resources are unable to buffer stress, the normal line of defense is broken, and disease often results.
The Neuman Systems Model emphasizes the importance of accuracy in assessment and interventions that promote optimal wellness using primary, secondary, and tertiary prevention strategies (Neuman and Fawcett, 2011). According to Neuman’s theory, the goal of primary prevention is to promote patient wellness by stress prevention and reduction of risk factors. Secondary prevention occurs after symptoms appear. The nurse determines the meaning of the illness and stress to the patient and the patient’s needs and resources for meeting them. Tertiary prevention begins when the patient’s system becomes more stable and recovers. At the tertiary level of prevention the nurse supports rehabilitation processes involved in healing and moving the patient back to wellness and the primary level of disease prevention.
Factors Influencing Stress and Coping
Potential stressors and coping mechanisms vary across the life span. Adolescence, adulthood, and old age bring different stressors. The appraisal of stressors, the amount and type of social support, and coping strategies all balance when assessing stress and depend on previous life experiences. Furthermore, situational and social stressors place people who are vulnerable at higher risk for prolonged stress.
Situational Factors
Situational stress arises from personal or family job changes or relocation. Stressful job changes include promotions, transfers, downsizing, restructuring, changes in supervisors, and additional responsibilities. Adjusting to chronic illness leads to situational stress. Common diseases such as obesity, hypertension, diabetes, depression, asthma, and coronary artery disease provoke stress. Uncertainty associated with treatment and illness triggers stress in patients of all ages. Paying for treatment and limited access to providers also create stress. Although being a family caregiver for someone with a chronic illness such as Alzheimer’s disease is associated with stress, the actions of competent health care providers often minimize the stress for caregivers (Box 37-2).
Maturational Factors
Stressors vary with life stage. Children identify stressors related to their physical appearance, their families, their friends, and school. Preadolescents experience stress related to self-esteem issues, changing family structure as a result of divorce or death of a parent, or hospitalizations. As adolescents search for their identity with peer groups and separate from their families, they experience stress. In addition, they face stressful questions about using mind-altering substances, sex, jobs, school, and career choices. Stress for adults centers around major changes in life circumstances. These include the many milestones of beginning a family and a career, losing parents, seeing children leave home, and accepting physical aging. In old age stressors include the loss of autonomy and mastery resulting from general frailty or health problems that limit stamina, strength, and cognition (Box 37-3).
Sociocultural Factors
Environmental and social stressors often lead to developmental problems. Potential stressors that affect any age-group but are especially stressful for young people include prolonged poverty and physical handicap. Children become vulnerable when they lose parents and caregivers through divorce, imprisonment, or death or when parents have mental illness or substance abuse disorders. Living under conditions of continuing violence, disintegrated neighborhoods, or homelessness affects people of any age, especially young people (Pender et al., 2011). A person’s culture also influences stress and coping (Box 37-4).
Critical Thinking
When caring for a patient experiencing stress, use critical thinking skills to understand the patient’s stressor and the stress response. Integrate knowledge from nursing and other disciplines, previous experiences, and information gathered from patients to understand stress and its impact on the patient and family. Know the neurophysiological changes that occur in the patient experiencing the alarm reaction, resistance stage, and exhaustion stage of the general adaptation syndrome. In addition, know communication principles that contribute to assessing patient’s behaviors. Give utmost attention to determining the patient’s perception of the situation and his or her ability to cope with the stress. If the patient’s usual coping skills have not helped or his or her support systems have failed, use crisis intervention counseling.
Experience teaches you to understand the patient’s unique perspective and view each person as an individual, recognizing that no two people are exactly alike. Experience with patients also helps you to recognize responses to stress. In addition, personal experiences with stress and coping increase your ability to empathize with a patient temporarily immobilized by stress.
Be confident in the belief that you and your patients can effectively manage stress. Patients who feel overwhelmed and perceive events as being beyond their capacity to cope rely on you as an expert. Patients respect your advice and counsel and gain confidence from your belief in their ability to move past the stressful event or illness. Patients overwhelmed by life events are often unable, at least initially, to act on their own behalf and require either direct intervention or guidance. Integrity is an essential attitude through which you respect the patient’s perception of the stressor. Make the effort to have the patient explain his or her unique viewpoint and situation.
The practice standards for psychiatric mental health nursing (ANA, 2007) guide assessment of a patient’s stress, coping mechanisms, and support system before intervening. Use linguistic and culturally effective communication skills to clearly and precisely understand a patient’s perception of stress. Focus on factors relevant to his or her well-being. In addition, the patient expects you to exhibit confidence and integrity when he or she feels vulnerable. Be especially aware of the ethical responsibility in caring for someone who has diminished autonomy as a result of stress.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Through the Patient’s Eyes
Assessment of a patient’s stress level and coping resources requires that you first establish a trusting nurse-patient relationship because you are asking a patient to share personal and sensitive information. Learn from the patient both by asking questions and by making observations of nonverbal behavior and the patient’s environment. Synthesize the information and adopt a critical thinking attitude while observing and analyzing patient behavior (Fig. 37-3). Often the patient has difficulty expressing exactly what is most bothersome about the situation until there is an opportunity to discuss it with someone who has time to listen.
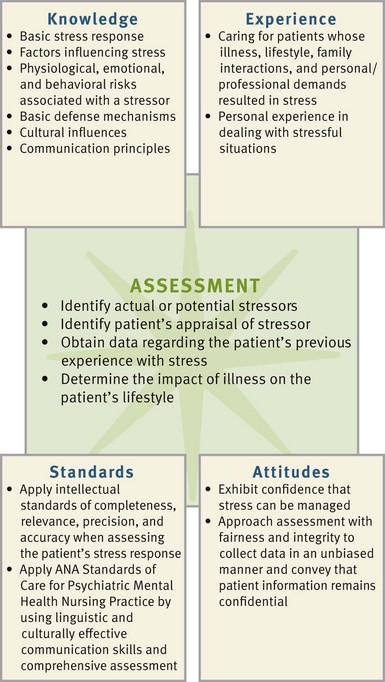
FIG. 37-3 Critical thinking model for stress and coping assessment. ANA, American Nurses Association.
Begin your assessment with an open-ended question such as, “What is happening in your life that caused you to come today?” or “What happened in your life that is different?” This requires some focusing by the patient. Next assess the patient’s perception of the event, available situational supports, and what he or she usually does when there is a problem that he or she cannot solve. Determine if a person is suicidal or homicidal by asking directly. For example, ask, “Are you thinking of killing yourself or someone else?” If so, determine in a caring and concerned manner if the person has a plan and determine how lethal the means are.
Take time to understand a patient’s meaning of the precipitating event and the ways in which stress is affecting his or her life. Allow time for him or her to express priorities for coping with stress. For example, in the case of a woman who has just been told that a breast mass was identified on a routine mammogram, it is important to know what the patient wants and needs most from the nurse. Although some women in this situation identify their need for information about biopsy or mastectomy as their personal priority, others need guidance and support in discussing how to share the news with family members. In some cases, when there is nothing that will change or improve the situation, allowing the patient to use denial as a coping mechanism is helpful. Gaining an understanding of patient expectations does not mean excluding certain types of care that are important simply because a patient does not identify them as needs. However, by inquiring about patient expectations and priorities, you are better able to ensure that you address all of the patient’s needs in some way.
Stress also occurs in a family or a community. Stress in a family is sometimes from a critically ill family member, the sudden loss of a job, a move, or becoming homeless. An example of stress in a community is a natural disaster such as a major flood or the sudden, unexpected death of a beloved teacher or teenager. To develop appropriate and safe nursing care when caring for families or communities, ensure that you understand the meaning that the stress has for that group.
Subjective Findings
When assessing a patient’s level of stress and coping resources, create a nonthreatening physical environment for the interaction. Assume the same height as the patient, arranging the interview environment so you can maintain or avoid eye contact comfortably. You do this by placing chairs at a 90-degree angle or side by side to reduce the intensity of the interaction (Varcarolis and Halter, 2010). Gather information about the health status of the patient from his or her perspective and begin the process of developing a trusting relationship with him or her. Use the interview to determine the patient’s view of the stress, coping resources, any possible maladaptive coping, and adherence to prescribed medical recommendations such as medication or diet (Box 37-5). If the patient is using denial as a coping mechanism, be alert to whether he or she is overlooking necessary information. As in all interactions with the patient, respect the confidentiality and sensitivity of the information shared.
Objective Findings
Obtain objective findings related to stress and coping through observation of the appearance and nonverbal behavior of a patient. Observe grooming and hygiene, gait, characteristics of the handshake, actions while sitting, quality of speech, eye contact, and the attitude of the patient during the interview. Before the interview begins or at the end of the interview, depending on the anxiety level of the patient, obtain basic vital signs to assess for physiological signs of stress such as elevated blood pressure, heart rate, or respiratory rate. Make certain to incorporate cultural components of interpreting the patient’s nonverbal communication behaviors.
Nursing Diagnosis
A review of assessment data leads the nurse to cluster data that indicate a potential or actual stressor and the patient’s response. Clustering data, along with the application of the nurse’s knowledge and experiences with patients in stress, leads to individualized nursing diagnoses (Box 37-6).
Nursing diagnoses for people experiencing stress generally focus on coping. Specifically major defining characteristics of ineffective coping include verbalization of an inability to cope and an inability to ask for help. To identify defining characteristics, ask the patient what is of most concern at the time of the interview. It is important to allow him or her sufficient time to answer. Observe for nonverbal signs of anxiety, fear, anger, irritability, and tension in a patient who is experiencing ineffective coping. Other defining characteristics include the presence of life stress, an inability to meet role expectations and basic needs, alteration in societal participation, self-destructive behavior, change in usual communication patterns, high rate of accidents, excessive food intake, drinking, smoking, and sleep disturbances. Stress often results in multiple nursing diagnoses. Examples of these diagnoses include but are not limited to the following:
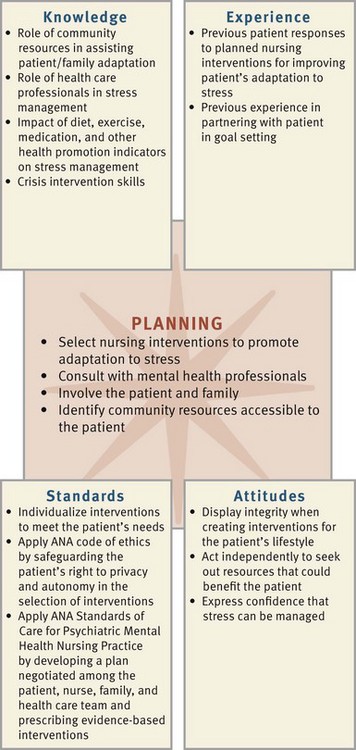
Planning
Desirable outcomes for persons experiencing stress frequently include effective coping, family coping, caregiver emotional health, and psychosocial adjustment: life change. The nurse often selects interventions for stress and improved coping such as coping enhancement and crisis intervention in addition to individualized interventions after considering the nursing diagnosis, the resources available to the patient, and the goals identified by the patient and nurse (Fig. 37-4).
Nursing interventions are designed within the framework of primary, secondary, and tertiary prevention. At the primary level of prevention you direct nursing activities to identifying individuals and populations who are possibly at risk for stress. Nursing interventions at the secondary level include actions directed at symptoms such as protecting the patient from self-harm. Tertiary-level interventions assist the patient in readapting and can include relaxation training and time-management training. The nurse and the patient assess the level and source of the existing stress and determine the appropriate points for intervention to reduce it (Pender et al., 2011) (see the Nursing Care Plan).
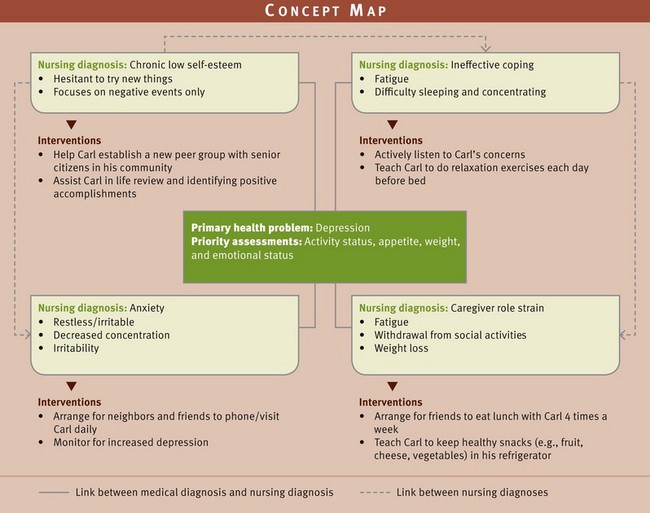
Another method of planning care is through the use of a concept map (Fig. 37-5 on p. 740). Concept maps identify multiple nursing diagnoses from the assessment database and show how they are related. In this example the nursing diagnoses are linked to the patient’s medical diagnosis of depression. In addition, the concept map shows the relationship among the nursing diagnoses chronic low self-esteem, ineffective coping, anxiety, and caregiver role strain. Use of a concept map requires critical thinking skills to organize patient data and assists in planning for patient-centered care.
Just as the nursing assessment of the patient’s stress and coping depends on the patient’s perception of the problem and coping resources, the interventions focus on a partnership with the patient and support system, usually the family. In the case of a family or community stressor and impaired family or community coping, the view of the situation and resources is broader.
Setting Priorities
Consider the patient’s perspective and responses to assessment questions when setting priorities for care (see the Nursing Care Plan). The patient’s clinical condition and perception of stress determine which nursing diagnosis has the greatest priority. As in all areas of nursing, safety of the patient and others in his or her environment is the first priority.
If suicide or homicide is not an issue, examine other potential threats to the safety of vulnerable people who are under the care of the patient. Provide for their temporary care or supervision if necessary. Other potential threats to safety include nutritional deficits; insomnia; self-care deficits; and poor judgment and impulsiveness that possibly lead to unsafe decisions about sex, drugs, money, or damage to personal relationships that the person might later regret. Determine the degree of work, school, home, and family disruption in the person’s life. When you have completed immediate assessment and ensured safety, begin the problem-solving process.
Teamwork and Collaboration
Collaborate with occupational therapists, dietitians, pastoral care professionals, and health care professionals from other clinical specialties, depending on the patient’s situation. The scope of your nursing practice cannot meet all of the patient’s needs. Patients experiencing stress from medical conditions or psychiatric disorders present needs that make it necessary for you to consult with advanced practice mental health nurses, psychiatrists, psychologists, or psychiatric social workers. A multidisciplinary approach addresses the holistic needs of the patient. Recognize the need for collaboration and consultation; inform the patient about potential resources; and make arrangements for interventions such as consultations, group sessions, or therapy as needed. A hospital social worker shares ideas for available resources both within the hospital and in the community. A home care nurse knows community services, groups, and appropriate contacts.
In addition to maximizing use of available resources for the patient, collaborative care also benefits the nurse. While working with patients experiencing stress, you gain a broad understanding of the multitude of health care disciplines. Work becomes more satisfying. Contacts with other members of the multidisciplinary team and the community provide a feeling of contributing to the teamwork of providing holistic care.
Implementation
Three primary modes of intervention for stress are to decrease stress-producing situations, increase resistance to stress, and learn skills that reduce physiological response to stress (Pender et al., 2011). Educate patients and families about the importance of health promotion (Box 37-7).
Regular Exercise: A regular exercise program improves muscle tone and posture, controls weight, reduces tension, and promotes relaxation. In addition, exercise reduces the risk of cardiovascular disease and improves cardiopulmonary functioning. Patients who have a history of a chronic illness, are at risk for developing an illness, or are older than 35 years of age should begin a physical exercise program only after discussing the plan with a health care provider (Fig. 37-6).
Support Systems: A support system of family, friends, and colleagues who listen, offer advice, and provide emotional support benefits a patient experiencing stress. Many support groups are available to individuals (e.g., those sponsored by the American Heart Association and the American Cancer Society, local hospitals and churches, and mental health organizations).
Time Management: Time management techniques include developing lists of prioritized tasks. For example, help patients list tasks that require immediate attention, those that are important and can be delayed, and those that are routine and can be accomplished when time becomes available. In many cases setting priorities helps individuals identify tasks that are not necessary or can be delegated to someone else.
Guided Imagery and Visualization: Guided imagery is based on the belief that a person significantly reduces stress with imagination. It is a relaxed state in which a person actively uses imagination in a way that allows visualization of a soothing, peaceful setting. Typically the image created or suggested uses many sensory words to engage the mind and offer distraction and relaxation.
Progressive Muscle Relaxation: In the presence of anxiety-provoking thoughts and events, a common physiological symptom is muscle tension. Diminish physiological tension through a systematic approach to releasing tension in major muscle groups. Typically an individual achieves a relaxed state through deep chest breathing. Once the patient is breathing deeply, direct him or her to alternately tighten and relax muscles in specific groupings.
Assertiveness Training: Assertiveness includes skills for helping individuals communicate effectively regarding their needs and desires. The ability to resolve conflict with others through assertiveness training is important for reducing stress. Teaching assertiveness in a group setting increases the benefits of the experience.
Journal Writing: For many people keeping a private, personal journal provides a therapeutic outlet for stress. Suggest that patients keep journals, especially during difficult situations. In a private journal patients are able to express a full range of emotion and vent their honest feelings without hurting anyone else’s feelings and without concern for how they appear to others.
Stress Management in the Workplace: Stressors such as rapid changes in health care technology, diversity in the workforce, organizational restructuring, and changing work systems place stress on employees. Burnout occurs as a result of chronic stress. In nursing burnout frequently results from intense caregiving and manifests as emotional exhaustion, loss of a sense of personal identity, and feelings of failure.
If you or your patients experience burnout, it helps to make changes in behavior to cope with workplace stress. An important step is identifying the limits and scope of responsibilities at work. Recognizing the areas over which you have control and can change and those for which you do not have responsibility is a vital insight. Making a clear separation between work and home life is also crucial. Strengthening friendships outside of the workplace, arranging for temporary social isolation for personal “recharging” of emotional energy, and spending off-duty hours in interesting activities all help reduce burnout.
Acute Care
Crisis Intervention: When stress overwhelms a person’s usual coping mechanisms and demands mobilization of all available resources, it becomes a crisis. A crisis creates a turning point in a person’s life because it changes the direction of his or her life in some way. The precipitating event usually occurs approximately 1 to 2 weeks before the individual seeks help, but sometimes it has occurred within the past 24 hours. Generally a person resolves the crisis in some way within approximately 6 weeks. Crisis intervention aims to return the person to a precrisis level of functioning and promote growth (Fig. 37-7).

FIG. 37-7 Crisis intervention model. (Redrawn from Aguilera DC: Crisis intervention: theory and methodology, ed 8, St Louis, 1998, Mosby.)
Because an individual’s or family’s usual coping strategies are ineffective in managing the stress of the precipitating event, the use of new coping mechanisms is necessary. This experience forces the use of unfamiliar strategies and results in either a heightened awareness of previously unrecognized strengths and resources or deterioration in functioning. Thus a crisis is often referred to as a situation of both danger and opportunity. Some individuals or families emerge from a crisis state functioning more effectively, whereas others find themselves weakened, and still others are completely dysfunctional.
Crisis intervention is a specific type of brief psychotherapy with prescribed steps. It is more directive than traditional psychotherapy or counseling, and any member of the health care team who has been trained in its techniques can use it. The basic approach is problem solving, and it focuses only on the problem presented by the crisis.
When using a crisis intervention approach, you help the patient make the mental connection between the stressful event and his or her reaction to it. This is crucial because he or she is sometimes unable to see the whole situation clearly. You also help the person become aware of present feelings such as anger, grief, or guilt to help him or her reduce feelings of tension. In addition, you help the patient explore coping mechanisms, perhaps identifying new methods of coping. Finally you help the person increase social contacts if he or she has been isolated and overly self-focused.
Restorative and Continuing Care
A person under stress recovers when the stress is removed or coping strategies are successful; however, a person who has experienced a crisis has changed, and the effects often last for years or for the rest of the person’s life. The final stage of adapting to a crisis is acknowledgment of the long-term implications of the crisis. If a person has successfully coped with a crisis and its consequences, he or she becomes more mature and healthy. When a person recovers from a stressful situation, the time is right for introducing stress management skills to reduce the number and intensity of stressful situations in the future.
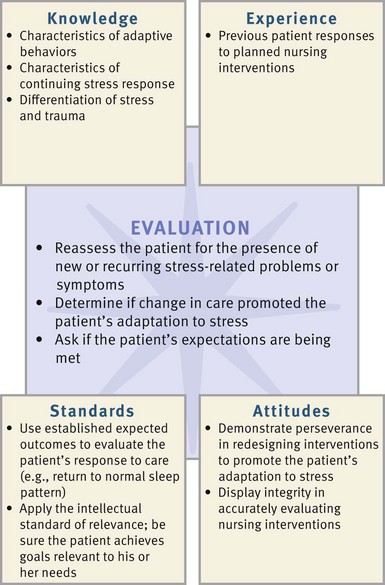
Evaluation
A patient recovering from acute stress often spontaneously reports feeling better when the stressor is gone. The recovery from chronic stress occurs more gradually as the patient emerges from the strain. In either situation reassess the patient for the presence of new or recurring stress-related symptoms (Fig. 37-8). Observe patient behaviors and talk with the patient and family if appropriate. Ask the patient about sleep patterns, appetite, and ability to concentrate. Ask about coping strategies that the patient uses and determine their effectiveness. Ask patients to compare current feelings and behaviors with feelings and behaviors 6 months ago. If desired outcomes have been met, the patient reports feeling better now than 6 months ago.
Patient Outcomes
Remember that coping with stress takes time. Maintain ongoing communication with patients regarding their coping. Patients under severe stress, or trauma, often experience feelings of powerlessness, vulnerability, and loss of control. The nurse addresses these feelings by actively involving patients and families in the processes of problem identification (assessment), prioritizing, goal setting, and evaluation. Involving patients in these processes gives them an opportunity to direct their energy in a positive way and moves them toward taking greater responsibility for health maintenance and promotion.
Engaging the patient as a partner in health care sets the stage for open communication. In such an environment the patient feels freer to give important feedback about interventions that are successful and helps the nurse better understand why some interventions fail to meet the established goals. If he or she reports continued acute stress, assess for safety by asking about whether or not there have been any recent accidents at home, in the car, or at work. Ask about coping strategies to determine if the patient is using unsafe, maladaptive strategies. If the patient reports continued chronic stress, ask about his or her perception of the stressor and coping behaviors used. Discuss the stressor with the patient to determine if it needs to be redefined. If contact with a patient ends before you have achieved the resolution of goals, it is important to refer him or her to appropriate resources so progress is not delayed or interrupted.
An essential part of the evaluation process is collaborating with patients to determine if their own expectations from nursing have been met. Any revision in the plan of care includes steps to address patient expectations.
Key Points
• The general adaptation syndrome is an immediate physiological response of the whole body to stress and involves several body systems, especially the autonomic nervous and endocrine systems. Physiological responses to stress also include immunological changes.
• Stress can make people ill as a result of increased levels of powerful hormones that change bodily processes.
• A person is under psychological stress only if he or she evaluates the event or circumstance as personally significant. Such an evaluation of an event for its personal meaning is called primary appraisal.
• There are several types of stress, including work, family, chronic, and acute stress; daily hassles; trauma; and crisis.
• Nurses recognize and respond to caregiver stress of family members of patients.
• Rapid changes in health care technology, diversity in the workforce, organizational redesign, and changing work systems place stress on employees, including nurses.
• Potential stressors and coping mechanisms vary across the life span.
• Coping means making an effort to manage psychological stress.
• Coping is a process that constantly changes to manage demands on a person’s resources.
• Three primary modes for stress intervention are to decrease stress-producing situations, increase resistance to stress, and learn skills that reduce physiological response to stress.
• A patient whose stress is so severe that he or she is unable to cope using any of the means that have worked before is experiencing a crisis.
• A crisis is a turning point in life and is developmental, situational, or adventitious.
• Generally a crisis is resolved in some way within approximately 6 weeks. Crisis intervention aims to return the person to a precrisis level of functioning and to promote growth.
Clinical Application Questions
Preparing for Clinical Practice
1. You are making a home visit to see 80-year-old Carl and 81-year-old Evelyn because Evelyn has Alzheimer’s dementia and her health care provider is concerned about her nutrition. He also wants to know if she is taking her medications. Carl has been providing Evelyn’s care, and he is also worried about his own health. Discuss the various stressors that need to be considered when assessing their situation.
2. Carl reports dizziness; however, based on your thorough assessment, you do not identify any physical findings that would account for this. As you talk with Carl, he tells you that his life is very stressful and he is barely coping. He is the sole caregiver for his wife, Evelyn, who has dementia. He is worried about what might happen to her if his health failed. He has not been able to play golf with his friends or go to church in months. His only social activity is a trip to the grocery store while his neighbor stays with Evelyn. He is worried that they will spend all their life savings if she needs to go to a nursing home, and he loses his patience with her. Develop nursing diagnoses related to this situation.
3. Carl is admitted to the hospital with a fractured hip sustained from a fall when he got up during the night to check on Evelyn who was wandering in the house. Before his injury he cared for Evelyn, who suffers from advancing Alzheimer’s disease. While he is hospitalized, Evelyn stays with a niece who lives 100 miles away, but this cannot be a permanent situation because their niece is also in frail health. Carl and Evelyn’s children live across the country and are very involved in their careers. He is concerned about who will care for Evelyn and how he will manage when he is discharged. What approach would be the best to take in planning Carl’s care?
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. When teaching a patient about the negative feedback response to stress, the nurse includes which of the following to describe the benefits of this stress response?
2. A nurse observes that a patient whose home life is chaotic with intermittent homelessness, a child with spina bifida, and an abusive spouse appears to be experiencing an allostatic load. As a result, the nurse expects to detect which of the following while assessing the patient?
3. A patient who is having difficulty managing his diabetes mellitus responds to the news that his hemoglobin A1C, a measure of blood sugar control over the past 90 days, has increased by saying, “The hemoglobin A1C is wrong. My blood sugar levels have been excellent for the last 6 months.” The patient is using the defense mechanism:
4. When doing an assessment of a young woman who was in an automobile accident 6 months before, the nurse learns that the woman has vivid images of the crash whenever she hears a loud, sudden noise. The nurse recognizes this as ____________.
5. A grandfather living in Japan worries about his two young grandsons who disappeared after a tsunami. This is an example of:
6. During the assessment interview of an older woman experiencing a developmental crisis, the nurse asks which of the following questions?
1. How is this flood affecting your life?
2. Since your husband has died, what have you been doing in the evening when you feel lonely?
3. How is having diabetes affecting your life?
4. I know this must be hard for you. Let me tell you what might help.
7. The nurse plans care for a 16-year-old male, taking into consideration that stressors experienced most commonly by adolescents include which of the following?
1. Loss of autonomy caused by health problems
2. Physical appearance, family, friends, and school
3. Self-esteem issues, changing family structure
4. Search for identity with peer groups and separating from family
8. A child who has been in a house fire comes to the emergency department with her parents. The child and parents are upset and tearful. During the nurse’s first assessment for stress the nurse says:
1. “Tell me who I can call to help you.”
2. “Tell me what bothers you the most about this experience.”
3. “I’ll contact someone who can help get you temporary housing.”
4. “I’ll sit with you until other family members can come help you get settled.”
9. When assessing an older adult who is showing symptoms of anxiety, insomnia, anorexia, and mild confusion, one of the first assessments includes which of the following?
10. After a health care provider has informed a patient that he has colon cancer, the nurse enters the room to find the patient gazing out the window in thought. The nurse’s first response is which of the following?
1. “Don’t be sad. People live with cancer every day.”
2. “Have you thought about how you are going to tell your family?”
3. “Would you like for me to sit down with you for a few minutes so you can talk about this?”
4. “I know another patient whose colon cancer was cured by surgery.”
11. A 34-year-old man who is anxious, tearful, and tired from caring for his three young children tells you that he feels depressed and doesn’t see how he can go on much longer. Your best response would be which of the following?
1. “Are you thinking of suicide?”
2. “You’ve been doing a good job raising your children. You can do it!”
12. The nurse is evaluating the coping success of a patient experiencing stress from being newly diagnosed with multiple sclerosis and psychomotor impairment. The nurse realizes that the patient is coping successfully when the patient says:
1. “I’m going to learn to drive a car so I can be more independent.”
2. “My sister says she feels better when she goes shopping, so I’ll go shopping.”
3. “I’ve always felt better when I go for a long walk. I’ll do that when I get home.”
4. “I’m going to attend a support group to learn more about multiple sclerosis.”
13. A patient newly diagnosed with type 2 diabetes says, “My blood sugar was just a little high. I don’t have diabetes.” The nurse responds:
1. “Let’s talk about something cheerful.”
2. “Do other members of your family have diabetes?”
3. “I can tell that you feel stressed to learn that you have diabetes.”
14. A staff nurse is talking with the nursing supervisor about the stress that she feels on the job. The supervising nurse recognizes that:
1. Nurses who feel stress usually pass the stress along to their patients.
2. A nurse who feels stress is ineffective as a nurse and should not be working.
3. Nurses who talk about feeling stress are unprofessional and should calm down.
4. Nurses frequently experience stress with the rapid changes in health care technology and organizational restructuring.
15. A crisis intervention nurse working with a mother whose Down syndrome child has been hospitalized with pneumonia and who has lost her entitlement check while the child is hospitalized can expect the mother to regain stability after how long?
Answers: 1. 1; 2. 3; 3. 1; 4. Posttraumatic stress disorder (PTSD); 5. 3; 6. 2; 7. 4; 8. 2; 9. 3; 10. 3; 11. 1; 12. 4; 13. 4; 14. 4; 15. 2.
References
Aldwin, CM. Stress, coping and development: an integrative perspective, ed 2. New York: Guilford Press; 2007.
American Nurses Association (ANA):. Psychiatric–mental health nursing: scope and standards of practice. Silver Spring, Md: ANA; 2007.
Diamond, JW. Allostatic medicine: bringing stress, coping, and chronic disease into focus. Part 1. Integrat Med. Dec 2009/Jan 2010;8(6):40.
Lazarus, RS. Stress and emotion: a new synthesis. In: Monat A, Lazarus RS, Reevy G, eds. The Praeger handbook on stress and coping. Westport, Conn: Praeger, 2007.
McEwen, BS. Stressed or stressed out: what is the difference. J Psychiatry Neurosci. 2005;50(5):315.
Neuman B, Fawcett J, eds. The Neuman Systems Model, ed 5, Upper Saddle River, NJ: Pearson, 2011.
Pender, NJ, Murdaugh, C, Parsons, MA. Health promotion in nursing practice, ed 6. Upper Saddle River, NJ: Howorth Press; 2011.
Varcarolis, EM, Halter, MJ. Foundations of psychiatric mental health nursing: a clinical approach, ed 6. St Louis: Saunders; 2010.
Research References
Anngela-Cole, L, Hilton, JM. The role of attitudes and culture in family caregiving for older adults. Home Health Care Services Q. 2009;28:59.
Bertisch, SM, Wee, CC, Phillips, RS, McCarthy, EP. Alternative mind-body therapies used by adults with medical conditions. J Psychosom Res. 2009;66(6):511.
Folkman, S, et al. Age differences in stress and coping. Psychol Aging. 1987;2(2):171.
Haley, WE, et al. Problems and benefits reported by stroke family caregivers: results from a prospective epidemiological study. Stroke J Am Heart Assoc. 2009;40:2129.
Marziali, E, Garcia, LJ. Dementia caregivers’ responses to 2 internet-based intervention programs. Am J Alzheimers Dis Other Dementias. 2011;26(1):36.
Oken, BS, et al. Pilot controlled trial of mindfulness meditation and education for dementia caregivers. J Altern Complement Med. 2010;16:1031.
Pressler, SJ, et al. Family caregiver outcomes in heart failure. Fam Crit Care. 2009;18:149.
Ruppar, TM, Conn, VS. Interventions to promote physical activity in chronically ill adults. Am J Nurs. 2010;110(7):30.
Sussman, T, Regehr, C. The influence of community-based services on the burden of spouses caring for their partners with dementia. Health Social Work. 2009;34(1):29.
Yancura, LA, Aldwin, CM. Coping and health in older adults. Curr Psych Rep. 2008;10:10.