CHAPTER 25 Considerations for the Use of Dental Implants With Removable Partial Dentures
Dental implants are increasingly being used in a variety of ways in the replacement of teeth. Providing implants to support all teeth needing replacement is often preferable if indicated and if the patient can afford to do so. If the patient is unable to pursue an implant-only supported prosthesis, this should not keep him or her from considering an implant, because the patient still may benefit from a carefully selected implant used for critical clinical performance advantage when removable partial dentures are pursued. Additionally, implants can be used for removable partial dentures to allow future implant-only treatment options.
This chapter presents basic considerations in the selection of implants to improve prosthesis performance by increasing functional stability. Prosthesis instability, a commonly stated problem with removable prostheses, is presented as a potentially confounding and unique component of oral sensory-motor function at issue when patients are challenged with removable prostheses. When all the relevant information necessary to adequately address how best to manage a patient’s tooth loss is considered,* one aspect that should be kept in mind is that among the various prostheses from which we choose (conventional fixed partial denture, implant-supported partial denture, and removable partial denture), the removable partial denture is the most unique. Exactly how we describe this uniqueness to our patients is critical to their appropriate prosthesis selection and provides a clue to us as to how dental implants can best be used in conjunction with removable partial dentures (RPDs).
Physiologic Distinction Between Prostheses
Although physiologic aspects of replacement prostheses have not been adequately researched, the fact that removable partial dentures are less like teeth than fixed prostheses strongly suggests that we should delineate this to our patients. The most obvious difference between treatment options is the manner in which they are supported—conventional fixed partial dentures using teeth with periodontal ligaments versus implant prostheses using osseointegrated implants versus RPDs using teeth, or teeth and mucosa. An additional difference is the rigidity associated with the prosthesis-tooth interface connection—cemented prostheses rigidly connected to teeth versus screw-retained implant prostheses rigidly connected between implants versus clasp/attachment-retained removable partial denture prostheses.
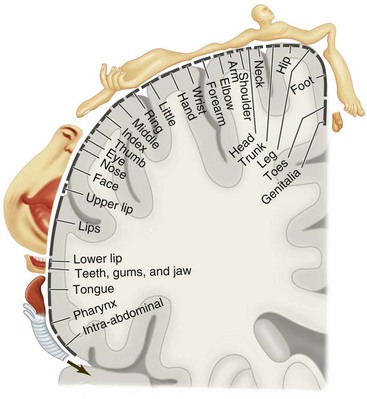
Given this support and rigid connection difference, it is easy to recognize that one distinguishing difference between fixed prostheses (tooth or implant supported) and tooth-tissue–supported RPDs is the potential for movement under function. The impact that such movement will have on related oral sensory and oral functional expectations of patients is potentially critical to understand. These patient-specific perspectives are variable because some of our patients are better at distinguishing oral sensory input than others and some are more functionally capable than others. The importance of sensory-functional considerations is evident when it is realized that the oral cavity is unique from a sensory perception standpoint, because the sensory input from the mouth regions involved in the task of mastication represents one of the largest collections of sensory information processed for a single functional act in the body, rivaled closely by the multifunctional hand (Figure 25-1).
Replacing Anatomy and Functional Ability
With this relative importance of oral sensory function associated with mastication in mind, it would be helpful to consider what exactly we are attempting to replace when we discuss with our patients the management of missing teeth. This involves both the physical tools for mastication and the oral ability for precise and stable neuromuscular functions to manipulate a bolus of food. Analysis of chewing studies shows that the oral receptor feedback that guides movement of the mandible comes from various sources. The most sensitive input (i.e., the input that provides the most refined and precisely controlled movement) comes from the periodontal mechanoreceptors (PMRs), with additional input coming from the gingiva, mucosa, periosteum/bone, and temporomandibular joint (TMJ) complex. Loss of teeth leads to loss of guidance precision, which may be caused by the deficit in PMRs. No artificial replacements reestablish the same ability inherent in the PMR guidance. Yet prostheses may vary in their ability to affect the deficit on the basis of sensory-related dynamics. This notion of variable prosthesis impact suggests that either the prostheses are not the same or patients may vary in terms of neuromuscular* ability.
What is meant by the term neuromuscular ability? This is the task-specific sensory-motor performance “ability” that a specific patient possesses for the task/act of mastication. It involves multiple factors, including the selection of a prosthesis that may vary in qualitative neuromuscular ability compared with the gold standard—natural teeth. This prosthesis influence can be favorable when replacements are more like teeth (in their neuromuscular sensory input nature), or it can be unfavorable if they are unlike teeth and potentially cause confounding sensory input that diminishes function (e.g., implant fixed partial denture vs. denture base). This therapeutic variability suggests that prostheses differ in the influence they have on oral sensory receptors; therefore this may affect our patient’s perspective on how much we have improved the rehabilitation of oral function (i.e., neurophysiologic ability rehabilitation).
Stability under function is critical for limiting confounding sensory input because instability is a significant confounder of normal function. Whether a prosthesis is stable or unstable influences whether it provides a positive or a negative contribution to an already reduced peripheral receptor influence. This is compounded by the inherent neuromuscular variability seen between patients. Consequently, in some of our patients, replacement teeth may have less of a “margin” for sensory contribution without creating functional impediments.
Strategically Placed Implants for RPD Stability and Improved Patient Accommodation
To decide which treatment option is best from a patient accommodation perspective, it must be determined whether this specific patient possesses the ability to meet the challenge posed by the neuromuscular deficit. If the answer is yes, then the patient may be an appropriate candidate for an RPD. However, if the answer is no and for good reasons an RPD is chosen, the use of strategically located implants to assist the patient in meeting the challenge should be discussed.
Stated differently, the success of any prosthesis may be compromised by a significant level of sensory loss. In addition, if the patient also possesses an inherently poor neurophysiologic ability, the choice of a prosthesis that creates an additional sensory “burden” may make the situation too challenging for the patient. The greatest contributing factor to the challenge is instability, and stability is most efficiently improved by the use of dental implants.
Movement Control with Selective Implant Placement
The most beneficial use of an implant with a removable partial denture is to reduce the negative impact of any sensory input resulting from prosthesis movement. The greatest potential for movement is seen with Kennedy Class I and II prostheses. Consequently, the greatest benefits in the use of implants with Class I and II removable partial dentures are to gain stability, control prosthesis movement, and reduce unnatural sensations that are movement related.
The clinician who is deciding exactly where to place an implant for the greatest benefit should take into consideration many factors. The ultimate decision will likely be influenced by a combination of important clinical issues. Basic considerations include factors associated with support, stability, and retention; residual ridge anatomy; strategic tooth loss; opposing occlusal influence; and the condition of a terminal tooth.
Placement for Support versus Retention
When considering where to place an implant to assist an RPD, we should ask, “What will best serve the patient over time?” Certainly, we want the prostheses to be adequately retained, but as we consider what the retentive need for our removable partial denture is, we should also ask, “Is it the most important issue that patients face?”
Support for prostheses is the characteristic that resists the greatest functional forces—those associated with chewing. A well-supported prosthesis is likely to impart less displacement to the soft tissue; less displacement likely is associated with a more comfortable prosthesis. If the major concern is comfort, then support is more often the best treatment target for an implant. The most effective location for resisting force would be the posterior occlusal contact position—that position where the forces of occlusion are likely the greatest.
Anatomic Concerns for Class I and II Arches
It is clear that placement of implants within the alveolar ridge requires adequate bone volume. Tooth loss commonly leads to residual ridge resorption; the longer from the time of extraction that a patient is seen, the more alveolar resorption is expected.
When this occurs in the posterior jaw, vertical loss of volume at the ridge crest is complicated by the maxillary sinus and inferior alveolar nerve at the apical location. These anatomic boundaries require careful consideration of surgical manipulation and must be considered as potentially more burdensome to the patient (i.e., they increase surgical risk). It is unclear at this time whether shortened implants (≤ 8 mm) in posterior edentulous regions are adequate for the necessary resistance. Certainly, the opposing occlusion contributes to this decision and natural teeth would be expected to generate more forceful occlusal function demanding greater implant resistance, compared with an opposing complete denture prosthesis.
Benefits of Implant versus Surveyed Crown
Surveyed crowns have long been used to maximize support, stability, and retention for removable partial dentures. The ability to control expected movement in the removable prosthesis can be improved by the use of such a carefully contoured crown. The same can be said for an implant, which presents a logical comparison as to which is a better choice for patients.
As an example, if a patient is deciding between a crown on tooth #6 versus an implant at site #5, what should he or she be considering? Both can be used to provide support, stability, and retention. If the crown is designed to accommodate an attachment, it can also be used without a visible clasp. This is a more technically demanding intervention and carries with it more challenging maintenance requirements. Also, the typical consideration regarding caries risk should be discussed. This suggests the need to think about long-term needs when deciding between options.
The implant at site #5 can reduce the need for a clasp, while at the same time providing a reasonably simple maintenance requirement for managing attachment needs. The implant attachment can be easily accommodated within a simple RPD framework that accommodates the #5 replacement tooth and available prosthetic space for attachment needs. Variable retention is available based on the type of attachment selected—an advantage over the use of a clasp, which carries the risk of fracture with repeated adjustment over time.
Strategically Lost Tooth and Implant Use
Loss of a canine or molar abutment in an existing removable prosthesis can have a significantly negative impact on the prosthesis. Resistance to movement toward the tissue and across the tissue (aspects of support and stability) is greatly affected. Previous interventions for strategic tooth loss, such as the Swing-Lock prosthesis, have been based on recognition of the need to use more teeth to meet the demands for comfortable, stable function. Use of an implant in this situation can directly address the loss of a strategic component that controls functional movement and may be able to utilize the existing prosthesis.
Use of Abutment for Support and/or Retention
As an implant is placed more distally (in a distal extension), it serves more of a support function than a retention function. In a situation where support and retention are desired, the connecting design (the actual attachment male-female components) must allow adequate resistance to supporting forces without premature deformation of the retentive component and reduction of the retaining properties.
Generally a component designed to primarily provide retention may not serve a supportive role for the desired period of time before replacement. Use of a more resistant retentive element to better resist supportive forces may provide retention in excess of the patient’s ability to comfortably remove the prosthesis for daily hygiene.
Influence of Opposing Occlusion on Implant Location and Implant Abutment Design
Distal extension removable partial dentures are significantly influenced by the type and plane of orientation of the opposing dentition. Opposing complete dentures, which exhibit a regular occlusal plane, encourage equal force distribution associated with occlusion, allowing an optimum scenario for comfort.
Irregular occlusal planes created by super-erupted opposing natural teeth make control of functional forces more challenging at the residual alveolar ridge level. Use of implants for such oral conditions may improve prosthesis comfort, especially if support is fully utilized (i.e., no retainer function). In such a scenario, implant abutment design should serve to control movement toward and across the denture bearing area. This places a premium on nonresilient and nonretentive abutment designs. Care should be taken to closely follow such designs during the early postinsertion phase because the potential for excessive occlusal loads could have detrimental effects on abutment connections and implant stability.
Treatment Planning
Survey Considerations: Path of Insertion for Teeth and Implants
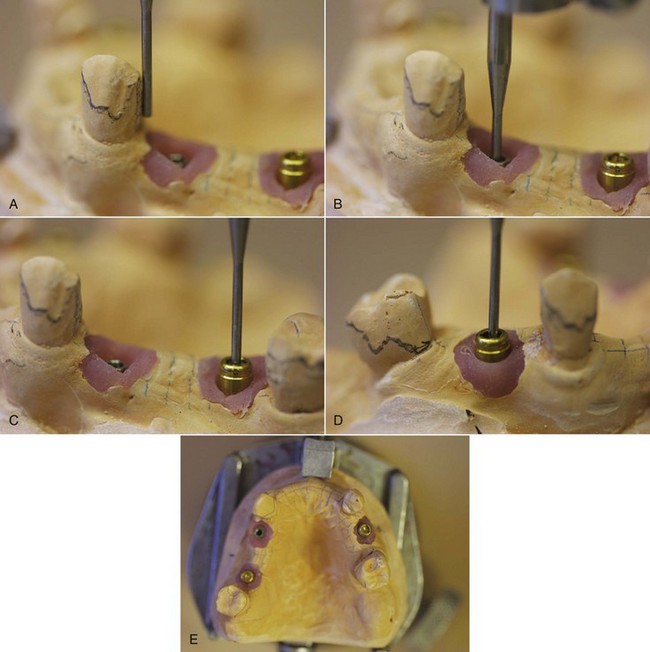
Engagement of implant abutments requires consideration of the prosthesis path of insertion (POI). An implant placed coincident with the POI allows greater prosthetic flexibility in abutment selection and a more favorable removable partial denture connection (Figure 25-2).
Location Influenced by Anatomic and Opposing Occlusal Factors
Implant use requires interocclusal space sufficient for prosthetic materials: denture base with framework minor connector, attachment housing, and denture tooth. Therefore the opposing occlusion should be evaluated preoperatively. This becomes even more critical when less residual ridge resorption occurs.
With excessive maxillary residual ridge resorption, the implant location may be more palatal/lingual, requiring consideration of the impact that such a location may have on palatal or lingual contours.
Clasp Assembly Requirements If an Implant Is Used Adjacent to Tooth
Engagement of an implant abutment to provide horizontal and vertical resistance supplements the resistance derived from tooth engagement. Consequently, less tooth coverage may be necessary for regions of the arch that have an implant.
If implant use is directed primarily to retention, tooth engagement for maximum resistance remains necessary to improve stability. If this is not achieved, deterioration in retention may be more rapid because of excessive forces directed to the retentive element, which could result in more rapid material deformation.
Clinical Examples
Figures 25-3 to 25-6 present clinical examples.

Figure 25-3 Significant residual ridge resorption with a strategically missing tooth #22. The implant provided sufficient support to improve functional comfort and occlusal function.

Figure 25-4 A long span modification space across the mandibular midline. The implant provided support and retention improved function and comfort while reducing functional stress on the mandibular incisors.
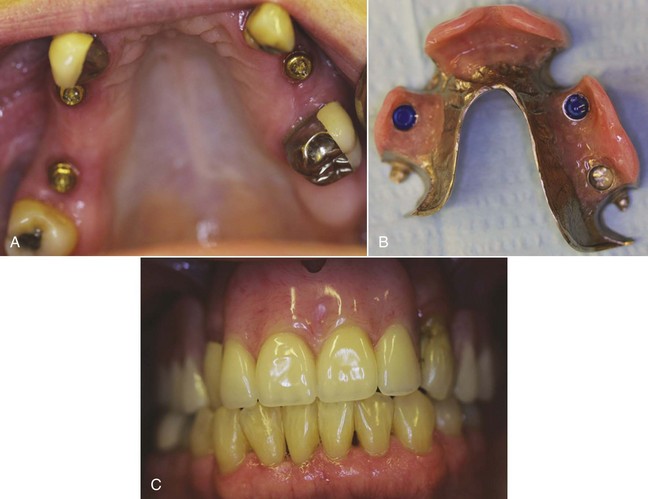
Figure 25-5 Support provided by the cingulum and mesial-occlusal rests of the teeth, and by the implant at site #3. Implants at sites #5 and #12 provide retention. Guide-plane surfaces augment implants for sufficient retention without clasps.

Figure 25-6 An implant-assisted Class III removable partial denture with minimum interocclusal space in an elderly patient desiring no prosthesis clasps. Denture teeth were shaped and positioned for optimum esthetics, allowing creation of occlusal contours by acrylic-resin, attaching the teeth to the frame and attachment housings.
Summary
Removable partial dentures are unique compared with prostheses supported by natural teeth. Their uniqueness largely relates to their potentially significant negative impact on oral sensory input during function, as well as on the prosthetic bulk required. Because of this, RPDs may present a challenge to accommodation, of which patients should be made aware during the treatment planning stage.
Patient sensory perception and neuromuscular variability may influence prosthesis selection. The sensory deficit associated with tooth loss can be complicated by unstable prostheses; for challenging RPDs, the use of implants can significantly contribute to stability.
The authors would like to acknowledge Dr. Tom Salinas for his helpful input during the writing of this chapter.