Feeding Intervention
1 Describe the acquisition of feeding, eating, and swallowing skills as developmental milestones.
2 Describe the anatomic landmarks and four phases of swallowing or deglutition.
3 Outline the cranial nerves involved in feeding and swallowing.
4 Explain the components of a feeding, eating, and swallowing evaluation.
5 Assess feeding difficulties in children within the larger context of the family’s cultural, social, and behavioral routines around food and mealtimes.
6 Classify common abnormalities and disorders related to the phases of swallowing.
7 Identify factors that may warrant further evaluation, including a videofluoroscopic swallow study.
8 Describe additional diagnostic and medical testing that may be used in a comprehensive evaluation.
9 Understand the developmental and psychosocial implications for a child whose nutritional intake is altered.
10 Identify medical, developmental, behavioral, and social issues that contribute to feeding, eating, and swallowing problems.
11 Explain the team approach to evaluating and treating the child from a biopsychosocial perspective.
12 Describe intervention strategies for feeding, eating, and swallowing deficits.
FEEDING: DEFINITION AND OVERVIEW
The process of feeding, eating, and swallowing is critical for health and wellness and plays an integral part in the child’s social, emotional, and cultural maturation. At the most basic level, the process of taking in adequate nutrition is essential for normal growth and development.
Throughout childhood, from infancy and all the way through adolescence, dietary requirements are constantly changing. At the same time, a child’s development gradually moves from complete dependence toward independent self-feeding. This dynamic process depends on the acquisition of both complex oral motor and fine motor skills. Indeed, mealtimes allow a child to explore new tastes and textures, while at the same time encouraging the development of motor skills through finger feeding and the use of utensils. Equally important, the feeding process is marked by social contact with other children, parents, and family and is thus essential for development of social interaction skills in the child. Children learn to communicate needs and desires through verbal and nonverbal cues. Feeding is one of the earliest instances in a child’s life where he or she learns to signal hunger, satiety, and thirst among other needs and desires. Finally, because this complex process is shaped by cultural and social norms, it often lays the foundation for the acquisition of certain customs and rules of sociocultural behavior.
Feeding—sometimes called self-feeding—is defined as the process of setting up, arranging, and bringing food from the plate or cup to the mouth. Eating is the ability to keep and manipulate food or fluid in the mouth and swallow it. Swallowing is a complex act in which food, fluid, medication, or saliva is moved from the mouth through the pharynx and the esophagus, and into the stomach.4
Children develop problems with feeding, eating, and swallowing as a result of medical, oral, sensorimotor, and behavioral factors, either alone or in combination.55 Medical conditions include prematurity, neuromuscular abnormalities, structural anomalies, gastroesophageal diseases, food allergies, and tracheostomy. Children with developmental disabilities may fail to meet basic nutritional needs because of delayed or deficit oral motor and self-feeding skills. Oral motor dysfunction causing poor nutrition is strongly associated with poor growth and adverse health outcomes.27,63 Clinical findings may include food refusal/selectivity, vomiting, swallowing difficulty, prolonged mealtimes, poor weight gain, and failure to thrive.
Behavioral problems are very common in children with feeding disorders. Food refusal and/or food selectivity can often signal negative interaction between children and their caregivers. However, they may be, and often are, secondary to underlying medical causes such as reflux or food allergy. In fact, both medical and behavioral etiologic factors are often present, making definitive diagnosis difficult.
The Role of the Occupational Therapist
Of all the activities of daily living, none is more life-sustaining than eating. Occupational therapists and occupational therapy assistants have long played an integral role in providing essential services and comprehensive management to children who have problems with one or more aspects of the feeding process. A competent occupational therapist should therefore be familiar with the following:
• Basic anatomy and physiology
• Growth and developmental milestones
Some occupational therapists work in specialized facilities as part of a multidisciplinary team that often consists of pediatric specialists, including gastroenterologists, developmental pediatricians, allergists, otolaryngologists (also known as ENTs), nurse practitioners, nutritionists, speech–language pathologists, behavioral psychologists, and social workers, all of whom work in tandem to evaluate and manage complex cases. However, many therapists work in school settings or as solo practitioners and are often the first to detect a child’s difficulties with feeding. In either instance, the occupational therapist has a well-defined, unique role in the assessment and management of feeding, eating, and swallowing disorders.
THE MEALTIME: AN OVERVIEW
Mealtime is generally a family time that provides physical, cognitive, and emotional nourishment of all members. Meals arrange the day temporally, organizing it into periods and signaling that certain activities end and new ones begin. Mealtimes provide a routine and a structure and offer a time for relaxation, communication, and socialization. At mealtimes, parents and children communicate symbolically and emotionally while at the same time satisfying very basic needs.22 Many believe that to nourish a child is to nurture a child. Thus, mealtimes are cultural rituals and, as such, an integral part of a family’s life, a time for bonding and sharing.
Caregivers and children engage in both shared and individual roles during mealtimes. Usually, the child is expected to remain seated, to attend to the caregiver, to feed himself or herself, to communicate with others at the table, and, generally, to follow the table manners and routines. The caregiver is expected to provide food in quantities sufficient to satisfy hunger, to assist in feeding younger children, to communicate and interact with other family members, and to establish mealtime norms and routines.
A child’s mealtime participation changes as he or she goes through the different stages of growth and development, from infancy to adulthood. During infancy, the parents are responsible for feeding or assisting the child. During the preschool and school-age years, the parents’ role shifts toward oversight, communication, and discipline. Almost all parents try to create a pleasant and relaxing family atmosphere during meals. This could be challenging and not always easy to achieve if a child has a disability that affects eating performance. The child’s temperament, health, and disposition and the parent’s health and mood are all important factors contributing to mealtime social interactions.
Contextual Influences on Mealtime
Family composition determines who is present at mealtime. The child may be fed in an isolated setting alone with his mother or may sit with all family members around the dinner table. Large families may have chaotic or noisy mealtimes. Such an environment creates difficulties for a child with hypersensitivities or high sensory arousal. Caregivers may not notice that a child has poor intake when many are present at the dinner table. On the flipside, large families have extra hands to assist in a child’s feeding if needed. Sometimes, children who need a quieter environment or who need maximal assistance are fed separately before or after the other family members. Sometimes only one family member can feed the child successfully. When a child has only one feeder, the responsibility for feeding around the clock can, over time, become stressful and exhausting for the feeder.
In some cultures, children are fed by a caregiver throughout the preschool years, whereas in others, infants are encouraged to self-feed despite the ensuing mess. For example, Puerto Rican mothers may continue to feed their children well into their preschool years, whereas Anglo mothers encourage self-feeding much earlier. Puerto Rican mothers who feed their children as toddlers generally emphasize respectful relations and appropriate interpersonal relationships during the meal. In contrast, Anglo mothers who allow self-feeding at 12 months of age tend to emphasize the young child’s independence and autonomy.59 Cultural beliefs also determine the amount and type of food that parents believe their children should eat. For example, southern African American children are often given sweetened tea to supplement their diet, because parents believe that tea enhances the physical and cognitive abilities of a child.41 The tea, however, may replace other drinks (e.g., milk) that have more vitamins and nutrients.
A family’s socioeconomic status also has an impact on mealtime and feeding patterns. Families in poverty may be unable to provide sufficient food or may eat cheaper foods that tend to be high in carbohydrates and fat. A parent’s educational level, which is often related to socioeconomic status, can affect a child’s diet because an undereducated parent may lack knowledge of basic nutrition. Obesity and hunger coexist in high-poverty areas. Diets of low-income consumers may be high in sugars and fat because they are the cheapest source of nutrition.
According to the results of the annual survey of the U.S. Census Bureau, those at greatest risk of being hungry live in households that are headed by a single woman; that are Hispanic or Black; or with incomes below the poverty line. Overall, households with children have food insecurity at almost double the rate for households without children. According to survey undertaken by the U.S. Department of Agriculture in 2006, 35.5 million persons are food insecure, of which 12.6 million are children.24 Food insecurity refers to the lack of access to enough food to fully meet basic needs at all times because of a lack of financial resources.47 UNICEF defines undernutrition as being underweight for age, too short for age (stunted growth), dangerously thin for height (wasted), and deficient in vitamins and minerals.66
A single parent may be under greater stress and may not be able to provide structured mealtimes, causing the child to have chaotic mealtime patterns. In the absence of mealtime structure, the child may graze throughout the day whenever hungry, eating whatever is easily available. Adolescent parents may not have access to information on child development and feeding and may feed their young children inappropriate foods or foods with poor nutritional value.
Feeding and mealtime patterns vary from family to family, and factors beyond the ones described above may be at play. Interviewing parents about the degree of flexibility they allow a child who refuses to eat, Humphry and Thigpen-Beck found that older, better-educated parents were more likely to be flexible.36 Parents who placed emphasis on discipline and obedience were less likely to be flexible with a child’s refusal to eat. Clearly, social context can be helpful in understanding a family’s feeding strategy and how parents interpret and respond to a child’s mealtime behavior.37
Personal Influences on Mealtime
A caregiver’s personality traits and other individual factors can also shape mealtime and affect a child’s ability to feed. When the caregiver does not enjoy feeding a child or approaches it as a chore, the task can lose much of its meaning, changing the mealtime experience for both the adult and the child. For example, some caregivers are anxious about feeding and tend to be controlling when the child is a poor eater. The caregiver may have preconceived ideas about how much the child should eat and force food on the child or become disappointed with the child’s intake. A controlling parent may find that the child desires control of what he or she eats, and a battle of the wills may result.
Personal/individual factors that influence mealtime include the child’s health, eating skills, and communication/interaction skills. Children with feeding/eating problems can require extra time, special food preparation, adaptive equipment, and a structured protocol for the caregiver. This chapter discusses some health problems and delayed or deficient oral motor skills that can affect feeding. Occupational therapists are often called on to provide intervention in such circumstances.
DEVELOPMENTAL SEQUENCE OF MEALTIME PARTICIPATION
Progression of Mealtime Participation
In the first 6 months of life, parents feed their infant in their arms. Feeding is a time for bonding, characterized by close holding and warmth, eye contact, and nonverbal communication between the parents (or other primary caregivers) and the child. A typical interaction between child and parent may be the parent’s stroking and touching the infant, who responds by grasping the mother’s breast or hair or the father’s shirt or fingers. Although the parent determines what the infant eats, it is the infant who typically sets the pace, duration, and end of a meal. When this interaction is less than smooth, the parent may compensate by trying to exercise more control. Positive early mealtime experiences solidify the bond between parent and child and strengthen the relationship between them.
An infant becomes more independent between 7 and 24 months. For example, a 7-month-old infant can usually finger feed. By 18 months, the child is typically attempting to use a spoon and a cup. As independence grows, so do the chaos and messiness of mealtimes. Although the parent continues to select the foods for the child, the child can now choose whether to eat or refuse the food. During this time, the toddler gets a greater variety of foods. The child moves out of the parents’ arms and into a high chair or a booster seat. The toddler studies his or her foods and truly enjoys making a mess. Most toddlers explore the sensory qualities of foods, such as texture, with their hands and tongues. Parents encourage their child’s efforts at self-feeding and allow him or her to try different foods, while ensuring they limit those difficult to chew and/or digest. Eating, however, continues to be time for communication, by now both verbal and nonverbal. Parents begin to describe the child’s foods and thus provide a source for new vocabulary. In fact, words denoting food are often among the first words acquired by many toddlers.
Once the child is about 2 years old and is feeding relatively independently, he or she usually becomes a full participant in family mealtime. The child sits at the table, where she or he can observe and mimic the actions and behaviors of fellow meal participants. By preschool, children begin to eat some or all of the foods that other family members are eating. Family members become models for appropriate feeding behaviors and instruct the child in the basics of self-feeding. For most preschool children, mealtimes are enjoyable social times, marked by a sense of togetherness and an altogether positive, relaxing environment. Disability, however, can have a negative effect on mealtimes and hinder or slow the progression and accomplishment of these outcomes. Too much pressure on preschoolers to eat more, eat neatly, or eat certain foods may create anxiety about eating and may be harmful in the long run by making eating a less than enjoyable physical, sensory, and social activity.
Development of Oral Structures
Intact oral structures and cranial nerves are prerequisites for normal eating and drinking. Various aspects of oral motor development emerge as the child begins to control jaw, tongue, cheek, and lip movement. The anatomic structures of the mouth and throat change significantly during the first 12 months. The growth and development of the oral structures allow for increasingly mature feeding patterns. Table 15-1 lists the oral structures involved in feeding.
TABLE 15-1
Functions of Oral Structures in Feeding
| Structure | Parts | Function during Feeding |
| Oral cavity | Hard and soft palate, tongue, fat pads of cheeks, upper and lower jaws, and teeth | Contains the food during drinking and chewing and provides for initial mastication before swallowing |
| Pharynx | Base of tongue, buccinator, oropharynx, tendons, and hyoid bone | Funnels food into the esophagus and allows food and air to share space; the pharynx is a space common to both functions |
| Larynx | Epiglottis and false and true vocal folds | Valve to the trachea that closes during swallowing |
| Trachea | Tube below the larynx supported by cartilaginous rings | Allows air to flow into bronchi and lungs |
| Esophagus | Thin and muscular esophagus | Carries food from the pharynx, through the diaphragm, and into the stomach; it is collapsed at rest and distends as food passes through it |
Modified from Wolf, L. S., & Glass, R. P. (1992). Feeding and swallowing disorders in infancy: Assessment and management. Tucson, AZ: Therapy Skill Builders.
The newborn has a small oral cavity filled with fat pads inside the cheeks and the tongue. The small and tight oral cavity allows the child to grasp and easily compress the nipple during breast-feeding and to achieve automatic suction. The negative pressure caused by the sucking movements of the jaw extracts liquid from the nipple.44 Thus, a full-term healthy newborn can suck easily and successfully from a breast or bottle nipple.
The structures in an infant’s throat are also in close proximity to one another. The epiglottis and soft palate are in direct approximation. As a result, the liquid from the nipple safely passes from the base of the tongue to the esophagus. During swallowing, the larynx elevates and the epiglottis falls over it to protect the trachea. Therefore, aspiration is less likely before 4 months of age, and the infant can safely feed in a reclined position.
As the infant grows, the neck elongates, and the configuration of the oral and throat structures changes. The oral cavity becomes larger and more open, the tongue becomes thinner and more muscular, and the cheeks lose much of their fatty padding. With the increase in oral cavity space, the tongue, lips, and cheeks provide greater control of liquid and food within the mouth. New sucking patterns develop enabling the infant to handle liquid without the structural advantages of early infancy. These include up-and-down movements of the tongue to extract liquid from the nipple. The increasing oral space also provides room to advance food texture and to move the tongue in the rotary pattern required during chewing.69
As the infant approaches 12 months of age, the hyoid, epiglottis, and larynx descend, creating space between these structures and the base of the tongue. The hyoid and larynx become more mobile during swallowing, elevating with each swallow. The greater complexity of the suck-swallow-breathe sequence leads to greater coordination among these structures. The elongated pharynx increases the risk of aspiration during feeding in reclined position as the pull of gravity accelerates the flow of liquid into the entrance of the esophagus. Figure 15-1 shows the structures of the mouth and pharynx of the infant.
Phases of Swallowing
There are four defined phases of swallowing. The oral preparatory phase is under voluntary control and the area of oral motor/feeding intervention. Oral manipulation using the jaw, lips, tongue, teeth, cheeks, and palate results in the formation of a bolus. The amount of time varies depending on the texture of food/liquid. The trigeminal (V), facial, (VII), glossopharyngeal (IX), and hypoglossal (XII) cranial nerves are listed in Box 15-1.
The second phase is the oral phase, also under voluntary control. This phase begins when the tongue elevates against the alveolar ridge moving the bolus posteriorly and ends with the onset of the pharyngeal swallow lasting for 1 to 3 seconds. The third phase is the pharyngeal phase, also lasting 1 to 3 seconds, which starts with the trigger of the swallow at the anterior faucial arches. The hyoid and larynx move upward and anteriorly, and the epiglottis retroflexes to protect the opening of the airway. It ends with the opening/relaxation of the cricopharyngeal sphincter. The final phase is the esophageal, which, along with the pharyngeal phase, is not under voluntary control. It starts with the contraction of the cricopharyngeus muscle and ends with relaxation of the lower esophageal sphincter, allowing food to enter the stomach. The duration is 8 to 10 seconds.
ORAL MOTOR DEVELOPMENT ASSOCIATED WITH EATING SKILLS
Sucking, drinking, biting, and chewing are closely linked to the child’s overall motor development. Oral patterns evolve along with the child’s changing nutritional needs, growing desire for self-feeding, and increasingly greater ability to communicate.7 Table 15-2 summarizes the sequence of eating skills development.
TABLE 15-2
Developmental Sequence of Eating Skills
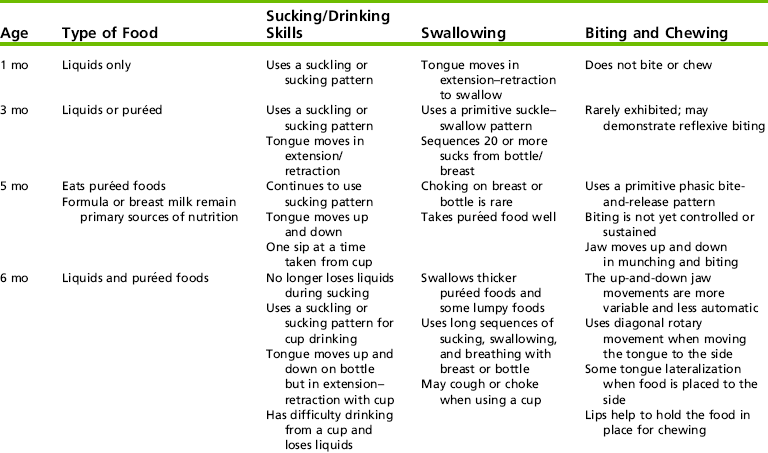
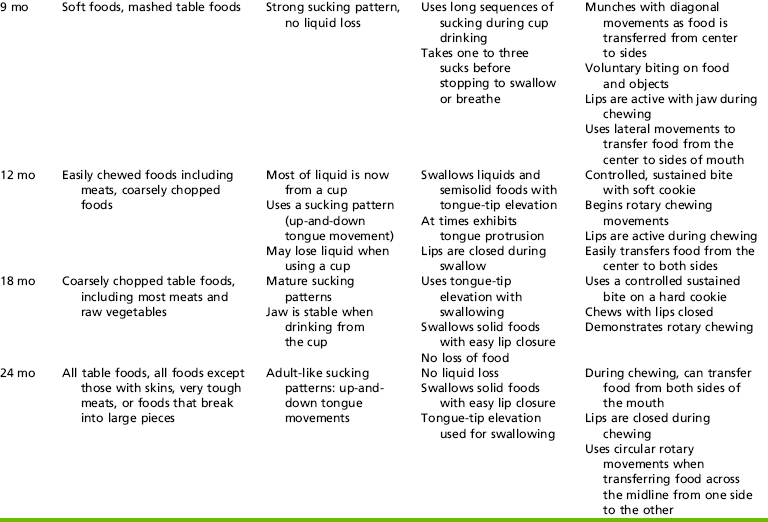
Ages are approximate and may vary among infants.
Adapted from Glass, R., & Wolf, L. (1998). Feeding and oral motor skills. In J. Case-Smith (Ed.), Pediatric occupational therapy and early intervention. Boston: Butterworth Heinemann; Morris, S. E., & Klein, M. (2000). Prefeeding skills (2nd ed.). San Antonio, TX: Therapy Skill Builders.
Coordination of Sucking, Swallowing, and Breathing
The sucking reflex is present in the fetus and is the predominant method of feeding during the first 8 to 10 months of life. Sucking can be either nonnutritive or nutritive, and each one is different. Nonnutritive sucking, the goal of which is not to feed but rather to calm, occurs when a child is sucking on a pacifier. It is marked by rapid, rhythmic movements, occurring at a speed of about two sucks per second. By contrast, the nutritive pattern occurs when a child is sucking on a source of nutrition, such a bottle nipple. It is rhythmic, but its rhythm is marked by alternating bursts with pauses, which allows the infant to breathe and rest between sucking bursts.
Premature infants of 33 weeks’ gestational age or less are typically fed by nonoral methods such as an intravenous line or a nasogastric tube. The reason for this is that infants younger than 33 weeks, although capable of rhythmic nonnutritive sucking, have insufficient strength and endurance for nipple feeding. A 35-week-old healthy premature baby typically has sufficiently strong jaw and tongue movements to be fed orally, at least part of the time.
Two important factors that determine the ability to feed are sucking rhythm and type of suction (i.e., negative pressure for expression of liquid) that the infant achieves and sustains over time.21 Both compression and suction are required for the expression of liquid.69
To achieve suction and compression, the infant seals his or her lips around the nipple and simultaneously moves the tongue back and forth and up and down. By 36 weeks of gestational age, most premature infants can take all food by mouth and are able to suck nearly as well as a full-term infant.
The full-term infant (37 to 42 weeks’ gestation) has strong oral reflexes that enable him or her to take in liquid nutrition without difficulty. Exposed to tactile stimulation near the mouth (such as gentle touching of the lips), the hungry infant reacts by turning the head (rooting reflex), which permits him or her to latch onto any potential source of nutrition. The infant also exhibits gag and cough reflexes to prevent liquid from entering the airway.
The amount of liquid consumed during a meal is determined by three factors: rate or speed of sucking, force of suction or compression, and length of feeding time. Thus, infants who suck faster and pull more forcefully on the nipple and take in more fluid may finish eating in less time than those who suck more slowly or weakly. The sucking pattern of the full-term infant is rhythmic, sustained, and efficient. Sucking speed and force begin to decrease with satiety. Each infant has a unique sucking pattern that may vary from feeding to feeding depending on factors such as fatigue and hunger. Most infants complete an oral feeding in 20 to 25 minutes.
An infant’s first sucking pattern is called suckling.44 During suckling, the tongue moves back and forth, and the jaw opens and closes, following the movement of the tongue.70 Typically, the tongue extends to, but not beyond, the border of the lips. Suckling is the predominant sucking pattern during the first 4 months of life. At 1 month of age, a hungry infant usually performs one suck per swallow. However, as the infant becomes satiated, he or she decreases the force of suction, taking in less and less liquid with each sucking motion. The rate slows down to about two to three sucks per swallow. Slight liquid loss and air intake may occur with suckling and are primarily observed in the second and third months, after the infant’s physiological flexion has disappeared but before the infant has acquired mature oral motor control.
At 4 months of age, the tongue begins to move up and down, the hallmark movement of true sucking. The wide jaw excursions of the young infant are reduced, less liquid is lost, and nipple suction force increases. By 4 months of age, the infant is capable of taking in 20 or more sucks from the breast or bottle before pausing. Swallowing occurs intermittently (after four to five sucks) and without pausing. Breathing slows during sucking and occurs within and between sucking sequences. Occasionally, the infant may cough or choke when he or she momentarily loses coordination of sucking, swallowing, and breathing.
The 6-month-old infant demonstrates strong up-and-down tongue movement with minimal jaw excursion during sucking. Jaw stability increases and allows for better control of tongue movement. The lip seal is tighter, and liquid loss no longer occurs. In fact, 6 months is the age when many caregivers in the United States introduce the cup, usually a sipper cup with a spout. When first presented with a cup, the infant will try to use a suckling pattern so the jaw continues to move up and down, and the tongue moves back and forth in the mouth. The wide jaw excursions can result in some liquid loss. An infant’s early attempts at cup feeding may be accompanied by some coughing.
At 9 months of age, the infant continues to feed from the bottle nipple using strong sucking patterns. When drinking from a cup, the jaw is not consistently stable on the rim of the cup, which makes drinking from a cup somewhat messy at that age. The infant stops to swallow or breathe after one to three sucks from the cup.
At 12 months of age, many infants make a full transition from bottle to cup for drinking during mealtime but may continue to bottle-feed at other times. Jaw stability, and consequently cup support, continues to be somewhat of a challenge. The infant may try to overcompensate by protruding his or her tongue slightly beneath the cup for additional support. At this age, elevation of the tongue tip during swallowing occurs for the first time. He or she bites on the rim of the cup to make the jaw more stable and obtain greater control of the cup. By 12 months of age, sequences of three suck-swallows occur during cup drinking.44
By 15 to 18 months of age, the infant has excellent coordination of sucking, swallowing, and breathing. When drinking from a cup, the infant’s swallowing follows sucking without pauses. Coughing or choking rarely occurs.
At 24 months of age, the child can efficiently drink from a cup. He or she uses both up-and-down tongue movements and tongue tip elevation. Internal jaw stabilization develops, and the jaw appears still. The jaw becomes stable enough to support the rim of the cup, and biting on it is no longer necessary. The child swallows with easy lip closure and does not lose liquids from the cup. Lengthy suck-swallow sequences occur.
As the infant gains more control of jaw, tongue, and lip movement, he or she also learns to coordinate and arrange oral movements into rhythmic patterns of sucking, swallowing, and breathing.16 The intricate synchronization among the oral structures is perhaps more important to the feeding process than the development of control of any one oral structure by itself.
Biting and Chewing
An infant’s first biting or chewing movements are reflexive. At 4 to 5 months of age, the infant uses a rhythmic, stereotypic, phasic bite-and-release pattern on almost any substance placed in the mouth (e.g., a soft cookie, a cracker, or a toy). The jaw moves up and down rather than sideways and diagonally. When the phasic bite-and-release pattern occurs rhythmically and repeatedly, it is called munching. A munching pattern is characterized by vertical jaw movement and a back-and-forth tongue movement. The ability to move the tongue and jaw sideways is not yet developed at this age. The munching pattern allows the infant to successfully eat pureed or soft foods that dissolve quickly.65
By 7 to 8 months of age, the infant begins to exhibit variations in this up-and-down munching pattern. He or she begins to use some diagonal jaw movement when the texture of the food requires the jaw to move both horizontally and vertically. The infant continues to use the phasic bite-and-release pattern when he or she bites on a cookie; thus, the jaw closes abruptly on the cookie and the infant sucks on it. The jaw holds the cookie, but the infant cannot yet successfully bite through it. A piece is broken off while the jaw remains closed on the cookie. When the infant receives food on a spoon, the upper lip actively cleans it from the spoon. The lips become more active during sucking and maintaining the food within the mouth.
By 9 months of age, the infant handles pureed and soft foods well. He or she continues to use a munching pattern, but the up-and-down jaw movements are now interspersed with diagonal movements. The infant transfers the food from the center of the mouth to the side using lateral tongue movements. The same lateral movements keep the food on the side during munching, making that process effective in mastication of soft or mashed table food. The lips are active during chewing, so they make contact as the jaw moves up and down.
Rotary chewing movements develop at approximately 12 months of age and are made possible by the increasing stability, control, and mobility of the jaw, evidenced by the child’s sustained, well-graded bite on soft cookies. The tongue is actively involved in chewing by moving food from the center of the mouth to the sides, licking food from the lips, and demonstrating tip elevation on occasion. The infant is able to retrieve food on the lower lip by drawing it inward into the mouth.
At 18 months of age, the infant exhibits well-coordinated rotary chewing. He or she is able to chew soft meat and various table foods. The child can control and sustain bites and can bite off a piece of a hard cookie or a pretzel. The tongue becomes increasingly mobile and efficiently moves food within the mouth.
At 24 months of age, the child can eat most meats and raw vegetables.65 The child can grade and sustain the bite and can easily bite on hard foods. The circular jaw movements that characterize mature chewing are present at this age. The tongue transfers food from one side of the mouth to the other using a rolling movement and moves skillfully to clear the lips and gums. Lip closure during chewing prevents loss of food.
Self-Feeding
The caregiver can introduce new challenges to the feeding process even before the child shows full mastery in a certain area of performance. Table 15-3 outlines the developmental sequence of self-feeding. The ages are approximate and overlapping.
Children are often eager to feed themselves. As early as 6 months of age, the infant may bring his or her hands up to the bottle and try to hold it. The caregiver should not prop the bottle because the infant lacks the motor skills necessary to remove the bottle if choking occurs. Also, the infant typically lacks the cognitive understanding that a dropped bottle can be retrieved and put back into the mouth. Infants older than 8 months of age actively hold the bottle, but caregivers should monitor their self-feeding to ensure adequate intake, because infants are easily distracted once they satisfy their initial hunger.
Typically, finger feeding develops quickly and naturally by about 8 months of age when the infant receives soft cookies or crackers to hold. At this age, infants exhibit a radial digital grasp, which positions the cookie for entry into the mouth. From 9 to 13 months of age, the infant develops several important abilities, including better control of sitting posture, improved sitting balance, refined pincer grasp with controlled release, and refined isolated forearm and wrist movements, all of which greatly improve self-feeding skills. By 12 months of age, finger feeding is generally a preferred and enjoyed activity and occurs simultaneously with certain psychosocial changes that signal the infant’s increased desire for independence, often manifested by refusal to be fed. The selection of finger foods should match the child’s oral–motor skills (e.g., cooked vegetables are easily grasped and mashed with the tongue and gums).
Infants younger than 1 year of age will grasp, wave, and bang spoons during feeding. Around 12 months of age, the infant demonstrates an understanding of the spoon’s function by poking at a bowl of food with a spoon and bringing it to the mouth. Because visual monitoring of the spoon’s position is poor and the infant has difficulty sequencing scooping movements or adjusting the forearm and wrist, the food often slips from the spoon before it reaches the mouth. Attending to the whole activity and recognizing when the spoon is empty, which requires sufficient cognitive changes to use feedback, is necessary before the infant starts to control the wrist and forearm sufficiently for spoon-feeding. Infants will frequently insist on self-feeding even though independence means less success at satisfying hunger.
Full spoon-feeding proficiency emerges between 15 and 18 months of age when the infant begins to bring a spoon with sticky food, such as yogurt, into the mouth with minimal spillage. The infant holds the spoon in a pronated gross grasp and uses primarily shoulder movement to bring it to the mouth. By 24 months of age, the child spoon-feeds without spillage, balancing the spoon to hold a variety of foods. He or she holds the spoon in the radial fingers with the forearm supinated and is able to obtain the food and efficiently place the spoon into the mouth. Between 30 and 36 months of age, the child may begin to prefer a fork for stabbing foods and may learn to eat foods that are more difficult to balance on a spoon (e.g., cold cereal and rice with gravy).
Drinking
Infants as young as 6 months may demonstrate interest in drinking from a cup, but cup-drinking skills do not emerge fully until 12 months of age. At that time, the infant is better able to correctly position the cup to the mouth and to tip it at a degree that makes spillage less likely. There are several types of cups that can facilitate an infant’s acquisition of cup-drinking skills. The first type used by the infant is a cup with a lid and a spout. It may have handles or it may be a small cup that the infant can hold in one hand. Placing only a little liquid in the cup initially decreases spillage and allows the child to control the flow. At 24 months of age, the child may begin to use a small 4- to 6-ounce cup without a lid, but spillage is inevitable at this juncture.
The ability to drink from a straw emerges at about 2 years of age, but it may become a skill even earlier if the caregiver exposes the child to straw drinking at a younger age. Use of a straw requires good lip seal and strong suction to bring the liquid into the mouth (Figure 15-2). In addition to the oral motor skills required to draw the liquid into the mouth, cognitive skills are needed to figure out how to use the straw. The infant often bites or blows on the straw before learning how to suck through it. This framework of typical development should help the therapist identify problems and establish realistic intervention goals and expected outcomes.16
EVALUATION
The process of analyzing and identifying problematic areas should always start by asking parents and caregivers questions about feeding, eating, and swallowing. In addition, the therapist should elicit information about the child’s medical history and evaluate the child for clinical signs of underlying disorders (Box 15-2).
Any evaluation for possible feeding problems should start by assessing mealtime participation, as well as by gathering information and impressions of the feeding situation from the caregivers. The child’s developmental status and health history are also important in identifying feeding problems, as well as for making decisions about further evaluation and subsequent intervention. Usually, such information can be easily obtained from the child’s medical records, from written and oral interviews with the parents and caregivers, and by mere observation. Such data often give the occupational therapy practitioner a general picture and may point to the feeding problem and, sometimes, to its underlying cause. The therapist obtains information about current feeding practices by asking the parents to describe feeding over the course of a typical day. This open-ended inquiry, as opposed to multiple-choice questions, allows the parents to bring forward their concerns. After these initial impressions, the therapist can ask more targeted questions, focusing on certain areas of interest, and obtain even more comprehensive information.
A discussion of the feeding problem from the parents’ perspective is critical because it helps identify their primary concerns. For example, are the parents most concerned about weight gain or is it the length of time required for feeding that poses a problem Does the child seem to lose most of the food consumed during feeding (e.g., through vomiting or reflux) Is the child’s behavior during feeding causing distress for the entire family during mealtime Although the parents’ expressed concerns become the focus of the subsequent intervention, the therapist should always consider other concerns expressed by professionals (such as doctors or other health care personnel) in developing a feeding plan, especially when these concerns differ from those expressed by the parents.
The parents also provide the team with information about the child’s developmental and feeding histories. Obtaining this information helps the therapist identify the root of the feeding problem (e.g., if longstanding sensory or behavioral issues have affected feeding). Inquiring about the feeding history helps the therapist get a sense of any possible frustration and the parents’ ability to cope with the child’s feeding issues. The techniques used by parents may be helpful in identifying appropriate intervention strategies. Parents whose children have received therapy services in the past probably have important information to share regarding interventions that worked and those that did not. The interview can also help the therapist determine which parent or caregiver would do best in implementing recommendations, initiating a referral to an oral motor or feeding program, and discussing information about the child’s progress in developing eating/feeding skills.
Recorded developmental histories are important because they supplement the parents’ report and offer additional insights for the therapist. The written reports of other occupational and physical therapists, speech-language pathologists, early childhood specialists, and teachers provide fundamental knowledge about the child. For example, a child with a sustained hospitalization may not have had enough opportunities to progress, or an early history of restricted upper extremity movement may lead to restricted oral play, influencing sensory systems and, by extension, the ability to eat. Understanding the child’s developmental course and rate of change in other occupational performance areas such as object play and social interactions is important for the therapist to set realistic goals, prioritize objectives, and choose appropriate intervention strategies.
Although these issues are discussed separately, feeding problems are seldom attributable to a single cause and usually are the result of delays or impairments in multiple areas. For example, children with severe sensory problems generally have oral motor skill delays, and children with swallowing disorders often have motor deficits.
Neuromotor Evaluation
The occupational therapist then completes a “hands-on” evaluation of generalized muscle tone, neuromuscular status, and general developmental level. Observation of movement initiation and transition patterns allows the occupational therapist to observe whether abnormal tone could be affecting feeding, eating, and/or swallowing. Muscle tone abnormalities interfere with the ability to maintain upright posture and head/neck alignment. They may also lead to difficulty grading or sustaining oral motor patterns, uncoordinated breathing, drooling, decreased oral exploration, and limited self-feeding. The use of adapted seating systems during the evaluation helps determine the optimal position for feeding. For many children, the upright position is the most effective and provides airway protection. For others some degree of recline may allow for better head control and retention of food.
Examination of Oral Structures and Oral Motor Patterns
The oral sensorimotor examination is the third part of the evaluation. The initial step is observation of symmetry, size, and range of motion of oral structures, including the jaw and larynx proceeding intraorally to the gums, dentition, hard and soft palate, and tongue. A thorough examination of the tongue is critical because the tongue serves many functions in feeding/eating and swallowing. At rest, the tongue should have a well-defined shape, with a nicely rounded tip and a central groove, and be seated inside on the bottom of the oral cavity. Increased oral tone may cause the tongue to be retracted, humped, or have tip elevation and may often be the primary cause of feeding difficulties. Children with food refusal and normal oral tone sometimes use these tongue positions as a defensive posture. In contrast, hypotonia may cause the tongue to be flat, lack a midline groove, and extend beyond the lips.
Eating and Feeding Performance
The final aspect of the comprehensive clinical assessment is the observation of the actual feeding/eating and swallowing process to assess level of performance and to analyze how motor, sensory, cognitive, and communication skills contribute to performance. It is important that the observation mimic those conditions as closely as possible under which the child normally eats and uses foods the child would typically eat. Parents or caregivers can either bring a meal from home or help the therapist select the menu. The therapist places the child in his or her typical feeding position, provides familiar utensils, and asks a parent or caregiver to feed the child the initial portion of the meal.
Observing the parent–child interaction gives the therapist clues about factors that may affect the child’s food intake. During this time, the therapist reflects on the potential meaning of the occupation of eating to the child and his or her interest in participating. Observing the parent–child interaction also provides insights into the everyday context of feeding to help formulate recommendations. The following are signs to watch for:
• Does the parent talk to the child
• Does the child send clear cues regarding readiness to eat, satiation, or preferences to foods
The therapist also needs to use a variety of textures while observing the child eating if this is age appropriate. When possible, the therapist precedes a trial of different textures with relaxed play with the child so that he or she becomes comfortable. Nonintrusive play can also help to establish rapport.
To observe the child’s sensory responses, the therapist should use various textures and attempt placement of food in different parts of the mouth. When the child exhibits aversive responses to food inside the mouth, the parent is asked if the responses are typical or exaggerated because of discomfort with an unfamiliar feeder.
Videofluoroscopic Swallow Study (VFSS)
To further analyze the child’s feeding and eating issues, the therapist may need to return to the child’s medical record for additional information. Does the child have a medical condition that leads to feeding problems or poor weight gain Instances of pneumonia and frequent and prolonged upper respiratory infection may indicate a swallowing problem. To confirm or rule out swallowing problems, a videofluoroscopic swallow study may be needed.
The modified barium swallow study is the radiographic procedure of choice for assessing the oral, pharyngeal, and upper esophageal anatomy, and the physiology of the stages of swallowing. It is particularly useful in identifying aspiration or the risk of aspiration and in tailoring treatment for infants and children with feeding disorders. The test can also be helpful in detecting problems related to head and neck positioning, bolus characteristics, rate and sequence of presentation, and food/liquid consistencies. The results of the test can be helpful in identifying compensatory techniques to minimize the risk of aspiration and maximize eating efficiency.9 The therapist selects the types of food textures based on the child’s current diet and feeding goals and mixes them with liquid or paste barium.58 It is important to remember that the VFSS only shows a brief sample of swallowing, and positioning, amount, and order of food/liquid bolus presentation is up to the occupational therapist or speech pathologist conducting the study.8
VFSS is used to analyze the swallow mechanism and is particularly important for children who aspirate or are at high risk for aspiration because of severe motor problems.29 Factors that suggest swallowing problems include gagging, coughing, choking, nasopharyngeal reflux, increased congestion, wet vocal quality, and the occurrence of respiratory infections and/or pneumonia.46 Aspiration may be silent, so a thorough history and feeding observation are critical. The therapist should distinguish aspiration from penetration. Penetration describes the flow of food or liquid underneath the epiglottis into the laryngeal vestibule but not into the airway. It does not pass through the vocal folds. Aspiration refers to food entering the airway before, during, or after a swallow. Because the recording shows the food traveling through the mouth and pharynx, the therapist receives real-time, detailed information about the swallowing problem.60,69 The results of the VFSS indicate the safety and appropriateness of oral feeding and guide the therapist’s recommendations.71 These may include modified positions and textures for the parents to use during feeding that appear to result in optimal swallowing patterns without aspiration. Although the VFSS gives the therapist important information and insight about the swallowing problem, it may not always be representative of the child’s typical feeding in a more natural environment.
Medical Conditions Affecting Eating
Feeding problems may be associated with specific medical diagnoses. Children with cerebral palsy may be either hypotonic or hypertonic. Facial hypotonia often results in an open-mouth resting posture, drooling, and decreased sensory awareness. Children with hypertonia often present with a strong tongue thrust or bite reflex.54 Congenital oral–facial anomalies such as cleft lip and palate and micrognathia may be associated with Pierre-Robin malformation sequence or may be part of Stickler syndrome.69 Children with Down syndrome often have a small oral cavity, hypotonia, and macroglossia, all of which can contribute to feeding difficulties. Other structural abnormalities that could impact feeding are tracheoesophageal fistula and esophageal atresia, as well as gastrointestinal problems such as gastroesophageal reflux and dysmotility.
Complicated pulmonary and feeding issues are well documented in the premature infant.34,67 The Neonatal Oral-Motor Assessment Scale (NOMAS)50 is the visual observation method most commonly used to assess the nonnutritive sucking and the nutritive sucking skills of infants up to approximately 8 weeks postterm.20
Behavioral difficulties often manifest as food refusal or food selectivity but are often associated with some medical problem such as pain from reflux or an allergic reaction and are often maintained over time by behavioral factors.15 Food refusal can also be associated with poor dentition or sensitive gums. Caregivers sometimes neglect oral hygiene in children with oral motor dysfunction, oral hypersensitivity, or in those demonstrating food refusal.
Gastroesophageal reflux (GER) is an increasingly common problem in the general population and may be an underlying cause of swallowing dysfunction in children. GER occurs when the lower esophageal sphincter does not close properly or opens spontaneously, and stomach contents move upward (acid reflux) into the esophagus. During the first year of life, mild GER is common, resulting in occasional spitting up or vomiting, but it is transient and is generally not considered a medical problem. True gastroesophageal reflux disease (GERD) results from more prolonged reflux that causes clinical signs and symptoms including regurgitation, nausea, chest pain, coughing, and other respiratory problems. During feeding, infants or young children with GERD may be unusually irritable, arch their backs, and refuse food completely, which leads to poor weight gain.45
The presence and extent of GERD can be confirmed by an esophageal pH probe. The probe is inserted into the esophagus through the nose to monitor abnormal acid levels, usually over a 24-hour period. Radiology studies including barium swallow or upper GI series can detect anatomic abnormalities such as hiatal hernia and assess peristalsis in the esophagus. If the GERD causes aspiration, the x-ray film may show lung changes. An upper endoscopy with esophageal biopsy (also referred to as an esophagogastroduodenoscopy [EGD]) can diagnose inflammatory conditions such as reflux esophagitis or eosinophilic esophagitis, commonly associated with allergies. Fiberoptic endoscopic evaluation of swallowing with sensory testing (FEESST) is a relatively new tool that allows direct visualization of the larynx and pharynx to observe penetration, aspiration, spillage, and residual material.45 Gastroesophageal scintigraphy or “milk scan” assesses the severity of GERD using a noninvasive nuclear medicine scanning technique that involves the ingestion and tracking of radiolabeled milk as it moves through the esophagus and stomach.53
Contextual Factors
Evaluation of the context (environment) in which feeding occurs is essential to the development of intervention plans. In some cases, feeding problems are based primarily on contextual issues, including physical, social, temporal, and cultural. Box 15-3 lists some of the contextual factors that should be considered in assessing feeding.
Understanding the contextual factors that influence mealtimes and feeding performance helps determine the basis for the problem and possible solutions. Certain contextual factors can be changed easily (e.g., a child can be positioned in a chair that is more upright and has straps that maintain good alignment); however, cultural beliefs and family routines are less amenable to change and should be accommodated in the intervention plan. Contextual factors may determine the success of the intervention (i.e., which recommended strategies the family will implement). For example, if the caregivers do not value or prioritize the child’s independence in feeding, they are unlikely to follow through with suggestions to increase feeding independence.
The assessment findings are discussed and interpreted by team members, including the family, to develop a cohesive intervention plan. Any intervention for feeding problems should be holistic, meaning that it considers the whole child, involves the family, and involves collaboration with professionals from other disciplines as needed.60,64
INTERVENTION: GLOBAL CONSIDERATIONS
Problems with feeding, eating, and swallowing are caused by multiple underlying factors. If feeding problems persist as the child grows older, new problems or skill impairments may appear that further complicate the intervention needs. For example, children with dysphagia who require nonoral feeding for an extended period of time may experience subsequent developmental delays in self-feeding skills because of lack of experience. Occupational therapists can provide direct intervention for children with feeding, eating, and swallowing disorders to improve functional participation in mealtimes. Throughout the intervention process, therapists must consider medical and nutritional problems that often coexist with the child’s feeding disorder and collaborate with physicians and nutritionists to create an optimal intervention plan.
Feeding activities occur multiple times throughout the day within a variety of natural environments, and occupational therapists must work closely with families and other caregivers to ensure carryover within daily routines. Children with oral feeding difficulties often require one-on-one attention or increased caregiver time and effort throughout each day. Mealtimes may be quite stressful for parents, especially when the child’s oral feeding difficulties create ongoing problems with nutrition and growth. Whenever possible, typical family mealtime routines should be preserved within the intervention program. Therapists should consider the caregivers’ time investment and provide realistic recommendations that do not significantly increase the burden of care within the family system. Parents of children with feeding, eating, and swallowing disorders may benefit from peer support groups, which have been shown to strengthen caregivers’ abilities to cope with stressful problems on a day-to-day basis.17
Occupational therapists use a holistic approach when developing a treatment plan for children with feeding, eating, and swallowing disorders. Consideration is given to many different overlapping areas described within the Occupational Therapy Practice Framework, including child factors, performance skills, activity demands, contexts, and family patterns.5 A comprehensive intervention plan may include environmental adaptations, positioning recommendations, sensory development activities, behavioral strategies, neuromuscular handling techniques, food texture modifications, adaptive equipment, or suggestions to improve independence in self-feeding.
Safety and Health
Basic safety guidelines should be followed when providing occupational therapy treatment. Children who demonstrate clinical signs of aspiration may require additional assessment with videofluoroscopy to determine appropriate feeding goals. Therapists must also consider the child’s nutritional status and prioritize treatment goals to maximize a child’s ability to meet basic nutritional needs. Some interventions may require implementation outside of regular meal sessions, so as not to disrupt the child’s ability to meet oral intake requirements.
The Occupational Safety and Health Administration mandates the use of gloves during therapy activities when there is potential for contact with mucous membranes within the mouth.48 Another critical factor when working with different food textures is the understanding that certain foods carry a high choking risk and require modifications or close supervision with young children, especially round slices of hot dogs, small hard candies, nuts, popcorn, raw carrots, fruits with seeds, and chewing gum.
INTERVENTION STRATEGIES
Occupational therapists often recommend changes to the mealtime environment to promote success with oral feeding. Environmental adaptations may be recommended to change the structure of the child’s daily mealtime routines. Specifically, therapists may provide intervention recommendations for scheduling and location of meals, length of meal periods, sensory stimulation within the environment, or changes to the order of mealtime activities.
Children often benefit from regularly scheduled meals at consistent times or locations from day to day. When parents allow children to snack or consume liquids throughout the day, there may be little opportunity for children to become hungry during mealtimes, when more nutritious foods are presented. Consistently scheduled meals and snacks allow the child to experience periods of time without eating, which may promote hunger cues and more interest in eating.44 Children should also have a consistent location for meals, such as sitting in a high chair or at a specific table. Wandering around while eating or having meals in different locations every day may be distracting for young children and does not help to establish positive mealtime behaviors.39
Some children may require shorter meal lengths. Children with neuromuscular impairments may eat slowly and have long meal periods because of oral motor or self-feeding difficulties. Parents of children with poor growth may prolong mealtimes to try to encourage more food intake. When mealtimes are longer than 30 to 40 minutes on a regular basis, the demands on the child and the caregiver become extremely high. Children who become fatigued during prolonged meals may expend increased energy to sustain the feeding, outweighing any benefits from additional oral intake.29 Children with delayed gastric emptying or gastroesophageal reflux may benefit from smaller, more frequent meals throughout the day.44 Larger meals may create more discomfort or episodes of vomiting in children with gastrointestinal disorders.
The amount of sensory stimulation and number of distractions within the environment may also impact a child’s oral feeding skills. Many children show improved oral feeding when environmental distractions are limited. Limiting the sensory stimuli within the environment may be beneficial for children who are concentrating on independent self-feeding, children who are hypersensitive to environmental stimuli, and infants with disorganized suck-swallow-breathe coordination. A calming sensory environment can be created with dim lights, reduced noise, soft or rhythmic music, and limited interruptions. Alternatively, some children may eat better when environmental distractions are present during mealtimes. Active toddlers may consume more food or have improved ability to remain seated at a meal when they are allowed access to a favorite toy or television show. The use of distraction may also help some children with defensive behaviors, to reduce the child’s focus on the discomfort of the oral feeding activity.50
Occupational therapists may also consider the order of presenting foods and liquids during meal sessions. Some children have more success when challenging oral feeding activities are presented at the beginning of the meal, when the child is feeling hungry and their muscles are less fatigued. When the challenging task creates disruption or distress and impacts the child’s oral intake for the remainder of the meal, therapists may consider implementing a new intervention outside of meals or during a smaller snack session.
Positioning Adaptations
Oral motor and feeding activities require skilled movement and coordination of many small muscle groups. Children with postural instability and neuromuscular impairments have difficulty with oral motor control if they do not have adequate positioning support. Positioning changes may have an immediate impact on some difficult oral motor problems such as tonic bite and tongue thrust movement patterns. When a therapist is making positioning adaptations, proximal support (i.e., support at the trunk and neck) influences distal movement and control. For this reason, therapists should consider positioning throughout the child’s whole body. Positioning of the feet, legs, and pelvis influences the child’s trunk stability. Stability, muscle tone, and activity in the trunk muscles affect the child’s ability to move or stabilize the head and neck. The position and muscle activation of the child’s head and neck influence jaw movements. Finally, good jaw stability and freedom of movement influence the child’s tongue and lip control.44 Providing external postural stability, excellent alignment, and comfort during oral feeding activities optimizes a child’s oral motor skills and oral intake.
In general, positioning adaptations provide stability in the trunk and support the child in a midline orientation with the head and neck aligned in neutral or slight flexion during oral feeding. The child’s age, size, neuromuscular status, and self-feeding skills must be considered, as well as the caregiver’s position and comfort. Lastly, positioning adaptations should promote social interaction and communication during mealtimes.
Infants may be supported in a variety of positions during oral feeding. Side-lying within the caregiver’s arms is a common position during breast-feeding. This position may also be recommended for children who have difficulty coordinating sucking, swallowing, and breathing, because the impact of gravity does not immediately draw the liquid into the pharyngeal space. It may be difficult for the caregiver to hold a child in a side-lying position for prolonged periods, especially with older children or infants with hypotonia. Infants may also be supported in supine position within the caregiver’s arms or on a caregiver’s thighs facing the caregiver (Figure 15-3). The supine position provides excellent alignment and midline orientation for infants who take formula from a bottle. An infant seat, car seat, or a Tumble Forms Feeder Chair (Figure 15-4) may be adapted with small rolls to provide head and trunk support or slight shoulder protraction to help an infant hold his or her own bottle. Both of these positioning options allow the feeder to have two hands free, creating opportunities to provide oral motor support or implement handling techniques.
For older infants and toddlers who are engaging in spoon-feeding activities, additional positioning options are available. A regular high chair may provide adequate trunk support and can be easily adapted with small towel rolls for additional foot support or lateral support. The height of a standard high chair also allows caregivers to sit comfortably at a table, promoting social interaction between the child and the family.
Older children with neuromuscular impairments may require a wheelchair or a Rifton chair (Figure 15-5) to provide optimal support during oral feeding. A variety of options and accessories are available for customization of these positioning devices. Within a seated position, the child should have supported feet and neutral pelvic alignment. Lateral trunk or arm supports, a pelvic strap, or a tray may help to provide more stability for the trunk. Wheelchairs may also be customized with a padded vest strap or humeral wings to help promote a forward position of the shoulders and arms for added stability.

FIGURE 15-5 Rifton chair provides a firm base of support to trunk and feet during self-feeding. (Courtesy Kennedy Krieger Institute.)
Research has been conducted to evaluate the use of adaptive seating in children with neuromuscular impairments and developmental delays. Results from this research indicate that children demonstrated improved head control, reaching, grasping, sitting posture, and visual tracking when using positioning devices, as well as decreased dependence on caregivers during activities of daily living.35 Hulme and colleagues reported that optimal positioning included vertical head and trunk position, hip flexion greater than 90 degrees, knee flexion at 90 degrees, and feet supported on a flat surface.35
Therapists may need to work with families to determine whether positioning equipment will fit comfortably within the home and to evaluate caregiver perceptions about adaptive equipment. Reilly and Skuse studied positioning during mealtimes within the home for children with cerebral palsy.52 They found that positioning problems were common among children with cerebral palsy; however, only 50% of parents who received adaptive positioning devices used the equipment regularly. Occupational therapists must evaluate each child and caregiver individually to determine the best options for positioning during oral feeding, provide education about the benefits of proper positioning, and suggest alternatives to adaptive equipment when necessary.
Interventions for Sensory Problems
Abnormal sensory processing, such as hypersensitivity to food tastes, textures, or smells, can create significant problems with oral feeding. Children with oral hypersensitivity often react negatively to touch near or within the mouth. They may turn away from feeding or tooth-brushing activities, restrict food variety, gag frequently, or have difficulty transitioning to age-appropriate food textures. Children diagnosed with generalized tactile defensiveness have a significantly higher incidence of oral hypersensitivity and oral feeding difficulties compared with typical peers.62 Oral hypersensitivity is also common in children who have received extensive medical interventions. Medical interventions such as intubation, orogastric or nasogastric tube feeding, or frequent oral suctioning may have caused ongoing distress or gagging, affecting the development of the sensory systems. Early feeding problems experienced in infancy, such as gastroesophageal reflux or swallowing difficulties, may have created negative associations between food consumption and discomfort.61 The child’s sensory system becomes overprotective, and hypersensitivities may continue long after the noxious stimuli or swallowing impairments are eliminated. Children with developmental and neurologic conditions, including diagnoses such as autism, pervasive developmental disorders, cerebral palsy, traumatic brain injury, genetic conditions, and generalized sensory integration dysfunction may also exhibit oral hypersensitivity.
In most young children, oral exploration and gradual adaptation are natural processes assisted by oral feeding and associated comfort and caregiver bonding. Children who experience prolonged periods of nonoral feeding may demonstrate signs of oral hypersensitivity.64 When the child’s oral sensory system is not challenged to explore tastes and textures of objects and foods during critical periods of development, the child may have difficulty adjusting to new oral stimuli at a later developmental stage.61
Occupational therapists create opportunities for gradual oral sensory exploration through play and positive experiences to reduce oral hypersensitivity. Children may tolerate greater sensory input if the activity is under the child’s control and provided in the context of a motivating, developmentally appropriate activity.14 Therapists provide access to textured objects, teethers, or vibrating toys, and playfully encourage the child to explore them with his or her hands, face, and mouth. Therapists may also engage the child in songs or games to encourage self-directed touch to the face, or play dress-up with hats, scarves, or sunglasses.
Children with oral hypersensitivity may benefit from generalized sensory deep pressure or calming strategies such as slow, linear rocking before oral stimulation. Infants may be encouraged to soothe themselves with hand-to-mouth activities or a pacifier.
Children may gradually improve acceptance of therapist-directed touch with firm pressure that is first applied distally on the body, such as on the arms or shoulders, before moving to touch near the face. A variety of tools can be used to provide stimulation within the mouth, including a gloved finger, a warm washcloth, a Nuk brush, a Pro-Prefer (nonridged) device, an infant or child toothbrush, or a teething ring. Applying firm pressure to the child’s gums or palate may help to reduce oral hypersensitivity. Older children with more mature oral motor skills may enjoy whistles, oral sound-making games, bubbles, and blow toys to improve oral sensory processing.
During feeding activities, the occupational therapist introduces new flavors and textures gradually. A lollipop or teething ring can be dipped into a new flavor of food. Children may advance their oral feeding skills when slight changes are made to their current preferred foods. The therapist can gradually thicken a food, combine strained baby foods with pureed table foods for stronger flavors, or change food temperatures to expand the child’s sensory experiences. The therapist or parent should provide consistent praise and encouragement for the child’s oral exploration and feeding attempts.
Some children with sensory integration dysfunction have low sensory registration and may demonstrate poor oral sensory awareness. These children may frequently seek oral sensory stimulation by mouthing their hands, toys, or clothing. They may have decreased awareness of drooling or try to overstuff their mouths when eating. Occupational therapists may establish a treatment program to provide enhanced oral sensory input intermittently throughout the day. Oral activities with a Nuk brush, cold washcloth, or vibrating device can be used to provide oral sensory stimulation.39 During mealtimes, foods with strong flavors and cold temperatures may help the child take appropriately sized bites of food. Children who consistently overstuff their mouths when eating may require foods that are cut into pieces, verbal cues, or supervision for safety.
Neuromuscular Interventions for Oral Motor Impairments
A wide range of children demonstrate oral motor impairments that affect the development of feeding skills. Oral motor problems are seen frequently in children with global neuromuscular impairments resulting from cerebral palsy, traumatic brain injury, prematurity, or genetic conditions such as trisomy 21. Children without neuromuscular impairments may also demonstrate oral motor problems when they are delayed in transitioning from a bottle to a cup or from puréed foods to textured foods. Inexperience with normal feeding activities may contribute to oral motor weakness and coordination difficulties. Oral hypersensitivity may cause a child to retract his tongue back within the mouth to avoid stimulation, contributing to maladaptive oral movement patterns. Occupational therapists include oral motor activities within a comprehensive intervention plan to promote strength and coordination for the development of functional oral feeding skills.
Whenever possible, oral motor activities should include foods or flavors to incorporate taste receptors and facilitate the integration of both sensory and motor skills for a functional response. Hypersensitive children may tolerate nonnutritive activities initially, before they are able to accept the additional sensory input that food flavors provide.
Jaw weakness is often seen in children with oral feeding difficulties. This may contribute to an open-mouth posture at rest, drooling, food loss during feeding, difficulty with chewing a variety of age-appropriate foods, or poor stabilization when drinking from a cup. Jaw weakness and instability may also affect lip closure for spoon feeding and control during swallowing. Occupational therapists may facilitate jaw strength with a variety of nonnutritive or nutritive activities. Nonnutritive strengthening activities may include sustained biting or repetitive chewing on a resistive device or flexible tubing (Figure 15-6) before the introduction of food textures. Nutritive jaw strengthening activities may include biting or chewing on fruits or vegetables encased in a mesh pouch or progressive resistive activities with a variety of solid or chewy foods placed over the molar surfaces.56

FIGURE 15-6 Using a resistive device to improve oral motor skills for advanced food textures. (Courtesy of Kennedy Krieger Institute.)
Children with neuromuscular impairments may have strong patterns of abnormal oral movement. A tonic bite may be seen, in which a child bites down forcefully in response to a stimulus and has subsequent difficulty opening or relaxing the jaw. Poor trunk and head control and positioning in an extension pattern may contribute to a tonic bite. Assisting the child into flexion of the neck with good trunk and shoulder support helps to reduce this pattern. A strong tongue thrust movement pattern may also be present, where the tongue forcefully protrudes beyond the border of the lips during oral feeding activities. A well-supported and slightly flexed position reduces the severity of this abnormal movement pattern. Children with tongue thrust may also benefit from oral motor activities to facilitate tongue lateralization and placement of the spoon or food bolus to the sides of the mouth rather than at midline.11
Children may demonstrate immature forward-backward tongue movements during feeding, poor dissociation of the tongue from the jaw, and poor tongue lateralization to control textured food over the molar surfaces. Occupational therapists may engage the child in activities to facilitate tongue movements such as encouraging the child to make silly faces in a mirror or to lick lollipops or favorite flavors at the corners of the mouth or within the cheeks. Stimulating the sides of the tongue and inside the cheeks with a Nuk brush or oral motor tool may encourage tongue lateralization. Elevation of the tongue tip can be facilitated when touching the tip of the tongue with an oral motor device and providing slight pressure on the anterior hard palate just behind the front teeth.11,33
Problems affecting the lips and cheeks include abnormal tightness or weakness. Children may demonstrate lip or cheek retraction, making it difficult for the child to assume or sustain lip closure. Good lip closure and lip seal are needed to assist the child with oral food control and prevent anterior spillage during feeding. It is also very difficult to swallow with retracted lips and cheeks because the lips seal the oral cavity to create pressure to propel the food bolus into the pharyngeal cavity. Slow perioral and intraoral cheek stretches can help promote lip closure before initiating functional activities with spoon-feeding or whistles.
Evidence reporting the efficacy of oral motor intervention is extremely limited. Research Note 15-1 describes one study evaluating oral motor intervention in children with cerebral palsy. However, numerous authors suggest that oral motor therapy is an important component of a global treatment approach for children with feeding problems.6,18,42
Adaptive Equipment
A variety of adaptive equipment is available for feeding activities, including adaptive spoons, forks, cups, and straws. Adaptive equipment may promote improvement in oral motor control, increase independence in self-feeding, or compensate for a motor or sensory impairment.
Occupational therapists should consider the properties of the spoon or fork used in feeding activities. A spoon with a shallow bowl may help a child with decreased lip closure. A spoon with bumps or ridges on the bottom of the bowl or a chilled metal spoon may provide additional sensory input for a child with decreased sensory registration. A rubber-coated or dense plastic spoon may be used as an alternative to a metal spoon for a child who bites down on the utensil. Utensils with shorter handles or larger grip diameters may help a child to self-feed more independently.39
A child first learning to drink from a straw may do well with a shorter or smaller straw, such as one that typically comes with a juice box. These straws require less oral suction and deliver a smaller liquid bolus. Children who require thickened liquids or those with decreased lip closure may benefit from the use of a relatively short straw with a larger diameter. Therapists may also consider using a straw with a specialized one-way valve. When liquid is pulled into a valved straw, it does not fall back into the cup if the child loses suction. A cup with a handle on it may help a child with poor fine motor skills to drink more independently. U-shaped cut-out cups help to maintain a neutral head position when drinking liquid. Clear cut-out cups also allow the therapist or caregiver to easily see liquid entering the child’s mouth when physical assistance is provided for drinking activities.
Modifications to Food and Liquid Properties
Different consistencies of liquid require different oral motor and oral sensory demands (Box 15-4). Thin liquids presented from an open cup are the most difficult to control within the mouth. Thick, lumpy, or pasty foods such as oatmeal require more oral motor strength and sensory tolerance when compared with smoother and thinner puréed foods. Occupational therapists may recommend changes to food or liquid properties to compensate for a variety of swallowing, oral motor, and oral sensory deficits.
Thickened liquid is easier to control with the lips and tongue, moves more slowly within the mouth, and allows the child more time to organize a bolus for effective swallowing without early spillage into the pharyngeal cavity. Children with dysphagia may not be able to coordinate swallowing with thin liquids, and aspiration and penetration events are more common with thin liquids when evaluated with videofluoroscopic swallow studies.13,26,43 Thickened liquids may also be used to compensate for oral motor difficulties when a child is first learning to drink from an open cup, even when the child has pharyngeal competence with thin liquids from a bottle or sip cup. When a therapist recommends thickened liquids, the child’s liquid intake and hydration status must be closely monitored to ensure the child is meeting daily fluid requirements.
A variety of foods and supplements can be used to thicken liquids. Simply Thick is one type of commercial gel thickener; it is tasteless and does not add any texture to the liquid, even after the liquid has been sitting out for some time. Other commercial thickeners include powder thickeners such as Diafoods Thick-It and Thick-It 2, and Resource Thicken-Up. Puréed or baby food fruits and vegetables may be used to create blenderized smoothies. Dried infant cereals or mashed potato flakes may be added to thicken formula or milk. Yogurt or pudding may be added to create blenderized milkshakes. Each thickener has different sensory, nutrition, and thickening properties, all of which should be considered in a therapist’s recommendations.
There are also multiple different textures and sensory properties of foods that may be considered within an intervention plan. Foods with a smooth, even, cohesive consistency, such as yogurt and strained fruits or vegetables, are easier to manage when a child has oral sensory and oral motor impairments. Foods that are dense, crunchy, sticky, or uneven in consistency are more difficult to manage. Table 15-4 provides examples of food progressions based on texture and consistency.
The National Dysphagia Diet provides standardized terminology when describing food texture modifications in dysphagia management.3 Although pediatric therapists often use additional descriptors for food textures, such as “junior” or “ground,” some institutions have begun using the terminology from the National Dysphagia Diet (Box 15-5).
When presenting foods and liquids, therapists may alter the size of the bite or sip of liquid. When first beginning to advance with a new skill for the child, therapists may present a food or liquid in a small, consistent bolus size. For example, offering one teaspoon of liquid (5 mL) from a small cut-out cup may help a therapist to clearly evaluate the child’s oral motor and swallowing skills when compared with unmeasured free access sips. Similarly, offering a smaller food bolus when trying a new taste or texture may promote greater success for the child.
Consideration should be given to other sensory properties of foods, such as taste or temperature. Cold foods or foods with strong flavors, including tangy, salty, or sour foods, may be beneficial for children with decreased oral sensory awareness. Bland, room-temperature, or slightly warm foods may increase intake in hypersensitive children.
Behavioral Interventions
Food refusal often begins with the presence of underlying medical or skill problems. Children with gastroesophageal reflux, constipation, or food allergies may feel uncomfortable when eating and develop food refusal behaviors as a result.61 Children who gag with textured foods or refuse cup-drinking may not have adequate sensory or motor skills to manage these feeding activities. However, a child’s refusal behaviors and oral aversion may persist long after the initial medical, sensory, or skill problems have been adequately managed. Inconsistencies may be seen in which the child accepts cup-drinking in the preschool setting but refuses to drink from a cup at home. Behavioral “power struggles” may develop during mealtimes. In many cases, occupational therapists may need to include behavioral treatment strategies within the comprehensive intervention program to promote successful advancement of oral feeding.
Separate from underlying medical or skill problems, many typical children refuse new foods when they are first introduced as toddlers. Evidence has been reported that it takes multiple presentations of a food before a child feels comfortable with it and before a true food preference can be determined.12,40 Some caregivers will try a new food once or twice and then give up. Children with autism or food refusal behaviors may become more selective over time, gradually eliminating foods from their diet. Therapists should encourage parents to offer small amounts of a new food across multiple meal sessions to allow the child sufficient time to adapt to the new taste or texture.
A child’s refusal to eat may contribute to caregiver stress, and mealtimes may become a battleground, with increasing levels of negative or stressful interactions.31 Therapists try to create new positive interactions and child associations around feeding activities and mealtimes. Therapists and caregivers should have a relaxed, confident, and caring demeanor during oral feeding and therapy activities. Offering choices and turn taking during an activity may help a child have a sense of control and increase willingness to participate during mealtimes. For example, a caregiver may offer a choice of two different foods or the therapist may allow the child to choose which activity is performed first.
When implementing behavior management strategies, it is important to determine an appropriate form of praise or reinforcement for the child’s positive behaviors. The occupational therapist can provide clear expectations and break the activity down into small, achievable steps. When the expectations are small and achievable, the child has the opportunity to experience praise and positive reinforcement for participation and success. Consistent success with an activity should be attained before the demand is increased.23 If the demands are increased rapidly or if the activity is continued indefinitely until the child’s refusal behaviors intensify, he or she may quickly learn to refuse more strongly to escape the activity the next time it is presented. When behavioral strategies are implemented with gradual progression of new skills, positive reinforcement, and clear expectations, the child learns to trust the therapist or caregiver, and the negative behaviors may quickly decrease in frequency and intensity.
It is not unusual for children with feeding disorders to experience negative behaviors when trying new oral feeding activities. Negative behaviors may include crying, pushing the spoon or cup away, or spitting the food out. Children may also occasionally cough, gag, or perhaps even vomit when trying new oral feeding activities. When parents or therapists react strongly to these events and immediately end the activity, the child may begin to gag, cough, or cry more frequently at the onset of the meal as a way to quickly escape the demand. Multiple research studies have supported the use of differential attention during mealtimes, where positive reinforcement is combined with ignoring or redirection of inappropriate behaviors to improve oral intake.10,38,51 Another study showed that positive reinforcement and regular exposure to nonpreferred foods significantly improved oral consumption and self-feeding skills.68 Occupational therapists may suggest the use of a visual schedule or timer set in advance to help the child clearly understand when the activity is finished, rather than having the parent end the meal when the child’s behavior has escalated. This clear end to the activity may also help the child transition from the difficult or new task back to their usual routine of feeding.
Interventions to Improve Self-Feeding
Children experience delays in self-feeding skills because of physical or neuromuscular deficits, cognitive or visual impairments, sensory processing difficulties, behavioral refusal, or poor motivation to eat. Each of these underlying causes creates different challenges for the intervention plan. Children will have the most success when they have begun to demonstrate an interest in self-feeding and an interest in exploring food more independently. Within each intervention plan, the therapist’s goal is to facilitate the child’s success and gradually decrease the amount of physical assistance or adaptive equipment required in self-feeding.
For children with physical or neuromuscular deficits, it is particularly important to create a balance between the effort of self-feeding, oral motor, and swallowing safety, the overall length of the meal, and the child’s nutritional needs. Therapists may implement self-feeding activities for only a portion of the meal, or during a smaller snack session, to allow practice and skill development opportunities. Adaptive positioning or adaptive feeding equipment can be used to facilitate grasp patterns or hand-to-mouth movements. When providing positioning recommendations, therapists attempt to support correct postural alignment and stability to allow the child greater control of the arm in space while bringing the spoon to the mouth. Adaptive positioning to support self-feeding activities may include a chair that provides good postural support and allows access to a stable tray or table for increased arm stability. A raised tray or table surface may provide more trunk and shoulder stability while decreasing the distance the child needs to move the spoon or fork from the bowl to the mouth. Stabilizing the elbow on the table or tray can also help reduce the physical demand of self-feeding, prolonging the child’s endurance.
Dycem or a nonskid placemat may help to prevent movement of the dish or bowl to compensate for uncoordinated arm movements. Children may have improved independence when self-feeding with foods that stick to the spoon or with a scoop-dish that has raised edges. Some dishes also have a suction cup on the bottom to help secure them to the table.
A utensil with a built-up handle that is not weighted may help to compensate for a weak grasp pattern. Children with severely impaired grasping skills may benefit from a utensil that has straps to secure it to the hand in a stable position. Toddlers who are first learning to self-feed may benefit from a utensil that has a shorter handle. A curved handle may help to compensate for limited forearm or wrist coordination.
There are also a variety of adaptations that can be made to help children drink liquids more independently. Cups with a wide base or cups with lids may help reduce spillage when the child is placing the cup on a table. Some children may benefit from a long straw placed within a cup that is secure in a cup-holder, reducing the need to lift or move the cup with the hands.
Children with cognitive or behavioral problems may benefit from backward chaining of self-feeding, with gradually decreasing levels of assistance provided. During the first step of this backward chain, children may be required only to move the spoon with their hand for the last few inches before it reaches the mouth. The therapist can scoop the food onto the spoon or provide hand-over-hand assistance for the remainder of the task. Klein and Delaney suggest a utility hand-hold for providing physical assistance during spoon feeding, whereby the caregiver uses the middle or index finger to hold the spoon within the child’s hand, and places the thumb on the back of the child’s wrist (Figure 15-7).39 Using this technique, the therapist can apply varying amounts of pressure in the palm to facilitate grasp, while also assisting with appropriate wrist movements needed for self-feeding. The occupational therapist praises and encourages the child for each step of his or her progress toward independent self-feeding.

FIGURE 15-7 The therapist supports and guides the child’s hand during self-feeding using the thumb on hand dorsum and finger in his palm.
When encouraging self-feeding in children with visual impairments, therapists may recommend consistent orientation of food and drink on the placemat. For example, placing the cup in the 2 o’clock position next to the plate or placing different foods in consistent locations within the dish may improve the child’s awareness of the mealtime environment for improved independence.
Children with sensory defensiveness may be less willing to explore food with their hands to finger feed independently. Therapy activities to reduce generalized hypersensitivity outside of mealtimes are indicated to prepare the child for self-feeding. During mealtimes, therapists may try a variety of spoons, such as those with a small diameter or smooth handle, to improve a child’s tolerance. Some children may be more willing to try self-feeding when they are simply provided with a napkin or moist cloth to reduce their discomfort if the feeding activity becomes messy.
INTERVENTION: SPECIFIC REFERRAL PROBLEMS AND MEDICAL DIAGNOSES
When aspiration or pharyngeal dysphagia affects a child’s ability to eat safely, occupational therapists may recommend food or liquid consistency adaptations, such as thickened liquids for children who aspirate with thin liquids. When thickened liquids are recommended, collaboration with physicians and nutritionists is required to help ensure the child’s nutrition and hydration needs are met. Some children who are prescribed thickened liquids have poor acceptance of the new liquid and reduce their oral intake. Therapists may consider a variety of liquid thickeners to benefit the child to help improve compliance. More recent research suggests there may also be alternatives to thickeners, such as carbonated liquids, to reduce aspiration or penetration (Research Note 15-2). Comprehensive caregiver training is needed to ensure understanding of clinical signs of aspiration, methods for modifying liquids, and safety precautions during oral feeding.
Positioning is also very important for children who have dysphagia. Supportive positioning can have a major impact on the child’s oral motor and swallowing skills. A chin-tuck position may be recommended when the child has delayed swallow initiation. During a videofluoroscopic swallow study, a delay is typically seen as pooling of food or liquid in the pharyngeal space located close to the opening of the larynx. When the child is positioned with a slight chin tuck, the laryngeal opening may become smaller, reducing the risk of aspiration or penetration. Occasionally, a chin-tuck position may be contraindicated for young infants who have laryngomalacia or tracheomalacia (softening of the cartilage within the larynx or trachea), because their soft tissues may be more prone to collapse.57 Garon also reported problems associated with the chin-tuck position in dysphagic adults with abnormal epiglottic movement patterns after a neurologic insult.28 Occupational therapists need to make individualized positioning recommendations based on a comprehensive assessment and provide follow-up services to evaluate the outcomes of positioning changes on oral feeding skills.
Adaptations to the mealtime structure may be made to compensate for dysphagia. Occupational therapists may recommend reducing the meal length to compensate for weakness or muscle fatigue. Some children with poor oral control require multiple swallows to clear one bite of food. If a child is unable to complete a subsequent swallow in response to a verbal prompt, an empty spoon offered in the same way as a bite of food may stimulate oral movements to prompt a second swallow. Therapists may also provide recommendations for the pace of oral feeding to allow the child sufficient time to swallow and to promote safety. More difficult foods, liquids, or self-feeding activities may need to be limited or presented within the first few minutes of a meal session when the child is less fatigued. Children may also benefit from a smaller food or liquid bolus achieved through the use of a controlled-flow cup, small, measured sips, or a smaller spoon.
Occupational therapists may consider implementing oral motor activities with cold stimulation or thermal gustatory stimulation to the anterior faucial arches located in the back of the mouth to facilitate a reflexive swallow response.2 Cold stimulation may also be provided with a frozen lemon-glycerin swab, a cotton swab dipped in water and frozen, or small amounts of lemon sherbet on a Nuk brush or other oral device. Offering chilled foods or liquids may also help to create a more efficient swallow.57
Research studies have been completed with adult and pediatric clients evaluating the use of neuromuscular electrical stimulation (NMES) in the treatment of dysphagia. In some cases, NMES resulted in significant improvements in swallow function when other traditional interventions had failed.19,25 VitalStim therapy has been approved by the U.S. Food and Drug Administration as a safe treatment modality. The neuromuscular electrical stimulation is provided to strengthen or reeducate muscles on the face and anterior neck to promote swallowing and reduce dysphagia. VitalStim therapy may be administered only by therapists who obtain specialty training and certification.
Food Refusal or Selectivity
Some children referred to occupational therapists are highly selective or “picky” eaters. Initial recommendations may include consultation with physicians to consider gastroesophageal reflux disease, food allergies, digestive problems, or structural abnormalities. Occupational therapists may also work to address underlying skill deficits or swallowing safety concerns, which may contribute to food refusal behaviors. When management of medical or skill problems has been optimized, children may continue to demonstrate ongoing food refusal or food selectivity behaviors.
Children with food refusal or selectivity often benefit from environmental adaptations, including mealtime structure for consistent feeding times, reducing grazing, or excessive liquid consumption outside of meals, consistent eating locations, and consistent length of meals. These environmental strategies will promote hunger cues, limit access to less nutritious foods, and create structure within the meal to establish positive eating patterns.
Occupational therapists may also consider interventions to reduce oral hypersensitivity and improve oral sensory exploration skills. Children with food selectivity frequently react to the sensory properties of new foods. Interventions to reduce oral hypersensitivity and generalized defensiveness outside of meal sessions may help the child to prepare for the new feeding challenges.
Finally, therapists may recommend or implement behavioral treatment strategies within a comprehensive intervention program to reduce food refusal and food selectivity. Behavioral strategies may include positive reinforcement when a child explores, tastes, or swallows a nonpreferred food and adapting the activity demand to gradually build on small, achievable steps.
Delayed Transition to Textured Foods
Children who are unable to transition to age-appropriate food textures frequently have a combination of oral sensory and oral motor problems, and some may also demonstrate behavioral refusal. Occupational therapists may implement nonnutritive oral motor activities to reduce hypersensitivity and improve oral motor coordination. Jaw strengthening and repetitive chewing activities without the demand for swallowing may assist the child to build oral motor skills. Increased tolerance for food textures is typically addressed by placing crumbs on a piece of chewy tubing or slowly adding rice flakes to a puréed food. Children who consume baby foods should begin to transition to puréed table foods to adjust to stronger flavors and a wider variety of oral sensations. Children may practice chewing foods encased within a mesh feeding bag to experience repetitive chewing with less risk for gagging or choking. Therapists may provide praise or behavioral reinforcement for the child’s participation in challenging new activities. When a child is able to take a few small bites of textured food safely outside of primary meal sessions, therapists may begin to integrate these new skills slowly within meals, such as during the first 5 to 10 bites. Rapidly increasing the demands within the meal session before the child has adequate motor or sensory skills may affect oral intake or nutritional status and create stressful child–caregiver interactions. Box 15-6 is helpful in recognizing the foods that may be indicated and contraindicated in children with immature oral motor skills.
Delayed Transition from Bottle to Cup
There are a variety of reasons why a child may have difficulty transitioning from breast or bottle-feeding to drinking from a cup. Efficient cup-drinking requires more mature oral motor movements. Difficulty transitioning from the bottle to the cup can be caused by poor jaw stability, oral control, or pharyngeal coordination to manage a more unpredictable liquid bolus. Children with a history of failure-to-thrive may have prolonged dependence on bottle or breast feeding as the most reliable method to meet their nutritional or hydration needs. When a child is orally hypersensitive, he or she may dislike the intermittent touch of the cup on the outside of the lips or spillage that often occurs during early cup-drinking activities.39 Hypersensitive children may also seek the calming, organizing sensory input that comes from sucking during bottle or breast feeding.
To help children prepare for cup-drinking activities, therapists may initially work on jaw stability, lip closure, tongue movements, and oral sensitivity through positioning, handling, and oral motor activities. Cups with nonspill valves within the lid require stronger lip closure and oral suction abilities and may be more difficult to use for children with neuromuscular impairments. A spouted cup may initially make it easier for a child to suck the liquid or form a bolus within the mouth. Spouted cups may also provide similar sensory input to bottle-feeding for children with sensory defensiveness. When drinking from a cup with a spout, the child may need to tilt the head back, which may create additional difficulties if the child has extensor posturing, poor head control, or pharyngeal swallowing problems. Use of a cut-out cup may help to reduce head and neck extension and allows the therapist to easily observe the flow of liquid and the child’s mouth movements during drinking activities.
With free-flowing liquid from an open cup or nonvalved spouted cup, children should be positioned in a more upright position to encourage bolus formation within the mouth, without the impact of gravity creating an uncontrolled flow into the pharyngeal space. Children may also benefit from thickened liquids when first learning to drink from a cup to compensate for decreased oral control or pharyngeal swallowing skills. External jaw support can be provided by the therapist, where the therapist’s index finger is underneath the lower mandibular bone, and the thumb is placed on the anterior chin. Providing jaw support while sitting beside the child with the arm around the back of the child’s neck may allow the therapist to provide additional stability for the child to maintain adequate head alignment (Figure 15-8). Children often bite on the rim or spout of the cup to gain additional jaw stability. They also may push the cup into the corners of their lips or rest their tongue on the rim of the cup for additional sensory input.39 These patterns should decrease over time as the child becomes more skilled in managing liquids from a cup.
Cleft Lip and Palate
A cleft lip or palate is a separation of parts of the mouth usually joined together at midline during the early weeks of fetal development. A cleft lip is separation of the upper lip and often the upper dental ridge. A cleft palate is a separation of the hard or soft palate and may occur with or without a cleft lip. Because of the lack of closure between the oral and nasal cavities, young infants have difficulty creating suction to express liquid from a nipple.30 After surgical repair of the cleft, older children may have difficulty with active lip movement, oral defensiveness, or nasopharyngeal reflux during oral feeding.
Occupational therapists typically recommend compensatory positioning, equipment, and strategies for oral feeding before surgical repair of the cleft. A variety of nipples are available to compensate for oral structural problems. The Habermann nipple was developed specifically for infants with cleft palate to deliver flow without requiring suction (Figure 15-9). It has a one-way valve that allows the infant to express fluid through compression alone, without requiring suction.30 This nipple allows the infant to independently control milk flow. Long nipples may help deposit liquid toward the back of the infant’s mouth beyond the cleft to decrease liquid flow into the nasal passageway. Additional considerations for choosing appropriate nipples for infants with cleft palate are provided in Table 15-5. Some children with an open cleft may require a special bottle that can be squeezed by the parent to deposit formula into the infant’s mouth. Children with an open cleft may have more success when positioned upright or in the side-lying position during oral feeding. They also may require frequent breaks to allow for burping during oral feeding.
TABLE 15-5
Nipple Characteristics Related to Use with Children Who Have Oral Structural Defects
| Nipple Type | Characteristics |
| Long, thin nipples | Work well when the tongue is recessed; can bring the tongue forward |
| Single nipple hole | Results in a steady liquid stream, which can be easier to handle than bursts of liquid |
| Wide nipple | Can be compressed for liquid expression for the child with a cleft palate |
| Broad-based nipple | Can help the infant with a cleft lip gain suction |
| Nipple with cross-cut hole | Can create an uneven liquid flow or a burst of fluid that is difficult for the infant to control |
| Nipple with enlarged hole | Should be used with great care; when the caregiver enlarges the hole, it is difficult to predict what type of liquid flow will result |
| Soft, pliable nipple | Appropriate for infants with cleft palates who are unable to achieve suction |
| Nuk nipple | Has the hole on top of the nipple and should not be used with children with cleft palates; this nipple may be functional if its position on the tongue is reversed |
After surgical repair of a cleft, occupational therapists may perform scar massage, initiate activities to reduce oral hypersensitivity, and reassess the oral feeding method. Some children may have ongoing problems with nasopharyngeal reflux during oral feeding, where food or liquid enters the nasal cavity. Therapists may evaluate which food or liquid textures are more problematic for the child, suggest alternating bites of food with sips of liquid, or recommend a specific bolus size to reduce the functional impairment.
Other Structural Anomalies
Other structural anomalies include micrognathia and macroglossia. Micrognathia is defined as a small, recessed jaw. Macroglossia is a term used when the tongue is disproportionately large in comparison with the size of the mouth or jaw. Therapists need to consider the impact of the size and position of oral structures on respiration and oral movement patterns during feeding. Therapists may use different nipples, utensils, or positioning adaptations to help compensate for these structural differences. For example, infants with micrognathia may benefit from prone positioning to help draw the tongue into a more forward position, allowing improved respiration and nipple compression during bottle-feeding.
Structural anomalies of the esophagus include esophageal strictures, tracheoesophageal fistula, and esophageal atresia. With tracheoesophageal fistula or esophageal atresia, the structural abnormalities are repaired surgically. Children with structural anomalies of the esophagus are at increased risk for functional problems with feeding, eating, and swallowing associated with poor esophageal motility. Esophageal motility describes how quickly foods and liquids move through the esophagus and empty into the stomach. Liquids and smooth, runny foods empty into the stomach more quickly than thick, fibrous, or more solid foods. Children who have a history of esophageal structural anomalies may have problems advancing to higher food textures as a result of decreased esophageal motility. Occupational therapists may recommend adapting food textures to maximize oral intake, alternating bites of food with sips of liquid to help clear the esophagus, slowing the pace of feeding, or encouraging a subsequent dry swallow after each bite of food to help compensate for delayed esophageal motility.
Transition from Nonoral Feeding to Oral Feeding
Nonoral feeding with a gastrostomy, nasogastric tube, or other method is indicated when a child is unable to meet his or her nutrition or hydration needs by mouth. Nonoral feeding methods may be used when the child has dysphagia; complex heart, respiratory, or other medical conditions; or gastrointestinal problems. Other children require nonoral feeding methods simply because they are unable to consume enough food or liquid by mouth to demonstrate adequate growth and hydration. Inadequate nutrition or hydration can severely limit a child’s motor development, cognitive development, and health.29 The placement of a gastrostomy tube or the use of other nonoral feeding methods can be a temporary measure to promote the child’s nutritional status and growth.64
When children receive nonoral feeding, they are at risk for developing oral motor and oral sensory impairments because of limited oral feeding experiences. Nasogastric and orogastric tubes may also create sensory distress for the child during the placement of the tube. When these tubes are needed over a long period of time, they are typically re-inserted or replaced every month, causing further sensory distress to the child. Occupational therapists may provide an intervention program to provide ongoing oral exploration activities and social engagement during nonoral feeding. The goal is to create positive social and oral exploration experiences on a daily basis and ultimately link these pleasurable experiences with the satiation of hunger.
If there is a history of aspiration dysphagia or if oral feeding is not medically safe, the child may suck on a pacifier or engage in mouth play with teethers, spoons, and toys during nonoral feeding. Therapists and caregivers can engage in games that include touch and exploration around the face and mouth. Children may also benefit from games that encourage them to make different sounds with their mouth, give kisses, or blow whistles or bubbles. Whenever possible, therapists should encourage families to include their child in mealtime routines, such as sitting with the family at the table during tube feedings and oral play activities.
When the child is medically cleared to have nutritive stimulation, therapists and caregivers can provide flavors or tastes of foods by dipping a finger, pacifier, spoon, or toy into juice, formula, or puréed foods. Children who receive nonoral feeding may have limited opportunities to experience typical feelings of hunger. This is especially true when children require nonoral feedings on a continuous schedule across many hours during the day. Children who are able to tolerate more compressed bolus feedings may have more opportunities to experience hunger, which may increase the child’s motivation to consume some foods by mouth. As the child is beginning to advance oral intake skills, therapists need to collaborate with physicians or nutritionists, who can determine appropriate schedule changes and reductions in nonoral nutrition.
Children who have tracheostomies often require nonoral feeding methods. The risk and complications of aspiration are significantly increased in a child with a tracheostomy because of the fragility of the respiratory system.1 This may be related to the changes in pressure created by the new opening in the laryngeal cavity or poor laryngeal mobility. Children with a tracheostomy may be ready for nutritive stimulation when they are able to manage their own saliva without frequent suctioning and can tolerate a Passy Muir valve or cap, which may help to create more normalized pharyngeal swallowing coordination.32 Occupational therapists must collaborate with physicians and complete comprehensive assessments of swallowing before initiating nutritive oral feeding activities in children with tracheostomies. Before receiving medical clearance for oral feeding, children with tracheostomies will benefit from oral exploration and desensitization activities when oral feeding is not possible.
When children are medically cleared and have sufficient oral motor and swallowing skills to consume larger amounts of food by mouth, they may continue to demonstrate strong oral aversions, hypersensitivity, or refusal to engage in oral feeding activities. Transitioning from nonoral to oral feeding is a gradual process and may require a variety of oral sensory, skill development, and behavioral intervention activities over a period of time.
SUMMARY
The causes of pediatric feeding, eating, and swallowing disorders are diverse and complex. Occupational therapists must consider the whole child during the assessment and intervention process, including multiple overlapping child factors and performance skills, activity demands and contexts, and family patterns (Case Study 15-1). This chapter has provided a foundation of knowledge for the occupational therapist to improve a child’s safety during oral feeding, promote acceptance of age-appropriate foods or liquids, and advance functional independence during mealtimes. The assessment and treatment of pediatric feeding disorders require interdisciplinary collaboration between the occupational therapist and other members of the child’s treatment team. As with most occupational therapy interventions, inclusion of primary caregivers within all stages of the assessment and treatment program is extremely important to the child’s ultimate success within natural environments.
REFERENCES
1. Abraham, S.S., Wolf, E.L. Swallowing physiology of toddlers with long-term tracheostomies: A preliminary study. Dysphagia. 2000;15:206–212.
2. Ali, G.N., Laundl, T.M., Wallace, K.L., deCarle, D.J., Cooke, I.J. Influence of cold stimulation on the normal pharyngeal swallow response. Dysphagia. 1996;11:2–8.
3. American Dietetic Association: National Dysphagia Diet Task Force. National dysphagia diet: Standardization for optimal care. Chicago: American Dietetic Association, 2002.
4. American Occupational Therapy Association. Specialized knowledge and skills in feeding, eating, and swallowing for occupational therapy practice. Bethesda, MD: American Occupational Therapy Association, Inc, 2006.
5. American Occupational Therapy Association. Occupational therapy practice framework: Domain and process, second edition. The American Journal of Occupational Therapy. 2008;62(6):609–639.
6. Arvedson, J.C. Management of pediatric dysphagia. Otolaryngologic Clinics of North America. 1998;31:453–476.
7. Arvedson, J.C. Swallowing and feeding in infants and young children. GI Motility, 2006. Retrieved May 27, 2007, from, http://www.nature.com/gimo/contents/pt1/full/gimo17.html.
8. Ardveson, J.C., Brodsky, L. Instrumental evaluation of swallowing. In: Arvedson J.C., Brodsky L., eds. Pediatric swallowing and feeding: Assessment and management. 2nd ed. Albany: Singular/Thomson Learning; 2002:356.
9. Arvedson, J.C., Lefton-Greif, M.A. Pediatric videofluoroscopic swallow studies: A professional manual with caregiver guidelines. San Antonio: Communication Skill Builders, 1998.
10. Babbitt, R.L., Hoch, T.A., Coe, D.A., Cataldo, M.F., Kelly, K.J., Stackhouse, C., et al. Behavioral assessment and treatment of pediatric feeding disorders. Journal of Developmental and Behavioral Pediatrics. 1994;15:278–291.
11. Beckman, D. Oral motor assessment and intervention. Paper presented at the Oral Motor Assessment and Intervention I conference, Charlotte, NC, 2000.
12. Birch, L.L., Marlin, D.W. I don’t like it; I never tried it: Effects of exposure on two-year-old children’s food preferences. Appetite. 1982;3:353–360.
13. Bulow, M., Olsson, R., Ekberg, O. Videoradiographic analysis of how carbonated thin liquids and thickened liquids affect the physiology of swallowing in subjects with aspiration on thin liquids. Acta Radiologica. 2003;44:366–372.
14. Bundy, A.C., Koomar, J.A. Orchestrating intervention: The art of practice. In Bundy A.C., Lane S.J., Murray E.A., eds.: Sensory integration: Theory and practice, 2nd ed., Philadelphia: F.A. Davis, 2002.
15. Byars, K., Burklow, K.A., Ferguson, K., O’Flaherty, T., Santoro, K., Kaul, A. A multicomponent behavioral program for oral aversion in children dependent on gastrostomy tube feedings. Journal of Pediatric Gastroenterology and Nutrition. 2003;37:473–480.
16. Carruth, B.R., Skinner, J.D. Feeding behaviors and other motor development in healthy children (2-24 months). Journal of the American College of Nutrition. 2002;21(2):88–96.
17. Chamberlin, J., Henry, M.M., Roberts, J.D., Sapsford, A.L., Courtney, S.E. An infant and toddler feeding group program. The American Journal of Occupational Therapy. 1991;45:907–911.
18. Christensen, J.R. Developmental approach to pediatric neurogenic dysphagia. Dysphagia. 1989;3:131–134.
19. Christiaanse, M., Glynn, J., Bradshaw, J. Experience with transcutaneous electrical stimulation: A new treatment option for the management of pediatric dysphagia. Winston-Salem, NC: Wake Forest School of Medicine, University Health Sciences, 2003.
20. da Costa, S.P., van der Schans, C.P. The reliability of the Neonatal Oral-Motor Scale. Acta Paediatrica. 2008;97:21–26.
21. Daniels, H., Devlieger, H., Casaer, P., Eggermont, E. Nutritive and non-nutritive sucking in preterm infants. Journal of Developmental Physiology. 1986;8:117–121.
22. DeVault, M.L. Feeding the family: The social organization of caring as gendered work. Chicago: Chicago Press, 1991.
23. Fischer, E., Silverman, A. Behavioral conceptualization, assessment, and treatment of pediatric feeding disorders. Seminars in Speech and Language. 2007;26:223–231.
24. Food Research Action Center Hunger in the U.S., 2006. Retrieved September 2008 from, http://www.frac.org.
25. Freed, M.L., Freed, L., Chatburn, R.L., Christian, M. Electrical stimulation for swallowing disorders caused by stroke. Respiratory Care. 2001;46:466–474.
26. Friedman, B., Frazier, J.B. Deep laryngeal penetration as a predictor of aspiration. Dysphagia. 2000;15:153–158.
27. Fung, E.B., Samson-Fang, L., Stallings, V.A., Conaway, M., Liptak, G., Henderson, R.C. Feeding dysfunction is associated with poor growth and health status in children with cerebral palsy. Journal of the American Dietetic Association. 2002;102:361–368.
28. Garon, B. Swallow dysfunction: New research evidence. Paper presented at Keep Pace Seminars conference, Baltimore, 2003.
29. Gisel, E.G., Applegate-Ferrante, T., Benson, J.E., Bosma, J.F. Effect of oral sensorimotor treatment on measures of growth, eating efficiency and aspiration in the dysphagic child with cerebral palsy. Developmental Medicine and Child Neurology. 1995;37:528–543.
30. Glass, R.P., Wolf, L.S. Feeding management of infants with cleft lip and palate and micrognathia. Infants and Young Children. 1999;12:70–81.
31. Greer, A.J., Gulotta, C.S., Masler, E.A., Laud, R.B. Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. Journal of Pediatric Psychology. 2008;33:612–620.
32. Gross, R.D., Mahlmann, J., Grayhack, J.P. Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. The Annals of Otology, Rhinology, and Laryngology. 2003;112:143–152.
33. Hanson, J. Lip prints: Home program for oral-motor skills. Austin, TX: Pro-Ed, 2004.
34. Hawdon, J.M., Beauregard, N., Kennedy, G. Identification of neonates at risk of developing feeding problems in infancy. Developmental Medicine and Child Neurology. 2000;42:235–239.
35. Hulme, J.B., Gallacher, K., Walsh, J., Niesen, S., Waldron, D. Behavioral and postural changes observed with the use of adaptive seating by clients with multiple handicaps. Physical Therapy. 1987;67:1060–1067.
36. Humphry, R., Thigpen, B. Caregiver role: Ideas about feeding infants and toddlers. Occupational Therapy Journal of Research. 1997;17:237–263.
37. Humphry, R., Thigpen-Beck, B. Parenting values and attitudes: Views of therapists and parents. The American Journal of Occupational Therapy. 1998;52:835–843.
38. Kerwin, M.E. Empirically supported treatments in pediatric psychology: Severe feeding problems. Journal of Pediatric Psychology. 1999;24:193–214.
39. Klein, M.D., Delaney, T.A. Feeding and nutrition for the child with special needs. Tucson, AZ: Therapy Skill Builders, 1994.
40. Koivisto Hursti, U.K. Factors influencing children’s food choice. Annals of Medicine. 1999;31(Suppl. 1):26–32.
41. Lee, E.J., Murry, V.M., Brody, G., Parker, V. Maternal resources, parenting, and dietary patterns among rural African American children in single-parent families. Public Health Nursing. 2002;19:104–111.
42. Logemann, J.A. Evaluation and treatment of swallowing disorders, 2nd ed. Austin, TX: Pro-Ed, 1998.
43. Miller, C.K., Willging, J.P. Advances in the evaluation and management of pediatric dysphagia. Current Opinion in Otolaryngology & Head and Neck Surgery. 2003;11:442–446.
44. Morris, S.E., Klein, M.D. Pre-feeding skills, 2nd ed. Tucson, AZ: Therapy Skill Builders, 2000.
45. National Digestive Disease Information Clearinghouse. Heartburn, Gastroesophageal Reflux (GER), and Gastroesophageal Reflux Disease (GERD), 2008. Retrieved May from, http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/.
46. Newman, L.A., Keckley, C., Petersen, M.C., Hamner, A. Swallowing function and medical diagnoses in infants suspected of dysphagia. Pediatrics. 2001;108(6):E106.
47. Nord, M., Andrews, M., Carlson, S., Household food security in the United States. Economic research report No. (ERR. 49). United States Department of Agriculture, 2006. Retrieved May 2008 from, http://www.ers.usda.gov/Publications/ERR49/.
48. Occupational Safety and Health Administration. Federal Register, 1991;56(235).
49. Palmer, M.M. Identification and management of the transitional suck pattern in premature infants. Journal of Perinatal and Neonatal Nursing. 1993;7:66–75.
50. Palmer, M.M., Heyman, M.B. Assessment and treatment of sensory- versus motor-based feeding problems in very young children. Infants and Young Children. 1993;6:67–73.
51. Piazza, C.C., Patel, M.R., Gulotta, C.S., Sevin, B.M., Layer, S.A. On the relative contributions of positive reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2003;36:309–324.
52. Reilly, S., Skuse, D. Characteristics and management of feeding problems of young children with cerebral palsy. Developmental Medicine and Child Neurology. 1992;34:379–388.
53. Rogers, B., Arvedson, J., Buck, G., Smart, P., Msall, M. Characteristics of dysphagia in children with cerebral palsy. Dysphagia. 1994;9:69–73.
54. Rogers, B., Senn, K. Pediatric Dysphagia. In: Accardo P.J., ed. Capute & Accardo’s neurodevelopmental disabilities in infancy and childhood. 3rd ed. Baltimore: Paul H. Brookes; 2008:145–167.
55. Rommel, N., DeMeyer, A.M., Feenstra, L., Veereman-Wauters, G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. Journal of Pediatric Gastroenterology and Nutrition. 2003;37:75–84.
56. Rosenfeld-Johnson, S. Assessment and treatment of the jaw. Tucson: Talk Tools Innovative Therapists International, 2005.
57. Ruark McMurtrey, J., Best practices for behavioral management of pediatric dysphagia. Pediatric Feeding and Dysphagia Newsletter, Salt Lake City, UT, Hiro Publishing, 2007;7:1–5. [(3)].
58. Schuberth, L.M. The role of occupational therapy in diagnoses and management. In: Tuchman D.N., Walter R., eds. Disorders of feeding and swallowing in infants and children. San Diego, CA: Singular Publishing Group; 1994:115–1300.
59. Schulze, P.A., Harwood, R.L., Schoelmerich, A. Feeding practices and expectations among middle-class Anglo and Puerto-Rican mothers of 12-month-old infants. Journal of Cross-Cultural Psychology. 2001;32:397–406.
60. Schwarz, S.M. Feeding disorders in children with developmental disabilities. Infants and Young Children. 2003;15:29–41.
61. Skuse, D. Identification and management of problem eaters. Archives of Disease in Childhood. 1993;69:604–608.
62. Smith, A.M., Roux, S., Naidoo, N.T., Venter, D.J. Food choice of tactile defensive children. Nutrition. 2005;21:14–19.
63. Sullivan, P.B., Juszezak, E., Lambert, B.R., Rose, M., Ford-Adams, M.E., Johnson, A. Impact of feeding problems on nutritional intake and growth: Oxford feeding study II. Developmental Medicine and Child Neurology. 2002;44:461–467.
64. Tarbell, M.C., Allaire, J.H. Children with feeding tube dependency: Treating the whole child. Infants and Young Children. 2002;15:29–41.
65. Toomey, K. Feeding strategies for older infants and toddlers. Pediatric Basics: The Journal of Pediatric Nutrition and Development. 2002;100:2–11.
66. UNICEF—Progress for Children Nutrition, survival, and development, 2006. Retrieved May 2008 from, http://www.unicef.org/progressforchildren/2006n4/undernutritiondefinition.html.
67. Vergara, E.R., Bigsby, R. Developmental and therapeutic interventions in the NICU. Baltimore: Brookes, 2004.
68. Werle, M.A., Murphy, T.B., Budd, K.S. Treating chronic food refusal in young children: home-based parent training. Journal of Applied Behavior Analysis. 1993;26:421–433.
69. Wolf, L.S., Glass, R.P. Feeding and swallowing disorders in infancy: Assessment and management. Tucson, AZ: Therapy Skill Builders, 1992.
70. Yokochi, K. Oral motor patterns during feeding in severely physically disabled children. Brain & Development. 1997;19:552–555.
71. Zerilli, K.S., Stefans, V.A., DiPietro, M.A. Protocol for the use of videofluoroscopy in pediatric swallowing dysfunction. The American Journal of Occupational Therapy. 1990;44:441–446.
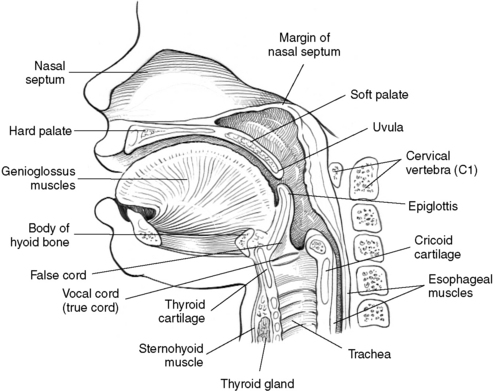
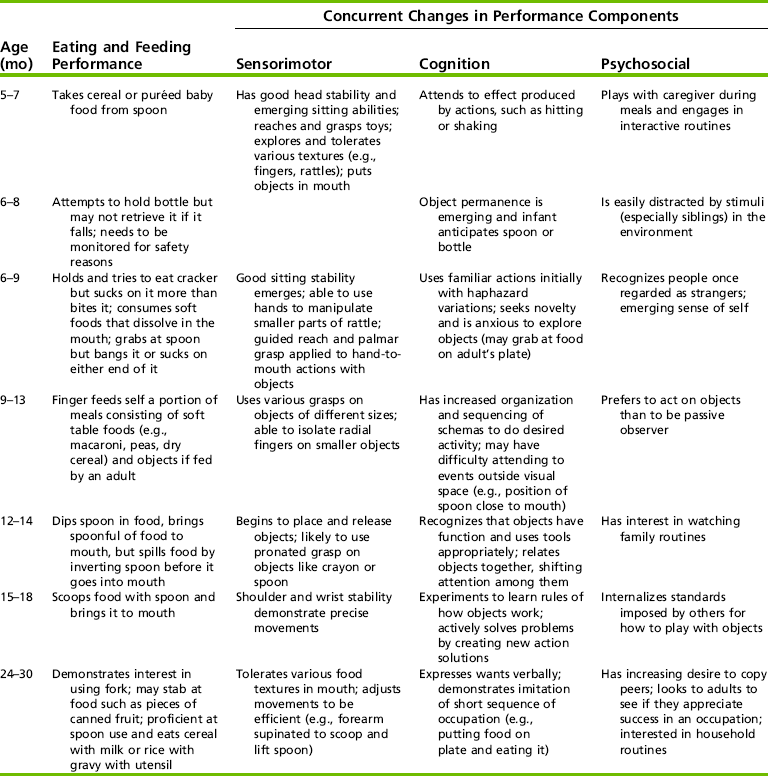



 RESEARCH NOTE 15-1
RESEARCH NOTE 15-1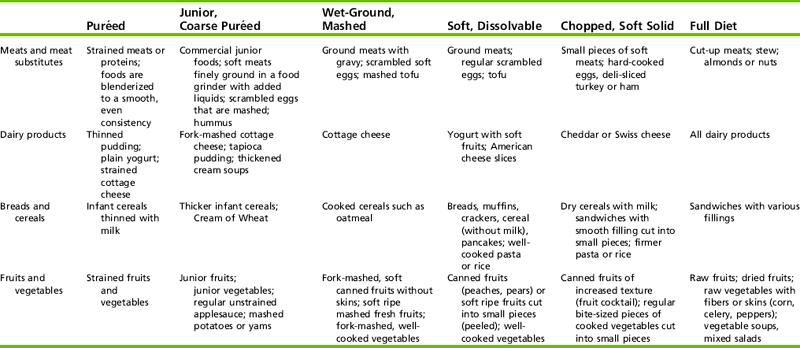
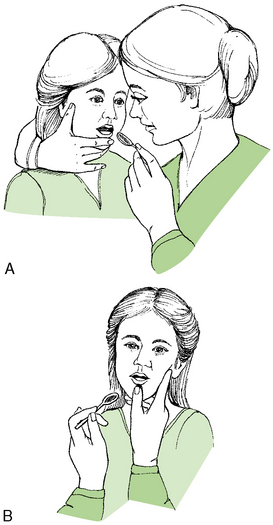

 CASE STUDY 15-1
CASE STUDY 15-1