Mobility
1 Understand the importance of mobility to child development.
2 Apply a mobility assessment model to children with different levels of motor function.
3 Identify alternative methods of mobility appropriate to meet the child’s developmental and functional needs.
4 Describe wheelchair features and designs that meet the needs of children with various levels of motor control.
5 Identify power mobility devices currently available.
6 Describe power mobility assessment and intervention.
7 Describe new technology in assessing seating and positioning and new equipment available to children with unique seating and positioning needs.
8 Explain the biomechanical principles important to positioning and seating.
This chapter presents an overview of the importance of mobility for growth and development and the implications of impaired mobility. Responsibilities of the occupational therapist for evaluating and recommending appropriate mobility devices are emphasized. Guidelines and criteria for selecting mobility equipment are defined, and descriptions of mobility devices are provided. This chapter also describes the importance of positioning and other factors that influence successful use of assistive devices.
Mobility is fundamental to an individual’s overall development and functioning in the occupations of self-care, work, and leisure and is essential to quality of life. The definition of functional mobility includes moving from one position or place to another (e.g., bed mobility, wheelchair mobility, and transfers [wheelchair, bed, car, tub or shower, toilet, or chair]), performing functional ambulation, and transporting objects. Community mobility is defined as moving oneself in the community and using public or private transportation (e.g., driving or accessing buses, taxicabs, or other public transportation systems). This chapter addresses primarily mobility as a means of locomotion, with an emphasis on evaluation and intervention principles.
DEVELOPMENTAL THEORY OF MOBILITY
The newborn has little independent control of any part of the body. Motor and sensory symmetry and midline orientation develop gradually, followed by controlled purposeful movements and the beginning of alternating coordinated movements. The first form of mobility that the infant experiences is rolling, first from side to supine, then prone to supine, and finally in either direction. The 6-month-old infant achieves mobility by pivoting in the prone position. The infant continually becomes more active against gravity (Figure 21-1). Most 8-month-old infants creep and move from sitting to quadruped positioning and back. By the ninth to tenth month, the infant has a strong desire to move upward. First infants pull to stand and cruise along furniture, such as a coffee table; then they hold onto someone or something as they take their first steps. The average age at independent walking is 11.2 months, and most children achieve independent upright ambulation between 9 and 15 months of age.8,14
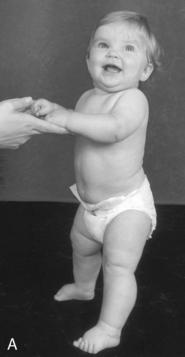

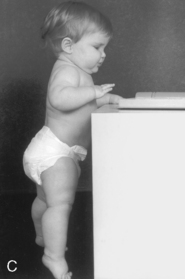
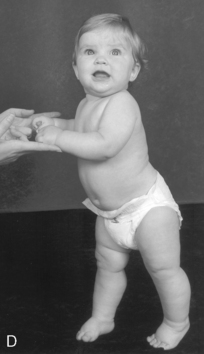


FIGURE 21-1 Development of locomotion. A, Infant bears full weight on feet by 7 months. B, Infant can maneuver from sitting to kneeling position. C, Infant can stand holding onto furniture at 9 months. D, While standing, infant takes deliberate step at 10 months. E, Infant crawls with abdomen on floor and pulls self forward, and then (F) creeps on hands and knees at 9 months. (From Hockenberry, M. J., Wilson, D., & Winkelstein, M. L. [2005]. Wong’s essentials of pediatric nursing [7th ed]. St. Louis: Mosby; photos by Paul Vincent Kuntz, Texas Children’s Hospital.)
With the developmental theory of mobility, developmental theorists accept that physical and psychologic developments are interrelated and that early experiences influence subsequent behavior. “Through their motor interactions infants and toddlers learn about things and people in their world and also discover they can cause things to happen” (p. 18).12 During the first months of life, children seek physical control of their environment and continue to do so by building and enhancing their motor skills day by day.
During the first 4 years of life, the child gains independence through mastery of important life tasks such as locomotion, ability to manipulate, bowel and bladder control, language development, and social interactions. The most fundamental of these, with the widest influence in all spheres of development, are movement about the environment and use of language as a communicative and information processing system.
Children gain various learning experiences as they move about. Locomotion and other motor skills, which develop rapidly during the first 3 years of life, become the primary vehicles for learning and socialization and for the growth of a healthy sense of independence and competence. Piaget viewed self-produced movement as a crucial building block of knowledge. He theorized that the intercoordination of vision and audition with movements, including locomotion, laid the basis for the child’s understanding of space, objects, causality, and self.53 The ability of children to influence their environment and to affect or alter it through their own actions is intrinsically motivating. Early experiences are believed to foster curiosity, exploration, mastery, and persistence, and are therefore important for later intellectual functioning.
IMPAIRED MOBILITY
Children with physical disabilities who have difficulty achieving independent motor control are often deprived of opportunities for self-initiated or self-produced mobility. When these children do experience mobility, it is of a passive nature, as in being held or pushed in a stroller. Because they lack the necessary movements to explore and act on their environment, important learning opportunities are hindered. Mobility-impaired toddlers who cannot move across a room to reach out and touch an object or interact with a person are at a great disadvantage. They cannot experience the sensorimotor and developmental activities of their peers who have achieved upright mobility, such as pushing and pulling toys, opening and closing drawers, or moving around and under objects. Psychologists who have studied normal development have observed improvements in social-emotional, cognitive, perceptual, and motor functioning in infants when they first gain mobility.71 Researchers who have studied the impact of early exploration on a child’s development have also suggested that self-produced locomotion and active choice are important for the development of perception and cognition.13,25,40,64 It appears that young children who actively seek to learn about their environment exhibit higher intelligence and cognitive ability at school age. Young children who at 3 years were high stimulation–seeking demonstrated increased cognitive, scholastic, and neuropsychologic test performance at 11 years.55
“When development along any line is restricted, delayed, or distorted, other lines of development are adversely affected as well” (p. 66).11 Restricted experiences and mobility during early childhood can have a diffuse and lasting influence. Long-term physical restriction during infancy or early childhood can significantly alter and disrupt the entire subsequent course of emotional or psychologic development in the involved child.36 Such deprivation of physical and social contingencies can lead to secondary developmental problems, which are motivational. Infants born with significant motor impairments quickly “begin to lose interest in a world which they do not expect to control” (p. 113).9 This motivational effect is termed learned helplessness, a condition in which the child gives up trying to control his or her own world because of motor disability and diminished expectations of caregivers.23,56 Butler found that children whose mobility is limited during early childhood develop a pattern of apathetic behavior—specifically, a lack of curiosity and initiative.11 These character traits are believed to have a critical influence on intellectual performance and social interaction. The detrimental effects of limited early exploration were identified in a study comparing shortcut choices in a simulated maze of able-bodied teenagers with those of teenagers who had varying histories of mobility impairment. Despite equivalent levels of mobility, participants whose mobility was more limited early in development were poorer in the task than those whose mobility had deteriorated with age. The results suggest that early independent exploration is important in the development of spatial knowledge and that the detrimental effects of limited early exploratory experience may persist into the teenage years.58
In children with severe physical disabilities, newly gained independent mobility can have a positive effect on emotional, social, and intellectual states.20,29 Paulsson and Christoffersen found that children with disabilities using mobility devices became less dependent on controlling their environment through verbal commands, more interested in all mobility skills, and more active in peer activities.52 Butler found that children who had some means of ambulation could and would make choices, but those who did not ambulate were much less likely to exercise available options.10 The lack of ambulation appeared to severely restrict the child’s opportunities to practice decision making, thus giving him or her no reason to express an opinion or desire.
Intervention for young children with physical disabilities often includes the provision of adapted equipment: supported chairs, standers, bath seats, and adapted strollers. This equipment provides a means for properly and safely positioning a child, but it does not provide a means for accessing the environment or experiencing the stages of development that occur with self-initiated mobility. Children who have a means for self-initiated mobility decide where, when, and how to move. It is the responsibility of the occupational and physical therapist to determine how young children with disabilities can access their environment, explore their surroundings, and experience developmentally appropriate activities. Mobility devices, which provide a physically disabled child with a means to access and explore the environment, not only provide a means for mobility but also facilitate psychosocial, language, and cognitive development. Such devices include prone scooters, handheld walkers, support walkers, manual and power wheelchairs, and alternative powered mobility devices. However, professionals lack agreement when and if mobility devices for very young children, particularly support walkers and powered mobility devices, are appropriate.
A support walker differs from a handheld walker in that it typically includes a seat with postural supports pelvis, trunk, and sometimes the head. In the past, therapists were reluctant to recommend support walkers for children with cerebral palsy because they would often use undesirable postures during ambulation, and they believed it might increase the child’s spasticity. However, many support walkers are now designed with features that complement the child’s therapeutic goals (Figure 21-2).49,51,76 In addition, several studies have demonstrated that resistive exercise does not increase spasticity in individuals with cerebral palsy.7,21,26,44

FIGURE 21-2 The Pommel Walker allows an 18-month-old child with a developmental delay to explore his environment. (Available from Freedom Concepts.)
Although further study is needed, at least one study of persons with cerebral palsy concluded that a progressive strength-training program can improve muscle strength and walking ability without increasing spasticity.2
Professionals and third-party payers may resist providing a powered mobility device to a young child with physical disabilities, particularly before the age of 5 years. Indeed, most children born with congenital mobility impairments are not given their first wheelchair until the age of at least 3 years, and most of these do not receive a chair they can propel independently until age 5.27,29 Children with a physical disability under the age of 5 years are often denied the opportunity for using a powered mobility device because they are considered too young to have the cognitive skills to understand how to use it. However, “Clinical experience and research projects have established that powered mobility devices offer children at least as young as 17 months of age a safe and efficient method of independent locomotion” (p. 18).12 Research continues to substantiate the fact that children as young as 18 months can achieve independent skills in powered mobility.27,29
Caregivers often believe that use of a power wheelchair will reduce the likelihood of their child’s achieving independent mobility through ambulation. Research has not demonstrated that use of a powered mobility device prevents or delays the child’s acquisition of motor skills. On the contrary, researchers have found positive changes in children’s development after the introduction of a powered mobility device.46,52,73 During mobility training, children with severe motor disabilities demonstrated improved head control and trunk stability, increased motivation, and greater self-confidence in movement.10 Deitz, Swinth, and White concluded that for some young children with severe motor impairments and developmental delay, use of a powered mobility device may potentially increase self-initiated movement occurrences during free play.19 Nilsson and Nyberg analyzed case studies of preschool children with profound cognitive disabilities participating in power wheelchair training experiences.46 They concluded that the training experiences increased wakefulness and alertness, stimulated a limited use of arms and hands, and promoted the understanding of very simple cause-and-effect relationships.
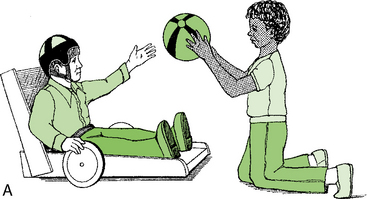
In another study, children 15 months to 5 years of age with physical disabilities who participated in a 2-week mobility exploration day camp demonstrated a variety of positive behavioral changes.73 The children experienced mobility by using the Mini-Bot, a standing powered mobility device, to explore the environment (Figure 21-3). They participated in daily 1½-hour sessions for 2 weeks. Behavioral changes that caregivers and occupational therapists observed in some children included increased eye contact, increased verbalization and communication, improved sleeping patterns, increased active arm use, and a more positive disposition.

FIGURE 21-3 The Mini-Bot provides early, exploratory, self-initiated mobility experiences. A 2-year-old child with arthrogryposis stands and moves in the Mini-Bot using a joystick or switches. (Manufactured by Innovative Products, Inc.)
The current trend is for mobility devices to be recommended at young ages, when typical children are first ambulating. Many professionals believe that if self-initiated mobility does not occur in the first year, the use of devices for mobility should be considered. Mobility appears to be a priority issue for children with disabilities and others in their environment. When researchers surveyed the occupational performance needs of school-age children with physical disabilities in the school system and community, most teachers, parents, and children identified mobility as their greatest area of concern.54 However, it can be a challenging task for a therapist to suggest consideration of a mobility device, particularly a power wheelchair, to the family of a young mobility-impaired child. Many caregivers consider the suggestion as a symbol of giving up hope for independent ambulation. For this reason, use of a walker, support walker, or alternative powered mobility device may be more accepted by the families of very young children. The therapist must convey to the family the concept that all children need a means of mobility to access the environment for exploration to encourage development in the visual perceptual, language, social, and cognitive domains. The mobility device is intended to assist the child in achieving independence in exploration until and if another method is acquired.
AUGMENTATIVE MOBILITY
Butler introduced the term augmentative mobility to describe all types of mobility that supplement or augment ambulation. “Given augmentative mobility, disabled children can experience more success in directly controlling their environment, thereby reducing or avoiding secondary social, emotional and intellectual handicaps” (p. 18).12
The concept of augmentative mobility for functional mobility can be expanded to include transitional mobility. Transitional mobility allows the child to use a mobility device to have self-initiated movement without the expectation that it must be functional. The child may not consistently move the mobility device in a desired direction but uses it as a means for exploring the effects of movement and learning how to move. The therapist can best provide transitional mobility by allowing the child to move the device in a large room with open space where the child is free to explore. These experiences can then help the child make the transition to a more functional level of purposeful mobility. Not all children are able to achieve functional mobility; in these instances, transitional mobility remains an important means for the child to explore the environment.
The team must consider several factors before selecting the type of mobility device that is appropriate for a child. These factors include the purpose or goals for using the device, environments for intended use, and the child’s physical and psychosocial abilities and limitations. When selecting a mobility device, the team considers the advantages and disadvantages of the device, the modifications that may be needed for comfort and control, the congruence to intervention goals, and the cost-benefit ratio. Ideally, a mobility-impaired child should have more than one type of mobility device for use in indoor and outdoor environments. Any methods that are chosen for mobility require close cooperation among all professionals working with the child and family.
ASSESSMENT AND INTERVENTION
Classification of Mobility Skills
Children’s mastery of functional mobility skills has been classified and categorized in several ways. Hays examined current existing diagnostic conditions of children without locomotion and divided them into four functional groups34:
1. Children who will never ambulate. This category includes children with cerebral palsy with severe involvement and spinal muscular atrophy types I and II. Generally, these children have no opportunity for independent mobility.
2. Children with inefficient mobility who ambulate but are unable to do so at a reasonable rate of speed or with acceptable endurance. This category includes children with cerebral palsy with less involvement and myelomeningocele with upper-extremity involvement. For these children, assisted mobility may provide an efficient means of mobility above that which they are capable of producing themselves. Warren uses the term marginal ambulators for this group.70
3. Children who have lost their independent mobility. This category includes victims of trauma and children with progressive neuromuscular disorders. The developmental implications may be less critical than in the first two groups, and the issue is acceptance of assisted mobility as an adaptation to the acquired disability.
4. Children who temporarily require assisted mobility and often progress to independent mobility with age. This category includes many children with osteogenesis imperfecta and arthrogryposis. Functional considerations in this group are both developmental and practical.
There are significant differences among these groups that may have implications for mobility and its integration into the child’s overall concept of disability, as well as for evaluation and intervention. Group I children may achieve independent mobility through the use of a support walker and power wheelchair. Group II children may be able to independently propel a manual wheelchair, ambulate in a support walker indoors, and use a power wheelchair for community mobility. Children in groups III and IV will use a variety of mobility methods during the transition period.
Mobility Assessments
Evaluation of children has traditionally focused on the achievement of developmental milestones. Occupational therapists have discussed the limitation of such evaluations because underlying impairments (e.g., motor control deficits) cannot fully explain the extent and form of functional difficulties seen in children with disabilities.17 Furthermore, the tasks that are most relevant for daily independence in mobility function have not been well defined in traditional developmental milestone tests. Using a top-down evaluation process, the therapist focuses on what the child needs or wants to do, the context in which he or she typically engages occupations, and the limitations that he or she may experience.17,24 Therapists assess underlying performance abilities only to the extent that is needed to help clarify the possible sources of limitations in occupational performance. In mobility evaluation, occupational therapists focus on the child’s overall pattern of locomotion and transfer skills in relation to a particular performance context.
Two instruments that evaluate children’s functional abilities, including mobility, are the Pediatric Evaluation of Disabilities Inventory (PEDI)32 and the Functional Independence Measure for Children (WeeFIM).68 The PEDI rates two dimensions of performance: ability to perform functional skills and the level of caregiver assistance needed. The functional mobility subscale measures basic transfer skills (e.g., getting in and out of a car) and body transportation activities (e.g., walking up and down stairs). WeeFIM is based on the Functional Independence Measure (FIM) and is for children from 6 months to 7 years of age. This scale measures the child’s independence in mobility: transfers, locomotion, and stairs and provides useful information for progress assessment, program planning, and communication with caregivers.
The Canadian Occupational Performance Measure (COPM)42 is a semistructured interview that focuses on the identification of problems in self-care, productivity, and leisure. It provides a framework to help clients articulate the difficulties they are encountering in their daily lives and appears to be responsive to change after occupational therapy intervention.42 In the case of mobility, the COPM can address the concerns of children and caregivers, help them identify what is important to them, and help them prioritize goals. The COPM also provides a baseline assessment for measuring outcomes on reassessment.
Tefft, Furumasu, and Guerette, at the Rehabilitation Engineering Research Center on Technology for Children with Orthopedic Disabilities at Rancho Los Amigos Medical Center, developed a cognitive assessment battery and a wheelchair mobility training and assessment program to help clinicians determine a young child’s readiness to drive a power wheelchair.61,62 The Pediatric Powered Wheelchair Screening Test (PPWST) and the Powered Mobility Program (PMP) were developed and validated for children ages 20 to 36 months with orthopedic disabilities who used a joystick to control the wheelchair.30,31 Through this research, the cognitive domains of spatial relations and problem solving were found to be significant predictors of power wheelchair mobility performance.63 The research team continues to study the validity of the assessment battery for children, with neurologic conditions such as cerebral palsy, who use a joystick or switches to drive power wheelchairs.
Occupational therapists evaluate several components of performance (e.g., motor, perceptual, and cognitive factors) that influence mobility. Human functions important to mobility include neuromotor status (vision, hearing, and seizure disorders), orthopedic conditions, and psychosocial variables. Therapists also consider both chronologic and developmental age and the child’s environments. The therapist must make the mobility devices and positioning system available during the evaluation process so that the child and the caregivers have an opportunity to gain experience using potential mobility devices. These trials provide the caregivers and the child with information and experience that will assist them in becoming informed consumers and full participants in deciding which mobility device best meets their needs.
Mobility Evaluation Team Models
Selection of the most appropriate positioning and mobility device requires the skills of a therapy team working in close collaboration with the school team, prescribing physician, child, parent or caregiver, and assistive technology professional (ATP). The ATP is “a service provider who analyzes the needs of individuals with disabilities, assists in the selection of the appropriate equipment, and trains the consumer on how to properly use the specific equipment. This equipment may include manual and power wheelchairs, alternate computer access, augmentative and alternative communication devices, and other technology to improve the function and quality of life for an individual with a disability” (resna.org). The ATP is credentialed through the Rehabilitation Engineering and Assistive Technology Society of North America (RESNA). Occupational and physical therapists who make recommendations for assistive technology equipment often seek an ATP credential. This organization also provides certification for a Rehabilitation Engineering Technologist (RET) who designs, customizes, and modifies assistive technology (AT). The ATP is responsible for maintaining updated knowledge of available equipment and assisting in identifying choices of mobility devices according to the features that the child requires to use it optimally.
The physical or occupational therapist, together with the child and family, determines the needs of the child and establishes goals to identify the features and options in a mobility device or devices that will meet the desired outcomes and assist the family in setting appropriate functional goals and expectations for using the mobility device. The therapist is responsible for assisting the family in becoming informed consumers who can make decisions regarding a mobility device. Once the mobility device is selected and provided to the family, the therapist is responsible for periodically reevaluating the fit and function of the device to determine if it meets the stated goals and objectives.
Most funding agencies do not approve replacement of a mobility device, such as a wheelchair, within 3 to 5 years of the purchase date. If the equipment is not appropriate, the child and family may not have another option for several years. The limitations in reimbursement become critical when a misunderstanding during the evaluation or ordering process results in a device that does not meet the predetermined outcomes. It is imperative that the therapist, ATP, and family immediately decide how to best resolve these issues.
The occupational therapist selects among a variety of mobility evaluation models to evaluate a child for a mobility device. The most common is for the therapist to request a local supplier of durable medical equipment or ATP to bring the device under consideration to the therapy session. The ATP offers input about what features and options are available on the device and how to adjust it properly. The difficulty encountered with this model is that one supplier typically has a limited selection of devices available for demonstration, so only one device may be evaluated at each session. Therefore, the therapist does not have the opportunity to compare the child’s performance in various types of mobility devices. Without direct comparison of the mobility devices, decisions about which devices are optimal for the child are difficult for the therapist to make. The decision is less risky when side-by-side comparisons of different devices are available during the evaluation. This method enables evaluation of performance with each mobility device under consistent child and environmental conditions.
Several AT centers and rehabilitation engineering centers throughout the country use a multidisciplinary team approach and side-by-side evaluation methods to assess seating and mobility needs, particularly with individuals who have severe disabilities. The teams consist of occupational therapists, physical therapists, rehabilitation engineers, speech pathologists, RETs, and ATPs working with the child’s therapy team, school team, physician, and family. These centers offer the advantage of being able to consider all the needs of the child and offering a concentrated level of expertise.
MOBILITY DEVICES
Selection of a specific type of a mobility device depends on several factors. The therapy team must first decide on the purpose for using the mobility device or devices. Does the child need a means for exploring and accessing the environment (self-propelled manual, power wheelchair, or hands-free support walker) or do the caregivers need a convenient way to transport the child (stroller or manual wheelchair)? The next, most critical aspect of evaluating a mobility device is to consider the environments in which it is to be used by the child and caregivers. If the child’s home has high pile carpet, propelling a manual wheelchair or using a walker with wheels smaller than 5 inches in diameter will be quite difficult. The force needed to move a wheelchair over various surfaces has been measured. Using concrete as the baseline, the increase in force needed to cross each surface is 3% for linoleum, 20% for low-pile carpet, and 62% for high-pile carpet.1 The effort required by the individual to use the device will affect functional performance. If the mobility device is too complicated or the child must exert too much effort, it will not be used.
The occupational therapist must consider the features, adaptations, and hardware options needed for optimal use across all environments such as school, home, and community; the system must not reduce performance in functional activities such as eating, personal hygiene, transfers, and augmentative communication. Also important to consider are the needs and concerns of the caregivers and school personnel who will be transferring the child into and out of the device, transporting it, maintaining the equipment, and the costs versus benefits.
The occupational therapist must use the skills of an investigator during the mobility assessment process. Thoughtful planning and careful analysis of person-device-environment fit are necessary for the therapist to ensure that the child and family receive the optimal device. When a device is ordered without a comprehensive mobility evaluation, the child may end up with a wheelchair that will not fit into the family van with the user in it, tips over when the augmentative communication device is mounted on it, cannot be self-propelled outside because the family lives in a hilly area, or is too large to maneuver efficiently in the classroom environment. Case Study 21-1 provides an example of a child whose need for a mobility device—a support walker—was not evaluated properly.
Alternative Mobility Devices
Tricycles (Figure 21-4) are a means for mobility, although third-party funding is typically not available because tricycles are not considered a medical necessity. However, they can provide community mobility outdoors and on playgrounds. Many types of tricycles are available with adaptations, such as trunk supports, and hand-propelled models are available for children who do not have the ability to pedal with their legs (e.g., children with spina bifida). A unique and helpful feature for both the child and the care provider is a handle at the back of the Freedom Concepts tricycle, which enables the adult to steer the front wheel while the child pedals. This assists a child with limited upper extremity function who may not have the ability to hold onto the handle bars to steer the tricycle.
Prone Scooters
Prone scooters (Figure 21-5) require use of the arms and the ability to lift the head while moving. The advantages of using a prone scooter include access for participating in play activities on the floor, the ability to get on and off independently, and the ability to change direction more easily than with other types of manual mobility devices. Disadvantages include fatigue from maintaining neck and back extension, vulnerability of the head to hitting objects, the possibility of the hands getting caught in the casters or rubbed on rough surfaces, and difficulty viewing the environment above the ground level. Children with spina bifida may find the prone scooter functional because they have the upper extremity function and strength to propel it and the scooter can support their legs.
Caster Carts
Caster carts offer another means of mobility to children with upper-extremity function (e.g., those with spina bifida) (Figure 21-6, A). Children can use caster carts indoors or on flat outdoor surfaces. Some children may be able to transfer on and off independently because of the close proximity to the floor. The device requires a considerable amount of energy expenditure for propelling long distances because of the small diameter of the wheels. Children with lower-extremity muscle contractures or tightness, such as in the hamstring muscles, may find it difficult to sit comfortably and securely because they are often unable to tolerate long-leg sitting. These children may feel more comfortable with a triangular-shaped wedge placed under the knees to support their legs in knee flexion. A battery-powered scooter from Enabling Devices allows a child to move either in a circular motion with one switch input or in all directions using several switches or a joystick (Figure 21-6, B).
Aeroplane Mobility Device
The aeroplane mobility device was designed by an occupational therapist for children with cerebral palsy who can move their legs but need support of the upper body (Figure 21-7). The device provides developmentally appropriate positioning, particularly for children with spasticity, because the child is positioned with hip abduction and extension with knee flexion, and the upper extremities are in a weight-bearing position. This position often assists in reducing undesirable posturing in children who have spastic cerebral palsy, especially for children who exhibit extensor posturing in standing. Other advantages include ease in viewing the environment, the handmade nature of the device, and acceptance by parents, because it looks like a toy rather than an assistive device. The aeroplane mobility device is not available commercially but can be fabricated from wood. Disadvantages include lack of adjustability for growth, difficulty turning and moving backward, and heaviness.
Mobile Stander
If a child has upper extremity function to push and maneuver wheels, a mobile stander may provide another means for mobility. These devices allow the child to experience lower extremity weight bearing in a standing position. The child achieves mobility using large hand-held wheels for self-propulsion (Figure 21-8, A). If the child is unable to propel the wheels independently or functionally, but would like to achieve mobility in standing, a joystick-operated motorized stander such as the Standing Dani can provide mobility (Figure 21-8, B).
Walkers
Children who have the ability to pull to a standing position, maintain a grip on a handle, and steer with their arms may be able to use a hand-held walker. These walkers are designed for use either in front of (anterior walker) or behind (posterior walker) the child (Figure 21-9, A). Children with mild to moderate cerebral palsy or lower levels of spina bifida with leg bracing most commonly use hand-held walkers. Walkers can have three or four wheels and are available in various wheel sizes. The smaller the caster, the more difficult it is for use outdoors and over uneven surfaces. Posterior walkers are available with a feature in which the casters lock when the walker is pushed backward. This feature enables the child to stand and lean against the walker or the seat during rest periods. However, this feature makes maneuvering the walker more difficult because the child cannot move the walker in a reverse direction, which is needed when backing away and turning, without lifting it up to overcome the anti-rollback mechanism. Casters can be fixed rather than swiveled, which allows movement only in the forward direction so the user must lift the walker to turn it. Swivel casters allow the child to turn the walker without lifting it, but this feature requires more postural control from the child to direct the walker. The advantages of hand-held walkers are their low cost and convenient transportability. The disadvantages for some users include poor body alignment when pushing a walker and the fact that the hands are not free for performing tasks.



FIGURE 21-9 Walkers. A, The Crocodile posterior walker is designed for children from 2 to 14 years of age. (Manufactured by Snug Seat.) B, A young child helps with chores while using the Walkabout, a hands-free, weight-relieving walker. (Manufactured by Mulholland Positioning Systems, Inc.) C, A 2-year-old boy with spastic cerebral palsy uses the Pommel Walker in a forward pitch position, with a widely padded seat and a tray and hand grip to provide upper body support while pushing a toy vacuum. (Manufactured by Freedom Concepts.)
Support walkers are designed for children who have some ability to move their legs reciprocally but need support at the pelvis, chest, and possibly the upper extremities and head. It is critical to identify the purpose for using the support walker and in which environment it is to be used, to achieve maximum benefit for the child. If the purpose of the support walker is to provide self-initiated mobility for a child to access the indoor home environment, allowing the child to reach objects and people, then features should include wheels that are a minimum of 5 inches in diameter, which move more efficiently over carpets and thresholds than smaller wheels, and a design that does not include hardware, arm troughs, or a tray in front of the child, which would limit the ability to reach during exploratory activities (Figure 21-9, B). However, children with limited arm and hand function as a result of hypotonia or spasticity may require modifications to the support walker such as a tray, which limits getting close to objects and people, but encourages spatial awareness through movement (Figure 21-9, C).
Decisions regarding available options and features on a walker are made based on the child’s physical function and the environment. Selection of appropriate features and adjustments that provide optimal positioning will increase functional use of these types of walkers. Children who adduct or scissor their legs as a result of spasticity may propel the walker more efficiently if a wider and longer padded seat is provided to reduce adduction and maintain leg alignment during ambulation. A young child with hypotonia or weakness may be more successful using a lightweight walker with all swivel casters over smooth flat surfaces such as linoleum (see Figure 21-2). Adjustable posterior tilt, a feature that positions the child slightly behind vertical, may also assist a weak child in maintaining an upright trunk and head position. Children with spastic cerebral palsy may need to be tilted in a slightly forward lean position, which along with a properly positioned pelvis (in neutral or anteriorly tilted position) assists in placing the feet behind the pelvis and trunk, thereby making it easier for the child to initiate movement in a forward direction. If the pelvis is not positioned optimally, the child’s feet may move in front of the pelvis, allowing the child to only be able to push backwards.
Support walkers can provide children with the opportunity to explore their environment in an upright, hands-free position while providing capability for active range of motion. Therapists are being encouraged to promote more activity in children with cerebral palsy by using mobility-enhancing devices.18 However, many support walkers have limitations in maneuverability, particularly indoors, because they require a large turning radius. The KidWalk is a new type of mobility system designed by an occupational therapist to promote use of the upper extremities during exploration.51 It is designed with minimal hardware in front of the child so the child can use self-initiated mobility to be within arm’s reach of people and objects to access and explore the environment and perform developmental activities such as pushing, pulling, opening and closing drawers, reaching, and carrying objects to achieve occupational therapy goals. The KidWalk allows a high degree of maneuverability, particularly over carpeted surfaces and thresholds, because of the placement of a large wheel located at the vector of the child’s body, which also encourages rotation of the upper body over the pelvis, a more desirable movement. It incorporates a mechanism for weight shifting during ambulation and a dynamic swivel seat to encourage reciprocal leg movements and does not depend on upper body function to maneuver it. The upper body supports can be removed as the child develops balance and control.
Alternative Powered Mobility Devices for Young Children
A variety of alternative powered mobility devices are available for children who cannot achieve self-initiated mobility using reciprocal leg movements or by pushing large wheels. Motorized toy vehicles are available for children to provide early mobility experiences using a joystick; adapted models with special electronics for using up to four switches are also available. From the caregiver’s perspective, the greatest advantage for use of these toy vehicles is that they look like a toy that any other child would use, rather than an assistive device. They are also an option for providing a child with the opportunity to learn how to drive a motorized device in preparation for using a power wheelchair. Disadvantages include difficulty using these vehicles indoors because of limited maneuverability; large size, which prevents the child from getting close to objects in the environment for reaching, exploring, and interacting with others; and sometimes noisy operation.
The MiniBot and the GoBot were developed by an occupational therapist (see Figure 21-3).74,75 Each is a powered mobility device designed to enable physically challenged preschool children from 12 months to about 6 years of age to move in an upright position and explore the environment by getting close enough to objects and peers to reach and touch. It is intended for transitional mobility indoors or for use outdoors on flat surfaces. The child can be positioned in either a standing, semi-standing, or seated position. A joystick or multiple switches can be positioned at any location at which the child can reach the controls for driving the device. The MiniBot is not a power wheelchair; it is a therapeutic and educational tool intended to provide developmental opportunities equivalent to those experienced by able-bodied peers, such as pushing or pulling toys, kicking balls, moving quickly, moving slowly, and problem solving. The MiniBot is intended to increase the child’s opportunities for hands-free exploration and provide new sensory experiences (particularly vestibular, visual motor, and spatial relations). The MiniBot is intended for children who would otherwise spend their early developmental years passively sitting in a stroller or manual wheelchair.
WHEELED MOBILITY SYSTEMS
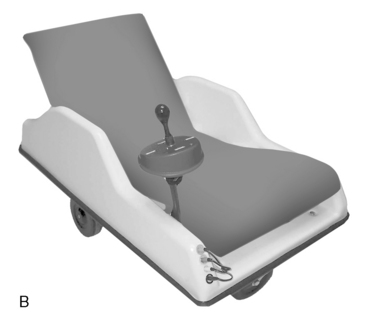
Wheeled mobility systems include dependent mobility systems, independent manual mobility systems, and independent powered mobility systems. The first mobility system most children acquire is a stroller, which is considered to be a dependent mobility system because the user is depending on others for mobility. Parents often prefer the ease of use of a stroller and feel the appearance is more acceptable than that of a wheelchair when the child is very young.15 A young child may be able to use a standard infant stroller, but if the seat does not provide supportive positioning, then a seating insert designed to provide support at the pelvis and trunk, such as the KidSert or Sit-to-Go, should be considered (Figure 21-10, A). Mobile positioning systems, which provide more support than a stroller, while still being lightweight and easily foldable, are available through durable medical equipment providers. Some of these models, such as the Convaid Mountee, include bus or van anchors for transporting the child in a vehicle (Figure 21-10, B).
Other dependent seating and positioning systems offer an adjustable height chassis to position the child close to the floor or up to various table heights (Figure 21-11). The seating system is fully adjustable by the therapist to accommodate the needs of a variety of users so a custom seating system is not necessary. Dependent mobility systems can provide convenience for care providers and teachers, as well as optimal positioning for function. The seating system can also be removed on some models to transfer the seat to another type of base such as an outdoor base. The greatest disadvantage of a dependent mobility system is that the child must depend solely on others for mobility and has no means for self-initiated mobility and exploration. Dependent mobility systems that can be retrofitted into a larger wheel base should be considered if the team believes that the child will be able to self-propel within the next few years. Peers may also perceive an older child with a disability who uses a dependent mobility system such as a stroller, as being less able and less approachable than a child of similar age who sits in a wheelchair.
Manual Wheelchairs
Independent manual mobility systems include manual wheelchairs that allow the user to move independently by pushing two large wheels. A manual wheelchair is appropriate for a child who has the ability to functionally and efficiently propel it. It is also used as a means of transportation by caregivers or as a backup wheelchair when the child’s power wheelchair is not working. Great strides in design and material selection have resulted in lighter frames than the standard 35-pound wheelchair (Figure 21-12, A). Weights can range as low as 14 pounds for lightweight, ultra-lightweight, and high-performance manual wheelchairs.41 Manual wheelchairs for playing court sports such as tennis and basketball or racing are designed specifically for the sport.16 These wheelchairs have a rigid frame and a high degree of camber in the rear wheels, and use small rollerblade-type casters in front.

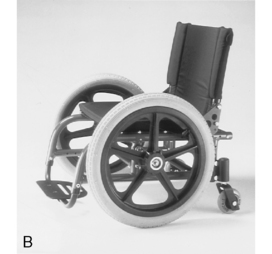



FIGURE 21-12 Manual wheelchairs. A, Chelsea, age 9 years with paraplegia at the L1 level, selects a TiLite TR for its features of lightweight, durability, and smooth ride. (Courtesy TiLite.) B, Quickie Kidz manual wheelchair features wider rear wheels for maximum pushing surface so that the chair can be propelled with either a push or pull motion. (Courtesy Sunrise Medical, Carlsbad, Calif.) C, Quickie Xtender provides power assist to a manual wheelchair by designing a motor unit into the hub of the quick release wheel. (Courtesy Sunrise Medical, Carlsbad, Calif.) D, The LEVO KID wheelchair provides a sit-to-stand feature in a manual wheelchair with the touch of a button. (Available through LEVO USA, Inc.) E, Kids ROCK wheelchair. (Manufactured by ART Group, a division of Sunrise Medical, Carlsbad, Calif.)
Wheelchairs with large rear tires are most common, but models with large front tires and small back casters are available (Figure 21-12, B). Propelling a wheelchair with large front tires may be more efficient for the child because more surface area of the tire is exposed for gripping the wheel and pushing. However, the large front tires can limit access to the environment, such as when transferring and sitting at tables. The wheelchair with large front tires is also more difficult to push over curbs and uneven surfaces because of interference from the rear casters.
If the user has a single functional arm for wheelchair propulsion, such as a child with hemiplegia, an adapted manual wheelchair with a one-arm drive feature can provide independent mobility. The wheelchair is designed with two rims on the wheel the child uses to propel. One of the rims is connected through an axle to the other wheel. If either rim is pushed separately, it turns the wheelchair. If both rims are pushed simultaneously, the wheelchair moves forward or backwards. A manual wheelchair can also be propelled with the feet if the wheelchair has a low seat-to-floor height, known as hemi-height.
A power assist unit, designed into the hub of a special wheel attached to a manual wheelchair, provides the convenience of a manual wheelchair without the extra effort involved with propulsion (Figure 21-12, C). The LEVO Kid wheelchair includes a powered sit-to-stand feature, which can provide peer height interaction and the benefits of convenient standing throughout the day (Figure 21-12, D).
A new concept in mobility systems is the Kids ROCK active wheelchair, which provides dynamic seating for children with movement disorders such as children with cerebral palsy who posture into extension and find it difficult to be functional in a static seated position. The Kids ROCK active wheelchair allows the wheelchair seat to move when the child moves but maintains proper postural alignment and assists in reducing sacral sitting. When the child moves using hip and knee extension, the backrest reclines and the footrests move in an upward direction extending in a 35° range. When the child relaxes, the compressed springs move the backrest and footrests to the starting position (Figure 21-12, E).
Power Wheelchairs
Powered mobility wheelchairs have a motorized unit that the user operates by means of a joystick or alternative controls such as pneumatic sip-and-puff, ultrasonic head controls, proximity switches that operate by the user moving close to the switch but not touching it, or multiple push switches. If a child cannot propel a wheelchair long distances at the same speed and efficiency as demonstrated by the average person walking, then the therapist should consider recommending a power wheelchair to increase the child’s independence and function. The advantages of a power wheelchair over a manual are increased speed capability, ease of maneuvering, and less energy expenditure required for moving, particularly for long distances. Some children who use a power wheelchair also have a manual wheelchair for use in environments that are not accessible to a power wheelchair or when the power wheelchair is being repaired.
Power wheelchairs are available in several styles with various options and are differentiated by the placement of the drive wheel, which may be mid-wheel (Figure 21-13, A), front-wheel (Figure 21-13, B), or rear-wheel drive (Figure 21-13, C). Attributes that are affected by the drive wheel position include maneuverability, stability, traction, and performance (speed, efficiency, obstacle climbing, and crossing a side slope). Maneuverability depends on the turning radius. Mid-wheel drive wheelchairs tend to have greater maneuverability because of the smaller turning radius.37 Some mid-wheel power wheelchair manufacturers claim to have a 19-inch turning radius, versus a minimum 33-inch radius with a rear-wheel drive. However, mid-wheel drive wheelchairs require a third set of stabilizing caster wheels, which may extend up to 17 inches behind the user. This feature may make it difficult for users to turn around without catching the casters on objects, particularly if spatial awareness is not optimal.



FIGURE 21-13 Power wheelchairs. A, Q610. B, Permobil 450. (Courtesy of Permobil, Lebanon, Tenn.) C, Skippi power wheelchair. (Manufactured by Otto Bock.)
Front-wheel drive works well over various types of terrain, uphill and downhill, because the power in front wheels pulls the user over obstacles. Children who have used a rear-wheel drive wheelchair may find maneuvering a front-wheel drive wheelchair more challenging because the back end of the wheelchair may fishtail at higher speeds. The recent trend in power wheelchair design is to provide a full suspension system in the front and rear casters or tires. This allows the user to move over a variety of terrains and drive up 3-inch curbs, even at slow speeds.
Standard rear-wheel drive wheelchairs are optimal for children who have limited vision and spatial awareness difficulty, because most of the wheelchair hardware is within their field of vision. Most wheelchair manufacturers provide a choice of several models that are intended for joystick operation and models that include sophisticated microcomputer electronics for alternative input methods for driving and for remotely operating environmental devices. Features of power wheelchair electronics can accommodate the needs of various users. Such features include adjustments for torque, tremor damping for children having difficulty directing the joystick, a short-throw joystick option for users with muscle weakness who do not have the strength to push the joystick to its end range, speed adjustments, and acceleration settings so that the wheelchair can be set to increase speed rapidly or gradually. Some manufacturers now offer electronics, such as the True Track Technology (Invacare Corp.), that enable the wheelchair to track straight on slopes and uneven surfaces. Speeds can be as high as 15 mph, but typically range from 3 to 10 mph. Distance traveled on one battery charge can be as far as 25 miles.
Several features can be made available on power wheelchairs to increase a child’s function and level of independence. Technology-dependent children who require oxygen support can become mobile by using portable ventilator carts attached to the wheelchair.5 Another useful feature for accessing the environment enables the child to independently move from a sitting to a standing position and drive around while standing (Figure 21-14, A). A powered elevating seat, which raises the child to various heights for greater accessibility in the environment, is also available (Figure 21-14, B). Additional features include power tilt-in-space, which tilts the seat backward to about 45° while maintaining the same seat-to-back angle (Figure 21-14, C), and power recline, which places the child in the supine position by reclining the back of the chair. These two features are useful for individuals who need frequent relief of pressure under their buttocks, such as those with spinal cord injury and muscle weakness or for those with hip, back, and neck pain.



FIGURE 21-14 Useful features for a power wheelchair. A, The Chairman 2 K Stander. Standing can be achieved from a sitting position or gradually from supine. B, K450 from Permobil Playman Robo’s seat will lower to the ground and elevate, covering a total of 25 inches height difference for vertical mobility. (Lebanon, Tenn.) C, Permobil K300 PS Jr. with tilt. Chairman 2 K front- wheel drive power wheelchair with the Corpus seating system and 45° of tilt in space. (A-C, Courtesy Permobil, Lebanon, Tenn.)
Power wheelchairs are typically controlled with a joystick. A proportional joystick allows the driver to increase acceleration and speed of the wheelchair in relation to the distance the joystick is moved. The farther the user pushes the proportional joystick, the more rapidly the wheelchair moves. A non-proportional joystick (digital or microswitch) does not affect the wheelchair’s speed; any amount of force used to push the joystick results in the same speed. An attendant joystick is another option for a power wheelchair. It is typically a small joystick mounted to the back of the wheelchair and is accessed by the caregivers who need to drive the power wheelchair when accuracy is required, such as moving up a narrow ramp.
Power wheelchairs do not typically fold for transporting in a vehicle. Accessible vans that have been modified with a lift are required for transporting the user and power wheelchair in a vehicle. However, there is a pediatric power wheelchair, the Skippi from Otto Bock, that can be disassembled so that it can be transported in a vehicle without the need for a van (see Figure 21-13, C). If the child can be transferred to a car seat, a covered trailer can be hitched to the back of a vehicle for transporting a power wheelchair.
Three-wheeled scooters are another option for powered mobility. The individual who uses a scooter typically has good sitting balance, requires minimal positioning adaptation, and can understand and physically operate the tiller handle bar controls.
A manual wheelchair can be converted to a power wheelchair by purchasing an add-on unit that includes two motors that are placed on the tires to rotate them, batteries, an electronic control unit, and a joystick. The electronic controls for the add-on units are not as sophisticated or adjustable as those found on standard power wheelchairs. This makes it more difficult for some children with impaired motor responses to accurately operate the chair. Add-on units are also not highly recommended for individuals who use their wheelchairs outdoors and over rough terrain because they are not designed to withstand the forces that a power wheelchair must endure.
The power wheelchairs today offer sophisticated electronics that provide opportunities to integrate mobility with augmentative communication devices and electronic aids to daily living (EADLs) so the child can turn on lights, operate the television, and access a computer through the power wheelchair electronics.
Selection of Wheelchair Features
If a child will be independently propelling a manual wheelchair, it is critical that the wheelchair and seating be designed to allow use of proper biomechanics for efficient propulsion. The therapist achieves this by selecting the proper size of wheelchair frame and an appropriate seating system. Most wheelchair manufacturers include wheelchair growth kits, which accommodate the need to widen or lengthen the frame without entirely replacing the wheelchair. The therapist must select a wheelchair that fits the child’s present needs, rather than a wheelchair that is too large with the goal that the child will “grow into” it. A wheelchair that is too wide is more difficult for the child to propel. If the seat is too long, the child’s pelvis cannot achieve a neutral position; it will be pulled into a posterior tilt, reducing upper extremity function and causing the child to sit on the sacrum with a rounded back, which contributes to the risk of sliding out of the seat.
The therapist simultaneously considers what type of seating or positioning system is needed and how it will interface with the mobility base for optimal function and performance. For example, in ordering a seat cushion, the child’s functional mobility skills, the frame size of the manual wheelchair, and the desirable seat to floor height must be considered. If the cushion is placed on top of the wheelchair frame, the child may be positioned too far from the wheels for reaching and propelling them efficiently. To prevent this situation, the therapist will need to consider the height of the wheelchair seat when ordering the cushion; a workable alternative in this instance is a narrower cushion that can be recessed into the wheelchair frame.
Another common situation that reinforces the need to assess seating and wheelchair mobility simultaneously is recommending a backrest cushion for a child without considering the features of the wheelchair. The cushion may position the child too far forward of the axle’s wheel. If the child’s center of gravity is forward of the rear wheels instead of directly over the rear wheel axle, propulsion is more difficult and inefficient. Many wheelchairs have a standard axle plate where the hub of the wheel is mounted to the frame and the wheels cannot be relocated within the child’s reach. However, if the therapist recommends an adjustable axle plate for the wheelchair in combination with the appropriate front caster size, the wheels can be relocated and mounted in the best location for the child to reach the wheels for propulsion.
Wheelchair features are recommended based on needs in the areas of mobility (being able to reach and propel the wheels of a manual wheelchair or reach the floor to propel with the feet), accessibility (moving through doorways, maneuvering in small spaces, and fitting under tables), transfer techniques (dependent or independent), seating and positioning, communication (which may include mounting a speech-generating device to the wheelchair), and transportation (if the child will be transported while sitting in the wheelchair; in a motor vehicle certain transportation options will need to be included on the wheelchair). The features available in a manual wheelchair that may affect the child’s posture and function include the ability to mount an appropriate seating system and options such as tilt-in-space, recline, and capability for multiple axle positions for adjusting the wheel location.
Wheelchairs are available in standard or custom sizes as measured by the seat width and depth, height of the seat from the floor, and backrest height. The therapist must carefully consider features and options on wheelchairs and select the wheelchair to accommodate the child’s growth and physical and functional needs as well as the needs of the caregivers. The therapist should begin selection of a wheelchair by evaluating and documenting the child’s current physical and functional abilities, with consideration of physical changes that may occur and the positioning and mobility goals for the child. Wheelchair selection depends on the type of seating and positioning system the individual requires. For example, if a child needs to sit with a medial thigh pad or abductor to keep the knees apart, then a wider space between the leg rest hangers will be required. Wheelchairs are typically designed with equal clearance between the footrest hangers, but some models have a narrower, tapered footrest hanger. A tapered footrest hanger will not be appropriate for a child who needs to sit with an abducted leg position. The therapist must also consider the environments in which the child will use the wheelchair, what method the child will use for propelling the wheelchair, how the caregivers will transport it, and the sources of funding. The therapist is often responsible for providing a medical justification for the seating and mobility system.
Once the child’s needs have been identified, the therapist matches them to the specific features available in a wheelchair. If a child cannot shift weight independently and is at risk for developing pressure-related problems, then a wheelchair with a pressure relief cushion and either a manual or powered tilt-in-space feature may be necessary to shift weight from under the buttocks to the back (see Figure 21-14, C). The manual tilt-in-space feature allows the caregiver to activate a lever that allows the frame of the wheelchair to be tilted backwards while the seating positioning system maintains the same seat-to-back angle. This differs from a reclining wheelchair, which opens the seat-to-back angle so that the person is lying supine with hip extension. Powered tilt-in-space is an option available on either manual or power wheelchairs so that the user has independent control of tilting the frame. The therapist must be aware of the impact that the tilt-in-space position may have on a child’s field of vision. When tilted backwards, the child’s visual field will be in an upward direction toward the ceiling. In this position the child will need to flex his or her head forward to view the surroundings. A tilted position may also stimulate the sleep mechanism rather than placing the child more upright in a “work-ready” position. A tilt-in-space feature can also provide a few degrees of anterior tilt to position the child slightly forward, which may encourage trunk and neck extension for a more work-ready position.
The therapist should consider the following wheelchair features:
• Style of frame: Folding manual wheelchair (has lots of flexibility; folds side to side or forward onto the seat); non-folding or rigid manual wheelchair (lightest weight, has “tightest” responsive ride, back folds down, and wheels are removable); modular folding (frames come apart, separating the seating system from the base, which folds for manual and power wheelchairs); modular non-folding (can be disassembled into several parts for manual and power wheelchairs).
• Tilt-in-space: Tilt adjusts the seat backward as an entire unit while maintaining the same seat-to-back angle. It can be manual or powered for independent operation by the user. Tilt ranges are 45° to 65°. Tilt can accommodate users with insufficient head and trunk control, individuals who require pressure relief under the pelvis, or those with back or hip pain. The greater the degree of tilt, the more weight is distributed from the pelvis to the back.
• Recline: Recline positions the user in a reclined position in which the seat-to-back angle opens from the seated angle to about 170°. It can be operated manually by a caregiver or operated with power by the user. Some children with gastrointestinal issues may need to recline after a meal. This feature may also assist the care provider by allowing a reclined position for diaper changes.
• Footrest style: Footrests support the user’s feet and may act as a step for transfer in and out. Features include single plate or double plate, fixed, pull-up, swing-in or swing-out, and manual and powered elevating leg rests. The typical angle of footrests is 70° or 90° to accommodate fixed positions of the legs and feet. Many children sit more upright with 90° footrest hangers to accommodate tight hamstring muscles. If footplates are too far in front, placing a stretch on tight hamstrings, the pelvis will be pulled into a sacral sit position, thereby promoting a rounded trunk, which will adversely affect the child’s head position. Footrest hangers that are angled less than 90° make the length of the wheelchair frame longer, thereby decreasing maneuverability in tight places.
• Armrest style: Armrest styles can be full length, which makes it difficult to get close to a table or desk, or arm length, which incorporates a notched area in the frame of the armrest for getting under surfaces. Armrests can be height adjustable, fixed or removable, with pull-out or swing-away option. Some users may benefit from wider, contoured armrest pads for more arm support, particularly when using a joystick for driving a power wheelchair.
• Backrest height: A high backrest may be needed to support the seating and positioning needs of a client with a severe disability or for tilt and recline. A low backrest may be more functional for a client with good upper body function. A backrest that ends at the top of the shoulders is preferred so an adjustable height-contoured headrest can be positioned under the child’s occiput.
• Backrest adjustability: An angle-adjustable back provides the ability to set the seat-to-back angle to accommodate the child’s position. A child who extends or pushes backwards may benefit from a decreased back angle, whereas a child who is hypotonic and has difficulty maintaining a vertical head position may benefit from a greater than 90° seat-to-back angle.
• Height and adjustability features of push handles for the adult pushing the wheelchair.
• Floor-to-seat height: Seat height is important for transfers and getting under surfaces like tables. A lower seat height is typically preferred for younger children, particularly if a seating system will be integrated into the chair, which may raise the user higher.
• Style and location of wheel locks or brakes.
• Type, size, and placement of wheels and casters on a manual wheelchair for maximum efficiency during propulsion and to accommodate weight distribution: An adjustable axle plate can provide individualized wheel placement for the child to reach the tire. This may also assist children who are positioned forward of the push wheel because of a short seat depth, which places too much weight over the forward casters, thereby increasing resistance during propulsion. Tires can be pneumatic (air filled for a cushioned ride), semi-pneumatic (gel insert for flat-free maintenance), or solid (no maintenance but provides the stiffest ride and may add extra weight).
• Additional features include sit-to-stand in a manual wheelchair (see Figure 21-12, D) or a power wheelchair, whereby the child can move independently from a seated position to standing. The advantage of this feature is the ability to reach various heights, bear weight, and stretch throughout the day, and for some boys, the efficiency of standing without needing to transfer for toileting needs, as when using a urinal.
POWERED MOBILITY EVALUATION AND INTERVENTION
The therapist, teacher, child, and caregivers must first define the goals for using a powered mobility device. Are the goals to provide functional and independent home, school, and community mobility, or are the goals to provide transitional mobility experiences so that the child can have new opportunities to learn how to move, explore, and interact within the environment? Maneuverability features of the powered device are important in considering the various environments in which the device will be used (e.g., such as indoors in limited spaces such as a classroom or home, outdoors over rough terrain, or on a playground). What are the table heights the child’s chair must fit under at school, the home, and community? If it is necessary for the child to reach various heights in the wheelchair, then a powered lift seat may be justified. Will the child need the ability to tilt in space or recline? How is the child transferred into and out of the wheelchair? How will the mobility device be transported? Will it need to be disassembled to fit inside the trunk of a vehicle? If the wheelchair is to be transported in a van, is head clearance sufficient for the child when entering the vehicle and can the wheelchair be secured to the van for transport? Will the environments need to be made accessible with ramps into doorways or powered lifts into vehicles?
The next consideration is to determine how the child will access or drive the power wheelchair, and which power wheelchairs provide the control interface methods that the child needs now and may need in the near future, if there is a change in motor performance. The therapist begins an evaluation of the child’s ability to drive a power wheelchair by assessing the child’s position to determine how to optimize motor function for efficient and accurate access of the controls. It may be necessary to use an evaluation seating system or interim modifications to the child’s own seating system during the powered mobility evaluation. The child must feel secure, comfortable, and stable, particularly in the pelvis, trunk, and head, before attempting to operate a power wheelchair.
A joystick is the standard and often the preferred method for the individual who can maneuver it efficiently and accurately. The user can operate a joystick using a hand, foot, forearm, chin, head pointer, or even the back of the head, by using an adaptation that connects the joystick to a bracket that is attached to a moveable headrest. Some children may find it difficult to accurately use a joystick placed in its traditional location at the front end of the armrest. These children may have better motor control if the joystick is placed inside the armrest, in midline, or rotated several degrees toward the body (Case Study 21-2). A micro-joystick, or attendant joystick, which is smaller in size than a standard joystick, may be necessary for these types of situations and are available for most power wheelchairs. The small joystick is easier to position in midline or under the chin. Another feature that can assist in improving control or efficiency during joystick use is a support (such as a wide armrest or trough) under the elbow, forearm, or wrist. If the child has difficulty moving the joystick in the desired direction, the therapist can place a template with a cross shape cut out inside the control box to limit deviation of the joystick to the desired directions. The therapist can also position the joystick with proper hardware to another location, in which control be enhanced. During the evaluation for joystick operation, the therapist not only must evaluate the positioning needs of the child and placement of the joystick, but must consider the type of joystick, type of joystick knob, and desired location of the on-off switch for either independent access or may unintentional access by the user.
Joystick knobs are available in various styles, shapes, and sizes to accommodate various hand and wrist positions. The most common shapes are round, T-shaped, and I-shaped. A child with weakness of the upper extremities may find it more efficient to use a U-shaped joystick so that the hand is supported in the palm and at the sides. Joysticks can be highly sensitive, such that they require only slight movement of one finger, which may be useful for a child with muscle disease. Selection of the most appropriate style of joystick and its placement directly affects the ability to accurately and efficiently drive a power wheelchair. Case Study 21-3 provides an example of a child whose position is evaluated for more accurate use of a powered mobility device.
Children with severe physical disabilities may be able to operate a power wheelchair but often are not given the opportunity because they are physically unable to operate a joystick. Alternative control interfaces or access methods are available for these individuals.
If a child does not have the physical ability to control a joystick with the hand, foot, or head, the therapist should consider alternative control interfaces or access methods such as switch operation, particularly for individuals with cerebral palsy. Switch access of a powered mobility device is typically achieved using three or four switches, one for each direction of movement. Various types of switches can be placed at the hand, head, elbows, or feet, where the child has the most reliable, accurate, and efficient movements. Before selecting the type of switch, the therapist should determine the movements that the child can use to access a switch. If the child can nod “yes” and “no,” then he or she may have the ability to use switches around the back of the head.
The therapist may need to evaluate switch placement by allowing the child to first use switches to operate modified battery-operated toys.72 The therapist first identifies the most reliable and efficient movements that the child can voluntarily use to access the switches. Switch placement should begin at the hands and proceed to the head, elbows, knees, feet, and any other location determined appropriate. An adjustable mounting bracket, such as that available through AbleNet Incorporated, is extremely helpful for positioning a switch in multiple locations.
Switches are either momentary or latched. Momentary switches require the user to maintain contact on the switch to activate it. The child needs to be able to maintain contact on the switch long enough to move the wheelchair in a desired direction. A latching mode allows the user to press the switch one time to activate it, rather than holding it in the “on” position. A second activation turns the switch “off.” If the child needs to use switches to drive a power wheelchair, at least three switch sites are preferred: for driving forward and turning both directions. Reverse can be operated by a fourth switch or the adult. If the child can operate only one or two switches, the therapist may need to consider a scanning method; however, the scanning method requires a higher degree of cognitive function and concentration because of the complexity of the task.
An input method used frequently by individuals with spinal cord injuries is pneumatic sip-and-puff, which the user activates by gently inhaling or exhaling into a straw-like device held in the mouth. Another alternative method is the head-switch sensing array from Adapted Switch Labs, which consists of proximity switches embedded into a headrest that detect head movements for driving the wheelchair. These switches are operated not by making contact on the switch, but rather by getting close or proximal to the switch. The same switches can be embedded in a wheelchair lap tray so the child waves an arm above each switch to operate the wheelchair.
The Tongue Touch Keypad by New Abilities is a custom-made retainer in which small switches are embedded. The user activates each switch by touching it with the tongue. Multiple switch access is available in which push switches are placed around the body part that is able to reach the switches. The wheelchair is driven in one of four directions, depending on which switch is activated. It is even possible for the individual to drive a power wheelchair with one switch that operates a scanning light on a display. A recent development is the use of an interface tablet steering device to navigate a power wheelchair.50
Once the therapist has determined an accurate and reliable motor response, the child can assess the switch on a powered mobility device. However, the quality of motor control and accuracy is directly dependent on the child’s body position and the extent to which the position influences stability, mobility, muscle tone, and energy expenditure. Therefore, an evaluation of power wheelchair mobility control must simultaneously include a seating evaluation to determine how the child’s motor control is influenced by body position.
Several factors can interfere with a person’s ability to drive a powered mobility device. If a child has difficulty, the occupational therapist should first consider if the wheelchair, electronics, and interface, such as switches, are working properly. The brakes must be released and the wheels must be engaged. If the child continues to have difficulty, the type and placement of the controls should be reevaluated. Simultaneously, the therapist evaluates the child’s position to determine whether changes in the child’s posture influence motor control. Other considerations include undetected visual and perceptual difficulties, impairment in hearing, processing and response time, seizures, motivation, and behavior. Children with visual impairment often find it difficult to drive a power wheelchair outdoors in bright sun, preferring to do so indoors in large areas such as a clinic or classroom.
Many children may not initially be successful using a power wheelchair because of the overwhelming amount and degree of sensory input that is required. Imagine being a child with a severe disability who has difficulty with motor planning, coordination, visual perception, and communication, and is experiencing movement in a powered device for the first time. It would be overwhelming to experience the excitement and vestibular sensation of moving while trying to view the surroundings, which are quickly passing by, and simultaneously listen to an adult telling you how and where to move.
The therapist should assess a young child for powered mobility, whenever feasible, by providing a method that promotes exploration, problem solving, and self-learning for the child. Such a method requires an open space with activities and toys strategically placed around the room to facilitate experiences in movement and exploration.
The therapist should “limit physical and verbal commands as much as possible to avoid sensory overload on the part of the child” (p. 85).60 If a child is trying to move toward an object, the therapist should state the desired outcome, such as “come closer,” rather than specific commands, such as “push the joystick left” or “push the red switch and come over here.” Feedback should also be positive, such as “you found the wall,” rather than “oops, you crashed again.”73 If further assistance is needed to help the child understand the operation of the control, the therapist can facilitate the proper response by physically guiding the child’s movements for the desired response. The therapist must understand that children respond to visual, auditory, and sensory demands at different rates. A child with spastic cerebral palsy or quadriplegia may require much longer to make a visual motor response than a child with athetoid cerebral palsy, a spinal cord injury or muscle disease.
The most common method for evaluating a person’s ability to use a powered mobility device is to have the device available for trial use during the evaluation. A facility typically cannot afford to purchase power wheelchairs for evaluation purposes. Fortunately, ATPs often lend power wheelchairs to a clinical therapy unit for short-term evaluation purposes. The positioning and mobility equipment with the specific features that the child will need to operate the device should be available during the evaluation. Equipment used during an evaluation should be in optimal working condition. The therapist should begin the evaluation by test-driving the equipment to learn the forces and movements required to drive it, select the best speed for the client, and set any other adjustments, such as sensitivity of the controls.
It may also be beneficial to lend or rent a power wheelchair to children and their families for an extended evaluation. This allows more time for the child to learn how to use the controls and for the family to become familiar with the features of a power wheelchair to assist them in becoming more informed consumers. It also provides an opportunity for the family to experience the responsibilities of maintaining and transporting a power wheelchair.
Computer programs are also available for powered mobility assessment and training.59 R. J. Cooper and Associates has developed a joystick and mouse training program and a wheelchair simulation program. The programs display a power wheelchair on the screen that the user must navigate through a maze or room. Hasdai, Jessel, and Weiss studied whether a driving simulator would help a child master skills that are comparable with those required to drive a power wheelchair.33 Their results indicated benefits from using such a program to prepare children for powered mobility.
Researchers have explored the use of virtual reality for assessing and training powered mobility skills.67 The user wears a helmet that has a screen display of a three-dimensional room through which the person must navigate by using a joystick. More research is needed to determine if virtual reality is an effective means for assessing and training powered mobility and to determine whether children will integrate the skills of wheelchair driving if they have not participated in the actual task.
SEATING AND POSITIONING
Positioning is critical to the successful use of any mobility device because posture and task performance are interrelated.16 How an individual is positioned in a mobility device, whether it be standing or sitting, can have an effect on several physiologic factors, including visual and motor performance, postural control,45 ranges of movement, muscle tone,47 endurance, comfort, respiration, and digestion. These factors can affect functional performance activities such as hand function,48 levels of independence in mobility, self-care, activities of daily living (ADLs) such as transfers, and social interaction with others.35
Understanding the Biomechanics of Seating
To identify the positioning needs of a child, the occupational therapist must first have a thorough understanding of the biomechanical forces and neurophysiologic factors that can influence posture and movement. Biomechanical considerations are critical to obtaining proper alignment of the pelvis, spine, and head when postures are flexible or when accommodating individuals who no longer have active or passive range of motion as a result of contractures. The position and stability of the pelvis provide a foundation for movements that occur above and below the pelvis. Box 21-1 presents exercises that stress the importance of good alignment in sitting. Neurophysiologic factors include the child’s reaction to tactile input, body reactions to orientation in space, and movement.
Seating Guidelines
Optimal seating provides a stable place for the child’s pelvis and spine, from which a range of controlled movements for achieving functional tasks can occur. Seating is not static. Rather, it is a series of active movements or postures an individual uses to accomplish a series of motor tasks, such as maintaining the pelvis, trunk, and head upright against gravity while using the movements of the eyes, arms, and hands to access the controls of a power wheelchair or push the wheels of a manual wheelchair. For this reason, a series of postures must be made available to the child, not by restraining the child with straps and harnesses, but rather by supporting and guiding the child’s movements with an appropriate seating and mobility system. The occupational therapist needs to consider the biomechanical forces of an individual’s movements to determine what may be contributing to undesirable postures and, therefore, limited function.
The goals of seating are to provide optimal alignment and stability to improve distal motor function while minimizing undesirable tone and reflexes that interfere with alignment and stability; distribute seated pressures to maintain skin integrity; improve physiologic function such as breathing, swallowing, and digestion; increase independence in ADLs, and provide comfort.
The key points in achieving functional seating are the position and stability of the pelvis. A pelvis in a slight anterior tilt or neutral position is preferred. The angle of hip flexion can also affect postural control in sitting. Children with extensor tone may have a reduction of muscle tone with less than 90° of hip flexion combined with hip abduction. Stability at the pelvis can be achieved through contact points around the pelvis. These include the surfaces under, at the sides, and on top of the pelvis. The therapist must determine how a child responds to various types of seat surfaces and contours under the pelvis such as a flat seat surface or a contoured seat (a seat cushion that provides a recessed pocket for the pelvis and blocks forward movement of the ischial tuberosities).
The three types of seating surfaces are planar, contoured, and custom molded. Planar seating consists of flat surfaces with no contours. This type of seating may be more appropriate for individuals with mildly affected development who require only minimal body contact with the support surfaces of the seat. Contoured seating systems allow the body to have more contact with the support surface because its shape conforms to the curves of the spine, buttocks, and thighs. A contoured seat can be fabricated by layering various densities of foam that respond to the shape and weight of the person, thereby contouring around the bony prominences and other body curves. The therapist can recommend a standard size contoured back and seat cushion that can be adjusted to fit individual needs (Figure 21-16, A). Custom-molded seat cushions are designed specifically for an individual by taking an impression of the body and making a mold, which is sent to the manufacturer for fabrication (Figure 21-16, B). Another method uses a computer-generated graphic picture taken from the impression, which is sent to the manufacturer, which then uses a computer-assisted milling machine to fabricate the cushions.

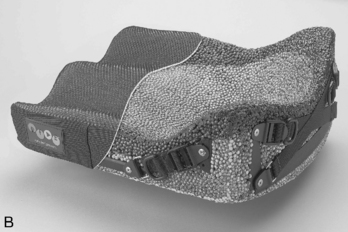
FIGURE 21-16 A, Infinity DualFlex 10 by Invacare. The Infinity DualFlex 10 is a modular seating system that accommodates a wide range of position needs. B, Ride designs cushion can be custom molded for an individual. (A, Courtesy Invacare, Elyria, Ohio.)
Cushions can also be custom molded using foam-in-bag technology, in which liquid foam is poured into an upholstered bag that is positioned around the person’s body, providing a molded cushion that is then upholstered. This technique is more difficult to use because the individual’s position must be held in place while the foam is being formed. If the child moves, the quality of the foam mold is negatively affected.
The therapist can also improve stability of the pelvis and trunk by ensuring that the femur is properly supported along its entire length, from the back of the pelvis to approximately 1 inch from the popliteal area under the knee. One exception is to use a much shorter seat depth for a client who can propel a wheelchair using the legs and feet. In this situation, a shorter seat with a slight anterior tilt would be preferred. Some individuals require support at the sides of the pelvis to maintain a symmetrical position and reduce pelvic shift to either side. Support at the sides of the pelvis can be contoured into the seat or added as lateral hip guides. Stability can be provided above the pelvis to reduce sliding in an upward and forward direction. The therapist typically accomplishes this by placing a positioning belt at a 45° angle to the seat or closer to the thighs. A new device for dynamically positioning the pelvis while allowing for functional pelvic movements is the Hip Grip Pelvic Stabilization Device from Body Point (Figure 21-17). Made of a contoured padded harness, the Hip-Grip attaches to the lower part of the wheelchair backrest and around the sacral area of the pelvis. A positioning belt with sub-ASIS pads is secured in front of the pelvis. A rotational mechanism at the sides of the HipGrip maintains postural stability while allowing the user to move the pelvis in the anterior and posterior directions, as when reaching or propelling the wheelchair. Other components, such as footplates, lap trays, arm rests or arm troughs, a contoured backrest, and headrests, can provide additional support to the pelvis and trunk.
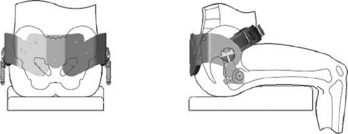
FIGURE 21-17 Hip Grip, a dynamic pelvic stabilization device. (Available through Bodypoint Inc.; http://www.bodypoint.com.)
The use of orthotics, or devices for bracing the extremities or body, may also assist in achieving optimal positioning in the seated and standing positions. Ankle-foot orthoses are most commonly recommended to align the foot and ankle and assist in either reducing muscle tone or supporting a weak limb. A thoracic-lumbar-sacral orthosis (TLSO), or body jacket, may be another alternative for individuals with scoliosis to use for support in the seated position.
Young children who exhibit an increase in extensor movements and asymmetry when being evaluated for a seating system may benefit from using a “barrier” vest as proposed by Kangas.39 The vest is made from Plastazote foam, which is not strong enough to totally support the child and does allow the child to have some movement. It is worn to decrease the child’s sensitivity to individual points of contact from hands touching the body during handling or from pads on a seating system, which can set off the extensor body reaction. The child wears the vest for up to 6 months while developing greater postural stability.
Evaluation
The therapist should begin the initial assessment by observing the child using any existing seating and mobility systems to note posture, movements, comfort, satisfaction with the equipment, and other factors that may affect function. During the seating evaluation, the therapist will need to consider (1) the angle between the seat and the back surfaces, (2) the tilt of the system in space (orientation), and (3) the type of surface on which the child will be seated.6
The therapist should begin the evaluation by positioning the child on a low mat table so that he or she can complete a postural assessment to determine whether any limitations in ranges of movement exist that may interfere with the upright and seated positions. The therapist obtains further information by positioning the child in a sitting position while using the hands to support the child to identify key points of control and positions that provide a desirable change in posture, muscle tone, and movements. These key points become the necessary components of the seating system. The positions, such as the angle of hip flexion and the orientation in space of the child, become the pitches and angles of the components necessary in the seating system and wheelchair hardware.16
Once the therapist gathers information from the postural assessment, other methods are also available that use evaluation equipment for assessment of the child’s position to determine what components, angles, and sizes are needed in a seating system. Simulators are self-contained, adjustable fitting chairs that the therapist can adjust to fit a child or an adult, to determine what type of seating components and angles are appropriate.65 The simulator allows the therapist to “evaluate the client in the system, alter angles of the seat to the back, try varying positions in space, and determine component sizes and accessories that are required before making recommendations for a particular system” (p. 73).66
The therapist and the ATP can use simulators to evaluate planar, contoured, and molded seating (Figure 21-18). The therapist first completes a postural evaluation of the individual to determine which seating components are necessary and then adjusts the simulator to the individual’s size. The therapist selects angles, which include seat-to-back and tilt. Further adjustments can be made to determine how position influences movement and function. The advantages of using a seating simulator include (1) use as a single evaluation tool for various ages, sizes, and diagnoses; (2) source of information about the various types of seating systems, such as planar versus molded; and (3) options to motorize simulators to evaluate powered mobility access and the effect of positioning on motor control. The problem that the assessment team often encounters when using simulators is difficulty in transferring the information from the simulator into an actual seating system and knowing how that system will integrate into a mobility base. Children may also respond negatively to the simulator evaluation because its mechanical appearance and large size may intimidate them.
Another method for evaluating seating and positioning is use of a modular mockup or adjustable evaluation seat system that can be placed in a mobility base. These are typically available in planar or contoured seating devices rather than in custom-molded devices. The main advantage of using this method is that the child can use the actual mobility device while seated in the mockup seat. This is particularly important because positioning can influence body movements and therefore functional outcomes. The disadvantages are that more equipment must be available to fit a range of individuals, and pitches and angles cannot always be accurately assessed.
Children with hypotonia, such as those with muscle disease or cerebral palsy, have specific needs. A useful positioning system includes a biangular back design that supports the sacrum in a neutral position but angles the remaining backrest about 15° away from the back at the posterior superior iliac spine. This provides a resting position of the trunk behind the pelvis and accommodates the forces of gravity in the upright position (see Figure 21-16, B). Consideration of a tilt-in-space feature in the mobility base and an adjustable seat-to-back angle may also provide the hypotonic or weak child with greater tolerance for sitting upright.
Children with increased muscle tone and spasticity who adduct their legs and extend their hips and spine are often more difficult to position. The therapist must identify key points of control for positioning these children. For example, the therapist determines the desired degree of hip and knee flexion, hip abduction, and reduction of asymmetrical positioning that positively influences muscle tone and control of extremity movement. The critical factor for reducing the degree and frequency of extensor posturing is to determine what factors contribute to these undesirable movements. Kangas observed that certain children become more asymmetrical as hypertonus increases, and that this increase in muscle tone is stimulated when they feel pressure behind their head or neck from a headrest.39 These children may also have better postural control in the upright position rather than reclined or tilted.47 In other children who extend forcibly in combination with rotation of one side of the body forward, the resulting pelvic obliquity may place strain on the soft tissue when the child is positioned symmetrically with both legs forward. These children often prefer to have one leg abducted (almost off the seat cushion) and one leg forward. This often reduces the strength and frequency of hip extension and rotation of the upper body as the child extends.
The therapist must frequently reevaluate a child’s position, particularly in a seated mobility device, to accommodate postural, developmental, and physiologic changes. Once a child receives a seating mobility system, the therapist should reevaluate its fit and function every 4 to 6 months. Positioning and mobility literature and support materials are available,15,22,65,66 and more specific information and techniques on positioning are available through additional reading and workshops.
TRANSPORTATION OF MOBILITY SYSTEMS
Many manufacturers of wheelchair mobility systems do not recommend using them as a seat in a motor vehicle. However, most families do not recognize this warning and allow the child to travel while seated in the wheelchair in a motor vehicle or school bus. Manufacturers are now providing safer options for transporting a wheelchair with the child in it because of a voluntary ANSI/RESNA standard called WC-19, Wheelchairs Used as Seats in Motor Vehicles.3 Wheelchairs are considered WC-19–compliant if they have four accessible and identifiable points to secure the chair to the vehicle, as well as seating, a frame, and other components designed to allow better fit of a lap and shoulder belt. The standard requires wheelchairs to be dynamically crash-tested at 30 miles per hour and 20g crash conditions, which are the standards used to test child safety seats.
It is important that occupational therapists recommend wheelchairs that are WC-19–compliant and educate clients and families on safe methods for transporting a wheelchair in a motor vehicle. Standards have also been developed to recognize the safety of a specialized seating system that may be used in another manufacturer’s wheelchair bases. The ANSI/RESNA WC-20 standards are for seating devices for use in motor vehicles.4 One standard requires that all students being transported in a wheelchair on a bus must face forward. Wheelchairs that are transported in a side-facing position are more likely to deform and collapse in a crash and the shoulder belt is ineffective.57 School-based occupational therapists must work with transportation personnel to educate them on the importance of forward-facing positions for wheelchair riders, as well as the proper use of tie-downs. The lap belt must be snug and low on the pelvis and the shoulder belt positioned over the middle of the clavicle and across the sternum, where it connects to the pelvic belt over the hip. Any device such as an augmentative communication device or computer and lap tray must be removed and tied down separately.
FACTORS THAT INFLUENCE THE SUCCESSFUL USE OF MOBILITY DEVICES
Successful use of mobility devices depends on the fit of the child to the device, the features of the device, and the physical and social environments. Studies have shown a significant relationship between certain standardized tests of cognition and perception and use of powered mobility. Specific functional performance tasks correlate with the ability with use a power wheelchair. Preliminary findings indicate a relationship between specific cognitive scales and readiness for powered mobility, particularly in the areas of spatial relations and problem solving.28,63,69
Another factor that influences a child’s ability to use a powered device is the ability of the professional or the caregiver to determine the most accurate and efficient means for the child to access the device. If a child is having significant difficulty in maneuvering a powered mobility device successfully, the therapist must first reevaluate the position of the child and the access method to determine whether it is the most effective means. The longer it takes a child to successfully demonstrate use of a control, the more likely it is that either the access method is inappropriate or the child’s seating needs have not been met. Case Study 21-4 describes this type of situation.
The therapist must consider changes that the child will have in the future, both expected and unexpected, when recommending equipment. For example, the therapist must determine whether the system can be easily changed as the child gains new skills, grows, or changes physically. This is particularly important for the therapist to consider when ordering a power wheelchair. For example, a child with a progressive disability may be able to operate a joystick at the time the chair is ordered. However, electronic options need to be included, such as the ability to readily change the input method, if the child’s functional status changes and use of a joystick is no longer feasible. It is more economical in most cases to initially order options on equipment rather than retrofit the equipment at a later date.
The therapist must also determine where and how augmentative communication equipment will be mounted to the child’s wheelchair. Selection of the appropriate mounting bracket depends on the tube size of the wheelchair frame and locations on the wheelchair where it can be attached. A problem that therapists often encounter with manual wheelchairs is positioning the child or rear wheels too far forward of the center of gravity in the wheelchair, which often causes the wheelchair to tip forward when the communication device is mounted. The most frequent problem encountered with mounting augmentative communication devices on power wheelchairs is finding a place to mount the bracket on the frame and making certain it does not interfere with moving through doorways.
The therapy team and ATP have a responsibility to assist the family and child in becoming informed consumers by identifying seating and mobility issues and needs, then presenting several alternatives during the evaluation. The family should make the final decision on the specific type of mobility device after considering the options that the therapy team presents. The most important and significant contribution that the therapist can make is to evaluate access methods and help caregivers develop and implement strategies to meet identified goals. The therapist must reevaluate the outcome as the child progresses. This includes providing periodic evaluations of fit and function of the equipment.
SUMMARY
The literature indicates that independent mobility plays a facilitative role in cognitive, language, and social development.38 Therefore, when mobility is severely delayed or restricted, emotional and psychosocial development are affected. Augmentative mobility devices can provide either functional or transitional mobility. These devices can provide children with physical disabilities greater opportunities to develop and become initiators and active participants in daily occupations and experiences. Occupational therapists emphasize methods of adapting the child’s environments to maximize his or her functional mobility. The occupational therapist is responsible for ensuring that children with physical disabilities receive opportunities for mobility at the earliest age possible to promote participation and development more equal to their able-bodied peers.
Case Studies 21-5 and 21-6 include comprehensive information about the children’s equipment and adapted environments. These descriptions demonstrate how mobility equipment is integrated with other AT and environmental adaptations to best meet the children’s functional needs.
REFERENCES
1. Americans with Disabilities Act & Accessible Information Technology Center. Bulletin #4. Retrieved July 2009 from http://www.adaproject.org, 2003.
2. Andersson, C., Grooten, W., Hellsten, M., Kaping, K., Mattsson, E. Adults with cerebral palsy: Walking ability after progressive strength training. Developmental Medicine and Child Neurology. 2003;45:220–228.
3. ANSI/RESNA Subcommittee on Wheelchairs and Transportation. ANSI/RESNA WC, Vol.1/Sect. 19, Wheelchairs used as seats in motor vehicles. Arlington, VA: RESNA, 2000.
4. ANSI/RESNA Subcommittee on Wheelchairs and Transportation. ANSI/RESNA WC. Vol. 4/Sect. 20, Seating systems used in motor vehicles. Arlington, VA: RESNA, 2008.
5. Backer, G., Howell, B. Physical therapy goals and intervention for the ventilator-assisted child or adolescent. In: Driver L., Nelson V., Warschausky S., eds. The ventilator assisted child. San Antonio, TX: Communication Skill Builders, 1997.
6. Bergen, A., Presperin, J., Tallman, T. Positioning for function: Wheelchairs and other assistive technologies. New York: Valhalla Rehabilitation Publications, 1990.
7. Blundell, S., Shepherd, R., Dean, C., Adams, R., Cahill, B. Functional strength training in cerebral palsy: A pilot study of a group circuit training class for children aged 4–8 years. Clinical Rehabilitation. 2003;17:48–57.
8. Bly, L. Motor skills acquisition in the first year. Tucson, AZ: Therapy Skill Builders, 1994.
9. Brinker, R.P., Lewis, M. Making the world work with microcomputers: A learning prosthesis for handicapped infants. Exceptional Children. 1982;49:163–170.
10. Butler, C. Effects of powered mobility on self-initiated behaviors of very young children with locomotor disability. Developmental Medicine and Child Neurology. 1986;28:325–332.
11. Butler, C. High tech tots: Technology for mobility, manipulation, communication, and learning in early childhood. Infants and Young Children. 1988;2:66–73.
12. Butler, C. Powered tots: Augmentative mobility for locomotor disabled youngsters. American Physical Therapy Association Pediatric Publication. 14(19), 1988.
13. Campos, J.J., Bertenthal, B.I., Locomotion and psychological development in infancy. Jaffe K.M., ed. Childhood powered mobility: Developmental, technical, and clinical perspectives. Proceedings of the RESNA First Northwest Regional Conference, Washington, DC, RESNA Press, 1987:11–42.
14. Cech, D., Martin, A. Functional movement development across the life span. Philadelphia: W.B. Saunders, 1995.
15. Cook, A., Polgar, J. Technologies that enable mobility. In: Cook A., Polgar J., eds. Assistive technologies: Principles and practice. 3rd ed. St. Louis: Mosby; 2008:408–442.
16. Cooper, R. Biomechanics and ergonomics of wheelchairs. In: Cooper R., ed. Wheelchair selection and configuration. New York: Demos, 1998.
17. Coster, W. Occupation-centered assessment of children. American Journal of Occupational Therapy. 1998;52:337–344.
18. Damiano, D.L. Activity, activity, activity: Rethinking our physical therapy approach to cerebral palsy. Physical Therapy. 2006;86:1534–1540.
19. Deitz, J., Swinth, Y., White, O. Powered mobility and preschoolers with complex developmental delays. American Journal of Occupational Therapy. 2002;56:86–96.
20. Douglas, J., Ryan, M. A preschool severely disabled boy and his powered wheelchair: A case study. Child Care, Health and Development. 1987;13:303–309.
21. Eagleton, M., Iams, A., McDowell, J., Morrison, R., Evans, C.L. The effects of strength training on gait in adolescents with cerebral palsy. Pediatric Physical Therapy. 2004;16:22–30.
22. Engstrom, B. Ergonomics, wheelchairs and positioning. Hasselby, Sweden: Posturalis Books, 1993.
23. Everand, L. Early mobility means easier integration. Canadian Review of Sociology and Anthropology. 1997;34:224–234.
24. Fisher, A.G. Uniting practice and theory in an occupational framework. American Journal of Occupational Therapy. 1998;52:509–519.
25. Foreman, N., Foreman, D., Cummings, A., Owens, S. Journal of General Psychology. 1990;117:195–233.
26. Fowler, E.G., Ho, T.W., Nwigwe, A.I., Dorey, F.J. The effect of quadriceps femoris muscle strengthening exercises on spasticity in children with cerebral palsy. Physical Therapy. 2001;81:1195–1223.
27. Furumasu, J., Guerrette, P., Tefft, D. The development of a powered wheelchair mobility program for young children. Technology and Disability. 1996;5:41–48.
28. Furumasu, J., Guerette, P., Tefft, D. Relevance of the Pediatric Powered Wheelchair Screening Test (PPWST) for children with cerebral palsy. Developmental Medicine and Child Neurology. 2004;46:468–474.
29. Furumasu, J., Tefft, D., Guerette, P. Pediatric powered mobility: Readiness to learn. Team Rehab. 1996:29–36.
30. Guerette, P., Tefft, D., Furumasu, J. Pediatric powered mobility: Results of a national survey of providers. Assistive Technology. 2005;17:144–158.
31. Guerette, P., Tefft, D., Furumasu, J., Moy, F. Development of a cognitive assessment battery for young children with physical impairments. Infant-Toddler Intervention: The Transdisciplinary Journal. 1999;9:169–181.
32. Haley, S.M., Coster, W.J., Ludlow, L.H., Haltiwanger, J., Andrellos, P. Pediatric Evaluation of Disability Inventory (PEDI). San Antonio, TX: Psychological Corp, 1992.
33. Hasdai, A., Jessel, A.S., Weiss, P.L. Use of computer simulator for training children with disabilities in the operation of a powered wheelchair. American Journal of Occupational Therapy. 1998;52:195–220.
34. Hays, R., Childhood motor impairments: Clinical overview and scope of the problem. Jaffe K.M., ed. Childhood powered mobility: Developmental, technical, and clinical perspectives. Proceedings of the RESNA First Northwest Regional Conference, Washington, DC, RESNA Press, 1987.
35. Hulme, J., Poor, R., Schulein, M., Pezzino, J. Perceived behavioral changes observed with adaptive seating devices for multi-handicapped developmentally disabled individuals. Physical Therapy. 1983;62:204–208.
36. Hundert, J., Hopkins, B. Training supervisors in a collaborative team approach to promote peer interactions of children with disabilities in integrated preschools. Journal of Applied Behavior Analysis. 1992;25:385–400.
37. Hune, K., Guarrera-Bowlby, P., Deutsch, J. The clinical decision-making process of prescribing power mobility for a child with cerebral palsy. Pediatric Physical Therapy. 2007;19:254–260.
38. Jones, M.A., McEwen, I.R., Hansen, L. Use of power mobility for a young child with spinal muscular atrophy. Physical Therapy. 2003;83:253–262.
39. Kangas, K., Chest supports: Why they are not working. Presented at the Seventeenth International Seating Symposium, 2001:41–44. [February 22–24].
40. Kermoian, R. Locomotion experience and psychological development in infancy. In: Furumasu J., ed. Pediatric powered mobility: Developmental perspectives, technical issues, clinical approaches. Arlington, VA: RESNA Press; 1997:7–22.
41. Lange, M. Manual wheelchairs: Understanding these general categories can help therapists meet individual needs. ADVANCE. 2008:31–33.
42. Law, M., Baptiste, S., Carswell, A., McColl, M.A., Polatajko, H., Pollock, N. The Canadian Occupational Performance Measure, 2nd ed. Toronto, ON: CAOT Publications, 2005.
43. Margolis, S.A., et al. The Subasis Bar: An effective approach to pelvic stabilization in seated positioning. The Proceedings of the 8th Annual Conference on Rehabilitation Engineering, 1985:45–47.
44. McBurney, H., Taylor, N.F., Dodd, K.J., Graham, H.K. A qualitative analysis of the benefits of strength training for young people with cerebral palsy. Developmental Medicine and Child Neurology. 2003;45:658–663.
45. Myhr, U., Wendt, L. Improvement of functional sitting position for children with cerebral palsy. Developmental Medicine and Child Neurology. 1991;33:246–256.
46. Nilsson, L., Nyberg, P. Driving to learn: A new concept for training children with profound cognitive disabilities in a powered wheelchair. American Journal of Occupational Therapy. 2003;57:229–233.
47. Nwaobi, O. Effects of body orientation in space on tonic muscle activity of patients with cerebral palsy. Developmental Medicine and Child Neurology. 1986;28:41–44.
48. Nwaobi, O. Effect of unilateral arm restraint on upper extremity function in cerebral palsy. Proceedings of the Annual RESNA Conference, Washington, DC, RESNA Press, 1987:311–313.
49. Paleg, G. Made for walking: A comparison of gait trainers. Team Rehab Report. 1997:41–45.
50. Paleg, G. What’s new in mobility accessories. Rehab Management. 2007:24–27.
51. Paleg, G., Moving forward. Rehab Management, 2008. Retrieved July 2009 from, http://www.rehabpub.com/issues/articles/2008-06_02.asp.
52. Paulsson, K., Christoffersen, M. Psychological aspects of technical aids: How does independent mobility affect the psychological and intellectual development of children with physical disabilities. Proceedings of the Second Annual Conference on Rehabilitation Engineering, Washington, DC, RESNA Press, 1984:282–286.
53. Piaget, J. The construction of reality in the child. New York: Basic Books, 1954.
54. Pollock, N., Stewart, D. Occupational performance needs of school-aged children with physical disability in the community. Physical and Occupational Therapy in Pediatrics. 1998;18:55–68.
55. Raine, A., Reynolds, C., Venables, P.H., Mednick, S.A. Stimulation seeking and intelligence: A retrospective longitudinal study. Journal Personality and Social Psychology. 2002;82:663–674.
56. Seligman, M. Helplessness: On depression, development, and death. San Francisco: W.H. Freeman, 1975.
57. Shutrump, S., Manary, M., Buning, M. Safe transportation for students who use wheelchairs on the school bus. OT Practice. 2008:8–12.
58. Stanton, D., Wilson, P.N., Foreman, N. Effects of early mobility on shortcut performance in a simulated maze. Behavioral Brain Research. 2002;136:61–66.
59. Taplin, C.S. Powered wheelchair control, assessment, and training. RESNA ‘89: Proceedings of the 12th annual conference, Washington, DC, RESNA Press, 1989:45–46.
60. Taylor, S., Monahan, L. Brubaker C., ed. Considerations in assessing for powered mobility. Wheelchair IV: Report of a conference on the state of the art of powered wheelchair mobility, December 7–9, 1988, Washington, DC, RESNA Press, 1989.
61. Tefft, D., Furumasu, J., Guerette, P. Cognitive readiness for powered wheelchair mobility in the young child. Proceedings of the RESNA 1993 Annual Conference, Washington, DC, RESNA Press, 1993:338–340.
62. Tefft, D., Furumasu, J., Guerette, P. Development of a cognitive assessment battery for evaluating readiness for powered mobility. In: Proceedings of the RESNA 1995 Annual Conference. Washington, DC: RESNA Press; 1995:320–322.
63. Tefft, D., Guerette, P., Furumasu, J. Cognitive predictors of young children’s readiness for powered mobility. Developmental Medicine and Child Neurology. 1999;41:665–670.
64. Telzrow, R., Campos, J., Shepherd, A., Bertenthal, B., Atwater, S., Spatial understanding in infants with motor handicaps. Jaffe K.M., ed. Childhood powered mobility: Developmental, technical and clinical perspectives. Proceedings of the RESNA First Northwest Regional Conference, Seattle, WA, RESNA Association for the Advancement of Rehabilitation Technology, 1987:62–69.
65. Trefler, E., Then and now: Saving time with simulators. Team Rehab, February, 1999:32–36.
66. Trefler, E., Hobson, D., Taylor, S., Monahan, L., Shaw, C. Seating and mobility. Tucson, AZ: Therapy Skill Builders, 1993.
67. Trimble, J., Morris, T., Crandall, R. Virtual reality: Designing accessible environments. Team Rehab Report. 1992;3:8–12.
68. Uniform Data System for Medical Rehabilitation. Functional Independence Measure for Children (WeeFIM) (Outpatient version 5.0). Buffalo, NY: State University of New York at Buffalo, 1999.
69. Verburg, G., Field, D., Jarvis, S. Motor, perceptual, and cognitive factors that affect mobility control. Proceedings of the 10th Annual Conference on Rehabilitation Technology, Washington, DC, RESNA Press, 1987.
70. Warren, C.G. Powered mobility and its implications. Journal of Rehabilitation Research and Development. Clinical Supplement. 1990;27:74–85.
71. Woods, H. Moving right along: Young disabled children can now experience the developmental benefits of moving and exploring on their own. Stanford Medicine. 1998, Fall:15–19.
72. Wright, C., Nomura, M. From toys to computers, access for the physically disabled child, 1985. [San Jose, CA].
73. Wright-Ott, C. The transitional powered mobility aid: A new concept and tool for early mobility. In: Furumasu J., ed. Pediatric powered mobility. Washington, DC: RESNA Press; 1997:58–69.
74. Wright-Ott, C. Designing a transitional powered mobility aid for young children with physical disabilities. In: Gray D., Quatrano L., Lieverman M., eds. Designing and using assistive technology: The human perspective. Baltimore: Brookes; 1998:285–295.
75. Wright-Ott, C., A transitional powered mobility aid for young children with physical disabilities. Presented at ICORR 99 Sixth International Conference on Rehabilitation Robotics, July 1999, Stanford, CA, 1999.
76. Wright-Ott, C., Escobar, R., & Leslie, S. Encouraging exploration. Rehab Management. Retrieved June 2002 from http://www.rehabpub.com/features/672002/3.asp
Bertenthal, B.I., Campos, J.J., Barrett, K.C. Self-produced locomotion: An organizer of emotional, cognitive, and social development in infancy. In: Emde R.N., Harmon R.J., eds. Continuities and discontinuities in development. New York: Plenum Press, 1984.
Cook, A., Polgar, J. Assistive technologies: Principles and practice, 3rd ed. St. Louis: Mosby, 2008.
Fuhrman, S., Buning, M., Karg, P., Wheelchair transportation: Ensuring safe community mobility. OT Practice, October, 2008:10–13.
Tefft, D., Furumasu, J., Guerette, P. Ready, set, go: Pediatric powered mobility with young children training video and manual. Downey CA: LAREI, 1996.
Tefft, D., Furumasu, J., Guerette, P. Pediatric powered mobility: Influential cognitive skills. In: Furumasu J., ed. Pediatric powered mobility: Developmental perspectives, technical issues, clinical approaches. Washington, DC: RESNA Press; 1997:70–91.
Werner, D. Disabled village children: A guide for community health workers, rehabilitation workers and families. Retrieved at http://disabledvillagechildren.projects.unamesa.org.
 CASE STUDY 21-1
CASE STUDY 21-1