Practice 12. Chest Drainage: Underwater Seal or Chest Drainage System
Learning outcomes
By the end of this section, you should know how to:
▪ support and prepare the patient for these three nursing practices
▪ collect and prepare the equipment necessary to insert a chest drain and connect it to underwater seal drainage, change a chest drainage bottle and assist with removal of an underwater seal chest drain
▪ assist the medical practitioner in parts 1 and 3
▪ care for the patient who has a chest drain connected to underwater seal drainage.
Background knowledge required
Revision of the anatomy, physiology and pathology of the respiratory system, including the structures of the chest wall
Revision of ‘Aseptic technique’ (seep. 386).
Revision of local policy on chest drainage.
1. INSERTION OF AN UNDERWATER SEAL CHEST DRAIN
Indications and rationale for insertion of an underwater seal chest drain
Chest drainage refers to a closed system of drainage that allows air or fluid to pass in one direction only, from the pleural space to either a collecting bottle or flutter valve system. It may be required in a variety of situations when ventilation is impaired, such as traumatic injuries, malignancy, post-thoracic surgery or following spontaneous collapse of the lung (pneumothorax). Chest drainage may therefore be used to remove air, blood, fluid or pus from the pleural space to improve ventilation capacity.
Chest drains may also be inserted to allow drug administration to occur, for example in lung cancer.
The choice of drainage system will depend upon the clinical status and underlying condition of the patient, the nature of the expected drainage and whether the drain is being inserted perioperatively or in a ward or outpatient unit. Underwater seal drainage bottles are at risk of being knocked over, inhibit patient mobilisation and need to be monitored on an inpatient basis. Flutter valve systems are useful for draining air though they cannot be used for draining fluid. The flutter valve system has the advantage of allowing mobilisation.
The drain insertion site will also vary according to the clinical status of the patient. Confirmation of the insertion site should be made following clinical examination and chest X-ray in all cases, apart from tension pneumothorax when it would be a priority to insert the drain quickly. Sometimes the drain is inserted with the aid of imaging such as ultrasound (Laws et al 2003). For many of the indications for chest drain insertion, the site will be the third, fourth or fifth intercostal space in the mid axillary line.
Position of the patient
During insertion, the patient's clinical status will determine the optimum position to be adopted. It is often sitting upright and the patient may use a table with a pillow to rest on.
Outline of the procedure
Using an aseptic technique, the medical practitioner cleanses the patient's skin with iodine or an alcohol-based antiseptic (as per local skin preparation policy), over the selected site of entry for the drain, injects a local anaesthetic and waits for it to take effect. The method of drain insertion will vary depending on the size of drain required. The aim is to avoid excessive force that may cause damage to intrathoracic structures. Sometimes an introducer is used, or blunt dissection of the subcutaneous tissue using forceps may be used for larger sizes of drainage tube. Once the tube is in place, the medical practitioner connects the drain to the equipment already prepared by the nurse. A suture is inserted round the entry site of the drain to seal the site off when the drain is eventually removed. A purse-string suture should not be used (Laws et al 2003). A sterile transparent dressing is placed over the site to help to prevent infection of the small wound (Fig. 12.1).
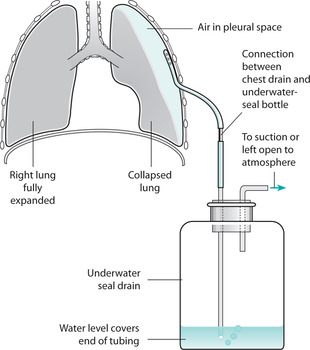 |
| FIGURE 12.1Underwater seal chest drainage systemFrom Brooker& Nicol 2003, with permission |
 Equipment
Equipment1. Trolley
2. Sterile dressings pack
3. Sterile gloves
4. Iodine preparation or alcohol-based antiseptic (as per local policy on skin cleansing)
5. Local anaesthetic and equipment for its administration
6. Sterile scalpel and blade and/or Spencer Wells forceps
7. Sterile black silk suture
8. Sterile chest drain and introducer
9. Sterile drainage equipment, e.g. Pleurovac or Argyle double-seal system
10. Two pairs of tubing clamps
11. Receptacle for soiled disposable items
12. Sharps box.
▪ help to explain the procedure to the patient to gain informed consent and co-operation. Patients should be encouraged to be active partners in care
▪ ensure the patient's privacy to help maintain dignity
▪ administer a pre-medication if prescribed by the medical staff to help to reduce the patient's anxiety
▪ administer analgesia as prescribed to minimize pain during and after the procedure
▪ collect the equipment, for efficiency of practice
▪ help the patient into the position suggested by the medical staff to allow best access to the site for insertion of the drain
▪ observe the patient throughout this activity to detect signs of discomfort, distress or adverse effects
▪ ensure that the drainage equipment is assembled correctly and ready for connection to the drain when required, for efficient practice
▪ open the sterile equipment and help the medical practitioner as requested
▪ seal all connections to ensure that they are airtight, as this is necessary for maximum functioning of the drain
▪ ensure that the collection equipment is always below the level of the patient's chest so that there is no reflux into the pleural space (Fig. 12.2)
 |
| FIGURE 12.2Patient with underwater seal chest drainage |
▪ check that the apparatus is functioning; the fluid should be oscillating in the long underwater tube in time with the patient's respiration indicating patency of the tube. If positive suction is required, connect the short rod of the drainage bottle to the long rod of a second drainage bottle using tubing. The short rod of this second drainage bottle is then connected by tubing to a suction machine, the pressure of which has been decided by the medical practitioner
▪ apply a sterile transparent dressing to the wound site to help to prevent infection and to facilitate observation of the site
▪ ensure that the patient is left feeling as comfortable as possible, to maintain the quality of this practice
▪ dispose of the equipment safely to comply with health and safety and infection-control requirements
▪ document the procedure appropriately, monitor the after-effects and report any abnormal findings immediately to ensure safe practice and enable prompt, appropriate medical and nursing intervention to be initiated
▪ monitor vital signs to assess response to intervention
▪ observe and record amount, type and consistency of drainage to monitor patient's progress and maintain fluid balance
▪ in undertaking this practice, nurses are accountable for their actions, the quality of care delivered and record-keeping according to the Code of Professional Conduct: Standards for Conduct, Performance and Ethics (Nursing and Midwifery Council 2004) and Guidelines for Records and Record Keeping (Nursing and Midwifery Council 2005).
Indications and rationale for changing a drainage bottle
As drainage from the pleural space accumulates and approaches the three-quarters-full level, the drainage bottle has to be changed:
▪ to enable the equipment to continue functioning efficiently as increased volume in the bottle may cause resistance to drainage (Allibone 2003).
 Equipment
Equipment1. Sterile drainage bottle, cap, glass or plastic rods and tubing or a disposable set
2. 500 ml of sterile water or normal saline
3. Receptacle for soiled disposable items.
 Guidelines and rationale for this nursing practice
Guidelines and rationale for this nursing practice▪ collect and prepare the equipment for efficiency of practice
▪ explain this practice to the patient to encourage active participation in care
▪ observe the patient throughout this activity to detect signs of discomfort, distress or adverse effects
▪ clamp off the chest drain, one close to the chest wall and one below the connection to the drainage tubing to prevent any backflow of air or fluid (Parkin 2002)
▪ disconnect the tubing
▪ connect the fresh tubing and apparatus
▪ ensure that all the connections are airtight and that the drainage bottle is below chest level so that it will function correctly
▪ release the clamps and check the oscillation of the fluid in the underwater tube to confirm that the apparatus is functioning correctly
▪ ensure that the patient is left feeling as comfortable as possible to maintain the quality of this practice
▪ dispose of the equipment safely for the protection of others
▪ document this nursing practice and report abnormal findings immediately so that action can be taken to relieve any problems
▪ observations and recording of vital signs should be performed following the procedure to monitor the patient's progress
▪ observation and monitoring of drainage should continue to monitor patient's progress and maintain fluid balance
▪ in undertaking this practice, nurses are accountable for their actions, the quality of care delivered and record-keeping according to the Code of Professional Conduct: Standards for Conduct, Performance and Ethics (Nursing and Midwifery Council 2004) and Guidelines for Records and Record Keeping (Nursing and Midwifery Council 2005).
Indications and rationale for removal of an underwater seal chest drain
Underwater seal drainage is a temporary measure and is removed:
▪ when radiological examination demonstrates that the patient's lung has fully reinflated
▪ when air or fluid no longer drains and when breath sounds have improved.
 Equipment
Equipment1. Trolley
2. Sterile dressings pack
3. Sterile stitch-cutter
4. Sterile artery forceps
5. Receptacle for soiled disposable items.
 Guidelines and rationale for this nursing practice
Guidelines and rationale for this nursing practiceTwo nurses, one of whom must be qualified, or the nurse and a medical practitioner are required to carry out this practice.
▪ explain the nursing practice to the patient to gain consent and co-operation. Patients should be encouraged to be active partners in their care
▪ ensure the patient's privacy to maintain dignity and a sense of self
▪ administer analgesia if it is prescribed by the medical practitioner to manage pain
▪ collect the equipment for efficiency of practice
▪ prepare and assist the patient into a suitable position that is as comfortable as possible to allow clear access to the drain site
▪ observe the patient throughout this activity to detect any signs of discomfort and distress
▪ remove the dressing from the drain site
▪ tell the patient to take 3 deep breaths and then hold their breath while the drain is removed to equalize intrapulmonary pressure
▪ when the drain has been removed, smoothly and firmly, the assistant will quickly tie the previously placed suture to close the wound and form an airtight seal around the wound
▪ tell the patient to breath normally
▪ order a chest X-ray to ensure that the lung is functioning normally
▪ ensure that the patient is left feeling as comfortable as possible, to maintain the quality of this practice
▪ dispose of the equipment safely for the protection of others
▪ document the nursing practice, monitor the after-effects and report any abnormal findings immediately to provide a written record and assist in the implementation of any action should an abnormality or adverse reaction to the practice be noted
▪ in undertaking this practice, nurses are accountable for their actions, the quality of care delivered and record-keeping according to the Code of Professional Conduct: Standards for Conduct, Performance and Ethics (Nursing and Midwifery Council 2004) and Guidelines for Records and Record Keeping (Nursing and Midwifery Council 2005).
Ensure that the tubing is not being compressed or kinked by the patient lying on it, as this will cause the equipment to function inefficiently. It is imperative that the drainage bottle is kept below the level of the patient's chest, unless double-clamped, or there may be a backflow of fluid into the pleural cavity.
When the drain is being removed, care must be taken to prevent a pneumothorax (i.e. the entry of air into the pleural space).
Because of breathlessness, the patient may have difficulty in talking. A pencil and paper may help communication with staff and visitors, and the nurse call system should always be to hand to summon assistance if necessary.
Analgesics may be prescribed to help relieve any pain or discomfort.
If the equipment is functioning correctly, the patient's respiratory rate should gradually return to the normal range after the drain has been inserted.
The patient's respiration should be closely monitored after the removal of the drain so that the potential complication of pneumothorax can be quickly detected.
Some assistance with washing and dressing may have to be given to those who are attached to underwater seal drainage equipment as their mobility is reduced. Light, loose clothing should be worn so that breathing is not unduly impaired.
Movement will be restricted by the equipment, but the patient should be encouraged to be as independent as possible.
The patient's normal sleeping pattern may be altered because of difficulty with breathing and because of the presence of the equipment, so the nurse should take measures that help to induce sleep.
 Patient/carer education Key points
Patient/carer education Key pointsThe patient should be given clear information about the procedure to ensure they are able to give informed consent and to encourage their participation in care. The patient and carers should be informed of the need to keep the drainage system below the level of the chest. Specific information about mobilising safely should also be given. Written educational leaflets should also be available. The patient should be encouraged to report any problems such as pulling of the tube or increased dyspnoea. Adequate pain relief should be available to the patient. Patients should be informed of the nursing observations that will be made when the chest drain is in place to alleviate anxiety.
References
L Allibone, Nursing management of chest drains, Nursing Standard 17 (22) (2003) 45–56.
C Brooker, M Nicol, Nursing adults: the practice of caring. (2003) Mosby, Edinburgh .
D Laws, E Neville, J Duffy, BTS guidelines for the insertion of a chest drain, Thorax 58 (2003) 53–59.
Nursing and Midwifery Council, Code of professional conduct: standards for conduct, performance and ethics. (2004) NMC, London .
Nursing and Midwifery Council, Guidelines for records and record keeping. (2005) NMC, London .
C Parkin, A retrospective audit of chest drain practice in a specialist cardiothoracic centre and concurrent review of chest drain literature, Nursing in Critical Care 7 (1) (2002) 30–36.
British Thoracic Society: http://www.brit-thoracic.org.uk
Thorax Online: http://www.thorax.bmjjournals.com
1. Describe the indications for chest drain insertion.
2. Consider what you would say to a patient to prepare them for chest drain insertion.
3. What aspects of the procedure might pose an infection control risk?
4. What observations would you make on the patient who has a chest drain in place?
5. How would you know if the chest drainage system could be removed?
