Pediatric Computed Tomography
Son Nguyen* and Scott Lipson
The objective of the pediatric computed tomography (CT) examination is to acquire optimum diagnostic images with the minimum discomfort and radiation exposure to the patient. To this end, two basic tenets apply: (1) the technologist should be knowledgeable and well prepared and (2) the technologist should be honest and upfront with the patient and family. A well-prepared technologist plays an important role in avoiding delays and helps reduce the time the patient must be on the table of the CT scanner.
The CT technologist taking care of children should be honest in terms of the exact details of the CT examination. This helps ensure the cooperation of young patients and their parents during the procedure. The results can be successful, especially when the patient and parents are well informed. In most institutions, parents are encouraged to remain in the CT room during the examination.
In addition, a relaxed, nonthreatening environment helps gain the confidence and cooperation of the pediatric patient. Toys, books, and puzzles are a welcome diversion for the child who is waiting for a CT examination. In the CT room, interesting posters (Fig. 19-1) or pictures hung on the walls or ceiling help provide a friendly atmosphere. Young children are encouraged to bring a favorite blanket or cuddly toy with them for reassurance.
Fortunately, the current generation of multidetector CT (MDCT) scanners has made the CT examination much shorter and better tolerated by children. A trained CT technologist enlisting the cooperation of the parents is now able to scan the majority of children quickly, painlessly, and without sedating them.
MULTIDETECTOR CT
Differences Versus Single-Detector CT
MDCT is fundamentally different from single-slice spiral CT (SSCT). With SSCT a single detector is present. The x-ray tube rotates around the patient, and a single image is produced for every rotation. The slice thickness of the image is determined by beam collimation. An MDCT scanner, however, contains multiple detector elements and can therefore generate multiple images from each rotation of the x-ray tube. Current CT scanners can yield up to 64 images per rotation. Image slice thickness is determined not by beam collimation but by the size of the detector elements that are used during the scan acquisition.
The size, number, and arrangement of detector elements are different for each scanner. Some scanners have detector elements that are of uniform size throughout the entire detector, whereas other scanners may contain central elements that are smaller and more peripheral elements that are larger. Detector elements may be combined to produce thicker slices and more coverage or used individually for higher-resolution images. The num-ber of data channels present in the scanner determines the maximum number of images that can be produced per rotation. Each channel can use information from a single row or multiple detector rows. The scanner is named by the number of data channels present (e.g., a 16-slice scanner has 16 data channels capable of producing up to 16 images per gantry rotation). This scanner will have more than 16 rows of detector elements, however, because more than one row may be combined into a single channel.
Advantages of Multidetector CT in Pediatric Imaging
Advantages of MDCT are substantial for pediatric imaging. Faster scanners allow for substantially more rapid acquisition of data, producing better patient tolerance, reduced motion artifacts, and better use of contrast media. This is particularly important in pediatric imaging, where motion is a constant issue and scan time is of the essence. In addition, there is substantial improvement in spatial resolution. These qualities make MDCT especially useful in multiplanar and volume reconstructions and have opened up a plethora of new applications. Volumetric data acquisitions with very thin slices produce data sets that can be reconstructed in any plane with virtually no loss in image quality. This makes patient positioning for examinations easier and eliminates the need to obtain direct coronal images for examinations such as sinuses, temporal bone, and extremities. This helps keep radiation dose lower in children.
One inherent disadvantage with MDCT scanning is that the radiation dose may be increased when submillimeter slices are acquired. These thin slices will increase the effects of dose buildup of the radiation penumbra (the radiation penumbra is that portion of the radiation from a point source that falls outside the detector opening and therefore contributes to patient radiation dose but does not contribute to image formation). The thinner the slices, the more the penumbra effect can increase dose. This effect is dependent on the number of slices acquired per rotation and can be significant with four-slice scanners but is small with 16-slice scanners and negligible in 32- and 64-slice scanners.
New Pediatric Applications Possible with Multidetector CT
Many new applications and techniques for pediatric imaging are now possible with MDCT because of the ability to acquire thinner images in a shorter duration. These include three-dimensional (3D) volume- and surface-rendering techniques, allowing the radiologist to look at 3D relationships of anatomical structures, airway reconstructions, virtual bronchoscopy, and colonoscopy. CT angiography (CTA) by use of MDCT has blossomed, with detail never before possible. CTA has virtually replaced conventional angiography in many areas, including evaluation of the aorta and pulmonary arteries. CTA is useful in pediatric imaging, especially to delineate aortic arch anomalies, cardiac anomalies (before and after surgery), and aberrant vasculature, such as in cases of pulmonary sequestration or vascular malformations. Cerebrovascular evaluation for aneurysms and vascular malformations is also helpful. Because of the speed of MDCT, it is frequently possible to obtain images with reduced contrast dose compared with older scanners. CTA offers many advantages compared with catheter angiography. It is noninvasive and safer and radiation dose is lower. CTA also allows evaluation of structures adjacent to and outside of the vasculature.
Another major growth area is orthopedic imaging. Characterization of fractures and congenital abnormalities of the skeletal system is greatly improved with advanced visualization techniques. MDCT allows for a single volumetric data set to be produced and reconstructed in any plane or projection. It is no longer necessary to scan patients in more than one plane. Current-generation scanners generate much less artifact in patients with metal hardware in place and are useful to evaluate patients who have undergone surgery with internal fixation devises.
ROLE OF THE CT TECHNOLOGIST
Pediatric patients need constant attention and monitoring. The technologist should work to ensure that the scanner is ready when the patient arrives and needed information such as clinical history and scan protocol has been determined. This will minimize delays and distractions that can interfere with the technologist’s duty to care for the patient (Box 19-1).
The parents are usually an important ally of the technologist and should be included in the process whenever possible. One parent can be given a lead apron and remain in the room with the child during the entire procedure. This frequently helps reduce anxiety of both the child and the parent. If no parent is available, other ancillary staff such as nurses or assistants may be able to fill this role and comfort the child. The principal duty of the technologist, however, is to ensure that the scan is done safely, quickly, and accurately.
Neonatal Patients
To minimize the risk of infection to the neonatal patient, CT personnel who handle the infant should remove rings and watches, wash hands thoroughly with antibacterial soap, and always wear a cover gown. During the scanning procedure, it is important to maintain the infant’s body temperature. This can be achieved by increasing the temperature in the CT scanning room before the arrival of the patient, wrapping the infant in a warm blanket, and covering the infant’s head with a cap or small towel to prevent rapid heat loss. Equally important is placing a heating blanket under the infant positioned on the scanning table or focusing a heat lamp on the patient with special attention to the correct distance of the lamp from the patient. Finally, a nurse who accompanies the patient to the radiology department should monitor the patient’s vital signs and body temperature throughout the CT examination.
Sedation
The use of sedation is inevitable in pediatric CT scanning. Image degradation from patient motion remains a problem. The introduction of MDCT has been a tremendous advance in pediatric imaging. Most scans can be completed in less than 30 seconds, and with current 16- to 64-slice scanners, scan times as short as 5 to 10 seconds can be routinely achieved while the highest image quality is maintained. This substantially decreases the need for sedation.
With MDCT sedation is rarely required for routine head and sinus studies, where some motion is tolerable. Sedation may still be required for studies requiring advanced multiplanar and volume reconstructions because motion artifact can significantly reduce the quality of these types of studies. Common examples would include studies of the temporal bone and CTA.
Sedation protocols and standards should be cooperatively established by the departments of radiology and anesthesiology to ensure high-quality care for the sedated patient. Any syndrome or condition with a respiratory risk that contraindicates sedation is recorded and brought to the attention of the radiologist. The decision to sedate a child should be a cooperative effort of the radiologist, the nurse, and the child’s parent. Factors affecting the decision to sedate are summarized in Box 19-2.
Preparation for sedation requires patients to ingest nothing by mouth 4 to 6 hours for solid foods, 2 to 4 hours for formula or breast milk, and 2 hours for clear liquids before the examination. CT department personnel should inform parents of the correct preparation and sedation instructions at the time the examination is scheduled to help minimize any misunderstanding on the day of the examination. Any child who potentially may need sedation should be given preparation instructions for this at the time of scheduling. When the patient arrives in the radiology department, the CT technologist or the radiology nurse performs a careful assessment of the child’s ability to undergo the CT examination without sedation.
Children less than 6 months of age rarely require sedation. Wrapping them in a warm blanket and providing them with a pacifier and use of a table restraint system to immobilize them can be all that is needed for a successful scan. Sleep deprivation is another technique that can be used with infants. With faster scanners, good patient communication, and the proper use of restraints, the need for sedation can be minimized.
For older infants and toddlers requiring sedation, oral or rectal chloral hydrate is the most commonly used drug. The typical starting dose is 50 to 75 milligrams (mg) per kilogram (kg) to a maximum dose of 100 mg/kg. This is generally effective and can be routinely administered by a radiology nurse under the direction of a radiologist.
Children older than toddler age can usually be talked through a CT study with the help of a parent. When this does not work, oral or intravenous (IV) midazolam (Versed) with or without morphine may be used for conscious sedation. Some children and toddlers may not adequately respond to these drugs and will require deep sedation with drugs such as IV pentobarbital sodium (Nembutal). This group may also include children with delayed development, sleep apnea, or chronic respiratory problems. Pentobarbital is generally administered by specially trained personnel such as a dedicated pediatric sedation team or anesthesiologists.
All sedation patients require continuous monitoring by nursing staff including pulse oximetry, blood pressure, and respiratory rate. Paradoxical hyperactivity and agitation is a side effect of chloral hydrate and has been reported with pentobarbital sodium as well. When this does occur, it is necessary to keep the child safely under observation until the effect passes.
Resuscitative supplies are kept in the CT scan room at all times. When the study is completed, the sedated child is moved to the recovery room for monitoring. Patients are discharged when they are easily aroused, have enough muscle tone to hold up their heads, and can drink clear fluids. The parents are given an information sheet about care of the sedated child that includes a telephone number to call if they have any concerns after their return home.
Immobilization
Immobilization of the child is essential to ensure patient safety and to provide images free of motion artifacts. For patients less than 5 years old, the immobilizer (Fig. 19-2) is a comfortable device that secures the patient’s arms beside the head during body examinations. This device is secured to the patient scanning table with adhesive straps after the patient has been positioned.
Larger children are generally immobilized by other methods, such as adhesive straps placed under the mattress and over the patient. After the patient has been immobilized, the CT technologist should still carefully monitor the child by closed-circuit television or direct visualization.
Some time of immobilization is important in nearly every case. Sedated children should be gently immobilized with soft straps or paper tape. Cooperative older children should also have immobilization to help remind them not to move.
Use of Intravenous Contrast Media
The routine use of nonionic contrast media almost eliminates minor reactions such as pain, nausea, vomiting, and urticaria. This is especially important in pediatric CT, and the use of nonionic contrast media is therefore recommended in those examinations requiring contrast media. The removal of these potential reactions and discomforts helps ensure the cooperation of the patient and provides a safer examination for the sedated child. Fortunately, severe allergic reactions to contrast media are rare in children. Informed consent should be obtained before IV contrast injection.
The dose of contrast material for children is 2 to 3 milliliters (ml)/kg to a maximum of 150 ml. Power injectors are now commonly used because they provide a constant rate of injection that allows more accurate timing of the bolus and better organ enhancement. The deciding factor for use of a power injector depends on the IV site and size. Only peripheral IV sites can be obtained on most children. The injection rate is determined by the size of the IV catheter; injection rates of 2-3 ml per second can be used with 22-gauge catheters, whereas a 24-gauge catheter can be injected at 1 to 2 ml per second. Butterfly-type needles and percutaneous indwelling central venous catheter lines are almost always hand injected rather than by use of power injectors.
Scan timing is very important for contrast enhanced imaging, particularly of the neck, chest, and body. Unlike in adult patients where routine scan delays are effective in most people, scan delay in children must be individualized depending on the size of the child, the site of the IV, the injection rate, and the duration of the scan. If a power injector is used, standard delays can be used in most patients. For neck and chest examinations, delays of 35 to 45 seconds are effective. For studies of the abdomen and pelvis, longer delays of 50 to 70 seconds are used. Infants generally require shorter delays because the volume of contrast injected is so small. When hand injection is used, the scan should start when the injection is almost complete. Timing for contrast-enhanced studies of the brain is less critical. These scans are usually begun after all of the contrast has been given.
Another option to determine scan delay to produce optimal vascular enhancement is available on most MDCT scanners (e.g., Toshiba’s SureStart, General Electric’s SmartPrep, Phillips Dose-Right). This software uses bolus-tracking to trigger the start of the scan. The operator places a region of interest (ROI) on a vessel or organ at the start of the study. Contrast injection is begun and serial low dose scans are performed in the same location. The enhancement curve is tracked in real time. The scan can be triggered automatically when the Hounsfield units (HU) reach a predetermined threshold or manually by the technologist on the basis of the visual appearance of the vessel. In children manual triggering is usually preferred because the small size of the vessels may make automatic triggering unreliable if the child moves at all. Bolus tracking is the preferred method to initiate the scan for CT angiography, but it can also be useful for scans of the neck, chest, and abdomen. One disadvantage of this technique is increased radiation dose to the region where the monitoring scan is performed.
Regardless of the injection type, it is important to monitor the IV site during injection. If manual injection is used, filling the contrast medium into smaller syringes facilitates injection compared with the use of a large syringe.
Radiation Protection
Growing cells are the most sensitive to radiation. For any particular milliamperage (mA), pediatric organ doses are higher compared with those of an adult. Because of these factors, and the cumulative effect over a lifetime of exposure, radiation exposure has a potentially higher risk for the pediatric patient than for the adult patient. It has been shown that even small radiation doses carry the same relative risk of cancer mortality as low-dose exposure for atomic bomb survivors. These radiation doses are in the range typically seen with CT scans with adult scan parameters not adjusted for children. Therefore, radiation protection is an integral part of the pediatric CT examination. The ALARA principle should be followed, in that radiation dose should be kept as low as can be reasonably achieved.
This issue has generated substantial interest in both the popular press and the radiology literature. It is the responsibility of every person involved with imaging pediatric patients to make sure that diagnostic scans are obtained with the minimum radiation dose. This goal requires a comprehensive approach that addresses all aspects of the CT examination from ordering procedures to examination planning to specific examination parameters chosen by the technologist at the CT console.
Scan Planning and Preparation: Radiation exposure control begins with a careful review of all orders to ensure that the study is indicated and appropriate. Some requests may need to be redirected to ultrasonography or magnetic resonance imaging (MRI), depending on the indication. Additional clinical information from the ordering physician may be needed to ensure that the proper study is performed the first time.
Once it is determined the examination is necessary, the proper protocol must be chosen. Coverage should be limited to the area of interest. Multiphase scans should be minimized in children. Scans both with and without contrast should not be performed routinely. Pediatric specific examination protocols should be created and used. Lead shielding should be routinely used to cover body parts that are outside the ROI. Particular attention should be made to avoid scanning sensitive areas such as the breasts, genitalia, and lens whenever possible.
Scan Parameters: Particular attention must be paid to many different scan parameters in order to minimize dose. Factors such as tube current (mA) and peak kilovoltage (kVp) have an obvious effect on radiation dose, but many other variables used in spiral/MDCT such as pitch, slice thickness, and rotation time can also significantly affect dose.
Increasing pitch is an effective way to decrease dose. A pitch of 1.5 can lower the dose by about 25% compared with a pitch of 1, whereas a pitch of 2 can reduce the exposure by about 50%. Shorter rotation times will also decrease dose. A rotation time of 0.5 seconds gives half the dose of a 1-second rotation time if all other parameters are constant. With MDCT scanners, very thin slice thickness (less than 1 millimeter [mm]) can result in increased dose secondary to overlapping of the radiation penumbra. This effect can be significant with four-slice scanners but is minor in scanners with 16 or more slices. Care should be used when acquiring submillimeter scans on a four-slice machine.
Slice thickness may be a consideration in pediatric patients. One inherent disadvantage with MDCT scanning is that the radiation dose may be increased when submillimeter slices are acquired. These thin slices will increase the effects of dose buildup of the radiation penumbra. The thinner the slices, the more the penumbra effect can increase dose. This effect is dependent on the number of slices acquired per rotation and can be significant with four-slice scanners but is small with 16-slice scanners and negligible in 32- and 64-slice scanners. In fact, 64-slice scanners can produce images of superior quality compared with scanners with fewer detectors with the same radiation dose (same scan parameters). Facilities using four-slice scanners should use submillimeter slices with caution in children.
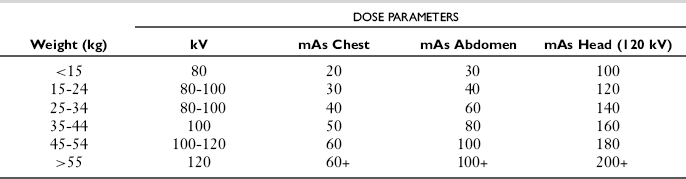
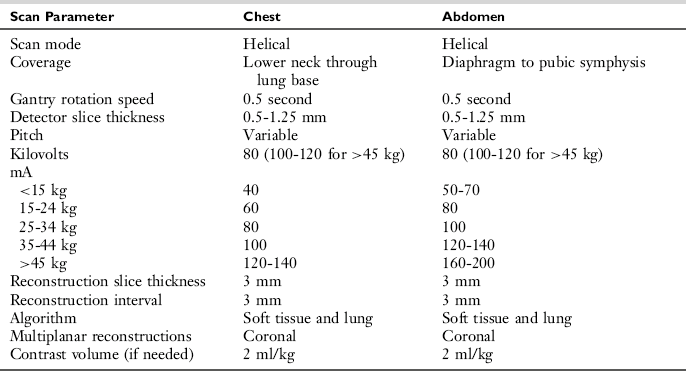
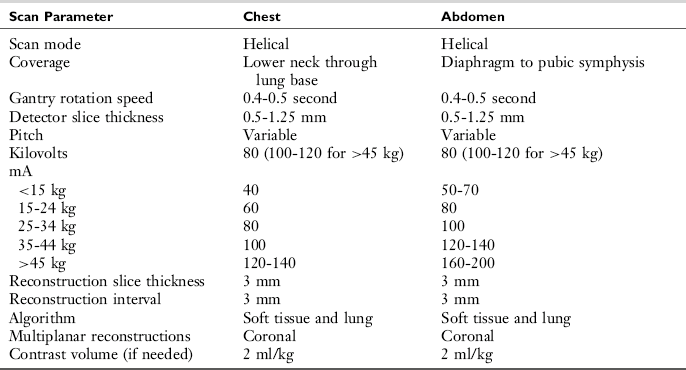
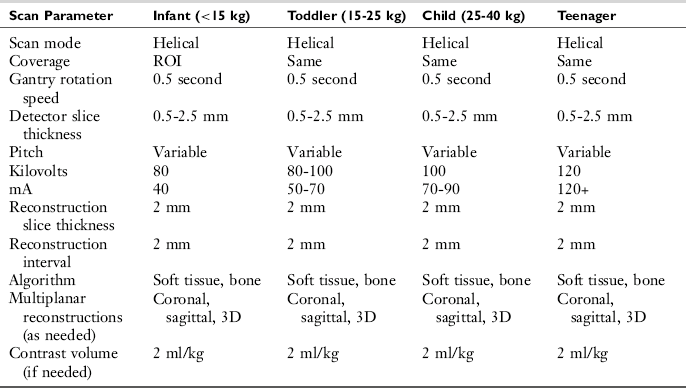
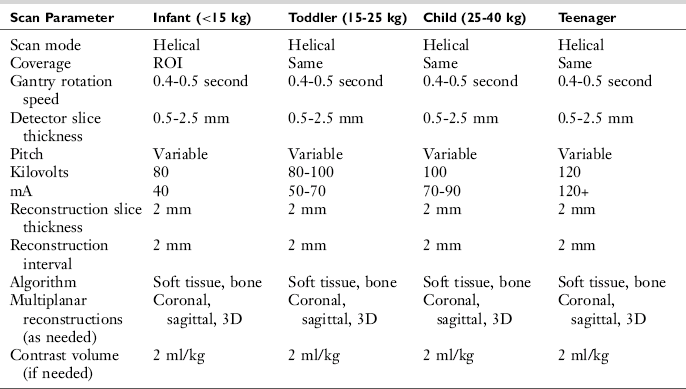
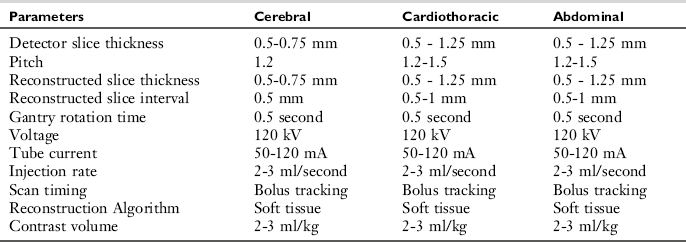
Modification of dose parameters is the most straightforward and important method to reduce dose. There are two primary methods to optimize CT dose parameters. The first way is for the CT technologist to individually tailor the dose parameters for each patient on the basis of the patient’s weight and the body part being imaged (Table 19-1). Alternatively, multiple different protocols can be created in the scanner for each type of examination on the basis of the patient’s size/weight with appropriate kVp/mA parameters built into each protocol. Although this approach can be effective if the protocols are built and followed correctly, it is somewhat cumbersome and is easily subject to error if the technologist chooses the wrong protocol.
Recognizing the limitations of the previous methods, CT manufacturers have focused much attention on methods to control, monitor, and reduce the radiation dose from CT examinations. As a result, most MDCT scanners now have some form of automatic exposure control available. There are different techniques used by the CT manufacturers, but the basic principles are similar. The most common approach relies on attenuation measurements derived from the actual patient obtained during scout image acquisition to create a radiation dose profile for the examination that is individually tailored to that patient. The dose will actually vary during the examination depending on the attenuation of the body. For example, in a chest study the radiation dose will be much higher through the shoulders and much lower through the lungs. The most sophisticated systems now allow the operator to select appropriate image quality on the basis of noise levels and the scanner and then apply the appropriate tube current regardless of patient size. This relieves the operator of the need to vary conditions on the basis of patient size or weight.
Finally, it is important to have a quality assurance program to consistently monitor the entire process to ensure that protocols are up to date, scan techniques are optimized, technologists understand and follow the protocols, and the CT scanner is properly maintained and tested with phantoms. Steps used to minimize radiation dose in children are summarized in Box 19-3.
CT OF THE HEAD, NECK, AND SPINE
Imaging of the head and spine in children depends on a number of factors, including the age of the child, medical condition, ability to cooperate, and above all the indication for the examination. These factors will determine which modality is best suited to the overall assessment of the patient’s medical problem. The majority of neuroimaging examinations in children are performed with CT or MRI. The main exception to this is the neonate, in whom ultrasonography is the dominant imaging technique. Plain films have a small role, usually for the spine. Indications for diagnostic pediatric neuroangiography are limited and have been replaced by magnetic resonance angiography (MRA) and CTA. Catheter angiography is primarily a therapeutic tool used to treat children with aneurysms and vascular malformations.
Indications
With some exceptions, most indications for examination of the central nervous system (CNS) are best studied by MRI. MRI retains several advantages over CT for neuroimaging. MRI uses no ionizing radiation and has inherently better soft tissue contrast that can be used to characterize normal anatomy and pathology of the CNS. CT has several advantages over MRI, primarily speed of acquisition and accessibility. CT is also superior to identify acute hemorrhage and calcifications and to characterize abnormalities of the bone.
CT of the Brain: Primary indications for CT over MRI include assessment of trauma in the acute phase (Fig. 19-3), detection of acute hemorrhage, and the detection of calcification such as in cases of prenatal TORCH (toxoplasmosis, other [congenital syphilis and viruses], rubella, cytomegalovirus, and herpes simplex virus) infections or postnatal infection such as cysticercosis. CT is also recommended for skull lesions and fractures (Fig. 19-3).
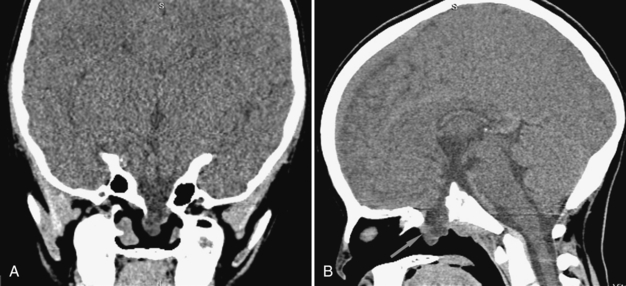
FIGURE 19-3 Sphenoidal encephalocele. High-resolution 0.5-mm coronal (A) and sagittal (B) images in soft tissue window. There is a left parasagittal defect in the sphenoid bone with herniation of meninges and cerebrospinal fluid into the sphenoid sinus. The pituitary tissue is shown at the bottom of the encephalocele (arrow).
Either CT or MRI can adequately evaluate many other indications for brain imaging. In these instances CT is often preferred because it is quicker and easier to obtain and often can be done without sedation. Common indications include evaluation of hydrocephalus and shunt malfunction, screening evaluation for children with headaches or abnormal head size, and evaluation and follow-up of children with congenital abnormalities such as Chiari malformations or Dandy-Walker syndrome.
MRI is the preferred modality for evaluation of many other indications such as seizures, known or suspected brain tumors, acute and chronic ischemia, most CNS infections and inflammatory diseases, vascular malformations, congenital syndromes such as neurofibromatosis and tuberous sclerosis, diseases of white matter and demyelination such as acute disseminated encephalomyelitis (ADEM), and evaluation of the pituitary gland. Although MRI may be the study of choice in most instances, CT is frequently performed in these patients either in the acute setting when the child is in the emergency department or for follow-up after the initial evaluation and treatment. CT can also serve as the primary evaluation modality when MRI is not available.
CT of the Face and Neck: Primary indications for CT include assessment of facial and orbital trauma, evaluation of osseous abnormalities of the maxilla or mandible, assessment of the temporal bone and middle ear in children with infection or hearing loss, evaluation of the sinuses for sinusitis, and evaluation of the airway. Either CT or MRI may be performed to evaluate the face and neck to characterize masses, enlarged lymph nodes, salivary gland evaluation, and infectious processes.
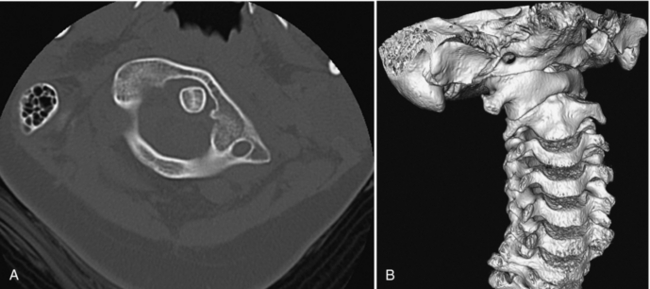
CT of the Spine: CT is primarily used to evaluate suspected spinal trauma. CT is also useful to characterize congenital bony abnormalities such as scoliosis, lesions of the vertebral bodies, and osteomyelitis (Fig. 19-4). MRI is the primary modality for evaluation of the spinal cord and tumors of the cord and canal. Evaluation for disk conditions is uncommon in pediatric patients but is preferable with MRI.
Patient Positioning
When positioning the patient for CT of the brain and face, it is essential to have the patient’s head geometrically centered in the gantry to ensure artifact-free images. In this respect, the patient’s head must be centered accurately from right to left in the head holder and from front to back in the gantry. Multiple small positioning sponges can be used to secure the patient’s head in the head holder. For the accurate assessment of midline structures, care must be taken to position the head so that the right and left sides are symmetrical and not tilted.
Direct coronal images are important for evaluation of structures such as the orbits, sinuses, and temporal bone. When older-generation scanners are used, it is still important to obtain direct coronal images for these examinations. Newer MDCT scanners, particularly 16-slice and 64-slice scanners, have obviated the need to obtain direct coronal images. A single high-resolution data set can be reconstructed into any plane.
The coronal position is usually comfortable for the pediatric patient and is easily achieved with even sedated children. Patients are placed prone with the chin extended forward. The CT gantry is tilted to obtain images in the coronal plane. Occasionally, a patient cannot tolerate the coronal position. An alternate position is a Water’s view, in which the patient’s head is extended to maximum tolerance. With the aid of a scout view, the scans are prescribed as close to 90 degrees to the clivus as possible.
Technical Considerations
Scans of the brain can be obtained with either conventional sequential axial images or with the helical technique. Some radiologists have traditionally felt that sequential technique produces images that are sharper with better contrast. This technique requires a very cooperative or sedated child and is particularly susceptible to motion artifacts. Helical scanning offers many benefits. The scans are quicker, less sensitive to motion, and generate fewer partial volume and streak artifacts, and, above all, high-resolution data sets can be obtained that can be reconstructed into different planes. With current-generation MDCT scanners it is generally possible to obtain image quality from helical scans that is equal or nearly equal to that of sequential scans. For these reasons, we prefer to use helical scanning in the brain for pediatric patients.
Scans of the face, sinuses, temporal bone, neck and spine should all be obtained helically for obvious reasons. Multiplanar images should routinely be generated and reviewed in these cases.
Most pediatric neurological scans can be performed without contrast. The most common indications such as trauma, headaches, and hydrocephalus do not require contrast. Certain indications such as known or suspected infection or neoplasm do benefit from contrast administration. When the brain is imaged, scans before and after contrast are generally obtained in these patients. However, for evaluation of the face and neck precontrast scans are usually not needed and will needlessly increase the radiation dose to the child.
Timing for contrast studies of the head and face is usually less critical than for body studies and CTA. Contrast can be administered by either hand injection or power injector and the scans begun once all the contrast is injected. If a rapid injection is performed, an additional 10- to 20-second delay should be applied before the scan is started.
As in all pediatric CT examinations, the technologist must be careful to ensure that scan parameters chosen for the study are appropriate to the size and age of the child.
Scanning Protocols
Scanning protocols are usually established to include information that covers data acquisition and reconstruction and image transfer. These protocols are intended to assist the technologist performing the CT examination and generally help increase the overall efficiency of the examination. Comprehensive examination protocols help ensure that the proper study is performed and minimize wasted time for both the technologist and the radiologist.
Acquisition parameters include patient position, prescan localization (scout view), scan range, acquisition slice thickness, pitch, gantry rotation speed, and specific dose parameters. Dose parameters can be determined by the technologist on the basis of the patient’s age or weight or automatically chosen by the scanner by use of one of the automated exposure control programs. Reconstruction parameters include reconstruction algorithm (e.g., soft tissue, and bone), reconstructed slice thickness, and multiplanar or 3D reconstructions. The protocol should also describe which information is to be archived on PACS (picture archiving and communication system) or film and whether data should be sent to a 3D workstation for additional postprocessing.
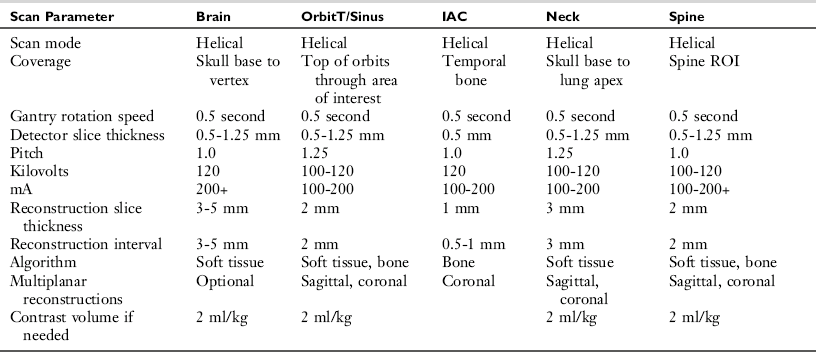
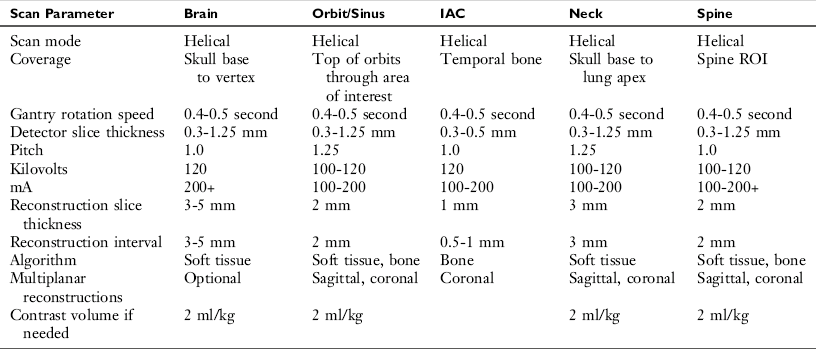
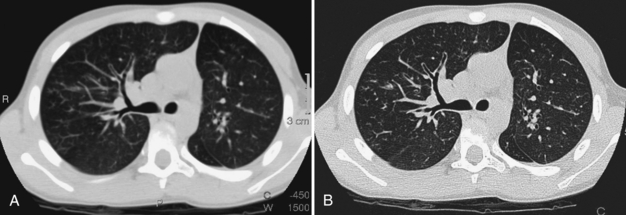
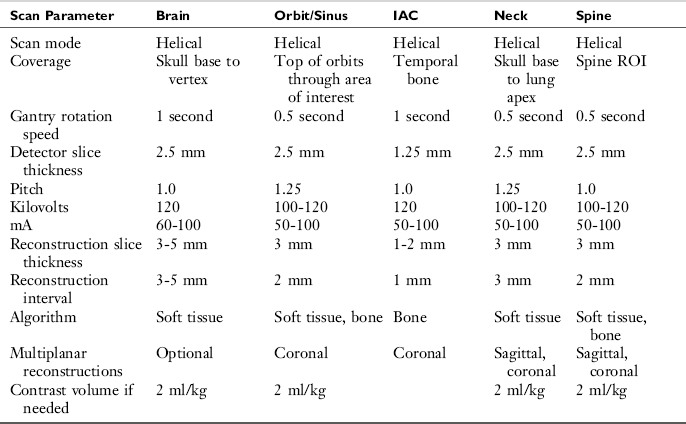
Tables 19-2 through 19-4 are examples of generalized protocols of the head, orbit/sinus, temporal bone/IAC (internal auditory canal), and spine used for four-,16-, and 64-slice scanners. These protocols are generalizations and must be modified for each scanner. On 64-slice scanners, the mAs can be decreased slightly compared with 16-slice scanners for a comparable result. All manufacturers have some differences in detector configuration, scan features, and reconstruction options.
TABLE 19-2
Pediatric Neurological Protocols: Techniques for Four-Slice Multidetector Computed Tomography
CT OF THE CHEST AND ABDOMEN
Body CT in children (unlike adults) is generally more of an ancillary imaging modality. Ultrasonography remains the primary screening modality for the abdomen and pelvis, but CT is a very important modality for many indications.
Indications
Trauma: CT is the modality of choice for examination of the abdomen after blunt injury or high-speed trauma to evaluate possible laceration of liver, spleen, pancreas, or kidney (Fig. 19-5). IV and oral contrast (through a nasogastric [NG] tube) should be used in trauma cases. It is usually not possible to give a substantial amount of oral contrast through an NG tube in an unconscious patient because of the risk of aspiration, but a small amount can be given to at least outline the duodenum.
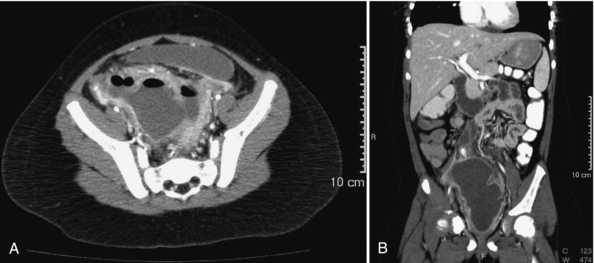
Infections: The most common infections where CT is used in children are pneumonia, pyelonephritis, and appendicitis. IV contrast is needed when there is a pleural effusion or empyema. Oral or rectal contrast, with IV contrast, is needed to evaluate appendicitis and possible abscesses (Fig. 19-6). CT is often used in postoperative patients to look for abscess.
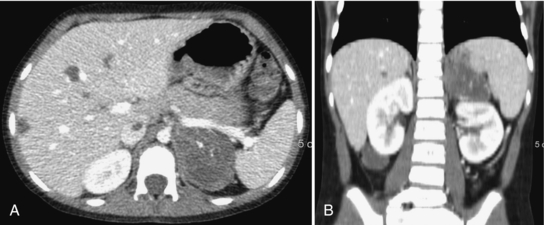
Tumors: CT is an integral part of the diagnostic workup and posttreatment assessment of pediatric solid tumors, including lymphoma (e.g., Burkitt’s or Hodgkins) and abdominal tumors (e.g., Wilms’ tumor of the kidney, neuroblastoma, rhabdomyosarcoma, and hepatoblastoma) (Fig. 19-7). The investigation of these oncological diseases generally includes a noncontrast chest CT to look for lung metastases. Chest CT for mediastinal disease requires a contrast examination because unenhanced mediastinal vessels may mimic masses or adenopathy on a noncontrast scan.
CT of the Chest: CT of the chest is used to evaluate central and peripheral airways, pulmonary nodules, vascular anatomy, lung parenchyma, and congenital masses (lung cysts, cystic adenomatoid malformations) (Fig. 19-8). CT is an excellent modality to assess foreign body aspirations, when the material is of low density and does not show up well on chest x-ray. MDCT is also used to evaluate the trachea for stenosis, malacia, and atresia with virtual endoscopy (Fig. 19-9). Because these evaluations are limited by the ability of patients to hold the breath for the scan, the use of this technology may be limited in pediatrics. CT for infections, pleural effusions, and malignancy should be with IV contrast.
High-Resolution CT: High-resolution CT is sometimes performed on the pediatric patient for the assessment of parenchymal lung disease such as cystic fibrosis or bronchiectasis (Fig. 19-10). However, in most cases bronchiectasis can be well seen by using conventional CT, so high-resolution CT is not necessary. This consideration is important because an increased radiation dose is required to acquire the thinner images in high-resolution CT.
Patient Positioning
The patient can be placed head or feet first into the scanner. Placing the patient feet first may be less intimidating for young children. This position also allows the parent or technologist a clear view of the child for monitoring and comforting. The patient must be centered correctly in the gantry, which may involve the use of immobilization sponges or blankets and tape.
Technical Considerations
For chest CT, shallow breathing in the young child will be adequate. Instructions for breath-hold may not work, and misregistration or motion artifacts are risked if the child takes another deep breath. Older children can be instructed to withhold their breaths, especially in high-resolution CT. Children on ventilators may be briefly taken off ventilation during image acquisition, provided they are monitored and can tolerate this action.
Scanning of the chest can be initiated by bolus tracking or can be started just before the end of contrast injection. Scans about 30 to 50 seconds after beginning injection will demonstrate adequate vascular enhancement in older children. In infants, this time frame will be shorter, with maximal enhancement probably around 10 to 20 seconds after the beginning of injection. In infants, abdominal scans should begin sooner than the usual 70- to 90-second delay of adult scans, probably right at the end of the contrast bolus.
For abdominal and pelvic CT scans, oral contrast should always be used if the patient can tolerate it. This is especially important in the evaluation of intra-abdominal abscess or bowel obstruction. A long (at least 2-hour) preparation should be performed for studies where there may be conditions of the colon. For trauma patients, a small amount of oral contrast can be injected through the NG tube to delineate the duodenum. Rectal contrast may be used in cases of appendicitis. About 250 ml of contrast is usually adequate to opacify the colon in this patient population (5-15 years old), or contrast can be instilled by gravity drip until the patient feels full.
Noncontrast CT scans can be used to evaluate renal stones. Delayed scans (5-10 minutes) are needed to evaluate hemangiomas/hemangioendotheliomas. Renal excretion of contrast peaks at around 3 to 5 minutes after injection. Delayed scans to evaluate urinary tract obstruction should therefore be longer than this period (around 10 minutes after injection), with the patient placed prone because the kidneys drain anteriorly.
Scanning Protocols
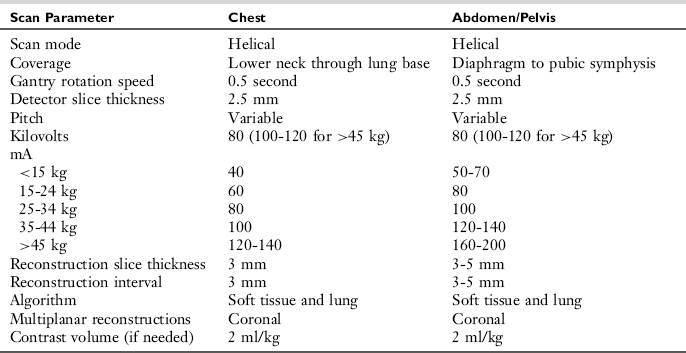
Protocols for pediatric CT of the chest, abdomen, and pelvis are summarized in Tables 19-5 through 19-7.
TABLE 19-5
Pediatric Chest and Abdomen Protocols: Technique for Four-Slice Multidetector Computed Tomography
MUSCULOSKELETAL CT
MDCT has had a significant impact on pediatric orthopedic imaging. Isotropic data acquisition with 3D reconstruction techniques has proved valuable for many different indications.
Indications
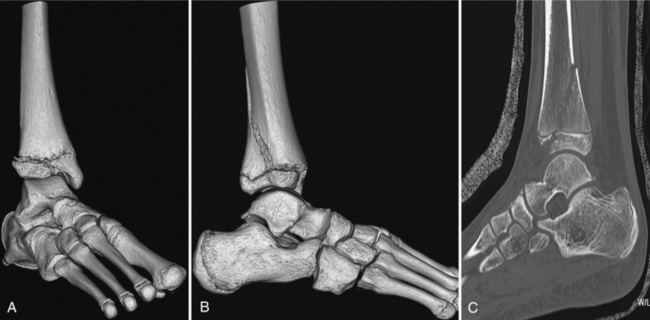
Complex Fractures: MDCT is the study of choice to evaluate complex fractures, particularly of the acetabulum/pelvis and the upper and lower extremities. Surface-rendered and multiplanar reconstructions can give the orthopedic surgeon a clear 3D picture of the fracture planes and are valuable in planning operative repair (Fig. 19-11). Segmentation of the images is very helpful to show the joint surfaces.
Tumors: Osseous tumors (e.g., Ewing’s sarcoma and osteogenic sarcoma) are best imaged with MRI, which can delineate soft tissue and marrow involvement much better than CT. CT is used to visualize the cortex itself, or calcifications (Fig. 19-12). It is not good at defining soft tissue involvement.
Infections: Osseous infections are best evaluated using bone scan or MRI. The infection must be fairly aggressive and advanced to produce bony changes. CT findings may therefore be absent in early stages of an infection. Soft tissue infections are also better evaluated by MRI. CT may be used to delineate soft tissue abscesses. IV contrast must be used.
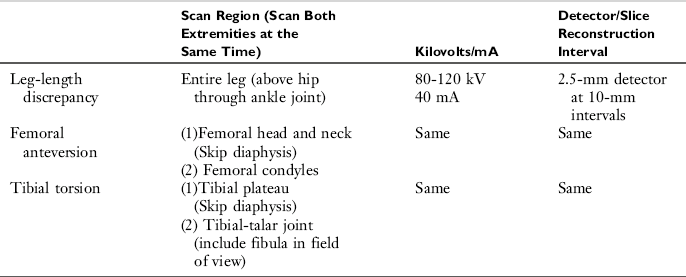
Deformities: CT can be used to evaluate femoral anteversion or tibial torsion and is also valuable in assessing congenital hip and shoulder dysplasias (Fig. 19-13). CT is also an excellent way to evaluate leg-length discrepancy. Imaging for this purpose can be done by using a low radiation dose method, which imparts lower radiation than the corresponding plain film study.
Patient Positioning
The area being imaged must be placed as close to the center of the gantry as possible and away from the body (if possible) to minimize scatter artifacts. For studies of deformities or leg-length studies, the ankles should be taped in the neutral (usually upright) position to eliminate movement and artifacts. Both legs should be as parallel to each other as possible. Always scan both extremities at the same time for leg length, tibial torsion, and femoral anteversion studies.
Technical Considerations
Because most cases of osseous tumors and infections are better evaluated by MRI, it should always be considered whether MRI is the more appropriate examination for the patient. IV contrast should be used whenever there is a question of soft tissue mass or infection. Contrast generally does not help for evaluation of the bone.
MDCT has eliminated the need to scan patients in multiple planes. A single isotropic acquisition can be performed and reconstructed to the desired planes on the scanner or workstation. It is therefore very important to use thin slice images whenever possible. Scans should be reconstructed with both a soft tissue and a bone filter. Bone algorithm produces higher quality multiplanar reconstructions, but the soft tissue algorithm produces smoother, better-looking 3D images.
Scans for alignment (e.g., tibial torsion) and leg-length studies can be done with a minimal radiation dose because high bone detail is not needed in these types of studies. All patients should have aggressive shielding of the body adjacent to the area being scanned.
Scanning Protocols
Generalized protocols for musculoskeletal CT are presented in Tables 19-8 through 19-10.
CT ANGIOGRAPHY
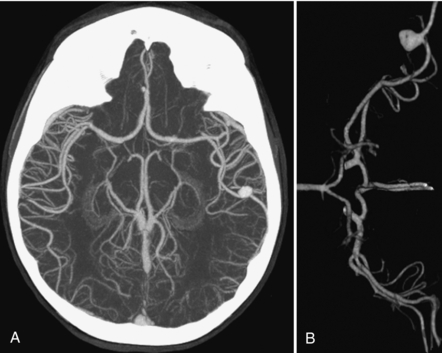
CTA and MRA have replaced diagnostic catheter angiography in children for almost all indications. Advantages of MRA include no ionizing radiation and no need for iodinated contrast. CTA, however, is much faster (better patient tolerance, less motion artifact) and has higher spatial resolution, which is important to evaluate small vessels in infants and children.
Indications
CTA is useful throughout the head and body primarily to evaluate vascular anomalies such as aberrant vessels, aneurysms and vascular malformations, and manifestations of congenital or acquired diseases such as sickle cell anemia, vasculitis, and thrombotic states (Figs. 19-14 and 19-15). CTA is also the test of choice for traumatic vascular injury.
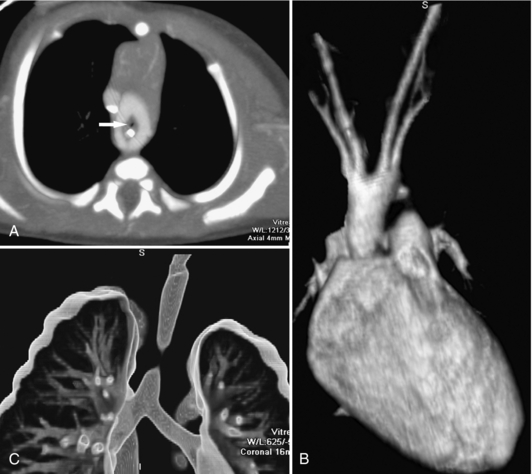
FIGURE 19-14 Complete vascular ring with tracheal compression. A, A 10-mm thick axial maximum intensity projection image demonstrates a complete vascular ring. The trachea (white arrow) is seen as a tiny dot of air. The esophagus has a high-density NG tube within it. The volume-rendered image (B) demonstrates a double aortic arch. The two arches are nearly symmetrical and both give rise to a subclavian and a carotid artery. Thin slab (11 mm) volume-rendered image with high transparency (C) shows a very high-grade tracheal compression resulting from the vascular ring.
Patient Positioning and Preparation
High-quality CTA requires motion-free images for 3D reconstructions. To this end, proper immobilization of the patient is essential. Infants can usually be immobilized without the need for sedation. Toddlers and young children may require sedation to obtain a good-quality study. CTA in older children can often be performed without sedation if proper coaching and parental support is provided. Older children should also be coached in breath holding, which is particularly important in chest studies.
For studies of the abdomen, it is important that patients do not receive any oral contrast because this will interfere with 3D reconstructions.
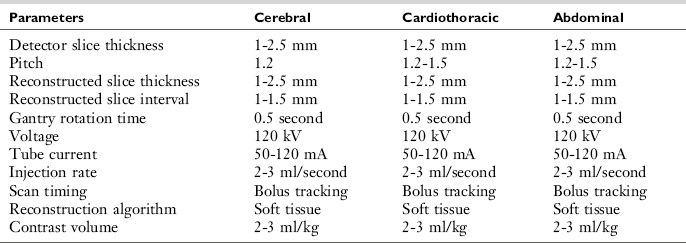
Technical Considerations
Successful CTA requires optimization of scan technique and contrast administration. Speed is important for image acquisition to minimize motion artifacts and maximize coverage and contrast density. The shortest rotation time available on the scanner should be used. Pitch values of 1.25 to 1.5 will also reduce scan time. Slice thickness is a tradeoff between resolution and scan time (coverage). This can require a difficult decision with a four-slice scanner but is usually not a factor with 16-slice scanners. In general, the thinnest slice thickness that will allow adequate coverage within an appropriate scan time should be used.
Proper delivery of contrast media is essential for CTA. Power injection with a rate of at least 2 ml per second (3 ml/second is preferred) is strongly recommended. This can be easily achieved with a 22-gauge peripheral IV and occasionally achieved with a 24-gauge IV if the catheter is in an adequate vein. Hand injection and butterfly needles are not recommended for CTA. High-density contrast such as 350 to 380 mg of iodine per ml is also recommended because this will improve vascular enhancement.
The timing of the scan should be initiated with bolus-tracking software whenever possible because this will minimize the chance of error caused by mistiming the bolus. Scans can be triggered either manually on the basis of the visual appearance of the vessel or automatically when a certain threshold for HU is achieved. Empirical delays can also be used but will need to be varied depending on the size of the patient, the body part scanned, the IV site, the injection rate, and the presence of certain medical conditions such as heart disease.
After the scan, the thinnest slice thickness available should be reconstructed on the scanner and sent to PACS or the 3D workstation to allow for postprocessing of the images. Overlapping reconstructions are also helpful to improve reconstruction quality if the slice thickness of the data acquisition is greater than 1 mm.
Scanning Protocols
Generalized CTA protocols for four-, 16-, and 64-slice scanners are presented in Tables 19-11 and 19-12.
Aitken, GF, et al. Leg length determination by CT digital radiograph. AJR Am J Roentgenol. 1985;144:613–615.
Brenner, DJ, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296.
Chan, FP, et al. MDCT angiography of pediatric vascular diseases of the abdomen, pelvis, and extremities. Pediatr Radiol. 2005;35:40–53.
Daneman, A. Pediatric body CT. New York: Springer-Verlag, 1987.
Donelly, LF, et al. Minimizing radiation dose for pediatric body applications of single-detector helical CT. AJR Am J Roentgenol. 2001;176:303–306.
Flodmark, O, et al. Periventricular leukomalacia radiologic diagnosis. Radiology. 1987;162:119–124.
Frush, D, Donnelly, LF. Helical CT in children: technical considerations and body applications. Radiology. 1998;209:37–48.
Frush, D, et al. Challenges of pediatric spiral CT. Radiographics. 1997;17:939–959.
Huda, W, et al. An approach for the estimation of effective radiation dose at CT in pediatric patients. Radiology. 1997;203:417–422.
Jacob, RP, et al. Tibial torsion calculated by computerized tomography. J Bone Joint Surg. 1980;62B:238–242.
Jacquenier, M, et al. Acetabular anteversion in children. J Pediatr Orthop. 1992;12:373–375.
Keeter, S, et al. Sedation in pediatric CT: national survey of current practice. Radiology. 1990;175:745–752.
Patterson, A, et al. Helical CT scan of the body: are settings adjusted for pediatric patients? AJR Am J Roentgenol. 2001;176:297–301.
Siegel, MJ. Multiplanar and three-dimensional multi-detector row CT of thoracic vessels and airways in the pediatric population. Radiology. 2003;229:641–650.
Ozonoff, MB. Pediatric orthopedic radiology, 2. Philadelphia: WB Saunders, 1992.
*This chapter was originally written by Victoria Bigland, RTR; Gordon Culham, MD, FRCPC; and Kenneth Poskitt, MDCM, of the British Columbia Children’s Hospital, Department of Radiology. It was revised for the second edition by Jeremy Lysne, RT(R)(CT), Department of Radiology, Denver Children’s Hospital, and for the third edition by Dr. Scott Lipson, MD, Department of Radiology, Long Beach Memorial Medical Center, and Dr. Son Nguyen, MD, Department of Radiology, Miller Children’s Hospital, Long Beach Memorial Medical Center.