CHAPTER 40 Nitrous Oxide–Oxygen Analgesia
Delivery of nitrous oxide (N2O) in combination with oxygen (O2) is an inhalation method of conscious sedation known as nitrous oxide–oxygen analgesia. This conscious sedation method can significantly enhance the clinician’s ability to meet the client’s need for freedom from pain, stress, and fear in a safe and effective way. When used as the sole sedative, N2O-O2 suffices to relax individuals who are mildly apprehensive about the dental or dental hygiene experience and provides pain control for procedures that are only slightly or moderately painful. Such procedures include scaling hypersensitive root surfaces, removing periodontal sutures, cementing crowns or inlays, irrigating under an inflamed operculum, or administering a local anesthetic agent. If significant pain is anticipated during a dental or dental hygiene procedure, then N2O-O2 is accompanied by local anesthesia. N2O-O2 is used in combination with other general anesthetics, such as halothane and meperidine (Demerol), by oral surgeons to achieve surgical anesthesia. When used alone, N2O-O2 is a very weak anesthetic but an intense analgesic.1 This pharmacologic property of N2O-O2 makes it ideal for use in dental hygiene care because clients often are mildly apprehensive and require minor pain control but also must remain conscious and responsive.
Several synonyms refer to N2O-O2 analgesia, including the following1:
Conscious sedation refers to the fact that during the administration of N2O-O2 the client is always awake and able to respond to verbal commands, breathe automatically, and cough so that aspiration is avoided.2 Inhalation sedation reflects that the N2O and O2 gases are inhaled through the nose. N2O psychosedation refers to the fact that N2O acts on the psyche or the central nervous system in such a way that pain impulses are not relayed to the cerebral cortex or their interpretation is altered. Relative analgesia refers to the state of sedation produced—mood is altered and pain reaction threshold is increased, but pain sensations are not totally blocked.
CHEMISTRY
Nitrous Oxide
Nitrous oxide is a colorless, tasteless, sweet-smelling agent that supports combustion. It is stored in both the liquid and gaseous states in a blue compressed-gas cylinder (Figure 40-1). The pressure of the N2O vapor floating above the liquid N2O is approximately 700 to 750 pounds per square inch (psi) (Figure 40-2). Although it is stored as a liquid and vapor (gas) in equilibrium, N2O is delivered as a gas to the client. The pressure within the cylinder, indicated by the needle reading on the pressure gauge, reflects the pressure created by the N2O gas in the cylinder (see Figure 40-2). As the client inhales the gaseous N2O from the cylinder, liquid N2O vaporizes to replace it. The pressure of this “new” gas is 700 to 750 psi until no more liquid remains to replace the gas. The pressure gauge for N2O therefore cannot be used as an accurate measurement of the contents of the cylinder (Figure 40-3). Once all of the liquid N2O is gone and only gaseous N2O remains, the pressure gauge will fall in relation to the pressure of gas remaining.

Figure 40-1 A portable gas machine with a green cylinder containing O2 and a blue cylinder containing N2O, stored directly on the gas machine.
(Courtesy Dr. Mark Dellinges.)
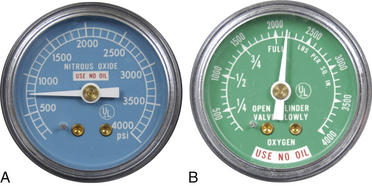
Figure 40-2 Pressure gauges on inhalation sedation unit. A, N2O pressure gauge for N2O cylinder. B, O2 pressure gauge for O2 cylinder. Note color-coding of blue for N2O and green for O2.
(Courtesy Dr. Mark Dellinges and Cory Price.)
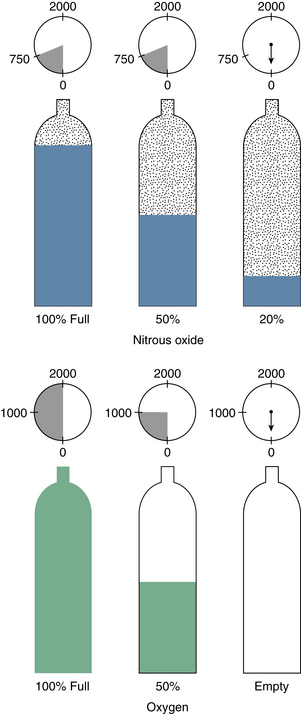
Figure 40-3 Pressure gauge readings for N2O and O2 cylinders.
(From Clark MS, Brunick AL: Handbook of nitrous oxide and oxygen sedation, ed 3, St Louis, 2008, Mosby.)
Consequently, clinicians use their N2O for a considerable amount of time before the pressure gauge reads 500 psi. Once the pressure reading drops to 500 psi, the pressure gauge precipitously drops, indicating that the cylinder is empty. Because the amount of N2O in the cylinder cannot be determined by the pressure gauge reading until the cylinder is almost empty, it is important for the operator to keep a close eye on the N2O pressure gauge of portable gas machines. This monitoring allows the clinician to detect when the pressure begins to fall and to substitute a full N2O cylinder before the original cylinder is empty. In addition, each N2O cylinder should be marked with the date the full tank was opened and the dates and lengths of subsequent use to facilitate the monitoring process and to prevent the clinician from running out of N2O before the client care procedure is completed.
The blood-gas solubility coefficient of N2O is 0.47, meaning that 100 mL of blood dissolves 47 mL of N2O. This blood-gas solubility coefficient accounts for the rapid onset and rapid recovery from the analgesic effects of N2O sedation. Because N2O is 15 times more soluble in blood than nitrogen, it displaces nitrogen in the blood. It does not compete with O2 and carbon dioxide for combination with the hemoglobin molecule.1
Oxygen
O2 is stored as a gas in green compressed-gas cylinders and is delivered as a gas (see Figure 40-1). The contents of the O2 cylinder can be determined by the reading on the pressure gauge. A full tank of O2 is reflected by a pressure gauge reading of 2100 psi (see Figure 40-2). As the O2 is depleted in the cylinder as a result of use, the pressure falls correspondingly, as indicated by the needle position on the O2 pressure gauge (see Figure 40-3). Consequently, one has an accurate assessment of how much O2 is left in the cylinder at all times.
PHARMACOLOGY
N2O has no effect on the heart rate, blood pressure, liver, or kidney as long as an adequate amount of O2 is delivered concurrently.2 It does, however, have an effect on all sensations, such as hearing, touch, pain, and warmth. With regard to hearing, clients report that they can hear distant sounds better than close sounds. Consequently, clients under the influence of N2O may key in to background sounds such as music or the conversation in the next room rather than to what the clinician is saying. In addition, N2O reduces the gag reflex but does not eliminate it. Therefore if a client tends to gag, this sedation modality should be considered for use.1
PHYSIOLOGY
N2O acts to depress the central nervous system. Specifically, it affects the cerebral cortex, thalamus, hypothalamus, and reticular activating system. The exact mechanism of action is unknown; however, it results in either altering the relay of nerve impulses to the cerebral cortex or causing them to be interpreted differently.2 As a result, the individual experiences reduced anxiety and increased pain tolerance. Pain perception is not blocked, however, and N2O-O2 must be used in combination with a local anesthetic for many procedures. N2O does not combine with any body tissues, and it is the only anesthetic used that is not metabolized. The N2O molecule enters the blood through the lungs, where it displaces nitrogen, and eventually exits unchanged through the lungs.1
Nevertheless there are toxic reactions associated with oversedation with N2O. Hypoxia (lack of O2 to the tissues), characterized by a headache and nausea, is associated with receiving too much N2O and lack of a subsequent oxygenation period. In addition, bone marrow depression and white blood cell depression have been reported after prolonged administration of 2 to 4 days.
STAGES OF ANESTHESIA
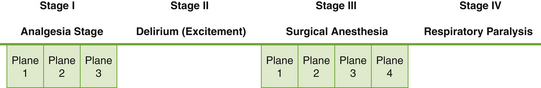
The four stages of anesthesia are depicted in Figure 40-4.
 Stage I is the analgesia stage. In analgesia the person feels pain but does not care. The analgesia stage of anesthesia has three planes. The first two planes are relative analgesia, and these are the planes appropriate for dental hygiene care.
Stage I is the analgesia stage. In analgesia the person feels pain but does not care. The analgesia stage of anesthesia has three planes. The first two planes are relative analgesia, and these are the planes appropriate for dental hygiene care. Stage II is the delirium or excitement phase of light anesthesia. This stage of anesthesia is characterized by hyperresponsiveness to stimuli, exaggerated inspirations, and loss of consciousness. For individuals receiving dental hygiene care, the immediate treatment of entry into the excitement stage of anesthesia is to increase the percentage of O2 immediately to 100% and to turn the N2O off.
Stage II is the delirium or excitement phase of light anesthesia. This stage of anesthesia is characterized by hyperresponsiveness to stimuli, exaggerated inspirations, and loss of consciousness. For individuals receiving dental hygiene care, the immediate treatment of entry into the excitement stage of anesthesia is to increase the percentage of O2 immediately to 100% and to turn the N2O off. Stage III is surgical anesthesia, and it has four planes. Oral and maxillofacial surgeons take their patients to this level of anesthesia, and it is acceptable; dental hygienists never need to provide this level of anesthesia for their clients. Loss of consciousness by an individual receiving dental hygiene care indicates oversedation, and the immediate treatment is to increase the percentage of O2 immediately to 100% and to turn the N2O off. The 0.47 blood-gas solubility coefficient for N2O promotes rapid recovery of the individual.
Stage III is surgical anesthesia, and it has four planes. Oral and maxillofacial surgeons take their patients to this level of anesthesia, and it is acceptable; dental hygienists never need to provide this level of anesthesia for their clients. Loss of consciousness by an individual receiving dental hygiene care indicates oversedation, and the immediate treatment is to increase the percentage of O2 immediately to 100% and to turn the N2O off. The 0.47 blood-gas solubility coefficient for N2O promotes rapid recovery of the individual. Stage IV anesthesia is surgical anesthesia with respiratory paralysis. This level of anesthesia is reserved for use when a person undergoes major surgery in a hospital setting.
Stage IV anesthesia is surgical anesthesia with respiratory paralysis. This level of anesthesia is reserved for use when a person undergoes major surgery in a hospital setting.N2O produces intense analgesia, but it is a very weak anesthetic. In fact, usually one would need to give more than 80% N2O to achieve surgical anesthesia.1 This pharmacologic property makes N2O-O2 a good pain and anxiety control modality for use in dental hygiene care.
INDICATIONS FOR USE
N2O-O2 analgesia is recommended for use in the following situations1,2:
Mild Apprehension
Individuals who are fearful of, or mildly anxious about, the oral healthcare experience are good candidates for N2O-O2 because it relaxes them and takes the edge off their apprehension.
Allergy to or Refusal of Other Anesthetics
Individuals who are allergic to all types of local anesthetics, those who refuse a local or general anesthetic for other reasons, and those who are unable to experience good local anesthesia because use of a vasoconstrictor is medically contraindicated are good candidates for N2O-O2 analgesia.
Hypersensitive Gag Reflex
Individuals who are prone to gagging easily during oral healthcare procedures, such as those having impressions taken or their third molars scaled, are good candidates for N2O-O2 because this analgesic reduces the gag response.
Inability to Tolerate Sitting for Long Periods
N2O-O2 analgesia is recommended for persons with back problems or other conditions that make them unable to tolerate sitting in the dental chair for long periods. This recommendation is based on the fact that N2O-O2 makes one perceive that time is passing quickly.
Cardiovascular Disease and Hypertension
Individuals who have cardiovascular disease or hypertension are good candidates for N2O-O2 because it decreases stress and exposes the individual to more O2 than is normally available. For example, even at a gas ratio of 50:50, the client is receiving 50% O2 compared with the 22% O2 available in room air. This O2 enrichment coupled with stress reduction is a major advantage of N2O-O2 sedation for these medically complex clients.
Asthma
Individuals who have asthma are candidates for N2O-O2 because during sedation they receive more O2 than normally is available to them. This O2 enrichment facilitates breathing and decreases stress.
Cerebral Palsy and Intellectually and Developmentally Challenged Persons
Persons with cerebral palsy and who are developmentally or cognitively challenged are candidates for N2O-O2 because they are sometimes difficult to manage in the oral healthcare setting, and this analgesic relaxes them. The client, however, must be able to communicate with the operator, breathe through the nose, and cooperate by leaving the mask in place.
RELATIVE CONTRAINDICATIONS TO USE
There are no absolute medical contraindications to use of N2O-O2 analgesia, but there are some relative contraindications that make it a poor choice for certain clients. The following conditions contraindicate the use of N2O-O2 sedation1,2:
Pregnancy
N2O-O2 analgesia is not recommended for individuals who are pregnant. Although there is no evidence that sufficient N2O crosses the placenta to produce depression of the fetal central nervous system, it is better to err on the side of caution with pregnant women given that long-term exposure to N2O is associated with spontaneous abortion.1 In general, all unnecessary drugs are avoided during pregnancy, especially during the first trimester.
Communication Barrier
Individuals who have a language barrier or with whom communication is difficult should not be given N2O-O2 because communication between the client and the operator is essential for success with conscious sedation. The operator must question the client during the administration of N2O-O2 to determine the appropriate level of sedation and the client’s response to the drug. Communication barriers make it difficult or impossible for this monitoring to occur.
Nasal Obstructions
Individuals who have a cold, allergy, or other type of nasal obstruction are not good candidates for N2O-O2 because the gas is inhaled. Nasal obstruction prevents the client from obtaining the benefit of the drug. Also, respiratory infections contaminate the tubing and reservoir bag.
Chronic Obstructive Pulmonary Disease
The respiratory systems of persons with emphysema or chronic bronchitis function on less O2 than those of healthy individuals because these diseases affect the lung’s capacity to exchange air. Consequently, they depend on a lowered blood O2 level to stimulate respiration. The increased blood O2 saturation made available with N2O-O2 removes the stimulus of the lowered O2 blood level and may indicate to the brain that the individual need not perform as many inspirations, thus producing apnea.2
Emotional Instability
N2O-O2 is contraindicated for individuals who are emotionally unstable. Because this type of sedation causes a distortion of one’s perception of reality, it can precipitate problems for clients with a history of schizophrenia or alcoholism. Moreover, individuals who have recently experienced the death of a loved one or who are going through a painful divorce often go through a period of emotional instability. It is, therefore, not recommended to use N2O-O2 sedation because unpleasant feelings may surface under the influence of this drug and cause the client to cry uncontrollably.
Epilepsy
N2O-O2 analgesia may trigger epileptic seizures in individuals with epilepsy. Therefore, its use is not recommended for clients with a history of epilepsy.
Fear of Nitrous Oxide–Oxygen Sedation
Individuals who are fearful of having N2O-O2 or those with compulsive personalities who must always be in control may suddenly tear off the sedation mask from fear of the unknown or of becoming unconscious. In the dental hygiene care setting, a good rule of thumb is never to talk someone into being sedated with N2O-O2. Individuals should be willing and wanting to try this sedation method.
ADVANTAGES OF USE
The following are advantages associated with N2O-O2 analgesia:
 It is an excellent choice of sedation for the high-risk person with a history of cardiovascular disease.
It is an excellent choice of sedation for the high-risk person with a history of cardiovascular disease. It is a simple, relatively safe procedure to perform and does not require the services of special personnel such as an anesthetist.
It is a simple, relatively safe procedure to perform and does not require the services of special personnel such as an anesthetist. Individual is awake and responsive at all times, and the depth of sedation can be controlled moment to moment.
Individual is awake and responsive at all times, and the depth of sedation can be controlled moment to moment. Most adults being sedated do not have to be accompanied to their appointment by another responsible adult.
Most adults being sedated do not have to be accompanied to their appointment by another responsible adult.DISADVANTAGES OF USE
The following are disadvantages associated with N2O-O2 analgesia:
 Production of vertigo, nausea, or vomiting may occur if too much N2O is given or if the operator fluctuates the levels of N2O too much during administration of the agent. Aspiration is not a problem, however, because the client is awake and the gag reflex is not eliminated (Figures 40-5 and 40-6).
Production of vertigo, nausea, or vomiting may occur if too much N2O is given or if the operator fluctuates the levels of N2O too much during administration of the agent. Aspiration is not a problem, however, because the client is awake and the gag reflex is not eliminated (Figures 40-5 and 40-6).SIGNS AND SYMPTOMS OF NITROUS OXIDE–OXYGEN SEDATION
A sign is something that can be directly observed. A symptom is something that must be reported to one person by another. Thus signs of N2O-O2 sedation are observed objectively by the operator, and symptoms of N2O-O2 sedation are reported subjectively by the client. Based on this information, the dental hygienist determines when an appropriate level of sedation has been achieved to relax the client sufficiently to begin treatment.
Signs
Objective signs that clients have reached a desirable level of N2O-O2 sedation are that they are awake but drowsy and relaxed in appearance (e.g., feet pointing out and hands limp; Figure 40-7). They have reduced reaction to painful stimuli, and respiration is normal and smooth. In contrast, if a client demonstrates hyperresponsiveness to stimuli and exaggerated inspirations, these are signs of oversedation (i.e., entry into the excitement stage of anesthesia) and of the need to give 100% O2 to the person and discontinue the N2O altogether.
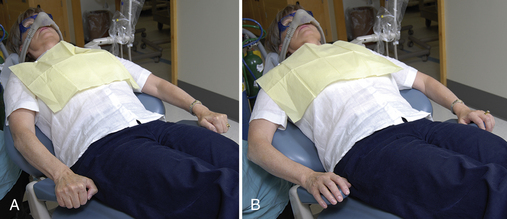
Figure 40-7 A, White-knuckle syndrome exhibited by apprehensive client at start of procedure. B, Relaxation of hands is commonly observed when client becomes sedated.
(Courtesy Dr. Mark Dellinges.)
Other signs that clients have reached a desirable level of N2O-O2 sedation are that their blood pressure and pulse, eye reaction, and pupil size are observed to be normal.2 Little or no gagging or coughing is observed. The client’s speech is slow and tends to be guttural.1 There may be some perspiration and lacrimation (tearing). Heavy perspiration and lacrimation, although possibly reflecting appropriate sedation for oral surgery treatment, are inappropriate for dental hygiene care and indicate a need to turn down the N2O by about 2 L and increase O2 by 2 L. Likewise, uncontrollable laughing by the client indicates a need to turn down the N2O level (by about 2 L) and increase the O2 level by an amount equal to the N2O reduction (Box 40-1).
Symptoms
Subjective symptoms of N2O-O2 sedation can be determined by direct questioning of the client as well as by observation. For example, asking “How do you feel?” or “Do you feel relaxed?” elicits desired information. If clients report that they are relaxed or that sounds seem distant and if they indicate an indifference to their surroundings, these are symptoms that the desired level of sedation for dental hygiene care has been achieved. For instance, if the operator says to the client, “Shall I go ahead and numb up this area?” and the client replies “I don’t care,” indifference is apparent. Other desirable symptoms are client reports of lessened pain awareness, for example, during probing of a previously sensitive tooth, and of feeling tingling, lightheadedness, a floating sensation, or waves of warmth over the entire body. A tingling sensation in the fingers and toes and then in the arms and the legs is usually one of the first symptoms reported, indicating a desirable level of sedation. The operator may begin by asking the client, “Do you feel any tingling in your fingers or toes or in your arms and legs?”
The point at which the client reports a relaxed pleasant floating sensation can be taken as the baseline level of sedation. Baseline is the term used to designate the ideal minimal amount of N2O-O2 needed to relax the client (Box 40-2). Once baseline sedation is obtained, the client should then be maintained at a slightly reduced N2O level by decreasing the N2O level by 1 to 2 L and increasing the O2 level by 1 to 2 L.
Reported feelings of heaviness in the chest or of vibration or spinning, although reflecting appropriate sedation for oral surgery treatment, are not symptoms of appropriate sedation levels for dental hygiene care. Instead, they indicate a need to turn down the N2O level (e.g., by 2 L) and to increase the O2 level by a similar amount. If the client does not respond to questioning, this indicates that he or she has sunk below the desirable level of sedation. The operator should immediately decrease the liter flow of N2O and increase the O2 by 2 L. If this does not produce a client response, 100% O2 should be given and N2O discontinued.
The percentage of N2O delivered to the lungs determines the sedative effect on the central nervous system. Although individual reactions at any given concentration of N2O may vary greatly from individual to individual, a range of responses may occur at given concentrations, as summarized in Table 40-1.
TABLE 40-1 Signs and Symptoms in Response to Nitrous Oxide and Oxygen Conscious Sedation
| Concentration N2O | Response |
|---|---|
| 10%-20% | Body warmth |
| Tingling of hands and feet | |
| 20%-30% | Circumoral numbness |
| Numbness of thighs | |
| 20%-40% | Numbness of tongue |
| Numbness of hands and feet | |
| Droning sounds present | |
| Hearing distinct but distant | |
| Dissociation begins and reaches peak | |
| Mild sleepiness | |
| Analgesia (maximum at 30%) | |
| Euphoria | |
| Feeling of heaviness or lightness of body | |
| 30%-50% | Sweating |
| Nausea | |
| Amnesia | |
| Increased sleepiness | |
| 40%-60% | Dreaming, laughing, giddiness |
| Further increased sleepiness, tending toward unconsciousness | |
| Increased nausea and vomiting | |
| 50% and over | Unconsciousness and light general anesthesia |
From Bennett CR: Conscious sedation in dental practice, ed 2, St Louis, 1978, Mosby.
EQUIPMENT
The armamentarium for the delivery of N2O-O2 inhalation sedation consists of a supply of the gases stored in containers called cylinders, an apparatus for their delivery to the client, called a gas machine, and a nasal inhaler or mask through which the client breaths the N2O-O2 analgesic. The modern gas machine or inhalation sedation unit is a compact, continuous-flow machine used for the administration of compressed gases under controlled conditions. The N2O-O2 inhalation sedation unit is altered to deliver only two gases: N2O and O2.
Cylinders
N2O and O2 are dispensed in steel containers called cylinders, which are colored green for O2 and blue for N2O (see Figure 40-1). Compressed-gas cylinders are manufactured in a variety of sizes. In inhalation sedation with N2O-O2, the cylinder size used commonly in portable units for both N2O and O2 is the E size, whereas larger cylinders are used in central storage systems, specifically G cylinders for N2O and H cylinders for O2.
Cylinders should always be returned to the appropriate vendor for refilling. It is hazardous to refill a small cylinder from a larger one, and this should not be attempted by oral healthcare personnel. For quality control, the Hazardous Materials regulations of the U.S. Department of Transportation require that cylinders be tested every 5 years by the manufacturer to ensure their integrity. The date of the test is permanently stamped on the cylinder.
Cylinders should be stored in an upright position, away from a heat source, and chained to the wall to prevent them from falling on their cylinder valve stem, which could cause the cylinder to explode. In addition, at high pressures O2 and N2O can form an explosive mixture in the presence of grease or oil. Therefore grease or oil should never be used on cylinder valves or gauges on the gas machine. Box 40-3 lists important considerations for handling compressed-gas cylinders.
BOX 40-3 Handling Compressed-Gas Cylinders
Adapted from Malamed SF, ed: Sedation: a guide to patient management, ed 4, St Louis, 2003, Mosby.
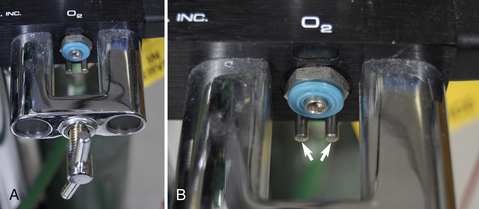
Cylinders may be stored directly on the gas machine (see Figure 40-1) or in an area away from the gas machine (Figure 40-8). When cylinders are stored in an area away from the gas machine, regulation copper tubing with a ⅜-inch outside diameter is fed through drilled holes in the wall to a quick-coupling type of outlet. A quick-coupling outlet on the wall of the treatment room is ideal because it permits rapid hookup and disengagement of the gas machine (Figure 40-9).

Figure 40-8 A, N2O and O2 cylinders stored in an area away from the gas machine. B, Gas is carried under low pressure to each station outlet in the individual operatories through specially designed wall plumbing.
(Courtesy Dr. Mark Dellinges and Cory Price.)
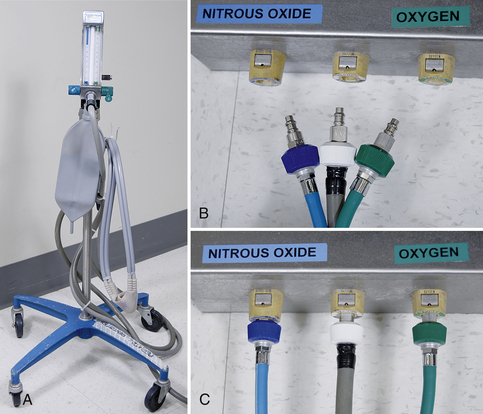
Figure 40-9 A, Quick-coupling gas machine (cylinders are stored in an area away from the gas machine). B, Quick-coupling outlets at base of unit or wall. Note different shapes of coupling plugs for N2O and O2 as a safety mechanism. C, Quick-coupling plug plugged into base of chair.
(Courtesy Dr. Mark Dellinges and Cory Price.)
Continuous-Flow Gas Machines
N2O-O2 continuous-flow gas machines are available as a portable system (Figure 40-10; see Figure 40-1) or as a central storage system (see Figure 40-8). Although each is the same basic unit, the differences between them are the manner in which compressed gases are delivered to the unit and their portability. In the portable system (see Figure 40-10) compressed-gas cylinders are attached to the gas machine at the yoke assembly. This system is used in offices where the frequency of N2O-O2 use is low or in situations in which the expense of a central storage system is prohibitive.

Figure 40-10 Portable gas machine. Compressed gases are attached to the unit at the yoke assembly.
(Courtesy Dr. Mark Dellinges.)
Components of portable continuous-flow gas machines are yokes, control valves, flowmeters, pressure gauges, a reservoir bag, and a gas hose (Figure 40-11). These major components will be discussed in depth below that the dental hygienist will be knowledgeable about this equipment and comfortable with its clinical use.
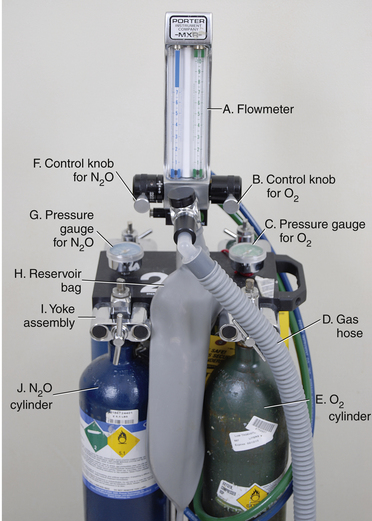
Figure 40-11 Continuous-flow inhalation sedation unit (portable, front view). A, Flowmeter. B, Control knob for O2. C, Pressure gauge for O2. D, Gas hose. E, O2 cylinder. F, Control knob for N2O. G, Pressure gauge for N2O. H, Reservoir bag. I, Yoke assembly. J, N2O cylinder.
(Courtesy Dr. Mark Dellinges.)
Yokes
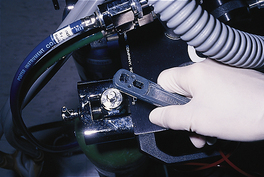
In the portable continuous-flow gas machine, yokes hold the cylinders in contact with the gas machine (Figure 40-12). From each yoke, gas goes through an automatic pressure-reducing valve and then to a fine-control valve that allows the gas to be delivered to the client at 50 psi.
Flowmeters
The flowmeter indicates the rate of flow of the gas. A small ball floats in the stream of gas that flows upward through a tapered tube. The greater the flow of volume of the gas used, the higher the ball rises. Separate color-coded flowmeters are used for N2O and O2, and each is calibrated to measure the volume of gas delivered in liters per minute (L/min) (Figure 40-13). In the United States the O2 control knob is green in color, whereas the N2O control knob is blue. In North America the O2 flowmeter is positioned on the right side of the bank of flowmeters. Flowmeters show the exact volume and proportions of gas output from the gas machine.
Pressure Gauge
The pressure gauge indicates the pressure of the cylinder contents (see Figures 40-2 and 40-3).
Reservoir Bag
Reservoir bags are bladder-type bags made of rubber or silicone and ranging in size from 1 to 8 L. The 3-L reservoir bag is the most frequently used in dentistry. The reservoir bag is attached to the gas machine. A portion of the gases being delivered through the unit to the client is diverted into the reservoir bag, where it is mixed and stored for use if the respiratory demands of the client exceed the gas flow being delivered from the machine. During normal respiration the client receives only gases delivered from the sedation unit, with little or none being taken from the reservoir bag. However, should the client take an especially deep breath, the machine will be unable to accommodate the necessary volume. In this event, additional gas is drawn from the reservoir bag. In the absence of the reservoir bag, the client will experience a feeling of suffocation. The reservoir bag prevents or minimizes this occurrence so that the client has a plentiful supply on which to draw for breathing. The gas hose delivers the gas mixture from the reservoir bag to the client’s mask continually at the volumes and proportions set by the clinician on the flowmeter.
Another use of the reservoir bag during conscious sedation is to serve as a monitoring device for respiration. Assuming an airtight seal of the mask and no mouth breathing, the reservoir bag inflates slightly with every exhalation and deflates slightly with each inspiration, permitting the dental hygienist to observe the respiratory rate (Figure 40-14).

Figure 40-14 A, Deflated reservoir bag usually indicates either a leak around the mask or a deficient tidal volume. B, Partially inflated reservoir bag usually indicates adequate seal and tidal volume. C, Distended reservoir bag indicates either an overly large minute volume or occluded breathing tubes.
(Courtesy Dr. Mark Dellinges and Cory Price.)
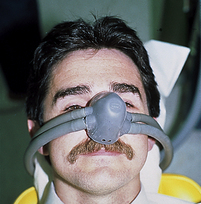
Nasal Mask
The nasal mask is the nasal inhaler through which the client breathes the N2O-O2 analgesic. Masks come with and without a scavenger system. With concern over the possible long-term effects of trace levels of N2O on chairside personnel, the scavenging nasal mask has been developed. The scavenging mask is the most effective means of minimizing N2O contamination in the oral healthcare treatment area.1,2
Although there are a number of scavenging nasal masks available, the principle behind their effectiveness is similar. The Brown nosepiece was one of the earliest scavenging devices and serves as the example in Figure 40-15. In general, scavenging nasal masks have a double nosepiece that consists of a smaller inner mask receiving anesthetic gases from the machine and a slightly larger outer mask that sits directly over the first, which removes exhaled gases from the treatment area. The outer nosepiece is connected to the suction device in the dental unit, permitting exhaled gases to be vented from the treatment area through the vacuum system.1,2 The instrument used to calibrate the degree of suction in the high-suction vacuum system is a suction calibrator; it ensures that the suction removes the exhaled N2O-O2 at an appropriate rate—not so fast that gas is removed before air has been inhaled, and not so slow that gas overaccumulates in the mask and leaks into the breathing zone of the clinician. The suction calibrator is attached to the high-speed vacuum system (Figure 40-16), and the suction is adjusted until the steel ball in the calibrator is made to float in the green zone of the calibrator window (Figure 40-17). If there is no scavenger system in place, the mask will have only one hose coming off each side of it (Figure 40-18). These hoses carry the N2O-O2 to the client. However, if there is a scavenger system in place, the mask has two hoses coming off each side of it (Figure 40-19). One pair of hoses delivers the N2O-O2 to the client, and the other pair carries away the exhaled N2O-O2 into the suction system. Therefore the purpose of a scavenger system is to reduce the N2O exhaled into the air by the client and breathed by the operator. Scavenger systems reduce the amount of N2O breathed into the environment from 900 parts per million (ppm) to 30 ppm. The ideal maximal amount of N2O-O2 allowable in the healthcare environment is 50 ppm.
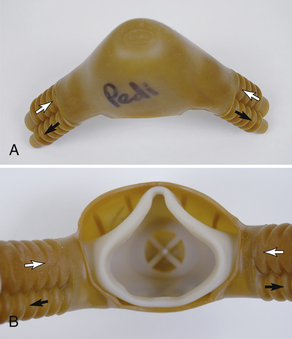
Figure 40-15 A, An exterior view of a nasal mask. Gas intake (white arrows), waste gas removal (black arrows). B, An interior view of a Brown mask revealing the double-mask construction and gas flow.
(Courtesy Dr. Mark Dellinges.)
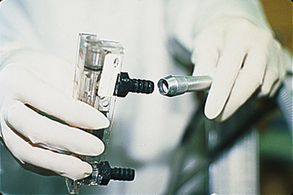
Figure 40-16 Suction calibrator is attached to the high-speed vacuum and adjusted to obtain the optimal level of suction for the scavenger system.
SAFETY MEASURES
Safety features are built into cylinders and gas machines to prevent the inadvertent delivery of N2O when one is intending to deliver O2 to the client. These failsafe mechanisms are as follows1,2:
Color-Coding
Cylinders, quick-coupling tubing, outlets, flowmeters, and pressure gauges are color-coded according to the gas they contain and monitor. Green indicates O2 and blue indicates N2O.
Pin Indexing System
The pin indexing safety system consists of prongs (pins) on the yoke that hold the O2 cylinder and the corresponding holes on the O2 cylinder head that are placed a specific distance apart, which is different from that of their counterparts on the N2O yoke and cylinder (Figure 40-20). Thus the holes on the N2O cylinder do not fit the prongs in the yoke that holds the O2 cylinder and vice versa.
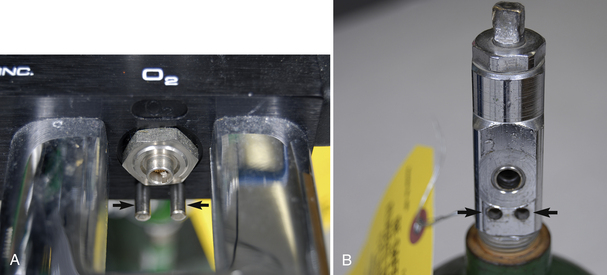
Figure 40-20 A, Pins (arrows) which are located on the yoke of the gas machine are aligned to permit attachment of only one specific type of compressed gas, either O2 or NO2 but not both. B, O2 cylinder head with holes (arrows) placed at a specific distance apart to fit the prongs on the yoke designed to hold O2 cylinder.
(Courtesy Dr. Mark Dellinges.)
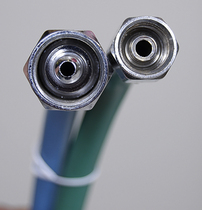
Diameter Indexing System
The diameter index safety system is designed to ensure that the correct medical gas enters the correct part of the gas machine to prevent delivering N2O to an individual in the mistaken belief that O2 is being delivered. Accidental attachment is prevented in two ways. First, the diameter of the attachments differs considerably, and second, the threading of the attachments differs, making it physically impossible to inadvertently attach tubing to the wrong inlet on the gas machine (Figure 40-21). Once in the machine, the gases are directed to the appropriate flowmeters where precise volumes may be delivered to the client.1,2
Indicators that Oxygen is Depleted
Many gas machines have an alarm that goes off when the O2 runs out. Other machines simply turn off automatically when the O2 is depleted. These features prevent the operator from administering 100% N2O to the client.
Automatic Maintenance of Minimal O2 Levels
On most gas machines the O2 flowmeter cannot go below 2 to 3 L of O2. When the machine is turned on, the O2 volume automatically goes to 2 to 3 L. This constant flow of O2 is provided at all times when the gas machine is on, thus preventing the possibility of providing 100% N2O to the client.
ADMINISTRATION
Administration of N2O-O2 includes the following:
Although a step-by-step approach to N2O-O2 administration is explained in Procedure 40-1, the general points are highlighted for emphasis in the following sections.
Procedure 40-1 ADMINISTRATION OF NITROUS OXIDE–OXYGEN ANALGESIC USING THE CONSTANT LITER FLOW TECHNIQUE
STEPS
Prepare Equipment
Prepare the Client
If mask is impinging on a sensitive area on the face or if mask is too big, place a gauze square under the edge of the mask (Figure 40-35).
Determine Exact Tidal Volume
Begin Titration of N2O
Terminate the Flow of N2O and Begin Oxygenation
Discharge the Client, and Document Procedure in Chart
Preparation
The office should have a quiet atmosphere throughout the sedation period. It is recommended that all oral healthcare personnel who interact with clients personally experience the sensations produced by N2O-O2 sedation. This experience allows them to relate their feelings to clients. In addition, the dental hygienist prepares the N2O-O2 armamentaria before seating clients scheduled to receive the sedation procedure. On seating, clients are asked if they need to visit the restroom. Those who wear contact lenses also are asked to remove them because sometimes gas escaping from the mask can dry out the cornea and increase the risk of corneal abrasion.
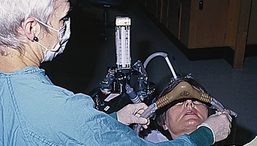
After reviewing the health history and vital signs, the dental hygienist explains to the client what is about to happen and describes the sensations of warmth and tingling that will be experienced. For example, clients are told that they will feel very relaxed, as if they have had a couple of alcoholic drinks. The dental hygienist assures clients that they are in complete control throughout the sedation procedure in the sense that if they feel they are receiving too much N2O-O2 sedation, they just need to inform the operator, who will turn down the N2O and turn up the O2, which will increase the feeling of normalcy. The client then is positioned in a comfortable, reclined position in the dental chair. The partially reclined position may be used for client comfort and clinician convenience during the procedure (Figure 40-22).
Estimate Tidal Volume, Start Flow of Oxygen, Secure Nasal Mask over Client’s Nose
Starting the flow of O2 before placing the nasal mask on the client prevents the client from feeling suffocated when breathing through the nose. The client’s tidal volume is estimated. Tidal volume is the amount of air a person needs for one respiration cycle. For an average adult, it could be from 6 to 8 L, depending on the size and metabolic rate of the individual. A flow of O2 is introduced based on the estimated tidal volume. For example, if the tidal volume is estimated to be 6 L, the O2 flowmeter is set to a 6-L/min flow of 100% O2, and the nose mask is placed over the nose and centered on the face snugly to prevent leakage at the edges of the mask. The nasal mask should have two pairs of hoses on each side of it. These are placed around the sides of the dental chair, and the nasal mask is secured by adjusting the slip ring behind the back of the chair (Figure 40-23). The client may be asked to hold the nasal mask in a comfortable position as this is being done. If the mask is too big and gas is escaping at its edges, a gauze square may be used to contour around the mask to adapt it to the client’s nose and plug some of the leakage spaces (Figure 40-24). After mask adjustment, clients are asked if they have enough air to breathe comfortably. If not, the tidal volume of 100% O2 is increased. If the air is reported to be blowing up the client’s nose, the tidal volume of O2 is decreased. The client must be able to breathe comfortably before the start of N2O flow in order to be comfortable throughout the procedure.1
Titration of Nitrous Oxide–Oxygen
Titration is the process of adjusting the percentage of gases (N2O and O2) to the desired concentration of N2O and O2 gases while keeping the total liter flow of gases (tidal volume) constant. The goal of titration is to produce baseline sedation signs and symptoms in the client. Once the correct tidal volume has been established with 100% O2 and documented in the client’s record, a constant liter flow technique is used to introduce N2O at the rate of 0.5 to 1 L/min while decreasing the O2 flow at a similar rate. This constant liter flow technique keeps the total liter flow of gases (N2O and O2) per minute constant throughout the procedure. For example, given a tidal volume of 6 L/min, the dental hygienist increases the N2O flow to 1 L/min and then decreases the O2 flow rate to 5 L/min. A 1- to 2-minute pause is made after each adjustment, during which the dental hygienist observes the client for signs of baseline. After the pause the hygienist asks the client how he or she is feeling, to evaluate responses for symptoms indicating the client has reached baseline. This process is repeated until the baseline state is reached. Generally for dental hygiene care, 50% N2O or less is effective for achieving baseline. Once baseline is reached, the operator should drop back on the N2O flow about 0.5 to 1 L because with time the intensity of the sedation increases. This titration technique minimizes the risk of overshooting baseline and causing a problem by carrying the person too deeply into the excitement stage of general anesthesia.
Once baseline is reached, the dental hygienist works efficiently and quietly, asking clients periodically how they are doing. Unnecessary talking is avoided to allow clients to relate to the sedation and because their talking expels N2O into the immediate environment of the practitioner.
Oxygenation, Client Discharge, and Documentation
When scaling and root planing are completed, the N2O is turned off and the O2 increased to maintain the tidal volume. For every 15 minutes of exposure to N2O, the client must receive 5 minutes of 100% O2. Therefore if clients receive 45 minutes of N2O-O2 sedation, they should receive 15 minutes of 100% O2 at the end of the sedation procedure. If clients are sedated for less than 5 minutes, they still are oxygenated for a minimum of 5 minutes. This oxygenation period is essential to prevent tissue hypoxia, characterized by headache and upset stomach, on completion of the sedation procedure.
The tidal volume, the time baseline was reached, and the amount or percentage of gases administered should be recorded in the client’s chart. To calculate the percentage of gases administered, the flow rate of a specific gas is divided by the tidal volume and multiplied by 100 (Box 40-4). For example, if the client’s tidal volume (TV) is 7 L/min, the O2 flow is 5 L/min, and the N2O flow rate is 2 L/min, the percentage of N2O delivered is  × 100, which is 29% of total flow, and the percentage of O2 delivered is
× 100, which is 29% of total flow, and the percentage of O2 delivered is  × 100, which is 71%. Notation for documentation would be as follows:
× 100, which is 71%. Notation for documentation would be as follows:
In addition to the tidal volume and the percentages of gases used, the duration of sedation, the length of the oxygenation period, the client’s response, and the dental hygiene care delivered should all be documented in the client’s chart (Figure 40-25).
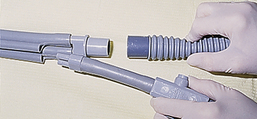
Figure 40-29 Attaching the larger adaptor of the sterilized nasal mask to the gas machine gas hose (held in right hand).

Figure 40-30 Attaching the smaller adaptor on the sterilized nasal mask to calibrated high-speed suction to provide for the scavenging system.

Figure 40-34 Client holding nasal mask in a comfortable position while dental hygienist adjusts the mask tubes to hold the mask in place.
The specific techniques for N2O-O2 administration are presented in Procedure 40-1.
POTENTIAL COMPLICATIONS
Complications1 associated with N2O-O2 can be mitigated by carefully selecting candidates based on their health and personal history, and by adopting the technique described in Procedure 40-1 for the administration of this sedation modality. Specifically, inducing clients to an individualized baseline level by the process of titration and oxygenating them for an appropriate amount of time facilitate the avoidance of some complications with this somewhat innocuous agent. The possible complications associated with N2O-O2 sedation are as follows1:
Diffusion Hypoxia
Diffusion hypoxia, a lack of O2 to the tissues, is characterized by headache, grogginess, nausea, and what generally may be described as a “hungover” feeling after exposure to N2O-O2 analgesia. This complication is related to not being oxygenated for an appropriate period after the completion of the sedation procedure.
Head Injury during Expectoration
Sedated clients are at risk for bumping their heads on the cuspidor if they attempt to expectorate while under sedation. Consequently, a saliva ejector or high-vacuum suction should be used in place of allowing the client to rinse or expectorate into a cuspidor. If such expectoration cannot be avoided, however, the clinician should place her or his hand on the client’s forehead to guide the client to the cuspidor and prevent possible injury.
Nausea and Vomiting
Nausea and vomiting are associated with giving the client too much N2O-O2 sedation, although it also may occur when the client consumes a heavy meal before the dental hygiene care appointment. In addition, nausea can be brought on by fluctuating the N2O levels back and forth during the titration process. For example, giving a client 3 L of N2O then increasing the amount to 5 L and decreasing it back down to 4 L and then back up to 6 L in a short period can produce nausea. If a client indicates nausea (either verbally by self-report or nonverbally by holding the stomach), the N2O should be turned down by 2 L and O2 increased by 2 L. If the nausea persists, N2O should be discontinued and the client should be given 100% O2 for an appropriate oxygenation period.
If vomiting occurs, the N2O must be turned off immediately, the mask removed, and the client’s head turned to the side away from the operator to facilitate emesis (see Figure 40-5). A high-vacuum suction may be used to facilitate removal of vomitus (see Figure 40-6). Give the client a cool, wet towel to clean up, and clean the treatment area as quickly as possible. Reassure the individual that he or she will feel better after breathing 100% O2.
Corneal Irritation
Leakage of gas from the mask can dry out the eyes and cause corneal abrasion in individuals wearing contact lenses. This problem can be prevented by having clients remove their contact lenses before the N2O-O2 sedation is administered to them.
Behavioral Problems
Several types of behavioral problems can be associated with N2O-O2 sedation. Repeated closing of the mouth and a rigidity of the mandible are usually signs of too much N2O. Turning the N2O down by 2 L and increasing the O2 by 2 L eliminates the problem.
Individuals who do not like to give up control are often threatened by the tingling and floating feelings characteristic of this mode of sedation. As a result, they may respond by suddenly sitting forward and taking off the mask because of fear of the unknown or of becoming unconscious. This problem can be prevented by carefully screening candidates for this sedation method, thoroughly explaining what they can expect to experience, and never talking clients into having N2O-O2.
Individuals who are going through a period of emotional instability may be prone to crying under the influence of N2O-O2 sedation. If this occurs, the N2O should be discontinued and 100% O2 should be given for an appropriate oxygenation period. Careful screening of candidates before offering this sedation modality prevents this problem, which can be embarrassing to both client and clinician.
Sexual fantasies and attempts at amorous behavior have been reported in individuals who have been given N2O concentration greater than 50% and who were sedated without an assistant as a witness in the room. Decreasing the amount of N2O by at least 2 L and increasing the O2 by a corresponding amount may solve the problem. If not, the N2O should be discontinued and 100% O2 given to the client for an appropriate amount of time. Individuals who respond with this type of behavior problem should not be judged harshly because they have placed themselves in the care of the clinician and have allowed their sense of reality to be altered based on the trust and confidence they have in the clinician. It is the responsibility of the clinician to protect the client while the client is under the clinician’s care.
Equipment Malfunction
Contaminated N2O cylinders can contain nitrogen dioxide and on administration may produce nitric acid with serious consequences to a client. Valves on the N2O cylinders must be kept closed when not in use to prevent this dire circumstance from occurring.1
Hazards to Personnel
The effects of chronic exposure to N2O (1000 to 15,000 ppm) reported in animal and human studies of operating room personnel and of oral surgeons and others who used N2O in their practice include the following:
Hazardous concentrations of N2O in the oral healthcare setting can be reduced from 900 ppm to 30 ppm using a combination of the following methods:
 Maintaining the anesthetic equipment, testing for leakage, and inspecting the connectors at frequent intervals
Maintaining the anesthetic equipment, testing for leakage, and inspecting the connectors at frequent intervals Monitoring N2O in the oral healthcare environment; a badge can be worn to detect N2O levels in the operator’s breathing zone
Monitoring N2O in the oral healthcare environment; a badge can be worn to detect N2O levels in the operator’s breathing zone Opening a window in the treatment area to improve air circulation or using a nonrecycling air-conditioning system
Opening a window in the treatment area to improve air circulation or using a nonrecycling air-conditioning systemCLIENT EDUCATION TIPS
 Explain the sensations that will be experienced, and describe them in positive terms (e.g., warmth, tingling).
Explain the sensations that will be experienced, and describe them in positive terms (e.g., warmth, tingling).LEGAL, ETHICAL, AND SAFETY ISSUES
 The dental hygienist has the legal responsibility to practice within the scope authorized by state law concerning nitrous oxide–oxygen (N2O-O2) analgesia administration.
The dental hygienist has the legal responsibility to practice within the scope authorized by state law concerning nitrous oxide–oxygen (N2O-O2) analgesia administration. The dental hygienist must carefully evaluate the client’s health history to determine suitability for N2O-O2 sedation.
The dental hygienist must carefully evaluate the client’s health history to determine suitability for N2O-O2 sedation.KEY CONCEPTS
 Delivery of nitrous oxide (N2O) in combination with oxygen (O2) is an inhalation method of conscious sedation known as N2O-O2 analgesia. It relaxes individuals who are mildly apprehensive about the dental or dental hygiene experience and provides pain control for procedures that are only slightly or moderately painful.
Delivery of nitrous oxide (N2O) in combination with oxygen (O2) is an inhalation method of conscious sedation known as N2O-O2 analgesia. It relaxes individuals who are mildly apprehensive about the dental or dental hygiene experience and provides pain control for procedures that are only slightly or moderately painful. The treatment of entry into the excitement stage of analgesia is increasing the percentage of O2 immediately to 100%.
The treatment of entry into the excitement stage of analgesia is increasing the percentage of O2 immediately to 100%. Light anesthesia rather than relative analgesia may be indicated by the patient becoming hyperresponsive to stimuli and producing exaggerated inspiration.
Light anesthesia rather than relative analgesia may be indicated by the patient becoming hyperresponsive to stimuli and producing exaggerated inspiration. Subjective symptoms of relative analgesia include heaviness of limbs, floating sensation, tingling, decreased fear, decreased pain memory, desire to maintain that state, feeling of warmth, and decreased awareness of time.
Subjective symptoms of relative analgesia include heaviness of limbs, floating sensation, tingling, decreased fear, decreased pain memory, desire to maintain that state, feeling of warmth, and decreased awareness of time. Objective signs of a desired level of sedation are normal eye reaction and pupil size, normal blood pressure and pulse, ability to answer questions, and relaxation of hands, fingers, and mandible.
Objective signs of a desired level of sedation are normal eye reaction and pupil size, normal blood pressure and pulse, ability to answer questions, and relaxation of hands, fingers, and mandible. Relative contraindications to N2O-O2 include breathing difficulties, communication difficulties, epilepsy, pregnancy, nasal obstruction, chronic obstructive pulmonary disease, multiple sclerosis, negative past experience, fear of sedation, and emotional instability.
Relative contraindications to N2O-O2 include breathing difficulties, communication difficulties, epilepsy, pregnancy, nasal obstruction, chronic obstructive pulmonary disease, multiple sclerosis, negative past experience, fear of sedation, and emotional instability. N2O-O2 sedation may be particularly useful for clients with a history of hypertension, asthma, and cardiovascular disease.
N2O-O2 sedation may be particularly useful for clients with a history of hypertension, asthma, and cardiovascular disease. After the administration of N2O-O2 analgesia, O2 alone should be given for a minimum of 5 minutes for each 15 minutes of use before the client is released.
After the administration of N2O-O2 analgesia, O2 alone should be given for a minimum of 5 minutes for each 15 minutes of use before the client is released. When adjusting the proportions of N2O and O2 to achieve the desired level of analgesia, each adjustment should be at the rate of ½ to 1 L N2O for at least 1 minute.
When adjusting the proportions of N2O and O2 to achieve the desired level of analgesia, each adjustment should be at the rate of ½ to 1 L N2O for at least 1 minute. A scavenger system incorporated into the N2O-O2 units takes out N2O that is exhaled through the mask.
A scavenger system incorporated into the N2O-O2 units takes out N2O that is exhaled through the mask. The effects of chronic exposure to N2O may include spontaneous abortion, birth defects, bone marrow depression, anemia, hepatic and renal diseases, and cancer.
The effects of chronic exposure to N2O may include spontaneous abortion, birth defects, bone marrow depression, anemia, hepatic and renal diseases, and cancer. To reduce N2O exposure, the dental hygienist uses a scavenging mask system, discourages unnecessary client talking, and has all the equipment leak-tested regularly.
To reduce N2O exposure, the dental hygienist uses a scavenging mask system, discourages unnecessary client talking, and has all the equipment leak-tested regularly. Before the mask is placed on the client, a predetermined mixture of N2O and O2 should never be established.
Before the mask is placed on the client, a predetermined mixture of N2O and O2 should never be established.CRITICAL THINKING EXERCISES
Profile: A 35-year-old woman arrives for dental hygiene care. She wears contact lenses.
Chief Complaint: “My teeth really need to be cleaned. I have finally got up my courage to come in and have it done.”
Dental History: Client makes regular dental visits, but she is 12 months overdue for her dental hygiene care appointment. She reports her teeth are sensitive.
Social History: Client is single and lives with her mother.
Health History: Client’s blood pressure is 140/90 mm Hg. She reports she is trying to control it with diet and exercise and is under the care of her physician.
Oral Self-Care Assessment: Client reports brushing once a day but does not floss or use any other interdental cleaning device.
Supplemental Notes: Client presents with moderate subgingival calculus and gingival inflammation throughout. Mesial and distal probing depths of 4 to 5 mm are in all posterior teeth.
Refer to the Procedures Manual where rationales are provided for the steps outlined in the procedure presented in this chapter.
1. Malamed S.F. Sedation: a guide to patient management, ed 4. St Louis: Mosby, 2003.
2. Clark M.S., Brunick A. Handbook of nitrous oxide and oxygen sedation, ed 3. St Louis: Mosby, 2008.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..