CHAPTER 59 Abuse and Neglect
Oral health professionals are uniquely positioned to identify and report abuse because about 50% to 65% of all physical manifestations of abuse are found on the victim’s head, face, mouth, and neck.1,2 However, only 1% of all reports of abuse from healthcare professionals are made by dental care providers.1,2 This low reporting of suspected abuse by dental professionals reflects a lack of information on how to recognize and report abuse. Legislation in all 50 states mandates the reporting of suspected child abuse to social or law enforcement authorities, and many states also mandate the reporting of suspected spousal abuse and elder abuse.
DETECTING AND REPORTING ABUSE
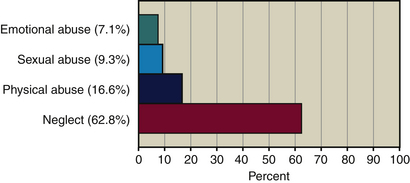
Although all states define abuse differently based on the broad federal definition, all 50 states agree that child maltreatment falls into four distinct categories, in order of prevalence: neglect, the most common type of maltreatment, followed by physical abuse, sexual abuse, and lastly emotional abuse (Table 59-1). Research shows that parents of abused children will frequently change physicians in order to prevent detection, but they are more likely to continue to visit the child’s dentist.2 This makes it increasingly important that dental professionals identify types of abuse, oral and dental aspects of abuse, and physical as well as nonphysical indicators of abuse and know how to identify and report abuse.
| Category | Description |
|---|---|
| Neglect | Deprivation of adequate food, water, clothing, shelter, medical care, or supervision; also includes failure to educate a child as required by law. |
| Physical abuse | Nonaccidental injury or threatened injury, e.g., kicking, biting, hitting, pushing, choking, assault with weapons. |
| Sexual abuse | Use of sex to hurt, degrade, dominate, humiliate, and gain power over the victim. As a violent act of aggression, forced sexual activity, marital rape, and sexual sadism are forms of sexual domestic violence and often accompany physical abuse. |
| Emotional and/or psychologic abuse | Intimidation with gestures, yelling, smashing things, or destroying the victim’s property; threats to harm a child or children or keep them from the victim; isolating the victim from family and friends; and economic domination. Destroys the victim’s self-esteem; includes verbal abuse, excessive demands on the child’s performance, and withholding love and affection. Scars of emotional and/or psychologic abuse are traumatic and long-term. |
Neglect accounts for over 60% of all reported cases of abuse, followed by reports of physical abuse, sexual abuse, and emotional abuse (Figure 59-1). The U.S. Department of Health and Human Services reports that over 899,000 children were victims of maltreatment in 2005,3 and that trend has been on the rise since 1985 according to the Child Welfare League of America, which categorized child abuse as an epidemic.4
DEFINING ABUSE
Abuse can encompass an array of different victimizing social issues including but not limited to child maltreatment, spousal or intimate partner violence (IPV), and elder or vulnerable adult abuse. Although each is defined slightly differently, all have common, defining characteristics such as control and often violent behavior, evidence of which can often be detected clinically. Dental hygienists, as first-line healthcare providers, must know signs and symptoms of abuse and neglect, indicators of family violence and elder abuse, and procedures for documenting and reporting suspected abuse to the appropriate social or law enforcement authorities.
Child Abuse
The Federal Child Abuse Prevention and Treatment Act (CAPTA) (42USCA §5106g) as amended by the Keeping Children and Families Safe Act of 2003, broadly defines abuse and neglect as follows:
 Any recent act or failure to act on the part of a parent or caretaker that results in death, serious physical or emotional harm, sexual abuse, or exploitation, or
Any recent act or failure to act on the part of a parent or caretaker that results in death, serious physical or emotional harm, sexual abuse, or exploitation, orEach state is then responsible for establishing its own definitions within the minimum standards set by federal legislation.
The National Center on Child Abuse and Neglect, created by CAPTA, serves as an information clearinghouse and provides more specific definitions—for example, child physical abuse is “[t]he physical injury or maltreatment of a child under the age of 18 by a person who is responsible for the child’s welfare under circumstances which indicate that the child’s health or welfare is harmed or threatened thereby.”
This definition also encompasses sexual abuse, sexual exploitation, physical or emotional abuse, and willful cruelty or unjustifiable punishment of a child.
Although CAPTA defines neglect as the deprivation of adequate food, clothing, shelter, and medical care, dental neglect as promulgated by the American Academy of Pediatric Dentistry is “[t]he willful failure of parent or guardian to seek and follow through with treatment necessary to ensure a level of oral health essential for adequate function and freedom from pain and infection.”
Domestic or Intimate Partner Violence
Spousal abuse or intimate partner violence ranks as the primary cause of traumatic injury to women and one of the leading causes of death for pregnant women in the United States.5 Battering, one type of physical abuse, is the most frequent cause of injury to women, accounting for more emergency room visits than the combination of automobile accidents, muggings, and rapes. Although over 4.8 million women are reportedly battered each year, only a few states have mandatory reporting requirements for IPV.6 Many states do, however, encompass domestic violence reporting requirements under laws requiring the reporting of injuries resulting from violence, criminal acts, or deadly weapons.
Although controversy exists regarding mandatory reporting with all types of abuse, opponents of mandatory reporting of IPV seem to receive the most attention. Opponents of mandated reporting of domestic violence include both victims and healthcare providers who believe that mandatory reporting may increase violence by the perpetrators, diminish clients’ autonomy, and compromise client-clinician confidentiality. Oral health professionals should check with their state bar association or search their state’s government website to identify domestic violence reporting requirements in their legal jurisdictions.
Elder Abuse
According to the U.S. Department of Health and Human Services Administration on Aging, elder or vulnerable adult abuse includes any knowing, intentional, or negligent act by a family member or caregiver that risks or causes harm to the elder or vulnerable adult, including physical abuse, sexual abuse, emotional or psychologic abuse, financial or material exploitation, neglect, self-neglect, and abandonment.7 Currently, all 50 states have elder abuse prevention laws and methods for reporting suspected abuse. A complete state-by-state list of toll-free elder abuse reporting numbers can be found in the Web Resources section of the  website. Most states mandate that healthcare professionals report suspected elder abuse; some states additionally mandate reporting by financial professionals owing to the prevalence of financial scams targeting elderly people.
website. Most states mandate that healthcare professionals report suspected elder abuse; some states additionally mandate reporting by financial professionals owing to the prevalence of financial scams targeting elderly people.
Elder neglect, which encompasses neglect by caregivers and elder self-neglect, accounts for over 50% of all cases of elder abuse reported to social services.8 Neglect of an elder or dependent adult includes failure of caregivers to provide for basic needs such as personal hygiene, nutrition, clothing, or shelter and failure to provide protection from health and safety hazards.
Often, because of social isolation and limited mobility, visits to the doctor or dentist are the only contact that elderly or vulnerable adults have outside the home. This places the burden of identifying abuse, neglect, and self-neglect in the hands of healthcare professionals. Awareness of signs and symptoms and ability to ask the right questions are critical to identification.
IDENTIFYING ABUSE AND NEGLECT
Oral and Perioral Manifestations9,10
The lips are the most common site for injuries associated with child abuse, followed by injuries to oral mucosa, teeth, gingivae, and tongue.9 Tooth avulsion and tooth fracture occur subsequent to oral trauma and often signal abuse (Figure 59-2). Aside from blows to the face, many oral injuries are caused by forced feeding with utensils, bottles, cups, or fingers or of scalding liquids or caustic substances.9

Figure 59-2 A, Tooth avulsion in a child as a consequence of being punched in the mouth. B, Tooth fracture of central and lateral incisors consequent to a beating when child landed against a chest of drawers.
(Courtesy Dr. Lynn Douglas Mouden, cofounder of PANDA [Prevention of Abuse and Neglect through Dental Awareness].)
Although difficult to identify, neglect is typically a failure by the parent or guardian to provide for basic physical, educational, or emotional needs. Dental neglect manifests as poor oral hygiene, rampant dental caries, or failure to follow through with dental treatment (Figure 59-3). Because these conditions can lead to pain, infection, and loss of function, dental neglect can become serious if unreported.
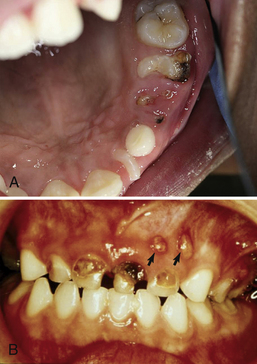
Figure 59-3 A, Dental neglect. Rampant dental caries destroyed primary maxillary molar to the root. B, Dental neglect. Multiple paruli caused by rampant tooth decay.
(Courtesy Dr. Lynn Douglas Mouden, cofounder of PANDA [Prevention of Abuse and Neglect through Dental Awareness].)
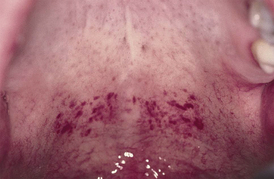
Signs of sexual abuse, often present in a child’s oral cavity, may be hard to identify. Some oral indicators of sexual abuse include condyloma acuminatum (venereal warts), which appear as a cauliflower-like growth on the lips, palate, gingiva, or tongue (Figure 59-4); syphilis, which may emerge as an ulcerated chancre or mucous patch (Figure 59-5); gonorrhea, which may appear as pharyngitis, tonsillitis, or gingivitis; and herpes, which can manifest as gingivostomatitis (Figure 59-6). Presences of petechiae or bruising of the soft palate at the junction of the hard and soft palates may also indicate forced oral sex.

Figure 59-4 Indicator of oral sexual abuse. Condylomas. Venereal warts transmitted to the oral cavity through sexual abuse.
(Courtesy Dr. Lynn Douglas Mouden, cofounder of PANDA [Prevention of Abuse and Neglect through Dental Awareness].)
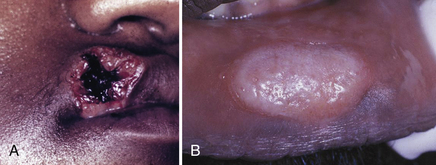
Figure 59-5 A, Indicators of oral sexual abuse. Syphilis emerging as an ulcerated chancre on lip. B, Syphilis emerging as a mucous patch on lip.
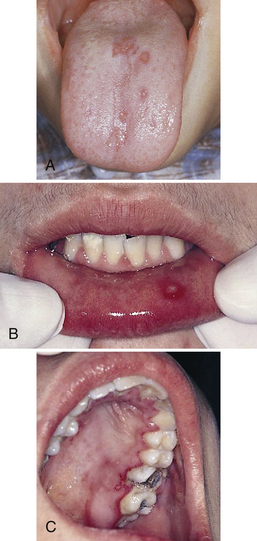
Figure 59-6 A, Indicators of oral sexual abuse. Herpetic gingivostomatitis in a child. B, Herpetic gingivostomatitis in an adolescent. C, Herpetic gingivostomatitis in an adolescent.
As with all indicators of abuse or neglect, the dental hygienist records any oral or perioral indicators of sexually transmitted disease, as these are a clear indicator of sexual abuse in children especially if confirmed by a history of oral-genital contact; for example, palatal petechiae could be a sign of forced oral sex (Figure 59-7).10 After documenting all observations and obtaining a complete client history, the hygienist consults with the dentist and immediately reports suspicions to Child Protective Services (CPS) or law enforcement so that an investigation can be initiated. Common indicators of abuse to look for during oral assessment are found in Table 59-2.10 The dental hygienist examines the oral cavity for evidence of contusions, lacerations, burns, or scarring; inquires about their origin; and documents findings in the client record.
TABLE 59-2 Indicators of Abuse and Neglect in Clients
∗ Normal childhood injuries tend to occur on bony protrusions, e.g., knees and elbows. Bruises caused by abuse are often found on nonbony areas, e.g., arms, legs, and neck.
Physical Indicators of Abuse and Neglect10
Other manifestations of abuse and neglect identifiable on the head, neck, and face include injuries such as bruises, welts, bite marks, burns, lacerations, and abrasions (Figure 59-8). Behavioral and emotional signs of abuse include expressions of aggression, disruptive behavior, anger, rage, or unusual anxiety or fear. Inappropriate seasonal clothing worn to cover injuries to the arms and legs, hard-to-believe stories about how the injuries occurred, and evidence of repeated injuries or multiple bruises in various stages of healing may indicate frequent violent abuse.

Figure 59-8 Infant with bilateral facial bruises from multiple beatings.
(Courtesy Dr. Lynn Douglas Mouden, cofounder of PANDA [Prevention of Abuse and Neglect through Dental Awareness].)
Neglect, intentional or unintentional, is the deprivation of basic needs such as adequate food, clothing, shelter, supervision, education, and medical care Whatever the reason, the dental hygienist should be cognizant of the indicators of dental neglect such as untreated rampant caries, poor hygiene, and willful failure to seek dental care and follow through with dental care plans. Unintentional neglect may be due to knowledge deficits, poor parenting skills, family isolation, lack of dental insurance, or poverty.
The client may confide in the caregiver, complain of hunger or thirst, or display a lack of interest in the surroundings. Abuse victims may exhibit passive or withdrawn behavior, poor self-image, sexual acting out, depression, anxiety disorders, substance and alcohol abuse, eating disorders, hostility, lack of cooperation, self-destructive or self-abusive behavior, suicidal thoughts, social or academic problems, and/or reluctance to return to a waiting adult. The victim’s abuser may monitor interactions, answer questions directed to the client, seem overly solicitous, refuse to leave the treatment area, or display hostility.
Disclosures of Abuse
Given a relationship of trust and rapport, clients may disclose personal information or confide in the dental hygienist. Dental hygienists who suspect abuse can create an opportunity for the client to mention an abuse problem by saying something like the following:
 “Now that violence against women is so common, and there is help available for those who suffer from abuse, I am asking all clients routinely about violence in their lives.”
“Now that violence against women is so common, and there is help available for those who suffer from abuse, I am asking all clients routinely about violence in their lives.”Although maintaining confidentiality is important, allegations or reports of abuse must be reported as required by law and ethics (referred to as disclosure). When a client reports abuse, the hygienist must document that disclosure in the client record and report the disclosure to CPS. Of all substantiated reports of abuse or neglect made to CPS, two thirds are made by doctors, nurses, educators, social workers, dentists, and dental hygienists.
It is not the responsibility of the dental professional to diagnose or investigate suspected abuse; rather, law enforcement and CPS have the expertise and resources to investigate such reports.
Abuse versus Accidental Injury
Frequently children have accidental or unintentional injuries that mimic abuse. Healthcare providers use their professional judgment and clinical skill to assess the location, size, shape, and mode of injuries. Accidental injuries normally heal at the same time, whereas injuries from abuse will be in various stages of healing. Accidental injuries also normally occur over bony prominences such as knees and elbows, whereas injuries from abuse often occur on surfaces away from bony prominences such as the neck, head, trunk, buttocks, hands, and upper arms.11
REPORTING ABUSE
Mandatory Reporters
All 50 states have laws that require certain healthcare professionals (also know as the mandated reporter) to report suspected child abuse or neglect to CPS or law enforcement. Most states require that suspected domestic violence, spousal abuse, elder abuse, or vulnerable adult abuse be reported as well. Failure to report suspected neglect and/or abuse by a mandated reporter can carry harsh penalties including fines and prison time. Penalties for failing to report neglect or abuse can range from 10 days’ to 5 years’ imprisonment and fines ranging from $100 to $5000. Although penalties vary, most states classify a first failure to report as a misdemeanor; however, several states upgrade a second failure to report to a felony.
Because definitions for what constitutes a negligent or abusive act can vary from state to state, dental hygienists as well as all healthcare providers should be familiar with their state’s definitions to better understand what is reportable. According to the Child Welfare Information Gateway, many states define abuse in terms of harm or threatened harm to the health or welfare of a child. In defining neglect the standards of many states include “acts or omissions,” “reckless failures or refusals to act,” or “failure to provide” as guidelines for mandatory reporters in deciding whether to make a report to CPS.12
For a complete list of definitions and reporting requirements, go to the website of the Children’s Bureau, Administration for Children and Families, U.S. Department of Health and Human Services, www.childwelfare.gov, and select “State Statutes Search.” Other domestic abuse resources are listed in Box 59-1 and the Web Resources section of the  website.
website.
Methods for Reporting
Each state has its own reporting mechanisms for suspected abuse and/or neglect. For example, suspected child abuse or neglect can be reported to CPS, but the mechanisms for reporting suspected IPV, domestic violence, and elder or vulnerable adult abuse can vary. Some states have dedicated Family Violence or Adult Protective Services, but regardless of the state or type of abuse suspected, oral health professionals may always report suspected abuse as an emergency by dialing 911.
Oral healthcare professionals do not gather evidence to build an abuse or neglect case if they suspect abuse; rather, their duty is to report their suspicions to the appropriate authority and document their observations in the client record. As a legal document, the treatment record must document objectively all findings and disclosures made by the client.
Why Dental Health Professionals Fail to Report
The American Dental Association’s Principles of Ethics and Code of Professional Conduct states that its members “shall be obliged to become familiar with the signs of abuse and neglect and to report suspected cases to the proper authorities.” Nonetheless, lack of reports of suspected abuse and neglect by dental providers stems from lack of knowledge of requirements and procedures; Thomas et al.2 reported the following:
 Approximately 36% of dentists reported that they suspected child abuse in one or more of their patients.2
Approximately 36% of dentists reported that they suspected child abuse in one or more of their patients.2 Approximately 73% of dentists and 69% of dental hygienists did not know where to report suspected child abuse.2
Approximately 73% of dentists and 69% of dental hygienists did not know where to report suspected child abuse.2Dental hygienists and dentists must be aware of reporting requirements and maintain a reporting policy and procedure in their practices.
CLIENT EDUCATION TIPS
LEGAL, ETHICAL, and SAFETY ISSUES
 Given certain state requirements and the litigation protection provided to mandated reporters, failure to report suspected neglect and/or abuse by a mandated reporter can carry harsh penalties, including fines and prison time.
Given certain state requirements and the litigation protection provided to mandated reporters, failure to report suspected neglect and/or abuse by a mandated reporter can carry harsh penalties, including fines and prison time.KEY CONCEPTS
 Dental hygienists should be especially cognizant of physical abuse, because 60% to 75% of all physical signs of abuse occur on the neck and craniofacial regions.
Dental hygienists should be especially cognizant of physical abuse, because 60% to 75% of all physical signs of abuse occur on the neck and craniofacial regions. Legislation in all 50 states mandates that certain members of the dental healthcare team report suspicions of abuse and neglect to social services or law enforcement agencies and provides protection from retaliatory litigation from parents or caregivers.
Legislation in all 50 states mandates that certain members of the dental healthcare team report suspicions of abuse and neglect to social services or law enforcement agencies and provides protection from retaliatory litigation from parents or caregivers. Failure of a mandated reporter to report suspected abuse is a misdemeanor in most states, punishable by fine and/or imprisonment.
Failure of a mandated reporter to report suspected abuse is a misdemeanor in most states, punishable by fine and/or imprisonment. Parents or guardians of abused children often change physicians, but they are more likely to continue to visit their child’s dentist.
Parents or guardians of abused children often change physicians, but they are more likely to continue to visit their child’s dentist. Each state establishes its own definitions for abuse within the minimum standards set by federal legislation.
Each state establishes its own definitions for abuse within the minimum standards set by federal legislation. The American Academy of Pediatrics reports that lips are the most common site of injuries associated with child abuse.
The American Academy of Pediatrics reports that lips are the most common site of injuries associated with child abuse. Oral indicators of abuse include a wide range of oral injuries that are clearly evident during an oral examination.
Oral indicators of abuse include a wide range of oral injuries that are clearly evident during an oral examination. Because the dental treatment record is a legal document, the dental hygienist should record all indicators of abuse or neglect accurately and clearly.
Because the dental treatment record is a legal document, the dental hygienist should record all indicators of abuse or neglect accurately and clearly.CRITICAL THINKING EXERCISES
Consider these questions when analyzing the following cases:
Case Study 1: You are the hygienist treating an 11-year-old boy whose family has both health and dental insurance. Over the past year, the boy failed to show up for four previously scheduled appointments. On examination you find very poor oral hygiene and several obvious carious lesions on the maxillary and mandible primary molars although he does not complain of any pain or discomfort. On review of the boy’s record, you note that the caries and poor dental hygiene were also documented during his last visit. At the end of the appointment, you speak with the boy’s father and explain the importance of good oral hygiene and the control of the oral infection and recommend that the carious teeth be restored before they become painful and infect others in the family. The boy’s father first says that they’ll be out of town and then says that he doesn’t have his planner with him and that he will have to call the appointment desk to schedule an appointment. You fear that he will not return for this son’s dental care.
Discussion of Case 1: Initially, this scenario may appear to be a case of neglect given that the patient has several untreated carious lesions and parents failed to keep four previous appointments despite being fully insured. According to the CAPTA definition of abuse, because the client is not in any pain and there is no evidence of impaired function or quality of life, this scenario, although sad, most likely does not qualify as a case of neglect. There is no indication that the parent or guardian willfully failed to ensure a level of oral health essential for adequate function and freedom from pain and infection.
This may also be an example of cultural beliefs about health and disease—for example, that professional dental care is necessary only as a solution to pain. The parent, knowing that the teeth are primary teeth, may not want to put the child through the experience of anesthesia and restoration for teeth that will be replaced by permanent teeth. Nevertheless, the dental hygienist is expected to document findings in the client’s chart and seek confirmation if in doubt.
Case Study 2: You are the dental hygienist treating a 7-year-old girl who has been a client in your practice for several years. The child appears withdrawn and won’t make eye contact when you speak to her but otherwise appears normal. The girl winces on oral assessment and you observe a torn frenum and cuts and bruising of the maxillary gingivae. When asked how the injuries occurred, the child says that she doesn’t know. Suspicious, you review the client chart to see if there are any past references to oral injuries and discover that the girl had similar injuries several visits ago, reportedly from being hit in the mouth with a basketball. You look carefully at the client’s face, neck, and arms for any other signs or suggestions of abuse but see none. When you ask the child’s mother about the injuries, she pauses and then says that she thinks that she mentioned being hit in the face with a ball. Suddenly she becomes concerned about the time and wants to take her daughter home before the end of the visit.
Discussion of Case 2: Although the child’s oral injuries are somewhat consistent with oral trauma from being hit with a hard ball, they are also consistent with being slapped or force-fed, for example, having a cup or utensil forced into the mouth. When the mother’s sudden change in behavior and the child’s withdrawn demeanor are considered along with a documented history of the same type of injury, there is most likely enough information to arouse suspicion. If you suspect abuse, as a dental health professional you have a legal and moral obligation to report your suspicions to law enforcement or Child Protective Services.
1. Thomas J.E., Straffon L., Inglehart M.R., Habil P. Milieu in dental school and practice. J Dent Educ. 2006;70:558.
2. Thomas J.E., Straffon L., Inglehart M.R. Knowledge and professional experiences concerning child abuse: an analysis of provider and student responses. Pediatr Dent. 2006;28:438.
3. U.S. Department of Health and Human Services, Administration of Children, Youth and Families. Child maltreatment, 2005. Washington, DC: U.S. Government Printing Office; 2007.
4. Thomas P. Rise in child abuse called national “epidemic”: states in crisis as abuse cases increase in middle class. ABC News, World News Tonight. April 25, 2005.
5. Johnston B.J. Intimate partner violence screening and treatment: the importance of nursing caring behaviors. J Forensic Nurs. 2006;2:184.
6. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Understanding intimate partner violence. Available at: http://www.cdc.gov/ncipc/dvp/ipv_factsheet.pdf. Accessed October 13, 2008.
7. Department of Health and Human Services Administration on Aging: Elder rights and resources: elder abuse. Available at: http://www.aoa.gov/eldfam/Elder_Rights/Elder_Abuse/Elder_Abuse.aspx. Accessed October 13, 2008.
8. National Committee for the Prevention of Elder Abuse and The National Adult Protective Services Association: The 2004 survey of state adult protective services: abuse and adults 60 years of age and older. Available at: http://www.ncea.aoa.gov/NCEAroot/Main_Site/pdf/2-14-06%20FINAL%2060+REPORT.pdf. Accessed October 13, 2008.
9. American Academy of Pediatrics Committee on Child Abuse and Neglect and American Academy of Pediatric Dentistry Council on Clinical Affairs: Guideline on oral and dental aspects of child abuse and neglect. Available at: http://www.aapd.org/media/Policies_Guidelines/G_Childabuse.pdf. Accessed October 13, 2008.
10. Kellogg N. American Academy of Pediatrics Committee on Child Abuse and Neglect: Oral and dental aspects of child abuse and neglect. Pediatrics. 2005;116:1565.
11. Kellogg N.D. American Academy of Pediatrics Committee on Child Abuse and Neglect: Evaluation of suspected child physical abuse. Pediatrics. 2007;19:1232.
12. Child Welfare Information Gateway: Definitions of child abuse and neglect: state statutes series. Available at: http://www.childwelfare.gov/systemwide/laws_policies/statutes/define.cfm. Accessed October 13, 2008.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..