Digital Imaging
After completion of this chapter, the student will be able to do the following:
• Define the key terms associated with digital imaging
• Describe the purpose and use of digital imaging
• Discuss the fundamentals of digital imaging
• List and describe the equipment used in digital imaging
• List and describe the two types of digital imaging
• Describe the patient and equipment preparations required for digital imaging
• List and discuss the advantages and disadvantages of digital imaging
For more than a century, film has been the only medium and recording device for dental radiography. Today, digital technology can be found in many aspects of a dental office, including intraoral digital cameras, digital blood pressure cuffs, and electronic patient files. Advances in technology have also produced a significant impact in the field of dental digital imaging.
Such advances in computer technology have resulted in a unique “filmless” radiography system known as digital imaging. Since its introduction to dentistry in 1987, digital imaging has influenced not only how dental disease is recognized but also how it is diagnosed. Digital imaging is a dependable and versatile technique that improves the diagnostic capabilities in the field of dentistry. Before the dental radiographer can use this very specialized technology, an understanding of the basic concepts, which include terminology, purpose, use, and fundamentals, is necessary. In addition, the dental radiographer must have a working knowledge of the equipment used in digital imaging.
The purpose of this chapter is to present the basic concepts of digital imaging, to introduce the types of digital imaging, and to discuss the advantages and disadvantages of digital imaging.
Basic Concepts
Digital imaging is a technique used to record radiographic images. Unlike conventional dental radiography techniques discussed in the previous chapters, no film or processing chemistry is used. Instead, digital imaging uses an electronic sensor as well as a computerized imaging system that produces radiographic images almost instantly on a computer monitor. Before the dental radiographer can use this technique competently, a thorough understanding of the terminology and fundamentals of digital imaging is necessary. Knowledge of radiation exposure, equipment, and types of digital imaging is also required.
Terminology
Analog image: Radiographic image produced by conventional film.
Bit-depth image: Number of possible gray-scale combinations for each pixel (e.g., 8 bit-depth image has gray-scale combination of 28, which equals 256 shades of gray).
Charge-coupled device (CCD): Solid-state detector used in many devices (e.g., fax machine, home video camera); in digital imaging, CCD is an image receptor found in the intraoral sensor.
Digital imaging: Filmless imaging system; a method of capturing a radiographic image using a sensor, breaking it into electronic pieces, and presenting and storing the image using a computer.
Digital image: An image composed of pixels.
Digital subtraction: One feature of digital imaging; a method of reversing the gray scale as an image is viewed; radiolucent images (normally black) appear white, and radiopaque images (normally white) appear black.
Digitize: In digital imaging, to convert an image into a digital form that, in turn, can be processed by a computer.
Direct digital imaging: Method of obtaining a digital image, in which an intraoral sensor is exposed to x-radiation to capture a radiographic image that can be viewed on a computer monitor.
Indirect digital imaging: Method of obtaining a digital image, in which an existing radiograph is scanned and converted into a digital form by using a CCD camera.
Line pairs/millimeter (lp/mm): Measurement used to evaluate the ability of the computer to capture the resolution (or detail) of a radiographic image.
Pixel: A discrete unit of information. In digital electronic images, digital information is contained in, and presented as, discrete units of information; also termed picture element.
Sensor: In digital imaging, a small detector that is placed intraorally to capture a radiographic image.
Storage phosphor imaging: Method of obtaining a digital image in which the image is recorded on phosphor-coated plates and then placed into an electronic processor, where a laser scans the plate and produces an image on a computer screen.
Purpose and Use
The purpose of digital imaging is to generate images that can be used in the diagnosis and assessment of dental disease. The images produced are diagnostically equivalent to film-based imaging and enable the dental radiographer to identify many conditions that may otherwise go undetected, as well as to see conditions that cannot be identified clinically. Similar to film-based radiographic procedures, digital imaging allows the radiographer to obtain a wealth of information about teeth and supporting structures. Uses of digital imaging include the following:
• To detect lesions, diseases, and conditions of teeth and surrounding structures
• To confirm or classify suspected disease
• To provide information during dental procedures (e.g., root canal therapy instrumentation and surgical placement of implants)
• To evaluate growth and development
• To illustrate changes secondary to caries, periodontal disease, or trauma
• To document the condition of a patient at a specific point in time
Fundamentals
The term digital imaging refers to a method of capturing a radiographic image using a sensor, breaking the image into electronic pieces, and presenting and storing the image using a computer. Remember that film-based images are produced when x-ray photons strike an intraoral film; the information recorded on the film is known as an analog image. Analog images are depicted by a continuous spectrum of gray shades between the extremes of white and black. It might be helpful to visualize a painting done entirely in black, grays, and white; these shades flow together on a canvas, and it is difficult to see where one shade ends and another begins. In digital imaging, the sensor receives the analog information and converts it to a digital image in the computer processing unit. The digital image is an array of picture elements, called pixels, with discrete gray values for each pixel. Imagine the same black, gray, and white painting just described, but in a mosaic pattern instead of the shades flowing together. Each tiny square of the mosaic is similar to an individual pixel.
Traditional film-based radiography consists of x-radiation interacting with the silver halide crystals of the emulsion, production of a latent image, and chemical processing to convert the latent image into a visible image. In digital imaging, a sensor, or small detector, is placed inside the mouth of the patient to capture the radiographic image. The sensor is used in place of intraoral dental film. As in conventional radiography, the x-ray beam is aimed to strike the sensor. An electronic charge is produced on the surface of the sensor; this electronic signal is digitized, or converted into “digital” form. The sensor, in turn, transmits this information to a computer, and the computer stores the incoming electronic signal. Data acquired by the sensor are communicated to the computer in analog form and are then converted into digital form by the use of an analog-to-digital converter (ADC). Software is used to store the image electronically. The image is displayed within seconds to minutes and may be readily manipulated to enhance the appearance for interpretation and diagnosis.
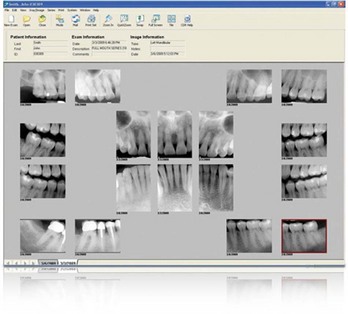
With digital imaging, the term image (not radiograph or x-ray film) is used to describe the pictures that are produced (Figure 25-1). Digital imaging systems are not limited to intraoral images; panoramic, cephalometric, and other extraoral images may also be obtained (Figure 25-2). For example, the extraoral film traditionally used in panoramic radiography is replaced with an electronic sensor that delivers the image information to a computer for storage in digital format. As with intraoral radiography, the extraoral images are displayed on a computer monitor and may be stored for future use.
Radiation Exposure
Digital imaging requires less x-radiation than does conventional radiography. Less x-radiation is necessary to form a digital image on the sensor because the typical sensor is more sensitive to x-radiation than is conventional film. Exposure times for digital imaging are 50% to 90% less than those required for conventional radiography. For example, the typical exposure time required to produce an image for digital imaging is 3 impulses (3/60 or 0.05 second). This exposure time is much less than the 12 impulses (12/60 or 0.2 second) required for intraoral film used in conventional radiography. With less radiation exposure, the absorbed dose to the patient is significantly reduced.
Equipment
Digital imaging requires the use of specialized equipment. The essential components of a digital imaging system include an x-radiation source, an intraoral sensor, and a computer.
X-Radiation Source
Most digital imaging systems use a conventional dental x-ray unit as the x-radiation source. The conventional x-radiation source is compatible with the digital imaging system; however, the x-ray unit timer must be adapted to allow exposures in a time frame of 1/100 of a second. A standard x-ray unit that is adapted for digital imaging can still be functional for conventional radiography (Figure 25-3).
Intraoral Sensor
As previously defined, the sensor is a small detector that is placed intraorally to capture the radiographic image. Some sensors are thick, bulky, and rigid, whereas others mimic conventional film in size and flexibility (Figure 25-4). Most manufacturers produce sensors similar in dimension to sizes 0, 1, 2, and 4 of intraoral films. Intraoral sensors used in digital imaging systems may be wired or wireless. The term wired refers to the fact that the imaging sensor is physically linked by a fiberoptic cable to a computer that records the generated signal (Figure 25-5). In wired systems, the cable varies in length from 8 to 35 feet; the shorter the cable, the more limited is the range of motion. The term wireless refers to an imaging sensor that is not linked by a cable; the wireless sensor sends data to the computer electronically.

FIGURE 25-4 A #2 intraoral film, which is similar in size and shape to a sensor used in digital imaging.

FIGURE 25-5 A wired sensor used with digital imaging showing the intraoral sensor at one end and the link to the computer at the other end. (Courtesy of DEXIS, Des Plaines IL.)
The most popular types of sensor technology include the charge-coupled device and the complementary metal oxide semicondutor.
Charge-Coupled Device: The charge-coupled device (CCD) is one of the most common image receptors used in dental digital imaging. The CCD technology used in digital imaging relies on a specialized fabrication process that is costly to manufacture.
The CCD is not a new technology; it was initially developed in the 1960s. Currently, CCD technology is used in many devices, including fax machines, home video cameras, microscopes, and telescopes. The CCD is a solid-state detector that contains a silicon chip with an electronic circuit embedded in it. This silicon chip is sensitive to x-radiation or light.
The electrons that compose the silicon CCD can be visualized as being divided into an arrangement of blocks or picture elements known as pixels. A pixel is a small box, or “well,” into which the electrons produced by the x-ray exposure are deposited. A pixel is the digital equivalent of a silver crystal used in conventional radiography. As opposed to a film emulsion that contains a random arrangement of silver crystals, a pixel is structured in an ordered arrangement. The CCD is 640 × 480 individual pixels in size. Consequently, the CCD contains 307,200 pixels and functions to sense transmitted light and translate it into an electronic message.
The x-ray photons that come into contact with the CCD cause electrons to be released from the silicon and produce a corresponding electronic charge. Consequently, each pixel arrangement, or electron potential well, contains an electronic charge proportional to the number of electrons that reacted within the well. Furthermore, each electronic well corresponds to a specific area on the linked computer screen. When x-radiation activates electrons and produces such electronic charges, an electronic latent image is produced. The latent image is then transmitted and stored in a computer and can be converted to a visible image on screen or printed on paper.
Complementary Metal Oxide Semiconductor/Active Pixel Sensor: Another sensor technology that is used in digital imaging is the complementary metal oxide semiconductor/active pixel sensor (CMOS/APS). Although the CMOS process is the standard in the making of semiconductor chips, it was not until APS was developed that CMOS became useful as a sensor in dental digital imaging. The CMOS detector is silicon based and differs from the CCD detector in the way that the pixels are read. At this time, one digital imaging manufacturer uses a CMOS/APS sensor instead of a CCD and claims that it has a 25% greater resolution. Additional advantages of the CMOS/APS technology are the lower production cost of the chip and greater durability than the CCD.
Computer
A computer is used to store the incoming electronic signal. The computer is responsible for converting the electronic signal from the sensor into a shade of gray that is viewed on the computer monitor. Each pixel is represented numerically in the computer by location and the color level of the gray. The range of numbers for a pixel varies from 0 to 255, which creates 256 shades of gray, referred to as a pixel’s gray-scale resolution. In comparison, the human eye can only perceive 32 shades of gray.
The number of possible gray-scale combinations per pixel is known as the bit-depth image. The bit-depth image is determined by the computer software for the digital system. For each pixel, the number of possible gray-scale combinations is 2N; for example, an 8 bit-depth image has a gray-scale combination of 28, which equals 256 shades of gray. The software also allows for manipulation of the pixels, enhancing contrast and density without additional x-ray exposure of the patient.
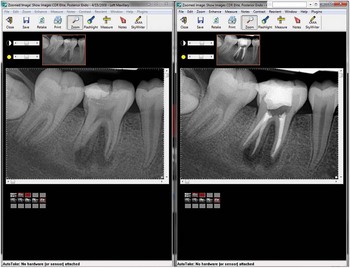
The computer digitizes, processes, and stores information received from the sensor. The exposure can be viewed immediately on the computer monitor. An image is recorded on a computer monitor in 0.5 to 120 seconds, much less time than required for conventional film processing (Figure 25-6). This speed of image recording is extremely useful during certain dental procedures, such as the placement of surgical implants or during endodontic instrumentation. The image may be stored permanently in the computer, printed out as a hard copy for the patient record, or transmitted electronically to insurance companies or referring dental specialists.

FIGURE 25-6 A digital image of the mandibular right periapical region as seen on a computer monitor.
Various computer viewing features are available with digital imaging systems. Digital systems feature split-screen technology, which allows the operator to view and compare multiple images on the same screen (Figure 25-7). This feature is helpful for comparison and for the evaluation of progression of caries or periodontal disease. For example, caries progression can be evaluated by comparing successive bite-wing images. Digital systems also provide a feature that allows specific images to be magnified up to four times the original size. This feature is helpful when evaluating the apical area of a tooth. Many digital systems include a measurement tool as part of the imaging software. Measurement tools are valuable in therapies such as endodontic procedures or in implant treatment planning. Linear and angular measurements must be made with the proper projection geometry, avoiding such errors as elongation or foreshortening, which may distort the measurements (Figure 25-8).
Types of Digital Imaging
Two methods of obtaining a digital image currently exist: (1) direct digital imaging and (2) indirect digital imaging.
Direct Digital Imaging
The essential components of a direct digital imaging system include an x-ray machine, an intraoral sensor, and a computer monitor. A sensor with a fiberoptic cable linked to the computer is placed into the mouth of the patient and exposed to x-radiation (Figure 25-9). The sensor captures the radiographic image and then transmits the image to a computer monitor. Within seconds of exposing the sensor to radiation, an image appears on the computer screen. Software is then used to enhance and store the image.
Indirect Digital Imaging
Scanning Traditional Radiographs
The essential components of an indirect digital imaging system include a CCD camera and a computer. In the scanning method, an existing radiograph is digitized using a CCD camera. The CCD camera scans the image on the film, digitizes or converts the image, and then displays it on the computer monitor. This concept is similar in theory to scanning an image, for example, a photograph, to a computer screen. Indirect digital imaging is inferior to direct digital imaging because the resultant image is similar to a “copy” of an image versus the “original” image.
Storage Phosphor Imaging
A second type of indirect digital imaging is storage phosphor imaging, which is a wireless digital imaging system. Storage phosphor imaging is also referred to as photo-stimulable phosphor imaging (PSP). In this system, a reusable imaging plate coated with phosphors is used instead of a sensor with a fiberoptic cable. The phosphor-coated plate is flexible and is placed into the mouth in the same way as intraoral film (Figure 25-10). A phosphor-coated plate resembles an intensifying screen used to expose an extraoral film in that it converts x-ray energy into light. The images are cleared from the plates by exposure to viewbox light for several minutes, or the images may be erased from the plates immediately after the scanning process. Once the image is erased, the plates may be wrapped in plastic and sterilized for reuse.

FIGURE 25-10 A beam alignment device, which holds a PSP digital sensor for a bite-wing image exposure. (Courtesy of Schick Technologies, Long Island City, NY.)
Storage phosphor imaging records diagnostic data on a plate after x-ray exposure and then uses a high-speed scanner to convert the information into electronic files. After exposure, the plate is removed from the mouth and placed into an electronic processor, where a laser scans the plate and produces an image that is transferred to a computer screen. Because of this step involving laser scanning, which can take 30 seconds to 5 minutes, this type of digital imaging is less rapid than direct digital imaging (Figure 25-11). The dental radiographer must take care in placing the phosphor plates in the mouth and exposing them correctly. Currently, some PSP systems are unable to distinguish images that have been exposed backward (similar to placing a film in the mouth with the colored tab facing the beam of radiation). It is recommended that the dental radiographer view the mounted images and confirm all the findings while the patient remains seated in the dental chair.
Step-By-Step Procedures
Step-by-step procedures for the use of digital imaging systems vary from manufacturer to manufacturer. It is critical to refer to the manufacturer’s instruction booklet for information on the operation of the system, equipment preparation, patient preparation, and exposure. Only general guidelines concerning sensor preparation and placement are provided here.
Sensor Preparation
Digital imaging involves the placement of the intraoral sensor in the mouth of the patient, using the same technique as in conventional film placement. Whether using indirect or direct digital imaging, it is important that the individual sensors are kept sterile. Storage phosphor sensors are sealed and waterproofed (Figure 25-12). For infection control purposes, sensors used in direct digital imaging must be covered with a disposable barrier or sleeve because they cannot withstand heat sterilization (Figure 25-13).

FIGURE 25-12 A, Barrier envelopes used to seal and protect the PSP sensors from contamination. B, An example of a PSP sensor, the blue side facing the teeth and the radiation source and the black side facing the tongue. (From Bird DL, Robinson DS: Modern dental assisting, ed 10, St. Louis, 2011, Elsevier.)
Sensor Placement
The sensor is held in the mouth by bite-block attachments or devices that aim the beam and sensor accurately. The paralleling technique is the preferred exposure method because of the dimensional accuracy of images produced and the ease of standardizing such images. Paralleling technique beam alignment devices must be used to stabilize the sensor in the mouth. As with conventional intraoral film, the sensor is centered over the area of interest. Various manufacturers have produced beam alignment devices that can be used not only with film but with wired sensors and PSP plates as well (Figure 25-14).
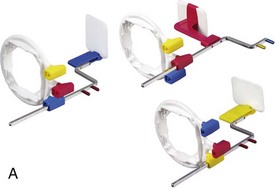


FIGURE 25-14 A, Beam alignment devices holding film for anterior, posterior, and bite-wing exposures. B, The same beam alignment devices now holding digital sensors for anterior, posterior, and bite-wing exposures. (Courtesy of Dentsply RINN, Elgin, IL.) C, Beam alignment bite-blocks manufactured with adhesive backing to hold PSP digital sensors firmly in place. (Courtesy of Schick Technologies, Long Island City, NY.)
Advantages and Disadvantages
As with any intraoral radiographic technique, digital imaging has both advantages and disadvantages.
Advantages of Digital Imaging
1. Superior gray-scale resolution. A primary advantage of digital imaging is the superior gray-scale resolution that results. Digital imaging uses up to 256 (over 16,000, depending on the manufacturer) shades of gray compared with the 16 to 25 shades of gray differentiated on conventional film. This advantage is critical because diagnosis is often based on contrast discrimination. The ability to manipulate the density and contrast of the digital image without additional exposure of the patient to x-radiation is also an important advantage (Figure 25-15). In addition, studies have investigated the diagnostic capability of the intraoral sensor used in digital imaging. Digital imaging enables the dental professional to identify dental disease just as with traditional film methods. One of the ways to measure the diagnostic value of digital imaging is through its ability to capture detail, or resolution. Line pairs/millimeter (lp/mm) is a measurement of the ability of the digital system to capture the detail in an image. Most digital imaging manufacturers maintain a range of 6 to 22 lp/mm. The human eye can only recognize approximately 8 lp/mm. All the current digital systems produce a diagnostically acceptable image.

FIGURE 25-15 Magnification of a periapical image from a full mouth series, which allows the dental professional to take a closer look at teeth #18 and #19. (Courtesy of Schick Technologies, Long Island City, NY.)
2. Reduced exposure to x-radiation. Another primary advantage of the digital imaging system is the reduction in patient exposure to x-radiation. Decreased exposure results from the sensitivity of the CCD. The radiation exposure for digital imaging systems is 50% to 90% less than that required for E-speed film used in conventional radiography.
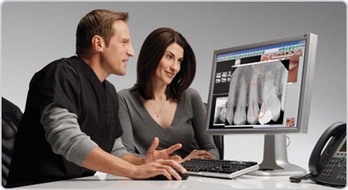
3. Increased speed of image viewing. Dental professionals as well as patients are able to view the digital images instantaneously, which allows for immediate interpretation and evaluation. Chairside viewing of the digitized image on a computer monitor within moments after exposure continues to be a compelling reason for the growing popularity of this technology.
4. Lower equipment and film cost. Long-term digital imaging eliminates the need for purchasing conventional film, costly processing equipment, and processing solutions. With digital imaging, darkroom and processing solutions and maintenance are unnecessary. Also, environmental costs are reduced because the disposal hazards of processing chemicals, silver salts in film emulsion, and lead foil sheets are avoided. The elimination of darkroom processing errors is also an advantage.
5. Increased efficiency. Dental professionals can be more productive because digital imaging does not interrupt routine patient treatment or care. Dental practices that also use electronic charting have the advantage of the operator’s ability to access both patient data and digital images simultaneously (Figure 25-16). Both image storage and communication are easier with digital networking. The digital image can be incorporated into the electronic record of the patient, and the radiographic image can be printed out whenever needed. Digital images can also be electronically transmitted to referring dentists and specialists, insurance companies, or consultants.

FIGURE 25-16 Two computer monitors side by side allowing the dental professional to view the patient’s electronic chart and the panoramic image at the same time. (From Bird DL, Robinson DS: Modern dental assisting, ed 10, St. Louis, 2011, Elsevier.)
6. Enhancement of diagnostic image. Features such as colorization and zooming allow users to highlight conditions such as bone resorption caused by periodontal disease or to help detect small areas of decay. Another feature that can be used to enhance a diagnostic image is digital subtraction. With digital subtraction, the gray-scale is reversed so that radiolucent images (normally black) appear white and radiopaque images (normally white) appear black (Figure 25-17). Digital subtraction also eliminates distracting background information. For example, this feature permits the operator to remove all anatomic structures that have not changed between radiographic examinations to facilitate identification of changes in diagnostic information. Additional features commonly available in image software include brightness, contrast, sharpness, image orientation, and pseudo-color alteration.
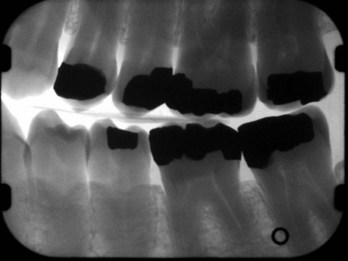
FIGURE 25-17 An example of digital subtraction of a bite-wing image. (Courtesy of Dr. Donald Tyndall, The University of North Carolina School of Dentistry, Chapel Hill, NC.)
7. Effective patient education tool. Digital images can be an effective tool in patient education and interaction. Patients can view radiographic images along with the operator, which facilitates dialogue and rapport and increases a patient’s understanding of the disease process and acceptance of treatment modalities. In addition, the size of the digitized image on the 15-inch or 17-inch computer screen (compared with a 2-inch piece of film) makes the digital image an attractive patient education tool (Figure 25-18).
Disadvantages of Digital Imaging
1. Initial setup costs. The initial cost of purchasing a digital imaging system is a significant disadvantage. The cost depends on the manufacturer, the level of computer equipment currently in the office, and auxiliary features such as the intraoral camera. Maintenance and repairs must also be considered.
2. Image quality. At one time, image quality was a source of debate. The spatial resolution of an image is defined as the number of line pairs per millimeter (lp/mm). Conventional dental x-ray film has a resolution of 12 to 20 lp/mm. A digital imaging system using a CCD has a resolution closer to 10 lp/mm. Considering that the human eye can only perceive 8 to 10 lp/mm, a CCD system is significantly more effective in the recognition of dental disease. Many studies have reported on the ability of the digital image to capture early caries, bone loss, periapical radiolucencies, and so on. The majority of the research has shown that the digital imaging performs at least as well as, and at times even better than, traditional radiography.
3. Sensor size and thickness. Some digital sensors are thicker and less flexible than intraoral film. Patients may complain about the bulkiness of the sensor, which may cause discomfort or elicit the gag reflex. However, with increasing experience and familiarity with the use of these rigid sensors, sensor placement becomes less of an issue. In addition, manufacturers have produced many varieties of beam alignment devices to aid sensor placement (Figure 25-19).
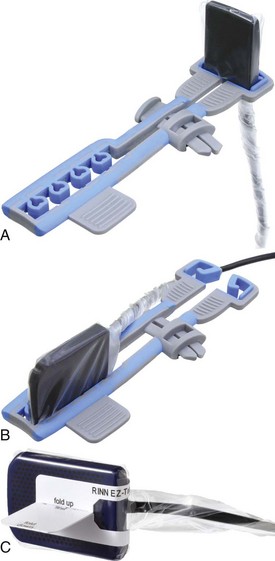
FIGURE 25-19 A, B, Examples of anterior and posterior beam alignment devices holding a direct digital sensor. C, A direct digital sensor fitted with an adhesive bite-wing tab. (Courtesy of Dentsply RINN, Elgin, IL.)
4. Infection control. Some digital sensors cannot withstand heat sterilization. Therefore, these sensors require complete coverage with disposable plastic sleeves that must be changed between patients every time to prevent cross-contamination.
5. Wear and tear. The receptors used in the PSP system are vulnerable to wear and tear and may have a limited lifespan. The phosphor plates are not designed to have their edges bent or softened to accommodate individual patient anatomy. If bending or scratching of the plates occurs, permanent defects will appear on all images exposed, which may obscure diagnostic information.
6. Legal issues. Because the original digital image can be enhanced, it is questionable whether digital images can be used as evidence in lawsuits. To address this concern, manufacturers (for example, Kodak, with its Digital Science Dental Scanning System) have included in the software a warning feature that appears if the image displayed on the monitor is not comparable with the original image. A file copy of the original image should always be kept on the computer, even when characteristics such as density and contrast have been changed.
Summary
• Digital imaging is a method of capturing a radiographic image and displaying it on a computer screen; no film is used, and no film processing chemicals are required.
• A conventional dental x-ray unit is used as the radiation source in digital imaging. A sensor or small detector is placed inside the patient’s mouth, and the x-ray beam is aimed to strike the sensor. The electronic charge produced on the sensor is digitized (or converted into digital form) and can be viewed on a computer monitor.
• Advantages of digital imaging include superior gray-scale resolution, reduced patient exposure to x-radiation, increased speed of image viewing, lower equipment and receptor costs, increased time efficiency, enhanced patient education, and many viewing options to enhance the diagnostic information of the image.
• Disadvantages of digital imaging include initial setup costs of the digital system, image quality, size of the intraoral sensor, wear and tear of sensors, legal issues, and the inability to heat-sterilize the sensor.
Brennan, J. An introduction to digital radiography in dentistry. J Orthod. 2002;29:66–69.
Frommer, HH, Savage-Stabulas, JJ, Digital imaging. Radiology for the dental professional, ed 9, St. Louis, Mosby, 2011.
Levato, C. Are you ready for digital radiography? Dent Pract Finance. 1999;7:17–24.
Lusk, LT. Comparison of film-based and digital radiography. J Pract Hygiene. 1998;7:45–50.
Miles, DA, Van Dis, ML, Jensen, CW, Williamson, GF, Digital imaging. Radiographic imaging for the dental team, ed 4, St. Louis, Saunders, 2009.
Parks, ET, Williamson, GF. Digital radiography: An overview. J Contemp Dent Pract. 2002;3(4):23–39.
Razmus, TF, Williamson, GF. An overview of oral and maxillofacial imaging. In: Current oral and maxillofacial imaging. Philadelphia: Saunders; 1996.
Schleyer, T, et al. The technologically well-equipped dental office. J Am Dent Assoc. 2003;134:30–40.
Tyndall, DA, Ludlow, JB, Platin, E, et al. A comparison of Kodak Ektaspeed Plus film and the Siemens Sidexis digital imaging system for caries detection using receiver operating characteristic analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:113–118.
Van der Stelt, PF. Better imaging: The advantages of digital radiography. J Am Dent Assoc. 2008;139(3):7S–13S.
Van der Stelt, PF. Filmless imaging: The uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136(10):1379–1387.
White, SC, Pharoah, MJ, Digital imaging. Oral radiology: principles and interpretation, ed 6, St. Louis, Mosby, 2009.
Matching
For questions 1 to 9, match each term with its corresponding definition.
________ 1. A small detector that is placed intraorally to capture the radiographic image.
________ 2. An image receptor found in the intraoral sensor.
________ 3. A form of indirect digital imaging in which the image is recorded on phosphor-coated plates and then placed into an electronic processor, where a laser scans the plate and produces an image on a computer screen.
________ 4. To convert an image into digital form that, in turn, can be processed by a computer.
________ 5. A method of obtaining a digital image in which an intraoral sensor is exposed to x-rays to capture a radiographic image that can be viewed on a computer monitor.
________ 6. A discrete unit of information; a picture element.
________ 7. A method of obtaining a digital image, in which an existing radiograph is scanned and converted into a digital form using a CCD camera.
________ 8. A method of reversing the gray scale as a digital image is viewed.
________ 9. A filmless imaging system; a method of capturing a radiographic image using a sensor, breaking the image into electronic pieces, and presenting and storing the image using a computer.
True or False
________ 10. In digital imaging, the term used to describe the picture that is produced is radiograph.
________ 11. Digital imaging requires more x-radiation than does conventional radiography.
________ 12. The x-radiation source used in most digital imaging systems is a conventional dental x-ray unit.
________ 13. Compared with film emulsion, the pixels used in digital imaging are structured in an orderly arrangement.
________ 14. All intraoral sensors can be heat-sterilized after use.
________ 15. The preferred exposure method for intraoral digital imaging is the paralleling technique.
________ 16. One advantage of a digital imaging system is the superior gray-scale resolution that results.
________ 17. Digital subtraction is an advantage in digital imaging because distracting background information is eliminated from the image.
________ 18. The manipulation of the original digital images can be considered a legal issue.
Multiple Choice
________ 19. Digital imaging was introduced to dentistry in:
________ 20. Digital imaging can be used for:
a. detecting conditions of teeth and surrounding structures
b. evaluating the growth and development of jaws
________ 21. Digital imaging requires less radiation than does conventional radiography because:
________ 22. The method of obtaining a digital image similar to scanning a photograph to a computer screen is termed:
________ 23. The image receptor found in the intraoral sensor is termed:
________ 24. Digital imaging systems can be used for:
________ 25. All of the following are advantages of digital imaging except: