6. The Model of Human Occupation
Embracing the complexity of occupation by integrating theory into practice and practice into theory
Kirsty Forsyth and Gary Kielhofner
Overview
Every day, occupational therapists must answer questions such as:
• What are the occupational needs of this client?
• How do I best support the client to engage in this activity?
• What goals does this client want and need to achieve?
• How can I assist in the achievement of these goals?
To answer these and other practice questions, occupational therapists need comprehensive ways of understanding the client situation.
Evidence suggests that, worldwide, occupational therapists use the Model of Human Occupation (MOHO) more than any other framework to address these types of practice question (Law and McColl, 1989, Haglund et al., 2000, National Board for Certification in Occupational Therapy. 2004, Lee et al., 2009 and Taylor et al, 2009). Widespread use of this model reflects the fact that MOHO has the concepts, evidence and practical resources to enable occupational therapists to plan and implement high-quality, evidence-based, client-centred and occupation-focused practice.
This chapter will first take an overview of how and why MOHO was developed. It will then introduce its major concepts and note their relevance to understanding clients and to therapy. Following this, the chapter discusses some of the available resources for using MOHO in practice. Finally, the use of MOHO will be illustrated through a case example.
• MOHO is a client centred, occupation focused, evidence based conceptual model of practice
• MOHO provides a way of embracing the complexity of client?s occupational needs
• MOHO provides specific occupationally focused outcomes measures to measure occupational participation
• MOHO provides a range of therapeutic intervention options
• MOHO has been applied successfully across cultures and used extensively internationally
Why and how MOHO was developed
From the 1960s onward, there was a recognition that occupational therapy had become too concerned with remediating impairment and needed to recapture its original focus on occupation (Reilly, 1962, Shannon, 1970 and Kielhofner and Burke, 1977). The Model of Human Occupation (MOHO) was the first occupation-focused model to be introduced in the profession (Kielhofner, 1980a, Kielhofner, 1980b, Kielhofner and Burke, 1980 and Kielhofner et al., 1980). It was developed by three occupational therapy practitioners who wanted to organize concepts that could guide their delivery of occupation-focused practice. In the three decades since MOHO was first formulated, numerous practitioners and researchers throughout the world have contributed to its development. Today, a literature of approximately 500 published works undergirds this model, making it the most evidence-based, occupational-focused model in the field.
The developers of this model have always sought to ensure that its concepts and tools are relevant and useful in practice. MOHO has been developed through an approach called ‘the scholarship of practice’. This approach emphasizes the importance of an ongoing dialogue between theory/research and practice (Taylor et al 2002). Consequently, the scholarship of practice represents a commitment to scholarship, which supports occupational therapy practice, as well as a commitment to partner clinicians who are involved in the application of MOHO (Fig. 6.1). Moreover, the collaboration ensures that the needs and circumstances of practice shape theory development and research. All participants (for example, clients, therapists, managers, educationalists, students, researchers) take on the role of ‘practice scholars’, sharing responsibility for developing and applying MOHO. MOHO is, therefore, driven by practice concerns, and practice shapes how its theory is articulated and applied. This approach has not only assured MOHO's usefulness in practice, but has also enhanced the profile of occupational therapists, resulting in greater client understanding and satisfaction, and more respect for the occupational therapy contribution made by managers, policy-makers and interdisciplinary colleagues.
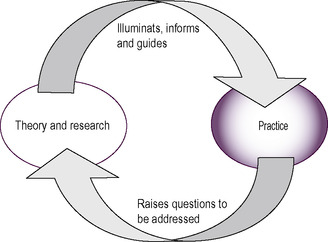 |
| Fig 6.1 • Scholarship of practice. Reproduced with the permission of Professor G. Kielhofner from Challenges of the New Millennium: Keynote Address, WFOT Conference, Stockholm 2003. |
In 1985 the book A Model of Human Occupation: Theory and Application introduced an expanded theory and a wide range of clinical applications (Kielhofner 1985). Revisions of the model were completed in 1995 and 2002, and the fourth edition (Kielhofner 2008) presents the authoritative and most current understanding of this theory and its application; it should be considered the primary reference on the model. For therapists who wish to apply MOHO, this text is a necessary resource.
Other published literature provides additional sources of theoretical discourse, discussions of programmatic applications, cases examples and research findings. The literature on this model is published worldwide. A current bibliography of literature, an evidence-based search engine and hundreds of evidence briefs, along with a wide range of assessment tools and intervention protocols on the model, can be found on a website: http://www.moho.uic.edu/. The website also provides an opportunity to join a list serve where students and practitioners can post practice questions and receive expert advice.
MOHO theory
A conceptual model of practice proposes theory to address certain phenomena with which the model is concerned (Kielhofner 2008). MOHO provides theory to explain occupation and occupational problems that arise in association with illness and disability. Its concepts address:
• the motivation for occupation
• the routine patterning of occupational performance
• the nature of skilled performance
• the influence of environment on occupation.
The following section will address the main conceptual ideas in MOHO (Fig. 6.2), namely:
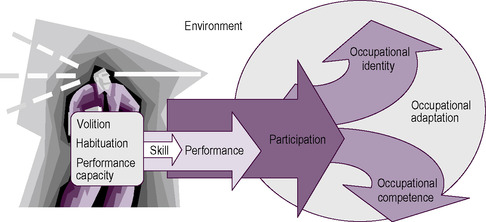 |
| Fig 6.2 • MOHO concepts. Reproduced from Kielhofner, G., 2008. A Model of Human Occupation: Theory and Application, 4th edn, published by Lippincott Williams & Wilkins, Baltimore |
1. embracing the complexity of human occupation
2. components of the person
3. environment
4. occupational performance.
Embracing the complexity of human occupation in practice
MOHO recognizes that occupation (i.e. what a person does in work, play and self-care) is influenced by many factors inside and outside the person. MOHO further emphasizes that each person's inner characteristics and external environment are linked together into a dynamic whole. In order to embrace this complexity, MOHO theory includes a range of concepts. These concepts seek not only to offer explanations of the factors that influence occupation, but also to provide a framework for gathering data about a client's circumstances, generating an understanding of the client's occupational strengths and limitations, and selecting and implementing a course of occupational therapy.
Further, MOHO theory views therapy as a process in which people are helped to do things in order to shape their occupational abilities and occupational identities. MOHO provides a framework for successfully and meaningfully engaging people in occupations, which helps to maintain, restore, or reorganize their occupational lives.
Components of the person
To explain how occupational participation is chosen, patterned and performed, MOHO conceptualizes people as composed of three interconnected ideas:
• volition
• habituation
• performance capacity.
Volition refers to the process by which persons are motivated toward and choose what they do. Habituation refers to a process whereby doing is organized into patterns and routines. Performance capacity refers to both the underlying mental and physical abilities and the lived experience that shapes performance. Each of these three components of the person is discussed in more detail below.
Volition
Volition refers to the process by which people are motivated toward and choose what they do. The concept of volition asserts that all humans have a desire to engage in occupations, and that this desire is shaped by ongoing experiences as we do things. Volition consists of thoughts and feelings that occur in a cycle of anticipating possibilities for doing, choosing what to do, experiencing what one does, and subsequent interpretation of the experience. These thoughts and feelings are concerned with three issues:
1. how effective one is in acting on the world (personal causation)
2. what one holds as important (values)
3. what one finds enjoyable and satisfying (interests).
Personal causation
Personal causation is reflected in our awareness of present and potential abilities (Harter, 1983 and Harter and Connel, 1984) and our sense of how able we are to do what we want to do (Rotter, 1960 and Lefcourt, 1981). Our own culture and social environment tell us what capacities we should have and why they matter. For example, a performer on stage, a taxi driver in a large city, a secondary school teacher, and a farmer in the countryside will each be concerned about very different kinds of ability. Also, developmental level will affect the experience of personal causation. A young child typically will be concerned with developing such skills as walking and playing with toys. An older child may be mostly concerned with school performance and ability to get along with peers and perform in sports. Adolescents usually begin to think about capacity for further education and entry into a line of work. Adults will focus on such things as the capacity for work performance and management of other adult responsibilities such as parenting. Older adults will often be concerned with loss of capacity associated with ageing and how to maintain abilities for personally important things.
Consequently, personal causation is never static, but rather a dynamic unfolding set of thoughts and feelings about our capacities and our efficacy in doing what we want to do. Our unique personal causation influences how we anticipate, choose, experience and interpret what we do. Consequently, the thoughts and feelings that make up personal causation are powerful motivational influences and they also guide how we experience what we do and how we look forward to the future.
Values
Choices of occupations are also influenced by our values. Values are beliefs and commitments that define what we see as good, right and important; they shape our sense of what is worth doing, how we ought to act, and what is the right way of doing things (Lee 1971). The child who plays nicely with other children because he has learned that playing in this way is important is expressing values. The worker who feels she needs to excel, the father who believes it is important to spend time with his children, and the old person who feels compelled to volunteer his services to his church are all examples of people whose values shape what they do. When we cannot live up to our values, we may feel guilty or inadequate and we experience a lack of meaning (Bruner 1990). The worker who has a stroke and subsequently loses his job, the mother whose mental illness interferes with parenting her child, the child whose learning disability makes it difficult to do as well in school as he thinks he should, and the elderly person whose fear of falling interferes with being able to engage in meaningful occupations are all examples of persons who are unable to enact their values.
Interests
Being interested in an occupation means that one feels an attraction based on anticipation of a positive experience in doing that occupation. The experience of pleasure and/or satisfaction in doing something may come from positive feelings associated with either the exercise of capacity, intellectual or physical challenge, fellowship with others, aesthetic stimulation, or other factors. We are more likely to enjoy what we can perform with some level of proficiency when skill is involved in the performance. Csikszentmihalyi (1990) describes flow, a form of ultimate enjoyment in occupations that occurs when a person's capacities are optimally challenged. Often, this preference is manifested as a pattern of related interests such as athletic interest or cultural interests, including theatre and art. Preferring certain occupations over others influences what we are motivated to choose to do.
Illness or impairment can interfere with doing what one is interested in. For instance, a person might lose the capacity to do something he previously enjoyed, or an individual may find that engaging in an interest is no longer pleasurable because it evokes too much pain or fatigue. Persons with depression may find that they no longer enjoy doing what was previously pleasurable. Being able to engage in occupations that interest us and provide us with enjoyment and satisfaction is essential to well-being, and when illness or impairment interferes with this engagement, quality of life is reduced.
Summary
Our interests, values and personal causation affect what everyday activity we are motivated to do, what activities we choose to engage in and how we experience doing them. Illness and disability can interfere with volition in many ways. When this is the case, occupational therapists need to be able to assess and address volitional problems.
Additionally, volition is critical to the occupational therapy process. In order to provide therapy, occupational therapists must enable clients to engage in meaningful activity. Choosing a therapeutic activity and experiencing it as meaningful is a function of volition. Therapy cannot be meaningful unless occupational therapists attend to their client's volition.
The outcomes of therapy also depend on volition. It is not enough to improve a client's capacity. If the client leaves therapy and has no volitional motivation to use that capacity by engaging in activities of value and interest, then the client will not use what he or she has gained in therapy. Thus, therapy should always support the client's volition. Good therapy outcomes require that clients will choose to use their capacity, to develop new capacities, or make adjustments for their limitations because they can see these efforts as providing a life with value and satisfaction over which they can exercise reasonable control.
Habituation
Occupation is more than simply doing things. Every person has some kind of life pattern that is made up of everyday routines and roles. Habituation refers to the process by which people organize their occupational performance into the recurrent patterns of behaviour. These patterns integrate us into our physical and temporal world (when and where we do things) and our social and cultural world (doing things that reflect what we are expected to do by virtue of our position in society). Moreover, they allow us to carry out our daily lives efficiently and automatically. Habituated patterns of action are governed by:
• habits
• roles.
Habits
Habits involve learned ways of doing occupations that unfold automatically. The way we bathe and dress ourselves each morning, and how we drive, take a bus or ride a bike to work or school are examples of habits. We learn these habits through repeated experience. When we learn a habit, we acquire a way of appreciating and behaving in our familiar environments. So, for instance, we recognize the ring of the alarm clock as an indication that it is time to rise and bathe and dress; we know where to find the toothbrush and reach for it without thinking. We know how to turn on the shower and do it unreflectively. Because we do not have think about these things as we go about our morning routine, our routines take less effort and concentration. Our habits always involve cooperation with our environment (Dewey 1922). When our environment changes, our habits may no longer work automatically. For instance, when we find ourselves in an unfamiliar environment such as a hotel room, we may suddenly find that we have consciously to think about and figure out how to do a routine task such as turning on the shower. As the example illustrates, when habits cannot guide our behaviour automatically, it takes more concentration and effort to complete our routines. Consequently, habits give us our bearings throughout daily life and allow us to do routine things with relative ease.
Habits also organize our underlying capacities. When we reach for the toothbrush or turn on the shower, we are using our vision, our cognition and our motor capacity. If we were to experience a loss of any of these capacities, our habits would disintegrate. For example, if the power is out and one has to feel one's way about the bathroom at night without the benefit of sight, habits go out of the window. If one has a broken arm and one's dominant hand is in a cast, simple things like turning on the shower, brushing one's teeth or putting on clothes take a lot more thinking and effort or may be impossible. When clients develop impairments, their habits become disrupted and their everyday routines take additional effort and thought or cannot be done without help. When one suddenly must use a wheelchair, the environment is changed and familiar habits no longer work. Getting into the shower and reaching to the medicine cabinet for the toothbrush are suddenly no longer habitual or possible. All the familiarity and ease of everyday life is disrupted. An important function of occupational therapy is to help clients develop new habits of everyday life in order to restore some of the ease and familiarity of daily life.
Roles
People see themselves as students, workers and parents, and recognize that they should behave in certain ways to enact these roles. Much of what we do is done as a spouse, parent, worker, student and so on (Mancuso & Sarbin 1983). The presence of these and other roles helps assure that what we do is regular (e.g. we go to school or work according to a schedule). Roles also give us a sense of identity and belatedly a sense of what we are obligated to do. When we tell someone we are a parent, a student, a worker or a member of some group, we are telling them who we are. Moreover, we know what is expected of us in those roles. Parents take care of children. Students attend lectures, study and take exams. Members of a bicycling club plan and go on bicycle trips together.
The roles that we have internalized serve as a kind of framework for looking out on the world and for engaging in occupation. When one is engaging in an occupation within a given role, it may be reflected in how one dresses, one's demeanour, the content of one's actions and so on. For instance, one would dress differently for work from when engaging in a leisure role. We do quite different things when we are in the role of student from when we are in the role of a friend.
Having an impairment can compromise one's ability to engage in meaningful life roles. If the impairment is severe, it can prevent or alter the way a person engages in all of their life roles. People with chronic disabilities often inhabit many fewer roles than those who do not have impairments. As a consequence, they have fewer opportunities to develop a sense of identity and to fill their lives with meaningful activities. In order to understand fully how a disability has influenced a client, the occupational therapist must understand its impact on their roles. Moreover, the aim of occupational therapy should be to support clients to enable them to engage in those roles that are most important or necessary for them.
Summary
Habituation regulates the patterned, familiar and routine features of what we do. Habits and roles give regularity, character and order to what we do and how we do it. They make our everyday lives familiar and they give us a sense of who we are. Disability can invalidate established habits and roles. Having a disability may require one to develop new habits for managing everyday routines and it may interfere with being able to engage in a role or alter how one can do that role. Understanding how a disability affects any person requires that the occupational therapist pays careful attention to the client's habituation.
Moreover, it is not sufficient that a client develops skills for doing everyday routines; it is also critical that the client develops the habits to integrate these skills into effective ways of doing everyday life tasks. Similarly, having abilities does little good, if clients are not able to access and identify with roles that call upon them to use those abilities. Therapy that focuses only on augmenting capacity without considering how the client will go about organizing everyday life is incomplete. Moreover, knowing what roles and habits are part of a client's life will also provide important information to enable us to prioritize the kinds of skill development on which to focus. Clients do not simply do things; they do them in order to enact daily routines and discharge their roles.
Performance capacity
The capacity for performance is affected by the status of one's musculoskeletal, neurological, cardiopulmonary and other bodily systems. A number of occupational therapy frameworks provide detailed concepts for understanding performance capacity. For example, the biomechanical framework seeks to explain human movement as the function of a complex organization of muscles, connective tissue and bones (Trombly 1989), while the sensory integration framework (Ayres, 1972, Ayres, 1979 and Ayres, 1986) explains how the brain organizes sensory information for executing skilled movement. Because these frameworks already address performance capacity, MOHO does not address this aspect of performance capacity. Consequently, occupational therapists using MOHO routinely use other frameworks for understanding and addressing performance capacity.
MOHO (Kielhofner et al 2008) concepts offer a different but complementary way of thinking about performance capacity. This view of performance capacity builds upon phenomenological concepts from philosophy (Husserl, 1962 and Merleau-Ponty, 1962) and focuses on the subjective experience of performing. It asks occupational therapists to pay more attention to how it feels to perform with a disability. By having a better understanding of a client's pain, fatigue, confusion or other subjective aspects of performance, therapists can be more client-centred and more helpful in assisting clients to learn or relearn skills.
Interweaving of volition, habituation and performance capacity
The things we do reflect a complex interplay of our motives, habits and roles, and performance capacity. Volition, habituation and the subjective experience of performance always operate in concert with each other. We cannot fully understand a client's occupation without considering all these contributing factors. For example, a person with low personal causation will tend to feel anxious when attempting to perform. This anxiety in turn can negatively affect performance. Another example is that if a person does not have interests and values that lead him to use his capacities, those capacities will diminish through disuse. For this reason, it is important that occupational therapists gather information about all the aspects of a client (performance capacity, values, interests, personal causation, roles and habits) in order truly to understand that client and provide the best services.
The environment
Just as volition, habituation and performance capacity are inter-related and interdependent, people and their environments are also inseparable (Kielhofner 2008). Our environments offer us opportunities, resources, demands and constraints. Whether and how these environmental potentials affect us depends on our values, interests, personal causation, roles, habits and performance capacities. Because each individual is unique, any environment will have somewhat different effects on each individual within it.
The physical environment consists of natural and human-made spaces and the objects within them. Spaces can be the result of nature (e.g. a forest or a lake) or the result of human fabrication (e.g. a house, classroom or theatre). Similarly, objects may be those that occur naturally (e.g. trees and rocks) or those that have been made (e.g. books, cars and computers). The social environment consists of groups of persons, and the occupational forms or tasks that persons belonging to those groups perform. Groups allow and prescribe the kinds of thing their members can do. Occupational forms or tasks refer to the things that are available to do in any social context (for example, in a classroom the kinds of thing that are typically done include writing notes, giving a lecture, answering questions, taking exams and so forth). Every context has certain occupational forms or tasks associated with it.
Any setting within which we perform is made up of spaces, objects, occupational forms/tasks and/or social groups. Typical settings in which we engage in occupational forms are the home, neighbourhood, school or workplace.
The environment can be both a barrier and an enabler for disabled persons. For example, snow dampens the sound used by blind persons to help navigate without sight and may make the pavement inaccessible to the wheelchair user. Much of the built environment limits opportunities and poses constraints on those with disabilities because it often has been designed for persons without impairments. On the other hand, careful design of spaces can facilitate daily functioning of disabled persons. Similarly, while most fabricated objects in the environment are created for use by able-bodied, sighted, hearing and cognitively intact individuals, there are also a large number of objects designed to compensate for impairments. Occupational therapists are experts in providing and training clients in the use of these specialized objects.
People with a physical and mental impairment often contradict cultural values, making others uncomfortable and evoking a range of reactions. These attitudes can limit the person with disability. Moreover, disability may remove people from or alter the positions they can assume in social groups. The occupational forms available to the person with a disability may be limited or altered. Performance limitations can make doing some occupational forms impossible. Persons with disabilities often must give up or relinquish to others occupational forms that have become impossible to do.
In short, the physical and social environment can have a multitude of positive or negative impacts on the disabled person, which can make all the difference in that person's life. The environment is not only a pervasive factor influencing disability. It is a critical tool for supporting positive change in the disabled person's life. A therapist may purposefully alter the physical setting to remove constraints or to facilitate function. An example of this is a ramp that replaces inaccessible steps. Therapists can remove objects that are barriers or provide objects such as assistive technology that facilitate functioning. The therapist may provide, monitor or seek to change social groups such as families or work colleagues. Finally, the therapist may provide or help a client select occupational forms to undertake, or to modify how an occupational form is done.
Understanding occupational performance
Personal causation, values and interests motivate what we choose to do. Habits and roles shape our routine patterns of doing. Performance capacities and subjective experience provide the capacity for what we do. The environment provides opportunities, resources, demands and constraints for our doing. We can also examine the doing itself and what consequence it has over time. Doing can be examined at different levels:
• skills
• occupational performance
• occupational participation
• occupational identity/occupational competence
• occupational adaptation.
Skills
Within occupational performance we carry out discrete purposeful actions called skills. For example, making a cup of tea has a culturally recognizable occupational form in the UK. To do so, one engages in such purposeful actions as gathering together tea, kettle and a cup, handling these materials and objects, and sequencing the steps necessary to brew and pour the tea. These actions that make up occupational performance are referred to as skills (Fisher and Kielhofner, 1995, Fisher, 1999a and Forsyth et al., 1998). In contrast to performance capacity (which refers to underlying ability, e.g. range of motion, strength, cognition), skill refers to the discrete actions seen within an occupation performance. There are three types of skill: motor skills, process skills, and communication and interaction skills.
If a person has difficulty ‘reaching’, an occupational therapist may conclude that the client has a limited range of motion in the shoulder joint. However, using Figure 6.2 to support theoretical clinical reasoning, we could hypothesize other reasons for the client not ‘reaching’. For example, the client may not think he has the capacity to reach (personal causation); he may not see the activity as important and therefore fail to reach (values); he may not find the activity satisfying or enjoyable and therefore fail to reach (interest); it may not be part of his role responsibilities and therefore he fails to reach as he knows someone else will do this for him (roles); the environment may not be supporting the reach; the occupational form may not be within the person's culture and so they do not know they need an object to complete the occupational form and so fail to reach; and so on. Skills can therefore be influenced by a range of personal and environmental factors. Having a theoretical framework supports clinical reasoning to understand why a client is having difficulty exhibiting skill to complete the occupational form.
Occupational performance
When we complete an occupational form or task, we perform. Occupational forms for a lecturer may include lecturing, writing, administering and marking exams, creating courses and counselling students. Taking care of ourselves may involve performing the occupational forms of showering, dressing and grooming. Other examples of occupational performance are when persons do such tasks as walking the dog, baking a chicken, vacuuming a rug or mowing the lawn. These people are performing those occupational forms.
Occupational participation
Participation refers to engagement in work, play, or activities of daily living that are part of one's sociocultural context and are desired and/or necessary to one's well-being. Examples of occupational participation include working in a full- or part-time job, engaging routinely in a hobby, maintaining one's home, attending school and participating in a club or other organization. This definition is consistent with the World Health Organization's view that participation is ‘taking part in society along with their experiences within their life context’ (World Health Organization 1999, p.19). Each area of occupational participation involves a cluster of related things that one does. For example, maintaining one's living space may include paying the rent, doing repairs, and cleaning.
Occupational identity and occupational competence
Our participation helps to create our identities. Occupational identity is defined as a composite sense of who one is and who one wishes to become as an occupational being, generated from one's history of occupational participation. Occupational identity includes one's sense of capacity and effectiveness for doing; what things one finds interesting and satisfying to do; who one is, as defined by one's roles and relationships; what one feels obligated to do and holds as important; a sense of the familiar routines of life; perceptions of one's environment and what it supports and expects. These are garnered over time and become part of one's identity. Occupational identity reflects accumulative life experiences that are organized into an understanding of who one has been and a sense of desired and possible directions for one's future.
Occupational competence is the degree to which one sustains a pattern of occupational participation that reflects identity. Competence has to do with putting your identity into action. It includes fulfilling the expectations of one's roles and one's own values and standards of performance; maintaining a routine that allows one to discharge responsibilities; participating in a range of occupations that provide a sense of ability, control, satisfaction and fulfilment; and pursuing one's values and taking action to achieve desired life outcomes.
Occupational adaptation
Occupational adaptation is the construction of a positive occupational identity and achieving occupational competence over time in the context of the environment.
Resources for practice
MOHO was initiated with the specific goal of developing resources to guide and enhance occupation-focused practice. Practitioners have collaborated in the development of a wide range of tools for partnerships. Academic/practice partnerships were built around how the tools developed. This ensured that the tools were theoretically driven and had robust research to support them while simultaneously being flexible and useful within busy clinical workplaces.
MOHO tools are specifically built to support occupation-focused practice. Examples are:
Box 6.1
MOHO assessment tools
Overview assessments
Occupational Performance History Interview (OPHI-II)
As a historical semi-structured interview, the OPHI-II seeks to gather information about a patient or client's past and present occupational performance. The OPHI-II is a three-part assessment, which includes:
• a semi-structured interview that explores a client's occupational life history
• rating scales that provide a measure of the client's occupational identity, occupational competence and the impact of the client's occupational behaviour settings
• a life history narrative designed to capture salient qualitative features of the occupational life history.
Occupational Circumstances Interview and Rating Scale (OCAIRS)
The OCAIRS is a semi-structured interview focused on the present and seeks to understand clients' occupational abilities on the full range of MOHO issues. It is an outcome measure. It is appropriate for clients who are conversational and is used when time is limited, as it is shorter than the OPHI-II interview.
Assessment of Occupational Functioning (AOF)
The AOF is a semi-structured interview, designed to identify strengths and limitations in areas of occupational functioning derived from MOHO (personal causation, values, roles, habits and skills). The AOF includes two parts:
• an interview schedule
• a rating scale.
Occupational Self-Assessment (OSA) and the Child Occupational Self-Assessment (COSA)
The OSA is an update of the Self-Assessment of Occupational Functioning (SAOF) and is designed to capture clients' perceptions of their own occupational competence and of the impact of their environment on their occupational adaptation. As such, the OSA is designed to be a client-centred assessment, which gives voice to the client's view. Once clients have had an opportunity to assess their occupational behaviour and their environments, they review the items in order to establish priorities for change, which can be translated into therapy goals.
Model of Human Occupational Screening Tool (MOHOST) and Short Child Occupational Profile (SCOPE)
These are relatively new assessments based on MOHO. Similar in format and administration, they were developed with clinicians in response to their request for a comprehensive assessment that is quick and simple to complete. MOHOST and SCOPE may be scored by the therapist using any combination of observation, interview, information from others who know the client, and chart audit. Because of their flexibility, the two tools can be used in a wide range of settings and with a wide range of clients. Moreover, the tools can be administered in a way that is client-centred.
Observational assessments
Assessment of Communication and Interaction Skills (ACIS)
The ACIS is a formal observational tool designed to measure an individual's performance in an occupational form and/or within a social group of which the person is a part. The instrument aims to assist occupational therapists in determining a client's ability in discourse and social exchange in the course of daily occupations.
Assessment of Motor and Process Skills (AMPS)
The AMPS (Fisher 1999b) represents a fundamental and substantive reconceptualization in the development of occupational therapy functional assessments. The AMPS is a structured, observational evaluation. It is used to evaluate the quality or effectiveness of the actions of performance (motor and process skills) as they unfold over time when a person performs daily life tasks.
Volitional Questionnaire (VQ) and the Paediatric Volitional Questionnaire (PVQ)
Traditionally, it has been difficult to assess volition in clients who have communication and cognitive limitations, due to the complex language requirements of most assessments of volition. The Volitional Questionnaire is an attempt to recognize that, while such clients have difficulty formulating goals or expressing their interests and values verbally, they are often able to communicate them through actions. The client is observed in a number of occupational behaviour settings so that a picture of the person's volition and the environmental supports required to support the expression can be identified.
Self-reports
Interest Checklist and the Paediatric Interests Profiles (PIP)
Although a number of versions of the Interest Checklist exist, the revised version appears to be the one most commonly used by occupational therapists utilizing the Model of Human Occupation and will be the one referred to in this discussion. This version consists of 68 activities or areas of interest. A revision within the UK is currently under way. There is a paediatric version available.
National Institutes of Health Activity Record (ACTRE)
The NIH ACTRE was developed as an outcome measure for a study of patients with rheumatoid arthritis. This instrument provides a 24-hour log of a patient's activities and is an adaptation of the Occupational Questionnaire (described below). The ACTRE aims to provide details of the impact of symptoms on task performance, individual perceptions of interest, significance of daily activities, and daily habit patterns.
Occupational Questionnaire (OQ)
The OQ is a pen-and-paper, self-report instrument that asks the individual to provide a description of typical use of time and utilizes Likert-type ratings of competence, importance, and enjoyment during activities. The client completes a list of the activities they perform each half-hour on a typical weekday. After listing the activities, the client is asked to answer four questions for each activity.
Role Checklist
The Role Checklist is a self-report checklist that can be used to obtain information about the types of role people engage in and which organize their daily lives. This checklist provides data on an individual's perception of their roles over the course of their life and also the degree of value, i.e. the significance and importance that they place on those roles. The Role Checklist can be used with adolescents, adults or geriatric populations.
Vocational assessments
Worker Role Interview (WRI)
The WRI is a semi-structured interview designed to be used as the psychosocial/environmental component of the initial rehabilitation assessment process for the injured worker. The interview is designed to have the client discuss various aspects of their life and job setting that have been associated with past work experiences. The WRI combines information from an interview with observations made during the physical and behavioural assessment procedure of a physical and/or work capacity assessment. The intent is to identify the psychosocial and environmental variables that may influence the ability of the injured worker to return to work.
Work Environment Impact Scale (WEIS)
The WEIS is a semi-structured interview designed to gather information about how individuals with disabilities experience and perceive their work settings. The focus of the interview is the impact of the work setting on a person's performance, satisfaction and well-being. An important concept underlying this scale is that workers are most productive and satisfied when there is a ‘fit’ or ‘match’ between the worker's environment and their needs and skills. Hence, the same work environment may have a different impact on different workers. It is important to remember that the WEIS does not assess the environment. Rather, it assesses how the work environment affects a given worker.
School assessments
Occupational Therapy Psychosocial Assessment of Learning (OT PAL)
The OT PAL is an observational and descriptive assessment tool. It assesses a student's volition (ability to make choices), habituation (roles and routines), and environmental fit within the classroom setting. The observational portion consists of 21 items that address the major areas of making choices, habits/routines and roles. In addition to the observation portion, there is a pre-observation form and interview guidelines. The pre-observation form is designed to gather environmental information, as well as assist in determining an appropriate time to complete the observation. The semi-structured interviews of the teacher, the student and the parent(s) are designed to have the teacher, student and parent describe various psychosocial aspects of learning related to school.
The School Setting Interview (SSI)
The SSI is a semi-structured interview designed to assess student–environment fit and identify the need for accommodations for students with disabilities in the school setting. The SSI is a client-centred interview intended to assist the occupational therapist in the planning of intervention by examining the student's interaction with the physical and social environments at school. The SSI provides the occupational therapist with a picture of the child's functioning in 14 content areas. This assessment is designed to be used collaboratively with the student and is therefore intended for students who are able to communicate adequately enough to discuss their feelings.
 |
| Fig 6.3 • Choosing a MOHO assessment. (NIH = National Institutes of Health). Reproduced from Kielhofner, G., 2008, A Model of Human Occupation: Theory and Application, 4th edn, published by Lippincott Williams & Wilkins, Baltimore |
• published case examples, as well as videotapes, illustrating application of the model in assessment, treatment planning and intervention (Box 6.2)
Box 6.2
Published articles and videotapes
There are a large number of published case examples, as well as videotapes, illustrating application of the model in assessment, treatment planning and intervention. A selection are referenced below:
Case illustrations through articles
Affleck A, Bianchi E, Cleckley M et al 1984 Stress management as a component of occupational therapy in acute care settings. Occupational Therapy in Health Care 1(3):17–41
Baron KB, Littleton MJ 1999 The model of human occupation: a return to work case study. Work: A Journal of Prevention, Assessment & Rehabilitation 12(1):37–46
Barrett L, Beer D, Kielhofner G 1999 The importance of volitional narrative in treatment: an ethnographic case study in a work program. Work: A Journal of Prevention, Assessment & Rehabilitation 12(1):79–92
Curtin C 1991 Psychosocial intervention with an adolescent with diabetes using the model of human occupation. Occupational Therapy in Mental Health 11(2/3):23–36
DePoy E, Burke JP 1992 Viewing cognition through the lens of the model of human occupation. In Katz N (ed.), Cognitive Rehabilitation: Models for Intervention in Occupational Therapy. Butterworth-Heinemann, Stoneham, MA, pp.240–257
Froehlich J 1992 Occupational therapy interventions with survivors of sexual abuse. Occupational Therapy in Health Care 8(2/3):1–25
Gusich R 1984 Occupational therapy for chronic pain: a clinical application of the model of human occupation. Occupational Therapy in Mental Health 4(3):59–73
Helfrich C, Kielhofner G 1994 Volitional narratives and the meaning of occupational therapy. American Journal of Occupational Therapy 48:319–326
Helfrich C, Kielhofner G, Mattingly C 1994 Volition as narrative: an understanding of motivation in chronic illness. American Journal of Occupational Therapy 42:311–317
Kavanaugh J, Fares J 1995 Using the model of human occupation with homeless mentally ill patients. British Journal of Occupational Therapy 58(10):419–422
Mentrup C, Niehaus A, Kielhofner G 1999 Applying the model of human occupation in work-focused rehabilitation: a case illustration. Work: A Journal of Prevention, Assessment & Rehabilitation 12(1):61–70
Neville A 1985 The model of human occupation and depression. Mental Health Special Interest Section Newsletter 8:1–4
Oakley F 1987 Clinical application of the model of human occupation in dementia of the Alzheimer's type. Occupational Therapy in Mental Health 7(4):37–50
Pizzi MA 1990 The model of human occupation and adults with HIV infection and AIDS. American Journal of Occupational Therapy 44:257–264
Pizzi MA 1990 Occupational therapy: creating possibilities for adults with human immunodeficiency virus infection, AIDS related complex, and acquired immunodeficiency syndrome. Occupational Therapy in Health Care 7(2/3/4):125–137
Series C 1992 The long-term needs of people with head injury: a role for the community occupational therapist? British Journal of Occupational Therapy 55(3):94–98
Woodrum SC 1993 A treatment approach for attention deficit hyperactivity disorder using the model of human occupation. Developmental Disabilities Special Interest Section Newsletter 16(1):1–2
Case illustrations through videotapes
Facilitating Empowerment and Promoting Self-Advocacy: ADA
Population: Disabled workers
Author: Renee Moore-Corner
OPHI-II
Population: Adults who can reflect upon and talk about their life history
Authors: Gary Kielhofner, Trudy Mallinson, Carrie Crawford, Meika Nowak, Matt Rigby, Alexis Henry, Deborah Walens
Understanding the Work-hardening Client
Population: Injured workers
Authors: Clare Curtin, Trudy Mallinson
Work Environment Impact Scales
Population: Adult workers with recent/current work experience
Authors: Renee Moore-Corner, Linda Olson, Gary Kielhofner
Worker Role Interview
Population: Injured workers
Authors: Craig Velozo, Gary Kielhofner, Gail Fisher
• published papers and manuals describing the implementation of programmes based on the model (Box 6.3). There is an evidence-based search engine and downloadable evidence briefs on the MOHO website to make it easier for practitioners to focus on the evidence for their areas of practice.
Box 6.3
Example manuals for MOHO-based programmes
The Banfield Assessment
Population: Disabled long-term residential clients
Authors: Hazel Broadley, Guylaine Desharnais
Remotivation Manual
Population: People with poor volitional status
Author: Carmen Gloria de la Heras
Wellness and Lifestyle Renewal: A Manual for Personal Change
Population: ‘Worried well’ adults
Author: Mark S. Rosenfeld
Work Readiness: Day Treatment for Persons with Chronic Disabilities
Population: Unemployed adults with chronic disabilities
Author: Linda Olson
Work Rehabilitation in Mental Health Programs
Population: Adults with mental illness
Authors: Trudy Mallinson, Dorianne LaPlante, Jan Holmann-Smith
Questions and answers
Since its inception and over the past four decades, the development of this model has been accompanied by a history of questions and critiques. Central questions have been:
• Can MOHO be used with other models of practice?
• Is MOHO client-centred?
• Is MOHO flexible enough to embrace a range of social, geographic and cultural environments?
• Why is there specific language?
• Can MOHO embrace the complexity of human occupation?
• Is MOHO applicable to lower functioning clients?
• Is MOHO an evidence-based choice?
• Can MOHO be used when selecting adaptive equipment?
We will attempt to address these issues through a series of questions and answers.
Can MOHO be used with other models of practice?
Yes. A common question is, ‘Is it MOHO or nothing?’ This question involves the extent to which MOHO can be used in an integrative way with other models of practice. As mentioned above, MOHO does not provide theoretical arguments to understand the capacity for performance that is supported by one's musculoskeletal, neurological, cardiopulmonary, mental or cognitive abilities such as memory, and planning and other bodily systems. A number of occupational therapy conceptual models of practice seek to explain performance capacities that make possible occupational performance. These models provide detailed concepts for understanding some aspect of performance capacity. Consequently, occupational therapists using MOHO will also need to use other frameworks in order to understand and address performance capacity. A combination of frameworks can, therefore, be used to support a full understanding of the client's occupational engagement. Figure 6.4 identifies how this can be achieved. Overarching values and beliefs of occupation therapy (e.g. occupation is important for health, it is important to consider both the mind and the body, it is important to be client-centred, and so on) inform occupation-focused conceptual models of practice (e.g. MOHO). MOHO has very specific detail on how to carry out occupation-focused practice. Both the values and beliefs of occupational therapy and MOHO provide support for the concept of an ‘occupation filter’ (Mallinson & Forsyth 2000). The occupation filter is a way of viewing knowledge from outside occupational therapy and bringing it into our practice in an occupation-focused way (Fig. 6.5). This allows the integration of a range of theories, yet avoids the ‘cutting and pasting’ of bodies of knowledge from outside occupational therapy into our practice and calling it occupational therapy when it in fact closely resembles other professionals' practice. For example, ‘cutting and pasting’ cognitive behavioural therapy into occupational therapy without using an ‘occupation-focused filter’ will result in practice that looks like that of a psychologist and perpetuate role confusion within occupational therapy.
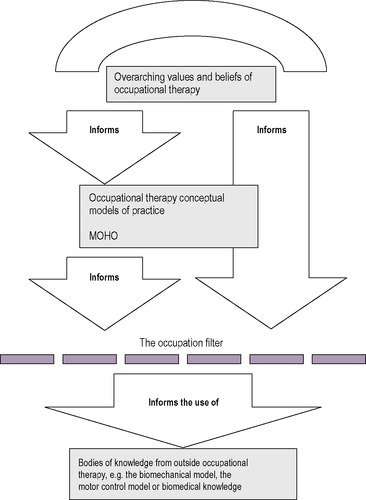 |
| Fig 6.4 • MOHO integration. Reproduced with permission from Forsyth & McMillan, personal communication, 2001. |
 |
| Fig 6.5 • Components of the occupational filter. Reproduced with the permission of T Mallinson & K Forsyth, personal communication, 2000 |
Is MOHO client-centred?
MOHO is recognized as a model consistent with client-centred practice (Law, 1998 and Sumsion, 1999). MOHO concepts require therapists to have knowledge of their client's values, sense of capacity and efficacy, value, roles, habits, performance experience and personal environment. MOHO-based assessments are designed to gather information on and provide clients with opportunities to provide their perspectives on these factors. The client's unique characteristics, in combination with the theory, guide the development of an understanding of the client's unique situation. The understanding of the client, in turn, provides the rationale for therapy. Moreover, since MOHO conceptualizes the client's own doing, thinking and feeling as the central dynamic in achieving change, therapy must support the client's choice, action and experience.
MOHO is, therefore, inherently a client-centred model in two important ways. Firstly, it views each client as a unique individual whose characteristics fundamentally influence the rationale for and nature of the therapy goals and strategies. MOHO theory both focuses the therapist on the unique characteristics of the client and provides concepts that allow the therapist to appreciate the client's perspective and situation more deeply. Secondly, MOHO views what the client does, thinks and feels as the central mechanism of change (Kielhofner 2002). MOHO concepts also propose that the client's occupational engagement (i.e. what the client does, thinks and feels) is the central dynamic of therapy (Kielhofner 2002). MOHO-based intervention supports the client's doing, thinking and feeling in order to achieve change. MOHO-based practice, therefore, requires a client–therapist relationship in which the therapist must understand, respect and support their client's values, sense of capacity and efficacy, value, roles, habits, performance experience and personal environment.
Is MOHO flexible enough to embrace a range of social, geographic and cultural environments?
Some have questioned whether MOHO is flexible and pragmatic enough to be used in a wide range of social, geographic and cultural environments.
With respect to the social environment, the third edition of MOHO has been influenced by the disabilities studies literature (Miller and Oertel, 1983, Hull, 1990 and Gill, 1997). This literature argues that many of the problems faced by persons with disabilities can more properly be located in the environment — in everything from physical barriers to stigmatizing attitudes and outright discrimination. A growing theme is that disability occurs because of a lack of fit between person and environment. This implies, of course, that change must include altering the environment. Accordingly, MOHO calls attention to the environment as both an enabler of and a barrier to occupation (Kielhofner 2002). Throughout, an effort has been made to call attention to circumstances both within the person and within the environment that contribute to a person's motivation, patterns of behaviour and occupational performance. The assessment tools that have been developed routinely contain an environmental component and examine the fit between the person and their environment. A MOHO-based assessment that is entirely focused on the environment has been developed (Moore-Corner et al 1998), and others incorporate the environment as an aspect of the assessment.
There have been questions raised about the portability of MOHO to different geographic and cultural environments. The scholarship of practice approach to MOHO development has encouraged an international community of occupational therapists to use and contribute to the development of MOHO. MOHO has, therefore, become an international conceptual practice model. MOHO has received significant attention, including criticism, elaboration, application and empirical testing by occupational therapists throughout the world in such diverse countries as Australia, New Zealand, the Netherlands, Sweden, Denmark, Japan, Korea, Spain, Italy, Portugal, Chile and Colombia.
The theory itself incorporates a respect for each client's individuality and cultural narrative into its concepts, and many of the assessments are specifically designed to capture a client's unique cultural perspective. For example, the OPHI-II (Kielhofner et al 1997) elicits and considers culturally influenced values, interests and roles through the use of narrative ethnography as a predominant interviewing method. For this reason, the OPHI-II and similar assessments are particularly useful when therapists desire to gather information about the client's culturally influenced thoughts, feelings and actions. Concepts of occupational form can also be helpful in identifying how different cultures define how everyday occupations are completed. Each culture includes a wide range of occupational forms that constitute the opportunities and demands that culture will put on its members for doing everyday things. Knowing how occupational forms are culturally defined for each client (for example, the occupational form of dressing has different social expectations based on cultural norms from culture to culture) helps occupational therapists to be sensitive to cultural differences in the ways of doing everyday activity.
Assuring that assessments are relevant and valid with persons from diverse cultural backgrounds requires ongoing development and research. Such work is being undertaken across the MOHO-based assessments. Assessments have been developed in collaboration with therapists and clients representing multiple cultures and languages. Many of the MOHO standardized assessments are now translated into different language versions. Research indicates that many of the MOHO-based assessments do not reflect cultural biases. For example, studies of the WRI (Haglund et al 1997), the WEI (Kielhofner et al 1999), the OPHI-II (Kielhofner et al 2001), the ACIS (Forsyth, Salamy, Simon et al 1997 and the OS (Kielhofner & Forsyth 2001) indicate that these assessments are valid cross-culturally. The UK is very influential in the development of MOHO theory and application. An active group of both researchers and practitioners are working together to contribute to the development of MOHO.
Why is there specific language?
The words that are selected to describe therapy are very important. Complex conditions or procedures can be conveyed and immediately understood when such professional terminology is used. Occupational therapists acquire the professional languages of several disciplines. In college we learn medical language to support our communication with medical colleagues. For example, we can say ‘Alzheimer's disease’ and immediately the multidisciplinary team have a sense of the issues faced by the person under discussion and then can enter into specifics of how the condition has affected this particular person. The medical definition of Alzheimer's disease is very long and having language to name and frame the issue supports effective communication with others who are familiar with the terms. Therefore, one strength of having a unique language is that MOHO terminology can be used in consultation with others who are familiar with the model to convey complex concepts accurately and succinctly. For example, the term ‘volition’ conveys a complex set of ideas about how people are motivated toward their occupations. When someone refers to a client having a volitional challenge, those who know the terminology can anticipate that the challenge involves the client's values, personal causation and interests, and how this manifests in the way clients anticipate, choose, experience and interpret what they do every day. In this way, MOHO terminology can succinctly convey information.
Deciding whether and how to use MOHO terminology in communication and documentation requires consideration of several factors. MOHO terms, like those of any other professional language, offer benefits and pose challenges. The major disadvantage of all professional language is that everyone needs to have a common understanding of the terms. It is, therefore, ineffective to use MOHO terms (or, indeed, medical terms) with colleagues, clients and others who will not understand what the words mean. Therefore, therapists should carefully decide when and how they use MOHO terms in communicating to clients, lay persons and other professionals. Because practitioners, clients and settings differ greatly in terms of their knowledge and understanding of languages associated with particular theoretical models, it is ultimately the clinicians' responsibility and judgement that count in terms of translating the MOHO terms into verbal and written language that accurately conveys the intended knowledge. There follow two examples where MOHO was used to understand the client's situation. Example 1 involves a situation where the occupational therapist decided not to use MOHO terminology and example 2 describes a situation where the occupational therapist found it helpful to use the terminology.
The following is an example of an entry into a multidisciplinary record. It frames Sophie's occupational life using MOHO; however, specific MOHO terminology was not used because the multidisciplinary team was not familiar with MOHO language. MOHO constructs have been placed in brackets for illustration only.
‘Sophie states she was previously a very active person (occupational identity). She worked behind the bar of a local pub (role) for 20 years before her retirement (role change) 5 years ago. She was very social and felt that a lot of the “regulars” at the pub were like friends (social environment). She enjoyed (interests) the social aspect of her job. Since retirement (role change) she has felt isolated (social environment). She is extremely house-proud (values), always had high standards (values) of cleaning and ran the household very efficiently (homemaker role). It was important (values) for Sophie always to present herself well. She took great care of her appearance (self-care role), liked to be “well turned out” (values) and had her hair set once a week (habit). She enjoyed spending time with her daughter and family (interest/social environment). She was particularly close to her granddaughter (role) and they had previously spent time together every Saturday out in the community (habit). She also enjoyed board games and knitting (interest). She previously volunteered at a local sheltered housing complex (role), where she made soup and meals. She was involved in church events (role) and ran charity events for the women's guild (role).’
The following is an example of using MOHO language to help understand a client called Jane. An occupational therapist may routinely document in their notes the following statement:
Statement A
‘Jane lacks confidence and is overly dependent.’
Using MOHO framework and language makes the definition of the challenge Jane faces more specific:
Statement B
‘Jane's personal causation is characterized by lacking a clear sense of her own capacity. As a result, she anticipates performance situations with anxiety and frequently chooses to avoid doing things for which she has adequate skills. She also habitually seeks advice and help from others, which leads to her being unnecessarily dependent on others.’
In this situation the therapist decided to use statement B because using the terminology of MOHO resulted in documentation that was more precise and detailed. Moreover, while statement A describes Jane's behaviour, it does not explain it. The MOHO framework and language in statement B offered an explanation that also provides a rationale for the following interventions:
• Advise Jane on a course of occupational therapy that will support a graded engagement in occupations to challenge her sense of capacity increasingly.
• Provide Jane with feedback around her occupational performance to enable a more accurate sense of her own capacities to engage in occupations.
• Encourage Jane to sustain occupational performance in the face of anxiety.
• Structure the environment to provide the opportunity for Jane to practise engaging in occupations with more autonomy.
Precision in language, including the use of theoretical terms, can clarify what we understand clients’ occupational challenges to be and how we plan to address them.
Can MOHO embrace the complexity of human occupation?
Human occupation is complex (Creek 2003). Most people come into occupational therapy with significant impairments and major disruptions to their lives. Others struggle with declining function or recurring exacerbations of their diseases. A large proportion of clients face the task of rebuilding all or part of their lives. In short, their occupational problems tend to be complex and challenging. The strength and application of MOHO is neither simple nor formulaic. Instead, it aims to understand important multiple dimensions of each client's unique experience and bring a sophisticated understanding to bear on the life issues facing each client in practice.
In occupational therapy, a number of frameworks address aspects of occupational performance and the capacities that underlie it, but these theories tend to exist in isolation from one another. For example, occupational therapy theories that concentrate on physical performance have generally attended to the bodily components (brain and musculoskeletal system) involved in physical doing, while motives have been seen as part of a separate domain. By contrast, MOHO offers an approach to thinking about the capacity for occupational performance that complements existing theory. There is growing recognition of the importance of considering body and mind together in explaining phenomena (Kielhofner, 1995 and Trombly, 1995). After all, motivation for a task can influence the extent of physical effort directed to that task (Yoder et al, 1989 and Riccio et al., 1990), while physical impairments can weigh down the desire to do things (Murphy,, 1987 and Toombs, 1992). Conceptually, MOHO seeks to avoid dividing humans into separate physical and mental components, and instead embraces the complexity of human occupation. MOHO seeks to explain how occupation is motivated, patterned and performed, and implicates both body and mind in each of these major concepts. By offering explanations of such diverse phenomena, MOHO offers a broad and integrative view of human occupation. Consequently, it can be used to explain and guide practice involving a wide range of phenomena and corresponding concepts. Moreover, as stated above, therapists often use MOHO in combination with other conceptual models of practice or with theories borrowed from other disciplines or professions.
Is MOHO applicable to lower-functioning clients?
Some have questioned the relevance of MOHO in addressing issues of motivation in children and in lower-functioning clients. This perception is perplexing, since those clients who are least able to self-describe and self-advocate most deserve careful assessment of their volition. This can be achieved through careful observation of the client's volitionally relevant actions. The VQ (de las Heras et al 2001), the PVQ (Geist et al 2001) and the MOHOST (Parkinson et al 2001) work well with such clients. A therapist can, therefore, readily gain insight into the volition of children or lower-functioning clients. Additionally, therapists can make good use of unstructured means of assessment for such clients (Kielhofner 2002) that allow for complete flexibility within the assessment process.
Is MOHO an evidence-based choice?
Yes. Since MOHO was first published in the early 1980s it has built up an evidence base (see http://www.moho.uic.edu/). The majority of these studies were completed in the last decade, indicating an accelerating growth in research on MOHO, and it is now the most internationally researched, occupation-focused, conceptual model of practice. MOHO provides theoretical evidence for its practice theory and it provides research evidence for its tools for practice.
Theoretical evidence for practice
Such research examines whether the concepts of MOHO theory are supported by evidence. It also involves asking whether the theory can account for and predict the kinds of client change it seeks to explain. Therefore, theoretical evidence on MOHO has included the following kinds of study:
• construct validity studies that seek to verify MOHO concepts
• correlative studies that examine the accuracy of relationships between constructs proposed in MOHO theory
• studies comparing groups on concepts from MOHO theory to test whether they explain group differences
• prospective studies that examine the potential of MOHO concepts and propositions to predict future behaviour or states
• qualitative studies that explore MOHO concepts and propositions in depth.
This kind of theoretical evidence for practice yields findings that may lead one to have confidence in the theory and/or to eliminate, change or expand a concept and/or proposition.
Evidence for technology for practice application
In addition to offering a practice-based theory to embrace the complexity of therapy, conceptual models of practice like MOHO additionally generated a technology for application (e.g. assessments and intervention strategies) for use in practice. Examples of this kind of research are:
• psychometric studies leading to the development of outcome measures
• studies of how MOHO concepts influence therapeutic reasoning and practice
• studies that examine what happens in therapy
• outcomes studies that identify the effectiveness of occupational therapy services
• predictive studies that identify whether certain occupational outcomes can be predicted by the occupational therapist.
This kind of research provides practical tools for therapists to use within their practice and evidence to argue for additional occupational therapy resources.
While we can distinguish theoretical and application research within the MOHO research base, it is important to recognize that many MOHO-based studies incorporate both theoretical and application research aims to be addressed simultaneously. This is reflective of a ‘scholarship of practice’ approach to building evidence for the field, whereby research for theory and application are simultaneously achieved. For example, some studies that primarily sought to examine the dependability of an assessment tool have identified new concepts that were later incorporated into the theory (Mallinson et al 1998).
Can MOHO be used when selecting adaptive equipment?
Yes. Social service colleagues have asked the question, ‘How would I apply MOHO to a client who is having difficulty bathing?’ A biomechanical way of framing this challenge may be to state that the person is having difficulty ‘physically getting in and out of the bath’. A MOHO way of framing the challenge is to state that the person is having ‘difficulty engaging in the bathing activity’. MOHO, therefore, supports therapists in embracing the complexity of bathing rather than reducing it to only an issue of moving the client's body into/out of the bath. MOHO would support the therapist in asking the following questions:
• Does the person feel confident doing this activity?
• Have they had difficult past experiences doing this activity? (personal causation)
• Do they find this activity enjoyable/satisfying? (interest)
• How important is this activity for them?
• How important is it that they complete the activity alone?
• What meaning will adaptive equipment have for the person? (values)
• Can they physically do the activity? (motor skills)
• Do they have enough concentration — sequencing and so on — to complete the activity? (process skills)
• Do they have the full responsibility for doing the activity? (role)
• Does someone help them? (social environment)
• Where do they bathe?
• Where do they undress?
• Do they have any equipment to help them?
• Can they describe the environment when the bath is full — slippy, with lots of steam and on on? (physical environment)
• Do they have a routine when doing this activity?
• What time of day do they bathe? (habits)
• Are they satisfied with their morning/evening routine and when bathing happens?
• How does the time of day affect their abilities to bathe? (habits)
MOHO can, therefore, provide a framework for understanding the life within which occupational therapy is entering and whether adaptive equipment is appropriate. It also provides an understanding of the meaning attached to the equipment and how it might be adapted into the routine of the client. A lack of attention to these details may mean that the equipment is hidden away due to the client not wanting to be seen as ‘disabled’, or the equipment being removed because it was not adopted into the client's habitual routine.
Can you use MOHO as an activity analysis structure?
Yes. The analysis of occupations and their use within therapy are among the unique skills of the occupational therapist (Hagedorn 2000). There are many structures that provide a framework for analysing activity (Fidler and Fidler, 1963, Mosey, 1986, Lamport et al., 2001, Creek, 2002 and Foster and Pratt, 2002). Recently, however, there has been some discussion that advocates using theories as a framework for activity analysis (Crepeau, 2003 and Toglia, 2003).
Practitioners analyse activities from the perspective of practice theories to understand problems in performance and intervention strategies.
MOHO provides an evidence-based practice theory that supports a therapist in analysing a person's occupational life. Practice-based theories have the added advantage of providing an understanding of how different elements of analysis relate to each other and provide an insight into the change process (Creek 2009). MOHO has an established evidence base to support how different theoretical constructs relate to each other (e.g. Lederer et al., 1985, Barris et al., 1986, Ebb et al., 1989, Davies Hallet et al., 1994, Peterson et al., 1999 and American Occupational Therapy Association, 2002) and has a theory of how therapeutically supported change happens (Kielhofner 2002). It could, therefore, be argued that using evidence-based theory (e.g. MOHO) to analyse activities has several advantages over traditional activity analysis frameworks. MOHO-driven activity analysis simultaneously:
• provides an analysis of the person's occupational life
• examines how the different aspects of this analysis relate to each other
• looks at how this analysis relates to the changes that potentially can be made to support the client's re-engagement in everyday life.
This view has been supported by the inclusion of motor and process skills (Fisher and Kielhofner, 1995 and Kielhofner, 2002), along with communication and interactions skills (Forsyth et al 1998, Kielhofner 2000) in the occupational therapy practice framework (Butts, Nelson 2007). As described in a previous section, MOHO would need to be used with other frameworks (e.g. biomechanical, motor control, sensory integration and so on) to support a complete activity analysis that included analysing performance capacities.
The case below illustrates the use of the MOHO framework to understand the occupational participation of a client called Sophie Bronson. The occupational therapy report shown below was developed from observations of Sophie within her home environment, and from face-to-face discussion with Sophie and Sophie's husband, in addition to telephone contact with Sophie's daughter. The therapist decided not to use MOHO terminology in the report due to the multidisciplinary audience.
Sophie: occupational therapy report1
1The Model of Human Occupation Screening Tool (MOHOST) assessment was used to complete this assessment. Parkinson, S., Forsyth, K., Kielhofner, G., 2002. ‘A User's Manual for the Model of Human Occupation Screening Tool (MOHOST), Version 1.0, Research Version, MOHO Clearinghouse, University of Illinois at Chicago.
Name: Sophie Bronson
Address: 12 Church Street, Edinburgh
Date of Birth: 12.03.30
GP: Dr Watson
Consultant: Dr Wallace
Data sources:
14 March 2005 Home visit with Sophie and her husband present
15 March 2005 Telephone contact with Sophie's daughter
Date of report: 16 March 2008
Referral and reason for assessment
The referral was received from Sophie's GP, Dr Watson, on 24 February 2005. The referral stated that Sophie was now reporting ‘difficulties with coping and mobility’. It also stated that Sophie has been diagnosed as having early dementia and has a previous medical history of osteoarthritis and congestive heart failure. The reason for the assessment, therefore, was to look at Sophie's engagement with everyday activity and make recommendations to support Sophie in feeling as if she can ‘cope and manage her mobility’ issues and with other potential unidentified difficulties engaging in activity.
Sources of information for report
This report is a compilation of information gathered on a home visit (Sophie, her husband and her occupational therapist present) and a telephone contact with Sophie's daughter.
History of activity
Information from Sophie
She was previously a very active person. She worked behind the bar of a local pub for 20 years before her retirement. She was very social and felt that a lot of the ‘regulars’ at the pub were like friends. She enjoyed the social aspect of her job. Since retirement she has felt isolated. She is extremely house-proud, always had high standards of cleaning and ran the household very efficiently. It was important for Sophie always to present herself smartly. She took great care of her appearance, liked to be ‘well turned out’ and had her hair set once a week. She enjoyed spending time with her daughter and family. She was particularly close to her granddaughter and they had previously spent time together every Saturday out in the community. She also enjoyed board games and knitting. She previously volunteered at a local sheltered housing complex, where she made soup and meals. She was involved in church events and ran charity events for the women's guild.
Information from Sophie's husband and daughter
They both confirmed the above information from Sophie and so it could be concluded that Sophie is an accurate historian. They stated that Sophie's activity levels reduced when she retired 5 years ago. There has been a gradual deterioration in activity levels over a 12-month period. She has been sitting in her chair all day doing very little since her recent hospital admission 6 months ago.
Current mental/physical health
A. Current mental health
On the visit Sophie was observed to be responsive and cooperative; she reported that her mood has been low for 6 months and that she no longer took any interest in activities that were once meaningful. Sophie identified the source of her low mood as including
• her inability to mobilize out of doors
• her recent hospital admission (6 months ago)
• a flood incident in the flat above.
She states that she is not coping with any activities that were previously meaningful to her and she is frustrated by this.
Sophie's daughter feels that her mother's current low mood is due to social isolation since retiring and to having reduced mobility ascending/descending stairs because of her painful and swollen feet. Sophie's social isolation has worsened recently because she is not taking as much care of her physical appearance and now would not want anyone to see her in an unkempt state.
B. Current physical health
Sophie needs a Zimmer frame to mobilize around her environment. She was observed to mobilize in her flat independently and safely using this frame. She has not gone outside for the past 12 months due to her inability to ascend/descend stairs. She was observed to have swollen feet, with hyper-extended big toes. The podiatrist and physiotherapist are involved, which has improved the situation; however, Sophie still reports pain. She wears glasses, although states she is able to read without them. She reports deteriorated eyesight since a cataract operation. She states that she has hearing aids, which she was not wearing during the visit. She was observed to be answering questions appropriately and followed the conversations; therefore, she could hear people talking.
Current engagement in activity
A. Physical environment
Sophie was observed to live in a two-bedroom, first-floor flat. External access is by two steps (no rails) into the building, a 100-yard paved corridor, then 16 steps broken halfway with a landing (with rail right side ascending). The physical condition of the flat was well maintained; it is centrally heated and connected by a telephone.
B. Social environment
Sophie states that she has had a home carer for the last 3 months who attends three times per day, 7 days a week. Sophie says she has not been enjoying the company of her granddaughter recently and feels guilty about this.
Sophie lives with her husband and he states that he is in good health. He says he is frustrated by his wife's lack of engagement in activities and her perception that he is not completing tasks to her standards.
Sophie's daughter states that she and her husband live close by. They both work full-time but Sophie's daughter visits every evening to support her parents. She has two teenage children, a son and a daughter, who now only visit sporadically.
Sophie has asked friends not to visit any longer. She states that she does not want them to see her unkempt.
C. Daily routine
Sophie's husband states that she rises at 9am when the home care assistant attends. She goes through her morning routine then has breakfast at 9.30am. She sits in her lounge chair watching TV all day and evening. The homecare assistant attends at 1pm to carry out domestic tasks. She then attends at 10pm to support Sophie with her night routine. Sophie states that she is not happy with this routine but cannot ‘be bothered to do anything’.
D. Roles
i. Self-care:
Sophie's self-care routine takes place entirely within her bedroom. Sophie does not:
• strip-wash at the bathroom sink
• use the shower
• use the perch stool
due to lack of confidence in her balance. Sophie states that to wash herself she has an established routine and sits on the bedside commode. The care assistant arranges needed objects to support this lack of mobility and provides verbal encouragement (to support Sophie's lack of confidence). Sophie and her daughter both state that she then has the skills to dress herself independently on the commode. Grooming herself is very important to Sophie; she says that she is currently unable to set her hair and can no longer get out of her flat to access the hairdresser.
Sophie was observed on the visit to:
• independently transfer on/off a 40 cm high commode using a Zimmer frame with a safe technique
• independently transfer on/off a 40 cm high toilet, using a 5 cm raised toilet seat and right wall grab rail, with a safe technique.
Bed transfer was not observed. Sophie did not want to attempt shower transfer, as she is not currently using the shower and is comfortable with her current arrangement of strip-washing at the bedside.
ii. Productivity
• Cooking. The kitchen was observed to have a gas cooker with overhead grill, microwave, electric kettle, continuous surfaces, and a table and chairs. Although Sophie stated that she previously enjoyed cooking for the sheltered housing volunteer position, her husband now does all the cooking and hot drinks at home. She states that she has ‘no interest’ in cooking now, although does occasionally help prepare meals with her husband. She feels she cannot do the cooking now and feels she will not be able to do this independently. They have a diet of toast in the morning, banana and bread for lunch and a cooked meal in the evening. Sophie states that she does not eat the vegetables because her husband does not prepare them well enough. Sophie's husband feels that Sophie still has the skill, supportive environment and previous habits to cook but she is not motivated to do so. He is frustrated by his wife's lack of engagement with cooking.
• Task on visit: making a hot drink. Sophie stated that she would not be able to manage to complete the activity. She did, however, manage to make the hot drink independently with the following skill level:
○ Motor skills. She was unsteady at times and slow, but managed physically without intervention. She demonstrated some stiffness and reduction in strength. She appeared to lack energy and sat at regular intervals during the activity.
○ Process skills. Sophie managed to use knowledge, plan and organize the activity. She did, however, have challenges problem-solving.
• Sophie did not view this as an achievement because it was not completed to her standard.
• Laundry/cleaning and shopping. These activities are completed by the home carer and Sophie's husband. They are happy to continue to support; however, Sophie feels these activities are not completed to ‘her standards’.
• Volunteer job. Sophie has not been involved with her volunteer job for 3 years. She states she misses the social contact and the feeling of ‘being useful’.
iii. Leisure:
Sophie could identify interests that she engaged in the past. She specifically identified the social aspect of these interests as being enjoyable and satisfying.
Sophie now appears to have reduced leisure opportunities. She could identify specific TV programmes that she enjoys watching. She now receives a weekly visit at home from the church. She could not identify anything else that she does that brings her enjoyment.
Sophie's daughter is particularly concerned that Sophie is not engaging with previous leisure activities. Her daughter states she feels that this is the key for supporting her mother to ‘re-engage in life’.
E. Goals
Sophie was unable to identify any goals for the future. Sophie feels very pessimistic about her ability to return to a meaningful life. She states she feels ‘hopeless’ about the future.
F. Readiness for change
Sophie's current situation is not supportive of her mental or physical health. The combination of high performance standards and less skill means that Sophie lacks motivation to engage in doing activities that were meaningful to her in the past and she cannot identify any goals, develop plans and follow them through. Although socially isolated by not being able to ascend/descend external stairs, Sophie stated that she is not prepared to consider moving to alternative accommodation on the ground floor. The couple have been buying their council flat and moving would be ‘too large an upheaval’. Sophie now has carer support and has developed strong habits and dependence on this support. Although Sophie is unhappy with her circumstances, she is not ready to change independently and, therefore, requires further extended occupational therapy input.
Occupational therapy perspective (Fig. 6.6)
Sophie gives the impression of a person who has given up on life. She has previously been an active woman but has had a reduction in activity in the past 5 years since retiring; this has further reduced in the past 12 months and was accelerated within the last 6 months following a hospital admission. This situation was brought about primarily by a difficult transition from working to retirement, physical limitations and pain when mobilizing. This has been compounded by the identification of the start of a dementia process.
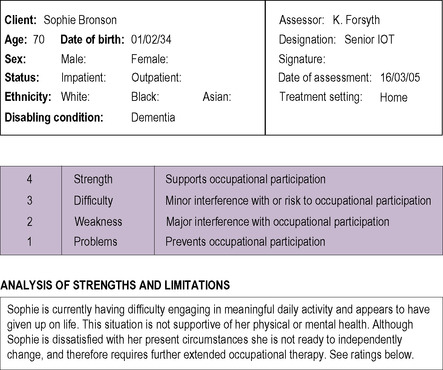 |
 |
 |
 |
 |
| Fig 6.6 • The Model of Human Occupation Screening Tool (MOHOST). Copyright © Patkinson, S., Forsyth, K., Kielhofner, G., 2005. The Model of Human Occupation Tool (MOHOST), version 2.0. Reproduced with the permission of Parkinson, Forsyth & Kielhofner. |
Motivation for activity:
Currently Sophie lacks motivation to engage in previously held meaningful activity. Specifically, she has difficulty appraising her own abilities, leading to her being dependent on others. She does not expect success in the future, which leads to fear of failing and not meeting her high standards. She cannot identify any activities that bring her enjoyment and is unable to set goals for the future. These characteristics create a situation where Sophie does not make choices to do activity, apart from basic self-care.
Pattern of activity:
Sophie has had substantial role loss over the last 5 years, which has led to an empty routine, a poor sense of belonging and avoidance of previously held responsibility. She demonstrates an unwillingness to agree to changes in her current routines and ways of doing activities, even though these habits do not support her preferred lifestyle.
Skill for activity:
Sophie has adequate communication and interaction skills but is now having challenges maintaining relationships. She has physical difficulties with balance, stiffness, strength and energy. She has adequate processing skills but has difficulty with problem-solving.
Environment:
Sophie's physical environment is problematic, as her flat is accessed by stairs and she cannot ascend/descend them. This will not be easily resolved. Her social environment is very supportive; however, carers are not supporting the development of Sophie's ability to engage in daily activities.
Overall recommendation
Sophie's current situation is not supportive of her mental or physical health. Although Sophie wants to change her circumstances, she is not ready to change independently and therefore requires further extended occupational therapy input.
NAME: Kirsty Forsyth
GRADE: Senior I
LOCATION: Edinburgh Community Rehabilitation Team
cc: GP, PT.
Summary
MOHO provides a way for occupational therapists to embrace the complexity of human occupation within their practice. It provides an understanding of the choice, order and performance of occupation within people's lives. It also provides assessment and intervention techniques to support the integration of MOHO theory into practice. MOHO is built for and with an international community of occupational therapists, with the ultimate goal of fully embracing the unique occupational characteristics of our clients and supporting them in their re-engagement with meaningful self-care, productivity and leisure.
Think of a recent OT client you have been involved with (either as a student on placement or as a qualified OT) and ask yourself the following questions:
• What is the person's occupational identity? (Prompt: what roles do they identify with? Father, brother, sibling, worker)
• What is the person's occupational competence? (Prompt: what skills does the person feel they have to meet role responsibilities? Is this accurate appraisal?)
• What are the positive occupational issues for the person? (Prompt: Think about engagement in self-care, work and/or leisure & personal causation, values, interests, habits, role, performance capacity, skills or environment? or a combination of these)
• Why is the person unable or having challenges engaging in occupations? (Prompt: Think about challenges engagement in self-care, work and/or leisure & personal causation, values, interests, habits, role, performance capacity, skills or environment? or a combination of these)
• Write a summary statement using the answers to the above questions in order to capture the main occupational issues for the client
References
American Occupational Therapy Association, Occupational therapy practice framework: Domain and process, American Journal of Occupational Therapy 56 (2002) 609–639.
Ayres, A.J., Sensory Integration and Learning Disorders. (1972) Western Psychological Services, Los Angeles.
Ayres, A.J., Sensory Integration and the Child. (1979) Western Psychological Services, Los Angeles.
Ayres, A.J., Developmental Dyspraxia and Adult Onset Apraxia. (1986) Sensory Integration International, Torrance, CA.
Butts, D.S.; Nelson, D.L., Agreement between Occupational Therapy Practice Framework classifications and occupational therapists' classifications, American Journal of Occupational Therapy. Sep-Oct; 61 (5) (2007) 603–604.
Barris, R.; Kielhofner, G.; Burch, R.M.; et al., Occupational function and dysfunction in three groups of adolescents, Occupational Therapy Journal of Research 6 (1986) 301–307.
Bruner, J., Acts of Meaning. (1990) Harvard University Press, Cambridge, MA.
Creek, J., The knowledge base of occupational therapy, In: (Editor: Creek, J.) Occupational Therapy and Mental Health (2002) Churchill Livingstone, Edinburgh.
Creek, J., Occupational Therapy Defined as a Complex Intervention. (2003) College of Occupational Therapists, London.
Creek, J., Occupational therapy defined as a complex intervention: a 5-year review, British Journal of Occupational Therapy 72 (3) (2009) 105–115; Retrieved from CINAHL with Full Text database.
Crepeau, E., Activity analysis: a way of thinking about occupational performance, In: (Editors: Crepeau, E.B.; Schell, B.; Cohn, E.) Willard and Spackman's Occupational Therapy (2003) Lippincott Williams & Wilkins, Philadelphia.
Csikszentmihalyi, M., Flow: The Psychology of Optimal Experience. (1990) Harper & Row, New York.
Davies Hallet, J.; Zasler, N.; Maurer, P.; et al., Role change after traumatic brain injury in adults, American Journal of Occupational Therapy 48 (1994) 241–246.
de las Heras, C.G.; Geist, R.; Kielhofner, G.; et al., The Volitional Questionnaire (VQ) (Version 4.1). (2001) Model of Human Occupation Clearinghouse. Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago, Chicago.
Dewey, J., Human Nature and Conduct. (1922) Henry Holt, New York.
Ebb, E.W.; Coster, W.; Duncombe, L., Comparison of normal and psychosocially dysfunctional male adolescents, Occupational Therapy in Mental Health 9 (1989) 53–74.
Fidler, G.; Fidler, J., Occupational Therapy: a Communication Process in Psychiatry. (1963) Macmillan, New York.
Fisher, A.; Kielhofner, G., Skill in occupational performance, In: (Editor: Kielhofner, G.) A Model of Human Occupation: Theory and Applicationsecond ed (1995) Williams & Wilkins, Baltimore.
Fisher, A.G., Uniting practice and theory in an occupational framework, American Journal of Occupational Therapy 532 (7) (1999) 509–520.
Fisher, A.G., Assessment of Motor and Process Skills. 3rd ed (1999) Three Star Press, Ft. Collins, CO.
Forsyth, K.; Salamy, M.; Simon, S.; et al., Assessment of Communication and Interaction Skills. (1997) University of Illinois, Model of Human Occupation Clearinghouse, Chicago.
Forsyth, K.; Salamy, M.; Simon, S.; et al., A user's guide to the Assessment of Communication and Interaction Skills (ACIS) Chicago: Model of Human Occupation Clearinghouse. (1998) Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago, Chicago.
Foster, M.; Pratt, J., Activity analysis, In: (Editors: Turner, A.; Foster, M.; Johnston, S.E.) Occupational Therapy and Physical Dysfunction: Principles, Skills and Practice (2002) Churchill Livingstone, Edinburgh.
Geist, R.; Kielhofner, G.; Basu, S.; et al., The Pediatric Volitional Questionnaire (PVQ) (Version 1.1). (2001) Model of Human Occupation Clearinghouse, Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago, Chicago.
Gill, C.J., Four types of integration in disability identity development, Journal of Vocational Rehabilitation 9 (1997) 39–46.
Hagedorn, R., Tools for Practice in Occupational Therapy. (2000) Churchill Livingstone, Edinburgh.
Haglund, L.; Karlsson, G.; Kielhofner, G.; et al., Validity of the Swedish version of the Worker Role Interview, Scandinavian Journal of Occupational Therapy 4 (1–4) (1997) 23–29.
Haglund, L.; Ekbladh, E.; Thorell, L.; et al., Practice models in Swedish psychiatric occupational therapy, Scandinavian Journal of Occupational Therapy 7 (3) (2000) 107–113.
Harter, S., The development of the self-system, In: (Editor: Hetherington, M.) Handbook of Child Psychology: Social and Personality Development, vol. 4 (1983) John Wiley, New York.
Harter, S.; Connel, J.P., A model of relationships among children's academic achievement and self perceptions of competence, control, and motivation, In: (Editor: Nicholls, J.) The Development of Achievement Motivation (1984) JAI, Greenwich, CT.
Hull, J.M., Touching the Rock: An Experience of Blindness. (1990) Vintage, New York.
Husserl, E., Ideas: General introduction to Pure Phenomenology. (1962) Collier, London; (W.R.B. Gibson, Trans.).
Kielhofner, G., A Model of Human Occupation, part three. Benign and vicious cycles, American Journal of Occupational Therapy 34 (1980) 731–737.
Kielhofner, G., A Model of Human Occupation, part two. Ontogenesis from the perspective of temporal adaptation, American Journal of Occupational Therapy 34 (1980) 657–663.
Kielhofner, G., A Model of Human Occupation: Theory and Application. (1985) Williams & Wilkins, Baltimore.
Kielhofner, G., A Model of Human Occupation: Theory and Application. second ed. (1995) Williams & Wilkins, Baltimore.
Kielhofner, G., Conceptual Foundations of Occupational Therapy. (1997) FA Davis, Philadelphia.
Kielhofner, G., A Model of Human Occupation: Theory and Application. third ed. (2002) Williams & Wilkins, Baltimore.
Kielhofner, G., A Model of Human Occupation: Theory and Application. fourth ed. (2008) Lippincott Williams & Wilkins, Baltimore.
Kielhofner, G.; Burke, J.P., Occupational therapy after 60 years: an account of changing identity and knowledge, American Journal of Occupational Therapy 31 (1977) 675–689.
Kielhofner, G.; Burke, J., A Model of Human Occupation, part one. Conceptual framework and content, American Journal of Occupational Therapy 34 (1980) 572–581.
Kielhofner, G.; Forsyth, K., Development of a client self-report for treatment planning and documenting therapy outcomes, Scandinavian Journal of Occupational Therapy 8 (3) (2001) 131–139.
Kielhofner, G.; Burke, J.; Heard, I.C., A Model of Human Occupation, part four. Assessment and intervention, American Journal of Occupational Therapy 34 (1980) 777–788.
Kielhofner, G.; Mallinson, T.; Crawford, C.; et al., A user's guide to the occupational performance history interview-II (OPHI-II) (version 2.0). (1997) Model of Human Occupation Clearinghouse, Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago, Chicago.
Kielhofner, G.; Lai, J.S.; Olson, L.; et al., Psychometric properties of the work environment impact scale: a cross-cultural study. Work: a Journal of Prevention, Assessment & Rehabilitation 12 (1) (1999) 71–77.
Kielhofner, G.; Mallinson, T.; Forsyth, K.; et al., Psychometric properties of the second version of the Occupational Performance History Interview (OPHI-II), American Journal of Occupational Therapy 55 (2001) 260–267.
Lamport, N.; Coffey, M.; Hersch, G., Activity Analysis and Application Building Blocks of Treatment. (2001) Slack, Thorofare, NJ.
Law, M., Client-centred Occupational Therapy. (1998) Slack, Thorofare, NJ.
Law, M.; McColl, M.A., Knowledge and use of theory among occupational therapists: a Canadian survey, Canadian Journal of Occupational Therapy 56 (4) (1989) 198–204.
Lederer, J.; Kielhofner, G.; Watts, J., Values, personal causation and skills of delinquents and non delinquents, Occupational Therapy in Mental Health 5 (1985) 59–77.
Lee, D., Culture and the experience of value, In: (Editor: Maslow, A.H.) Neural Knowledge in Human Values (1971) Henry Regnery, Chicago.
Lee, S.; Kielhofner, G.; Taylor, R., Choice, knowledge, and utilization of a practice theory: a national study of occupational therapists who use the Model of Human Occupation, Occupational Therapy in Health Care 23 (1) (2009) 60–71.
Lefcourt, H.M., Research with the Locus of Control Construct, vol. 1: Assessment and Methods. (1981) Academic Press, New York.
Mallinson, T.; Mahaffey, L.; Kielhofner, G., The Occupational Performance History Interview: evidence for three underlying constructs of occupational adaptation, Canadian Journal of Occupational Therapy 65 (4) (1998) 219–228.
Mancuso, J.; Sarbin, T., The self-narrative in the enactment of roles, In: (Editors: Sarbin, T.R.; Scheibe, K.E.) Studies in Social Identity (1983) Praeger, New York.
Merleau-Ponty, M., Phenomenology of perception. (1962) Routledge & Kegan Paul, London; Translated by C. Smith from the French original version, Phénoménologie de la perception.
Miller, J.F.; Oertel, C.B., Powerlessness in the elderly: preventing hopelessness, In: (Editor: Miller, J.F.) Coping with Chronic Illness: Overcoming Powerlessness (1983) FA Davis, Philadelphia.
Moore-Corner, R.; Kielhofner, G.; Olsen, L., Work Environment Impact Scale (WEIS) (Version 2). (1998) Model of Human Occupational Clearinghouse, Department of Occupational Therapy, College of applied Health Sciences, University of Illinois at Chicago, Chicago.
Mosey, A., Psychosocial Components of Occupational Therapy. (1986) Raven, New York.
Murphy, R., The Body Silent. (1987) Henry Holt, New York.
National Board for Certification in Occupational Therapy, A practice analysis study of entry-level occupational therapist registered and certified occupational therapy assistant practice, OTJR, Occupation, Participation and Health Volume 24 (Supplement 1) (2004) S3–31; Spring.
Parkinson, S.; Forsyth, K.; Kielhofner, G., The Model of Human Occupation Screening tool (MOHOST), version 1.0. (2001) Model of Human Occupation Clearinghouse, Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago, Chicago.
Peterson, E.; Howland, J.; Kielhofner, G.; et al., Falls self-efficacy and occupational adaptation among elders, Physical & Occupational Therapy in Geriatrics 16 (1999) 1–16.
Reilly, M., Occupational therapy can be one of the great ideas of 20th century medicine, American Journal of Occupational Therapy 16 (1962) 1–9.
Riccio, C.M.; Nelson, D.L.; Bush, M.A., Adding purpose to the repetitive exercises of elderly women, American Journal of Occupational Therapy 44 (1990) 714–719.
Rotter, J.B., Generalized expectancies for internal versus external control of reinforcement, Psychological Monographs: General Applications 80 (1960) 1–28.
Shannon, P., The work-play model: A basis for occupational therapy programming, American Journal of Occupational Therapy 24 (1970) 215–218.
Sumsion, T., Client-centred Practice in Occupational Therapy: A Guide to Implementation. (1999) Churchill Livingstone, Edinburgh.
Taylor, R.; Braveman, B.; Forsyth, K., Occupational science and the scholarship of practice: implications for practitioners, New Zealand Journal of Occupational Therapy 49 (2002) 37–40.
Taylor, R.R.; Lee, S.W.; Kielhofner, G.; Ketkar, M., Therapeutic use of self: A nationwide survey of practitioners? attitudes and experiences, American Journal of Occupational Therapy 63 (2009) 198–207.
Toglia, J.P., The multicontext treatment approach, In: (Editors: Crepeau, E.B.; Schell, B.; Cohn, E.) Willard and Spackman's Occupational Therapy (2003) Lippincott Williams & Wilkins, Philadelphia.
Toombs, K., The Meaning of Illness: A Phenomenological Account of the Different Perspectives of Physician and Patient. (1992) Kluwer Academic, Boston.
Trombly, C.A., Occupational Therapy for Physical Dysfunction. (1989) Williams & Wilkins, Baltimore.
Trombly, C., Occupation: purposefulness and meaningfulness as therapeutic mechanisms, American Journal of Occupational Therapy 49 (1995) 960–972.
World Health Organization, ICIDH-2: International Classification of Functioning and Disability. Beta-2 draft, full version. (1999) WHO, Geneva.
Yoder, R.; Nelson, D.; Smith, D., Added-purpose versus rote exercise in female nursing home residents, The American Journal of Occupational Therapy: Official Publication of The American Occupational Therapy Association 43 (9) (1989) 581–586.