Chapter 17 Ultrasonographic Examination of Joints
Ultrasonography has become an essential imaging technique for assessing joint lesions.1-6 It provides information complementary to radiography but does have some limitations. Ultrasonography requires a precise knowledge of anatomy, not only bone anatomy,4 and a systematic approach. Examining the joints of the distal part of the limb is physically uncomfortable for the imager and is time-consuming: complete examination of a joint may take up to 30 minutes. Quick examination of joints requires several years of daily practice.
The indications for ultrasonographic examination of equine joints include synovial fluid distention, local swelling, pain on passive manipulation of the joint, improvement in lameness after intraarticular or perineural analgesia, and positive radiological or scintigraphic findings. The area to be examined should be clipped, not shaved, and washed with hot water. High-resolution transducers (7.5- to 13-MHz linear probes) and a standoff pad are used for superficial structures. Convex array 2.5- to 5-MHz transducers are preferable for deeper structures. Both left and right joints should be examined to improve sensitivity and specificity. The image quality depends not only on the frequency of the transducer but also on the quality of the machine (from treatment of the signal to display on the monitor) and the skill of the operator in placing and orienting the transducer.
A comprehensive description of all joints cannot be given in this book. The fetlock joint is a model for a general approach to ultrasonography of joints because of its simple anatomy. Some aspects of examination of the stifle and hock also are presented.
Fetlock
Each aspect of the joint should be examined systematically using 7.5- to 13-MHz linear transducers and a thin standoff pad.
Dorsal Aspect
Figure 17-1 shows normal ultrasonographic anatomy.4,5 In normal fetlock joints the articular capsule is echogenic (except if too relaxed), and the articular margins of the proximal phalanx and the condyles of the third metacarpal bone (McIII) are smooth.

Fig. 17-1 Sagittal ultrasonographic image of the dorsal aspect of the fetlock, normal appearance. Proximal is to the left. 1, Skin; 2, dorsal joint capsule; 3, proximal synovial fold; 4, subchondral bone of the condyle of the third metacarpal bone; 5, articular cartilage of the condyle of third metacarpal bone; 6, proximal phalanx.
Ultrasonography is a useful technique for the differential diagnosis of soft tissue injuries on the dorsal aspect of the fetlock joint. These lesions include subcutaneous swelling or abscess, bursitis of the subtendonous bursa of the extensor tendons, extensor tendonitis, capsulitis, synovial fluid distention of the dorsal recess of the metacarpophalangeal joint (Figure 17-2), and chronic proliferative synovitis of the proximodorsal synovial fold of this joint (Figure 17-3). Thinning, fibrillation, and fissures of the articular cartilage of the dorsal and distal aspects of the condyle of the McIII can be identified with high-resolution transducers. Subchondral bone lesions can sometimes be detected before they are visible radiologically. Ultrasonography may be more sensitive than radiography for detection of the site and number of osteochondral fragments.7
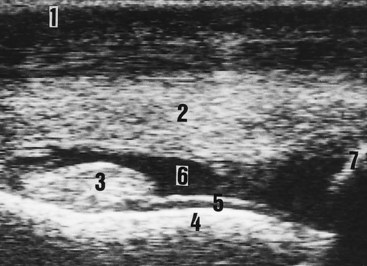
Fig. 17-2 Sagittal ultrasonographic image of the dorsal aspect of the fetlock joint. An abnormal synovial fluid accumulation appears between the joint capsule and the articular surface. The diagnosis is synovial fluid effusion, indicative of synovitis. Proximal is to the left. 1, Skin; 2, dorsal joint capsule; 3, proximal synovial fold; 4, subchondral bone of the condyle of the third metacarpal bone; 5, articular cartilage of the condyle of the third metacarpal bone; 6, synovial fluid; 7, proximal phalanx.
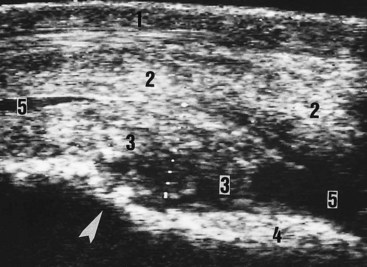
Fig. 17-3 Sagittal ultrasonographic image of the dorsal aspect of the fetlock joint. An abnormal hypoechogenic mass appears between the capsule and the condyle of the third metacarpal bone. The proximal aspect of this condyle is irregular, indicating bone lysis (arrowhead). The diagnosis is chronic proliferative synovitis. 1, Skin; 2, dorsal joint capsule; 3, proximal synovial fold tremendously thickened and echogenic; 4, condyle of the third metacarpal bone; 5, synovial fluid.
Dorsomedial and Dorsolateral Aspects
Examination of the dorsomedial and dorsolateral aspects of the joint is especially useful for complete evaluation of the articular margins, which are smooth in a normal joint. The most common abnormal finding is the presence of periarticular osteophytes. Other injuries are subcutaneous lesions (fibrosis, swelling) and capsulitis.
Medial and Lateral Aspects
The medial and lateral collateral ligaments have superficial and deep layers.4 If the transducer is parallel to the skin (the ultrasound beam is perpendicular to fiber interface), the superficial layer of the collateral ligament is echogenic and the deep layer is hypoechogenic. Either layer may be damaged (Figure 17-4). If both layers are affected, joint instability, subluxation, or luxation occurs.
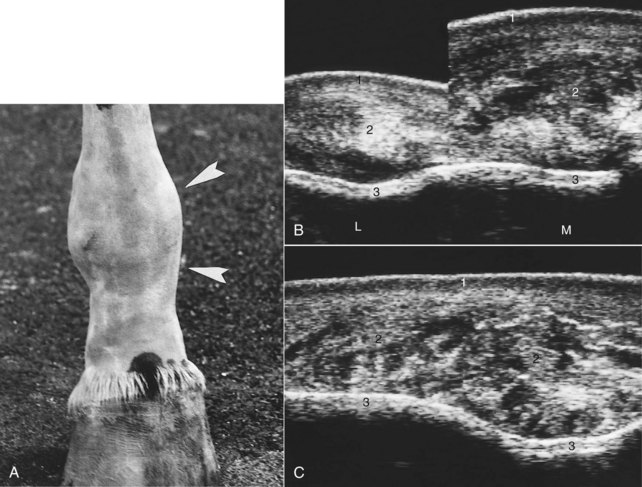
Fig. 17-4 A, Physical appearance of an injured right hind fetlock joint (arrowheads show medial enlargement). Radiography found no bony abnormalities. B, Transverse ultrasonographic images of the lateral (L) and medial (M) aspects of the injured fetlock. The size and architecture differ greatly between the normal lateral collateral ligament and the injured medial ligament. C, Longitudinal ultrasonographic image of the medial aspect of the fetlock shows the thickening and architectural alterations of the medial collateral ligament. The diagnosis is chronic desmopathy of the medial collateral ligament. 1, Skin; 2, collateral ligament; 3, condyle of the third metatarsal bone.
Palmar Aspect
A normal fetlock joint has a small amount of anechogenic synovial fluid in the proximopalmar recess of the fetlock joint. Abnormal findings observed in affected horses include synovial fluid distention, often associated with enlarged synovial folds, indicative of synovitis (Figure 17-5).
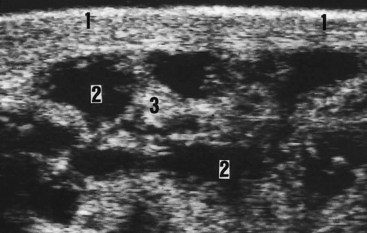
Fig. 17-5 Longitudinal ultrasonographic image of the palmarolateral aspect of the fetlock demonstrating a marked fluid distention of the palmaroproximal recess of the fetlock. The diagnosis is synovial fluid effusion indicative of synovitis. 1, Skin; 2, synovial fluid; 3, synovial membrane and villi.
Echogenic material may be observed in the synovial fluid in any view. Small echogenic spots may represent fibrin or cartilaginous debris. Larger echogenic masses are compatible with osteochondral fragments. These abnormal findings are more easily seen after movement of the joint. A homogeneous increase in echogenicity of the fluid is compatible with hemarthrosis or infectious synovitis.
Stifle
Ultrasonography has considerably improved the knowledge and the diagnosis of soft tissue injuries of the femoropatellar and femorotibial joints.
Femoropatellar Joint
The femoropatellar joint is examined using 5- to 10-MHz linear transducers with a thin standoff pad. The normal patellar ligaments are homogeneously echogenic.1-3 The articular cartilage is thicker over the lateral trochlear ridge compared with the medial. Each femoral trochlea has a regular hyperechogenic subchondral bone surface.
Medial patellar desmopathy usually is iatrogenic (i.e., caused by medial patellar desmotomy or desmoplasty). Desmopathy of the intermediate (middle) patellar ligament is an injury that occurs in athletic horses.8 Lateral patellar desmopathy often is caused by trauma (Figure 17-6).

Fig. 17-6 Longitudinal ultrasonographic image of the lateral patellar ligament demonstrating localized enlargement. At the site of the lesion (arrowheads) the ligament is hypoechogenic and shows severe architectural changes. Diagnosis is traumatic lateral patellar desmopathy. 1, Skin; 2, lateral patellar ligament; 3, lateral ridge of the femoral trochlea (subchondral bone surface); 4, patella.
Osteochondrosis of the trochlear ridges is easy to diagnose, and ultrasonography provides information on the extent of the lesion (especially in a lateromedial direction), the size and location of the osteochondral fragments, and the severity of alteration of the subchondral bone.9 Evaluation of the synovial fluid and membrane may also be useful to assess the consequences of ligamentous and osteochondral lesions in the joint.
Medial and Lateral Femorotibial Joints
Examination of the femorotibial joint requires 5- to 10-MHz linear transducers and a thin standoff pad.10-13 In normal joints the medial recess of the medial femorotibial joint is less than 3 cm long in a craniocaudal direction, and the synovial fluid is totally anechogenic. The normal medial collateral ligament and medial meniscus are homogeneously echogenic,1-3 provided that the ultrasound beam is perpendicular to the orientation of the fibers. The normal articular margins of the medial femoral condyle and tibial plateau are smooth and regular.
The medial recess of the medial femorotibial joint can be considered a mirror of the joint, because its size and content are influenced by all joint lesions. Abnormalities include synovial effusion (Figure 17-7); chronic proliferative synovitis; hemarthrosis (Figure 17-8); echogenic spots compatible with fibrin, cartilaginous, or meniscal debris (Figure 17-9); osteochondral fragments; and calcinosis circumscripta. The caudal recess of the medial femorotibial joint can be examined with 2.5- to 5-MHz sector or convex array probes. Distention of this recess always indicates severe femorotibial disease. Distention of the subextensorius recess on the craniolateral aspect of the lateral femorotibial joint can be observed in lateral femorotibial arthropathy or femoropatellar joint lesions.

Fig. 17-7 Transverse ultrasonographic image of the medial recess of the medial femorotibial joint. Anechogenic synovial fluid has distended this recess. The diagnosis is synovial effusion compatible with synovitis and other potential injuries of the femorotibial joint. 1, Skin; 2, medial femoral fascia; 3, synovial membrane; 4, medial recess of the medial femorotibial joint; 5, medial aspect of the distal femur.
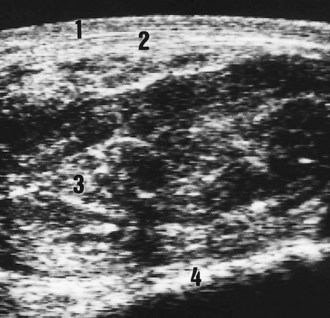
Fig. 17-8 Transverse ultrasonographic image of the medial recess of the medial femorotibial joint. Echogenic material distends the recess. The diagnosis is hemarthrosis compatible with other potential ligament or bone injuries of the femorotibial joint. 1, Skin; 2, medial femoral fascia; 3, medial recess of the medial femorotibial joint; 4, medial aspect of the distal femur.
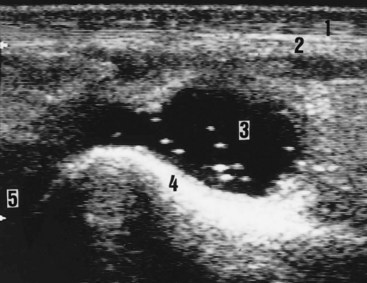
Fig. 17-9 Longitudinal ultrasonographic image of the medial recess of the medial femorotibial joint. Echogenic material floats in the synovial fluid. These echogenic spots represent fibrin, cartilaginous debris, or meniscal debris. Proximal is to the right. 1, Skin; 2, medial femoral fascia; 3, medial recess of the medial femorotibial joint; 4, medial femoral condyle; 5, medial meniscus (anechogenic because of the orientation of the ultrasound beam).
Desmopathy of the medial collateral ligament may be identified as disruption in the normal parallel fiber pattern (Figure 17-10).
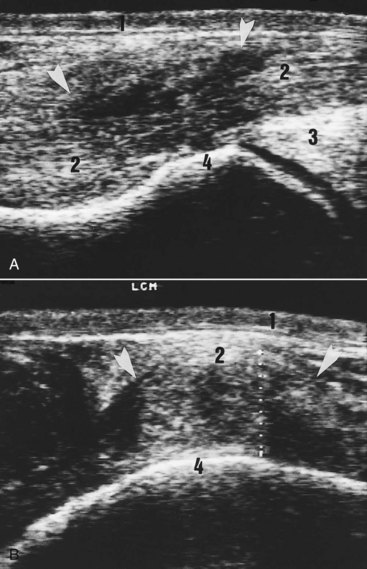
Fig. 17-10 A, Longitudinal ultrasonographic image (proximal is left) of the medial collateral ligament of the femorotibial joint. This ligament is enlarged and hypoechogenic (arrowheads). Diagnosis is traumatic medial collateral desmopathy. B, Transverse ultrasound scan of the medial collateral ligament. 1, Skin; 2, medial collateral ligament; 3, medial meniscus; 4, medial femoral condyle.
Meniscal injuries can be observed alone or with other ligamentous or bone injuries (Figure 17-11). In horses, approximately 75% of these lesions are found in the medial meniscus and 25% in the lateral meniscus. A wide range of type and severity of medial meniscal injuries may be seen (see Figures 17-11 and 17-12).
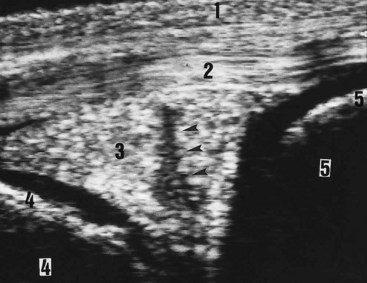
Fig. 17-11 Proximodistal ultrasonographic image of the medial aspect of the medial femorotibial joint showing a transverse section of the body of the medial meniscus. An obvious hypoechoic defect (arrowheads) is seen. The diagnosis is medial meniscal lesion. 1, Skin; 2, medial collateral ligament; 3, medial meniscus; 4, medial femoral condyle (with anechoic articular cartilage); 5, medial tibial condyle (with anechogenic articular cartilage).
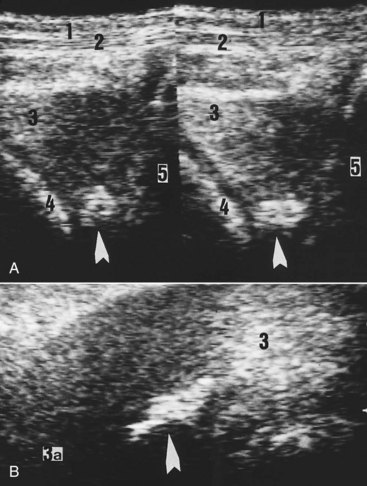
Fig. 17-12 A, Proximodistal ultrasonographic image of the craniomedial aspect of the medial femorotibial joint showing transverse sections of the cranial horn of the medial meniscus. Hyperechogenic material is present in the deep (axial) part of this horn (arrowheads). B, Transverse ultrasonographic image of the craniomedial aspect of the medial femorotibial joint showing a horizontal section of the cranial horn of the medial meniscus. This scan confirms presence of hyperechogenic material in the horn. The diagnosis is that hyperechogenic material is a focal site of mineralized metaplasia in a meniscus. 1, Skin; 2, medial femoral fascia; 3, medial meniscus; 3a, cranial attachment; 4, medial femoral condyle; 5, medial tibial condyle.
If a transducer is held vertically and moved in a caudocranial direction, complete examination of the articular margins of the femoral condyles is possible. Ultrasonography may be more sensitive than radiography in detecting periarticular osteophytes. If the stifle is examined in flexion, the cartilage and subchondral bone surface of the femoral condyles can be imaged.1-3 Alterations of the subchondral bone surface and echogenicity may be detected.
Collateral Ligaments of the Hock
The causes of soft tissue enlargement of the hock may be difficult to assess clinically and radiologically. The medial and lateral collateral ligaments of the hock are highly echogenic fibrous structures.14 Each is divided into a long collateral ligament, which inserts distally on the distal aspect of the tarsus and the proximal aspect of the metatarsal region, and a short collateral ligament with two fasciculi: a calcanean fasciculus and a talien one.
Proximal avulsion fracture of the calcanean fasciculus of the medial collateral ligament has been identified (Figure 17-13). Lesions of this ligament also can be identified in hocks with no radiological abnormality (Figure 17-14). In old lesions the long medial collateral ligament remains thickened and may have focal echogenic sites associated with mineralization.
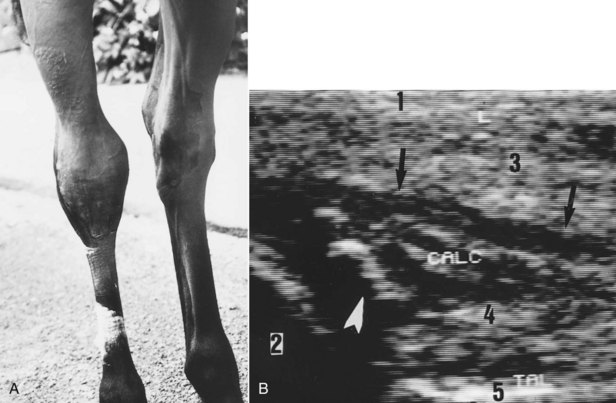
Fig. 17-13 A, Acute medial collateral desmopathy in a 15-month-old filly. Physical appearance of the hock with a medial swelling. B, Longitudinal ultrasonographic image of the calcanean fasciculus of the medial collateral ligament. This structure is thickened and hypoechogenic with evidence of fiber disruption. An echogenic osteochondral fragment (arrowhead) appears close to the medial malleolus of the tibia. The diagnosis is severe desmopathy with avulsion fracture involving the calcanean fasciculus of the medial collateral ligament. 1, skin; 2, medial malleolus of the tibia; 3, long medial collateral ligament; 4, short medial collateral ligament—calcanean fasciculus (CALC); 5, medial aspect of the talus (TAL).
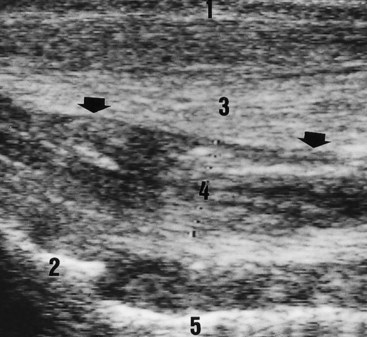
Fig. 17-14 Longitudinal ultrasonographic image of the calcanean fasciculus of the medial collateral ligament of a 9-year-old Three Day Event gelding after injury 3 months previously. This structure (black arrows) is thickened and has architectural changes. The diagnosis is desmopathy of the calcanean fasciculus of the medial collateral ligament. 1, Skin; 2, medial malleolus of the tibia; 3, long medial collateral ligament; 4, short medial collateral ligament—calcanean fasciculus (arrowheads); 5, medial aspect of the talus.
Several types of injury of the lateral collateral ligament have been identified, including desmopathy of the long lateral collateral ligament, avulsion fracture of the short lateral collateral ligament at the proximal insertion on the lateral malleolus of the tibia (distal portion of the fibula), and desmitis of the short lateral collateral ligament associated with sudden synovial distention of the tarsocrural joint capsule.