Chapter 51Diagnosis and Management of Sacroiliac Joint Injuries
Anatomical and Functional Features
The sacroiliac joint is a synovial articulation located at the junction between the ventral aspect of the wing of the ilium and the dorsal aspect of the wing of the sacrum (Figure 51-1). The sacroiliac joint functions in pelvic attachment to the axial skeleton, providing support during weight bearing and helping to transfer propulsive forces of the hindlimb to the vertebral column. The sacroiliac joint is an atypical synovial articulation because of hyaline cartilage on the sacral articular surface and a thin layer of fibrocartilage on the ilial articular surface.1 The articular surfaces of the sacroiliac joint are nearly flat and closely apposed to support gliding movements. The sacroiliac articular surfaces diverge cranially at about 40 degrees from a transverse plane and are angled craniodorsally to caudoventrally at about 60 degrees from the horizontal plane. The joint capsule is thin and closely follows the margins of the sacroiliac articular cartilage. The sacroiliac joint capsule is reinforced ventrally by the ventral sacroiliac ligament.2 A small amount (<1 mL) of synovial fluid is normally present in the joint.1 Because of articular surface remodeling, the size and shape of the sacroiliac joint margins vary considerably according to age and body weight.3 Typically the sacroiliac joint outline is L-shaped, with the convex border directed caudoventrally.
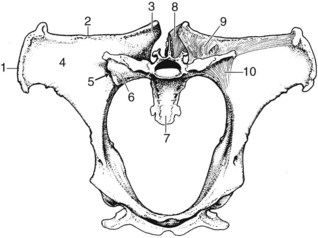
Figure 51-1 Diagram of the pelvis, sacrum, and sacroiliac ligaments (cranial view). 1, Tuber coxae; 2, ilial crest; 3, tuber sacrale; 4, ventral surface of the ilial wing; 5, sacroiliac articulation; 6, sacral wing; 7, sacrum; 8, dorsal sacroiliac ligament; 9, interosseous sacroiliac ligament; 10, ventral sacroiliac ligament.
(Modified from Dyce KM, Sack WO, Wensing CJG: Textbook of veterinary anatomy, ed 2, Philadelphia, 1996, Saunders.)
The pelvis is firmly attached to the axial skeleton by sacroiliac and sacrosciatic ligaments, which form a strong ligamentous sling (see Figure 51-1). The weight of the caudal aspect of the vertebral column is suspended from the sacroiliac ligaments, which function similarly to the fibromuscular sling found between the proximal aspect of the forelimb and the lateral thoracic body wall. Subsequently the sacroiliac articular cartilage may never be fully weight bearing, unlike most articular cartilage. The sacroiliac joint is supported by three pairs of strong ligaments: the dorsal, interosseous, and ventral sacroiliac ligaments. The dorsal sacroiliac ligament consists of dorsal and lateral portions (Figure 51-2). The dorsal portions form two round cords that span from the dorsal aspects of the tubera sacrale to the dorsal apices of the sacral spinous processes. The lateral portion forms a sheet of connective tissue that spans from the caudal margin of each tuber sacrale and iliac wing to the lateral border of the sacrum. The lateral portion of the sacroiliac ligament is continuous ventrally with the sacrosciatic ligament. The interosseous ligament of the sacroiliac joint is robust and consists of a series of vertical fibers that connect the ventral aspect of the wing of the ilium to the dorsal aspect of the wing of the sacrum (see Figure 51-1). The interosseous sacroiliac ligament provides the major resistance to vertically oriented weight-bearing forces acting on the sacrum. The ventral sacroiliac ligament interconnects the ventral aspects of the wings of the ilium and sacrum. The ventral sacroiliac ligament is thin and closely applied to the ventral margins of the sacroiliac joint capsule.
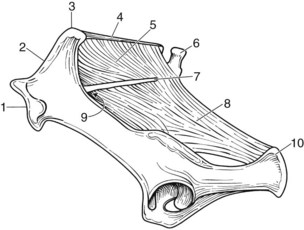
Figure 51-2 Diagram of the pelvis, sacrum, and sacroiliac ligaments (lateral view). 1, Tuber coxae; 2, ilial crest; 3, tuber sacrale; 4, dorsal sacroiliac ligament (dorsal portion); 5, dorsal sacroiliac ligament (lateral portion); 6, first coccygeal vertebrae; 7, lateral portion of sacrum; 8, sacrosciatic ligament; 9, greater sciatic foramen; 10, ischial tuberosity.
Neurovascular structures adjacent to the sacroiliac joint include the sciatic nerve, cranial gluteal nerve, and cranial gluteal artery and vein. These structures collectively travel through the greater sciatic foramen, ventromedial to the sacroiliac articulation (see Figure 51-2). The cranial gluteal artery and vein arise from the internal iliac vessels and travel over the ventral sacroiliac ligament and the caudomedial aspect of the sacroiliac joint before emerging at the greater sciatic foramen. The cranial gluteal artery and vein continue dorsally into the gluteal musculature. The middle and accessory gluteal muscles originate from the dorsal aspect of the ilial wing and have attachments near the caudomedial aspect of the sacroiliac joint. Within the pelvic canal, a portion of the internal obturator and iliacus muscles covers the ventral sacroiliac joint margins.
The robust sacroiliac and sacrosciatic ligaments limit motion at the sacroiliac articulations.4 Shear forces would be expected at the sacroiliac articular surfaces more than compressive forces, which are common in most limb articulations.5 Sacroiliac joint movements are restricted to small amounts of approximately 1 degree during flexion (nutation) and extension (counternutation), with an apparent axis of rotation oriented transversely near the caudomedial aspect of the joint.6,7 As a result of coupled sacroiliac joint motion of flexion-extension, lateral bending, and axial rotation combined with concurrent pelvic deformation, motion at the sacroiliac joints is complex.8 Lateral movements at the sacroiliac articulations are severely restricted, primarily because of lateral attachments of the ventral sacroiliac ligaments and, to a lesser degree, the lateral portion of the dorsal sacroiliac ligaments and the sacrosciatic ligaments. The wings of the ilium overlay the sacral articular surfaces dorsally and laterally, which precludes any axial rotation from occurring at the sacroiliac joint. Dorsal displacement of the ilial wings is limited by the robust interosseous ligament, the ventral sacroiliac ligament, and lateral portion of the dorsal sacroiliac ligaments.9 Propulsive forces of the hindlimb are transmitted dorsally and cranially to the vertebral column by the articular configuration of the overlapping and divergent ilial wings over the sacrum and by reinforcement from the dorsal and interosseous sacroiliac ligaments. The dorsal sacroiliac ligament also provides resistance against contraction of the powerful longissimus muscle and robust thoracolumbar fascia, which attach along the cranial border of the ilial wing.
Pathological Conditions
The antemortem diagnosis of sacroiliac joint injury in horses is difficult and often based on a diagnosis of exclusion.10 Diagnosis is complicated by anatomical inaccessibility, mild chronic clinical signs so that opportunities for correlation with necropsy findings are uncommon, and ongoing controversies over the clinical relevance and prevalence of pathological conditions of the articular surface and ligaments.4 Terms used to describe pathological conditions of the sacroiliac joint include sacroiliac sprain or instability,11,12 sacroiliac joint subluxation,13 and sacroiliac arthrosis.14,15 The prevalence of pathological conditions of the sacroiliac joint in performance horses is probably high, and many may go undiagnosed.4,14,16 In a necropsy survey of 36 Thoroughbred (TB) racehorses with no known back or sacroiliac joint problems, we observed various degrees of degenerative sacroiliac joint changes in all specimens.17 The clinical importance of osseous sacroiliac joint pathological conditions is difficult to determine because many presumed normal horses have osteoarthritic changes similar to horses with known back or sacroiliac problems.1,4 Possibly the majority of sacroiliac joint pathological conditions are subclinical; however, if similar findings were noted in any other musculoskeletal location, the articular changes would be considered clinically relevant and a likely contributing cause of lameness. A more likely scenario is that deep sclerotogenous pain (e.g., vertebral or sacroiliac joint osteoarthritis [OA]) is often poorly localized and perceived as deep aching pain, based on reports of similar pathological conditions of the sacroiliac joint in affected people. Clinically the most common reported signs of sacroiliac joint disorders in horses are poor performance, lack of impulsion, and a mild, chronic hindlimb lameness, which can easily be overlooked or dismissed as not clinically relevant.4,18 Obvious signs of lameness and localized pain or inflammation are not typical clinical characteristics of sacroiliac joint or pelvic injuries, unless pelvic fractures or substantial joint disruption is present.
OA of the sacroiliac joints is usually a bilateral condition and may be present despite symmetry of the tubera sacrale.19 Degenerative changes of the sacroiliac joint include (in apparent order of increasing severity) articular surface lipping, cortical buttressing, articular recession, osteophytes, and intraarticular erosions (Figure 51-3). In our survey of 36 TB racehorses, sacroiliac degenerative changes were classified as mild in 8% of specimens, moderate in 61%, and severe in 31%. Age was not associated with overall prevalence or severity of sacroiliac joint degenerative changes.17 Osseous changes are usually bilaterally symmetrical and most commonly located at the caudomedial aspect of the articulation.1,17 The pathogenesis of proliferative sacroiliac joint changes is uncertain, but it is thought to be related to chronic instability resulting in gradual remodeling and subsequent enlargement of the caudomedial joint surfaces. Histologically the caudomedial extensions consist of apparently normal cancellous bone.4 Articular cartilage erosion is a lytic process of articular surfaces that presumably leads to eventual sacroiliac joint ankylosis.17 However, ankylosis of the sacroiliac joint is rare, which is surprising based on the limited joint motion and the potential severity of osseous pathological conditions present.1,17,20 Fibrous interconnections between the articular surfaces have also been reported in presumed normal sacroiliac joints.1 Articular cartilage discoloration, a presumed indicator of sacroiliac joint degeneration, is common in racehorses, but it has a reported higher prevalence in Standardbreds (STBs) compared with TBs.14 One theory is that these changes are caused by differences in pelvic and sacroiliac joint biomechanics associated with pacing and trotting (i.e., lateral bending or shear forces) in STBs compared with galloping (i.e., flexion and extension movements) in TBs.21 Biomechanical studies are warranted to support or refute these claims.

Figure 51-3 Bilateral osteoarthritis of the sacroiliac articulations (ventral view). Severe proliferative changes of the caudomedial third of the sacroiliac joints (arrows) in an 8-year-old racing Thoroughbred gelding that was euthanized because of an acute colic episode. Normal sacroiliac joint margins are typically smooth and linear as represented by the cranial half of the sacroiliac articulations.
Sacroiliac desmitis, the most common soft tissue injury, was documented by ultrasonography in the dorsal portion of the dorsal sacroiliac ligament.22 A diagnosis of sacroiliac desmitis is based on loss of normal echogenicity on a transverse image and a decrease in parallel fiber pattern on a longitudinal image. Sacroiliac ligament injuries usually occur because of acute trauma, but few horses with documented injury were reported.17,23
Complete sacroiliac ligament disruption is most likely caused by substantial trauma, such as flipping over backward, or catastrophic musculoskeletal injuries associated with race training.17 Post mortem findings associated with traumatic sacroiliac ligament injuries include either unilateral or bilateral joint capsule disruption, avulsion fractures of the sacroiliac ligament attachment sites, and noticeable sacroiliac joint laxity. Dorsal or ventral sacroiliac ligaments can be affected, depending on the inciting mechanism of injury.9,17,23 Complete sacroiliac ligament disruption may produce unilateral or bilateral dorsal displacement of the tubera sacrale, depending on the extent of injury (Figure 51-4).
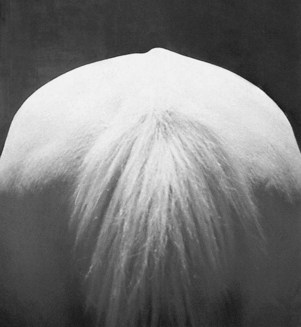
Figure 51-4 Photograph of tubera sacrale height asymmetry (caudal view). The tuber sacrale on the right side is dorsally displaced, with apparent gluteal muscle symmetry.
(Courtesy Al Kane, Ft. Collins, Colo, United States.)
Acute sacroiliac ligament injuries have been reported to contribute to development of chronic sacroiliac joint instability.11,23 However, the presence and relevance of chronic sacroiliac ligament injury and sacroiliac joint laxity are controversial. Rooney et al23,24 documented chronic sacroiliac joint injuries of the cranial portion of the ventral sacroiliac ligaments, which were found to be elongated or torn on the affected side. Desmitis of the insertion site of the dorsal portion of the dorsal sacroiliac ligament at the insertion on the tuber sacrale was reported.9 In other studies osseous changes were found at the caudomedial sacroiliac joint margins in horses suspected of having chronic sacroiliac injury; however, no obvious sacroiliac ligament laxity was observed.4,11,12 Radiologically some of these horses had an apparent increase in the sacroiliac joint space; however, no visible sacroiliac ligament injury, joint laxity, or subluxation was observed at necropsy.4,12 In our necropsy survey of 36 TB racehorses, no evidence of chronic ligament injury or sacroiliac joint subluxation was observed.17 However, this could be related to the previous removal of horses from race training with poor performance or hindlimb lameness associated with chronic sacroiliac joint injury.
The pathogenesis of apparent spontaneous or insidious differences in tuber sacrale height needs to be further researched.4 Unilateral or bilateral dorsal displacement of the tubera sacrale is often a presumed indication of sacroiliac subluxation.25 In my opinion, variable degrees of tubera sacrale height asymmetry occur frequently and may be caused by chronic asymmetric muscular or ligamentous forces acting on the malleable osseous pelvis and not by direct sacroiliac ligament injury.26 Tubera sacrale height asymmetries are common in horses without documented sacroiliac joint injuries (see Figure 51-4). In only a few horses have tubera sacrale height asymmetries been associated with chronic sacroiliac ligament injuries or joint laxity.24 In a study of 4-year-old STB trotters with tubera sacrale height asymmetries of more than 1 cm, associations were found with poor performance, but otherwise the asymmetry was of questionable clinical importance.16 If substantial tubera sacrale height differences are identified, which side is affected is unclear and difficult to determine: the seemingly dorsally displaced tuber sacrale or the less prominent tuber sacrale on the opposite side.4,16 Presumed sacroiliac joint subluxation produces an elevated tuber sacrale on the affected side, whereas complete ilial wing fractures (the most common type of pelvic fracture) typically produce a palpably depressed tuber sacrale on the affected side.27
Clinical Presentation
Horses with sacroiliac joint injuries vary in clinical presentation, usually based on the duration and extent of injury present. The history of horses with acute sacroiliac joint injury usually includes slipping, falling, or trauma that causes pelvic rotation or induces high stresses.25 Horses with acute sacroiliac joint injuries often have noticeable lameness and localized sensitivity to palpation of the surrounding soft tissues or tubera sacrale (Figure 51-5), which must be differentiated from other sources of back, pelvic, or hindlimb pain. Diagnosis of acute sacroiliac ligament rupture and subsequent sacroiliac joint subluxation or luxation is based on history, physical examination, and diagnostic imaging. Because the majority of horses have some degree of tuber sacrale height asymmetry, a diagnosis of acute sacroiliac joint subluxation can only be confirmed if symmetry of the tuber sacrale was documented immediately before the injury, and subsequently gross asymmetry of the tubera sacrale is noted with localized signs of pain or inflammation.
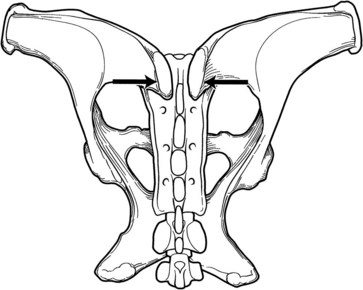
Figure 51-5 Diagram of sacroiliac joint provocation test (dorsal view). Firm pressure is applied bilaterally with both hands, compressing the dorsal aspects of the tubera sacrale.
Important historical findings in horses with chronic sacroiliac joint injuries usually involve repetitive overuse versus a single traumatic event.14 The most consistent clinical feature of chronic sacroiliac joint injury is a prolonged, nonprogressive history of reduced or poor performance.4 In a recent study Warmblood horses involved in dressage and show jumping were most commonly affected.28 Changes in performance included back stiffness, unwillingness to work, lack of impulsion from one or both hindlimbs, and refusing jumps. The duration of clinical signs varied from 1 month to more than 1 year, and to an untrained observer many of the horses appeared clinically normal.28 Subtle gait asymmetries may be noticed at slow speeds during ground work or dressage movements and in harness horses at racing speeds.4 Signs are often markedly accentuated when the horse is ridden, especially with changes in direction through tight circles in trot, half passes, or flying lead changes in canter.19 Chronic sacroiliac joint injuries usually produce a low-grade or intermittent hindlimb lameness or stiffness that cannot be localized by routine lameness examination techniques and is improved only temporarily with antiinflammatory medications.4 The affected sacroiliac joint usually corresponds to the side of lameness or reduced cranial swing phase of the affected hindlimb, but bilateral gait abnormalities can occur. Gait asymmetries involve subtle differences in pelvic movement or reduced hindlimb flexion or stride lengths. Affected horses commonly resent standing on the affected hindlimb while the contralateral hindlimb is lifted off the ground during hock flexion or shoeing.18 Affected horses may also drag a hind foot and have mild hindlimb abduction before hoof contact (i.e., plaiting or rope walking).4 Disuse atrophy of the gluteal musculature is an inconsistent finding; however, some horses have pelvic asymmetry with a lower tuber coxae and noticeable gluteal muscle atrophy on the affected side.4,29 Observation of the tubera sacrale may reveal unilateral or bilateral (i.e., hunters’ or jumpers’ bumps) differences in height or dorsal prominence (see Figure 51-4). Unilateral or bilateral prominence of the tubera sacrale varies between horses and may be related to conformation of the back or pelvis.19 Poor thoracolumbar epaxial or gluteal muscle development may cause the tubera sacrale to be more visually prominent in horses that have chronic back or sacroiliac pain or lack proper collection and engagement of the hindlimbs.
Two clinical manifestations of sacroiliac joint dysfunction were proposed.30 Horses in one category exhibit pain and poor performance that is responsive to local analgesia, tubera sacrale symmetry, and poorly defined pelvic or sacroiliac joint pathology (i.e., functional instability caused by altered neuromotor control). Those in the second category display poor performance and marked gait alterations, bony and soft tissue asymmetry, small improvements with local analgesia, and pathological changes associated with chronic joint instability (i.e., structural instability). Further research is needed to assess whether these proposed categories are clinically useful and distinct or whether they represent a continuum of sacroiliac joint dysfunction.
Physical Examination
Clinical signs of sacroiliac joint injury vary and may occur in conjunction with other sources of hindlimb lameness or poor performance. The sacroiliac joint is relatively inaccessible to direct evaluation or palpation, and the normally small amount of sacroiliac joint motion is difficult to detect clinically.31 Horses with acute sacroiliac joint injuries may have localized sensitivity to palpation of the surrounding soft tissues in the dorsal aspect of the croup.4 A localized region of edema may occasionally be palpated over the lumbosacral junction32; however, this is not a specific finding related to sacroiliac joint injury. Protective muscle spasms may be palpated in the adjacent middle gluteal musculature and the vertebral portions of the biceps femoris, semitendinosus, and semimembranosus muscles. In horses with acute sacroiliac injuries, asymmetry in gluteal muscle development is uncommon, unless pronounced osseous pelvic asymmetry is also present. Pain may be elicited by applying firm digital pressure over the dorsal aspects of the tubera sacrale or caudal lumbar and sacral dorsal spinous processes. Unilateral or bilateral prominence of the tubera sacrale may be noted, but it is not usually clinically relevant unless associated with clinical signs of localized pain or inflammation, or positive findings on diagnostic imaging are found (e.g., scintigraphy). In horses with sacroiliac joint pain, the tubera sacrale may appear grossly symmetrical despite asymmetric croup musculature.28 Normally the tubera sacrale move in unison during pelvic movement in locomotion. A palpable or visible independent movement of the tubera sacrale at a walk or during treadmill locomotion indicates sacroiliac joint subluxation or a complete pelvic fracture. Crepitus associated with sacroiliac joint instability or complete pelvic fracture may be palpable or auscultated with a stethoscope placed over the gluteal musculature as the pelvis is repeatedly rocked laterally. Horses with acute sacroiliac joint injuries may also resent flexion of the hindlimb on the affected side or rectal palpation in the region of the sacroiliac joint.
Horses with chronic sacroiliac joint injuries often have compensatory stiffness and pain in the proximal aspect of the hindlimb.25 Concurrent forelimb or hindlimb lameness needs to be excluded with perineural and intraarticular diagnostic analgesia.28 Upper limb flexion is often negative.4 Mild discomfort can be produced in some horses by picking up one pelvic limb and inducing a gentle lateral sway on the weighted limb.19 Farriers often complain that affected horses have difficulty or refuse to stand while being shod, presumably because of strain or pain induced in the affected single weight-bearing limb.28 Rectal examination for chronic sacroiliac joint subluxation is usually unrewarding and will not be diagnostic unless bone proliferation, excess joint motion, or joint crepitus during externally applied movements is identified.25 A pain response or palpable muscle hypertonicity in the iliopsoas muscles may be noted during rectal examination. Serum chemistry indicators of skeletal muscle injury or inflammation (i.e., creatine kinase [CK] and aspartate transaminase [AST]) are often negative.
The apex of the second sacral spinous process is a reliable landmark used to evaluate relative unilateral or bilateral tubera sacrale displacement. The robust dorsal portion of the dorsal sacroiliac ligament spans between the tubera sacrale and the sacral spinous processes. Normally the dorsal apices of the tubera sacrale and the second sacral spinous process lie in close apposition and follow the contour of the croup. Using palpation, ultrasonography, or radiology, a physical discrepancy in height often can be identified between the dorsal profile of the sacral spinous processes (which should remain constant, unless fractured) and the potentially dorsally or ventrally displaced tuber sacrale. In this manner, unilateral (i.e., tubera sacrale height asymmetry) or bilateral tubera sacrale displacement (i.e., hunters’ or jumpers’ bumps) can be diagnosed, depending on whether one or both tubera sacrale are elevated relative to the apices of the sacral spinous processes. Bilateral tubera sacrale displacement has an unknown clinical relevance and may occur without clinical signs in many high-level competition horses.32 Theoretically the hunters’ or jumpers’ bumps may provide a longer lever arm for the strong longissimus and thoracolumbar fascia to produce extension at the lumbosacral joint, resulting in increased impulsion and range of hindlimb motion, with subsequent improved performance.
Firm digital pressure applied to the dorsal aspect of each tuber sacrale was reported to produce a variable and inconsistent pain response.18 The tolerance to palpation and applied pressure to soft tissues and bony landmarks of the sacroiliac joint region are subjective assessments. Pressure algometry has the potential to quantify muscle or bone pain in horses with sacroiliac joint injuries.33 Affected horses have lower mechanical nociceptive thresholds and greater left-right differences compared with control horses. In my experience, dramatic pain responses have been produced in affected horses with specific provocation tests, which are useful to establish a presumptive diagnosis of pelvic stress fracture or sacroiliac joint injury. The first procedure involves simultaneous manual compression of the dorsal aspects of both tubera sacrale, which induces a bending moment on the iliac wing and presumably compresses the sacroiliac articulations (see Figure 51-5). Acutely affected horses may have a dramatic reaction to this manipulation and demonstrate sudden hindlimb flexion and an apparent inability to bear weight in the hindlimbs when pressure is applied. Clinicians should gradually apply increasing pressure because affected horses may actually collapse in the hindlimbs and fall to the ground if excess force is applied to the painful tubera sacrale. A negative response is characterized by minimal pain response and slight extension of the lumbosacral joint during manual compression of the tubera sacrale. This test is not specific for pathological conditions of the sacroiliac joint because horses with incomplete or stress fractures of the ilial wing may respond even more dramatically to the applied pressure.
A second procedure used to identify sacroiliac ligament injury involves rhythmically applying a ventrally directed force over the lumbosacral dorsal spinous processes to stress the supporting sacroiliac ligaments. This procedure requires the clinician to get up on an elevated surface (e.g., mounting block) so that the applied forces can be directed vertically over the sixth lumbar and second sacral dorsal spinous processes. Horses with sacroiliac ligament injuries would be expected to resent the induced movement because it specifically stresses the interosseous sacroiliac ligament (i.e., ligamentous sling of the sacropelvic junction). Horses with lumbosacral vertebral joint dysfunction (i.e., localized pain, reduced joint motion, and muscle hypertonicity without structural pathological conditions) may also resent this procedure. Rhythmically applied ventrally directed forces over the dorsal spinous processes at the sacrocaudal junction would be expected specifically to stress the dorsal portion of the dorsal sacroiliac ligament. A positive response to this test combined with positive ultrasonographic findings of desmitis of the dorsal sacroiliac ligament would be highly suggestive of clinically relevant sacroiliac ligament injury.
A similar procedure involves rhythmically applying a ventrally directed force over each tuber coxae to induce general sacroiliac and lumbosacral joint motion. A normal response to the induced movement is fluid vertical motion of the lumbosacral region, with an amplitude of 1 to 2 cm of dorsoventral movement measured over the lumbar dorsal spinous processes. Affected horses have a noticeable pain response, resent the induced movement, or have protective gluteal or sublumbar muscle spasms. The vertically directed force also induces movement at the lumbosacral junction, which must be differentiated from sacroiliac joint injury.
Additional procedures used to localize sacroiliac joint or ligament injuries involve indirectly evaluating pain and ligamentous laxity in the sacroiliac joint using laterally applied forces (Figures 51-6 and 51-7). These procedures are similar to valgus-varus stress tests used to evaluate collateral ligaments of the distal limb articulations. Caution should be taken not to apply excessive force because of the long lever arm action of the sacral apex on the sacroiliac ligaments, which can unduly stress unstable or partially torn ligaments or aggravate an acutely inflamed sacroiliac joint. The proposed mechanism of action of these tests is to use the base of the tail and sacrum as a handle to apply a lateral (horizontal plane) stress to the sacroiliac joint as the wing of the ilium is stabilized. The technique involves two parts. First, the base of the hand closest to the horse’s head is placed over the lateral aspect of the tuber sacrale. The hand closest to the tail grasps the base of the tail head (the second and third coccygeal bones). The sacroiliac joints are then evaluated as firm pressure is simultaneously applied by both hands, pushing with the hand at the tuber sacrale away from the clinician and pulling with the hand at the tail head toward him or her (see Figure 51-6, A). Theoretically this maneuver produces compression of contralateral sacroiliac articular surfaces and distraction of the ipsilateral sacroiliac articular surfaces.
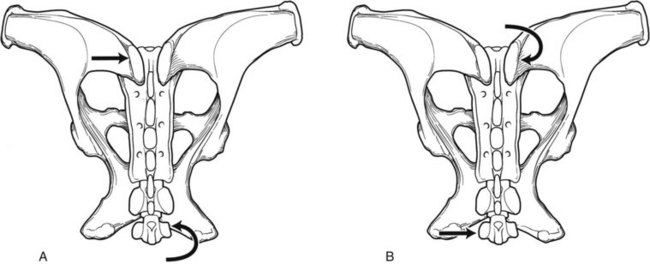
Figure 51-6 Diagram of second sacroiliac joint provocation test (dorsal view). A, Firm pressure is applied by both hands, pushing with the hand at the ipsilateral tuber sacrale away from the clinician while simultaneously pulling with the hand at the tail head toward him or her. B, Firm pressure is applied by both hands, pulling with the hand at the contralateral tuber sacrale toward the clinician while simultaneously pushing with the hand at the tail head away from him or her.
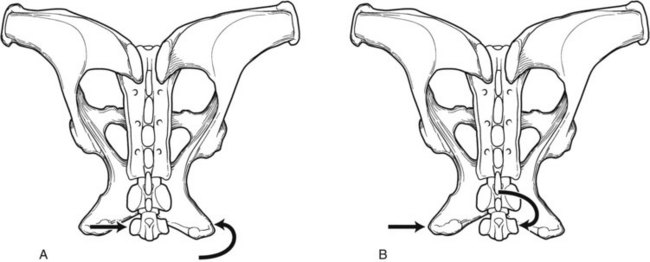
Figure 51-7 Diagram of third sacroiliac joint provocation test (dorsal view). A, Firm pressure is applied by both hands, pushing with the hand at the tail head away from the clinician while simultaneously pulling with the hand at the contralateral ischial tuberosity toward him or her. B, Firm pressure is applied by both hands, pulling with the hand at the tail head toward the clinician while simultaneously pushing with the hand at the ipsilateral ischial tuberosity away from him or her.
The second portion of the technique involves repeating the procedure and reversing the direction of the applied forces (see Figure 51-6, B). The fingers of the hand closest to the horse’s head are placed over the contralateral tuber sacrale, and the base of the hand closest to the tail is placed against the ipsilateral base of the tail head (second and third coccygeal bones). The sacroiliac joints are again evaluated as firm pressure is applied by both hands, pulling with the hand at the tuber sacrale toward the clinician and pushing with the hand at the tail head away from him or her. Theoretically the contralateral sacroiliac articular surfaces are distracted, and the ipsilateral sacroiliac articular surfaces are compressed. A pain response to the induced movements may be identified unilaterally or bilaterally, depending on the extent of inflammation or injury present. In general, sacroiliac joint compression would be expected to aggravate osteoarthritic changes, whereas joint distraction would be expected to stress any injured or inflamed sacroiliac ligaments.
A variation of this basic technique uses repeatedly applied laterally directed forces over the ischial tuberosity instead of the tuber sacrale (see Figure 51-7). This procedure incorporates two long lever arms to stress the supporting sacroiliac ligaments. Again caution should be taken not to apply excessive force because of the long lever arm action of the sacral apex and ischial tuberosities on the sacroiliac ligaments. Lastly, proximal hindlimb manipulation is done to assess coxofemoral and stifle joint range of motion and the willingness to actively extend the hindlimb. Concurrent joint stiffness or muscle hypertonicity can be identified and localized as the proximal aspect of the hindlimb is passively protracted, abducted, flexed, and retracted.
Local Analgesia
Intraarticular analgesia of the sacroiliac joint is nearly impossible because of its deep anatomical location and inaccessible joint capsule.34 Experimentally, intraarticular sacroiliac injections have been accomplished by drilling a hole through the wing of the ilium, dorsal to the sacroiliac joint.18 Regional perfusion with local anesthetic solutions or antiinflammatory drugs for diagnostic or therapeutic purposes was described.35 Approaches from the cranial aspect of the wing of the ilium and the lumbosacral junction are typically used32; however, because of the wide overlying wing of the ilium, the proximity and diffusion of the medication near the sacroiliac joint are questionable.
I recommend a caudomedial approach to the sacroiliac joint region because of anatomical and pathological considerations.34 The caudomedial portion of the sacroiliac joint is the most frequent site of pathological conditions of the sacroiliac joint.1,4,17 Therefore diagnostic analgesia or therapeutic analgesia or antiinflammatory drugs should be directed toward the caudal aspect of the sacroiliac joint in the region of documented pathological condition. Two approaches are described, using 20- to 25-cm-long needles, depending on the depth and conformation of the gluteal musculature (Figure 51-8). Surgical preparation of the injection site is recommended, similar to other joint injection techniques. Ultrasound guidance is also recommended to allow the caudomedial aspect of the sacroiliac joint to be seen and identification of neurovascular structures that must be avoided at the greater sciatic foramen (see Figure 51-2).34,35 The cranial gluteal artery and nerve emerge laterally around the caudal margin of the ilial wing and travel dorsocaudally, adjacent to the sacroiliac joint. Other vital structures, including the sciatic nerve, lie ventral to the sacroiliac joint and travel on or within the substance of the sacrosciatic ligament.
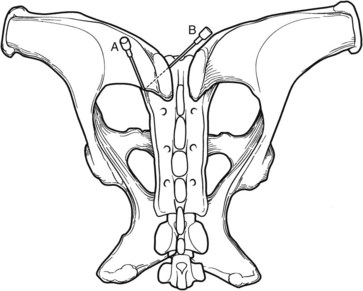
Figure 51-8 Diagram of two approaches to the sacroiliac joint for diagnostic analgesia and therapeutic analgesia or administration of antiinflammatory drugs (dorsal view). A, Dorsal approach over the ipsilateral iliac wing near the caudomedial aspect of the affected sacroiliac joint. B, Medial approach from the cranial aspect of the contralateral tuber sacrale with the needle directed toward the caudomedial aspect of the affected sacroiliac joint.
The first approach involves needle placement dorsally over the iliac wing, ipsilateral to the affected sacroiliac joint (see Figure 51-8, A). This approach is technically easier, but it potentially has a higher risk of injury to the adjacent neurovascular structures. The needle is directed ventrally, toward the region of the sacroiliac joint, and walked off the caudal border of the iliac wing in the region of the sacroiliac joint. Care must be taken to avoid the deeper neurovascular structures. The needle is not advanced once it is walked off the caudal aspect of the iliac wing. Diffusion of the injected material occurs within the middle or accessory gluteal muscles, near the caudomedial attachments of the ventral sacroiliac ligament.
A second preferred approach involves needle placement at the cranial margin of the contralateral tuber sacrale (see Figure 51-8, B). This approach is slightly more technically challenging but has a lower risk of injury to the adjacent neurovascular structures. The needle is inserted along the cranial aspect of the contralateral tuber sacrale and directed toward the cranial edge of the ipsilateral greater trochanter. The needle is placed contralaterally to the affected sacroiliac joint because the needle has to be guided between the divergent sixth lumbar and first sacral dorsal spinous processes and directed into the space formed by the ventral aspect of the ilial wing and the dorsal portion of the sacrum. The needle is advanced caudolaterally along the medial aspect of the affected ilial wing toward the caudomedial portion of the affected sacroiliac joint until contact is made with bone, near the sacroiliac joint margin. Diffusion of the injected material is expected to occur within the longissimus muscle or interosseous sacroiliac ligament. The dorsal nerve branches of the sacral nerves possibly may also be affected with this approach because the nerves exit the first and second dorsal sacral foramina.
Diagnostic Imaging
Ultrasonography has been used to evaluate the dorsal surface of the iliac wing and caudal margin of the sacroiliac articulation to identify dorsal cortex irregularities associated with incomplete and complete ilial wing fractures.36,37 The dorsal sacroiliac ligament can be readily imaged on either side of the sacral dorsal spinous processes caudal to the tubera sacrale.9 Abnormal ultrasound images of the dorsal sacroiliac ligament include enthesopathies at the tubera sacrale attachment sites, hypoechoic changes within the ligament, and modification of fiber orientation.9,22,38 Increased cross-sectional area of the dorsal sacroiliac ligament was reported to cause acute lameness, whereas decreased cross-sectional area was observed in horses with chronic lameness associated with sacroiliac injuries.38 The thoracolumbar longissimus fascia and tendon lie medial to the dorsal portion of the dorsal sacroiliac ligament and blend with its fibers as it inserts on the sacral spinous processes.10 Longissimus tendonitis needs to be differentiated from dorsal sacroiliac desmitis because management of the two conditions may vary considerably.39 The interosseous sacroiliac ligament has not been imaged because of its inaccessible location underneath the ventral aspect of the ilial wing. In contrast, the ventral sacroiliac ligament and the ventral joint margins of the sacroiliac joint can be seen using transrectal ultrasonography.9 Ventral periarticular modeling of the sacroiliac joint was observed with transrectal ultrasound approaches.39
Primary indications for radiography of the pelvis include acute or severe pelvic asymmetries, upper hindlimb lameness, and pelvic crepitus or fractures.40 The deep anatomical location of the sacroiliac joint and superimposition of abdominal viscera make radiographic imaging difficult at best. Ventilation-induced blurring of the abdominal viscera during general anesthesia with horses in dorsal recumbency is a simple technique to help delineate the bony structures of the sacroiliac region.41 The radiological features of chronic sacroiliac joint disease are minimal and include nonspecific increases in the joint space and enlargement of the caudomedial aspect of the sacroiliac joint.4 Radiography is not a sensitive indicator of sacroiliac joint disease because presumably normal horses may have dramatic differences in sacroiliac joint shape.41 Linear tomography was used to examine the lumbosacral and sacroiliac regions of horses, but limited access to equipment has restricted its clinical usefulness.15 Positive findings include widening of the sacroiliac joint and irregular joint outlines, with osteophyte formation at the caudal aspect of the joint. Osseous changes are common bilaterally, but they may be more pronounced on the clinically more affected side.15
Nuclear scintigraphy is considered by some authors to be an accurate and diagnostically useful technique for identifying acute and chronic sacroiliac joint injuries. However, ilial wing and soft tissue attenuation (from 71% to 82%), large distance between the ilial wing and camera face, horse movement, and background activity severely compromise the pelvic scintigraphic image, and only dramatic radiopharmaceutical uptake (RU) can be reliably detected.42,43 In addition, large variations exist in RU in both affected and unaffected horses. Young horses have well-defined tubera sacrale and relatively less RU in the adjacent regions of the sacroiliac joints.44 Older horses and horses with sacroiliac joint pathology have less distinct differences in RU between the tubera sacrale and the sacroiliac joints.19 Subjective evaluation or quantitative analysis of bone scans typically is able to identify asymmetric RU over the affected tuber sacrale or wing of the ilium in the region of the sacroiliac joint. However, presumed normal horses, without a history of hindlimb or sacroiliac joint injuries, may have mild asymmetric RU over the tubera sacrale and sacroiliac joint regions.19 Non–motion-corrected scintigraphic images are often not of diagnostic quality and can be misinterpreted as abnormal.44 Motion-corrected images are much more likely to give accurate diagnostic information. A dorsal image of the sacrum is considered the most diagnostic image for evaluating and comparing the sacroiliac joints.18 However, RU in the relatively superficial tubera sacrale may mask RU in the sacroiliac joints in a dorsal image. Oblique images of the ilial wings are recommended to confirm left to right asymmetries in RU, especially when identifying stress fractures, and to separate the tuber sacrale dorsally from the sacroiliac joint region ventrally.45 However, oblique images may be difficult to interpret because of inconsistent camera positioning on the left and right sides. The thick overlying gluteal musculature may also attenuate RU from an affected sacroiliac joint.43 Any left-right asymmetry in gluteal muscle mass will produce a false-positive interpretation of RU on the side with the atrophic or reduced muscle mass.42 Stress fractures of the ilial wing may be difficult to differentiate from sacroiliac joint injuries because of the common location and extension of the incomplete fracture line into the sacroiliac joint.18,27,46 Increased RU (IRU) within the pelvis does not necessarily indicate a primary cause of pain.47 A compensatory response within the osseous pelvis, insufficient pelvic pain to cause lameness, and other sources of lameness that cause more discomfort than the pelvic lesion associated with the area of IRU may all cause disassociation between a positive scintigraphic finding and the primary source of pain. Nuclear scintigraphy should also include the caudal thoracolumbar spine to rule out concurrent pathology, such as impinging dorsal spinous processes.19
Thermography is used to diagnose muscle strain or inflammation in the sacroiliac and croup regions. Horses with sacroiliac joint injuries are expected to have protective muscle spasms in the adjacent musculature. Palpation of muscle sensitivity has been correlated with abnormal thermographic images in most horses.48 Thermographic imaging of horses with sacroiliac injuries demonstrates a change in the normal temperature pattern over the croup, with increased temperature associated with acute desmitis and decreased temperature over the sacroiliac area on the affected side in horses with chronic sacroiliac injury.38 In the Editors’ experience thermography may be helpful in the identification of acute desmitis of the dorsal sacroiliac ligament, but is usually of no value in the assessment of horses with chronic sacroiliac joint region pain. All diagnostic imaging modalities need to be carefully evaluated with respect to clinical signs exhibited by the individual horse.19,49
Differential Diagnosis
Causes of sacroiliac joint pain or injury were postulated to result from sacroiliac or lumbosacral arthrosis, sacroiliac desmitis or sprain, sacroiliac subluxation or luxation, pelvic stress fractures, complete ilial wing fractures, or sacral fractures.32 Additional differential diagnoses include aortoiliac thromboembolism, exertional rhabdomyolysis, trochanteric bursitis, and impinged dorsal spinous processes in the lumbar vertebrae.25 Horses with presumed thoracolumbar vertebral problems may also have concurrent chronic sacroiliac joint injuries. In a report on 443 horses with back problems, chronic sacroiliac joint problems were identified in 15%.11 Clinical signs of lower hindlimb lameness may overlap and mimic signs of presumed pathological conditions of the sacroiliac joint. It is important that a thorough and complete lower limb lameness evaluation is completed before, or along with, an upper hindlimb or sacroiliac joint workup.
Based on a review of the literature, OA of the sacroiliac joint is the most prevalent disease process affecting horses with sacroiliac joint pain or dysfunction.1,4,11,17 Sacroiliac desmitis was documented in horses and may be an important cause of pathological conditions in horses with acute sacroiliac joint injuries.9 Documented complete rupture of the sacroiliac ligaments was only reported in a few horses with acute and chronic disease.17,24 The presumed diagnosis of sacroiliac joint subluxation based solely on tubera sacrale height asymmetry is inappropriate.31 Horses with chronic sacroiliac problems and presumed sacroiliac joint subluxation have not had identifiable changes in the sacroiliac ligaments at necropsy.4 In addition, STB trotters with substantial tubera sacrale height asymmetries did not have significant increases in sacroiliac pain compared with horses with lesser degrees of asymmetry.16 In my opinion, an antemortem diagnosis of sacroiliac joint luxation can only be supported if an acute change in tubera sacrale height caused by substantial trauma has been documented or if sacroiliac joint instability (i.e., crepitus or independent tubera sacrale movement) is evident during physical examination. Pelvic stress fractures should be ruled out in horses with sacroiliac pain or dysfunction.50 A high prevalence of occult pelvic stress fractures was reported in TB racehorses.46 The incomplete fracture lines extend into the caudomedial aspect of the sacroiliac joint, which could possibly produce concurrent sacroiliac joint inflammation and OA. A diagnosis of sacroiliac joint injury is often based on a diagnosis of exclusion because of difficulties in clinical evaluation and diagnostic imaging. We are hopeful future investigations into sacroiliac joint problems in horses will produce a better and more comprehensive understanding of this often misdiagnosed clinical entity.
Treatment
Because definitive diagnosis of pathological conditions of the sacroiliac joint is difficult, treatment recommendations are usually symptomatic. Few studies on treatment efficacy have been reported in the equine literature. In people, analgesics, antiinflammatories, intraarticular and periarticular injections of corticosteroids, and prolotherapy (i.e., injection of sclerosing agents) were advocated as sole treatments for sacroiliac joint dysfunction. However, effective treatment and long-term rehabilitation of sacroiliac joint injuries often rely on the development of specific physical therapy and training programs that stimulate neuromotor and biomechanical restoration of articular, muscular, fascial, and ligamentous function.30 In general, rest and various forms of physical therapy are indicated for horses with ligamentous injuries. Prolonged rest (6 to 12 months) and systemic antiinflammatory medications are prescribed for horses with acute and chronic sacroiliac joint injuries. Complete box stall rest for 30 to 45 days was recommended to support ligamentous healing in horses with acute injuries.25 The local injection of irritants or sclerosing agents was suggested to stimulate fibrosis and subsequent sacroiliac joint stability.25 In my opinion, no scientific support or clinical indication exists for such proposed treatments of back or sacroiliac joint problems. With such haphazard and potentially injurious treatment modalities there appears to be a better chance of inducing further injury rather than of stimulating any healing response. Treatment of horses with chronic sacroiliac joint injury typically focuses on a gradual return to a low level of exercise to maintain muscle development of the back and gluteal regions to counteract the clinical signs of poor performance and reduced hindlimb impulsion.29 Extended rest is contraindicated because reduced muscle tone may exacerbate the injury.
Because of the deep and inaccessible location of the sacroiliac joint, intraarticular injections of local anesthetic solutions or antiinflammatory medications for diagnostic or therapeutic purposes are impractical.18 However, local perfusion of the sacroiliac joint with local anesthetic solutions or antiinflammatory drugs for diagnostic and therapeutic purposes is a viable alternative.32 Concurrent lameness of the ipsilateral lower hindlimb was reported in horses with signs of chronic sacroiliac joint injuries.18 Therefore a detailed lameness examination coupled with appropriate treatment of the pathological conditions of the lower hindlimb is often indicated. Additional factors such as corrective shoeing and modifications in exercise or training programs need to be addressed concurrently. Acupuncture and chiropractic are nontraditional approaches that are used by some clinicians to assist in the diagnosis and symptomatic treatment of horses with presumed sacroiliac joint problems. Efficacy of modalities needs to be confirmed before further recommendations can be made.
Prognosis
Long-term follow-up evaluation suggests that prognosis for horses with sacroiliac joint injury is poor for return to the previous level of activity.18 Some horses may have an improvement in performance or lameness but will not be able to return to normal athletic activities because of recurring, low-grade lameness. Most horses will be pasture sound or able to function only at low levels of exercise. We hope that improvements in providing a specific diagnosis of the type of sacroiliac joint injury present will provide affected horses with better and more specific treatment options in the future.