Chapter 85Analgesia and Hindlimb Lameness
The benefits to providing analgesia for both acute and chronic pain are well established in many species. Inadequate treatment of pain can result in inappetence and weight loss, increases in serum cortisol and catecholamines, tachycardia, hypertension, and compromise of the immune system.1 Increases in serum cortisol and catecholamines can cause derangements in serum glucose, protein metabolism, and immune function. In addition, horses with a painful limb may remain recumbent for prolonged periods, with resultant decubital ulcer formation and secondary infection.
Epidural Analgesia
Designing an appropriate plan for analgesia in a horse, particularly for those with severe, chronic pain, can be challenging. Parenterally administered opioids and α2-adrenergic agonists may be associated with side effects such as ataxia, excitement, and adverse effects on the gastrointestinal and cardiovascular systems. Nonsteroidal antiinflammatory drugs (NSAIDs) can cause gastrointestinal ulceration or renal disease, and they may be inadequate for horses with acute, intense pain. Epidural administration of drugs provides more localized analgesia and fewer systemic effects than parenteral administration.
Epidural drug administration places a drug in close proximity to its site of action within the spinal cord or the spinal nerves as they exit the spinal cord. A greater analgesic effect may be achieved with a smaller total dose of a drug. The duration of analgesia is usually longer than with parenteral administration. Pain that is related to a disease process of a hindlimb is particularly amenable to treatment with epidural analgesia. The site of injection for epidural drug administration in horses is usually the first coccygeal (caudal) interspace. When deposited into the epidural space, the drug diffuses across the meninges, into the cerebrospinal fluid (CSF), and then into the spinal cord. The degree of cephalad diffusion of the drug within the CSF depends on several factors, including the volume of the drug injected, concentration of the drug, and lipid solubility.2 Although studies in dogs and people have reported analgesic effects with epidural morphine or α2-agonists that extend to the midthoracic area or farther cranially,3,4 this is generally not the case in horses.5-8 This limits the use of epidural analgesia in horses to the treatment of hindlimb pain.
Technique for Epidural Administration
Caudal epidural drug administration can be done by single injection at the first coccygeal interspace or by placement of an epidural catheter at this same site for repeated drug administration. The lumbosacral space is also a potential site of injection, and its use may result in a more rapid onset of hindlimb analgesia. However, positioning the tip of the needle within the epidural space rather than the subarachnoid space can be difficult. Subarachnoid administration of drugs in the horse is certainly acceptable, but the dose should be reduced by 40% to 50%.
The first coccygeal interspace (between the first and second coccygeal vertebrae) is identified while raising and lowering the tail and palpating for the articulation between these two vertebrae. This space is just caudal to the most angular portion of the bend of the tail, about 5 cm cranial to the first long tail hairs (Figure 85-1). The site should be prepared aseptically. Administration of 2 to 3 mL of 2% lidocaine subcutaneously using a 25-gauge needle helps decrease the response of the horse to placement of the needle for epidural injection. An 18- or 20-gauge, 6.35-cm spinal needle with stylet is recommended for epidural injection in horses, although many clinicians use a standard 18-gauge needle. The bevel of a spinal needle is not as sharp as that of a standard needle and the bevel angle is less acute. This design makes it easier to identify penetration through the interarcuate ligament and the subsequent loss of resistance as the epidural space is entered. The needle is inserted at a 30- to 60-degree angle to horizontal, with the tip pointed cranioventrally, and is advanced until it contacts the floor of the vertebral canal (Figure 85-2). The depth of insertion is 3 to 6 cm, depending on the size of the horse and the angle of the needle. The needle placement can be tested by attempting to inject 2 to 3 mL of air or solution in a 3-mL syringe. Resistance to injection should be little or absent. Appropriate epidural injection of local anesthetic solution and xylazine often is confirmed when anal tone decreases and the tail relaxes, but because the drugs most commonly used for epidural analgesia of the hindlimb (morphine, detomidine) have little or no effect on motor nerves, these responses will be absent.

Fig. 85-1 The first coccygeal interspace between the first and second coccygeal vertebrae is identified while the clinician raises and lowers the tail and palpates for the articulation between these two vertebrae. This space is just caudal to the most angular portion of the bend of the tail.
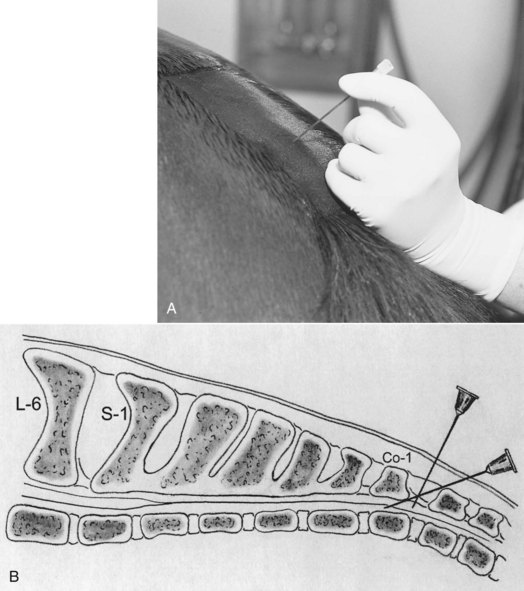
Fig. 85-2 A, The needle is inserted at a 30- to 60-degree angle to horizontal and is advanced until it contacts the floor of the vertebral canal. B, Sagittal view of the sacral vertebrae and placement of the needle within the epidural space. Co-1, First coccygeal vertebra; L-6, sixth lumbar vertebra; S-1, first sacral vertebra.
Epidural Catheter Placement
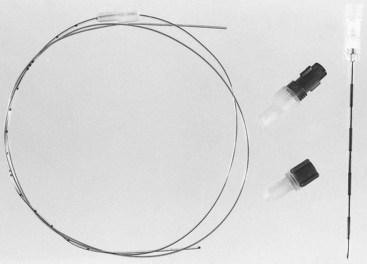
The site for insertion of an epidural catheter is the same as for a single epidural injection. Placement of the catheter requires the use of a needle with a curved point (Tuohy, Becton, Dickinson, Franklin Lakes, New Jersey, United States) that will direct the catheter cranially, along the floor of the vertebral canal (Figure 85-3). The epidural catheter is made of polyamide (nylon) or Teflon, with a closed or open end, and it can be purchased with a wire stylet if desired. I use an 18-gauge, 8.89-cm Tuohy needle and a 20-gauge, 100-cm radiodense, polyamide catheter with a closed tip (bullet tip) without a stylet (Figure 85-4). Epidural catheters have marks every centimeter and multiple marks at 10, 15, and 20 cm from the end. Before needle and catheter placement, slide the catheter inside the needle and note the distance from the tip of the needle to the hub on the catheter. The clinician then should determine which mark on the catheter will be at the hub of the needle once the catheter has been advanced to the desired position.
As with the single epidural injections, strict attention should be paid to aseptic technique, and sterile gloves must be worn. Lidocaine is injected into the subcutaneous tissues at the desired site. A small incision is made through the skin with a No. 11 scalpel, because the Tuohy needle has a blunt tip. Once the needle has been positioned, the bevel should be directed cranially (the notch on the hub of the needle should face cranially). The catheter is threaded through the needle and along the floor of the vertebral canal (Figure 85-5). Provided the needle is positioned in the epidural space, the advancing catheter receives little resistance. If the tip of the needle is angled incorrectly, the catheter tends to bump up against the vertebrae and will not advance. If this occurs, the needle is withdrawn 1 to 2 mm and the catheter is rotated slightly as it is advanced. It is critical that once the catheter has advanced any distance outside of the needle, it never be withdrawn back into the needle. This may result in cutting or shearing off of the catheter. The catheter is advanced 5 to 10 cm past the tip of the needle, and the tip is positioned in the midsacral region. Once the catheter has been positioned, the needle is carefully withdrawn over the catheter and removed (Figure 85-6). Most epidural catheters intended for human use are very long to facilitate positioning of the injection port in a convenient place on the body. I usually cut the catheter with a scalpel (scissors tend to crush the catheter), leaving about 10 cm of the catheter to secure to the horse. The catheter or syringe adapter is attached, and an injection cap is secured to the adapter. A portion of tape is secured to the catheter at the point of insertion and then sutured to the skin (Figure 85-7). The syringe adapter also should be sutured to the skin, making sure tension will be minimal on the catheter during any movement of the horse. The catheter and injection cap then are covered with a sheer, adhesive dressing. Each injection into the catheter is made through the catheter cap after thoroughly cleaning it with alcohol, while wearing sterile gloves. It is critical that the catheter system remains sterile. A bacterial filter can be inserted between the syringe adapter and the catheter cap as an added precaution. The catheter site should be examined daily for signs of inflammation or infection, which would necessitate removing the catheter and submitting the tip for culture. With diligent aseptic technique and catheter care, I have kept catheters in place for 2 weeks in horses, and some researchers have reported epidural catheters being maintained for 5 weeks in research horses.9
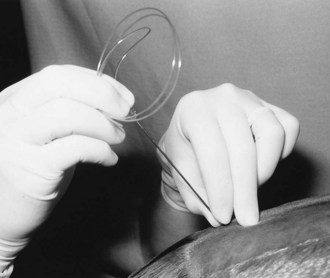
Fig. 85-5 The epidural catheter is threaded through the needle and along the floor of the vertebral canal. If the catheter will not advance, the needle is withdrawn 1 to 2 mm, and the tip of the needle is angled up slightly.
Drug Selection
Epidural Opioids
The primary advantage of epidural administration of an opioid is the intense and prolonged, segmental (localized) analgesia achieved without either sedation or the possible excitement that may accompany the parenteral administration of an opioid. Unlike epidural local anesthetic solutions or xylazine, epidural opioids do not affect neuromuscular function or the sympathetic nerves.
The analgesia obtained with epidural opioids is primarily from the effect of the opioid within the spinal cord rather than from a supraspinal location. Opioids bind to presynaptic receptors of the afferent nerve terminals in the dorsal horn and inhibit the release of excitatory neurotransmitters such as glutamate and substance P. Opioids also act postsynaptically to inhibit transmission of impulses in ascending tracts. Evidence also shows that opioids enhance the effects of descending inhibitory pathways on the processing of pain within the dorsal horn.10
The onset and duration of action of epidural opioids vary greatly among drugs. The time to onset of analgesia reflects the time required for a drug to diffuse from the epidural space, across the meninges, into the spinal fluid, and ultimately into the spinal cord. Physicochemical properties of the drug, such as molecular weight, molecular shape, degree of ionization, and particularly lipid solubility influence the diffusion across the meninges.3,11 The more lipid-soluble drugs, such as fentanyl and butorphanol, have a rapid onset but a shorter duration of action, whereas the more water-soluble drug, morphine, has a delayed onset and a very long duration of action (Table 85-1).3 This delay in onset of analgesia with morphine can be particularly long in horses, and the drug may not reach peak effect for several hours.12 The more water-soluble opioids also tend to have greater degree of cranial diffusion within the CSF.2
TABLE 85-1 Characteristics of Analgesia and Side-Effects after Epidural Administration of Various Drugs
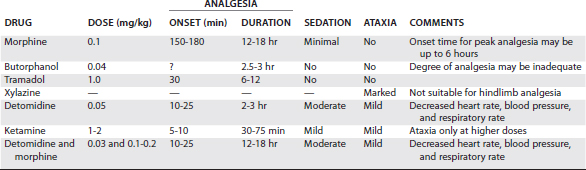
Morphine remains the opioid of choice even though numerous other opioids have been evaluated for epidural analgesia in horses (see Table 85-1).5-7,13-15 Fentanyl has a faster onset of action but a considerably shorter duration of action (4 to 6 hours). Butorphanol provides inadequate analgesia. Analgesia after epidural administration of hydromorphone and methadone has been described in research horses.15 The onset of analgesia is more rapid than with morphine, and the duration of analgesia in the lumbar and sacral regions is approximately 4 hours. There may be benefit to using a drug with a more rapid onset, particularly in horses with an epidural catheter, which can facilitate more frequent administration. The utility of these drugs in horses with hindlimb pain remains to be evaluated.
I use preservative-free morphine (Abbott Laboratories, North Chicago, Illinois, United States) that is intended for epidural use at a dose of 0.1 mg/kg. The disadvantage of this preparation is the volume required. There are parenteral preparations of morphine that have been used for epidural administration in horses in an attempt to lower the cost, but some of these may contain substances such as phenol or formaldehyde, which may be neurotoxic. A preparation of morphine (25 mg/mL) with sodium bisulfite as an antioxidant (morphine sulfate, Hospira, Lake Forest, Illinois, United States) has been used in the horse epidurally, but the dose to be administered should be diluted in 20 mL of sterile saline solution. Epidural morphine has been used at a dose of up to 0.2 mg/kg combined with epidural detomidine.16,17 The higher dose may potentially speed the onset of action and extend the drug’s duration, but it may increase the incidence of side effects.
Potential side effects include respiratory depression, pruritus,18 and urinary retention. These are rarely seen in horses and can be treated with naloxone (0.005 to 0.01 mg/kg). I have experience with a horse that developed substantial central nervous system effects after administration of morphine (0.2 mg/kg in 50 mL of saline solution), resulting in collapse, tachypnea, muscle rigidity, and hypoxemia. The horse was treated with naloxone (0.01 mg/kg), furosemide (2 mg/kg), diazepam (0.01 mg/kg), and a neuromuscular blocker to facilitate positive-pressure ventilation after intubation and anesthesia with isoflurane. The horse recovered.
Epidural α2-Adrenergic Agonists
Epidural administration of an α2-adrenergic agonist can induce profound analgesia mediated by α2-adrenergic receptors in the spinal cord.19 The exact mechanism for the analgesia is not known. However, the α2-adrenergic agonists traditionally were thought to induce analgesia by mimicking action of norepinephrine released from descending noradrenergic inhibitory pathways.20 Additional proposed mechanisms of action include modulation of pain via serotonergic and adenosinergic pathways, inhibition of the release of substance P, and effects on opiate receptors.21,22
Xylazine, an α1- and α2-receptor agonist, is commonly used to induce analgesia of the perineal area of horses.23 However, xylazine is not suitable for severe hindlimb lameness because of its effects on somatic motor innervation.8 Doses that exceed 0.25 mg/kg can cause substantial ataxia and have the potential to cause temporary hindlimb paralysis. Detomidine is a more selective α2-adrenergic agonist that primarily affects nerve fibers involved in pain transmission (C fibers and A delta fibers) and appears to have limited effect on somatic motor function at clinically used doses. Detomidine is therefore less likely to cause motor dysfunction and hindlimb paralysis, making it more appropriate for the treatment of horses with hindlimb pain. However, detomidine has a relatively short duration of action (see Table 85-1) and also has systemic effects, such as decreased blood pressure and heart and respiratory rates. Detomidine is best used with morphine and can provide additional analgesia. I use a combination of morphine (0.1 mg/kg) and detomidine (30 mcg/kg).
Other Drugs for Epidural Analgesia
Ketamine is an N-methyl-d-aspartate (NMDA) receptor antagonist that can be effective for pain resulting from central sensitization in the spinal cord and hyperalgesia caused by continuous nociceptive input from damaged tissue. Epidural ketamine has been administered to people and animals for treatment of acute and neuropathic pain with mixed results. Research horses given 1 mg of ketamine per kilogram epidurally had reduced postincisional pain (flank incision) for several hours and demonstrated no signs of ataxia or sedation.24 Epidural ketamine may be a suitable adjunct to other forms of analgesia, particularly in horses with inadequate analgesia from epidural morphine.
Tramadol is a centrally acting analgesic with effect on opiate, adrenergic, and serotonergic receptor systems. Tramadol (1.0 mg/kg) administered as a caudal epidural analgesic to horses induces analgesia, beginning at 20 minutes, that lasts approximately 6 hours in the sacral region and 5 hours in the lumbar and thoracic regions, with the analgesia in the more cranial regions being less intense.12 The duration of this analgesia is slightly shorter than that of epidurally administered morphine, with a faster onset of action.
Clinical Applications
Epidural analgesia can make a profound difference in the comfort and convalescence of horses and is frequently used in conjunction with other forms of analgesia, such as NSAIDs. Epidural analgesia is often used during the first stages of recovery from various disease processes, when the pain may be more intense, or immediately before or after surgical treatment of hindlimb injuries or disease. Procedures such as fracture repair and arthrodesis can cause pain intraoperatively and postoperatively. Preoperative administration of epidural opioids can decrease the concentration of inhalation anesthetic required, and some evidence shows that preoperative administration of epidural opioids is effective preemptive analgesia. Evidence also shows that effective preemptive analgesia can make postoperative pain management more successful. Because the onset of action of epidural morphine is prolonged in horses, administration of the drug 1 to 3 hours before induction of general anesthesia may be necessary to achieve the greatest effect postoperatively. A clinical impression exists that horses treated with epidural morphine have longer recovery times. My own impression is that recovery might be slightly prolonged, but not dangerously so, and that the horses are far more comfortable in the immediate postoperative period. Epidural administration of morphine provides analgesia that is far superior to what can be achieved with NSAIDs and parenterally administered opioid agonist-antagonists, such as butorphanol, without substantial systemic effects.
Horses with trauma to a hindlimb that require long-term therapy may benefit from the placement of an epidural catheter. I have left catheters in place for 1 to 2 weeks in some horses and as of yet have seen no complications attributable to the catheter. In some horses, however, the analgesia seems gradually to become less effective, despite increases in the dose and frequency of administration of epidural morphine. The addition of 30 mcg of epidural detomidine per kilogram every 6 to 8 hours has been beneficial in such horses. Ketamine,9 tramadol, or other α2-agonists, such as medetomidine, may have a role in treating horses with pain that is refractory to epidural morphine.
Contraindications and Complications
Complications associated with epidural analgesia can be grouped according to those caused by the drugs administered, those caused by the actual insertion of the needle or the catheter, and those secondary to the maintenance of an epidural catheter. Complications reported with epidural morphine are rare in horses. Detomidine may cause cardiopulmonary depression, sedation, and ataxia. Careful assessment of the horse’s cardiovascular status and appropriate dosage of the drug can minimize the risks associated with epidural detomidine.
Introduction of the needle or catheter into the epidural space potentially can cause trauma to the spinal nerve roots or the epidural venous sinus. Substantial bleeding in horses with normal clotting times and platelet numbers is unlikely. The possibility exists that if the tip of the needle is in the venous sinus, the drug administration will be intravenous as opposed to epidural and will not have the desired effect of prolonged, segmental analgesia. I have also, on one occasion, inadvertently catheterized the epidural venous sinus. If blood is obtained after aspiration of the catheter, the catheter (and needle if still in place) should be removed and a new catheter placed.
Potential complications secondary to the maintenance of an epidural catheter include localized soft tissue inflammation and, rarely, epidural abscess, vertebral osteomyelitis, and meningitis. The catheter site should be inspected daily for signs of infection or inflammation. Technical problems with the epidural catheter (dislodgement, kinking) are more likely to result in early removal of the catheter than other complications.25
Possibly the most serious potential complication would be the inadvertent injection of an inappropriate substance or an overdose of the drug into the epidural catheter. The epidural catheter should be clearly marked as such, and all personnel working with that horse should be instructed in the care of the catheter and the amount and type of drugs that are administered through the catheter.
Novel Analgesic Drugs and Adjunctive Therapies
The transdermal route of drug administration can be used for opioid administration in horses. The transdermal therapeutic system for fentanyl administration is used in horses by applying patches to either the neck or the lateral aspect of the antebrachium.26,27 Two 10-mg patches (Duragesic 100 mcg/hr, Janssen Pharmaceutical, Titusville, New Jersey, United States) are generally used for adult horses. A pharmacokinetic study of transdermal fentanyl found that serum levels of fentanyl considered to be analgesic were present within 8 to 15 hours and were maintained for up to 32 hours. The application of fentanyl patches in conjunction with NSAIDs in horses with pain from soft tissue and orthopedic disease resulted in decreased overall pain scores, but improvement in the horses with orthopedic disease was minimal and lameness scores did not change.27 My experience with transdermal fentanyl in horses is similar. Clinical signs in horses with soft tissue injuries and abdominal pain may improve, but the analgesic benefit in horses with acute or substantial orthopedic pain is questionable.
Subanesthetic doses of intravenous ketamine have been used to provide analgesia in small animals and people. A constant rate infusion of as low as 0.4 mg/kg/hr in horses results in plasma levels of ketamine above those needed to provide analgesia in people, and doses of 1.2 mg/kg/hr were analgesic in research horses with minimal changes in behavior.28,29 The efficacy of low-dose constant infusions of ketamine in painful horses is yet to be determined. I have used low-dose ketamine (0.3 mg/kg bolus and 1 mg/kg/hr) in a limited number of horses that were in pain despite opioid therapy, and horses appeared to show modest to marked improvement.
Other adjunctive analgesic agents used in veterinary medicine include the anticonvulsant gabapentin (Neurontin, Pfizer, New York, United States). The proposed analgesic mechanism is mediated by binding to a presynaptic voltage-gated calcium channel in the dorsal root ganglia and spinal cord, which inhibits calcium influx and subsequent release of excitatory neurotransmitters.30 Gabapentin has become an established therapy in some types of neuropathic pain, and its use for acute, perioperative pain is being investigated. Limited pharmacokinetic data in horses have revealed maximal plasma levels that were lower than those in people and dogs given a similar dose.31 There is a single case report of a mare with femoral neuropathy that was given 2.5 mg/kg of gabapentin every 8 hours. The authors concluded that gabapentin appeared to be an effective treatment for neuropathic pain in that horse.32 My only experience with gabapentin is in dogs with severe neuropathic or chronic pain, with responses varying from excellent to poor. One of the Editors (SJD) has treated several horses with suspected neuropathic pain with complete remission of clinical signs; however, horses with severe, chronic pain associated with laminitis have shown only limited improvement.