CHAPTER 50 Wrist and hand
SKIN AND SOFT TISSUE
SKIN
Dorsal skin versus palmar skin
The skin over the dorsum of the hand is thin and mobile and this allows for flexion at the metacarpophalangeal and interphalangeal joints. The dorsal skin is frequently hirsute over the dorsal aspect of the proximal phalanges and the ulnar aspect of the dorsum of the hand. In comparison, the palm is adapted for padding and anchorage. The palmar skin and the skin over the volar surface of the digits is thick and hairless, and has a well-defined stratum lucidum, a higher density of nerve endings, and eccrine sweat glands, but no sebaceous glands.
Skin creases and fingerprints
Flexure lines commonly crease the skin across the flexor surfaces of the wrist and hand (Fig. 50.1). Though not all directly over their functionally related subjacent skeletal joints, they are produced by adhesion of the skin to subjacent deep fascia and are sites of folding of the skin during movement. These flexures are useful landmarks. Less regular, but quite prominent, crease-line complexes are centred over the dorsal (extensor) aspects of the radiocarpal, carpal, metacarpophalangeal and interphalangeal joints. They are mainly transverse but display varying curvatures. During flexion the dorsal skin is stretched and the lines become less prominent (but can still be identified). During extension the now redundant skin becomes increasingly puckered and the lines are finally maximally prominent. (For a general review of ‘skin lines’ see p. 160.)
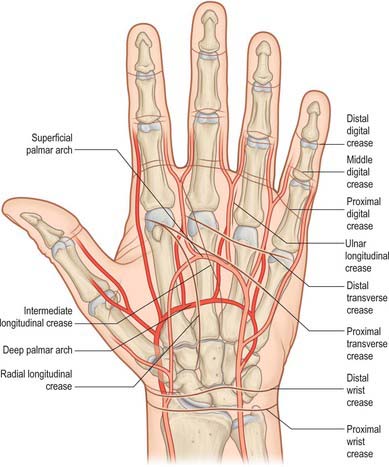
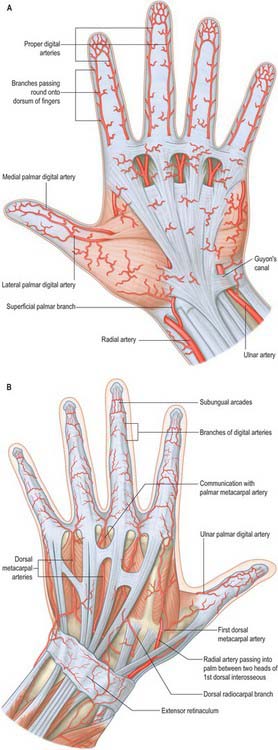
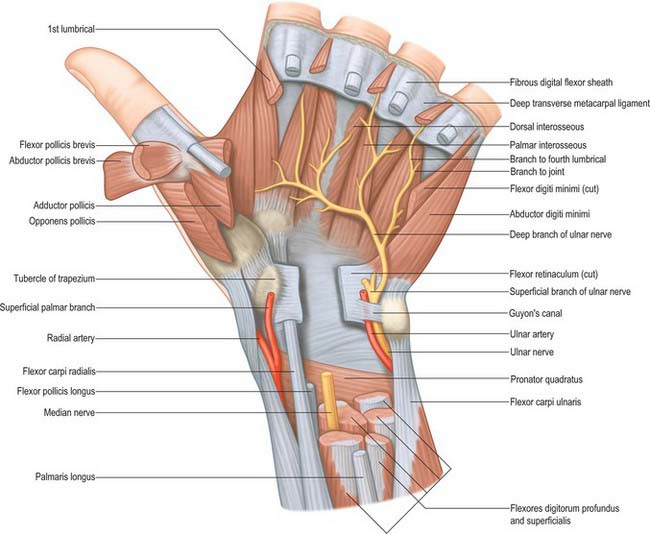
Fig. 50.1 Relation of the skin flexure lines and palmar arterial arches to the bones of the left hand.
(Adapted from Drake, Vogl and Mitchell 2005.)
Near the junction of the carpus and forearm there are usually three anterior transverse lines. The proximal marks the proximal limit of the flexor synovial sheaths, an intermediate line overlies the wrist joint, and a distal line is at the proximal border of the flexor retinaculum.
In the palm a curved radial longitudinal line encircles the thenar eminence, ending at the radial (lateral) margin of the palm. Several less constant longitudinal lines lie medial and roughly parallel to it. Proximal and distal transverse lines ascend medially across the palm. The proximal line begins at the distal end of the radial longitudinal line and runs obliquely to the middle of the hypothenar eminence across the shafts of the metacarpals. The distal line begins at or near the cleft between the index and middle finger and crosses the palm with a proximal convexity over the second to fourth metacarpal heads, near the proximal ends of the fibrous flexor sheaths.
The second to fifth digits show proximal, middle and distal sets of transverse lines. The proximal, often double, are at the digital roots, approximately 2 cm distal to the metacarpophalangeal joints. The middle lines are typically double, the proximal line lying directly over the proximal interphalangeal joint. The distal lines are usually single, and lie proximal to the distal interphalangeal joints: their levels are sometimes marked by a fainter, more distal line. The free pollicial base is partly encircled by a line which starts on the radial side and crosses distally over the metacarpophalangeal joint to end between the thumb and index finger level with the base of the proximal pollicial phalanx. There is a second, shorter crease usually 1 cm distal to this line. There are two lines comparable to the middle digital lines in other digits opposite the interphalangeal joint of the thumb (see also p. 160).
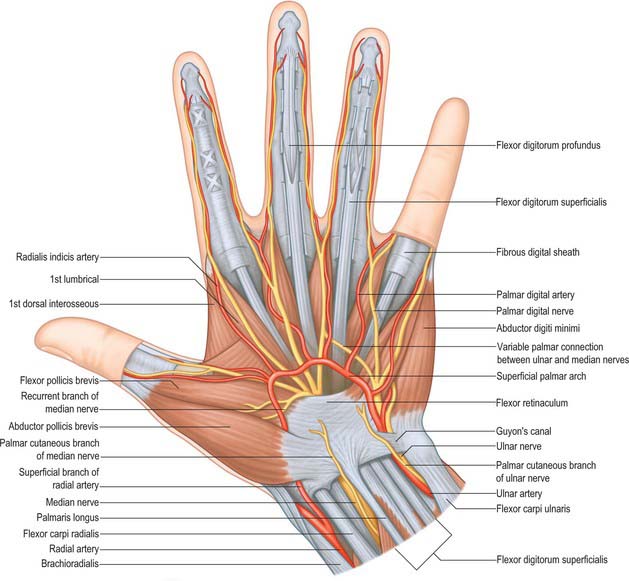
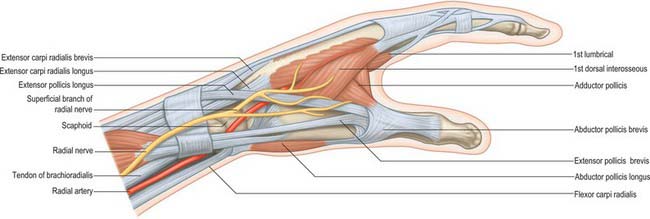
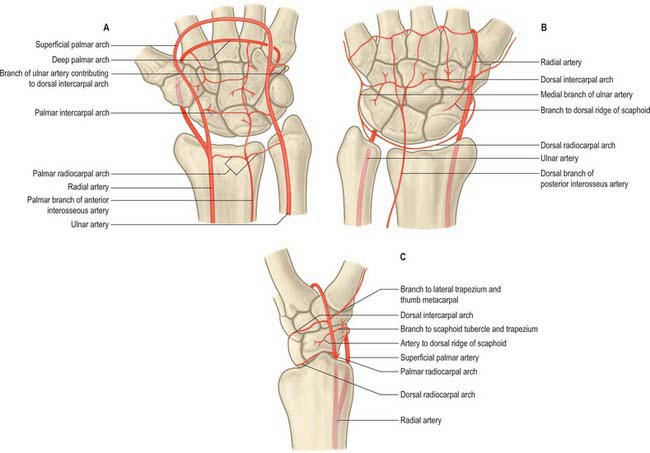
Cutaneous vascular supply
The skin of the volar aspect of the wrist is supplied directly by cutaneous branches from the superficial palmar branch of the radial artery, the ulnar artery and occasionally the median artery if it is large enough (Fig. 50.2). The skin over the thenar eminence is supplied by small perforating branches from the superficial palmar branch of the radial artery and the princeps pollicis. The skin over the hypothenar eminence is supplied by perforating branches from the ulnar artery, some of which pass through palmaris brevis. The remainder of the palm is supplied by small perforating branches from the common palmar digital arteries which pierce the palmar aponeurosis, and small branches from the radialis indicis artery. The blood supply to the volar aspect of the digital skin comes from small branches from each digital artery. At the level of the distal phalanx the two digital arteries typically form an H-shaped anastomosis from which cutaneous perforators fan out within the pulp. Deep digital veins accompanying the digital arteries are usually very small and frequently absent. More commonly, superficial palmar veins tend to pass dorsally and drain into the larger superficial dorsal venous system.
The skin of the dorsal aspect of the wrist is supplied by branches from a plexus overlying the extensor retinaculum. Branches from the radial artery, including its dorsal carpal branch, dorsal carpal branch of the ulnar artery, and anterior and posterior interosseous arteries all contribute to this plexus. The blood supply to the dorsum of the hand arises from longitudinal rows of four or five tiny branches from each of the dorsal metacarpal arteries, which usually arise either from the radial artery directly or the dorsal carpal arch. At the level of the neck of the metacarpals, where the second, third and fourth dorsal metacarpal arteries communicate with branches from the corresponding common palmar digital arteries, a large cutaneous perforating branch passes proximally to supply an area of skin as far as the dorsal aspect of the wrist.
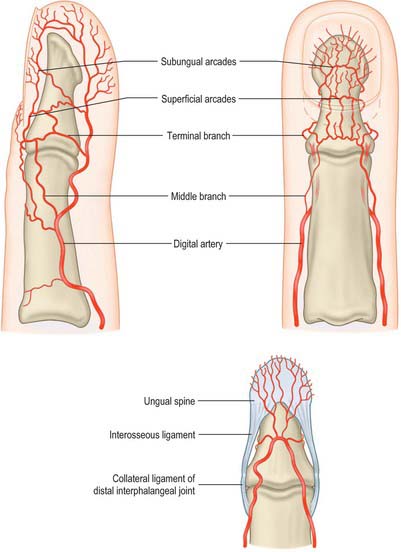
The blood supply to the dorsum of the fingers comes proximally from the terminal branches of the dorsal metacarpal arteries – supplying a region as far distally as the proximal interphalangeal joint – as well as from dorsal branches of the palmar digital arteries which are given off at each phalangeal level. At the level of the distal phalanx the cutaneous supply comes from three dorsal arcades: a superficial arcade over the base of the distal phalanx, and two distal subungual arcades. The skin of the dorsum of the thumb is supplied by longitudinal axial branches of the princeps pollicis and dorsal branches from the palmar digital arteries.
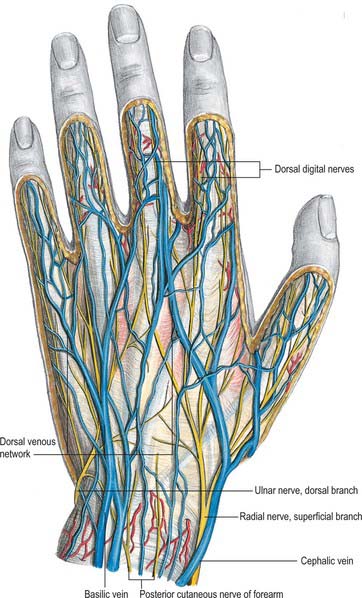
Cutaneous innervation
The skin of the volar aspect of the wrist is innervated by the terminal branches of the lateral and medial cutaneous nerves of the forearm. The skin of the palm is innervated by the palmar branches of the ulnar nerve and the palmar branch of the median nerve (Fig. 50.3; see also Fig. 50.45. The skin of the volar aspect of the thumb, index, middle and radial aspect of the ring fingers is supplied by cutaneous branches of the median nerve, while that of the little finger and ulnar side of the ring finger is supplied by the ulnar nerve.
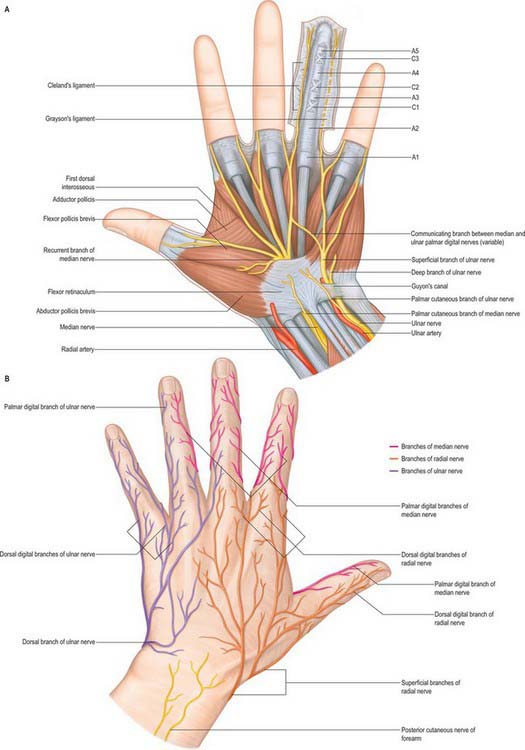
Fig. 50.45 Cutaneous nerves of the hand. A, Palmar aspect. The anular and cruciate pulleys are shown schematically in the ring finger. B, Dorsal aspect.
The cutaneous innervation of the radial aspect of the dorsum of the wrist and hand, as well as the dorsal aspect of the radial three and a half digits as far distally as the nail bed, arises from the terminal branches of the radial nerve, the dorsal digital nerves. Between two and five dorsal digital nerves supply each digit. The cutaneous innervation of the ulnar aspect of the dorsum of the wrist and hand, and the dorsal aspect of the ulnar one and a half digits as far distally as the nail bed, arises from the dorsal branch of the ulnar nerve, again ending as dorsal digital nerves. The skin of the dorsum of the middle and distal phalanges is also supplied by dorsal branches of the palmar digital nerves.
NAIL APPARATUS
The nail apparatus consists of the nail plate, proximal and lateral nail folds, nail matrix, nail bed and hyponychium. It is described on page 154.
SOFT TISSUE
Palmar fascial complex
The palmar fascia is a three-dimensional ligamentous system composed of longitudinal, transverse and vertical fibres (Fig. 50.4).
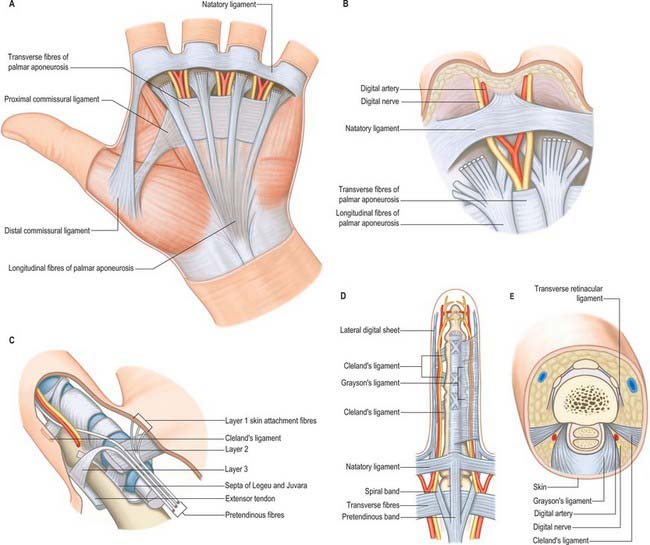
Fig. 50.4 Palmar aponeurosis and distal fascial complex. A, Schematic diagram of the palmar fascia. B, More detailed view of structures at the web space. C, Fate of the distal longitudinal fibres. D, E, Normal digital fascia.
Longitudinal fibre system
The longitudinal fibres represent the phylogenetically degenerated metacarpophalangeal joint flexor. They run distally from the palmaris longus tendon or the flexor retinaculum of the wrist across the whole width of the central third of the palm, producing four well-defined longitudinal bundles to the index, middle, ring and little fingers. A less well-defined bundle passes to the thumb. Distal to the transverse fibres of the palmar aponeurosis the longitudinal fibres pass in three layers (McGrouther 1982). The most superficial longitudinal fibres (layer 1) are inserted superficially into the skin of the distal palm between the distal palmar crease and the proximal digital crease. Some superficial fibres pass distally into the palmar midline of the digit. Deeper longitudinal fibres (layer 2) pass deep to the natatory ligament and neurovascular bundles into the apex of the web space skin and into the fingers themselves where they are continuous with Cleland’s ligaments and the lateral digital sheet. These are known as the spiral bands of Gosset. Deeper still, the longitudinal fibres in layer 3 perforate the deep transverse metacarpal ligament to pass around the sides of the metacarpophalangeal joint and attach to the metacarpal bone and proximal phalanx, and extensor tendon.
Transverse fibre system
The transverse fibre system consists of the natatory ligament (also known as superficial transverse metacarpal ligament), the transverse fibres of the palmar aponeurosis (also known as fibres of Skoog), and the transverse metacarpal ligament (also known as the deep transverse metacarpal ligament).
Natatory ligament (superficial transverse metacarpal ligament)
The fibres of the natatory ligament (superficial transverse metacarpal ligament) cross the apex of the web skin and extend into the digit to blend with the lateral digital sheet, thus limiting the spreading of the skin of the distal palm and the separation of the adjacent fingers. The natatory ligament in the first web is called the distal commissural ligament.
Transverse fibres of the palmar aponeurosis
The transverse fibres of the palmar aponeurosis (fibres of Skoog) lie more proximally than the natatory fibres and represent the deepest layer of the palmar fascia. They lie proximal to the distal palmar crease in a band approximately 2 cm wide, and connect the anterior fibres of the flexor tendon sheaths with one another and to the fasciae over the thenar and hypothenar muscles groups. The extension to the first ray is called the proximal commissural ligament.
Vertical fibre system
The vertical fibres are more delicate, and pass from the dermis, between the longitudinal and transverse fibres, to the fibrous flexor sheaths and the metacarpal bones. They are concentrated on either side of the palmar skin creases as well as the thenar and hypothenar eminences.
A series of vertical septa lie deep to the transverse fibres of the palmar aponeurosis, and connect it to the underlying deep transverse ligament. They provide compartments which contain the flexor tendons and the lumbricals and neurovascular bundles.
Dupuytren’s disease
Dupuytren’s disease (contracture) is a progressive condition of uncertain aetiology resulting from fibrous contracture of the palmar aponeurosis: the little and ring fingers are especially affected. Longitudinal thickening in the palm produces cords and thickened nodules which can progress to flexion deformities of the metacarpophalangeal and proximal interphalangeal joints of the affected fingers. The palmar aponeurosis only extends as far as the sides of the middle phalanx, therefore the distal interphalangeal joint is uncommonly involved. Indeed, in advanced cases, the distal interphalangeal joint can be hyperextended as the distal phalanx is pushed backwards against the palm.
The pattern of fascial involvement in this condition can be complex. For example, the normal anatomical position of the digital nerves and arteries may be distorted because they are often displaced medially. Since surgical treatment involves excising the affected area of palmar fascia, the digital nerves and arteries may be at risk in this procedure.
A similar contracture may affect the plantar fascia in the sole of the foot.
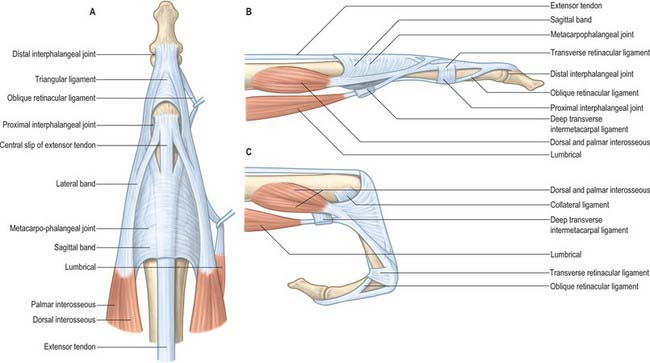
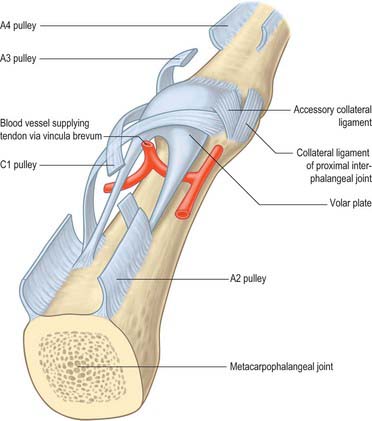
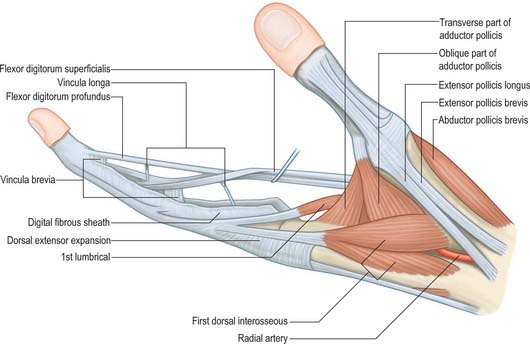
Digital fascial complex
The superficial fascia within the finger is fibrofatty in the palmar and dorsal aspects, but more sheet-like laterally, where it is termed the lateral digital sheet. Within the core of the finger the fascia is thickened in areas, forming the flexor sheath, Cleland’s, Grayson’s and Landsmeer’s ligaments (Fig. 50.4). The flexor sheath is discussed in detail on page 879. Cleland’s ligaments extend from the sides of the phalanges, pass dorsal to the neurovascular bundles and insert into the lateral digital sheet. Grayson’s ligaments are more delicate, may even be discontinuous and pass from the lateral sides of the phalanges volar to the neurovascular bundles to insert into the lateral digital sheet. Landsmeer’s ligaments are inconsistent anatomical structures made up of transverse and oblique retinacular ligaments (see Fig. 50.30). The transverse retinacular ligament passes from the A3 pulley of the fibrous flexor sheath at the level of the proximal interphalangeal joint to the lateral border of the lateral extensor band. The oblique retinacular ligament lies deep to the transverse retinacular ligament. It originates from the lateral aspect of the proximal phalanx and flexor sheath (A2 pulley) and passes volar to the axis of rotation of the proximal interphalangeal joint in a dorsal and distal direction to insert into the terminal extensor tendon.
Functions of the fascia of the hand
The fascial continuum of the hand performs a number of different, but inter-related, functions. It channels and provides a gliding surface for structures in transit between the forearm and the digits; transmits loads; anchors the skin; protects underlying vessels; and provides a framework for muscle attachments.
Channelling of structures in transit between forearm and digits
The vertical septa act as spacers between the tendons and neurovascular bundles of the individual digital rays. Where tendons change direction around a concave surface the channels are thickened. They perform a retinacular role, forming sheaths with specialized pulleys to prevent the tendon springing away from the underlying skeleton (see flexor tendon sheaths, p. 879).
Transmission of loads
At points where compressive loading is applied to the hand, such as the finger pulp and palm, loculi of fat act as shock absorbers. The loculi are contained within defined fibrous boundaries, which means that the shape, but not the volume, of each loculus can change. The compliance or deformability of the boundaries determines the amount of shock absorption. Local ‘turgor’ (deformability) and blood volume are measures of this anatomical property.
The palm also contains much larger fibrous compartments between skin and skeleton which transmit muscles, tendons and other structures. The honeycomb pattern of these compartments constitutes the palmar shock absorption system. The soft padded parts of the hand are able to conform to the contours of objects which are grasped, and this permits better interpretation of sensation and better grip.
The hand must also resist tensile loading. Tendons and ligaments are particularly suitable for resisting such forces but many other parts of the fascial continuum, e.g. the anchorage system of the palm, also play a major role in resisting ‘pulling’ forces.
Anchorage
Skin is retained by fascial ligaments which allow the hand to flex while retaining the skin in position. Skin folds at palmar and digital creases possess few deep-anchoring fibres. However, the skin on either side of the crease lines contains deep anchorage ligaments, and these allow the unanchored skin between them to fold in a repetitive pattern. The palmar creases have been described as skin ‘joints’. Fascial anchors may be vertical (perpendicular to the palm), e.g. in the midpalm where scattered vertical fibres run from the dermis down into the depths of the hand; horizontal (in the plane of the palm); or oblique to the skin surface.
The insertion of the longitudinal (pretendinous) fibres of the palmar aponeurosis is an example of a well-developed horizontal anchorage system. The most superficial longitudinal fibres insert into the dermis of the distal palm. This arrangement resists horizontal shearing force in gripping tasks, e.g. holding a golf club, where it prevents distal skin slippage or degloving of the palm on striking the golf ball. The characteristic blisters on the palms of those unaccustomed to such sports map out the sites of the skin anchorage points. This anchorage system can be demonstrated by flexing the palm until the skin of the distal palm folds loosely. An attempt to pull the loose skin distally will reveal the anchoring longitudinal fibres of the palmar aponeurosis.
Oblique anchors occur in the fingers where Cleland’s ligaments tether the skin of the proximal and middle segments of the digits to the region of the proximal interphalangeal joints.
Binding
Transversely orientated fascial structures help to maintain the transverse arch of the hand by ‘binding’ the underlying skeletal structures or the tendon sheaths.
Limiting or tethering
Joint motion is limited not only by joint ligamentous action, but also in some cases by skin tightness. Skin in the interdigital webs is generally reinforced by fascial ligamentous fibres which run just beneath the dermis in a direction which resists stretch: they are well developed in the thumb web.
Lubrication
There are many other gliding planes, e.g. between periosteum and the extensor apparatus, and between the latter and the skin, on the dorsum of the digits. The flexor tendon sheaths possess low friction and are lubricated by synovial fluid.
Vascular protection and pumping action
The blood vessels of the palm are surrounded by a cuff of tough fascia or by a fatty pad. When the hand is compressed, as in gripping, these relatively incompressible fascial structures function as a venous pumping mechanism to assist return of blood from the limb. In contrast, large capacitance veins on the dorsum of the hand lie in gliding skin, surrounded by loose areolar tissue, which allows venous dilatation.
Framework for muscle attachments
Many of the small muscles of the hand are attached to the fascial skeleton, at least in part, e.g. abductor pollicis brevis, palmaris longus. The fascial framework can be visualized as a harness by which muscles can act on the underlying skeleton, e.g. the metacarpophalangeal joint is moved by a ring of fascial and ligamentous structures that surround the joint and to which tendons are attached.
Digital and palmar spaces
There are many potential spaces within the hand, often with ill-defined margins.
The nail fold is a ‘U-shaped’ space made up of the eponychium and the lateral nail fold. The apical spaces at the tip of the finger are formed by the fibrous attachments of the distal phalanx to the tip of the digital pulp skin. The digital pulp spaces are confined compartments bounded by the digital creases which overlie the joints, and are attached to the underlying pulleys. The synovial flexor tendon sheaths are described on page 879. The web space is bounded distally by the skin and natatory ligament, by the deep transverse metacarpal ligament posteriorly, and by the deep attachments of the palmar fascia, together with their lateral attachments to the tendon sheaths proximally. The deep palmar space is a complex three-dimensional space limited proximally by the carpal tunnel. It lies deep to the palmar aponeurosis, between the radial and ulnar condensations of vertical fibres which connect the palmar aponeurosis to the thenar and hypothenar eminences. Partitions that pass deeply from the longitudinal bands of the palmar aponeurosis form eight narrow compartments: four contain the digital flexor tendons and four contain the lumbricals and the neurovascular bundles.
The spaces of the hand limit the spread of infection. Infections in the digit can occur in the nail fold (paronychia), the apical spaces at the very tip of the finger, the distal pulps (a felon) and the flexor sheaths. Anatomically, because the flexor synovial sheath of the thumb and the little finger are continuous throughout the palm, they have the potential to spread infection to the palm and so communicate with other sheaths within the carpal tunnel. Pus can certainly spread proximally within flexor tendon sheaths, but from a clinical point of view it is as disastrous in those digits whose sheaths do not communicate with the carpal tunnel sheaths (index, middle, ring) as it is in those that do (thumb, little finger). It is preferable, therefore, to know the structures rather than the potential spaces between them. Deep infections in the palm are usually not confined to any particular space.
BONE
The skeleton of the hand consists of the carpus, metacarpus and the phalanges. In the following description, proximal and distal are used in preference to superior and inferior, and palmar and dorsal, rather than anterior and posterior.
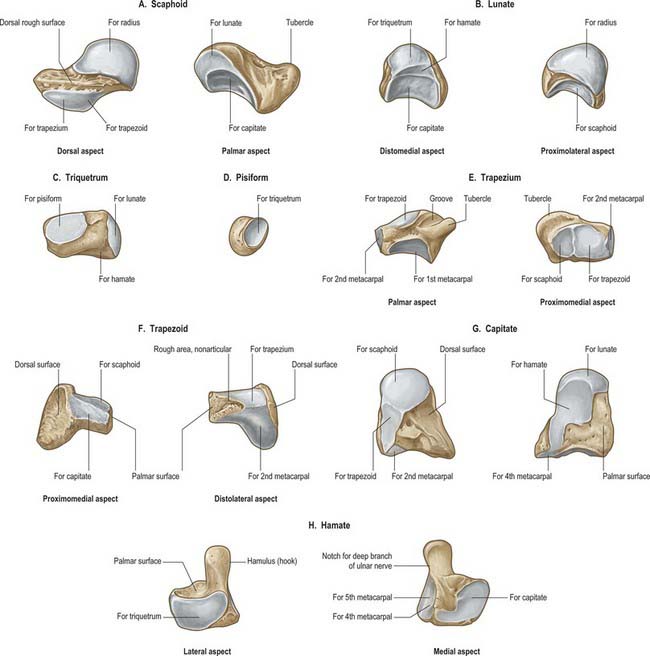
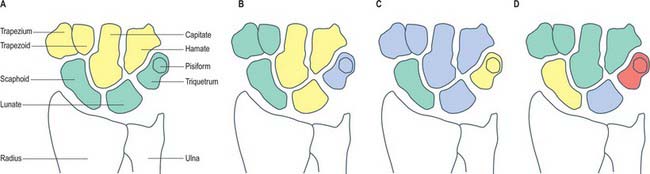
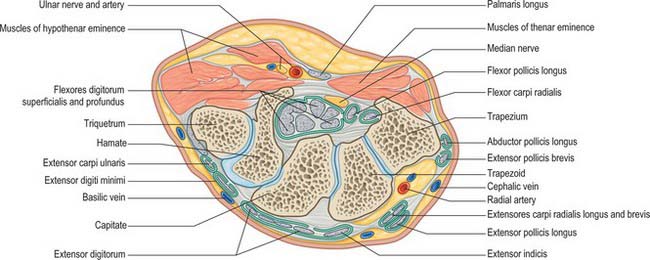
CARPAL BONES
The carpus contains eight bones: four each in proximal and distal rows (Fig. 50.5 and Fig. 50.6). In radial (lateral) to ulnar (medial) order, the scaphoid, lunate, triquetrum and pisiform make up the proximal row, and the trapezium, trapezoid, capitate and hamate make up the distal row. The pisiform articulates with the palmar surface of the triquetrum, and is thus separated from the other carpal bones, all of which articulate with their neighbours. The other three proximal bones form an arch which is proximally convex, and which articulates with the radius and articular disc of the distal radio-ulnar joint. The concavity of the arch is a distal recess embracing, proximally, the projecting aspects of the capitate and hamate. The two rows of carpal bones are thus mutually and firmly adapted without any loss of movement.
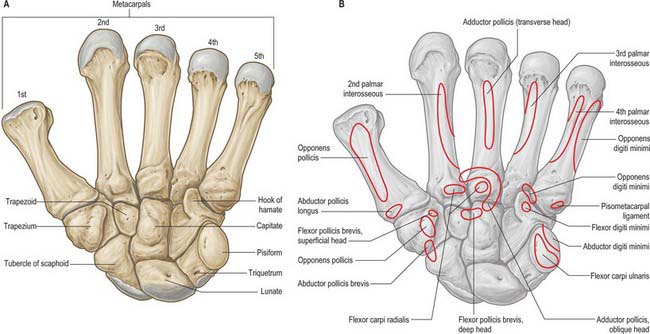
Fig. 50.5 A, Palmar aspect of the carpal and metacarpal bones of the left hand. Muscle attachments, except for the dorsal interossei, are shown in B.
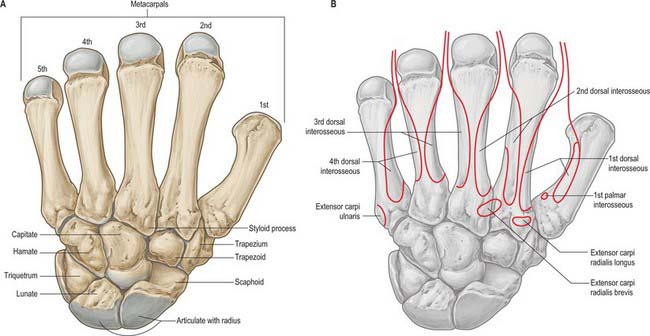
Fig. 50.6 A, Dorsal aspect of the carpal and metacarpal bones of the left hand. Muscle attachments are shown in B.
The dorsal carpal surface is convex. The palmar surface forms a deeply concave carpal groove, accentuated by the palmar projection of the radial (lateral) and ulnar (medial) borders. The ulnar projection is formed by the pisiform and the hamulus (hook), an unciform palmar process of the hamate. The pisiform is at the proximal border of the hypothenar eminence, on the ulnar side of the palm, and it is easily felt in front of the triquetrum. The hamulus is concave in a radial direction, its tip is palpable 2.5 cm distal to the pisiform, in line with the radial border of the ring finger. The superficial division of the ulnar nerve can be rolled on it. The radial border of the carpal groove is formed by the tubercles of the scaphoid and trapezium. The former is distal on the anterior scaphoid surface and palpable (sometimes also visible) as a small medial knob at the proximal border of the palmar thenar eminence, radial to the tendon of flexor carpi radialis. The tubercle of the trapezium is a vertically rounded ridge on the anterior surface of the bone, slightly hollow medially and just distal and radial to the scaphoid tubercle: it is difficult to palpate. (Both the scaphoid and trapezium may be grasped individually, and moved passively, by firm pressure between an opposed index finger and thumb applied to the palmar surface and ‘anatomical snuff-box’ simultaneously.) The carpal groove is made into an osseofibrous carpal tunnel by a fibrous retinaculum attached to its margins. The tunnel carries flexor tendons and the median nerve into the hand. The retinaculum strengthens the carpus and augments flexor efficiency. Radiocarpal, intercarpal and carpometacarpal ligaments are attached to the palmar and dorsal surfaces of all of the carpal bones, except the triquetrum and pisiform.
Individual carpal bones
Scaphoid
The scaphoid is the largest element in the proximal carpal row (Fig. 50.7A). It has a long axis which is distal, radial and slightly palmar in direction. A round tubercle on the distolateral part of its palmar surface is directed anterolaterally (Fig. 50.5), and provides an attachment for the flexor retinaculum and abductor pollicis brevis: it is crossed by the tendon of flexor carpi radialis. The rough dorsal surface is slightly grooved, narrower than the palmar, and pierced by small nutrient foramina, which are often restricted to the distal half (13%). The radial collateral ligament is attached to the lateral surface, which is also narrow and rough. The remaining surfaces are all articular. The radial (proximal) surface is convex, proximal and directed proximolaterally; the lunate surface is flat, semilunar, and faces medially; the capitate surface is large, concave and distal, and directed distomedially. The surface for the trapezium and trapezoid is continuous, convex and distal.
The scaphoid is the most frequently fractured carpal bone, typically as a result of a fall onto an outstretched hand. The fracture usually crosses the long axis of the bone. Fractures of its proximal part or its ‘waist’ may fail to unite because the proximal fragment has lost its blood supply: avascular necrosis of the proximal fragment is then inevitable.
Lunate
The lunate is approximately semilunar and articulates between the scaphoid and triquetrum in the proximal carpal row (Fig. 50.7B). Its rough palmar surface, almost triangular, is larger and wider than the rough dorsal surface. Its smooth convex proximal surface articulates with the radius and the articular disc of the distal radio-ulnar joint. Its narrow lateral surface bears a flat semilunar facet for the scaphoid. The medial surface, almost square, articulates with the triquetrum and is separated from the distal surface by a curved ridge, usually somewhat concave for articulation with the edge of the hamate in adduction (Fig. 50.7B, left). The distal surface is deeply concave to fit the medial part of the head of the capitate.
Triquetrum
The triquetrum is somewhat pyramidal and bears an oval isolated facet for articulation with the pisiform on its distal palmar surface (Fig. 50.7C). Its medial and dorsal surfaces are confluent, and marked distally by the attachment of the ulnar collateral ligament, but smooth proximally to receive the articular disc of the distal radio-ulnar joint in full adduction. The hamate surface, lateral and distal, is concavoconvex, broad proximally, narrow distally. The lunate surface, almost square, is proximal and lateral.
Pisiform
The pisiform is shaped like a pea, with a distolateral long axis (Fig. 50.7D). It bears a dorsal flat articular facet for the triquetrum. The tendon of flexor carpi ulnaris and the distal continuations of the tendon, the pisometacarpal and pisohamate ligaments, are all attached to the palmar non-articular area, which surrounds and projects distal to the articular surface: the pisiform therefore has attributes of a sesamoid bone.
Trapezium
The trapezium has a tubercle and groove on its rough palmar surface (Fig. 50.7E). The groove, which is medial, contains the tendon of flexor carpi radialis, and two layers of the flexor retinaculum are attached to its margins. The tubercle is obscured by the thenar muscles which are attached to it (opponens pollicis, flexor pollicis brevis and abductor pollicis brevis) (Fig. 50.5B). The elongated, rough dorsal surface is related to the radial artery. The large lateral surface is rough for attachment of the radial collateral ligament and capsular ligament of the thumb carpometacarpal joint. A large sellar surface faces distolaterally and articulates with the base of the first metacarpal. Most distally it projects between the bases of the first and second metacarpal bones and carries a small, quadrilateral, distomedially directed facet which articulates with the base of the second metacarpal. The large medial surface is gently concave for articulation with the trapezoid. The proximal surface is a small, slightly concave facet for articulation with the scaphoid. Its ridge, or ‘summit’, fits the concavity of the first metacarpal base, and extends in a palmar and lateral direction, at an angle of approximately 60° with the plane of the second and third metacarpals. Abduction and adduction occur in the plane of the ridge, which is shorter than the corresponding metacarpal groove. Their contours vary reciprocally: they are more curved near the second metacarpal base, whereas the radius of curvature is longer further away from this site. The two surfaces are not completely congruent, and the area of close contact probably moves towards the palm in adduction and dorsally in abduction. While the axis of flexion/extension passes through the trapezium, that for adduction/abduction is in the metacarpal base. Flexion is accompanied by medial rotation, and extension by lateral rotation (p. 875).
Trapezoid
The trapezoid is small and irregular. It has a rough palmar surface which is narrower and smaller than its rough dorsal surface: the former invades the lateral aspect (Fig. 50.7F). The distal surface, which articulates with the grooved base of the second metacarpal, is triangular, convex transversely and concave at right angles to this. The medial surface articulates by a concave facet with the distal part of the capitate, the lateral surface articulates with the trapezium, and the proximal surface articulates with the scaphoid.
Capitate
The capitate is the central and largest carpal bone. It articulates with the base of the third metacarpal via its triangular distal concavoconvex surface (Fig. 50.7G). Its lateral border is a concave strip for articulation with the medial side of the base of the second metacarpal. Its dorsomedial angle usually bears a facet for articulation with the base of the fourth metacarpal. The head projects into the concavity formed by the lunate and scaphoid: the proximal surface articulates with the lunate, and the lateral surface with the scaphoid. The facets for the scaphoid and trapezoid, though usually continuous on the distolateral surface, may be separated by a rough interval. The medial surface bears a large facet for articulation with the hamate, which is deeper proximally where it is partly non-articular. Palmar and dorsal surfaces are roughened for carpal ligaments, the dorsal being the larger.
Hamate
The hamate is cuneiform and bears an unciform hamulus (hook) which projects from the distal part of its rough palmar surface. The hamulus is curved with a lateral concavity and its tip inclines laterally, contributing to the medial wall of the carpal tunnel (Fig. 50.7H). The flexor retinaculum is attached to the apex of the hamulus. Distally, on the hamular base, a slight transverse groove may be in contact with the terminal deep branch of the ulnar nerve. The remaining palmar surface, like the dorsal, is roughened for attachment of ligaments. A faint ridge divides the distal surface into a smaller lateral facet which articulates with the base of the fourth metacarpal base, and a medial facet for articulation with the base of the fifth. The proximal surface, the thin margin of the wedge, usually bears a narrow facet which contacts the lunate in adduction. The medial surface is a broad strip, convex proximally, concave distally, which articulates with the triquetrum: distally a narrow medial strip is non-articular. The lateral surface articulates with the capitate by a facet covering all but its distal palmar angle.
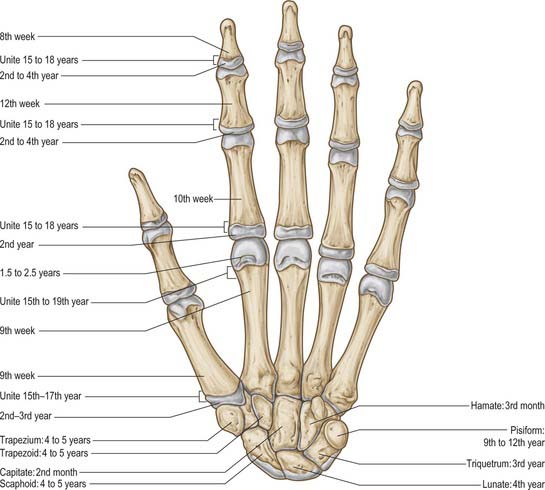
Ossification
Carpal bones are cartilaginous at birth, although ossification may have started in the capitate and hamate. Each carpal bone is ossified from one centre, capitate first, and pisiform last: the order in the others varies (Fig. 50.8, Fig. 5.9, Fig. 5.10, Fig. 5.11, Fig. 50.12). The capitate begins to ossify in the second month, the hamate at the end of the third month, the triquetrum in the third year, the lunate, scaphoid, trapezium and trapezoid in the fourth year in females and fifth year in males. The pisiform begins to ossify in the ninth or tenth year in females, and the twelfth in males. The order varies according to sex, nutrition and, possibly, race. Occasionally an os centrale occurs between the scaphoid, trapezoid and capitate bones: during the second prenatal month it is a cartilaginous nodule which usually fuses with the scaphoid. Occasionally, lunate and triquetral elements may fuse. Other fusions and accessory ossicles have also been described.

Fig. 50.8 Radiograph of a hand at 2½ years (male), dorsopalmar projection. Note early stages of ossification in the epiphyses at the proximal ends of the phalanges and first metacarpal; at the distal ends of the remaining metacarpals and radius; in the capitate, hamate and lunate. Typically, the centre for the lunate is preceded by the centre for the triquetrum. Compare with Figs 50.9 and 50.10.
METACARPALS
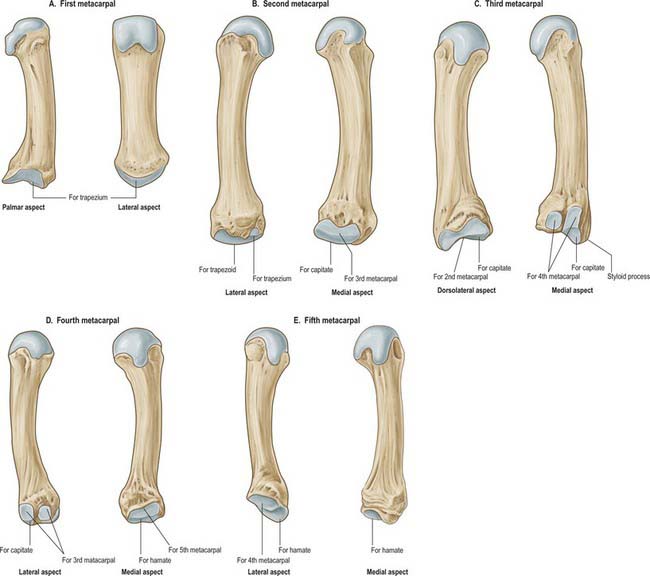
The metacarpus consists of five metacarpal bones, conventionally numbered in radio-ulnar order. These are miniature long bones, with a distal head, shaft and expanded base. The rounded heads articulate with the proximal phalanges. Their articular surfaces are convex, although less so transversely, and extend further on the palmar surfaces, especially at their margins. The knuckles are produced by the metacarpal heads. The metacarpal bases articulate with the distal carpal row and with each other, except the first and second. The shafts have longitudinally concave palmar surfaces, which form hollows for the palmar muscles. Their dorsal surfaces bear a distal triangular area, which is continued proximally as a round ridge. These flat areas are palpable proximal to the knuckles.
The medial four metacarpals are sometimes described as parallel; strictly speaking, they diverge somewhat, and radiate gently proximodistally. However, the first metacarpal, relative to the others, is more anterior and rotated medially on its axis through 90°, so that its morphologically dorsal surface is lateral, its radial border palmar, its palmar surface medial, and its ulnar border dorsal. Hence the thumb flexes medially across the palm and can be rotated into opposition with each finger. Opposition depends on medial rotation and is the prime factor in manual dexterity: when an object is grasped, fingers and thumb encircle it from opposite sides, greatly increasing the power and skill of the grip.
Individual metacarpal bones
First metacarpal
The first metacarpal is short and thick (Fig. 50.13A). Its dorsal (lateral) surface can be felt to face laterally; its long axis diverges distolaterally from its neighbour. The shaft is flattened, dorsally broad and transversely convex. The palmar (medial) surface is longitudinally concave and divided by a ridge into a larger lateral (anterior) and smaller medial (posterior) part. Opponens pollicis is attached to the radial border and adjoining palmar surface; the first dorsal interosseous muscle (radial head) is attached to its ulnar border and adjacent palmar surface. The base is concavoconvex and articulates with the trapezium. Abductor pollicis longus is attached on its lateral (palmar) side, the first palmar interosseous muscle to its ulnar side. The head is less convex than in other metacarpals and is transversely broad. Sesamoid bones glide on radial and ulnar articular eminences on its palmar aspect.
Second metacarpal
The second metacarpal has the longest shaft and largest base (Fig. 50.13B). The latter is grooved in a dorsopalmar direction for articulation with the trapezoid. Medial to the groove a deep ridge articulates with the capitate; laterally, nearer the dorsal surface of the base, there is a quadrilateral facet for articulation with the trapezium, and just dorsal to this facet a rough impression marks the attachment of extensor carpi radialis longus. On the palmar surface a small tubercle or ridge receives flexor carpi radialis. The medial side of the base articulates with that of the third metacarpal by a long facet, centrally narrowed. The shaft is prismatic in section and longitudinally curved, convex dorsally, concave towards the palm. Its dorsal surface is distally broad but proximally narrows to a ridge which is covered by extensor tendons of the index finger. Its converging borders begin at the tubercles, one on each side of its head for the attachment of collateral ligaments. Proximally the lateral surface inclines dorsally for the ulnar head of the first dorsal interosseous. The medial surface inclines similarly, and is divided by a faint ridge into a palmar strip for attachment of the second palmar interosseous, and a dorsal strip for attachment of the radial head of the second dorsal interosseous.
Third metacarpal
The third metacarpal has a short styloid process, projecting proximally from the radial side of the dorsal surface (Fig. 50.13C). Its base articulates with the capitate by a facet anteriorly convex but dorsally concave where it invades the styloid process on the lateral aspect of its base. A strip-like facet, constricted centrally, articulates with the bases of the second metacarpal (laterally) and the fourth metacarpal (medially), the latter by two oval facets. The palmar facet may be absent; less frequently the facets are connected proximally by a narrow bridge. The palmar surface of the base receives a slip from the tendon of flexor carpi radialis; extensor carpi radialis brevis is attached to its dorsal surface, beyond the styloid process. The shaft resembles that of the second metacarpal. The ulnar head of the second dorsal interosseous is attached to its lateral surface; the radial head of the third dorsal interosseous is attached to its medial surface, and the transverse head of adductor pollicis is attached to the intervening palmar ridge in its distal two-thirds. Its dorsal surface is covered by the extensor tendon.
Fourth metacarpal
The fourth metacarpal is shorter and thinner than the second and third (Fig. 50.13D). On its base it displays two lateral oval facets for articulation with the base of the third metacarpal; the dorsal is usually larger and proximally in contact with the capitate. A single medial elongated facet is for articulation with the base of the fifth metacarpal. The quadrangular proximal surface articulates with the hamate, and is anteriorly convex, dorsally concave. The shaft is like the second, but a faint ridge on its lateral surface separates the attachments of the third palmar interosseous and the ulnar head of the third dorsal interosseous. The radial head of the fourth dorsal interosseous is attached to the medial surface.
Fifth metacarpal
The fifth metacarpal (Fig. 50.13E) differs in its medial basal surface, which is non-articular and bears a tubercle for extensor carpi ulnaris. The lateral basal surface is a facet, transversely concave, convex from palm to dorsum, for articulation with the hamate. A lateral strip articulates with the base of the fourth metacarpal. The shaft bears a triangular dorsal area which almost reaches the base; the lateral surface inclines dorsally only at its proximal end. Opponens digiti minimi is attached to the medial surface. The lateral surface is divided by a ridge, which is sometimes sharp, into a palmar strip for the attachment of the fourth palmar interosseous and a dorsal strip for the ulnar part of the fourth dorsal interosseous.
Ossification
Each metacarpal ossifies from a primary centre for the shaft and a secondary centre which is in the base of the first metacarpal and in the heads of the other four (Figs 50.8-50.11). Ossification begins in the midshaft about the ninth week. Centres for the second to fifth metacarpal heads appear in that order in the second year in females, and between 1½ to 2½ years in males. They unite with the shafts about the 15th or 16th year in females, 18th or 19th in males. The first metacarpal base begins to ossify late in the second year in females, early in the third year in males, uniting before the 15th year in females and 17th in males. Sometimes the styloid process of the third metacarpal is a separate ossicle. The thumb metacarpal ossifies like a phalanx, and some authorities therefore consider that the thumb skeleton consists of three phalanges. Others believe that the distal phalanx represents fused middle and distal phalanges, a condition occasionally observed in the fifth toe. When the thumb has three phalanges, the metacarpal has a distal and a proximal epiphysis. It occasionally bifurcates distally. When it does, the medial branch has no distal epiphysis and bears two phalanges, while the lateral branch shows a distal epiphysis, and three phalanges. The existence of only a distal metacarpal epiphysis may be associated with a greater range of movement at the metacarpophalangeal joint. In the thumb, the carpometacarpal joint has the wider range, and the first metacarpal has a basal epiphysis. A distal epiphysis may appear in the first, and a proximal epiphysis in the second, metacarpal.

Fig. 50.9 Radiograph of a hand at 6½ years (male), dorsopalmar projection. Note the more advanced state of the centres of ossification which were already visible in Fig. 50.8, and the appearance of additional centres in the distal ulnar epiphysis and in the triquetrum, scaphoid, trapezium and trapezoid.

Fig. 50.10 Radiograph of a hand at 11 years (female), dorsopalmar projection. Note the maturing shapes of all the ossifications previously seen in Figs 50.8 and 50.9, with the addition of the pisiform.

Fig. 50.11 Radiograph of adult hand for comparison (male of 19 years), dorsopalmar projection. Note additional ossification in the sesamoid bones of the thumb. 1. Head of middle phalanx of middle finger. 2. Shaft of middle phalanx of middle finger. 3. Base of middle phalanx of middle finger. 4. Head of proximal phalanx of ring finger. 5. Shaft of proximal phalanx of ring finger. 6. Base of proximal phalanx of ring finger. 7. Head of fifth metacarpal. 8. Shaft of fifth metacarpal. 9. Base of fifth metacarpal. 10. Hook of hamate. 11. Hamate. 12. Pisiform. 13. Triquetrum. 14. Lunate. 15. Styloid process of ulna. 16. Head of ulna. 17. Distal phalanx of index finger. 18. Distal phalanx of thumb. 19. Proximal phalanx of thumb. 20. Sesamoid bone. 21. Trapezoid. 22. Trapezium. 23. Capitate. 24. Scaphoid. 25. Styloid process of radius. 26. Ulnar (sigmoid) notch of radius. 27. Radius.
(By permission from Weir J, Abrahams PH 2003 Imaging Atlas of Human Anatomy, 3rd edn, London: Mosby, and contributions from Anna-Maria Belli, Margaret Hourihan, Niall Moore and Philip Owen.)
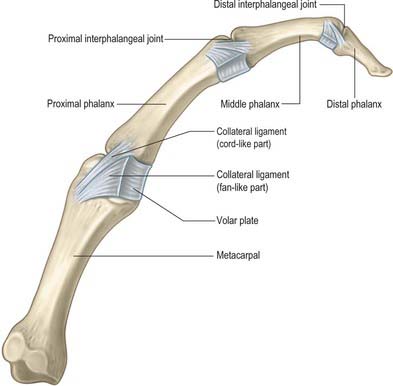
PHALANGES
There are 14 phalanges, three in each finger, two in the thumb. Each has a head, shaft and proximal base. The shaft tapers distally, its dorsal surface transversely convex. The palmar surface is transversely flat but gently concave anteriorly in its long axis. The bases of the proximal phalanges carry concave, oval facets adapted to the metacarpal heads. Their own heads are smoothly grooved like pulleys and encroach more on to the palmar surfaces. The bases of the middle phalanges carry two concave facets separated by a smooth ridge, conforming to the heads of the proximal phalanges. The bases of the distal phalanges are adapted to the pulley-like heads of the middle phalanges. The heads of the distal phalanges are non-articular and carry a rough, crescentic palmar tuberosity to which the pulps of the fingertips are attached.
Articular ligaments and numerous muscles are attached to the phalanges. A corresponding tendon of flexor digitorum profundus and, on its dorsal surface, extensor digitorum, are attached to the base of each distal phalanx on its palmar surface. A tendon of flexor digitorum superficialis and its fibrous sheath are attached to the sides of a middle phalanx, and a part of extensor digitorum is attached to the base dorsally. A fibrous flexor sheath is attached to the sides of a proximal phalanx, part of the corresponding dorsal interosseous is attached to its base laterally, and another dorsal interosseous is attached medially.
The phalanges of the little finger and the thumb differ. Abductor and flexor digiti minimi are attached to the medial side of the base of the proximal phalanx of the little finger. The tendon of extensor pollicis brevis and the oblique head of adductor pollicis (dorsally), and the oblique and transverse heads of adductor pollicis, sometimes conjoined with the first palmar interosseous (medially), are attached to the base of the proximal pollicial phalanx.
The margins of the proximal pollicial phalanx are not sharp, because the fibrous sheath is less strongly developed than it is in the other digits.
Ossification
Phalanges are ossified from a primary centre for the shaft and a proximal epiphysial centre (Figs 50.8-50.12). Ossification begins prenatally in shafts as follows: distal phalanges in the eighth or ninth week, proximal phalanges in the tenth, middle phalanges in the 11th week or later. Epiphysial centres appear in proximal phalanges early in the second year (females), and later in the same year (males), and in middle and distal phalanges in the second year (females), or third or fourth year (males). All epiphyses unite about the 15th to 16th year in females, and 17th to 18th year in males.
JOINTS
DISTAL RADIO-ULNAR JOINT
The distal radio-ulnar joint is a uniaxial pivot joint (Fig. 50.14).
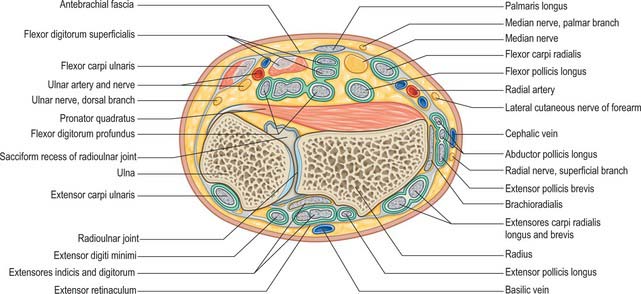
Fig. 50.14 Transverse section through the left wrist at the level of the distal radio-ulnar joint, showing the muscle tendons and their synovial sheaths.
(From Sobotta 2006.)
The articulating surfaces are between the convex distal head of the ulna and the concave ulnar notch of the radius, and are connected by an articular disc.
The fibrous capsule is thicker anteriorly and posteriorly, but the proximal part of the capsule is lax.
The articular disc is fibrocartilaginous (collagen with few elastic fibres in the young) and is triangular, binding the distal ends of the ulna and radius. Its periphery is thicker, its centre sometimes perforated. The disc is attached by a blunt, thick apex to a depression between the ulnar styloid process and distal articular surface, and by its wider thin base to the prominent edge between the ulnar notch and carpal articular surface of the radius. Its margins are united to adjacent carpal ligaments, its surfaces are smooth and concave: the proximal articulates with the ulnar head, the distal is part of the radiocarpal joint, and articulates with the lunate and, when the hand is adducted, the triquetrum. The disc shows age-related degeneration, becoming thinned and ultimately perforated in about half the subjects over the age of 60.
The capsule is lined by synovial membrane which projects proximally between the radius and ulna as a recessus sacciformis in front of the distal part of the interosseous membrane.
Vascular supply and lymphatic drainage
The arterial supply to the distal radio-ulnar joint and disc is mainly derived from the palmar and dorsal branches of the anterior interosseous artery, reinforced by the posterior interosseous and ulnar arteries.
The distal radio-ulnar joint is innervated by branches of the anterior and posterior interosseous nerves.
Movements at the radio-ulnar joint complex pronate and supinate the hand. In pronation the radius, carrying the hand, turns anteromedially and obliquely across the ulna, its proximal end remains lateral, its distal becomes medial. During this action the interosseous membrane becomes spiralled. In supination the radius returns to a position lateral and parallel to the ulna and the interosseous membrane becomes unspiralled. The hand can be turned through 140–150°: with the elbow extended, this can be increased to nearly 360° by humeral rotation and scapular movements. Power is greater in supination, a fact which has affected the design of nuts, bolts and screws, which are tightened by supination in right-handed subjects. Moreover, supination is an antigravity movement with a pendent upper arm and semiflexed forearm; in seizing objects for examination or manipulation, pronation is merely a preliminary and is aided by gravity.
Forearm rotation occurs between the articulation of the head of the ulna and sigmoid notch distally, and the head of the radius and the radial notch of the ulna proximally. These distal and proximal radio-ulnar joints are pivot-type synovial joints: they act as a pair permitting stable rotary motion (pronation 61–66°, supination 70–77°). During rotation, the radius moves around the ulnar head. The axis for pronation and supination is often represented as a line through the centre of the radial head (proximal) and the ulnar attachment of the articular disc (distal). More correctly this is the axis of movement of the radius relative to the ulna and it does not remain stationary. The radial head rotates in the fibro-osseous ring: its distal lower end and articular disc swing round the ulnar head. During rotation of the radial head its proximal surface spins on the humeral capitulum. As the forearm moves from full pronation into supination the ulna translocates medially by 9–10 mm, such that the axis of rotation shifts but still passes through the ulnar head. In addition the sigmoid notch changes its contact position with the ulnar head, lying dorsal proximal in pronation and volar distal in supination. The distal end of the ulna is not stationary during these movements; it moves a variable amount along a curved course, posterolaterally in pronation, anteromedially in supination. The axis of movement, as defined above, is therefore displaced laterally in pronation, medially in supination. Hence the axis for supination and pronation of the whole forearm and hand passes between the bones at both the superior and distal radio-ulnar joints when ulnar movement is marked, but through the centres of the radial head and ulnar styloid when it is minimal. The axis may be prolonged through any digit, depending on the medial or lateral displacement of the distal end of the ulna. The hand will rotate further than the forearm because of the sliding–rotatory movement which occurs between the carpal bones and the bases of the metacarpals and, to a very minor degree, at the radiocarpal joint.
RADIOCARPAL (WRIST) JOINT
The radiocarpal joint is a synovial biaxial and ellipsoid joint formed by articulation of the distal end of the radius and the triangular fibrocartilage with the scaphoid, lunate and triquetrum (Fig. 50.15 and Fig. 50.16). In the neutral position of the wrist, only the scaphoid and lunate are in contact with the radius and articular disc: the triquetrum comes into apposition with the disc only in full adduction of the wrist joint. The radial articular surface and distal discal surface form an almost elliptical, concave surface with a transverse long axis. The radial surface is bisected by a low ridge into two concavities. A similar ridge usually appears between the medial radial concavity and the concave distal discal surface. The proximal articular surfaces of the scaphoid, lunate and triquetrum, and their interosseous ligaments, form a smooth convex surface which is received into the proximal concavity.
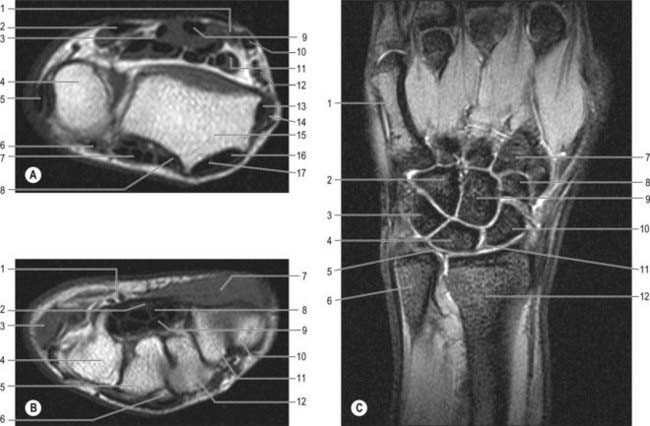
Fig. 50.16 MRI left wrist. A, Axial view at level of distal radio-ulnar joint. B, Axial view at level of carpal tunnel. C, Coronal MRI through the wrist demonstrating normal bony anatomy and the triangular fibrocartilage.
Part A: 1. Median nerve. 2. Flexor carpi ulnaris. 3. Flexor digitorum profundus. 4. Ulna. 5. Extensor carpi ulnaris. 6. Extensor digiti minimi. 7. Extensor digitorum and extensor indicis. 8. Extensor pollicis longus. 9. Flexor digitorum superficiales. 10. Flexor carpi radialis. 11. Flexor pollicis longus. 12. Radial artery. 13. Abductor pollicis longus. 14. Extensor pollicis brevis. 15. Radius. 16. Extensor carpi radialis longus. 17. Extensor carpi radialis brevis.
Part B: 1. Ulnar artery and nerve. 2. Median nerve. 3. Hypothenar muscles. 4. Hamate. 5. Capitate. 6. Base of 3rd metacarpal. 7. Thenar muscles. 8. Flexor digitorum superficialis. 9. Flexor digitorum profundus. 10. Base of 1st metacarpal. 11. Trapezium. 12. Trapezoid.
Part C: 1. 5th metacarpal. 2. Hamate. 3. Triquetrum. 4. Lunate. 5. Triangular fibrocartilage. 6. Distal ulna. 7. Base of 2nd metacarpal. 8. Trapezoid. 9. Capitate. 10. Scaphoid. 11. Scapholunate ligament. 12. Distal radius.
The fibrous capsule is lined by synovial membrane which is usually separate from that of the distal radio-ulnar and intercarpal joints. A protruding prestyloid recess (recessus sacciformis), anterior to the articular disc, is present and ascends close to the styloid process. The recess is bounded distally by a fibrocartilaginous meniscus, which projects from the ulnar collateral ligament between the tip of the ulnar styloid process and the triquetrum; both are clothed with hyaline articular cartilage. The meniscus may ossify. The capsule is strengthened by palmar radiocarpal and ulnocarpal, dorsal radiocarpal and radial and ulnar collateral ligaments.
The radiocarpal joint is supplied by branches of the anterior interosseous artery, anterior and posterior carpal branches of the radial and ulnar arteries, palmar and dorsal metacarpal arteries and recurrent rami of the deep palmar arch.
The radiocarpal joint is innervated by the anterior and posterior interosseous nerves with contributions from the median, ulnar and radial nerves.
Movements accompany those of the intercarpal and midcarpal joints and are described on page 871.
CARPAL JOINTS
The intercarpal joints interconnect the carpal bones. They may be summarized as the joints between the proximal and distal rows of carpal bones, and the midcarpal joint, a complex joint between the rows.
Carpal bones are connected by an extensive array of ligaments, not all of which are specifically named. The flexor retinaculum is an accessory intercarpal ligament. Articular surfaces are either sellar, ellipsoid or spheroidal.
Joints of the proximal carpal row
Joints of the proximal carpal row are between the scaphoid, lunate and triquetrum. In addition, the pisiform articulates with the palmar surface of the triquetrum at a small, oval, almost flat, synovial pisotriquetral joint.
A thin capsule surrounds the joint. The synovial cavity is usually separate but may communicate with that of the radiocarpal joint.
Joints of the distal carpal row
Joints of the distal carpal row are between the trapezium, trapezoid, capitate and hamate. There is virtually no movement at these joints.
Midcarpal joint
The midcarpal joint, between the scaphoid, lunate and triquetrum (proximally) and trapezium, trapezoid, capitate and hamate (distally) is a compound articulation that may be divided descriptively into medial and lateral parts. Throughout most of the medial compartment the convexity formed by the head of the capitate and hamate articulates with a reciprocal concavity formed by the scaphoid, lunate and much of the triquetrum. However, most medially the curvatures are reversed, forming a compound sellar joint. In the lateral compartment the trapezium and trapezoid articulate with the scaphoid, forming a second compound articulation, often said to be plane, but which is also sellar.
The carpal synovial membrane is most extensive, and lines an irregular articular cavity. Its proximal part is between the distal surfaces of the scaphoid, lunate and triquetrum and the proximal surfaces of the second carpal row. It has proximal prolongations between the scaphoid and lunate, and lunate and triquetrum, and three distal prolongations between the four bones of the second row. The absence of an interosseous ligament means that the prolongation between the trapezium and trapezoid and/or between the trapezoid and capitate is often continuous with corresponding carpometacarpal joints, variably from the second to the fifth, or often the second and third only. In the latter case, the joint between the hamate and fourth and fifth metacarpal bones has a separate synovial membrane and the carpometacarpal interosseous ligament is interposed. Synovial cavities of carpometacarpal joints are prolonged slightly between the metacarpal bases. The synovial joint between the pisiform and triquetrum is usually isolated.
The carpal joints are supplied by the posterior carpal branches of the radial and ulnar arteries and by the anterior interosseous artery.
Precise details about innervation of the carpal joints are lacking. They appear to be innervated by small branches from the deep terminal branch of the ulnar nerve, the median nerve and its anterior interosseous branch, the superficial radial nerve and the posterior interosseous branch of the radial nerve.
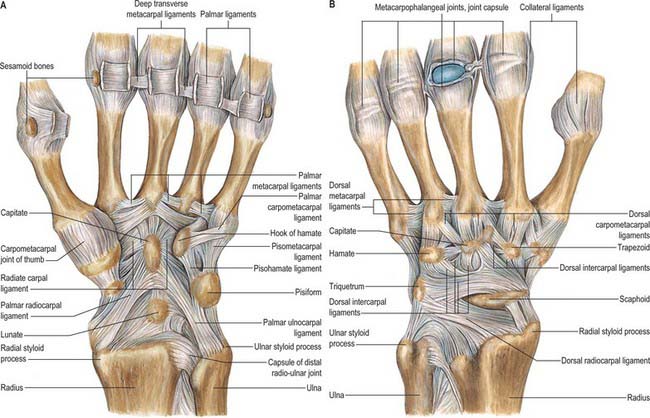
Wrist ligaments
Wrist ligaments situated between the fibrous and synovial layers of the wrist joint are termed intracapsular, while those lying superficial to the fibrous layer are extracapsular. Almost all ligaments of the wrist actually lie within the joint capsule and the only exceptions are the flexor and extensor retinaculae and the pisotriquetral ligament. The intracapsular ligaments appear to blend one into another and the edges of the ligaments may not be distinct or discrete.
The ligaments are further classified into extrinsic and intrinsic named ligaments. In addition there are superficial and deep parts to some of the extrinsic ligaments; the latter are identifiable at wrist arthroscopy, the former are not.
It is important to appreciate that the wrist ligaments are named from proximal to distal and from radial to ulnar. Thus a ligament passing between the capitate, scaphoid and radius is called the radioscaphocapitate ligament.
Extrinsic ligaments
Extrinsic ligaments connect the carpus with the forearm bones. The extrinsic ligaments as a group tend to be longer than the intrinsic ligaments. They are approximately one-third as strong but easier to repair following rupture.
Extrinsic palmar carpal ligaments
When the synovial lining of the carpal tunnel is dissected away, two V-shaped ligamentous bands are visible with their apices lying distally (Fig. 50.15A). The limbs of the ‘V’ take origin from the radius and ulna respectively: the apex of one ‘V’ attaches to the distal row and that of the second ‘V’ to the proximal row.
The radioscaphocapitate ligament originates from the radial styloid and the palmar lip of the radius. It courses distally and is then described by some authors as having three parts. The first is the most radial and inserts onto the lateral aspect of the waist of the scaphoid (radial collateral ligament). The second continues as part of the distal ‘V’ and inserts onto the distal pole of the scaphoid. The third passes over the proximal pole of the scaphoid towards the midcarpus and blends with the fibres originating from the ulnar side – part of the triangular fibrocartilage complex – to form the arcuate ligament over the palmar aspect of the capitate. A few of the fibres of the radioscaphocapitate ligament attach to the body of the capitate. There is a discrete interval between the inferior margin of this ligament and the palmar horn of the lunate which is known as the space of Poirier.
The long radiolunate ligament takes origin adjacent to the radioscaphocapitate ligament on the palmar lip of the radius. It passes over and supports the proximal pole of the scaphoid before inserting into the palmar horn of the lunate. This ligament is discrete from the radioscaphocapitate ligament and the visible separation is known as the interligamentous sulcus (continuous with the space of Poirier).
Radioscapholunate (ligament of Testut)
Histological studies have shown the radioscapholunate ligament is not a true ligament because it contains neurovascular structures which supply the scapholunate interosseous membrane and is covered by a thick synovial lining. However it a visible landmark inside the wrist joint when undertaking wrist arthroscopy.
The short radiolunate ligament is part of the proximal ‘V’. It arises from the palmar lip of the lunate fossa of the radius and passes directly to the palmar horn of the lunate. To the ulnar side its fibres blend with those of the palmar triangular fibrocartilage complex as these also pass to their insertion on the lunate. This ligament contributes to the stability of the lunate.
The ulnolunate ligament originates from the palmar aspect of the ulna adjacent to the short radiolunate ligament and inserts onto the palmar horn of the lunate. Part of this fibre complex arches radially and blends with part of the radioscaphocapitate complex, forming the arcuate ligament.
Ulnotriquetral (ulnar collateral) ligament
The ulnotriquetral ligament arises from the palmar aspect of the ulna and inserts into the medial aspect of the triquetrum. It continues distally to a further attachment to the medial aspect of the hamate. It is generally thought that the ulnolunate and ulnotriquetral ligaments also take some origin from the marginal ligament of the triangular fibrocartilage complex.
Extrinsic dorsal carpal ligaments
The dorsal wrist ligaments are comparatively thin. They are reinforced by the floor and septa of the fibrous tunnels for the six dorsal compartments. The extrinsic dorsal carpal ligaments and the intrinsic dorsal intercarpal ligaments have a ‘Z-shaped’ configuration (Fig. 50.15B). The pattern and shape of these ligaments is utilized in one surgical approach to the dorsum of the wrist joint where incisions are oriented parallel with the ligaments: this reduces scarring and restriction of subsequent motion caused by the arthrotomy.
Dorsal radiolunotriquetral ligament
The dorsal radiolunotriquetral ligament is a true intracapsular ligament. It is the only extrinsic ligament on the dorsum of the carpus and has superficial and deep components. The superficial part connects the radius and triquetrum, and the deep part connects the radius, lunate and triquetrum. The two components are inseparable. The wide superficial component arises from the dorsal margin of the distal radius and courses ulnarly to insert on the dorsal edge of the triquetrum. The deep component takes a narrower origin from the ulnar aspect of the distal dorsal radius and passes in an ulnar direction to attach to part of the lunotriquetral articulation and the intrinsic lunotriquetral ligament.
Intrinsic ligaments
Intrinsic ligaments of the wrist are attached to carpal bones. They are stronger and shorter than extrinsic ligaments and are connected with the extrinsic ligament complexes by interdigitating fibres. Rupture of one or more intrinsic ligaments frequently leads to a clinical instability of the carpus. The intrinsic ligaments are subdivided into ligaments which connect the carpal bones of the proximal and distal rows respectively and ligaments which connect the rows by crossing over the midcarpal joint.
Proximal row interosseous ligaments
The scapholunate and lunotriquetral ligaments are clinically and biomechanically important structures. In the sagittal plane they have an approximately horseshoe-shape configuration with palmar, midcarpal and dorsal components. The scapholunate ligament contains short transverse fibres connecting the dorsal aspect of the respective bones and more obliquely oriented fibres connecting the palmar aspect. The functional significance of this arrangement is that the tighter dorsal component of the ligament acts as a hinge facilitating flexion and extension of the scaphoid: these movements are important to carpal mechanics. The ligament continues on its midcarpal section as an interosseous membrane. The lunotriquetral ligament has similar dorsal, midcarpal interosseous and palmar components, but the fibres of the dorsal and palmar components are similarly rather than differentially oriented, which precludes the same pattern of preferential movement as occurs between the lunate and scaphoid. The interosseous membranes of the scapholunate and lunotriquetral ligaments separate the midcarpal from the radiocarpal joint spaces. Dye injected into one of these joint spaces which leaks to the other denotes a tear of one of these ligaments.
Distal row interosseous ligaments
The distal row interosseous ligaments are powerful ligaments between the capitate, hamate, trapezium and trapezoid, with an important stabilizing function for the distal carpal row. They have superficial and deep components, and unlike the ligaments of the proximal row, are seldom torn.
Anterolaterally lies the fan-shaped palmar scaphocapitate – trapezoid ligament which originates from the scaphoid tuberosity and is thought to be an important stabilizer of the scaphoid. This ligament may be subdivided into two parts known as the scaphotrapeziotrapezoidal ligament (having the attachments as its name suggests) and a more ulnar component known as the scaphocapitate ligament. The triquetrohamate and triquetrocapitate ligaments lie towards the ulnar side of the carpus.
The dorsal intercarpal ligament assists in stabilization of the proximal carpal row. It arises from the trapezoid and distal pole of scaphoid, and passes across the dorsal horn of the lunate to be attached to the triquetrum. The ligament forms the floor of the fourth and fifth extensor compartments. On the radial side is the lateral scaphotrapeziotrapezoidal ligament which acts as a stabilizer of the scaphoid and trapezium.
Triangular fibrocartilage complex (TFCC) and distal radio-ulnar ligaments
The triangular fibrocartilage complex (TFCC) is a ligamentous and cartilaginous structure which suspends the distal radius and ulnar carpus from the distal ulna. The TFCC stabilizes the ulnocarpal and radio-ulnar joints, transmits and distributes load from the carpus to the ulna, and facilitates complex movements at the wrist (Fig. 50.17). By definition, it is made up of the cartilaginous disc, the meniscus homologue (an embryological remnant of the ‘ulnar’ wrist that is only occasionally present), volar and dorsal distal radio-ulnar ligaments, ulnar collateral ligament, floor of extensor carpi ulnaris subsheath, ulnolunate and ulnotriquetral ligaments. The triangular fibrocartilage proper (TFC) is a biconcave body composed of chondroid fibrocartilage. It extends across the dome of the ulnar head and varies between 2 and 5 mm in thickness.
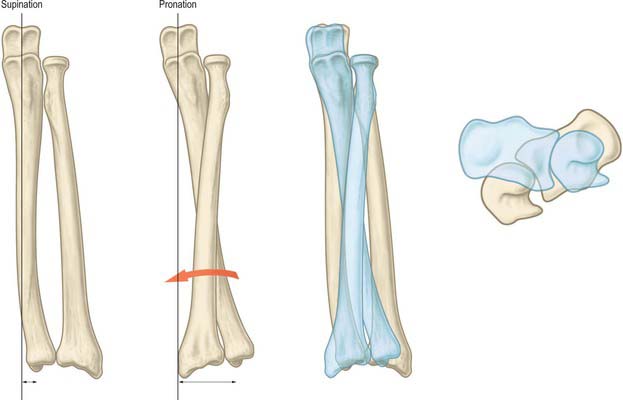
Fig. 50.17 Representation of the manner in which the radius moves around the ulna during forearm rotation. The curvature of the shaft of the radius is important in facilitating this movement. The axis of forearm rotation passes through the head of the ulna and varies slightly in position through the range of rotation. The degree of ulnar translocation of the ulna during pronation (shown by the difference in length between the two double arrowheads) can be seen with reference to the distance the ulnar styloid has moved from the plumb line (vertical black line shown)
From its distal aspect, the TFCC resembles a hammock supporting the ulnar carpus with the disc proper as the base of the hammock. From the proximal side, the TFCC appears in the shape of a fan extending from the fovea of the ulna along either side of the sigmoid notch. This fan-shaped structure is divided into dorsal, central and palmar portions where the central portion is the triangular fibrocartilage and the peripheral margins are thick lamellar collagen, structurally adapted to tensile loading and known as the distal (palmar and dorsal) radio-ulnar ligaments. In keeping with other extrinsic ligaments of the wrist joint proper there are thought to be superficial and deep components of the distal radio-ulnar ligaments which act as a functional couple stabilizing the rotation of the ulnar head on the sigmoid notch of the radius.
Stability of the distal radio-ulnar joint during forearm rotation is conferred by the TFCC complex, dorsal and volar distal radio-ulnar ligaments, interosseous membrane and subsheath of the extensor carpi ulnaris tendon (floor of sixth dorsal extensor compartment).
COORDINATED MOVEMENTS AND LOAD-BEARING AT THE WRIST JOINT
Wrist movements
The movements at the radiocarpal and intercarpal joints are considered together since they are both involved in all movements as well as being acted upon by the same muscles. Active movements are flexion (85°), extension (85°), adduction or ulnar deviation (45°), abduction or radial deviation (15°) and circumduction (all movements are approximate).
The range of flexion is greater at the radiocarpal joint, while in extension there is more movement at the midcarpal joint (Fig. 50.18). Hence the proximal surfaces extend further posteriorly on the lunate and scaphoid bones. These movements are limited chiefly by antagonistic muscles, and therefore the range of flexion is perceptibly diminished when the fingers are flexed, due to increased tension in the extensors. Only when the joints are forced to the limits of flexion or extension are the dorsal or palmar ligaments fully stretched (but see below).

Fig. 50.18 A, Radiograph of the hand and wrist in full flexion: lateral aspect. Compare with B, and note the relative positions of the capitate and lunate, and the lunate and radius. B, Radiograph of the hand and wrist: lateral aspect. The long axes of the third metacarpal, capitate and lunate are, approximately, in line with the long axis of the radius. Note the relative positions of the capitate and lunate, and the lunate and radius. C, Radiograph of the hand and wrist in full extension: lateral aspect. Compare with B and note the alterations in the relative positions of the capitate and lunate, and the lunate and the radius. 1. Capitate. 2. Lunate. 3. Tubercle of the trapezium. 4. Tubercle of the scaphoid.
Adduction of the hand is considerably greater than abduction, perhaps due to the more proximal site of the ulnar styloid process. Most adduction occurs at the radiocarpal joint. The lunate articulates with both the radius and articular disc when the hand is in the midposition, but in adduction it articulates solely with the radius, and the triquetrum now comes into contact with the articular disc (Fig. 50.19A). Much of the proximal articular surface of the scaphoid becomes subcapsular beneath the radial collateral ligament and forms a smooth, convex, palpable prominence in the floor of the ‘anatomical snuff-box’.

Fig. 50.19 A, Radiograph of the hand in full adduction (ulnar deviation), dorsopalmar projection. The arrows point to the scaphoid on the radial side and to the pisiform on the ulnar side. Note that the shadow of the pisiform bone overlaps the shadow of the tip of the styloid process of the ulna. Compare with B and observe that the movements occur at both the radiocarpal and intercarpal joints. B, Radiograph of the same hand in full abduction (radial deviation). The arrows point to the hamate and pisiform. Compare with A and note that: (1) the scaphoid and lunate have passed medially (ulnarly) so that the latter articulates to a large extent with the articular disc of the distal radio-ulnar joint; (2) the pisiform is now widely separated from the styloid process of the ulna; (3) the scaphoid, having rotated round a transverse axis, is much foreshortened; (4) the apex of the hamate has been thrust away from the lunate by the rotation of the capitate around an anteroposterior axis; (5) a gap has opened up between the distal portions of the hamate and triquetrum; and (6) the long axes of the capitate and lunate are now almost in the same straight line.
Abduction from the neutral position occurs at the midcarpal joint, the proximal carpal row not moving. Radiographs of abducted hands show that the capitate rotates round an anteroposterior axis so that its head passes medially and the hamate conforms to this: the distance between the lunate and the apex of the hamate is increased (Fig. 50.19B). The scaphoid rotates around a transverse axis, and its proximal articular surface moves away from the capsule to articulate solely with the radius. Movements are limited by antagonistic muscles and, at extremes, by the carpal collateral ligaments.
Circumduction of the hand is not rotatory, but involves successive flexion, adduction, extension and abduction or vice versa.
Muscles producing movements
Integrated model of wrist movement (carpal kinematics)
The proximal row (scaphoid, lunate and triquetrum) is an intercalated segment: no tendons insert onto the bones of the row. It is inherently unstable and controlled by specific retaining and gliding ligaments. Its relative position is determined by the spatial configurations of the radius, triangular fibrocartilage complex (TFCC) and ulna on one side, and the rigid distal carpal row on the other. The proximal carpal row is subject to two opposing moments: the scaphoid straddles the proximal and distal rows and tends to rotate the proximal row into flexion under axial load and radial deviation. At the same time there is a force tending to extend the proximal row which is initiated by the distal row and transmitted via the midcarpal ligaments to the triquetrum (Fig. 50.20). Stability of the midcarpal joint is thus ensured during both movement and loading.
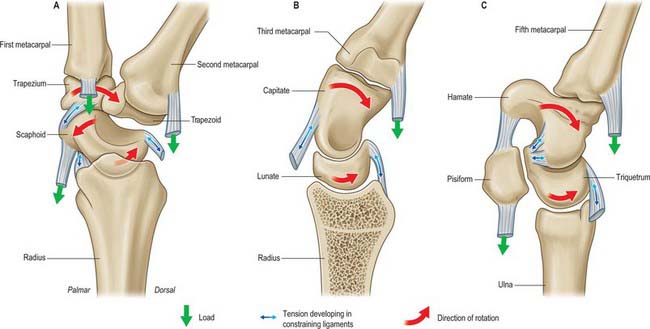
Fig. 50.20 The balance of rotatory moments occurring during axial loading are explained in this series of sagittal sections of the wrist. A, The scaphoid tends to move into flexion with axial loading and is simultaneously constrained palmarly by the scaphotrapeziotrapezoidal ligaments and dorsally by the scapholunate ligament. B, The lunate tends to follow the scaphoid restrained only by the dorsal radiolunate ligament. C, The triquetrum tends to flex along with the two other bones of the proximal carpal row and is constrained palmarly by the triquetrohamate and triquetrocapitate ligaments and dorsally by the radiotriquetral ligament.
The distal carpal row (trapezium, trapezoid, capitate and hamate) can be regarded as one rigid structure tightly bound together. The scaphoid bridges the proximal and distal carpal rows and provides a functional couple between the two.
The carpus was originally thought to move simply as proximal and distal rows (row or rigid body theory). According to this view, during the composite movement of wrist flexion and extension, approximately two-thirds of movement occurs at the radiocarpal joint and one-third at the midcarpal joint. The carpus was later judged to move in lateral central and medial columns more than it did in rows, and the radius–lunate–capitate was described as a three-bar linkage system (column theory). This theory was modified to incorporate the specific stabilizing role of the scaphoid as it bridges the proximal and distal rows. A further theory proposed that the bones were linked by their ligaments in a ring configuration, so that any breakage of the key links leads to instability (ring theory). Most recently the ‘four unit’ theory suggests that the distal carpal row moves as a single unit, and the scaphoid, lunate and triquetrum move in complex but characteristic relationships which are dependent on the given movement (Fig. 50.21). Clinical observation provides some support for each of these theories.
Wrist loading
Axial loading refers to load or force applied along a line parallel to the long bones of the arm and therefore corresponds to power grip manoeuvres, e.g. clenching the fist. In the normal activities of daily living, loading is usually multiplanar with a combination of vectors of force, e.g. grasping an object and then lifting it against gravity with the elbow flexed would engender transverse and axial loading with respect to the long axis of the forearm.
Force transmission
Radiocarpal joint
The articulation of the carpus with the radius (radiocarpal) and ulna (ulnocarpal) can be described in terms of specific fossae, i.e. the scaphoid and lunate fossae of the radius and the facet formed by the distal aspect of the TFCC. The scaphoid fossa contributes 43%, the lunate fossa 46%, and the TFCC 11%, of the total area of this articulating surface. Under physiological conditions, the contact area between this surface and the proximal carpal row is of the order of 20% of the whole. It varies consistently with position: greater contact is seen in forearm supination, radial deviation and dorsiflexion of the wrist, and lesser contact in forearm pronation, ulnar deviation and palmar flexion of the wrist. Further increase in contact area is seen with axial loading. Maximum contact areas are recorded at 40%. Force across the joint also varies with the position of the forearm and the degree of wrist flexion. For a given load in wrist neutral position, 50% of force passes across the scaphoid fossa, 35% through the lunate fossa, and 15% across the TFCC. With a power grip there is slight ulnar deviation, and the proportion of force passing across the scaphoid and lunate fossae reverses.
Midcarpal joint
With the wrist in neutral position, 50–60% of a given load is transmitted from the distal row through the capitate to the scaphoid and lunate. Up to 30% of the load is transmitted via the scaphotrapeziotrapezoid joint, and up to 20% via the hamate-triquetral joint.
Distal radio-ulnar joint (DRUJ)
The DRUJ is part of a more complex articulation that includes the proximal radio-ulnar joint and the interosseous membrane. Static axial loading of the wrist increases the contact areas of the joint surfaces of the distal radio-ulnar joint, DRUJ. Force transmitted across the DRUJ also increases with axial loading and varies with position of forearm rotation. It is maximal at 60° supination, when the ulnar head lies most directly under the ulnar-sided carpus, and least in full pronation. It has been shown that with the wrist in neutral position, 70–80% of axial load passes down the radius and 20–30% down the ulna. The proportion of force passing down the ulna varies with increasing load, and changes with position of the hand and carpus relative to the forearm bones. The interosseous membrane between the radius and ulna plays a role in distributing load in the forearm. Distal radio-ulnar joint loading also depends on relative radial and ulnar lengths, i.e. ulnar negative, neutral or positive variance.
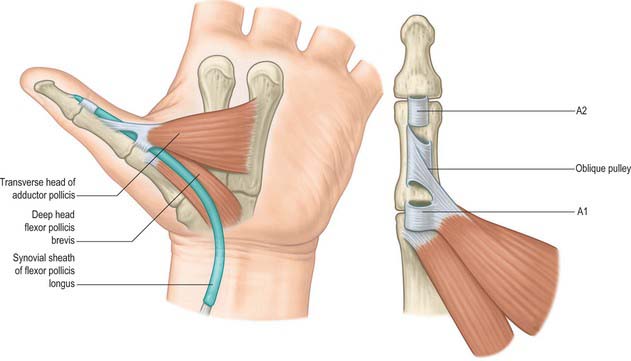
Specific actions
Power grip
There is a predictable pathway of force transmission during axial loading of the hand such as occurs in power grip. During this action the wrist is positioned in mid-dorsiflexion and the object is tightly gripped. Force is transmitted from the hand and wrist via the radiocarpal joint and TFCC to both bones of the forearm, through the elbow joint to the humerus, and thence via the glenohumeral joint to the pectoral girdle. Dynamic muscle action accounts for transmission of a large part of the force, and a smaller proportion is transmitted through the osseoligamentous structures. The distribution of force between the radius and ulna varies dynamically. It depends on the absolute value of load, degree of forearm rotation, and position of the carpus relative to the forearm.
Hammer action
The action exemplified by hammering, where the wrist alternates between the dorsoradial and the palmar-ulnar position, is an important movement. The reciprocal movement is more constrained and awkward to perform. The former movement is important in a wide variety of activities of daily living. In primates this movement is needed (along with forearm rotation at the distal radio-ulnar joint) for brachiation.
It is believed that load distributes dynamically as the position of the carpus moves relative to the forearm and there are consequent changes in the relative position of the carpal bones.
Wrist instability
During evolution the upper limb has developed to facilitate prehension, i.e. the placing of the hand in three-dimensional space. However, mobility of the hand on the forearm has evolved at the expense of stability. A wrist is said to be kinetically unstable when it cannot bear physiological loads without giving way or causing injury. A wrist is kinematically unstable when it exhibits sudden changes in carpal alignment, i.e. during a specific movement there is a ‘clunk’ as one or more of the carpal bones moves abnormally with respect to the others. Stability of the various joints such that the bones maintain normal anatomical relations with respect to each other throughout the normal range of motion is essential for physiological load-bearing.
Some degree of carpal instability may occur as part of inherent hypermobility in affected individuals, but usually it occurs only after rupture or attenuation of intrinsic and extrinsic carpal ligaments and may be detected either clinically or evidenced on radiographs as malalignment of the carpal bones (Fig. 50.22).

Fig. 50.22 Scapholunate dissociation shown in posteroanterior power grip view (A) and lateral view (B). Dissociation between the scaphoid and lunate as shown here leads to collapse of the scaphoid into flexion and the lunate into extension (dorsal intercalated segment instability, or DISI) thus removing the inbuilt tension across the proximal row. This causes the gap (so called Terry Thomas sign) between the scaphoid and lunate in the PA radiograph (marked with asterisk) and increased scapholunate angle above the upper limit of normal of 60 degrees, as shown in B.
CARPOMETACARPAL JOINTS
The first carpometacarpal joint, CMCJ, or basal joint of the thumb, is a modified saddle joint that permits opposition of the thumb and confers the ability to hold and manipulate objects: the actions of ‘pinch’ grip, ‘tripod’ pinch and ‘chuck’ grip are specifically facilitated. Significant forces pass across and compress this joint compared to the remaining CMCJs. The second to fifth CMCJs exhibit an increasing range of movement progressing from the radial to the ulnar side. Thus there is little mobility at the base of the index ray, but considerable mobility at the base of the small finger ray, which facilitates ‘cupping’ of the palm of the hand. Compressive forces between the metacarpals and the distal carpal row are estimated to be upwards of ten times the forces at the tips of the fingers during ‘pinch’ or ‘chuck’ grip.
Carpometacarpal joint of the thumb
The carpometacarpal joint of the thumb is a sellar (saddle) joint between the first metacarpal base and trapezium. It enjoys wide mobility due to its extensive articular surfaces and their topology.
The first metacarpal and trapezium are connected by lateral, anterior and posterior ligaments and a fibrous capsule. The broad lateral ligament runs from the lateral surface of the trapezium to the radial side of the metacarpal base. The palmar and dorsal ligaments are oblique bands which converge to the ulnar side of the metacarpal base from the palmar and dorsal surfaces of the trapezium respectively.
The carpometacarpal joint of the thumb receives its blood supply from the radial artery and its first dorsal metacarpal branch.
The carpometacarpal joint of the thumb is innervated by articular twigs from the posterior interosseous nerve and the superficial branch of the radial nerve.
Except at initiation, flexion is accompanied by medial rotation; conversely, medial rotation involves flexion. Linkage of movements is due largely to the shape of the articular surfaces (which impose some conjunct rotation), and to the obliquity of the dorsal ligament (which, when taut, anchors the ulnar side of the metacarpal base while its radial side continues to move). Contraction of flexor pollicis brevis, assisted by opponens pollicis, thus produces medial rotation with flexion; combined with abduction this brings the thumb pulp into contact with the pulps of the slightly flexed fingers, a movement termed opposition. (The flexed fingers have varying degrees of lateral metacarpophalangeal rotation, which is minimal in the index, and maximal in the minimus.) Conversely, full extension of the thumb metacarpal entails slight lateral rotation, attributable to the sellar form of the joint and to the action of the palmar ligament (which is similar to that of the dorsal ligament in flexion). (See also p. 888.)
The muscles producing movements at the carpometacarpal joint of the thumb are as follows.
Flexor pollicis brevis and opponens pollicis, aided by flexor pollicis longus when the other joints of the thumb are flexed. Flexion entails medial rotation.
Abductor pollicis longus and extensors pollicis brevis and longus. In full extension extensor pollicis longus, owing to its oblique pull and the disposition of the palmar ligament, rotates the thumb laterally and draws it dorsally, i.e. slightly adducts the thumb.
Abductors pollicis brevis and longus. When abduction is maximal the digit and metacarpal are not in line, and the thumb is abducted at both metacarpophalangeal and carpometacarpal joints.
Second to fifth carpometacarpal joints
The second to fifth carpometacarpal joints are synovial ellipsoid joints between the carpus and second to fifth metacarpals. Although widely classed as plane, they have curved articular surfaces which are often of complex sellar shape. The bones are united by articular capsules, and dorsal, palmar and interosseous ligaments.
The dorsal ligaments are the strongest, and connect the dorsal surfaces of the carpal and metacarpal bones. The second metacarpal has two ligaments, from the trapezium and trapezoid; the third has two, from the trapezoid and capitate; the fourth has two, from the capitate and hamate; the fifth has a single band from the hamate, which is continuous with a similar palmar ligament, forming an incomplete capsule.
The palmar ligaments are similar, except that the third metacarpal has three: a lateral from the trapezium, superficial to the tendon sheath of flexor carpi radialis, an intermediate from the capitate, and a medial from the hamate.
The interosseous ligaments consist of two short, thick, fibrous bands. They are limited to one part of the carpometacarpal articulation and connect contiguous distal margins of the capitate and hamate with adjacent surfaces of the third and fourth metacarpal bones: they may be united proximally.
The synovial membranes are often continuous with those of the intercarpal joints. Occasionally, the joint between the hamate and fourth and fifth metacarpal bones has a separate synovial cavity, bounded laterally by the medial interosseous ligament and its extensions to the palmar and dorsal parts of the capsule.
The second to fifth carpometacarpal joints are supplied by the posterior carpal branches of the radial and ulnar arteries, by twigs from the anterior interosseous artery, and from the palmar digital arteries.
INTERMETACARPAL JOINTS
The second to fifth metacarpal bases articulate reciprocally by small cartilage-covered facets connected by dorsal, palmar and interosseous ligaments.
The dorsal and palmar ligaments pass transversely from bone to bone. The interosseous ligaments connect contiguous surfaces just distal to their articular facets.
Movements at the carpometacarpal and intermetacarpal joints
Movements at the carpometacarpal and intermetacarpal articulations are limited to slight gliding, sufficient to permit some flexion–extension and adjunct rotation: ranges vary in different joints. They are partly accessory movements occurring when the palm is ‘cupped’, as in grasping an object. Active movements also occur and are familiar, e.g. to the pianist or violinist. The fifth metacarpal is most movable and the second and third are the least mobile. These variations are easily demonstrated by opposing each digit to the thumb over the palmar centre. About two-thirds of the movements are pollicial, as described above, but during opposition to minimus, the latter is flexed, abducted and laterally rotated, accounting for the remaining third of the movement. These actions occur at both the carpometacarpal and metacarpophalangeal joints. The close-packed position probably coincides with carpal extension, as in gripping. Further accessory movements are spiral twisting of the whole metacarpus on the carpus.
METACARPOPHALANGEAL JOINTS
The metacarpophalangeal joints are usually considered ellipsoid. However, the metacarpal heads are adapted to shallow concavities on the phalangeal bases: they are not regularly convex but partially divided on their palmar aspects and thus almost bicondylar (Fig. 50.23).
Each metacarpophalangeal joint has a palmar and two collateral ligaments.
The palmar (volar plates) ligaments are unusual. They are thick, dense and fibrocartilaginous, and sited between, and connected to, the collateral ligaments. They are attached loosely to the metacarpals but firmly to the phalangeal bases. Their palmar aspects are blended with the deep transverse palmar ligaments and are grooved for the flexor tendons, whose fibrous sheaths connect with the sides of the grooves. Their deep surfaces increase articular areas for the metacarpal heads.
Deep transverse metacarpal ligaments
The deep transverse metacarpal ligaments are three short, wide, flat bands which connect the palmar ligaments of the second to fifth metacarpophalangeal joints. They are related anteriorly to the lumbricals and digital vessels and nerves, and posteriorly to the interossei. Bands from the digital slips of the central palmar aponeurosis join their palmar surfaces. On both sides of the third and fourth metacarpophalangeal joints, but only the ulnar side of the second and radial side of the fifth, transverse bands of the dorsal digital expansions join the deep transverse metacarpal ligaments. The lumbricals and the phalangeal attachments of the dorsal interossei lie anterior to this band, and the remaining attachments of dorsal interossei and palmar interossei are posterior to it (see Fig. 50.30).
The collateral ligaments are strong, round cords which flank the joints. Each is attached to the posterior tubercle and adjacent pit on the side of its metacarpal head, and each passes distoanteriorly to the side of the anterior aspect of its phalangeal base (Fig. 50.23).
The metacarpophalangeal joints receive their blood supply from the dorsal and palmar metacarpal arteries, the arteria princeps pollicis, and the arteria radialis indicis.
The metacarpophalangeal joints are innervated by twigs from the palmar digital branches of the median nerve, the deep terminal branch of the ulnar nerve, and the posterior interosseous nerve.
Flexion, extension, adduction, abduction, circumduction and limited rotation all take place at the metacarpophalangeal joints. Rotation cannot occur in isolation, but may accompany flexion–extension. This may be initiated voluntarily in the free hand (e.g. each finger flexing and rotating to place its tip near the palmar centre); the range of rotation is frequently increased as a result of the resistance of a grasped object. Flexion is almost 90°, whereas extension is only a few degrees: both movements are limited mostly by antagonistic muscles. Flexion is often terminated by the resistance offered by a grasped object. The metacarpophalangeal joint of the thumb has a flexion–extension range of approximately 60°, which is almost entirely flexion. Slight lateral rotation accompanies digital flexion of digits 3–5. Flexion of the index finger may be accompanied by minimal lateral rotation or no rotation: a small degree of medial rotation is frequently observed. Other movements are adduction–abduction (maximal range 25°), which invariably accompanies the corresponding carpometacarpal movements and increases their combined range, and slight conjunct rotation, but greater adjunct rotation, which accompanies flexion–extension. Of the second to fifth metacarpophalangeal joints, the second is most mobile in adduction–abduction (approximately 30°), followed by the fifth, fourth, and third.
Accessory movements are further rotation (most marked in the thumb), anteroposterior and lateral translation of a phalanx or metacarpal, and distraction.
The muscles producing movements at the metacarpophalangeal joints are as follows.
Flexores digitorum superficialis and profundus, assisted by the lumbricals and interossei and, in the minimus, flexor digiti minimi brevis. In the thumb, flexores pollicis longus and brevis and the first palmar interosseous.
Extensor digitorum, assisted in the second and fifth digits by extensor indicis and extensor digiti minimi respectively. In the thumb, extensors pollicis longus and brevis.
In extended fingers, palmar interossei; the long flexors are predominant during flexion. In the thumb, limited metacarpophalangeal adduction is possible and may be attributable to adductor pollicis and the first palmar interosseous.
In extended fingers, dorsal interossei assisted by the long extensors (except in the middle finger), and abductor digiti minimi in the little finger. In the thumb, abductor pollicis brevis (which also contributes to opposition). When the fingers are flexed at the IP joints, active abduction is impossible: if the long digital flexors are inactive, passive abduction is free. Inability to abduct actively in this position may be due to shortening of the dorsal interossei and abductor digiti minimi by flexion. However the altered line of pull of the interossei relative to the axis of movement is probably the determining factor: in digital extension the axis of lateral movements is anteroposterior, whereas in flexion it is proximodistal, and the line of pull of the interossei is then nearly parallel to the axis.
The ulnar collateral ligament of the metacarpophalangeal joint of the thumb can be avulsed from its distal attachment to the base of the proximal phalanx by a combination of forced extension and radial deviation of the joint. The injury was reported to occur in gamekeepers while breaking the necks of game, but can occur following simple falls onto the outstretched hand, especially in skiers who have the straps of ski poles wrapped around their thumbs.
The ulnar collateral ligament is normally covered by the aponeurotic insertion of the adductor pollicis tendon. Following avulsion, the proximal end can become superficially displaced around the proximal free edge of the aponeurotic insertion of the adductor. This soft tissue interposition prevents the ends of the avulsed ligament from healing. If left untreated, a firm palpable inflammatory swelling occurs, known as the ‘Stener lesion’. Surgical repair requires division of the aponeurotic insertion of adductor pollicis, followed by bony reattachment of the avulsed ligament and repair of the aponeurosis.
INTERPHALANGEAL JOINTS
The interphalangeal joints are uniaxial hinge joints (Fig. 50.23).
Each interphalangeal joint has a palmar ligament (also known as the volar plate) and two collateral ligaments. The long extensor tendons take the place of the dorsal capsular ligaments. Extensions from the extensor expansion, each collateral ligament and the palmar ligament, all pass into the joint cavity and provide a significant increase to the articular surface area of the phalangeal base: their deformable nature improves joint congruence.
The volar plate constitutes the floor of the interphalangeal joint. In the proximal interphalangeal joint, the distal end of the volar plate is thickened laterally where it is firmly attached to the base of the middle phalanx at the position of the true collateral ligament attachment. Centrally, it is more delicate and blends with the volar periosteum of the middle phalanx. Proximally, the volar plate is also very delicate in its central portion, but it is thickened laterally to form the so-called check rein ligaments which attach to the periosteum of the proximal phalanx just within the walls of the A2 pulley component of the fibrous flexor sheath. Nutrient branches of the digital arteries pass underneath these check ligaments to reach the vinculae (Fig. 50.24). A detailed account of the anatomy of the volar plate can be found in Bowers et al (1980).
The interphalangeal joints are innervated by the palmar digital branches of the median nerve (to the thumb, index, middle and ring fingers), and the ulnar nerve (to the ring and little fingers).
Stability is conferred by the articular contours of the joint surfaces and the collateral ligaments. The flexor and extensor tendons and retinacular ligaments provide secondary stabilization. Stability against hyperextension of the proximal interphalangeal joint is enhanced by the three-dimensional box arrangement that is produced by the collateral ligament–volar plate complex.
Movements (active) at the interphalangeal joints are flexion and extension, and are greater in range at the proximal joints. Flexion is considerable, whereas extension is limited by tension of the digital flexors and terminated by tension in the palmar ligaments and nonarticular compression. Full extension is the close-packed position, which is assumed whenever the fingers are used as props to transmit body weight or powerful thrust. In contrast, the fully clenched fist may also be used for this purpose. Flexion and extension are accompanied by slight conjunct rotation: during flexion this turns the digital pulps slightly laterally, i.e. to face the opposed thumb, and an opposite rotation occurs during extension.
Accessory movements are limited rotation, abduction, adduction and anteroposterior translation. They permit the fingers to adapt to the shapes of gripped objects and help to protect against stresses and strains.
The muscles producing movements at the interphalangeal joints are as follows.
At proximal interphalangeal joints, flexores digitorum superficialis and profundus; at distal interphalangeal joints, flexor digitorum profundus; at the thumb interphalangeal joint, flexor pollicis longus.
Extensores digitorum, digiti minimi and pollicis longus, in association with abductor pollicis longus and extensor pollicis brevis. Extension occurs simultaneously in both joints in digits 2–5.
Simultaneous flexion at the metacarpophalangeal joints and extension at the interphalangeal joints of a digit are essential for the fine movements of writing, drawing, threading a needle, etc. The lumbricals and interossei have long been accepted as not only primary agents in flexing the metacarpophalangeal joints but also in extending the interphalangeal joints via their attachments to the dorsal digital expansions.
Mallet finger is a traumatic rupture, avulsion fracture or laceration of the terminal slip of the extensor tendon to the terminal phalanx of the finger. It can result from forced flexion of the distal phalanx of the fully extended finger and is a well-known injury in cricketers. The patient is unable actively to extend the terminal phalanx although the distal interphalangeal joint can be extended passively.
Swan neck deformity involves hyperextension of the proximal interphalangeal joint together with distal interphalangeal joint flexion. It is caused by a relative overactivity of the extensors acting at the proximal interphalangeal joint compared with the flexors. It arises as a result of intrinsic muscle spasm, long standing mallet finger or dysfunction of flexor digitorum superficialis and can only occur if there is also some laxity of the volar plate.
Boutonnière deformity is a flexion deformity of the proximal interphalangeal joint following either division or laxity in the central slip of the extensor tendon, which normally inserts into the base of the middle phalanx. An essential feaure is hyperextension at the distal interphalangeal joint. It usually occurs as a result of either trauma or rheumatoid arthritis which cause the lateral bands of the extensor tendon to migrate in a volar direction and the head of the proximal phalanx to migrate dorsally. Initially the deformity is passively correctable. With time, the soft tissues around the joint contract and a fixed deformity results.
MUSCLE
EXTRINSIC LONG FLEXORS AND EXTENSORS
The extrinsic long flexors and extensors are described on page 845.
Flexor retinaculum
The flexor retinaculum is a strong, fibrous band (Fig. 50.25). It crosses the front of the carpus and converts its anterior concavity into the carpal tunnel which transmits the flexor tendons of the digits and the median nerve. The retinaculum is short and broad, measuring 2.5–3 cm both transversely and proximodistally. It is attached medially to the pisiform and the hook of the hamate. Laterally, it splits into superficial and deep laminae. The superficial lamina is attached to the tubercles of the scaphoid and trapezium. The deep lamina is attached to the medial lip of the groove on the trapezium. Together with this groove, the two laminae form a tunnel, lined by a synovial sheath, which contains the tendon of flexor carpi radialis. The retinaculum is crossed superficially by the ulnar vessels and nerve – immediately radial to the pisiform – and by the palmar cutaneous branches of the median and ulnar nerves. A slender band of fascia, the superficial part of the flexor retinaculum, bridges over the ulnar neurovascular bundle and attaches to the radial side of the pisiform, forming a tunnel (Guyon’s canal) which is an occasional site of ulnar nerve entrapment. The tendons of palmaris longus and flexor carpi ulnaris are partly attached to the anterior surface of the retinaculum. Distally some of the intrinsic muscles of the thumb and little finger are attached to the retinaculum.
Long flexor tendon apparatus
Flexor tendon sheaths
The fibrous sheaths of the flexor tendons are specialized parts of the palmar fascial continuum. Each finger has an osseoaponeurotic tunnel which extends from midpalm to the distal phalanx. The thumb has a tunnel for flexor pollicis longus which extends from the metacarpal to the distal phalanx. The proximal border is to some extent a matter of definition, because the transverse fibres of the palmar aponeurosis may be considered to be a part of the pulley system. The sheath consists of arcuate fibres which arch anteriorly over bone, tendons (where the sheath is required to be stiff), and the centres of joints (where a bucket-handle of arcuate fibres is a mechanically favourable arrangement). In contrast, where the sheath is required to fold to permit joint flexion, it consists of cruciate fibres. These fibrous sheaths are lined by a thin synovial membrane which provides a sealed lubrication system containing synovial fluid. The synovial membrane extends from the distal phalanx to midpalm in the case of the index, middle and ring fingers, and further proximally in the case of the little finger (Fig. 50.26). The sheaths around the thumb and little finger are continuous with the flexor sheaths in front of the wrist. The parietal synovial membrane is reflected onto the surface of the flexor tendon, forming a visceral synovium.
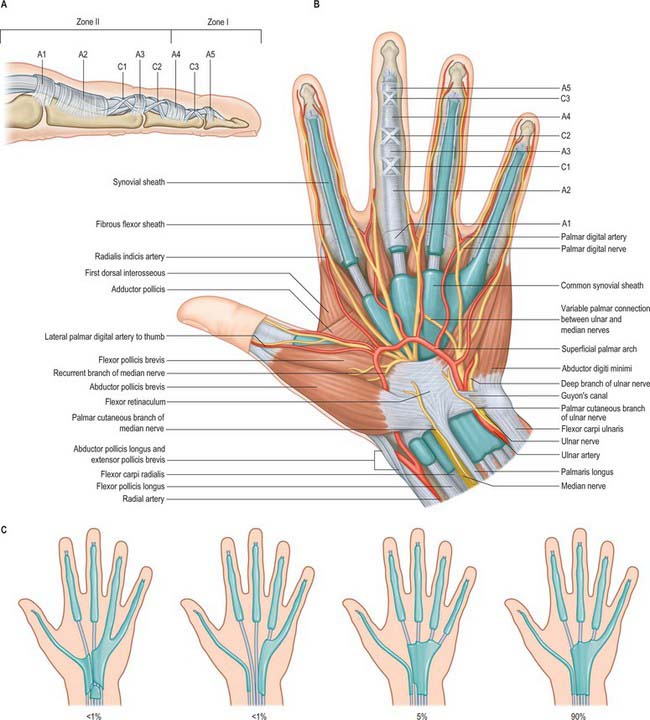
Fig. 50.26 Synovial sheaths of the tendons and flexor tendon sheaths on the flexor aspect of the left wrist and hand. Where they are exposed, the synovial sheaths are shown in blue. A, Lateral view of the anular and cruciate pulleys of the flexor tendon sheath. B, Palmar aspect showing the synovial sheaths and details of the anular and cruciate pulleys in the middle finger. Note the extension of the digital arteries and nerves to the end of the middle finger have been omitted to allow clarity in showing the pulley system. C, Variation in the arrangement to the synovial sheaths to the digits.
A standard nomenclature for the anular and cruciform pulleys that make up the sheath has been adopted by the American Society for Surgery of the Hand: the letters A and C respectively are used (Doyle & Blythe 1975).
The usual pattern is as follows (Fig. 50.26). The A1 pulley is situated anterior to the palmar cartilaginous plate of the metacarpophalangeal joint and may extend over the proximal part of the proximal phalanx. The A2 overlies the middle third of the proximal phalanx. It is the strongest pulley and arises from well-defined longitudinal ridges on the palmar aspect of the phalanx. Its distal edge is well developed. A pouch or recess of synovium extends superficial to the free edge of the pulley fibres so that the free edge forms a lip protruding into the synovial space. A3 is a narrow pulley lying palmar to the proximal interphalangeal joint. A4 overlies the middle third of the middle phalanx, and A5 overlies the distal interphalangeal joint. The cruciate fibres are numbered in a slightly different manner. C0 is palmar to the metacarpophalangeal joint. There are two cruciate zones, C1 and C2, at the proximal interphalangeal joint and they lie just proximal and distal respectively to A3. At the distal interphalangeal joint there is one pronounced cruciate system, C3, which lies between A4 and A5. Variations occur frequently. During flexion, the cruciate fibres become orientated more transversely in the digits and the edges of adjacent anular pulleys approximate so that they form, in full flexion, a continuous tunnel of transversely orientated fibres. Surgically the most important pulleys which prevent bowstringing of the flexor tendons are the A2 and A4 pulleys.
The pulley arrangement in the thumb is different from that in the other digits. There are three constant pulleys – two anular and one oblique (Fig. 50.27). The A1 pulley is located at the metacarpophalangeal joint. The oblique pulley is located over the mid-portion of the proximal phalanx, and its fibres pass from the ulnar aspect proximally to the radial aspect dorsally. The A2 pulley is thinner than the A1 pulley and is situated just proximal to the interphalangeal joint. The oblique pulley is the most important pulley in the thumb for maintaining the action of flexor pollicis longus.
Synovial sheaths of the carpal flexor tendons
Two synovial sheaths envelop the flexor tendons as they traverse the carpal tunnel, one for the flexores digitorum superficialis and profundus, the other for flexor pollicis longus (Fig. 50.25). These sheaths typically extend into the forearm for 2.5 cm proximal to the flexor retinaculum, and occasionally communicate with each other deep to it. The sheath of the flexores digitorum tendons reaches about halfway along the metacarpal bones, where it ends in blind diverticula around the tendons to the index, middle and ring fingers (Fig. 50.26). The sheath is prolonged around the tendons to the little finger and is usually continuous with their digital synovial sheath. A transverse section through the carpus shows that the tendons are invaginated into the sheath from the lateral side (Fig. 50.25). The parietal layer lines the flexor retinaculum and the floor of the carpal tunnel. It is reflected laterally as the visceral layer over the tendons of flexor digitorum superficialis ventrally and flexor digitorum profundus dorsally. Medially a recess formed by the visceral layer of the sheath insinuates between the two groups of tendons and passes laterally for a variable distance. The sheath of flexor pollicis longus, which is usually separate, is continued along the thumb as far as the insertion of the tendon.
Vincula
The phenomenon of tendon gliding within a fibrous sheath requires a very specialized arrangement of the vascular supply. Folds of synovial membrane containing a loose plexus of fascial fibres carry blood vessels to the tendons at certain defined points (Fig. 50.28). These folds, vincula tendinum, are of two kinds. Vincula brevia, of which there are two in each finger, are attached to the deep surfaces of the tendons near to their insertions. There is thus one vinculum brevium attaching flexor digitorum profundus to the region of the distal interphalangeal joint, and a more proximal vinculum deep to flexor digitorum superficialis at the proximal interphalangeal joint. Vincula longa are filiform: usually two are attached to each superficial tendon, one to each deep tendon.
Trigger finger
Trigger finger is a stenosing tenovaginitis which affects the fibrous flexor sheaths of the fingers or thumb within the palm. The affected sheath thickens and entraps the contained tendons, which become constricted at the site of entrapment and bulge distal to it, to produce a distinct nodule in the palm of the hand. The finger now snaps as the tendon nodule passes through the constriction on flexing the finger. The corresponding extensor muscle is insufficiently powerful to extend the affected finger. The patient does this passively, accompanied by a painful snap. Treatment frequently requires surgical division of the A1 pulley of the flexor sheath to relieve the stricture.
Extensor retinaculum
The extensor retinaculum is a strong, fibrous band which extends obliquely across the back of the wrist (Fig. 50.29). It is attached laterally to the anterior border of the radius, medially to the triquetral and pisiform bones, and, in passing across the wrist, to the ridges on the dorsal aspect of the distal end of the radius. It prevents bowstringing of the tendons across the wrist joint.
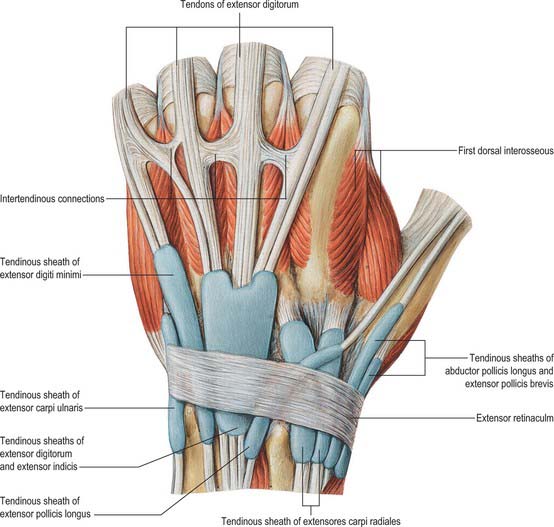
Fig. 50.29 The synovial sheaths of the tendons on the extensor aspect of the left wrist.
(From Sobotta 2006.)
Synovial sheaths of the carpal extensor tendons
Six tunnels deep to the extensor retinaculum transmit the extensor tendons, each contains a synovial sheath. The tendons of abductor pollicis longus and extensor pollicis brevis lie in a tunnel on the lateral side of the styloid process of the radius. Occasionally there may be a separate synovial sheath for each, or the tendon of the abductor may be double. The tendons of extensores carpi radiales longus and brevis lie behind the styloid process. The tendon of extensor pollicis longus lies on the medial side of the dorsal tubercle of the radius and the tendons of extensor digitorum and extensor indicis lie in a tunnel on the medial side of the tubercle. The tendon of extensor digiti minimi lies opposite the interval between the radius and ulna, and the tendon of extensor carpi ulnaris lies between the head and the styloid process of the ulna.
The tendon sheaths of abductor pollicis longus, extensores pollicis brevis and longus, extensores carpi radiales and extensor carpi ulnaris stop immediately proximal to the bases of the metacarpal bones; those of extensor digitorum, extensor indicis and extensor digiti minimi are sometimes prolonged a little more distally along the metacarpus.
De Quervain’s tenovaginitis is a stenosing tenovaginitis of unknown aetiology which occurs in the first dorsal compartment at the level of the radial styloid. It involves the common extensor sheath containing the tendons of abductor pollicis longus and extensor pollicis brevis. There is palpable thickening of the tendon sheath with painful limitation of extension of the thumb. Treatment frequently requires division of the thickened sheath, care being taken to avoid the adjacent superficial radial nerve. Division of the sheath produces no functional impairment.
Extensor tendon apparatus
The extensor digitorum tendons emerge through the fourth dorsal compartment onto the dorsum of the hand, where they are joined together distally by a varying pattern of oblique interconnections, the juncturae tendinae. These typically pass in a distal direction from middle finger to index finger and from ring finger to middle and little fingers. Proximal lacerations to the middle finger extensor tendon may result in only partial loss of extension because of these tendinous interconnections.
At the level of the metacarpophalangeal joint, each extensor tendon is held in a central position over the dorsum of the joint by a flat fibrous extensor expansion (Fig. 50.30). The expansion extends onto the dorsum of the proximal phalanx of each digit. It forms a movable hood, which moves distally when the metacarpophalangeal joint is flexed, and proximally when it is extended (in which position it is most closely applied to the joint).
Each extensor tendon blends with the extensor expansion along its central axis, and is separated from the metacarpophalangeal joint by a small bursa. The expansion is triangular in shape, with its base proximal. It receives the conjoined tendons of the intrinsic muscles. The expansion is almost translucent between its margins and the extensor digitorum tendon. Transverse fibres (the sagittal bands) pass to the volar plate and transverse metacarpal ligaments. They separate the phalangeal attachment of the dorsal interosseus from the rest of the muscle, and the palmar interosseus from the lumbrical muscle. Injuries to the sagittal bands can lead to subluxation of the extensor tendon.
The margins of the extensor expansions are thickened on the radial side by the tendons of lumbrical and interosseous muscles and on the ulnar side by the tendon of an interosseous alone or, in the case of the fifth digit, by abductor digiti minimi.
The interossei tendons join the extensor expansion at the level of the proximal portion of the proximal phalanx, while the lumbrical tendons join the extensor mechanism further distally at the mid-portion of the proximal phalanx. Their line of pull is proximal to the axis of rotation at the metacarpophalangeal joint, but dorsal to the axis of rotation at the proximal interphalangeal joint. The extensor mechanism trifurcates into a central slip and two lateral bands just proximal to the proximal interphalangeal joint. The central slip receives a contribution from the lumbrical and interosseous tendons via the lateral bands. Similarly, some fibres from the central region pass to each lateral band, producing a criss-cross arrangement of fibres. The central slip attaches to the base of the middle phalanx, while the lateral bands continue distally and eventually fuse together and insert into the distal phalanx. The tension in the central slip and the lateral bands varies as the finger moves between flexion and extension and plays a crucial role in coordinating synchronous activity between the proximal and distal interphalangeal joints.
The transverse and oblique retinacular ligaments of Landsmeer connect the fibrous flexor sheath to the extensor apparatus. The transverse retinacular ligament passes from the A3 pulley of the fibrous flexor sheath at the level of the proximal interphalangeal joint to the lateral border of the lateral extensor band. The oblique retinacular ligament lies deep to the transverse retinacular ligament. It originates from the lateral aspect of the proximal phalanx and flexor sheath (A2 pulley) and passes volar to the axis of rotation of the proximal interphalangeal joint but in a dorsal and distal direction to insert into the terminal extensor tendon.
INTRINSIC MUSCLES OF THE HAND
The intrinsic muscles of the hand are organized into three groups plus a superficial muscle. Flexor pollicis brevis, abductor pollicis brevis, opponens pollicis and adductor pollicis all act on the thumb and are known collectively as the thenar muscles. Abductor digiti minimi, flexor digiti minimi brevis and opponens digiti minimi all act on the little finger and are known collectively as hypothenar muscles. Interossei and lumbricals act on the fingers. Palmaris brevis is a superficial muscle that lies beneath the ulnar palmar skin.
Flexor pollicis brevis
Flexor pollicis brevis lies medial to abductor pollicis brevis (Fig. 50.31). It has superficial and deep parts. The superficial head arises from the distal border of the flexor retinaculum and the distal part of the tubercle of the trapezium, and passes along the radial side of the tendon of flexor pollicis longus. It is attached, by a tendon that contains a sesamoid bone, to the radial side of the base of the proximal phalanx of the thumb. The deep part arises from the trapezoid and capitate bones and from the palmar ligaments of the distal row of carpal bones, and passes deep to the tendon of flexor pollicis longus. It unites with the superficial head on the sesamoid bone and base of the first phalanx.
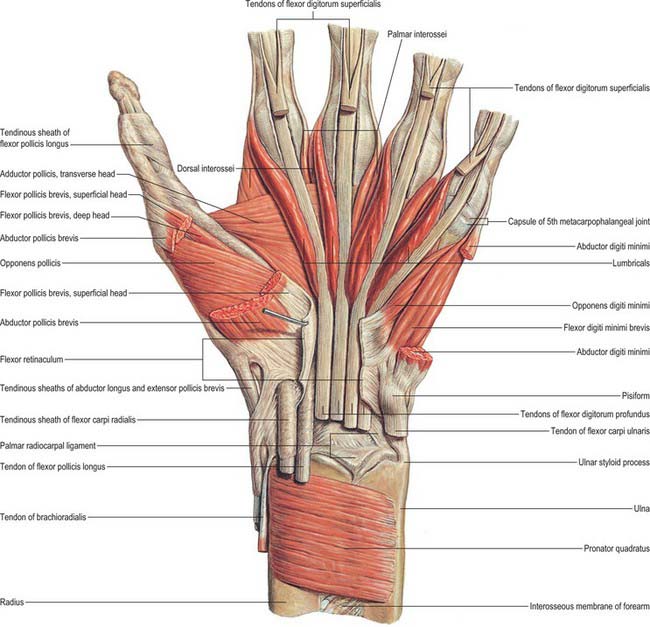
Fig. 50.31 Muscles of the left hand. Deep layer after cutting the flexor retinaculum and partial removal of several superficial muscles: palmar aspect.
(From Sobotta 2006.)
The superficial head is frequently blended with opponens pollicis. The deep head varies considerably in size and may even be absent.
Flexor pollicis brevis lies superficial in the thenar eminence and is distal to abductor pollicis brevis. It is crossed by the motor branch of the median nerve.
Flexor pollicis brevis is supplied by the superficial palmar branch of the radial artery, and branches from the princeps pollicis artery and radialis indicis artery.
Abductor pollicis brevis
Abductor pollicis brevis is a thin, subcutaneous muscle in the proximolateral part of the thenar eminence (Fig. 50.31). It arises mainly from the flexor retinaculum, but a few fibres spring from the tubercles of the scaphoid bone and trapezium, and from the tendon of abductor pollicis longus. Its medial fibres are attached by a thin, flat tendon to the radial side of the base of the proximal phalanx of the thumb, and its lateral fibres join the dorsal digital expansion of the thumb. The muscle may receive accessory slips from the long and short extensors of the thumb, opponens pollicis, or the styloid process of the radius.
Abductor pollicis brevis lies proximomedial to flexor pollicis brevis in the superficial part of the thenar eminence.
Abductor pollicis brevis is supplied by the superficial palmar branch of the radial artery, and often by an independent branch directly from the radial artery lying on the radial aspect of thumb.
Abductor pollicis brevis is innervated by the lateral terminal branch (motor branch) of the median nerve, C8 and T1. Note that this is the only muscle of the thenar eminence which is constantly supplied by the median nerve.
Abductor pollicis brevis draws the thumb ventrally in a plane at right angles to the palm of the hand (abduction).
The hand is placed with its dorsum on the table. The subject’s thumb is placed so that the nail is in a plane at right angles to the palm of the hand. The subject is instructed to touch with his thumb an object held vertically above the thumb. This is a highly specific test for a median nerve lesion.
Opponens pollicis
Opponens pollicis lies deep to abductor pollicis brevis (Fig. 50.31). It arises from the tubercle of the trapezium and the flexor retinaculum, and is attached to the whole length of the lateral border, and the adjoining lateral half of the palmar surface of the metacarpal bone of the thumb.
Opponens pollicis lies deep between the other two muscles of the thenar eminence and is only revealed when they are retracted.
Opponens pollicis is supplied by the superficial palmar branch of the radial artery, and by branches from the first palmar metacarpal artery (when present), princeps pollicis artery, radialis indicis artery and the deep palmar arch.
Adductor pollicis
Adductor pollicis arises by oblique and transverse heads (Fig. 50.31). The oblique head is attached to the capitate bone, the bases of the second and third metacarpal bones, the palmar ligaments of the carpus and the sheath of the tendon of flexor carpi radialis. Most of the fibres converge into a tendon (which contains a sesamoid bone), which unites with the tendon of the transverse head, and is attached to the ulnar side of the base of the proximal phalanx of the thumb. The deepest fibres may pass into the medial side of the dorsal digital expansion of the thumb. On the lateral side of the oblique head a considerable fasciculus passes deep to the tendon of flexor pollicis longus to join flexor pollicis brevis; this has been described as the ‘deep head’ of flexor pollicis brevis. The transverse head is the deepest of the pollicial muscles, it is triangular, and arises from the distal two-thirds of the palmar surface of the third metacarpal. The fibres converge to be attached, with the oblique head and the first palmar interosseous, to the base of the proximal phalanx of the thumb. The two parts of the adductor vary in relative size and degree of connection.
The deep palmar arch and the deep branch of the ulnar nerve pass between the two heads of the muscle. Anteriorly adductor pollicis is crossed by the flexor tendons of the index finger and their sheath, and the first lumbrical, and is overlapped by flexor pollicis brevis. Posteriorly it abuts against the first dorsal interosseous muscle: together these muscles form the mass of the first web space of the hand.
Adductor pollicis is supplied by the arteria princeps pollicis and the arteria radialis indicis (which are sometimes combined as the first palmar metacarpal artery) and by branches from the deep palmar arch.
Abductor digiti minimi
Abductor digiti minimi arises from the pisiform bone, the tendon of flexor carpi ulnaris and the pisohamate ligament (Fig. 50.31). It ends in a flat tendon which divides into two slips: one is attached to the ulnar side of the base of the proximal phalanx of the little finger, and the other to the ulnar border of the dorsal digital expansion of extensor digiti minimi.
The muscle may have two or three slips and may be fused with flexor digiti minimi brevis. An additional slip may arise from flexor retinaculum, antebrachial fascia, or tendons of palmaris longus or flexor carpi ulnaris. It may be partly attached to the fifth metacarpal by a slip from the pisiform.
Abductor digiti minimi lies along the ulnar border of flexor digiti minimi brevis and overlies opponens digiti minimi.
Abductor digiti minimi is supplied by the deep palmar branch of the ulnar artery, branches from the ulnar end of the superficial palmar arch and the palmar digital artery for the medial border of the little finger.
Flexor digiti minimi brevis
Flexor digiti minimi brevis arises from the convex surface of the hook of the hamate and the palmar surface of the flexor retinaculum. It inserts into the ulnar side of the base of the proximal phalanx of the little finger with abductor digiti minimi.
It may be absent, or fused with the abductor, and it may attach to the distal end of the fifth metacarpal by a muscular slip.
Flexor digiti minimi brevis lies lateral to the abductor. Its origin is separated from that of the abductor by the deep branches of the ulnar artery and nerve.
Flexor digiti minimi brevis is supplied by the deep palmar branch of the ulnar artery, branches from the ulnar end of the superficial palmar arch, and the palmar digital artery for the medial border of the little finger.
Opponens digiti minimi
Opponens digiti minimi is a triangular muscle, lying under cover of the flexor and abductor. It arises from the convexity of the hook of the hamate, and the contiguous portion of the flexor retinaculum, and inserts along the whole length of the ulnar margin of the fifth metacarpal bone, and the adjacent palmar surface.
The muscle is often divided into two lamellae by the deep branches of the ulnar artery and nerve. It blends to a variable degree with its neighbours.
Opponens digiti minimi lies on the ulnar margin and adjacent palmar surface of the fifth metacarpal, overlapped by, and often partly fused with, the other two muscles of the hypothenar eminence.
Opponens digiti minimi is supplied by the deep palmar branch of the ulnar artery, and branches from the medial end of the deep palmar arch.
Opponens digiti minimi flexes the fifth metacarpal bone, drawing it forwards and rotating it laterally at the carpometacarpal joint: this deepens the hollow of the palm. These actions, together with flexion and some lateral rotation at the metacarpophalangeal and interphalangeal joints, bring the digit into opposition with the thumb.
Palmaris brevis
Palmaris brevis is a thin, quadrilateral muscle, lying beneath the skin of the ulnar side of the palm (see Fig. 50.4). It arises from the flexor retinaculum and the medial border of the central part of the palmar aponeurosis, and is attached to the dermis on the ulnar border of the hand.
Palmaris brevis is superficial to the ulnar artery and the superficial terminal branch of the ulnar nerve.
Interossei
The interossei occupy the intervals between the metacarpal bones, and are divided into a palmar and a dorsal set.
Palmar interossei
Palmar interossei are smaller than dorsal interossei and lie on the palmar surfaces of the metacarpal bones rather than between them (Fig. 50.32). With the exception of the first, each of the three arises from the entire length of the metacarpal bone of one finger, and passes to the appropriate (adductor) side of the dorsal digital expansion.
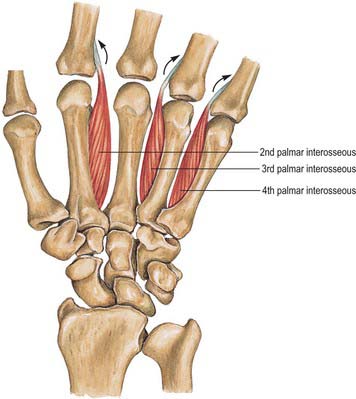
Fig. 50.32 Palmar interossei of the left hand: palmar aspect. Note that there is no first palmar interosseous in this specimen.
(From Sobotta 2006.)
The middle finger has no palmar interosseus. The remaining digits have palmar interossei on their aspects which face the middle finger. The first arises from the ulnar side of the palmar surface of the base of the first metacarpal bone, and is inserted into a sesamoid bone on the ulnar side of the proximal phalanx and from there passes to the phalanx and usually also into the dorsal digital expansion. It lies in front of the lateral head of the first dorsal interosseous, and is overlapped anteriorly by the oblique head of adductor pollicis (Fig. 50.31, Fig. 50.32). It is often very rudimentary because the thumb has its own powerful adductor. The second arises from the ulnar side of the second metacarpal bone, and is inserted into the same side of the digital expansion of the index finger. The third arises from the radial side of the fourth metacarpal bone, and is inserted together with the third lumbrical. The fourth arises from the radial side of the fifth metacarpal bone, and is attached with the fourth lumbrical and also to the base of the proximal phalanx. The attachment of these muscles to the dorsal digital expansions (Fig. 50.30) stabilizes the extensor tendons on the convex heads of the metacarpal bones during flexion and extension at the metacarpophalangeal joints.
The interossei show little variation in their arrangement. They are occasionally reduplicated.
The first palmar interosseous lies anterior to the lateral head of the first dorsal interosseous and is overlapped anteriorly by the oblique head of adductor pollicis, which also crosses anterior to the second palmar interosseous. The third and fourth are overlapped by the long flexor tendons of the ring and little finger respectively within their flexor sheaths.
Palmar interossei are supplied by branches from the deep palmar arch, princeps pollicis artery, radialis indicis artery, palmar metacarpal arteries, proximal and distal perforating arteries and common and proper digital (palmar) arteries.
Palmar interossei adduct the fingers to an imaginary longitudinal axis through the centre of the middle finger. Interossei have a considerable cross-sectional area and therefore contribute strongly to metacarpophalangeal joint flexion and interphalangeal extension. When paralysed, as in ulnar nerve paralysis, the grip strength of the hand is severely impaired and the arc of finger motion is abnormal, with a tendency for the fingers to claw. Each interosseous has a considerable ability to rotate the digit at the metacarpophalangeal joint. Generally this is not obvious, because interossei act in pairs, but it may occur where one interosseus is deficient as a result of injury or congenital deformity.
Adduction of the index, ring and little fingers against resistance. The subject grips a piece of paper between the index and middle fingers with the hand placed flat on the table. The examiner can assess the strength of adduction on trying to pull the paper away. This is a reliable test of ulnar nerve integrity.
Dorsal interossei
Dorsal interossei consist of four bipennate muscles, each arising from the adjacent sides of two metacarpal bones, but more extensively from the metacarpal bone of the finger into which the muscle passes (Fig. 50.33). They insert on the bases of the proximal phalanges and separately into the dorsal digital expansions. Between the double origin of each of these muscles there is a narrow triangular interval. The radial artery passes through the first of these intervals, and a perforating branch from the deep palmar arch passes through each of the others. The first and largest muscle is sometimes named abductor indicis. It is attached to the radial side of the proximal phalanx of the index finger and to the capsule of the adjoining metacarpophalangeal joint. The second and third are attached to the radial and ulnar sides of the middle finger, respectively. Whereas the second generally reaches the digital expansion and the proximal phalanx, the third usually extends only to the digital expansion (Fig. 50.30). The fourth may be wholly attached to the digital expansion, but it often sends an additional slip to the proximal phalanx.
The first dorsal interosseous abuts anteriorly with adductor pollicis. The other dorsal interossei occupy the spaces between the second and the fifth metacarpal bones.
Dorsal interossei are supplied by the dorsal metacarpal arteries (1st–4th), palmar metacarpal arteries (2nd–4th), radial artery (1st); princeps pollicis artery, radialis indicis artery, three perforating branches from the deep palmar arch (proximal perforating arteries), and three distal perforating branches. The tendons are supplied by branches from the common and proper palmar digital arteries and the dorsal digital arteries.
Dorsal interossei abduct the fingers from an imaginary longitudinal axis through the centre of the middle finger. See also Action of palmar interossei.
Abduction of the index, middle and ring fingers against resistance. Most conveniently, the first dorsal interosseous is tested with the subject’s fingers and palm flat upon the table. The subject tries to abduct the index finger against the examiner’s resistance. The muscle belly can be felt and seen. This provides a reliable test for the integrity of the ulnar nerve.
Lumbricals
The lumbricals are four small fasciculi which arise from the tendons of flexor digitorum profundus (Fig. 50.34). The first and second arise from the radial sides and palmar surfaces of the tendons of the index and middle fingers respectively. The third arises from the adjacent sides of the tendons of the middle and ring fingers, and the fourth from the adjoining sides of the tendons of the ring and little fingers. Each passes to the radial side of the corresponding finger, and is attached to the lateral margin of the dorsal digital expansion of extensor digitorum which covers the dorsal surface of the finger.
Variations in the attachments of the lumbricals are common. Any of them may be unipennate or bipennate. When they are bipennate, the two heads arise from adjoining tendons of flexor digitorum profundus, and, in the case of the first lumbrical, from the tendon of flexor pollicis longus. Accessory lumbrical slips may be attached to an adjacent tendon of flexor digitorum superficialis.
The first and second lumbricals are supplied by the first and second dorsal metacarpal and dorsal digital arteries. The third and fourth lumbricals are supplied by the second and third common palmar digital arteries, and the third and fourth dorsal digital arteries and their anastomoses with the palmar digital arteries.
The first and second lumbricals are innervated by the median nerve, C8 and T1, and the third and fourth lumbricals by the deep terminal branch of the ulnar nerve, C8 and T1. The third lumbrical frequently receives a supply from the median nerve. The first and second lumbricals are occasionally innervated by the deep terminal branch of the ulnar nerve.
Lumbricals arise from flexor tendons and insert into the extensor apparatus. Since both attachments are mobile, they have the potential for producing movement at either. The action on the extensor apparatus is easier to understand and consists of extension of both interphalangeal joints in a coordinated manner. The mode of action at the metacarpophalangeal joints is disputed, but if there is a flexor action it is very weak. The effect on the flexor digitorum profundus attachment is to pull the tendon distally. The combined action on both origin and insertion is therefore to alter the posture of the finger to allow more interphalangeal extension. Pinching the index finger against the thumb without a lumbrical would result in a nail-to-nail contact: the addition of the lumbrical increases the interphalangeal joint extension, and results in pulp-to-pulp pinch. Lumbricals contain many muscle spindles and have a long fibre length: it is therefore reasonable to assume that they play a role in proprioception.
Lumbricals cannot be tested in isolation, but the lumbrical–interosseous muscle complex can readily be examined together. The examiner holds the metacarpophalangeal joint of the index finger in hyperextension and the subject is the instructed to extend the two interphalangeal joints against resistance. This test is repeated seriatim on the middle, ring and little fingers.
COORDINATED MOVEMENTS OF THE HAND
The apparently simple human functions of closing the hand to grasp an object, or opening the palm to release it, are in reality tasks of considerable mechanical complexity, requiring the simultaneous contraction of many individual muscles. The isolated action of a single muscle may be inferred from the positions of its origin and insertion, and the estimated line of action (usually the centre line of the muscle) in relation to the axes of all the joints traversed by the muscle and its tendon. The limb can be regarded as a chain of joints crossed by muscles. If it is known which muscles are active, then the reason why one joint moves and others do not is a matter of simple mechanical relationships.
For example, flexor pollicis longus is considered to have a major role as a flexor of the interphalangeal joint of the thumb. However, the position of its tendon relative to more proximal joints in the limb gives it the potential for producing flexion at the metacarpophalangeal joint and also at the trapeziometacarpal and wrist joints. In the living subject the actual motion that takes place depends on which other muscle groups are acting, and so the potential for movement must be considered for each joint in the chain in turn. Motion at the wrist is generally balanced by wrist extensors. Motion at the trapeziometacarpal joint is balanced by abductor pollicis longus. Flexor pollicis longus will then have an action as a flexor of the metacarpophalangeal and interphalangeal joints only.
The factor that determines whether one or both of two joints will move is the turning moment at each. The greater the perpendicular distance from the line of muscle or tendon pull to the axis of the joint, the stronger is the turning effect of the muscle at the joint, but the smaller the range of joint motion that can be produced. In the case of flexor pollicis longus, the tendon is situated further from the axis of the metacarpophalangeal joint than from the axis of the interphalangeal joint: it will therefore tend to produce flexion preferentially at the metacarpophalangeal joint unless that joint is restrained by extensor pollicis brevis. In this way different postures of the thumb can be produced by the interplay of flexor and extensor forces. These simple guiding principles should provide an understanding of muscle action in the hand that is sufficient for most purposes.
In considering the role of a particular muscle, there is a tendency to concentrate on motion. Indeed, many muscles are named on the basis of the movements that they generate, although others – often those whose actions are the most difficult to interpret – are described according to their morphology or situation. A more important function may be the nature of the force generated. For example, although flexor pollicis longus flexes the thumb (see above), a large range of flexion is actually required in only a few activities, such as certain ripping tasks. In most pinch and manipulative tasks the role of the thumb is to apply isometric force, which it does with such precision that it is possible to pick up an egg and neither crush nor drop it. Thus for much of the time flexor pollicis longus behaves as an extremely sophisticated mechanism for the application of force, in which contraction and proprioception are equally important.
The anatomical position of the hand (palm flat and pointing anteriorly, forearm supinated) is a convenient standard for studying structural relationships. The hand in the relaxed (anaesthetized) position adopts a posture of partial flexion and mid-supination/pronation (the reader can verify this by relaxing completely and observing forearm and hand position).
SPECIAL FUNCTIONS OF THE HAND
Closing the hand
It is clear that the fingers and palm of the hand flex in gripping, grasping or making a fist, but there are subtle differences in hand posture in these various activities. The basic mechanisms of hand closure will be described before special grips are considered.
As the digits flex, the wrist usually extends (dorsiflexes) at the same time. The involvement of the long digital flexors in this movement will be considered first, followed by an analysis of the role of the wrist.
Role of the long digital flexors
Flexor digitorum superficialis acts principally to flex the proximal interphalangeal joints, through its insertions into the middle phalanges. However, in each digit it also has an action on the metacarpophalangeal joint, because the tendon passes anterior to that joint. The muscle has the potential to produce flexion at the wrist for the same reason. The fact that each tendon arises from an individual muscle slip allows the clinician to test one finger at a time. The reader can verify this by attempting to flex each digit individually while using the other hand to keep the distal interphalangeal joints of the remaining fingers in extension. This test is frequently used in clinical practice and is useful for the middle and ring fingers, where flexion of one finger alone must be attributed to flexor digitorum superficialis. The index finger, however, has its own profundus musculotendinous unit and may therefore move independently under the action of this tendon. Many individuals cannot flex the proximal interphalangeal joint of the little finger alone; usually this is because of linkage between the ring and little finger flexor digitorum superficialis tendons, but occasionally may be because superficialis is deficient. Most individuals can flex the metacarpophalangeal joint of the little finger using flexor digiti minimi.
Flexor digitorum profundus reaches further (to the distal phalanx), and is therefore the only muscle available for flexion of the distal interphalangeal joint. It also contributes, together with superficialis, to flexion at the proximal interphalangeal and metacarpophalangeal joints. These two long flexors (sometimes called extrinsic flexors, because the muscle bellies are outside the hand) can be considered to act together to flex the finger. However, their action alone would wind up the interphalangeal before the metacarpophalangeal joints and the finger would not move in a normal arc of flexion. This is precisely what happens in an ulnar nerve paralysis, in which the interossei and lumbricals are not functioning. These small (intrinsic) muscles have been described earlier in terms of their individual actions. For their role in coordinated activity it is sufficient to appreciate that their contribution changes the arc produced by the long flexors, increasing flexion at the metacarpophalangeal joint and reducing flexion at the proximal interphalangeal joint. All three joints are then angulated to the same degree and the fingers form a normal arc of flexion. As the finger flexes, the long extensor tendons (extensor digitorum, extensor indicis and extensor digiti minimi) aid the process by relaxing and allowing the extensor apparatus to glide distally on the dorsum of the phalanges. (See also p. 879.)
Role of the wrist
As the fingers wind up to make a fist, the wrist tends to extend, particularly when force is applied. This extension has a marked effect on the excursion of the long flexor tendons. On its own, digital flexion would require the long tendons to move proximally in their sheaths and the flexor muscles in the forearm would shorten. Extension of the wrist tends to produce a lengthening of the same muscles, which in normal use is almost enough to balance the shortening due to finger flexion; the net effect is a very slight shortening (approximately 1 cm) of the long flexors in the forearm. The wrist can therefore be seen as a mechanism for maximizing force, because it allows the fingers to flex while maintaining the resting length of the extrinsic muscles near to the peak of the force–length curve. It is, of course, possible to wind up the fingers with the wrist held in a neutral position, but the grip is somewhat weaker. With the wrist in full flexion it is not possible to flex the fingers fully.
Flexion of the fingers on gripping tends to result in a distal excursion of the long extensors. However, this tendency is counteracted by dorsiflexion of the wrist. The net effect is a very small proximal excursion of the long extensor tendons on gripping, mirroring the effect on the flexor surface. If the movement of the wrist is exaggerated so that the wrist is a little flexed on opening the hand, and fully dorsiflexed on closing it, the net excursion of long flexors and extensors is zero, i.e. this whole movement sequence can be completed with the forearm flexor and extensor muscles contracting isometrically.
The reader can observe the relationship between digits and wrist by performing the following manoeuvre. The wrist is held in a relaxed, mid-supinated position, with the elbow flexed at 90°. If the forearm is now rotated into pronation, the wrist will fall into flexion and the fingers will automatically extend. If the forearm is rotated into supination, the wrist will extend and the fingers flex. The finger movements compensate for the wrist movements and are entirely automatic; they are made without the need for any excursion of forearm flexor or extensor tendons. This test, the wrist tenodesis test, is a useful way of examining the limb for tendon injury. The pointing finger (which does not move with wrist motion) ‘points to’ a tendon injury.
Wrist motion is controlled principally by two wrist flexors (flexor carpi radialis and flexor carpi ulnaris) and three extensors (extensores carpi radialis longus and brevis, and extensor carpi ulnaris). Although the radiocarpal joint has some functional similarity to a ball and socket joint, it is possible to think of the wrist as a variable hinge joint, the axis of which may be set in a number of inclinations. For example, in using a hammer it is useful to rotate the wrist backwards and forwards about an axis that permits not only wrist flexion but also ulnar deviation. It would be very restricting to have a pure hinge joint with collateral ligaments of fixed length. In this context, the wrist flexors and extensors may be regarded as variable collateral ligaments which allow the joint to be set about a number of different axes.
For movement about major axes, the wrist tendons can be considered to act in pairs: flexores carpi radialis and carpi ulnaris produce wrist flexion; extensores carpi radialis longus and brevis, and extensor carpi ulnaris produce wrist extension; extensor carpi ulnaris and flexor carpi ulnaris produce ulnar deviation; flexor carpi radialis, extensores carpi radialis longus and brevis, extensor policis and abductor policis longus produce radial deviations. (See also p. 871.)
Making a tight fist
It is possible to observe and to palpate the muscle groups that are active in making a tight fist. The flexor compartment of the forearm is contracted tightly and electromyogram evidence confirms that flexor digitorum profundus and flexor digitorum superficialis are active. Flexor carpi ulnaris may be seen and felt to contract strongly. The extensor compartment is tightly contracted and the wrist extensors would certainly be expected to be active. Palpation of the long digital extensors on the back of the wrist will show these to be contracting as well. It seems that when the fingers are held tightly closed, the long digital extensors are unable to move the extensor apparatus: they have acquired a new fixed point on which to act, namely the proximal limit of the extensor apparatus over the metacarpophalangeal joint. They therefore perform the only task available to them and act together as an additional wrist extensor.
In the thumb web, palpation confirms that the first dorsal interosseous is contracting, as are all the other interossei and the thenar and hypothenar muscles. As the firm fist is swung forward in anger the brachioradialis stands out, and at the moment of impact virtually every muscle in the limb is in a state of contraction, with the exception of the lumbricals.
Opening the hand
The hand is opened from its relaxed balanced posture, e.g. when stretching out to reach an object. This motion is made up of extension of the distal interphalangeal, proximal interphalangeal and metacarpophalangeal joints. The hand is provided with an ingenious mechanism that allows this to happen. The laws of mechanics would suggest that one motor would be required for every joint in a chain, together with some sort of controlling mechanism to ensure that the chain of joints moved together in a coordinated fashion. In the hand this is achieved through an extensor apparatus which minimizes the number of motors required for movement by allowing the muscles to act on more than one joint, and by linking different levels in the mechanism so that the arc of motion is controlled.
The tendons of extensor digitorum run distally over the metacarpal heads, forming the major component of the extensor apparatus. Extensor digitorum has no insertion into the proximal phalanx and therefore exerts its extensor action on the metacarpophalangeal joint indirectly through more distal insertions. The first point of insertion is at the base of the middle phalanx (in clinical practice the term central slip has been adopted). Acting at this insertion alone, extensor digitorum can extend both metacarpophalangeal and proximal interphalangeal joints together. The interossei are also active in hand opening, since they will tend to increase extension of the proximal interphalangeal joint. There is therefore a range of possibilities. At one extreme, with no interosseous contribution, the long extensor will exert all of its action at the metacarpophalangeal joint: this leads to full extension, and even hyperextension, while the proximal interphalangeal joint remains flexed (the typical claw hand of ulnar nerve paralysis, or ‘intrinsic minus’ hand). At the other extreme, when the intrinsics act strongly together with extensor digitorum, the proximal interphalangeal joint will extend completely while the metacarpophalangeal joint remains flexed (‘intrinsic plus’ hand). Thus the hand possesses in the proximal part of the extensor apparatus a variable mechanism that allows different amounts of relative metacarpophalangeal or proximal interphalangeal joint motion.
In contrast, the more distal part of the extensor apparatus acts as an automatic or fixed mechanism which determines that the two interphalangeal joints, proximal and distal, will move together. The lateral slips of the extensor apparatus arise from extensor digitorum and pass distally on either side of the central slip and thus over the proximal interphalangeal joint: being further lateral, they are nearer the joint axis, because the dorsal surface curves away on each side. A helpful analogy that has been suggested for this arrangement is to consider it as two pulleys of different size on one axle. The central slip can be regarded as a cord that passes over the larger wheel, and each lateral slip as a cord that passes over the smaller wheel. Since these latter pulleys are smaller there is less longitudinal excursion for a given rotation of the wheel, and this allows some of the excursion to be used for another function, namely extension at the distal joint. There is an additional mechanism by which the lateral slips move laterally during flexion of the proximal interphalangeal joint. The effect of this lateral movement is to reduce further the distance between the lateral slips and the joint axis, thereby reducing the amount of excursion at the proximal interphalangeal joint still more and allowing more excursion at the distal joint. When the hand flexes, this mechanical linkage system allows both interphalangeal joints to flex together in a coordinated way.
The extensor expansion also receives contributions from the interossei and lumbricals, which approach the digits from the webs and join the corresponding expansion in the proximal segment of the digit. These small muscles can therefore act on the extensor apparatus at two levels: they can extend the proximal interphalangeal joint through fibres that radiate towards the central slip, and they can act on the distal interphalangeal joint through fibres that join the lateral slip.
Apart from the components of the extensor expansion that are concerned with joint function, the whole structure requires additional anchorage. This must be arranged in such a way that it is not displaced from the underlying skeleton, yet it must not restrict longitudinal movement. These difficult requirements are met by transverse retinacular ligaments at the level of the joints, the transverse ligaments running to relatively fixed attachment points in the region of the joint axis. As the expansion glides backwards and forwards the transverse fibres move like bucket handles. Smooth gliding layers are required under the expansion and retinacular ligaments to allow motion to occur without friction.
One final component of the extensor apparatus provides an additional automatic function. This is a fibrous anchorage system, Landsmeer’s oblique retinacular ligament, which anchors the distal expansion to the middle phalanx. The role of the oblique retinacular ligament is controversial (reviewed by Bendz 1985). Some argue it may act in a dynamic tenodesis effect to synchronize the movements of the interphalangeal joints, i.e. it may initiate extension of the distal interphalangeal joint as the proximal interphalangeal joint is extended from a fully flexed position, and relax with proximal interphalangeal joint flexion to allow full distal interphalangeal joint flexion. Others argue that it only becomes taut when the proximal interphalangeal joint is fully extended and the distal interphalangeal joint is flexed, so that it functions as a restraining force to stabilize the fingertip when it is flexed against resistance, e.g. in the hook grip. A further suggestion is that the ligament is merely a secondary lateral stabilizer of the proximal interphalangeal joint and that it acts to centralize the extensor components over the dorsum of the middle phalanx.
Movements of the thumb
An opposable thumb requires a different system of control from the other digits. Since the metacarpal is much more mobile than in the digits, muscles are needed to control the extra freedom of movement.
The thumb does not easily assume the classical anatomical position. Therefore the normal descriptive anatomical terms – anterior, posterior, medial and lateral – do not readily apply. The terms ‘palmar, dorsal, ulnar and radial’ have been adopted in clinical practice.
The basic active movements are flexion–extension, abduction–adduction, rotation, and circumduction. In the resting position of the first metacarpal, flexion and extension are parallel with the palmar plane, and abduction and adduction occur at right angles to this.
Flexion and extension should be confined to motion at the interphalangeal or metacarpophalangeal joints (Fig. 50.35A–C). Palmar abduction (Fig. 50.35D,E), in which the first metacarpal moves away from the second at right angles to the plane of the palm, and radial abduction (Fig. 50.35D,F), in which the first metacarpal moves away from the second with the thumb in the plane of the palm, occur at the carpometacarpal joint. The opposite of radial abduction is ulnar adduction, or transpalmar adduction, in which the thumb crosses the palm towards its ulnar border. In clinical practice the term adduction is generally used without qualification. Circumduction describes the angular motion of the first metacarpal, solely at the carpometacarpal joint, from a position of maximal radial abduction in the plane of the palm towards the ulnar border of the hand, maintaining the widest possible angle between the first and second metacarpals (Fig. 50.35G). Lateral inclinations of the first phalanx maximize the extent of excursion of the circumduction arc. Opposition is a composite position of the thumb achieved by circumduction of the first metacarpal, internal rotation of the thumb ray and maximal extension of the metacarpophalangeal and interphalangeal joints (Fig. 50.35H). Retroposition is the opposite to opposition (Fig. 50.35I). Flexion and adduction is the position of maximal transpalmar adduction of the first metacarpal: the metacarpophalangeal and interphalangeal joints are flexed and the thumb is in contact with the palm (Fig. 50.35J).
Rotary movements occur during circumduction. The simple angular movements described above combine with rotation about the long axis of the metacarpal shaft. In opposition, the shaft must rotate medially into pronation. In retroposition, the thumb must rotate laterally into supination. Axial rotation of the thumb metacarpal is produced by muscle activity (which moves the thumb through its arc of circumduction); the geometry of the articular surfaces of the trapeziometacarpal joint; tensile forces in the ligaments (which combine with forces exerted by the muscles of opposition and retroposition to produce axial rotation). The stability of the first metacarpal is greatest after complete pronation in the position of full opposition, when ligamentary tension, muscular contraction and joint congruence combine to maximal effect. (See also p. 875.)
Position of rest
The hand has a well-recognized position of rest, with the wrist in extension and the digits in some degree of flexion. The precise position of the thumb in the position of rest appears to be rather variable. Typically it is considered as the midpoint between maximal palmar abduction and maximal retroposition. In this position the carpometacarpal joint lies within 20° of radial abduction and 30° of palmar abduction, and from clinical observations it seems that the metacarpophalangeal joint lies within approximately 40° of flexion and the interphalangeal joint between extension and 10° of flexion.
Grips
From the position of rest, the tip of the thumb can approach the radial aspect of the fingers without incurring axial rotation because the palmar and dorsal trapeziometacarpal ligaments remain relaxed (see below).
From different positions of the arc of circumduction, numerous different types of pinch grip are possible (Fig. 50.36). In clinical practice these have been classified into two main types: tip pinch and lateral (or key) pinch. Many forces contribute to these configurations.
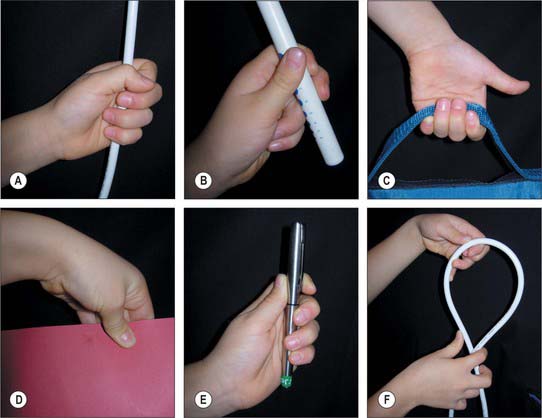
Fig. 50.36 Some of the many varieties of functional posture that may be adopted by the human hand. A, In the power grip, the fingers are flexed around an object, with counter pressure from the thumb. Any skill in wielding the object derives from the limb, including the wrist; relative movements of the thumb and fingers are not involved. B, The precision grip, which varies considerably with the task, stabilizes the object between the tips of one or more fingers and the thumb. The gross position of the object may be adjusted by movements at the wrist, elbow, or even shoulder, but the most skilled manipulations are carried out by the digits themselves, e.g. in advancing a thread through the eye of a needle. C, The hook grip is used to suspend or to pull open objects. The fingers are flexed around the object; the thumb may or may not be involved. It is a grip for the transmission of forces, not for skillful manipulation. D, Powerful opposition of the thumb to the radial side of the index finger produces a lateral pinch grip, e.g. to hold a door key; here the object is larger than a key, and all the fingers are involved. E, Many activities involve a combination of grips. Here a fountain pen is stabilized in a power grip by flexion of digits 4–5 against the palm, while the index finger and thumb, used in a precision grip, unscrew the cap. F, Complex manipulation.
(By courtesy of Olivia Pillai Johnson, Oxford.)
The thumb is a triarticular system, unlike the finger, which is a biarticular system. The thumb is activated by monoarticular muscles (abductor pollicis longus and opponens pollicis), biarticular muscles (extensor pollicis brevis, adductor pollicis, abductor pollicis brevis and flexor pollicis brevis), and triarticular muscles (extensor pollicis longus and flexor pollicis longus). It appears, however, that even a monoarticular muscle can change posture in all three joints by altering the overall balance of forces, and it is therefore very difficult to attribute function to the individual intrinsic muscles. However, the thumb muscles do seem to provide two broad functions. They control metacarpal positioning (the guy-rope function), an activity that is automatically accompanied by rotation. They also control the axial stability of the skeleton of the thumb.
The thumb muscles can be classified into those used for retroposition, opposition and pinch grip.
Retroposition muscles
The muscles that bring about retroposition are extensor pollicis longus, extensor pollicis brevis and abductor pollicis longus. As the thumb moves into retroposition, automatic axial rotation produces supination of the first metacarpal. This is produced by the off-axis action of two parallel, but oppositely directed, forces, one exerted by extensores pollicis longus and brevis and the other by abductor pollicis longus and the anterior oblique carpometacarpal ligament.
Opposition muscles
A succession of activity occurs in the thenar muscles during the movement of opposition. Three subgroups of radial (abductor pollicis longus and extensor pollicis brevis), central (abductor pollicis brevis and opponens pollicis) and ulnar (flexor pollicis brevis) muscles are involved. These forces act simultaneously but with different intensities, depending on the situation of the thumb. As the thumb moves into opposition there is automatic axial rotation of the first metacarpal shaft to produce pronation. This is produced by the paired action of oppositely directed forces: the opposition muscles provide one force, and the posterior oblique carpometacarpal ligament provides the other.
Pinch grip muscles
The muscles of pinch grip can be divided into lateral, medial and intermediate subgroups. The lateral subgroup (opposition muscles) moves the first metacarpal into palmar abduction. The metacarpal shaft rotates medially into pronation. Radial angulation at the metacarpophalangeal joint increases the span of the hand. The metacarpophalangeal joint is stabilized principally by extensor pollicis brevis and flexor pollicis brevis. Flexion of the proximal and distal phalanges is controlled. Muscles of the medial subgroup (abductor pollicis brevis and first dorsal interosseous) produce an approach of the first metacarpal towards the palm. Since they act with the lateral group they have a strong controlling effect on the position and rotation of the first metacarpal. The intermediate subgroup consists simply of flexor pollicis longus, which flexes the interphalangeal or metacarpophalangeal joint, as described earlier. Palpating the thenar eminence during tip and lateral pinch provides some appreciation of the action of the pinch grip muscles.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIES
Anastomoses occur between the radial and ulnar arteries at the wrist (via the palmar and dorsal carpal arches) and in the hand (via the superficial and deep palmar arches), and between their digital and metacarpal branches.
Radial artery
At the wrist the radial artery passes on to the dorsal aspect of the carpus between the lateral carpal ligament and the tendons of abductor pollicis longus and extensor pollicis brevis (Fig. 50.37). It crosses the scaphoid bone and trapezium (in the ‘anatomical snuff-box’), where again its pulsation is obvious, and as it passes between the heads of the first dorsal interosseous it is crossed by the tendon of extensor pollicis longus. Between the thumb extensors it is crossed by the start of the cephalic vein and the digital branches of the radial nerve which supply the thumb and index finger (Fig. 50.38). Occasionally it gives off a distal superficial dorsal branch which crosses the radial extensor tendons at the wrist together with the superficial radial nerve. Filaments of the lateral cutaneous nerve of the forearm run along its distal part as it curves round the carpus.
In the hand the radial artery passes through the first interosseous space between the heads of the first dorsal interosseous and crosses the palm. At first it lies deep to the oblique head of adductor pollicis and then passes between its oblique and transverse heads or through the transverse head. At the fifth metacarpal base it anastomoses with the deep branch of the ulnar artery, completing the deep palmar arch (Fig. 50.39).
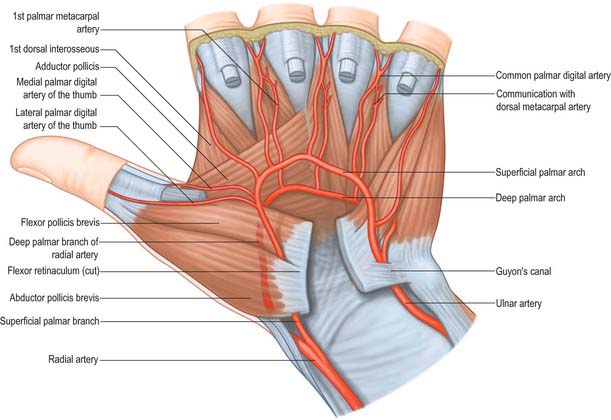
Fig. 50.39 The deep palmar arch and its branches. Note the palmar digital arteries to the thumb have a separate origin from the superficial palmar arch in this specimen; this variation occurs in 20% of cases. The princeps pollicis artery is absent in this specimen.
The palmar carpal branch is a small vessel which arises from the radial artery near the distal border of pronator quadratus (Fig. 50.40). It crosses the anterior surface of the distal end of the radius, near the palmar carpal surface, and passes medially to anastomose behind the long flexor tendons with the palmar carpal branch of the ulnar artery. This transverse anastomosis is joined by longitudinal branches from the anterior interosseous artery and recurrent branches from the deep palmar arch, to form a cruciate palmar carpal arch which supplies the carpal articulations and bones by descending branches. (Although so named, this anastomosis is usually sited near the wrist joint on the distal forearm bones.)
The superficial palmar branch arises from the radial artery just before it curves round the carpus. It passes through, and occasionally over, the thenar muscles, which it supplies, sometimes anastomosing with the end of the ulnar artery to complete a superficial palmar arch (Fig. 50.39).
The dorsal carpal branch arises deep to the thumb extensor tendons. It runs medially across the dorsal carpal surface under them and anastomoses with the ulnar dorsal carpal branch and also with the anterior and posterior interosseous arteries to form a dorsal carpal arch. The carpal arches are both close to bone and supply the distal epiphysial parts of the radius and ulna. From the dorsal arch three dorsal metacarpal arteries descend on the second to fourth dorsal interossei and bifurcate into the dorsal digital branches to supply the adjacent sides of all four fingers.
First dorsal metacarpal artery
The first dorsal metacarpal artery arises from the radial artery just before it passes between the heads of the first dorsal interosseous (Fig. 50.2). It divides almost at once into two branches which supply the adjacent sides of the thumb and index finger as far distally as the proximal interphalangeal joint. The radial side of the thumb receives a branch direct from the radial artery proper.
In the majority of cases the first dorsal metacarpal artery follows a fascial course overlying the first dorsal interosseous and parallel to the second metacarpal bone. Occasionally it may follow an intramuscular course. Distally, over the proximal phalanx, it anastomoses with the dorsal branches of the radiopalmar digital artery of the index finger. In a small number of cases, the first dorsal interosseous artery either arises from, or gives rise to, an ulnodorsal digital artery of the thumb. Occasionally it gives rise to the ulnopalmar digital artery of the thumb, and rarely may give rise to the second dorsal metacarpal artery.
The usual anatomical arrangement allows a flap of skin over the dorsum of the proximal phalanx of the index finger to be raised on this artery and its accompanying venae comitantes. This is particularly useful undercertain circumstances for reconstruction of the thumb following injury.
Second, third and fourth dorsal metacarpal arteries
The second to fourth dorsal metacarpal arteries arise from the dorsal carpal arch. Near their origins they anastomose with the deep palmar arch by proximal perforating arteries and, near their bifurcation, with dorsal perforating branches from the palmar metacarpal arteries which pass between the metacarpal necks. They also anastomose distally at the level of the web spaces with dorsal perforating branches from the palmar digital arteries from the superficial palmar arch. The third and fourth dorsal metacarpal arteries are much smaller than the first and second.
Cutaneous branches from the dorsal metacarpal arteries supply the dorsal skin as far distally as the proximal interphalangeal joint. At the level of the neck of the second, third and fourth metacarpals, a direct cutaneous branch is given off which passes proximally and supplies an area of skin between the two adjacent metacarpals (Fig. 50.41).
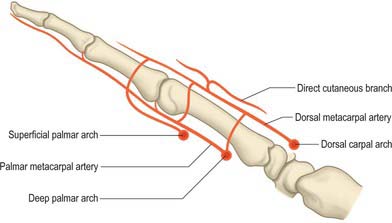
Fig. 50.41 Sagittal view showing communication between the palmar and dorsal metacarpal arteries and the direct cutaneous branch given off the dorsal metacarpal artery approximately 0.5–1.0 cm proximal to the metacarpophalangeal joint.
These anatomical arrangements permit the surgical elevation of flaps of dorsal skin to be based either proximally on the dorsal metacarpal arteries proper, or distally on the direct cutaneous branch. These flaps may be used for reconstructing areas of missing tissue elsewhere in the hand.
The arteria princeps pollicis arises from the radial artery as it turns into the palm to form the deep palmar arch. It descends on the palmar aspect of the first metacarpal under the oblique head of adductor pollicis lateral to the first palmar interosseous. At the base of the proximal phalanx, deep to the tendon of flexor pollicis longus, the artery divides into two branches. It appears between the medial and lateral attachments of the oblique head of adductor pollicis to run along both sides of the thumb. On the palmar surface of its distal phalanx it forms a pollicial arch which supplies the skin and subcutaneous tissue. The arteria princeps pollicis is the usual nutrient of supply to the first metacarpal bone.
The arteria radialis indicis is often a proximal branch of the arteria princeps pollicis. It descends between the first dorsal interosseous and transverse head of adductor pollicis, and along the lateral side of the index finger to its end (Fig. 50.37). It anastomoses with the indicial medial digital artery. At the distal border of the transverse head of adductor pollicis it anastomoses with the arteria princeps pollicis and links with the superficial palmar arch. It may arise from the superficial arch or from the first dorsal metacarpal artery.
The arteria princeps pollicis and radialis indicis may be combined as the first palmar metacarpal artery.
The deep palmar arch is formed by anastomosis of the end of the radial artery with the deep palmar branch of the ulnar artery (Fig. 50.39 and Fig. 50.42A). It crosses the bases of the metacarpal bones and interossei, covered by the oblique head of adductor pollicis, the digital flexor tendons and lumbricals. In its concavity, running laterally, is the deep branch of the ulnar nerve. Rarely the arch is incomplete. There are variations in the size of contribution from the ulnar artery.
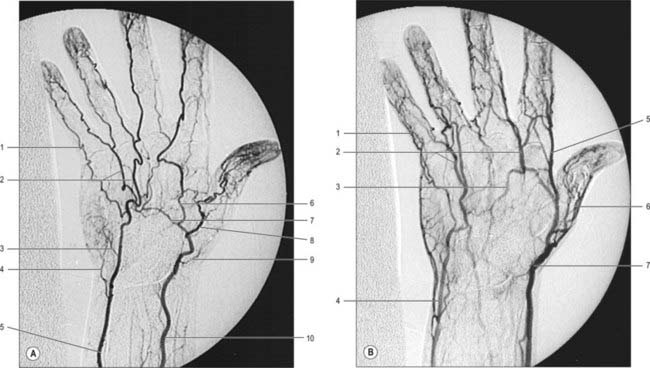
Fig. 50.42 A, Digitally subtracted hand arteriogram, dorsopalmar projection. Note that this patient has an incomplete superficial palmar arch. B, Venous phase of hand arteriogram. A, 1. Proper palmar digital artery. 2. Common palmar digital artery. 3. Palmar carpal branch of ulnar artery. 4. Deep palmar branch of ulnar artery. 5. Ulnar artery. 6. Palmar metacarpal artery. 7. Deep palmar arch. 8. Princeps pollicis artery. 9. Artery to radial aspect of thumb. 10. Radial artery. B, 1. Palmar digital vein. 2. Common palmar digital vein. 3. Superficial palmar arch. 4. Basilic vein. 5. Radialis indicis vein. 6. Princeps pollicis vein. 7. Cephalic vein.
(By permission from Weir J, Abrahams PH 2003 Imaging Atlas of Human Anatomy, 3rd edn, London: Mosby, and contributions from Anna-Maria Belli, Margaret Hourihan, Niall Moore and Philip Owen.)
The three palmar metacarpal arteries run distally from the convexity of the deep palmar arch on the interossei of the second to fourth spaces, and join the common digital branches of the superficial arch at the digital clefts (Fig. 50.39). They supply nutrient branches to the medial four metacarpals.
Ulnar artery
At the wrist the ulnar artery (Figs 50.37 and 50.39) is covered by skin, fasciae and palmaris brevis. It lies between the superficial and main parts of the flexor retinaculum, lateral to the ulnar nerve and pisiform.
A constant dorsoulnar perforator vessel is given off distally. It arises 2–5 cm proximal to the pisiform and accompanies the dorsal cutaneous branch of the ulnar nerve. It emerges between flexor carpi ulnaris and extensor carpi ulnaris. The cutaneous perforator can support a flap of skin on the medial aspect of the distal forearm just proximal to the wrist and is useful in reconstructing areas of missing skin in this region.
A small palmar carpal branch crosses the distal ulna deep to the tendons of flexor digitorum profundus (Fig. 50.40), and anastomoses with a palmar carpal branch of the radial artery to make a palmar carpal arch.
A dorsal carpal branch arises just proximal to the pisiform (Fig. 50.40). It curves deep to the tendon of flexor carpi ulnaris to reach the carpal dorsum, which it crosses laterally beneath the extensor tendons. It anastomoses with the dorsal carpal branch of the radial artery to complete the dorsal carpal arch. Near its origin it sends a small digital branch along the ulnar side of the fifth metacarpal to supply the medial side of the dorsal surface of the fifth finger.
The deep palmar branch is often double (Fig. 50.40). It passes between abductor and flexor digiti minimi, through or deep to opponens digiti minimi. It anastomoses with the radial artery, completing the deep palmar arch. The deep palmar branch accompanies the deep branch of the ulnar nerve.
Superficial palmar arch
The superficial palmar arch is an anastomosis fed mainly by the ulnar artery (Figs 50.2 and 50.39). The latter enters the palm with the ulnar nerve, anterior to the flexor retinaculum and lateral to the pisiform. It passes medial to the hook of the hamate, then curves laterally to form an arch that is convex distally and level with a transverse line through the distal border of the fully extended pollicial base. About a third of the superficial palmar arches are formed by the ulnar artery alone; a further third are completed by the superficial palmar branch of the radial artery; and a third by the arteria radialis indicis, a branch of either arteria princeps pollicis or the median artery. The superficial palmar arch is covered by palmaris brevis and the palmar aponeurosis and it is superficial to flexor digiti minimi, branches of the median nerve and the long flexor tendons and lumbricals.
Common and proper palmar digital arteries
Three common palmar digital arteries arise from the convexity of the superficial palmar arch (Fig. 50.39). They pass distally on the second to fourth lumbricals, each joined by a corresponding palmar metacarpal artery from the deep palmar arch, and divide into two proper palmar digital arteries. These run along the contiguous sides of all four fingers, dorsal to the digital nerves, between Grayson’s and Cleland’s ligaments, anastomosing in the subcutaneous tissue of the finger tips and near the interphalangeal joints. Each digital artery has two dorsal branches which anastomose with the dorsal digital arteries and supply the soft parts dorsal to the middle and distal phalanges, including the matrices of the nails. The palmar digital artery for the medial side of the little finger leaves the arch under palmaris brevis. Palmar digital arteries supply the metacarpophalangeal and interphalangeal joints and nutrient rami to the phalanges. They are the main digital supply, because the dorsal digital arteries are minute.
The origins of the palmar digital arteries of the thumb are quite variable. Both may arise from a single princeps pollicis, or they may arise separately from the superficial palmar arch. The ulnar digital artery may arise from the first dorsal metacarpal artery.
The terminal branches of the digital arteries contribute to a number of vascular arcades which provide a rich vascular supply for the distal elements of each digit (Fig. 50.43). Three distal phalangeal dorsal arterial arcades anastomose with each other and with those from the other side of the digit. The superficial arcade occurs at the level of the proximal nailfold and is supplied primarily by a dorsal branch from the palmar digital artery, which is given off at the level of the middle phalanx. The proximal subungual arcade is at the level of the lunula and is supplied by a terminal branch of the digital artery, which passes dorsally. The distal subungual arcade occurs more distally in the nail bed. It is supplied by a dorsal vessel which emerges from the point of confluence of the ‘H’-shaped anastomosis between the terminal portions of both digital arteries, and passes from volar to dorsal aspect of the digit under the interosseous ligament which connects the proximal and distal parts of the distal phalanx (Fig. 50.43).
Glomus tumours are very painful (often tiny and sometimes difficult to identify) tumours of the glomus bodies (small AV anastomoses involved in the regulation of peripheral skin temperature control; see Fig. 6.16). These typically occur in the proximal nailfold/subungual regions of the finger tips in association with the dorsal digital arterial arcades, although they can occur anywhere. They are diagnosed by exquisite point tenderness over the swelling with reduction of tenderness when the finger is exsanguinated. If the tumour is not visible (as is often the case) then the best way surgically to explore the dorsal fingertip region to look for the tumour is to incise the lateral nailfold and hyponychium and raise this as a flap along with the underlying periosteum pedicled on the blood supply from the opposite nailfold. The dorsal distal phalangeal digital arterial arcades are then identified from their deep surface and any glomus tumour identified.
VEINS
Superficial veins of the hand
Dorsal and palmar digital veins
Dorsal digital veins pass along the sides of the fingers, joined by oblique branches. They unite from the adjacent sides of the digits into three dorsal metacarpal veins (Fig. 50.44), which form a dorsal venous network over the metacarpus. This is joined laterally by a dorsal digital vein from the radial side of the index finger and both dorsal digital veins of the thumb, and is prolonged proximally as the cephalic vein (Fig. 50.42). Medially a dorsal digital vein from the ulnar side of minimus joins the network, which ultimately drains proximally into the basilic vein. A vein often connects the central parts of the network to the cephalic vein near the midforearm.
Palmar digital veins connect to their dorsal counterparts by oblique intercapitular veins which pass between metacarpal heads. They also drain to a plexus superficial to the palmar aponeurosis, extending over both thenar and hypothenar regions.
Deep veins of the hand
Superior and deep palmar venous arches
Superficial and deep palmar venous arches accompany their arterial counterparts and receive the corresponding branches. Thus common palmar digital veins join the superficial arch, and palmar metacarpal veins join the deep arch.
Palmar and dorsal metacarpal veins
Deep veins accompanying the dorsal metacarpal arteries receive perforating branches from the palmar metacarpal veins. They end in the radial veins and the dorsal venous network over the metacarpus. This network is joined laterally by a dorsal digital vein from the radial side of the index finger and by both digital veins of the thumb, and is prolonged proximally as the cephalic vein.
INNERVATION
Median nerve
The median nerve proximal to the flexor retinaculum is lateral to the tendons of flexor digitorum superficialis and lies between the tendons of flexor carpi radialis and palmaris longus (Fig. 50.45A). It passes under the retinaculum in the ‘carpal tunnel’ where it may be compressed in the carpal tunnel syndrome (see p. 897). Distal to the retinaculum the nerve enlarges and flattens, and usually divides into five or six branches: the mode and level of division are variable.
Palmar cutaneous branch
The palmar cutaneous branch starts about 3 cm proximal to the flexor retinaculum. It runs in a small tunnel in the sheath of flexor carpi radialis before piercing the deep fascia where it divides into lateral branches that supply the thenar skin and connect with the lateral cutaneous nerve of the forearm. Medial branches supply the central palmar skin and connect with the palmar cutaneous branch of the ulnar nerve.
Communicating branches, which may be multiple, often arise in the proximal forearm, sometimes from the anterior interosseous branch. They pass medially between flexores digitorum superficialis and profundus and behind the ulnar artery to join the ulnar nerve. This communication is a factor in explaining anomalous muscular innervation in the hand (see below).
Muscular branch (motor or recurrent branch)
The muscular branch is short and thick, and arises from the lateral side of the nerve; it may be the first palmar branch or a terminal branch which arises level with the digital branches. It runs laterally, just distal to the flexor retinaculum, with a slight recurrent curve beneath the part of the palmar aponeurosis covering the thenar muscles (Fig. 50.45A). It turns round the distal border of the retinaculum to lie superficial to flexor pollicis brevis, which it usually supplies, and continues either superficial to the muscle or traverses it. It gives a branch to abductor pollicis brevis, which enters the medial edge of the muscle, and then passes deep to it to supply opponens pollicis, entering its medial edge. Its terminal part occasionally gives a branch to the first dorsal interosseous, and may be its sole or partial supply. The muscular branch may arise in the carpal tunnel and pierce the flexor retinaculum, a point of surgical importance.
Palmar digital branches
The median nerve usually divides into four or five digital branches (Fig. 50.45A). It often divides first into a lateral ramus which provides digital branches to the thumb and the radial side of the index finger, and a medial ramus, which supplies digital branches to adjacent sides of the index, middle and ring fingers. Other modes of termination can occur.
Digital branches are commonly arranged as follows. They pass distally, deep to the superficial palmar arch and its digital vessels, at first anterior to the long flexor tendons. Two proper palmar digital nerves, sometimes from a common stem, pass to the sides of the thumb: the nerve supplying its radial side crosses in front of the tendon of flexor pollicis longus. The proper palmar digital nerve to the lateral side of the index also supplies the first lumbrical. Two common palmar digital nerves pass distally between the long flexor tendons. The lateral divides in the distal palm into two proper palmar digital nerves which traverse adjacent sides of the index and middle finger. The medial divides into two proper palmar digital nerves which supply adjacent sides of the middle and ring fingers. The lateral common digital nerve supplies the second lumbrical, and the medial receives a communicating twig from the common palmar digital branch of the ulnar nerve and may supply the third lumbrical. In the distal part of the palm the digital arteries pass deeply between the divisions of the digital nerves: the nerves lie anterior to the arteries on the sides of the digits. The median nerve usually supplies palmar cutaneous digital branches to the radial three and one-half digits (thumb, index, middle and the lateral side of the ring): sometimes the radial side of the ring finger is supplied by the ulnar nerve. Occasionally, there is a communicating branch between the common digital nerve to the middle and ring fingers (derived from the median nerve) and the common digital nerve to the ring and little fingers (derived from the ulnar nerve): this can explain variations in sensory patterns that do not conform to the classic pattern.
The proper palmar digital nerves pass along the medial side of the index finger, and both sides of the middle and the lateral side of the ring finger. They enter these digits in fat between slips of the palmar aponeurosis. Together with the lumbricals and palmar digital arteries, they pass dorsal to the superficial transverse metacarpal ligament and ventral to the deep transverse metacarpal ligament. In the digits, the nerves run distally beside the long flexor tendons (outside their fibrous sheaths), level with the anterior phalangeal surfaces and anterior to the digital arteries, between Grayson’s and Cleland’s ligaments. Each nerve gives off several branches to the skin on the front and sides of the digit (where many end in Pacinian corpuscles), and sends branches to the metacarpophalangeal and interphalangeal joints.
The digital nerves supply the fibrous sheaths of the long flexor tendons, digital arteries (vasomotor) and sweat glands (secretomotor). Distal to the base of the distal phalanx each digital nerve gives off a branch which passes dorsally to the nail bed. The main nerve frequently trifurcates to supply the pulp and skin of the terminal part of the digit. Distal to the base of the proximal phalanx, each proper digital nerve also gives off a dorsal branch to supply the skin over the back of the middle and distal phalanges. The proper palmar digital nerves to the thumb and the lateral side of the index finger emerge with the long flexor tendons from under the lateral edge of the palmar aponeurosis. They are arranged in the digits as described above, but in the thumb small distal branches supply the skin on the back of the distal phalanx only.
Other branches
In addition to the branches of the median nerve described above, variable vasomotor branches supply the radial and ulnar arteries and their branches. Some of the intercarpal, carpometacarpal and intermetacarpal joints are said to be supplied by the median nerve or its anterior interosseous branch: the precise details are uncertain.
Carpal tunnel syndrome
Carpal tunnel syndrome is the most common entrapment mononeuropathy. It is caused by compression of the median nerve as it passes through the fibro-osseous tunnel beneath the flexor retinaculum. The carpal tunnel may be narrowed by arthritic changes in the wrist joint, particularly rheumatoid arthritis; soft tissue thickening as may occur in myxoedema and acromegaly; and may also be associated with oedema, obesity or pregnancy. Usually the condition is idiopathic. Normally the median nerve slides smoothly in and out of the carpal tunnel during flexion and extension of the wrist: when the nerve is compressed, additional damage may be produced during these movements. The dominant hand is usually affected first, probably because this hand is used more frequently and more vigorously. Typically, the syndrome produces pain, paraesthesia and numbness in the thumb, index, middle and medial side of the ring finger, which is worse at night and on gripping objects. The palmar branch of the median nerve is spared since it does not pass through the carpal tunnel. With time, the compression leads to wasting and weakness of abductor pollicis brevis. Treatment is usually surgical decompression of the nerve by dividing the flexor retinaculum.
Median nerve division at the wrist
The median nerve is vulnerable to division from lacerations at the wrist. Division leads to paralysis of the lumbricals to the index and middle fingers and the thenar muscles (apart from flexor pollicis brevis and adductor pollicis), as well as loss of sensation to the thumb, index, middle and radial half of the ring fingers. The radial half of the hand becomes flattened as a result of wasting of the thenar muscles and the adducted posture of the thumb.
Ulnar nerve
At the wrist, the ulnar nerve passes under the superficial part of the flexor retinaculum (in Guyon’s canal) with the ulnar artery, and divides into superficial and deep terminal branches.
Dorsal branch
The dorsal branch arises approximately 5 cm proximal to the wrist. It passes distally and dorsally, deep to flexor carpi ulnaris, perforates the deep fascia, descends along the medial side of the back of the wrist and hand and then divides into two, or often three, dorsal digital nerves. The first supplies the medial side of the little finger, the second, the adjacent sides of the little and ring fingers, while the third, when present, supplies adjoining sides of the ring and middle fingers. The latter may be replaced, wholly or partially, by a branch of the radial nerve, which always communicates with it on the dorsum of the hand (Fig. 50.45A). In the little finger, the dorsal digital nerves extend only to the base of the distal phalanx, and in the ring finger they extend only to the base of the middle phalanx. The most distal parts of the little finger and of the ulnar side of the ring finger are supplied by dorsal branches of the proper palmar digital branches of the ulnar nerve. The most distal part of the lateral side of the ring finger is supplied by dorsal branches of the proper palmar digital branch of the median nerve.
Superficial and deep terminal branches
Superficial terminal branch
The superficial terminal branch supplies palmaris brevis and the medial palmar skin. It divides into two palmar digital nerves, which can be palpated against the hook of the hamate bone. One supplies the medial side of the little finger, the other (a common palmar digital nerve) sends a twig to the median nerve and divides into two proper digital nerves to supply the adjoining sides of little and ring fingers. The proper digital branches are distributed like those derived from the median nerve.
Deep terminal branch
The deep terminal branch accompanies the deep branch of the ulnar artery as it passes between abductor digiti minimi and flexor digiti minimi and then perforates opponens digiti minimi to follow the deep palmar arch dorsal to the flexor tendons (Fig. 50.46). At its origin it supplies the three short muscles of the little finger. As it crosses the hand, it supplies the interossei and the third and fourth lumbricals. It ends by supplying adductor pollicis, the first palmar interosseous and usually flexor pollicis brevis. It sends articular filaments to the wrist joint.
The medial part of flexor digitorum profundus is supplied by the ulnar nerve, as are the third and fourth lumbricals which are connected with the tendons of this part of the muscle. Similarly, the lateral part of flexor digitorum profundus and the first and second lumbricals are supplied by the median nerve. The third lumbrical is often supplied by both nerves. The deep terminal branch is said to give branches to some intercarpal, carpometacarpal and intermetacarpal joints: precise details are uncertain. Vasomotor branches, arising in the forearm and hand, supply the ulnar and palmar arteries.
Ulnar tunnel syndrome
Ulnar tunnel syndrome is an entrapment neuropathy of the ulnar nerve as it passes through Guyon’s canal at the wrist. Causes of compression at this site include a ganglion, trauma, and proximity of aberrant or accessory muscles. The symptoms include pain in the hand or forearm and sensory changes in the palmar aspect of the little and ulnar half of the ring fingers, however sensation on the ulnar aspect of the dorsum of the hand is normal. In addition there may be weakness and wasting of the intrinsic muscles of the hand supplied by the ulnar nerve, with clawing posture in extreme cases.
Surgical treatment involves decompression of the nerve by division of the roof of Guyon’s canal and removal of the causative lesion, e.g. ganglion.
Ulnar nerve division at the wrist
Division of the ulnar nerve at the wrist paralyses all the intrinsic muscles of the hand (apart from the radial two lumbricals). The intrinsic muscle action of flexing the metacarpophalangeal joint and extending the interphalangeal joints is therefore lost. The unopposed action of the long extensors and flexors of the fingers cause the hand to assume a clawed appearance with extension of the metacarpophalangeal joints and flexion of the interphalangeal joints. The clawing is less intense in the index and middle fingers because of their intact lumbricals, supplied by the median nerve. (For a detailed account of the hand posture adopted in ulnar nerve lesions, see Smith 2002.)
There is sensory loss over the little finger and the ulnar half of the ring finger. In comparison to an ulnar nerve division at the elbow, the skin over the ulnar aspect of the dorsum of the hand is spared because the dorsal branch of the ulnar nerve is given off approximately 5 cm proximal to the wrist joint.
A combined median and ulnar nerve palsy at the wrist results in a full claw hand with thenar and hypothenar flattening, and thumb adduction and flexion. This posture is known as a simian hand because of the similarity to the appearance of the hand of an ape.
Radial nerve
Branches of the superficial branch of the radial nerve reach the hand by curving around the wrist over the tendons of abductor pollicis longus and extensor pollicis brevis. They divide into dorsal digital nerves. On the dorsum of the hand they usually communicate with the posterior and lateral cutaneous nerves of the forearm.
Dorsal digital nerves
There are usually four or five small dorsal digital nerves. The first supplies the skin of the radial side of the thumb and the adjoining thenar eminence, and communicates with branches of the lateral cutaneous nerve of the forearm. The second supplies the medial side of the thumb; the third, the lateral side of the index finger; the fourth, the adjoining sides of the index and middle fingers; the fifth communicates with a ramus of the dorsal branch of the ulnar nerve and supplies the adjoining sides of the middle and ring fingers, but is frequently replaced by the dorsal branch of the ulnar nerve. The pollicial digital nerves reach only to the root of the nail, those in the index finger, midway along the middle phalanx, those to the middle and the lateral part of the ring finger may reach no further than the proximal interphalangeal joints. The remaining distal dorsal areas of the skin in these digits are supplied by palmar digital branches of the median and ulnar nerves. The superficial terminal branch of the radial nerve may supply the whole dorsum of the hand.
An K-N, Berger RA, Cooney WP. Biomechanics of the Wrist Joint. New York: Springer-Verlag, 1991.
Bendz P. The functional significance of the oblique retinacular ligament of Landsmeer. A review and new proposals. J Hand Surg. 1985;10:25-29.
Bowers WH, Wolf JWJr, Nehil JL, Bittinger S. The proximal interphalangeal joint volar plate. I. An anatomical and biochemical study. J Hand Surg [Am]. 1980;5:79-88.
Cormack GC, Lamberty BGH. The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone, 1994.
Doyle JR, Blythe WF. The finger flexor tendon sheath and pulleys: anatomy and reconstruction. In: AAOS Symposium on Tendon Surgery in the Hand. St Louis: Mosby; 1975:81-88.
Garcia-Elias M. Carpal kinetics. In: Büchler V, editor. Wrist Instability. London: Martin Dunitz, 1996. Chapter 2.
Green D, Hotchkiss R, Pederson W. Green’s Operative Hand Surgery, 4th edn. New York: Churchill Livingstone, 1999.
Kauer JMG. The functional anatomy of the carpal joint: the whole and its components. In: Wrist Instability. London: Martin Dunitz; 1996.
Kirk Watson H, Weinzweig J. The Wrist. Philadelphia: Lippincott, Williams & Wilkins, 2001.
McGrouther D. The microanatomy of Dupuytren’s contracture. The Hand. 1982;14:215-236.
Salmon M. Anatomic studies. In: Taylor GI, Razaboni RM. Book 1: Arteries of the muscles of the extremities and the trunk. Book 2: Arterial anastomotic pathways of the extremities. St Louis: Quality Medical Publishing, 1994.
Smith PJ. Lister’s The Hand. Diagnosis and Indications. 4th edn.. Edinburgh: Churchill Livingstone; 2002.
Spinner MJB. Kaplan’s Functional and Surgical Anatomy of the Hand, 3rd edn. Philadelphia: Lippincott, Williams & Wilkins, 1984.
Stanley J, Saffar P. Anatomy. In: Wrist Arthroscopy. London: Martin Dunitz; 1994.
Watson HK, Weinzweig J. The Wrist. Philadelphia: Lippincott Williams and Wilkins, 2001.
In particular the following chapters in this book: Garcia-Elias M, Anatomy of the wrist; and Ryu J, Biomechanics of the wrist..