CHAPTER 69 Gallbladder and biliary tree
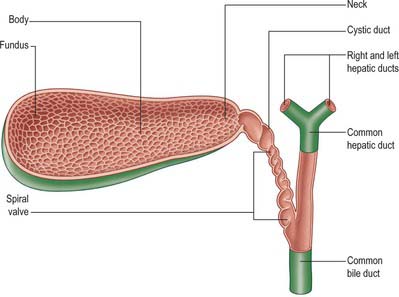
The biliary tree consists of the system of vessels and ducts which collect and deliver bile from the liver parenchyma to the second part of the duodenum. It is conventionally divided into intrahepatic and extrahepatic biliary trees. The intrahepatic ducts are formed from the larger bile canaliculi which come together to form segmental ducts. These fuse close to the porta hepatis into right and left hepatic ducts. The extrahepatic biliary tree consists of the right and left hepatic ducts, the common hepatic duct, the cystic duct and gallbladder and the common bile duct (Fig. 69.1).
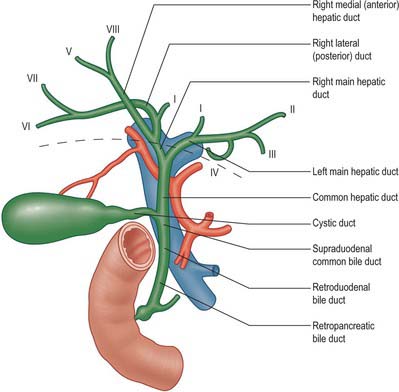
Fig. 69.1 Overall arrangement of the intrahepatic and extrahepatic biliary tree. The segmental ducts often branch just before, or are multiple, as they enter the main ducts, but for clarity are shown here as single ducts. Note that segment I usually has drainage from both right and left hepatic ducts. The level of the liver parenchyma at the porta hepatis is shown by the dashed brown line.
GALLBLADDER
The gallbladder is a flask-shaped, blind-ending diverticulum attached to the common bile duct by the cystic duct. In life, it is grey-blue in colour and usually lies attached to the inferior surface of the right lobe of the liver by connective tissue (Fig. 69.2). In the adult the gallbladder is between 7 and 10 cm long with a capacity of up to 50 ml. It usually lies in a shallow fossa in the liver parenchyma covered by peritoneum continued from the liver surface. This attachment can vary widely. At one extreme the gallbladder may be almost completely buried within the liver surface, having no peritoneal covering (intraparenchymal pattern); at the other extreme it may hang from a short mesentery formed by the two layers of peritoneum separated only by connective tissue and a few small vessels (mesenteric pattern). The gallbladder is described as having a fundus, body and neck. The neck lies at the medial end close to the porta hepatis, and almost always has a short peritoneal-covered attachment to the liver (mesentery); this mesentery usually contains the cystic artery. The mucosa at the medial end of the neck is obliquely ridged, forming a spiral groove continuous with the spiral valve of the cystic duct. At its lateral end the neck widens out to form the body of the gallbladder and this widening is often referred to in clinical practice as ‘Hartmann’s pouch’. The neck lies anterior to the second part of the duodenum.
The body of the gallbladder normally lies in contact with the liver surface. When the neck possesses a mesentery, this rapidly shortens along the length of the body as it comes to lie in the gallbladder fossa. It lies anterior to the second part of the duodenum and the right end of the transverse colon. The fundus lies at the lateral end of the body and usually projects past the inferior border of the liver to a variable length. It often lies in contact with the anterior abdominal wall behind the ninth costal cartilage where the lateral edge of the right rectus abdominis crosses the costal margin. This is the location where enlargement of the gallbladder is best sought on clinical examination. The fundus commonly lies adjacent to the transverse colon.
The gallbladder varies in size and shape. The fundus may be elongated and highly mobile. Rarely, the fundus is folded back upon the body of the gallbladder, the so-called Phrygian cap: on ultrasound, this may be wrongly interpreted as an apparent septum within an otherwise normal gallbladder. Again, rarely, the gallbladder may be bifid or completely duplicated, usually with a duplicated cystic duct.
INTRAHEPATIC BILIARY TREE
SEGMENTAL AND SECTORAL DUCTS
The segmental ducts of the left liver have a relatively constant pattern, although several segmental ducts may drain each particular segment. The left hepatic duct is formed by the union of segment II and III ducts behind the umbilical portion of the left portal vein (Fig. 69.1). The segment IV duct is more variable, but usually drains into the left hepatic duct. The right hepatic duct is formed by the union of the right medial (anterior) and lateral (posterior) sectoral ducts. These sectoral ducts in turn are formed by the segmental ducts: VII and VI from the lateral, and VIII and V from the medial duct. The right lateral sectoral duct is often identified on a cholangiogram as curving around the right medial duct before joining the medial side of the medial sectoral duct: this is often described as Hjortsjo’s crook, and has surgical importance for liver resections. The right hepatic duct and its branches are subject to more variations than the left ductal system, and these variations have been classified by Blumgart into six main types (Table 69.1).
Table 69.1 Variations of the right hepatic duct and its branches
| Type | Percentage of population | Description |
|---|---|---|
| A | 55 | Anatomy is normal. |
| B | 15 | There is no right hepatic duct and the common hepatic duct is formed by the right anterior, right posterior and left hepatic ducts as a trifurcation. |
| C | 20 | There is a low drainage of one the right sectoral ducts into the common hepatic duct. |
| D | 5 | One of the right sectoral ducts joins the left hepatic duct. |
| E | 5 | The common hepatic duct is formed by the union of two or more ducts from either lobe. |
| F | 5 | The right posterior sectoral duct drains into the cystic duct. |
EXTRAHEPATIC BILIARY TREE
CYSTIC DUCT
The cystic duct drains the gallbladder into the common bile duct. It is between 3 and 4 cm long, passes posteriorly to the left from the neck of the gallbladder, and joins the common hepatic duct to form the common bile duct. It almost always runs parallel to, and is adherent to, the common hepatic duct for a short distance before joining it. The junction usually occurs near the porta hepatis but may be lower down in the free edge of the lesser omentum. The cystic duct may have several important variations in its anatomy (Fig. 69.3). Rarely, the cystic duct lies along the right edge of the lesser omentum all the way down to the level of the duodenum before the junction is formed, but in these cases the cystic and common bile ducts are usually closely adherent. The cystic duct occasionally drains into the right hepatic duct, in which case it may be elongated, lie anterior or posterior to the common hepatic duct, and join the right hepatic duct on its left border. Rarely, the duct is double or even absent, in which case the gallbladder drains directly into the common bile duct. One or more accessory hepatic ducts occasionally emerge from segment V of the liver and join either the right hepatic duct, the common hepatic duct, the common bile duct, the cystic duct, or the gallbladder directly. These variations in cystic duct anatomy are of considerable importance during surgical excision of the gallbladder. Ligation or clip occlusion of the cystic duct must be performed at an adequate distance from the common bile duct to prevent angulation or damage to it. Accessory ducts must not be confused with the right hepatic or common hepatic ducts.
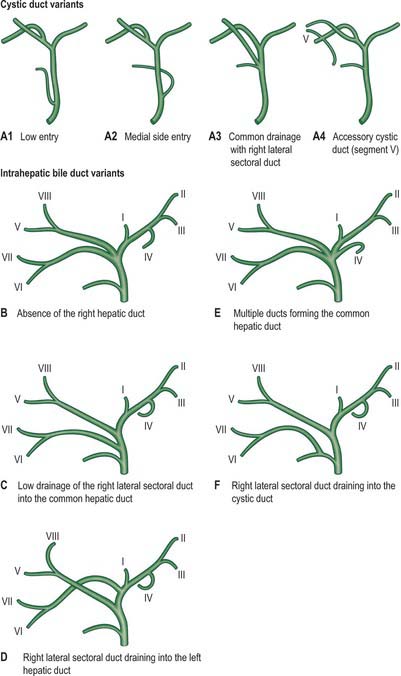
Fig. 69.3 Variations in the anatomy of the cystic and intrahepatic bile ducts. The cystic duct variations are labelled A1–A3 and the letters B–F are used for the variants of the intrahepatic ducts to ensure consistency with the Blumgart nomenclature.
The mucosa of the cystic duct bears 5–12 crescentic folds, continuous with those in the neck of the gallbladder. They project obliquely in regular succession, appearing to form a spiral valve when the duct is cut in longitudinal section. When the duct is distended, the spaces between the folds dilate and externally it appears twisted like the neck of the gallbladder.
HEPATIC BILE DUCTS
The main right and left hepatic ducts emerge from the liver and unite near the right end of the porta hepatis as the common hepatic duct. The extrahepatic right duct is short and nearly vertical while the left is more horizontal and lies along the base of segment IV. The common hepatic duct descends approximately 3 cm before being joined on its right at an acute angle by the cystic duct to form the common bile duct. The common hepatic duct lies to the right of the hepatic artery and anterior to the portal vein in the free edge of the lesser omentum.
COMMON BILE DUCT
The common bile duct is formed near the porta hepatis, by the junction of the cystic and common hepatic ducts (Figs 69.4 and 69.5), and is usually between 6 and 8 cm long. Its diameter tends to increase somewhat with age but is usually around 6 mm in adults. It descends posteriorly and slightly to the left, anterior to the epiploic foramen, in the right border of the lesser omentum, where it lies anterior and to the right of the portal vein and to the right of the hepatic artery. It passes behind the first part of the duodenum with the gastroduodenal artery on its left, and then runs in a groove on the superolateral part of the posterior surface of the head of the pancreas. The duct lies anterior to the inferior vena cava and is sometimes embedded in the pancreatic tissue. It may lie close to the medial wall of the second part of the duodenum or as much as 2 cm from it: even when it is embedded in the pancreas, a groove in the gland marking its position can be palpated behind the second part of the duodenum.
Hepatopancreatic ampulla (of Vater)
As it lies medial to the second part of the duodenum, the common bile duct approaches the right end of the pancreatic duct. The ducts enter the duodenal wall together, and usually unite to form the hepatopancreatic ampulla. Rarely the common bile duct and pancreatic duct drain into the duodenum separately. Circular muscle usually surrounds the lower part of the common bile duct (bile duct sphincter) and frequently also surrounds the terminal part of the main pancreatic duct (pancreatic duct sphincter) and the hepatopancreatic ampulla (sphincter of Oddi). When all elements are present, this arrangement may allow for separate control of pancreatic and common bile duct emptying. Division of the upper part of the ampulla and ampullary sphincter (sphincterotomy) may be required to allow access to the common bile duct during endoscopic retrograde cholangiography.
Calot’s triangle
The near triangular space formed between the cystic duct, the common hepatic duct and the inferior surface of segment V of the liver (Suzuki et al 2000), is commonly referred to as Calot’s triangle. It is enclosed by the double layer of peritoneum which forms the short mesentery of the cystic duct. Since the two layers are not closely opposed, there is an appreciable amount of loose connective tissue within the triangle. It is perhaps better described as a pyramidal ‘space’ with one apex lying at the junction of the cystic duct and fundus of the gallbladder, one at the porta hepatis, and two closer apices at the attachments of the gallbladder to the liver bed. The base of the triangle thus lies on the inferior surface of the liver. This space usually contains the cystic artery as it approaches the gallbladder, the cystic lymph node and lymphatics from the gallbladder, one or two small cystic veins, the autonomic nerves running to the gallbladder, and some loose adipose tissue. It may contain any accessory ducts which drain into the gallbladder from the liver. Appreciation of the variations in ductal and arterial anatomy as they relate to the triangle are of considerable importance during excision of the gallbladder in order to avoid mistakenly ligating the common hepatic or common bile duct.
BILIARY STONES
Gallstones usually form in the gallbladder. As the gallbladder empties, gallstones move towards the cystic duct. When small stones enter the cystic duct they may irritate the columnar mucosa, this leads to spasm of the smooth muscle in the cystic duct wall, and the spasm generates pain known as biliary colic, which is often very severe. The mucosal folds in the neck of the gallbladder and the cystic duct provide a common site of entrapment of gallstones. Stones occluding the neck of the gallbladder may cause a sterile distension of the gallbladder: providing the gallbladder has not undergone acute inflammation previously it remains non-fibrotic and readily distensible, and an enlarged fundus often becomes palpable below the costal margin. Stones lodged in the distal cystic duct may cause swelling in the tissues around the duct. The close relationship of the distal cystic duct to the common hepatic duct means that this swelling may cause secondary compression of the common hepatic duct, resulting in partial obstruction to the flow of bile and the appearance of mild jaundice, the so called ‘Mirizzi syndrome’. Once stones have passed through the cystic duct they often become impacted at the junction of the common bile duct and pancreatic duct just proximal to the hepatopancreatic ampulla, producing obstructive jaundice and/or acute pancreatitis.
ENDOSCOPIC CHOLANGIOGRAPHY
The common bile duct may be accessed endoscopically from the duodenum for diagnostic cholangiography and therapeutic interventions. The angled relationship of the distal common bile duct and pancreatic duct may make direct cannulation of the bile duct difficult. When the duct lies in a more vertical position, embedded within the wall of the duodenum, a direct incision in the base of the hepatopancreatic ampulla and the adjacent wall of the duodenum (pre-cut sphincterotomy) may expose the duct to allow cannulation. This is occasionally associated with haemorrhage from the duodenal wall vessels. Division of the smooth muscle fibres of the common bile duct sphincter may be necessary for endoscopic access to the bile duct, but it often results in uncontrolled reflux of duodenal contents into the distal common bile duct, and this may result in recurrent biliary infections.
BILIARY DRAINAGE
The proximity of the fundus of the gallbladder to the anterior abdominal wall provides a useful route of access for percutaneous drainage of a distended, obstructed gallbladder. It is rarely obscured by liver tissue, can often be accessed below the costal margin, and is most often performed under ultrasound guidance. Because of the small calibre and spiral conformation of the cystic duct, drainage of the gallbladder is rarely adequate to decompress the biliary tree if it is blocked, and this must be achieved endoscopically, surgically or by a percutaneous, transhepatic approach. This latter technique requires the identification of dilated intrahepatic bile ducts, usually by ultrasound imaging with direct guided puncture via a right subcostal approach. Percutaneous access is obtained via segment III in the left lobe of the liver and via segments V and VI in the right lobe of the liver.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
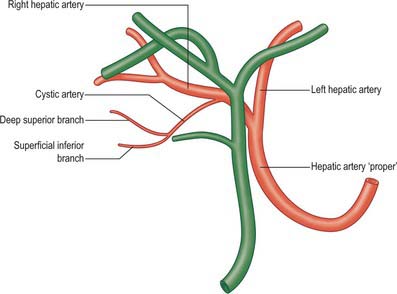
Cystic artery
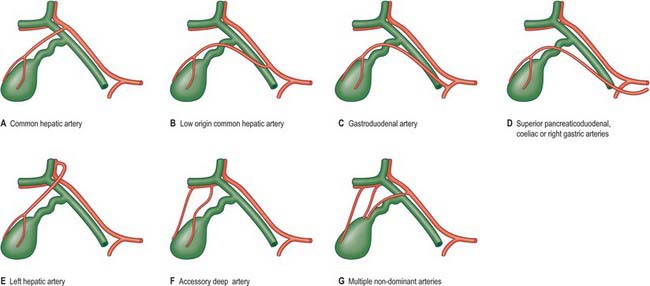
The cystic artery usually arises from the right hepatic artery (Fig. 69.6). It usually passes posterior to the common hepatic duct and anterior to the cystic duct to reach the superior aspect of the neck of the gallbladder and divides into superficial and deep branches. The superficial branch ramifies on the inferior aspect of the body of the gallbladder, the deep branch on the superior aspect. These arteries anastomose over the surface of the body and fundus. The origin of the cystic artery frequently varies (Fig. 69.7). The most common variant is an origin from the common hepatic artery (occasionally low down), sometimes from the left hepatic or gastroduodenal artery, and rarely from the superior pancreaticoduodenal, coeliac, right gastric or superior mesenteric arteries. In these cases, it crosses anterior (or less commonly posterior) to the common bile duct or common hepatic duct to reach the gallbladder. An accessory cystic artery may arise from the common hepatic artery or one of its branches and the cystic artery often bifurcates close to its origin, giving rise to two vessels which approach the gallbladder. Multiple fine arterial branches may arise from the parenchyma of segments IV or V of the liver and contribute to the supply of the body, particularly when the gallbladder is substantially intrahepatic. This makes the gallbladder relatively resistant to necrosis during inflammation which otherwise occludes the cystic artery.
The cystic artery gives rise to multiple fine branches which supply the common and lobar hepatic ducts and upper part of the common bile duct. These fine branches form a network which anastomoses with the vessels ascending around the common bile duct and with the vessels from the liver parenchyma which descend with the right and left hepatic ducts.
Ductal arteries
The common bile duct and hepatic ducts are supplied by a fine network of vessels which usually receives contributions from several sources, and which lies in close proximity to the ducts. Disruption of the network during surgical exposure of the bile ducts over a long length frequently causes chronic ischaemia and resultant stenosis of the duct. Approaches which spare the network are necessary to avoid this complication.
The common bile duct is fairly consistently supplied by two to four ascending and descending arteries which form long narrow anastomotic channels along the length of the duct: the most prominent of these are disposed into medial and lateral ‘trunks’, although they may lie more anterolateral and posteromedial. The largest contributions usually arise as one or two branches from the retroduodenal branch of the gastroduodenal artery as it crosses the anterior surface of the duct at the upper border of the duodenum. Three or four descending branches supply this network from the right hepatic and cystic arteries as these vessels pass close to the lower common hepatic duct: occasionally they are the dominant supply to the common bile duct.
Posteriorly, a retroportal artery often arises from the coeliac axis, superior mesenteric artery or one of their major branches close to the origin from the aorta, and runs upwards on the posterior surface of the portal vein. It usually ends by joining the retroduodenal artery close to the lower end of the supraduodenal bile duct, but occasionally it passes up behind the bile duct to join the right hepatic artery. When present, the retroportal artery contributes to the arterial network supplying the supraduodenal bile duct system.
The hilar and intrahepatic ducts are supplied by a fine network of periductal arteries that arise from the segmental arteries within the Glissonian sheaths.
Cystic veins
The venous drainage of the gallbladder is rarely by a single cystic vein. There are usually multiple small veins. Those arising from the superior surface of the body and neck lie in areolar tissue between the gallbladder and liver and enter the liver parenchyma to drain into the segmental portal veins. The remainder form one or two small cystic veins, which enter the liver either directly or after joining the veins that drain the hepatic ducts and upper bile duct. Only rarely does a single or double cystic vein drain into the right portal branch.
Lymphatics
Numerous lymphatic vessels run from the submucosal and subserosal plexuses on all aspects of the gallbladder and cystic duct. Those on the hepatic aspect of the gallbladder connect with the intrahepatic lymph vessels. The remainder drain into the cystic node, which usually lies above the cystic duct in the tissue of Calot’s triangle. This node, and some lymphatic channels which bypass the cystic node, drain into a node lying in the anterior border of the free edge of the lesser omentum. Hepatic nodes lying in the porta hepatis collect lymph from vessels that accompany the hepatic ducts and the upper part of the bile duct. Lymphatics from the lower part of the common bile duct drain into the inferior hepatic and upper pancreaticosplenic nodes.
INNERVATION
The gallbladder and the extrahepatic biliary tree are innervated by branches from the hepatic plexus. The retroduodenal part of the common bile duct and the smooth muscle of the hepatopancreatic ampulla are also innervated by twigs from the pyloric branches of the vagi.
MICROSTRUCTURE
GALLBLADDER
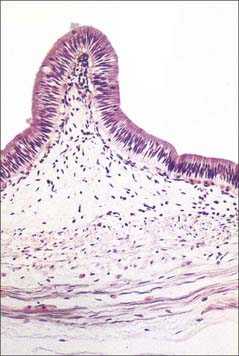
The fundus of the gallbladder is completely covered by a serosa, and the inferior surfaces and sides of the body and neck of the gallbladder are usually covered by a serosa. If the gallbladder possesses a mesentery the serosa extends around the sides of the body and neck onto the superior surface and continues into the serosa of the mesentery, whereas the serosa is limited to the inferior surfaces only if the gallbladder is intrahepatic. Beneath the serosa is subserous loose connective and adipose peritoneal tissue. The gallbladder wall microstructure generally resembles that of the small intestine. The mucosa is yellowish-brown and elevated into minute rugae with a honeycomb appearance (Fig. 69.2). In section, projections of the mucosa into the gallbladder lumen resemble intestinal villi, but they are not fixed structures and the surface flattens as the gallbladder fills with bile. The epithelium is a single layer of columnar cells with apical microvilli; basally, the spaces between epithelial cells are dilated (Fig. 69.8). Many capillaries lie beneath the basement membrane. The epithelial cells actively absorb water and solutes from the bile and concentrate it up to ten-fold. There are no goblet cells in the epithelium. The thin fibromuscular layer is composed of fibrous tissue mixed with smooth muscle cells arranged loosely in longitudinal, circular and oblique bundles.
BILE DUCTS
The walls of the large biliary ducts consist of external fibrous and internal mucosal layers (Fig. 69.9). The outer layer is fibrous connective tissue containing a variable amount of longitudinal, oblique and circular smooth muscle cells. The mucosa is continuous with that in the hepatic ducts, gallbladder and duodenum. The epithelium is columnar and there are numerous tubuloalveolar mucous glands in the duct walls.
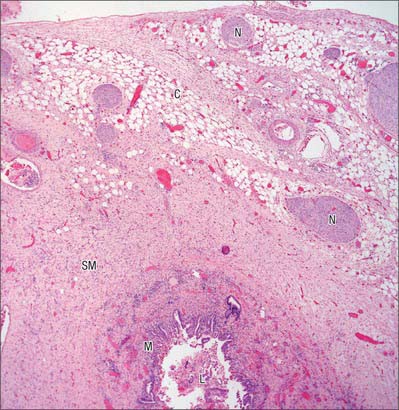
Fig. 69.9 Low power micrograph showing the human common bile duct structure. Shown are the lumen (L), mucosal lining (m), smooth muscle coat (SM) and outer connective tissue (C), with numerous nerve fibre bundles (N).
(By courtesy of Mr Peter Helliwell and Dr Joseph Mathew, Department of Histopathology, Royal Cornwall Hospitals Trust, UK.)
Expulsion of gallbladder contents is under neuroendocrine control. Fat in the duodenum causes the release of cholecystokinin (CCK), which stimulates the gallbladder to contract because muscle cells in its walls bear surface receptors for CCK. When the pressure exceeds 100 mm H2O of bile, the sphincter of Oddi relaxes and bile enters the duodenum. The termination of the united bile and pancreatic ducts is packed with villous, valvular folds of mucosa that contain muscle cells in their connective tissue cores. Contraction is thought to result in retraction and clumping of these folds, so preventing reflux of duodenal contents and controlling the exit of bile.