Anatomic Considerations
Trigeminal Nerve
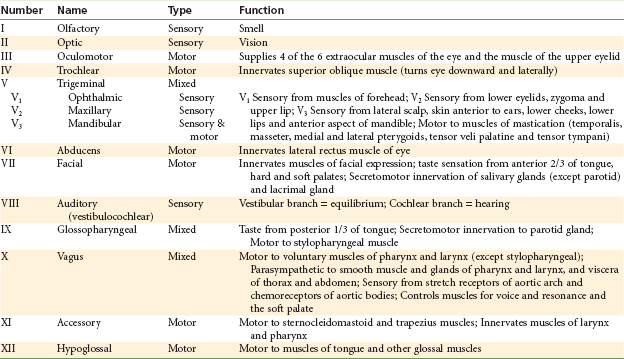
An understanding of the management of pain in dentistry requires thorough knowledge of the fifth (V) cranial nerve (Fig. 12-1). The right and left trigeminal nerves provide, among other functions, an overwhelming majority of sensory innervation from teeth, bone, and soft tissues of the oral cavity. The trigeminal nerve is the largest of the twelve cranial nerves. It is composed of a small motor root and a considerably larger (tripartite) sensory root. The motor root supplies the muscles of mastication and other muscles in the region. The three branches of the sensory root supply the skin of the entire face and the mucous membrane of the cranial viscera and oral cavity, except for the pharynx and base of the tongue. Table 12-1 summarizes the functions of the trigeminal nerve and the 11 other cranial nerves.
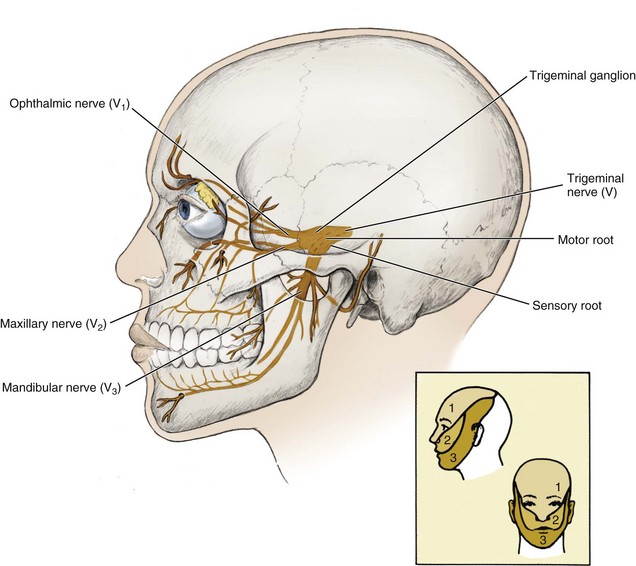
Figure 12-1 The general pathway of the trigeminal or fifth cranial nerve and its motor and sensory roots and three divisions (inset shows the pattern of innervation for each nerve division). (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
Motor Root
The motor root of the trigeminal nerve arises separately from the sensory root, originating in the motor nucleus within the pons and medulla oblongata (Fig. 12-2). Its fibers, forming a small nerve root, travel anteriorly along with, but entirely separate from, the larger sensory root to the region of the semilunar (or gasserian) ganglion. At the semilunar ganglion, the motor root passes in a lateral and inferior direction under the ganglion toward the foramen ovale, through which it leaves the middle cranial fossa along with the third division of the sensory root, the mandibular nerve (Figs. 12-3 and 12-4). Just after leaving the skull, the motor root unites with the sensory root of the mandibular division to form a single nerve trunk.
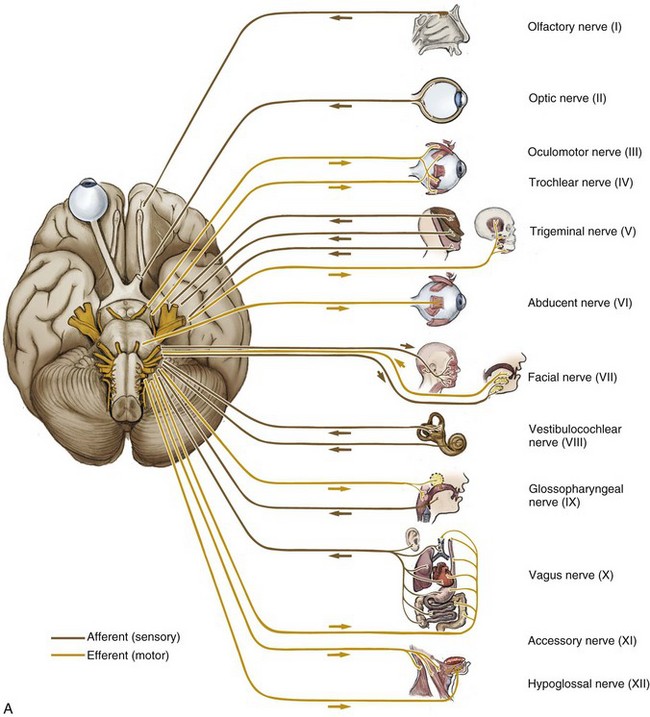
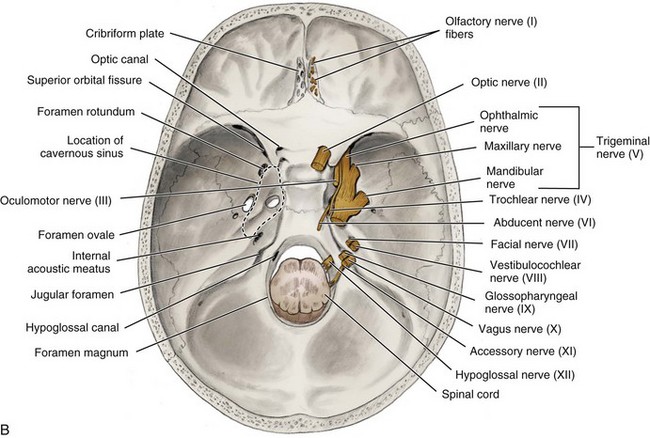
Figure 12-2 A, Inferior view of the brain showing cranial nerves and the organs and tissues they innervate. B, Internal view of the base of the skull showing cranial nerves exiting or entering the skull. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
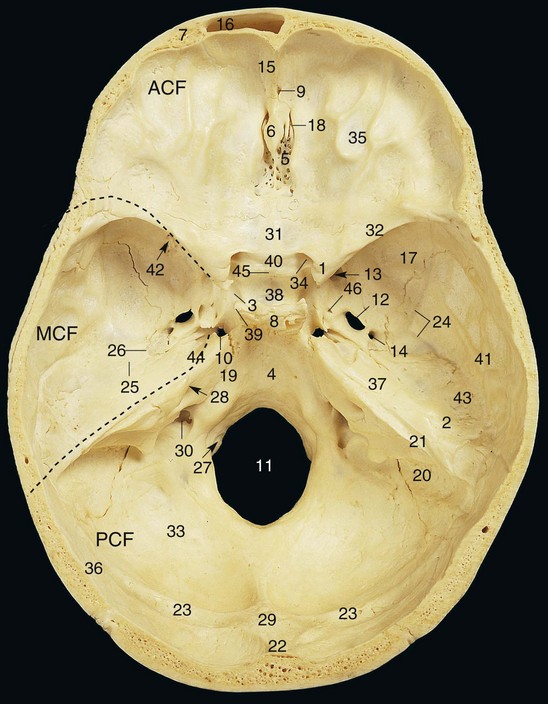
Figure 12-3 Internal surface of the base of the skull (cranial fossa). ACF, Anterior cranial fossa; MCF, middle cranial fossa; PCF, posterior cranial fossa. 1, Anterior clinoid process; 2, arcuate eminence; 3, carotid groove; 4, clivus; 5, cribriform plate of ethmoid bone; 6, crista galli; 7, diploë; 8, dorsum sellae; 9, foramen cecum; 10, foramen lacerum; 11, foramen magnum; 12, foramen ovale; 13, foramen rotundum; 14, foramen spinosum; 15, frontal crest; 16, frontal sinus; 17, greater wing of sphenoid bone; 18, groove for anterior ethmoidal nerve and vessels; 19, groove for inferior petrosal sinus; 20, groove for sigmoid sinus; 21, groove for superior petrosal sinus; 22, groove for superior sagittal sinus; 23, groove for transverse sinus; 24, grooves for middle meningeal vessels; 25, hiatus and groove for greater petrosal nerve; 26, hiatus and groove for lesser petrosal nerve; 27, hypoglossal canal; 28, internal acoustic meatus; 29, internal occipital protuberance; 30, jugular foramen; 31, jugum of sphenoid bone; 32, lesser wing of sphenoid bone; 33, occipital bone; 34, optic canal; 35, orbital part of frontal bone; 36, parietal bone (posteroinferior angle only); 37, petrous part of temporal bone; 38, pituitary fossa (sella turcica); 39, posterior clinoid process; 40, prechiasmatic groove; 41, squamous part of temporal bone; 42, superior orbital fissure; 43, tegmen tympani; 44, trigeminal impression; 45, tuberculum sellae; 46, venous foramen. (Data from Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
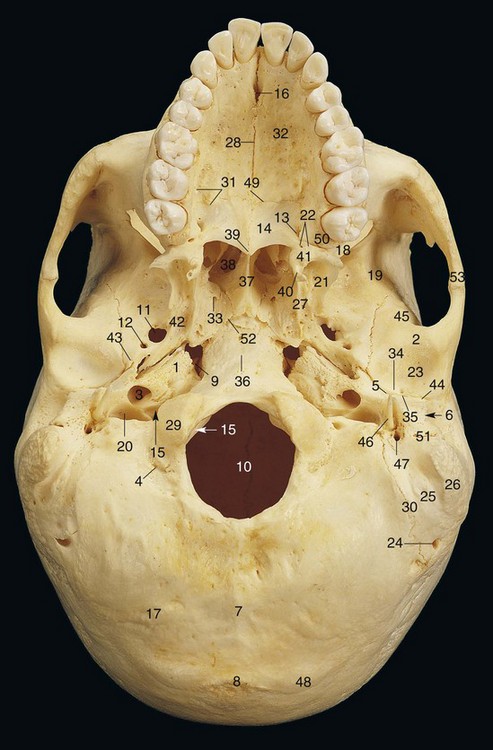
Figure 12-4 External surface of the base of the skull. 1, Apex of petrous part of temporal bone; 2, articular tubercle; 3, carotid canal; 4, condylar canal (posterior); 5, edge of tegmen tympani; 6, external acoustic meatus; 7, external occipital crest; 8, external occipital protuberance; 9, foramen lacerum; 10, foramen magnum; 11, foramen ovale; 12, foramen spinosum; 13, greater palatine foramen; 14, horizontal plate of palatine bone; 15, hypoglossal (anterior condylar) canal; 16, incisive fossa; 17, inferior nuchal line; 18, inferior orbital fissure; 19, infratemporal crest of greater wing of sphenoid bone; 20, jugular foramen; 21, lateral pterygoid plate; 22, lesser palatine foramina; 23, mandibular fossa; 24, mastoid foramen; 25, mastoid notch; 26, mastoid process; 27, medial pterygoid plate; 28, median palatine (intermaxillary) suture; 29, occipital condyle; 30, occipital groove; 31, palatine grooves and spines; 32, palatine process of maxilla; 33, palatinovaginal canal; 34, petrosquamous fissure; 35, petrotympanic fissure; 36, pharyngeal tubercle; 37, posterior border of vomer; 38, posterior nasal aperture (choana); 39, posterior nasal spine; 40, pterygoid hamulus; 41, pyramidal process of palatine bone; 42, scaphoid fossa; 43, spine of sphenoid bone; 44, squamotympanic fissure; 45, squamous part of temporal bone; 46, styloid process; 47, stylomastoid foramen; 48, superior nuchal line; 49, transverse palatine (palatomaxillary) suture; 50, tuberosity of maxilla; 51, tympanic part of temporal bone; 52, vomerovaginal canal; 53, zygomatic arch. (Data from Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
Motor fibers of the trigeminal nerve supply the following muscles:
Sensory Root
Sensory root fibers of the trigeminal nerve constitute the central processes of ganglion cells located in the trigeminal (semilunar or gasserian) ganglion. Two ganglia are present, one innervating each side of the face. They are located in Meckel’s cavity, on the anterior surface of the petrous portion of the temporal bone (see Fig. 12-3). The ganglia are flat and crescent shaped and measure approximately 1.0 × 2.0 cm; their convexities face anteriorly and downward. Sensory root fibers enter the concave portion of each crescent, and the three sensory divisions of the trigeminal nerve exit from the convexity:
1. The ophthalmic division (V1) travels anteriorly in the lateral wall of the cavernous sinus to the medial part of the superior orbital fissure, through which it exits the skull into the orbit.
2. The maxillary division (V2) travels anteriorly and downward to exit the cranium through the foramen rotundum into the upper portion of the pterygopalatine fossa.
3. The mandibular division (V3) travels almost directly downward to exit the skull, along with the motor root, through the foramen ovale. These two roots then intermingle, forming one nerve trunk that enters the infratemporal fossa.
On exiting the cranium through their respective foramina, the three divisions of the trigeminal nerve divide into a multitude of sensory branches.
Each of the three divisions of the trigeminal nerve is described, but more attention is devoted to the maxillary and mandibular divisions because of their greater importance in pain control in dentistry. Figure 12-5 illustrates the sensory distribution of the trigeminal nerve.

Figure 12-5 A, Cutaneous nerves of face. V1 (ophthalmic nerve): EN, External nasal nerve; IT, infratrochlear nerve; L, lacrimal nerve; SO, Supraorbital nerve; ST, supratrochlear nerve. V2 (maxillary nerve): IO, Infraorbital nerve; ZF, zygomaticofacial nerve; ZT, zygomaticotemporal nerve. V3 (mandibular nerve): AT, Auriculotemporal nerve; B, buccal nerve; M, mental nerve. Spinal nerve: GA, Great auricular nerve. B, Motor nerves to muscles of facial expression. Facial branches of cranial nerve (CN) VII: B, buccal branches; C, cervical branches; M, mandibular branches; T, Temporal branches; Z, zygomatic branches. (Data from Liebgott B: The anatomical basis of dentistry, ed 3, St Louis, 2010, Mosby.)
Ophthalmic Division (V1)
The ophthalmic division is the first branch of the trigeminal nerve. It is purely sensory and is the smallest of the three divisions. It leaves the cranium and enters the orbit through the superior orbital fissure (Fig. 12-6). The nerve trunk is approximately 2.5 cm long. It supplies the eyeball, conjunctiva, lacrimal gland, parts of the mucous membrane of the nose and paranasal sinuses, and the skin of the forehead, eyelids, and nose. When the ophthalmic nerve (V1) is paralyzed, the ocular conjunctiva becomes insensitive to touch.
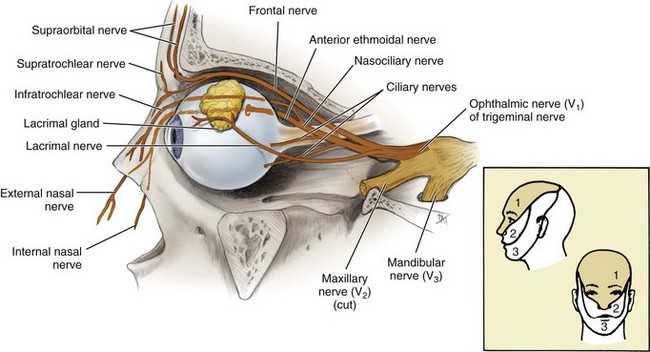
Figure 12-6 Lateral view of the cut-away orbit with the pathway of the ophthalmic nerve of the trigeminal nerve highlighted. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
Just before the ophthalmic nerve passes through the superior orbital fissure, it divides into its three main branches: nasociliary, frontal, and lacrimal nerves.
Nasociliary Nerve: The nasociliary nerve travels along the medial border of the orbital roof, giving off branches to the nasal cavity and ending in the skin at the root of the nose. It then branches into the anterior ethmoidal and external nasal nerves. The internal nasal nerve (from the anterior ethmoidal) supplies the mucous membrane of the anterior part of the nasal septum and the lateral wall of the nasal cavity. The ciliary ganglion contains sensory fibers that travel to the eyeball via the short ciliary nerves. Two or three long ciliary nerves supply the iris and cornea. The infratrochlear nerve supplies the skin of the lacrimal sac and the lacrimal caruncle, the posterior ethmoidal nerve supplies the ethmoidal and sphenoidal sinuses, and the external nasal nerve supplies the skin over the apex (tip) and the ala of the nose.
Frontal Nerve: The frontal nerve travels anteriorly in the orbit, dividing into two branches: supratrochlear and supraorbital. The frontal is the largest branch of the ophthalmic division. The supratrochlear nerve supplies the conjunctiva and skin of the medial aspect of the upper eyelid and the skin over the lower and mesial aspects of the forehead. The supraorbital nerve is sensory to the upper eyelid, the scalp as far back as the parietal bone, and the lambdoidal suture.
Maxillary Division (V2)
The maxillary division of the trigeminal nerve arises from the middle of the trigeminal ganglion. Intermediate in size between ophthalmic and mandibular divisions, it is purely sensory in function.
Origins: The maxillary nerve passes horizontally forward, leaving the cranium through the foramen rotundum (see Fig. 12-3). The foramen rotundum is located in the greater wing of the sphenoid bone. Once outside the cranium, the maxillary nerve crosses the uppermost part of the pterygopalatine fossa, between the pterygoid plates of the sphenoid bone and the palatine bone. As it crosses the pterygopalatine fossa, it gives off branches to the sphenopalatine ganglion, the posterior superior alveolar nerve, and the zygomatic branches. It then angles laterally in a groove on the posterior surface of the maxilla, entering the orbit through the inferior orbital fissure. Within the orbit, it occupies the infraorbital groove and becomes the infraorbital nerve, which courses anteriorly into the infraorbital canal.
The maxillary division emerges on the anterior surface of the face through the infraorbital foramen, where it divides into its terminal branches, supplying the skin of the face, nose, lower eyelid, and upper lip (Fig. 12-7). The following is a summary of maxillary division innervation:
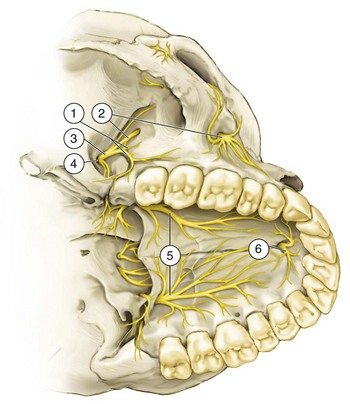
Figure 12-7 Distribution of the maxillary division (V2). 1, Posterior superior alveolar branches; 2, infraorbital nerve; 3, maxillary nerve; 4, foramen rotundum; 5, greater palatine nerve; 6, nasopalatine nerve. (Data from Haglund J, Evers H: Local anaesthesia in dentistry, ed 2, Södertälje, Sweden, 1975, Astra Läkemedel.)
Branches: The maxillary division gives off branches in four regions: within the cranium, in the pterygopalatine fossa, in the infraorbital canal, and on the face.
Branch Within the Cranium: Immediately after separating from the trigeminal ganglion, the maxillary division gives off a small branch, the middle meningeal nerve, which travels with the middle meningeal artery to provide sensory innervation to the dura mater.
Branches in the Pterygopalatine Fossa: After exiting the cranium through the foramen rotundum, the maxillary division crosses the pterygopalatine fossa. In this fossa, several branches are given off (Fig. 12-8): the zygomatic nerve, the pterygopalatine nerves, and the posterior superior alveolar nerve.
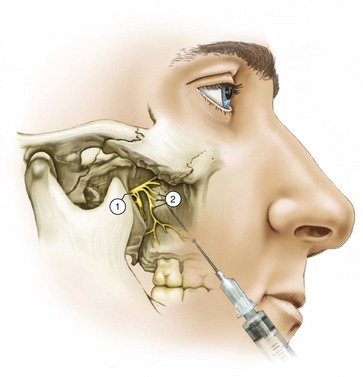
Figure 12-8 Branches of V2 in the pterygopalatine fossa. 1, Maxillary nerve; 2, posterior superior alveolar branches. (Data from Haglund J, Evers H: Local anaesthesia in dentistry, ed 2, Södertälje, Sweden, 1975, Astra Läkemedel.)
The zygomatic nerve comes off the maxillary division in the pterygopalatine fossa and travels anteriorly, entering the orbit through the inferior orbital fissure, where it divides into the zygomaticotemporal and zygomaticofacial nerves: the zygomaticotemporal supplying sensory innervation to the skin on the side of the forehead, and the zygomaticofacial supplying the skin on the prominence of the cheek. Just before leaving the orbit, the zygomatic nerve sends a branch that communicates with the lacrimal nerve of the ophthalmic division. This branch carries secretory fibers from the sphenopalatine ganglion to the lacrimal gland.
The pterygopalatine nerves are two short trunks that unite in the pterygopalatine ganglion and are then redistributed into several branches. They also serve as a communication between the pterygopalatine ganglion and the maxillary nerve (V2). Postganglionic secretomotor fibers from the pterygopalatine ganglion pass through these nerves and back along V2 to the zygomatic nerve, through which they are routed to the lacrimal nerve and the lacrimal gland.
Branches of the pterygopalatine nerves include those that supply four areas: orbit, nose, palate, and pharynx.
1. The orbital branches supply the periosteum of the orbit.
2. The nasal branches supply the mucous membranes of the superior and middle conchae, the lining of the posterior ethmoidal sinuses, and the posterior portion of the nasal septum. One branch is significant in dentistry, the nasopalatine nerve, which passes across the roof of the nasal cavity downward and forward, where it lies between the mucous membrane and the periosteum of the nasal septum. The nasopalatine nerve continues downward, reaching the floor of the nasal cavity and giving branches to the anterior part of the nasal septum and the floor of the nose. It then enters the incisive canal, through which it passes into the oral cavity via the incisive foramen, located in the midline of the palate about 1 cm posterior to the maxillary central incisors. The right and left nasopalatine nerves emerge together through this foramen and provide sensation to the palatal mucosa in the region of the premaxilla (canines through central incisors) (Fig. 12-9).
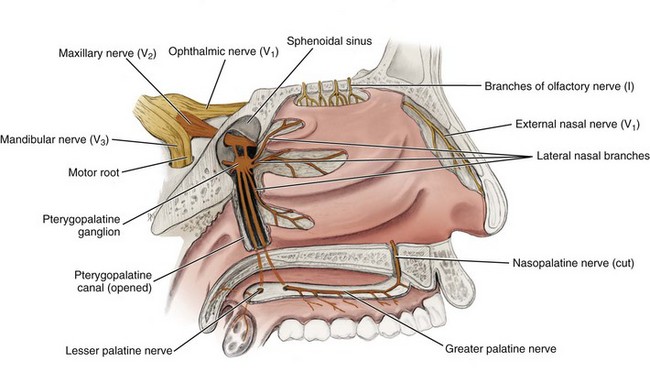
Figure 12-9 Medial view of the lateral nasal wall and the opened pterygopalatine canal highlighting the maxillary nerve and its palatine branches. The nasal septum has been removed, thus severing the nasopalatine nerve. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
3. The palatine branches include the greater (or anterior) palatine nerve and the lesser (middle and posterior) palatine nerves (Fig. 12-10). The greater (or anterior) palatine nerve descends through the pterygopalatine canal, emerging on the hard palate through the greater palatine foramen (which is usually located about 1 cm toward the palatal midline, just distal to the second molar). Sicher and DuBrul have stated that the greater palatine foramen may be located 3 to 4 mm in front of the posterior border of the hard palate.1 The nerve courses anteriorly between the mucoperiosteum and the osseous hard palate, supplying sensory innervation to the palatal soft tissues and bone as far anterior as the first premolar, where it communicates with terminal fibers of the nasopalatine nerve (see Fig. 12-10). It also provides sensory innervation to some parts of the soft palate. The middle palatine nerve emerges from the lesser palatine foramen, along with the posterior palatine nerve. The middle palatine nerve provides sensory innervation to the mucous membrane of the soft palate; the tonsillar region is innervated, in part, by the posterior palatine nerve.
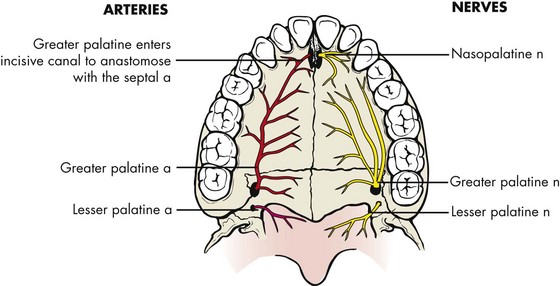
Figure 12-10 Blood and sensory nerve supply to hard and soft palate. a, Artery; n, nerve. (Data from Liebgott B: The anatomical basis of dentistry, ed 3, St Louis, 2010, Mosby.)
4. The pharyngeal branch is a small nerve that leaves the posterior part of the pterygopalatine ganglion, passes through the pharyngeal canal, and is distributed to the mucous membrane of the nasal part of the pharynx, posterior to the auditory (eustachian) tube.
The posterior superior alveolar (PSA) nerve descends from the main trunk of the maxillary division in the pterygopalatine fossa just before the maxillary division enters the infraorbital canal (see Fig. 12-7). Commonly there are two PSA branches, but on occasion a single trunk arises. Passing downward through the pterygopalatine fossa, they reach the inferior temporal (posterior) surface of the maxilla. When two trunks are present, one remains external to the bone, continuing downward on the posterior surface of the maxilla to provide sensory innervation to the buccal gingiva in the maxillary molar region and adjacent facial mucosal surfaces, whereas the other branch enters into the maxilla (along with a branch of the internal maxillary artery) through the PSA canal to travel down the posterior or posterolateral wall of the maxillary sinus, providing sensory innervation to the mucous membrane of the sinus. Continuing downward, this second branch of the PSA nerve provides sensory innervation to the alveoli, periodontal ligaments, and pulpal tissues of the maxillary third, second, and first molars (with the exception [in 28% of patients] of the mesiobuccal root of the first molar).
Branches in the Infraorbital Canal: Within the infraorbital canal, the maxillary division (V2) gives off two branches of significance in dentistry: the middle superior and anterior superior alveolar nerves. While in the infraorbital groove and canal, the maxillary division is known as the infraorbital nerve.
The middle superior alveolar (MSA) nerve branches off the main nerve trunk (V2) within the infraorbital canal to form a part of the superior dental plexus,1 composed of the posterior, middle, and anterior superior alveolar nerves. The site of origin of the MSA nerve varies, from the posterior portion of the infraorbital canal to the anterior portion, near the infraorbital foramen. The MSA nerve provides sensory innervation to the two maxillary premolars and, perhaps, to the mesiobuccal root of the first molar and periodontal tissues, buccal soft tissue, and bone in the premolar region. Traditionally it has been stated that the MSA nerve is absent in 30%2 to 54%3 of individuals. Loetscher and Walton4 found the MSA nerve to be present in 72% of the specimens examined. In its absence, its usual innervations are provided by either the PSA or the anterior superior alveolar (ASA) nerve, most frequently the latter.1
The anterior superior alveolar (ASA) nerve, a relatively large branch, is given off the infraorbital nerve (V2) approximately 6 to 10 mm before the latter exits from the infraorbital foramen. Descending within the anterior wall of the maxillary sinus, it provides pulpal innervation to the central and lateral incisors and the canine, and sensory innervation to the periodontal tissues, buccal bone, and mucous membranes of these teeth (Fig. 12-11).
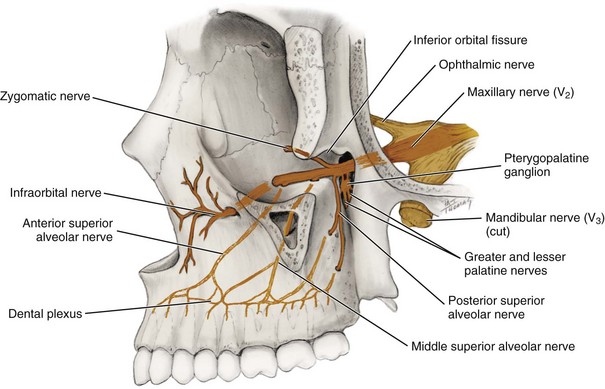
Figure 12-11 Lateral view of the skull (a portion of the lateral wall of the orbit has been removed) with the branches of the maxillary nerve highlighted. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
The ASA nerve communicates with the MSA nerve and gives off a small nasal branch that innervates the anterior part of the nasal cavity, along with branches of the pterygopalatine nerves. In persons without an MSA nerve, the ASA nerve frequently provides sensory innervation to the premolars and occasionally to the mesiobuccal root of the first molar.
The actual innervation of individual roots of all teeth, bone, and periodontal structures in both the maxilla and the mandible derives from terminal branches of larger nerves in the region. These nerve networks are termed the dental plexus.
The superior dental plexus is composed of smaller nerve fibers from the three superior alveolar nerves (and in the mandible, from the inferior alveolar nerve). Three types of nerves emerge from these plexuses: dental nerves, interdental branches, and interradicular branches. Each is accompanied along its pathway by a corresponding artery.
The dental nerves are those that enter a tooth through the apical foramen, dividing into many small branches within the pulp. Pulpal innervation of all teeth is derived from dental nerves. Although in most instances one easily identifiable nerve is responsible, in some cases (usually the maxillary first molar) more than one nerve is responsible.
The interdental branches (also termed perforating branches) travel through the entire height of the interradicular septum, providing sensory innervation to the periodontal ligaments of adjacent teeth through the alveolar bone. They emerge at the height of the crest of the interalveolar septum and enter the gingiva to innervate the interdental papillae and the buccal gingiva.
The interradicular branches traverse the entire height of the interradicular or interalveolar septum, providing sensory innervation to the periodontal ligaments of adjacent roots. They terminate in the periodontal ligament (PDL) at the root furcations.
Branches on the Face: The infraorbital nerve emerges through the infraorbital foramen onto the face to divide into its terminal branches: inferior palpebral, external nasal, and superior labial. The inferior palpebral branches supply the skin of the lower eyelid with sensory innervation, the external nasal branches provide sensory innervation to the skin on the lateral aspect of the nose, and the superior labial branches provide sensory innervation to the skin and mucous membranes of the upper lip.
Although anesthesia of these nerves is not necessary for adequate pain control during dental treatment, they are frequently blocked in the process of carrying out other anesthetic procedures.
Summary: The following is a summary of the branches of the maxillary division (italicized nerves denote those of special significance in dental pain control):
1. Branches within the cranium
2. Branches within the pterygopalatine fossa
3. Branches within the infraorbital canal
a. Middle superior alveolar nerve
b. Anterior superior alveolar nerve (Fig. 12-12)
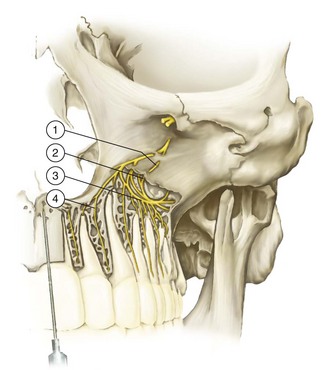
Figure 12-12 Anterior superior alveolar (ASA) nerve (bone over the nerves removed). 1, Branches of the ASA nerve; 2, superior dental plexus; 3, dental branches; 4, interdental and interradicular branches. (Data from Haglund J, Evers H: Local anaesthesia in dentistry, ed 2, Södertälje, Sweden, 1975, Astra Läkemedel.)
Mandibular Division (V3)
The mandibular division is the largest branch of the trigeminal nerve. It is a mixed nerve with two roots: a large sensory root and a smaller motor root (the latter representing the entire motor component of the trigeminal nerve). The sensory root of the mandibular division originates at the inferior angle of the trigeminal ganglion, whereas the motor root arises in motor cells located in the pons and medulla oblongata. The two roots emerge from the cranium separately through the foramen ovale, the motor root lying medial to the sensory. They unite just outside the skull and form the main trunk of the third division. This trunk remains undivided for only 2 to 3 mm before it splits into a small anterior and a large posterior division (Figs. 12-13 and 12-14).
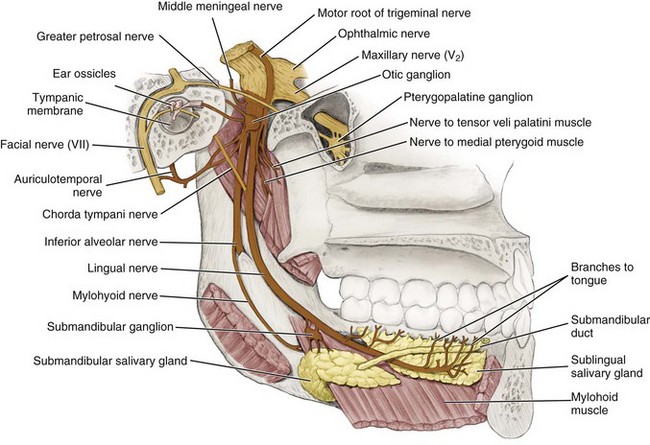
Figure 12-13 Medial view of the mandible with the motor and sensory branches of the mandibular nerve highlighted. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
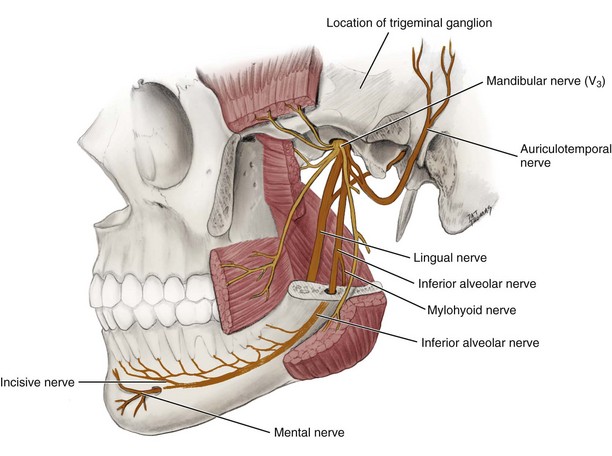
Figure 12-14 The pathway of the posterior trunk of the mandibular nerve of the trigeminal nerve is highlighted. (From Fehrenbach MJ, Herring SW: Anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
The areas innervated by V3 are included in the following outline:
Branches: The third division of the trigeminal nerve gives off branches in three areas: from the undivided nerve, and from the anterior and posterior divisions.
Branches from the Undivided Nerve: On leaving the foramen ovale, the main undivided nerve trunk gives off two branches during its 2- to 3-mm course. These are the nervus spinosus (meningeal branch of the mandibular nerve) and the medial pterygoid nerve. The nervus spinosus reenters the cranium through the foramen spinosum along with the middle meningeal artery to supply the dura mater and mastoid air cells. The medial pterygoid nerve is a motor nerve to the medial (internal) pterygoid muscle. It gives off small branches that are motor to the tensor veli palatini and the tensor tympani.
Branches from the Anterior Division: Branches from the anterior division of V3 provide motor innervation to the muscles of mastication and sensory innervation to the mucous membrane of the cheek and the buccal mucous membrane of the mandibular molars.
The anterior division is significantly smaller than the posterior. It runs forward under the lateral (external) pterygoid muscle for a short distance and then reaches the external surface of that muscle by passing between its two heads or, less frequently, by winding over its upper border. From this point, it is known as the buccal nerve. Although under the lateral pterygoid muscle, the buccal nerve gives off several branches: the deep temporal nerves (to the temporal muscle) and the masseter and lateral pterygoid nerves (providing motor innervation to the respective muscles).
The buccal nerve, also known as the buccinator nerve and the long buccal nerve, usually passes between the two heads of the lateral pterygoid to reach the external surface of that muscle. It then follows the inferior part of the temporal muscle and emerges under the anterior border of the masseter muscle, continuing in an anterolateral direction. At the level of the occlusal plane of the mandibular third or second molar, it crosses in front of the anterior border of the ramus and enters the cheek through the buccinator muscle. Sensory fibers are distributed to the skin of the cheek. Other fibers pass into the retromolar triangle, providing sensory innervation to the buccal gingiva of the mandibular molars and the mucobuccal fold in that region. The buccal nerve does not innervate the buccinator muscle; the facial nerve does. Nor does it provide sensory innervation to the lower lip or the corner of the mouth. This is significant because some doctors do not administer the “long” buccal injection immediately after completing the inferior alveolar nerve block until the patient’s lower lip has become numb. Their thinking is that the buccal nerve block will provide anesthesia to the lower lip and therefore might lead them to believe that their inferior alveolar nerve block has been successful, when in fact it has been missed. Such concern is unwarranted. The buccal nerve block may be administered immediately after completion of the inferior alveolar nerve block.
Anesthesia of the buccal nerve is important for dental procedures requiring soft tissue manipulation on the buccal surface of the mandibular molars.
Branches of the Posterior Division: The posterior division of V3 is primarily sensory with a small motor component. It descends for a short distance downward and medial to the lateral pterygoid muscle, at which point it branches into the auriculotemporal, lingual, and inferior alveolar nerves.
The auriculotemporal nerve is not profoundly significant in dentistry. It traverses the upper part of the parotid gland and then crosses the posterior portion of the zygomatic arch. It gives off a number of branches, all of which are sensory. These include a communication with the facial nerve, providing sensory fibers to the skin over areas of innervation of the following motor branches of the facial nerve: zygomatic, buccal, and mandibular; a communication with the otic ganglion, providing sensory, secretory, and vasomotor fibers to the parotid gland; the anterior auricular branches, supplying the skin over the helix and tragus of the ear; branches to the external auditory meatus, innervating the skin over the meatus and the tympanic membrane; articular branches to the posterior portion of the temporomandibular joint; and superficial temporal branches, supplying the skin over the temporal region.1-6
The lingual nerve is the second branch of the posterior division of V3. It passes downward medial to the lateral pterygoid muscle and, as it descends, lies between the ramus and the medial pterygoid muscle in the pterygomandibular space. It runs anterior and medial to the inferior alveolar nerve, whose path it parallels. It then continues downward and forward, deep to the pterygomandibular raphe and below the attachment of the superior constrictor of the pharynx, to reach the side of the base of the tongue slightly below and behind the mandibular third molar (see Figs. 12-13 and 12-14). Here it lies just below the mucous membrane in the lateral lingual sulcus, where it is so superficial in some persons that it may be seen just below the mucous membrane. It then proceeds anteriorly across the muscles of the tongue, looping downward and medial to the submandibular (Wharton’s) duct to the deep surface of the sublingual gland, where it breaks up into its terminal branches.
The lingual nerve is the sensory tract to the anterior two thirds of the tongue. It provides both general sensation and gustation (taste) for this region. It is the nerve that supplies fibers for general sensation, whereas the chorda tympani (a branch of the facial nerve) supplies fibers for taste. In addition, the lingual nerve provides sensory innervation to the mucous membranes of the floor of the mouth and the gingiva on the lingual of the mandible. The lingual nerve is the nerve most commonly associated with cases of paresthesia (prolonged or permanent sensory nerve damage).
The inferior alveolar nerve is the largest branch of the mandibular division (see Fig. 12-14). It descends medial to the lateral pterygoid muscle and lateroposterior to the lingual nerve, to the region between the sphenomandibular ligament and the medial surface of the mandibular ramus, where it enters the mandibular canal at the level of the mandibular foramen. Throughout its path, it is accompanied by the inferior alveolar artery (a branch of the internal maxillary artery) and the inferior alveolar vein. The artery lies just anterior to the nerve. The nerve, artery, and vein travel anteriorly in the mandibular canal as far forward as the mental foramen, where the nerve divides into its terminal branches: the incisive nerve and the mental nerve.
Bifid (from the Latin meaning “cleft into two parts”) inferior alveolar nerves and mandibular canals have been observed radiographically and categorized by Langlais and associates.5 Among 6000 panoramic radiographs studied, bifid mandibular canals were evident in 0.95%. The bifid mandibular canal is clinically significant in that it increases the difficulty of achieving adequate anesthesia in the mandible through conventional techniques. This is especially so in the type 4 variation (Fig. 12-15), in which two separate mandibular foramina are present on each side of the mouth.
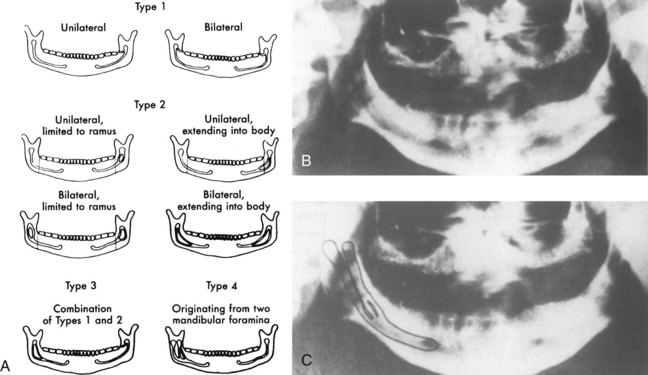
Figure 12-15 A, Variations in bifid mandibular canals. B and C, Radiographs of a type 4 bifid mandibular canal (B, on the patient’s right; C, outlined). (Data from Langlais RP, Broadus R, Glass BJ: Bifid mandibular canals in panoramic radiographs, J Am Dent Assoc 110:923–926, 1985.)
The mylohyoid nerve branches from the inferior alveolar nerve before entry of the latter into the mandibular canal (see Figs. 12-13 and 12-14). It runs downward and forward in the mylohyoid groove on the medial surface of the ramus and along the body of the mandible to reach the mylohyoid muscle. The mylohyoid is a mixed nerve, being motor to the mylohyoid muscle and the anterior belly of the digastric. It is thought to contain sensory fibers that supply the skin on the inferior and anterior surfaces of the mental protuberance. It also may provide sensory innervation to the mandibular incisors. Evidence suggests that the mylohyoid nerve also may be involved in supplying pulpal innervation to portions of the mandibular molars in some persons, usually the mesial root of the mandibular first molar.6
Once the inferior alveolar nerve enters the mandibular canal, it travels anteriorly along with the inferior alveolar artery and vein. The dental plexus serves the mandibular posterior teeth, entering through their apices and providing pulpal innervation. Other fibers supply sensory innervation to the buccal periodontal tissues of these same teeth.
The inferior alveolar nerve divides into its two terminal branches: the incisive nerve and the mental nerve at the mental foramen (see Fig. 12-14). The incisive nerve remains within the mandibular canal and forms a nerve plexus that innervates the pulpal tissues of the mandibular first premolar, canine, and incisors via the dental branches. The mental nerve exits the canal through the mental foramen and divides into three branches that innervate the skin of the chin and the skin and mucous membrane of the lower lip.
Osteology: Maxilla
In addition to the neuroanatomy of pain control in dentistry, one should be aware of the relationship of these nerves to the osseous and soft tissues through which they course.
The maxilla (more properly, the right and left maxillae) is the largest bone of the face, excluding the mandible. Its anterior (or facial) surface (Fig. 12-16) is directed both forward and laterally. At its inferior borders are a series of eminences that correspond to the roots of the maxillary teeth. The most prominent usually is found over the canine tooth and is often referred to as the canine eminence. Superior to the canine fossa (located just distal to the canine eminence) is the infraorbital foramen, through which blood vessels and terminal branches of the infraorbital nerve emerge. Bone in the region of the maxillary teeth is commonly of the more porous cancellous variety, leading to a significantly greater incidence of clinically adequate anesthesia than in areas where more dense cortical bone is present, such as in the mandible. In many areas, bone over the apices of the maxillary teeth is tissue-paper thin or shows evidence of dehiscence.
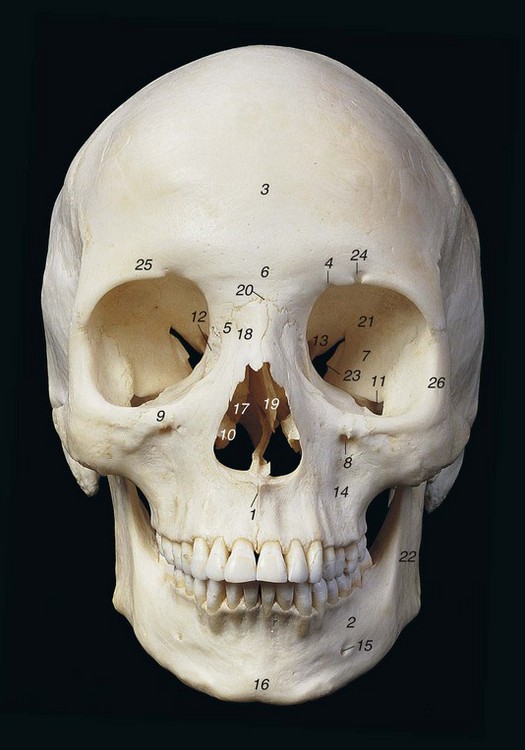
Figure 12-16 Anterior view of the skull. 1, Anterior nasal spine; 2, body of mandible; 3, frontal bone; 4, frontal notch; 5, frontal process of maxilla; 6, glabella; 7, greater wing of sphenoid bone; 8, infraorbital foramen; 9, infraorbital margin; 10, inferior nasal concha; 11, inferior orbital fissure; 12, lacrimal bone; 13, lesser wing of sphenoid bone; 14, maxilla; 15, mental foramen; 16, mental protuberance; 17, middle nasal concha; 18, nasal bone; 19, nasal septum; 20, nasion; 21, orbit (orbital cavity); 22, ramus of mandible; 23, superior orbital fissure; 24, supraorbital foramen; 25, supraorbital margin; 26, zygomatic bone. (Data from Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
The inferior temporal surface of the maxilla is directed backward and laterally (Fig. 12-17). Its posterior surface is pierced by several alveolar canals that transmit the posterior superior alveolar nerves and blood vessels. The maxillary tuberosity, a rounded eminence, is found on the inferior posterior surface. On the superior surface is a groove, directed laterally and slightly superiorly, through which the maxillary nerve passes. This groove is continuous with the infraorbital groove.

Figure 12-17 Infratemporal aspect of the maxilla. 1, Articular tubercle; 2, external acoustic meatus; 3, horizontal plate of palatine bone; 4, inferior orbital fissure; 5, infratemporal crest; 6, infratemporal (posterior) surface of maxilla; 7, infratemporal surface of greater wing of sphenoid bone; 8, lateral pterygoid plate; 9, mandibular fossa; 10, mastoid notch; 11, mastoid process; 12, medial pterygoid plate; 13, occipital condyle; 14, occipital groove; 15, pterygoid hamulus; 16, pterygomaxillary fissure and pterygopalatine fossa; 17, pyramidal process of palatine bone; 18, spine of sphenoid bone; 19, styloid process and sheath; 20, third molar tooth; 21, tuberosity of maxilla; 22, vomer; 23, zygomatic arch. (Data from Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
The palatal processes of the maxilla are thick horizontal projections that form a large portion of the floor of the nose and the roof of the mouth. The bone here is considerably thicker anteriorly than posteriorly. Its inferior (or palatal) surface constitutes the anterior three fourths of the hard palate (Fig. 12-18). Many foramina (passages for nutrient blood vessels) perforate it. Along its lateral border, at the junction with the alveolar process, is a groove through which the anterior palatine nerve passes from the greater palatine foramen. In the midline in the anterior region is the funnel-shaped opening of the incisive foramen. Four canals are located in this opening: two for the descending palatine arteries and two for the nasopalatine nerves. In many skulls, especially those of younger persons, a fine suture line extends laterally from the incisive foramen to the border of the palatine process by the canine teeth. The small area anterior to this suture is termed the premaxilla.
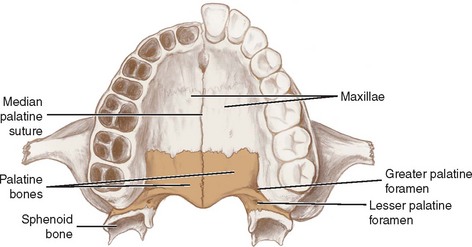
Figure 12-18 Inferior view of the hard palate. (Data from Fehrenbach MJ, Herring SW: Illustrated anatomy of the head and neck, ed 2, Philadelphia, 2002, WB Saunders.)
The horizontal plate of the palatine bone forms the posterior fourth of the hard palate. Its anterior border articulates with the palatine process of the maxilla, and its posterior border serves as the attachment for the soft palate. Foramina are present on its surface, representing the lower end of the pterygopalatine canal, through which descending palatine blood vessels and the anterior palatine nerve run.
Osteology: Mandible
The mandible is the largest and strongest bone of the face. It consists of a curved horizontal portion (the body) and two perpendicular portions (the rami). The buccal cortical plate of the adult mandible most often is sufficiently dense so as to preclude effective infiltration of anesthesia in its vicinity.7
The external (lateral) surface of the body of the mandible is marked in the midline by a faint ridge, an indication of the symphysis of the two pieces of bone from which the mandible is created (Fig. 12-19, A and C). The bone that forms the buccal and lingual alveolar processes in the anterior region (incisors) is usually less dense than that over the posterior teeth, permitting infiltration (supraperiosteal) anesthesia to be employed with some expectation of success.8,9 In the region of the second premolar on each side, midway between the upper and lower borders of the body, lies the mental foramen. Phillips and associates, in an evaluation of 75 dry, adult human mandibles, determined that the usual position of the mental foramen is below the crown of the second premolar.10 The mental nerve, artery, and vein exit the mandibular canal here. Bone along this external surface of the mandible is commonly thick cortical bone.
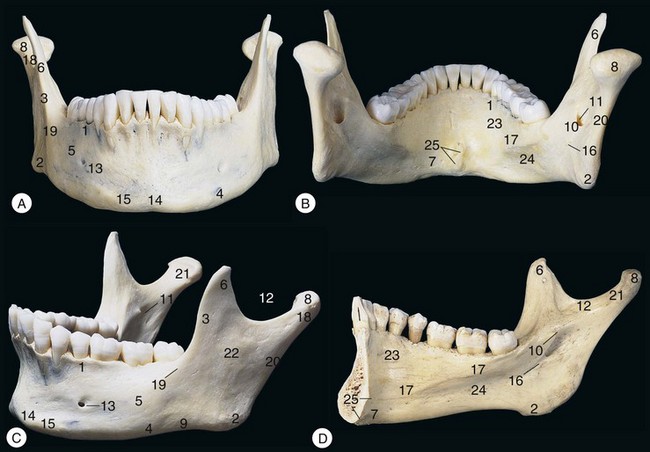
Figure 12-19 The mandible (A) from the front, (B) from behind and above, and (C) from the left and front, and (D) internal view from the left. 1, Alveolar part; 2, angle; 3, anterior border of ramus; 4, base; 5, body; 6, coronoid process; 7, digastric fossa; 8, head; 9, inferior border of ramus; 10, lingula; 11, mandibular foramen; 12, mandibular notch; 13, mental foramen; 14, mental protuberance; 15, mental tubercle; 16, mylohyoid groove; 17, mylohyoid line; 18, neck; 19, oblique line; 20, posterior border of ramus; 21, pterygoid fovea; 22, ramus; 23, sublingual fossa; 24, submandibular fossa; 25, superior and inferior mental spines (genial tubercles). (Data from Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
The lingual border of the body of the mandible is concave from side to side (Fig. 12-19, B and D). Extending upward and backward is the mylohyoid line, giving origin to the mylohyoid muscle. Bone along the lingual of the mandible is usually quite thick; however, in approximately 68% of mandibles, lingual foramina are located in the posterior (molar) region.11 The function of these foramina is as yet unclear, but some may contain sensory fibers from the mylohyoid nerve that innervate portions of mandibular molars.2 In addition, bone on the lingual surface of the incisor teeth frequently demonstrates multiple small perforations, perhaps explaining recent clinical trials in which mandibular lingual infiltration had significant success rates in providing pulpal anesthesia.8
The lateral surface of each ramus is flat, composed of dense cortical bone and providing attachment for the masseter muscle along most of its surface (see Fig. 12-19, C). The medial surface (see Fig. 12-19, D) contains the mandibular foramen, located roughly halfway between the superior and inferior borders and two thirds to three fourths the distance from the anterior border of the ramus to its posterior border.12 Other studies of the anteroposterior location of the mandibular foramen have provided differing locations. Hayward and associates13 found the foramen most often in the third quadrant from the anterior part of the ramus, Monheim14 found it at the midpoint of the ramus, and Hetson and associates15 located it 55% distal to the anterior ramus (range, 44.4% to 65.5%). The mandibular canal extends obliquely downward and anteriorly within the ramus. It then courses horizontally forward in the body, distributing small dental branches to the mandibular teeth posterior to the mental foramen. The mandibular foramen is the point of entrance through which the inferior alveolar nerve, artery, and vein enter the mandibular canal. The height of this foramen varies greatly, ranging from 1 to 19 mm or more above the level of the occlusal plane.13 A prominent ridge, the lingula mandibulae, lies on the anterior margin of the foramen. The lingula serves as an attachment for the sphenomandibular ligament. At the lower end of the mandibular foramen, the mylohyoid groove begins, coursing obliquely downward and anteriorly. In this groove lie the mylohyoid nerve and vessels.
Bone along the lingual surface of the mandible usually is dense (see Fig. 12-19, D). On rare occasions, bone over the lingual aspect of the third molar roots is less dense, permitting a greater chance that supraperiosteal anesthesia will be successful. However, the proximity of the lingual nerve to this site leads to cautions against attempting lingual infiltration in the area of the mandibular molars.
The superior border of the ramus has two processes: the coronoid anteriorly and the condylar posteriorly. Between these two processes is a deep concavity, the mandibular (sigmoid) notch. The coronoid process is thinner than the condylar. Its anterior border is concave—the coronoid notch. The coronoid notch represents a landmark for determining the height of needle penetration in the inferior alveolar nerve block technique. The condylar process is thicker than the coronoid. The condylar head, the thickened articular portion of the condyle, sits atop the constricted neck of the condyle. The condylar neck is flattened front to back. The attachment for the external pterygoid muscle is on its anterior surface.
When cut horizontally at the level of the mandibular foramen, the ramus of the mandible can be seen to be thicker in its anterior region than it is posteriorly. This is of clinical importance during the inferior alveolar nerve block. The thickness of soft tissues between needle penetration and the osseous tissues of the ramus at the level of the mandibular foramen averages about 20 to 25 mm. Because of increased thickness of bone in the anterior third of the ramus, the thickness of soft tissue is decreased accordingly (approximately 10 mm). Knowing the depth of penetration of soft tissue before contacting osseous tissues can aid the administrator in determining correct positioning of the needle tip.
References
1. DuBrul, EL. Sicher’s oral anatomy, ed 7. St Louis: Mosby; 1980.
2. Heasman, PA. Clinical anatomy of the superior alveolar nerves. Br J Oral Maxillofac Surg. 1984;22:439–447.
3. McDaniel, WL. Variations in nerve distributions of the maxillary teeth. J Dent Res. 1956;35:916–921.
4. Loetscher, CA, Walton, RE. Patterns of innervation of the maxillary first molar: a dissection study. Oral Surg. 1988;65:86–90.
5. Langlais, RP, Broadus, R, Glass, BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985;110:923–926.
6. Frommer, J, Mele, FA, Monroe, CW. The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc. 1972;85:113–117.
7. Blanton, PL, Jeske, AH. The key to profound local anesthesia: neuroanatomy. J Am Dent Assoc. 2003;134:753–760.
8. Yonchak, T, Reader, A, Beck, M, et al. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog. 2001;48:55–60.
9. Meechan, JG, Ledvinka, JI. Pulpal anaesthesia for mandibular central incisor teeth: a comparison of infiltration and intraligamentary injections. Int Endod J. 2002;35:629–634.
10. Phillips, JL, Weller, N, Kulild, JC. The mental foramen. Part III. Size and position on panoramic radiographs. J Endodont. 1992;18:383–386.
11. Shiller, WR, Wiswell, OB. Lingual foramina of the mandible. Anat Rec. 1954;119:387–390.
12. Bremer, G. Measurements of special significance in connection with anesthesia of the inferior alveolar nerve. Oral Surg. 1952;5:966–988.
13. Hayward, J, Richardson, ER, Malhotra, SK. The mandibular foramen: its anteroposterior position. Oral Surg. 1977;44:837–843.
14. Monheim, LM. Local anesthesia and pain control in dental practice, ed 4. St Louis: Mosby; 1969.
15. Hetson, G, Share, J, Frommer, J, et al. Statistical evaluation of the position of the mandibular ramus. Oral Surg. 1988;65:32–34.