Upper Extremity Prosthetics
1 Identify the characteristics of various upper extremity prosthetic devices.
2 Define the various causes and levels of amputation.
3 Differentiate between various levels of amputation.
4 Identify advantages and disadvantages of passive (semiactive), body-powered, externally powered, and recreational prostheses.
5 Differentiate the roles of the prosthetic team members.
6 Describe the sequence of training in prosthetic rehabilitation.
7 Explain the unique role of the occupational therapist in upper extremity prosthetic rehabilitation.
8 Identify psychosocial aspects of clients with amputations.
9 Describe upper extremity prosthetic intervention in children.
10 Discuss new updates in prosthetic technology and research.
Some readers may question the compatibility of a prosthetics chapter in this orthotics text. Several chapters in this text address needs of specific populations. This text is designed as a resource for those therapists interested in developing orthotic skills to address the needs of these populations. Therapists who treat persons with orthotic needs will naturally be called upon to provide services to persons with upper extremity amputations.
Orthotics and prosthetics are closely interrelated fields. Forty percent of American Board for Certification (ABC) certified practitioners hold credentials in both orthotics and prosthetics. This chapter is designed to serve as a resource for those therapists who serve this historically underserved population. Approximately 40,000 amputations occur each year in the United States. Thirty percent involve the upper extremity [Leonard and Meier 1988, Muilenburg and LeBlanc 1989], and upper extremity amputations represent approximately 10,000 people per year [Malone et al. 1984, Centers for Disease Control and Prevention 1996].
Approximately 50% of individuals are fitted with prostheses [Muilenburg and LeBlanc 1989]. Of the 50% fitted with a prosthesis, only half actually wear the device. Experts cite numerous reasons for this trend [Shurr and Cook 1990]. Fit and prosthetic training appear to be the most salient factors that affect prosthetic wear [Bennett and Alexander 1989]. The role of the prosthetist is to provide a well-fitting prosthetic device. It is the role of the occupational therapist to assist the individual to become an independent user of the device. The prosthesis is often heavy and awkward to use. If the fit is not tolerable, or if the potential wearer has not been properly trained to use the device, the prosthesis may end up on the closet shelf.
Unfortunately, only a small number of health care providers have extensive knowledge of the rehabilitation of the person with an upper extremity amputation. The typical therapist may encounter few individuals with upper extremity amputations. Thus, it is difficult to remain abreast of the current prosthetic trends and technologic developments that affect how therapists promote the maximal level of independence for the client with an upper extremity amputation. However, occupational therapists can make a substantial difference in the lives of individuals with amputations if they possess knowledge of the various factors that impact the life of a person with an amputation.
This chapter provides the therapist with general knowledge on upper extremity amputations and their impact on function. Next, the chapter delineates roles of the team members and discusses the various prosthetic options and componentry. Goals for occupational therapy (OT) throughout the prosthetic rehabilitation process are described. Finally, this chapter describes marketing strategies and recommendations for a therapist wanting to increase the number of prosthetic referrals received.
Amputation Levels and the Impact on Function
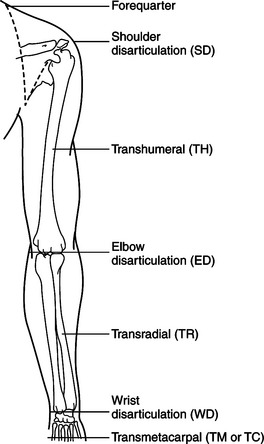
Figure 18-1 provides an outline of the various amputation levels, along with abbreviations associated with them [Santschi 1958]. The more distal the amputation the greater the degree of natural function retained. Consequently, less is demanded of the prosthesis [Law 1981]. For example, an individual who has an amputation at the midhumeral level may be functionally able to use shoulder internal and external rotation along with other shoulder motions. However, the person lacks elbow flexion and extension and forearm supination and pronation. This is a disadvantage. If an individual with a midhumeral amputation wants to receive money from a cashier, more effort is required.
First, positioning and locking the elbow in flexion is necessary. Next, the person manually rotates the terminal device to the palm-up position with the sound side. Finally, the person is ready to perform the act of receiving the money. Conversely, an individual with an amputation at the wrist level is functionally able to pronate and supinate, flex and extend the elbow, and retain full shoulder function in the completion of activities of daily living (ADL).
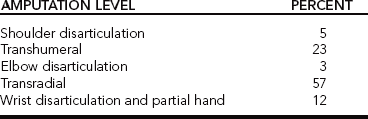
The ability to pronate and supinate serves as a substantial advantage, enabling the person with the amputation to turn the prosthetic hand palm up as if to receive money from a cashier without the substitution movements of shoulder external rotation. Whether or not an individual chooses to wear a prosthesis, the level of amputation directly impacts function. The estimated frequencies of levels of amputation of the 50% who wear a prosthesis are presented inTable 18-1, indicating which level is most common [Muilenburg and LeBlanc 1989]. It is apparent that most amputations occur at the transradial level.
Causes of Upper Extremity Amputations
The causes of upper extremity amputations differ from the causes of lower extremity amputations. Lower extremity amputations are largely a result of disease. The majority of upper extremity amputations result from trauma [Leonard and Meier 1988]. Other causes include disease, tumors, elective surgery, and genetic anomaly [Bennett and Alexander 1989]. Commonly, therapists work with individuals who before injury used their hands extensively in their daily occupations. Often these persons hope to regain a similar level of independence. A power-line worker describes his experience in the following words.
The 7,200-volt power line was approximately five feet from where I came in contact with it. It’s a strange thing, but I don’t remember touching it. According to my co-workers, I started screaming and there was a bright electrical arc between my hands for about 10 seconds. The foreman shut off the power and got the boom truck to get me down…. I noticed there was no flesh on my hands anymore. Both hands were charcoal black! I knew they would have to be amputated, but the only thing I was concerned with was getting to a hospital to relieve some of the unbearable pain…. I’ve had four major operations at St. Elizabeth for amputations. I didn’t know for sure at the time how much they would have to take off. They amputated just above the elbow the first time. And I remember that the stumps looked pretty long the first time, but the second time they got a little shorter, and then the third time they really got short. On the fourth operation they removed an infected area from my right stump and armpit. I was given medication to help build tissue to fill those holes back in [Crane 1979, p. 10].
The Team Members
The team treating a person with an amputation is instrumental in the prosthesis-fitting process. The team consists of the person with the amputation, the prosthetist, and the therapist. The primary goal of therapy is to provide the individual with the proper tools and techniques to regain independence. A team approach combines expertise and experience, creating a synergy of professionalism, with team members working together and promoting the maximal level of independence for the individual with the amputation. The best results in upper extremity rehabilitation include interdisciplinary teamwork [Baumgartner and Bota 1992].
The Client
The primary member of this team is the person with the amputation. Individual goals, desires, and needs establish the foundation for which the team develops the action plan. Clients’ priorities for rehabilitation can vary. Common concerns include cosmesis, function, weight, maintenance, and funding for the prosthesis [Atkins et al. 1996]. For example, the needs of an individual with a transradial amputation who works full-time and desires to return to work may vary from those of an individual who is a stay-at-home parent. The type of prosthesis selected would vary, depending on a precise analysis of the client’s work, leisure activities, and ADL.
An important aspect to the client is early postoperative prosthetic fitting. The advantages of early fitting are decreased edema, reduced postoperative and phantom pain, accelerated wound healing, improved rehabilitation, and decreased length of hospital stay [Malone et al. 1984].
The Prosthetist
The prosthetist has knowledge of the technology and componentry available. The prosthetist specializes in componentry, fit, and prosthesis fabrication. It is the responsibility of the prosthetist to understand the client’s primary diagnosis as it relates to the need for prosthetic services [Billock 2003]. The prosthetist must introduce, educate, and orient the client to the controls and functions of the prosthesis. Daily care and maintenance of the prosthesis are taught to the client by the prosthetist and should be reinforced by the therapist. The prosthetist and the therapist may collaborate when exploring the prosthetic options with the client.
The Occupational Therapist
A well-rounded rehabilitation program is advised because the quality of training will directly determine how the individual uses the prosthesis for the rest of his or her life [Lake 1997]. The therapist has many responsibilities. It is important that therapists know the basic differences in prostheses to make proper recommendations of components to the team. Therapists should also recognize the importance of collaboration with skilled upper extremity prosthetists, with the purpose of maximizing the training process and the degree of independence [Atkins and Alley 2003]. Without proper therapy, the benefits of prosthetic use may be limited.
The therapist reinforces and builds on residual movement, developing functional applications of the prosthesis to address the distinct ADL (e.g., brushing teeth) and instrumental ADL (e.g., driving) of each individual [Toren 2002]. The therapist is responsible for ensuring the client knows how to clean and maintain the prosthesis. In addition, the therapist provides opportunities for the client to practice using the prosthesis in specific daily activities. The therapist focuses on bilateral activities. Often, after amputation the individual becomes successful in performing some ADLs unilaterally. Thus, therapy must begin early in the rehabilitation process to facilitate use of the prosthesis in bilateral activities.
Initial prosthetic training begins with a reorientation to the prosthesis and basic open-and-close control. Training then includes controlled grasp, such as opening in small increments to grasp small items and then more fully to grasp larger items. Training emphasizes grasping objects of varied texture and density to be handled. Sessions incorporate work on prehension and timing of release. Functional and appropriate tasks are encouraged and require the client to use the prosthesis for gross and fine motor activities. Training also emphasizes tasks to achieve all of these components in a variety of planes [Patterson et al. 1991, Keenan 1995]. With the combined efforts of the team members, the appropriate prosthetic components are chosen so that the individual can achieve goals through therapy, practice, and education.
Prosthetic Options
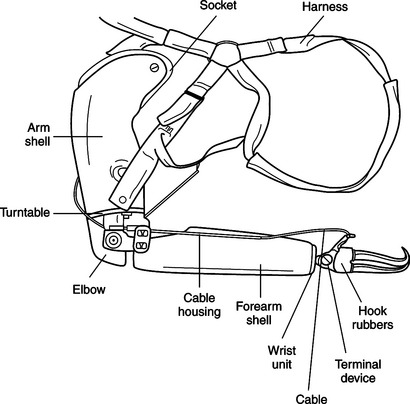
Generally, four categories of prosthetic options are available for the person with an upper extremity amputation. The options include (1) no prosthesis; (2) a passive (semiactive), cosmetic prosthesis; (3) a cable-driven body-powered prosthesis; and (4) an externally powered, electrically controlled prosthesis with either myoelectric sensors or specialized switches.Table 18-2 outlines the pros and cons of each prosthetic option [Law 1981, Muilenburg and LeBlanc 1989].
A prosthetic device cannot mechanically duplicate the amount of function, reliability, and cosmesis the human hand naturally provides. Therefore, it is important for the health care provider to possess knowledge of the various options continually being developed for future selection of prostheses. A fundamental understanding of these five components is necessary. These five components include the harness, socket, cable, terminal device, and glove.
No Prosthesis
Wearing no prosthesis is one option, and for some individuals it is the best option. For example, an individual may not be able to tolerate the prosthesis for reasons such as residual limb hypersensitivity, soft tissue adhesions, and excessive scarring [Atkins and Meier 1989]. Individuals who choose not to wear a prosthesis may find advantages and disadvantages with their decision, which are found inTable 18-2.
Advantages include increased proprioceptive and sensory input. Disadvantages include limited functional ability, difficulty in completion of bimanual tasks, and possibly the development of overuse syndrome and nerve entrapment in the contralateral limb [Reddy 1984]. Additional reasons an individual may not wear a prosthesis include not knowing the prosthetic options, having a bad first prosthetic experience, lack of funding, or reluctance to undergo revision surgery necessary for prosthetic fit and reduction of hypersensitivity [NovaCare 1991].
Passive Prosthesis
A passive (semiactive) prosthesis option is common for individuals who have had amputation distal to the elbow, in that they may maintain elbow flexion and extension and forearm pronation and supination. In this case, the obvious purpose is cosmetic. However, a passive prosthesis provides some degree of function. A passive prosthesis has many benefits, including its light weight, minimal (if any) harnessing, no cables, and low maintenance. Disadvantages include lack of prehensile abilities and difficulty in performing some bimanual tasks. Functionally, the digits of a passive prosthesis can be adjusted to assist with such activities as carrying a purse or a document or operating the gearshift in an automobile [Law 1981].
Body-powered Prosthesis
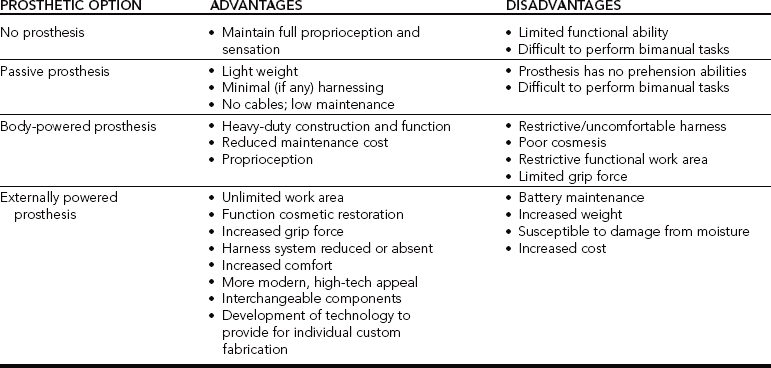
A body-powered prosthesis is a type of functional prosthesis most commonly used by clients with upper extremity amputations [Law 1981]. The body-powered prosthesis may not be cosmetically pleasing to everyone, but it is sturdy and allows for prehension. Body-powered upper limb prostheses are actuated by body motion, which generates tension in a cable. The cable courses from a shoulder harness through a helical coiled housing to a prosthetic component, such as a hook or elbow [Carlson et al. 1995]. In other words, the active movements of the shoulder and arm cause the tension in the cable to open and close the hand or handlike component (hook). The device is illustrated inFigure 18-2.
Benefits of a body-powered prosthesis include its heavy-duty function and construction, decreased maintenance cost, and increased proprioceptive input. Disadvantages may include the restrictive uncomfortable harness, potential for nerve entrapment or compression, decreased cosmetic appearance, restricted functional work area, and limited grip force. Body-powered terminal devices generally weigh less than the externally powered prostheses because they lack the heavy motors and circuitry placed within them to operate the myoelectric signals [Atkins and Meier 1989].
Body-powered Prosthetic Components
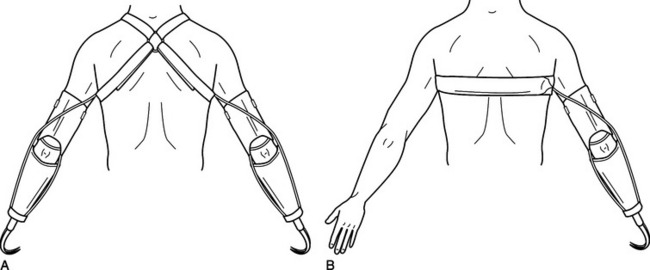
The Harness.: The purpose of the harness is to suspend the prosthesis on the residual limb. It transmits force from the body to the prosthesis for independent operation of the prosthetic components [Muilenburg and LeBlanc 1989]. The body-powered prosthesis always requires harnessing. There are two primary types of harness: a figure-of-eight and a chest strap. The figure-of-eight harness passes over the shoulder, across the back, and under the contralateral axilla. “The ring lies flat in the back, inferior to C-7 and just to the sound side of the center of the spine” [Shurr and Cook 1990].
The standard figure-of-eight shoulder harness (Figure 18-3A) for the upper extremity has an axilla loop on the sound side that is commonly uncomfortable and can cause numbness and nerve damage [Collier and Le Blanc 1996]. The chest strap offers an alternative method of harnessing. It travels across the back, under the contralateral axilla, and across the chest (Figure 18-3B). It is important that the harness, either figure-of-eight or chest strap, be tight enough to activate the terminal device (TD) without excessive effort and loose enough to be comfortable and allow freedom of movement of both arms and shoulders.
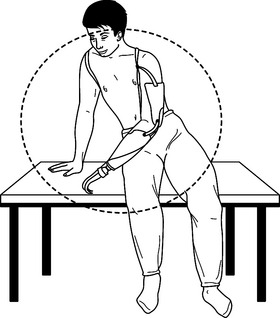
Long-term wear and inappropriate fit may cause discomfort or physical damage. The harness has been found to limit the functional work envelope, which is the space in front of the person who is able to use the prosthesis successfully for functional tasks. Harness systems limit successful prehension when the TD is outside the functional work area. With the body-powered prosthesis, function is limited above the head, behind the back, and near the ground, primarily because of the restricting harness (Figure 18-4). The prosthesis functions as a result of the ability to move in these planes.
Discomfort and neurologic and musculoskeletal disorders can result from inefficient harness design [Carlson et al. 1995] and long-term wear. After years of wearing a harness, the axilla of the sound side experiences increased force and pressure to operate the prosthesis repetitively throughout the day. This can result in neurologic damage. A strong case can be made for providing a myoelectric or externally powered prosthesis that either eliminates or reduces the harnessing. This prevents the risk of long-term nerve damage on the sound side.
The prosthetist is responsible for fabrication of the harness, and the therapist occasionally may make minor adjustments to improve function. Sometimes several harness options are attempted to find the type of system that best fits the amputee. It is often a trial-and-error process. Another important factor is the awareness of the increased workload in the remaining arm, which may produce symptoms ranging from minor aches to serious conditions such as nerve entrapment and overuse syndrome [Jones and Davidson 1999].
The Socket.: The socket is the part of the prosthesis that intimately fits over the individual’s residual limb. It is the connection between the prosthesis and the individual’s body. The socket is fabricated from an exact mold of the residual limb, and it is fabricated from various types of laminate or thermoplastic material. Development of high-temperature rigid plastic materials has made it possible to have total contact on the skin and allow decreased weight and increased durability. The use of carbon graphite and the introduction of flexible thermoplastics are more comfortable, lighter, and durable and have made soft sockets with windows possible. The prosthetist makes modifications over bony prominences and areas susceptible to torque and shear forces [Andrews and Bouvette 1996]. Typically, three to four sockets will be fabricated before the final one is delivered.
Intimate socket fit provides a stable foundation of support necessary to transfer forces from the TD. It provides evenly distributed pressure on the residual limb, which prevents skin breakdown or pressure sores. In the last decade, a multitude of design innovations have been incorporated, which have resulted in developing better comfort, suspension, stability, and range of motion. The new fitting techniques and socket designs appear to be more efficient for force of transmission and motion capture and more functionally consistent than traditional sockets [Alley 2002]. Occasionally, the prosthetist instructs the individual to wear the socket before all components are attached. This increases wearing tolerance and facilitates reshaping of the residual limb.
As the person with the amputation ages, physical and physiologic changes occur. The person may experience weight loss or gain or muscle bulk increase or decrease. These changes have an impact on the size and condition of the residual limb, and the socket may no longer fit as it should. A new socket must be fabricated to fit the exact shape of the residual limb when changes occur. When a new socket is fabricated, it replaces the poorly fitting one in the individual’s current prosthesis. An entirely new prosthesis is not needed because the socket is removable and replaceable. This saves on cost. The wearer of a body-powered prosthesis may benefit from using a second sheath or sock made of either a fabric or a gel-like substance to manage poor skin integrity, prevent breakdown, absorb moisture, or provide padding.
The Cable.: The harness allows placement of the cable, which is the transmitting force that operates the prosthesis. Body-powered prostheses are operated by body motion that generates tension in the cable. The cable is routed from the harness through a housing to the terminal device or elbow [Carlson et al. 1995]. The primary movement to operate the prosthesis is glenohumeral flexion. As the individual flexes the humerus, the TD opens. As the individual returns the humerus to neutral, the hook rubbers cause the TD to close. When the individual wishes to open the TD closer to the body, biscapular abduction is used and adduction or retraction of the scapula allows the TD to close (Figure 18-5). The following quotation from a client with an upper extremity amputation highlights the importance of the cable system for functional tasks.
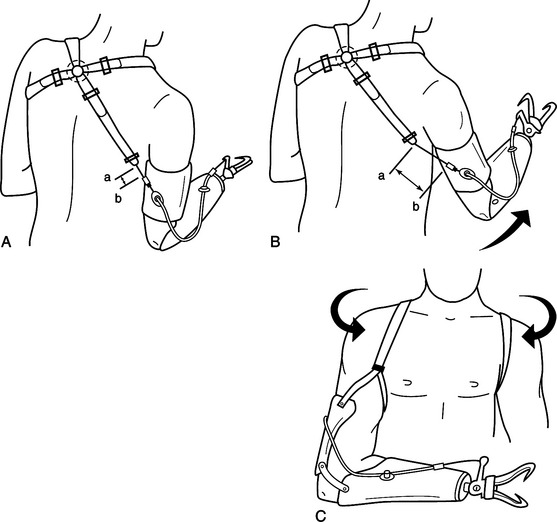
Figure 18-5 Body motions used to transmit force to terminal device: (A) Glenohumeral flexion, (B) biscapular abduction, (C) scapular adduction/retraction.
The rubber bands on my hooks regulate tension I put on objects. To force the hook open, I first lock the elbow in the desired position. Then I proceed to bring my shoulder forward, putting tension on the cables. After I have grasped the desired object, I bring my shoulder back to the original position [Crane 1979, p. 12].
Cables need periodic replacement when they fray or break. Cable replacement is generally the most common repair need for the body-powered prosthesis wearer [Crane 1979]. The occupational therapist and the client should know how to replace an old cable with a new one. The process is fairly simple, involving removal of the old cable and reattachment of the new cable to the TD and the harness. It is beneficial for the client to have two or three spare cables at home so that replacement is convenient.
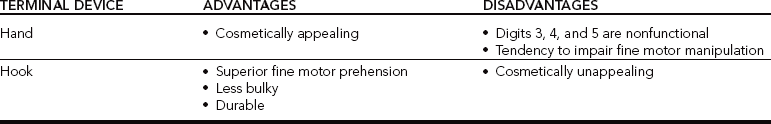
Terminal Device.: The TD is the hand component and appears in the form of a hand or a hook. Most body-powered prosthetic hands open and close in a three-point prehension pattern. The prosthetic hooks open and close in a lateral or tip pinch prehension pattern, depending on positioning of the TD. In addition, a variety of TDs are available for certain recreational activities, such as bowling, skiing, baseball, golfing, and volleyball [Radocy 1987] (Figure 18-6). Therapists should be familiar with TD options because they will most likely introduce the person with the amputation to the available options and provide education in their use.
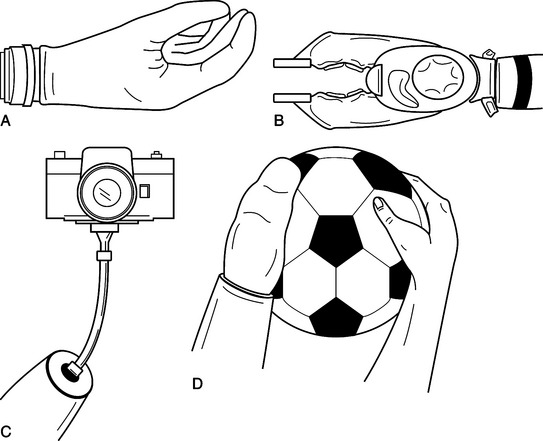
Figure 18-6 Terminal device options: (A) Hand, (B) greifer, (C) photography terminal device, (D) volley ball/soccer terminal device.
Generally, the initial goals of the prosthetist are to fit the person who has had an amputation with a standard prosthesis. The person with the amputation then requires time to adjust and become an independent user of the prosthetic device. This individual may not be visiting the prosthetist for some time but is interested in completing a specific activity. Sometimes the occupational therapist can fabricate a tool of thermoplastic or other material that can be attached to the TD to serve a specific function. At other times, collaboration with the prosthetist may be necessary to obtain a specific TD or a sophisticated adaptation.
Some individuals benefit from two TD options. Typically, an individual has some form of a hand and a hook, which are interchangeable. For example, the client uses the handlike TD for basic ADL and uses the hooklike TD for more challenging activities such as quilting or changing a tire. Every terminal device has its pros and cons. Differences exist between the hand and hook TDs (Table 18-3). The handlike TD seems to be more cosmetically pleasing. However, digits 3, 4, and 5 are nonfunctional, often impairing function and providing increased bulk. The hooklike TD allows for successful fine motor prehension, is less bulky, and is more durable. However, it may be less cosmetically appealing than the handlike TD.
Grip Strength of Body-powered TD.: The body-powered grip can vary from 5 to 20 pounds, depending on the number of hook rubbers used. Hook rubbers are similar to thick, wide rubber bands providing resistance to the grip of the TD. Each rubber band provides 1 pound of grip force, consequently increasing the amount of pressure placed in the axilla on the contralateral side.
The Glove.: The glove is the cosmetic covering of the handlike TD. Gloves are made of either latex or silicone substances and are removable and replaceable. Differences exist between the two types of glove. Latex gloves are sturdy and come in 10 to 15 shades of color. Individuals are matched to the shade that corresponds to their skin tone. Latex gloves easily absorb stains that do not wash off. However, latex gloves are more durable than silicone gloves.
A silicone glove is custom fabricated to match the individual in terms of shape, size, and coloring. It is difficult to differentiate between a silicone glove and a human hand by sight. Such a glove is truly a work of art. Silicone gloves are more costly and fragile than latex gloves. It is more difficult to permanently stain a silicone glove. However, they tear easily. Persons who have had an amputation generally request the silicone glove because of its lifelike appearance. Because silicone gloves are more expensive, funding for a silicone glove is difficult to obtain.
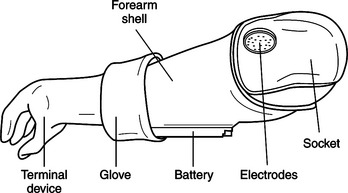
Externally Powered Prosthesis
The externally powered prosthesis is another prosthetic option. The externally powered prosthesis is also called a myoelectric prosthesis because it operates from the electromyographic (EMG) signal transmitted from the muscles of the residual limb. An externally powered prosthesis has several differences from the body-powered prosthesis, which are outlined inTable 18-2. Beneficial characteristics of a myoelectric prosthesis include an unlimited work area, functional cosmetic restoration, increased grip force, elimination of harnessing, increased comfort, interchangeable componentry, and individualized custom fabrication. Disadvantages of a myoelectric prosthesis include increased weight, increased cost, increased maintenance, and increased risk of damage.
Externally Powered Prosthetic Components
The externally powered prosthesis comprises various components, as shown inFigure 18-7. The components include a socket, a forearm shell, electrodes, battery, glove, and TD.
The Harness.: Most myoelectric prosthetic devices do not require a harness. Occasionally, a harness system is required if it is difficult to fit and maintain contact between the electrodes and the muscle signal or if the socket is loose because of weight loss or other factors. Because the harness system is either eliminated or reduced, the functional work area is expanded to include the areas above the head, behind the back, and near the ground compared with the body-powered prosthesis (Figure 18-8).
Externally Powered Prosthetic Socket.: The externally powered prosthetic socket is unique in that it has electrodes that detect the EMG signals of the muscle. The electrodes are mounted directly in the walls of the flexible socket. The EMG signal stimulates the motor in the prosthesis to produce a desired motion. Prosthetics for clients with upper extremity amputations have dramatically changed over the past several years. The main changes have occurred in components, socket fabrication, fitting techniques, suspension systems, and sources of power and electronic controls [Esquenazi et al. 2002].
There are a variety of electrodes available. Some are more sensitive than others in detecting the muscle EMG and controlling the movement of the TD. Through the collaborative effort of the team, the best-suited electrodes are determined. Single- or dual-site control systems are available. A single-site system is used if the client cannot differentiate and isolate control of two separate and opposing muscles for electrode sites. This may be beneficial for persons who are cognitively unable to control the dual site system, such as with pediatrics. For example, the TD would remain in the closed position when the individual’s muscles are relaxed and open when the muscle contracts. Thus, if the individual wanted to grasp an object he or she would contract the muscle to open the TD, position it around the desired object, and relax. Upon relaxation, the TD automatically closes and remains closed until the next muscle contraction.
Commonly, a dual-site control system is preferred over a single-site system. The dual-site control system is activated by two separate muscle contractions. For example, the individual with a transradial amputation will most likely contract the wrist extensor muscle group to open the TD and the wrist flexor muscle group to close the TD. The TD has the ability to remain in any position as long as the muscle signals are absent. For example, the same individual can open the TD with contraction of the wrist extensors. Once the muscles are relaxed, the TD will stay open as if to shake the hand of a friend. As soon as the wrist flexors are contracted, the TD will close. With this system, a sheath or sock cannot be worn because it would interrupt the connection between the muscle and the electrode. As a precaution, it is important to remember that the externally powered TD has a grip strength greater than that of the normal individual.
Externally powered terminal devices have a greater opening range, allowing for the ability to grasp objects of larger size. The externally powered prosthesis provides the ability to use prehension capabilities in all planes. This contributes to the expansion of the functional work area to include space above the head, behind the back, and near the ground.
Grip Strength of Externally Powered TD
There are differences between an externally powered TD and a body-powered TD. An externally powered TD presents with increased grip strength compared to the body-powered terminal device. The externally powered TD generally provides grip strength of approximately 20 to 30 pounds, compared with the 5 to 20 pounds of grip strength of the body-powered TD.
The Battery
Lithium-polymer battery technology advancements have improved the ease of externally powered prostheses. The lithium-polymer batteries are 80% lighter, 70% smaller, and offer 30% more storage capacity than nickel-cadmium batteries [Billock 2003].
Prosthetic Rehabilitation
The educational background of occupational therapists includes motor control, motor learning, and movement as they relate to the upper extremity function required for occupational performance. Education in the psychologic adjustment to disability is also the occupational therapist’s area of expertise. These strengths are vital because postsurgical therapy often incorporates wound care and contracture management. In addition, occupational therapists assist persons in adjusting to the amputation. Post-surgical goals include scar management, desensitization, pain management, swelling reduction, and limb shrinkage. Psychological intervention related to phantom pain and phantom sensation should be implemented as soon as possible.
The sooner therapy is initiated the faster the client will be prepared for prosthesis fitting and the chances of engaging in bimanual activities will increase. Note how one individual describes part of his post-surgical therapy. This range of motion deficit possibly could have been prevented with early intervention from therapy.
During the first three weeks in therapy, I didn’t have movement in my stumps. They were frozen solid. I just couldn’t believe it. They stood straight out, and that was about it. It took a long time to break this loose to where I could get movement in my stumps again…. It was a very painful experience [Crane 1979, p. 11].
Effective communication is vital between the prosthetist, the therapist, and the individual with the amputation to ensure that everyone is striving to best meet the goals of the client.
Phases of Rehabilitation
Prosthetic rehabilitation can be categorized into two phases: the pre-prosthetic phase and the post-prosthetic phase. The pre-prosthetic phase prepares the client for prosthesis wear and usage. The post-prosthetic phase primarily teaches the client to maintain and use the prosthesis in daily activity.
Pre-prosthetic Phase
The pre-prosthetic period begins when the individual with the amputation becomes a prosthesis candidate. The phase concludes upon prosthesis delivery. Time during the pre-prosthetic phase is crucial for reinforcement of realistic expectations. Individuals with amputations may be under the assumption that they will perform all activities at the same level of independence they had before the amputation. This assumption needs to be discussed with the client. Therapists should explain that the prosthetic device will not replace the arm. Rather, it is an assistive tool used to stabilize, support, and hold objects during bimanual activities [Doolan 2001].
Clients may experience disappointment when the prosthesis is delivered and they are unable to use it as they imagined. It is the duty of the team to inform individuals of the advantages and disadvantages of the various components to provide a realistic picture of rehabilitation. Clients are usually surprised when they realize that the prosthesis is hard, cold, heavy, and not a true replacement for the hand. With establishment of realistic expectations and acceptance, use of the device greatly improves [Atkins et al. 1996].
During the pre-prosthetic phase, individuals frequently visit the prosthetist for fittings and modifications of the socket. Clients also see the therapists for rehabilitation services. Individuals receiving body-powered prostheses move much quicker through the fabrication and rehabilitation process because electrodes are not required and muscle sites and signals do not need to be identified.
Electrode Training
If an individual is receiving an externally powered prosthesis, the best muscle sites are identified and trained to operate the prosthetic features. Finding the sites and training the muscles for electrode placement are primarily the responsibility of the therapist. During this phase, the occupational therapist provides extensive training, using biofeedback to teach the individual to contract the identified muscle or muscles on command. The therapist facilitates the improvement of muscle site control and focuses on isolated muscle contraction, strength, and endurance. Special biofeedback machines are often available from the prosthetist. It is important for the client to practice muscle contractions in a variety of positions, including lying, standing, and sitting. Practicing muscle contraction in different positions, with the extremity in various planes, enhances maximal success after delivery of the prosthesis.
Once electrode sites are established in therapy, the prosthetist is informed of the exact and most appropriate electrode location for the individual to obtain the most function. Locating and training for electrode sites is often a lengthy, rigorous, trial-and-error process. Once the socket and electrode sites are sufficient to work the prosthesis, the prosthesis is ready for final fabrication. There may be a period of time after the pre-prosthetic phase when the individual is discharged from occupational therapy with a home program until the prosthesis is ready for delivery and therapy can resume.
Additional goals of occupational therapy during this phase include preparation of the individual to tolerate wearing the prosthesis and using it independently for daily activities. Specifics include promoting wound care and preventing infection; maintaining range of motion and eliminating contractures; desensitizing the residual limb to pressure, pain, and weight; edema control; and unilateral independence.
Promoting Wound Care and Preventing Infection
Specific goals of the treatment include the client’s independence in dressing changes and good hygiene [Keenan 1995]. This may include instruction in dressing change techniques and scar mobilization to prevent adhesions and hypersensitivity.
Maintaining Range of Motion and Eliminating Contractures
By focusing on the residual joints of the affected extremity, the therapist prevents loss of motion. In some cases the therapist provides necessary stretching or joint mobilization to ensure adequate range of motion, and therefore successful function during use of the prosthesis. Home exercise programs are necessary. In addition, positioning or splinting techniques may be used if necessary.
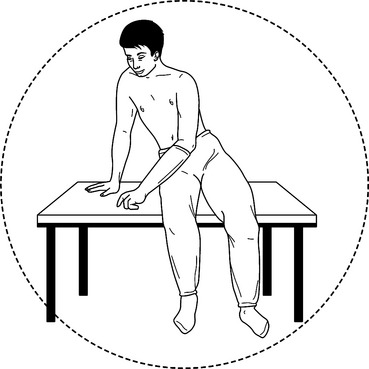
Desensitizing the Residual Limb to Pressure, Pain, and Weight
It is common for the client to experience residual limb sensitivity. The occupational therapist can intervene by teaching and implementing the following desensitization techniques: wrapping, massage, weight bearing, and pain management.
Phantom sensation and phantom pain are normal experiences most clients who have had an amputation encounter [Omer 1981]. The role of the team is to prepare clients and assure them that these sensations and pain are expected and are a normal phenomenon. Phantom sensation occurs when the individual feels as if the nonexistent limb is still present. The amputated extremity may feel exactly like the original limb in terms of shape, size, position, and ability to move. Rings or watches that were previously worn may be part of the sensation [Omer 1981]. Phantom sensation is described as a pins-and-needles or tingling sensation. Phantom sensation diminishes over time. It has been reported to persist from 6 months to 20 years [Frazier and Kolb 1970].
Phantom pain is different from phantom sensation. The phenomenon of phantom pain is not completely understood. Phantom pain is generally described as pain that does not follow nerve distribution patterns [Omer 1981]. The pain is extreme and can be managed through alternative medicine techniques, therapeutic modalities, and medication. The following statement from a person with an amputation describes his experience with phantom pain.
I never realized it before, but there is a type of pain called phantom pain. It felt like my hands were in rubber gloves and the rubber gloves were filled with water all the time. I was afraid if I told the doctor, he probably wouldn’t let me out of the hospital, or to go on to rehabilitation—he would think that I was nuts. When I got home it felt like a cigar butt had been put out in my hand, and it burned…. the first few days I walked the floor at nights with phantom pain. I couldn’t sleep at night. I walked and I walked. Finally, I told [my doctor] about my problem. He told me that it wasn’t unusual at all and prescribed some medicine. The pain didn’t go away entirely, but it became bearable [Crane 1979, p. 11].
Desensitization and pain management are additional components of the therapy. The therapist may provide modalities for pain as well as educate clients to manage the pain independently. Each client presents with different complaints, and the treatment is individualized.
Edema Control
Edema can be controlled through wrapping the residual limb in a diagonal design, so as not to compromise circulation. Another technique includes the use of compression socks. Compression has a direct impact on residual limb shrinkage and shaping. Elevation and retrograde massage are also useful alternatives to decrease edema. It is important for the therapist to reinforce the importance of edema management because it has a direct impact on socket fit and comfort.
Unilateral Independence
Unilateral independence involves using environmental adaptations and one-handed techniques, which are in an occupational therapist’s area of expertise. It may be necessary to teach the client to switch hand dominance if the dominant hand was amputated. Generally, the occupational therapist works to promote the maximal level of independence for the individual. Often therapists issue adaptive equipment. For the client with an amputation, it may promote better prosthetic success if the therapist does not issue adaptive equipment until after prosthetic training because the client may become efficient with the adaptive equipment and may not be motivated to learn to use the prosthesis.
Post-prosthetic Phase
Post-prosthetic training can be divided into four general phases: orientation, control training, use training, and daily living skills training [Keenan 1995]. The post-prosthetic phase is initiated once the prosthesis is delivered. This phase is the most important to the occupational therapist. A client’s visits to other members of the team decrease, and the occupational therapist acts as the team liaison. The following is a client’s perception of the post-prosthetic phase.
It took a lot of practice and patience to learn how to manipulate my new arms. For example, as a normal individual would reach for that first cup of coffee in the morning, I would ask myself, “How should I hold that cup of coffee? Shall I lock my elbow in at a 90-degree angle and put my hook around the cup, or should I grab the cup through the handle?” If I want to move my arm up, I have to extend my shoulder forward or my stump forward. In order to reach a certain direction, I have to lock my elbows in the desired height, whether it’s 45, 90, or 115 degrees, and then I lower my elbow to where the cable tightens up [Crane 1979, p. 12].
Orientation
Upon delivery of the prosthesis, the prosthetist educates the client about the prosthesis and its components. It is the responsibility of the therapist to reorient the client to the prosthesis. A prosthesis is a very complex tool, and it cannot be mastered in one instruction session. The client will not be independent with the prosthesis unless there is a complete understanding of all of the components.
Orientation for the client includes education on how to don, doff, operate switches and batteries, and care for the prosthesis. The therapist ensures that the fit and function of the prosthesis are adequate. This includes evaluation of the client’s independence with donning and doffing. The client must know how to properly care for the prosthesis so as to promote success and prevent unnecessary damage.
Control Training
This phase is the longest portion of post-prosthetic rehabilitation for the client because it is repetitive and difficult. During this time, the client learns to operate the controls of the prosthesis and practices until becoming proficient. Depending on the features of the prosthesis, this includes such tasks as opening and closing the terminal device, elevating and lowering the elbow, and rotating the wrist on command. Activities can be graded (for example, controlling the TD to open in 3, 4, or 5 separate steps).
Use Training
Use training involves applying the mechanics of operation to repetitive tasks to facilitate eventful functional use and endurance. This portion of rehabilitation includes using the prosthesis to grasp and release objects of various sizes, textures, and weights in different planes and positions. It can be difficult to grasp an object above the head because the individual must relax the wrist extensors and contract the flexors while the hand is elevated. This is difficult to accomplish because of the weight of the prosthesis. Examples of other activities practiced during this portion of the rehabilitation include holding and placing a tomato on a shelf without crushing it or playing a card game with the cards held by the TD.
Daily Living Skills and Functional Training
This phase of rehabilitation should be the most familiar and comfortable phase for the occupational therapist because the focus is on function of the individual. During this time, the therapist and the client address the specific skills gained and apply them to the client’s individual functional requirements, lifestyle, and interests. Training may include grooming and hygiene, meal preparation, dressing, child care, or other required tasks. The client may choose to work on any pertinent tasks that are meaningful.
Tasks may include preparation for return to employment or recreation. The primary focus of therapy with the prosthesis in rehabilitation should include bilateral activities, in which the individual is required to use the prosthesis in a functional manner because the primary advantage of a prosthesis for a unilaterally independent individual is the ability to complete bilateral activities never completed before. Individuals with amputations usually do not realize the functional benefits of the prosthesis until they experience success with bilateral tasks. This can be difficult for clients, especially if they have become proficient with one-handed techniques.
As stated earlier, the client is an active participant in the rehabilitation process. The therapist designs a home program for the client. The program is continually updated as the individual progresses to greater function and independence. It is important to schedule periodic follow-up visits with the client to review progress and prosthesis function. Often therapy will be reinitiated when clients find new skills they need help in learning. The occupational therapist serves as a resource for clients, enabling them to achieve maximal function and independence during the course of their lifetime.
Psychosocial Insights from Clients with Amputations
Having an amputation can impact many psychosocial dimensions of one’s life.
Family Dynamics
The dynamics of the family may be altered when a family member looses a limb. Significant others or direct family members of the injured person experience a series of losses and adjustments. Family members may fear that the individual is suffering and at risk of dying. Fear and anxiety may become overwhelming at times. Family members may worry about how the individual will adjust to his or her changed body. Issues about intimacy and dependency are common concerns. The therapist should encourage a reconnection between the person who has sustained an amputation and his or her partner [Kohl 1984a, 1984b].
Impact on Rehabilitation
The rehabilitation team should become knowledgeable about the individual’s response to the injury. Psychosocial aspects include change in self-image and body image, acceptance of the residual limb, and feeling comfortable in society as a person with an amputation. Some clients may be medically prepared to begin rehabilitation, but they are not psychologically ready. Health providers should not label the client as uncooperative and unmotivated. Rather, they should facilitate and reinforce good communication among the client and health care team. The client should be an active partner to establish rehabilitation goals.
Counseling People Who Have Amputations
According to Price and Fisher [2002], issues addressed during counseling sessions include depression, distress, sleeplessness, anxiety, changed body image, effects on relationships and intimacy, and feelings of anger and resentment. According to Kohl [1984a, 1984b], complaints of emotional distress in the early stages of rehabilitation seemed to be most apparent from 6 to 24 months after surgery.
Upper Extremity Prosthetic Intervention for Children
Early gross motor movements in children such as prone and sitting emerge between four and six months [Cronin and Mandich 2005]. These movements directly involve the use of hands in order to balance, support, and stabilize the trunk. As a result, fitting children with a prosthesis is considered necessary in order to maintain and preserve normal development [Shaperman 2003]. Exner [1989] stated that “The development of visual perception and eye-hand coordination skills in conjunction with cognitive and social development allow the child to engage in increasingly complex activities.”
Early Fitting
According to Hanson and Mandacina [2003], “The single most important advantage of early fitting is the immediate acceptance of the prosthetic arm by the child.” The most beneficial age range to receive a prosthesis is from two months to two years [Fisher 1976, Scotland and Galway 1986, Stark 2001]. Children fitted with a prosthesis at a young age and who wear their prostheses regularly will demonstrate spontaneous use in daily activities.
Children fitted at later ages are less spontaneous and more inclined to use the prosthesis passively [Atkins 2002, Bowers 2003, Hanson and Mandacina 2003]. In addition, because hand skills develop gradually children should be fitted early so that the prosthesis becomes naturally integrated with bilateral activities. While wearing their prostheses, children must practice activities that require crossing midline, hand position in space, grasping, bilateral tasks, and bringing hands to midline [Hubbard et al. 1991].Table 18-4 suggests types of prostheses, goals, assessments, and interventions for children of different age groups.
Table 18-4
Suggestions for Age Appropriate Prostheses, Goals, Assessment, and Interventions
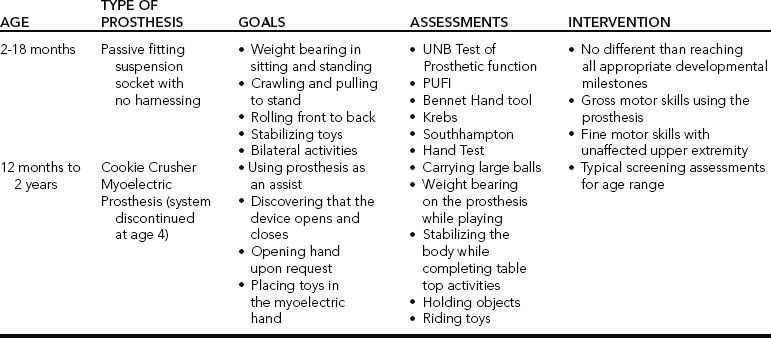
Data from Shaperman J, Landsberger SE, Setoguchi Y (2003). Early upper limb prosthesis fitting: when and what do we fit. Journal of Prosthetics and Orthotics. 15(1):11-17. Stocker D, Caldwell R, Wedderburn Z (1996). Review of infant fittings at the Institute of Biomedical Engineering: 13 years of service. ACPOC News 2:1-5.
Family Involvement
Acceptance of the prosthesis will involve the family. The family should be involved in donning and doffing the prosthesis, playing with the child while the prosthesis is on, and developing wearing schedules. The family should be educated about the importance and advantages of early and consistent prosthetic use. Futhermore, children who have myoelectric prostheses will require substantial one-to-one training and attention [Atkins 1997].
Marketing Strategies and Recommendations
To specialize in upper extremity prosthetic rehabilitation, the therapist must be motivated and persistent, as in any area of practice. There are many avenues for gathering basic information on upper extremity prosthetics, such as journals, books, agencies, other therapists, and the Internet. (See Appendix D.) Important information can be gathered from these resources to augment basic prosthetic knowledge. Next, the therapist should establish relations with a prosthetist who specializes in upper extremity prosthetics.
Much valuable information can be learned from spending a week with a prosthetist learning about the process of reimbursement, fabrication, and orientation to various options. The funding process can take much time, depending on the source of reimbursement and the insurance company’s specific benefits regarding prostheses. It is important to remain focused on the client and to serve as an advocate for the individual with the amputation. Phone calls and letters from health care professionals may expedite approval. Therapy can proceed without approval for the prosthetic device in order to accomplish goals from the pre-prosthetic phase.
In addition, it is important to locate area case managers and physicians who work with this population. Case managers and physicians will assist in establishing a referral base for those requiring therapy. It has been the experience of the author that physicians, prosthetists, and case managers are happy to know that a therapist exists who wants to work in upper extremity prosthetic rehabilitation. They are also often happy to refer their clients. The area of upper extremity prosthetics is a rewarding field.
1. How are levels of amputation differentiated?
2. What are the roles of the client, prosthetist, and occupational therapist when treating a person with an amputation?
3. What are four prosthesis options available for people with upper extremity amputations?
4. What are the advantages and disadvantages of passive, boy-powered and externally powered prostheses?
5. What psychosocial impacts may an amputation impose upon the client who has an amputation?
6. When treating a child with an amputation, what assessments and interventions can be used?
References
Alley RD (2002) Admancement of Upper Extremity Prosthetic Interface and Frame Design. Institute of Biomedical Engineering, University of New Brunswick, MEC’02, ‘The Next Generation.’
Andrews, KL, Bouvette, KA. Anatomy for fitting of prosthetics and orthotics. Physical Medicine and Rehabilitation. 1996;10(3):489–507.
Atkins, DJ. Pediatric prosthetics: A collection of considerations. In Motion. 1997;7(2):7–17.
Atkins, DJ. Early fitting is key to success. First Step Magazine. 2002;2:29–30.
Atkins, DJ, Alley, RD. Upper extremity prosthetics: An emerging specialization in a technologically advanced field. Journal of Prosthetics and Orthotics. 2003;2:1–8.
Atkins, DJ. A many-sided approach to kids with limb differences. In Motion. 2003;7(2):12–19.
Atkins, DJ, Heard, SCY, Donovan, WH. Epidemiologic overview of individuals with upper-limb loss and their reported research priorities. Journal of Prosthetics and Orthotics. 1996;8(1):2–11.
Baumgartner, R, Bota, P. Upper extremity amputation and prosthetics. Medicine Orthotic Technology. 1992;1:5–51.
Bennett, JB, Alexander, CB. Amputation levels and surgical techniques. In: Atkins DJ, Meier RH, eds. Comprehensive Management of the Upper-limb Amputee. New York: Springer-Verlag; 1989:28–38.
Billock, JN. Clinical evaluation and assessment principles in orthotics and prosthetics. Journal of Prosthetics and Orthotics. 2003;8(2):41–44.
Bowers, R. Facing congenital differences. First Step Magazine. 2003;4:23–26.
Carlson, LE, Veatch, BD, Frey, DD. Efficiency of prosthetic cable and housing. Journal of Prosthetics and Orthotics. 1995;7(3):96–99.
Centers for Disease Control and Prevention. National Health Interview Survey by the Office on Disability on Health. Atlanta, GA: National Center for Environmental Health, Centers for Disease Control and Prevention, 1996.
Collier, M, LeBlanc, M. Axilla bypass ring for shoulder harnesses for upper-limb prostheses. J Prosthet Orthot. 1996;8(2):130–131.
Crane, V. Amputee adjusts. Probe Magazine. 1979;4:10–14.
Cronin, A, Mandich, MB. Human Development and Performance Throughout the Lifespan. New York: Thomson/Delmar Learning, 2005;139–164.
Doolan, K. Use and training of cosmetic and functional arm prostheses. Inside Case Manager. 2001;7(10):12–15.
Esquinazi A, Meier R, Sears H (2002) The state of upper limb prosthetics. Presentation at Orlando, FL. National Prosthetic and Orthtotic Conference.
Exner, CE. Development of hand functions. In: Pratt PN, Allen AS, eds. Occupational Therapy for Children. Second Edition. St. Louis, MO: CV Mosby; 1989:235–259.
Fisher, A. Initial fitting of the congenital below-elbow amputee: Are we fitting early enough? Inter-Clinic Information Bulletin. 1976;15:7–10.
Frazier, SH, Kolb, LC. Psychiatric aspects of pain and the phantom limb. Orthopedic Clinics of North America. 1970;1:481–495.
Hanson, WJ, Mandacina, S. Microprocessor technology opens the door to success. The O&P Edge. 2003;5:36–38.
Hubbard, S, Bush, G, Kurtz, I, Naumann, I. Myoelectric prostheses for the limb deficient child. Physical Medicine Rehabilitation Clinical North America. 1991;2:847–866.
Jones, LE, Davidson, JH. Save the arm: a study of problems in the remaining arm of unilateral upper limb amputees. Prosthetics and Orthotics International. 1999;23:55–58.
Kohl, SJ. Emotional coping with amputation. In: Krueger DW, ed. Rehabilitation Psychology: A Comprehensive Textbook. New York: Aspen; 1984:272–281.
Kohl, SJ. The process of psychological adaptation to traumatic limb loss. In: Krueger DW, ed. Emotional Rehabilitation of Physical Trauma and Disability. Spectrum Publications; 1984:113–119.
Keenan, DD. Myoelectric prosthesis protocol. American Occupational Therapy Association Physical Disabilities Newsletter. 1995;18(1):1–4.
Lake, C. Effects of prosthetic training on upper-extremity prosthetic use. Journal of Prosthetics and Orthotics. 1997;9(1):3–9.
Law, HT. Engineering of upper limb prostheses. Orthopedic Clinics of North America. 1981;12(4):929–951.
Leonard, JA, Meier, RH. Prosthetics. In: DeLisa JA, ed. Rehabilitation Medicine Principles and Practice. Philadelphia: J B Lippincott, 1988.
Malone, JM, Fleming, LL, Roberson, J, Whitesides, TE, Leal, JM, Poole, JU, et al. Immediate, early and late postsurgical management of upper limb amputation. Journal of Rehabilitation Research Development. 1984;21:10–39.
Muilenburg, AL, LeBlanc, MA. Body-powered upper limb components. In: Atkins DJ, Meier RH, eds. Comprehensive Management of the Upper-limb Amputee. New York: Springer-Verlag, 1989.
NovaCare Orthotics and Prosthetics (1991) Client Information Packet. 1-800-522-4428.
Omer, GE. Nerve, neuroma, and pain problems related to upper limb amputations. Orthopedic Clinics of North America. 1981;12(4):751–761.
Patterson, DB, McMillan, PM, Rodriguez, RP. Acceptance rate of myoelectric prosthesis. Journal of the Association of Children’s Prosthetic-Orthotic Clinics. 1991;25(3):73–76.
Price, EM, Fisher, K. How does counseling help people with amputation. Journal of Prosthetics and Orthotics. 2002;14(2):102–106.
Radocy, B. Upper-extremity prosthetics: Considerations and designs for sports and recreation. Clinical Prosthetics and Orthotics. 1987;11(3):131–153.
Reddy, MP. Nerve entrapment syndromes in the upper extremity contralateral to amputation. Archives of Physical Rehabilitation. 1984;1(65):15–17.
Santschi, WR. Manual of Upper Extremity Prosthetics, Second Edition. Los Angeles: University of California Press, 1958.
Scotland, TD, Galway, HR. Long-term review in children with congential and acquired upper limb deficiency. Journal of Bone and Joint Surgery. 1986;65:346–349.
Shaperman, J, Landsberger, SE, Setoguchi, Y. Early upper limb prosthesis fitting: when and what do we fit. Journal of Prosthetics and Orthotics. 2003;15(1):11–17.
Shurr, DG, Cook, TM. Prosthetics and Orthotics. Norwalk, CT: Appleton & Lange, 1990.
Stark, G. Upper-extremity limb fitting. In Motion. 2001;12(4):47–52.