Physical Therapy and Rehabilitation
The Profession of Physical Therapy
The Profession of Physical Therapy for Animals
Indications for Referral to Physical Therapy
The Importance of the Physical Therapist Evaluation
Team Approach and the Role of the Veterinary Technician
Learn to Talk Like a Physical Therapist
Physical Therapy Interventions
When you have completed this chapter, you will be able to:
1 Differentiate between rehabilitation and physical therapy.
2 Describe the roles of the members of the animal rehabilitation team.
3 Describe the goals of and indications for use of physical therapy in animals.
4 List and describe the five elements of patient management in physical therapy.
5 Describe legal issues related to the practice of physical therapy.
6 List services commonly offered by physical therapists.
7 Differentiate between passive, active, and active-assistive exercise.
8 Describe the principles of hydrotherapy and explain methods to provide hydrotherapy to animal patients.
9 Define proprioception and give examples of proprioceptive activities performed with animal patients.
10 List supportive and assistive devices used with animal patients.
11 List and describe commonly used physical therapy modalities.
12 List common classifications of strokes used for myofascial manipulation.
13 Describe considerations in the design of training or conditioning programs for canine athletes.
14 Differentiate between orthotics and prosthetics.
15 Define common terms related to physical therapy and rehabilitation.
HISTORY OF PHYSICAL THERAPY
The field of human PT has an extensive international history. If you travel back in time, different forms of PT were used centuries ago. Hippocrates was an advocate of massage, and Hector used aquatic therapy in 460 BC.2 The first documented origin of PT as an established profession dates back to 1894 when the Chartered Society of Physiotherapy was formed in England.3 PT began in the United States in 1914 in Portland, Ore., by a small group of female nurses with a physical education background. At this time, graduates of Reed College and the Walter Reed Hospital were called “reconstruction aides,” a program that developed out of a need to manage the devastating injuries from World War I. Called the American Women’s Physical Therapeutic Association, the first professional association was formed in 1921 with 274 members.2 This was a landmark year because educational standards for university professional PT programs were instituted and programs became accredited by a national body. Scientific research and technology started to shape the profession.
By the end of the 1930s, membership grew to just under 1000, men were admitted, and the chapter changed its name to the American Physiotherapy Association. Ten years later, the official name changed to the American Physical Therapy Association (APTA) that opened its doors to their first office in New York City with a full-time staff.2
With the advent of World War II and a nationwide polio epidemic during the 1940s and 1950s, physical therapists were in greater demand than ever before. The Association’s membership swelled to 8000, and the number of PT education programs across the United States increased from 16 to 39. The first two association sections, school and private practice, were created to promote and develop specific objectives within the profession.2
By the 1960s, membership in the APTA grew to 15,000, and education programs offered in the country expanded to 52. Today, headquartered in Alexandria, Va., APTA represents more than 75,000 physical therapists and physical therapist assistants nationwide. The goal of this association is to continue to foster advancements in PT practice, education, and research. There are currently 180 institutions that offer PT education programs, and 236 physical therapist assistant education programs are offered in the United States.2
THE PROFESSION OF PHYSICAL THERAPY
You may be familiar with the terms “rehabilitation” and “physical therapy.” Rehabilitation is a more broad term that includes the processes of education and treatment for disabled individuals as a result of disease or injury that causes mental or physical impairments. PT is a more specialized term under the broader scope of rehabilitation. In the human realm, rehabilitation may include a variety of professionals, including a physiatrist (MD specializing in rehabilitation medicine), an occupational therapist, speech therapist, recreational therapist, and a physical therapist.
AMERICAN PHYSICAL THERAPY ASSOCIATION
According to the APTA, PT is defined as “a dynamic profession with an established theoretical and scientific base and widespread clinical applications in the restoration, maintenance, and promotion of optimal physical function.”2 The terms physiotherapy and physiotherapist are synonymous with physical therapy and physical therapist, respectively.
Physical therapists started to move beyond hospital-based practice in the 1950s. However, the majority of them continued to practice in a hospital setting through the 1960s. Today, physical therapists practice in a wide variety of settings to include outpatient orthopedic clinics, public schools, geriatric settings, skilled nursing facilities, factories and the workplace, outpatient rehabilitation and medical centers, and hospitals.
Physical therapists provide their services to patients with impairments, disabilities, functional impairments, or those with “changes in physical function and health status resulting from injury, disease, or other causes.”2 Physical therapists also interact and collaborate with a variety of different professionals; assess risk factors that may negatively impact optimal functioning; prevent and promote health, fitness and wellness; educate and provide consulting services to other businesses or health facilities; engage in research; and supervise and direct PT services to include support personnel. Today, physical therapists continue to strive for scientific-based medicine, and key elements of the past remain the same focus in our profession today to include practice, teaching, and research.
Areas of expertise are designed to promote lifelong learning and professional development. APTA’s special-interest sections were established to give members additional exposure to others who share their specific interests. Over the years, these specialties have continued to expand to a total of 18 special-interest sections, which include acute care; aquatic PT; cardiovascular and pulmonary; clinical electrophysiology and wound management; education; federal PT; geriatrics; hand rehabilitation; health, policy, and administration; home health; neurology; oncology; orthopedic; pediatrics; private practice; research; sports PT; and women’s health.2 Within each of these sections fall any number of special interest groups (SIGs) that focus on specific areas of PT practice. For example, within the neurology section of the APTA lie six SIGs: balance and falls, brain injury, degenerative diseases, spinal cord injury, stroke, and vestibular rehabilitation. Currently the animal physical therapist special interest group lies within the framework of the orthopedic section of the APTA.
THE PROFESSION OF PHYSICAL THERAPY FOR ANIMALS
In the past, there was little attention paid to postoperative care, and many animals were lost to follow-up following suture removal. This coupled with the notion that the animal would use the limb when it felt “good” and the reluctance on the part of veterinarians to urge early mobility were factors that limited the use and concept of PT. Despite recent advances, there are still veterinary surgeons that routinely immobilize their postoperative cranial cruciate repair patients for 4 to 6 weeks using casts, braces, or splints. Early motion has been shown to be efficacious in hastening recovery and limiting the effects of disuse on bone, cartilage, ligaments, and tendons.
Today’s current challenge is to prove that PT is as meritorious in the dog as it is in the human. There are many new studies done in man demonstrating the value of PT on earlier recovery, resumption of a normal lifestyle, return to athleticism, and enhanced quality of life. However, there have been a few studies on animals. Some of the first and most notable are Johnson and Johnson’s work on early use of electrostimulation4; Levine and Millis’ work on goniometry,5 and Steiss on ultrasound.6 The recent interest will only stimulate new areas of investigation and research. One of the most recent articles was published in the Journal of the American Veterinary Medical Association in 2007 entitled “Treatment of Traumatic Cervical Myelopathy With Surgery, Prolonged Positive-Pressure Ventilation and Physical Therapy in a Dog.”7
GOALS OF PHYSICAL THERAPY
The goal of PT is to return the affected area and the animal back to its prior level of function. This may be accomplished by: (1) Reducing pain and accelerating healing of injured and inflamed neurologic and musculoskeletal tissues; (2) maintaining or restoring normal range of motion in affected joints of the forelimb, hind limb, or spine; (3) preventing fibrosis or soft tissue contractures in injured, weak, or paralyzed limbs; (4) preventing disuse atrophy (i.e., preserving muscle mass) of an affected limb during the healing phase of neurologic or musculoskeletal insults; (5) gaining strength and improving function in weak or paralyzed limbs; (6) providing a positive psychologic effect maximizing both the patient’s and owner’s well-being; (7) educating and providing the owner with individualized home-care programs to maximize the animal’s functional mobility and preventing injury to the owner. Any one or a combination of these goals may be employed throughout the rehabilitation phase.
INDICATIONS FOR REFERRAL TO PHYSICAL THERAPY
Many veterinarians ask what type of patients may benefit from PT. Indications for referral to a physical therapist may be categorized by a specific pathologic condition or by a PT diagnosis (Box 24-1). Orthopedic cases may include those animals suffering from neurologic conditions or osteoarthritis, hip dysplasia, or tendinitis. Many are postoperative patients that have undergone a total hip replacement, bicipital tendon release or femoral head osteotomy, an arthrodesis or amputation, cruciate surgery (intracapsular or extracapsular procedures), or a fracture repair. General conditions may include delayed unions, geriatric support care or strengthening, and conditioning or weight loss programs. Wounds, such as degloving injuries, lick granulomas, and decubitus ulcers, are also rapidly resolved with rehabilitation. PT diagnoses focus more on a specific musculoskeletal problem. The list may include gait abnormalities or other movement dysfunction, pain and inflammation, decreased strength and endurance, joint stiffness, or loss of range of motion.
THE IMPORTANCE OF THE PHYSICAL THERAPIST EVALUATION
APTA’s Guide to Practice (2001) describes the integration of five major elements in patient management. These elements include examination, evaluation, diagnosis, prognosis, and intervention.8 Keeping these elements in mind, the ultimate goal of systematically carrying out these guidelines is to provide the best, most individualized, and effective quality of care for each patient. By conducting a comprehensive examination, the physical therapist is able to generate an accurate neuromusculoskeletal diagnosis. This allows the physical therapist to optimize the patient’s outcome and choose the most appropriate plan of care to reach those outcome goals.
Examination refers to the thorough screening of a patient and includes the history, tests, measures, and systems review.8 Evaluation is the clinical judgments made by the PT diagnosis and is directed more at neuromusculoskeletal deficiencies rather than a specific medical condition or disorder.8 For example, a veterinarian’s diagnosis may be a ruptured cranial cruciate ligament, whereas the physical therapist’s musculo- skeletal diagnosis is muscle atrophy, movement dysfunction, pain, and inflammation. A prognosis is a prediction of the level of improvement and how long it will take to reach those levels.8 Goals are established as part of the plan of care along with expected outcomes, level of predicted improvement, and interventions to be used, including duration and frequency. The interventions are the actual treatment techniques and procedures consistent with the diagnosis to improve a patient’s condition.8 A variety of physical therapy interventions will be discussed later in this chapter.
As with all evidence-based practice, it is the physical therapist’s responsibility to provide appropriate, effective, and comprehensive quality of care to our animal patients and estimated prognoses for the clients. As mentioned, the proven effects of PT demonstrated in man are inferred when transferred to the dog. Much work needs to be done to prove that PT is as meritorious and beneficial in animals, and documentation is the key.
By measuring, assessing, and reevaluating, the physical therapist is able to determine how the animal is progressing or regressing and change the treatment plan as appropriate. Is the chosen intervention nearing the outcome goals? Do changes need to be made in the plan of care? This information is also vital when improving or changing protocols and justifies treatment and benefits for the owner. Documentation allows us to objectify our efforts, teach and/or perform research, chart progress or lack thereof, provide a continuity of care, prevent medicolegal issues, and show proof of success.
LEGAL ISSUES
You will notice the terms physical therapy and physical rehabilitation have been used interchangeably throughout this chapter. Inconsistent language stems from individual state practice acts that define physical therapy differently across the nation. Each state owns the right to legally define physical therapy and regulate its practice.
For example, in the state of Colorado, the term physical therapy is not a protected term. In other words, anyone providing this type of service may deem it physical therapy. However, calling oneself a physical therapist implies that you have gone through a rigorous training program in an accredited PT school and have passed the national licensure examination. Thus the term physical therapist may only be used by those holding a PT license. However, in California, both the terms physical therapy and physical therapist may only be used by those individuals possessing a license to practice PT. As a result of the nature of individual practice acts, the term physical rehabilitation will be used throughout the remainder of this chapter.
Laws, in general, are in place to protect the consumer and the patient. With the field of animal physical rehabilitation continuing to blossom, regulations and policies will continue to expand to ensure that providers of physical rehabilitation services are competent. In Colorado, the veterinarian is the gatekeeper for animal care and in the past, the one solely responsible for conducting and directing patient care and the ultimately legally responsible party. The veterinary practice act stated that anyone could work under the direction of and on-site premises of a veterinarian. The PT practice defined PT as the examination, treatment, or instruction of human beings to detect, assess, prevent, correct, alleviate, or limit physical disability, movement dysfunction, bodily malfunction, or pain from injury, disease, and other bodily conditions. As of July 1, 2007, the PT Practice Act, through 3 years of legislative lobbying efforts, was changed to read “clients and patient” in place of “human beings.” With this change, comes the capability of a more comprehensive collaborative approach to patient care. With a veterinary medical clearance, instead of a referral, a physical therapist is now able to treat animal patients without direct supervision, in any environment desired, including home care. In addition, physical therapists are now responsible for half of the legal liability for treating offsite should a malpractice suit arise.
Under Colorado law, the veterinary technician must be under direct, on-site supervision of a veterinarian when performing tasks related to animal care. As a licensed or certified veterinary technician, you may not examine, evaluate, or develop a plan of care for an animal. In addition, most states require direct supervision of a technician by a veterinarian. Thus it is imperative that you are familiar with and abide by your state’s physical therapy and veterinary medical practice acts before performing any type of physical rehabilitation.
TEAM APPROACH AND THE ROLE OF THE VETERINARY TECHNICIAN
A number of differently trained professionals may be involved in animal rehabilitation. They include veterinarians, physical therapists, veterinary technicians, and physical therapist assistants (PTAs). Ideally, animal rehabilitation is a collaborative effort between the veterinarian and the physical therapist, with additional assistance from the veterinary technician and the PTA. The degree of supervision and amount of autonomy for the veterinary technician and PTA will vary by state for each of these professionals according to state laws and regulations related to their individual practice.
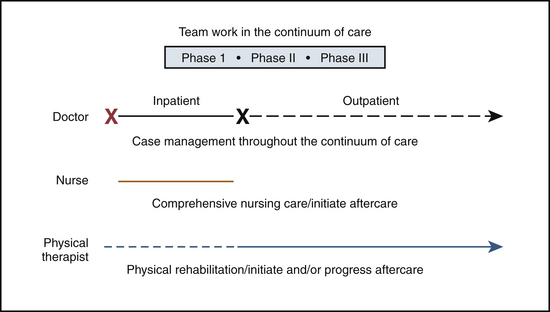
In the continuum of care (Figure 24-1), the veterinarian clears the animal of any zoonotic or concomitant disease and recommends PT. The veterinarian provides medical management and has the knowledge and expertise regarding the pathophysiology of the injury or problem. The role of the physical therapist is direct patient care. The physical therapist is responsible for performing the PT evaluation, predicting outcome goals, and delivers and progresses the rehabilitation according to an individualized care map, or protocol. The physical therapist interprets the results of the examination and uses the results as a guide to establish a PT diagnosis, or problem list (Box 24-2) and the patient’s prognosis. This would also include developing realistic goals and a plan of care for that individual patient. Many aspects within the PT plan of care are delegated to the veterinary technician and PTA who serve to assist the physical therapist in the provision of PT. The degree of direction and supervision will depend upon the individual’s education, experience, and responsibilities of the involved parties. Veterinary technicians and PTAs with additional education are competent to perform many delegated aspects of patient care, to include assessment, reassessment, and intervention techniques. With this combined effort, effective rehabilitation can get an animal “back on all fours” in no time.
LEARN TO TALK LIKE A PHYSICAL THERAPIST
As in any new professional endeaver, there arise differences in terminology. To help acquaint you with the PT profession, Box 24-3 lists many of the key terms used by physical therapists.
PHYSICAL THERAPY INTERVENTIONS
PT interventions include a variety of components. From admittance through discharge, the physical therapist is responsible for coordinating, communicating, and documenting the patient’s physical rehabilitation needs to ensure appropriate, comprehensive, and effective quality care. Other interventions may involve client-related education, instruction, and procedural interventions. Procedural interventions may include therapeutic exercise, manual therapy techniques, supportive or assistive devices, airway clearance techniques, integumentary repair and protection techniques, physical agents, and electrotherapeutic and mechanical modalities. See Box 24-4 for a more comprehensive list of services offered by physical therapists.
Education and home-care programs are necessary to provide the owner with a way to become involved in their animal’s rehabilitation phase. The program is individualized to each animal’s needs and is progressed accordingly. Topics may include information on surgical procedures or pathologic conditions, specific therapeutic exercises, clients’ education and/or recommendations on how to care for the animal without injury to the owner or further injury to the animal.
Therapeutic exercise, limited only by one’s imagination, plays a large role in rehabilitation and is the most cost efficient. Exercises may be structured according to the outcome desired, such as improving balance, coordination, endurance, strength, or flexibility. Exercise may be separated into passive, active-assistive, and active. Passive exercise mimics the normal muscle pumping action to improve blood flow and sensory awareness in affected limbs. It requires movement from an external force (e.g., gravity, a machine, or a person). There is no voluntary muscle contraction on the animal’s part. Passive exercise may be used when an animal is unable or not supposed to actively stress a body segment, in the presence of inflammation, or when active range of motion is painful. It helps to maintain soft tissue and joint integrity, enhance synovial movement for cartilage nutrition and diffusion of joint materials, and minimizes the potential for contracture formation. When performing passive range of motion exercises, the joint in question must be supported from above and below (Figure 24-2).
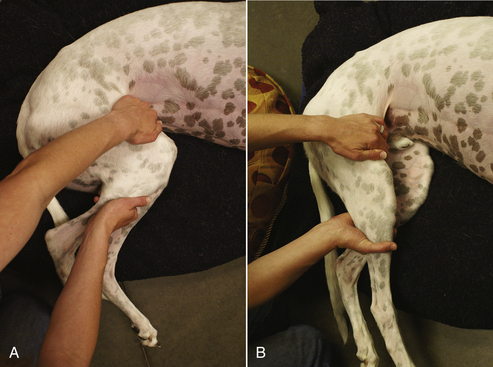
FIGURE 24-2 A, Passive range of motion exercise in flexion. B, Passive range of motion exercise in extension.
Follow the joint through a comfortable range of motion by slowly and gently flexing and extending. Ten to 15 repetitions are typically sufficient for one treatment session and repeated three to four times per day. Passive range of motion is not a stretch, and range of motion should never be forced.
Active-assistive exercise requires an outside force to assist with the range of motion (Figure 24-3). Whether mechanical or manual, the outside force must assist the animal in achieving range of motion against gravity. Because of weakness or disease, the prime mover muscles require some degree of assistance to complete a full range of motion. This type of exercise is usually prescribed for gentle stretching or for a weak body part.
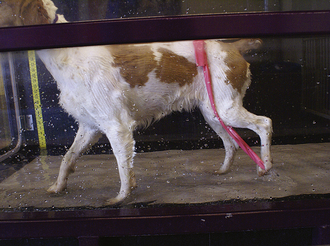
FIGURE 24-3 Use of Thera-Band to assist dorsiflexion and avoid knuckling of the right hind limb throughout the entire gait cycle.
Active exercises produce movement by active muscle contractions (Figure 24-4). The patient is able to move its body part independently against gravity throughout a range of motion. Active exercise serves to increase muscle strength, cardiovascular function, and coordination. It maintains physiologic elasticity and contractility of involved muscles, provides sensory feedback from contracting muscles, and provides a stimulus for bone and joint integrity.

FIGURE 24-4 One example of active exercise using Cavaletti rails. Note the increased balance, coordination, strength, and flexibility this animal is demonstrating during this exercise.
Hydrotherapy, via lakes or streams, an underwater treadmill (UT), pool, or whirlpool, is capable of reducing gravity, thus decreasing concussive forces on joints to allow earlier intervention and faster recovery times. Water provides resistance throughout the entire range of motion providing a closed chain exercise. The warm water assists in pain reduction and acceleration of the healing process. Older animals are capable of exercise effectively without undue stress. Water height is adjustable for the amount of desired weight bearing and capable of adjusting for different sized dogs.
Hydrotherapy uses five inherent properties of water (thermal, buoyancy, hydrostatic pressure, cohesion, and turbulence) to help strengthen, improve lung capacity, and increase blood flow. Thermal properties are provided by heated units, most notably an indoor pool and UT. Temperature ranges from the low 80° F to the low 90° F. Thermal properties allow for superficial heating of the involved limbs, increasing circulation to help decrease pain, relax skeletal muscle, and increase flexibility. Buoyancy is the upward thrust of water that is created when a patient is submersed, producing a decrease in body weight. Buoyancy will counteract weight allowing for modified ambulation when weight bearing is contraindicated or limited. In addition, for neurologic patients, buoyancy helps the body regain a vertical position if a patient is tipped from the midline. While the animal is submersed, pressure is exerted by stationary fluid on the body. This phenomenon is called hydrostatic pressure. The amount of pressure will increase with depth, allowing increased circulation in the extremities and a reduction in edema. The cohesion property is explained by water molecules adhering to one another. The greater the cohesive forces, the greater the viscosity, in this case, water. A force is required to separate the molecules. This adds resistance to the limbs while the animal is moving through water. Finally, many of the hydrotherapy devices are equipped with jet systems. These jets provide a certain velocity of water at a given point that varies in magnitude and direction. When moving a body through water, turbulence is created causing a greater resistance during movement. The amount of turbulence may be increased by adding the jet system to the treatment session. Turbulence also offers a superficial massage to the area targeted by the jet system.
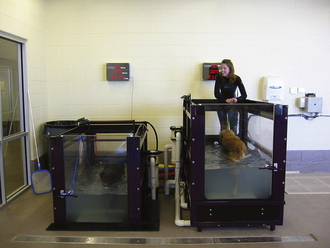
The most common forms of hydrotherapy in animal physical rehabilitation are UTs and pools. In the UT (Figure 24-5), dogs may walk comfortably on the treadmill without the “panic” of not being able to touch the bottom, as in a pool. Small dogs can even swim with adequate turning radius in an UT. UTs provide a more controlled, less erratic environment for more specific rehabilitation. However, should a dog exhibit an abnormal gait pattern, that pattern may be exacerbated and worsened by continued exercise in the UT if not addressed.
Most UTs have clear doors and windows for excellent viewing of an animal’s gait pattern. A digital display shows speed, distance, and time, allowing for appropriate documentation during rehabilitation. These treadmills are typically large enough for one to two therapists and the canine patient in the water at the same time. This becomes important in the case of the neurologic patient that is unable to walk independently.
A pool (Figure 24-6) allows for a more erratic, less controlled environment, unless the activity is better controlled by a rehabilitation therapist entering the pool with the animal. Waders, wet suits, or even scrubs may be worn in a pool while providing assistance to the animal. Potential for increased injury to the animal exists if the patient is allowed to run around the side of or jump into the pool. The pool tends to be used later in the rehabilitation plan of care, as the animal is capable of higher levels of active exercise.
Proprioceptive rehabilitation is a concept commonly overlooked in a patient. Proprioception refers to the conscious awareness of limb motion and position in space. Joint capsules, ligaments, synovium, and fat pads all contain a variety of highly specialized receptors that respond to varying types and degrees of sensory stimuli. Proprioceptive activities include exercises that facilitate rapid muscle contractions, focusing on closed kinetic chain exercises, and improve dynamic stability. Such examples may include a balance board, Theraball, figure eights, ambulating across couch cushions or different surfaces (Figures 24-7 and 24-8).
Manipulations and mobilizations may also be applied to decrease pain, restore pain-free functional range of motion, or increase flexibility in hypomobile joints. A manipulation is a passive motion of any kind as a form of treatment for musculoskeletal disorders. A manipulation pertains to all forms of passive movement, including mobilization. Manipulations are applied in a gentle fashion, with small changes in range of motion and are rarely forceful. A mobilization is also a passive movement, typically an oscillatory movement that produces a sustained stretch on a particular joint.
A physiologic movement is a motion that a patient actively performs himself (flexion, extension, abduction, adduction). However, to have full physiologic range of motion, a joint must possess full accessory movements. Accessory motions are the movements of a joint that contain spins, rolls, and glides. Each type of joint possesses different combinations of accessory movement. Restrictions of accessory joint motion may limit normal physiologic movement and cause pain.
It is because of the complex nature of joints and the specific knowledge gained through extensive training in manual therapy that the application of manual techniques is limited to only licensed physical therapists. If done improperly, damage, in some cases severe, to the joint may be produced.
Supportive and assistive devices can play an important role in the overall well-being of the animal patient with neurologic or orthopedic impairments. In addition to providing increased independence for the pet, these devices can provide additional autonomy for the owner. They provide support to a weak or nonfunctioning body part and may assist with rehabilitation. They can also help to prevent decubitus ulcers from forming, increase an animal’s mobility, and prevent future complications in recumbent patients. Supportive devices may range from a single orthotic to protect an animal from knuckling to proper fitting for animals in need of a hind limb cart. These devices are available in a variety of forms: boots, slings, and two-wheeled and four-wheeled carts.
Boots
Boots are an ideal way to protect the feet when conscious proprioceptive deficits are present. Boots will act as a socklike covering that is securely fashioned by a Velcro strap to protect the dorsum of the paw from scraping and abrasions. Most have a rubber sole to prevent slipping and are machine washable. These boots may also be used for working dogs to protect the feet from glass and other sharp debris, or on active dogs on long hikes, protecting them from jagged rocks and the elements.
It is important to remember to remove the boots periodically to preserve skin condition and it is advisable to remove boots before rehabilitation treatment. When performing therapeutic exercise, remove the boots to increase weight bearing and proprioception through the bottom of the pads. If not removed, these boots will decrease the amount of sensory input through the bottom of the paw in neurologically impaired patients. If not fitted properly, these boots can interrupt circulation, become cumbersome, and impede gait patterns or strides, potentially causing increased injury if the animal stumbles and falls. It is imperative that the proper size is ordered and appropriate instructions for skin care and rehabilitative exercises are communicated to the owner.
When choosing the proper boot, make sure that they are machine washable, waterproof, or water resistant. Be sure that they are manufactured out of durable material to prevent quick wear and tear and that they have a secure tread on the bottom to prevent slipping. Old socks may be considered for indoor use. However, exercise caution when securing the top with tape to prevent interrupting circulation.
Slings
Slings come in a variety of shapes, sizes, and manufacturers. Some may be wrapped around the belly or fitted around the forelimbs or hind limbs. They are equipped with long hand-held straps to prevent personal injury for the handler when supporting their pet. These devices aid the handler in transitioning a recumbent animal and assist with ambulation to prevent falls on slippery floors, especially after surgery to prevent further injury to the animal. Support slings are also available for forelimb assistance and patients with amputations or to reduce the weight on the front quarters after forelimb surgeries or injuries.
It is important to customize the size of the harness for the utmost safety and comfort of your patient. A wide variety of sizes are available, and they come conveniently designed for both male and female patients. With forelimb slings, the neckline should not obstruct respiration, and urine flow should not be compromised in the hind limb slings. A fleece or soft lining is recommended against the animal’s skin to prevent skin breakdown. Be cautious that the sling is not too narrow in diameter, especially around the groin and belly region, to prevent occlusion of vital arteries and nerves in addition to rubbing and skin irritation. Should these devices become soiled, most can be machine washed.
Carts
At times, total body support is necessary and may be achieved through two- and four-wheeled carts, or canine wheelchairs (Figure 24-9). These carts provide additional support of either hind limbs or all four limbs, independence for both owner and animal, and prevention of the deleterious effects of a continual recumbent position in downed dogs. The frames are lightweight, and some harnesses are designed to distribute weight throughout the entire mass of the dog, rather than concentrated in one area of the body (such as over the scapulae). The pneumatic wheels make it easy for a dog to traverse a variety of terrains, such as small curbs, rocks, roots, and grass.
Carts are not intended to be used in place of a physical rehabilitation program. If fitted too early in the rehabilitation phase, the animal and owner may become too dependent on the cart’s support and replace the rehabilitation program completely. The client must be encouraged to continue a home-care program to maximize neurologic return and maintain active movement as long as possible.
The transition into a cart should be a positive experience for the animal. Familiarize yourself with the cart and its parts before placing an animal in the device to prevent unnecessary stress on the animal. Animals should be supervised at all times when in a cart to avoid concern that they may fall out of the cart, tumble down a flight of stairs, or tip over or become stuck on a household or lawn object. Food bowls may need to be elevated; however, animals should have no problem eating in these carts. Frequent rest periods out of the cart are necessary, especially for larger dogs, because it is difficult for the animal to lie down and rest comfortably while placed in the cart.
MODALITIES
The term modality identifies a wide group of agents that may include thermal, acoustic, radiant, mechanical, or electrical energy. The goal of these modalities is to produce physiologic changes in tissues for therapeutic purposes. Modalities may include cryotherapy or heat therapy that act to decrease pain and inflammation, relax skeletal muscles, reduce muscle spasm, and decrease joint stiffness. Ultrasound may be used as a deep-heating agent that converts electrical energy into high-frequency sound waves. It is beneficial for problems such as muscle spasm and contractures and effective in accelerating wound healing, causing vasodilation and reducing pain. Electrical stimulation promotes muscle reeducation, slows muscle atrophy, and reduces pain and edema. Low-intensity laser therapy, in the form of infrared energy, acts to locally stimulate the production and release of nitric oxide concentrations. Nitric oxide has been shown to accelerate wound healing, decrease pain, retard scar tissue formation, and increase bone density. When documenting the use of a modality, the agent and the parameters used (intensity, duration, and frequency) must be included in the animal’s medical record. In addition, treatment time, location of the body where the treatment was applied, and any other special notes or instructions must be documented. These may include whether the animal’s fur is shaven or unshaven, any skin abnormalities, or any unusual reactions from prior treatments.
Cryotherapy may be applied in a number of ways. Cold packs, ice massage, cold baths, and cold compression units are common cryotherapeutic modalities used to treat pain and inflammation. Cold transferred to the patient’s skin, muscle, and tissue has several beneficial therapeutic effects. Vasoconstriction of the blood vessels in this localized area causes a decrease in the inflammation, thus reducing pain and swelling by anesthetizing the area, slowing nerve conduction velocities, and reducing the amount of painful chemical mediators. Cold also decreases hemorrhage (via vasoconstriction) and edema as a result of decreased histamine release. Muscle spasm caused or exacerbated by pain, ischemia, or muscle tension is also reduced by interrupting the pain cycle, and in neurologic patients, spasticity may be reduced. Cold application may be indicated in musculoskeletal trauma and in postsurgical cases.
Contraindications to the application of cold include frostbite, compromised circulation, improper thermoregulatory responses (in the very young and very old patient), and hypersensitivity to cold. Caution must be exercised when performing rapid exercises immediately after cold application because of the reduced speed of muscle contractions as a result of slower nerve conduction velocity.
Heat Therapy
Physical therapists may wrap a hot pack in several layers of towels and place them on the area in need of treatment. Hydrotherapy and ultrasound may also be used as a heating modality. The heat provided by these thermal agents causes vasodilation, or an increase in local circulation and metabolism. This causes an increase in permeability of capillaries and the lymphatic system to help reduce tissue swelling. Heat helps relax tight skeletal muscles, decreases pain, reduces muscle spasm, and decreases joint stiffness by increasing tissue extensibility.
Caution should be exercised over dermatologic conditions or infection, which may be exacerbated by moist heat. Vascular insufficiency, lack of sensation, application over bony prominences, and dogs on long-term steroids (thinner skin, fragile capillaries) are also considerations to keep in mind when applying heat. Avoid laying the animal directly over a hot pack because this will increase the amount of pressure, thus increasing the amount of heat applied to one area and the potential for burns.
Ultrasound
Ultrasound is the use of high-frequency sound waves that are produced by vibration of a membrane (e.g., vocal cords). When a synthetic crystal vibrates at a certain frequency (as a result of its specific shape and geometry), the crystal contracts and expands when exposed to an alternating current. Ultrasound, at a frequency of 1 MHz, may penetrate tissues from a depth of 2 to 5 cm. At a frequency of 3 MHz, tissue penetration is 0.5 to 2 cm.
Ultrasound may be applied for thermal or nonthermal purposes (Figure 24-10). Thermal indications for ultrasound include an increase in metabolic rate, enzyme activity, circulation, and tissue extensibility and a decrease in pain. The biologic effects of ultrasound involve increasing joint range of motion (improve flexibility), tissue healing, collagen extensibility, decrease muscle spasm, joint adhesions, tendon repair, and retardation of scar tissue formation. Using the nonthermal parameters of ultrasound helps to reduce muscle spasm and pain, accelerate healing, aid in tissue regeneration and repair of soft tissue, and reduce swelling.
Ultrasound should never be applied over pacemakers, eyes, malignancy, infected wounds, areas of decreased circulation and sensation, thrombi, a pregnant uterus, carotid sinus, or exposed spinal cord (hemilaminectomy or laminectomy). Care should be taken when applying ultrasound over bony prominences, implants (including plastic), major nerves and arteries, and over epiphyseal plates in young animals.
When ultrasound is applied, parameters will be chosen by the physical therapist. The technician must ensure that the area to be treated is shaven, especially when applying thermal parameters. Protein in the hair coat may absorb the heat emitted from the ultrasound head and potentially produce burns. Be sure the skin is cleaned with alcohol. Use a water-soluble gel with the application of the sound head. Never apply ultrasound without a conducting medium. Immersing the sound head in water is an effective treatment method for uneven skin surfaces. Be sure to hold the transducer head ∼0.5 cm away from the area to be treated. The treatment area should be no larger than twice the size of the transducer head.
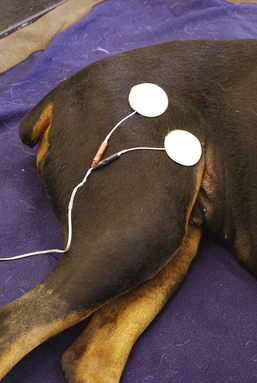
Electrical stimulation
Electrical stimulation (ES) is the application of an electrical current to stimulate nerves, muscles, and soft tissue (Figure 24-11). ES comes in many forms: neuromuscular ES (NMES), functional ES (FES), and transcutaneous electrical nerve stimulation (TENS) are some of the more common types. Electrical stimulation is used to enhance muscle performance, retard muscle atrophy, increase strength and range of motion, accelerate wound healing, reduce pain and edema, and enhance transdermal administration of medications (called iontophoresis).
There are numerous electrotherapy devices sold on the market, making use and selection of these devices quite confusing. The physical therapist must have a clear understanding of the desired outcome from the ES device and an accurate and in-depth knowledge of the appropriate parameters to choose in regards to treatment intensity, frequency, voltage, and current type.
When applying ES interventions, the physical therapist will choose the appropriate parameters. In preparation, fur or hair may need to be clipped to lower impedence. If the fur is short enough, simply wetting it down may be enough to achieve an adequate current. Skin should be cleaned to remove excess dirt and debris. ES requires constant supervision of the animal to prevent electrode migration. Parameters used with electrical stimulation intervention are defined below.
Frequency—pulses per second (PPS), Hertz (Hz) or pulse rate
Waveform—different current types (AC, DC, medium frequency, etc.); usually asymmetrical or biphasic
Pulse or phase duration—measured in microseconds; duration of a phase or pulse
Amplitude—intensity of the machine output
On-off time (duty cycle)—amount of time the stimulator is delivering a current versus rest time, usually measured in seconds
Ramp—(rise/decay time) allows current amplitude to build slowly (2 to 4 seconds)
Treatment time—15 minutes is an average treatment time, cycling through the duty cycle
Electrical stimulation should never be used over a neoplasm or infection site, skin lesion, carotid sinus, pacemaker, peripheral vascular disease, areas of analgesia, or an abdomen during pregnancy.
Low-Level Laser
The term, Equi-Light therapy, is synonymous with Anodyne. Equi-Light is used when referring to the application of a low-level laser on animals and Anodyne when applying this modality on human patients. Equi-Light is a low-intensity laser, or monochromatic infrared energy (MIRE) source, emitting a wavelength of 890 nm. At 890 nm, Equi-Light is capable of stimulating the local release of nitric oxide from hemoglobin. Nitric oxide has been shown to be beneficial in many capacities, notably one of the most natural vasodilators. It allows an increase in circulation to facilitate wound and soft tissue healing, increases lymphatic flow, decreases pain by stimulation of endorphin and enkephalin production, and retards and breaks down scar tissue.
This modality has shown promising results for human patients in treating decubitus ulcers, sprains, tendinitis, fasciitis, deep tissue bruising, rotator cuff injuries, fractures, and arthritic pain. It has been studied on horses for the treatment of wounds, pressure sores, and laminitis. Many promising results in dogs are proven to include the treatment of decubitus ulcers, lick granulomas, and delayed unions with other applications, such as generation of cartilage in osteoarthritic dogs, still being investigated in ongoing clinical trials.
Contraindications to Equi-Light therapy include its use over any active malignancy, over or near a pregnant uterus, or directly over a topical heating agent, such as BenGay (McNeil-PPC, Morris Plains, N.J.) or Icy Hot (Chattem, Inc., Chattanooga, Tenn.). Equi-Light may be used over metal implants, pins or screws, pacemakers, and defibrillators because of the absence of electrical current or deep heat with this device.
There are many devices on the market that employ a variety of wavelengths of photo energy. The term photo or light therapy must not be mistaken for monochromatic infrared energy. Photo or light therapy, is visible energy. Therapeutic monochromatic infrared energy sources are found just outside of the visible wavelengths on the light spectrum. At this specific wavelength (890 nm) of infrared light, photo dissociation of nitric oxide from hemoglobin has been proven. Currently, there is no evidence that other phototherapeutic devices affect serum nitric oxide levels in this manner.
Initially, Equi-Light was given FDA clearance for human use in 1994 to enhance circulation and reduce pain. The Equi-Light consists of a two- or four-pad flexible diode treatment pad configuration (Figure 24-12). Treatment times vary from 20 to 45 minutes, with constant monitoring of the animal treated to prevent pad migration.
MASSAGE
Touch is one of the most powerful forms of nonverbal communication. Myofascial manipulation, or massage, increases blood flow and lymphatic drainage to injured tissues. Specific techniques may be applied to stretch tendons and ligaments to decrease the potential for fibrosis and contractures.
Technique
When considering applying massage techniques, be sure to place the animal in a quiet room with minimal to no distractions. Place the animal on a soft blanket or pad and observe the temperament. Begin with gentle palpation of the dog’s body. Do you feel muscle tightness (hypertonicity), increased or decreased tissue temperature, abnormal texture (warts, lumps, lipomas) or tenderness?
Begin with gentle, slow rhythmic strokes, preferably along the length of the muscles and following the direction of fur. Your speed of stroke will depend on the purpose or goal of the massage. Generally a massage will last 20 to 45 minutes, depending on the animal’s tolerance.
During massage techniques, watch the animal for signs of discomfort, overstimulation, or pain. Should the dog attempt to move away, gently bring it back and begin again with less manual pressure. If a dog flinches during a technique, again reduce pressure and change the stroke.
Classification of Massage Strokes
Each class listed below contains several types of strokes, all requiring additional training, and each can be performed in either a soothing or a stimulating manner, depending upon the pressure and the rhythm applied. Many classifications occur with the most common listed below.
Effleurage is the most common stroke. It soothes and relaxes the nervous system, increases circulation, prepares the tissues for deeper work, and eliminates waste material from the tissues. Effleurage is a gliding movement that uses the palm of the entire hand following the contour of the body. Each hand is well molded, and at least one hand is in full contact with the body at all times.
Pétrissage is the foundation of a massage. The purpose of pétrissage is to also drain the tissues of waste material and increase circulation to the region massaged. Pétrissage contains a variety of strokes, such as shaking, vibration, muscle squeezing, skin rolling, chucking, kneading, and V-spread. Many of these techniques lift the muscles away from the underlying tissues and bone.
Shaking—skin is lifted and “shaken” over the underlying structures either using fingertips (small areas) or with the flat palm of the hand (large areas). The skin will move with your hands over the body parts.
Vibration is a quivering movement applied with fingertips or a flat hand. “Point vibration” uses only the thumb or fingertips for small, specific areas, and “flat-hand vibration” is used for larger areas.
Muscle squeezing uses one or two hands, palms only, to grasp and squeeze muscle; reduces muscle tension. Slow rhythm—to calm the nervous system; brisk rhythm—stimulates circulation and nervous system. Effective for the neck, legs, and tail.
Skin rolling uses both hands to grasp and lift superficial tissue with thumbs and fingers and rolls the tissues.
Chucking supports the foot with one hand while grasping tissue of the lower leg moving up and down along the length of the bone.
Kneading uses the surface of the middle three fingertips, providing overlapping movements, compressing against underlying bone structures, and pushing outward while maintaining contact at all times.
V-spread—place the thumbs together on the dog’s body; move them up and out (away from each other) to form a “V.”
Friction breaks down adhesions in muscles, tendons, ligaments, and fascia through circular or linear motion. This massage technique is often a heat-producing stroke. Use the tips of the thumb or middle three fingers for small areas or the heels of one or both hands for larger areas. Friction uses small, deep movements applied across the length or perpendicular to the muscle or fibrous tissue treated. This technique uses a fair amount of pressure that may be increased to tolerance.
Tapotement, or percussion, stimulates and energizes the body by increasing blood flow and lymph circulation and warms up muscle groups. Tapotement also assists with the toning of atrophied muscles. This technique applies a series of brisk blows, or repetitive striking movement in a rapid, alternating fashion. Hands are cupped, or the edges of hands are used for larger muscle groups and to penetrate into deeper tissues.
Certain behaviors elicited by the animal may indicate inappropriate massage techniques. All of the following behaviors may indicate that the masseuse needs to change his or her technique or apply less pressure: the animal’s eyes are wide open; pupils are dilated; taking rapid, shallow breaths; pulling away from pressure; turning quickly to look at the masseuse; placing its muzzle over your hands or possibly licking the masseuse’s hands; and attempting to rise and walk away.
MAXIMIZING PERFORMANCE OF THE CANINE ATHLETE
What is “performance?” What does “training” entail? There is much discussion surrounding these topics, and the “perfect” training program for our canine athletes remains a mystery. Of course, there are many components that may affect performance. In addition to proper training and conditioning, nutrition, the type of sporting event, and overall health of the animal must be considered. Before designing an optimal training or conditioning program for your four-legged athlete, a basic knowledge of tissue physiology is necessary. The focus of this section will include the necessary components to achieve maximal performance of your canine athlete. In addition, a better understanding of the optimal performance of involved tissues, including tendons, ligaments, muscles, bones, and cartilage, will be gained.
To maximize the function of each of these tissues, the “SAID” principle, “specific adaptation to imposed demands” is best applied.9 Simply stated, exercises designed for a specific training program should mimic the anticipated function. For example, if the specific activity requires more muscular endurance than it does strength, then the training program should be geared to improve muscular endurance. Building an exercise program should include the necessary foundation—a framework of specificity.
It is this principle that applies to all body systems and is an extension of the theory that body systems will adapt over time to the stresses placed upon them, or Wolff’s law.10
Improving cardiovascular endurance may be achieved by engaging in large muscle group activities, such as running, jogging, or swimming, at varying frequencies, durations, and intensities. Resistance training to enhance muscle strength, endurance and to maintain flexibility is equally as important.
Stretching is also a vital component to any training program. It improves joint range of motion and function, enhances muscle performance, and helps prevent musculoskeletal injuries. Pollock et al states that poor flexibility may lead to declining performance and subsequent injury. However, performance may be modified through flexibility training.11
The “warm-up” and “cool-down” phase of an exercise program is also a necessary component to achieving maximal performance. The purpose of a warm-up is to allow the body to make the physiologic adjustments necessary before the onset of activity. This allows the body to meet its physical requirements before physical activity. Following exercise, the cool-down period is necessary to prevent pooling of blood in the extremities and to enhance the recovery period by removing metabolic waste and replacing energy stores.
A basic understanding of the principles of exercise and a basic understanding of achieving maximal performance of important body tissues is a vital component when considering the development of an exercise plan. With these concepts, one is well on his or her way to developing an optimal training program for a canine athlete.
ORTHOTICS AND PROSTHETICS
Orthotic and prosthetic intervention has been a standard application in human PT to achieve mechanical and rehabilitative goals. An orthotic is defined as a device used to support an injured limb (see Figure 24-12). A prosthetic device is designed to replace a missing limb (Figure 24-13). Until recently the use of these assistive devices has been limited to the human realm of rehabilitation.

FIGURE 24-13 This Akita is donning a hind limb brace as an alternative to surgery to support an Achilles tendon rupture.
The goal of an orthosis includes: resting an injured limb, immobilizing or protecting a joint, controlling a limb, and/or to assist, prevent, or correct movement of an affected limb. If the physical therapist’s goal is to rest a part of the body, the orthosis must be able to substitute for or assist with the action of the injured or weak muscles. On the other hand, an orthosis may be used to immobilize a limb to reduce pain or provide joint protection immediately following surgery or injury. In these types of cases, the orthosis must take over the role of intrinsic stability normally achieved by the bony, ligamentous, or muscular components of the animal.
Before consideration of a prosthetic device, rehabilitation goals must be met in a patient that has undergone a limb amputation (Figure 24-14). It is imperative for positive functional outcomes that the spared muscle groups are identified and the respective functions understood. Each of the remaining joints in the involved extremity must maintain full range of motion. Improvement of cardiovascular endurance and a decrease in pain and inflammation can be met using appropriate modalities. Finally, adhesion and scar management must be addressed to maintain mobility of the surrounding soft tissues. Once these goals have been met, the appropriateness of a prosthetic device may be evaluated. Treatment of the entire animal is necessary, especially evaluation of the uninvolved limb(s) because the concern for fatigue and overloading may often be present.

FIGURE 24-14 A, Rubi is a 6-year-old Chihuahua that suffered a left forelimb amputation caused by complications from a blood clot. B, Rubi donning her custom prosthetic. A gel liner lessens shear forces on her skin and provides a cushion to prevent constant irritation of her residual limb.
Many other considerations are also important for achieving a successful outcome when considering an orthosis or prosthesis. Proper healing at the site of the amputation and sensitivity of the distal stump must be known. The orthotic should not impact daily activities of the patient. The patient should be able to freely perform normal daily functional tasks, such as transitioning from sitting to standing, especially in patients with concomitant neurologic or musculoskeletal deficits.
PROTECT YOURSELF
In the animal world, when discussing safety and protection, most people think of avoiding dog bites and how to safely handle and restrain animals. In addition, you must consider that the field of animal rehabilitation is extremely physically demanding. You will find yourself lifting large neurologically impaired patients and crawling around on the floor more often than sitting in a chair. Besides slips and falls, back injuries are one of the most common injuries in the workplace. More than 50% of injuries are due to improper lifting. Six hundred thousand back injuries per year are reported at a cost of $60 billion annually.
Most back injuries are due to microtrauma of the nucleus pulposus and annulus fibrosis that occur gradually with a slow onset. It is difficult to trace any one single cause or injury. Macrotrauma typically occurs from improper lifting techniques in addition to the gradual damage from microtrauma and weakening of the muscles, ligaments, and disks surrounding the vertebrae.
Contributing factors to back injury may include reaching, bending, or twisting while lifting, pushing, or pulling heavy objects. Poor posture in standing or sitting in addition to weak abdominal musculature, poor physical condition, and strength also play a role in the gradual breakdown of the back structures. In addition, staying in one position for too long, incorrect lifting techniques, poor footing while lifting, fatigue, and repetitive lifting in awkward positions play a role in the potential for back injury. Dogs pulling on a leash, restraining animals on the floor, sudden jerks or movements by an animal to get away from pain or from fear, and bending over to pet, hold, or lift a patient are a few clinical examples of potential contributing factors to back injury.
When lifting properly, you should maintain a wide base of support on a dry surface. Bend your knees and keep your back straight while centering your body over your feet as much as possible. Tighten your abdominal muscles to support the spine and pull the patient or object as close to your body as possible. If you have to change direction, move your feet instead of twisting your spine. If you are unable to move your feet, put one foot in front of the other in the direction you want to move.
Correct sitting techniques include pulling the chair forward to allow your back to be supported against the back of the chair. Your chair should have an adequate lumbar (lordotic) support, and your feet should touch flat on the floor. Your hips should be equal to or higher than your knee level, and your computer should be in front of you at eye level.
SUMMARY
The field of PT is a well-established profession that encompasses a wide variety of applications. This chapter provides a small portion of the skill and techniques available to physical therapists. Physical therapists train for many years to establish these basics, with continued education throughout the remainder of their career. The veterinary technician may become a skilled assistant in physical rehabilitation, working side by side with physical therapists. As this newly defined career continues to expand, specialty certificates recognized by national organizations may develop along with numerous employment opportunities within the veterinary community. With the collaborative efforts of all professionals involved, animal patients will continue to benefit from this rapidly growing field, and physical rehabilitation therapy will become a standard of care in veterinary medicine.
REFERENCES
2. American Physical Therapy Association, Alexandria, Va, www.apta.org.
3. Chartered Society for Physiotherapy, London, www.csp.org.uk.
4. Johnson, J.M., Johnson, A.L. Rehabilitation of dogs with surgically treated cranial cruciate ligament-deficient stifles by use of electrical stimulation of muscles. Am J Vet Res. 1997;58(12):1473–1478.
5. Jaegger, G., Marcellin-Little, D.J., Levine, D. Reliability of goniometry in Labrador Retrievers. Am J Vet Res. 2002;63(7):979–986.
6. Steiss, J.E., Adams, C.C. Effect of coat on rate of temperature increase in muscle during ultrasound treatment of dogs. Am J Vet Res. 1999;60(1):76–80.
7. Smarick, S.D., Rylander, H., Burkitt, J.M., et al. Treatment of traumatic cervical myelopathy with surgery, prolonged positive-pressure ventilation, and physical therapy in a dog. J Am Vet Med Assoc. 2007;230(3):370–374.
8. American Physical Therapy Association. Guide to physical therapist practice. Alexandria, Va: American Physical Therapy Association; 2001.
9. McArdle, W.D., Latch, F.I., Katch, V.L. Essentials of exercise physiology, ed 2. Philadelphia: Lippincott Williams & Wilkins; 2000.
10. Kisner, C., Colby, L.A. Therapeutic exercise: foundations and techniques, ed 4. Philadelphia: F.A. Davis; 2002.
11. Pollock, M.L., Gaesser, G.A., Butcher, J.D., et al. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exercise. 1998:975–991.
Kisner, C., Colby, L.A. Therapeutic exercise: foundations and techniques, ed 4. Philadelphia: F.A. Davis; 2002.
Lippert, L. Clinical kinesiology for physical therapist assistants, ed 3. Philadelphia: F.A. Davis; 2000.
McGowan, C., Goff, L., Stubbs, N. Animal physiotherapy: assessment, treatment and rehabilitation of animals. Oxford: Blackwell Publishing; 2007.
Michlovitz, S.L. Thermal agents in rehabilitation, ed 3. Philadelphia: F.A. Davis; 1996.
Millis, D.L., Levine, D., Taylor, R.A. Canine rehabilitation & physical therapy. Philadelphia: Elsevier; 2004.
Norkin, C.C., Levangie, P.K. Joint structure and function: a comprehensive analysis, ed 4. Philadelphia: F.A. Davis; 2005.
Snyder-Mackler, L., Robinson, A.J. Clinical electrophysiology: electrotherapy and electrophysiologic testing. Philadelphia: Lippincott Williams & Wilkins; 1995.
Berry, W.L., Reyers, L. Nursing care of the small animal neurological patient. J S Afr Vet Assoc. 1990;61(4):188–193.
Bocobo, C., Fast, A., Kingery, W., et al. The effect of ice on intra-articular temperature in the knee of the dog. Am J Phys Med Rehab. 1991;70(4):181–185.
Jaegger, G., Marcellin-Little, D.J., Levine, D. Reliability and goniometry of Labrador Retrievers. Am J Vet Res. 2002;63:979–986.
Jerrum, R.N., Hart, R.C., Schulz, K.S. Postoperative management of the canine spinal surgery patient. Compendium. 1997;19(2):147–161.
Johnson, J.M., Johnson, A.L., Pijanowski, G.J., et al. Rehabilitation of dogs with surgically treated cranial cruciate ligament-deficient stifles by use of electrical stimulation of muscles. Am J Vet Res. 1997;58(12):1473–1477.
Millis, D.L., Levine, D. The role of exercise and physical modalities in the treatment of osteoarthritis. Vet Clin N Am. 1997;27(4):913–930.
Steiss, J.E., Adams, C.C. Effect of coat on rate of temperature increase in muscle during ultrasound treatment of dogs. Am J Vet Res. 1999;60(1):76–80.
American Physical Therapy Association, www.apta.org
American Veterinary Medical Association, www.avma.org
Physical Rehabilitation Training
Animal Rehabilitation Institute, Loxahatchee, Fla, 561-651-0760, www.animalrehabinstitute.com.
North East Seminars, University of Tennessee, 800-272-2044, www.neseminars.com.
 TECHNICIAN NOTE
TECHNICIAN NOTE